Abstract
Micronutrients, vitamins and minerals accessible from the diet, are essential for biologic activity. Micronutrient status varies widely throughout pregnancy and across populations. Women in low-income countries often enter pregnancy malnourished, and the demands of gestation can exacerbate micronutrient deficiencies with health consequences to the fetus. Examples of efficacious single micronutrient interventions include folic acid to prevent neural tube defects, iodine to prevent cretinism, zinc to reduce of preterm birth, and iron to reduce the risk of low birth weight. Folic acid and vitamin D might also increase birth weight. While extensive mechanism and association research links antenatal multiple micronutrients to plausible materno-fetal health advantages, hypothesized benefits have often been absent, minimal or unexpected in trials. These findings suggest a role for population context in determining health responses and extensive gaps in knowledge. Multiple micronutrient supplements reduce risks of being born low birth weight, small for gestational age or stillborn in undernourished settings, and justify micronutrient interventions with antenatal care. Measurable health effects of gestational micronutrient exposure may persist into childhood but few data exists on potential long-term benefits. In this Review, we discuss micronutrient intake recommendations, risks and consequences of deficiencies, and the effects of interventions with a particular emphasis on offspring.
Introduction
Essential vitamins and minerals are dietary components required in small quantities to support virtually all metabolic activity, including cell signaling, motility, proliferation, differentiation and apoptosis that regulate tissue growth, function and homeostasis. These fundamental biological roles, in early life, enable the fetus to develop and mature into a healthy neonate. Vitamins and minerals support every stage of maternal, placental and fetal interaction to enable a healthy gestation. Most vitamins and trace minerals are referred to as ‘micronutrients’. Some essential nutrients, such as calcium, magnesium and phosphorus are considered ‘macro’ minerals because they are required in greater than trace quantities and will not be discussed in this Review; nor will semi-essential or conditionally required nutrients, such as arginine, choline and taurine. Micronutrients receiving most attention in pregnancy, and commonly provided as supplements, include vitamins A, D, E, folate, B12, B6, and C, iron, zinc, iodine, copper and selenium. Although other B-complex vitamins (such as, niacin, riboflavin and thiamin) are nearly always also included in dietary supplements, their individual metabolic roles are less well-specified in pregnancy. Consequently, to illustrate the B vitamin contributions, we focus on folate and vitamin B12, for which there is considerable interest and human data available supporting their functions in pregnancy.
In this Review, we discuss the metabolic roles of micronutrients that are known to contribute to an optimal pregnancy outcome. We illustrate their importance in regulating selected materno-fetal processes, and summarize the effects of antenatal micronutrient supplement use on fetal, infant and childhood health and emerging development outcomes of public health importance. Supplementation can be used in research to investigate causality of nutritional exposure in affecting health outcomes and as a public health approach to increase nutrient intakes specifically during pregnancy. Other strategies to improve micronutrient status during pregnancy are discussed, as are gaps in current methods of assessment and knowledge of function of micronutrients in enhancing reproductive health.
Recommended intakes during pregnancy
Micronutrient intake recommendations are determined by assessing the normal physiological requirements of nutrients to support a healthy pregnancy. These requirements might be determined, in part, by a woman’s diet and nutritional status before pregnancy, as well as environmental stressors that can lead to inflammation of body tissues and therefore deplete, or divert the use of, micronutrients. However, dietary recommendations determined by panels of nutrition experts are specific in guiding intakes for normally nourished populations to remain healthy.1, 2 However, setting appropriate recommendations for vitamin and mineral intakes during pregnancy is challenging. Micronutrient concentrations, which often serve as biomarkers to guide estimation of status and therefore physiological need, can be affected by plasma volume expansion and other adaptations to the pregnant state. As such, recommendations for pregnancy are often extrapolations from estimates of adult or adolescent (as appropriate) intake requirements, adjusted to account for fetal nutrient accumulation, additional maternal demands to support tissue accretion and metabolism, and changes in efficiency of nutrient absorption that may occur during pregnancy, as summarized in Table 1.3
Table 1.
Recommendations for micronutrient intake for women in the USA and Canada
| Nutrient | RDA* |
Criterion for setting level in pregnancy |
Physiological changes underlying pregnancy-specific recommendations |
|
|---|---|---|---|---|
| Pregnant | Nonpregnant/ nonlactating |
|||
| Vitamin A | 770 μg RAE | 700 μg RAE | Assure adequate vitamin A stores | Fetal liver and placenta acquire and store vitamin A; mother's stores may be mobilized as needed |
|
| ||||
| Vitamin B6 |
1.9 mg | 1.3 mg | Maintain adequate plasma pyridoxal phosphate and meet increased needs of pregnancy |
Fetal and utero-placental accumulation with increased maternal weight and metabolism with no gains in maternal absorption compared to non-pregnant state |
|
| ||||
| Vitamin B12 |
2.6 μg | 2.4 μg | Maintain hematological status and serum B12 levels and meet fetal needs |
Fetal accumulation; maternal absorption improves and transcobalamin I and III increase in 2nd and 3rd trimesters |
|
| ||||
| Folate | 600 μg DFE | 400 μg DFE | Maintain red blood cell folate | Enhanced single-carbon metabolism to support materno-placental tissue expansion and fetal growth; active materno-fetal folate transfer, but no gains in maternal absorption compared to non-pregnant state |
|
| ||||
| Vitamin C | 85 mg | 75 mg | Maintain adequate maternal neutrophil ascorbate (as indicator) and theoretical transfer to fetus |
Additional amount of vitamin C required for materno-fetal transfer is unknown; increment is theoretical |
|
| ||||
| Vitamin D | 600 IU | 600 IU | Maintain 25(OH)D concentrations necessary to support bone health |
No known increased requirement for pregnancy to increase calcium absorption |
|
| ||||
| Vitamin E¶ | 15 mg | 15 mg | Maintain plasma α-tocopherol and prevent hydrogen peroxide- induced hemolysis (based on non- pregnancy data) |
Nutrient transfers to the fetus but intakes presumed adequate in high income countries because plasma α- tocopherol concentrations increase across gestation |
|
| ||||
| Copper | 1000 μg | 900 μg | Maintain adequate indicators: plasma copper and ceruloplasmin, erythrocyte superoxide dismutase activity or platelet copper |
Recommendation based on estimated amount needed for expanded maternal, placental, and fetal tissues |
|
| ||||
| Iodine | 220 μg | 150 μg | Maintain positive iodine balance, prevent goiter, and meet estimated daily thyroid iodine uptake by the fetus |
Additional fetal requirement |
|
| ||||
| Iron | 27 mg | 18 mg | Meet physiological requirement for normal function assuming high absorption rate in second and third trimester |
Increase of red blood cells; basal losses; fetal iron uptake, iron deposition in fetal and placenta tissues; increased maternal absorption |
|
| ||||
| Selenium | 60 μg | 55 μg | Maximize the synthesis of the plasma selenoprotein glutathione peroxidase and meet fetal needs |
Additional fetal requirement for saturation of fetal selenoproteins |
|
| ||||
| Zinc | 11 mg | 8 mg | Factorial analysis of zinc absorption plus additional needs in late pregnancy |
Maternal and fetal tissue accumulation |
DFE, dietary folate equivalents; RAE, retinol activity equivalents; RDA, recommended dietary allowance; 25(OH)D, 25-hydroxyvitamin D.
From the Institute of Medicine reports on Dietary Reference Intakes for each nutrient (http://fnic.nal.usda.gov/dietary-guidance/dietary-reference-intakes/dri-nutrient-reports); for 19-30 y females, if recommendations differed by age of pregnant woman.
As α-tocopherol.
The Recommended Dietary Allowances (RDAs; Box 1)1 or Recommended Nutrient Intakes (RNIs)2 are most often used to guide usual population nutrient intakes in many countries. The RDAs were developed nutrient by nutrient over the period of more than a decade by groups of expert nutritionists convened by the Institute of Medicine in the USA. The RDA is one of several dietary reference intakes established to the diets of healthy populations in the USA and Canada. The expert groups examined the literature regarding functional tests or health outcome responses to nutrient intakes to derive requirement distributions for each nutrient. The median represented an intake that should be adequate for half of the population, a value termed the Estimated Average Requirement (EAR). With the requirement distribution assumed as normal, an RDA was set at two standard deviations above the EAR, or a level that would meet nutrient intake requirements for 97.5% of a population. Consequently, the EAR rather than RDA should be used to estimate prevalences of inadequate nutrient intake.1
Box 1. Dietary reference terms.
Dietary reference intakes (DRIs) for the USA and Canada
- Estimated average requirement (EAR)
- - Average daily intake level estimated to meet the needs of 50% of healthy individuals
- - Used to estimate deficiency prevalence in populations
- Recommended dietary allowance (RDA)
- - Intake level estimated to meet the needs of 97.5% of healthy individuals
- - Calculated from the distribution used to estimate the EAR
- - Used as a goal for individual intake
- - Amount most often provided in supplements
Recommended nutrient intakes (RNIs) from the WHO
Definition is equivalent to RDA above (although actual amounts can differ)
Details on the DRIs and RNIs can be found here: http://fnic.nal.usda.gov/dietary-guidance/dietary-reference-intakes/dri-tables-and-application-reports and http://apps.who.int/iris/bitstream/10665/42716/1/9241546123.pdf?ua=1
The RNIs were compiled by expert consultative processes under the auspices of the WHO, which followed a more empirical approach for each nutrient, including considering intake distributions required to maintain normal status, to estimate an EAR.2 Thus, while comparable in estimated values, the two sources are not identical in their approaches to derivation. Efforts are also underway to harmonize recommendations across Europe through the EURopean micronutrient REcommendations Aliqned (EURRECA) network.4 Despite these attempts to align recommendations, national adaptations can vary widely (for example, for folate5), reflecting differences in purpose of the estimates and national expert interpretation of requirements across dietary, cultural and environmental contexts in different countries. Thus, even with increasingly evidence-based recommendations, practical and reliable translation of micronutrient recommendations into dietary intakes remains a global challenge.
Table 1 provides RDAs for selected nutrients along with criteria for setting levels in pregnancy and explanations for why they might differ from an RDA for nonpregnant, nonlactating women. Although RDAs (and RNIs) for pregnancy may not differ than those set for the nonpregnant, nonlactating state, as seen with vitamin D and vitamin E, recommendations for some nutrients are set to intakes that are up to ~50% higher during pregnancy, as is the case for iron, folate, iodine and B6 to accommodate expected increased maternal, placental and fetal requirements.
Although representing the best possible estimates, micronutrient intake recommendations during pregnancy should be interpreted in context. For example, the RDAs are not applicable to individuals, and by extension to populations, who are malnourished and whose dietary needs to nutritionally recover and mitigate health risks of pre-existing micronutrient deficiencies might be greater than those who are well-fed. For this reason, and given accruing findings of health benefits, Table 2 illustrates supplemental micronutrients that the WHO considers essential in low-income settings, and provides a joint WHO/UNICEF/World Food Programme guideline for micronutrient supplementation under complex emergencies that may markedly increase malnutrition due to conflict, natural disasters, or general failures in markets that could lead to famine. These WHO guidelines, intended for programmatic planning, have essentially been also adopted as recommendations for healthcare workers by the International Federation of Gynecology and Obstetrics (FIGO).6 Further, the WHO/UNICEF/World Food Programme multiple micronutrient formulation has also become a de facto global recommendation.7 Specifically, the supplement that emerged from these guidelines for distribution to pregnant women in undernourished settings — called the United Nations Multiple Micronutrient Antenatal Preparation — contains 15 micronutrients at dosages approximating an RDA for pregnancy,8 and has been tested in trials in South Asia and Africa.9
Table 2.
Micronutrient supplement recommendations for pregnant women in low-income settings
| Nutrient | WHO* | Joint WHO, UNICEF & WFP for emergencies: multiple vitamin and mineral supplement‡ |
|---|---|---|
| Vitamin A | Up to 10,000 IU/day for ≥12 weeks to prevent night blindness in deficient settings |
800 μg RAE |
| Vitamin B6 | None | 1.9 mg |
| Vitamin B12 | None | 2.6 mg |
| Folate | 400 μg daily or 2.8 mg weekly as folic acid, all settings§ |
600 μg as folic acid |
| Vitamin C | None | 55 mg |
| Vitamin D | None | 200 IU |
| Vitamin E∥ | None | 15 mg |
| Copper | None | 1150 μg |
| Iodine | 250 μg daily or 400 mg once per year where iodized salt coverage is <20% |
250 μg |
| Iron | Daily 30-60 mg or weekly 120 mg elemental iron supplement, all settings§ |
27 mg |
| Selenium | None | 30 μg |
| Zinc | None | 10 mg |
RAE, retinol activity equivalents; UNICEF, United Nations Children’s Fund; WFP, World Food Programme.
WHO. Essential Nutrition Actions: improving maternal, newborn, infant and young child health and nutrition (World Health Organization, Geneva, 2013) http://www.who.int/nutrition/publications/infantfeeding/essential_nutrition_actions/en/.
WHO/UNICEF/WFP. Preventing and controlling micronutrient deficiencies in populations affected by an emergency: Multiple vitamin and mineral supplements for pregnant and lactating women, and for children aged 6 to 59 months. www.who.int/nutrition/publications/WHO_WFP_UNICEFstatement.pdf.
Combined iron and folic acid supplement is recommended.
As α-tocopherol.
Micronutrient deficiencies
Women living in low-income countries are often unable to meet the micronutrient demands of pregnancy due to a chronically poor diet.10 At the same time, the costs of assessing biochemical indicators of individual micronutrients have led to few population estimates of deficiencies during pregnancy. This situation has given rise to the term ‘hidden hunger’,11 referring to a lack of knowledge as to the extent and consequences of this nutritional burden.
Population data have been used to estimate the global prevalence of certain nutrient deficiencies during pregnancy,12 albeit without delineation by age, parity, socioeconomic status and other factors that might influence nutrition during gestation. Worldwide, the estimated prevalence of prenatal iron deficiency anaemia is 15–20%, calculated as half of women with anemia, defined as haemoglobin <110 g/l (because half respond to supplementation with iron based on data from population-based intervention trials).12 Vitamin A deficiency, classified by a low serum retinol (<0.70 μmol/l), affects an estimated 15% of pregnant women in low-income countries. 13 Eight percent of pregnant women have vitamin A deficiency high enough to lead to night blindness,13 an ocular consequence the deficiency. Iodine deficiency ranges from 17% in Oceania to 40% in Africa.12 These estimates are based on a median urinary iodine concentration falling below 150 μmol/l in population assessments of children aged 6–12 years, an age group regarded as ‘sentinel’ in reflecting geographic and population-level risk, although one that might underestimate iodine deficiency in pregnancy.14 While global estimates of other deficiencies are unavailable, population-based studies in South Asia, including India, Bangladesh and Nepal have reported deficiencies of zinc (15–74%), vitamin B12 (19–74%), vitamin E (as α-tocopherol, 50–70%), and folate (0–26%) in pregnant women.15-21 In a few instances, where a larger number of nutrients have been assessed in the same population, multiple deficiencies appear, although unequal in burden. For example, in Côte d’Ivoire in West Africa, the prevalence of deficiencies among women of reproductive age varied widely for vitamin A (1%), iron (17%), vitamin B12 (18%) and folate (86%).21 In the plains of southern Nepal, the percentage of pregnant women varied in deficiencies of vitamins A (7%), D (14%), E (moderate-to-severe, 25%), B12 (28%), B2 (33%) and B6 (40%), folate (12%), iron (40%) and zinc (61%), and only 4% were normal in status for all nutrients.14 Deficiencies in the surveyed area of southern Nepal varied by season, which is likely to be the result of seasonal shortages in available food sources and consequent diet, characteristic of rural agrarian societies.22 Although not well estimated during pregnancy, vitamin D deficiency (defined as 25-hydroxyvitamin D <30 nmol/l) is high in many countries including Turkey (50%), India (60%), and Pakistan (45%),23 and women and infants (reflective of maternal status) have lower vitamin D status in the Asia/Pacific region.24
In the absence of adequate data on biochemical status, quantitative dietary data in pregnant women can be used to estimate the prevalence of inadequate intake, based on the percentage of population intakes below the EAR (Box 1). With few exceptions, most estimates of average intake are below the EAR in low-income and middle-income countries for folate, iron, and zinc; and vitamin A intake is low particularly in Asia and Africa.25
In high-income countries, few clinical micronutrient deficiencies exist during pregnancy, a situation that has been attributed to year-round dietary diversity, dietary counseling during pregnancy, widespread intake of fortified foods (such as in the USA)26 and antenatal micronutrient supplement use.27 Nonetheless, mild deficiencies remain and dietary micronutrient inadequacy might be emerging as diets of higher fat and sugar and lower nutrient density are increasingly consumed.28 In a 2013 review of diets among pregnant women in high-income countries, intakes of folate, iron, and vitamin D were found to be below recommended intakes in each geographic region examined.29 Where diets are typically diverse and generally considered adequate, such as the UK, elsewhere in Europe and the USA, national surveys suggest that intrinsic (that is, nonfortified) intakes are low for vitamins A, D, C and folate, which increases the risk of antenatal deficiencies .30 Mild gestational iodine deficiency also remains endemic in parts of Europe, presumably due to inadequate use of iodized salt,31 and daily iodine intake in American pregnant women might be low based on a borderline median urinary iodine excretion, an indicator that reflects recent dietary intake.32 A public health success in the USA has been the markedly reduced prevalence of folate deficiency in the first trimester of pregnancy (based on low serum or red blood cell folate), from 55% in the early 1990s to ≤1% by 2010,33 owing to folic acid fortification of flour.34 Poor vitamin D status has been a re-emerging issue – with documented insufficiency in pregnancy the USA (28%)35 and the Mediterranean (50-65%).36 Causes of deficiency are complicated to determine due to the dual sources of diet and skin production, but lack of sun exposure is a contributor. Iron deficiency persists. In the USA, the National Health and Nutrition Examination Study (NHANES; 1999–2006) estimated 18% of American gravida to be affected, based on non-detectable total body iron.37
Micronutrient function during pregnancy
Micronutrients support maternal health and fetal development throughout gestation through processes that are integrated across maternal, placental and fetal compartments (FIG. 1). Micronutrient function in human pregnancy is typically inferred from in vitro studies and experimental animal models, observational data in human studies, and a limited number of human trials that have explored metabolic mechanisms and outcomes. Overall, we have a limited in vivo understanding of specific, causal mechanisms by which micronutrients act through the materno-placental fetal axis to influence human pregnancy outcomes.38
Figure 1. The function and timing of micronutrients that affect outcomes in offspring.
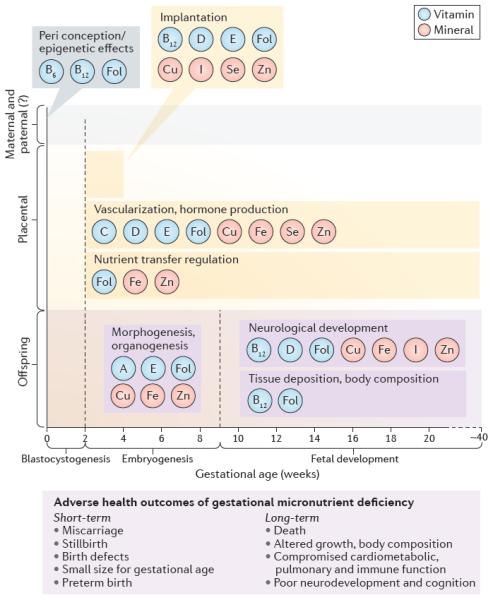
Insights on micronutrient function are primarily derived from reviews of data from in vitro studies, experimental animal models, observational data in human studies and a limited number of trials that have explored metabolic mechanisms and outcomes. The relevant time of action and the function of micronutrients is depicted, but the accumulation of fetal micronutrient stores, generally dependent on the status of the mother, is not. Availability of fetal micronutrient stores to support growth and developmental processes into infancy and beyond is, therefore, an implied pathway. Fol, folate.
Mother
Micronutrient nutriture affects maternal capacity to conceive and support pregnancy through to birth. Deficiencies in micronutrients involved in one-carbon metabolism, including folate and vitamins B6 and B12, might contribute to disturbances in gametogenesis, fertilization, and development of the embryo before implantation, which have been associated with elevated systemic and follicular homocysteine.39 These nutrient deficiencies might also adversely affect DNA and histone methylation of the oocyte (and sperm in the male partner), with long-term consequences.40 Reductions within normal dietary ranges in periconceptional (8 weeks before to 6 days post-conception) consumption of vitamin B12 and folate in sheep dams were associated with epigenetic changes in offspring DNA methylation and increased susceptibility to obesity, insulin resistance, and hypertension in adulthood.40 In a rare, randomized, placebo-controlled trial in a nutritionally compromised population, data from cord blood and at 9 months of infants in the Gambia revealed differential patterns of DNA methylation, particularly of genes affecting immune response, following maternal multiple micronutrient supplementation, demonstrating the potential for epigenetic responses to micronutrient interventions in humans.41 Beyond the periconceptional period, because folate and vitamin B12 are required for nucleotide and DNA synthesis to support cell division, deficiencies in these nutrients also increase risk of miscarriage and fetal malformations, including neural tube defects.39
Other micronutrient deficiencies have also been associated with early reproductive failure. Vitamin E (α-tocopherol) is required to protect essential fatty acids from oxidative degradation during embryogenesis based on animal and in vitro studies.42 Antioxidant roles, as well as roles in promoting enzyme induction, cell signaling and lipid membrane integrity could be mechanisms underlying the nearly doubled risk of miscarriage associated with early pregnancy vitamin E deficiency observed in women in rural Bangladesh.21 Severe selenium, zinc, and copper43 and iodine deficiencies,44 while now less common in human populations, have also been associated with miscarriage. Important maternal haemodynamic, cardiovascular, renal, and gastrointestinal adaptations occur throughout pregnancy, but little is known about specific micronutrient functions that might support or respond to these changes. Pregnancy-associated haemodilution reduces circulating concentrations of many micronutrient indicators during the second and third trimesters of pregnancy. This phenomenon is well established, for example, for iron status,45 while hormonal changes increase concentrations of nutrients such as vitamin E and copper.43 These changes limit our ability to accurately assess micronutrient status during pregnancy with conventional cutoffs for micronutrient status indicators, although lower cutoffs for second trimester haemoglobin concentrations are advocated for assessing anemia to account for this issue.45
Placenta
Vascularization of placental tissue requires invasion of the external trophoblast cells from the embryo into the maternal decidua, a process eliciting oxidative stress and thereby requiring modulation by antioxidant nutrients.43 The placenta is rich in micronutrient-requiring antioxidant enzymes, including glutathione peroxidases (selenium) and superoxide dismutases (copper, zinc, and manganese), essential for protecting the embryo and placenta from oxidative stress as maternal spiral arteries are invaded to initiate maternal-fetal circulation.43 Insufficient antioxidant activity has been posited to be associated with reductions in placental vascularization, potentially limiting blood flow to the fetus , which results in hypoxia and ischaemia and is likely to contribute to preeclampsia and poor fetal growth.43
Vitamin E, probably via phosphorylated α-tocopherol, might promotes vascularization of the placenta, presumably by enhancing expression of angiogenic factors like vascular endothelial growth factor (VEGF).46 The placenta expresses vitamin D receptors and can convert 25-hydroxyvitamin D [25(OH)D] to active calcitriol — which is probably utilized for localized paracrine/autocrine functions as calcitriol is not transferred to the fetus.47 Vitamin D promotes placental VEGF production,48 modulates immune function,49,50 and is thought to support implantation and placental metabolism,47 providing plausible mechanisms for positive associations between vitamin D status birth outcomes. Maternal iron levels have also been associated with pregnancy health. Placental size is inversely associated with maternal haemoglobin concentration, and maternal or fetal stress induced by hypoxia or iron deficiency might trigger release of placental corticotropin releasing hormone, which induces changes in signals for parturition and/or fetal macronutrient metabolism, respectively.51 Among a variety of roles played by zinc to support pregnancy,52 zinc deficiency was found to impede placental development, including trophoblast differentiation, placental size, weight, and protein expression in a mouse model of periconceptional zinc deficiency.53
Human placental lactogen (hPL), placental growth hormone (GH-2), and insulin-like growth factor-1 (IGF-1) released by the placenta into maternal circulation increase insulin resistance to ensure a supply of glucose to the fetus.54 However, growth-restricting maternal cortisol might be transferred to the fetus more efficiently in malnourished mothers whose placental production of the 11 β-hydroxysteroid dehydrogenase type 2 is reduced.54 In two trials in which multiple micronutrient effects on maternal (hPL, GH-2)55 and cord blood endocrine factors (insulin, IGF-1, and IGF binding protein-155 or IGF-1, insulin, free thyroxine, and cortisol56) were studied, no differences were found between multiple micronutrient and iron-folic acid supplemented groups. While levels of maternal or cord blood zinc have been examined in relation to cord blood or placental expression of IGF-1 in human pregnancies, associations of zinc and IGF-1 have been mixed despite a persistent association of IGF-1 with fetal growth57, 58 and evidence linking zinc with the IGF-1 axis and fetal growth in experimental animals.59
The mature placenta can adapt to maternal supply of, and fetal demand for, nutrients by altering the surface area across which nutrients are exchanged, the thickness of the barrier between maternal and fetal circulation, the number and type of nutrient transporters, blood flow, metabolic rate, and hormone production.60, 61 For several nutrients transported against concentration gradients (for example, folate, iron, zinc), nutrient-specific transporters are up-regulated when availability is limited to maintain fetal supply.45, 61-63 This is perhaps most clearly demonstrated with respect to iron status, where placental transferrin receptor (TfR) and natural resistance-associated macrophage protein 2 (also known as divalent metal transporter 1) have been shown to be upregulated in response to fetal iron status.45, 61 Other water soluble vitamins (such as, vitamins B6, B12 and C) are also actively transported to the fetus,64 while fat-soluble vitamins tend to cross the placenta along a gradient that parallels maternal status.46, 65, 66
Fetus
Basic organ structures of the offspring are established during the embryogenesis (2–8 weeks of gestation), and micronutrients are required for organogenesis, supporting the structural development of fetal organs. Later in gestation, adequate micronutrient status might have an impact on organ size or function. Cell division of the neural tube and crest during embryogenesis might double every 5 hours,62 which is consistent with the high requirement for folate in the embryo at this time. Vitamin A is also crucial for embryonic development early in fetal life, and roles for retinoic acid via nuclear receptors have been demonstrated in virtually every tissue studied in animal models, including the nervous system, eye, heart, skeleton, respiratory system, and pancreas,65 as well as ear structure.67 Retinoic acid availability and function must be tightly controlled by the developing offspring, as excessive maternal vitamin A has been shown to be teratogenic.65 Deficiency of micronutrients including vitamin A, iron, zinc, copper, vitamin E, and magnesium during fetal development has been postulated to result in organ structure alterations of the kidney, pancreas, and vasculature that might predispose the offspring to cardiometabolic disease in later life; this effect has been reviewed elsewhere.68, 69
Nutritional inadequacies of the developing fetal brain and central nervous system might compromise neurological development, function and cognition. The roles of micronutrients including iron, zinc, copper, choline, iodine, folic acid, and vitamin D in fetal and neonatal brain development have been extensively reviewed elsewhere.70-73 Briefly, micronutrient deficiencies in utero may affect specific brain structures, function, and neurochemistry, and have differential effects depending on timing of brain development.70 For example, gestational iron deficiency confers risk primarily to the developing hippocampus and alters brain energy metabolism, neurotransmitter systems and myelination.74 Zinc and many B vitamins contribute to DNA and RNA synthesis and energy metabolism within the brain and to neural synapse formation and function.75 Iodine deficiency is considered the most common cause of preventable mental deficits globally. Maternal thyroxine, an iodine containing thyroid hormone, crosses the placenta and is required for fetal brain development in the first and second trimester, before the independent function of the fetal thyroid gland, after which thyroid hormone of both maternal and fetal origin supports brain development and function.71
During the second and third trimesters of pregnancy, the fetus grows and accumulates nutrient stores. Iron stores, for example, accumulate in proportion to the length of gestation and are the major source of iron for the growing infant for the first 6 months of life.76 For a variety of vitamins and minerals, neonatal stores reflect both duration of gestation and maternal micronutrient status, and infants born either prematurely or to mothers with micronutrient deficiency might have insufficient stores to support rapid postnatal growth and development. Pregnancy is also crucial for ensuring optimal neonatal micronutrients when breast milk, as the primary source of infant postnatal nutrition, does not compensate for poor status at birth due to low nutrient content (such as vitamin D, iron, and zinc) — regardless of maternal status.77 Iron and vitamin D provide two classic examples. Transfer of iron to the fetus is greatest during the third trimester, such that preterm infants are born with limited iron stores and are at high risk for anemia by 1 year of age.45, 78 Another example is that the risk of developing rickets among infants of vitamin D-deficient mothers is associated with suboptimal infant status related to low transfer of 25(OH)D to the fetus in pregnancy and the limited contribution of breast milk. However, placental calcium transfer for fetal bone mineralization is preserved over a range of maternal vitamin D and calcium states during pregnancy.66
Micronutrients are likely to contribute to the biological processes that support fetal growth, resulting in enhanced birth weights; however, the specific mechanisms by which in utero micronutrient exposure elicits this effect is not yet established.38,79 An example of micronutrient deficiencies implicated in alterations in tissue deposition include folate and vitamin B12, which increased the amount of visceral body fat, inflammation, and dyslipidemia among offspring of deficient rat dams.80 Deficiencies in a variety of micronutrients (folate, vitamin B12, zinc) potentially predispose offspring to chronic disease outcomes, including obesity, insulin resistance, and dyslipidemia, later in life,81 although data from human populations are limited.
Antenatal effects across the lifespan
Micronutrients in the mother at the time of pregnancy can impact immediate, short-term, and long-term outcomes for the offspring. Randomized controlled trials (RCTs) of micronutrient supplementation provide the strongest available evidence of causal relationships between micronutrient intake and pregnancy-associated outcomes in human populations. A summary of meta-analyses of RCTs examining single nutrient effects on pregnancy and birth outcomes primarily conducted in low-income, undernourished populations is provided in Tables 3-4. Evidence of the short-term impact of multiple micronutrient supplements has been published in a 2015 Cochrane review.9 Supplements tested in humans have comprised single or combined micronutrient formulations, usually starting in the first trimester or at least first half of pregnancy to optimize nutrient exposures and, theoretically, to establish their influence on the complex nutrient-regulated mechanisms and pathways discussed above. However, only a limited number of studies have examined benefits of preconception or periconceptional micronutrient supplementation, when placentation and embryogenesis would be expected to benefit most. Systematic trial data on long-term outcomes past infancy from in utero exposure to micronutrients are also lacking and greatly needed.
Table 3.
Randomized controlled trials supplementing pregnant women with individual micronutrients included in meta-analyses
| No. of trials starting during each gestational period (weeks) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Micronutrient | No. trials |
Total no. of pregnancies [range between studies] |
Country income context |
Dose (times RDA)* |
Pre pregnancy |
1-10 | 11-20 | 21-30 | >31 |
| Vitamins | |||||||||
| Vitamin A‡ (McCauley 2015157) |
19 | 169,337 [27-102,952] |
Low to Middle |
1–3 | 2 | 1 | 9 | 5 | 2 |
|
| |||||||||
| Vitamin B6 (Salam 2015158) |
4 | 1623 [22-1532] |
Middle to High |
1–53 | – | – | 2 | 1 | 1 |
|
| |||||||||
| Folic acid (De-Regil 201092) |
5 | 8357 [218-5502] |
Low to High |
1–11 | 5 | – | – | – | – |
|
| |||||||||
| Folic acid (Lassi 2013103) |
31 | 13,396 [20-2928] |
Low to High |
0.3–42 | – | 1 | 16 | 13 | 1 |
|
| |||||||||
| Vitamin C§ (Rumbold 2015159) |
8 | 2007 [60-815] |
Low to High |
1–12 | – | 1 | 6 | 1 | |
|
| |||||||||
| Vitamin D∥ (De-Regil 2016105) |
9 | 1271 [40-260] |
Low to High |
1–8 | – | – | 1 | 8 | – |
|
| |||||||||
| Minerals | |||||||||
| Iodine¶ (Bougma 2013130 and Zhou 2013129) |
9 | 1521 [35-1047] |
Low to High |
436– 4364 |
2 | – | 6 | 1 | – |
|
| |||||||||
| Iron# (Peña-Rosas 2015102) |
44 | 22,802 [13-5828] |
Low to High |
1–37 | – | 2 | 27 | 12 | 2 |
|
| |||||||||
| Iron/IFA (Haider 2013101) |
48 | 17,793 [13-3929] |
Low to High |
0.3–33 | – | 3 | 30 | 12 | 2 |
|
| |||||||||
| Zinc (Ota 2015111) |
21 | 11,774 [56-2124] |
Low to High |
0.5–8 | 1 | – | 17 | 3 | – |
We did not identify a meta-analysis that met our criteria for vitamin B12 or selenium. We identified no individual studies for vitamin E, thiamin, riboflavin, niacin or copper. IFA, iron and folic acid.
RDA used for pregnant women aged 19–30 years as the referent group.
One study gave a bolus dose (600,000 IU).
Only includes trials comparing groups with vitamin C to groups without vitamin C (does not include trials of vitamin C and vitamin E tested together).
Only includes trials comparing groups with vitamin D to groups without vitamin D; four trials of vitamin D gave participants bolus doses (ranging from 60,000 to 600,000 IU).
Three trials of iodine gave bolus injections (96–1600 mg).
Only includes trials comparing groups with iron to groups without iron, does not include trials of iron and folic acid tested together.
Table 4.
Meta-analyses of RCTs supplementing pregnant women with micronutrients: pregnancy and early-life postnatal outcomes
| Micronutrient | Outcome (quality of evidence per meta-analysis: low; moderate; high)* |
|||
|---|---|---|---|---|
| During pregnancy |
At Birth | < 1 month | < 5 years | |
|
|
||||
| Vitamins | ||||
| Vitamin A4 (McCauley 2015157) |
No effect: stillbirth |
No effect: preterm birth, low birth weight |
No effect: neonatal mortality |
– |
|
| ||||
| Vitamin B6 (Salam 2015158) |
No effect: preeclampsia |
– | – | – |
|
| ||||
| Folic acid (De-Regil 201092) |
72% ↓ risk NTD (low) No effect: other birth defects, miscarriage |
– | – | – |
|
| ||||
| Folic acid (Lassi 2013103) |
No effect: stillbirth |
136 g ↑ birth weight (high) No effect: low birth weight |
No effect: neonatal mortality |
– |
|
| ||||
| Vitamin C‡ (Rumbold 2015159) |
No effect: stillbirth, preeclampsia |
36% ↓ risk preterm PROM (high) No effect: preterm birth; IUGR |
No effect: neonatal mortality |
– |
|
| ||||
| Vitamin D∥ (De-Regil 2016105) |
No effect: stillbirth, preeclampsia |
60% ↓ risk low birth weight (moderate); 64% ↓ risk preterm birth (moderate) No effect: preterm birth, birth weight, SGA |
No effect: neonatal mortality |
– |
|
| ||||
| Minerals | ||||
| Iodine (Bougma 2013130 and Zhou 2013129) |
– | – | – | 8 ↑ IQ points (high); ↓ risk cretinism |
|
| ||||
| Iron§ (Peña-Rosas 2015102) |
No effect: birth defects |
No effect: preterm birth, birth weight, low birth weight |
No effect: neonatal mortality |
– |
|
| ||||
| Iron/IFA (Haider 2013101) |
– | 41 g ↑ birth weight (low); 19% ↓ risk low birth weight (low) No effect: preterm birth, SGA |
– | – |
|
| ||||
| Zinc (Ota 2015111) |
No effect: stillbirth, preeclampsia, birth defects |
14% ↓ risk preterm birth (moderate) No effect: birth weight, low birth weight, SGA |
No effect: neonatal mortality |
– |
Most outcomes presented were not assessed in all trials (for example, birth weight was only assessed in five of 31 folic acid trials). Improvements in biochemical status or clinical issues that are not specific to pregnancy (such as nightblindness or anaemia) are not presented. IFA, iron-folic acid; IUGR, intrauterine growth restriction; PROM, premature rupture of the chorioamniotic membrane; RCT, randomized controlled trial; SGA, small for gestational age.
Quality of evidence is defined by the original meta-analysis.
Only includes trials comparing groups with vitamin C to groups without vitamin C (does not include trials of vitamin C and vitamin E tested together).
Only includes trials comparing groups with vitamin D to groups without vitamin D.
Only includes trials comparing groups with iron to groups without iron, does not include trials of iron and folic acid tested together.
Gestational effects
A number of possible short-term responses exist to changes in materno-placento-fetal nutriture that are attained by maternal improvement in micronutrient status. These can include differences in fetal survival affecting risk of pregnancy loss due to miscarriage and stillbirth; organ formation affecting risks of birth defects; duration of gestation affecting risks of preterm birth, and consequent low birth weight; and rate of fetal growth, affecting birth size and consequent risks of being born small for gestational age and/or having a low birth weight.
Pregnancy loss
Periconceptional deficiencies of vitamin E,21 thiamine,82 and selenium83 among others have been variably associated with spontaneous or recurrent pregnancy loss. Folate supplementation in an observational USA study of almost 16,000 women has been linked to a 20% lower risk of miscarriage (adjusted risk ratio [RR]: 0.80, 95% CI 0.71–0.90).84 However, trials that have examined effects of micronutrient supplementation on early pregnancy loss are currently lacking. For example, selenium deficiency has a hypothesized link with miscarriage,43 as discussed above, but no trials have been conducted to test its effect (Table 3). Vitamin A and folic acid supplementation have been tested but have shown no effect on lowering the risk of miscarriage (Table 4). Among the few trials conducted to assess vitamin supplementation before pregnancy and/or within the first half of pregnancy, no effect on early or late miscarriage has been identified,85 nor has miscarriage risk been lowered from multiple micronutrient use.9
By contrast, trial data exist on effects of individual and multiple micronutrient interventions on risk of stillbirth (Table 4). However, these studies are often statistically underpowered to measure this outcome, and meta-analyses of combined findings suggest no significant effect of antenatal supplementation with vitamin A, vitamin C, folic acid or zinc on stillbirth, while meta-analyses for this outcome have not been examined or reported for other individual micronutrients (Table 4).85, 86 In a trial comparing multiple micronutrient versus iron and folic acid (IFA) in Bangladesh (starting supplementation at ~9 weeks’ gestation), which was designed to evaluate stillbirth, multiple micronutrients reduced the incidence of stillbirth by 11% (95% CI 1–19%).87 Moreover, in a Cochrane systematic review of all randomized multiple micronutrient supplementation trials that combined effect estimates from 15 studies in low-income and middle-income countries, a 9% reduction in stillbirth (RR 0.91; 95% CI 0.85–0.98) was found compared with iron supplementation both with or without folic acid.9 Collectively, these data suggest that sustained and adequate antenatal micronutrient supplementation might indeed improve late fetal survival rates.
Birth defects
Periconceptional micronutrient inadequacy might increase the risk of congenital anomalies but folic acid is the only nutrient proven effective at reducing this outcome. Neural tube defects (NTDs), in particular, represent a complex group of multifactorial lesions (including anencephaly and spina bifida) that together affect 1 to 10 per 1000 births worldwide,88 with undernourished populations, for example, in India, seeming to be at the highest risk.89 NTDs have been associated with a deficiency in folate since the 1960s,90 which is attributed to the pivotal roles of folate in single-carbon metabolism and DNA synthesis and function, but the mechanisms are still not fully understood.91 Strong, consistent evidence from trials has established that periconceptional provision of folate markedly reduces risk of NTDs, by 72% (95% CI 48–85%), as well as recurrent NTDs,92 an effect that has been extended to public health application through folic acid fortification of grain products in the USA since the late 1990s.88,93 Other single micronutrients either have not been tested an effect on birth defects or have not shown an effect (iron and zinc; Table 4).
Adequate periconceptional folate nutriture may also reduce the risk of developing heart defects,94 an observation that awaits confirmatory trials.95 Beyond folate, antenatal vitamin B12 deficiency has been associated with a higher risk of NTDs64 and increased reported periconceptional intakes of thiamine, niacin and B6 have been associated with lower risks of orofacial cleft,96 although supplementation trials have yet to be done to test causality of these associations (Table 3). In several observational studies, antenatal multivitamin supplement use has been associated with lower risks of orofacial, heart, urinary tract, limb and other non-NTD birth defects,97 findings that evoke plausible mechanisms but that also require confirmation. The need for balanced micronutrient nutriture to guide normal fetal development is suggested by a potentially higher risk of neural crest defects with either severe vitamin A deficiency67 or excessive fetal retinoid exposure.98
Fetal growth
Low birth weight (LBW, <2.5 kg) can result from decrements in either fetal growth or length of gestation, while small for gestational age (SGA) is due to the former; however, both increase the risk of infant morbidity and mortality.99, 100 Inadequate maternal micronutrient nutriture might compromise birth size via either pathway. A number of antenatal supplement trials have assessed effects of single nutrients, most commonly iron and folic acid, on birth weight (Tables 3 & 4). A meta-analysis published in 2013 comparing antenatal iron (with or without folic acid) to no iron or placebo demonstrated an increase in birth weight (41 g) and 19% reduction in risk of LBW,101 although an updated estimate in 2015 incorporating more trials has yielded weaker and statistically nonsignificant effects of iron alone on birth weight (24 g; 95% CI –3–51 g) and the risk of LBW (RR 0.84; 95% CI 0.69–1.03).102 A pooled analysis if data from four trials of positive effects of antenatal folic acid on birth weight was deemed inconclusive due to low quality of evidence (potential selection bias and blinding issues) and a lack of other offspring benefits.103 At a policy level, IFA remains globally recommended by the WHO for antenatal use to reduce risks of maternal iron deficiency and consequent anaemia as well as risk of LBW.104 Folic acid is included in the WHO recommendation to help maintain maternal haemoglobin and reduce birth defects (if started periconceptionally) rather than increase birth weight.104 In other trials, vitamin A and zinc have each shown no impact on birth weight, SGA, or LBW.102, 103 In a meta-analysis of three small but high quality trials (n=493), supplemental vitamin D reduced the risk of LBW by 60% (RR: 0.40; 95% CI 0.24–0.67).105 The results of randomized trials have consistently shown antenatal, multiple micronutrient supplementation to modestly increase birth weight beyond that achieved with IFA, reducing LBW on average by 12% (95% CI: 9–15%),9 although nothing is known about the composition or tissue contribution(s) to the observed increment. While the results of meta-analyses suggest the effect is associated with a reduction in SGA (by 10%, 95% CI: 3–17%),9 implying increased intrauterine growth, a comparable reduction in LBW in a large trial in rural Bangladesh (by 12%, 95% CI: 9–15%) was associated with prolonged gestation rather than accelerated fetal growth and a lower risk of SGA.87
Preterm birth
Preterm birth, which occurs before 37 weeks’ gestation, is associated with increased risks of neonatal mortality,106, 107 poor postnatal growth108 and impaired cognition.109 A preterm infant also has less time to accrue adequate, late gestation nutritional reserves, which might contribute to postnatal micronutrient deficiency. However, evidence on whether maternal micronutrient deficiency predisposes a pregnancy to preterm birth is limited.86 Although antenatal iron or IFA improve fetal growth outcomes, their supplemental use during trials has not reduced risk of preterm birth.102, 110 Antenatal zinc supplementation can decrease risk of preterm birth, overall by 14%, but perplexingly without affecting birth size.111 Vitamin D, albeit with evidence from only 3 trials, reduces risk of preterm birth by a striking 64% (RR: 0.36, 95% CI: 0.14–0.93), complementing the effect on birth size noted above.105 In meta-analyses of the effects of multiple micronutrient trials in low-income countries around the world, but largely not powered to test effects of supplement use on preterm birth, have discerned no effect on this outcome.9 By contrast, in a large, adequately powered trial in Bangladesh investigators reported a 2–3 day longer gestation and 15% reduction in preterm birth (95% CI 9–20%) following daily antenatal multiple micronutrient versus IFA from the first trimester onward.87 These differing results suggest that pre-existing nutritional, disease and other environmental conditions might modify the public health impact of any given nutrition intervention.
Postnatal effects
Maternal micronutrient adequacy during pregnancy might alter the health and development of offspring during infancy, childhood, and even adulthood. Causal inferences can be drawn for effects when plausible biological pathways exist, the nutrient and comparative interventions were randomized, and compliance and follow-up of a cohort is high. The effects are likely to vary by nutrient and their interactions, ages of children when followed, metabolic networks and organ systems investigated, outcome indicators assessed as well as other ambient dietary, disease and contextual factors. Risk of death in the first year after birth is often examined as an endpoint. Outcomes investigated beyond the first year are few but have included child mortality, growth, body composition, cardiometabolic risk, immunity, respiratory function and cognition.
Infant and child mortality
In systematic reviews of iron supplementation both with and without folic acid, no impact on early neonatal (first 7 days),110 and neonatal (first 28 days) mortality have been reported.102 In Nepal, daily antenatal IFA with vitamin A (n=957 pregnancies) versus a control (vitamin A alone, n=1051) also did not reduce early infant mortality,112 but when followed up at 6–7 years of age at which point vital status was obtained on 96% of the cohort, a 34% reduction (Hazard ratio [HR]: 0.69; 95% CI 0.49–0.99) in mortality was noted in children born to mothers who received an antenatal IFA supplement.113 Mechanisms remain unexplained but are likely to be complicated given that a multiple micronutrient supplement also containing iron did not have a similar survival effect.113 A trial of antenatal selenium supplementation among women who had HIV in Tanzania reported a 57% reduction in post-neonatal mortality (HR: 0.43; 95% CI 0.19–0.99), though the effect was attenuated when neonatal and post-neonatal infant deaths were combined (HR: 0.64; 95% CI 0.36–1.13).114 In trials conducted in other low-income communities no effects on neonatal mortality have been found following randomized maternal supplementation with vitamin A or β-carotene, vitamin C, folic acid or zinc (Table 4).
Meta-analyses of multiple micronutrient supplementation trials, which although individually underpowered to detect differences in survival have, when combined to give adequate power , found no effect on neonatal mortality.9 However, the results of a few large and adequately powered trials have revealed more nuanced effects. For example, in a trial conducted in Indonesia, daily antenatal multiple micronutrient supplementation with vitamins A, D, E, B2, B3, B6, B9, B12 and C; iron, zinc, copper, selenium, and iodine had no effect on neonatal mortality but significantly reduced mortality by 3 months of age by 18% (RR 0.82, 95% CI 0.70–0.95), which suggests a latent benefit of these nutrients following fetal exposure.115 In Bangladesh, antenatal multiple micronutrient with the same formulation as used in Indonesia versus IFA supplementation had no effect on all-cause infant mortality in boys but lowered mortality in girls by 16%.87 In this study, the investigators suggested that a larger birth size for boys might have differentially increased the risk of dying from asphyxia in the first few days after birth, which was not seen in girls.87 Consequently, antenatal micronutrient supplementation might improve survival among offspring but the effect is likely to be modulated by local nutrition, disease and health care conditions. Unknown at present is the potential for preconceptional micronutrient interventions to affect survival of offspring during gestation and postnatally, which are effects requiring adequately sized population-based randomized trials with extended postnatal follow-up.86, 116
Growth and body composition
The modest increases in birth size following antenatal multi-nutrient versus IFA (or placebo) supplement use are generally not sustained during the preschool years. This finding is evident across nine trials that included children aged up to 5 years who had comparable distributions of weight, height and age-standardized indicators (weight-for-age, height-for-age, and weight-for-height z-scores).117 However, potentially important, is a sustained increment of 0.08 cm (95% CI: 0.00–0.15 cm) in head circumference that was larger in those exposed to multiple micronutrients as compared to the controls.117 By contrast, in Nepal, children aged 6–8 years and born to mothers who received folic acid, iron and zinc supplementation were taller by 0.64 cm (95% CI 0.04–1.25 cm) than children of mothers who received placebo.118 The increment was accompanied by smaller skinfold thicknesses, consistent with improved linear growth amidst comparable energy intakes.118 Inexplicably, a similar growth increment was not seen among children born to multiple micronutrient supplemented mothers, who received folic acid, iron, and zinc as part of their supplement,118 which we think implicates a chance growth effect or unknown nutrient interactions when multiple nutrients are regularly ingested in a single supplement.
Cardiometabolic, pulmonary and immune function
Experimental micronutrient depletion during gestation in multiple animal species has been shown to have cardiovascular consequences.69 However, evidence from childhood studies remains limited and inconclusive with respect changes in cardiometabolic risk indicators of blood pressure, kidney function and insulin resistance.69 In Nepal, where multiple micronutrient deficiencies co-exist,15 the investigators of one study reported a modest decrement in systolic blood pressure by 2.5 mmHg (95% CI 0.5–4.6 mmHg) at 2 years of age in children whose mothers received a multiple micronutrient versus IFA supplement during pregnancy;119 however, in two other studies, conducted in Nepal and Bangladesh, no differences in blood pressure were found by 4–8 years of age.120, 121 Neither was there an effect of maternal multi-nutrient supplementation on glomerular filtration measured in children aged 4 years.121
Plausible long-term effects of some individual nutrients, consistent with experimental data, have been discerned when provided as a sole nutrient during pregnancy in populations at high risk of deficiency. To illustrate, research primarily in mammalian and avian models has established roles of gestational vitamin A deficiency in compromising developing cardiovascular,122 pulmonary,122, 123 kidney,124 nervous,122 and immune125 systems. These findings have guided hypotheses of potential developmental effects among offspring of women supplemented with vitamin A in undernourished settings. For example, in rural Nepal, among 9-13 year old children born to mothers who were randomly assigned to receive weekly supplemental vitamin A (equivalent to an RDA) versus placebo before, during and after pregnancy had expanded lung capacity, which was evident by increased forced expiratory volume at 1 second and vital capacity.126 Innate immunity was also stimulated in children of vitamin A versus placebo-supplemented mothers, as evidenced by higher circulating concentrations of natural antibodies known to be secreted by lymphopoietic B1a cells, whose fetal progenitors have been shown to be sensitive to vitamin A nutriture.127 No effects were seen on blood pressure or microalbuminuria,128 seeming to reflect specificity in organ response to fetal vitamin A exposure in an endemic, vitamin A-deficient population.
Neurodevelopment and cognition
Maternal micronutrient deficiencies might also affect cognitive, motor, and socio-emotional development of offspring, although data examining these outcomes is inconclusive.60 A challenge in this area of research is the standardization and validation of methods that enable these outcomes across cultures to be measured comparably. The strongest, consistent evidence for cognitive improvement exists for iodine,129, 130 although only two RCTs of maternal supplementation have reported outcomes in children.129 Supplementing mothers before conception reduces (and possibly eliminates) the risk of cretinism when iodine deficiency is severe.129, 131 Observational studies suggest that mild maternal iodine deficiency is associated with an increased risk of cognitive impairment among offspring and that supplementation with iodine might be beneficial,31 although data from RCTs is lacking. Associations between gestational iron exposure and cognitive function have long been supported by mechanisms possibly involving iron in neuronal proliferation, myelination and metabolism to motivate antenatal trials. However, among mothers who are not anaemic living mostly in high-income countries, antenatal iron supplementation has had no detectable effects on cognitive or mental development test scores of offspring, although some improvement has been detected in psychomotor tests.132 In China, antenatal iron had no effects on the Bayley Scales of Infant Development (BSID) in infancy or on the intelligence quotient at 4 years of age.133 In Nepal, where iron deficiency is endemic, 7–9 year old children born to mothers randomized to receive IFA versus placebo during pregnancy exhibited improved intellectual, executive and motor test scores, effects that were attenuated in children whose mothers had also received antenatal zinc.134 While many plausible pathways exist linking zinc to neuronal development and function, trials of antenatal zinc supplementation in Peru, Nepal and Bangladesh have either had no effects134, 135 or, by 13 months of age, a potential negative effect on cognitive development, possibly due to competitive interactions with other nutrients such as iron or copper.136
A number of randomized, antenatal multiple micronutrient supplementation trials have been performed to assess the development outcomes in infancy or childhood. For example, in one study from Bangladesh, no overall cognitive or psychomotor developmental improvements were noted in children aged 7 months, although positive effects on motor scores (z score: 0.28; 95% CI 0.08–0.48) and activity ratings (z score: 0.24; 95% CI 0.037–0.45) were observed in children born to mothers with a low BMI.137 In China, there were supplementation benefits on the mental, but not psychomotor development scales, of the BSID in children reported at 1 year of age, yet no apparent differences between groups when children were evaluated at 7–10 years.138 Similarly, in Indonesia, no overall benefit of antenatal multiple micronutrient supplement use was seen on child development at 3 years of age; however, motor or visual attention/spatial abilities were improved compared to iron folic acid supplement use in children of mothers who were thin (arm circumference <23.5 cm) or anaemic (Hb <110 g/L).139 By contrast, no improvement in performance on tests of working memory, executive function, and motor ability was observed among Nepalese children aged 7–9 years whose mothers received a multiple micronutrient supplement versus placebo during pregnancy while positive effects on the same tests were seen following maternal receipt of IFA alone.134 In Tanzania, 6 to 18 month old infants born to mothers with HIV-1 infection who received multiple micronutrients during pregnancy scored higher on a psychomotor development index (β=2.6; 95% CI 0.1–5.1) and experienced a 60% reduction (RR: 0.4; 95% CI 0.2–0.7) in motor developmental delay compared to those in the placebo group.140 Taken together, little evidence exists to support the overall benefits of iron, zinc, or multiple micronutrients on motor or cognitive development, although though some benefits seem to be observed among high risk groups, such as children of mothers who are poorly nourished or have HIV infection. Stratified effects in trials merit caution, however, and future trials are need to reject or confirm these initial findings.
Prevention
The most desirable approach to prevent micronutrient deficiencies in pregnancy is to assure a sustained diet of various micronutrient dense foods.6 As such a diet is often difficult or expensive to attain, preventing adverse birth outcomes due to micronutrient deficiencies through supplementation represents a sound and effective strategy.141 The WHO has developed micronutrient supplement guidelines for pregnant women (Table 2). One of the most commonly adopted by many low-income countries is that of daily IFA supplementation as part of routine antenatal care to reduce the risk of low birth weight and maternal anaemia where iron deficiency is a public health problem.104 The WHO recommended daily dosage of iron is 30–60 g of elemental iron and 400 μg of folic acid beginning as early as possible in pregnancy.104 For low-income countries where the prevalence of anaemia among women of reproductive age (15-45 years) is ≥20%, intermittent IFA for menstruating women is also recommended.142 The International Federation of Gynecology and Obstetrics recommends the use of iodized salt to prevent gestational iodine deficiency disorders.6 However, iodine supplementation (250 μg per day) is recommended for pregnant women in countries where there is limited access to iodized salt. 143 Where the prevalence of vitamin A deficiency (hyporetinolemia) is 5% or more among pregnant women or in children aged 2 to under 5 years, WHO recommends gravida be supplemented with up to 10,000 IU daily or 25,000 IU weekly of vitamin A to prevent maternal night blindness.144 Even with evidence-based recommendations, implementation of these strategies is extremely challenging due to reasons of low rates of antenatal care, inadequate supply and poor adherence. For example, in one review, only 8% of women reported taking a full course of 180 or more iron-folic acid tablets during pregnancy.145
A balanced, diverse and nutritious diet is universally recommended to meet nutritional needs and maintain health during pregnancy. Daily antenatal multiple vitamin and mineral supplements are commonly taken prophylactically by women in the USA and other high-income countries, where there are few formal medical society recommendations to do so. More common are recommendations for individual micronutrients, such as in Germany, where pregnant women are advised to take folic acid and iodine supplements.146 In low-income countries, where evidence of fetal health benefit is increasing in support of multiple micronutrient supplement use during pregnancy, a WHO/UNICEF policy recommends that pregnant and lactating women to take a daily multiple micronutrient supplement in emergency settings (such as, refugee settings or natural disasters).7 Although the beneficial effects of antenatal multiple micronutrient supplementation on birth outcomes compared with IFA alone support change in global policy to promote this intervention in low-income and middle-income countries,9 no such broad WHO/UNICEF policy current exists for this purpose. Programmatic platforms, especially antenatal care visits, through which IFA supplements are distributed already exist although with variable success; Demographic and Health Survey data show any supplement use during pregnancy varies from ~10% to 90% of women across low-income countries.147 However, nutritional interventions that successfully increase birth size should be accompanied by adequate intrapartum care, via facility-based delivery or skilled birth attendants, especially where adolescent pregnancy and maternal stunting are common, to mitigate potential risks of intrapartum constraint and birth asphyxia-related complications.87
The preconceptional period is increasingly seen as a period of great influence in the life course, yet intervention efforts at this time are fewer than in pregnancy.86 In 53 countries worldwide, ranging from low-income to high-income, folic acid fortification of flour is mandatory (although this does not indicate compliance in all countries).148 Other strategies currently being tested but with potential impact on pregnancy outcomes include dual fortified salt (iron and iodine),149 iron-fortified flour,150 and biofortification of staple crops such as rice and maize.151 Overall, fortification is a promising strategy for improving micronutrient status during pregnancy, but data on health outcomes is scarce.152 Improving diets and the adequate and diverse intake of various food groups continues to be a long-term goal for enhancing maternal micronutrient status, regardless of geographical location or income status.
Knowledge gaps
Although evidence has rapidly accrued about roles of antenatal micronutrients on the health of the offspring, gaps in our knowledge still remain. Ascertaining nutritional risk during pregnancy will require refinement of dietary recommendations and pregnancy-specific tools for nutritional assessment. The Dietary Reference Intake reports for micronutrients all note a lack of pregnancy-specific data to accurately inform recommendations for this life stage.3, 153-155 Moreover, little information exists on specific requirements for women with pre-existing deficiencies, as the DRIs are established for healthy individuals. Improving micronutrient intake recommendations for pregnancy will require pregnancy-specific data and harmonized interpretation in order to use dietary recommendations and ascertain the risk of deficiencies in individuals and across populations. Understanding plasma volume in pregnancy and its impact on interpretation of biomarkers also deserves attention.78, 156 Improved global data on the prevalence or prevention of micronutrient deficiencies, beyond folate, iron, iodine, and vitamin A, using appropriate functional, biochemical or clinical indicators is also needed.
With better evidence of global deficiencies, more effective micronutrient delivery might be achievable through supplementation, the use of fortified (or biofortified) food, and dietary counseling or behavioural change programs. Current trials are lacking on effective strategies for influencing pregnancy-related diet and nutritional status in pregnancy in low-income contexts. Caveats for influencing dietary behavior during pregnancy must be better understood given that it is a life stage in which food aversions are common and cultural dietary practices, including food avoidance, persist, requiring qualitative research to understand barriers to improving micronutrient intakes. This gap in our knowledge needs to be urgently addressed.
Perhaps the most ambitious need is to establish a comprehensive understanding of the biological pathways and effects of single and multiple micronutrient interventions. Key questions for future research include what are the nutrient interactions, optimal timing and dosage of nutrient delivery, and the wide spectrum of metabolic and functional outcomes that are affected. Specifically, a better understanding is needed of the effects of micronutrients on gestational viability, epigenesis, implantation and placenta biology, as well as nutrient functions in pathways of morphogenesis, pattern formation, neurogenesis, and cardiovascular development. Micronutrient provision before and just after conception might be important to assure normal placentation and embryogenesis in malnourished populations, as intervening later in pregnancy might not realize the full potential impact. However, most interventions tested to date have begun supplementation only after the first trimester, leaving confirmatory effects of intervening earlier an unmet research need.
Randomized, controlled trials in pregnancy remain sparse to absent for evaluating vitamin B12, vitamin B6, vitamin E, copper and selenium, while other micronutrients of high interest (such as vitamin D) lack trials of adequate size to examine effects on outcomes such as preterm birth and preeclampsia. Although global multiple micronutrient supplement recommendations of approximately one RDA for a variety of nutrients are anticipated, increased amounts of some nutrients might be warranted, for example for iodine, zinc, vitamin B12, and vitamin D, if shown to be safe and beneficial.
Conclusions
Micronutrient deficiencies in pregnancy remain widespread globally. In low-resource settings, although the burden of the so called ‘hidden hunger’ during pregnancy remains to be fully revealed, diets are inadequate and micronutrient deficiencies are common. Although adequate food intake remains the preferred means for meeting dietary requirements for micronutrients, some nutrient needs are challenging to meet in pregnancy with diet alone. In response, some countries (across all income levels) fortify selected foods and/or recommend the use of dietary supplements. Micronutrient research in pregnancy has made dramatic advances in the past two decades. Antenatal multiple micronutrient supplement use has emerged as an important public health intervention for women in low-income countries and has benefits for birth outcomes over and above IFA, which is currently recommended for pregnant women by the WHO. Some individual micronutrients (for example, iodine, zinc, vitamin B12 and vitamin D) deserve more attention for their potential to further improve offspring outcomes beyond the single daily dose provided in a typical multi-supplement. Micronutrient deficiencies might also have consequences for longer term outcomes of survival, cognition, and cardiometabolic risk in the offspring, further attesting to their importance in early life, but this is not yet evident. Multiple micronutrient supplement is an effective strategy during the critically important biological period of pregnancy; however, much more research is warranted during the preconceptional period.
Key Points.
Micronutrient deficiencies during pregnancy are a global public health concern, yet the full extent of their burden and health consequences are unclear due to infrequent and inadequate assessment
Micronutrient deficiencies have been linked to compromised conception, length of gestation, and fetal development and growth, which can lead to pregnancy loss, preterm delivery, small birth size, birth defects, and long-term metabolic disturbances
Antenatal supplementation with multiple micronutrients can improve birth outcomes and merits policy and program consideration in low-income settings
Preconception and periconception intervention research is needed to further assess the full public health impact of micronutrient adequacy on pregnancy outcomes
Acknowledgements
The authors wish to thank R. Guida and C. Reynolds, Pennsylvania State University, PA, USA for assistance with the literature review. A.D.G. is supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under BIRCWH award number K12HD055882, ‘Career Development Program in Women’s Health Research at Penn State’. C.P.S. is supported by the Bill and Melinda Gates Foundation (Grant OPPGD759) and the Thrasher Research Fund (award number 11860).K.J.S, K.P.W.Jr. and P.C. gratefully acknowledge support from the Bill and Melinda Gates Foundation (Grants GH614 and OPP5241), Seattle, Washington, USA, and the Sight and Life Global Nutrition Research Institute, Baltimore, Maryland, USA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or Bill and Melinda Gates Foundation.
Footnotes
Author contributions
The authors contributed equally to all aspects of this article.
Competing interests statement
The authors declare no competing interests.
Review criteria
Our main search strategy for this paper was a PubMed search for articles in English using the MeSH terms “female AND humans AND pregnancy AND (“Meta-Analysis” [Publication Type] OR “review” [Publication Type])” plus the MeSH term for each vitamin or mineral of interest.
References
- 1.IOM . Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. The National Academies Press; Washington, D.C.: 2006. [Google Scholar]
- 2.WHO & FAO . Vitamin and mineral requirements in human nutrition: report of a joint FAO/WHO expert consultation, Bangkok, Thailand, 21-30 September 1998. World Health Organization; Geneva: 2004. [Google Scholar]
- 3.IOM . Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. The National Academies Press; Washington, DC: 2001. [PubMed] [Google Scholar]
- 4.De Backer G, Hautvast J. EURRECA (EURopean micronutrient RECommendations Aligned) Network of Excellence. Eur J Clin Nutr. 2010;64(Suppl 2):S1. doi: 10.1038/ejcn.2010.54. [DOI] [PubMed] [Google Scholar]
- 5.Stamm RA, Houghton LA. Nutrient intake values for folate during pregnancy and lactation vary widely around the world. Nutrients. 2013;5:3920–47. doi: 10.3390/nu5103920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanson MA, et al. The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition: "Think Nutrition First". Int J Gynaecol Obstet. 2015;131(Suppl 4):S213. doi: 10.1016/S0020-7292(15)30034-5. [DOI] [PubMed] [Google Scholar]
- 7.WHO, WFP & UNICEF . Joint statement by the World Health Organization, the World Food Programme and the United Nations Children’s Fund. World Health Organization; 2007. [Google Scholar]
- 8.UNICEF/WHO/UNU . Composition of a multi-micronutrient supplement to be used in pilot programmes among pregnant women in developing countries. UNICEF; New York: 1999. [Google Scholar]
- 9.Haider BA, Bhutta ZA. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev. 2015;1 doi: 10.1002/14651858.CD004905.pub4. CD004905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torheim LE, Ferguson EL, Penrose K, Arimond M. Women in resource-poor settings are at risk of inadequate intakes of multiple micronutrients. J Nutr. 2010:2051S–8S. doi: 10.3945/jn.110.123463. 0. [DOI] [PubMed] [Google Scholar]
- 11.Muthayya S, et al. The global hidden hunger indices and maps: an advocacy tool for action. PLoS One. 2013;8:e67860. doi: 10.1371/journal.pone.0067860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Black RE, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;2:427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 13.WHO . Global prevalence of vitamin A deficiency in populations at risk 1995-2005: WHO global database on vitamin A deficiency. World Health Organization; Geneva: 2009. [Google Scholar]
- 14.Wong EM, Sullivan KM, Perrine CG, Rogers LM, Pena-Rosas JP. Comparison of median urinary iodine concentration as an indicator of iodine status among pregnant women, school-age children, and nonpregnant women. Food Nutr Bull. 2011;2:206–12. doi: 10.1177/156482651103200304. [DOI] [PubMed] [Google Scholar]
- 15.Jiang T, Christian P, Khatry SK, Wu L, West KP., Jr. Micronutrient deficiencies in early pregnancy are common, concurrent, and vary by season among rural Nepali pregnant women. J Nutr. 2005;5:1106–12. doi: 10.1093/jn/135.5.1106. [DOI] [PubMed] [Google Scholar]
- 16.Akhtar S. Zinc status in South Asian populations--an update. J Health Popul Nutr. 2013;1:139–49. doi: 10.3329/jhpn.v31i2.16378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindstrom E, et al. Prevalence of anemia and micronutrient deficiencies in early pregnancy in rural Bangladesh, the MINIMat trial. Acta Obstet Gynecol Scand. 2011:47–56. doi: 10.1111/j.1600-0412.2010.01014.x. 0. [DOI] [PubMed] [Google Scholar]
- 18.Shamim AA, et al. Plasma zinc, vitamin B(12) and alpha-tocopherol are positively and plasma gamma-tocopherol is negatively associated with Hb concentration in early pregnancy in north-west Bangladesh. Public Health Nutr. 2013;6:1354–61. doi: 10.1017/S1368980013000475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pathak P, et al. Iron, folate, and vitamin B12 stores among pregnant women in a rural area of Haryana State, India. Food Nutr Bull. 2007;8:435–8. doi: 10.1177/156482650702800409. [DOI] [PubMed] [Google Scholar]
- 20.Siddiqua TJ, et al. Vitamin B12 supplementation during pregnancy and postpartum improves B12 status of both mothers and infants but vaccine response in mothers only: a randomized clinical trial in Bangladesh. Eur J Nutr. 2015 doi: 10.1007/s00394-015-0845-x. [DOI] [PubMed] [Google Scholar]
- 21.Shamim AA, et al. First-trimester plasma tocopherols are associated with risk of miscarriage in rural Bangladesh. Am J Clin Nutr. 2015;1:294–301. doi: 10.3945/ajcn.114.094920. [DOI] [PubMed] [Google Scholar]
- 22.Campbell RK, et al. Seasonal dietary intakes and socioeconomic status among women in the Terai of Nepal. J Health Popul Nutr. 2014;2:198–216. [PMC free article] [PubMed] [Google Scholar]
- 23.Palacios C, Gonzalez L. Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol. 2014;144(Pt A):138–45. doi: 10.1016/j.jsbmb.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hilger J, et al. A systematic review of vitamin D status in populations worldwide. Br J Nutr. 2014;1:23–45. doi: 10.1017/S0007114513001840. [DOI] [PubMed] [Google Scholar]
- 25.Lee SE, Talegawkar SA, Merialdi M, Caulfield LE. Dietary intakes of women during pregnancy in low- and middle-income countries. Public Health Nutr. 2013;6:1340–53. doi: 10.1017/S1368980012004417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berner LA, Keast DR, Bailey RL, Dwyer JT. Fortified foods are major contributors to nutrient intakes in diets of US children and adolescents. J Acad Nutr Diet. 2014;4:1009–1022. e8. doi: 10.1016/j.jand.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 27.Branum AM, Bailey R, Singer BJ. Dietary supplement use and folate status during pregnancy in the United States. J Nutr. 2013;3:486–92. doi: 10.3945/jn.112.169987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parisi F, Laoreti A, Cetin I. Multiple micronutrient needs in pregnancy in industrialized countries. Ann Nutr Metab. 2014;5:13–21. doi: 10.1159/000365794. [DOI] [PubMed] [Google Scholar]
- 29.Blumfield ML, Hure AJ, Macdonald-Wicks L, Smith R, Collins CE. A systematic review and meta-analysis of micronutrient intakes during pregnancy in developed countries. Nutr Rev. 2013;1:118–32. doi: 10.1111/nure.12003. [DOI] [PubMed] [Google Scholar]
- 30.Troesch B, Hoeft B, McBurney M, Eggersdorfer M, Weber P. Dietary surveys indicate vitamin intakes below recommendations are common in representative Western countries. Br J Nutr. 2012;8:692–8. doi: 10.1017/S0007114512001808. [DOI] [PubMed] [Google Scholar]
- 31.Trumpff C, et al. Mild iodine deficiency in pregnancy in Europe and its consequences for cognitive and psychomotor development of children: a review. J Trace Elem Med Biol. 2013;7:174–83. doi: 10.1016/j.jtemb.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Gahche JJ, Bailey RL, Mirel LB, Dwyer JT. The prevalence of using iodine-containing supplements is low among reproductive-age women, NHANES 1999-2006. J Nutr. 2013;3:872–7. doi: 10.3945/jn.112.169326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pfeiffer CM, Schleicher RL, Johnson CL, Coates PM. Assessing vitamin status in large population surveys by measuring biomarkers and dietary intake - two case studies: folate and vitamin D. Food Nutr Res. 2012;6 doi: 10.3402/fnr.v56i0.5944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crider KS, Bailey LB, Berry RJ. Folic Acid Food Fortification—Its History, Effect, Concerns, and Future Directions. Nutrients. 2011;3:370–384. doi: 10.3390/nu3030370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Looker AC, et al. Vitamin D status: United States, 2001-2006. NCHS Data Brief. 2011:1–8. [PubMed] [Google Scholar]
- 36.Karras SN, et al. Maternal vitamin D status during pregnancy: the Mediterranean reality. Eur J Clin Nutr. 2014;8:864–9. doi: 10.1038/ejcn.2014.80. [DOI] [PubMed] [Google Scholar]
- 37.Mei Z, et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999-2006. Am J Clin Nutr. 2011;3:1312–20. doi: 10.3945/ajcn.110.007195. [DOI] [PubMed] [Google Scholar]
- 38.Christian P. Micronutrients, birth weight, and survival. Annu Rev Nutr. 2010:83–104. doi: 10.1146/annurev.nutr.012809.104813. 0. [DOI] [PubMed] [Google Scholar]
- 39.Steegers-Theunissen RP, Twigt J, Pestinger V, Sinclair KD. The periconceptional period, reproduction and long-term health of offspring: the importance of one-carbon metabolism. Hum Reprod Update. 2013;9:640–55. doi: 10.1093/humupd/dmt041. [DOI] [PubMed] [Google Scholar]
- 40.Sinclair KD, et al. DNA methylation, insulin resistance, and blood pressure in offspring determined by maternal periconceptional B vitamin and methionine status. Proc Natl Acad Sci U S A. 2007;4:19351–6. doi: 10.1073/pnas.0707258104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khulan B, et al. Periconceptional maternal micronutrient supplementation is associated with widespread gender related changes in the epigenome: a study of a unique resource in the Gambia. Hum Mol Genet. 2012;1:2086–101. doi: 10.1093/hmg/dds026. [DOI] [PubMed] [Google Scholar]
- 42.Lebold KM, Traber MG. Interactions between alpha-tocopherol, polyunsaturated fatty acids, and lipoxygenases during embryogenesis. Free Radic Biol Med. 2014;6:13–9. doi: 10.1016/j.freeradbiomed.2013.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mistry HD, Williams PJ. The importance of antioxidant micronutrients in pregnancy. Oxid Med Cell Longev. 2011;1:841749. doi: 10.1155/2011/841749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stagnaro-Green A, Pearce E. Thyroid disorders in pregnancy. Nat Rev Endocrinol. 2012;8:650–8. doi: 10.1038/nrendo.2012.171. [DOI] [PubMed] [Google Scholar]
- 45.Cao C, O'Brien KO. Pregnancy and iron homeostasis: an update. Nutr Rev. 2013;1:35–51. doi: 10.1111/j.1753-4887.2012.00550.x. [DOI] [PubMed] [Google Scholar]
- 46.Zingg JM, Meydani M, Azzi A. alpha-Tocopheryl phosphate--an activated form of vitamin E important for angiogenesis and vasculogenesis? Biofactors. 2012;8:24–33. doi: 10.1002/biof.198. [DOI] [PubMed] [Google Scholar]
- 47.Levine MJ, Teegarden D. 1alpha,25-dihydroxycholecalciferol increases the expression of vascular endothelial growth factor in C3H10T1/2 mouse embryo fibroblasts. J Nutr. 2004;4:2244–50. doi: 10.1093/jn/134.9.2244. [DOI] [PubMed] [Google Scholar]
- 48.Cantorna MT. Mechanisms underlying the effect of vitamin D on the immune system. Proc Nutr Soc. 2010;9:286–9. doi: 10.1017/S0029665110001722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fabri M, et al. Vitamin D is required for IFN-gamma-mediated antimicrobial activity of human macrophages. Sci Transl Med. 2011;3:104ra102. doi: 10.1126/scitranslmed.3003045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu NQ, Hewison M. Vitamin D, the placenta and pregnancy. Arch Biochem Biophys. 2012;3:37–47. doi: 10.1016/j.abb.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 51.Allen LH. Biological mechanisms that might underlie iron's effects on fetal growth and preterm birth. J Nutr. 2001;1:581S–589S. doi: 10.1093/jn/131.2.581S. [DOI] [PubMed] [Google Scholar]
- 52.Uriu-Adams JY, Keen CL. Zinc and reproduction: effects of zinc deficiency on prenatal and early postnatal development. Birth Defects Res B Dev Reprod Toxicol. 2010;9:313–25. doi: 10.1002/bdrb.20264. [DOI] [PubMed] [Google Scholar]
- 53.Tian X, Anthony K, Neuberger T, Diaz FJ. Preconception zinc deficiency disrupts postimplantation fetal and placental development in mice. Biol Reprod. 2014:83. doi: 10.1095/biolreprod.113.113910. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gluckman PD, Pinal CS. Maternal-placental-fetal interactions in the endocrine regulation of fetal growth: role of somatotrophic axes. Endocrine. 2002;9:81–9. doi: 10.1385/ENDO:19:1:81. [DOI] [PubMed] [Google Scholar]
- 55.Gernand AD, et al. Effects of Prenatal Multiple Micronutrient Supplementation on Fetal Growth Factors: A Cluster-Randomized, Controlled Trial in Rural Bangladesh. PLoS One. 2015:e0137269. doi: 10.1371/journal.pone.0137269. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Roberfroid D, et al. Effect of maternal multiple micronutrient supplements on cord blood hormones: a randomized controlled trial. Am J Clin Nutr. 2010;1:1649–58. doi: 10.3945/ajcn.2009.28855. [DOI] [PubMed] [Google Scholar]
- 57.Akram SK, Akram M, Bhutta ZA, Soder O. Human placental IGF-I and IGF-II expression: correlating maternal and infant anthropometric variables and micronutrients at birth in the Pakistani population. Acta Paediatr. 2008;7:1443–8. doi: 10.1111/j.1651-2227.2008.00930.x. [DOI] [PubMed] [Google Scholar]
- 58.Akman I, et al. Maternal zinc and cord blood zinc, insulin-like growth factor-1, and insulin-like growth factor binding protein-3 levels in small-for-gestational-age newborns. Clin Exp Obstet Gynecol. 2006;3:238–40. [PubMed] [Google Scholar]
- 59.Hanna LA, Clegg MS, Ellis-Hutchings RG, Niles BJ, Keen CL. The influence of gestational zinc deficiency on the fetal insulin-like growth factor axis in the rat. Exp Biol Med (Maywood) 2010;5:206–14. doi: 10.1258/ebm.2009.009018. [DOI] [PubMed] [Google Scholar]
- 60.Fowden AL, Moore T. Maternal-fetal resource allocation: co-operation and conflict. Placenta. 2012;33(Suppl 2):e11–5. doi: 10.1016/j.placenta.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 61.Sandovici I, Hoelle K, Angiolini E, Constancia M. Placental adaptations to the maternal-fetal environment: implications for fetal growth and developmental programming. Reprod Biomed Online. 2012;5:68–89. doi: 10.1016/j.rbmo.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 62.Antony AC. In utero physiology: role of folic acid in nutrient delivery and fetal development. Am J Clin Nutr. 2007;5:598S–603S. doi: 10.1093/ajcn/85.2.598S. [DOI] [PubMed] [Google Scholar]
- 63.Donangelo CM, King JC. Maternal zinc intakes and homeostatic adjustments during pregnancy and lactation. Nutrients. 2012;4:782–98. doi: 10.3390/nu4070782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dror DK, Allen LH. Interventions with vitamins B6, B12 and C in pregnancy. Paediatr Perinat Epidemiol. 2012;26(Suppl 1):55–74. doi: 10.1111/j.1365-3016.2012.01277.x. [DOI] [PubMed] [Google Scholar]
- 65.Clagett-Dame M, Knutson D. Vitamin A in reproduction and development. Nutrients. 2011;3:385–428. doi: 10.3390/nu3040385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kovacs CS. The role of vitamin D in pregnancy and lactation: insights from animal models and clinical studies. Annu Rev Nutr. 2012;2:97–123. doi: 10.1146/annurev-nutr-071811-150742. [DOI] [PubMed] [Google Scholar]
- 67.Emmett SD, West KP., Jr. Gestational vitamin A deficiency: a novel cause of sensorineural hearing loss in the developing world? Med Hypotheses. 2014;2:6–10. doi: 10.1016/j.mehy.2013.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Szostak-Wegierek D. Intrauterine nutrition: long-term consequences for vascular health. Int J Womens Health. 2014;6:647–56. doi: 10.2147/IJWH.S48751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Christian P, Stewart CP. Maternal micronutrient deficiency, fetal development, and the risk of chronic disease. J Nutr. 2010:437–45. doi: 10.3945/jn.109.116327. 0. [DOI] [PubMed] [Google Scholar]
- 70.Georgieff MK. Nutrition and the developing brain: nutrient priorities and measurement. Am J Clin Nutr. 2007;5:614S–620S. doi: 10.1093/ajcn/85.2.614S. [DOI] [PubMed] [Google Scholar]
- 71.Williams GR. Neurodevelopmental and neurophysiological actions of thyroid hormone. J Neuroendocrinol. 2008:784–94. doi: 10.1111/j.1365-2826.2008.01733.x. 0. [DOI] [PubMed] [Google Scholar]
- 72.Morse NL. Benefits of docosahexaenoic acid, folic acid, vitamin D and iodine on foetal and infant brain development and function following maternal supplementation during pregnancy and lactation. Nutrients. 2012;4:799–840. doi: 10.3390/nu4070799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Levenson CW, Morris D. Zinc and neurogenesis: making new neurons from development to adulthood. Adv Nutr. 2011;2:96–100. doi: 10.3945/an.110.000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Georgieff MK. The role of iron in neurodevelopment: fetal iron deficiency and the developing hippocampus. Biochem Soc Trans. 2008;6:1267–71. doi: 10.1042/BST0361267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Prado EL, Dewey KG. Nutrition and brain development in early life. Nutr Rev. 2014;2:267–84. doi: 10.1111/nure.12102. [DOI] [PubMed] [Google Scholar]
- 76.Siddappa AM, Rao R, Long JD, Widness JA, Georgieff MK. The assessment of newborn iron stores at birth: a review of the literature and standards for ferritin concentrations. Neonatology. 2007;2:73–82. doi: 10.1159/000100805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Allen LH. Maternal micronutrient malnutrition: effects on breast milk and infant nutrition, and priorities for intervention. SCN News. 1994:21–4. [PubMed] [Google Scholar]
- 78.Tuttle S, Aggett PJ, Campbell D, MacGillivray I. Zinc and copper nutrition in human pregnancy: a longitudinal study in normal primigravidae and in primigravidae at risk of delivering a growth retarded baby. Am J Clin Nutr. 1985;1:1032–41. doi: 10.1093/ajcn/41.5.1032. [DOI] [PubMed] [Google Scholar]
- 79.Wu G, Imhoff-Kunsch B, Girard AW. Biological mechanisms for nutritional regulation of maternal health and fetal development. Paediatr Perinat Epidemiol. 2012;26(Suppl 1):4–26. doi: 10.1111/j.1365-3016.2012.01291.x. [DOI] [PubMed] [Google Scholar]
- 80.Kumar KA, et al. Maternal dietary folate and/or vitamin B12 restrictions alter body composition (adiposity) and lipid metabolism in Wistar rat offspring. J Nutr Biochem. 2013;4:25–31. doi: 10.1016/j.jnutbio.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 81.Rao KR, Padmavathi IJ, Raghunath M. Maternal micronutrient restriction programs the body adiposity, adipocyte function and lipid metabolism in offspring: a review. Rev Endocr Metab Disord. 2012;3:103–8. doi: 10.1007/s11154-012-9211-y. [DOI] [PubMed] [Google Scholar]
- 82.Ba A. Perinatal thiamine deficiency-induced spontaneous abortion and pup-killing responses in rat dams. Nutr Neurosci. 2013;6:69–77. doi: 10.1179/1476830512Y.0000000032. [DOI] [PubMed] [Google Scholar]
- 83.Abdulah R, et al. Reduced serum selenium concentration in miscarriage incidence of Indonesian subjects. Biol Trace Elem Res. 2013;4:1–6. doi: 10.1007/s12011-013-9701-0. [DOI] [PubMed] [Google Scholar]
- 84.Gaskins AJ, et al. Maternal prepregnancy folate intake and risk of spontaneous abortion and stillbirth. Obstet Gynecol. 2014;4:23–31. doi: 10.1097/AOG.0000000000000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rumbold A, Middleton P, Pan N, Crowther CA. Vitamin supplementation for preventing miscarriage. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD004073.pub3. CD004073. [DOI] [PubMed] [Google Scholar]
- 86.Ramakrishnan U, Grant F, Goldenberg T, Zongrone A, Martorell R. Effect of women's nutrition before and during early pregnancy on maternal and infant outcomes: a systematic review. Paediatr Perinat Epidemiol. 2012;26(Suppl 1):285–301. doi: 10.1111/j.1365-3016.2012.01281.x. [DOI] [PubMed] [Google Scholar]
- 87.West KP, Jr., et al. Effect of maternal multiple micronutrient vs iron-folic acid supplementation on infant mortality and adverse birth outcomes in rural Bangladesh: the JiVitA-3 randomized trial. JAMA. 2014;2:2649–58. doi: 10.1001/jama.2014.16819. [DOI] [PubMed] [Google Scholar]
- 88.Au KS, Ashley-Koch A, Northrup H. Epidemiologic and genetic aspects of spina bifida and other neural tube defects. Dev Disabil Res Rev. 2010;6:6–15. doi: 10.1002/ddrr.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Allagh KP, et al. Birth prevalence of neural tube defects and orofacial clefts in India: a systematic review and meta-analysis. PLoS One. 2015:e0118961. doi: 10.1371/journal.pone.0118961. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hibbard BM, Hibbard ED, Jeffcoate TN. Folic acid and reproduction. Acta Obstet Gynecol Scand. 1965;4:375–400. doi: 10.3109/00016346509155874. [DOI] [PubMed] [Google Scholar]
- 91.Molloy AM, Brody LC, Mills JL, Scott JM, Kirke PN. The search for genetic polymorphisms in the homocysteine/folate pathway that contribute to the etiology of human neural tube defects. Birth Defects Res A Clin Mol Teratol. 2009;5:285–94. doi: 10.1002/bdra.20566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.De-Regil LM, Fernandez-Gaxiola AC, Dowswell T, Pena-Rosas JP. Effects and safety of periconceptional folate supplementation for preventing birth defects. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD007950.pub2. CD007950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Williams J, et al. Updated estimates of neural tube defects prevented by mandatory folic Acid fortification - United States, 1995-2011. MMWR Morb Mortal Wkly Rep. 2015;4:1–5. [PMC free article] [PubMed] [Google Scholar]
- 94.Czeizel AE, Dudas I, Vereczkey A, Banhidy F. Folate deficiency and folic acid supplementation: the prevention of neural-tube defects and congenital heart defects. Nutrients. 2013;5:4760–75. doi: 10.3390/nu5114760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bortolus R, et al. Prevention of congenital malformations and other adverse pregnancy outcomes with 4.0 mg of folic acid: community-based randomized clinical trial in Italy and the Netherlands. BMC Pregnancy Childbirth. 2014;4:166. doi: 10.1186/1471-2393-14-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Krapels IP, et al. Maternal dietary B vitamin intake, other than folate, and the association with orofacial cleft in the offspring. Eur J Nutr. 2004;3:7–14. doi: 10.1007/s00394-004-0433-y. [DOI] [PubMed] [Google Scholar]
- 97.Botto LD, Olney RS, Erickson JD. Vitamin supplements and the risk for congenital anomalies other than neural tube defects. Am J Med Genet C Semin Med Genet. 2004;125C:12–21. doi: 10.1002/ajmg.c.30004. [DOI] [PubMed] [Google Scholar]
- 98.Teratology Society position paper: recommendations for vitamin A use during pregnancy. Teratology. 1987;5:269–75. doi: 10.1002/tera.1420350215. [DOI] [PubMed] [Google Scholar]
- 99.McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;2:82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- 100.Katz J, et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet. 2013;2:417–25. doi: 10.1016/S0140-6736(13)60993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Haider BA, et al. Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: systematic review and meta-analysis. BMJ. 2013;6:f3443. doi: 10.1136/bmj.f3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pena-Rosas JP, De-Regil LM, Garcia-Casal MN, Dowswell T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015;7 doi: 10.1002/14651858.CD004736.pub5. CD004736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lassi ZS, Salam RA, Haider BA, Bhutta ZA. Folic acid supplementation during pregnancy for maternal health and pregnancy outcomes. Cochrane Database Syst Rev. 2013;3 doi: 10.1002/14651858.CD006896.pub2. CD006896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.WHO . Guideline: Daily iron and folic acid supplementation in pregnant women. World Health Organization; Geneva: 2012. [PubMed] [Google Scholar]
- 105.De-Regil LM, Palacios C, Lombardo LK, Pena-Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2016;1 doi: 10.1002/14651858.CD008873.pub3. CD008873. [DOI] [PubMed] [Google Scholar]
- 106.Lawn JE, et al. Every Newborn: progress, priorities, and potential beyond survival. Lancet. 2014;4:189–205. doi: 10.1016/S0140-6736(14)60496-7. [DOI] [PubMed] [Google Scholar]
- 107.Platt MJ. Outcomes in preterm infants. Public Health. 2014;8:399–403. doi: 10.1016/j.puhe.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 108.Christian P, et al. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low- and middle-income countries. Int J Epidemiol. 2013;2:1340–55. doi: 10.1093/ije/dyt109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mwaniki MK, Atieno M, Lawn JE, Newton CR. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet. 2012;9:445–52. doi: 10.1016/S0140-6736(11)61577-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Imdad A, Bhutta ZA. Routine iron/folate supplementation during pregnancy: effect on maternal anaemia and birth outcomes. Paediatr Perinat Epidemiol. 2012;26(Suppl 1):168–77. doi: 10.1111/j.1365-3016.2012.01312.x. [DOI] [PubMed] [Google Scholar]
- 111.Ota E, et al. Zinc supplementation for improving pregnancy and infant outcome. Cochrane Database Syst Rev. 2015;2 doi: 10.1002/14651858.CD000230.pub5. CD000230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Christian P, et al. Effects of alternative maternal micronutrient supplements on low birth weight in rural Nepal: double blind randomised community trial. BMJ. 2003;6:571. doi: 10.1136/bmj.326.7389.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Christian P, et al. Antenatal and postnatal iron supplementation and childhood mortality in rural Nepal: a prospective follow-up in a randomized, controlled community trial. Am J Epidemiol. 2009:1127–36. doi: 10.1093/aje/kwp253. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kupka R, et al. Randomized, double-blind, placebo-controlled trial of selenium supplements among HIV-infected pregnant women in Tanzania: effects on maternal and child outcomes. Am J Clin Nutr. 2008;7:1802–8. doi: 10.1093/ajcn/87.6.1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Shankar AH, et al. Effect of maternal multiple micronutrient supplementation on fetal loss and infant death in Indonesia: a double-blind cluster-randomised trial. Lancet. 2008;1:215–27. doi: 10.1016/S0140-6736(08)60133-6. [DOI] [PubMed] [Google Scholar]
- 116.Potdar RD, et al. Improving women's diet quality preconceptionally and during gestation: effects on birth weight and prevalence of low birth weight--a randomized controlled efficacy trial in India (Mumbai Maternal Nutrition Project) Am J Clin Nutr. 2014:1257–68. doi: 10.3945/ajcn.114.084921. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lu WP, Lu MS, Li ZH, Zhang CX. Effects of multimicronutrient supplementation during pregnancy on postnatal growth of children under 5 years of age: a meta-analysis of randomized controlled trials. PLoS One. 2014;9:e88496. doi: 10.1371/journal.pone.0088496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Stewart CP, Christian P, LeClerq SC, West KP, Jr., Khatry SK. Antenatal supplementation with folic acid + iron + zinc improves linear growth and reduces peripheral adiposity in school-age children in rural Nepal. Am J Clin Nutr. 2009:132–40. doi: 10.3945/ajcn.2008.27368. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vaidya A, et al. Effects of antenatal multiple micronutrient supplementation on children's weight and size at 2 years of age in Nepal: follow-up of a double-blind randomised controlled trial. Lancet. 2008;1:492–9. doi: 10.1016/S0140-6736(08)60172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Stewart CP, et al. Antenatal micronutrient supplementation reduces metabolic syndrome in 6- to 8-year-old children in rural Nepal. J Nutr. 2009;9:1575–81. doi: 10.3945/jn.109.106666. [DOI] [PubMed] [Google Scholar]
- 121.Hawkesworth S, et al. Combined food and micronutrient supplements during pregnancy have limited impact on child blood pressure and kidney function in rural Bangladesh. J Nutr. 2013;3:728–34. doi: 10.3945/jn.112.168518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zile MH. Function of vitamin A in vertebrate embryonic development. J Nutr. 2001;1:705–8. doi: 10.1093/jn/131.3.705. [DOI] [PubMed] [Google Scholar]
- 123.Biesalski HK, Nohr D. New aspects in vitamin a metabolism: the role of retinyl esters as systemic and local sources for retinol in mucous epithelia. J Nutr. 2004;4:3453S–3457S. doi: 10.1093/jn/134.12.3453S. [DOI] [PubMed] [Google Scholar]
- 124.Bhat PV, Manolescu DC. Role of vitamin A in determining nephron mass and possible relationship to hypertension. J Nutr. 2008;8:1407–10. doi: 10.1093/jn/138.8.1407. [DOI] [PubMed] [Google Scholar]
- 125.Pino-Lagos K, Benson MJ, Noelle RJ. Retinoic acid in the immune system. Ann N Y Acad Sci. 2008;3:170–87. doi: 10.1196/annals.1443.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Checkley W, et al. Maternal vitamin A supplementation and lung function in offspring. N Engl J Med. 2010;2:1784–94. doi: 10.1056/NEJMoa0907441. [DOI] [PubMed] [Google Scholar]
- 127.Palmer AC, Schulze KJ, Khatry SK, De Luca LM, West KP., Jr. Maternal vitamin A supplementation increases natural antibody concentrations of preadolescent offspring in rural Nepal. Nutrition. 2015;1:813–9. doi: 10.1016/j.nut.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 128.Stewart CP, et al. Maternal supplementation with vitamin A or beta-carotene and cardiovascular risk factors among pre-adolescent children in rural Nepal. J Dev Orig Health Dis. 2010;1:262–70. doi: 10.1017/S2040174410000255. [DOI] [PubMed] [Google Scholar]
- 129.Zhou SJ, Anderson AJ, Gibson RA, Makrides M. Effect of iodine supplementation in pregnancy on child development and other clinical outcomes: a systematic review of randomized controlled trials. Am J Clin Nutr. 2013;8:1241–54. doi: 10.3945/ajcn.113.065854. [DOI] [PubMed] [Google Scholar]
- 130.Bougma K, Aboud FE, Harding KB, Marquis GS. Iodine and mental development of children 5 years old and under: a systematic review and meta-analysis. Nutrients. 2013;5:1384–416. doi: 10.3390/nu5041384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Pharoah PO, Buttfield IH, Hetzel BS. Neurological damage to the fetus resulting from severe iodine deficiency during pregnancy. Lancet. 1971;1:308–10. doi: 10.1016/s0140-6736(71)91040-3. [DOI] [PubMed] [Google Scholar]
- 132.Szajewska H, Ruszczynski M, Chmielewska A. Effects of iron supplementation in nonanemic pregnant women, infants, and young children on the mental performance and psychomotor development of children: a systematic review of randomized controlled trials. Am J Clin Nutr. 2010;1:1684–90. doi: 10.3945/ajcn.2010.29191. [DOI] [PubMed] [Google Scholar]
- 133.Zhou SJ, Gibson RA, Crowther CA, Baghurst P, Makrides M. Effect of iron supplementation during pregnancy on the intelligence quotient and behavior of children at 4 y of age: long-term follow-up of a randomized controlled trial. Am J Clin Nutr. 2006;3:1112–7. doi: 10.1093/ajcn/83.5.1112. [DOI] [PubMed] [Google Scholar]
- 134.Christian P, et al. Prenatal micronutrient supplementation and intellectual and motor function in early school-aged children in Nepal. JAMA. 2010;4:2716–23. doi: 10.1001/jama.2010.1861. [DOI] [PubMed] [Google Scholar]
- 135.Caulfield LE, et al. Maternal gestational zinc supplementation does not influence multiple aspects of child development at 54 mo of age in Peru. Am J Clin Nutr. 2010;2:130–6. doi: 10.3945/ajcn.2010.29407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hamadani JD, Fuchs GJ, Osendarp SJ, Huda SN, Grantham-McGregor SM. Zinc supplementation during pregnancy and effects on mental development and behaviour of infants: a follow-up study. Lancet. 2002:290–4. doi: 10.1016/S0140-6736(02)09551-X. 0. [DOI] [PubMed] [Google Scholar]
- 137.Tofail F, et al. Effects of prenatal food and micronutrient supplementation on infant development: a randomized trial from the Maternal and Infant Nutrition Interventions, Matlab (MINIMat) study. Am J Clin Nutr. 2008;7:704–11. doi: 10.1093/ajcn/87.3.704. [DOI] [PubMed] [Google Scholar]
- 138.Li Q, et al. Effects of maternal multimicronutrient supplementation on the mental development of infants in rural western China: follow-up evaluation of a double-blind, randomized, controlled trial. Pediatrics. 2009;3:e685–92. doi: 10.1542/peds.2008-3007. [DOI] [PubMed] [Google Scholar]
- 139.Prado EL, et al. Maternal multiple micronutrient supplements and child cognition: a randomized trial in Indonesia. Pediatrics. 2012:e536–46. doi: 10.1542/peds.2012-0412. 0. [DOI] [PubMed] [Google Scholar]
- 140.McGrath N, et al. Effect of maternal multivitamin supplementation on the mental and psychomotor development of children who are born to HIV-1-infected mothers in Tanzania. Pediatrics. 2006;7:e216–25. doi: 10.1542/peds.2004-1668. [DOI] [PubMed] [Google Scholar]
- 141.Darnton-Hill I, Mkparu UC. Micronutrients in pregnancy in low- and middle-income countries. Nutrients. 2015;7:1744–68. doi: 10.3390/nu7031744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.WHO . Guideline: Intermittent iron and folic acid supplementation in menstruating women. World Health Organization; Geneva: 2011. [PubMed] [Google Scholar]
- 143.Andersson M, de Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007:1606–11. doi: 10.1017/S1368980007361004. 0. [DOI] [PubMed] [Google Scholar]
- 144.WHO . Guideline: Vitamin A supplementation in pregnant women. World Health Organization; Geneva: 2011. [PubMed] [Google Scholar]
- 145.Sununtnasuk C, D'Agostino A, Fiedler JL. Iron+folic acid distribution and consumption through antenatal care: identifying barriers across countries. Public Health Nutr. 2015:1–11. doi: 10.1017/S1368980015001652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Koletzko B, et al. German national consensus recommendations on nutrition and lifestyle in pregnancy by the 'Healthy Start - Young Family Network'. Ann Nutr Metab. 2013;3:311–22. doi: 10.1159/000358398. [DOI] [PubMed] [Google Scholar]
- 147.Christian P. In: Handbook of Nutrition and Pregnancy. Lammi-Keefe CJ, Couch S, Philipson E, editors. Humana Press; New Jersey, USA: 2008. [Google Scholar]
- 148.CDC Grand Rounds: additional opportunities to prevent neural tube defects with folic acid fortification. MMWR Morb Mortal Wkly Rep. 2010;9:980–4. [PubMed] [Google Scholar]
- 149.Sultan S, Anjum FM, Butt MS, Huma N, Suleria HA. Concept of double salt fortification; a tool to curtail micronutrient deficiencies and improve human health status. J Sci Food Agric. 2014;4:2830–8. doi: 10.1002/jsfa.6634. [DOI] [PubMed] [Google Scholar]
- 150.Martorell R, et al. Effectiveness evaluation of the food fortification program of Costa Rica: impact on anemia prevalence and hemoglobin concentrations in women and children. Am J Clin Nutr. 2015;1:210–7. doi: 10.3945/ajcn.114.097709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Velu G, Ortiz-Monasterio I, Cakmak I, Hao Y, Singh RP. Biofortification strategies to increase grain zinc and iron concentrations in wheat. Journal of Cereal Science. 2014;9:365–372. [Google Scholar]
- 152.Das JK, Salam RA, Kumar R, Bhutta ZA. Micronutrient fortification of food and its impact on woman and child health: a systematic review. Syst Rev. 2013;2:67. doi: 10.1186/2046-4053-2-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.IOM . Dietary reference intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. The National Academies Press; Washington, DC: 1998. [PubMed] [Google Scholar]
- 154.IOM . Dietary Reference Intakes for Calcium and Vitamin D. The National Academies Press; Washington, DC: 2011. [PubMed] [Google Scholar]
- 155.IOM . Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. The National Academies Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- 156.Faupel-Badger JM, Hsieh CC, Troisi R, Lagiou P, Potischman N. Plasma volume expansion in pregnancy: implications for biomarkers in population studies. Cancer Epidemiol Biomarkers Prev. 2007;6:1720–3. doi: 10.1158/1055-9965.EPI-07-0311. [DOI] [PubMed] [Google Scholar]
- 157.McCauley ME, van den Broek N, Dou L, Othman M. Vitamin A supplementation during pregnancy for maternal and newborn outcomes. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD008666.pub3. 0, CD008666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Salam RA, Zuberi NF, Bhutta ZA. Pyridoxine (vitamin B6) supplementation during pregnancy or labour for maternal and neonatal outcomes. Cochrane Database Syst Rev. 2015;6 doi: 10.1002/14651858.CD000179.pub3. CD000179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Rumbold A, Ota E, Nagata C, Shahrook S, Crowther CA. Vitamin C supplementation in pregnancy. Cochrane Database Syst Rev. 2015;9 doi: 10.1002/14651858.CD004072.pub3. CD004072. [DOI] [PMC free article] [PubMed] [Google Scholar]


