Abstract
Background and Purpose
At age 45, Blacks have a stroke mortality approximately 3-times greater than their White counterparts, with a declining disparity at older ages. We assess whether this Black-White disparity in stroke mortality is attributable to a Black-White disparity in stroke incidence versus a disparity in case-fatality.
Methods
We first assess if Black-White differences in stroke mortality within 29,681 participants in the REasons for Geographic And Racial Differences in Stroke (REGARDS) cohort reflect national Black-White differences in stroke mortality, and then assess the degree to which Black-White differences in stroke incidence or 30-day case-fatality after stroke contribute to the disparities in stroke mortality.
Results
The pattern of stroke mortality within the study mirrors the national pattern, with the Black-to-White hazard ratio of approximately 4.0 at age 45 decreasing to approximately 1.0 at age 85. The pattern of Black-to-White disparities in stroke incidence shows a similar pattern, but no evidence of a corresponding disparity in stroke case-fatality.
Discussion
These findings show that the Black-White differences in stroke mortality are largely driven by differences in stroke incidence, with case fatality playing at most a minor role. Therefore to reduce the Black-White disparity in stroke mortality, interventions need to focus on prevention of stroke in Blacks.
Keywords: Stroke, race, Black, mortality, incidence, case fatality, longitudinal cohort study
Introduction
An excess stroke mortality among Blacks was documented as long ago as 1949 to 1951, with the Black-to-White mortality ratios over 3-times greater between the ages of 45–54, and a declining Black-to-White mortality ratio at older ages.1 These differences persist, where Figure 1 shows the age-specific Black-to-White stroke mortality ratio for the non-Hispanic US population between 2003 and 2007 (recruitment period for REGARDS).2
Figure 1.
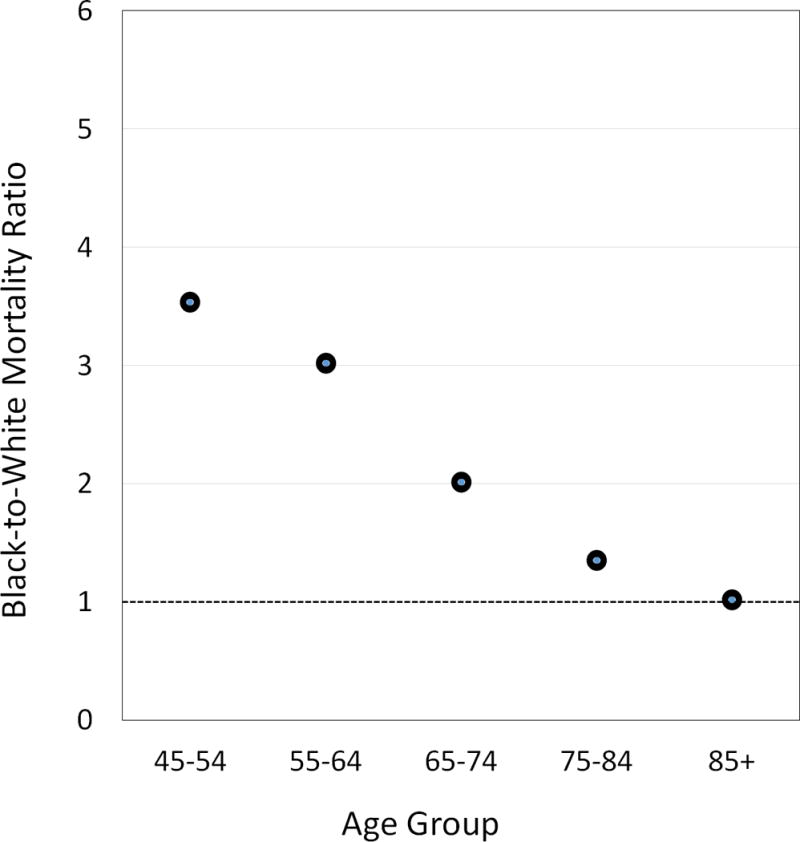
Age-specific (for age 45 and over) Black-to-White mortality ratio for deaths from cerebrovascular diseases (ICD-10: 160 – 169) in the United States for years 2003 to 2007 (inclusive). Note that both the number of people dying of stroke, and the number of people in the population, are from a census (Census of the population and U.S. Vital Statistics) and include all people in the US. As such, there is no sampling variation of the estimated age-specific mortality rates underlying the mortality ratio, and hence no sampling variation (and hence no confidence bounds) on the mortality ratios.
There are numerous factors contributing to the temporal decline in stroke mortality including prevention and improved control of stroke risk factors including hypertension and diabetes, smoking cessation programs, and advances in post-stroke care such as telemedicine and health system designs to enhance stroke care.3 However, improvements in these factors appear to benefit both the White and Black population and hence may not have contributed to changes in the magnitude of the Black-to-White disparity for stroke mortality (in fact, the disparity appears to be increasing4). In order to reduce the Black-White disparity in stroke, we need to understand what factors contribute to the higher mortality in Blacks and target interventions at these factors.
Disease-specific mortality is a product of the incidence rate (number of people developing the disease) and the case fatality (proportion of those developing the disease that die). Understanding whether higher stroke mortality in Blacks is attributable to a higher incidence or case fatality is central to the effort to target interventions to reduce the disparity. Specifically, if higher incidence is the primary contributor, then efforts to reduce the disparity must focus on primary prevention of stroke in the Black population. Conversely, if case fatality in Blacks is the primary contributor, then the reduction of the Black-White disparity must focus on efforts to reduce disparities in care of stroke patients.
Remarkably few studies have examined whether higher stroke incidence versus high case fatality in Blacks are the primary contributor to the higher stroke mortality in Blacks. The Greater Cincinnati/Northern Kentucky Stroke Study (GCNKSS) used stroke surveillance approaches, showed an age-specific pattern of Black-White differences in stroke incidence in 1999 in the Cincinnati region that is quite similar to the national age-specific pattern for Black-White differences in mortality, with stroke mortality 2.6 times greater in Blacks than Whites at age 45–54, but monotonically decreasing to 0.8 times for ages 85+.5 The GCNKSS also showed stroke case-fatality was 24% lower in Blacks than Whites. Likewise, data from the National Hospital Discharge Survey showed consistently higher discharge rates for stroke per 1,000 population for Blacks than Whites, but generally lower in-hospital mortality following stroke for Blacks than Whites.6 The pattern of a declining Black-White disparity in stroke incidence has been previously confirmed in the REGARDS cohort;7 however, case fatality data has not been reported from REGARDS. Collectively, these data suggest that the key to reducing the Black disparity in stroke mortality is through risk factor prevention or improved risk factor control to prevent strokes in Blacks, rather than improved care of Blacks once stroke has occurred. The goal of the current report is to confirm the findings in a national cohort of Black and White participants.
Methods
The REGARDS Study is a longitudinal cohort study of 30,239 Black and White participants aged 45+ years. The cohort was recruited from the 48 contiguous states in the United States between 2003 and 2007 through a combination of mail and telephone contacts. An interview assessing the risk profile was conducted by telephone, and an in-home visit was subsequently performed for assessment of blood pressure, height, waist circumference, weight and biological specimen collection. The cohort has been followed at 6-month intervals by telephone for surveillance of potential strokes, with medical records for suspected stroke events retrieved and adjudicated by a physician panel. Details of the study are available elsewhere.8 All participants provided written informed consent, and the study methods were approved by institutional review boards at all participating entities.
The excess stroke mortality in Blacks has been documented in the Vital Statistics Systems from the NCHS, with mortality approximately 3-times higher in Blacks than Whites at age 45, but a declining disparity at older ages.4 The first goal of this paper was to validate data from the REGARDS study by confirming whether the Black-White pattern of stroke deaths in REGARDS reflects these national data. “Incident fatal stroke” was defined as a death within 30-days of a physician-adjudicated stroke event, and as such represents the product of both incidence and case fatality. Because the disparity in NCHS mortality includes both initial and recurrent stroke, we included risk of incident fatal strokes among participants stroke-free at baseline and those self-reporting previous stroke at baseline. The potential of a Black-White disparity in fatal stroke was assessed using proportional hazards analysis, with factors for race, age, race-by-age interaction, and sex.
We then investigated whether the (potential) disparity in fatal strokes was attributable to:
Black-White disparities in stroke incidence (either fatal or non-fatal) during follow-up using an analytic approach identical to that described above for incident fatal stroke.
The Black-White difference in case fatality was assessed in analysis restricted to those participants with a documented stroke during follow-up. Case fatality was defined by the proportion of these participants dying within 30 days of an adjudicated stroke event. The Black-White difference in case fatality was assessed using logistic regression, with terms for race, age, race-by-age interaction, and sex.
The potential age-by-race interaction was tested in all models with an a priori α = 0.10, with a plan to remove the interaction term should it be non-significant.
Results
Of the 30,239 REGARDS participants, follow-up was available on 29,682 (98%). A description of the study population is provided in Table 1. The White participants were slightly older, more likely to be male, less likely to have low income or education, and generally fewer stroke risk factors. During an average follow-up of 6.8 ± 2.7 years, there were 1,168 strokes of which 242 were fatal.
Table 1.
Description of the study population by race
| Black | White | |
|---|---|---|
| N | 12,212 | 17,470 |
| Age (mean ± SD) | 64 ± 9 | 65 ± 9 |
| Male (%) | 38 | 50 |
| Income < $35K (%) | 61 | 39 |
| High school or less (%) | 48 | 32 |
| Previous stroke (%) | 8 | 5 |
| Hypertension (%) | 71 | 51 |
| Diabetes (%) | 31 | 16 |
| Current smoking (%) | 17 | 13 |
| Atrial fibrillation (%) | 8 | 10 |
| Left ventricular hypertrophy (%) | 15 | 06 |
| Heart disease (%) | 16 | 20 |
Analysis of Time to Incident Fatal Stroke
The interaction between race and age was significant (p = 0.0042), and as such the Black-White differences in the time to fatal stroke are described by age.
When age is categorized in decades, there is a monotonically decreasing Black-to-White stroke mortality ratio by age (see Figure 2A). There were only 5 fatal strokes in the youngest age stratum (4 in Black and 1 in White participants) resulting in a very wide confidence interval. For the older age strata, the Black-to-White mortality ratio approaches 1.0 (and is non-significantly lower than 1.0 for ages 85+).
Figure 2.
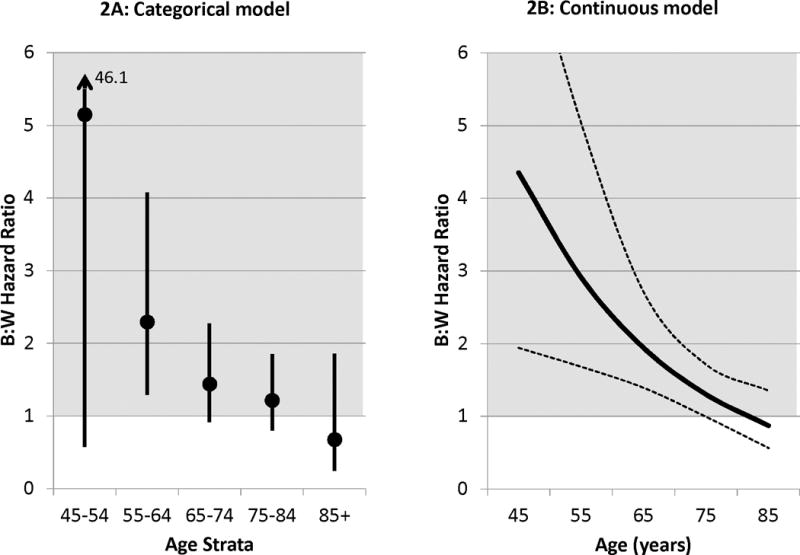
A and B: Black-to-White hazard ratio (with 95% confidence limits) for fatal stroke (mortality analysis) after adjustment for sex. Figure 1A provides the hazard ratio from a model with age as a categorical variable, while 1B from a model with age as a continuous variable.
The monotonically decreasing Black-to-White mortality ratios by decade supports the analysis with age as a continuous variable (Figure 2B), where the Black-to-White mortality ratio decreases from approximately 4.0 at age 45, down to 1.0 at age 85. This pattern generally reflects the Black-to-White mortality ratio from Vital Statistics.
Analysis of Time to Incident Stroke (Fatal or Non-Fatal)
For the time to any stroke, the interaction between race and age was significant (p = 0.0003), and as such the Black-White differences in the time to any stroke is described by age. Figure 3A shows the Black-to-White stroke incidence ratio with age categorized by decade, showing a monotonically decreasing Black-to-White ratio that is approximately 3.0 at age 45–54, but decreases to approximately 1.0 by age 75–84. This monotonically decreasing Black-to-White incidence ratio supports the analysis of the incidence ratio with age as a continuous variable (Figure 3B), where the Black-to-White incidence ratio decreases from approximately 2.5 at age 45, down to 1.0 at age 85. This pattern generally reflects the Black-to-White mortality ratio from Vital Statistics.
Figure 3.
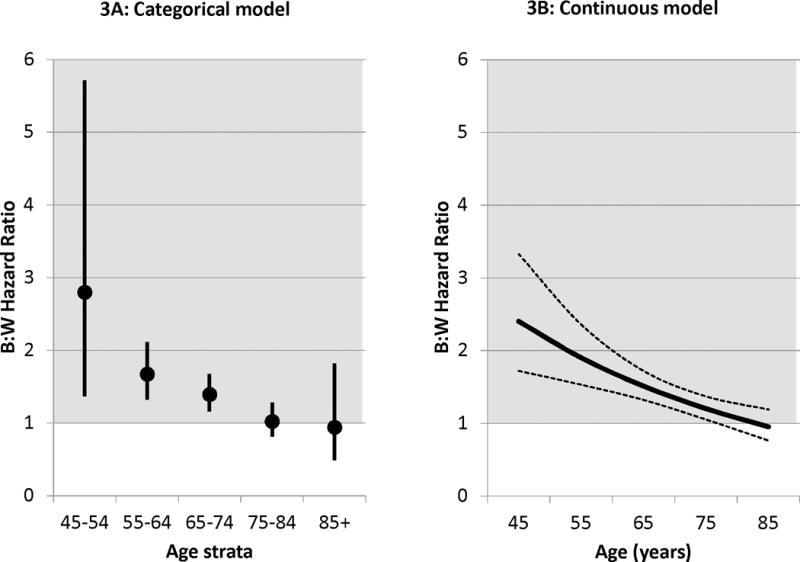
A and B: Black-to-White hazard ratio (with 95% confidence limits) for any stroke (incidence analysis) after adjustment for sex. Figure 2A provides the hazard ratio from a model with age as a categorical variable, while 2B from a model with age as a continuous variable.
Analysis of Case-Fatality
The age-specific number of fatal strokes and total strokes, with gender-adjusted Black-to-White odds ratio is shown in Table 2. There was no evidence of any two-way interactions between age, race and sex (p > 0.10), and as such only main effects were assessed. In multivariable analysis, the odds of a stroke being fatal increased by 61% with each decade (OR = 1.61; 95% CI: 1.35 – 1.91); but there was no evidence that either race (OR = 1.20; 95% CI: 0.89 – 1.62) or sex (OR = 1.02; 95% CI: 0.76 – 1.36) was associated with case fatality.
Table 2.
Number of deaths and number of stroke events (with percentage) for Black and White participants by age strata, and the gender-adjusted odds ratio (with 95% confidence interval)
| 45–54 | 55–64 | 65–74 | 75–84 | 85+ | |
| Black | 4/24 (16.7%) |
29/151 (19.2%) |
35/214 (16.4%) |
35/113 (31.0%) |
5/13 (38.5%) |
| White | 1/11 (9.1%) |
19/134 (14.2%) |
40/255 (15.7%) |
58/225 (25.8%) |
15/28 (53.6%) |
| Gender adjusted Black-White Odds Ratio (95% CI) |
1.99 (0.20 – 20.28) |
1.44 (0.76 – 2.71) |
1.05 (0.64 – 1.73) |
1.29 (0.78 – 2.13) |
0.54 (0.14 – 2.07) |
Discussion
These data support the previous findings that the increased stroke mortality among middle-aged (45 to 65 years) Blacks is attributable to Black-White differences in stroke incidence, and that Black-White differences in case-fatality is at most a minor contributor.5, 7 The finding that case-fatality is lower in Blacks than Whites is supported by recent reports from Get With The Guidelines hospitals, where after adjustment for patient and hospital characteristics, the odds of in-hospital death in Blacks was 0.90 (95% CI: 0.85 – 0.95) fold that of Whites.9 Hence, reducing the Black-to-White disparity in stroke mortality will require further understanding of and interventions to reduce the higher incidence of stroke in Blacks. While it is appropriate to work to reduce the disparities in stroke care,10 this will be unlikely to substantially reduce the disparity in stroke mortality. The key will be interventions focused on approaches to risk factor prevention and management, with primary care physicians and public health programs playing a key role.
The REGARDS study has already provided some insights to the Black-White disparity in stroke incidence, but much work remains. Previous reports from REGARDS have shown that approximately 40% of the Black-White incidence disparity between the ages of 45 to 65 can be attributed to prevalence of “traditional” risk factors (defined by the Framingham Stroke Risk Function11), particularly treated hypertension and prevalent diabetes, both of which are substantially higher in the Black population than in the White population.12 Eliminating the disparity in stroke risk factors will be challenging; however, failure implies the continued persistence of the disparity not only in risk factors, but also in stroke incidence and mortality.
While the prevalence in stroke risk factors accounts for approximately 40% of the disparity in stroke incidence, we have previously suggested12 that the remaining 60% of the disparity could be associated with:
Awareness, treatment and control of risk factors. Data from both NHANES and REGARDS have shown that while awareness and treatment for hypertension is higher in the Black population than in Whites, the likelihood of adequate control is much lower.13, 14 Hence, hypertension is a “triple threat” as a contributor to the Black-White disparity in stroke incidence as it has a higher prevalence, is less likely to be controlled, and the harm of lack of control has more potent impact. It has been suggested that the disparities in hypertension control may be attributable to differences in social conditions.15 In contrast, for dyslipidemia, Blacks are less likely to be aware, less likely to be treated, and less likely to be controlled.16–18 Likewise, Blacks have poorer control of diabetes19 and are less likely to be aware of or treated for atrial fibrillation.20 Interventions targeted to address prevention and control of risk factors in the stroke-free population are needed.
Risk factors having a differential impact by race, with a more potent effect in the Black population. For example, we have previously shown that the impact of high blood pressure is larger in the Black than White population, where after multivariable adjustment for other risk factors a 10 mmHg higher blood pressure is associated with an 8% increase risk of stroke in Whites, but a 24% increase risk in Blacks.21 This apparent differential susceptibility could be playing a major role, as there were no disparities in stroke incidence in subjects with well-controlled (< 120 mmHg) systolic blood pressure.
Disparities in non-traditional risk factors. Beyond the Framingham stroke risk factors, there are a plethora of risk factors that are both shown to be related to stroke and where Blacks have a disadvantage in the prevalence or severity.22, 23 Among the risk factors declared as “well-documented” in the primary prevention guidelines, Blacks suffer a disadvantage in prevalence or severity for physical inactivity,24, 25 diet,26 and obesity.27 In addition there are numerous less-well documented risk factors, such as psychosocial factors including depressive symptoms, anger, hostility and discrimination that are likely related to stroke, for which Blacks are at a disadvantage for prevalence or severity.28 Blacks are also at a disadvantage for environmental and neighborhood exposures that are related to stroke risk, including an alarmingly disproportionate number living in poverty, one of the strongest risk factors for stroke as well as other CVD outcomes.29, 30 Much work remains to continue to document non-traditional risk factors that are related to stroke where Blacks are at a disadvantage for prevalence or severity of the risk factor, so that interventions and policies can address them.
Measurement error and residual confounding: All regression models (including both the proportional hazards and logistic models employed here) assume that the predictor variables are measured with precision. For the predictor variables in this analysis (age, race and sex), it is reasonably safe to assume that this is not a major issue. However, in other analyses such as those described above, for example, where we are estimating the proportion of Black excess risk attributable to the traditional risk factors, this could be a greater concern and lead to an underestimation of the proportion of the excess explained.
Despite the dramatic decline in stroke deaths for both Blacks and Whites, the Black-White disparity in stroke mortality persists (or may be growing).4 While some inroads have been made to understand the contributors to the higher risk of stroke incidence in Blacks, there is much work remaining. The challenge for REGARDS and other epidemiological cohorts is to intensify the focus of investigations to identify the contributors, so that clinical trials can be developed to test the targeting of interventions to reduce this Black-White stroke mortality disparity.
On the surface, it would appear that disparities in secondary stroke prevention could also play a role. Of the estimated 795,000 stroke events in the US, about 185,000 (23%) are recurrent events.31 While much less is known about the role of risk factors and the Black-White disparities for secondary stroke events,32 data from REGARDS have shown no Black-White differences in the risk of recurrent stroke,33 and as such it is relatively unlikely that secondary stroke prevention is a pathway to reducing the Black-White disparity in stroke mortality.
It is clear that there are substantial Black-White differences in care following stroke,34 and we explicitly do not want to minimize the importance of addressing disparities in stroke care. However, case-fatality following stroke did not differ between Blacks and Whites in either this REGARDS analysis or the previous GCNKSS, suggesting that these disparities in care are unlikely to be contributors to the disparities in stroke mortality. This is not to say that it is unimportant to reduce documented Black-White disparities in care, where after adjustment for patient and hospital characteristics, Black stroke patients were less likely than Whites to receive IV tPA, be discharged on antithrombotics, be provided the use of anticoagulation for atrial fibrillation, to have low density lipoproteins treated to 100 mg/dL, and to receive smoking cessation counselling;9 it is only that these disparities do not appear to be major contributors to the Black-White disparity in stroke mortality. In addition, the distinction between pre- and post-stroke is not always crisp, and many of our study participants could have some level of cerebrovascular disease that could affect memory and functional assessment prior to an acute stroke event.
Conclusion
The substantial Black-White differences in stroke mortality between the ages of 45 to 65 are largely driven by Black-White disparities in stroke incidence. This observation should bring attention to the need to focus efforts to reduce the Black-White disparity on contributors to higher stroke incidence in Blacks. A substantial proportion of the excess risk of incident stroke in Blacks is attributable to a higher prevalence of traditional risk factors in Blacks, and we need to “go further upstream” to make inroads to reduce this pathway (i.e., why do Blacks have a higher prevalence of hypertension and diabetes). However, there are many other pathways, including differential susceptibility to risk factors, disparities in the control and treatment of risk factors, socioeconomic inequities, and novel or emerging risk factors, where Blacks have a disadvantage. We are at the early phase of processes to better understand these alternative pathways that potentially contribute to the Black-White disparity in stroke incidence, and we need to redouble our efforts to the investigations of these pathways.
Acknowledgments
The authors thank the investigators, staff, and participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Sources of Funding
This research project was supported by cooperative agreement U01-NS041588 from the National Institute of Neurological Disorders and Stroke, NIH.
Footnotes
Disclosures
The authors report no disclosures
References
- 1.Wylie CM. Recent trends in mortality from cerebrovascular accidents in the united states. J Chronic Dis. 1960;14:213–220. doi: 10.1016/0021-9681(61)90154-0. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention, National Center for Health Statistics. (Data are from the Compressed Mortality File 1999–2014 Series 20 No. 2T, 2015, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program).Compressed Mortality File 1999–2014 on CDC WONDER Online Database, released December 2015. Accessed at http://wonder.cdc.gov/cmf-icd10.html on Jan 10, 2016 4:41:08 PM.
- 3.Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, et al. Factors influencing the decline in stroke mortality: A statement from the American Heart Association/American Stroke Association. Stroke. 2014;45:315–353. doi: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howard G. Ancel keys lecture: Adventures (and misadventures) in understanding (and reducing) disparities in stroke mortality. Stroke. 2013;44:3254–3259. doi: 10.1161/STROKEAHA.113.002113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kleindorfer D, Broderick J, Khoury J, Flaherty M, Woo D, Alwell K, et al. The unchanging incidence and case-fatality of stroke in the 1990s: A population-based study. Stroke. 2006;37:2473–2478. doi: 10.1161/01.STR.0000242766.65550.92. [DOI] [PubMed] [Google Scholar]
- 6.Kennedy BS, Kasl SV, Brass LM, Vaccarino V. Trends in hospitalized stroke for blacks and whites in the United States, 1980–1999. Neuroepidemiology. 2002;21:131–141. doi: 10.1159/000054810. [DOI] [PubMed] [Google Scholar]
- 7.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69:619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The REasons for Geographic And Racial Differences in Stroke Study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 9.Schwamm LH, Reeves MJ, Pan W, Smith EE, Frankel MR, Olson D, et al. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010;121:1492–1501. doi: 10.1161/CIRCULATIONAHA.109.881490. [DOI] [PubMed] [Google Scholar]
- 10.Johnston SC, Fung LH, Gillum LA, Smith WS, Brass LM, Lichtman JH, et al. Utilization of intravenous tissue-type plasminogen activator for ischemic stroke at academic medical centers: The influence of ethnicity. Stroke. 2001;32:1061–1068. doi: 10.1161/01.str.32.5.1061. [DOI] [PubMed] [Google Scholar]
- 11.Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: A risk profile from the Framingham Study. Stroke. 1991;22:312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 12.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: Lessons from the half-full (empty?) glass. Stroke. 2011;42:3369–3375. doi: 10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 14.Howard G, Prineas R, Moy C, Cushman M, Kellum M, Temple E, et al. Racial and geographic differences in awareness, treatment, and control of hypertension: The REasons for Geographic And Racial Differences in Stroke Study. Stroke. 2006;37:1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 15.Thorpe RJ, Jr, Bowie JV, Smolen JR, Bell CN, Jenkins ML, Jr, Jackson J, et al. Racial disparities in hypertension awareness and management: Are there differences among African Americans and whites living under similar social conditions? Ethn Dis. 2014;24:269–275. [PMC free article] [PubMed] [Google Scholar]
- 16.Zweifler RM, McClure LA, Howard VJ, Cushman M, Hovater MK, Safford MM, et al. Racial and geographic differences in prevalence, awareness, treatment and control of dyslipidemia: The REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. Neuroepidemiology. 2011;37:39–44. doi: 10.1159/000328258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hyre AD, Muntner P, Menke A, Raggi P, He J. Trends in atp-iii-defined high blood cholesterol prevalence, awareness, treatment and control among U.S. Adults. Ann Epidemiol. 2007;17:548–555. doi: 10.1016/j.annepidem.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 18.Safford MM, Gamboa CM, Durant RW, Brown TM, Glasser SP, Shikany JM, et al. Race-sex differences in the management of hyperlipidemia: The REasons for Geographic and Racial Differences in Stroke Study. Am J Prev Med. 2015;48:520–527. doi: 10.1016/j.amepre.2014.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Egan BM, Li J, Wolfman TE, Sinopoli A. Diabetes and age-related demographic differences in risk factor control. J Am Soc Hypertens. 2014;8:394–404. doi: 10.1016/j.jash.2014.03.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meschia JF, Merrill P, Soliman EZ, Howard VJ, Barrett KM, Zakai NA, et al. Racial disparities in awareness and treatment of atrial fibrillation: The REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. Stroke. 2010;41:581–587. doi: 10.1161/STROKEAHA.109.573907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med. 2013;173:46–51. doi: 10.1001/2013.jamainternmed.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bang OY, Ovbiagele B, Kim JS. Nontraditional risk factors for ischemic stroke: An update. Stroke. 2015;46:3571–3578. doi: 10.1161/STROKEAHA.115.010954. [DOI] [PubMed] [Google Scholar]
- 23.Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:3754–3832. doi: 10.1161/STR.0000000000000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clark DO. Racial and educational differences in physical activity among older adults. Gerontologist. 1995;35:472–480. doi: 10.1093/geront/35.4.472. [DOI] [PubMed] [Google Scholar]
- 25.Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: Results from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Prev Med. 2000;18:46–53. doi: 10.1016/s0749-3797(99)00105-1. [DOI] [PubMed] [Google Scholar]
- 26.Judd SE, Gutierrez OM, Newby PK, Howard G, Howard VJ, Locher JL, et al. Dietary patterns are associated with incident stroke and contribute to excess risk of stroke in black Americans. Stroke. 2013;44:3305–3311. doi: 10.1161/STROKEAHA.113.002636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Differences in prevalence of obesity among black, white, and Hispanic adults - United States, 2006–2008. MMWR Morb Mortal Wkly Rep. 2009;58:740–744. [PubMed] [Google Scholar]
- 28.Everson-Rose SA, Roetker NS, Lutsey PL, Kershaw KN, Longstreth WT, Jr, Sacco RL, et al. Chronic stress, depressive symptoms, anger, hostility, and risk of stroke and transient ischemic attack in the Multi-Ethnic Study of Atherosclerosis. Stroke. 2014;45:2318–2323. doi: 10.1161/STROKEAHA.114.004815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown AF, Liang LJ, Vassar SD, Stein-Merkin S, Longstreth WT, Jr, Ovbiagele B, et al. Neighborhood disadvantage and ischemic stroke: The Cardiovascular Health Study (CHS) Stroke. 2011;42:3363–3368. doi: 10.1161/STROKEAHA.111.622134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M, et al. Air pollution and cardiovascular disease: A statement for healthcare professionals from the expert panel on population and prevention science of the American Heart Association. Circulation. 2004;109:2655–2671. doi: 10.1161/01.CIR.0000128587.30041.C8. [DOI] [PubMed] [Google Scholar]
- 31.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics–2015 update: A report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 32.Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:227–276. doi: 10.1161/STR.0b013e3181f7d043. [DOI] [PubMed] [Google Scholar]
- 33.Howard G, Kissela BM, Kleindorfer DO, McClure LA, Soliman EZ, Judd SE, et al. Differences in risk factors for first versus recurrent stroke: The REasons for Geographic And Racial Differneces in Stroke (REGARDS) Study. Neurology. 2016;86:637–642. doi: 10.1212/WNL.0000000000002376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, et al. Racial-ethnic disparities in stroke care: The American experience: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2091–2116. doi: 10.1161/STR.0b013e3182213e24. [DOI] [PubMed] [Google Scholar]


