Abstract
Objective
To describe 1) cross-sectional associations between domain-specific physical activity, sitting time and different measures of overweight/obesity and 2) longitudinal associations between patterns of change in physical activity and overweight/obesity ten years later.
Methods
Cross-sectional and longitudinal analyses based on the first and second follow-up of the Swiss cohort study SAPALDIA (SAP) were conducted (SAP2 in 2002/03, SAP3 in 2010/11). Physical activity was assessed by self-report using the long International Physical Activity Questionnaire (IPAQ) and four short questions regarding moderate and vigorous activities. Overweight/obesity were defined based on body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), waist-to-height ratio (WHtR) and percent body fat based on bioelectric impedance analysis (BIA), all measured objectively. Multivariable logistic regression was used for analyses.
Results
Cross-sectionally, leisure-time and vigorous physical activity were inversely associated with all obesity parameters. Most consistent associations were found with BIA percent body fat. There were no associations between work-related and domestic activities and overweight/obesity. Sitting time was positively associated with BIA percent body fat, but not with BMI, WHR and WHtR. Longitudinally, remaining inactive from SAP2 to SAP3 was associated with obesity and BIA percent body fat at SAP3 and with weight increase, becoming inactive with BIA percent body fat and weight increase.
Conclusions
The results support associations between physical activity and overweight/obesity cross-sectionally and longitudinally. Most consistent associations were found for BIA percent body fat. For prevention purposes, the results indicate that physical activity can have an important contribution to weight management.
Keywords: Adults, Bioelectric impedance analysis, Domains of physical activity, Switzerland
Highlights
-
•
Consistent cross-sectional associations were found for percent body fat.
-
•
LTPA was associated with different obesity parameters independent of sitting time.
-
•
Low compared to high sitting was not independently associated with body composition.
-
•
Remaining and becoming inactive were associated with percent body fat and weight increase.
Introduction
Physical activity and sports contribute to between 25% and 50% of total daily energy expenditure (Bouchard et al., 2007) and can thus be important factors for weight control. There is evidence that active individuals have a healthier body mass and composition than inactive individuals (Physical Activity Guidelines Advisory Committee, 2008, Fogelholm and Kukkonen-Harjula, 2000). Total physical activity is usually composed of different aspects such as transport-related, job-related, domestic, and leisure-time physical activity, and there may be different associations between domain of physical activity and overweight/obesity. For example, an inverse relationship has been found for active transport (walking and cycling) and overweight/obesity (Wanner et al., 2012). In addition, there are indications that sedentary behavior represents a risk that is distinct from physical inactivity (Thorp et al., 2011). However, there is not much known about the impact of either different domains of physical activity or of different patterns of physical activity on weight status.
Furthermore, overweight and obesity is mostly defined according to body mass index (BMI), often based on self-reported weight and height, which can be associated with limitations such as (selective) misclassification due to social desirability (Larson, 2000). Moreover, BMI has been criticized as not being an optimal measure of overweight and obesity, especially in terms of disease risks (Lee et al., 2008). Measures of central obesity like waist circumference (WC) (Czernichow et al., 2011), waist-to-hip ratio (WHR) (Czernichow et al., 2011, Petursson et al., 2011) and waist-to-height ratio (WHtR) (Lee et al., 2008) have been shown to be better discriminators for mortality and cardiovascular and metabolic disease phenotypes. However, it is not clear yet whether central fat is more strongly associated with health outcomes than fat located in other regions of the body, or whether central obesity measures are better measures of overall body fat. Furthermore, these measures can also be biased, e.g. depending on the body fat distribution.
Several factors may confound associations between physical activity and body weight. Some of the more obvious ones, such as age, education, smoking, and ethnicity, are often taken into account in analyses. However, not all studies have assessed other potential confounders such as information on dietary intake or self-reported general health status. Finally the role of reverse causality (individuals with higher weight being less likely to be active due to their body weight) is not clear yet. Longitudinal studies are needed to shed light on such associations.
The aims of the present study in a general adult population of Switzerland are: 1) To describe cross-sectional associations of domain-specific and total physical activity as well as sitting time with different objective measures of overweight and obesity: BMI, percent body fat based on bioelectric impedance analysis (BIA), WC, WHR, and WHtR, taking into account several potential confounders including health-related variables such as self-reported general health status, sleep duration, smoking, alcohol consumption and energy intake; 2) To describe longitudinal associations between patterns of change in general physical activity and different measures of overweight and obesity ten years later. The specific contribution of this study are the detailed information on domain-specific physical activity, information on weight status beyond BMI, the adjustment for a number of important potential confounders, and the longitudinal dimension in addition to the cross-sectional analyses.
Methods
Study design, procedures and participants
The present analysis is part of the SAPALDIA cohort study (Swiss Cohort Study on Air Pollution and Lung and Heart Disease in Adults), which started in 1991 with 9651 randomly selected adults aged 18–60 years from eight regions in Switzerland (Martin et al., 1997). No physical activity data was obtained at baseline (SAP 1). The first follow-up assessment (SAP 2) took place in 2002/03 and included four short questions regarding physical activity. 8047 individuals provided questionnaire data and 6500 additional data from physiological measurements (Ackermann-Liebrich et al., 2005). The second follow-up (SAP 3) was carried out in 2010/11 with questionnaire data available for 5921 and physiological data for 4808 surviving individuals who had participated in SAP2.
Measures
Weight-related measures
All overweight/obesity variables based on different objective measurement methods are summarized in Supplementary Material Table 1. Height and weight were measured according to standard operating procedures in SAP2 and SAP3. BMI was calculated as weight in kilograms divided by height in meters squared and categorized as overweight (25–29.99) and with obesity (≥ 30) according to WHO definitions (World Health Organization, 2000). Table 1 shows the different cut points used to classify overweight and obesity for the different weight variables.
Table 1.
Different measures of overweight and obesity and the cut-off points used.
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| Normal weight | Overweight | With obesity | Normal weight | Overweight | With obesity | |
| Body Mass Index (BMI) (World Health Organization, 2000) | < 25 | 25–29.99 | ≥ 30 | < 25 | 25–29.99 | ≥ 30 |
| Waist circumference (WC) (World Health Organization, 2000, Lean et al., 1995, World Health Organization, 2008) | < 94 | 94–101.9 | ≥ 102 | < 80 | 80–87.9 | ≥ 88 |
| Waist-to-hip ratio (WHR) (World Health Organization, 2000, National Institute of Health and National Heart Lung and Bloo) | < 0.9 | 0.9–0.99 | ≥ 1.0 | < 0.8 | 0.8–0.84 | ≥ 0.85 |
| Waist-to-height ratio (WHtR) (Browning et al., 2010, Ashwell, 2012) | < 0.5 | ≥ 0.5 | ≥ 0.6 | < 0.5 | ≥ 0.5 | ≥ 0.6 |
| BIA percent body fat (Peterson et al., 2014, Snitker, 2010) | ≤ 25% | > 25% | ≤ 32% | > 32% | ||
Waist and hip circumference were measured in SAP 3 only with participants in relaxed standing position using a SECA 201 measuring tape (SECA GmbH&Co, Hamburg, Germany). WC categories defined by Lean et al. (1995), supported by World Health Organization, 2000, World Health Organization, 2008 and commonly used in research (de Hollander et al., 2012) were used to define overweight and obesity and increased risk of metabolic complications.
Waist-to-hip ratio was calculated and categorized as overweight (> 0.8 for women, > 0.9 for men) (National Institute of Health and National Heart Lung and Blood Institute, 1998) and with obesity (> 0.85 for women, > 1.0 for men) (World Health Organization, 2000).
Waist-to-height ratio has been shown to be a good discriminator for cardiovascular disease risk (Lee et al., 2008, Ashwell et al., 2012) and was therefore additionally included. Cut-offs of ≥ 0.5 for overweight (Browning et al., 2010) and of ≥ 0.6 for obesity (Ashwell, 2012) were used for both gender groups.
Percent body fat was measured with BIA using the device Helios (Helios, Forana, Frankfurt, Germany). Cut-offs of > 25% for men (Peterson et al., 2014) and > 32% for women (which is between the commonly used values of 30% (Snitker, 2010) and 35% (Peterson et al., 2014)) were used.
Physical activity measures
Physical activity measures are summarized in Supplementary Material Table 1. For cross-sectional analyses, data on different domains of physical activity and on sitting time were available from the long version of the International Physical Activity Questionnaire (IPAQ) in a random sub sample of SAP 3 participants (3042 individuals). The IPAQ has been validated in several countries (Craig et al., 2003) and a validation study has also been carried out in the SAPALDIA population (Wanner et al., under review). The IPAQ data have been processed according to the IPAQ Scoring protocol (International Physical Activity Questionnaire team, 2005). For each domain and intensity of physical activity the MET-minutes per week were computed. MET (metabolic equivalent) is a physiological measure that expresses the energy cost of physical activities. One MET is the energy expended at rest. For sedentary time, hours per day spent sitting were analyzed.
For cross-sectional and longitudinal analyses, four short questions on physical activity based on the Swiss Health Survey were available at SAP 2 and SAP 3 assessing frequency and duration of moderate- and vigorous-intensity activities (Lamprecht and Stamm, 2016, Meyer et al., 2005). Minutes per week spent in moderate and vigorous activities were calculated. Furthermore, individuals were categorized as active if they spent at least 150 min in at least moderate activities per week and as inactive for less activity. Finally individuals were also categorized as active and inactive based on MET-minutes per week dichotomized at the median. Patterns of change in physical activity were defined as follows: remaining active (active at SAP 2 and SAP 3), becoming active (inactive at SAP 2, active at SAP 3), becoming inactive (active at SAP 2, inactive at SAP 3), and remaining inactive (inactive both at SAP 2 and SAP 3).
Covariates
Based on previous research regarding potential confounders in analyses between physical activity and overweight/obesity, the following socio-demographic variables based on questionnaire data were included as covariates in the regression models: age (continuous), male versus female, nationality (Swiss versus non-Swiss), education (tertiary education versus lower education), and language region (German, French and Italian speaking). To reflect health and behavior, general health status (very good, good, not so good/bad based on the first question of the SF36 (Ware and Sherbourne, 1992)), smoking status (current smoker versus current non-smoker), sleep duration (≥ 6 h/night versus less) (Xiao et al., 2013), alcohol intake (< 3 times/week versus more) and total energy intake (kcal) were included in the analyses. The nutritional information was derived from a detailed Food Frequency Questionnaire (FFQ) used in SAP 3 (Steinemann et al., 2014). The FFQ was developed for Switzerland. The Swiss nutritional database SwissFIR was used to calculate the intake of different micro- and macronutrients as well as fat, carbohydrate, protein and total energy intake.
Statistical analyses
Multivariable logistic regression models were used for all analyses with binary overweight/obesity outcome variables (either overweight versus normal weight or with obesity versus normal weight), physical activity as primary independent variable and socio-demographic, health- and behavior-related variables as potential confounders. For cross-sectional associations, MET-minutes per week of the various physical activity variables were categorized into tertiles (low, medium, high). Adjusting for sitting time in addition did not change the results and was therefore not included. The lowest tertile was taken as reference category. Furthermore, four categories were defined based on IPAQ leisure-time physical activity (LTPA) and sitting time (i.e., low LTPA/high sitting; low LTPA/low sitting; high LTPA/high sitting, high LTPA/low sitting were defined by splitting the two variables at their median) and associations of this variable with different measures of overweight/obesity were assessed.
For longitudinal analyses, a categorical variable (referred to as “longitudinal activity pattern”) with levels “remaining active”, “becoming active”, “becoming inactive” and “remaining inactive” was defined. Different binary overweight and obesity parameters at SAP 3 were used as dependent variables, longitudinal activity pattern as main independent variable and socio-demographic and health- and behavior-related variables as well as BMI at SAP 2 as potential confounder variables. An increase in weight of 3% between SAP 2 and SAP 3 (compared to those with less than 3% weight increase or weight decrease) was used as additional outcome. The 3% threshold corresponded to the upper tertile of relative weight change. Furthermore, categories combining the longitudinal activity pattern (SAP 2-SAP 3) and the four categories of LTPA and sitting (SAP 3) were defined: consistently active: inactive or active at SAP 2 and active at SAP 3 and high LTPA/low sitting at SAP 3; consistently inactive: inactive or active at SAP 2 and inactive at SAP 3 and low LTPA/high sitting at SAP 3; inconsistent pattern: all other combinations of changes in physical activity (SAP 2-SAP 3) and LTPA/sitting (SAP 3). Associations between these three categories and different measures of overweight/obesity were analyzed.
Results
Characteristics of study participants
The characteristics of the participants for the cross-sectional analyses (SAP 3 participants with IPAQ data) are displayed in Table 2; for the longitudinal analyses (basic data on physical activity at SAP 2 and SAP 3), the characteristics of the participants at SAP 2 are displayed in Supplementary Material Table 2. The age range was 37 to 81 years. Table 2 shows that estimated physical activity levels were substantially higher according to the IPAQ compared to the short questionnaire, however the sex differences were apparent in both measures (i.e., with men reporting higher levels of physical activity).
Table 2.
Characteristics of study population in 2010/11, SAPALDIA 3, Switzerland.
|
N |
Total |
SD |
N |
Men |
SD |
N |
Women |
SD |
|
|---|---|---|---|---|---|---|---|---|---|
| Mean/% | Mean/% | Mean/% | |||||||
| Socio-demographic variables | |||||||||
| Age, years | 3042 | 59.3 | 10.8 | 1440 | 59.5 | 10.9 | 1602 | 59.1 | 10.8 |
| Sex (%) | 3042 | 1440 | 1602 | ||||||
| Men | 47.3 | ||||||||
| Women | 52.7 | ||||||||
| Nationality (%) | 3042 | 1440 | 1602 | ||||||
| Swiss | 89.9 | 88.6 | 91.1 | ||||||
| Non-Swiss | 10.1 | 11.4 | 8.9 | ||||||
| Language region (%) | 3042 | 1440 | 1602 | ||||||
| German | 57.7 | 58.4 | 57.1 | ||||||
| French | 32.3 | 31.9 | 32.7 | ||||||
| Italian | 10.0 | 9.7 | 10.2 | ||||||
| Education (%) | 3042 | 1440 | 1602 | ||||||
| Lower than tertiary education | 69.0 | 59.9 | 77.1 | ||||||
| Tertiary education | 31.0 | 40.1 | 22.9 | ||||||
| Health-related variables | |||||||||
| BMI, kg/m2 | 3041 | 26.1 | 4.6 | 1440 | 27.0 | 3.9 | 1601 | 25.4 | 5.1 |
| BMI category (%) | 3041 | 1440 | 1601 | ||||||
| Normal weight | 44.8 | 32.9 | 55.6 | ||||||
| Overweight | 37.7 | 48.5 | 28.0 | ||||||
| With obesity | 17.5 | 18.6 | 16.4 | ||||||
| Waist circumference (WC), cm | 3014 | 90.0 | 13.9 | 1429 | 96.6 | 11.4 | 1585 | 84.0 | 13.2 |
| Waist-to-hip ratio (WHR) | 3011 | 0.9 | 0.1 | 1428 | 1.0 | 0.1 | 1583 | 0.8 | 0.1 |
| Waist-to-height ratio (WHtR) | 3014 | 0.5 | 0.1 | 1429 | 0.6 | 0.1 | 1585 | 0.5 | 0.1 |
| BIA % body fat | 2887 | 31.0 | 7.6 | 1365 | 26.2 | 5.8 | 1522 | 35.4 | 6.2 |
| Health status (%) | 2898 | 1382 | 1516 | ||||||
| Not so good or bad | 4.7 | 4.4 | 4.9 | ||||||
| Good | 45.0 | 44.6 | 45.5 | ||||||
| Excellent or very good | 50.3 | 51.0 | 49.6 | ||||||
| Smoking status (%) | 3041 | 1440 | 1601 | ||||||
| Current non-smoker | 84.6 | 83.5 | 85.6 | ||||||
| Current smoker | 15.4 | 16.5 | 14.4 | ||||||
| Alcohol intake (%) | 3009 | 1426 | 1583 | ||||||
| 1 or 2 times a week or less | 63.9 | 51.3 | 75.3 | ||||||
| Several times a week or daily | 36.1 | 48.7 | 24.7 | ||||||
| Sleeping (%) | 3010 | 1427 | 1583 | ||||||
| ≥ 6 h of sleep/night | 90.9 | 91.0 | 90.8 | ||||||
| < 6 h of sleep/night | 9.1 | 9.0 | 9.2 | ||||||
| Physical activity related variables | |||||||||
| Total PA according to IPAQ, MET-min/week | 3042 | 5046.1 | 4398.7 | 1440 | 5176.8 | 4609.8 | 1602 | 4928.7 | 4197.8 |
| Sitting, h/day | 2730 | 6.1 | 3.0 | 1321 | 6.6 | 3.2 | 1409 | 5.7 | 2.7 |
| PA according to short questionnaire, MET-min/week | 2975 | 1237.3 | 1172.2 | 1413 | 1354.2 | 1239.3 | 1562 | 1131.5 | 1097.7 |
| Dietary variables | |||||||||
| Energy intake, kcal | 2969 | 2128.0 | 888.8 | 1402 | 2301.6 | 996.2 | 1567 | 1972.7 | 747.1 |
| Fat intake, g | 2969 | 79.6 | 39.0 | 1402 | 86.3 | 43.6 | 1567 | 73.6 | 33.2 |
| Carbohydrate intake, g | 2969 | 297.5 | 135.2 | 1402 | 312.0 | 149.3 | 1567 | 284.5 | 119.7 |
| Protein intake, g | 2969 | 102.0 | 48.4 | 1402 | 112.8 | 56.2 | 1567 | 92.2 | 37.7 |
Abbreviations: BIA, bioelectric impedance analysis; BMI, body mass index; IPAQ, International Physical Activity Questionnaire; MET, metabolic equivalent; N, numbers; PA, physical activity; SD, standard deviation.
Cross-sectional associations between physical activity, sitting time and overweight/obesity (SAPALDIA 3)
Table 3 (extract) and Supplementary Material Table 3 (full table) show the cross-sectional associations between different domains and intensities of physical activity and various measures of overweight and obesity. Total, leisure-time and vigorous physical activity showed significant negative associations with all obesity parameters. Consistent dose-dependent associations with lower OR for the high than for the medium tertiles of physical activity were observed for leisure-time physical activity only. For example, compared to an individual in the lowest tertile of leisure-time physical activity, an individual in the highest tertile had a 40% lower risk of being in the high BIA percent body fat category (OR = 0.60).
Table 3.
Cross-sectional associations of categorical measures of physical activity and sitting time with various measures of overweight/obesity (based on multivariable logistic regression) in 2010/11, SAPALDIA 3, Switzerland (extract, for full table with all exposure and outcome variables see Supplementary Material Table 3).
Cross-sectional associations of categorical measures of physical activity and sitting time with various measures of overweight/obesity (based on multivariable logistic regression) in 2010/11, SAPALDIA 3, Switzerland (extract, for full table with all exposure and outcome variables see Supplementary Material Table 3).
| Cut points for tertiles | BMI ≥ 30 |
WC ≥ 102/≥88 |
WHtR ≥ 0.6 |
BIA % body fat > 25%/>32% |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | |||
| IPAQ | ||||||||||||||
| Total physical activity (MET min/week) | Low | < 2528 | 1730 | 1.00 | 2119 | 1.00 | 1500 | 1.00 | 2657 | 1.00 | ||||
| Medium | 2528 to 5910 | 0.65 | 0.50–0.86 | 0.74 | 0.60–0.93 | 0.64 | 0.47–0.88 | 0.63 | 0.51–0.78 | |||||
| High | > 5910 | 0.71 | 0.54–0.94 | 0.65 | 0.51–0.81 | 0.67 | 0.49–0.92 | 0.60 | 0.48–0.74 | |||||
| Leisure-time physical activity (MET min/week) | Low | < 460 | 1671 | 1.00 | 2050 | 1.00 | 1453 | 1.00 | 2570 | 1.00 | ||||
| Medium | 460 to 1515 | 0.69 | 0.52–0.91 | 0.68 | 0.54–0.86 | 0.66 | 0.48–0.91 | 0.69 | 0.56–0.86 | |||||
| High | > 1515 | 0.63 | 0.47–0.85 | 0.56 | 0.44–0.71 | 0.50 | 0.36–0.69 | 0.60 | 0.48–0.74 | |||||
| Total moderate activities (MET min/week) | Low | < 910 | 1729 | 1.00 | 2118 | 1.00 | 1499 | 1.00 | 2656 | 1.00 | ||||
| Medium | 910 to 2900 | 0.80 | 0.61–1.05 | 0.85 | 0.68–1.06 | 0.65 | 0.48–0.88 | 0.76 | 0.62–0.93 | |||||
| High | > 2900 | 0.82 | 0.62–1.08 | 0.79 | 0.63–1.00 | 0.88 | 0.65–1.21 | 0.67 | 0.55–0.83 | |||||
| Total walking (MET min/week) | Low | < 570 | 1729 | 1.00 | 2117 | 1.00 | 1499 | 1.00 | 2655 | 1.00 | ||||
| Medium | 570 to 1800 | 0.93 | 0.71–1.22 | 0.97 | 0.77–1.21 | 1.04 | 0.77–1.42 | 1.05 | 0.86–1.28 | |||||
| High | > 1800 | 0.78 | 0.59–1.04 | 0.72 | 0.57–0.91 | 0.71 | 0.52–0.99 | 0.94 | 0.76–1.17 | |||||
| Total vigorous activities (MET min/week) | Low | 0 | 1725 | 1.00 | 2112 | 1.00 | 1495 | 1.00 | 2649 | 1.00 | ||||
| Medium | 1 to 960 | 0.50 | 0.36–0.70 | 0.68 | 0.53–0.87 | 0.47 | 0.33–0.68 | 0.71 | 0.57–0.89 | |||||
| High | > 960 | 0.72 | 0.55–0.95 | 0.66 | 0.53–0.83 | 0.53 | 0.39–0.73 | 0.59 | 0.49–0.73 | |||||
| Sitting (h/day) | Low | < 4.58 | 1569 | 1.00 | 1913 | 1.00 | 1352 | 1.00 | 2407 | 1.00 | ||||
| Medium | 4.58 to 6.86 | 1.01 | 0.76–1.36 | 1.14 | 0.90–1.45 | 1.13 | 0.82–1.57 | 1.39 | 1.12–1.72 | |||||
| High | > 6.86 | 1.14 | 0.85–1.54 | 1.25 | 0.98–1.59 | 1.03 | 0.73–1.45 | 1.59 | 1.28–1.98 | |||||
Note: significant results are in bold.
Abbreviations: BIA, bioelectric impedance analysis; BMI, body mass index; CI, confidence intervals; IPAQ, International Physical Activity Questionnaire; MET, metabolic equivalent; OR, odds ratio; WC, waist circumference; WHtR, waist-to-height ratio.
Adjusted for sex, age, nationality (Swiss versus non-Swiss), education (tertiary versus lower), language region (German-, French-, Italian-speaking), smoking (current versus non-smoker), alcohol intake (less than 3 times a week versus more), health status (very good, good or not so good/bad), sleeping hours (≥ 6 versus < 6 h/night), and total energy intake.
Associations were most consistent across different physical activity parameters for BIA percent body fat. All activities in Table 3 except walking were significantly associated with BIA percent body fat. High BIA percent body fat and WC (medium tertile) were the only overweight/obesity parameters significantly associated with sitting time. Interestingly, total energy intake was not significantly associated with overweight/obesity (OR = 1.00 for total energy intake association with BIA percent body fat, adjusted for all other variables in the model including total physical activity, p = 0.94, data not shown).
There were no associations of work-related and domestic activities with any overweight/obesity parameter (Supplementary Material Table 3). For transport-related physical activity, there was a difference between the highest and the lowest tertile for obesity parameters but not for BIA percent body fat.
Regarding the physical activity variables based on the short questionnaire at SAP 3 (Supplementary Material Table 3), there were significantly decreased obesity and BIA percent body fat rates in the highest tertiles of physical activity.
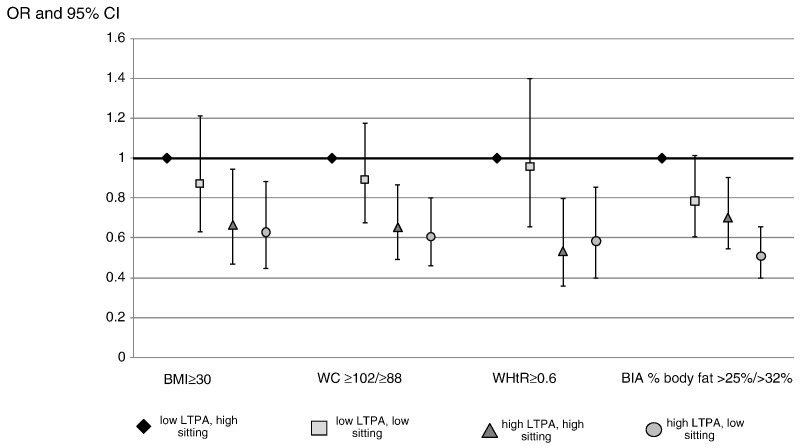
Fig. 1 displays the cross-sectional associations between the four categories of low and high LTPA/sitting time and different measures of overweight/obesity. The distribution of participants in the four categories was 26.4% for low LTPA/high sitting, 24.5% for low LTPA/low sitting, 23.7% for high LTPA/high sitting and 25.4% for high LTPA/low sitting. The odds of having BMI ≥ 30, WC ≥ 102/≥88 or WHtR ≥ 0.6 was significantly lower for individuals with high LTPA levels independent of sitting time, while low compared to high sitting time was not significantly associated with body weight status. For BIA percent body fat, there was a dose-dependent association with lowest OR for high LTPA/low sitting.
Fig. 1.
Adjusted odds ratios (based on multivariable logistic regression) of overweight/obesity associated with various patterns of physical activity and sitting time in 2010/11, SAPALDIA 3, Switzerland.
Legend: BIA, bioelectric impedance analysis; BMI, body mass index; CI, confidence intervals; LTPA, leisure-time physical activity; OR, odds ratio; WC, waist circumference; WHtR, weight-to-height ratio.
Associations between longitudinal activity patterns and overweight/obesity
The longitudinal analyses (Table 4) revealed that individuals remaining inactive had significantly higher rates of obesity according to BMI, WC, WHtR and BIA percent body fat, and were more likely to increase weight more than 3% between SAP 2 and SAP 3 compared to individuals remaining active. Becoming inactive significantly increased the risk of being in the higher BIA percent body fat category and of increasing at least 3% of body weight between SAP 2 and SAP 3. Becoming active was comparable to remaining active with regard to body weight and composition.
Table 4.
Longitudinal associations between physical activity (pattern over time) and overweight and obesity (based on multivariable logistic regression) at SAPALDIA 3, 2002/03 and 2010/11, SAPALDIA 2 and 3, Switzerland.
| BMI ≥ 30 at SAP 3 |
WC ≥ 102/≥88 |
WHtR ≥ 0.6 |
BIA % body fat > 25%/>32% |
Weight increase⁎ |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | |
| Not adjusted for energy intake at SAP 3 | 2259 | 2843 | 1966 | 3559 | 3787 | ||||||||||
| Remaining active | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Becoming active | 1.11 | 0.47–2.67 | 1.10 | 0.80–1.50 | 0.91 | 0.50–1.68 | 1.09 | 0.88–1.37 | 1.18 | 0.99–1.42 | |||||
| Becoming inactive | 1.66 | 0.67–4.09 | 0.78 | 0.55–1.11 | 0.85 | 0.44–1.62 | 1.31 | 1.01–1.68 | 1.35 | 1.11–1.65 | |||||
| Remaining inactive | 2.78 | 1.23–6.27 | 1.54 | 1.13–2.10 | 2.06 | 1.15–3.69 | 1.60 | 1.28–2.00 | 1.36 | 1.14–1.62 | |||||
| Adjusted for energy intake at SAP3 | 1511 | 1874 | 1299 | 2336 | 2444 | ||||||||||
| Remaining active | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Becoming active | 1.80 | 0.65–5.00 | 0.91 | 0.62–1.32 | 0.83 | 0.40–1.71 | 1.01 | 0.77–1.33 | 1.23 | 0.98–1.54 | |||||
| Becoming inactive | 2.04 | 0.71–5.89 | 0.84 | 0.53–1.31 | 1.10 | 0.48–2.48 | 1.68 | 1.22–2.31 | 1.42 | 1.10–1.84 | |||||
| Remaining inactive | 2.71 | 1.05–6.98 | 1.40 | 0.95–2.06 | 1.14 | 0.55–2.37 | 1.57 | 1.19–2.08 | 1.38 | 1.10–1.73 | |||||
Note: significant results are in bold.
Abbreviations: BIA, bioelectric impedance analysis; BMI, body mass index; CI, confidence intervals; OR, odds ratio; SAP, SAPALDIA (Swiss Cohort Study on Air Pollution and Lung and Heart Disease in Adults); SAP 3, second follow-up of SAPALDIA; WC, waist circumference; WHtR, waist-to-height ratio.
Adjusted for sex, age, nationality (Swiss versus non-Swiss), education (tertiary versus lower), language region (German-, French-, Italian-speaking), BMI at SAP 2, smoking (current versus non-smoker), alcohol intake (less than three times a week versus more), health status (very good, good or not so good/bad).
Weight increase: gaining ≥ 3% of SAP 2 weight between SAP 2 and SAP 3 (compared to gaining less than 3% or losing weight); 3% was chosen based on the distribution of the data (see statistical analysis section).
Categorization of “active”/”inactive”: active: ≥ 150 min/week of moderate activity; inactive: < 150 min/week of moderate activity.
Remaining active: categorized as active both in SAP2 and SAP3.
Becoming active: categorized as inactive in SAP2 and as active in SAP3.
Becoming inactive: categorized as active in SAP2 and as inactive in SAP3.
Remaining inactive: categorized as inactive both in SAP2 and SAP3.
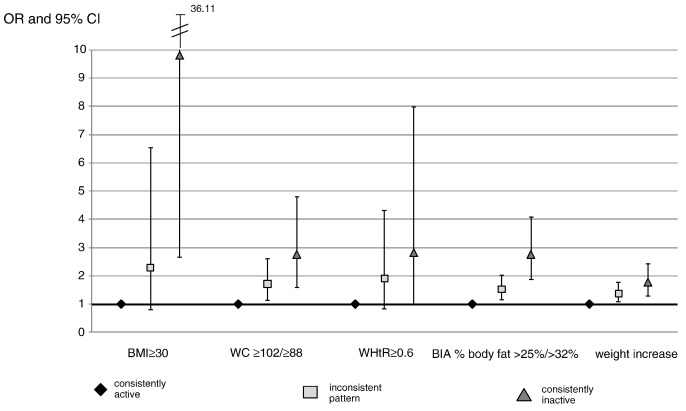
Fig. 2 shows the associations of different activity patterns involving changes over time (SAP 2-SAP 3) and LTPA/sitting at SAP 3 with different overweight/obesity parameters at SAP 3, as well as weight change between SAP 2 and SAP 3. The distribution of participants in the three activity pattern categories was 19.0% for “consistently active”, 14.6% for “consistently inactive” and 66.4% for the inconsistent patterns. Being consistently inactive was associated with higher odds of having overweight/obesity according to all outcomes (borderline significant for WHtR ≥ 0.6 (p = 0.05)) compared to being consistently active. Compared to individuals who were consistently active, those with inconsistent patterns had significantly higher odds for the outcomes WC ≥ 102/≥88, BIA percent body fat and a weight increase of at least 3% between SAP 2 and SAP 3.
Fig. 2.
Adjusted odds ratios of overweight/obesity (in SAPALDIA 3, based on multivariable logistic regression) associated with different patterns of change in physical activity between 202/03 and 2010/11, SAPALDIA 2 and 3, Switzerland.
Legend: BIA, bioelectric impedance analysis; BMI, body mass index; CI, confidence intervals; OR, odds ratio; SAP, SAPALDIA (Swiss Cohort Study on Air Pollution and Lung and Heart Disease in Adults); WC, waist circumference; WHtR, weight-to-height ratio; weight increase: gaining ≥ 3% of SAP 2 weight between SAP 2 and SAP 3 (compared to gaining less than 3% or losing weight); consistently active: inactive-active (SAP 2-SAP 3) and high LTPA/low sitting (SAP 3) or active-active (SAP 2-SAP 3) and high LTPA/low sitting (SAP 3); consistently inactive: inactive-inactive (SAP 2-SAP 3) and low LTPA/high sitting (SAP 3) or active-inactive (SAP 2-SAP 3) and low LTPA/high sitting (SAP 3); inconsistent pattern: all other combinations of changes in physical activity (SAP 2-SAP 3) and LTPA/sitting (SAP 3).
Discussion
The cross-sectional associations with different obesity parameters were most apparent for LTPA and vigorous physical activity based on the IPAQ. We did not find any associations for work-related and domestic physical activities with any overweight and obesity parameters. Most consistent associations were found for BIA percent body fat, also regarding sitting time. But according to Fig. 1, low versus high sitting was not associated with the obesity outcomes BMI, WC and WHtR, while LTPA was, indicating that LTPA is a more important factor for obesity than sitting time. In Fig. 1, a dose-dependent relationship was only observed for BIA percent body fat for the different categories of high and low LTPA/sitting time. According to longitudinal analyses, remaining and becoming active were factors that helped maintain a healthy weight, while remaining inactive was a strong risk factor for obesity at SAP 3.
Other studies have reported associations between domain-specific physical activity and overweight/obesity. In a systematic review, studies reporting physical activity behavior both at baseline and follow-up found relatively consistent evidence that a large volume of physical activity was associated with less weight gain (Fogelholm and Kukkonen-Harjula, 2000). However, the increase in physical activity needed to improve weight maintenance was high with an estimate of between 1500 and 2000 kcal/week, an increase which is difficult to achieve. Unlike our results, other studies reported inverse associations between occupational physical activity and obesity (Florindo et al., 2009, Steeves et al., 2012) and body weight (Monda et al., 2008). For domestic physical activity, most studies reported no association (Monda et al., 2008, Stamatakis et al., 2009), except for a Chinese study that found an association in men only (Monda et al., 2008). Similar to our results, transport physical activity was inversely associated with obesity in a cross-sectional study (Florindo et al., 2009) and with BMI, WC and changes in BMI in a large cohort of middle-aged men over 5 years of follow-up (Wagner et al., 2001). Most evidence for an association with body composition is available for LTPA (Wareham et al., 2005), probably because only few studies have included other domains of physical activity. A large longitudinal study in women found an increased risk of becoming overweight or with obesity after a median follow-up of 11.6 years for low vigorous and total LTPA, however the associations decreased when baseline BMI was taken into account (Britton et al., 2012). Inverse associations were also reported in other studies (Florindo et al., 2009, Stamatakis et al., 2009, Wagner et al., 2001), especially for high-intensity activity (Wagner et al., 2001).
Even though we did not find associations between work-related and domestic physical activity and overweight/obesity, we do not assume that physical activity in these domains is less effective for weight control than for example LTPA. It is possible that LTPA was better remembered and duration and intensity more accurately reported than work-related and domestic physical activity, so that measurement error may conceal the possible associations for work-related and domestic activities. IPAQ validation results in the present study population indicate that correlations were moderate for LTPA and vigorous activities but low or non-existent for work-related and domestic activities (Wanner et al., under review), indicating that reporting or recall bias may have influenced the results of this study.
The large differences in physical activity levels according to the IPAQ and the short questions is probably due to the fact that the IPAQ explicitly asks for activities in four different domains while it is likely that participants mostly included leisure-time physical activity when responding to the short questions. Total physical activity reported in the IPAQ in our study group (5045 MET-minutes per week) is comparable to amounts reported in a Swedish study (4536 MET-minutes per week) (Hagstromer et al., 2010).
Regarding sitting and overweight/obesity, Stamatakis et al. reported an increased risk of obesity according to BMI and WC for more than 2 h of television viewing and other screen-based activities (Stamatakis et al., 2009). However, comparability with our results is limited as that study did not include all sedentary activities. In general, results from studies investigating prospective relationships of sedentary behavior with obesity incidence, weight gain, weight maintenance and measures of obesity have been mixed (Thorp et al., 2011). Especially, associations often diminished after adjustment for baseline BMI. Furthermore, most studies used BMI or WC as measures of overweight/obesity and not BIA percent body fat.
Interestingly, there were no associations between estimated total energy intake and any overweight/obesity parameters in the adjusted analyses. These results are in line with recent analyses of NHANES data showing that BMI and waist circumference trends were associated with physical activity level, but not caloric intake (Ladabaum et al., 2014).
The fact that the most consistent associations were found for BIA percent body fat is in line with other research indicating that BMI may not be a good discriminator for mortality or other health outcomes (Lee et al., 2008). Studies reporting on the obesity paradox stating better survival in patients with obesity are mainly based on BMI (McAuley and Blair, 2011), however the commonly used BMI cut offs seem to have a low sensitivity to diagnose adiposity at the individual level as they fail to identify half of the people with excess percent body fat (Okorodudu et al., 2010). Our results suggest that BIA percent body fat is the best measure of physical activity related overweight/obesity. Lack of associations with other measures such as BMI and WC may be due to measurement error. Correlations of around 0.7 have been reported between BMI and percent body fat in another study (Farrell et al., 2010), indicating a good agreement between these two measures. In several studies looking at overweight/obesity and health outcomes, fitness or physical activity levels are not taken into account, neglecting the fact that fat but fit individuals have a substantially lower mortality risk than normal-weight but unfit individuals (McAuley and Blair, 2011).
The strengths of this study are its large underlying population-based cohort, the domain-specific information on physical activity and different objective measures of weight status and body composition including BIA percent body fat, the 10-year follow-up for patterns of physical activity change, and the inclusion of important potential confounders. However, the study has also some limitations. In the first follow-up assessment (serving as the baseline for the current analyses), no domain-specific information on physical activity or objective measures of overweight and obesity beyond BMI were assessed. Moreover, only a sub sample of 3042 individuals (of 5921 in total) completed the long IPAQ in the second follow-up assessment. Participants were more likely to be female, higher educated and had a healthier lifestyle (see Supplementary Material Table 4). However, selective participation is likely to have had the same effect on physical activity and overweight/obesity and should therefore not bias the results. Finally, causal inferences can at best be drawn from our longitudinal results.
Conclusions
We found cross-sectional associations between different physical activity variables (especially LTPA and vigorous physical activity) and different obesity parameters, with most consistent associations for BIA percent body fat. Sitting time was significantly associated only with BIA percent body fat. No associations were found for work-related and domestic physical activity, and for most overweight parameters. According to the longitudinal analyses, remaining inactive and becoming inactive were associated with BIA percent body fat at SAP 3 and weight increase, while remaining active and becoming active seemed to have a favorable effect on weight status. For prevention purposes, the results indicate that physical activity can have an important contribution to weight management.
The following are the supplementary related to this article.
Summary of measures of overweight/obesity and physical activity in SAP 2 and SAP 3 used in the present analyses.
Characteristics of study population in 2002/03 (SAP 2).
Cross-sectional associations between domains of physical activity, sitting time and different measures of overweight/obesity.
Drop out analysis (N = 3042 in sample).
Funding sources
This study was part of the SAPALDIA study. The SAPALDIA study is supported by grants from the Swiss National Science Foundation (grant nos. 33CSCO-108796, 3247BO-104283, 3247BO-104288, 3247BO-104284, 3247-065896, 3100-059302, 3200-052720, 3200-042532, 4026-028099), the Federal Office for Forest, Environment and Landscape, the Federal Office of Public Health, the Federal Office of Roads and Transport, the Canton's Government of Aargau, Basel-Stadt, Basel-Land, Geneva, Luzern, Ticino, Valais, and Zürich, the Swiss Lung League, the Canton's Lung League of Basel Stadt/ Basel Landschaft, Geneva, Ticino, Valais and Zurich, SUVA, Freiwillige Akademische Gesellschaft, UBS Wealth Foundation, Talecris Biotherapeutics GmbH, Abbott Diagnostics, European Commission 018996 (GABRIEL), Wellcome Trust WT 084703MA.
Conflict of interest
The authors declare that there are no conflicts of interest.
Transparency document
Transparency document.
Acknowledgments
Study directorate: T Rochat (p), JM Gaspoz (c), N Künzli (e/exp), NM Probst Hensch (e/g), C Schindler (s).
Scientific team: JC Barthélémy (c), W Berger (g), R Bettschart (p), A Bircher (a), O Brändli (p), C Brombach (n), M Brutsche (p), L Burdet (p), M Frey (p), U Frey (pd), MW Gerbase (p), D Gold (e/c/p), E de Groot (c), W Karrer (p), R Keller (p), B Martin (pa), D Miedinger (o), U Neu (exp), L Nicod (p), M Pons (p), F Roche (c), T Rothe (p), E Russi (p), P Schmid-Grendelmeyer (a), A Schmidt-Trucksäss (pa), A Turk (p), J Schwartz (e), D. Stolz (p), P Straehl (exp), JM Tschopp (p), A von Eckardstein (cc), E Zemp Stutz (e).
Scientific team at coordinating centers: M Adam (e/g), E Boes (g), PO Bridevaux (p), D Carballo (c), E Corradi (e), I Curjuric (e), J Dratva (e), A Di Pasquale (s), E Dupuis Lozeron (s), M Germond (s), L Grize (s), D Keidel (s), S Kriemler (pa), A Kumar (g), M Imboden (g), N Maire (s), A Mehta (e), H Phuleria (exp), E Schaffner (s), GA Thun (g) A Ineichen (exp), M Ragettli (e), M Ritter (exp), T Schikowski (e), M Tarantino (s), M Tsai (e), M Wanner (pa).
(a) allergology, (c) cardiology, (cc) clinical chemistry, (e) epidemiology, (exp) exposure, (g) genetic and molecular biology, (m) meteorology, (n) nutrition, (o) occupational health, (p) pneumology, (pa) physical activity, (pd) pediatrics, (s) statistics.
The study could not have been done without the help of the study participants, technical and administrative support and the medical teams and field workers at the local study sites.
Local fieldworkers: Aarau: S Brun, G Giger, M Sperisen, M Stahel, Basel: C Bürli, C Dahler, N Oertli, I Harreh, F Karrer, G Novicic, N Wyttenbacher, Davos: A Saner, P Senn, R Winzeler, Geneva: F Bonfils, B Blicharz, C Landolt, J Rochat, Lugano: S Boccia, E Gehrig, MT Mandia, G Solari, B Viscardi, Montana: AP Bieri, C Darioly, M Maire, Payerne: F Ding, P Danieli A Vonnez, Wald: D Bodmer, E Hochstrasser, R Kunz, C Meier, J Rakic, U Schafroth, A Walder.
Administrative staff: C Gabriel, R Gutknecht.
Master student involved in data assessment: Michèle Geissbühler.
Footnotes
The Transparency document associated with this article can be found, in the online version.
References
- Ackermann-Liebrich U., Kuna-Dibbert B., Probst-Hensch N.M. Follow-up of the Swiss Cohort Study On Air Pollution and Lung Diseases in Adults (SAPALDIA 2) 1991–2003: methods and characterization of participants. Soz. Praventivmed. 2005;50(4):245–263. doi: 10.1007/s00038-005-4075-5. [DOI] [PubMed] [Google Scholar]
- Ashwell M. Plea for simplicity: use of waist-to-height ratio as a primary screening tool to assess cardiometabolic risk. Clin. Obes. 2012 doi: 10.1111/j.1758-8111.2012.00037.x. [DOI] [PubMed] [Google Scholar]
- Ashwell M., Gunn P., Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes. Rev. 2012;13(3):275–286. doi: 10.1111/j.1467-789X.2011.00952.x. [DOI] [PubMed] [Google Scholar]
- Bouchard C., Blair S.N., Haskell W.L. Why study physical activity and health? In: Bouchard C., SN B., WL H., editors. Physical Activity and Health. second ed. Human Kinetics; Champaign, IL: 2007. p. 12. [Google Scholar]
- Britton K.A., Lee I.M., Wang L. Physical activity and the risk of becoming overweight or obese in middle-aged and older women. Obesity (Silver Spring) 2012;20(5):1096–1103. doi: 10.1038/oby.2011.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning L.M., Hsieh S.D., Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr. Res. Rev. 2010;23(2):247–269. doi: 10.1017/S0954422410000144. [DOI] [PubMed] [Google Scholar]
- Craig C.L., Marshall A.L., Sjostrom M. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Czernichow S., Kengne A.P., Stamatakis E., Hamer M., Batty G.D. Body mass index, waist circumference and waist-hip ratio: which is the better discriminator of cardiovascular disease mortality risk?: evidence from an individual-participant meta-analysis of 82,864 participants from nine cohort studies. Obes. Rev. 2011;12(9):680–687. doi: 10.1111/j.1467-789X.2011.00879.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Hollander E.L., Bemelmans W.J., Boshuizen H.C. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: a meta-analysis of 29 cohorts involving more than 58,000 elderly persons. Int. J. Epidemiol. 2012 doi: 10.1093/ije/dys008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell S.W., Fitzgerald S.J., McAuley P.A., Barlow C.E. Cardiorespiratory fitness, adiposity, and all-cause mortality in women. Med. Sci. Sports Exerc. 2010;42(11):2006–2012. doi: 10.1249/MSS.0b013e3181df12bf. [DOI] [PubMed] [Google Scholar]
- Florindo A.A., Guimaraes V.V., Cesar C.L., Barros M.B., Alves M.C., Goldbaum M. Epidemiology of leisure, transportation, occupational, and household physical activity: prevalence and associated factors. J. Phys. Act. Health. 2009;6(5):625–632. doi: 10.1123/jpah.6.5.625. [DOI] [PubMed] [Google Scholar]
- Fogelholm M., Kukkonen-Harjula K. Does physical activity prevent weight gain — a systematic review. Obes. Rev. 2000;1(2):95–111. doi: 10.1046/j.1467-789x.2000.00016.x. [DOI] [PubMed] [Google Scholar]
- Hagstromer M., Ainsworth B.E., Oja P., Sjostrom M. Comparison of a subjective and an objective measure of physical activity in a population sample. J. Phys. Act. Health. 2010;7(4):541–550. doi: 10.1123/jpah.7.4.541. [DOI] [PubMed] [Google Scholar]
- International Physical Activity Questionnaire team: Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). In.; 2005: 6–12.
- Ladabaum U., Mannalithara A., Myer P.A., Singh G. Obesity, abdominal obesity, physical activity, and caloric intake in U.S. adults: 1988–2010. Am. J. Med. 2014 doi: 10.1016/j.amjmed.2014.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamprecht M., Stamm H.P. Statsanté Resultate zu den Gesundheitsstatistiken in der Schweiz. Swiss Federal Statistical Office; Neuchâtel: 2006. Bewegung, Sport, Gesundheit. Fakten und Trends aus den Schweizerischen Gesundheitsbefragungen 1992, 1997 und 2002 (Physical activity, sport, health. Facts and trends from the Swiss Health Surveys 1992, 1997, and 2002) [Google Scholar]
- Larson M.R. Social desirability and self-reported weight and height. Int. J. Obes. Relat. Metab. Disord. 2000;24(5):663–665. doi: 10.1038/sj.ijo.0801233. [DOI] [PubMed] [Google Scholar]
- Lean M.E., Han T.S., Morrison C.E. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311(6998):158–161. doi: 10.1136/bmj.311.6998.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C.M., Huxley R.R., Wildman R.P., Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J. Clin. Epidemiol. 2008;61(7):646–653. doi: 10.1016/j.jclinepi.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Martin B.W., Ackermann-Liebrich U., Leuenberger P. SAPALDIA: methods and participation in the cross-sectional part of the Swiss Study on Air Pollution and Lung Diseases in Adults. Soz. Praventivmed. 1997;42(2):67–84. doi: 10.1007/BF01318136. [DOI] [PubMed] [Google Scholar]
- McAuley P.A., Blair S.N. Obesity paradoxes. J. Sports Sci. 2011;29(8):773–782. doi: 10.1080/02640414.2011.553965. [DOI] [PubMed] [Google Scholar]
- Meyer K., Rezny L., Breuer C., Lamprecht M., Stamm H.P. Physical activity of adults aged 50 years and older in Switzerland. Soz. Praventivmed. 2005;50(4):218–229. doi: 10.1007/s00038-005-4093-3. [DOI] [PubMed] [Google Scholar]
- Monda K.L., Adair L.S., Zhai F., Popkin B.M. Longitudinal relationships between occupational and domestic physical activity patterns and body weight in China. Eur. J. Clin. Nutr. 2008;62(11):1318–1325. doi: 10.1038/sj.ejcn.1602849. [DOI] [PubMed] [Google Scholar]
- National Institute of Health, National Heart Lung and Blood Institute: Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. The Evidence Report. In.: National Institute of Health; 1998: 178.
- Okorodudu D.O., Jumean M.F., Montori V.M. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int. J. Obes. 2010;34(5):791–799. doi: 10.1038/ijo.2010.5. [DOI] [PubMed] [Google Scholar]
- Peterson M.D., Al Snih S., Stoddard J., Shekar A., Hurvitz E.A. Obesity misclassification and the metabolic syndrome in adults with functional mobility impairments: nutrition examination survey 2003–2006. Prev. Med. 2014;60:71–76. doi: 10.1016/j.ypmed.2013.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petursson H., Sigurdsson J.A., Bengtsson C., Nilsen T.I., Getz L. Body configuration as a predictor of mortality: comparison of five anthropometric measures in a 12 year follow-up of the Norwegian HUNT 2 study. PLoS One. 2011;6(10) doi: 10.1371/journal.pone.0026621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee . U.S. Department of Health and Human Services; Washington, DC: 2008. Physical Activity Guidelines Advisory Committee Report 2008. [DOI] [PubMed] [Google Scholar]
- Snitker S. Use of body fatness cutoff points. Mayo Clin. Proc. 2010;85(11):1057. doi: 10.4065/mcp.2010.0583. (author reply 1057-1058) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamatakis E., Hirani V., Rennie K. Moderate-to-vigorous physical activity and sedentary behaviours in relation to body mass index-defined and waist circumference-defined obesity. Br. J. Nutr. 2009;101(5):765–773. doi: 10.1017/S0007114508035939. [DOI] [PubMed] [Google Scholar]
- Steeves J.A., Bassett D.R., Jr., Thompson D.L., Fitzhugh E.C. Relationships of occupational and non-occupational physical activity to abdominal obesity. Int. J. Obes. 2012;36(1):100–106. doi: 10.1038/ijo.2011.50. [DOI] [PubMed] [Google Scholar]
- Steinemann N., Grize L., Schuh K., Kauf P., Probst-Hensch N., Brombach C. Wissenschaftlicher Kongress der Deutschen Gesellschaft für Ernährung e V. Paderborn. 2014. Validation of a Swiss Food Frequency Questionnaire for the SAPALDIA Study. [Google Scholar]
- Thorp A.A., Owen N., Neuhaus M., Dunstan D.W. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am. J. Prev. Med. 2011;41(2):207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- Wagner A., Simon C., Ducimetiere P. Leisure-time physical activity and regular walking or cycling to work are associated with adiposity and 5 y weight gain in middle-aged men: the PRIME Study. Int. J. Obes. Relat. Metab. Disord. 2001;25(7):940–948. doi: 10.1038/sj.ijo.0801635. [DOI] [PubMed] [Google Scholar]
- Wanner M., Gotschi T., Martin-Diener E., Kahlmeier S., Martin B.W. Active transport, physical activity, and body weight in adults: a systematic review. Am. J. Prev. Med. 2012;42(5):493–502. doi: 10.1016/j.amepre.2012.01.030. [DOI] [PubMed] [Google Scholar]
- Ware J.E., Jr., Sherbourne C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Wareham N.J., van Sluijs E.M., Ekelund U. Physical activity and obesity prevention: a review of the current evidence. Proc. Nutr. Soc. 2005;64(2):229–247. doi: 10.1079/pns2005423. [DOI] [PubMed] [Google Scholar]
- World Health Organization . WHO Technical Report Series 894. WHO; Geneva: 2000. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. [PubMed] [Google Scholar]
- World Health Organization . Report of a WHO Expert Consultation, Geneva, 8–11 December 2008. WHO; Geneva: 2008. Waist circumference and waist–hip ratio. [Google Scholar]
- Xiao Q., Arem H., Moore S.C., Hollenbeck A.R., Matthews C.E. A large prospective investigation of sleep duration, weight change, and obesity in the NIH-AARP Diet and Health Study cohort. Am. J. Epidemiol. 2013;178(11):1600–1610. doi: 10.1093/aje/kwt180. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Summary of measures of overweight/obesity and physical activity in SAP 2 and SAP 3 used in the present analyses.
Characteristics of study population in 2002/03 (SAP 2).
Cross-sectional associations between domains of physical activity, sitting time and different measures of overweight/obesity.
Drop out analysis (N = 3042 in sample).
Transparency document.