Abstract
The British Association for Psychopharmacology guidelines specify the scope and targets of treatment for bipolar disorder. The third version is based explicitly on the available evidence and presented, like previous Clinical Practice Guidelines, as recommendations to aid clinical decision making for practitioners: it may also serve as a source of information for patients and carers, and assist audit. The recommendations are presented together with a more detailed review of the corresponding evidence. A consensus meeting, involving experts in bipolar disorder and its treatment, reviewed key areas and considered the strength of evidence and clinical implications. The guidelines were drawn up after extensive feedback from these participants. The best evidence from randomized controlled trials and, where available, observational studies employing quasi-experimental designs was used to evaluate treatment options. The strength of recommendations has been described using the GRADE approach. The guidelines cover the diagnosis of bipolar disorder, clinical management, and strategies for the use of medicines: in short-term treatment of episodes, relapse prevention and stopping treatment. The use of medication is integrated with a coherent approach to psychoeducation and behaviour change.
Keywords: bipolar disorder, treatment, evidence-based guidelines, antipsychotics, antidepressants, mood stabilizers, lithium, psychoeducation, Cognitive Behaviour Therapy
Introduction
Bipolar disorder has been and still is a relatively neglected condition. This feeds a perception, which we broadly share, that treatment could and should be improved. Guidelines provide an opportunity to enhance quality of care by advocating particular treatment approaches through systematically derived statements that can help individual patients and clinicians to make decisions. They have had an important impact on patterns of prescribing for bipolar patients (Bjorklund et al., 2015).
Guideline recommendations are based on evidence. Nevertheless, the principal recommendations usually derive from average effects in patient populations. Such recommendations may be expected to apply about 70% of the time so we have used expressions like “Clinicians should consider…‥” in the text. However, there will be occasions when adhering to such a recommendation unthinkingly could do more harm than good.
We will also describe treatment options in a way that is not prescriptive. They recognise that implementation will depend on individual and local circumstances. Options will reflect up-to-date evidence and may highlight current uncertainties.
Finally, we make consensus statements, the implications of which should shape and inform decision making.
This guideline should be read alongside NICE 2014 Bipolar disorder: assessment and management (NICE2014) (https://www.nice.org.uk/guidance/cg185 ), the recommendations from which are in places compared with our own.
The quality of the evidence base
Evidence categories (I to IV) traditionally imply a hierarchy from the best evidence, based on high quality randomized trials, to the weakest, based on opinion/clinical impression (Shekelle et al., 1999). This approach explicitly downgrades non-experimental descriptive studies of treatment effects in favour of any RCT; in so doing, it confounds design with quality.
In previous editions (Goodwin, 2003; Goodwin, 2009), we ranked individual recommendations on the basis of the supporting evidence using this scheme. This can be unduly formulaic. For example, weight may be given to positive findings from small, inconclusive studies simply because they were randomized trials. Like others (Kessing, 2015), we have been impressed by new observational data linking treatment exposures with clinical outcome. In the past such data would have been rated inferior to RCTs as a matter of principle (see Table 1). However, the quality and scale of some routinely collected data sets can provide relatively unbiased and reliable evidence for the effectiveness and safety of a treatment. While non-randomized, such evidence is more convincing than any but the highest quality RCTs, and with superior external validity. In addition, the availability of network meta-analysis of RCTs has given us the opportunity to re-think how to contextualize the quality of the evidence for an individual drug in the overall treatment strategy.
Table 1. Traditional evidence categories.
Randomized Controlled Trials (RCTs) must have an appropriate control treatment arm; for primary efficacy this should include a placebo condition although for psychological treatments this may not be met. BAP: British Association for Psychopharmacology.
| Evidence categories | Treatment studies | Observational studies |
|---|---|---|
| I | Meta-analysis of RCTs, at least one large, good quality, RCT or replicated, smaller RCTs | Large representative population samples |
| II | Small, non-replicated RCTs, at least one controlled study without randomization or evidence from at least one other type of quasi-experimental study | Small, well designed but not necessarily representative samples |
| III | Non-experimental descriptive studies, such as uncontrolled, comparative, correlation and case-control studies | Non-representative surveys, case reports |
| IV | Expert committee reports or opinions and/or clinical experience of BAP expert group. | |
The need for a more flexible appraisal of the evidence has been recognized by the Cochrane Collaboration’s GRADE system (http://handbook.cochrane.org/chapter_12/12_2.htm). Even though we could not adopt the detailed methodology recommended for its full implementation, as a bottom up procedure, we followed the spirit of the GRADE approach, top down, to justify the quality standard of recommendations in our different treatment sections. We already have the major data synthesis conducted for NICE2014, so we did not replicate their efforts. The point of the GRADE system is to make the basis for choosing recommendations transparent.
Finally we have made many recommendations for standards of care. Standards are intended to apply rigidly. Many standards are driven by ethical or clinical consensus rather than formal evidence. Where standards are evidence-based, confidence and consensus must be very high, requiring that standards be adhered to most of the time. We have phrased such recommendations without qualification and marked (S), so ‘Clinicians should …… (S)’.
Throughout, a particular recommendation will imply an estimation of average benefit/risk. In fact, the estimation of potential benefits and harms is not a widely understood science. It is very encouraging that the European Medicines Agency has allowed pioneering work in recent years to apply decision theory to the approval process of new drugs (Phillips et al., 2011). This demonstrates the potential to understand benefit-risk using quantitative models (Mt-Isa et al., 2014). It is an approach that has also informed the estimate of relative harms by drugs that are used ‘recreationally’ (Nutt et al., 2010). In a better future, such models could be used by doctors or patients who want robust estimates of benefits and harms, to inform decisions in an individual case. For the time being, we have made do with opinion based on research evidence, the decisions of regulators to approve particular medicines and clinical experience.
Methodology
This document is the result of an initial meeting held on 9th February 2015. Expert participants were asked to review specific areas in which new data have become available from systematic reviews, randomized controlled trials (RCTs) or observational studies. After brief presentation, a discussion identified consensus and areas of uncertainty. A narrative literature review was assembled to illustrate the consensus points. This draft was circulated to participants. Their feedback was, as far as possible incorporated into the final version of the guidelines.
Identification of Relevant Evidence
All the consensus points and the guideline recommendations can be linked to relevant evidence through the literature review. As already explained, our methodology did not allow for a systematic review of all possible data from primary sources and the recent NICE2014 bipolar guideline provided a comprehensive collation of relevant data to about two years ago (http://www.nice.org.uk/guidance/cg185). Additional publications were identified from MEDLINE searches to December 2015.
Strengths of Evidence and Recommendations for Guidelines
Strengths of Recommendation
Grade of recommendations are shown in Table 2. This approach allows for judgement to be made that downgrades some evidence (e.g. results, even if consistent, from small clinical trials, where bias is highly likely), and upgrades other findings (e.g. from observational studies in large samples with strong quasi-experimental designs). Where evidence is sparse, it has been necessary to extrapolate from relevant evidence where it is available. Weaker levels of recommendation may cover key areas of practice. Recommendations will be starred as in Table 2.
Table 2. Grades of recommendation and their relationship with supporting levels of evidence.
| Grade of recommendation | Underlying methodology | Symbol |
|---|---|---|
| High | RCTs or double upgraded observational studies | **** |
| Moderate | Downgraded RCTs or upgraded observational studies | *** |
| Low | Double downgraded RCTs or observational studies | ** |
| Very low | Triple downgraded RCTs or downgraded observational studies or case series/reports | * |
Scope and Target of the Guidelines
The content of the guidelines is relevant for all doctors treating patients with bipolar disorder. We hope that in most cases these will be doctors who are specialists in psychiatry. However we have also written the guidelines to help inform general practitioners, patients and their families, and other health care professionals involved in the management of patients with bipolar disorder.
Clinical psychologists and other colleagues providing psychotherapy to patients with bipolar disorder are a particularly important group who need to understand and acknowledge the complementary roles for patients of medication and psychological treatment.
We have emphasized our interest in evidence. However, we could not review all the relevant literature in the detail required to give a fully comprehensive text. Even distilling the evidence and summarising points of consensus, relating mainly to medical management of bipolar disorder, does not result in a format that is particularly brief or easy to use. Accordingly, the document consists of two parts. Part 1 abstracts the key recommendations (and some of the key points of evidence) and can inform everyday practice. Part 2 indicates consensus points that emerged and briefly summarises the evidence. The structure and content are broadly but not precisely aligned between Parts 1 and 2.
Finally, in Part I, we identified a list of quality standards for audit based on our most important recommendations.
Nomenclature
In this manuscript, we will avoid, where possible, the use of generic terms for drugs based on indication and instead prefer to use descriptions of mode of action. The Neuroscience based Nomenclature (NbN) is a new system to promote the description and classification of psychotropic drugs in this way. It aims to provide an app-based update of relevant and specific scientific, regulatory and clinical information, to support rational prescribing (https://www.ecnp.eu/projects-initiatives/nomenclature.aspx ). The use of a pharmacologically driven nomenclature, which highlights pharmacological targets and modes of action, helps clinicians to make informed choices (for example by combining two different targets or adding a complementary mode of action). It is a work in progress, and the voluntary suppression of the familiar terms antipsychotic, antidepressant and anticonvulsant can only be partial. When we use the term antidepressant, for example, it should be understood that we are referring to drugs used in the treatment of unipolar depression. The problem is, of course, that not all the drugs used for unipolar depression are currently described as antidepressants and antidepressants are not active specifically in depression. Thus, antipsychotics are effective in psychosis, mania and, in some cases, depression, and anticonvulsants are effective in epilepsy but also mania and depression. NbN will give us a larger vocabulary and a better grasp of what our medicines actually do if we make the necessary effort.
Caveats
We are committed to the principle of basing recommendations on the best possible evidence and, for treatment efficacy, this will usually be evidence from randomized controlled trials (RCTs). However, there are important limitations to such evidence. We highlight these limitations here so what follows is informed by this perspective.
Drug treatment trials
Drug trials are usually conducted by companies seeking to register new compounds. Such trials are now usually of good quality: matched placebo medication, randomized and concealed allocation, blinded treatment and pre-specified analysis plans. Nevertheless, it is often stated that sponsor (allegiance) bias influences the outcome of clinical trials of new medicines (in favour of the sponsored product). One important explanation for this global conclusion is that company sponsored studies may more often be placebo controlled than independent studies, and will tend to have larger effect sizes for that reason. Indeed, for dopamine antagonists and serotonin reuptake inhibitors there were no differences in effect size between industry supported and non-industry supported trials when the designs were similar (Lundh et al., 2012). The unthinking position that companies can fix the results of their studies to inflate positive effects is wrong, and is not the main reason we should treat such studies with caution.
In fact, sponsors can only easily influence outcomes by biasing the design of the study: for example, choice of dose, comparator or unblinding (if adverse reactions are obvious). Unblinding could lead to inflation of effect sizes by biasing assessment. Measures of blinding should be included in all such studies for patients and raters, but are often omitted or not reported. This potential problem should be kept in mind when examining the coherence of network meta-analyses which include placebo as the main comparator.
The reporting of adverse reactions in clinical trials is also less systematic than it could be, and has often relied on ambiguous tick-box categories to capture usually subjective complaints. The controversy arising from how self harm or suicidality should be identified as an adverse reaction has been particularly problematic(Gibbons et al., 2015; Posner et al., 2007). This means that the balance between benefits and harms can be difficult to assess from trial data. In describing outcomes that patients may experience themselves or that may be detectable by observation we will refer to “adverse reactions”; “adverse effects” are unwanted, measured consequences of drug treatment (Aronson, 2013).
Sponsor bias is also confused with publication bias. There is no doubt that the way industry-supported data was published has been a major problem in past decades. This mainly took the form of over-stating product advantages and cherry picking for publication the most positive trials or the most positive outcome measures. Non-publication of negative results was also very common. This is now partially corrected by trial registration and disclosure of ‘negative’ studies by companies. In addition, full disclosure of all analysed data has long been required by the regulatory authorities and this information is usually accessible if not actually published.
The quality and reproducibility of individual trials is critical. As a rule, companies must convince regulators that new drugs are better than placebo. Can they recruit representative patients into the necessary trials? While the patients recruited into company trials meet diagnostic criteria for BD, the list of inclusion/exclusion criteria is often so long as to render the resulting sample highly atypical, and not representative of the most ill patients with multiple co-morbidities we actually see in practice. The exclusion of patients with co-morbid substance misuse in trials of mania and of patients with suicidality in bipolar depression has the highest impact (Hoertel et al., 2013). This is compounded by heterogeneous rates of recruitment and associated with heterogeneous results across sites in multi-centre trials. In acute studies, high placebo response rates at some sites will drown out efficacy signals at others with lower placebo responses (Yatham et al., 2015b). In addition, many acute treatment studies in psychiatry are only 6-8 weeks in duration and the artificial nature of clinical trial procedures and the difficulties of recruitment mean dropout rates are high. This severely reduces the power to detect effects, so trial methodology is probably as likely to under-estimate drug effect as to magnify it.
Substantial drop out rates are common even in quite short-term RCTs. The right to drop out of studies is actually emphasized in the information given to participants in trials! However, high attrition rates have negative consequences for the power to detect effects and obviously defeat the purpose of longer-term studies. The effect is sometimes described as a bias, and NICE2014 heavily downgrades many of the RCTs for the medication of bipolar disorder on this basis. We have not taken the same view, because it is clearly a limitation of RCTs in general, but when particularly severe, it must limit the validity and generalizability of any conclusions (Leon et al., 2006).
Finally, outcomes in acute treatment studies are often rating scale scores, which are arbitrary counts of symptoms and their severity. These are measures rarely used by clinicians because they are tedious to obtain by interview. They are intermediate measures suspended between biomarkers, which can prove a drug has had the predicted pharmacological effect, and real outcomes relevant to patients (for example return to work). Real outcomes are too distal to provide sensitivity in a short clinical trial.
For all these reasons, caution is required in extrapolating the results of such trials to practice, whether or not presented as a meta-analysis.
Independent trials have often been less well-resourced and small scale, but may lack the stigma attaching to industry sponsorship. The results of such trials have the potential to be very misleading due to the whole range of potential biases. However, where quality is maintained and sample size is reasonable, they can offer important independent support to prove efficacy. They may also recruit patients in a less distorted way than commercial clinical research organizations and so generalize more convincingly. Positive studies of this kind have been particularly important in shaping some of our recommendations (e.g. the use of lithium and lamotrigine).
One final consideration is that when small trials are negative, caution is required in claiming that the trial proves lack of efficacy: underpowered studies by definition run a high risk of type II statistical error.
In conclusion, RCTs provide an important evidence base for all medical practice. Effect sizes in psychiatry, in common with the rest of medicine, are moderate (Leucht et al., 2012) but deliver worthwhile patient benefit. Nihilism about the results of RCTs should be avoided. However, RCTs are essentially experiments; their results are most plausible when confirmed by large scale, independent, pragmatic RCTs conducted in real world patient samples. There are few examples of such trials in psychiatry. More relevant currently are pharmaco-epidemiological studies using quasi-experimental designs. In such studies patients can act as their own controls before, during and after treatment, patient numbers can be very large and observation periods can be long. Furthermore, the measured outcomes can be objective and highly clinically relevant: admission to hospital, suicide, acts of violence etc. Such studies are crucial in supporting our recommendations for the long-term use of drugs in bipolar disorder.
Psychotherapy trials
Psychotherapy trials pose difficulties for evidence-based practice that have not been sufficiently recognized. The choice of a fair comparison treatment is much more challenging than for medicines. It is often simply ducked by using a poorly specified ‘treatment as usual’ (TAU) condition. While this may be defensible in a pragmatic study of effectiveness, it creates problems of interpretation for a proof of concept or efficacy study. If, as is commonly the case, the active treatment is superior to TAU, no specificity can be claimed for its content. The alternative ‘waiting list’ control group is also problematic because any superiority for an active treatment may be due to (or amplified by) a waiting list’s expected nocebo effect. Hence, many positive trials of particular therapies are pseudo-specific, in the sense that we do not know what elements of the psychotherapy are actually effective.
The collection of ‘adverse reactions’ to psychological treatment also appears to be unsystematic and hence under-appreciated (Nutt and Sharpe, 2008).
These inherent problems require an approach to refining best practice based on meticulous trial design and execution and sequential refinement of the psychotherapy content. Biomarkers or more experimental designs could also inform treatment development in psychotherapy trials (Button and Munafo, 2015). Unfortunately, development funding is often not available in the way that is taken for granted for the development of new drugs by industry.
As a corollary of limited funding, psychotherapy trials are often small scale and suffer from all the disadvantages of similar, independent trials of medicines. Moreover, psychotherapy trials may be particularly subject to allegiance bias. This will mean that investigators are heavily invested professionally in showing that ‘their’ treatment works. This may consciously or unconsciously influence how trials are designed, treatments delivered and results described. It can also influence how results are analysed, if statistical methods are not pre-specified. Publication in a high profile journal or endorsement in a guideline will increase the demand for workshops and training that may remunerate a provider personally, and will be used to demonstrate impact by their employing institution. Thus, declaration of interest should be taken seriously in the publication of psychosocial interventions (Dragioti et al., 2015). Given a strong appetite from patients for psychological solutions, there is a prevailing pressure to reach positive but premature judgements.
Publication bias is objectively as important a problem for psychotherapy trials as for drug trials (Flint et al., 2015). However, there is not the safeguard that is provided by the formal disclosure of negative studies in the regulation of drug treatments.
Meta-analysis cannot resolve uncertainty where the methodology of the individual RCTs is flawed. In the case of bipolar disorder, the paucity of research in psychological and psychosocial treatments is as regrettable as for the other domains of treatment. Future studies that can avoid the mistakes of the past and present can therefore be enthusiastically anticipated. For now, we have favoured caution in interpreting the findings from trials of psychosocial interventions. Just as for drug treatments, more large-scale data with harder outcomes (admission to hospital, offending) would be very welcome, but is not currently available.
Relapse prevention trial designs
These studies are required by The European Medicines Agency (EMA) as proof of continuing efficacy for drugs shown to be effective in short-term studies of acute illness. They offer a further proof of acute efficacy since they take patients who have recovered while taking a particular active treatment and randomize to continue that treatment or be switched to placebo. If patients on placebo relapse to the same pole as the index episode, this is taken as further evidence that the drug worked acutely.
If these studies are extended over one or even two years, there must be a point at which we can infer further that the drug-placebo difference represents prevention of new episodes. Since there is no clear discontinuity in the boundary between preventing relapse of the original episode and the prevention of new episodes, perhaps they are essentially different sides of the same coin? Relapse prevention studies have been interpreted in that way in previous BAP guidelines. However, it is recognized that much of the difference between active treatment arms and placebo are due to early events, and dropout rates tend to be very high. Retention of patients in a 1-2 year study may be as low as 10%. Hence, interpretation of such studies, except in relation to acute efficacy may be questionable.
It may also be objected that such studies are ‘enriched’ with patients who have preferentially responded to the drug under investigation. Clearly this is true, but in actual practice this may often reflect the clinical question a psychiatrist asks: what will happen if I discontinue the drug? Knowing that there will be a risk of relapse is useful and informs clinical practice. This is really the only experimental evidence that supports the belief that what gets patients well will often keep them well. Relapse prevention studies underline that lesson, and offer us more safety data than are available in acute studies.
Finally, the definition of relapse in relapse prevention studies requires care. Acute withdrawal of a drug may lead to subjective changes and effects on sleep, which are often the mirror image of adverse reactions to taking the drug (for example vivid dreams after withdrawal of drugs that suppress REM sleep). Withdrawal reactions of this kind by definition immediately follow drug discontinuation and are relatively transient. However, in theory, withdrawal effects could be mistaken for relapse; if so, this must result in an excess of cases of very early relapse which are artefactual. Studies in which such an effect is observed are very difficult to interpret. More subtly, such effects could lead to unblinding and bias the assessment of patients later in the course of follow up.
On the other hand, drug withdrawal effects may also trigger an excess of true cases of early relapse compared with untreated patients. At present such an effect has only been convincingly shown with lithium, where it is a clinically important phenomenon (Suppes et al., 1991; Goodwin, 1994)). In theory, such effects might be more likely with those treatments that most modify the risk of relapse and act most proximal to the brain mechanisms involved in, for example, the onset of mania.
NICE2014 effectively discounted much of the longer term data generated by relapse-prevention studies. In contrast, we accept them for what they are while recognizing their limitations. Further where randomized data and high quality naturalistic data support the same the conclusions, then those findings are likely to be of particular validity and should clearly influence treatment recommendations.
Choice of treatment and network meta-analysis
We are impressed by the power of network meta-analysis for understanding treatment efficacy and we will refer to such analyses in supporting the use of medicines to treat different aspects of bipolar disorder. The principle is to use all the available data that meets quality standards and include all trials where medicines are compared directly or indirectly via a common comparator (often placebo) (Cipriani et al., 2013b). This can identify when a data set is internally consistent (A beats B, B beats C, so A should also beat C). Where there is consistency between comparisons with placebo on one hand, and active comparators on the other, it is less likely that effects have been biased by unblinding. In our view, this is probably the most important current test that RCTs are indeed reliable and provide a secure evidence base for clinical decision making. In GRADE terminology, a coherent network supports strong ranking for treatment recommendations based on RCTs; a sparse or unstable network does not.
Network meta-analysis can also provide a kind of league table to rank different medicines against each other (and against placebo). Such findings have strongly influenced the NICE recommendations for the treatment of mania and depression. However, confidence intervals around the rankings were wide. As we argue in the preceding paragraph, practice can be underpinned by the knowledge that the efficacy of the treatment choices has been established in RCTs with a coherent network. It does not follow that practice be dominated by evidence that one effective treatment is, on average, slightly better than another. In addition, extrapolating from average effects in RCTs and meta-analyses to what might work amongst a range of effective treatments in a given individual requires experience and judgement. Previous history of response, willingness to adhere to a treatment, potential benefits and risks given an individual’s personal situation all have a bearing on therapeutic outcome.
The key to success with individual patients is cautious but confident prescribing of adequate doses and monitoring of effects, both positive and negative. Moreover, drug choice is an important clinical freedom in developing treatment with the individual patient in relation to both efficacy and adverse reactions. While NICE2014 is at pains to emphasize the need to respect patient choice, as are we, they are less liberal in what choices they actually sanction.
Part 1. Guidelines
In making recommendations that will be of practical value to clinicians who treat patients with bipolar disorder, we stand on the consensus view of the evidence reviewed in the accompanying document. The clinical practice guideline developed by NICE2014, has also been considered. We have sometimes reached different conclusions. These differences result from different weights placed on the available evidence. Differences of opinion, of course, are most likely to occur when the evidence is less than compelling.
Along with grading of specific recommendations for a strategy or individual treatment, the guideline includes statements, the implications of which should also influence practice. The strength of the evidence is rated as in Table 1 (and may relate to RCTs or observational findings).
Currently, medication remains the key to successful practice for most patients in the long term. The objective is to achieve a personalized choice of medicine (effective and well tolerated), informed adherence and an understanding of illness course shared with the patient and all most involved in their care. This needs to be established as early as possible in patients who present with severe illness.
Fundamentals of Patient Management
1. Diagnosis
Clinicians should make accurate diagnoses of hypomania, mania and depression (Standard of Care, (S)). Individual episodes may display mixed features of the opposite pole (Category I evidence, (I)).
Consider the identification of the core symptoms of mania or depression against a check list as in DSM-5 to improve confidence in, and the reliability of diagnosis (S). There is a new requirement in DSM-5 for an observable increase in energy and activity in addition to subjective mood elevation for hypomania and mania. Practice may also be made more comprehensive with a patient-completed screening instrument (Category IV evidence, (IV)).
Failure to use some form of structured record increases the likelihood that bipolar disorder will be missed and/or confused with another diagnosis (Category II evidence, (II)).
The term hypomania should be used as defined in DSM-5, where it is confined to elated states WITHOUT significant functional impairment (S).
Be careful not to dismiss or minimize mood elevation when it is the cause of disturbed behavior; personality problems or situational disturbance should be invoked only if mania (or hypomania) is absent (IV).
Bipolar patients may present with depression, especially in adolescence (I). Ask about a history of distinct periods of elated, excited or irritable mood of any duration and a family history of mania in all patients with depression (S).
Anxiety disorders are highly co-morbid with bipolar disorder (I) from a lifetime perspective. Anxiety symptoms are often persistent between episodes and may contribute to mood instability (I).
Anxiety disorders are associated with increased illness burden and poor outcome (I): they require assessment and treatment (S).
Stimulant drugs may mimic manic symptoms (II). A drug-induced state, including psychosis, should wane with the clearance of the offending drug (II): use 5 half-lives as the relevant interval (and the longest half-life stated in a range). Levodopa and corticosteroids are the most common prescribed medications associated with secondary mania (I).
More commonly, alcohol and/or drug use is co-morbid with manic or depressive mood change (I). The mood state will then significantly outlast the drugged state and a diagnosis of bipolar disorder can be made (S).
Borderline personality disorder is an important diagnosis that may either be confused with or be co-morbid with bipolar disorder. Reliable diagnosis of either condition can only be achieved by using operational criteria properly (S).
Organic conditions, such as thyroid disease, multiple sclerosis or any lesion(s) involving right-sided sub-cortical or cortical areas may be associated with secondary mania (II) and should be considered in the differential diagnosis (S). These conditions are most likely to occur in the elderly (I).
The diagnosis of bipolar disorder in childhood has been controversial. The narrow definition of the condition, now endorsed in DSM-5 and described in the latest NICE guideline (NICE2014), recognizes unequivocal euphoria and an episodic course as the defining characteristics in pre-pubertal children (S). One should not make the diagnosis in children or young people unless there has been a period of prospective longitudinal monitoring by appropriately experienced clinicians taking into account the child or young person’s educational and social functioning (S).
Within many child and adolescent services, bipolar disorder may well be missed and the challenge is to enhance its recognition. The approach to diagnosis in children is poorly operationalized: diagnostic instruments are available that could aid clinical practice (II).
The so-called broad bipolar phenotype of childhood has been replaced by a new diagnosis in DSM-5: disruptive mood dysregulation disorder (DMDD). This is not a bipolar diagnosis and is likely to be rather common in comparison with bipolar disorder, which is rare in prepubescent children (I).
Following puberty, the familiar adult criteria can be used with increasing confidence (IV).
Bipolar symptoms such as irritability or aggression may appear, with the benefit of hindsight, to be misdiagnosed by clinicians when a patient is first seen (I). In fact, diagnosis can only be reliable after a clear-cut episode of (hypo)mania (S).
2. Access to services and the safety of the patient and others
Specialized services for bipolar patients of all ages have not been a priority for the NHS, and so provision is variable and too often poor (IV).
Early intervention is a highly desirable objective in the management of young people with bipolar disorder (S). There are numerous systemic barriers to its provision and development in UK services (IV). This is an urgent problem.
When mania is diagnosed, always consider admission to hospital or intensive community management (S). The particular risks to the patient and others will be the result of poor judgment and associated actions in areas of work, personal relationships, alcohol/drug use, spending, driving and sexual activity (I).
Always try to obtain third party information if in any doubt when making a risk assessment (S).
When any patient is in a mixed state or depressed, ask about suicidal ideation, intention to act on these ideas and extent of plans, means or preparation for suicide (S). Social isolation, substance use, psychosis (especially with command hallucinations), personality disorder, family history of suicide, recent exposure to suicide and any prior suicide attempts may all increase the risk (I).
The increased incidence of completed suicide soon after an assessment in bipolar patients (I), suggests that current practice may under-estimate suicide risk (IV).
Bipolar patients may be vulnerable to exploitation or violence when in an abnormal mental state, which may make admission more desirable (IV). The risk of violence and offending more generally (by the patient) is also increased in bipolar disorder (I) and assessment should address this risk (S).
Carefully document your decisions in formulating a care plan (S).
The fractionation of clinical services, for example between in and out patients, ‘assessment’ and ‘treatment’ runs counter to the needs of bipolar patients in all stages of their treatment but particularly in managing follow up (IV). Premature discharge to primary care can further dilute the treatment package available in the early stages of managing the illness (IV).
3. Enhanced care
a). Establish and maintain a therapeutic alliance
A doctor should take responsibility for diagnosis, physical examination, investigations and explanation of the medical plan of management (S). Communicate clearly and honestly what you think (S). Take the time to listen to what is bothering the patient (S).
Very disorganized psychotic patients with bipolar disorder will have social needs that merit assertive management (IV).
b). Educate the patient and his or her family about the disorder
Doctors, patients and carers tend to bring different experiences and beliefs to the therapeutic relationship (II) and make different estimates of future risks. Make use of evidence to address poor insight, the seriousness of the illness, reluctance to give up the experience of hypomania or mania, the risk of relapse and the benefit of therapeutic engagement (II).
c). Enhance treatment adherence
Treatment adherence is often poor, particularly in younger patients early in the illness course (I).
While respecting patient preferences, education about the illness after an acute episode should include information on the potential benefits and risks of medication and emphasize the need to continue on it long-term (S).
The known tolerability and safety of available medicines should guide prescribing: inform patients about possible adverse reactions and monitor their possible emergence (S). Make the reduction of adverse reactions a priority - by using different scheduling (e.g. by prescribing all sedative medicines at bed time), alternative formulations or lower dosages (Category III evidence, (III)). Patience may be required to establish that lower doses are effective (IV).
d). Promote awareness of stressors, sleep disturbance, early signs of relapse, and regular patterns of activity
Sleep disruption is often the final common pathway triggering manic episodes and is also associated with depression: stressors that lead to reduced sleep may contribute to relapse (II).
Regular patterns of daily activities should be promoted (II). Identify and try to modify habitual, very irregular patterns of activity, which are common in patients with bipolar disorder: consider using diaries or apps to self-monitor mood or activities (III).
Since alcohol and drug use are associated with a poor outcome, they require assessment, appropriate advice and treatment (S).
Help the patient, family members, and significant others recognize emerging symptoms of manic or depressive episodes so that they may know when to request early intervention (S).
A consistent long-term flexible alliance between the patient, the patient’s family and key members of a psychiatric team, including an effective, appropriately trained psychiatrist, is the ideal arrangement for outpatient care. The input of family members may also enhance the patient’s treatment adherence (S).
e). Evaluate and manage functional impairments
Full functional recovery seldom occurs within twelve weeks following the remission of mood symptoms (I). Advise the patient in scheduling respite from work or other responsibilities when necessary (S). Discourage major life decisions being made while in a depressive or manic state (S).
Patients may experience considerable difficulty performing at the level for which their education has prepared them (I). Manage patient expectations of their capacity to work (S).
Consider the needs of carers and children of patients with bipolar disorder: provide information about local or national support groups (S).
f). Consider physical health in clinical assessment and treatment planning
Bipolar patients have premature mortality, owing partly to cardiovascular disease (I). In large part this is driven by weight gain. Weight and other relevant risk factors should be monitored at least annually and treatment offered appropriately (S).
Consult BAP guideline on management of weight gain and metabolic disturbances associated with psychosis and antipsychotic drug treatment (S).
g). Consider the use of alcohol and drugs (including caffeine)
The use of alcohol or drugs may be excessive. Quantify their consumption and discuss setting targets for reducing harm (S). Caffeine (in coffee and other drinks) may significantly disturb sleep and exacerbate anxiety symptoms in sensitive individuals (III).
h). Consider risks for various adverse outcomes, including self harm, suicide, victimization, violence and criminality
Bipolar patients are at substantially increased risks of self harm, suicide, victimization, violence and criminality (I).
Risk factors whose modification could reduce the risks of suicide and criminal outcomes include comorbid drug and alcohol use disorders and illness severity (II).
i). Increase the focus of care planning in women of child-bearing potential
The postpartum period is one of very high risk for relapse in women with bipolar disorder (I). Psychosis or mania is a particular risk for bipolar I disorder: it is increased further by a previous post-partum episode. Depression is a substantial risk for both bipolar I and II disorder. Women need to decide about using medication in pregnancy and during breastfeeding (or whether to breast feed), bearing in mind the very high risk of severe illness at this time (S). See section on special situations below.
Treatment of Different Phases of Bipolar Illness
Prescribers should be aware of the limitations imposed by licences for different medicines and potential safety concerns documented in product descriptions (S). Marketing authorizations are primarily designed to limit the actions of companies, NOT clinicians. Accordingly, ‘Off label’ prescribing of licensed medicines is implied by some of the recommendations incorporated below. However, seek expert advice if unsure about the efficacy or safety of any individual medicine or its use in combination (S).
Residual symptoms predict eventual relapse (II), so the objective of short term treatment is remission of symptoms (S).
We have not specified doses in this section. See Annex for additional information about individual medicines and relevant Product Information Sheets.
1. Acute Manic Episodes
Choice of an initial treatment
Most patients with mania will require short-term treatment with medicine(s) in an appropriate clinical setting (I). The evidence from network meta-analysis of many RCTs is coherent and supports efficacy of a range of different medicines (I). Thus, comparisons in RCTs include many indirect (placebo) and direct comparisons; this reduces the risk that unblinding and other bias has significantly distorted the results in individual studies. Choice of medicine should respect the balance between the benefit of efficacy and the harm of short-term adverse reactions or adverse effects in an individual with mania.
No psychotherapy currently provides an alternative strategy for management.
a). For patients not already taking long-term treatment for bipolar disorder
For severe manic episodes, consider oral administration of a dopamine antagonist when seeking rapid anti-manic effect (****). Systematic comparison of data from clinical trials suggests that haloperidol, olanzapine, risperidone and quetiapine are particularly effective in short-term reduction of symptoms. Valproate is an alternative treatment with less risk of adverse motor reactions but should not be used for women of child bearing potential because of its unacceptable risk to the foetus of teratogenesis and impaired intellectual development. Aripiprazole, other dopamine antagonists and partial agonists, carbamazepine and lithium are also options.
Where an agitated patient requires parenteral treatment to control behaviour without their full consent, the use of dopamine antagonists/partial agonists and GABA modulators (benzodiazepines) should follow established protocols (S). The lowest doses necessary should be used (S). Do not escalate the dose of dopamine antagonists simply to obtain a sedative effect (S).
For less ill, non-psychotic manic patients or for hypomania, treatment can be extrapolated from practice in mania (IV).
To promote sleep for agitated overactive patients in the short term, consider adjunctive treatment with GABA modulating drugs (***).
When possible, treatment selection should be guided by a patient’s previous experiences and preferences especially if expressed in the form of an advance directive under the Mental Capacity Act 2005 (S) or an advance statement.
Antidepressant drugs (i.e. drugs approved for the treatment of unipolar depression) should usually be tapered and discontinued in a manic episode (**).
If successful treatment has been initiated for mania, long-term treatment should be considered (see below) (S).
b). For patients who suffer a manic episode while taking long-term treatment
If the current presentation is due to inadequate symptom control, ensure that the highest well-tolerated dose of the current treatment is offered (S). For a dopamine antagonist or partial agonist, or valproate raising the dose may be sufficient to control manic symptoms (IV).
For lithium, check whether serum concentrations are within the usual target range; consider aiming for a higher serum concentration within the target range (0.6 - 0.8 mmol/l (or mEq/l)); concentrations of 0.8-1.0 mmol/l may be more effective but carry a greater risk of harm if continued long term (I).
If the patient is taking lithium, consider adding a dopamine antagonist or partial agonist, or valproate, as in a) above (****). In general, follow the same principles as for a first episode or an episode occurring off short-term treatment.
If the current episode is due to poor adherence, establish the cause and offer appropriate intervention (S). For example, if non-adherence is associated with an adverse reaction, consider dose reduction, assuming the adverse effect is dose related, or a switch to a more tolerable alternative regimen. If poor adherence is deliberate, and not related to tolerability, use of lithium long term may not be indicated due to the risk of ‘withdrawal’ mania and depression (I).
c). If symptoms are inadequately controlled with optimized doses of the first-line medicine and/or mania is very severe, add another medicine
Consider the combination of lithium or valproate with a dopamine antagonist/partial agonist (****).
Consider clozapine in more refractory illness (**).
Electroconvulsive therapy (ECT) may be considered for patients whose mania is particularly severe or treatment-resistant, those who express a preference for ECT and patients with severe mania during pregnancy (***).
d). The presence of mixed features in a manic or hypomanic episode
DSM-5 encourages the identification of mixed features rather than a ‘mixed episode’ (as in DSM-IV). The implications for treatment are uncertain. Existing data from secondary analysis of trials for mixed episodes, suggest that treatment as for mania is appropriate (I).
e). Assess contribution of substance use to a manic or hypomanic episode and consider if medically assisted withdrawal is required (S)
f). Discontinuation of short-term treatments
Drug discontinuation should be planned in relation to the need for long-term maintenance treatment (S). Many medicines shown to be effective for the treatment of mania have also been shown to be effective in relapse prevention (I).
Medicines only used for the acute treatment of mania, may be reduced in dose and discontinued (tapering over four weeks or more) after full remission of symptoms has been achieved (IV). Remission will often occur within three months (I) but mood stability may require six months or more to achieve.
Any medication used adjunctively for symptomatic effect to promote sleep or sedation should be discontinued as soon as symptoms improve (S).
2. Acute Depressive episode
The evidence from network meta-analysis of available RCTs supports the efficacy of a limited range of individual medicines with different pharmacology and different weights of evidence. In particular, there is uncertainty (and difference of opinion) over the option of choosing antidepressants (i.e. drugs shown to be effective in major depressive episodes with a unipolar course) (IV).
Most of the evidence concerns patients with a bipolar I illness course; however, extrapolation to bipolar II disorder appears logical (IV).
a). For patients not already taking long-term treatment for bipolar disorder
Consider quetiapine, lurasidone or olanzapine (***). Dopamine antagonists have the inherent advantage of being anti-manic treatments (I).
Antidepressants (meaning drugs for a major depressive episode in a unipolar illness course) have not been adequately studied in bipolar disorder. Only the combination of fluoxetine with olanzapine has support as a specific treatment (***). The common use of other antidepressants in patients with bipolar disorder is an extrapolation from effects established in a unipolar illness course. When considered, they should be co-prescribed with a drug for mania (e.g. dopamine antagonists, lithium, valproate) in patients with a history of mania (S).
Consider initial treatment with lamotrigine, with the necessary incremental dosing schedule, usually as an addition to agents preventing recurrence of mania (****).
Consider ECT for patients with high suicidal risk, treatment resistance, psychosis, severe depression during pregnancy or life-threatening inanition (***). Consider simplifying pre-existing polypharmacy, which may have raised the seizure threshold. It is very unusual for ECT to be used under mental health legislation without a patient’s consent; fears that this may occur should be allayed
When depressive symptoms are less severe, and despite limited evidence, lithium may be considered, especially as a prelude to long-term treatment (**).
Consider family-focused, cognitive behavior therapy or interpersonal rhythm therapy as an additional treatment, when available, since these may shorten the acute episode (**).
b). For patients who suffer a depressive episode while taking long-term treatment
Ensure that the current choice of long-term treatments is likely to protect the patient from manic relapse (e.g. lithium, valproate, dopamine receptor antagonist/partial agonist drugs), by checking adequate doses of medicines and/or serum concentrations of lithium within the usual target range (S). Address current stressors, if any (S).
If the patient fails to respond to optimization of long-term treatment, and especially if depressive symptoms are significant, initiate treatment as above. See also section on treatment-resistant depression below.
c). Choice of drug for a depressive episode
Treatment preference cannot be securely based on the current database of RCTs (IV). The available network meta-analyses may not be stable because rankings are strongly influenced by inclusion criteria and indirect comparisons sometimes contradict the findings from direct comparisons.
There is a risk of a switch to mania or mood instability during treatment for depression (I). While this will often reflect the natural history of the disorder, it may be increased by monotherapy with antidepressants. The dual action monoamine re-uptake inhibitors (venlafaxine, duloxetine, amitriptyline and imipramine)(II)) carry a greater risk of precipitating a switch to mania than single action drugs (especially selective serotonin reuptake inhibitors) (II).
Antidepressant drugs appear unlikely to induce mania when used in combination with a drug for mania (I).
In bipolar II disorder, if an antidepressant is prescribed as monotherapy, any increase in dose should be gradual and there should be vigilance for and early management of any adverse reactions such as hypomania, mixed states or agitation (IV).
In contrast to the common use of antidepressants, audit data suggest that lamotrigine is too little used outside specialist centres, given its efficacy in bipolar I, and suitability for bipolar II disorder.
If successful treatment has been initiated for depression de novo in a bipolar illness course, long-term treatment should be considered (see below) (S).
d). Tapered discontinuation of antidepressant drugs may be considered after full remission of symptoms (IV)
Depressive episodes that remit in bipolar disorder tend to be shorter than in unipolar disorder (I); in the absence of strong data for maintenance efficacy, consider discontinuation of antidepressants after as little as twelve weeks in remission (*).
Longer treatment with antidepressants is justified if patients relapse on their withdrawal (IV).
e). Treatment of resistant depression
Relative or even marked treatment resistance may occur in depressed bipolar patients (I). This would mean failure to respond not just to an antidepressant but also quetiapine, olanzapine, lurasidone and lamotrigine singly and in combination. There is very little information from trials on the treatment of such refractory bipolar patients. ECT is an option (***). Augmentation strategies may be translated from experience in unipolar patients (*; see BAP guideline on the use of antidepressants: Management when initial treatment fails), but not before evidence-based bipolar options have been exhausted. Adequate anti-manic cover with lithium, valproate or a dopamine antagonist/partial agonist will be necessary (S).
Choice of initial treatment: psychosocial treatments
There is very little evidence of efficacy of psychological treatments alone (without pharmacotherapy) in the treatment of acute bipolar depression.
Recommendations for psychotherapy alone (as in NICE2014, for example) are surprising and based on very low quality data (*). More evidence is needed that this is really an effective approach (IV).
3. Long-term treatment
a). Prevention of new episodes
Consider long-term treatment following a single severe manic episode (i.e. diagnosis of bipolar I disorder) (***).
However, without active acceptance of the need for long-term treatment, adherence may be poor (I). Consider a wider package of treatment offering enhanced psychoeducation, motivational and family support especially in the early stages of illness to promote behaviour change and adherence to medication (***).
When a patient has accepted treatment for several years and remains well, they should be advised to continue indefinitely, because the risks of relapse remain high (***).
Consider extrapolating the advice for bipolar I to bipolar II disorder, given increasing evidence for common efficacy from clinical trials (**).
b). Options for long-term treatment
At present the preferred strategy is for continuous rather than intermittent treatment with oral medicines to prevent new mood episodes. The network meta-analysis of available RCTs with relapse prevention designs support the efficacy of a limited range of individual medicines with different pharmacology and different weights of evidence: lithium, olanzapine, quetiapine, risperidone LAI (long acting injection) and valproate (albeit marginally) prevented manic relapse. Only lamotrigine, lithium and quetiapine were convincingly shown to prevent depressive relapse. Lurasidone also prevents relapse to depression.
Relatively few patients remain in such trials for as long as 6 months, but lithium is exceptional in having strong evidence for relapse prevention from RCTs in which patients were not enriched for an acute response to lithium (I).
Most of the evidence concerns patients with a bipolar I illness course; however, extrapolation to bipolar II disorder appears logical (IV).
Short-term add ons (e.g. GABA modulators or dopamine antagonists/partial agonists) are necessary when an acute stressor is imminent or present, early symptoms of relapse (especially insomnia) are present or anxiety becomes prominent (IV). Consider supplying these medicines prospectively to patients with instructions how to use at their discretion (*). Higher doses of long-term treatments may also be effective, instead of add-ons (*).
Since the optimum long-term treatment strategy is not established, clinicians and patients are encouraged to participate in clinical trials designed to answer key therapeutic questions (S).
c). Choice of long-term medicines
In addition to the relapse prevention RCTs, naturalistic data, allowing comparison of rates of hospital admission on and off treatment over four years, are strongly supportive of efficacy for lithium> valproate>olanzapine>lamotrigine>quetiapine>carbamazepine (I).
Consider lithium as initial monotherapy (****).
Lithium monotherapy is effective against both manic, depressive and mixed relapse (I), has better evidence for prevention of new episodes than other agents (I) and a more substantial evidence base documenting the risks of prolonged exposure (I). Lithium is associated with a reduced risk of suicide in patients with bipolar disorder in RCTs and in both self harm and suicide in observational studies (I).
Biochemical monitoring of lithium treatment, including plasma lithium concentrations, is a standard of care (S); the target range is 0.6-0.8 mmol/l. Lithium concentrations above 0.8 mmol/l are associated with an increased risk of renal impairment especially in women (I).
Clinicians should know that NICE2014 recommended monitoring lithium concentrations at 3 monthly intervals for the first year of treatment in otherwise healthy patients, and 6 monthly thereafter (S).
Consider other options if lithium is ineffective, poorly tolerated or if patients are unlikely to be adherent: valproate, dopamine antagonists/partial agonists (S).
Valproate is often accorded an equivalent place to lithium as a ‘mood stabilizer’. It has a weaker evidence base from RCTs, but upgraded naturalistic data supports its position ahead of other options (I). Safety concerns in women have already been noted.
Additional evidence for efficacy of specific treatments comes, as already indicated, from trials in which patients have responded favourably to a particular medication in an acute indication. Accordingly, in an individual patient, if a medicine leads to prompt remission from the most recent manic or depressive episode, this may be considered evidence in favour of its long-term use as monotherapy (IV). Because effective in the short term, this may lead to preferential use of dopamine antagonists; active consideration of lithium as a better alternative should be promoted (IV).
Carbamazepine is less effective in maintenance treatment than lithium but may sometimes be used as monotherapy if lithium is ineffective and especially in patients who do not show the classical pattern of episodic euphoric mania (II). It appears to be almost exclusively effective against manic relapse (I). Be aware of the pharmacokinetic interactions that are a particular problem with carbamazepine. Oxcarbazepine may be considered by extrapolation because of its lower potential for such interactions (I).
Consider long acting (“depot”) formulations if prophylaxis against recurrence of mania is required and adherence to oral medication is erratic or injection preferred (**). Various long-acting injectable (LAI) dopamine antagonist/partial agonists are available, including fluphenazine decanoate, haloperidol decanoate, olanzapine pamoate, risperidone microspheres, paliperidone palmitate, and aripiprazole monohydrate. Only risperidone has RCT support (II). Use of other options will represent extrapolation from oral efficacy or class effect of dopamine antagonists/partial agonists and clinical experience (IV).
Lamotrigine and quetiapine may be considered as monotherapy in bipolar II disorder (***). In bipolar I disorder, lamotrigine will usually require combination with an antimanic long-term agent (IV).
d). If the patient fails to respond to monotherapy and continues to experience sub-threshold depressive symptoms or relapses, consider long term combination treatment (GRADE: variable for different combinations)
When the burden of disease is mania, it may be logical to combine two predominantly anti-manic agents (e.g. lithium, valproate, a dopamine antagonist or a dopamine partial agonist) (IV). When the burden is depressive, a combination of lithium, lamotrigine, quetiapine, lurasidone or olanzapine may be more appropriate (IV).
The role of antidepressants in long-term treatment is not established by controlled trials; nevertheless they appear to be used effectively in a minority of patients in the long term (**).
Consider continuation of clozapine if effective in refractory mania (**).
Maintenance ECT may be considered for patients who respond to ECT during an acute episode but respond poorly to all oral agents (*).
Consider adjunctive psychotherapy to address subthreshold symptoms (**; see (h)).
e). If rapid cycling poses particular long-term management problems
Identify and treat conditions such as hypothyroidism or substance use that may contribute to cycling (**).
Consider tapering and discontinuing antidepressants that may contribute to cycling (*).
There are no specific treatments for rapid cycling. As an often disabling expression of bipolar disorder, many patients require combinations of medicines. Evaluate anti-cycling effects over periods of 6 months or more by tracking mood states longitudinally. Discontinue ineffective treatments to avoid unnecessary polypharmacy (*).
f). Discontinuation of long-term treatment
Following discontinuation of medicines, the risk of relapse remains, even after years of sustained remission (II). Accordingly, if discontinuation is considered, it should be accompanied by an informed assessment of the potential dangers (S).
Discontinuation of any medicine should normally be tapered over at least 4 weeks and preferably longer (S). Early relapse to mania is an early risk of abrupt lithium discontinuation (I).
Discontinuation of medicines should not lead to withdrawal of services to patients; short-term care and monitoring will still be required if medication is discontinued together with a management plan to recognise and treat early warning signs of future relapse to mania or depression (S).
h). Specific psychosocial interventions
Psychosocial interventions may enhance care, reduce subthreshold symptoms and reduce risk of relapse (II). Psychoeducation is a component of good clinical practice, because clinical communication cannot be effective without it (S); it is formally supported by manualized approaches tested formally in clinical trials (****).
A number of differently named therapies (Family focused therapy, Cognitive behavior therapy, Interpersonal Social Rhythm therapy) have also been studied in relapse prevention. It is striking that they share many elements with each other and with psychoeducation. Psychological interventions appear to be more successful with patients early in their illness course (I).
The functional impairments of bipolar patients may merit cognitive and functional remediation strategies (II).
User groups can provide useful support and information about bipolar disorder and its treatment (IV).
4. Treatment of alcohol use disorder
See BAP’s Evidence based guidelines for the pharmacological management of substance abuse, harmful use, addiction and co-morbidity. In heavy drinkers, modest reductions in consumption may result in substantial health gains (I).
Offer naltrexone or nalmefene as part of a behavioural programme to help patients reduce their alcohol consumption (**).
Offer acamprosate if naltrexone has not been effective to help patients remain abstinent (*).
Consider disulfiram if patient wants abstinence and if acamprosate and naltrexone have failed. The patient must be able to understand the risks of taking disulfiram and have their mood monitored (*).
5. Treatment of co-morbid borderline personality disorder
In co-morbid patients both disorders may require treatment. Hence, avoid a polarizing choice between medication (usually required for bipolar disorder) and psychological treatment (the preferred approach to borderline problems) (S).
In the absence of relevant evidence, there is no reason to withdraw or withhold appropriate treatment for bipolar disorder or borderline personality disorder. Although the place of pharmacotherapy for borderline symptoms is based on limited evidence, the shared symptom of mood instability may be appropriately treated by medicines (e.g. lamotrigine, lithium, olanzapine, risperidone, aripiprazole and quetiapine) and borderline symptoms improved (*).
6. Treatment of anxiety and other co-morbid disorders
Consider treatment along the lines suggested by BAP guidelines for the treatment of anxiety disorders, attention deficit hyperactivity disorder and substance use disorders (*). Care in the use of antidepressants is required (S).
7. Treatment in special situations
In children and young people
For mania
Consider aripiprazole as first line because it is licensed in adolescents (over 13 years) with bipolar I disorder (***). Otherwise refer to adult recommendations; there is some primary evidence that olanzapine, quetiapine, and risperidone are efficacious in adolescents (**).
Refer to the British National Formulary (BNF) for Children to modify drug doses (S). Be aware of the increased potential for a range of adverse reactions, particularly weight gain (S).
For bipolar depression
Consider medicines and psychological treatments largely by extrapolation from data in adults (*).
Drugs for depression may induce switch to mania more frequently in children and young people than adults (II).
The need for long-term treatment should be considered in young people because of the potentially disruptive effect of relapse and mood instability on cognitive and emotional development (S).
In elderly people
Consider lower doses of psychotropic medicines of all classes for all phases of treatment when adverse reactions or effects are evident with conventional dosing (check the SPC for prescribing recommendations) (*).
In women and pregnancy
Women who may become pregnant
There is a risk of teratogenicity from valproate and carbamazepine (I). The risk/benefit for valproate contraindicates its use in women of child bearing potential under normal circumstances (I).
Concerns about lithium and cardiac malformation appear to have been disproportionate (II).
Since as many as 50% of pregnancies currently occur unplanned, access to family planning advice should be ensured whenever feasible (S).
Women who are pregnant
Low or no risk of teratogenesis appears to be associated with dopamine antagonists/partial agonists, antidepressants, lamotrigine and lithium. However, risks from new compounds are usually unknown and always justify caution. Any teratogenic risk putatively associated with the use of medicines should be considered in the poorly appreciated context of a relatively high, age-related, baseline risk for congenital malformations and spontaneous abortion and confounding by indication (S).
Women are not protected from relapse by pregnancy. Discontinuation of medicines risks destabilising mood (IV). Hence, the possible risks of medicines to the foetus needs to be balanced with the risk of mental illness in the mother and its effects on the health of the baby (S).
Many psychotropic drugs used to treat bipolar disorder can cause neonatal symptoms (II & III). Neonates should be monitored for possible adverse reactions in the hours and days following birth (S)
Women are at high risk of relapse to mania or depression following childbirth (I). Vigilance is essential and effective prophylactic treatment should always be considered and usually recommended (S).
Adverse reactions attributed to maternal psychotropic medicines have been sporadically reported in breast-fed infants but the prevalence is unclear (III).
Women who continue to take psychotropic medication after childbirth should choose between breast and bottle feeding after a full explanation of the relevant benefits and harms (S). If a mother takes medication and breast feeds, the infant should be monitored for possible adverse reactions (S).
There are regular reports of adverse outcomes in the development of the children of women treated with antidepressants or other psychotropic drugs. Too often such studies appear inadequately controlled for confounding by indication. Accordingly, claims that drugs used in pregnancy cause adverse behavioural outcomes should be treated cautiously.
NICE has published perinatal guidelines relevant to these recommendations (http://pathways.nice.org.uk/pathways/antenatal-and-postnatal-mental-health).
Part 2. Consensus Points and Review Fundamentals of Patient Management
1. Diagnosis and psychopathology
DSM-5 criteria provide the appropriate schema for diagnosis of Bipolar Disorder. DSM-5 mania defines bipolar I Disorder (S).
Hypomania is not associated with significant functional impairment. With major depression, a history of hypomania defines bipolar II disorder (S).
Hypomania and mania apparently precipitated by antidepressants or stimulants does not disallow the diagnosis of bipolar disorder (IV).
Incidence per lifetime is, together, about 1% for bipolar I and conservatively defined DSM-5 bipolar II disorder (I). Other Specified Bipolar and Related Disorders add a further 2-3% of bipolar diagnoses in adults.
Bipolar I disorder is highly heritable (up to 80%) and caused by many common genetic variations of small effect.
Bipolar I disorder (mania) occurs rarely in pre-pubertal children, but its improved diagnosis in children and young adults is an important priority(S).
Relapse in bipolar I and bipolar II disorder occurs with a higher frequency than in unipolar depression (I).
The clinical presentation of major depression is similar for unipolar and bipolar patients. Suicide, deliberate self harm and violence are important risk outcomes across the life span for bipolar patients (I).
Anxiety disorders are the commonest co-morbid conditions in bipolar disorder (I) but are often missed or ignored (IV).
Alcohol use is common in bipolar disorder (I). Drug use is more relevant to younger patients with mania (I). Established addictive problems should be assessed and treated (S).
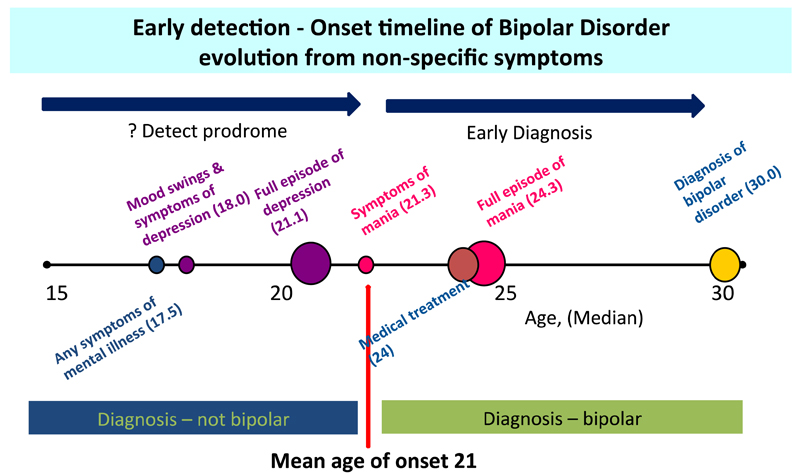
Delay in diagnosis occurs because the illness may start non-specifically, the diagnosis of mood elevation is missed or symptoms are attributed to substance use or personality disturbance (II).
There is an unexplained resistance on the part of some clinicians to diagnose bipolar disorder even when the syndrome of mania has clearly been present (IV).
Key uncertainties
Severity of mania, presence of psychotic features and mixed features may all influence outcome but are poorly characterised in relation to treatment response.
The diagnosis of hypomania in DSM-5 sets an arbitrary minimum time requirement of 4 days. Many more cases of ‘unipolar’ major depression appear to have had shorter periods of hypomania or simply hypomanic symptoms, so approaching or meeting criteria for ‘other Specified Bipolar and Related Disorders’.
DSM-5 encourages the use of ‘mixed feature’ specifiers for individual episodes to capture symptoms of the opposite pole of the illness. The relationship between MDD with mixed features and bipolar disorder is uncertain. It may be more common in the presence of co-morbid borderline personality disorder (II).
The mechanisms linking bipolar states to self harm or other violent acts (for example, impulsivity, disinhibition, inducing or exacerbating low mood via alcohol/drugs) are poorly understood.
DSM-5 has introduced a new syndrome (disruptive mood dysregulation disorder or DMDD) to capture a childhood syndrome, which may have nothing to do with bipolar disorder, but is classified as a mood disorder.
Reliable diagnosis was arguably the major achievement of the last century in psychiatry. It depends upon the use of operational criteria to define cases, and its most important framework is provided by DSM-IV (American Psychiatric Association, 1994) and DSM-5 (American Psychiatric Association, 2013). We will recommend DSM-5 criteria in this text. However, some of the changes in diagnostic sub-typing with specifiers will have uncertain implications for current treatments. We also recognize that in clinical practice the precise use of research criteria may be too exacting a standard. It is however, the standard to which we should aspire.
Reliability of diagnosis, especially for mania, is high under optimal conditions. The use of checklists and standardised interviews could ensure improved diagnosis under ordinary clinical conditions (Hiller et al., 1993). However, we recognize that field trials for DSM-5 showed only average reliability for bipolar diagnoses (Freedman et al., 2013). Practice may also be made more comprehensive with a patient-completed screening instrument like the Mood Disorders Questionnaire (MDQ) (Hirschfeld et al., 2003), the Hypomania/Mania Symptom Checklist (HCL-32) (Meyer et al., 2007) or the Computerized Adaptive Technology for Mental Health (CAT-MH) (Achtyes et al., 2015).
Bipolar disorder is, at present, the most commonly used term to describe serial elevations of mood usually along with intercurrent depressions of mood. Descriptions consistent with Bipolar Disorder exist since antiquity but Kraepelin first used the term manic-depressive psychosis to include all cases of affective psychosis. Patients with unipolar, commonly psychotic depression were included in the diagnosis whether or not they had experienced mania. The central emphasis on mania and thus on bipolarity emerged relatively recently. Bipolar I disorder is defined by episodes of mania and also, usually, depression. The incidence of bipolar I disorder is estimated between 2-21 per 100,000, per year. Differences in reported rates are probably due to the definition of cases. Differences based on first admissions to hospital, which is a proxy estimate of severity, show figures that are less variable and, on average, represent a rate of about 3-4 people per 100,000 per year. Incidence per life-time of bipolar disorder is approximately 0.5%-1% for Bipolar I disorder (I, (Angst and Sellaro, 2000; Lloyd and Jones, 2002; Merikangas et al., 2007)).
Bipolar II disorder is characterised by episodes of hypomania and, invariably, major depression. As defined by DSM-IV, its lifetime incidence has also been described as about 1% (I, (Angst, 1998; Merikangas et al., 2007). This estimate depends on where the boundary between bipolar II and sub-threshold bipolarity is drawn. A figure nearer 0.5% may be more appropriate (Merikangas and Lamers, 2012) giving 1% as the figure for lifetime diagnosis if bipolar I and II combined.
Bipolar I disorder is prominent in secondary care because it is a highly prevalent rather than a highly incident condition. It follows a relapsing, often chronic course, with an average 8 episodes over the 10 years following diagnosis. The rate of relapse is higher than that seen in unipolar disorder of comparable severity (I, (Winokur et al., 1993; Angst and Preisig, 1995)).
The known aetiology of bipolar disorder is primarily genetic with estimated heritability as high as 0.93 (I, (Potash and DePaulo, 2000; Kieseppa et al., 2004)). This means it is one of the most heritable disorders in medicine. Genome-wide association (GWA) studies have now been conducted on sufficiently large samples to give complete confidence in a growing number of specific genes. These small effects when combined can now account for about 20% of the heritability (Cross-Disorder Group of the Psychiatric Genomics et al., 2013). Bipolar disorder is highly polygenic so leaving little room for causation by rare genes of large effect. Genetic effects are not susceptible to errors of reverse causation, otherwise common in observational epidemiological studies. Therefore, these positive findings confirm that the DSM diagnosis has some biological validity. However, there is clear evidence of overlap with risk genes for both schizophrenia and major depression. This genetic architecture was predicted by the elevated rates of bipolar disorder, unipolar depression, and psychosis in first-degree relatives of bipolar patients (Gershon et al., 1982). Compared with schizophrenia, there is weaker evidence for presumed environmental aetiologies such as obstetric complications or inner city residence (I, (Bain et al., 2000; Browne et al., 2000; Lloyd and Jones, 2002)).
Factors such as early abuse and neglect are elevated in bipolar disorder and increase the risks for other co-morbid psychiatric disorders; this probably worsens the course of bipolar illness (II, (Leverich et al., 2002)). Abuse and neglect are also associated with impairments of memory and executive function in bipolar patients (Savitz et al., 2008) and may increase the risk of psychosis (Read et al., 2005).
The overlap of risk genes for bipolar I disorder with those for ADHD is apparently negligible, even though current significant alleles account for about 20% of the risk of each disorder separately (Cross-Disorder Group of the Psychiatric Genomics et al., 2013). This is perhaps the first example of where genetics may eventually guide psychiatric diagnosis (see below).
The differential diagnosis of elated states in Bipolar Disorder
Mania defines bipolar I disorder. DSM-IV criteria for mania, which form the basis for most of the studies cited in these guidelines, are as follows (American Psychiatric Association, 1994):
-
1
A distinct period of abnormally and persistently elevated, expansive, or irritable mood, lasting at least 1 week (or any duration if hospitalisation is necessary).
-
2
During the period of mood disturbance, three (or more) of the following symptoms have persisted (four if the mood is only irritable) and have been present to a significant degree:
-
a.
inflated self-esteem or grandiosity
-
b.
decreased need for sleep (e.g. feels rested after only 3 hours of sleep)
-
c.
more talkative than usual or pressure to keep talking
-
d.
flight of ideas or subjective experience that thoughts are racing
-
e.
distractibility (i.e. attention too easily drawn to unimportant or irrelevant external stimuli)
-
f.
increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation
-
g.
excessive involvement in pleasurable activities that have a high potential for painful consequences (e.g. engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments)
-
a.
-
3
The symptoms do not meet criteria for a Mixed Episode.
-
4
The mood disturbance is sufficiently severe to cause marked impairment in occupational functioning or in usual social activities or relationships with others, or to necessitate hospitalisation to prevent harm or self or others, or there are psychotic features.
-
5
The symptoms are not due to the direct physiological effects of a substance (e.g. a drug of abuse, a medication, or other treatment) or a general medical condition (e.g. hyperthyroidism).
DSM-5 (American Psychiatric Association, 2013) has modified Criterion 1 by adding the requirement for increased activity/energy as a core symptom of mood elevation. This represents an effort to reduce over-diagnosis of bipolar disorder driven by subjective report, and increase specificity (Suppes et al., 2014).
The symptoms must be present for one week and/or require hospital admission. Most critically, the criteria include a judgement that function is impaired. Admission to hospital obviously defines loss of function and autonomy quasi objectively. Less obvious impairment will require identification of failure in normal working and personal relationships and judgement. Intelligent patients may be very difficult to assess from this point of view without corroborating evidence from third parties. The contribution this makes to misdiagnosis will be considered below. This definition of mania underpins the distinction made between bipolar I disorder and milder elated subtypes. Psychotic mania is usually regarded as reflecting severity rather than a subtype. Thus, psychotic symptoms wax and wane within individual subjects and are not invariably present from one episode to another. As a rule, psychotic symptoms in mania are mood congruent and represent an extension of grandiose interpretations, paranoid ideation or heightened awareness. They are relatively common (McElroy et al., 1996; Dunayevich and Keck, 2000). However, in a study of over 500 patients with mania, only 20% had a presentation dominated by psychosis (Sato et al., 2002). This may mean that such symptoms can often be missed in routine clinical practice.
In a minority of cases, symptoms seem to be mood incongruent and in some cases this is diagnosed as schizo-affective disorder. Strictly defined schizo-affective disorder (according to DSM-IV and 5) is relatively uncommon in clinical samples because patients must meet diagnostic criteria for both bipolar disorder and schizophrenia simultaneously. It may also be unreliable (II, (Maj et al., 2000)). The meaning of a schizo-affective diagnosis also remains controversial. It may represent forms of illness in some sense intermediate between the two Kraepelinian psychosis types, so supporting the unity of psychotic states, or it may be the co-occurrence of the two different disorders (II, (Kendell, 1987; Kendell and Gourlay, 1970)). Genetic findings are increasingly supportive of the former view (Craddock and Owen, 2010).
Although euphoric mania is the classic type of presentation, a significant number of cases of mania are far from euphoric and may have a mixture of different symptom dimensions. These dysphoric presentations require diagnostic expertise for detection. The most striking example is where patients meet the criteria for both mania and depression simultaneously as was required for the diagnosis of a mixed state in DSM-IV. However, some significant admixture of dysphoric (depressive) symptoms occurs in many manic episodes. Factor analyses of the symptoms of manic patients have been relatively consistent in suggesting that the atypical features of depressive mood, irritable aggression, and psychosis load on separate uncorrelated factors (II, (Cassidy et al., 1998; Sato et al., 2002)). This agreement suggests the potential to distinguish several relatively separate syndromes among manic patients. Subsequent analysis has confirmed that there are at least two mixed mania presentations. One has a dominant mood of severe depression with labile periods of pressured irritable hostility and paranoia, but a complete absence of euphoria or humour. The second has a true mixture of affects with periods of classical euphoria switching frequently to moderately depressed mood with anxiety and irritability (II, (Cassidy et al., 2001)). These putative subtypes are not identified by existing diagnostic criteria and hence are not distinguished in treatment studies. The change in approach to mixed states in DSM-5 is discussed below.
Severity of mania, presence of psychotic features and the admixture of depressive symptoms may all influence outcome but are also poorly characterised in relation to treatment response. Future advice on acute treatment may take account of differential effects of medicines on the common symptom dimensions. However, at present, only severity, especially expressed as over-activity, imposes itself on current treatment options.
With DSM-5, it is now accepted that mania associated with antidepressant treatment should usually be regarded as defining bipolar disorder, except when the symptoms are reliably locked in time to exposure to a specific antidepressant, like other drug-induced psychoses as discussed below (IV, opinion of the consensus group).
The diagnosis of hypomania
Both the use of the term and the criteria for hypomania have been controversial. Its definition has been crucial to the diagnosis of elated states outside bipolar I disorder. DSM-IV recognised core symptoms of hypomania as a checklist like that for mania itself; DSM-5 has modified Criterion 1 by adding the requirement for increased activity/energy as a core symptom of mood elevation in line with its new definition of mania (see above). This is intended to make diagnosis more reliable, but will thereby exclude individuals with purely subjective experiences of mood elevation from a bipolar II diagnosis.
The time requirement is for four days of symptoms. Patients must display observable but not impaired change in function. This will include mood elevations and increases in energy that are often positively valued by individuals with bipolar disorder. In contrast ICD-10 chooses a slightly different set of symptoms and requires for hypomania, “some interference with personal functioning”. Essentially hypomania under this definition is mild mania and should not include DSM-5 cases of hypomania. ICD-10 hypomania contributes little but confusion to current classification because it tends to encourage the use of the term for frankly manic states (IV, (Goodwin, 2002)).
There is continuing interest in the extension of a bipolar diagnosis to a spectrum of cases with less severe elated states. Bipolar disorder NOS is a DSM-IV category that includes any of the following:(1) recurrent subthreshold hypomania in the presence of intercurrent major depression, (2) recurrent (at least two episodes) hypomania in the absence of recurrent major depression with or without subthreshold major depression, and (3) recurrent subthreshold hypomania in the absence of intercurrent major depression with or without subthreshold major depression. The number of required symptoms for a determination of subthreshold hypomania is confined to 2 criterion B symptoms (from the DSM-IV requirement of 3, or 4 if the mood is only irritable) to retain the core features of hypomania in the subthreshold definition. DSM-5 has changed the ‘Bipolar NOS’ grouping to ‘Other Specified Bipolar and Related Disorder’ but covers the same still ill-defined group of disorders; they have a 2.4% community lifetime incidence (Merikangas et al., 2007).
In fact, on the basis of symptom endorsement over a life time in clinic samples, (Cassano et al., 2004) have suggested that mood elevation forms a continuous bridge between unipolar and bipolar disorder. The intensity of illness, either depressive or manic, increased in parallel and simply showed a higher baseline of elated experience for the bipolar group compared to the unipolar cases. If there is indeed no qualitative break between unipolar and bipolar disorder, the question becomes one of calibration. At what point on this continuum of experience does mood elevation influence treatment choice?
DSM-5 has introduced the concept of a mixed features specifier (see below), which formalizes the identification of manic symptoms in depressive episodes (Angst et al., 2011). These proposed diagnoses still do not yet have clear implications for treatment. However, to call such cases bipolar would increase the temptation for treatment choices to be extrapolated from bipolar I/II data.
The differential diagnosis of depressed states in Bipolar Disorder
Major depression in the context of bipolar disorder is similar to major depression arising in a unipolar illness course, when severity is comparable. Within episodes of depression, grades of intensity – mild moderate and severe – should be distinguished. The use of a scale such as the Inventory of Depressive Symptomatology (IDS) or Quick Inventory of Depressive Symptomatology (QIDS), which maps to the diagnostic features, gives a severity estimate. The QIDS, in particular, is useful in its self-administered form (Rush et al., 2003).
Bipolar patients may be more likely to demonstrate psychomotor-retarded melancholic and atypical depressive features and to have had previous episodes of psychotic depression (II, (Mitchell et al., 2001)). Retarded or psychotic depression, particularly in young people, should raise the suspicion of a bipolar illness course. Indeed, there are a number of other clinical features suggesting a bipolar illness, such as ‘atypical’ depressive features (hypersomnia, hyperphagia, and leaden paralysis), pathological guilt and lability of mood, but none can convey a categorical certainty. There may be scope for the development of such features as a measure of probability that an episode of depression is the manifestation of bipolar disorder in the absence of evidence of mood elevation (Mitchell et al., 2008).
Poor outcomes in bipolar disorder
Deliberate self harm and completed suicide are important risks in bipolar disorder and are associated with depression and mixed states (I, (ten Have et al., 2002; Black et al., 1987a)). For patients identified by admission to hospital, absolute rates of suicide are about 0.4% per year (Tondo et al., 2003). This is 20 fold greater than population rates and translates into risks at long term follow-up between 3-6% (I, (Chesney et al., 2014; Crump et al., 2013), which are amongst the highest for any psychiatric disorder. The increased odds of self harm and suicide compared with sibling controls, arguably a more relevant comparison, is still 6-8 fold (Webb et al., 2014).
The risk of violent and non-violent crime is also elevated in bipolar patients, especially males. The increase compared with sibling controls is 2-4 fold. This risk may not be as widely appreciated as the risk for suicide, but offending is actually a more common outcome and thus associated with a higher absolute risk. Rates of violent crime in male patients were 8% and, for non-violent crime, 18% in one population cohort study, with most of these patients committing their crimes within 5 years of diagnosis (Webb et al., 2014).
Suicide has always received more attention than other adverse outcomes. The risk of suicide is highest early in the course of the illness (Hoyer et al., 2000). Suicide is independently associated with male gender, previous self harm, alcohol and drug use disorders, and previous criminality (Webb, 2014). An early review identified hopelessness at index admission as another risk factor (Hawton et al., 2005). A longer list of possible contributory factors emerges from a broad review of the literature (Pompili et al., 2013); the contribution of individual risks is poorly quantified and many are likely to be confounded.
The lifetime prevalence of non-fatal suicidal behaviour (self harm or attempted suicide) in those with bipolar disorder is approximately 30% (Chen and Dilsaver, 1996; Tondo et al., 2003) and may be as high as 50% in secondary care samples (Valtonen et al., 2005). A recent Swedish population study estimated rates of hospital-presenting self harm at 10% in male patients and 14% in female patients (Webb et al., 2014). Studies have shown that a wider range of factors are associated with self harm than suicide itself, presumably because the former is a more common outcome. These factors include mixed states, rapid cycling, alcohol and drug use, comorbid anxiety, a positive family history of suicide, and, possibly, early abuse or a bipolar II diagnosis (Hawton et al., 2005; Schaffer et al., 2015). Bipolar patients have the highest rate of suicide of all psychiatric disorders. In addition, independent associations have been found for female gender, previous criminality, parental psychiatric disorders and low family income (Webb et al., 2014). Aggression and impulsivity may also be associated with suicide attempts (Oquendo et al., 2000; Oquendo et al., 2004).
Specifiers in DSM-5
DSM-5 has introduced a device to recognize the heterogeneity of episodes in bipolar disorder in the form of specifiers. These can be used with any primary diagnosis (mania, hypomania, depression) to enrich the clinical description.
The mixed features specifier
In DSM-IV, a mixed episode was defined as requiring the full syndrome of mania and major depression to be present simultaneously for at least 1 week. In practice this proved to be a rare diagnosis, although it was widely recognized that symptoms from the opposite pole might be present in a bipolar episode: this has already been discussed above for mania. DSM-5 has dropped the category ‘mixed episode’ and introduced a new feature to the diagnosis of a primary manic, hypomanic or depressive episode: the mixed feature specifier. A specifier requires the presence of three symptoms from a list restricted to those symptoms unique to the pole in question. Thus a manic episode can be said to have mixed features (of depression) if there are three or more of subjective depression, worry, self-reproach/guilt, negative evaluation of self, hopelessness, suicidal ideation or behaviour, anhedonia, fatigue or psychomotor retardation.
The BRIDGE study of over 5000 adults with a major depressive episode identified 47.0% (95% CI, 45.7%-48.3%) as meeting the bipolarity specifier criteria. Associations (odds ratio > 2; P <.001) with bipolarity were observed for family history of mania/hypomania, multiple past mood episodes and comorbid substance use disorder (Angst et al., 2011).
This change may have important implications for clinical care, education, and research in the future (Vieta and Valenti, 2013). For the moment, we do not know whether a more precise categorization of episodes in this way will influence indications for treatment. A particular potential confusion is the possibility to add a mixed feature specifier to a depressive episode in a unipolar illness course. This appears to be most likely when there is a co-morbid borderline diagnosis (Perugi et al., 2015).
Rapid cycling specifier
Patients with four or more episodes of depression, mania, mixed state or hypomania in the preceding 12 months are conventionally described as showing rapid cycling. Rapid cycling is another specifier. It conflates patients with frequent illnesses allowing remission between episodes with those who cycle continuously (or switch continually) from one polarity to the other without euthymia (II, (Maj et al., 1999)). The lifetime risk of rapid cycling is around 16% and it is weakly associated with female gender, bipolar II disorder, current hypothyroidism and a poor response to lithium (especially the depressive component) (II-III, (Calabrese et al., 2001)). Rapid cycling obviously implies temporal severity and it may often be difficult to treat. In 30-40% of cases it may be preceded by exposure to antidepressants, and worsened by treatment with antidepressants (see below: treatment of depression), but there is no proof of a causal relationship.
NICE2014 has chosen not to make specific recommendations for treatment of rapid cycling bipolar disorder, commenting “Offer people with rapid cycling bipolar disorder the same interventions as people with other types of bipolar disorder because there is currently no strong evidence to suggest that people with rapid cycling bipolar disorder should be treated differently.” This is understandable given the paucity of evidence and we agree with their conclusion.
Other specifiers in DSM-5
Other specifiers that may be included in the description of a relevant episode are anxious distress, mood congruent psychotic features, mood incongruent psychotic features, catatonia, peripartum onset, seasonal pattern and for a depressive episode, melancholic feature or atypical features. Their value either for research or clinical practice remains to be established.
Predominant polarity
Although not included in DSM-5 as a course specifier, the majority of patients with bipolar disorder have a tendency to develop more episodes of one pole over the other. This has relevant clinical and therapeutic implications and can be clinically useful in planning drug and psychological treatment (Carvalho et al., 2015; Colom et al., 2006).
Gender
Women with Bipolar disorder have a slightly different profile of illness on average from men. The differences include more rapid cycling, a more seasonal pattern, more and longer depressive episodes, more mixed and dysphoric mania, more bipolar II cases, more comorbidity with medical disorders (e.g. thyroid disease, migraine, obesity) and anxiety disorders, less substance abuse, fewer completed suicides and later onset (Diflorio and Jones, 2010). Except for the implications of pregnancy and childbirth, such differences do not carry implications for treatment.
Co-morbidity
Co-morbidity of bipolar disorder with a range of other psychiatric conditions poses problems of two diametrically different kinds. First, non-specific psychological symptoms and disturbed behaviour may be the harbinger of bipolar disorder in young people. Diagnostic uncertainty or the wrong diagnosis at the very early stages of the illness can delay its accurate recognition (I, (Lish et al., 1994)). Secondly, in the presence of recognised bipolar disorder, co-morbid conditions may contribute to poor treatment response and outcome.
Anxiety disorders and persistent anxiety symptoms
Community samples show replicated, high lifetime co-morbidities of Bipolar I disorder with a range of anxiety related disorders and substance use (I, (Kessler et al., 1997; Merikangas et al., 2007)). Lifetime rates are extremely high in some estimates: as many as 90% of bipolar I patients reported at some time to have had an anxiety disorder in the influential US National co-morbidity survey (I-II, (Freeman et al., 2002; Merikangas et al., 2007)). The most recent meta-analysis of 40 studies, including 14,914 individuals from North America, Europe, Australia, South America, and Asia, suggested a more conservative lifetime prevalence of anxiety disorders of about 45% (95% CI 40–51) (Pavlova et al., 2015).
This raises the question of how to view anxiety symptoms within the behavioural phenotype in bipolar disorder. The earliest symptoms that a patient experiences may be those of anxiety but the dominant picture subsequently may be mania and depression. On the other hand, anxiety is not uncommon between acute episodes and in bipolar depression. Mixed affective states can be misdiagnosed as anxiety and vice versa.
Where the anxiety disorder dominates the outcome, this must clearly influence evaluations of successful treatments. Anxiety disorder co-morbidity is associated with a range of worse outcomes in bipolar disorder such as worse functioning, poorer quality of life, increased suicide rates, rapid cycling and the transition from unipolar to bipolar depression (Fagiolini et al., 2007; Simon et al., 2004) and yet has received little specific attention in developing treatments. For adequate assessment, anxiety should be regularly monitored (in addition to the usual focus on depression and mania).
In fact anxiety in bipolar disorder may have particular features that should influence approaches to treatment development. There is scope to improve assessment to consider bipolar-specific features like anxiety-provoking mental imagery (Hales et al., 2011; Ivins et al., 2014) because this may amplify the expectation of future threat. Mental imagery involves “seeing in the mind’s eye”. While this may relate to intrusive past events (‘flash backs’ as in PTSD) it is also relevant as a ‘flash forward’ experience. Previously suicidal patients may, for example, vividly simulating a future outcome such as jumping off a cliff (Hales et al., 2011). Such experience can be asked about in assessment (in addition to the content of verbal thoughts) (Di Simplicio et al., 2012).
Alcohol and drug use
As with anxiety, excessive use of alcohol or drugs is so common in bipolar patients that there seems to be a shared vulnerability to either or both outcomes. Experimental studies even suggest how this may arise for alcohol dependence (Yip et al., 2012). The risk of alcohol dependence is, therefore, another common (and clinically significant) comorbidity of bipolar I and perhaps to a lesser extent bipolar II disorder. Drug, especially stimulant, use is more relevant to younger patients with bipolar II disorder and is associated with poorer outcome. It can confound the diagnosis and makes engagement with treatment more difficult (I, (Strakowski et al., 2000)). Indeed, mania appears to be induced by a range of stimulant drugs. Where elated states are sustained and meet criteria for mania, a diagnosis of ‘drug induced psychosis’ is likely to be wrong and a diagnosis of Bipolar disorder more useful. A true drug-induced psychosis should either wane with the clearance of the offending drug or be a transient effect associated with drug withdrawal (see definition of Substance-induced psychotic disorder in DSM-IV).
Levodopa and corticosteroids are the most common prescribed medications associated with secondary mania (I-II, (Young et al., 1997; Brown et al., 2002; Brown et al., 1999)).
It is an important principle that bipolar patients with significant alcohol or other drug use should have these issues appropriately assessed and treated, and consideration given to involving the specialist addictions service, or dual diagnosis team, if available. There is evidence that effective treatment of substance use can improve compliance and bipolar outcomes (Ib, (Salloum and Thase, 2000)).
Caffeine is an obvious but often over-looked drug which may contribute to sleep disturbance, anxiety and perhaps mood elevation in bipolar patients. Sensitivity to caffeine, related to its actions at the Adenosine A2 receptor, appear to be genetically determined and modulated by a common polymorphism (Urry and Landolt, 2015). The importance of caffeine in bipolar patients is poorly documented by formal research. Systematic recording of caffeine consumption and efforts to cut down may be helpful in vulnerable individuals.
Gambling, over-spending and shop lifting
Gambling has an increased prevalence in bipolar patients (Jones et al., 2015a), and may be a major clinical problem. There is evidence that gambling is in part a way to regulate mood but mood elevation also enhances enjoyment (Lloyd et al., 2010). There is limited evidence that lithium may have an independent effect in problem gamblers (Rogers and Goodwin, 2005) again pointing to a shared vulnerability. There has been little formal study of the management of problem gambling in bipolar patients.
Overspending and shoplifting can also be problems for people with bipolar disorder compared to other disorders and the general population even between manic and depressive episodes (Blanco et al., 2008). The mechanism is unclear but it can be a significant problem for clinical management.
Personality disorder
Personality disorder may be an important accompaniment of Bipolar disorder, although the categorical approach to personality disturbance has important limitations (Blacker and Tsuang, 1992). As with the co-morbidities already described, the greater risk probably lies in allowing a personality diagnosis to blind the clinician to bipolar disorder, rather than vice versa. DSM-5 retains borderline, obsessive-compulsive, avoidant, schizotypal, antisocial and narcissistic personality disorders, but also recognizes dependent, histrionic, paranoid and schizotypal. The borderline diagnosis is the most critical for confusion with bipolar disorder. Histrionic personality disorder falls in the so-called ‘dramatic’ or cluster B grouping with borderline, narcissistic and antisocial disorders; it is also not uncommon in bipolar disorder, but has received little clinical attention.
Borderline personality disorder may be co-morbid in as many as 20% of bipolar I and II cases. The dual diagnosis is associated with worse outcomes: hospitalisation (Colom et al., 2000), suicidal ideation and deliberate self harm (Leverich et al., 2003), increased service utilisation (Lembke et al., 2003), substance abuse (Kay et al., 2002), poor symptomatic outcome (George et al., 2003) and worse adherence & treatment response (Colom et al., 2000; Bieling et al., 2007).
The relatively high rate of co-morbidity is problematic because clinicians usually seek to make an exclusive diagnosis of one or other disorder. Moreover, they appear to try and do so without really enquiring systematically about borderline symptoms in particular (Saunders et al., 2015). Finally, even if there is a systematic enquiry about symptoms, there is a potentially confusing overlap between borderline symptoms, bipolar spectrum and rapid cycling bipolar disorder.
The key symptoms that distinguish the borderline diagnosis are the pervasive presence of efforts to avoid real or imagined abandonment, unstable and intense personal relationships, an unstable image of self and chronic feelings of emptiness. The defining feature of bipolar disorder is (hypo)mania, which is not satisfied by identifying simply the anger which is such a strong feature colouring the presentation of borderline patients. The diagnoses can only be made by systematic enquiry about symptoms and construction of the longitudinal course of the illness. Symptoms in bipolar disorder are episodic and in borderline patients pervasive and enduring. It is a grave clinical error to interpret bipolar episodes as pervasive and personality driven if they are not. Early abuse and neglect is common in psychiatric patients in general and not diagnostic of borderline personality disorder, as widely believed (Saunders et al., 2015).
Organic conditions
Organic conditions, such as thyroid disease, multiple sclerosis, neurosyphilis or any lesion(s) involving right-sided sub-cortical or cortical areas may be associated with secondary mania (II-III, (Cummings and Mendez, 1984; Mendez, 2000; Strakowski et al., 1994)) and should be considered in the differential diagnosis. Secondary mania is commonest in older patients (Dols et al., 2014).
Early diagnosis of bipolar disorder
The early diagnosis of bipolar disorder may not be easy. The delay described in surveys of patients with bipolar disorder is, on average, a decade (I, (Lish et al., 1994)). A number of factors contribute. In part it will be because, as noticed in the previous section, the first developments may be non-specific anxiety, depression or substance use. Bipolar disorder cannot be diagnosed if an episode of (hypo)mania has not yet occurred, and it would be unhelpful to say that a diagnosis has been missed in these circumstances. Notwithstanding such reservations, the diagnosis of (hypo)mania or sub-syndromal mood elevation may indeed often be missed in young adults. Misdiagnosis contributes to the problems for patients and their families when accepted diagnostic criteria are either not applied or ignored. In young patients, generally, behavioural disturbance may be interpreted as the maturational tensions of adolescence. Alternatively, ‘personality’ diagnoses are still perhaps too readily employed (III, e.g. (Tyrer and Brittlebank, 1993)). To miss a diagnosis of a treatable condition may be harmful. Second opinions from bipolar specialists are potentially helpful.
Finally, before the expression of frank (hypo)mania, a significant number of bipolar patients diagnosed with unipolar depression may run into difficulties because of inadequate or inappropriate treatment. In addition to morbidity, the failure to diagnose bipolar disorder appears to incur significant additional costs (McCombs et al., 2007). Any patient who is being treated for depression should be asked if they have a personal history of abnormal mood elevation of any duration or a family history of affective disorder (D, opinion of consensus group).
Diagnosis of bipolar disorder in children
It is fully accepted that Bipolar I disorder can present before puberty and should be diagnosed as such. It is a relatively rare condition and its recognition should rest on the detection of the symptoms of mania - specifically euphoria and grandiosity and never simply irritability. Most studies of childhood bipolar disorder have been conducted in the absence of empirically supported guidelines for determining the presence of the manic syndrome, which poses real operational problems for definition in children. For example, what constitutes grandiosity at age 8 versus age 15 and at what point does silliness and laughing, usually associated with normal childhood behavior, become indicative of mania? NICE2014 recommends that the diagnosis of mania in a person under 18 years of age requires a distinct period of abnormally and persistently elevated or expansive mood. Plus, there has to be a change in the person’s normal pattern of behaviour that is not developmentally appropriate and which is associated with impairment. Therefore, the condition is episodic, not chronic. It is quite likely that mania is more often mis-diagnosed than over-diagnosed in the UK context. It is very important clinically to recognize that the first presentation is often depression; so those with recurrent depression, or with treatment-resistant depression may have bipolar disorder. Because it is proportionally more common in young people (unipolar depression tending to a later incidence) it may often be a diagnosis that is over-looked.
NICE2014 recommends that “Diagnosis of bipolar disorder in children or young people should be made only after a period of intensive, prospective longitudinal monitoring by a healthcare professional or multidisciplinary team trained and experienced in the assessment, diagnosis and management of bipolar disorder in children and young people, and in collaboration with the child or young person’s parents or carers”. It should take into account the child or young person’s educational and social functioning. The group endorse this as a standard of care. However, it should not be an injunction that simply delays diagnosis (and appropriate treatment) when diagnostic criteria are already, clearly met.
There is some consistency in reports of the prevalence of bipolar diagnoses in young people in different countries. The average rate for age 7-21 years was 1.8% (95% CI, 1.1%-3.0%). This is probably higher than appreciated (Van Meter et al., 2011). The developmental trajectory is still to be established definitively by prospective studies. People of above average ability are over-represented in bipolar cohorts (MacCabe et al., 2010).
Diagnosis became controversial because ‘childhood bipolar’ diagnoses became increasingly common in some services in North America (II, (Geller et al., 1995)), but generally not in the rest of the world (II, (Wals et al., 2001)). In North America rates of diagnosis increased forty-fold in children and young people in a decade (Blader and Carlson, 2007; Moreno et al., 2007). The desire to move diagnosis earlier in the life history is entirely understandable. Unfortunately to do so inevitably risks sacrificing specificity to sensitivity. At the risk of over-simplification, softening the diagnosis of bipolar disorder to allow irritability and chronicity risks confounding with more common problems such as ADHD and oppositional disorder. Indeed, these disorders were usually described as very commonly comorbid with childhood bipolar diagnoses in US case series. Affective instability is undoubtedly a component of what troubles many children, but it does not allow ‘early diagnosis’ of true bipolar disorder.
DSM-5 moved to diffuse the problem of diagnosing overactive children with emotional instability as ‘bipolar’ by inventing the diagnosis of Disruptive Mood Dysregulation Disorder (DMDD). This is accordingly defined by severe recurrent temper outbursts manifested as verbal rages and/or behaviourally (physical aggression toward people or property) that are grossly out of proportion in intensity or duration to the situation or provocation. It is required to be inconsistent with developmental and to occur frequently (on average, three or more times per week). It appears to have links in later life with depression, a common outcome at follow up. However, it remains questionable whether this is really a diagnosis that merits classification as a mood disorder, rather than as a particularly severe form or variant of oppositional defiant disorder or ADHD. The separation from the latter is a potential source of confusion in the coming years.
It is now clear that clinical assessment should be supported by structured assessment tools to increase reliability and validity of diagnosis (Youngstrom and Van Meter, 2015). Instruments exist for the children themselves, parents and teachers. The detection of mania is more reliable on the basis of mothers’ reports than either the children themselves or teachers (Youngstrom et al., 2015). This has implications for the assessment of young people who have left home and for whom parental evidence may be lacking.
2. Access to services and the safety of the patient and others
The Department of Health’s ‘National Service Framework’ in the UK set a template for specialist mental health clinical services to focus on ‘psychosis’; this remains broadly unchanged with a consequent lack of understanding among policymakers of the need for high quality specialised services for bipolar patients (IV), either in relation to early intervention or to provision of adult services.
This contrasts with the approach to schizophrenia even though the burden of disease for bipolar I disorder is comparable with schizophrenia (I).
Mania is usually a medical emergency.
Assessment should be offered by a trained psychiatrist with an understanding of both the medicines and psychological treatments available for the management of bipolar disorder (S).
Patients should have access to early intervention, which must include the option of hospital admission (S).
Appropriate use of legal powers of detention is essential for the successful management of risk in some patients with acute mania and severe depression (S).
Consistent outpatient follow up is necessary and many individual patients may require complex interventions in community settings (S).
Risk assessment has poor positive predictive value for adverse outcomes and should not be over-emphasized in management (I).
There is an increased incidence of completed suicide soon after an assessment in bipolar patients (I), which suggests that current practice under-estimates suicide risk (IV).
Early intervention
Early detection and intervention is an increasing aspiration for mental health services. In the UK, the development of all mental health services has been distorted by an emphasis on psychosis and, in early intervention, psychosis has also been the paradigm focus. This could imply that a significant proportion of manic patients will be seen and treated, but actual practice appears to be inconsistent. A psychosis criterion will usually exclude patients with bipolar I disorder who present with depression until they become manic and will completely exclude bipolar II cases.
The illness model proposed for schizophrenia was based on two related ideas. First to reduce duration of untreated psychosis and provide a service that was geared to treating younger people; avoiding stigma was a key element. The secondary purpose was inspired by the idea of a prodromal presentation and early intervention to prevent onset of syndromal illness. There is an inherent contradiction for these two approaches being pursued by the same service. Earlier detection of established illness implies diagnostic confidence and an earlier choice of evidence based treatments. In contrast, a prodrome is likely to be a relatively non-specific predictor of subsequent illness, in the absence of a diagnostic biomarker. Hence, there would be tolerance of diagnostic uncertainty, and no established approach to treatment.
Early presentations with affective disorder pose the same dilemma. The necessary diagnostic tools to identify bipolarity in the prodrome are under active investigation (Howes et al., 2011; Youngstrom et al., 2015). However, we lack the necessary service structure to deliver any clinical programme.
One version of a staging model for bipolar disorder is shown in Fig. 1. An important caveat is that staging implies predictable progression (most classically in the context of a cancer diagnosis) and bipolar illness course is much less predictable. Indeed the high rates of symptomatic diagnoses in young people suggest the outcome can be benign in a significant number of individuals assessed as teenagers (Tijssen et al., 2010).
Figure 1. The problem for early detection of bipolar disorder.
Adapted from (Berk et al., 2007).
There is a reluctance to make a diagnosis in young people with bipolar disorder, which is to some extent reinforced by NICE2014. Thus, NICE recommendations place an emphasis on specialist and detailed assessment. Much as this may always be desirable, it may be unnecessary if symptoms and history are obvious. If detailed assessment is not available, one result is likely to be failure to intervene in a way that might engage younger people with bipolar disorder at a time when treatment has most potential to be both effective and efficient (Kessing et al., 2013; Jones et al., 2015b). The first symptoms of bipolar disorder commonly occur in the teenage years, with a mean age of onset by age 20 but many diagnoses are not made before the age of 30 (Fig. 1).
First and early episodes
Early-onset bipolar patients are about twice as likely to present with depression as mania (see Fig 1 and (Biffin et al., 2009)). Depression with psychosis in young people may predict subsequent bipolar disorder (Tohen et al., 2012). Highly recurrent illness and a family history may also raise the index of suspicion that a young person with a depressive episode has bipolar disorder. The use of antidepressants (i.e. drugs for unipolar depression) in these patients appears to be quite common. There is very little controlled data, but the findings from large naturalistic studies suggest that a patient whose diagnosis subsequently changes to bipolar is more likely to receive multiple treatments for their first depressive episode and so may be relatively treatment-resistant (Goodwin, 2012). This may be a further clue to diagnosis. Additionally, the drugs themselves may increase the risk of manic switch or mood instability. In either case, they do not lend strong support to the use of antidepressants for unipolar depression in bipolar cases (see later).
Even where the diagnosis can be made with confidence there is a dearth of evidence concerning the optimal management of a first syndromal episode. The key objective must be to prevent recurrence and the accrual of disability in young people because they tend to have poor clinical outcomes (Coryell et al., 2013). The optimal treatment choices or combinations are not established; the available data to be reviewed below concern mature patients.
Any acute episode, regardless of polarity, should receive active treatment. Mania, in particular, is a relative emergency because of the important personal and social consequences that result from the errors of judgement that are intrinsic to a highly elevated mood state. The complexity of bipolar disorder makes it desirable that assessment should be offered by a trained psychiatrist with an understanding of both the medicines and psychological treatments available for the management of bipolar disorder. Patients should have access to early intervention within an episode, which must include the option of hospital admission.
Appropriate use of legal powers of detention is essential for the successful management of some patients with acute mania and psychotic depression. Patients who are unlikely to co-operate with treatment because of difficulties in accepting their diagnosis, who use drugs, or in whom violence, risk taking or self harm complicate their mood change may require complex, community-based interventions, although the optimal approach remains controversial (Burns et al., 2002).
Risk assessment in bipolar disorder
There has been considerable emphasis in mental health policy and corresponding research interest in risk assessment in the UK and other high income countries. This approach is problematic if it is based on the notion of accurate prediction – the predictive value of assessment scales for suicide and violent risk are currently poor to moderate, and the ability of these tools to identify high risk groups is uncertain. For outcomes with very low base rates such as suicide, risk factors will only be weakly predictive of the event, and most suicides will occur in patients who, in statistical terms, are at low risk (Powell et al., 2000); this is also called the prevention paradox. Therefore, the idea that high risk groups can be appropriately targeted in providing services is a fallacy.
All bipolar patients are at risk of suicide, especially if admitted to hospital, when their first episode is depressive, if prone to recurrent depression and mixed states, have co-morbid anxiety (Harris and Barraclough, 1997; Schaffer et al., 2015) or comorbid drug and alcohol use disorders (Webb et al., 2014). The logical approach is to provide good long-term clinical care to as many of them as possible.
One area where suicide risk assessment needs to be examined more carefully is in self-harm patients with bipolar disorder presenting to hospital. Here the subsequent risk of suicide is high in the following year particularly (Tidemalm et al., 2008), and therefore risk assessment really may enable more effective targeting of those that need enhanced follow-up. This is important because risk may be under-estimated in bipolar patients. Thus, in a large survey of suicides in the UK, more than 60% of the bipolar group were in contact with services the week prior to suicide but were assessed as low risk (Clements et al., 2013). A diagnosis of bipolar disorder should modify an optimistic risk assessment of a symptomatic patient.
Concerns about the risk of violence by psychiatric patients (not necessarily bipolar patients), has led to a proliferation of often very lengthy assessment schedules. A systematic review of the better known instruments suggest that they perform quite well at predicting individuals at low risk of offending, but the positive predictive value for those who will offend is not strong (Fazel et al., 2012). Thus, there is little evidence to support the routine use of the current set of commonly used instruments in bipolar disorder. New instruments will have to be assessed on their own merits, using multiple measures of performance. They need to be scalable, evidence-based, and not lead to patient harms (as positive predictive values will be low).
In conclusion, the central purpose of risk assessment should be clinical diagnosis and estimation of severity of depression. For suicide and violence risk, beyond identifying comorbid substance abuse and past history of self harm and criminality, further quantification of risk is unlikely to help plan treatment and services. Many suicides occur in the first year after a serious episode of self harm, so reinforcing the need for attention to this clinical context and to early treatment engagement. Prisoners represent another high risk group who merit the same consideration (Fazel and Seewald, 2012; Fazel et al., 2013).
The potential for the prevention of suicide and violent offending
The most important perspective for risk assessment is the potential for successful long-term treatment to reduce suicide risks by preventing new episodes or reducing chronic symptoms. Suicide has never been the primary outcome measure for a clinical trial in bipolar disorder, because in practice observable rates are too low. However, naturalistic studies have long suggested that suicide rates are lower in patients who receive long-term treatment (Angst et al., 2002). Furthermore lithium may have particular efficacy. This conclusion is again based largely on naturalistic comparison of patient cohorts on and off lithium, but the findings from different centres are consistent and the treatment effect is very large (I, (Tondo et al., 2001; Toffol et al., 2015)). One short-term RCT also found suicides and attempted suicides to be associated with carbamazepine and not lithium treatment (Ib, (Thies-Flechtner et al., 1996)). Indeed, meta-analysis of all the randomized controlled data for lithium suggests an important effect on suicide in studies which are individually inconclusive because of inadequate power (I, (Cipriani et al., 2013a)). An emerging study of a large Swedish data base which allows within subject comparisons on and off treatment in a so-called quasi-experimental design, has confirmed lithium’s effect in reducing suicide attempts by 30%; the same effect was not seen with valproate (Song et al.). Both lithium and valproate treatment were associated with 90% reduction in completed suicide.
There is also recent evidence that treatment may be effective in reducing the rate of violent crime in patients with bipolar disorder. The data again comes from record linkage of medications and outcome. Dopamine antagonists halved the rates of offending in bipolar disorder and schizophrenia. Drugs for relapse prevention (‘mood stabilizers’ so lithium and valproate mainly) had an equally potent effect in bipolar disorder (but not in schizophrenia) (Fazel et al., 2014). These results are impressive because the events are relatively common, effect sizes are so large and the outcomes so important. As already emphasized in relation to data quality, they move the argument for benefit to a completely different level, compared with effects on symptoms or even symptomatic relapse. Consequently we have upgraded them in assessing the evidence supporting the use of medications in the long term.
The National Confidential Inquiry data for England and Wales (1997–2006) included 1243 bipolar patients (10% of the sample) who had died from suicide, and been in contact with mental health services in the previous 12 months (Clements et al., 2013). They make sobering reading. Only 390 (31%) were adherent with medication at time of death. This is an important measure of how ineffective management strategies currently are for our patients. Only 13 (about 3%) died by poisoning with prescribed drugs, so the benefit/risk potential appears favourable. The challenge appears to be the delivery of effective treatment.
The need for a service model
The neglect of the specific needs of bipolar patients in UK government policy (Morriss et al., 2002) justifies our restating the obvious in the previous paragraphs. The term bipolar disorder or manic depression was given no special consideration (and entirely omitted from the glossary of key terms) in the National Service Framework for mental disorders in the United Kingdom (Department of Health, 1999). It remains a monolithic social model of mental illness, which is inappropriate to bipolar disorder (Goodwin and Geddes, 2007).
The complexity of the disorder, the resulting need for specialist and expert care and the potential for preventing bad outcomes by early treatment all argue for a concerted effort to improve treatment. The recent NICE guideline implied that this objective could be achieved by the appropriate deployment of existing services. We are very sceptical. In our view, a separate, serious effort to extend early intervention to young people with affective disorder, with appropriate identified funding, is long overdue. The absence of early stage specificity has led to pioneering approaches to youth mental health services in Australia, where distress rather than a diagnostic criterion applies, and bipolar patients can, in principle, make appropriate access (McGorry et al., 2007).
In addition to the lack of focus on bipolar disorder, and certainly contributing to making it worse, is the traditional fault line between child and adolescent services and adult services. This falls at exactly the point where continuity is most obviously needed for young people developing severe psychiatric disorder (IV).
Nevertheless, there remains a need for better quality evidence on which to argue for an improved approach to care. According to an analysis for the charity MQ, funding for research on bipolar disorder has been about one third that for schizophrenia in the decade to 2013 (http://www.joinmq.org/pages/mental-health-research-funding-landscape-report). It is hardly surprising that our knowledge base is less than it might be: this must change.
The best service model?
The single most relevant study concerned bipolar patients discharged from inpatient care for their first, second or third episode of bipolar disorder in Denmark (Kessing et al., 2013); they were randomized to either specialised or standard care. The specialized care reduced re-admission over the subsequent 6 years by about 20%. This approach would not necessarily be cost effective for less severely ill patients, but it translates into very appreciable cost savings in a group of patients at high risk of relapse and re-admission.
The key ingredients of expert care appear to have been psychoeducation (based on the Barcelona model (Colom and Vieta, 2006)), an algorithmic psychopharmacology (based on the previous BAP Guidelines) and continuity/consistency of care. A critical ingredient of psychoeducation is likely to be active monitoring for signs of relapse to mania and this approach should be a standard of care (Morriss et al., 2007). The system in Denmark is broadly comparable to the UK, so these results may well generalize. They deserve very serious consideration in arguing for a better future in the care of bipolar patients.
In the USA, a collaborative care model has been proposed involving a key worker to keep close contact with the patient, encourage adherence to treatment algorithms and guidelines and follow up in the case of non-attendance. Two similar studies showed small positive effects on a number of outcomes (Bauer et al., 2006a; Bauer et al., 2006b; Simon et al., 2006). This may have been mediated in part by improved adherence in the collaborative care arms of the studies (Bauer et al., 2009). Finally collaborative care focused on physical health improved blood pressure in a small RCT (Kilbourne et al., 2013). The lessons of these findings are less easy to translate to the UK because primary care and community provision is usually so limited in the USA and so there is the potential for a much bigger impact of service outreach. This was the lesson previously drawn from systematic comparisons of community care models for schizophrenia, which outside the USA had less if any impact on outcomes (Fiander et al., 2003).
Finally one negative or failed trial (Crowe et al., 2012) has the possible lesson that collaborative care needs to be an integral part of a service, rather than an add-on that risks disrupting the continuity of the core service provision.
NICE2014 published evidence from patients that supported employment initiatives are highly relevant to improving social outcomes. There are a few specific issues like risks of overspending, recklessness that may require some safeguards, undesirability of shift work for some bipolar disorder patients and the ability to take time off relatively quickly if early signs of mania or depression emerge. Psychiatrists and other professionals should be aware of these issues when counselling return to usual employment as well.
In conclusion, very little work has pragmatically addressed the best model of service delivery for bipolar patients. Our conclusions are summarized alongside those reached by NICE (2014) in Table 1. The NICE approach essentially proposes that generic NHS care can be readily extrapolated to the needs of bipolar patients who require admission and access to secondary care services.
Our primary conclusion is that we really do require more evidence of what works at the systems level. In Table 5 most of the recommendations by NICE2014 are not based on formal evidence, certainly for applicability to bipolar disorder. Instead they appear largely driven by what is currently provided in theory by psychosis-orientated NHS services. However, it appears a priori self-evident that services should be led by specialists with expertise in guideline-based psychopharmacology, there should be continuity of care and psychosocial management should be informed by and apply lessons from psychoeducation.
Table 5. Comparison of emphasis in planning service provision for bipolar patients.
The items where benefit is uncertain, or based on no formal evidence for bipolar disorder, are marked with an asterisk.
| NICE | BAP |
|---|---|
| Access to early intervention for psychosis | Access to early intervention from experts in bipolar disorder(S). For mania, always consider admission to hospital or intensive community management (S). |
| Care programme approach* Continue in specialized service or integrated CMHT but offer those stable the option of a return to primary care* |
Long-term specialist services with a consistent flexible alliance (S) with a specifically trained psychiatrist(S) |
| Discuss self-management and engagement | Help patient and carers recognize early signs of relapse |
| Intensive case management for those likely to disengage. Crisis management* | Disorganised patients need assertive management |
| Offer a structured psychological intervention Offer family intervention Offer supported employment programme* |
Consider offering enhanced psychological and social support |
Recent further fractionation of clinical services, for example between in and out patients, ‘assessment’ and ‘treatment’ is a recent concern. It runs counter to the needs of bipolar patients in all stages of their treatment but particularly in managing follow up. Premature discharge to primary care can further dilute the treatment package available in the early stages of managing the illness (IV).
3. Enhanced clinical care
Enhancement of patient care can be achieved by structured interventions based on psychoeducation (II). This has the potential to complement and inform treatment with medicines, not replace it (IV).
While, the evidence for efficacy in preventing relapse comes from mature patient samples, the same approach can inform early assessment and intervention with young people (IV).
We support NICE’s assertion that assessment and management of bipolar disorder should ideally involve partners, families and carers.
Bipolar patients are at high risk of cardiovascular, metabolic and respiratory disease: there should be an annual auditable check for hypertension, central obesity, raised blood glucose, and dyslipidaemia annually (S).
Assess consumption of alcohol and drugs. Drinking up to 14 units of alcohol per week represents lower risk drinking levels for men and women (<1% increase in excess mortality). High risk drinking (10% excess mortality) is 35 units or over per week.
Bipolar patients may have a particular problem with the use of tobacco (I). Treatment with effective nicotine substitutes will often be indicated (IV).
Key uncertainty
The optimal approaches to enhanced care are evolving rapidly with the rapid development of self-monitoring and instruction from mobile apps.
As noticed in the previous section, the services in which care is delivered clearly constrain what is possible. However, good individual clinical practice is a commonplace but essential objective. Psychiatrists must take responsibility for diagnosis, physical examination, investigations and explanation of the medical plan of management. They must communicate clearly and effectively. A therapeutic alliance between doctor and patient is essential for the management of any complex chronic condition, which bipolar disorder certainly is.
The role of structured psychological treatment in the management of bipolar disorder remains at an experimental and exploratory level. However, the findings are already important because they suggest that enhanced care can improve outcomes in bipolar I and, probably, bipolar II patients. Broadly speaking the interventions that have been offered in bipolar disorder are pragmatically directed to identified clinical problems. They do not depend on specific models of psychopathology. There is also appreciable overlap in content of the different approaches although it is conventional to consider them under separate headings. The following general principles are important.
-
1)
Bipolar disorder is a long-term problem, so psychological treatments should produce enduring behavioural change. Acute effects of any psychological approach need also to be considered in the longer term.
-
2)
We endorse the NICE statement on caregiver involvement. In essence, partners, families and carers can contribute significantly to the assessment process, the management of acute episodes, the promotion of long-term recovery and the prevention of relapse. This has the further implication that carers may benefit from information and support to improve how they achieve these objectives.
Knowledge (or ‘Psychoeducation’)
There is a consensus that good clinical management of patients with bipolar disorder involves an appreciable educational component for both patients and their relatives. The objective of acquiring knowledge about the illness is prevention of relapse. Successful long-term management involves a high degree of patient involvement and autonomous judgement about return of symptoms etc. It is essential to address the seriousness of the illness, any reluctance to give up the experience of hypomania or mania, the risk of relapse and the benefit of therapeutic engagement (IV). For patients to know what to do, and why, appears usually to be an essential prelude to actually doing it.
One option is to provide a formal group course, the efficacy of which was shown in a randomized controlled trial (II, (Colom et al., 2003)). This compared psychoeducation with an equivalent group experience in which the content was simply unstructured supportive discussion. The use of an appropriate control intervention gives this trial particular credibility and the benefits of psychoeducation appear to be sustained because mood episodes of all types were reduced over a 5 year follow up of the original trial participants (Colom et al., 2009). The effect size compared to other psychoeducation RCTs makes it an optimistic outlier (Bond and Anderson, 2015). Nevertheless, the findings described previously from Denmark over six years may also underline the potential for long clinically relevant effects in patients with recent illness onset (Kessing et al., 2013). Comparison with other alternatives, notably CBT (see also below), has also illustrated the economy of a more educational approach (Parikh et al., 2012).
Despite our endorsement, virtually as a standard of care, negative or just marginally positive findings have been common in trials of psychoeducation. Pellegrinelli et al (2013) failed to show any difference in clinical outcomes for 16 psychoeducation versus non-psychoeducation sessions using the Barcelona manual; a slightly different psychoeducational approach run in UK mental health teams failed to separate convincingly from treatment as usual (Lobban et al., 2010). A related, more sustained intervention (the Life Goals program) showed minor effects on manic symptoms over 2 years (Simon et al., 2006) but more substantial gains in function (not reduced symptoms) over 3 years (Bauer et al., 2006b). These failed or marginally positive trials indicate the methodological challenge to future treatment development.
Failure to find a difference between groups is associated with higher proportions of patients with more previous episodes (Scott et al., 2007). Age appears not to vary between studies of adult patients, so intensity rather than length of illness appears to be the limiting factor. Clearly, lack of efficacy in large numbers of patients with more recurrent illness represents a challenge to understand the failure of existing approaches and an unmet need to develop better treatment approaches in the future.
The key ingredients of all psychotherapies so far found useful for bipolar disorder (including psychoeducation) are as follows (Miklowitz et al., 2008):
-
1.
Monitor moods and early warning signs
-
2.
Recognize and manage stress triggers and interpersonal conflicts
-
3.
Develop relapse prevention plans
-
4.
Stabilize sleep/wake rhythms and daily routines
-
5.
Encourage medication adherence
-
6.
Reduce self-stigmatization
-
7.
Reduce alcohol or drug use (including caffeine in sensitive individuals)
The involvement of carers/family is highlighted in family-focused treatment for younger patients, which has similar ingredients (Geddes and Miklowitz, 2013). In fact, these elements are also commonly present in treatments formally described in clinical trials as something other than psychoeducation (e.g. cognitive behaviour therapy (CBT) and inter-personal social rhythm therapy (IPSRT)), which is a source of confusion. The role of CBT will be considered in a little more detail in relation to the treatment of bipolar depression and relapse prevention.
Optimal delivery of psychoeducation
The group format may not be culturally generalizable, so individual or family, rather than group approaches to psychoeducation, are also likely to be helpful and can inform ordinary practice. Facilitated use of a 5 session psychoeducational package increased comprehension of the principles and practice of self-management compared with self-instruction (Miklowitz et al., 2012).
Current practice also favours didactic teaching, live or by video, written materials or guided internet searching for high quality material (e.g. the National Electronic library for mental health: http://www.nelh.nhs.uk/). There is also an explosion of self-help apps, most still of rather low quality (Nicholas et al., 2015), that may incorporate personal mood and activity monitoring on mobile devices. The approach has enormous intuitive appeal, but systematic examination of the effects of self-monitoring has not led to immediate proof of concept (Faurholt-Jepsen et al., 2015). Such individual, rather than group approaches, includes the use of auto-didactic on line psychoeducation (Barnes et al., 2011): to see this in action visit http://www.beatingbipolar.org. The possibility of recording therapy sessions on patients’ phones for subsequent review also has the potential to enhance patient care. This is an area likely to see major advances in the coming years and, hopefully, clarification of what really helps.
A time very early in the illness course may not be the most propitious for patient acceptability; however, it may be a critical period for the greatest impact of behavioural change on clinical outcome. Thus, the goals of education need to be sustained and incremental. There also needs to be a shared and consistent approach across mental health disciplines. Psychoeducation also appears to offer an approach to intervention in the early stages of the disorder before diagnosis is necessarily established and medicines are indicated.
Adherence to medicines
As we will review, there is good evidence that long-term treatment is effective in preventing relapse in bipolar disorder. However, adherence to prescribed medicines is poor in most chronic illness (I, (Horne et al., 2013)). Bipolar disorder is no exception (II, (Johnson and McFarland, 1996; Lingam and Scott, 2002; Scott and Pope, 2002)). The simplest framework for understanding adherence weighs the perceived need for treatment against concerns about its possible effects (Clatworthy et al., 2009). Understanding need will necessarily be a matter for education and personal experience. Adverse reactions are a major consideration given the limitations of existing medicines and should be minimised by all possible means. These include once daily administration (e.g. at bed time), switching between formulations and dose adjustments. Other efforts to improve adherence such as user-friendly packaging, monitoring of pill taking, delivery of supplies of medicine may contribute to successful treatment in certain individuals.
The motivation to take tablets is heavily dependent upon the attitudes, beliefs and perceptions of risk shown by patients and their carers. These cultural factors may often divide clinical staff from patients. Pragmatic motivational interviewing to improve adherence to prescribed medicines has already been shown to be moderately effective in patients with psychosis. The best-known early study included a sub-group with bipolar disorder (II, (Kemp et al., 1998)). Since non-adherence with treatment occurs in up to 50% of most clinical samples (Scott and Pope, 2002), the development of a focused and generally applicable approach to this problem would be welcome. The published methodology emphasises the involvement of a third party and there is clearly a potential role here for pharmacists who occupy an advisory role for patients in other contexts. Where barriers to adherence are identified and targeted interventions delivered, adherence is more likely to improve (Staring et al., 2010). Patient-related factors include younger age, male gender, low educational level, alcohol and drug use. Disorder-related factors include severity, insight and lack of awareness of illness. And treatment-related factors are obviously adverse reactions to medications and perceived lack of efficacy. To improve adherence, clinical practice should address the underlying causes of non-adherence within the overall frame work of psychoeducation (Leclerc et al., 2013). If the bottom line for adherence is the balance between the perceived necessity of drug treatment and concerns about it, this should inform clinical efforts to improve it.
Clinical trials, in bipolar disorder as in other conditions, are likely directly to enhance patient care (I, (Ashcroft, 2000)). We believe that participation per se in well-designed clinical trials is a benefit for both doctors and patients. To put it bluntly, a controlled experiment is likely to be better than participation in the uncontrolled experiment that is ordinary practice. Furthermore the results from trials will eventually enhance the evidence base for improving patient care. Participation in trials is potentially related to adherence and hence we make the point here
Awareness of stressors, sleep disturbance and early signs of relapse, and regular patterns of activity
Manic relapse in particular may follow a relatively stereotyped course in individual patients. Sleep disturbance is perhaps the most commonly described final common pathway to mania (II, (Wehr et al., 1987)). The sleep of bipolar patients between episodes is often disturbed in a very similar way to that of patients with primary insomnia (Harvey et al., 2005). Despite this, formal trials to improve sleep in bipolar disorder are only just beginning. Pilot data suggest effects of CBT for insomnia generalize to bipolar symptoms (Harvey et al., 2015).
The more usual emphasis is on tell tale signs and symptoms of relapse; this may take the form of particular impulses and preoccupations which accompany or even precede it. Efforts to train patients on individual scripts which access their own experience and enable them to take evasive action appears to be effective in avoiding new episodes of mania (II, (Perry et al., 1999)). This approach was less successful with episodes of depression. The original intensive trial involved up to 12 sessions of training and there is a need to know whether a more dilute approach or one focused uniquely on personal scripts for relapse into mania would be more widely applicable. The involvement of family members with experience of previous episodes may be helpful (Reinares et al., 2008).
Interpersonal social rhythms therapy (IPSRT) developed out of particular ideas about what behavioural features contribute to relapse in bipolar disorder (II, (Swartz and Frank, 2001)). The reestablishment of routine and regular activity for those behaviours that recur at least once per week is a primary goal in treatment. IPSRT provides a simple framework for practical advice and feedback. It has also informed the development of a phone based app for sensing activity and providing feedback to shape social activity (Matthews et al., 2014).
The further role of structured psychotherapy will be considered in relation to relapse prevention. All such therapy recognizes as axiomatic the value of a highly collaborative therapeutic relationship with the patient. The commitment by a clinician to see a patient long term can contribute to an optimal management plan.
The general point emerges that outcomes for patients can be improved simply by enhancing ordinary clinical care, most obviously by adopting a consistent approach to psychoeducation or knowledge sharing. Translating this observation into enhanced care for more patients should be an important objective for treatment.
Functional impairments
Clinicians must anticipate the need to give advice about expectations and capacity to work. Major life decisions may not be auspicious when made in a depressive or manic state. Furthermore, patients may experience considerable difficulty performing at the level for which their education may have prepared them (II, (MacQueen et al., 2001)). This may be a result of common sub-syndromal symptoms of depression or anxiety (I, (Denicoff et al., 2000)) or other barriers to psychological well-being (II, (Scott, 1996)). Factors specific to bipolar disorder such as experience when high, or personality style, may also conspire to widen the gap between aspiration and achievement. Finally, there is evidence that objective impairments of neuropsychological function are both significant and enduring (I, (Bourne et al., 2013)). These objective problems in sustaining attention, memory and executive function appear to be made worse by repeated episodes (Clark et al., 2002; Martinez-Aran et al., 2004) and are more severe in bipolar I patients (Bourne et al., 2015). In other words they may be a quasi-toxic consequence of the intensity of the illness course. Polypharmacy may also compound the problem (Clark et al., 2002; Frangou et al., 2005).
The National Service Framework for Mental Health recognised the vital role of informal carers in the delivery of mental health care (Department of Health, 1999)). However, it treated the needs of adults of working age as generic and was probably influenced by evidence from research in schizophrenia (I, (Fadden et al., 1987)) and the dementias (I, (Clyburn et al., 2000)). The literature concerning bipolar disorder is sparse, but the perceptions and beliefs of carers about it, as for other diseases, may have important effects on levels of burden that are experienced (II, (Perlick et al., 1999)). There is scope to develop improved psychosocial interventions tailored to bipolar patients and their families. A particular uncertainty, neglected hitherto, is the impact of manic states upon carers, and indeed their children. A preliminary investigation of the families of 86 stable patients showed that caregivers still showed a moderate level of subjective burden. The highest levels of distress related to the patient’s hyperactivity, irritability, sadness and withdrawal. The illness had also affected the carers’ emotional health and life in general. Poorer social and occupational functioning, an episode in the last 2 years, history of rapid cycling and the caregiver being responsible for medication intake explained a quarter of the variance of the subjective burden (Reinares et al., 2006).
It seems reasonable to note the emphasis on recovery with return of function as the modern aspiration for bipolar patients. Cognitive impairment is a barrier to good outcomes and there is preliminary evidence that cognitive remediation can play a part in improving function (Torrent et al., 2013).
Physical health, alcohol and drug use
In this country, a retrospective cohort study compared 46,136 patients with ‘severe mental illness’ (SMI) with 300,426 without SMI (using the GP Research Database). Hazard ratios (HRs) for coronary heart disease (CHD) mortality in people with SMI compared with controls were 3.22 (95% confidence interval (CI), 1.99-5.21) for people 18-49 years old and 1.86 (95% CI, 1.63-2.12) for those 50-75 years old. For stroke deaths, the respective HRs were 2.53 (95% CI, 0.99-6.47) and 1.89 (95% CI, 1.50-2.38). Event rates in these age groups are quite low, but increased HRs for CHD mortality occurred irrespective of sex, SMI diagnosis, or prescription of medication during follow-up (Osborn et al., 2007).
The risk across the life span has been documented in a series of studies for bipolar disorder specifically. In most countries the estimate of years lost in bipolar patients is between 10 and 20 years (Chesney et al., 2014). Put another way, just under 25% of the male population in Sweden die before the age of 70 years. The corresponding age for bipolar patients is just over 50 (Laursen and Nordentoft, 2011). Cardiovascular causes account for almost 40% of the deaths, which is nearly twice the number of suicides and accidental deaths; the risk is elevated across the life span. Moreover, the survival in the 5 years from diagnosis of a cardiovascular event is substantially reduced in bipolar patients (Westman et al., 2015), which may mean either that patients present later in their illness course or receive inferior treatment (or both).
The metabolic syndrome/obesity and type II diabetes are important in the mediating pathologies to cardiovascular disease. In a meta-analysis of the data from bipolar patients, rates of the metabolic syndrome were elevated about two fold compared with controls (Vancampfort et al., 2013). Treatment with dopamine antagonist drugs was associated with a rate of 43%, compared with 32% in those not so treated. However, the variation from country to country suggested a major contribution from dietary habits as well. In impressive population data from Taiwan, the times to initiation of treatment for both hyperlipidaemia and diabetes were significantly delayed for patients with bipolar disorder compared with the general population (Bai et al., 2013)).
Thus, effective medical management of physical illness in patients with severe bipolar disorder is a major challenge. The higher risk of cardiovascular disease in bipolar patients is not solely due to medication, and life style factors like smoking, diet and lack of exercise are also important. Consequently, a bipolar diagnosis should imply annual screening for metabolic risk factors even if a dopamine antagonist is not prescribed.
The metabolic syndrome is a composite of biochemical, blood pressure and weight indices. It is associated with older age, higher body mass index, and higher values for each individual criterion of the metabolic syndrome. The absolute waist circumference (>102 centimetres (40 in) in men and >88 centimetres (35 in) in women) and the waist-hip ratio (>0.9 for men and >0.85 for women) are both used as measures of central obesity. In a small study, the presence of central obesity is the most sensitive indicator (92.0%) and fasting glucose 7.0 mmol/l or over was most specific (95.2%) in correctly identifying the presence of metabolic syndrome (Straker et al., 2005). The treatment of blood pressure over 120/80 mmHg, and the use of statins in bipolar patients should follow existing medical practice.
Weight gain, in part driven by medication, is a particular problem. A comprehensive guideline, much of which will be relevant to bipolar patients as well as patients with psychosis, is provided by ‘The BAP guideline on the management of weight gain and metabolic disturbances associated with psychosis and antipsychotic drug treatment’ currently in preparation for this journal.
The consumption of alcohol and drugs will contribute to both physical and psychiatric morbidity and mortality. The assessment of these contributory factors and lifestyle advice are key to a more synergistic approach to treatment in bipolar disorder. Public Health England suggest that up to 14 units of alcohol per week for men and women represents lower risk drinking levels (excess mortality <1%). There is a monotonic increase in the risk of alcohol related death with higher levels of consumption. Excess mortality exceeds 10% at a consumption around 35 units per week. It is recommended that drinking is spread over the week but with 2 or more alcohol free days. This represents a tightening of advice for men particularly, based on new data showing an increased excess of cancers in drinkers (https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/489797/CMO_Alcohol_Report.pdf ).
Advice on the use of tobacco is also essential because in data from the US, bipolar disorder has the highest rate of current and lifetime use and the lowest quit rate of any other psychiatric disorder (I, (Lasser et al., 2000)). Treatment with effective nicotine substitutes will often be indicated (I, https://www.nice.org.uk/guidance/ph45 ).
Audit of current practice: Prescribing Observatory for Mental Health (POMH-UK)
The POMH-UK is based at the Royal College of Psychiatrists’ Centre for Quality Improvement and runs audit-based quality improvement programmes (QIPs). The vast majority of UK mental health trusts participate in these traditional audit, intervention, re-audit cycles. For some QIPs it is possible to abstract current prescribing practice for people with bipolar disorder specifically and for other QIPs data relating to those with a diagnosis of an affective disorder.
Treatment with dopamine antagonist agents should always trigger screening for four cardio-metabolic risk factors (hypertension, central obesity, raised blood glucose, and dyslipidaemia). In a national POMH audit conducted in 2012 (Prescribing Observatory for Mental Health, 2013), 22% of patients with an affective disorder who were prescribed antipsychotic medication had been screened for all 4 of these measures in the previous year, 54% for up to 3 measures, and 24% had received no screening. The respective figures for those with a diagnosis of a schizophrenia or related disorder were 36%, 49% and 15%. Thus, despite the major cardiovascular health risks for bipolar patients, these audit findings suggest that, when receiving antipsychotic medication, they are less likely to have physical health screening and monitoring than patients on such treatment with a diagnosis of schizophrenia.
When prescribing lithium, the practice standards (derived from NICE guidance) require that a patient be informed at the start of treatment about the potential adverse reactions, how they could recognise toxicity and how they should avoid toxicity. Audit data at baseline revealed that the proportion of patients provided with this information at the start of lithium treatment ranged between 42 and 62% (Prescribing Observatory for Mental Health, 2013). At a subsequent audit, conducted after provision of a bespoke, patient-held lithium information pack, the respective figures rose to between 54 and 68% (Paton et al., 2013).
A further finding was that approximately one in five patients who started lithium had no documented baseline test of renal function or thyroid function and this proportion remained relatively consistent over 5 years (2008-2013). However, there is some evidence that monitoring of serum lithium, renal and thyroid function improved over the same period; at baseline, there had been no documented monitoring of these parameters in the previous year for 10%, 19% and 18% respectively, but by the fourth audit, these proportions had fallen to 5%, 7% and 10%. Serum lithium concentrations within the usual target range (0.4-1 mmol/L) are found in almost 100% of patients in some NHS Trusts, but the proportion is as low as 50% in others.
Psychotropic drug prescribing for bipolar patients in the UK was fairly consistent over time. For patients taking lithium, around 20% took lithium alone, 45-50% took a second drug, about 30% a third, and 5% a fourth. This underlines current levels of polypharmacy. The added medicines are dopamine antagonists/partial agonists (55-60%), antidepressants (35-40%), valproate (13%), lamotrigine (5%), and depot or long acting drug (5%). For valproate, age/child-bearing potential did not seem to influence prescribing.
Given these data, antidepressants appear to be relatively over-prescribed and lamotrigine relatively under-prescribed given the evidence of benefit (q.v.). However, when prescribed, lamotrigine use seems to follow the indications presented in guidelines (Grande et al., 2012).
A template for audit of bipolar disorder is suggested in Table 4.
Table 4. Recommendations for audit in bipolar patients.
| Diagnosis |
| Is there a structured patient-completed (or structured interview) record? |
| Is there a record of the manic symptoms in mania? |
| Is there a record of the depressive symptoms in depression? |
| Have symptoms of borderline personality disorder been recorded as present or absent? |
| Is there a record of anxiety symptoms? |
| Has the history of alcohol and drug use (including caffeine) been documented? |
| Has impairment of memory and executive function (or functional impairment) been considered? |
| Risk assessment |
| Is suicide risk recorded? |
| Is neglect of self and dependents, exploitation by others considered? |
| Is risk of violence or offending considered? |
| Physical health |
| Is a physical health screen conducted annually? |
| weight, blood pressure, lipids, fasting glucose |
| renal and thyroid function, calcium concentration if taking lithium |
| Has appropriate treatment been offered for physical health problems? |
| Treatment |
| Lithium |
| Has lithium been offered for maintenance treatment? |
| Is the use of lithium safe? |
| (baseline eGFR, lithium concentrations, thyroid function, calcium) |
| Are serum concentrations of lithium measured regularly? |
| Are serum concentrations of lithium maintained above 0.6 and below 0.8mEq/l? |
| Dopamine antagonists/partial agonists. |
| Are doses within accepted limits? |
| Are multiple dopamine antagonists/partial agonists being prescribed together? |
| Is long-term use justified? |
| Drugs for bipolar depression |
| Is prescription of antidepressants for depression or anxiety? |
| Is there evidence of treatment response to the antidepressant? |
| Is use justified? |
| Have options with a better evidence base for treating depression been considered (e.g lamotrigine, quetiapine) |
| Valproate |
| Is valproate being used in women of childbearing age? |
| If so, is a written justification recorded in the case notes? |
| Has the patient clearly understood the risks? |
| Has effective contraception been offered? |
| Psychological interventions |
| Has psychoeducation been offered? |
| Is there a mechanism in place for regular mood monitoring? |
| Is there a plan which anticipates the actions required when the patient relapses with mania, develops a worsening of depressive symptoms or expresses suicidal ideas? |
| Is the person delivering the psychological intervention linked to other members of the care team? |
Treatment of Different Phases of Bipolar Disorder
Terminology and treatment strategy
Bipolar disorder usually presents for treatment in an acute illness episode (mania, depression or mixed state) (I). The objective of short-term treatment is to reduce the severity and shorten the duration of the acute episode and achieve remission of symptoms (S).
Long-term treatment is indefinite for the prevention of new episodes and to achieve adequate inter-episode control of residual or chronic mood symptom (S).
Because of the high risk of relapse and the apparent progression to more frequent episodes, long-term treatment with appropriate medicines is advocated from as early in the illness course as is acceptable to a patient and their family (S).
Between episodes, mood instability or chronic depressive symptoms are common (I) and generally underestimated.
Key uncertainty
Current strategies emphasize the treatment and prevention of syndromal relapse. Disabling aspects of long-term outcome such as chronic depressive symptoms, mood instability, co-morbid anxiety, enduring neurocognitive impairment or oxidative status may be important future therapeutic targets.
It is usual to think of bipolar disorder as a sequence of acute illness episodes (mania, depression or mixed states) interspersed with relative euthymia. This view of the illness conditions how treatment strategies and actual treatment phases are distinguished. Short-term treatments will refer to episodes and will often imply the intention to discontinue a medicine on recovery. Long-term treatment is indefinite and for the prevention of new episodes. Although it is conventional in discussing unipolar disorder to distinguish relapse (the early return of symptoms treated in an acute episode) from recurrence (the return of symptoms after remission), this is a distinction that is rarely helpful in bipolar disorder with relatively frequent episodes. We will refer to long-term treatment for prevention of relapse.
Currently neglected in the bipolar literature are the times between episodes. These represent most of the patient’s life and may be characterized by a variable sub-syndromal level of mood symptoms. Euthymia, the absence of symptoms and the presence of positive stable mood is actually quite unusual. Chronic symptoms in bipolar disorder are commonly depressive (II, (Judd et al., 2002; Judd et al., 2003; Kupka et al., 2007)) and significant levels of residual symptoms are predictive of relapse (Judd et al., 2008). As already noticed, there are also cognitive distortions similar to those seen in depressive disorder (II, (Scott, 1996)), sometimes disabling anxiety (Albert et al., 2008) and neuropsychological deficits that are still largely ignored (Bourne et al., 2013). These negative aspects of long-term outcome are often accepted as the natural history of the disease. In addition, there is evidence for increased oxidative stress, measured as enzyme activity in brain post mortem (Andreazza et al., 2013), in peripheral tissues in life (Andreazza et al., 2008) or as increased concentrations of oxidized circulating glutathione (Rosa et al., 2014). Inflammatory markers are also disturbed in bipolar patients (Modabbernia et al., 2013). Along with measures of social adjustment, these alternative measures of outcome represent key areas of focus for current uncertainty.
1. Acute Manic Episodes and DSM-IV mixed states
Treatment choice should be dictated by the clinical context and, whenever possible, by patient preference and experience (S). However, systematic comparison of the performance of drugs for mania suggests that haloperidol, olanzapine, risperidone and quetiapine have the highest efficacy.
Drugs and dosages should be chosen that do not produce Extra-Pyramidal motor Side effects (S), which is of particular significance in bipolar patients because of their apparently greater risk of adverse motor reactions compared with schizophrenia (I for haloperidol).
When combined with lithium or valproate, a number of dopamine antagonists/partial agonists have been shown to be superior to lithium or valproate alone (I). Combination treatment can be considered especially when patients show break-through mania with the first agent.
GABA modulators (benzodiazepines) are useful adjunctive agents and can induce sedation or sleep (II).
ECT is an important treatment option in cases of delirious mania, since this may be a medical emergency, and in treatment of resistant mixed states.
Discontinuation of short-term treatments for mania can be considered after full remission of symptoms. The required duration will often be of the order of 12 weeks although higher doses may be reduced earlier (IV).
Key uncertainty
Switch to depression after mania may occur in any illness course: it is not established which treatments, if any, make this more likely.
Dopamine antagonists/partial agonists (Antipsychotic drugs)
Mania can develop extremely quickly and incur risks both for the patient and for others. In its more severe form, mania is almost invariably treated with dopamine receptor antagonists/partial agonists and patients with psychotic mania were among the first patients treated successfully with chlorpromazine. Dopamine receptor antagonists/partial agonists are antimanic not simply sedative. However, despite their widespread use by an earlier generation of psychiatrists, placebo controlled data to show that the older dopamine antagonists (“first generation” antipsychotics) were effective in mania were very limited before the turn of the century (e.g. II, (Johnstone et al., 1988)). This changed when placebo controlled studies of new drugs included haloperidol as a comparator.
While the neurobiology of mania is still poorly understood, mania may be a hyperdopaminergic state appropriately treated by blockade of dopamine D2/3 receptors with antagonists or partial agonists. This is a common effect of the anti-manic drugs described below. The detailed additional pharmacology is described for some of the drugs in the section on treating depression, because it may be more relevant for that indication.
A series of RCTs have been completed showing the efficacy for mania of aripiprazole, asenapine, cariprazine, haloperidol, olanzapine, paliperidone, quetiapine, risperidone and ziprasidone in comparison with placebo (Yildiz et al., 2011; Yildiz et al., 2015). Olanzapine, aripiprazole and ziprasidone are also available in parenteral formulations for acute use. Ziprasidone and cariprazine are not available in the UK.
The newer antipsychotic drugs were developed with a primary objective to reduce the incidence of extra-pyramidal symptoms (EPS). Therefore their efficacy showed that an anti-manic action could be achieved in the absence of EPS (II, (Keck et al., 2000)). This is an important clinical message, which should influence prescribing practice, for all dopamine antagonists.
The marketing of the newer drugs as ‘atypical’ implied a qualitative break from the past (the ‘typical’ antipsychotics) in regard to EPS. This was misleading. The reduced tendency to produce EPS depends on dose and pharmacology. The use of muscarinic antagonists (antiparkinsonian medication) provides a proxy for clinically significant EPS. In head-to-head studies (Rummel-Kluge et al., 2012), risperidone was associated with more use of such medication than clozapine, olanzapine, quetiapine, and ziprasidone. Quetiapine showed significantly less such use than olanzapine and risperidone. In addition, patients with bipolar disorder may be more at risk for EPS than patients with schizophrenia, for example when treated with high potency dopamine antagonists like haloperidol (Cavazzoni et al., 2006). Accordingly, successful treatment of mania without EPS is an important practical clinical objective that can be facilitated by differentiation between drugs that are anti-manic.
The relative efficacy and acceptability of the treatments for mania has been analysed using network meta-analysis or NMN (Cipriani et al., 2011; Yildiz et al., 2015). All the dopamine antagonists (and the partial agonist, aripiprazole), showed superiority to placebo. NMN demonstrated an order of relative superiority that ranked risperidone, olanzapine, quetiapine and haloperidol at the top; haloperidol was less well ranked for acceptability (drop outs from trials). The network was highly coherent and so strongly supports the validity of the overall recommendation to use dopamine antagonist/partial agonists in mania. The individual rankings of drugs are of interest but show considerable overlap in confidence intervals.
Clozapine may also be considered by extrapolation from its likely superiority in treating psychosis (Leucht et al., 2013) and limited observational data in treatment resistant mania (Green et al., 2000; Li et al., 2015).
Other factors that influence the choice of drug include properties such as sedation, which may be desirable in the short term but not in the long term, and the choice of formulation. Finally, in the UK only aripiprazole is licensed for up to 12 weeks’ treatment of moderate to severe manic episodes in bipolar I disorder in young people (13 years and older).
The availability of parenteral formulations is valuable in emergencies and should form part of any local protocol for treating highly agitated patients (I, (Wilson et al., 2012)). In the past, often in an effort to achieve sedation, patients were habitually treated with high doses of, for example, haloperidol or droperidol (the latter now withdrawn in the UK), which could produce marked extrapyramidal symptoms unless combined with a muscarinic antagonist. When possible, such extrapyramidal adverse reactions should be avoided, even when managing an emergency.
If sedation is the aim, benzodiazepines such as diazepam, lorazepam and clonazepam are more appropriate and can usually produce adequate sedation. When prescribed regularly at night they may also facilitate the return of a normal sleep wake cycle (II (Post et al., 1996)).
Other medicines for acute mania: lithium, carbamazepine and valproate
Acute treatment trials support the use of lithium, carbamazepine and valproate in mania (Yildiz et al., 2011; Yildiz et al., 2015). Network meta-analysis ranks them below the more efficacious dopamine antagonists (Cipriani et al., 2011), but their use may often be considered if planning their long-term continuation. Expert guidelines in the USA have in the past made lithium and valproate (“mood stabilizers”), their first line preference for mania for this reason (American Psychiatric Association, 2002).
The low therapeutic index of lithium means that lithium is usually commenced at a low dose and increased incrementally approximately every 5 to 7 days depending on results of serum lithium levels. Thus, one cannot usually start a patient on a therapeutic dose of lithium on the first day of treatment whereas this can often be achieved with a dopamine antagonist or partial agonist. The much improved evidence base for the use of the dopamine antagonists and partial agonists has resulted in a convergence of practice and experiment in their acceptance as first line for mania.
Valproate is the term that is often used to describe different formulations of valproic acid, the active chemical entity. Sodium valproate has been widely used in epilepsy and is also available in a sustained release formulation. Valproate semisodium (also known as divalproex) is a non-covalent dimer molecule (comprised of sodium valproate and valproic acid) which has been studied in bipolar disorder and is licensed in the UK as ®Depakote (see Annex for information on dosing of different formulations).
Valproate semisodium is effective in severe mania (II, (Macritchie et al., 2003)), when the dose should be titrated upwards quickly to get control: 750mg on day one and 20mg/kg+ on day two. Previous US Guidelines gave unusual weight to the efficacy data for valproate and the conviction that lithium and valproate are “mood stabilizers” (see below).
Exposure to valproate in utero is associated with developmental disorders and foetal malformations in women. Warnings against its use in women of child bearing potential, and the need for their informed consent if proposing to do so have been strengthened recently (https://www.gov.uk/drug-safety-update/medicines-related-to-valproate-risk-of-abnormal-pregnancy-outcomes).
The combination of a dopamine antagonist drug with lithium or valproate in acute mania
In practice, patients may already be taking lithium or valproate when mania occurs as a breakthrough during long-term treatment. Under these conditions it would be common to optimise the maintenance treatment and/or add a dopamine antagonist/partial agonist drug. Optimisation is favoured if symptoms are not severe, the history suggests that lithium or valproate has been effective until the current ‘breakthrough’, the current treatment is well tolerated and in the case of lithium the most recent plasma level suggests that a dose increase will not push the level above the upper limit of the normal therapeutic range. Otherwise, combination treatment with a dopamine antagonist/partial agonist will be favoured. Most patients included in trials which have compared combination/augmentation therapy versus monotherapy with lithium or valproate had prior treatment with lithium or valproate, whereas most participants in trials comparing combination/augmentation therapy versus dopamine antagonist as monotherapy had not been on medications or were washed out from their previous medication before randomization (Ogawa et al., 2014). The clearest effect was demonstrated when the antipsychotic is added to lithium or valproate not the reverse. Also, in Swedish database studies, the impact of long-term combination treatment on violence was only seen when antipsychotics were added to mood stabilizers and not vice versa (Fazel et al., 2014). Thus, the asymmetry may be a consistent finding and reflect the greater acute efficacy of dopaminergic drugs.
The issue of long-term treatment with lithium and valproate will be addressed below. While it may seem logical to initiate one or other option in acute mania as a prelude to long-term continuation (in combination with a dopamine antagonist), there are no reasons to make this mandatory. Lithium in particular is sometimes difficult to use in exhausted, dehydrated patients. Moreover, efforts to prescribe lithium for patients with poor adherence may be misplaced. Patients very often stop taking lithium; the median time to discontinue was only 6 months in Denmark (Kessing et al., 2007). Discontinuation is associated with admission to hospital (I, (Johnson and McFarland, 1996)). This association will be due, in large part, to relapse of mania, which can be provoked by abrupt lithium discontinuation. Unless patients are adherent to lithium therapy for a minimum of two years, these withdrawal effects will nullify any potential prophylactic effect (Goodwin, 1994).
Carbamazepine is not the optimal partner for combination therapy. Carbamazepine induces the metabolism of many other drugs and combinations are better avoided (Monaco and Cicolin, 1999). Alternatives, licensed for use in epilepsy and less likely to interact with other drugs, include oxcarbamazepine and eslicarbazepine acetate (rapidly converted to eslicarbazepine after oral administration). Eslicarbazepine acetate failed in trials on mania on primary but not all secondary outcomes in trials limited by high placebo response rates (Grunze et al., 2015). Thus, the use of alternatives to carbamazepine represents a plausible extrapolation, not well supported by direct evidence.
GABA modulators (benzodiazepines)
Diazepam, lorazepam, clonazepam and related agents are useful in the management of acutely agitated manic states (Allen et al., 2001). They are adjunctive, so are indicated when sedation or tranquillisation is a priority and when there is a pressing need to induce sleep. Their safety in relatively high sedative doses and the absence of important pharmacokinetic interactions with other agents are advantages.
The use of adjunctive GABA modulators can help to avoid excessive doses of antipsychotic drugs with the attendant risk of cardiovascular and other adverse reactions, including the neuroleptic malignant syndrome.
The switch into depression following mania
It is often stated that treatment with relatively selective and potent dopamine antagonists, like haloperidol, is more likely than treatment with lithium or valproate to result in a switch from mania to depression. This is also a reason that is sometimes given for preferring a drug with dopaminergic/serotonergic effects like olanzapine or risperidone. Evidence is very limited but one large, naturalistic study suggested switch rates of about 5% in the 12 weeks following initiation of treatment for mania (Vieta et al., 2009). Patients with previous depressive episodes, substance abuse and illness severity were more at risk. The study was deliberately enriched for olanzapine (together with an assortment of other ‘atypical’ and ‘typical’ antipsychotic drugs, not specified). The choice of atypical drugs (usually implying a mixed dopaminergic/serotonergic pharmacology) was associated with 10% fewer depressive relapses in confirmation of clinical impression. Controlled data for perphenazine (an older drug) supports the potential negative impact of some dopamine antagonists (Zarate and Tohen, 2004); however, this was a small study and perphenazine’s pharmacology is not very different from the newer dopaminergic/serotonergic antagonists (http://www.guidetopharmacology.org/). The data from the lamotrigine/lithium/placebo relapse prevention trials are a reminder that the risk of relapse of the index episode will usually be higher than the risk of switching (Goodwin et al., 2004).
At present, it would be unwise to base an acute treatment strategy on the assumed risk of switch to depression. However, high doses of dopamine antagonists, especially those with high affinity for dopamine receptors may cause akathisia and dysphoria and should be avoided (Mizrahi et al., 2007).
Discontinuation of short-term treatments
Doses of drugs used in short-term treatment of mania, particularly dopamine antagonists/partial agonists, should be reduced only after complete remission of symptoms, and preferably after 8 or more weeks of euthymia. Benefits of continuation of olanzapine and risperidone were still seen six months (but not 12 months) after illness onset (Yatham et al., 2015a). As a precaution, doses should not be reduced abruptly but tapered over several weeks (IV).
Lithium or valproate, if used in treatment of an acute manic episode, are potentially a rational choice for long-term continuation. However, if either is to be discontinued after full remission of an acute manic episode, the same consideration applies. Lithium discontinuation should occur over a minimum of four, preferably 8 weeks, given the risk of premature relapse (Suppes et al., 1991). Tapering is also preferable to sudden discontinuation for valproate (IV) (Franks et al., 2008).
Adjunctive drugs used during short-term treatment of mania, particularly GABA modulators, should be reduced gradually once the symptoms for which they were prescribed (e.g. agitation, insomnia) have responded and in addition the underlying manic illness has responded to the primary anti-manic treatment.
All patients who have recovered from a manic episode, including their first manic episode, should consider subsequent maintenance treatment. The patient and clinician may decide to continue the drug that proved effective in the treatment of acute mania; this will often be a dopamine antagonist/partial agonist. However, consideration should also be given to switching to lithium (see below) (IV).
Short-term treatments of mixed states
Most treatment recommendations for mixed states (DSM-IV-TR) have resulted from sub-group or secondary analysis of data from trials in mania. Pooled data from acute efficacy trials of dopamine antagonists/partial agonists have not suggested important differences in sub-group effects (Baldessarini et al., 2003). With the accumulation of new data fom acute (3–6 week) studies of dopamine antagonists (asenapine, olanzapine, paliperidone-ER, risperidone, and ziprasidone) and aripiprazole, either as monotherapy or as adjunctive therapy, versus placebo, meta-analysis has confirmed efficacy in treating acute mixed episodes with predominant manic symptoms (Muralidharan et al., 2013). Their efficacy in treating depressed episodes with mixed features remains unclear.
The demise of the mixed state diagnosis in favour of the extended specifier description will have implications for future trials, but as yet little has emerged that is of relevance to choice of treatment.
There is no indication to either start or continue treatment with an antidepressant in a mixed state (IV).
Electroconvulsive therapy
Electroconvulsive therapy (ECT) may be considered for manic patients who are severely ill, whose mania is treatment-resistant (including mixed states (Valenti et al., 2008)), who express a preference for ECT and patients with severe mania during pregnancy. Formal evidence for efficacy in mania is limited; patients with severe mania are difficult to enter into trials. However, audit findings of clinical practice support high rates of response and remission (Mukherjee et al., 1994). Indeed an earlier study suggested a 60% remission rate in manic patients who had previously responded poorly to lithium or dopamine antagonists/partial agonists (Black et al., 1987b). This observational data is strong and consistent enough to merit moderate ranking in the GRADE system.
It can be argued that ECT should be considered especially in cases of delirious mania, since this may be a medical emergency when accompanied by fever, dehydration, and autonomic dysfunction and in treatment of resistant mixed states (Medda et al., 2015).
In view of the polypharmacy common in bipolar disorder, vigilance is required because fit thresholds may be altered and the potential for either too brief or prolonged seizures during ECT increased.
It is more usual for ECT to be considered in depression (see below).
Comparison with NICE guidelines
There are no substantial differences between the conclusions of the NICE committee and ourselves regarding the treatment of an acute manic episode.
2. Short-term treatment of Depressive episodes
Quetiapine has the most convincing short-term efficacy and relapse prevention profile for bipolar depression (I). Olanzapine (in combination with fluoxetine and to a lesser extent as monotherapy) and lurasidone also have data supporting acute efficacy.
Antidepressant drugs approved for unipolar depression may be effective for treating depression in bipolar disorder but the evidence base is very poor. The case is based primarily on extrapolation. They require co-prescription of another agent that will reduce the risk of mania (lithium, valproate or dopamine antagonist/partial agonist drug) in bipolar I disorder (I).
Lamotrigine has evidence for acute efficacy and relapse prevention (I).
The risk of a switch to mania is greater for tricyclic antidepressants or other dual action medications, such as venlafaxine, than with SSRIs (II).
While they are unlikely to provoke a manic switch, lithium, valproate, and carbamazepine have poor evidence for acute efficacy in bipolar depression.
ECT has efficacy in treatment-resistant bipolar depression (II): other options have not been adequately studied.
Discontinuation of an antidepressant should follow BAP recommendations for unipolar depression, but with a more rapid taper in rapid cycling patients (IV).
Key uncertainties
There is a paucity of evidence to decide between different agents in the treatment of bipolar depression.
Refractory depression is not uncommonly associated with a bipolar illness course.
Folate may impair the response to lamotrigine.
Most data are for a bipolar I illness course: it is often uncertain whether the treatment of bipolar II and particularly the other specified bipolar disorder cases with depression should be different from the treatment of unipolar cases.
There may be a risk in bipolar II disorder, that antidepressants induce hypomania, mixed states or rapid cycling. It is uncertain whether this is mitigated by concurrent anti-manic medication.
The role of psychological treatments in bipolar depression remains uncertain, in the absence of replicated good quality evidence. Negative trials of CBT in bipolar disorder suggest caution in extrapolation of the approach from experience in unipolar depression.
Dopamine antagonist drugs (antipsychotic drugs) in bipolar depression
The use of dopamine antagonist drugs in bipolar depression has assumed increasing importance as doubt has grown over the role of conventional antidepressants. Efficacy can only be supported for specific agents, not for the class. This is because the relevant pharmacology is probably not antagonism at dopamine receptors per se. The affinities at other receptors are both multiple and varied (Michl et al., 2014). What among these properties confers antidepressant efficacy is not known. This is partly because not all drugs have been studied equally for depression, so the data on which to map efficacy to drug action are very incomplete.
Most of the controlled data comes from studies of major depressive episodes in a bipolar I illness course. Where there is sufficient evidence from secondary analysis of bipolar II sub-groups it will be noted in the following. Relapse prevention studies offer supporting evidence for acute efficacy. Such studies compare the effect of double blind continuation of an active drug with its discontinuation to placebo. The active drug is used to treat the index episode. Where the index episode is depression, the data will support efficacy in depression. Such designs will be relatively uninformative about preventing relapse to mania (and vice versa when the index episode is mania). All such studies are associated with high dropout rates, so that interpretation of drug/placebo differences over the longer term (the prevention of new episodes) will be problematic.
Quetiapine
In common with a number of other drugs for psychosis, quetiapine has moderate affinity for dopamine D2 and serotonin 5-HT2A receptors. At doses of 300 and 600 mg/day it produced large and early attenuation of depressive symptoms in bipolar patients compared with placebo (Calabrese et al., 2005; Thase et al., 2006). Pooled analysis of these two similar trials, together randomizing nearly 1000 patients, showed effects in bipolar I and bipolar II participants (with slightly lower response rates to active treatment in the latter subgroup) (Weisler et al., 2008). The only concern about the relatively large effect sizes in these trials is the problem of unblinding, which must occur for quetiapine, owing to its sedating subjective effects. This justifies downgrading the trials in the GRADE system.
In relapse prevention studies of patients responding to quetiapine and randomized to continued quetiapine or switch to placebo, continuing quetiapine is associated with fewer episodes of mania, mixed mania and depression after recovery from either mania or depression (Suppes et al., 2013). This further supports the evidence for acute efficacy and, arguably, for relapse prevention (see below).
Current uncertainties relate to the dose: even 300mg produces substantial rates of somnolence and sedation, with associated dropout from treatment and the longer term risks of metabolic disturbance. After only 8 weeks there is evidence of weight gain and significant increases in triglycerides and blood glucose. While not of great importance in short-term treatment, these changes are an important signal to monitor and treat such problems in the medium to long term. There are important differences in metabolic impact between different dopamine antagonist drugs, and quetiapine appears to lie towards the more problematic end of the spectrum (Leucht et al., 2013).
Quetiapine may have unusual properties relative to other dopamine antagonists; one suggestion is that an active metabolite, nor-quetiapine, binds with moderate affinity to the noradrenaline transporter (Goldstein et al., 2007). This may contribute to its antidepressant action (Cross et al., 2015).
If norquetiapine is the active antidepressant agent, implications follow from the polypharmacy common in bipolar disorder. The nor-alkylation (N-desalkylation) is catalysed primarily by CYP3A4. This enzyme may not only be inhibited, but also induced by other drugs (http://medicine.iupui.edu/flockhart/table.htm). Relevant agents that block N-desalkylation include fluvoxamine and norfluoxetine, and inducers include carbamazepine, modafinil, and St John’s wort. Thus, fluvoxamine increases quetiapine concentrations by 159%, while carbamazepine can reduce them by 86% (Castberg et al., 2007); effects on norquetiapine concentrations have not been reported but might be the reverse depending on its route of metabolism.
Quetiapine has also been investigated and found effective in unipolar depression and generalized anxiety (Zhornitsky et al., 2011). Hence it would be misleading to think of it as a selective drug for bipolar depression: by the same token its efficacy in bipolar depression is not evidence for a biological difference between bipolar and unipolar depression although the effect size was larger in the bipolar trials.
Olanzapine
Olanzapine has affinity for dopamine D2, serotonin 5-HT2A, muscarinic and histamine receptors. Interest in the use of dopamine antagonists or partial agonists as monotherapy began when a large RCT showed that olanzapine had a weak antidepressant effect in bipolar I depression compared with placebo (Tohen et al., 2003). A second study has been pooled with the original data and also supports modest efficacy for olanzapine (I, (Tohen et al., 2013)). Its combination with fluoxetine in the original study showed even better separation from placebo. A relapse prevention study against placebo also supported efficacy against depressive relapse (Tohen et al., 2006).
Olanzapine is accordingly an option for the treatment of bipolar depression: its combination with fluoxetine will be discussed below. Similar considerations to those for quetiapine (sedation, unblinding) mean RCT evidence may have been subject to bias so downgrading its quality rating.
Lurasidone
Lurasidone is an antagonist at D2, 5-HT2A, and 5-HT7 receptors, and a partial agonist at 5-HT1A receptors. It has lower binding affinity for α2C and 5-HT2C receptors. It has been demonstrated to show efficacy in two short-term studies in bipolar depression: one as monotherapy and the other as add-on to lithium or valproate (Loebel et al., 2014a; Loebel et al., 2014b). Lurasidone has a low subjective adverse reactions burden and produced minimal changes in weight, blood lipids, or glycaemic control. The commonest reported adverse reactions are akathisia and somnolence. At the time of publication it did not have a license for use in bipolar depression in Europe, but has an indication for schizophrenia. In the US it has a license for the acute treatment of bipolar depression as well as schizophrenia.
Aripiprazole
Aripiprazole is a partial agonist at D2 and 5-HT1A receptors. Data on aripiprazole are of interest. In two 8-week monotherapy studies in bipolar depression, it failed to separate from placebo at the pre-specified 8-week endpoint although separation at earlier times was evident (Thase et al., 2008a). It has been conventional to accept this negative finding as definitive, along with the failure to demonstrate efficacy on the depressive pole in the existing relapse prevention study (Keck et al., 2007). However, the monotherapy studies in bipolar depression may have failed because of shortcomings in the trial design and the relapse prevention study was clearly under-powered to detect effects on depressive relapse.
By contrast, in treatment-resistant unipolar patients two trials of adjunctive aripiprazole suggested antidepressant efficacy (Thase et al., 2008b). There is no comparable controlled evidence for refractory bipolar depression, but a small, uncontrolled case series claimed benefit from adding aripiprazole to a variety of other treatments (Ketter et al., 2006).
Any use of aripiprazole for bipolar depression is clearly an extrapolation from the unipolar data, but its dopamine partial agonist activity gives it modest plausibility as a treatment option with a different mode of action.
Cariprazine
Cariprazine is a highly selective dopamine D3 and D2 receptor partial agonist with preferential binding to D3 receptors. Its mechanism of action is therefore novel and of potential interest for the treatment of bipolar depression. Evidence for efficacy in bipolar depression has been published (Durgam et al., 2015a; Durgam et al., 2015b).
Antidepressants
Antidepressants are commonly prescribed for people with bipolar depression (35–40% prevalence in the POMH-UK audit). Their use is nevertheless controversial (Pacchiarotti et al., 2013). The usual criticisms are either that antidepressants lack efficacy in bipolar depression or they destabilize mood and cause switch to mania. This is undeniably contradictory since it seems to imply either too little or too much effect. Unfortunately, there is a real dearth of placebo controlled trials on which to make an evidence based recommendation. Meta-analysis a decade ago compared the few drugs tested, as a group, versus placebo (imipramine, fluoxetine and tranylcypromine). Most randomized data were obtained in patients also receiving lithium or valproate and, in aggregate, comparison with placebo supported efficacy for antidepressants in general (Gijsman et al., 2004). The STEP-BD trial weakened that conclusion (Sidor and Macqueen, 2011), but did not contradict it. The exception was fluoxetine in combination with olanzapine, which has shown individual efficacy versus placebo and, modestly, lamotrigine (Brown et al., 2006; Tohen et al., 2003).
Recently there has been a double blind comparison of venlafaxine with lithium in bipolar II depression suggesting an important advantage to venlafaxine in continuation treatment (Amsterdam et al., 2015). This adds to other small studies in bipolar II patients suggesting an advantage for fluoxetine compared with lithium and provides the very limited evidence favouring the use of antidepressants in bipolar II disorder (McInerney and Kennedy, 2014). Expert opinion has also proposed SSRIs to stabilize mood in significant numbers of bipolar II patients (Parker et al., 2006). It is recommended that if an antidepressant is prescribed as monotherapy in bipolar II disorder, any increase in dose is gradual and that there be vigilance for, and early management of, any adverse reactions such as hypomania, mixed states or agitation (IV).
In contrast to the dearth of evidence in bipolar patients, there has been a very large number of trials examining the efficacy of antidepressants in unipolar major depression (I, (Anderson, 2001; Undurraga and Baldessarini, 2012)); these studies systematically excluded patients with a bipolar illness course. The drugs tested enhanced noradrenaline and/or serotonin function by inhibiting monoamine re-uptake or metabolism. Hence their actions are likely to be rather homogeneous. The unipolar data support this: network meta-analysis shows major overlap of efficacy for SSRIs with venlafaxine, duloxetine and mirtazapine. Reboxetine, a selective noradrenergic re-uptake inhibitor, was the only clear outlier (Cipriani et al., 2009). Accordingly, the general finding of antidepressant efficacy in bipolar depression may be supported by the experience of treating unipolar depression. It means that the use of these drugs as a class in bipolar patients is essentially an extrapolation.
The anergic pattern of illness often seen in bipolar patients may favour the use of activating antidepressants such as monoamine oxidase inhibitors (MAOIs) (IV). It is usual to caution that while efficacy may be extrapolated for classes of drugs, adverse reactions may be less predictable. However, the extensive experience of using antidepressants in unipolar disorder means that this is not an important limitation, except potentially with the risk for switch to mania. If antidepressants can cause a switch to mania or the emergence of a mixed state, it seems further to imply efficacy, even if it is an argument against using antidepressants except with considerable vigilance.
Another approach to comparing unipolar and bipolar depression has been to audit the response to the same treatments in hospitalised patients (II, (Bottlender et al., 2001; Moller et al., 2001)): the severity of illness and times to response with tricyclic antidepressants appeared to be identical for bipolar and unipolar groups. Less positively, audit data from a very large Taiwanese database suggested that a poor response (usually to SSRIs) in first episodes of depression was predictive of a subsequent bipolar diagnosis (Li et al., 2012). This may imply that compared with unipolar patients, bipolar patients are simply more difficult to treat, but an equally plausible interpretation would be that antidepressants are less effective in the bipolar group (Goodwin, 2012). The issue is inevitably confounded in an observational study.
The view that we cannot safely extrapolate efficacy from unipolar to bipolar depression is widely held. There are several negative studies cited to support it. The STEP-BD study compared paroxetine and bupropion with placebo and the results were certainly negative (Sachs et al., 2007). However, whether this result represents a failure of the trial or of the active treatments is a moot point. The EMBOLDEN-II study compared two doses of quetiapine with placebo and included paroxetine as a comparator (McElroy et al., 2010). Paroxetine did not separate from placebo. However, half the patients in the study were treated with quetiapine, which arguably carries an appreciably higher risk of unblinding than paroxetine and this may have reduced the chances of finding a positive effect. Finally, agomelatine failed in a placebo controlled trial in which very high placebo response rates will have reduced assay sensitivity (Yatham et al., 2015b). Such negative studies provide a poor basis for the conclusion that antidepressants do not work at all in bipolar patients. Comparable studies can also fail in unipolar populations for a variety of technical reasons (Schalkwijk et al., 2014) and the studies themselves were powered to detect conventional positive effects, not to determine equivalence with placebo (non-inferiority).
The argument that antidepressants work in unipolar but not in bipolar depression also implies that there must be an important neurobiological difference between the two conditions. This is not expressed phenomenologically except in the sense that severity appears to increase across the bipolar spectrum (Moreno et al., 2012); one exception could be where depression emerges immediately out of a manic episode and the episode itself is effectively bipolar or mixed, but this is atypical. Neurobiological differences appear likely to be quantitative rather than qualitative (Redlich et al., 2015), although potentially of great interest. Indeed, if there are differences in the responsiveness to antidepressants between bipolar and unipolar groups, it provides a starting point for further dissection of how antidepressants work. For example, one hypothesis is that antidepressant action involves correction of negative emotional bias (Harmer et al., 2009); if bipolar subjects have less negative emotional bias, it might correlate with the reduced effectiveness of conventional antidepressants.
Anticonvulsants in depression
There is no basis for supposing antidepressant effects to be a class effect of anticonvulsant action. However, lamotrigine is of particular interest since it may offer important clues to common or unique mechanisms of action relevant to the development of new treatments.
Lamotrigine
Lamotrigine inhibits voltage-sensitive sodium channels in the brain, which may limit cell firing. It also blocks L-, N-, and P-type calcium channels and is a weak 5-HT3 receptor antagonist. It is a weak inhibitor of dihydrofolate reductase (DHFR).
The efficacy of lamotrigine has been uncertain for acute bipolar depression. The original published study of lamotrigine suggested benefits in bipolar depression compared with placebo (Calabrese et al., 1999) and a second study was also supportive (III, (Frye et al., 2000)). However, four previously unpublished trials conducted by GSK individually failed to show a separation from placebo. These negative findings appeared paradoxical when relapse prevention studies were positive (see below (Goodwin et al., 2004)). How can a drug prevent relapse to depression if it does not have efficacy in the acute episode?
A pooled analysis of the original patient data from all five trials was, in fact, able to show a modest benefit for lamotrigine in bipolar I and II patients with acute depression (I, (Geddes et al., 2009)). Further analysis of the patients with HAM-D scores of 24 and above at baseline showed, as predicted, a more substantial effect. By contrast, patients with scores below 24 at entry simply showed too high a placebo response to allow detection of an effect of the active treatment in any of the individual studies. These findings give limited support for the use of lamotrigine as a monotherapy treatment for bipolar depression.
The addition of lamotrigine to lithium proved effective in bipolar depression in an independent European study (van der Loos et al., 2009; van der Loos et al., 2011). This combination would have the additional theoretical benefit of combining two drugs with positive long-term data and complementary polarity indices (Popovic et al., 2012; Popovic et al., 2014). Similarly, in the CEQUEL trial of depressed bipolar patients already taking quetiapine, addition of lamotrigine showed both an early effect on depressive symptoms compared with placebo and important benefits for remission, sustained to 1 year of follow (Geddes et al., 2015). Finally, an under-powered, open label comparison in treatment-resistant bipolar depression also suggested benefits as an add-on compared with risperidone and inositol (Nierenberg et al., 2006).
The CEQUEL trial included a folate 500 microgm/placebo comparison as a factorial addition. It was expected that folate might augment treatment effects, but in fact the converse was the case. Folate impaired the response to lamotrigine. This effect is noted here because folate is believed to be neutral or beneficial for mood, and widely used in pregnancy, of course. Negative effects on mood might be an important adverse reaction to patients taking lamotrigine. The known interaction of lamotrigine with the enzyme DHFR, makes it more likely that the effect is real (and would implicate this pathway in its mechanism of action).
In summary, lamotrigine has established acute efficacy both as a monotherapy and in combination with lithium and quetiapine. The acute findings are supported by relapse prevention studies (see below). While the need to titrate the dose might seem likely to delay its onset of action, this was not evident in the acute trial data. Nevertheless, the slow titration may be a consideration in monotherapy when speed of action is a priority. Its low burden of adverse reactions mean unblinding in RCTs was unlikely and risk of bias low.
The presence of a recent rapidly unstable mood or a mixed state may be a particular reason to consider lamotrigine (IV).
Lamotrigine is uncommonly a single first-line agent in bipolar I but it can be considered in bipolar II on the basis of limited positive evidence, including benefit in rapid cycling patients (Bowden et al., 1999).
Valproate
In a recent review and meta-analysis, four small studies support an effect of valproate in bipolar depression (Smith et al., 2010). This accords with relapse prevention data for depression (see below). A larger, more convincing study is required to establish acute efficacy.
Lithium in depression
Treatment guidelines (Sachs et al., 2000) have repeatedly suggested an overwhelming expert preference for the use of lithium as first line treatment rather than antidepressants. However, the actual evidence for acute efficacy of lithium in bipolar depression, either as a sole agent or in combination with others, is disappointing (II, ((Bhagwagar and Goodwin, 2002; Young et al., 2010)). Relapse prevention and anti-suicide effects are tangible benefits however (see below).
Dopamine agonists
The reported efficacy of cariprazine in controlled studies and the evidence for aripiprazole's efficacy in resistant depression suggests that dopamine agonism or partial agonism might be a potential mechanism of antidepressant action. The full agonist pramipexole has also been reported to show efficacy in small studies in treatment-resistant unipolar and bipolar depression (Dell'Osso and Ketter, 2013; Zarate et al., 2004). Adverse neurological reactions to dopamine agonists, well established in the treatment of Parkinson’s disease, include oro-facial and other dyskinesias and compulsive behaviours.
Modafinil
Modafinil has some antagonist affinity for the dopamine reuptake site and perhaps as a partial agonist at the dopamine D2 receptor. It elevates histamine concentrations in the brain. Its indication is as a wakefulness-promoting agent in narcolepsy, with additional clinical use in shift work sleep disorder and excessive daytime sleepiness associated with obstructive sleep apnea. It has also been studied as the R-enantiomer (armodafinil). In bipolar depression (and unipolar disorder) there is very limited evidence for efficacy (Goss et al., 2013).
Ketamine
There is considerable interest in the potential for ketamine, a NMDA (N-methyl-D-aspartate) receptor antagonist, to be an important addition to treatment options in major depression (Abdallah et al., 2015). This is particularly the case in relatively Treatment-resistant cases. However, there is only limited evidence in bipolar depression for efficacy of a single intravenous dose of ketamine (as add-on therapy to mood stabilizers), not for remission. Ketamine's psychotomimetic effects tend to compromise study blinding and no studies so far have tried to control for this. The use of ketamine and other bipolar modulators has been the subject of a Cochrane review. (http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD011611.pub2/epdf/standard). There are considerable uncertainties about how any acute benefit from ketamine, which is often clinically evident, can best be sustained. The obvious approach is to give repeat doses and to titrate response on an individual basis. The main concerns relate to the safety of repeat administration, which has not been systematically established. Ketamine is not widely available outside research centres in the UK.
Electro-convulsive therapy (ECT) and Vagal Nerve Stimulation (VNS)
ECT is effective in severe depression: the relevant trials will have included bipolar cases, although trials exclusively in bipolar disorder did not exist before one important review (I, (The UK ECT Review Group, 2003)) and remain rare. However, in a recent study, ECT proved superior to an evidence-based drug treatment algorithm in a RCT in treatment-resistant bipolar patients (Schoeyen et al., 2015), although full remission was not much improved by ECT.
ECT’s efficacy against both poles of bipolar disorder predicts it would be a reasonable choice for patients with mixed features (bipolar or unipolar). As noted above, an observational cohort study that described high rates of response and remission to ECT in bipolar patients with a DSM-IV-TR defined mixed state (Medda et al., 2015) has supported this conjecture.
Beliefs about ECT in the general population appear to remain influenced by unfavourable media portrayal (Lebensohn, 1999) and this has not diminished (IV). While clinicians have a responsibility not to pander to ignorance and prejudice, it may be helpful to allay fears that ECT is often used against the will of individual patients (S). In fact it is unusual for ECT to be used without a patient's consent, and under mental health legislation, even in services with a high utilization rate; even then, outcomes appear reassuring (Wheeldon et al., 1999).
VNS has limited support for use in treatment-resistant depression: there is no specific role identified in bipolar disorder (Shah et al., 2014).
The risk of a switch to mania during treatment of a depressive episode
One short-term outcome of treatment for depression is a switch to mania. This may occur as a consequence of illness course or because some treatments have a greater potential to cause switching than others. Of course, clinically there is an obvious gradient between patients with highly variable mood and those with a much more episodic pattern. There have been few efforts to differentiate the treatment responses along this gradient, except by reference to ‘rapid cycling’, which is an imprecise course specifier.
In a meta-analysis of patients without a previous history of mania, treatment with tricyclic antidepressants was twice as likely to result in a manic event as treatment with SSRIs or placebo (Peet, 1994)). In short-term bipolar treatment trials with antidepressants, switch rates were low but there was again a higher rate of switch for tricyclic antidepressants compared with other antidepressants (SSRIs in particular) (Gijsman et al., 2004). Fluoxetine plus olanzapine was effective in reducing depressive symptoms without provoking manic relapse (Tohen et al., 2003). However, a broader meta-analysis of the available data reached the pessimistic conclusion that drugs for unipolar depression may produce switching even in the presence of mood stabilizers, although the study could not exclude confounding effects as an alternative explanation (Tondo et al., 2010).
Venlafaxine may also increase the risk of switching patients, perhaps because of its action on serotonin and noradrenaline re-uptake. In the Stanley network study, patients treated with venlafaxine switched to mood elevation (defined as a YMRS rating over 13) in 31% of case, compared with sertraline (15%) and bupropion (14%): response rates were similar at around 50%, but there was no placebo control (Post et al., 2006). These rates are high which seems likely have been due to the inclusion of rapid cycling patients.
High quality naturalistic data has much to offer this question. Recent linkage of clinical data with prescribing data in Sweden suggested that monotherapy with drugs for unipolar depression is indeed associated with manic relapse in bipolar I patients, compared with combination with a mood stabilizer (Viktorin et al., 2014). There was no increase in the rate of manic relapse in patients taking lithium, valproate or carbamazepine. This employed a powerful within individual, longitudinal design to determine relative risk although patient numbers in the monotherapy group were small.
The naturalistic data, and clinical common sense suggest that a drug for mania in combination with the drug for depression may reduce the risk of a manic switch in depressed patients with a high risk of mania. The drug for mania could be lithium, valproate or a dopamine antagonist/partial agonist. The International Society for Bipolar Disorders (ISBD) consensus on the use of antidepressants in bipolar patients highlighted the clinical consensus discouraging their use in patients with rapid cycling, depressive episodes with mixed features and as monotherapy (Pacchiarotti et al., 2013).
Discontinuation of long-term treatment for depression
There is uncertainty about the value of long-term treatment with antidepressants, so it is frequently implied that early discontinuation is desirable ((Montgomery et al., 2000)). This has been echoed more dogmatically in recent NICE guidance. Absence of evidence is not evidence of absence, in this case, of short-term benefit (see also below). Indeed, the International Society for Bipolar Disorders Task Force report recommended to continue antidepressants over the long term in those who had had a relapse in depression after stopping antidepressants (Pacchiarotti et al., 2013).
Both the antimanic and the antidepressant medicines should be terminated together if the intention is that treatment should be simply for an acute episode. Discontinuation of an antidepressant should follow recommendations in related BAP guidelines and taper over 4 weeks if possible (Cleare et al., 2015). In particular, the possibility of adverse withdrawal effects should be discussed and reassurance offered.
Paradoxical manic episodes have been described during withdrawal of antidepressant drugs in patients with bipolar and unipolar depression (Narayan and Haddad, 2011).
In patients who do switch to mania during treatment, the antidepressant should be tapered and discontinued (consensus opinion).
Conclusions: the comparative efficacy and acceptability of different drugs for bipolar depression
NICE2014 used network meta-analysis to shape its recommendations. The analysis plan required a minimum sample size and handled each treatment separately. Most of the comparisons between treatments were indirect (via placebo). The conclusion was that six interventions were statistically superior to placebo (valproate>the combination of fluoxetine and olanzapine>lurasidone>quetiapine> olanzapine alone=lamotrigine). Other interventions that were included in the network but were not statistically superior to placebo were imipramine, lithium, moclobemide, paroxetine, and ziprasidone.
An independent approach to the same data combined the SSRIs and the tricyclic antidepressants for comparison with the better-studied treatments (Taylor et al., 2014). The exact order of the resulting ranks was different but not radically so. The question posed by this analysis is whether it can/should usefully inform clinical practice, since it depends so heavily on small studies and indirect comparisons. In discussion, our consensus group noted a number of contradictions. For example, SSRIs (which included paroxetine) ranked higher than quetiapine even though paroxetine was inferior to quetiapine in the only head-to-head trial (McElroy et al., 2010). In addition, venlafaxine was excluded from the analysis, because studies were not double blind, but appeared to have a relatively large effect (Vazquez et al., 2013). It was agreed that the limitations of the data prevented uncritical acceptance of final rankings, and new data might well change the outcome in the coming years. Nevertheless they provided a useful summary of where the field currently is, in all its weakness.
The most controversial issue was NICE2014’s endorsement of the use of fluoxetine, an antidepressant, with olanzapine. While this was a specific recommendation, there seems little reason not to regard fluoxetine as a representative SSRI. Therefore, to rank it first line is to rank SSRIs in general first line by extrapolation. In bipolar I patients antidepressants should then be prescribed only as an adjunct to anti-manic medications (not necessarily olanzapine, of course). Opinion was divided between those inclined to accept this extrapolation and those who feel strongly that the limited bipolar depression data is inconclusive as it stands. Currently it is not possible to resolve these opposing views. However, given that there are limited options to treat bipolar depression, the group concluded that it was reasonable to consider a trial of an antidepressant in a patient with bipolar depression if other treatments with a stronger evidence base were ineffective or not tolerated. The group noted that the ISBD international task force, in trying to balance the same opposite opinions, did not broadly endorse antidepressant use, but acknowledged the experience that individual bipolar patients may benefit nevertheless. The frequent current use of antidepressants appears not to be proportionate to the established benefit in bipolar I patients. Their role in bipolar II patients is equally controversial.
The group noted that quetiapine has an unusual weight of evidence to support its use in adults with bipolar depression and may have a unique combination of pharmacological actions which account for this. It therefore merits first line status. Olanzapine, and lurasidone, may also be considered as options, though neither is currently licensed in Europe to treat bipolar depression. Lurasidone appears to have a more favourable metabolic profile than either quetiapine or olanzapine (Leucht et al., 2013).
There is little evidence to guide next step treatment if the first choice fails. Before resorting to strategies derived from unipolar patients with treatment resistant depression, the options shown to be effective in bipolar depression should be exhausted first, perhaps in combination.
The use of aripiprazole can only be by extrapolation, given the failed trials in bipolar depression, but cariprazine, also a dopamine partial agonist, has now shown efficacy in two studies (Durgam et al., 2015a; Durgam et al., 2015b). This seems to support the pharmacological argument that dopamine agonism (or partial agonism) contributes to antidepressant action.
Dopamine antagonists should not be regarded as potential options for the treatment of bipolar depression in the absence of appropriate trials.
Finally, lamotrigine has supportive data for an acute effect, notably from two independent adjunctive studies, which together with longer term data, should make it a more widely used option. It appears currently to be under-used outside expert centres.
Unlike NICE2014, the group did not see evidence to support psychotherapy alone for the treatment of depression. NICE2014 made a distinction between primary and secondary care implying that there are mild cases of bipolar disorder that can be managed with psychological treatment alone. It may apply to young people with possible diagnoses of bipolarity, mild symptoms (and a good prognosis). However, the prominent endorsement of psychological treatments for bipolar disorder, without qualification, as ‘Key priorities for implementation’ goes well beyond the evidence. The partial way in which the data appears to have been reviewed by NICE2014 to justify their conclusions has also been highlighted (Jauhar et al., 2016).
3. Long-term treatment
Lithium remains the most effective treatment preventing relapse and admission to hospital in bipolar I disorder (I). Lithium should be considered for all patients with bipolar I disorder willing to take it reliably (S).
Lithium prevents relapse to mania and, less effectively, depression (I). The highest dose that produces minimal adverse reactions and effects should be employed. Concentrations below 0.6 mmol/l are potentially too low to be fully effective and adverse reactions and effects become important above 0.8 mmol/l. Lithium may be effective in a minority of patients as monotherapy (I).
Lithium reduces the risk of suicide (I).
Valproate as monotherapy has limited trial data, is somewhat less effective than lithium in the prevention of relapse and should not usually be considered for women of child bearing potential (I).
Carbamazepine as monotherapy is less effective than lithium, has little if any effect on relapse to depression and is liable to interfere with the metabolism of other drugs (I).
Lamotrigine is effective against depression in long-term treatment (I) and should be considered where depression is the major burden of the illness (IV).
Dopamine receptor antagonists and partial agonists reduce the risk or relapse and admission in long-term treatment (I). Relative effects on the manic and depressive poles of the illness appear to depend on the complex pharmacology of the drugs but may be predicted by acute treatment effects.
Antidepressants to which patients have shown an acute treatment response may, appropriately, be continued long term when the risk of a severe depressive relapse is high (III). In bipolar I disorder, they should be used in combination with a medicine that has long-term antimanic efficacy (II).
Discontinuation of long-term treatment is not indicated when there is good clinical control of the illness. When it is necessary, it should be tapered (IV). In the case of lithium there is a specific risk of manic relapse if it is discontinued within a two-week interval (I). Poor adherence is a contra-indication to lithium because of the risk of new illness episodes on discontinuation (I).
Key uncertainties
There is uncertainty in relation to the effects of short-term treatment on day-to-day or week-to-week mood stability.
Successful long-term management often appears to require combination treatment (III). Combination of lithium with valproate, or quetiapine with lithium or valproate is superior to monotherapy. At present there is little to guide practice other than safety concerns and pragmatic outcomes in individual cases.
The long-term value of antidepressants is not sufficiently established.
Extrapolation of long-term strategies for bipolar I disorder to bipolar II or the bipolar spectrum remains speculative.
Bipolar disorder tends to be a long-term, indeed, life-long challenge. At present the preferred strategy to prevent relapse is for continuous rather than intermittent treatment with oral medicines, to prevent new mood episodes. That means a negotiated decision to take one or more medicines for the long term – in effect, indefinitely. Such a decision is best made when patients are in remission, and ideally, the evidence for the efficacy and safety of any treatment should have been established over long periods of time. In practice, controlled data may cover much shorter periods of time, and for that reason NICE have been resistant to considering the data from such trials. As already explained, we take a more nuanced view, especially where practice can be supported by naturalistic data and clinical experience.
There is now good naturalistic data from Denmark that, for patients treated with lithium, starting early in the illness course is more often associated with a very good outcome than those starting later (Kessing et al., 2014). There is no RCT data to support the validity of this finding but its plausibility supports the intention to initiate treatment early in the bipolar illness course. However, the study illustrates the population challenge because under 20% of patients started on lithium early remained without relapse at 10 years follow up. Early relapse (within two years) was the rule.
The central problem is that, whatever the intention, adherence to long-term treatment appears to be poor (Kessing et al., 2007). To underline this point, about 40% of bipolar patients who commit suicide are not receiving long-term lithium or valproate (Clements et al., 2013). For this reason, early psychoeducation should receive high priority in clinical management. With rational psychopharmacology, it appears to work in practice to improve outcome (Kessing et al., 2013).
Medicines with putative efficacy against depressive and (hypo)manic relapse are sometimes described as mood stabilizers. We do not favour this terminology because it implies equal efficacy in the prevention of depression and mania (which is not seen with most drugs) and does not refer to a mechanism of action. In fact, the long-term use of a variety of agents alone or in combination may contribute to mood stability.
The management plan must incorporate additional flexible treatment when an acute stressor is imminent or present, early symptoms of relapse (especially insomnia) occur, or anxiety becomes prominent. Higher doses of long-term treatments or, perhaps more simply, short-term add-ons (e.g. GABA modulators) will be necessary. The focus will often be sleep disturbance, so the patient may keep a benzodiazepine or other hypnotic in small supply.
Dopamine antagonists/partial agonists may also be kept on hand with the doctor’s agreement, and, if taken at the onset of a manic episode, may reduce its severity. It may also be agreed that the patient can increase the doses of their other medicines under specific circumstances. This approach serves two purposes: the individual is more likely to comply with the treatment regimen if they feel they have greater control, and they can also take immediate action, when it may otherwise take too long to get an appointment with their psychiatrist.
Finally, if a patient has accepted treatment for several years and remains well, they should still be strongly advised to continue indefinitely, because the risks of relapse remain high. This can be concluded from the findings in several small studies of lithium responders. Even when lithium withdrawal was supervised and intended to be slow, relapse was much more common in the withdrawn group (Biel et al., 2007; Yazici et al., 2004). That said, patients may, of course, decide to discontinue long-term treatment. This may be most propitious when they have made a full recovery from their last episode, have had no bipolar episodes in the preceding four years, have no history of severe consequences from mania or bipolar depression and no previous history of cycling with many bipolar episodes. Naturalistic data certainly suggest that patients with residual symptoms have significantly worse outcomes, so drug discontinuation in a poor prognosis group would not be rational (Judd et al., 2008; Angst et al., 2003). Whatever the circumstances, short-term support and a management plan to recognise and treat early warning signs of mania or depression will be necessary.
Long-term treatment with Lithium
Lithium occupies a particularly important place in the management of bipolar I disorder. Thus, the strongest evidence among medicines that are often referred to as mood stabilisers for bipolar I disorder is still for lithium. Lithium certainly prevents relapse to mania and depression.
Adequate numbers of patients have been randomized into placebo-controlled short-term or ‘maintenance’ trials of lithium treatment dating from soon after its introduction (I, (Burgess et al., 2001)), and more recently when lithium has been a reference compound for other treatments (Severus et al., 2014). The relative risk of relapse on lithium over a year or more was 0.6 compared with placebo. So of 753 patients on lithium 258 (34%) relapsed; of 827 on placebo, 467 (56%) relapsed. That means in general that one would need to treat about 5 patients for about a year with lithium to avoid one relapse.
Considering relapse to either pole of the illness individually, there was a greater relative reduction in the risk of manic relapses (0.5) compared with depressive relapses for lithium (0.7-.8). In fact, on current evidence, lithium is only modestly effective in protecting against depressive relapse (Severus et al., 2014).
The largest study of lithium to date was a double-blind comparison of switching to lithium or placebo in patients who responded acutely to quetiapine (Weisler, 2014). A post hoc analysis suggested that a lithium level of 0.6 mmol/L or higher was more effective than lower doses for Li monotherapy maintenance in the prevention of relapse (Nolen and Weisler, 2013). There has been uncertainty over the years about whether single daily dosing is safer than more frequent dosing regimes. Twice daily, versus once daily dosing of lithium gives sustained higher minimum concentrations and this has been linked to more pathological renal changes on biopsy (and a higher risk of polyuria (Carter et al., 2013)). Given the advantage for adherence of once daily dosing, we recommend once daily night time dosing for lithium (IV).
Lithium concentrations in blood should be regularly monitored. How regularly is open to debate. This is problematic because failure to follow guidance may have legal implications for doctors. NICE2014 recommended measurement every 3 months for the first year of treatment and every 6 months thereafter (with a number of exceptions). Doctors should probably try to adhere to this recommendation. In reality, however, an annual check of all relevant blood indices is probably adequate in stable, physically healthy patients (McKnight et al., 2012). It is unclear whether the common failure to do any monitoring at all in some services is affected by what frequency is actually recommended.
Vigilance and increase monitoring is required when patients become physically ill or when they add medications with the potential to modify the clearance of lithium (non-steroidal anti-inflammatory drugs, for example).
Long-term treatment with anticonvulsants
There is no basis as yet for equating anticonvulsant action with ‘mood stabilization’, as has sometimes been claimed (Post et al., 1998). Anticonvulsants have a heterogeneous pharmacology and there is no evidence to suggest a class effect, such that anticonvulsants stabilize mood. Thus, valproate, carbamazepine, lamotrigine, gabapentin and topiramate are all anticonvulsants with different modes of action. In the case of the latter two compounds, there is almost no reliable evidence at all favouring their use either in acute mood episodes or to prevent relapse. Specifically, for gabapentin and topiramate controlled studies in acute mania were negative (gabapentin I, (Pande et al., 2000); topiramate I, (Kushner et al., 2006)). There remains some interest in using topiramate for weight reduction in obese bipolar patients (Chengappa et al., 2006).
Valproate
Valproate is often referred to, with lithium, as a mood stabilizer. Data on valproate are much more limited than that for lithium, however. The comparison with placebo is driven by a single RCT of valproate (as valproate semisodium, ®Depakote), which showed rates for all relapse of 24% against placebo at 38%. This suggests an absolute risk reduction of about 15%, numerically comparable with lithium (22%) but statistically non-significant. In fact the effect for depressive relapse was higher than for mania in this study (Cipriani et al., 2013c). The BALANCE trial specifically compared valproate, lithium and the combination in a randomized, non-blind maintenance study with a run in on the combination treatment to minimize drop-outs after randomization. Lithium alone and in combination with valproate was superior to valproate alone (Geddes et al., 2010). Nevertheless, observational data supports an effect for valproate not much less than lithium’s in practice
Carbamazepine
Carbamazepine was the first agent after lithium to be advocated for long-term treatment of bipolar disorder (II, review by (Okuma and Kishimoto, 1998)). It has been re-examined in two other trials, which showed a substantial benefit with lithium compared with carbamazepine in preventing relapse (I, (Greil et al., 1997; Hartong et al., 2003)).
Lamotrigine
Two maintenance trials of lamotrigine as monotherapy supported an effect against depression, not mania (I, (Goodwin et al., 2004)). The samples were enriched for lamotrigine responders, and compared lamotrigine, lithium and placebo. In one, the index episode was mania and, in the other, depression. The results from both trials are mutually supportive in showing an advantage for lamotrigine in the prophylaxis of depression. There was a comparable advantage to lithium for prophylaxis of mania. There was no excess of depressive episodes in lithium treated patients nor manic episodes in lamotrigine treated patients compared with placebo. Indeed for both agents there was a trend towards effects against the opposite pole of the illness. Thus, neither provoked mood instability to the opposite polarity. CEQUEL also demonstrated benefit over 12 months for combination treatment with lamotrigine (Geddes et al., 2015).
Long-term treatment with Dopamine antagonists/partial agonists
Dopamine antagonists/partial agonists have long been used in bipolar outpatients as long-term treatment. They have been prescribed for some patients in depot formulations, either as monotherapy or in combination with other agents. Before the development of the newer dopamine/serotonin antagonists and partial agonists, their use was poorly supported by formal evidence for patient benefit. There is a clinical impression that the newer agents offer advantages because they are less likely to produce dysphoria or provoke depressive relapse
Most of the newer, so-called second-generation dopamine antagonists/partial agonists have been studied in relapse prevention trial designs. Such studies enrich the study sample for acute responders to the drug of interest, and the active drug may be withdrawn abruptly, which risks amplifying any drug/placebo difference with withdrawal effects. This can be inferred from an excess of early relapses seen for example in a study of this design with olanzapine (Tohen et al., 2006). Therefore such studies, with occasional exception, primarily support short to medium-term use.
Use in the longer term is mainly an extrapolation, albeit supported by strong naturalistic data. Comparison of rates of hospital admission on and off treatment over four years, are strongly supportive of efficacy for lithium (Hazard Ratio (HR): 0.66, 95% CI: 0.62; 0.70), valproate (HR: 0.72, 95% CI: 0.67; 0.79), lamotrigine (HR: 0.79, 95% CI: 0.73; 0.84), olanzapine (HR: 0.77, 95% CI: 0.71; 0.82), and quetiapine (HR: 0.82, 95% CI: 0.75; 0.89)(Joas et al., 2016). Lithium, valproate, carbamazepine, olanzapine, and quetiapine (but not lamotrigine) treatment periods were associated with reduced rates of manic episodes. Lithium, valproate, lamotrigine, quetiapine, and olanzapine (but not carbamazepine) were associated with reduced rates of depressive episodes. Lithium only was associated with reduced rates of mixed episodes.
Olanzapine
Olanzapine has been studied as a comparator to depot risperidone and showed a reduction in manic and depressive relapse (Vieta et al., 2012). There was no enrichment for olanzapine responders so, notwithstanding a dropout rate of 40-50% over 18 months, this trial offers good evidence for patient benefit as a maintenance treatment. Olanzapine was also slightly superior to lithium as monotherapy after acute response to the combination of lithium with olanzapine but produced significant excess weight gain (Tohen et al., 2005; Zarate and Tohen, 2004). This study suggests that olanzapine prevents early manic relapse after lithium withdrawal, although the lithium dose was tapered over 4 weeks to prevent very early withdrawal effects.
Quetiapine
Quetiapine has been shown to be effective as monotherapy, and in combination with lithium or valproate (Suppes et al., 2009), in the prevention of relapse to either pole of the illness. These findings are consistent for patients entering treatment from either pole of the illness. The doses employed in trials were high (300-600mg/day) and in the monotherapy trial the median dose was 546mg/day (Weisler et al., 2011).
Lurasidone
Lurasidone may prove useful in bipolar depression (see above). Its long term use is supported by a relapse prevention study in which 28 weeks of continued treatment with adjunctive lurasidone was associated with a trend significant risk reduction in time to recurrence of any mood event compared with placebo plus lithium or valproate, and a significant reduction in time to recurrence of a depressive episode. Patients entered the study and were stabilized from either pole of the illness (Calabrese et al., 2015).
Aripiprazole, ziprasidone, paliperidone
Aripiprazole was more effective than placebo after acute and continuation treatment of mania: acute withdrawal of the aripiprazole did not produce an excess of early relapse in this study (Keck et al., 2007). Ziprasidone has positive adjunctive data (Bowden et al., 2010) and paliperidone only proved effective preventing mania (Berwaerts et al., 2012).
Dopamine antagonists/partial agonists may be appropriate for the long-term management of bipolar patients especially where non-mood congruent psychotic features are prominent.
Dopamine antagonists/partial agonists may be useful in difficult-to-treat cases of rapid cycling (III, e.g.(Lowe and Batchelor, 1986; Carvalho et al., 2014)). When added to usual treatment, principally with lithium or anticonvulsants, combination with clozapine was superior to usual treatment alone over one year in treatment–resistant bipolar patients including those with rapid cycling and mixed states (II, (Suppes et al., 1999)), but rapid cycling remains a major clinical challenge. Secondary analysis of the acute depression studies with quetiapine suggest efficacy in the short term for rapid cyclers (Vieta et al., 2007), but the real problem is long-term stability.
A small pilot study of vagal nerve stimulation is also compatible with some benefit in resistant rapid cycling patients, a very disabled group (Marangell et al., 2008).
Long acting dopamine antagonists
Various long-acting injectable (LAI) antipsychotics are available, including fluphenazine decanoate, haloperidol decanoate, olanzapine pamoate, risperidone microspheres, paliperidone palmitate, and aripiprazole monohydrate. Their primary indication is in the treatment of psychosis, but logically, LAIs could be used in bipolar patients where the treatment plan is continuation of treatment with dopamine antagonists, but adherence to oral medication is poor. Evidence to support their use in bipolar disorder is very limited (Bond et al., 2007; Gigante et al., 2012). The data for long-acting injectable risperidone is consistent in being positive for preventing mania, not depression (Quiroz et al., 2010; Vieta et al., 2012).
When switching from an oral drug to an LAI form, it is good practice to start with the oral antipsychotic for the length of time required to establish the effective, best tolerated dose before switching to the LAI form (Llorca et al., 2013).
Long-term treatment with antidepressants
Whether or not antidepressants should be used long term in bipolar disorder remains uncertain. One small maintenance study (II, (Prien et al., 1984)) has had an important influence because it suggested that the treatment of bipolar patients with imipramine alone resulted in an unacceptable number of manic relapses over a one to two year follow up period. This effect was prevented by co-treatment with lithium. It supports the recommendation that monotherapy with antidepressants is unwise in patients with bipolar I disorder.
Long-term treatment of bipolar I patients with antidepressants is common in clinical practice. Given the significant burden of disease imposed by chronic depressive symptoms and recurrent depressive episodes, this may not be surprising. The evidence supporting their use in the long-term prophylaxis of unipolar depression is strong (I, (Geddes et al., 2003)). The equivalent evidence for bipolar patients is almost non-existent. There is non-random evidence for successful short-term prophylaxis with antidepressants drugs in bipolar patients also receiving combination treatments such as lithium, valproate, carbamazepine and antipsychotics (Altshuler et al., 2001; Altshuler et al., 2003). But the patients in whom this is evident are about 10% of the total sample included. These and the few other relevant findings are far from compelling (Ghaemi et al., 2001; Pacchiarotti et al., 2013). Clinicians will have to use clinical judgement in deciding whether an individual patient should continue with an antidepressant
The uncontrolled and audit experience of using antidepressants is substantial, and, of course, applies to real clinical populations. As others have commented, some guidelines for the treatment of acute bipolar depression have gone too far in their proscription (Moller and Grunze, 2000).
Bipolar II patients and, in particular, patients with bipolar spectrum depression have not been sufficiently investigated. Anecdotally, it is possible that effective treatment with antidepressants is possible without an additional anti-manic drug (Parker et al., 2006). This is an area that merits further investigation, as the diagnostic issues become more widely understood.
The comparative efficacy and acceptability of different drugs for long-term treatment
Network meta-analysis of long-term treatments suggests comparable efficacy for most of the drugs described above (Miura et al., 2014). However, the value of the quantitative comparisons was limited by the design weaknesses already described. Lithium, olanzapine, quetiapine, risperidone LAI and valproate prevented manic relapse. Only lamotrigine, lithium and quetiapine were convincingly shown to prevent depressive relapse.
Long-term treatment: winning combinations
For perhaps too long, monotherapy with lithium was believed to be the best treatment for bipolar disorder. It was speculated in previous editions of this guideline that effective prevention of progression to frequent relapse or chronicity may require combination treatment from quite early in the illness course. Increasingly, combinations of agents are being prescribed for the majority of patients who fail on monotherapy. They will derive from apparently effective combinations used to control acute symptoms. Indeed
There is a strong evidence base to support the combination of a dopamine antagonist/partial agonist plus lithium or valproate to treat acute mania that has not responded adequately to lithium or valproate in monotherapy (Ogawa et al., 2014). However, there are only a limited number of studies that compare long-term monotherapy versus combination treatment.
Two RCTs have shown that, when acute mania or depression responds to the combination of quetiapine with valproate or lithium, then continuing the combination, versus switching to lithium/ valproate monotherapy, is associated with a lower rate of relapse of both depression and mania (Vieta et al., 2008; Suppes et al., 2009). For olanzapine (Tohen et al., 2004) and aripiprazole (Marcus et al., 2011), a single RCT has shown that, when the combination of either drug with lithium or valproate is effective in treating acute mania, then continuing the combination is associated with a lower risk of manic relapse than switching to lithium or valproate alone. The BALANCE study showed that over 2 years valproate monotherapy was inferior to both lithium monotherapy and valproate/ lithium combination in terms of total relapses (Geddes et al., 2010). However combination treatment, compared to monotherapy, carries a greater risk of medication side effects.
Maintenance ECT
Continuation and maintenance electroconvulsive therapy (ECT) is sometimes currently employed in patients who have failed pharmacotherapy but responded to an acute course of ECT. The evidence for this approach consists of case reports and retrospective chart reviews, with little focus on bipolar disorder per se (Frederikse et al., 2006; Petrides et al., 2011). There are supportive chart reviews for patients with bipolar disorder (Santos Pina et al., 2015).
Suicide
As a rule, suicide is associated with depression, and risk assessment should always be emphasized during acute episodes of depression in bipolar patients. Assessment of suicide risk should be as for other depression diagnoses and should follow widely accepted principles of good clinical practice (Hawton, 1987). Suicidality will often be related to illness severity and may guide the need for admission. Suicide in bipolar patients is a risk that persists across the lifespan.
There have been reports of suicidal acts in association with antidepressant treatment in younger people. Whether these are caused by antidepressants has been the subject of considerable hype, but appears unlikely (Gibbons et al., 2015). One speculation was that this might be more likely in undiagnosed bipolar depression. However, the onset of suicidality in bipolar patients was not associated with the use of antidepressants in the STEP-BD study, although the numbers were small (Bauer et al., 2006c).
Adverse reactions to long-term treatment
Weight gain is a major problem associated with the use of many of the medicines offered long term to bipolar patients (Torrent et al., 2008). The use of olanzapine and quetiapine is particularly associated with unfavourable metabolic indices, especially when the patient population is obese (Lieberman et al., 2005). Efforts are necessary to alert patients to the need both to maintain normal levels of exercise and moderate calorie intake. While this has traditionally been a cosmetic concern, strongly felt by patients, it has important medical implications particularly related to the risk of future cardiovascular disease (see BAP guideline on the management of weight gain and metabolic disturbances associated with psychosis and antipsychotic drug treatment).
A rise in serum prolactin caused by dopamine receptor antagonism, is a frequent and neglected problem (Pacchiarotti et al., 2015). It may lead to secondary hypogonadism (Howes et al., 2007) and low bone mineral density (BMD), the most important risk factor for osteoporotic fractures. Lifetime risk of such fractures for women in the general population is already high at approximately 50%. Decreased BMD and increased fracture risk have been shown in patients with severe mental illness (Howard et al., 2007; Meyer and Koro, 2004; Lehman and Meyer, 2005). Prolactin and gonadal function are hardly ever assessed in women on dopamine antagonists, BMD is not measured, and osteoporosis remains undiagnosed, let alone prevented or treated. All pre-menopausal women on amisulpride and most on risperidone (including at low doses) are at risk of amenorrhoea, low or undetectable oestradiol concentrations and many will also have low BMD. Hence, prevention and treatment of osteoporosis must become a target for improvement in physical health of potentially neglected populations of patients.
Tardive dyskinesia (TD) remains a concern for patients treated long term with dopamine antagonists/partial agonists (Keck et al., 2000). Acute EPS are still regarded as a predictor of subsequent TD, and are probably more common in bipolar patients (Gao et al., 2008). Hence the lower EPS associated with the use of the lower potency dopamine /serotonin antagonists and the use of the drugs like haloperidol at lower doses should reduce the long term risk. Current data on TD are supportive if not conclusive of much reduced risks with the newer agents (O'Brien, 2015).
Conclusions
Like NICE2014, the group highlighted the superior evidence base for lithium and the need for its advantages to be emphasized in training and practice.
In view of the long term problem of depressive symptoms in bipolar patients, the potential role of lamotrigine and its currently low rates of utilization in most NHS centres have been highlighted. In contrast, the common long-term use of antidepressants appears less easy to justify on the basis of the evidence.
NICE2014 was more restrictive in it recommendations for long-term treatment with dopamine antagonists/partial agonists (Table 7). Naturalistic data supports a broad range of efficacy for these medicines. Moreover, in an individual patient, if a medicine leads to prompt remission from the most recent manic or depressive episode, this may be considered evidence favouring long-term use as monotherapy (IV). Because effective in the short term, this may lead to their preferential use; active consideration of lithium as a better alternative should be promoted.
Table 7. Comparison with NICE guidelines: long-term treatment.
| NICE | BAP |
|---|---|
| Offer lithium as a first-line | Consider lithium as first line treatment in adherent patients |
| If lithium is ineffective, consider adding valproate | If lithium alone is ineffective consider combination treatment (depression predominant: ADD lamotrigine, quetiapine or lurasidone to lithium; mania predominant: ADD valproate or a dopamine antagonist/partial agonist to lithium) |
| if lithium is poorly tolerated or unsuitable, consider valproate or olanzapine or (if acutely effective) quetiapine | If lithium is poorly tolerated or unsuitable, consider other options: valproate, dopamine antagonists/partial agonists |
| Consider lamotrigine as monotherapy in bipolar II disorder when depression is the major burden | |
| Within 4 weeks of resolution of symptoms, discuss …. whether to continue psychological or pharmacological treatment for bipolar depression or start long-term treatment | Consider the strategy for long-term treatment as patient recovers |
However, the greatest challenge is the early adoption of a long-term treatment strategy acceptable to patient and family. The complex need for access to a responsive and intelligent clinical service, psychoeducation and relevant behavioural change, adherence to prescribed medicines and informed prescribing is difficult to meet within current services for too many patients.
Specific Psychological interventions for relapse prevention in bipolar disorder
Psychoeducation is the preferred or ‘first line’ psychological intervention.
Uncritical endorsement of CBT as a generic method for relapse prevention in bipolar disorder is not justified.
In general, psychological interventions appear to demonstrate efficacy most convincingly with patients early in their illness course.
Key uncertainties
Whether psychological interventions can be modified to be efficacious in patients with many previous episodes.
Efficacy and feasibility of on line psychological intervention
Group and individual Psychoeducation
As already indicated, we recommend psychoeducation as the preferred or first line psychological intervention.
Cognitive behaviour therapy (CBT)
While bipolar patients share many of the common cognitive distortions and attitudes described in unipolar patients (II, (Scott et al., 2000)), a cognitive model is not convincing as a complete theory of the illness. Nevertheless, cognitive theories can fruitfully address some specific problems bipolar patients bring to treatment. Therapy derives pragmatically from clinical experience with bipolar patients (review by (Scott, 1996)). A preliminary trial in 42 subjects suggested that CBT could speed recovery from depression and prevents the cascade of isolated manic symptoms into full-blown episodes (Scott et al., 2001). A formal trial of CBT for currently euthymic bipolar patients produced important reductions in rates of syndromal relapse, depression symptom reduction, less mania symptom fluctuation and higher social functioning over a one-year period compared with treatment as usual (Lam et al., 2003). The study targeted patients who had taken mood stabilisers and were still suffering from frequent relapses. Compared with treatment as usual, such enhancement of clinical care appeared to be helpful. Treatment included components of education, motivation to take medicines reliably, self-monitoring, active relapse prevention measures and problem solving. Action plans and modification of behaviours often do not depend solely on the patient to recognize abnormal mood states. Disappointingly, the findings from the Lam study were not replicated in a larger, more pragmatic CBT study, which showed no benefit at all for a large sample of patients versus treatment as usual (Scott et al., 2006). A secondary analysis suggested that patients earlier in their illness course were slightly more likely to show benefit – as for psychoeducation (see below). Pilot data in an early onset group also weakly support this conclusion (Jones et al., 2015b). Negative findings for CBT include evidence for equivalence to a cheaper group psychoeducational approach (Parikh et al., 2012) and a simpler supportive individual approach (Meyer and Hautzinger, 2012).
Resources for complex psychotherapy are always likely to be limited and provision should be focused on those patients most likely to benefit. Patients with particularly severe personal and social disturbance early in their illness course should probably be given priority access. Uncritical endorsement of CBT as a generic method for relapse prevention in bipolar disorder is not justified.
Interpersonal and social rhythm therapy (IPSRT)
The principles of IPSRT derive from interpersonal therapy (IPT), which has never itself been studied in bipolar patients (Frank et al., 2000). It places a particular emphasis on preserving sleep and regular daily activities. A comparison of IPSRT with ‘intensive clinical management’ suggested benefit from this approach. Patients assigned to IPSRT in the acute treatment phase developed greater regularity of social rhythms at the end of acute treatment and survived longer without a new affective episode over 2 year follow up (Frank et al., 2005). IPSRT is of particular interest because it has obvious potential to be adapted for automatic monitoring and feedback of diurnal activity from mobile phone apps (Nicholas et al., 2015). If it works, a personalized approach to IPSRT-derived self management could be made widely available and integrated into clinical care.
Family/Caregivers interventions
Family interventions are effective in the short and long-term treatment of bipolar disorder (Miklowitz et al 2008; Reinares et al, 2008), although not all patients are candidates to those treatments. They are mostly based on psychoeducational and CBT paradigms with some extra emphasis on expressed emotions. Involvement of family members is clearly of most value in younger patients. The key components are psychoeducation about bipolar disorder, communication skills training and problem solving skills training.
Cognitive and functional remediation
Even those patients who achieve full clinical remission present, in many cases, with long-term cognitive problems and social dislocation. Cognitive and functional remediation, as prescribed in group format (Vieta et al., 2014), may be helpful to improve global as well as interpersonal and occupational functioning (Torrent et al., 2013).
Further work is required to determine whether there are real differences between therapies and whether simpler interventions are worthwhile. The provision of greatly increased levels of psychotherapy to vulnerable patients is not without its risks, most notably of sexual or financial exploitation by the therapist (Nutt and Sharpe, 2008). The disinhibition of bipolar patients in a manic state poses a particular hazard.
Comparison with NICE guidelines: specific psychological treatments
The primary focus of the BAP guideline is a balanced recommendation for the use of medicines in the context of a coherent and integrated psychoeducational framework. The consensus around the common elements of promising psychological interventions seems more convincing than specific therapies, and more immediately applicable through a broadly understood goal of psychoeducation for all patients.
NICE2014 made more specific recommendations for psychological treatment of bipolar depressive episodes:
‘a psychological intervention that has been developed specifically for bipolar disorder and has a published evidence-based manual describing how it should be delivered or a high-intensity psychological intervention (cognitive behavioural therapy, interpersonal therapy or behavioural couples therapy) in line with the NICE clinical guideline on depression.’
We are not convinced that extrapolation from unipolar depression is justified (IV).
4. Treatment of alcohol and substance use disorder
The commonest co-morbidity of bipolar disorder is alcohol or substance use disorder. Patients appear more likely to present with dysphoric manic states and so bipolar disorder should be considered in the differential diagnosis of such presentations. The co-morbidity is often present at the first episode.
It is now a clinical consensus that alcohol and substance use co-morbidity should not be seen as a secondary phenomenon that will remit with treatment of the bipolar disorder. The treatment of alcohol and substance use disorder should be planned in its own right. Contemporary approaches are summarized in another BAP guideline and will not be repeated at length here.
Thus, we support NICE’s recommendation to ‘Discuss the use of alcohol, tobacco, prescription and non-prescription medication and illicit drugs with the person, and their carer if appropriate. Explain the possible interference of these substances with the therapeutic effects of prescribed medication and psychological interventions.’
It will be helpful to clarify the treatment target choosing from among assisted withdrawal, reduction, relapse prevention or maintenance of controlled drinking. In very heavy drinkers, even modest reductions in consumption will significantly reduce the potential physical harms.
As described in full in the BAP guideline, naltrexone or nalmefene may help patients to reduce their alcohol consumption (III). Acamprosate should be offered if naltrexone has not been effective (IV). Disulfiram may be considered if the patient wants abstinence and acamprosate and naltrexone have failed. The patient must be able to understand the risks of taking disulfiram and have their mood monitored (IV).
It may be helpful also to specify caffeine use and treat its reduction as a valid target in sensitive patients.
There is a paucity of studies on which to shape a specific approach to treatment of bipolar disorder in patients with alcohol or substance use disorder. One small trial in a relevant population supports the combination of valproate with lithium rather than lithium alone (Kemp et al., 2009).
5. Treatment of borderline personality disorder
There is very limited evidence on the treatment of borderline personality disorder especially when co-morbid with bipolar disorder. The NICE guideline on borderline personality disorder (https://www.nice.org.uk/guidance/cg78) understandably addresses the stigmatization and barriers to treatment of this patient group. However, it is dogmatic about the use of medication: ‘1.3.5.1 Drug treatment should not be used specifically for borderline personality disorder or for the individual symptoms or behaviour associated with the disorder (for example, repeated self-harm, marked emotional instability, risk-taking behaviour and transient psychotic symptoms).’ And ‘1.3.5.6 Review the treatment of people with borderline personality disorder who do not have a diagnosed comorbid mental or physical illness and who are currently being prescribed drugs, with the aim of reducing and stopping unnecessary drug treatment.’
Despite these recommendations, patients with borderline symptoms are not uncommonly offered medication in part as an extrapolation from practice in bipolar patients or as treatment for depression. Such practice is supported by poor quality studies of lamotrigine, lithium, olanzapine, risperidone, aripiprazole and quetiapine, which suggest some symptomatic benefit in borderline samples (III, (Lieb et al., 2010)).
The data from patients co-morbid for borderline and bipolar disorders, again very limited, also suggest improvement from lamotrigine and valproate on borderline symptoms (Frankenburg and Zanarini, 2002; Preston et al., 2004). In the lamotrigine study this appeared to be associated with, and so perhaps secondary to, improved control of bipolar symptoms.
There are four approaches to psychological treatment of borderline personality; two are considered psychodynamic in nature: mentalization-based treatment and transference-focused psychotherapy. The other two are considered to be cognitive-behavioral in nature: dialectical behavioral therapy and schema-focused therapy (Zanarini, 2009). They have been investigated in poor quality clinical trials (III or less). In terms of an evidence base, there is less to choose between medication and psychological treatment than the NICE guidance suggests.
While the NICE borderline guideline acknowledges in passing that the condition is commonly co-morbid with bipolar disorder, and implicitly acknowledges that its treatment should continue, this probably needs emphasis so as to avoid a polarizing approach in the services caring for patients with borderline problems. In fact NHS audit suggests that borderline patients with bipolar disorder usually do receive appropriate medication as much as 80% of the time (Paton et al., 2015).
6. Treatment of anxiety
The NICE Bipolar disorder clinical guideline (185: 2014. p. 108) states
“Offer people with bipolar disorder and coexisting disorders, such as personality disorder, attention deficit hyperactivity disorder, anxiety disorders or substance misuse, treatment in line with the relevant NICE clinical guideline, in addition to their treatment for bipolar disorder”….” be alert to the potential for drug interactions and use clinical judgement.” We recommend the corresponding BAP guidelines for attention deficit hyperactivity disorder (Bolea-Alamanac et al., 2014), anxiety disorders (Baldwin et al., 2014) or substance misuse (Lingford-Hughes et al., 2012).
Anxiety disorders should be routinely assessed alongside mood symptoms in patients with bipolar disorder. The anxiety co-morbidity in bipolar disorder is widely distributed: approximate proportions are social anxiety (22%), generalised anxiety disorder (18%), post-traumatic stress disorder (17%), panic disorder with / without agoraphobia (17%), obsessive compulsive disorder (10%), and agoraphobia without panic (9%) (McIntyre et al., 2006). The NICE and BAP guidelines for these primary anxiety disorders detail the specific pharmacological approaches. In bipolar patients there is need for caution in the use of dual action monoamine re-uptake inhibitors such as venlafaxine and duloxetine because of the risk of switch to mania: pregabalin may have advantages because of its mode of action (via calcium channels, not GABA receptors as its structure and name might lead one to expect). Specific anxiety-focussed psychological treatment – such as trauma-focussed CBT and CBT for social anxiety- are recommended rather than ‘generic CBT’. In general effect sizes for drug treatment of anxiety disorders appear to be greater than for psychological treatments (Bandelow et al., 2015).
Psychological treatments do potentially offer adjunctive approaches for addressing anxiety in bipolar disorder where anxiety-specific medication is contra-indicated and/or in line with a patient’s preference. However, bipolar disorder is typically an exclusion criterion in the trials of psychological treatments so such recommendations represent extrapolation. Moreover, only 22 psychological treatment studies had been published by 2014 with an anxiety-related outcome measure in adults with bipolar disorders (Stratford et al., 2015). Thus, few psychological treatment studies have explicitly targeted anxiety, since historically depression has been the focus. Stratford et al conclude that preliminary data are promising for CBT for post-traumatic stress disorder and generalised anxiety disorder in bipolar disorders. There was no evidence that psychoeducation alone reduced anxiety. There is early evidence that when cognitive behavioural therapy (CBT) incorporated an anxiety treatment component, anxiety symptoms were reduced in cyclothymia, “refractory” and rapid cycling bipolar disorder, whereas standard bipolar CBT treatments had only a modest effect on anxiety. CBT during euthymic phases had the greatest weight of evidence, although still there is only relatively weak evidence and for limited benefit. The preliminary evidence for mindfulness-based cognitive therapy was mixed. Where reported, psychological therapy appeared acceptable and safe, but more systematic collection and reporting of safety and acceptability information is needed.
Development of specific psychological models and treatment protocols for anxiety in bipolar disorders may help improve outcomes. However, separate parallel approaches to bipolar patients with different anxiety disorders will be unwieldy and restrictive. A current theme is that ‘bipolar anxiety’ is perceived to be a common clinical problem even if its intensity and structure do not make an anxiety diagnosis. Moreover, anxiety symptoms can be argued to have many core features across anxiety diagnoses. The challenge is how to develop such a generic approach for bipolar patients. One proposal is to take a highly patient-led approach based on qualitative interview and patient experience (Jones et al., 2013) from which, if effective, generalizability may be difficult. A more mechanistic approach might identify specific psychological treatment components responsible for reducing anxiety in bipolar disorder, like the intensity of imagery (i.e. experience like perception in the absence of a percept, such as intrusive images of traumatic events, or images of performing badly in a social situation, relevant to PTSD / social anxiety respectively) (Holmes et al., 2008; Holmes et al., 2011). Anxiety requires treatment in its own right, and since anxiety may exacerbate other mood symptoms, its treatment may contribute to overall improved mood stability. There is wide consensus that research and development is required (Mitchell, 2015).
As discussed above, in youth prodromes the earliest symptoms may be anxiety (NICE 2014 p. 91). Further research is especially warranted for prodromal phases and youth populations in which anxiety is prominent. We agree with the NICE guidelines 2014 (p. 304) “it is important to know the form of psychological therapy that can benefit young people with bipolar disorder”. Evidence-based psychological therapy - even for example within CBT - takes disorder-specific forms and may need to be targeted to bipolar specific features as well delivered in forms acceptable to youth.
There is a widely perceived need for closer integration between psychological and pharmacological approaches, with psychological intervention a potential adjunctive treatment for anxiety in the context of long-term maintenance pharmacotherapy for mood symptoms. The NICE clinical guideline 185: 2014. p. 264: suggests that psychological therapists applying anxiety (or depression) treatment protocol to bipolar disorder “should have experience of bipolar”. Further work needs to be done on standards of training and gaining experience of this clinical group. Reading these BAP guidelines should be part of this (see comment above in Scope of this Guidance). In addition it is recommended that psychological therapists and those prescribing maintain and active clinical links when working with the same patient.
7. Treatment in special situations
Children and young adults
In previous versions of this guideline there was little attempt to make specific recommendations for children and young people, so one inference could have been that treatment options for this group should be extrapolated from adult data. One worry has been such extrapolation to children falsely diagnosed with ‘bipolar disorder’. In the absence of independent evidence of benefit and from appropriate trials in such children, the extrapolation could not be encouraged. A more conservative consensus about diagnosis has emerged and there has been some increase in information available since the last edition on both efficacy and adverse reactions. Most new studies were conducted in the USA and will have included patients with broadly defined bipolar disorder, so the diagnosis of mania may have had limited validity. There are studies showing advantages compared with placebo of aripiprazole, olanzapine, quetiapine, risperidone (and ziprasidone) and further evidence that effect sizes for these medicines is greater than lithium or valproate (Correll et al., 2010). Adverse effects on weight were very prominent for olanzapine, quetiapine and risperidone (in descending order of harm). Aripiprazole, lithium and valproate were better (Singh et al., 2010).
Currently only aripiprazole (for 12 weeks) and lithium are licensed for treatment of mania in the UK (children of 12 years and older).
Medications approved by the U.S. Food and Drug Administration (FDA) to treat youth with bipolar disorder are risperidone, aripiprazole, quetiapine and olanzapine. Specifically, ‘short-term treatment with risperidone can help reduce symptoms of mania or mixed mania in children ages 10 and up. Some research has indicated that risperidone is more effective in treating mania in young children than other medications. Aripiprazole and quetiapine are approved to treat mania symptoms in children 10–17 years old who have bipolar I, while olanzapine is approved for use in children ages 13–17.’ (http://www.nimh.nih.gov/health/publications/bipolar-disorder-in-children-and-adolescents/index.shtml#pub7).
Empirical data on the treatment of bipolar depression in children and young people are scarce. Thus, no trials of SSRIs have been conducted in bipolar depression, a study of quetiapine did not separate from placebo and there is only low quality evidence from open trials for lithium (Patel et al., 2006) and lamotrigine (Chang et al., 2006).
NICE suggested a structured psychological intervention (individual cognitive behavioural therapy or interpersonal therapy) of at least 3 months’ duration for bipolar depression. This is a simple extrapolation from unipolar practice. Child and adolescent mental health professionals usually take a family-based approach (in the sense of non-specific support and psychoeducation) and we note a further need to support the education of these patients because manic episodes are easily misunderstood.
Most of the trial data in young people come from family therapy or multi-family psychoeducation groups with a focus on relapse prevention so a more balanced view of this alternative would be appropriate. Family focussed psychotherapy is currently the most relevant manualized approach to the problem (Miklowitz, 2015; Vallarino et al., 2015).
The recommendation to treat co-morbidities in accordance with other guidelines could imply additional treatment approaches. An integrated treatment that addresses multiple presentations of the illness may be more relevant in young people (IV).
For bipolar depression that is moderate to severe, we would consider a pharmacological intervention that follows the recommendations for pharmacological interventions for adults with appropriate consideration of dosing and potential harms.
Elderly patients
Patients with bipolar disorder grow old, and older people may develop bipolar disorder de novo. Indeed, up to 10% of individuals develop bipolar disorder over the age of 50, an increasing number as population longevity increases (Sajatovic, 2002). Treatment follows the same principles as for other patient groups, although few studies have been directed specifically at the elderly. As a group they are more susceptible to adverse reactions, owing increased end-organ sensitivity, impaired circulation, and reduced hepatic and renal clearance. This may be especially the case with lithium (Sproule et al., 2000). In general treatment doses are lower than those used in younger adults and should be more carefully titrated (Naranjo et al., 1995).
Bipolar disorder and pregnancy
Bipolar patients may wish to get pregnant. Some psychotropic medicines may reduce fertility. Thus, an increased incidence of polycystic ovarian syndrome (Joffe, 2007), putatively associated with valproate use, may reduce fertility but be reversible on stopping medication. Some dopamine antagonists may impair ovulation by causing hyperprolactinaemia and disruption of the hypothalamic-gonadal axis. Conversely, switching to a prolactin-sparing dopamine antagonist/partial agonist may cause return of fertility and unplanned pregnancy. Carbamazepine reduces the effectiveness of oral contraceptives (OC) by enzyme induction: double dosing of the OC is one practical solution.
Risks of discontinuation of medication
There appears to be a high probability that women who are taking lithium and become pregnant will discontinue it. The figure from the UK Health Improvement Network primary care database was almost 70% by the 6th week of pregnancy. There is a high risk of relapse in affective disorder if medication is discontinued. Thus, 52% of women who discontinued lithium during pregnancy relapsed and 70% of the women who remained stable after lithium discontinuation during pregnancy relapsed in the post-partum period (Meyer and Koro, 2004; Viguera et al., 2000). A systematic review of over 4000 women with bipolar disorder or post-partum psychosis confirmed that postpartum relapse rates were significantly higher among those who were medication free during pregnancy (66%, 95% CI=57, 75) than those who used prophylactic medication (23%, 95% CI=14, 37) (Wesseloo et al., 2015). Risk of post-partum illness is especially high in women with a history of previous post-partum psychosis. Treatment may involve exposure to higher doses of psychotropic medicines than would be implied by long-term maintenance treatment. Maternal depression has a negative effect on child development (Rice et al., 2007).
Risk of medication harms
The risk of major congenital malformations in the general population is surprisingly high at 2–4% and increases with maternal age. Cohort studies have shown that the risk increases to 11% in valproate-exposed babies (II, (Kaneko et al., 1999)), and 6% in those exposed to carbamazepine (II(Rosa, 1991)), and these risks are usually unacceptable. Of course, the great majority of women who conceive while taking either drug will still deliver a normal baby. Carbamazepine and valproate are associated with a range of congenital abnormalities, including neural tube defects (incidence 1% with carbamazepine and 1–2% with valproate (Omtzigt et al., 1992)) and the fetal hydantoin syndrome (facial dysmorphophobia, cleft lip and palate, cardiac defects, digital hypoplasia, and nail dysplasia), which was originally described with phenytoin. The risk of congenital abnormalities is dose related with valproate (blood concentrations over 70 micrograms/ml are implicated) and increases with the number of antiepileptic agents prescribed (II, (Samren et al., 1999)). Valproate has been particularly singled out for concern because of apparently higher risks of developmental impairments when compared with women taking other anticonvulsants (for epilepsy) (see https://www.gov.uk/drug-safety-update/medicines-related-to-valproate-risk-of-abnormal-pregnancy-outcomes). The problems describe include lowered IQ and development disorders.
Lamotrigine appears not to increase the risk of foetal malformation in the epilepsy population (Vajda et al., 2014).
Lithium’s potential teratogenicity remains less well characterized, because it is a less common prescription (and is probably often avoided in pregnancy). In the past, lithium’s ‘specific association’ with Ebstein’s anomaly was believed to represent a high risk. But recent analysis suggests that first trimester exposure to lithium is actually associated with a 0.05–0.1% risk of cardiovascular anomalies (a low absolute risk but perhaps still higher than in the general population) (I, (Cohen et al., 1994)). Some studies are still interpreted to justify echocardiography to check for cardiac problems in exposed babies (Diav-Citrin et al., 2014). However, studies have never been large enough (and so included too few cases) to be decisive (McKnight et al., 2012).
Many of the risks for bipolar patients may be unavoidable, because population figures of 30% are given for unplanned pregnancy, and this rate may be higher again in patients with mania. Most of the danger for organ development is in the first two months, which may be before a woman is aware that she is pregnant. Consequently, all female patients of childbearing age should be advised about the importance of effective contraception (II, (Smith and Whitfield, 1995)). Pregnancy should be planned in consultation with the psychiatrist and should include a full explanation of the treatment options and their benefit to harm balance. Treatment options include continuing the existing medication throughout pregnancy, switching to alternative medicines associated with lower foetal risk before conception, withdrawing some or all medication before conception, and reintroducing it either after the first trimester or immediately after birth. The chosen option will depend on the patient’s past history, response to treatment and the patient’s and clinician’s preferences. If lithium or valproate is continued during pregnancy, prescribing slow-release formulations twice or more times daily can minimize high peak concentrations. Some authorities consider withdrawal or reduction of lithium before (planned) delivery and re-establishing the original dose as before pregnancy immediately after delivery (see NICE2014).
Patients who take lithium, valproate, or carbamazepine during the first trimester should be advised about prenatal diagnosis and offered maternal alpha-fetoprotein screening and a high resolution ultrasound scan at 16–18 weeks gestation. Folate supplementation is advised for all pregnant women, but it is unclear whether this reduces the increased risk of neural tube defects associated with carbamazepine and valproate.
Maternal physiological changes during pregnancy may necessitate dosage adjustments. For example the glomerular filtration rate increases during pregnancy, causing many medications to be excreted more rapidly. As a result serum concentrations may fall and the mother may require higher doses to prevent a relapse. After birth these changes reverse and there is a risk that higher serum concentrations will results in adverse reactions, unless doses are reduced. These issues are most relevant to lithium, given its low therapeutic index.
ECT can be administered to pregnant women without immediate adverse reactions or effects but primary data is very sparse and confounding prevents any comment about the safety for the unborn child (Leiknes et al., 2015).
Neurotoxicity of maternal psychotropic medication after birth
In patients who have taken medicines up to childbirth, both toxic effects and withdrawal effects have been described in clinical case reports/series, although proving causality is often difficult (Ebbesen et al., 2000). Vigilance in caring for babies of mothers taking psychotropic agents is recommended. Pre-term babies are at particular risk if breast-fed due to reduced hepatic capacity. Benzodiazepines may depress neonatal respiration or cause drowsiness, hypotonia, or withdrawal symptoms. Dopamine antagonists/partial agonists can cause EPS. Tricyclics can cause urinary retention and functional bowel obstruction. Lithium has been associated with goitre, hypotonia, and cyanosis. Carbamazepine has caused neonatal bleeding and is an indication for prophylactic vitamin K.
In the case of antidepressants, which are prescribed in as many as 6.5% of women delivering babies, revised class labelling has emphasized an increased risk of jitteriness, poor feeding, crying, and seizures. The mechanisms are unclear but are clearly attributable to toxicity, withdrawal, or a combination of factors (Haddad et al., 2005). Discontinuation in pregnancy, or a switch to fluoxetine, whose long half-life may reduce withdrawal effects, are management options.
Breastfeeding requires an understanding by patients of the potential risks of toxicity to the neonate and the need for vigilance in their care. All maternal drugs enter breast milk, but the ratio between infant and maternal plasma concentrations varies greatly. The rate of adverse reactions attributable to maternal psychotropic medicines is most uncertain and depends on sporadic reports of, for example, toxicity due to lithium, hepatic dysfunction due to carbamazepine, and thrombocytopenia or anaemia attributed to valproate. These risks need to be balanced against the benefits of breast feeding (I, (Austin and Mitchell, 1998)). Owing to its narrow therapeutic index lithium is generally regarded as being a relative contraindication to breast feeding (I, (Chaudron and Jefferson, 2000)) because it is present in breast milk at 40% of the maternal serum concentration (American Academy of Paediatrics Committee on Drugs, 2000).
In general, the risks to the infant are the same as those for any patient exposed to the medicine, so clozapine is usually regarded as contraindicated because of the risk of agranulocytosis. Lamotrigine will carry the possibility of rash. Antidepressants are usually present in breast milk in low concentration but there is large individual variation and some infants have developed plasma concentrations higher than maternal plasma concentrations. Abrupt withdrawal of sertraline may have caused neonatal withdrawal effects.
The BUMPS website provides a useful resource for clinical staff and pregnant mothers themselves concerned about the use of medicines: http://medicinesinpregnancy.org. NICE have revised their guidelines for antenatal and postnatal mental health (http://www.nice.org.uk/guidance/cg192).
Bottle feeding
A pragmatic alternative to breastfeeding is bottle feeding. This obviously avoids concerns about drugs in breast milk and means adherence to drug treatment may be more likely. It also has the advantage that responsibility for night feeds may be shared. This may in turn protect against the deleterious impact of sleep deprivation on bipolar mood at a critical time for mother and infant. Unfortunately, patients may encounter an over-zealous approach to breast-feeding advice which assumes they ought to do so. Common sense may well dictate otherwise and women should feel confident to make an informed decision that suits them (IV).
The risk of relapse
Childbirth increases the risk of relapse in patients with bipolar I disorder in the post-partum period (Robertson et al., 2005). In fact, this effect is most striking in first babies and for first psychiatric admissions (I, (Terp and Mortensen, 1998)). The potential benefits of adherence to long-term treatment for a mother with bipolar affective disorder are to remain free of symptoms, enjoy normal bonding with her child, and facilitate neonatal development. Failure to control symptoms will risk harm to the mother/child relationship directly or via co-morbid alcohol, drug, and nicotine consumption. Against the benefits there are some risks. These include teratogenesis, neonatal adverse reactions that may reflect drug toxicity, and withdrawal effects.
Patients with bipolar II disorder are at an increased risk of mood episodes in general (and during pregnancy) but not particularly in the post-partum periods. A history of child-hood sexual abuse is associated with an increased risk of post-partum depression (Robertson et al., 2005).
Suicide is a major cause of maternal death in developed countries (Oates, 2003) and is sometimes associated with infanticide. It is a sombre note on which to conclude, but perhaps helps underline just how fatal a disease bipolar disorder sometimes is.
Annex: Additional information about medicines
Table 3. Treatment of different phases of bipolar illness: summary and grade.
NMA: Network meta-analysis
| Phase of illness | Modality and Format | Underlying methodology | Recommended Treatments | GRADE |
|---|---|---|---|---|
| Manic episode | Medication: hierarchy of effective treatments | Coherent plausible NMA; RCTs | Dopamine antagonists, valproate, lithium | **** |
| Depressive episode | Medication: choice of alternative treatments (NMA not likely to be stable) | Downgraded RCTs (risk of unblinding) | Quetiapine | *** |
| Downgraded RCTs (small size) | Olanzapine, Olanzapine plus fluoxetine Antidepressants | *** | ||
| RCTs | Lurasidone Lamotrigine as combination | **** | ||
| Psychotherapy (as add on to medication) | Downgraded RCTs | FFT, CBT, ISPT | ** | |
| Psychotherapy alone | Extrapolation from unipolar depression | CBT | * | |
| Long term | Medication: hierarchy of effective treatments (NMA supportive not decisive) | RCTs; double upgraded observational studies | Lithium (Mania, depression, suicide) | **** |
| Downgraded RCTs; double upgraded observational studies | Dopamine antagonists and partial agonists,, valproate (mainly mania) | **** | ||
| RCTs; double upgraded observational studies | Lamotrigine (depression) | **** | ||
| Psychotherapy (as add on to medication) | RCTs | PsychoeducationFFT | **** | |
| Downgraded RCTs | CBT, IPSRT | ** |
Table 6. Comparison with NICE guidelines: bipolar depression.
| NICE2014 | BAP |
|---|---|
| Offer fluoxetine combined with Olanzapine (OFC), or quetiapine monotherapy. | Consider quetiapine, lurasidone or olanzapine monotherapy |
| Consider either olanzapine (without fluoxetine) or lamotrigine monotherapy. | Consider initial treatment with lamotrigine, … usually as an addition to agents preventing recurrence of mania |
| If there is no response to OFC or quetiapine, consider lamotrigine monotherapy. | Consider the use of an antidepressant with an antimanic drug in bipolar I patients |
| ECT noticed but not recommended. | Consider ECT in severe or refractory depression |
| Offer a psychological intervention that has been developed specifically for bipolar disorder. | Consider family-focused, cognitive behavior therapy or interpersonal rhythm therapy as an additional treatment (not as a primary treatment option) |
| Within 4 weeks of resolution of symptoms, discuss …whether to continue treatment for bipolar depression or start long-term treatment | Consider the strategy for long-term treatment as patient recovers |
Acknowledgements
Special thanks are due to Susan Chandler and Lynne Harmer who organized the logistics. The expenses of the meeting itself were defrayed by BAP exclusively.
Footnotes
For disclosure of competing interests for all authors, visit http://www.bap.org.uk
References
- Abdallah CG, Sanacora G, Duman RS, et al. Ketamine and rapid-acting antidepressants: a window into a new neurobiology for mood disorder therapeutics. Annual review of medicine. 2015;66:509–523. doi: 10.1146/annurev-med-053013-062946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achtyes ED, Halstead S, Smart L, et al. Validation of Computerized Adaptive Testing in an Outpatient Nonacademic Setting: The VOCATIONS Trial. Psychiatr Serv. 2015;66:1091–1096. doi: 10.1176/appi.ps.201400390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert U, Rosso G, Maina G, et al. Impact of anxiety disorder comorbidity on quality of life in euthymic bipolar disorder patients: differences between bipolar I and II subtypes. Journal of Affective Disorders. 2008;105:297–303. doi: 10.1016/j.jad.2007.05.020. [DOI] [PubMed] [Google Scholar]
- Allen MH, Currier GW, Hughes DH, et al. The Expert Consensus Guideline Series. Treatment of behavioral emergencies. PostgradMed. 2001:1–88. [PubMed] [Google Scholar]
- Altshuler L, Kiriakos L, Calcagno J, et al. The impact of antidepressant discontinuation versus antidepressant continuation on 1-year risk for relapse of bipolar depression: a retrospective chart review. J Clin Psychiatry. 2001;62:612–616. doi: 10.4088/jcp.v62n0807. [DOI] [PubMed] [Google Scholar]
- Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. American Journal of Psychiatry. 2003;160:1252–1262. doi: 10.1176/appi.ajp.160.7.1252. [DOI] [PubMed] [Google Scholar]
- American Academy of Paediatrics Committee on Drugs. Use of psychoactive medications during pregnancy and possible effects on the fetus and newborn. Pediatrics. 2000;105:880–887. doi: 10.1542/peds.105.4.880. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders (DSM-IV) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder (revision) Am J Psychiatry. 2002;159:1–50. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders (DSM-5) Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Amsterdam JD, Lorenzo-Luaces L, Soeller I, et al. Safety and effectiveness of continuation antidepressant versus mood stabilizer monotherapy for relapse-prevention of bipolar II depression: A randomized, double-blind, parallel-group, prospective study. Journal of Affective Disorders. 2015;185:31–37. doi: 10.1016/j.jad.2015.05.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson IM. Meta-analytical studies on new antidepressants. Br Med Bull. 2001;57:161–178. doi: 10.1093/bmb/57.1.161. [DOI] [PubMed] [Google Scholar]
- Andreazza AC, Kauer-Sant'Anna M, Frey BN, et al. Oxidative stress markers in bipolar disorder: A meta-analysis. Journal of Affective Disorders. 2008;111:135–144. doi: 10.1016/j.jad.2008.04.013. [DOI] [PubMed] [Google Scholar]
- Andreazza AC, Wang JF, Salmasi F, et al. Specific subcellular changes in oxidative stress in prefrontal cortex from patients with bipolar disorder. Journal of Neurochemistry. 2013;127:552–561. doi: 10.1111/jnc.12316. [DOI] [PubMed] [Google Scholar]
- Angst F, Stassen HH, Clayton PJ, et al. Mortality of patients with mood disorders: follow-up over 34-38 years. J Affect Disord. 2002;68:167–181. doi: 10.1016/s0165-0327(01)00377-9. [DOI] [PubMed] [Google Scholar]
- Angst J. The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord. 1998;50:143–151. doi: 10.1016/s0165-0327(98)00142-6. [DOI] [PubMed] [Google Scholar]
- Angst J, Azorin JM, Bowden CL, et al. Prevalence and characteristics of undiagnosed bipolar disorders in patients with a major depressive episode: the BRIDGE study. Arch Gen Psychiatry. 2011;68:791–798. doi: 10.1001/archgenpsychiatry.2011.87. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Sellaro R, et al. Recurrence of bipolar disorders and major depression. A life-long perspective. Eur Arch Psychiatry Clin Neurosci. 2003;253:236–240. doi: 10.1007/s00406-003-0437-2. [DOI] [PubMed] [Google Scholar]
- Angst J, Preisig M. Course of a clinical cohort of unipolar, bipolar and schizoaffective patients. Results of a prospective study from 1959 to 1985. Schweiz Arch Neurol Psychiatr. 1995;146:5–16. [PubMed] [Google Scholar]
- Angst J, Sellaro R. Historical perspectives and natural history of bipolar disorder. Biol Psychiatry. 2000;48:445–457. doi: 10.1016/s0006-3223(00)00909-4. [DOI] [PubMed] [Google Scholar]
- Aronson JK. Distinguishing hazards and harms, adverse drug effects and adverse drug reactions : implications for drug development, clinical trials, pharmacovigilance, biomarkers, and monitoring. Drug safety. 2013;36:147–153. doi: 10.1007/s40264-013-0019-9. [DOI] [PubMed] [Google Scholar]
- Ashcroft R. Giving medicine a fair trial. Trials should not second guess what patients want. BMJ. 2000;320:1686. doi: 10.1136/bmj.320.7251.1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin MP, Mitchell PB. Use of psychotropic medications in breast-feeding women: acute and prophylactic treatment. Aust NZJ Psychiatry. 1998;32:778–784. doi: 10.3109/00048679809073866. [DOI] [PubMed] [Google Scholar]
- Bai Y-M, Su T-P, Chen M-H, et al. Risk of developing diabetes mellitus and hyperlipidemia among patients with bipolar disorder, major depressive disorder, and schizophrenia: a 10-year nationwide population-based prospective cohort study. Journal of Affective Disorders. 2013;150:57–62. doi: 10.1016/j.jad.2013.02.019. [DOI] [PubMed] [Google Scholar]
- Bain M, Juszczak E, McInneny K, et al. Obstetric complications and affective psychoses. Two case-control studies based on structured obstetric records. Br J Psychiatry. 2000;176:523–526. doi: 10.1192/bjp.176.6.523. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Hennen J, Wilson M, et al. Olanzapine versus placebo in acute mania - Treatment responses in subgroups. Journal of Clinical Psychopharmacology. 2003;23:370–376. doi: 10.1097/01.jcp.0000085410.08426.9a. [DOI] [PubMed] [Google Scholar]
- Baldwin DS, Anderson IM, Nutt DJ, et al. Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: a revision of the 2005 guidelines from the British Association for Psychopharmacology. Journal of psychopharmacology (Oxford, England) 2014;28:403–439. doi: 10.1177/0269881114525674. [DOI] [PubMed] [Google Scholar]
- Bandelow B, Reitt M, Rover C, et al. Efficacy of treatments for anxiety disorders: a meta-analysis. Int Clin Psychopharmacol. 2015;30:183–192. doi: 10.1097/YIC.0000000000000078. [DOI] [PubMed] [Google Scholar]
- Barnes E, Simpson S, Griffiths E, et al. Developing an online psychoeducation package for bipolar disorder. Journal of mental health (Abingdon, England) 2011;20:21–31. doi: 10.3109/09638237.2010.525565. [DOI] [PubMed] [Google Scholar]
- Bauer MS, Biswas K, Kilbourne AM. Enhancing multiyear guideline concordance for bipolar disorder through collaborative care. The American journal of psychiatry. 2009;166:1244–1250. doi: 10.1176/appi.ajp.2009.09030342. [DOI] [PubMed] [Google Scholar]
- Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder: Part I. Intervention and implementation in a randomized effectiveness trial. Psychiatric Services. 2006a;57:927–936. doi: 10.1176/ps.2006.57.7.927. [DOI] [PubMed] [Google Scholar]
- Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder: Part II. Impact on clinical outcome, function, and costs. Psychiatric Services. 2006b;57:937–945. doi: 10.1176/ps.2006.57.7.937. [DOI] [PubMed] [Google Scholar]
- Bauer MS, Wisniewski SR, Marangell LB, et al. Are antidepressants associated with new-onset suicidality in bipolar disorder? A prospective study of participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD) Journal of Clinical Psychiatry. 2006c;67:48–55. doi: 10.4088/jcp.v67n0108. [DOI] [PubMed] [Google Scholar]
- Berk M, Hallam KT, McGorry PD. The potential utility of a staging model as a course specifier: a bipolar disorder perspective. J Affect Disord. 2007;100:279–281. doi: 10.1016/j.jad.2007.03.007. [DOI] [PubMed] [Google Scholar]
- Berwaerts J, Melkote R, Nuamah I, et al. A randomized, placebo- and active-controlled study of paliperidone extended-release as maintenance treatment in patients with bipolar I disorder after an acute manic or mixed episode. Journal of Affective Disorders. 2012;138:247–258. doi: 10.1016/j.jad.2012.01.047. [DOI] [PubMed] [Google Scholar]
- Bhagwagar Z, Goodwin GM. The role of lithium in the treatment of bipolar depression. Clinical Neuroscience Research. 2002;2:222–227. [Google Scholar]
- Biel MG, Peselow E, Mulcare L, et al. Continuation versus discontinuation of lithium in recurrent bipolar illness: a naturalistic study. Bipolar Disorders. 2007;9:435–442. doi: 10.1111/j.1399-5618.2007.00389.x. [DOI] [PubMed] [Google Scholar]
- Bieling PJ, Green SM, Macqueen G. The impact of personality disorders on treatment outcome in bipolar disorder: A review. Personality and Mental Health. 2007;1:2–13. [Google Scholar]
- Biffin F, Tahtalian S, Filia K, et al. The impact of age at onset of bipolar I disorder on functioning and clinical presentation. Acta Neuropsychiatrica. 2009;21:191–196. doi: 10.1111/j.1601-5215.2009.00399.x. [DOI] [PubMed] [Google Scholar]
- Bjorklund L, Horsdal HT, Mors O, et al. Trends in the psychopharmacological treatment of bipolar disorder: a nationwide register-based study. Acta Neuropsychiatrica. 2015:1–10. doi: 10.1017/neu.2015.52. [DOI] [PubMed] [Google Scholar]
- Black DW, Winokur G, Nasrallah A. Suicide in subtypes of major affective disorder. A comparison with general population suicide mortality. Arch Gen Psychiatry. 1987a;44:878–880. doi: 10.1001/archpsyc.1987.01800220040007. [DOI] [PubMed] [Google Scholar]
- Black DW, Winokur G, Nasrallah A. Treatment of Mania - a Naturalistic Study of Electroconvulsive-Therapy Versus Lithium in 438 Patients. Journal of Clinical Psychiatry. 1987b;48:132–139. [PubMed] [Google Scholar]
- Blacker D, Tsuang MT. Contested boundaries of bipolar disorder and the limits of categorical diagnosis in psychiatry. Am J Psychiatry. 1992;149:1473–1483. doi: 10.1176/ajp.149.11.1473. [DOI] [PubMed] [Google Scholar]
- Blader JC, Carlson GA. Increased rates of bipolar disorder diagnoses among U.S. child, adolescent, and adult inpatients, 1996-2004. Biol Psychiatry. 2007;62:107–114. doi: 10.1016/j.biopsych.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Grant J, Petry NM, et al. Prevalence and correlates of shoplifting in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Am J Psychiatry. 2008;165:905–913. doi: 10.1176/appi.ajp.2008.07101660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolea-Alamanac B, Nutt DJ, Adamou M, et al. Evidence-based guidelines for the pharmacological management of attention deficit hyperactivity disorder: update on recommendations from the British Association for Psychopharmacology. Journal of psychopharmacology (Oxford, England) 2014;28:179–203. doi: 10.1177/0269881113519509. [DOI] [PubMed] [Google Scholar]
- Bond DJ, Pratoomsri W, Yatham LN. Depot antipsychotic medications in bipolar disorder: a review of the literature. Acta psychiatrica Scandinavica Supplementum. 2007:3–16. doi: 10.1111/j.1600-0447.2007.01054.x. [DOI] [PubMed] [Google Scholar]
- Bond K, Anderson IM. Psychoeducation for relapse prevention in bipolar disorder: a systematic review of efficacy in randomized controlled trials. Bipolar Disord. 2015;17:349–362. doi: 10.1111/bdi.12287. [DOI] [PubMed] [Google Scholar]
- Bottlender R, Rudolf D, Strauss A, et al. Mood-stabilisers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patients. J Affect Disord. 2001;63:79–83. doi: 10.1016/s0165-0327(00)00172-5. [DOI] [PubMed] [Google Scholar]
- Bourne C, Aydemir O, Balanza-Martinez V, et al. Neuropsychological testing of cognitive impairment in euthymic bipolar disorder: an individual patient data meta-analysis. Acta Psychiatrica Scandinavica. 2013;128:149–162. doi: 10.1111/acps.12133. [DOI] [PubMed] [Google Scholar]
- Bourne C, Bilderbeck AC, Drennan R, et al. Verbal learning impairment in euthymic bipolar disorder: BDI v BDII. Journal of Affective Disorders. 2015;182:95–100. doi: 10.1016/j.jad.2015.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowden CL, Calabrese JR, McElroy SL, et al. The efficacy of lamotrigine in rapid cycling and non-rapid cycling patients with bipolar disorder. Biological Psychiatry. 1999;45:953–958. doi: 10.1016/s0006-3223(99)00013-x. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Vieta E, Ice KS, et al. Ziprasidone plus a mood stabilizer in subjects with bipolar I disorder: a 6-month, randomized, placebo-controlled, double-blind trial. The Journal of clinical psychiatry. 2010;71:130–137. doi: 10.4088/JCP.09m05482yel. [DOI] [PubMed] [Google Scholar]
- Brown EB, McElroy SL, Keck PE, Jr, et al. A 7-week, randomized, double-blind trial of olanzapine/fluoxetine combination versus lamotrigine in the treatment of bipolar I depression. J Clin Psychiatry. 2006;67:1025–1033. doi: 10.4088/jcp.v67n0703. [DOI] [PubMed] [Google Scholar]
- Brown ES, Khan DA, Nejtek VA. The psychiatric side effects of corticosteroids. Ann Allergy Asthma Immunol. 1999;83:495–503. doi: 10.1016/S1081-1206(10)62858-X. [DOI] [PubMed] [Google Scholar]
- Brown ES, Suppes T, Khan DA, et al. Mood changes during prednisone bursts in outpatients with asthma. J Clin Psychopharmacol. 2002;22:55–61. doi: 10.1097/00004714-200202000-00009. [DOI] [PubMed] [Google Scholar]
- Browne R, Byrne M, Mulryan N, et al. Labour and delivery complications at birth and later mania. An Irish case register study. Br J Psychiatry. 2000;176:369–372. doi: 10.1192/bjp.176.4.369. [DOI] [PubMed] [Google Scholar]
- Burgess S, Geddes J, Hawton K, et al. Lithium for maintenance treatment of mood disorders. Cochrane Database Syst Rev. 2001:CD003013. doi: 10.1002/14651858.CD003013. [DOI] [PubMed] [Google Scholar]
- Burns T, White I, Byford S, et al. Exposure to case management: relationships to patient characteristics and outcome. Report from the UK700 trial. Br J Psychiatry. 2002;181:236–241. doi: 10.1192/bjp.181.3.236. [DOI] [PubMed] [Google Scholar]
- Button KS, Munafo MR. Addressing risk of bias in trials of cognitive behavioral therapy. Shanghai archives of psychiatry. 2015;27:144–148. doi: 10.11919/j.issn.1002-0829.215042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese J, Pikalov A, Cucchiaro J, et al. Lurasidone Adjunctive to Lithium or Divalproex for Prevention of Recurrence in Patients with Bipolar I Disorder: Results of a 28-Week, Randomized, Double-Blind, Placebo-Controlled Study. Neuropsychopharmacology. 2015;40:S479–480. [Google Scholar]
- Calabrese JR, Bowden CL, Sachs GS, et al. A double-blind placebo-controlled study of lamotrigine monotherapy in outpatients with bipolar I depression. Lamictal 602 Study Group. J Clin Psychiatry. 1999;60:79–88. doi: 10.4088/jcp.v60n0203. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Keck PE, Jr, Macfadden W, et al. A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. Am J Psychiatry. 2005;162:1351–1360. doi: 10.1176/appi.ajp.162.7.1351. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Shelton MD, Rapport DJ, et al. Current research on rapid cycling bipolar disorder and its treatment. J Affect Disord. 2001;67:241–255. doi: 10.1016/s0165-0327(98)00161-x. [DOI] [PubMed] [Google Scholar]
- Carter L, Zolezzi M, Lewczyk A. An updated review of the optimal lithium dosage regimen for renal protection. Can J Psychiatry. 2013;58:595–600. doi: 10.1177/070674371305801009. [DOI] [PubMed] [Google Scholar]
- Carvalho AF, Dimellis Ds, Gonda X, et al. Rapid cycling in bipolar disorder: a systematic review. The Journal of clinical psychiatry. 2014;75:e578–586. doi: 10.4088/JCP.13r08905. [DOI] [PubMed] [Google Scholar]
- Carvalho AF, Quevedo J, McIntyre RS, et al. Treatment Implications of Predominant Polarity and the Polarity Index: A Comprehensive Review. International Journal of Neuropsychopharmacology. 2015;18 doi: 10.1093/ijnp/pyu079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassano GB, Rucci P, Frank E, et al. The mood spectrum in unipolar and bipolar disorder: arguments for a unitary approach. Am J Psychiatry. 2004;161:1264–1269. doi: 10.1176/appi.ajp.161.7.1264. [DOI] [PubMed] [Google Scholar]
- Cassidy F, Forest K, Murry E, et al. A factor analysis of the signs and symptoms of mania. Archives of General Psychiatry. 1998;55:27–32. doi: 10.1001/archpsyc.55.1.27. [DOI] [PubMed] [Google Scholar]
- Cassidy F, Pieper CF, Carroll BJ. Subtypes of mania determined by grade of membership analysis. Neuropsychopharmacology. 2001;25:373–383. doi: 10.1016/S0893-133X(01)00223-8. [DOI] [PubMed] [Google Scholar]
- Castberg I, Skogvoll E, Spigset O. Quetiapine and drug interactions: Evidence from a routine therapeutic drug monitoring service. Journal of Clinical Psychiatry. 2007;68:1540–1545. doi: 10.4088/jcp.v68n1011. [DOI] [PubMed] [Google Scholar]
- Cavazzoni PA, Berg PH, Kryzhanovskaya LA, et al. Comparison of treatment-emergent extrapyramidal symptoms in patients with bipolar mania or schizophrenia during olanzapine clinical trials. Journal of Clinical Psychiatry. 2006;67:107–113. doi: 10.4088/jcp.v67n0116. [DOI] [PubMed] [Google Scholar]
- Chang K, Saxena K, Howe M. An open-label study of lamotrigine adjunct or monotherapy for the treatment of adolescents with bipolar depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:298–304. doi: 10.1097/01.chi.0000194566.86160.a3. [DOI] [PubMed] [Google Scholar]
- Chaudron LH, Jefferson JW. Mood stabilizers during breastfeeding: a review. J Clin Psychiatry. 2000;61:79–90. doi: 10.4088/jcp.v61n0202. [DOI] [PubMed] [Google Scholar]
- Chen YW, Dilsaver SC. Lifetime rates of suicide attempts among subjects with bipolar and unipolar disorders relative to subjects with other axis I disorders. Biological Psychiatry. 1996;39:896–899. doi: 10.1016/0006-3223(95)00295-2. [DOI] [PubMed] [Google Scholar]
- Chengappa KNR, Schwarzman LK, Hulihan JF, et al. Adjunctive topiramate therapy in patients receiving a mood stabilizer for bipolar I disorder: A randomized, placebo-controlled trial. Journal of Clinical Psychiatry. 2006;67:1698–1706. doi: 10.4088/jcp.v67n1105. [DOI] [PubMed] [Google Scholar]
- Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13:153–160. doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cipriani A, Barbui C, Salanti G, et al. Comparative efficacy and acceptability of antimanic drugs in acute mania: a multiple-treatments meta-analysis. Lancet (London, England) 2011;378:1306–1315. doi: 10.1016/S0140-6736(11)60873-8. [DOI] [PubMed] [Google Scholar]
- Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373:746–758. doi: 10.1016/S0140-6736(09)60046-5. [DOI] [PubMed] [Google Scholar]
- Cipriani A, Hawton K, Stockton S, et al. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ (Clinical research ed) 2013a;346:f3646. doi: 10.1136/bmj.f3646. [DOI] [PubMed] [Google Scholar]
- Cipriani A, Higgins JPT, Geddes JR, et al. Conceptual and technical challenges in network meta-analysis. Annals of internal medicine. 2013b;159:130–137. doi: 10.7326/0003-4819-159-2-201307160-00008. [DOI] [PubMed] [Google Scholar]
- Cipriani A, Reid K, Young AH, et al. Valproic acid, valproate and divalproex in the maintenance treatment of bipolar disorder. The Cochrane database of systematic reviews. 2013c;10:CD003196. doi: 10.1002/14651858.CD003196.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark L, Iversen SD, Goodwin GM. Sustained attention deficit in bipolar disorder. Br J Psychiatry. 2002;180:313–319. doi: 10.1192/bjp.180.4.313. [DOI] [PubMed] [Google Scholar]
- Clatworthy J, Bowskill R, Parham R, et al. Understanding medication non-adherence in bipolar disorders using a Necessity-Concerns Framework. Journal of Affective Disorders. 2009;116:51–55. doi: 10.1016/j.jad.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Cleare A, Pariante CM, Young AH, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: A revision of the 2008 British Association for Psychopharmacology guidelines. Journal of psychopharmacology (Oxford, England) 2015;29:459–525. doi: 10.1177/0269881115581093. [DOI] [PubMed] [Google Scholar]
- Clements C, Morriss R, Jones S, et al. Suicide in bipolar disorder in a national English sample, 1996-2009: frequency, trends and characteristics. Psychological Medicine. 2013;43:2593–2602. doi: 10.1017/S0033291713000329. [DOI] [PubMed] [Google Scholar]
- Clyburn LD, Stones MJ, Hadjistavropoulos T, et al. Predicting caregiver burden and depression in Alzheimer's disease. J Gerontol B Psychol Sci Soc Sci. 2000;55:S2–13. doi: 10.1093/geronb/55.1.s2. [DOI] [PubMed] [Google Scholar]
- Cohen LS, Friedman JM, Jefferson JW, et al. A reevaluation of risk of in utero exposure to lithium. JAMA. 1994;271:146–150. [PubMed] [Google Scholar]
- Colom F, Vieta E. Psychoeducation manual for bipolar disorder. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- Colom F, Vieta E, Daban C, et al. Clinical and therapeutic implications of predominant polarity in bipolar disorder. Journal of Affective Disorders. 2006;93:13–17. doi: 10.1016/j.jad.2006.01.032. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Martinez-Aran A, et al. Clinical factors associated with treatment noncompliance in euthymic bipolar patients. J Clin Psychiatry. 2000;61:549–555. doi: 10.4088/jcp.v61n0802. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Martinez-Aran A, et al. A randomized trial on the efficacy of group psychoeducation in the prophylaxis of recurrences in bipolar patients whose disease is in remission. Archives of General Psychiatry. 2003;60:402–407. doi: 10.1001/archpsyc.60.4.402. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Sanchez-Moreno J, et al. Group psychoeducation for stabilised bipolar disorders: 5-year outcome of a randomised clinical trial. The British journal of psychiatry : the journal of mental science. 2009;194:260–265. doi: 10.1192/bjp.bp.107.040485. [DOI] [PubMed] [Google Scholar]
- Correll CU, Sheridan EM, DelBello MP. Antipsychotic and mood stabilizer efficacy and tolerability in pediatric and adult patients with bipolar I mania: a comparative analysis of acute, randomized, placebo-controlled trials. Bipolar Disorders. 2010;12:116–141. doi: 10.1111/j.1399-5618.2010.00798.x. [DOI] [PubMed] [Google Scholar]
- Coryell W, Fiedorowicz J, Leon AC, et al. Age of onset and the prospectively observed course of illness in bipolar disorder. J Affect Disord. 2013;146:34–38. doi: 10.1016/j.jad.2012.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craddock N, Owen MJ. The Kraepelinian dichotomy - going, going… but still not gone. Br J Psychiatry. 2010;196:92–95. doi: 10.1192/bjp.bp.109.073429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross AJ, Widzowski D, Maciag C, et al. Quetiapine and its metabolite norquetiapine: translation from in vitro pharmacology to in vivo efficacy in rodent models. British journal of pharmacology. 2015 doi: 10.1111/bph.13346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross-Disorder Group of the Psychiatric Genomics C. Lee SH, Ripke S, et al. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nature genetics. 2013;45:984–994. doi: 10.1038/ng.2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe M, Inder M, Carlyle D, et al. Nurse-led delivery of specialist supportive care for bipolar disorder: a randomized controlled trial. Journal of psychiatric and mental health nursing. 2012;19:446–454. doi: 10.1111/j.1365-2850.2011.01822.x. [DOI] [PubMed] [Google Scholar]
- Crump C, Sundquist K, Winkleby MA, et al. Comorbidities and mortality in bipolar disorder: a Swedish national cohort study. JAMA Psychiatry. 2013;70:931–939. doi: 10.1001/jamapsychiatry.2013.1394. [DOI] [PubMed] [Google Scholar]
- Cummings JL, Mendez MF. Secondary mania with focal cerebrovascular lesions. Am J Psychiatry. 1984;141:1084–1087. doi: 10.1176/ajp.141.9.1084. [DOI] [PubMed] [Google Scholar]
- Dell'Osso B, Ketter TA. Assessing efficacy/effectiveness and safety/tolerability profiles of adjunctive pramipexole in bipolar depression: acute versus long-term data. International Clinical Psychopharmacology. 2013;28:297–304. doi: 10.1097/YIC.0b013e3283639015. [DOI] [PubMed] [Google Scholar]
- Denicoff KD, Leverich GS, Nolen WA, et al. Validation of the prospective NIMH-Life-Chart Method (NIMH-LCM-p) for longitudinal assessment of bipolar illness. Psychol Med. 2000;30:1391–1397. doi: 10.1017/s0033291799002810. [DOI] [PubMed] [Google Scholar]
- Department of Health. A national service framework for mental health. London: Department of Health; 1999. [Google Scholar]
- Di Simplicio M, McInerney JE, Goodwin GM, et al. Revealing the Mind's Eye: Bringing (Mental) Images Into Psychiatry. American Journal of Psychiatry. 2012;169:1245–1246. doi: 10.1176/appi.ajp.2012.12040499. [DOI] [PubMed] [Google Scholar]
- Diav-Citrin O, Shechtman S, Tahover E, et al. Pregnancy outcome following in utero exposure to lithium: a prospective, comparative, observational study. The American journal of psychiatry. 2014;171:785–794. doi: 10.1176/appi.ajp.2014.12111402. [DOI] [PubMed] [Google Scholar]
- Diflorio A, Jones I. Is sex important? Gender differences in bipolar disorder. Int Rev Psychiatry. 2010;22:437–452. doi: 10.3109/09540261.2010.514601. [DOI] [PubMed] [Google Scholar]
- Dols A, Kupka RW, van Lammeren A, et al. The prevalence of late-life mania: a review. Bipolar Disord. 2014;16:113–118. doi: 10.1111/bdi.12104. [DOI] [PubMed] [Google Scholar]
- Dragioti E, Dimoliatis I, Evangelou E. Disclosure of researcher allegiance in meta-analyses and randomised controlled trials of psychotherapy: a systematic appraisal. BMJ Open. 2015;5:e007206. doi: 10.1136/bmjopen-2014-007206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunayevich E, Keck PE., Jr Prevalence and description of psychotic features in bipolar mania. Curr Psychiatry Rep. 2000;2:286–290. doi: 10.1007/s11920-000-0069-4. [DOI] [PubMed] [Google Scholar]
- Duncan S. Polycystic ovarian syndrome in women with epilepsy: a review. Epilepsia. 2001;42(Suppl 3):60–65. doi: 10.1046/j.1528-1157.2001.042suppl.3060.x. [DOI] [PubMed] [Google Scholar]
- Durgam S, Earley W, Lipschitz A, et al. An 8-Week Randomized, Double-Blind, Placebo-Controlled Evaluation of the Safety and Efficacy of Cariprazine in Patients With Bipolar I Depression. Am J Psychiatry. 2015a doi: 10.1176/appi.ajp.2015.15020164. appiajp201515020164. [DOI] [PubMed] [Google Scholar]
- Durgam S, Starace A, Li D, et al. The efficacy and tolerability of cariprazine in acute mania associated with bipolar I disorder: a phase II trial. Bipolar Disord. 2015b;17:63–75. doi: 10.1111/bdi.12238. [DOI] [PubMed] [Google Scholar]
- Ebbesen F, Joergensen A, Hoseth E, et al. Neonatal hypoglycaemia and withdrawal symptoms after exposure in utero to valproate. Arch Dis Child Fetal Neonatal Ed. 2000;83:F124–F129. doi: 10.1136/fn.83.2.F124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadden G, Bebbington P, Kuipers L. The burden of care: the impact of functional psychiatric illness on the patient's family. Br J Psychiatry. 1987;150:285–292. doi: 10.1192/bjp.150.3.285. [DOI] [PubMed] [Google Scholar]
- Fagiolini A, Frank E, Rucci P, et al. Mood and anxiety spectrum as a means to identify clinically relevant subtypes of bipolar I disorder. Bipolar Disorders. 2007;9:462–467. doi: 10.1111/j.1399-5618.2007.00443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faurholt-Jepsen M, Ritz C, Frost M, et al. Mood instability in bipolar disorder type I versus type II-continuous daily electronic self-monitoring of illness activity using smartphones. Journal of Affective Disorders. 2015;186:342–349. doi: 10.1016/j.jad.2015.06.026. [DOI] [PubMed] [Google Scholar]
- Fazel S, Seewald K. Severe mental illness in 33,588 prisoners worldwide: systematic review and meta-regression analysis. Br J Psychiatry. 2012;200:364–373. doi: 10.1192/bjp.bp.111.096370. [DOI] [PubMed] [Google Scholar]
- Fazel S, Singh JP, Doll H, et al. Use of risk assessment instruments to predict violence and antisocial behaviour in 73 samples involving 24 827 people: systematic review and meta-analysis. BMJ. 2012;345:e4692. doi: 10.1136/bmj.e4692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel S, Wolf A, Geddes JR. Suicide in prisoners with bipolar disorder and other psychiatric disorders: a systematic review. Bipolar Disord. 2013;15:491–495. doi: 10.1111/bdi.12053. [DOI] [PubMed] [Google Scholar]
- Fazel S, Zetterqvist J, Larsson H, et al. Antipsychotics, mood stabilisers, and risk of violent crime. Lancet. 2014;384:1206–1214. doi: 10.1016/S0140-6736(14)60379-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferner RE, Coleman J, Pirmohamed M, et al. The quality of information on monitoring for haematological adverse drug reactions. British journal of clinical pharmacology. 2005;60:448–451. doi: 10.1111/j.1365-2125.2005.02440.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiander M, Burns T, McHugo GJ, et al. Assertive community treatment across the Atlantic: comparison of model fidelity in the UK and USA. The British journal of psychiatry : the journal of mental science. 2003;182:248–254. doi: 10.1192/bjp.182.3.248. [DOI] [PubMed] [Google Scholar]
- Flint J, Cuijpers P, Horder J, et al. Is there an excess of significant findings in published studies of psychotherapy for depression? Psychol Med. 2015;45:439–446. doi: 10.1017/S0033291714001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frangou S, Donaldson S, Hadjulis M, et al. The Maudsley Bipolar Disorder Project: Executive dysfunction in bipolar disorder I and its clinical correlates. Biological Psychiatry. 2005;58:859–864. doi: 10.1016/j.biopsych.2005.04.056. [DOI] [PubMed] [Google Scholar]
- Frank E, Kupfer DJ, Thase ME, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Archives of General Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- Frank E, Swartz HA, Kupfer DJ. Interpersonal and social rhythm therapy: managing the chaos of bipolar disorder. Biol Psychiatry. 2000;48:593–604. doi: 10.1016/s0006-3223(00)00969-0. [DOI] [PubMed] [Google Scholar]
- Frankenburg FR, Zanarini MC. Divalproex sodium treatment of women with borderline personality disorder and bipolar II disorder: a double-blind placebo-controlled pilot study. The Journal of clinical psychiatry. 2002;63:442–446. doi: 10.4088/jcp.v63n0511. [DOI] [PubMed] [Google Scholar]
- Franks MA, Macritchie KAN, Mahmood T, et al. Bouncing back: is the bipolar rebound phenomenon peculiar to lithium? A retrospective naturalistic study. Journal of psychopharmacology (Oxford, England) 2008;22:452–456. doi: 10.1177/0269881107085238. [DOI] [PubMed] [Google Scholar]
- Frederikse M, Petrides G, Kellner C. Continuation and maintenance electroconvulsive therapy for the treatment of depressive illness: a response to the National Institute for Clinical Excellence report. The journal of ECT. 2006;22:13–17. doi: 10.1097/00124509-200603000-00003. [DOI] [PubMed] [Google Scholar]
- Freedman R, Lewis DA, Michels R, et al. The initial field trials of DSM-5: new blooms and old thorns. Am J Psychiatry. 2013;170:1–5. doi: 10.1176/appi.ajp.2012.12091189. [DOI] [PubMed] [Google Scholar]
- Freeman MP, Freeman SA, McElroy SL. The comorbidity of bipolar and anxiety disorders: prevalence, psychobiology, and treatment issues. J Affect Disord. 2002;68:1–23. doi: 10.1016/s0165-0327(00)00299-8. [DOI] [PubMed] [Google Scholar]
- Frye MA, Ketter TA, Kimbrell TA, et al. A placebo-controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clin Psychopharmacol. 2000;20:607–614. doi: 10.1097/00004714-200012000-00004. [DOI] [PubMed] [Google Scholar]
- Gao KM, Kemp DE, Ganocy SJ, et al. Antipsychotic-induced extrapyramidal side effects in bipolar disorder and schizophrenia: a systematic review. Journal of Clinical Psychopharmacology. 2008;28:203–209. doi: 10.1097/JCP.0b013e318166c4d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geddes JR, Calabrese J, Goodwin GM. Lamotrigine for treatment of bipolar depression: independent meta-analysis and metaregression of individual patient data from five randomized trials. Br J Psychiatry. 2009;194:4–9. doi: 10.1192/bjp.bp.107.048504. [DOI] [PubMed] [Google Scholar]
- Geddes JR, Carney SM, Davies C, et al. Relapse prevention with antidepressant drug treatment in depressive disorders. Lancet. 2003;361:643–651. doi: 10.1016/S0140-6736(03)12599-8. [DOI] [PubMed] [Google Scholar]
- Geddes JR, Gardiner A, Rendell J, et al. Comparative evaluation of quetiapine plus lamotrigine combination versus quetiapine monotherapy (and folic acid versus placebo) in bipolar depression (CEQUEL): a 2 x 2 factorial randomised trial. Lancet Psychiatry. 2015 doi: 10.1016/S2215-0366(15)00450-2. [DOI] [PubMed] [Google Scholar]
- Geddes JR, Goodwin GM, Rendell J, et al. Lithium plus valproate combination therapy versus monotherapy for relapse prevention in bipolar I disorder (BALANCE): a randomised open-label trial. Lancet (London, England) 2010;375:385–395. doi: 10.1016/S0140-6736(09)61828-6. [DOI] [PubMed] [Google Scholar]
- Geddes JR, Miklowitz DJ. Treatment of bipolar disorder. Lancet (London, England) 2013;381:1672–1682. doi: 10.1016/S0140-6736(13)60857-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller B, Sun K, Zimerman B, et al. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord. 1995;34:259–268. doi: 10.1016/0165-0327(95)00023-g. [DOI] [PubMed] [Google Scholar]
- George EL, Miklowitz DJ, Richards JA, et al. The comorbidity of bipolar disorder and axis II personality disorders: prevalence and clinical correlates. Bipolar Disord. 2003;5:115–122. doi: 10.1034/j.1399-5618.2003.00028.x. [DOI] [PubMed] [Google Scholar]
- Gershon ES, Hamovit J, Guroff JJ, et al. A Family Study of Schizoaffective, Bipolar-I, Bipolar-Ii, Unipolar, and Normal Control Probands. Archives of General Psychiatry. 1982;39:1157–1167. doi: 10.1001/archpsyc.1982.04290100031006. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Lenox MS, Baldessarini RJ. Effectiveness and safety of long-term antidepressant treatment in bipolar disorder. J Clin Psychiatry. 2001;62:565–569. doi: 10.4088/jcp.v62n07a12. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Coca Perraillon M, Hur K, et al. Antidepressant treatment and suicide attempts and self-inflicted injury in children and adolescents. Pharmacoepidemiol Drug Saf. 2015;24:208–214. doi: 10.1002/pds.3713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gigante AD, Lafer B, Yatham LN. Long-acting injectable antipsychotics for the maintenance treatment of bipolar disorder. Cns Drugs. 2012;26:403–420. doi: 10.2165/11631310-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Gijsman HJ, Geddes JR, Rendell JM, et al. Antidepressants for bipolar depression: A systematic review of randomized, controlled trials. Am J Psychiatry. 2004;161:1537–1547. doi: 10.1176/appi.ajp.161.9.1537. [DOI] [PubMed] [Google Scholar]
- Goldstein J, Nyberg S, Takano A, et al. PET-measured D2, 5HT2A, and NET occupancy by quetiapine and n-desalkyl-quetiapine (norquetiapine) in non-human primates. International Journal of Psychiatry in Clinical Practice. 2007;11:322–322. [Google Scholar]
- Goodwin GM. Recurrence of mania after lithium withdrawal. Implications for the use of lithium in the treatment of bipolar affective disorder. Br J Psychiatry. 1994;164:149–152. doi: 10.1192/bjp.164.2.149. [DOI] [PubMed] [Google Scholar]
- Goodwin GM. Hypomania - whats in a name? British Journal of Psychiatry. 2002;181:94–95. doi: 10.1017/s000712500016177x. [DOI] [PubMed] [Google Scholar]
- Goodwin GM. Evidence-based guidelines for treating bipolar disorder: recommendations from the British Association for Psychopharmacology. Journal of Psychopharmacology. 2003;17:149–173. doi: 10.1177/0269881103017002003. [DOI] [PubMed] [Google Scholar]
- Goodwin GM. Evidence-based guidelines for treating bipolar disorder: revised second edition-recommendations from the British Association for Psychopharmacology. Journal of Psychopharmacology. 2009;23:346–388. doi: 10.1177/0269881109102919. [DOI] [PubMed] [Google Scholar]
- Goodwin GM. Bipolar depression and treatment with antidepressants. The British Journal of Psychiatry : the journal of mental science. 2012;200:5–6. doi: 10.1192/bjp.bp.111.095349. [DOI] [PubMed] [Google Scholar]
- Goodwin GM, Bowden CL, Calabrese JR, et al. A pooled analysis of 2 placebo-controlled 18-month trials of lamotrigine and lithium maintenance in bipolar I disorder. Journal of Clinical Psychiatry. 2004;65:432–441. doi: 10.4088/jcp.v65n0321. [DOI] [PubMed] [Google Scholar]
- Goodwin GM, Geddes JR. What is the heartland of psychiatry? British Journal of Psychiatry. 2007;191:189–191. doi: 10.1192/bjp.bp.107.036343. [DOI] [PubMed] [Google Scholar]
- Goss AJ, Kaser M, Costafreda SG, et al. Modafinil augmentation therapy in unipolar and bipolar depression: a systematic review and meta-analysis of randomized controlled trials. The Journal of clinical psychiatry. 2013;74:1101–1107. doi: 10.4088/JCP.13r08560. [DOI] [PubMed] [Google Scholar]
- Grande I, Balanza-Martinez V, Jimenez-Arriero MA, et al. Clinical factors leading to lamotrigine prescription in bipolar outpatients: Subanalysis of the SINDEPRES study. Journal of Affective Disorders. 2012;143:102–108. doi: 10.1016/j.jad.2012.05.035. [DOI] [PubMed] [Google Scholar]
- Green AI, Tohen M, Patel JK, et al. Clozapine in the treatment of refractory psychotic mania. The American journal of psychiatry. 2000;157:982–986. doi: 10.1176/appi.ajp.157.6.982. [DOI] [PubMed] [Google Scholar]
- Greil W, Ludwig-Mayerhofer W, Erazo N, et al. Lithium versus carbamazepine in the maintenance treatment of bipolar disorders--a randomised study. J Affect Disord. 1997;43:151–161. doi: 10.1016/s0165-0327(96)01427-9. [DOI] [PubMed] [Google Scholar]
- Grunze H, Kotlik E, Costa R, et al. Assessment of the efficacy and safety of eslicarbazepine acetate in acute mania and prevention of recurrence: experience from multicentre, double-blind, randomised phase II clinical studies in patients with bipolar disorder I. J Affect Disord. 2015;174:70–82. doi: 10.1016/j.jad.2014.11.013. [DOI] [PubMed] [Google Scholar]
- Haddad PM, Pal BR, Clarke P, et al. Neonatal symptoms following maternal paroxetine treatment: Serotonin toxicity or paroxetine discontinuation syndrome? Journal of Psychopharmacology. 2005;19:554–557. doi: 10.1177/0269881105056554. [DOI] [PubMed] [Google Scholar]
- Hales SA, Deeprose C, Goodwin GM, et al. Cognitions in bipolar affective disorder and unipolar depression: imagining suicide. Bipolar Disorders. 2011;13:651–661. doi: 10.1111/j.1399-5618.2011.00954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmer CJ, Goodwin GM, Cowen PJ. Why do antidepressants take so long to work? A cognitive neuropsychological model of antidepressant drug action. Br J Psychiatry. 2009;195:102–108. doi: 10.1192/bjp.bp.108.051193. [DOI] [PubMed] [Google Scholar]
- Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Hartong EGTM, Moleman P, Hoogduin CAL, et al. Prophylactic efficacy of lithium versus carbamazepine in treatment-naive bipolar patients. Journal of Clinical Psychiatry. 2003;64:144–151. doi: 10.4088/jcp.v64n0206. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Schmidt DA, Scarna A, et al. Sleep-related functioning in euthymic patients with bipolar disorder, patients with insomnia, and subjects without sleep problems. Am J Psychiatry. 2005;162:50–57. doi: 10.1176/appi.ajp.162.1.50. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Soehner AM, Kaplan KA, et al. Treating insomnia improves mood state, sleep, and functioning in bipolar disorder: a pilot randomized controlled trial. J Consult Clin Psychol. 2015;83:564–577. doi: 10.1037/a0038655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K. Assessment of suicide risk. Br J Psychiatry. 1987;150:145–153. doi: 10.1192/bjp.150.2.145. [DOI] [PubMed] [Google Scholar]
- Hawton K, Sutton L, Haw C, et al. Suicide and attempted suicide in bipolar disorder: A systematic review of risk factors 12. Journal of Clinical Psychiatry. 2005;66:693–704. doi: 10.4088/jcp.v66n0604. [DOI] [PubMed] [Google Scholar]
- Hiller W, Dichtl G, Hecht H, et al. An empirical comparison of diagnoses and reliabilities in ICD-10 and DSM-III-R. Eur Arch Psychiatry Clin Neurosci. 1993;242:209–217. doi: 10.1007/BF02189965. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Calabrese JR, Weissman MM, et al. Screening for bipolar disorder in the community. J Clin Psychiatry. 2003;64:53–59. doi: 10.4088/jcp.v64n0111. [DOI] [PubMed] [Google Scholar]
- Hoertel N, Le Strat Y, Lavaud P, et al. Generalizability of clinical trial results for bipolar disorder to community samples: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2013;74:265–270. doi: 10.4088/JCP.12m07935. [DOI] [PubMed] [Google Scholar]
- Holmes EA, Deeprose C, Fairburn CG, et al. Mood stability versus mood instability in bipolar disorder: a possible role for emotional mental imagery. Behaviour Research and Therapy. 2011;49:707–713. doi: 10.1016/j.brat.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EA, Geddes JR, Colom F, et al. Mental imagery as an emotional amplifier: application to bipolar disorder. Behaviour Research and Therapy. 2008;46:1251–1258. doi: 10.1016/j.brat.2008.09.005. [DOI] [PubMed] [Google Scholar]
- Horne R, Chapman SC, Parham R, et al. Understanding patients' adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the Necessity-Concerns Framework. PLoS One. 2013;8:e80633. doi: 10.1371/journal.pone.0080633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard L, Kirkwood G, Leese M. Risk of hip fracture in patients with a history of schizophrenia. British Journal of Psychiatry. 2007;190:129–134. doi: 10.1192/bjp.bp.106.023671. [DOI] [PubMed] [Google Scholar]
- Howes OD, Lim S, Theologos G, et al. A comprehensive review and model of putative prodromal features of bipolar affective disorder. Psychol Med. 2011;41:1567–1577. doi: 10.1017/S0033291710001790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howes OD, Wheeler MJ, Pilowsky LS, et al. Sexual function and gonadal hormones in patients taking antipsychotic treatment for schizophrenia or schizoaffective disorder. The Journal of clinical psychiatry. 2007;68:361–367. doi: 10.4088/jcp.v68n0302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyer EH, Mortensen PB, Olesen AV. Mortality and causes of death in a total national sample of patients with affective disorders admitted for the first time between 1973 and 1993. British Journal of Psychiatry. 2000;176:76–82. doi: 10.1192/bjp.176.1.76. [DOI] [PubMed] [Google Scholar]
- Ivins A, Di Simplicio M, Close H, et al. Mental imagery in bipolar affective disorder versus unipolar depression: Investigating cognitions at times of 'positive' mood. Journal of Affective Disorders. 2014;166:234–242. doi: 10.1016/j.jad.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jauhar S, McKenna PJ, Laws KR. NICE guidance on psychological treatments for bipolar disorder: searching for the evidence. The Lancet Psychiatry. 2016 doi: 10.1016/S2215-0366(15)00545-3. [DOI] [PubMed] [Google Scholar]
- Joas E, Karanti A, Song J et al. 2016 [Google Scholar]
- Joffe H. Reproductive biology and psychotropic treatments in premenopausal women with bipolar disorder. Journal of Clinical Psychiatry. 2007;68:10–15. [PubMed] [Google Scholar]
- Johnson RE, McFarland BH. Lithium use and discontinuation in a health maintenance organization. Am J Psychiatry. 1996;153:993–1000. doi: 10.1176/ajp.153.8.993. [DOI] [PubMed] [Google Scholar]
- Johnstone EC, Crow TJ, Frith CD, et al. The Northwick Park “functional” psychosis study: diagnosis and treatment response. Lancet. 1988;2:119–125. doi: 10.1016/s0140-6736(88)90682-4. [DOI] [PubMed] [Google Scholar]
- Jones L, Metcalf A, Gordon-Smith K, et al. Gambling problems in bipolar disorder in the UK: prevalence and distribution. The British journal of psychiatry : the journal of mental science. 2015a;207:328–333. doi: 10.1192/bjp.bp.114.154286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones S, McGrath E, Hampshire K, et al. A randomised controlled trial of time limited CBT informed psychological therapy for anxiety in bipolar disorder. BMC psychiatry. 2013;13:54. doi: 10.1186/1471-244X-13-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones SH, Smith G, Mulligan LD, et al. Recovery-focused cognitive-behavioural therapy for recent-onset bipolar disorder: randomised controlled pilot trial. The British journal of psychiatry : the journal of mental science. 2015b;206:58–66. doi: 10.1192/bjp.bp.113.141259. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59:530–537. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- Judd LL, Schettler PJ, Akiskal HS, et al. Residual symptom recovery from major affective episodes in bipolar disorders and rapid episode relapse/recurrence. Arch Gen Psychiatry. 2008;65:386–394. doi: 10.1001/archpsyc.65.4.386. [DOI] [PubMed] [Google Scholar]
- Judd LL, Schettler PJ, Akiskal HS, et al. Long-term symptomatic status of bipolar I vs. bipolar II disorders. The international journal of neuropsychopharmacology / official scientific journal of the Collegium Internationale Neuropsychopharmacologicum (CINP) 2003;6:127–137. doi: 10.1017/S1461145703003341. [DOI] [PubMed] [Google Scholar]
- Kaneko S, Battino D, Andermann E, et al. Congenital malformations due to antiepileptic drugs. Epilepsy Res. 1999;33:145–158. doi: 10.1016/s0920-1211(98)00084-9. [DOI] [PubMed] [Google Scholar]
- Kay JH, Altshuler LL, Ventura J, et al. Impact of axis II comorbidity on the course of bipolar illness in men: a retrospective chart review. Bipolar Disord. 2002;4:237–242. doi: 10.1034/j.1399-5618.2002.01165.x. [DOI] [PubMed] [Google Scholar]
- Keck P-EJ, McElroy SL, Strakowski SM, et al. Antipsychotics in the treatment of mood disorders and risk of tardive dyskinesia. J Clin Psychiatry. 2000;61(Suppl 4):33–38. [PubMed] [Google Scholar]
- Keck PE, Calabrese JR, McIntyre RS, et al. Aripiprazole monotherapy for maintenance therapy in bipolar I disorder: A 100-week, double-blind study versus placebo. Journal of Clinical Psychiatry. 2007;68:1480–1491. doi: 10.4088/jcp.v68n1003. [DOI] [PubMed] [Google Scholar]
- Kemp DE, Gao KM, Ganocy SJ, et al. A 6-month, double-blind, maintenance trial of lithium monotherapy versus the combination of lithium and divalproex for rapid-cycling bipolar disorder and Co-occurring substance abuse or dependence. The Journal of clinical psychiatry. 2009;70:113–121. doi: 10.4088/jcp.07m04022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp R, Kirov G, Everitt B, et al. Randomised controlled trial of compliance therapy. 18-month follow-up. Br J Psychiatry. 1998;172:413–419. doi: 10.1192/bjp.172.5.413. [DOI] [PubMed] [Google Scholar]
- Kendell RE. Diagnosis and classification of functional psychoses. Br Med Bull. 1987;43:499–513. doi: 10.1093/oxfordjournals.bmb.a072198. [DOI] [PubMed] [Google Scholar]
- Kendell RE, Gourlay J. The clinical distinction between the affective psychoses and schizophrenia. Br J Psychiatry. 1970;117:261–266. [PubMed] [Google Scholar]
- Kessing L. Treatment Options in Bipolar Disorder: Lessons from Population-Based Registers with Focus on Lithium. Curr Treat Options Psych. 2015;2:218–228. [Google Scholar]
- Kessing LV, Hansen HV, Hvenegaard A, et al. Treatment in a specialised out-patient mood disorder clinic v. standard out-patient treatment in the early course of bipolar disorder: randomised clinical trial. Br J Psychiatry. 2013;202:212–219. doi: 10.1192/bjp.bp.112.113548. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Sondergard L, Kvist K, et al. Adherence to lithium in naturalistic settings: results from a nationwide pharmacoepidemiological study. Bipolar Disorders. 2007;9:730–736. doi: 10.1111/j.1399-5618.2007.00405.x. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Vradi E, Andersen PK. Starting lithium prophylaxis early v. late in bipolar disorder. Br J Psychiatry. 2014;205:214–220. doi: 10.1192/bjp.bp.113.142802. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Rubinow DR, Holmes C, et al. The epidemiology of DSM-III-R bipolar I disorder in a general population survey. Psychol Med. 1997;27:1079–1089. doi: 10.1017/s0033291797005333. [DOI] [PubMed] [Google Scholar]
- Ketter TA, Wang PW, Chandler RA, et al. Adjunctive aripiprazole in treatment-resistant bipolar depression. Annals of clinical psychiatry : official journal of the American Academy of Clinical Psychiatrists. 2006;18:169–172. doi: 10.1080/10401230600801176. [DOI] [PubMed] [Google Scholar]
- Kieseppa T, Partonen T, Haukka J, et al. High concordance of bipolar I disorder in a nationwide sample of twins. American Journal of Psychiatry. 2004;161:1814–1821. doi: 10.1176/ajp.161.10.1814. [DOI] [PubMed] [Google Scholar]
- Kilbourne AM, Goodrich DE, Lai Z, et al. Randomized controlled trial to assess reduction of cardiovascular disease risk in patients with bipolar disorder: the Self-Management Addressing Heart Risk Trial (SMAHRT) J Clin Psychiatry. 2013;74:e655–662. doi: 10.4088/JCP.12m08082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripalani M, Shawcross J, Reilly J, et al. Lithium and chronic kidney disease. BMJ (Clinical research ed) 2009;339:b2452. doi: 10.1136/bmj.b2452. [DOI] [PubMed] [Google Scholar]
- Kupka RW, Altshuler LL, Nolen WA, et al. Three times more days depressed than manic or hypomanic in both bipolar I and bipolar II disorder. Bipolar Disord. 2007;9:531–535. doi: 10.1111/j.1399-5618.2007.00467.x. [DOI] [PubMed] [Google Scholar]
- Kushner SF, Khan A, Lane R, et al. Topiramate monotherapy in the management of acute mania: results of four double-blind placebo-controlled trials. Bipolar Disorders. 2006;8:15–27. doi: 10.1111/j.1399-5618.2006.00276.x. [DOI] [PubMed] [Google Scholar]
- Lam D, Watkins E, Hayward P, et al. A randomised controlled study of cognitive therapy of relapse prevention for bipolar affective disorder - outcome of the first year. Archives of General Psychiatry. 2003;60:145–152. doi: 10.1001/archpsyc.60.2.145. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, et al. Smoking and mental illness - A population-based prevalence study. Jama-Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Laursen TM, Nordentoft M. Heart disease treatment and mortality in schizophrenia and bipolar disorder - Changes in the danish population between 1994 and 2006. Journal of Psychiatric Research. 2011;45:29–35. doi: 10.1016/j.jpsychires.2010.04.027. [DOI] [PubMed] [Google Scholar]
- Lebensohn ZM. The history of electroconvulsive therapy in the United States and its place in American psychiatry: a personal memoir. Compr Psychiatry. 1999;40:173–181. doi: 10.1016/s0010-440x(99)90000-7. [DOI] [PubMed] [Google Scholar]
- Leclerc E, Mansur RB, Brietzke E. Determinants of adherence to treatment in bipolar disorder: a comprehensive review. Journal of Affective Disorders. 2013;149:247–252. doi: 10.1016/j.jad.2013.01.036. [DOI] [PubMed] [Google Scholar]
- Lehman D, Meyer JM. Decreased bone mineral density in male schizophrenia patients. Schizophrenia Research. 2005;76:131–133. doi: 10.1016/j.schres.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Leiknes KA, Cooke MJ, Jarosch-von Schweder L, et al. Electroconvulsive therapy during pregnancy: a systematic review of case studies. Arch Womens Ment Health. 2015;18:1–39. doi: 10.1007/s00737-013-0389-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lembke A, Miklowitz D, Otto M, et al. Psychosocial service utilization by patients with bipolar disorder. Biological Psychiatry. 2003;53:52s–52s. [Google Scholar]
- Leon AC, Mallinckrodt CH, Chuang-Stein C, et al. Attrition in randomized controlled clinical trials: methodological issues in psychopharmacology. Biological Psychiatry. 2006;59:1001–1005. doi: 10.1016/j.biopsych.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Leucht S, Cipriani A, Spineli LM, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet (London, England) 2013;382:951–962. doi: 10.1016/S0140-6736(13)60733-3. [DOI] [PubMed] [Google Scholar]
- Leucht S, Hierl S, Kissling W, et al. Putting the efficacy of psychiatric and general medicine medication into perspective: review of meta-analyses. Br J Psychiatry. 2012;200:97–106. doi: 10.1192/bjp.bp.111.096594. [DOI] [PubMed] [Google Scholar]
- Leverich GS, Altshuler LL, Frye MA, et al. Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network. Journal of Clinical Psychiatry. 2003;64:506–515. doi: 10.4088/jcp.v64n0503. [DOI] [PubMed] [Google Scholar]
- Leverich GS, McElroy SL, Suppes T, et al. Early physical and sexual abuse associated with an adverse course of bipolar illness. Biol Psychiatry. 2002;51:288–297. doi: 10.1016/s0006-3223(01)01239-2. [DOI] [PubMed] [Google Scholar]
- Li C-T, Bai Y-M, Huang Y-L, et al. Association between antidepressant resistance in unipolar depression and subsequent bipolar disorder: cohort study. The British journal of psychiatry : the journal of mental science. 2012;200:45–51. doi: 10.1192/bjp.bp.110.086983. [DOI] [PubMed] [Google Scholar]
- Li XB, Tang YL, Wang CY, et al. Clozapine for treatment-resistant bipolar disorder: a systematic review. Bipolar Disord. 2015;17:235–247. doi: 10.1111/bdi.12272. [DOI] [PubMed] [Google Scholar]
- Lieb K, Vollm B, Rucker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. The British journal of psychiatry : the journal of mental science. 2010;196:4–12. doi: 10.1192/bjp.bp.108.062984. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Stroup TS, Mcevoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New England Journal of Medicine. 2005;353:1209–1223. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- Lingam R, Scott J. Treatment non-adherence in affective disorders. Acta Psychiatr Scand. 2002;105:164–172. doi: 10.1034/j.1600-0447.2002.1r084.x. [DOI] [PubMed] [Google Scholar]
- Lingford-Hughes AR, Welch S, Peters L, et al. BAP updated guidelines: evidence-based guidelines for the pharmacological management of substance abuse, harmful use, addiction and comorbidity: recommendations from BAP. Journal of psychopharmacology (Oxford, England) 2012;26:899–952. doi: 10.1177/0269881112444324. [DOI] [PubMed] [Google Scholar]
- Lish JD, Dime-Meenan S, Whybrow PC, et al. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994;31:281–294. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- Llorca P-M, Abbar M, Courtet P, et al. Guidelines for the use and management of long-acting injectable antipsychotics in serious mental illness. BMC psychiatry. 2013;13:340. doi: 10.1186/1471-244X-13-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd J, Doll H, Hawton K, et al. How psychological symptoms relate to different motivations for gambling: an online study of internet gamblers. Biological Psychiatry. 2010;68:733–740. doi: 10.1016/j.biopsych.2010.03.038. [DOI] [PubMed] [Google Scholar]
- Lloyd T, Jones PB. The epidemiology of first-onset mania. In: Tsuang MT, Tohen M, editors. Textbook in psychiatric epidemiology. New York; Chichester: Wiley-Liss; 2002. pp. 445–458. [Google Scholar]
- Lobban F, Taylor L, Chandler C, et al. Enhanced relapse prevention for bipolar disorder by community mental health teams: cluster feasibility randomised trial. Br J Psychiatry. 2010;196:59–63. doi: 10.1192/bjp.bp.109.065524. [DOI] [PubMed] [Google Scholar]
- Loebel A, Cucchiaro J, Silva R, et al. Lurasidone monotherapy in the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. The American journal of psychiatry. 2014a;171:160–168. doi: 10.1176/appi.ajp.2013.13070984. [DOI] [PubMed] [Google Scholar]
- Loebel A, Cucchiaro J, Silva R, et al. Lurasidone as adjunctive therapy with lithium or valproate for the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. The American journal of psychiatry. 2014b;171:169–177. doi: 10.1176/appi.ajp.2013.13070985. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Batchelor DH. Depot neuroleptics and manic depressive psychosis. IntClin Psychopharmacol. 1986;1(Suppl 1):53–62. [PubMed] [Google Scholar]
- Lundh A, Sismondo S, Lexchin J, et al. Industry sponsorship and research outcome. The Cochrane database of systematic reviews. 2012;12:MR000033. doi: 10.1002/14651858.MR000033.pub2. [DOI] [PubMed] [Google Scholar]
- MacCabe JH, Lambe MP, Cnattingius S, et al. Excellent school performance at age 16 and risk of adult bipolar disorder: national cohort study. Br J Psychiatry. 2010;196:109–115. doi: 10.1192/bjp.bp.108.060368. [DOI] [PubMed] [Google Scholar]
- MacQueen GM, Young LT, Joffe RT. A review of psychosocial outcome in patients with bipolar disorder. Acta PsychiatrScand. 2001;103:163–170. doi: 10.1034/j.1600-0447.2001.00059.x. [DOI] [PubMed] [Google Scholar]
- Macritchie K, Geddes JR, Scott J, et al. Valproate for acute mood episodes in bipolar disorder (Cochrane Review) Cochrane Database Syst Rev. 2003:CD004052. doi: 10.1002/14651858.CD004052. [DOI] [PubMed] [Google Scholar]
- Maj M, Pirozzi R, Formicola AM, et al. Reliability and validity of the DSM-IV diagnostic category of schizoaffective disorder: preliminary data. JAffectDisord. 2000;57:95–98. doi: 10.1016/s0165-0327(99)00059-2. [DOI] [PubMed] [Google Scholar]
- Maj M, Pirozzi R, Formicola AM, et al. Reliability and validity of four alternative definitions of rapid-cycling bipolar disorder. Am J Psychiatry. 1999;156:1421–1424. doi: 10.1176/ajp.156.9.1421. [DOI] [PubMed] [Google Scholar]
- Marangell LB, Suppes T, Zboyan HA, et al. A 1-year pilot study of vagus nerve stimulation in treatment-resistant rapid-cycling bipolar disorder. Journal of Clinical Psychiatry. 2008;69:183–189. doi: 10.4088/jcp.v69n0203. [DOI] [PubMed] [Google Scholar]
- Marcus R, Khan A, Rollin L, et al. Efficacy of aripiprazole adjunctive to lithium or valproate in the long-term treatment of patients with bipolar I disorder with an inadequate response to lithium or valproate monotherapy: a multicenter, double-blind, randomized study. Bipolar Disorders. 2011;13:133–144. doi: 10.1111/j.1399-5618.2011.00898.x. [DOI] [PubMed] [Google Scholar]
- Martinez-Aran A, Vieta E, Reinares M, et al. Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. American Journal of Psychiatry. 2004;161:262–270. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- Matthews M, Abdullah S, Gay G, et al. Tracking Mental Well-Being: Balancing Rich Sensing and Patient Needs. Computer. 2014;47:36–43. [Google Scholar]
- McCombs JS, Ahn J, Tencer T, et al. The impact of unrecognized bipolar disorders among patients treated for depression with antidepressants in the fee-for-services California Medicaid (Medi-Cal) program: A 6-year retrospective analysis. Journal of Affective Disorders. 2007;97:171–179. doi: 10.1016/j.jad.2006.06.018. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Keck P-EJ, Strakowski SM. Mania, psychosis, and antipsychotics. J Clin Psychiatry. 1996;57(Suppl 3):14–26. [PubMed] [Google Scholar]
- McElroy SL, Weisler RH, Chang W, et al. A double-blind, placebo-controlled study of quetiapine and paroxetine as monotherapy in adults with bipolar depression (EMBOLDEN II) The Journal of clinical psychiatry. 2010;71:163–174. doi: 10.4088/JCP.08m04942gre. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Tanti C, Stokes R, et al. headspace: Australia's National Youth Mental Health Foundation--where young minds come first. Med J Aust. 2007;187:S68–70. doi: 10.5694/j.1326-5377.2007.tb01342.x. [DOI] [PubMed] [Google Scholar]
- McInerney SJ, Kennedy SH. Review of evidence for use of antidepressants in bipolar depression. The primary care companion for CNS disorders. 2014;16 doi: 10.4088/PCC.14r01653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre RS, Soczynska JK, Bottas A, et al. Anxiety disorders and bipolar disorder: a review. Bipolar Disorders. 2006;8:665–676. doi: 10.1111/j.1399-5618.2006.00355.x. [DOI] [PubMed] [Google Scholar]
- McKnight RF, Adida M, Budge K, et al. Lithium toxicity profile: a systematic review and meta-analysis. Lancet (London, England) 2012;379:721–728. doi: 10.1016/S0140-6736(11)61516-X. [DOI] [PubMed] [Google Scholar]
- Medda P, Toni C, Mariani MG, et al. Electroconvulsive therapy in 197 patients with a severe, drug-resistant bipolar mixed state: treatment outcome and predictors of response. The Journal of clinical psychiatry. 2015;76:1168–1173. doi: 10.4088/JCP.14m09181. [DOI] [PubMed] [Google Scholar]
- Mendez MF. Mania in neurologic disorders. Curr Psychiatry Rep. 2000;2:440–445. doi: 10.1007/s11920-000-0030-6. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64:543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Lamers F. The 'true' prevalence of bipolar II disorder. Curr Opin Psychiatry. 2012;25:19–23. doi: 10.1097/YCO.0b013e32834de3de. [DOI] [PubMed] [Google Scholar]
- Meyer JM, Koro CE. The effects of antipsychotic therapy on serum lipids: a comprehensive review. Schizophrenia Research. 2004;70:1–17. doi: 10.1016/j.schres.2004.01.014. [DOI] [PubMed] [Google Scholar]
- Meyer TD, Hammelstein P, Nilsson LG, et al. The Hypomania Checklist (HCL-32): its factorial structure and association to indices of impairment in German and Swedish nonclinical samples. Compr Psychiatry. 2007;48:79–87. doi: 10.1016/j.comppsych.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Meyer TD, Hautzinger M. Cognitive behaviour therapy and supportive therapy for bipolar disorders: relapse rates for treatment period and 2-year follow-up. Psychological Medicine. 2012;42:1429–1439. doi: 10.1017/S0033291711002522. [DOI] [PubMed] [Google Scholar]
- Michl J, Scharinger C, Zauner M, et al. A multivariate approach linking reported side effects of clinical antidepressant and antipsychotic trials to in vitro binding affinities. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2014;24:1463–1474. doi: 10.1016/j.euroneuro.2014.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ. Intervening early in children with bipolar disorder: is there a pot at the end of the Rainbow? Evidence-based mental health. 2015;18:65–66. doi: 10.1136/eb-2015-102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Goodwin GM, Bauer MS, et al. Common and specific elements of psychosocial treatments for bipolar disorder: a survey of clinicians participating in randomized trials. Journal of psychiatric practice. 2008;14:77–85. doi: 10.1097/01.pra.0000314314.94791.c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Price J, Holmes EA, et al. Facilitated Integrated Mood Management for adults with bipolar disorder. Bipolar Disorders. 2012;14:185–197. doi: 10.1111/j.1399-5618.2012.00998.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell PB. Bipolar disorder and anxiety: a comorbidity needing better treatments. The Lancet Psychiatry. 2015;2:671–672. doi: 10.1016/S2215-0366(15)00209-6. [DOI] [PubMed] [Google Scholar]
- Mitchell PB, Goodwin GM, Johnson GF, et al. Diagnostic guidelines for bipolar depression: a probabilistic approach. Bipolar Disord. 2008;10:144–152. doi: 10.1111/j.1399-5618.2007.00559.x. [DOI] [PubMed] [Google Scholar]
- Mitchell PB, Wilhelm K, Parker G, et al. The clinical features of bipolar depression: a comparison with matched major depressive disorder patients. J Clin Psychiatry. 2001;62:212–216. [PubMed] [Google Scholar]
- Miura T, Noma H, Furukawa TA, et al. Comparative efficacy and tolerability of pharmacological treatments in the maintenance treatment of bipolar disorder: a systematic review and network meta-analysis. The Lancet Psychiatry. 2014;1:351–359. doi: 10.1016/S2215-0366(14)70314-1. [DOI] [PubMed] [Google Scholar]
- Mizrahi R, Rusjan P, Agid O, et al. Adverse subjective experience with antipsychotics and its relationship to striatal and extrastriatal D-2 receptors: A PET study in schizophrenia. American Journal of Psychiatry. 2007;164:630–637. doi: 10.1176/ajp.2007.164.4.630. [DOI] [PubMed] [Google Scholar]
- Modabbernia A, Taslimi S, Brietzke E, et al. Cytokine alterations in bipolar disorder: a meta-analysis of 30 studies. Biol Psychiatry. 2013;74:15–25. doi: 10.1016/j.biopsych.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Moller HJ, Bottlender R, Grunze H, et al. Are antidepressants less effective in the acute treatment of bipolar I compared to unipolar depression? J Affect Disord. 2001;67:141–146. doi: 10.1016/s0165-0327(01)00449-9. [DOI] [PubMed] [Google Scholar]
- Moller HJ, Grunze H. Have some guidelines for the treatment of acute bipolar depression gone too far in the restriction of antidepressants? Eur Arch Psychiatry Clin Neurosci. 2000;250:57–68. doi: 10.1007/s004060070035. [DOI] [PubMed] [Google Scholar]
- Monaco F, Cicolin A. Interactions between anticonvulsant and psychoactive drugs. Epilepsia. 1999;40(Suppl 10):S71–S76. doi: 10.1111/j.1528-1157.1999.tb00888.x. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Schatzberg AF, Guelfi JD, et al. Pharmacotherapy of depression and mixed states in bipolar disorder. J Affect Disord. 2000;59(Suppl 1):S39–S56. doi: 10.1016/s0165-0327(00)00178-6. [DOI] [PubMed] [Google Scholar]
- Moreno C, Hasin DS, Arango C, et al. Depression in bipolar disorder versus major depressive disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Bipolar Disorders. 2012;14:271–282. doi: 10.1111/j.1399-5618.2012.01009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64:1032–1039. doi: 10.1001/archpsyc.64.9.1032. [DOI] [PubMed] [Google Scholar]
- Morriss R, Marshall M, Harris A. Bipolar affective disorder-left out in the cold. Too late for the national service framework but local initiatives may be possible. BMJ. 2002;324:61–62. doi: 10.1136/bmj.324.7329.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morriss RK, Faizal MA, Jones AP, et al. Interventions for helping people recognise early signs of recurrence in bipolar disorder. The Cochrane database of systematic reviews. 2007:CD004854. doi: 10.1002/14651858.CD004854.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mt-Isa S, Hallgreen CE, Wang N, et al. Balancing benefit and risk of medicines: a systematic review and classification of available methodologies. Pharmacoepidemiol Drug Saf. 2014;23:667–678. doi: 10.1002/pds.3636. [DOI] [PubMed] [Google Scholar]
- Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years' experience. Am J Psychiatry. 1994;151:169–176. doi: 10.1176/ajp.151.2.169. [DOI] [PubMed] [Google Scholar]
- Muralidharan K, Ali M, Silveira LE, et al. Efficacy of second generation antipsychotics in treating acute mixed episodes in bipolar disorder: A meta-analysis of placebo-controlled trials. Journal of Affective Disorders. 2013;150:408–414. doi: 10.1016/j.jad.2013.04.032. [DOI] [PubMed] [Google Scholar]
- Naranjo CA, Herrmann N, Mittmann N, et al. Recent advances in geriatric psychopharmacology. Drugs Aging. 1995;7:184–202. doi: 10.2165/00002512-199507030-00004. [DOI] [PubMed] [Google Scholar]
- Narayan V, Haddad PM. Antidepressant discontinuation manic states: a critical review of the literature and suggested diagnostic criteria. Journal of psychopharmacology (Oxford, England) 2011;25:306–313. doi: 10.1177/0269881109359094. [DOI] [PubMed] [Google Scholar]
- Nicholas J, Larsen ME, Proudfoot J, et al. Mobile Apps for Bipolar Disorder: A Systematic Review of Features and Content Quality. Journal of medical Internet research. 2015;17:e198. doi: 10.2196/jmir.4581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nierenberg AA, Ostacher MJ, Calabrese JR, et al. Treatment-resistant bipolar depression: a STEP-BD equipoise randomized effectiveness trial of antidepressant augmentation with lamotrigine, inositol, or risperidone. Am J Psychiatry. 2006;163:210–216. doi: 10.1176/appi.ajp.163.2.210. [DOI] [PubMed] [Google Scholar]
- Nolen WA, Weisler RH. The association of the effect of lithium in the maintenance treatment of bipolar disorder with lithium plasma levels: a post hoc analysis of a double-blind study comparing switching to lithium or placebo in patients who responded to quetiapine (Trial 144) Bipolar Disorders. 2013;15:100–109. doi: 10.1111/bdi.12027. [DOI] [PubMed] [Google Scholar]
- Nutt DJ, King LA, Phillips LD, et al. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–1565. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- Nutt DJ, Sharpe M. Uncritical positive regard? Issues in the efficacy and safety of psychotherapy. Journal of psychopharmacology (Oxford, England) 2008;22:3–6. doi: 10.1177/0269881107086283. [DOI] [PubMed] [Google Scholar]
- O'Brien A. Comparing the risk of tardive dyskinesia in older adults with first-generation and second-generation antipsychotics: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2015 doi: 10.1002/gps.4399. [DOI] [PubMed] [Google Scholar]
- Oates M. Suicide: the leading cause of maternal death. British Journal of Psychiatry. 2003;183:279–281. doi: 10.1192/bjp.183.4.279. [DOI] [PubMed] [Google Scholar]
- Ogawa Y, Tajika A, Takeshima N, et al. Mood stabilizers and antipsychotics for acute mania: a systematic review and meta-analysis of combination/augmentation therapy versus monotherapy. Cns Drugs. 2014;28:989–1003. doi: 10.1007/s40263-014-0197-8. [DOI] [PubMed] [Google Scholar]
- Okuma T, Kishimoto A. A history of investigation on the mood stabilizing effect of carbamazepine in Japan. Psychiatry Clin Neurosci. 1998;52:3–12. doi: 10.1111/j.1440-1819.1998.tb00966.x. [DOI] [PubMed] [Google Scholar]
- Omtzigt JG, Los FJ, Grobbee DE, et al. The risk of spina bifida aperta after first-trimester exposure to valproate in a prenatal cohort. Neurology. 1992;42:119–125. [PubMed] [Google Scholar]
- Oquendo MA, Lizardi D, Greenwald S, et al. Rates of lifetime suicide attempt and rates of lifetime major depression in different ethnic groups in the United States. Acta Psychiatrica Scandinavica. 2004;110:446–451. doi: 10.1111/j.1600-0447.2004.00404.x. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Waternaux C, Brodsky B, et al. Suicidal behavior in bipolar mood disorder: clinical characteristics of attempters and nonattempters. Journal of Affective Disorders. 2000;59:107–117. doi: 10.1016/s0165-0327(99)00129-9. [DOI] [PubMed] [Google Scholar]
- Osborn DPJ, Levy G, Nazareth I, et al. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom's General Practice Research Database. Archives of General Psychiatry. 2007;64:242–249. doi: 10.1001/archpsyc.64.2.242. [DOI] [PubMed] [Google Scholar]
- Pacchiarotti I, Bond DJ, Baldessarini RJ, et al. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. The American journal of psychiatry. 2013;170:1249–1262. doi: 10.1176/appi.ajp.2013.13020185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacchiarotti I, Murru A, Kotzalidis GD, et al. Hyperprolactinemia and medications for bipolar disorder: systematic review of a neglected issue in clinical practice. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2015;25:1045–1059. doi: 10.1016/j.euroneuro.2015.04.007. [DOI] [PubMed] [Google Scholar]
- Pande AC, Crockatt JG, Janney CA, et al. Gabapentin in bipolar disorder: a placebo-controlled trial of adjunctive therapy. Gabapentin Bipolar Disorder Study Group. Bipolar Disord. 2000;2:249–255. doi: 10.1034/j.1399-5618.2000.20305.x. [DOI] [PubMed] [Google Scholar]
- Parikh SV, Zaretsky A, Beaulieu S, et al. A randomized controlled trial of psychoeducation or cognitive-behavioral therapy in bipolar disorder: a Canadian Network for Mood and Anxiety treatments (CANMAT) study [CME] The Journal of clinical psychiatry. 2012;73:803–810. doi: 10.4088/JCP.11m07343. [DOI] [PubMed] [Google Scholar]
- Parker G, Tully L, Olley A, et al. SSRIs as mood stabilizers for Bipolar II Disorder? A proof of concept study. Journal of Affective Disorders. 2006;92:205–214. doi: 10.1016/j.jad.2006.01.024. [DOI] [PubMed] [Google Scholar]
- Patel NC, DelBello MP, Bryan HS, et al. Open-label lithium for the treatment of adolescents with bipolar depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:289–297. doi: 10.1097/01.chi.0000194569.70912.a7. [DOI] [PubMed] [Google Scholar]
- Paton C, Adroer R, Barnes TRE. Monitoring lithium therapy: the impact of a quality improvement programme in the UK. Bipolar Disorders. 2013;15:865–875. doi: 10.1111/bdi.12128. [DOI] [PubMed] [Google Scholar]
- Paton C, Crawford MJ, Bhatti SF, et al. The use of psychotropic medication in patients with emotionally unstable personality disorder under the care of UK mental health services. J Clin Psychiatry. 2015;76:e512–518. doi: 10.4088/JCP.14m09228. [DOI] [PubMed] [Google Scholar]
- Pavlova B, Perlis RH, Alda M, et al. Lifetime prevalence of anxiety disorders in people with bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry. 2015;2:710–717. doi: 10.1016/S2215-0366(15)00112-1. [DOI] [PubMed] [Google Scholar]
- Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164:549–550. doi: 10.1192/bjp.164.4.549. [DOI] [PubMed] [Google Scholar]
- Perlick D, Clarkin JF, Sirey J, et al. Burden experienced by care-givers of persons with bipolar affective disorder. Br J Psychiatry. 1999;175:56–62. doi: 10.1192/bjp.175.1.56. [DOI] [PubMed] [Google Scholar]
- Perry A, Tarrier N, Morriss R, et al. Randomised controlled trial of efficacy of teaching patients with bipolar disorder to identify early symptoms of relapse and obtain treatment. BMJ. 1999;318:149–153. doi: 10.1136/bmj.318.7177.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perugi G, Angst J, Azorin JM, et al. Mixed Features in Patients With a Major Depressive Episode: the BRIDGE-II-MIX Study. Journal of Clinical Psychiatry. 2015;76:E351–E358. doi: 10.4088/JCP.14m09092. [DOI] [PubMed] [Google Scholar]
- Petrides G, Tobias KG, Kellner CH, et al. Continuation and maintenance electroconvulsive therapy for mood disorders: review of the literature. Neuropsychobiology. 2011;64:129–140. doi: 10.1159/000328943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips L, Fasolo M, Zafiropoulos N, et al. Is quantitative benefit–risk modelling of drugs desirable or possible? Drug Discovery Today: Technologies. 2011;8:e3–10. doi: 10.1016/j.ddtec.2011.03.001. [DOI] [PubMed] [Google Scholar]
- Pompili M, Gonda X, Serafini G, et al. Epidemiology of suicide in bipolar disorders: a systematic review of the literature. Bipolar Disord. 2013;15:457–490. doi: 10.1111/bdi.12087. [DOI] [PubMed] [Google Scholar]
- Popovic D, Reinares M, Goikolea JM, et al. Polarity index of pharmacological agents used for maintenance treatment of bipolar disorder. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2012;22:339–346. doi: 10.1016/j.euroneuro.2011.09.008. [DOI] [PubMed] [Google Scholar]
- Popovic D, Torrent C, Goikolea JM, et al. Clinical implications of predominant polarity and the polarity index in bipolar disorder: a naturalistic study. Acta Psychiatrica Scandinavica. 2014;129:366–374. doi: 10.1111/acps.12179. [DOI] [PubMed] [Google Scholar]
- Posner K, Oquendo MA, Gould M, et al. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants. The American Journal of Psychiatry. 2007;164:1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry. 2006;189:124–131. doi: 10.1192/bjp.bp.105.013045. [DOI] [PubMed] [Google Scholar]
- Post RM, Denicoff KD, Frye MA, et al. A history of the use of anticonvulsants as mood stabilizers in the last two decades of the 20th century. Neuropsychobiology. 1998;38:152–166. doi: 10.1159/000026532. [DOI] [PubMed] [Google Scholar]
- Post RM, Ketter TA, Pazzaglia PJ, et al. Rational polypharmacy in the bipolar affective disorders. Epilepsy Res Suppl. 1996;11:153–180. [PubMed] [Google Scholar]
- Potash JB, DePaulo J-RJ. Searching high and low: a review of the genetics of bipolar disorder. Bipolar Disord. 2000;2:8–26. doi: 10.1034/j.1399-5618.2000.020103.x. [DOI] [PubMed] [Google Scholar]
- Powell J, Geddes J, Deeks J, et al. Suicide in psychiatric hospital in-patients - Risk factors and their predictive power. British Journal of Psychiatry. 2000;176:266–272. doi: 10.1192/bjp.176.3.266. [DOI] [PubMed] [Google Scholar]
- Prescribing Observatory for Mental Health. Topic 7d. Monitoring of patients prescribed lithium: Supplementary report. Prescribing Observatory for Mental Health. 2013 [Google Scholar]
- Preston GA, Marchant BK, Reimherr FW, et al. Borderline personality disorder in patients with bipolar disorder and response to lamotrigine. Journal of Affective Disorders. 2004;79:297–303. doi: 10.1016/S0165-0327(02)00358-0. [DOI] [PubMed] [Google Scholar]
- Prien RF, Kupfer DJ, Mansky PA, et al. Drug therapy in the prevention of recurrences in unipolar and bipolar affective disorders. Report of the NIMH Collaborative Study Group comparing lithium carbonate, imipramine, and a lithium carbonate-imipramine combination. Arch Gen Psychiatry. 1984;41:1096–1104. doi: 10.1001/archpsyc.1983.01790220086014. [DOI] [PubMed] [Google Scholar]
- Quiroz JA, Yatham LN, Palumbo JM, et al. Risperidone long-acting injectable monotherapy in the maintenance treatment of bipolar I disorder. Biological Psychiatry. 2010;68:156–162. doi: 10.1016/j.biopsych.2010.01.015. [DOI] [PubMed] [Google Scholar]
- Read J, van Os J, Morrison AP, et al. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatrica Scandinavica. 2005;112:330–350. doi: 10.1111/j.1600-0447.2005.00634.x. [DOI] [PubMed] [Google Scholar]
- Redlich R, Dohm K, Grotegerd D, et al. Reward Processing in Unipolar and Bipolar Depression: A Functional MRI Study. Neuropsychopharmacology. 2015;40:2623–2631. doi: 10.1038/npp.2015.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinares A, Vieta E, Colom F, et al. What really matters to bipolar patients' caregivers: Sources of family burden. Journal of Affective Disorders. 2006;94:157–163. doi: 10.1016/j.jad.2006.04.022. [DOI] [PubMed] [Google Scholar]
- Reinares M, Colom F, Sanchez-Moreno J, et al. Impact of caregiver group psychoeducation on the course and outcome of bipolar patients in remission: a randomized controlled trial. Bipolar Disorders. 2008;10:511–519. doi: 10.1111/j.1399-5618.2008.00588.x. [DOI] [PubMed] [Google Scholar]
- Rice F, Jones I, Thapar A. The impact of gestational stress and prenatal growth on emotional problems in offspring: a review. Acta Psychiatrica Scandinavica. 2007;115:171–183. doi: 10.1111/j.1600-0447.2006.00895.x. [DOI] [PubMed] [Google Scholar]
- Robertson E, Jones I, Haque S, et al. Risk of puerperal and non-puerperal recurrence of illness following bipolar affective puerperal (post-partum) psychosis. British Journal of Psychiatry. 2005;186:258–259. doi: 10.1192/bjp.186.3.258. [DOI] [PubMed] [Google Scholar]
- Rogers R, Goodwin G. Lithium may reduce gambling severity in pathological gamblers with bipolar disorder. Evidence-based mental health. 2005;8:80. doi: 10.1136/ebmh.8.3.80. [DOI] [PubMed] [Google Scholar]
- Rosa AR, Singh N, Whitaker E, et al. Altered plasma glutathione levels in bipolar disorder indicates higher oxidative stress; a possible risk factor for illness onset despite normal brain-derived neurotrophic factor (BDNF) levels. Psychological Medicine. 2014;44:2409–2418. doi: 10.1017/S0033291714000014. [DOI] [PubMed] [Google Scholar]
- Rosa FW. Spina bifida in infants of women treated with carbamazepine during pregnancy. N Engl J Med. 1991;324:674–677. doi: 10.1056/NEJM199103073241006. [DOI] [PubMed] [Google Scholar]
- Rummel-Kluge C, Komossa K, Schwarz S, et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophrenia Bulletin. 2012;38:167–177. doi: 10.1093/schbul/sbq042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711–1722. doi: 10.1056/NEJMoa064135. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Printz DJ, Kahn DA, et al. The Expert Consensus Guideline Series: Medication Treatment of Bipolar Disorder 2000. Postgrad Med. 2000 Spec No: 1-104. [PubMed] [Google Scholar]
- Sajatovic M. Treatment of bipolar disorder in older adults. Int J Geriatr Psychiatry. 2002;17:865–873. doi: 10.1002/gps.719. [DOI] [PubMed] [Google Scholar]
- Salloum IM, Thase ME. Impact of substance abuse on the course and treatment of bipolar disorder. Bipolar Disord. 2000;2:269–280. doi: 10.1034/j.1399-5618.2000.20308.x. [DOI] [PubMed] [Google Scholar]
- Samren EB, van Duijn CM, Christiaens GC, et al. Antiepileptic drug regimens and major congenital abnormalities in the offspring. Ann Neurol. 1999;46:739–746. [PubMed] [Google Scholar]
- Santos Pina L, Bouckaert F, Obbels J, et al. Maintenance Electroconvulsive Therapy in Severe Bipolar Disorder: A Retrospective Chart Review. The journal of ECT. 2015 doi: 10.1097/YCT.0000000000000253. [DOI] [PubMed] [Google Scholar]
- Sato T, Bottlender R, Kleindienst N, et al. Syndromes and phenomenological subtypes underlying acute mania: a factor analytic study of 576 manic patients. Am J Psychiatry. 2002;159:968–974. doi: 10.1176/appi.ajp.159.6.968. [DOI] [PubMed] [Google Scholar]
- Saunders KEA, Bilderbeck AC, Price J, et al. Distinguishing bipolar disorder from borderline personality disorder: A study of current clinical practice. European psychiatry : the journal of the Association of European Psychiatrists. 2015;30:965–974. doi: 10.1016/j.eurpsy.2015.09.007. [DOI] [PubMed] [Google Scholar]
- Savitz JB, van der Merwe L, Stein DJ, et al. Neuropsychological task performance in bipolar spectrum illness: genetics, alcohol abuse, medication and childhood trauma. Bipolar Disorders. 2008;10:479–494. doi: 10.1111/j.1399-5618.2008.00591.x. [DOI] [PubMed] [Google Scholar]
- Schaffer A, Isometsa ET, Azorin JM, et al. A review of factors associated with greater likelihood of suicide attempts and suicide deaths in bipolar disorder: Part II of a report of the International Society for Bipolar Disorders Task Force on Suicide in Bipolar Disorder. Aust N Z J Psychiatry. 2015;49:1006–1020. doi: 10.1177/0004867415594428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schalkwijk S, Undurraga J, Tondo L, et al. Declining efficacy in controlled trials of antidepressants: effects of placebo dropout. The international journal of neuropsychopharmacology / official scientific journal of the Collegium Internationale Neuropsychopharmacologicum (CINP) 2014;17:1343–1352. doi: 10.1017/S1461145714000224. [DOI] [PubMed] [Google Scholar]
- Schoeyen HK, Kessler U, Andreassen OA, et al. Treatment-resistant bipolar depression: a randomized controlled trial of electroconvulsive therapy versus algorithm-based pharmacological treatment. The American journal of psychiatry. 2015;172:41–51. doi: 10.1176/appi.ajp.2014.13111517. [DOI] [PubMed] [Google Scholar]
- Scott J. Cognitive therapy of affective disorders: a review. J Affect Disord. 1996;37:1–11. doi: 10.1016/0165-0327(95)00069-0. [DOI] [PubMed] [Google Scholar]
- Scott J, Colom F, Vieta E. A meta-analysis of relapse rates with adjunctive psychological therapies compared to usual psychiatric treatment for bipolar disorders. The international journal of neuropsychopharmacology / official scientific journal of the Collegium Internationale Neuropsychopharmacologicum (CINP) 2007;10:123–129. doi: 10.1017/S1461145706006900. [DOI] [PubMed] [Google Scholar]
- Scott J, Garland A, Moorhead S. A pilot study of cognitive therapy in bipolar disorders. Psychological Medicine. 2001;31:459–467. doi: 10.1017/s0033291701003373. [DOI] [PubMed] [Google Scholar]
- Scott J, Paykel E, Morriss R, et al. Cognitive-behavioural therapy for severe and recurrent bipolar disorders - Randomised controlled trial. British Journal of Psychiatry. 2006;188:313–320. doi: 10.1192/bjp.188.4.313. [DOI] [PubMed] [Google Scholar]
- Scott J, Pope M. Nonadherence with mood stabilizers: prevalence and predictors. J Clin Psychiatry. 2002;63:384–390. doi: 10.4088/jcp.v63n0502. [DOI] [PubMed] [Google Scholar]
- Scott J, Stanton B, Garland A, et al. Cognitive vulnerability in patients with bipolar disorder. Psychol Med. 2000;30:467–472. doi: 10.1017/s0033291799008879. [DOI] [PubMed] [Google Scholar]
- Severus E, Taylor MJ, Sauer C, et al. Lithium for prevention of mood episodes in bipolar disorders: systematic review and meta-analysis. International journal of bipolar disorders. 2014;2:15. doi: 10.1186/s40345-014-0015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah A, Carreno FR, Frazer A. Therapeutic modalities for treatment resistant depression: focus on vagal nerve stimulation and ketamine. Clin Psychopharmacol Neurosci. 2014;12:83–93. doi: 10.9758/cpn.2014.12.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shekelle PG, Woolf SH, Eccles M, et al. Clinical guidelines: developing guidelines. BMJ. 1999;318:593–596. doi: 10.1136/bmj.318.7183.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidor MM, Macqueen GM. Antidepressants for the acute treatment of bipolar depression: a systematic review and meta-analysis. The Journal of clinical psychiatry. 2011;72:156–167. doi: 10.4088/JCP.09r05385gre. [DOI] [PubMed] [Google Scholar]
- Simon GE, Ludman EJ, Bauer MS, et al. Long-term effectiveness and cost of a systematic care program for bipolar disorder. Archives of General Psychiatry. 2006;63:500–508. doi: 10.1001/archpsyc.63.5.500. [DOI] [PubMed] [Google Scholar]
- Simon NM, Otto MW, Wisniewski SR, et al. Anxiety disorder comorbidity in bipolar disorder patients: Data from the first 500 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD) American Journal of Psychiatry. 2004;161:2222–2229. doi: 10.1176/appi.ajp.161.12.2222. [DOI] [PubMed] [Google Scholar]
- Singh MK, Ketter TA, Chang KD. Atypical antipsychotics for acute manic and mixed episodes in children and adolescents with bipolar disorder: efficacy and tolerability. Drugs. 2010;70:433–442. doi: 10.2165/11534540-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LA, Cornelius VR, Azorin JM, et al. Valproate for the treatment of acute bipolar depression: systematic review and meta-analysis. Journal of Affective Disorders. 2010;122:1–9. doi: 10.1016/j.jad.2009.10.033. [DOI] [PubMed] [Google Scholar]
- Smith LF, Whitfield MJ. Women's knowledge of taking oral contraceptive pills correctly and of emergency contraception: effect of providing information leaflets in general practice. Br J Gen Pract. 1995;45:409–414. [PMC free article] [PubMed] [Google Scholar]
- Song J, Sjolander A, Bergen S, et al. Suicidal behavior during lithium and valproate medication for bipolar disorder: a register based study. 2015 [Google Scholar]
- Sproule BA, Hardy BG, Shulman KI. Differential pharmacokinetics of lithium in elderly patients. Drugs Aging. 2000;16:165–177. doi: 10.2165/00002512-200016030-00002. [DOI] [PubMed] [Google Scholar]
- Staring ABP, Van der Gaag M, Koopmans GT, et al. Treatment adherence therapy in people with psychotic disorders: randomised controlled trial. The British journal of psychiatry : the journal of mental science. 2010;197:448–455. doi: 10.1192/bjp.bp.110.077289. [DOI] [PubMed] [Google Scholar]
- Straker D, Correll CU, Kramer-Ginsberg E, et al. Cost-effective screening for the metabolic syndrome in patients treated with second-generation antipsychotic medications. American Journal of Psychiatry. 2005;162:1217–1211U1210. doi: 10.1176/appi.ajp.162.6.1217. [DOI] [PubMed] [Google Scholar]
- Strakowski SM, DelBello MP, Fleck DE, et al. The impact of substance abuse on the course of bipolar disorder. Biol Psychiatry. 2000;48:477–485. doi: 10.1016/s0006-3223(00)00900-8. [DOI] [PubMed] [Google Scholar]
- Strakowski SM, MeElroy SL, Keck P-WJ, et al. The co-occurrence of mania with medical and other psychiatric disorders. Int J Psychiatry Med. 1994;24:305–328. doi: 10.2190/CM8E-46R5-9AJL-03FN. [DOI] [PubMed] [Google Scholar]
- Stratford HJ, Cooper MJ, Di Simplicio M, et al. Psychological therapy for anxiety in bipolar spectrum disorders: a systematic review. Clinical psychology review. 2015;35:19–34. doi: 10.1016/j.cpr.2014.11.002. [DOI] [PubMed] [Google Scholar]
- Suppes T, Baldessarini RJ, Faedda GL, et al. Risk of recurrence following discontinuation of lithium treatment in bipolar disorder. Archives of General Psychiatry. 1991;48:1082–1088. doi: 10.1001/archpsyc.1991.01810360046007. [DOI] [PubMed] [Google Scholar]
- Suppes T, Frank E, DePaulo JR, et al. Letter to the editor in response to 2012 article by Frances and Jones. Bipolar Disord. 2014;16:214–215. doi: 10.1111/bdi.12176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suppes T, Vieta E, Gustafsson U, et al. Maintenance Treatment with Quetiapine When Combined with Either Lithium or Divalproex in Bipolar I Disorder: Analysis of Two Large Randomized, Placebo-Controlled Trials. Depression and Anxiety. 2013;30:1089–1098. doi: 10.1002/da.22136. [DOI] [PubMed] [Google Scholar]
- Suppes T, Vieta E, Liu S, et al. Maintenance treatment for patients with bipolar I disorder: results from a north american study of quetiapine in combination with lithium or divalproex (trial 127) The American journal of psychiatry. 2009;166:476–488. doi: 10.1176/appi.ajp.2008.08020189. [DOI] [PubMed] [Google Scholar]
- Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trial of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry. 1999;156:1164–1169. doi: 10.1176/ajp.156.8.1164. [DOI] [PubMed] [Google Scholar]
- Swartz HA, Frank E. Psychotherapy for bipolar depression: a phase-specific treatment strategy? Bipolar Disord. 2001;3:11–22. doi: 10.1034/j.1399-5618.2001.030102.x. [DOI] [PubMed] [Google Scholar]
- Taylor DM, Cornelius V, Smith L, et al. Comparative efficacy and acceptability of drug treatments for bipolar depression: a multiple-treatments meta-analysis. Acta Psychiatrica Scandinavica. 2014;130:452–469. doi: 10.1111/acps.12343. [DOI] [PubMed] [Google Scholar]
- ten Have M, Vollebergh W, Bijl R, et al. Bipolar disorder in the general population in The Netherlands (prevalence, consequences and care utilisation): results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) J Affect Disord. 2002;68:203–213. doi: 10.1016/s0165-0327(00)00310-4. [DOI] [PubMed] [Google Scholar]
- Terp IM, Mortensen PB. Post-partum psychoses. Clinical diagnoses and relative risk of admission after parturition. Br J Psychiatry. 1998;172:521–526. doi: 10.1192/bjp.172.6.521. [DOI] [PubMed] [Google Scholar]
- Thase ME, Jonas A, Khan A, et al. Aripiprazole monotherapy in non-psychotic bipolar I depression. Journal of Clinical Psychopharmacology. 2008a;28:13–20. doi: 10.1097/jcp.0b013e3181618eb4. [DOI] [PubMed] [Google Scholar]
- Thase ME, Macfadden W, Weisler RH, et al. Efficacy of quetiapine monotherapy in bipolar I and II depression: a double-blind, placebo-controlled study (the BOLDER II study) J Clin Psychopharmacol. 2006;26:600–609. doi: 10.1097/01.jcp.0000248603.76231.b7. [DOI] [PubMed] [Google Scholar]
- Thase ME, Trivedi MH, Nelson JC, et al. Examining the efficacy of adjunctive aripiprazole in major depressive disorder: a pooled analysis of 2 studies. Primary care companion to the Journal of clinical psychiatry. 2008b;10:440–447. doi: 10.4088/pcc.v10n0603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The UK ECT Review Group. Electroconvulsive therapy - systematic review and meta-analysis of efficacy and safety in depressive disorders. The Lancet. 2003;361:799–808. doi: 10.1016/S0140-6736(03)12705-5. [DOI] [PubMed] [Google Scholar]
- Thies-Flechtner K, Muller-Oerlinghausen B, Seibert W, et al. Effect of prophylactic treatment on suicide risk in patients with major affective disorders. Data from a randomized prospective trial. Pharmacopsychiatry. 1996;29:103–107. doi: 10.1055/s-2007-979553. [DOI] [PubMed] [Google Scholar]
- Tidemalm D, Langstrom N, Lichtenstein P, et al. Risk of suicide after suicide attempt according to coexisting psychiatric disorder: Swedish cohort study with long term follow-up. BMJ. 2008;337:a2205. doi: 10.1136/bmj.a2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tijssen MJA, van Os J, Wittchen HU, et al. Evidence that bipolar disorder is the poor outcome fraction of a common developmental phenotype: an 8-year cohort study in young people. Psychological Medicine. 2010;40:289–299. doi: 10.1017/S0033291709006138. [DOI] [PubMed] [Google Scholar]
- Toffol E, Hatonen T, Tanskanen A, et al. Lithium is associated with decrease in all-cause and suicide mortality in high-risk bipolar patients: A nationwide registry-based prospective cohort study. Journal of Affective Disorders. 2015;183:159–165. doi: 10.1016/j.jad.2015.04.055. [DOI] [PubMed] [Google Scholar]
- Tohen M, Calabrese JR, Sachs GS, et al. Randomized, placebo-controlled trial of olanzapine as maintenance therapy in patients with bipolar I disorder responding to acute treatment with olanzapine. American Journal of Psychiatry. 2006;163:247–256. doi: 10.1176/appi.ajp.163.2.247. [DOI] [PubMed] [Google Scholar]
- Tohen M, Chengappa KNR, Suppes T, et al. Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. The British journal of psychiatry : the journal of mental science. 2004;184:337–345. doi: 10.1192/bjp.184.4.337. [DOI] [PubMed] [Google Scholar]
- Tohen M, Greil W, Calabrese JR, et al. Olanzapine versus lithium in the maintenance treatment of bipolar disorder: A 12-month, randomized, double-blind, controlled clinical trial. American Journal of Psychiatry. 2005;162:1281–1290. doi: 10.1176/appi.ajp.162.7.1281. [DOI] [PubMed] [Google Scholar]
- Tohen M, Katagiri H, Fujikoshi S, et al. Efficacy of olanzapine monotherapy in acute bipolar depression: a pooled analysis of controlled studies. Journal of Affective Disorders. 2013;149:196–201. doi: 10.1016/j.jad.2013.01.022. [DOI] [PubMed] [Google Scholar]
- Tohen M, Khalsa HM, Salvatore P, et al. Two-year outcomes in first-episode psychotic depression the McLean-Harvard First-Episode Project. J Affect Disord. 2012;136:1–8. doi: 10.1016/j.jad.2011.08.028. [DOI] [PubMed] [Google Scholar]
- Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry. 2003;60:1079–1088. doi: 10.1001/archpsyc.60.11.1079. [DOI] [PubMed] [Google Scholar]
- Tondo L, Hennen J, Baldessarini RJ. Lower suicide risk with long-term lithium treatment in major affective illness: a meta-analysis. Acta Psychiatr Scand. 2001;104:163–172. doi: 10.1034/j.1600-0447.2001.00464.x. [DOI] [PubMed] [Google Scholar]
- Tondo L, Isacsson G, Baldessarini RJ. Suicidal behaviour in bipolar disorder - Risk and prevention. Cns Drugs. 2003;17:491–511. doi: 10.2165/00023210-200317070-00003. [DOI] [PubMed] [Google Scholar]
- Tondo L, Vazquez G, Baldessarini RJ. Mania associated with antidepressant treatment: comprehensive meta-analytic review. Acta Psychiatrica Scandinavica. 2010;121:404–414. doi: 10.1111/j.1600-0447.2009.01514.x. [DOI] [PubMed] [Google Scholar]
- Torrent C, Amann B, Sanchez-Moreno J, et al. Weight gain in bipolar disorder: pharmacological treatment as a contributing factor. Acta Psychiatrica Scandinavica. 2008;118:4–18. doi: 10.1111/j.1600-0447.2008.01204.x. [DOI] [PubMed] [Google Scholar]
- Torrent C, Bonnin CdM, Martinez-Aran A, et al. Efficacy of functional remediation in bipolar disorder: a multicenter randomized controlled study. The American journal of psychiatry. 2013;170:852–859. doi: 10.1176/appi.ajp.2012.12070971. [DOI] [PubMed] [Google Scholar]
- Tyrer SP, Brittlebank AD. Misdiagnosis of bipolar affective disorder as personality disorder. Can J Psychiatry. 1993;38:587–589. doi: 10.1177/070674379303800903. [DOI] [PubMed] [Google Scholar]
- Undurraga J, Baldessarini RJ. Randomized, placebo-controlled trials of antidepressants for acute major depression: thirty-year meta-analytic review. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2012;37:851–864. doi: 10.1038/npp.2011.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urry E, Landolt H-P. Adenosine, caffeine, and performance: from cognitive neuroscience of sleep to sleep pharmacogenetics. Current topics in behavioral neurosciences. 2015;25:331–366. doi: 10.1007/7854_2014_274. [DOI] [PubMed] [Google Scholar]
- Vajda FJE, O'Brien TJ, Lander CM, et al. The teratogenicity of the newer antiepileptic drugs - an update. Acta neurologica Scandinavica. 2014;130:234–238. doi: 10.1111/ane.12280. [DOI] [PubMed] [Google Scholar]
- Valenti M, Benabarre A, Garcia-Amador M, et al. Electroconvulsive therapy in the treatment of mixed states in bipolar disorder. European Psychiatry. 2008;23:53–56. doi: 10.1016/j.eurpsy.2007.10.011. [DOI] [PubMed] [Google Scholar]
- Vallarino M, Henry C, Etain B, et al. An evidence map of psychosocial interventions for the earliest stages of bipolar disorder. Lancet Psychiatry. 2015;2:548–563. doi: 10.1016/S2215-0366(15)00156-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valtonen H, Suominen K, Mantere O, et al. Suicidal ideation and attempts in bipolar I and II disorders. Journal of Clinical Psychiatry. 2005;66:1456–1462. doi: 10.4088/jcp.v66n1116. [DOI] [PubMed] [Google Scholar]
- van der Loos MLM, Mulder P, Hartong EGTM, et al. Long-term outcome of bipolar depressed patients receiving lamotrigine as add-on to lithium with the possibility of the addition of paroxetine in nonresponders: a randomized, placebo-controlled trial with a novel design. Bipolar Disorders. 2011;13:111–117. doi: 10.1111/j.1399-5618.2011.00887.x. [DOI] [PubMed] [Google Scholar]
- van der Loos MLM, Mulder PGH, Hartong EGTM, et al. Efficacy and safety of lamotrigine as add-on treatment to lithium in bipolar depression: a multicenter, double-blind, placebo-controlled trial. The Journal of clinical psychiatry. 2009;70:223–231. doi: 10.4088/jcp.08m04152. [DOI] [PubMed] [Google Scholar]
- Van Meter AR, Moreira AL, Youngstrom EA. Meta-analysis of epidemiologic studies of pediatric bipolar disorder. J Clin Psychiatry. 2011;72:1250–1256. doi: 10.4088/JCP.10m06290. [DOI] [PubMed] [Google Scholar]
- Vancampfort D, Vansteelandt K, Correll CU, et al. Metabolic Syndrome and Metabolic Abnormalities in Bipolar Disorder: A Meta-Analysis of Prevalence Rates and Moderators. American Journal of Psychiatry. 2013;170:265–274. doi: 10.1176/appi.ajp.2012.12050620. [DOI] [PubMed] [Google Scholar]
- Vazquez GH, Tondo L, Undurraga J, et al. Overview of antidepressant treatment of bipolar depression. The international journal of neuropsychopharmacology / official scientific journal of the Collegium Internationale Neuropsychopharmacologicum (CINP) 2013;16:1673–1685. doi: 10.1017/S1461145713000023. [DOI] [PubMed] [Google Scholar]
- Vieta E, Angst J, Reed C, et al. Predictors of switching from mania to depression in a large observational study across Europe (EMBLEM) Journal of Affective Disorders. 2009;118:118–123. doi: 10.1016/j.jad.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Vieta E, Calabrese JR, Goikolea JM, et al. Quetiapine monotherapy in the treatment of patients with bipolar I or II depression and a rapid-cycling disease course: a randomized, double-blind, placebo-controlled study. Bipolar Disorders. 2007;9:413–425. doi: 10.1111/j.1399-5618.2007.00479.x. [DOI] [PubMed] [Google Scholar]
- Vieta E, Montgomery S, Sulaiman AH, et al. A randomized, double-blind, placebo-controlled trial to assess prevention of mood episodes with risperidone long-acting injectable in patients with bipolar I disorder. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2012;22:825–835. doi: 10.1016/j.euroneuro.2012.03.004. [DOI] [PubMed] [Google Scholar]
- Vieta E, Suppes T, Eggens I, et al. Efficacy and safety of quetiapine in combination with lithium or divalproex for maintenance of patients with bipolar I disorder (international trial 126) Journal of Affective Disorders. 2008;109:251–263. doi: 10.1016/j.jad.2008.06.001. [DOI] [PubMed] [Google Scholar]
- Vieta E, Torrent C, Martinez-Aran A. Functionl remediation for Bipolar disorder. Cambridge University Press; 2014. [Google Scholar]
- Vieta E, Valenti M. Mixed states in DSM-5: Implications for clinical care, education, and research. Journal of Affective Disorders. 2013;148:28–36. doi: 10.1016/j.jad.2013.03.007. [DOI] [PubMed] [Google Scholar]
- Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157:179–184. doi: 10.1176/appi.ajp.157.2.179. [DOI] [PubMed] [Google Scholar]
- Viktorin A, Lichtenstein P, Thase ME, et al. The risk of switch to mania in patients with bipolar disorder during treatment with an antidepressant alone and in combination with a mood stabilizer. The American journal of psychiatry. 2014;171:1067–1073. doi: 10.1176/appi.ajp.2014.13111501. [DOI] [PubMed] [Google Scholar]
- Wals M, Hillegers MH, Reichart CG, et al. Prevalence of psychopathology in children of a bipolar parent. J Am Acad Child Adolesc Psychiatry. 2001;40:1094–1102. doi: 10.1097/00004583-200109000-00019. [DOI] [PubMed] [Google Scholar]
- Webb RT, Lichtenstein P, Larsson H, et al. Suicide, Hospital-Presenting Suicide Attempts, and Criminality in Bipolar Disorder: Examination of Risk for Multiple Adverse Outcomes. Journal of Clinical Psychiatry. 2014;75:E809–+. doi: 10.4088/JCP.13m08899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehr TA, Sack DA, Rosenthal NE. Sleep reduction as a final common pathway in the genesis of mania. Am J Psychiatry. 1987;144:201–204. doi: 10.1176/ajp.144.2.201. [DOI] [PubMed] [Google Scholar]
- Weisler RH. Continuation of Quetiapine Versus Switching to Placebo or Lithium for Maintenance Treatment of Bipolar I Disorder (Trial 144: A Randomized Controlled Study) (vol 72, pg 1452, 2011) Journal of Clinical Psychiatry. 2014;75 doi: 10.4088/JCP.11m06878. [DOI] [PubMed] [Google Scholar]
- Weisler RH, Calabrese JR, Thase ME, et al. Efficacy of quetiapine monotherapy for the treatment of depressive episodes in bipolar I disorder: A post hoc analysis of combined results from 2 double-blind, randomized, placebo-controlled studies. Journal of Clinical Psychiatry. 2008;69:769–782. doi: 10.4088/jcp.v69n0510. [DOI] [PubMed] [Google Scholar]
- Weisler RH, Nolen WA, Neijber A, et al. Continuation of quetiapine versus switching to placebo or lithium for maintenance treatment of bipolar I disorder (Trial 144: a randomized controlled study) The Journal of clinical psychiatry. 2011;72:1452–1464. doi: 10.4088/JCP.11m06878. [DOI] [PubMed] [Google Scholar]
- Wesseloo R, Kamperman AM, Munk-Olsen T, et al. Risk of Postpartum Relapse in Bipolar Disorder and Postpartum Psychosis: A Systematic Review and Meta-Analysis. Am J Psychiatry. 2015 doi: 10.1176/appi.ajp.2015.15010124. appiajp201515010124. [DOI] [PubMed] [Google Scholar]
- Westman J, Wahlbeck K, Laursen TM, et al. Mortality and life expectancy of people with alcohol use disorder in Denmark, Finland and Sweden. Acta Psychiatrica Scandinavica. 2015;131:297–306. doi: 10.1111/acps.12330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeldon TJ, Robertson C, Eagles JM, et al. The views and outcomes of consenting and non-consenting patients receiving ECT. Psychol Med. 1999;29:221–223. doi: 10.1017/s0033291798007193. [DOI] [PubMed] [Google Scholar]
- Wilson MP, Pepper D, Currier GW, et al. The psychopharmacology of agitation: consensus statement of the american association for emergency psychiatry project Beta psychopharmacology workgroup. West J Emerg Med. 2012;13:26–34. doi: 10.5811/westjem.2011.9.6866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winokur G, Coryell W, Keller M, et al. A prospective follow-up of patients with bipolar and primary unipolar affective disorder. Arch Gen Psychiatry. 1993;50:457–465. doi: 10.1001/archpsyc.1993.01820180059006. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Beaulieu S, Schaffer A, et al. Optimal duration of risperidone or olanzapine adjunctive therapy to mood stabilizer following remission of a manic episode: A CANMAT randomized double-blind trial. Mol Psychiatry. 2015a doi: 10.1038/mp.2015.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatham LN, Vieta E, Goodwin GM, et al. Agomelatine or placebo as adjunctive therapy to a mood stabiliser in bipolar I depression: randomised double-blind placebo-controlled trial. The British Journal of Psychiatry. 2015b doi: 10.1192/bjp.bp.114.147587. [DOI] [PubMed] [Google Scholar]
- Yazici O, Kora K, Polat A, et al. Controlled lithium discontinuation in bipolar patients with good response to long-term lithium prophylaxis. Journal of Affective Disorders. 2004;80:269–271. doi: 10.1016/S0165-0327(03)00133-2. [DOI] [PubMed] [Google Scholar]
- Yildiz A, Nikodem M, Vieta E, et al. A network meta-analysis on comparative efficacy and all-cause discontinuation of antimanic treatments in acute bipolar mania. Psychological Medicine. 2015;45:299–317. doi: 10.1017/S0033291714001305. [DOI] [PubMed] [Google Scholar]
- Yildiz A, Vieta E, Leucht S, et al. Efficacy of antimanic treatments: meta-analysis of randomized, controlled trials. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2011;36:375–389. doi: 10.1038/npp.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip SW, Doherty J, Wakeley J, et al. Reduced subjective response to acute ethanol administration among young men with a broad bipolar phenotype. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2012;37:1808–1815. doi: 10.1038/npp.2012.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AH, McElroy SL, Bauer M, et al. A double-blind, placebo-controlled study of quetiapine and lithium monotherapy in adults in the acute phase of bipolar depression (EMBOLDEN I) The Journal of clinical psychiatry. 2010;71:150–162. doi: 10.4088/JCP.08m04995gre. [DOI] [PubMed] [Google Scholar]
- Young BK, Camicioli R, Ganzini L. Neuropsychiatric adverse effects of antiparkinsonian drugs. Characteristics, evaluation and treatment. Drugs Aging. 1997;10:367–383. doi: 10.2165/00002512-199710050-00005. [DOI] [PubMed] [Google Scholar]
- Youngstrom E, Genzlinger J, Egerton G, et al. Multivariate Meta-Analysis of the Discriminative Validity of Caregiver, Youth, and Teacher Rating Scales for Pediatric Bipolar Disorder: Mother Knows Best About Mania. Archives of Scientific Psychology. 2015;3:112–137. [Google Scholar]
- Youngstrom E, Van Meter A. The state of assessment for pediatric bipolar disorder: it is time to throw away the old textbook. Bipolar Disorders. 2015;17:23–23. [Google Scholar]
- Zanarini MC. Psychotherapy of borderline personality disorder. Acta Psychiatrica Scandinavica. 2009;120:373–377. doi: 10.1111/j.1600-0447.2009.01448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarate CA, Payne JL, Singh J, et al. Pramipexole for bipolar II depression: A placebo-controlled proof of concept study. Biological Psychiatry. 2004;56:54–60. doi: 10.1016/j.biopsych.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Zarate CA, Tohen M. Double-blind comparison of the continued use of antipsychotic treatment versus its discontinuation in remitted manic patients. American Journal of Psychiatry. 2004;161:169–171. doi: 10.1176/appi.ajp.161.1.169. [DOI] [PubMed] [Google Scholar]
- Zhornitsky S, Potvin S, Moteshafi H, et al. Dose-response and comparative efficacy and tolerability of quetiapine across psychiatric disorders: a systematic review of the placebo-controlled monotherapy and add-on trials. Int Clin Psychopharmacol. 2011;26:183–192. doi: 10.1097/YIC.0b013e3283430a0e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.