Abstract
Objectives
Ebola and Marburg viruses (EBOVs and MARVs, respectively) are causative agents of severe hemorrhagic fever with high mortality rates in humans and nonhuman primates. In 2014, there was a major Ebola outbreak in various countries in West Africa, including Guinea, Liberia, Republic of Sierra Leone, and Nigeria. EBOV and MARV are clinically difficult to diagnose and distinguish from other African epidemic diseases. Therefore, in this study, we aimed to develop a method for rapid identification of the virus to prevent the spread of infection.
Methods
We established a conventional one-step reverse transcription-polymerase chain reaction (RT-PCR) assay for these pathogens based on the Superscript Reverse Transcriptase-Platinum Taq polymerase enzyme mixture. All assays were thoroughly optimized using in vitro-transcribed RNA.
Results
We designed seven primer sets of nucleocapsid protein (NP) genes based on sequences from seven filoviruses, including five EBOVs and two MARVs. To evaluate the sensitivity of the RT-PCR assay for each filovirus, 10-fold serial dilutions of synthetic viral RNA transcripts of EBOV or MARV NP genes were used to assess detection limits of viral RNA copies. The potential for these primers to cross react with other filoviruses was also examined. The results showed that the primers were specific for individual genotype detection in the examined filoviruses.
Conclusion
The assay established in this study may facilitate rapid, reliable laboratory diagnosis in suspected cases of Ebola and Marburg hemorrhagic fevers.
Keywords: Ebola, Filoviridae, Marburg, reverse transcription-polymerase chain reaction
1. Introduction
Filoviruses are RNA viruses that belong to the family Filoviridae, which includes zoonotic pathogens of Ebola viruses (EBOVs), Marburg viruses (MARVs), and Cuevaviruses. EBOVs and MARVs cause Ebola and Marburg hemorrhagic fevers, respectively [1]. These viruses cause severe and often fatal hemorrhagic fever, with case fatality rates ranging from 25% to 90% depending on the strain or species.
Currently, EBOVs are subdivided into five species with different pathogenicities [2]. Zaire EBOV (ZEBOV), the most lethal species (case fatality rate of up to 90%), has caused numerous human outbreaks between 1976 and 2008 in the Democratic Republic of the Congo, Republic of the Congo, and Gabon 3, 4. Sudan EBOV (SEBOV; case fatality rate of approx. 50%) has caused three documented outbreaks in Sudan and one in Uganda 5, 6. Taï Forest EBOV (TEBOV; previously known as Côte d'Ivoire Ebola virus) has been linked to a single, nonfatal human case [7], and the newly discovered Bundibugyo EBOV (BEBOV) caused an outbreak with a 25% case fatality rate in 2007 in Uganda [8]. Reston EBOV (REBOV), which has caused outbreaks in nonhuman primates and swine in the Philippines, appears to be nonpathogenic in humans [9].
MARV consists of one species with two members, namely, Ravn virus (RMARV) and MARV; RMARV includes four strains [MARV-Popp, MARV-Musoke (MMARV), MARV-Ozolin, and MARV-Angola] [10]. MARV has been shown to be responsible for at least nine outbreaks since 1967, with four occurring in the past decade, including a recent outbreak that began in September 2012 in Uganda [11]. The increased frequency of MARV outbreaks together with the fact that these viruses are potential agents of bioterrorism has increased public health concern regarding filoviruses.
A number of diagnostic methods are available for the detection and identification of filoviruses. These methods include virus isolation, enzyme-linked immunosorbent assays for detection of antigen or antibodies, reverse transcription-polymerase chain reaction (RT-PCR), and electron microscopy, all of which have played major roles in the diagnosis of filovirus infections. In particular, RT-PCR targeting viral nucleic acid is a rapid, sensitive technique to detect filoviruses. There are a number of commercial and in-house PCR assays for detection of filoviruses with different targets.
In this study, we developed a one-step RT-PCR method using primers for amplifying a specific RNA sequence by expressing the nucleocapsid protein (NP) of EBOV or MARV. Using this method, the presence of EBOV or MARV genes in the samples may be identified more accurately and detected more rapidly. Moreover, through application of specific primers, this method could be used for specific detection of seven types of filoviruses, including the five known EBOVs and two known MARVs.
2. Materials and methods
2.1. Primers design
Nucleotide sequences of the N-protein-encoding segments of seven known EBOVs and MARVs were aligned using the CLUSTAL W multiple alignment algorithm (MegAlign program, Lasergene sequence analysis software; DNASTAR Inc., Madison, WI, USA) to identify conserved regions. Primers for each segment were designed using Primer Express software (Version 3.0; PE Applied Biosystems, Foster City, CA, USA). The specificity of each primer was checked using the Basic Local Alignment Search Tool search against the National Center for Biotechnology Information database and then appraised using a primer selection program in Lasergene software. The sequences and details of primers are listed in Table 1.
Table 1.
Primers for reverse transcription-polymerase chain reaction used in the study.
| Virus | Primer | Sequence (5′→3′) | Position | Size (bp) |
|---|---|---|---|---|
| BEBOV | Forward | GCAGAAATATGCTGAATCTCGTGAAC | 1062 | 418 |
| Reverse | ATCATCCTCGTCCTCAAGGTCAAAA | 1479 | ||
| REBOV | Forward | CCAACAATATGCTGAGTCCAGAGAA | 1062 | 419 |
| Reverse | CATCCTCATGATCGTCAAGATCG | 1480 | ||
| SEBOV | Forward | ACACGTGAGTTGGACAACCTT | 1078 | 402 |
| Reverse | GTCATCGTCGTCGTCCAAATTGAA | 1479 | ||
| TEBOV | Forward | AATCTCGCGAGCTTGACCAT | 1076 | 404 |
| Reverse | CTCGTCACCATCTTCAAGGTCAAA | 1479 | ||
| ZEBOV | Forward | CGAACTTGACCATCTTGGACTTG | 1083 | 399 |
| Reverse | TCCTCGTCGTCCTCGTCTAGAT | 1481 | ||
| MMARV | Forward | AGGCGACATGAACATCAGGAAATT | 1012 | 398 |
| Reverse | TCGTCCTCATTCAGCAGTGCAAAT | 1409 | ||
| RMARV | Forward | GCGACATGAACACCAGGAAATTC | 1014 | 412 |
| Reverse | ATTTTCAAGAGTATCCTCGTCTTCG | 1425 |
BEBOV = Bundibugyo EBOV; bp = base pair; MARV = Marburg virus; MMARV = MARV-Musoke; REBOV = Reston EBOV; RMARV = Ravn virus; SEBOV = Sudan EBOV; TEBOV = Taï Forest EBOV; ZEBOV = Zaire EBOV.
2.2. Synthesis of RNA transcripts
Seven templates from the MMARV NP gene (2,088 nt), the SEBOV NP gene (2,217 nt), the TEBOV NP gene (2,220 nt), the BEBOV NP gene (2,220 nt), the RMARV NP gene (2,088 nt), the REBOV NP gene (2,220 nt), and the ZEBOV NP gene (2,220 nt) were cloned into pET 28a (Novagen, Madison, WI, USA). The template plasmids were linearized by digestion with the HindIII restriction enzyme. The RNA transcripts were synthesized using an mMESSAGE mMACHINE T7 kit (Ambion, Austin, TX, USA). The residual template DNA after in vitro transcription was removed by TURBO DNase digestion, and the RNA was purified using an RNA purification procedure.
2.3. One-step RT-PCR
Synthesized RNAs were extracted using the TRIzol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer's instructions. The final product was dissolved in 50 μL RNase-free water. The one-step RT-PCR was performed using a DiaStar 2X OneStep RT-PCR premix kit (SolGent, Daejeon, South Korea) with designed primers. The RT-PCR conditions were as follows: an initial step of 30 minutes at 50°C for reverse transcription and 15 minutes at 95°C for denaturation; 35 cycles of 20 seconds at 95°C, 40 seconds at 58°C, and 30 seconds at 72°C; and a final extension step of 5 minutes at 72°C.
3. Results
3.1. Analytical sensitivity and reproducibility
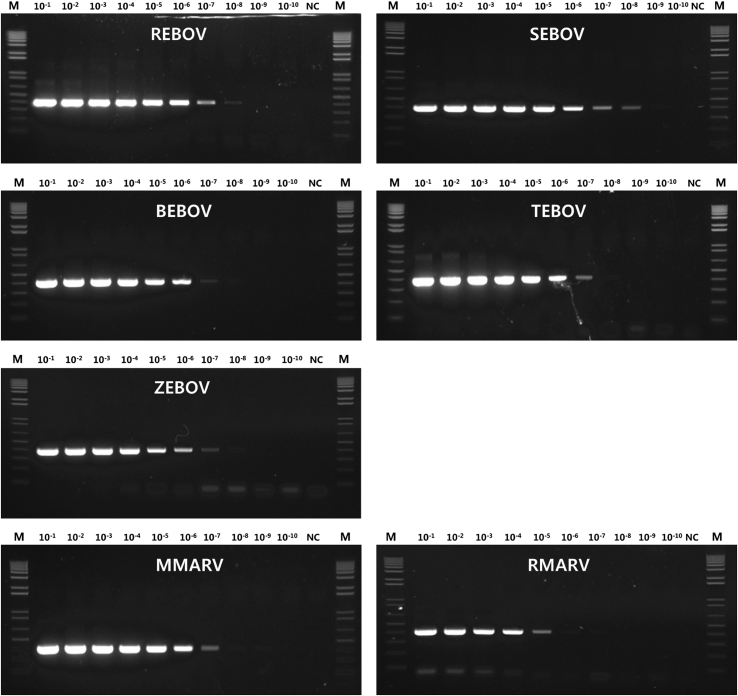
To evaluate the sensitivity of the RT-PCR assay for filovirus (5 EBOVs and 2 MARVs), 10-fold serial dilutions of synthetic viral RNA transcripts of EBOV or MARV NP genes were used to assess detection limits of viral RNA copy or virus infection load. The starting dilution was 50 ng/μL. The detection limits of the RT-PCR assays were 10−7 for BEBOV, TEBOV, and ZEBOV and 10−8 for REBOV and SEBOV. In the case of MARV, the detection limits of MMARV and RMARV were 10−7 and 10−5, respectively (Figure 1). In the RT-PCR assay, with the exception of RMARV, most viral genes were detectable at a 10-million-fold diluted concentration (5 fg/μL). However, the detection limit for RMARV was slightly higher (500 fg/μL). In other words, these RT-PCR assays were able to detect most of the specific targets at a similar dilution. There were no significant differences in detection limits or reproducibility using each of the primer sets.
Figure 1.
Sensitivity of conventional RT-PCR, amplified with specific primers for filoviruses. Determination of the detection limit of filoviral RNAs using RT-PCR and 10-fold serial dilutions of RNA transcripts. Input RNA dilutions are indicated above the lanes. BEBOV = Bundibugyo EBOV; EBOV = Ebola virus; Lane M = 1-kb DNA ladder; Lane NC = negative control; MARV = Marburg virus; MMARV = MARV-Musoke; REBOV = Reston EBOV; RMARV = Ravn virus; RT-PCR = reverse transcription-polymerase chain reaction; SEBOV = Sudan EBOV; TEBOV = Taï Forest EBOV; ZEBOV = Zaire EBOV.
3.2. Analytical specificity
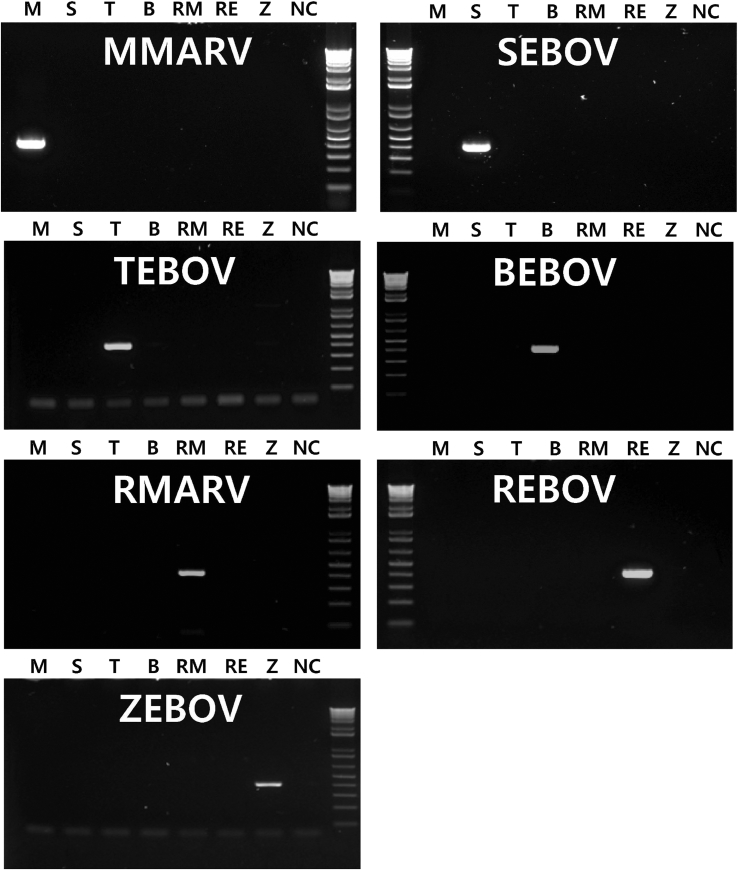
We compared seven primer sets of NP genes based on sequences from seven filovirus strains. To assess the potential for these primer sequences to cross react with other filoviruses, the assays were tested against synthetic RNA transcripts of the BEBOV, TEBOV, ZEBOV, REBOV, SEBOV, MMARV, and RMARV NP genes. For each primer set, no positive results were obtained for other RNA transcripts (Figure 2). As a result, the primer set for each viral NP gene was confirmed to specifically detect only its own viral NP gene.
Figure 2.
Specificity of conventional RT-PCR, amplified with specific primers for filoviruses. BEBOV = Bundibugyo EBOV; EBOV = Ebola virus; Lane B = primers for the Bundibugyo strain; Lane M = primers for the Musoke strain; Lane NC = negative control; Lane RE = primers for the Reston strain; Lane RM = primers for the Ravn strain; Lane S = primers for the Sudan strain; Lane T = primers for the Tai Forest strain; Lane Z = primers for the Zaire strain; MARV = Marburg virus; MMARV = MARV-Musoke; REBOV = Reston EBOV; RMARV = Ravn virus; RT-PCR = reverse transcription-polymerase chain reaction; SEBOV = Sudan EBOV; TEBOV = Taï Forest EBOV; ZEBOV = Zaire EBOV.
4. Discussion
In general, conventional RT-PCR is performed to detect known sequences. However, because this method has high specificity for strains belonging to EBOVs and MARVs, differential detection is possible in unknown samples. In addition, RT-PCR is typically performed at a concentration of 50–100 ng RNA; however, the current method allowed for detection of the viral gene at very low concentrations (5 fg/μL = 4,420 copies). Thus, our current report showed that the virus could be detected using only very small amounts of RNA extracted from the serum. Huang et al [12] reported the detection of NP of ZEBOV and MARV by real-time TaqMan PCR assay. This assay could detect 10,000 copies of viral RNA of ZEBOV or 1,000 copies of viral RNA of MARV. A comparison of our data with those of Huang et al [12] suggests that our gel-based one-step RT-PCR assay has sufficiently high specificity and sensitivity to detect filoviruses. Moreover, the RT-PCR assays designed in this study were suitable for the differential detection of the seven viruses examined herein. These results represent an important advancement in detection of viruses by RT-PCR.
Rapid identification of the virus is required to prevent spread of the infection. Thus, development of more rapid, simple, sensitive, and specific real-time TaqMan PCR assay for the diagnosis of filoviruses is needed. However, the development of filovirus detection methods based on nucleic acid amplification and applicable to clinical samples has been limited. Therefore, it is necessary to study diagnosis of filoviruses with filovirus isolates in Biosafety Level 4 laboratories in the future.
Conflicts of interest
All authors have no conflicts of interest to declare.
Acknowledgments
We thank all employees who worked in the Regional Health Institutes. This study was supported by the National Institute of Health, Korea Centers for Disease Control and Prevention (Grant No. 4840-302-210-13).
References
- 1.Bray M., Murphy F.A. Filovirus research: knowledge expands to meet a growing threat. J Infect Dis. 2007 Nov;196(Suppl. 2):S438–S443. doi: 10.1086/520552. [DOI] [PubMed] [Google Scholar]
- 2.Kuhn J.H., Bào Y., Bavari S. Virus nomenclature below the species level: a standardized nomenclature for filovirus strains and variants rescued from cDNA. Arch Virol. 2014 May;159(5):1229–1237. doi: 10.1007/s00705-013-1877-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Report of a WHO/international study team. Ebola haemorrhagic fever in Zaire, 1976. Bull World Health Organ. 1978;56(2):271–293. [PMC free article] [PubMed] [Google Scholar]
- 4.Grard G., Biek R., Tamfum J.J. Emergence of divergent Zaire Ebola virus strains in Democratic Republic of the Congo in 2007 and 2008. J Infect Dis. 2011 Nov;204(3):S776–S784. doi: 10.1093/infdis/jir364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Albariño C.G., Shoemaker T., Khristova M.L. Genomic analysis of filoviruses associated with four viral hemorrhagic fever outbreaks in Uganda and the Democratic Republic of the Congo in 2012. Virology. 2013 Aug;442(2):97–100. doi: 10.1016/j.virol.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okware S.I., Omaswa F.G., Zaramba S. An outbreak of Ebola in Uganda. Trop Med Int Health. 2002 Dec;7(12):1068–1075. doi: 10.1046/j.1365-3156.2002.00944.x. [DOI] [PubMed] [Google Scholar]
- 7.Le Guenno B., Formenty P., Wyers M. Isolation and partial characterisation of a new strain of Ebola virus. Lancet. 1995 May;345(8960):1271–1274. doi: 10.1016/s0140-6736(95)90925-7. [DOI] [PubMed] [Google Scholar]
- 8.MacNeil A., Farnon E.C., Wamala J. Proportion of deaths and clinical features in Bundibugyo Ebola virus infection, Uganda. Emerg Infect Dis. 2010 Dec;16(12):1969–1972. doi: 10.3201/eid1612.100627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jahrling P.B., Geisbert T.W., Dalgard D.W. Preliminary report: isolation of Ebola virus from monkeys imported to USA. Lancet. 1990 Mar;335(8688):502–505. doi: 10.1016/0140-6736(90)90737-p. [DOI] [PubMed] [Google Scholar]
- 10.Towner J.S., Khristova M.L., Sealy T.K. Marburgvirus genomics and association with a large hemorrhagic fever outbreak in Angola. J Virol. 2006 Jul;80(13):6497–6516. doi: 10.1128/JVI.00069-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rougeron V., Feldmann H., Grard G. Ebola and Marburg haemorrhagic fever. J Clin Virol. 2015 Mar;64:111–119. doi: 10.1016/j.jcv.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang Y., Wei H., Wang Y. Rapid detection of filoviruses by real-time TaqMan polymerase chain reaction assays. Virol Sin. 2012 Oct;27(5):273–277. doi: 10.1007/s12250-012-3252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]