Abstract
♦ Background:
Patients are satisfied with their kidney care but want more support in making dialysis choices. Predialysis leaflets vary across services, with few being sufficient to enable patients' informed decision making. We describe the acceptability of a patient decision aid and feasibility of evaluating its effectiveness within usual predialysis practice.
♦ Methods:
Prospective non-randomized comparison design, Usual Care or Usual Care Plus Yorkshire Dialysis Decision Aid Booklet (+YoDDA), in 6 referral centers (Yorkshire-Humber, UK) for patients with sustained deterioration of kidney function. Consenting (C) patients completed questionnaires after predialysis consultation (T1), and 6 weeks later (T2). Measures assessed YoDDA's utility to support patients' decisions and integration within usual care.
♦ Results:
Usual Care (n = 105) and +YoDDA (n = 84) participant characteristics were similar: male (62%), white (94%), age (mean = 62.6; standard deviation [SD] 14.4), kidney disease severity (glomerular filtration rate [eGFR] mean = 14.7; SD 3.7); decisional conflict was < 25; choice-preference for home versus hospital dialysis approximately 50:50. Patients valued receiving YoDDA, reading it on their own (96%), and sharing it with family (72%). The +YoDDA participants had higher scores for understanding kidney disease, reasoning about options, feeling in control, sharing their decision with family. Study engagement varied by center (estimated range 14 – 49%; mean 45%); participants varied in completion of decision quality measures.
♦ Conclusions:
Receiving YoDDA as part of predialysis education was valued and useful to patients with worsening kidney disease. Integrating YoDDA actively within predialysis programs will meet clinical guidelines and patient need to support dialysis decision making in the context of patients' lifestyle.
Keywords: Patient decision aid, shared decision making, dialysis, conservative care, renal replacement therapy, implementation science
Predialysis education programs are recommended best practice for services (1–3). There is little guidance on how best to support patients making informed treatment decisions and, unsurprisingly, programs vary in their content and delivery across providers (4–6). All services provide leaflets to inform patients about their kidney disease and/or local services, but few are designed explicitly to support informed decision making (7). Studies indicate patients are satisfied with their involvement in kidney care and disease management (5) but want more support in making dialysis decisions (6,8,9). Patients usually describe the dialysis decision as being between ‘dialysis’ and ‘no dialysis’, often commenting they had no choice about dialysis type (8,10–12). Few studies report any pre-choice reasoning by patients to consider which dialysis option fits best into their life.
Decision aids use decision science to structure the healthcare problem in a way that supports people's ability to make reasoned decisions (13,14). Decision aids encourage people to consider accurate information about all options and their consequences without bias, evaluate this information in accordance with their values, make a decision based on trade-offs between evaluations (15,16), and, in the healthcare context, discuss their reasoning with others to implement an agreed choice (17,18). Decision aids include different components to facilitate decision making about the following (19–22): patients making reasoned decisions between options, i.e. patient decision aids (e.g. leaflets); professionals making accurate treatment choices, i.e. clinical decision support (e.g. guidelines); patients and professionals collaborating more effectively in the process of choosing healthcare within consultations, i.e. shared decision making support (e.g. patient/professional prompts/training) (Supplementary Figure S1: Informed, evidence-based and shared decisions).
Delivering information that is evidence-based and enables understanding of the healthcare problem is fundamental to ensuring patients' preferences are informed and essential to patients' deliberation with professionals about why a given option fits better into their lifestyle, at this time, than another. This paper describes the development of a patient decision aid, the Yorkshire Dialysis Decision Aid (YoDDA) booklet (23), and investigates a) its acceptability to people making dialysis decisions, and b) the feasibility of evaluating its effectiveness within usual care.
Methods
Setting and Design
The study was carried out across all 6 predialysis services within Yorkshire-Humber (UK) from February 2012 to March 2013. Between 5 and 30 patients with sustained deterioration of kidney function are referred, per center, to this region's predialysis services each month. About 2,300 patients have dialysis; 80% have center hemodialysis (CHD; hospital or satellite units), and 20% have home therapies (home hemodialysis, HHD; automated peritoneal dialysis, APD; continuous ambulatory peritoneal dialysis, CAPD) (24).
We selected a prospective non-randomized comparison study design with historic controls to minimize the impact of the research infrastructure on YoDDA's assimilation into usual predialysis education practice (18,25,26). It is an appropriate design for investigating with rigor a) YoDDA's efficacy and acceptability to predialysis patients and staff, and b) the feasibility of evaluating this complex intervention's effectiveness within usual care (27). The comparison groups were:
Usual Care – all patients referred to predialysis services in February 2012 – August 2012; usual care involved education (e.g. consultations, leaflets/videos, peer meetings, home visits) about conservative care and renal replacement therapy options for patients delivered by predialysis staff.
+YoDDA – all patients referred to predialysis services in September 2012 – March 2013; +YoDDA included usual predialysis care plus a copy of the YoDDA booklet, or the YoDDA booklet with additional self-report questions about their lifestyle and values (VT), delivered by predialysis staff.
Intervention
The YoDDA booklet is designed for people with worsening kidney disease, and their family members, to make informed decisions between 2 dialysis options delivered in 2 ways, in the context of their lifestyle: hemodialysis, in a medical center (CHD) or at home (HHD); peritoneal dialysis, at home in an automated (APD) or continuous ambulatory (CAPD) form. Its purpose is to a) help people reason to the best of their ability about which dialysis option suits them, or their family member, at this time (13) and b) support discussions with health professionals about lifestyle, values, and medical history of relevance to their choice and its integration within their kidney disease management (17–19).
The YoDDA booklet was developed using a systematic method (18,28), including: review of clinical guidelines, service frameworks and existing patient information (Supplementary Box S2: Patient resources and experts) (1–3,7,29–32); patient and professional surveys of dialysis choices and kidney disease experience (5,9–12,33–38) using decision analysis (39) and behavioral decision support guidance (13–15,40–47) to critique the healthcare problem and patient information; testing its face-validity and utility prior to this acceptability research (Supplementary Table S3: Steps of YoDDA development). We applied decision support techniques to identify and structure the decision-relevant information in the context of disease management (48–50), de-bias the information presented, and encourage active reasoning about options in accordance with a person's values (Supplementary Table S4: Function of techniques).
The YoDDA booklet can be used independently by patients, their carers and their family, and/or with staff delivering predialysis care. It is 44 pages long (14 point font) with 5 sections: Introduction – service's contact details, provenance, how to use YoDDA, and contents page; Section A – chronic and progressive kidney disease, end stage renal failure, and conservative care and renal replacement treatments information; Section B – dialysis options, thinking about the decision, common features of dialysis, and differences; Section C – decision-attribute summary table, and prompts to focus people on their lifestyle activities and treatment preferences; Section D – glossary, further information, research used. The Booklet's average readability scores are an 8 – 9th grade education level (11 – 14 years old) (44).
Sample
All adult patients with chronic kidney disease referred to the Yorkshire-Humber predialysis services over the study period were eligible for inclusion in this study, an estimated 67 patients per month. Statistical guidance (51) of 5 – 10 cases per outcome variable was used to estimate our sample size, i.e. a minimum of 80 – 100 patients per phase for measures assessing acceptability of information and patient-reported outcomes of informed decision making (52). Ethical approval was granted in October 2010 (ref: 10/H1302/72), and protocols registered (www.clinicaltrials.gov/show/NCT01671228).
Materials
We developed: for patients – a study recruitment letter, information sheet, consent form, questionnaires (T1 after the predialysis education consultation, T2 6 weeks later); for staff – a clinical data sheet to record the number of patients referred to the service and participants' details, a consultation checklist for predialysis nurses to note issues discussed with patients, and post-research impact questions for experiences of using YoDDA (contact authors for measures).
The questionnaire included both validated and pre-tested questions (13,19,52–55) (Supplementary Table S3: Steps of YoDDA development) to capture the varied outcomes of a complex intervention (27) evaluated within the delivery and experience of predialysis care, such as: staff disseminating, and patients reading, YoDDA; staff and patient experiences of using YoDDA and predialysis care; the efficacy of YoDDA to support patients' informed decision making between dialysis options. The feasibility study explored the performance of several measures of decision making process and outcome. In predialysis care, decisions are made over time, are made with several professionals and/or consultations, are only implemented when their disease worsens, may change as a result of a change in lifestyle or health state, impact on their daily management of chronic kidney disease, and can be reversed; decision quality measures have been validated in contexts with one-off, non-reversible decisions between treatment options in unfamiliar and acute health contexts, implemented immediately, or very soon after, a preference is stated (52). Patient measures assessed:
Characteristics (T1; clinical data sheet): age; sex; marital status; ethnicity; highest education level attained; annual income; disease state (estimated glomerular filtration rate [eGFR]) and patient-reported health related quality of life (EQ-5D, 3-level version) (56).
Usefulness of written information: how easy were leaflets to read, useful in helping understand kidney disease, dialysis and the decision, sufficient to make a decision (0 – 6; not at all – extremely) (T1, T2); satisfaction with predialysis care (0 – 10; not at all – extremely) (T2); use of YoDDA, i.e. read/show it to others (yes/no; T2).
Decision-making processes: views of control over choice, sharing decision with spouse/family/health professionals, knowing other patients' choices (0 – 6; not at all – extremely) (T1, T2); views of others in decision making, and difficulty in refusing health professional's recommendation (0 – 6; not at all – extremely) (T1, T2); dialysis choice preference (rank order CHD; HHD; APD; CAPD) (T1, T2); dialysis and chronic kidney disease knowledge (9 multiple-choice items; T1, T2); perceived seriousness and risk complications HD and PD (0 – 6; T1; T2); Brief Illness Perception Questionnaire (8 items with 0 – 10 scale; T1) (57).
Validated decision-making process and outcome measures: Stage of Decision Making (58) — one response from 6 statements about reaching a preference (consent; T1, T2); Preparation for Decision Making (59) — we used 5 of the 10 items assessing usefulness of written information to inform people about the decision and engage with health professionals (not at all, a little, somewhat, quite a bit, a great deal) (T1); Decisional Conflict Scale (60) – 16 items about making a reasoned decision (strongly disagree, disagree, neither agree nor disagree, agree, strongly agree) (T2).
Procedure
The study team worked with the local hospital research nurses (part of the Comprehensive Local Research Network at Sheffield, Leeds, Doncaster, York, Bradford, and Hull NHS hospitals, funded by the UK National Institute of Health Research) and predialysis nurses to identify patients referred to the service prior to their consultation. Research nurses informed patients of the study either at clinic or by mail. Participants completed a consent form (C); non-participants continued with usual care; their details were forwarded to the University study team (HLB, AEW, TG, LM), who sent out a questionnaire immediately after participants' predialysis education consultation (T1), and 6 weeks later (T2). Patients not returning questionnaires were contacted by telephone and sent another questionnaire (AEW, TG, LM). Research nurses recorded clinical data about participants from notes, and the number of patients using the service. Predialysis teams delivered usual care to all patients independently of patients' study participation; in phase 2 staff handed out YoDDA to fit in with their predialysis education practices. (Supplementary Figure S5: Study Flow Diagram.)
Analysis
Descriptive statistics summarize sample characteristics. MANOVA assess differences in information quality and decision making experience by Usual Care and +YoDDA groups, at T1 and T2; repeated measures analyses examine differences in experiences over time. Data were analyzed using SPSS (version 20, SPSS, Chicago, IL, USA). We noted this sample was less likely to complete all questionnaire items than participants from other decision aid studies (53–55). Variables with missing responses > 10% were excluded from the analyses; mean substitution was used for variables with < 10% missing data (51). Those completing both questionnaires were older, more likely to be women, and less likely to want to have CHD compared with those who completed consent and T1.
Results
Acceptability of YoDDA Within Predialysis Programs
Overall, 189/274 (69%) consented patients completed questionnaire T1 (Usual Care, 72%; +YoDDA, 65%); 156/274 (57%) completed questionnaire T1 and T2 (Usual Care, 59%; +YoDDA, 54%) (see Figure 1). Patient characteristics were similar across groups, when captured (Table 1). Participants' mean eGFR was M = 14.5 (standard deviation [SD] = 4.22) and M = 14.8 (SD = 3.51) (Usual Care/+YoDDA respectively; F(1,87) = 0.15, p = 0.70), with noticeable deterioration in their health state (56) (Table 1). Patients' dialysis preferences were around 50:50 for home:hospital options (Table 1). The study sample was representative of the region (24).
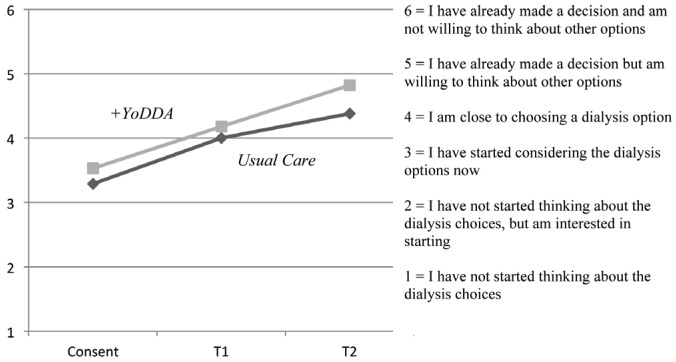
Figure 1 —
Stage of Decision Making (58) Mean Responses at Consent, T1 & T2 by group. YoDDA = Yorkshire Dialysis Decision Aid.
TABLE 1.
Socio-Demographic and Clinical Characteristics by Study Group at T1
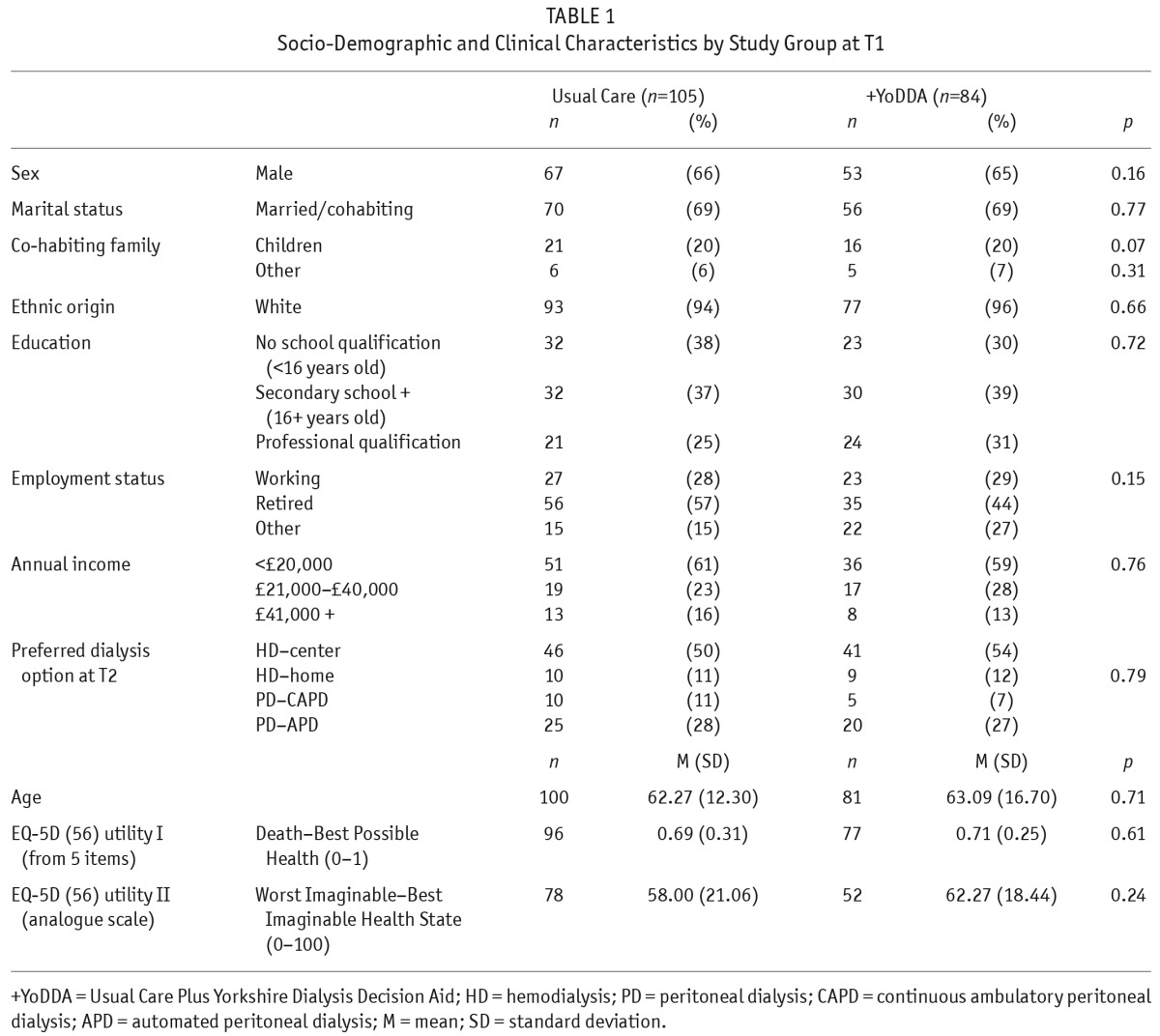
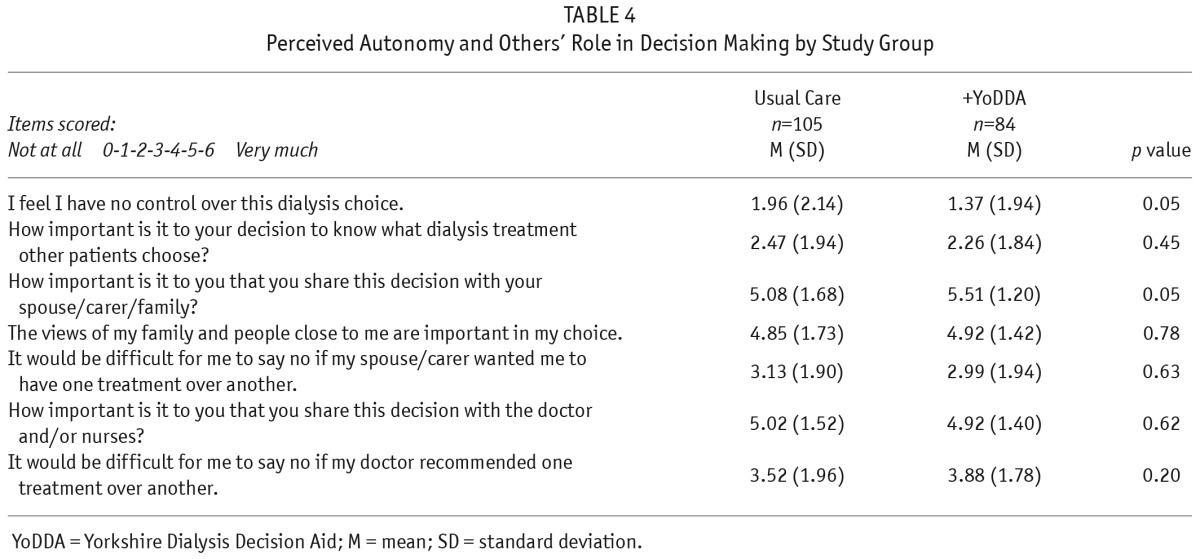
The +YoDDA patients had higher scores than Usual Care patients for the usefulness of written information to support understanding about kidney disease and dialysis options (Table 2), clarity of thinking about the decision in accordance with their values (59) (Table 3), and feeling in control of the choice, and sharing decision making with their family (Table 4). For all participants, the views of family and professionals, but not other patients, were important to their decision making (Table 4); satisfaction with the predialysis team was high (Usual Care M = 8.13, SD = 2.34; +YoDDA M = 8.66, SD = 1.67; F(1,187) = 3.04, p = 0.08) and participants felt able to engage with kidney health professionals (59) (Table 3).
TABLE 2.
Patient Views of Predialysis Written Information by Study Group
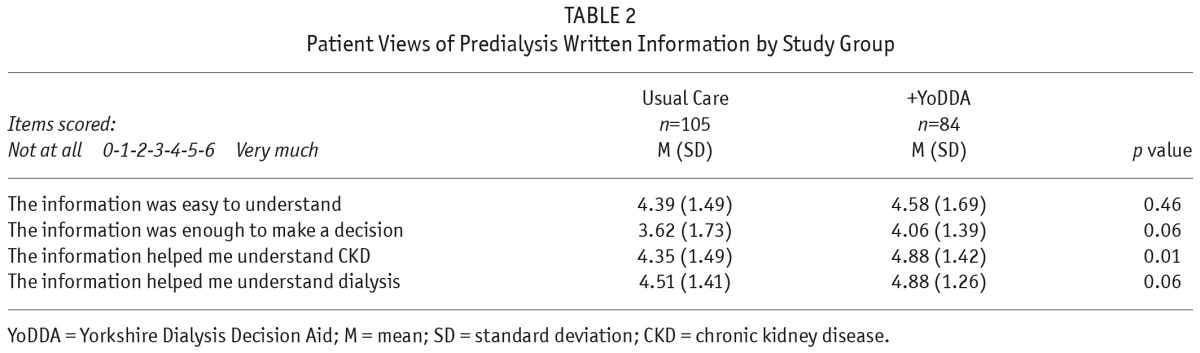
TABLE 3.
Preparation for Decision Making (59) by Study Group
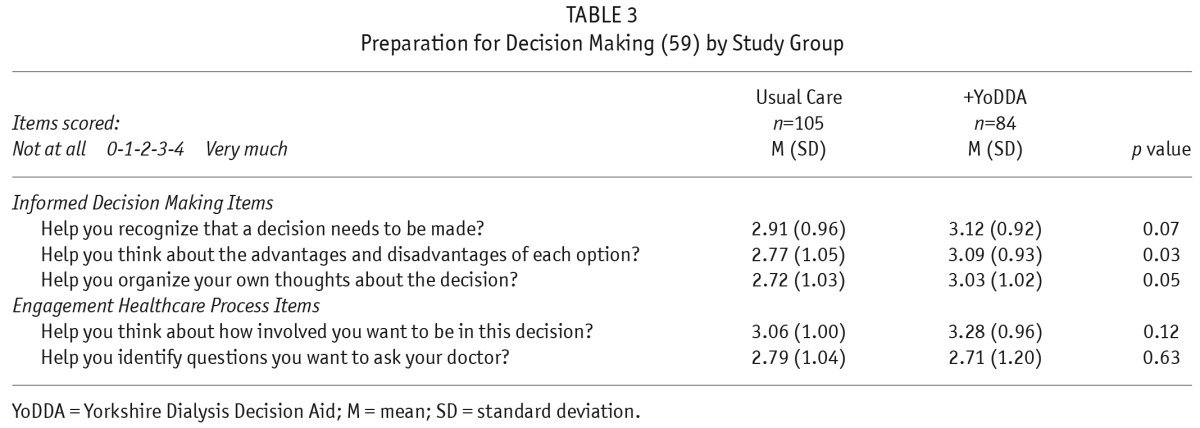
TABLE 4.
Perceived Autonomy and Others' Role in Decision Making by Study Group
Most (96%) patients reported reading YoDDA, 66% more than once; 72% showed it to someone else; 23% wrote notes in it. Patients' comments (from questionnaire and pilot interviews) were positive, focusing on:
Content: “All the information enclosed was useful explicit and informative. I feel the booklet cannot be improved upon. Perfect” (patient 52)
Length/Literacy: ‘I like the fact that it's got a lot more information, you can come and just do sections of it. It's very easy to read … it wouldn't be a chore to go through it’ (patient 20 – pilot)
Balance/Neutral: ‘I think it's good… written in a way that it makes it easier to take in and understand. It is aimed at patients not at people that are treating patients… it gives an overview to everything evenly so you can make a proper informed choice rather than thinking that [it is] sponsored by X’ (patient 21 – pilot)
Medium: ‘So I don't think you would be able to do a computer thing would you really? You best … just stick with this [booklet]…’ (patient 3 – pilot interview)
Utility: ‘Yeah, I think you know, in paper form people can just flip over it they think they know it and they just skim read it and go ‘know that’ (patient 16 – pilot)
Integration into services: “The information was good to use alongside the help from the predialysis team” (patient 94)
Supporting informed decision making: “The description of the different treatments…allowed me to make my treatment decision” (patient 62)
Improvements: “The booklet needs to indicate more where all support for the patient can be found from including benefit support and carers support and how to access this support” (patient 126)
Patients completing consent (C), T1, and T2 questionnaires engaged with making a choice over time (58) (Usual Care, Wilk's Lambda = 0.76, F(2,99) = 15.73, p = 0×00); +YoDDA, Wilk's Lambda = 0.66, F(2,78) = 20.40, p = 0.00). A larger number of +YoDDA patients formed a treatment preference over this time than Usual Care patients (Usual Care M = 4.38; +YoDDA M = 4.82, F(1,187) = 3.12, p = 0.08) (Figure 1) (52).
Feasibility of Evaluating YoDDA Within Usual Practice
Delays by hospital research and development offices, annual leave, and staff changes meant centers did not start capturing data at the same time. Few centers captured all patients referred to predialysis services, only those consenting to the study. Using average, pre-study estimated referral rates to the 6 centers for 7 months (n = 469), a conservative estimated study uptake was Usual Care = 31% and +YoDDA = 28% with by-center variation (Usual Care, 0 – 81%; +YoDDA, 11 – 97%). When captured by centers, +YoDDA study uptake was 45% (58/129), with by-center variation (14 – 49%).
Predialysis staff disseminated YoDDA in ways to suit their delivery of care: adding YoDDA to their usual leaflet pack; adding YoDDA to their leaflet pack and encouraging patients to read it; giving YoDDA as the only leaflet. The predialysis teams distributed 2 versions of YoDDA when pre-stacked in alternate order. Only one participant (2%) reported not receiving YoDDA. Four centers continued handing out YoDDA post study.
Staff did not complete the consultation checklists. Participants did not complete several items in self-report questionnaires, including: knowledge; risk perceptions; balance of information; values toward treatment attributes; Brief Illness Perception Questionnaire (39). Patients' decisional conflict scores (60) were lower than 25, suggesting participants were not experiencing decisional conflict and/or the measure was unable to capture decisional uncertainty in this context (Usual Care M = 13.83, SD = 9.37; +YoDDA M = 13.60 SD = 9.75; F(1,187) = 0.03, p = 0.87).
Discussion
Study participants valued receiving YoDDA when making treatment decisions about established kidney disease, finding it acceptable to read on their own and share it with family members. The pattern of results suggest YoDDA is valid (13–15,16,18,19) providing a more efficacious way of helping patients' assimilate, and reason about, accurate information about all treatment options for their worsening kidney disease in order to make trade-offs between the consequences for their health and lifestyle. In keeping with previous research (5,8,10), patients report being satisfied with their predialysis service and engagement with kidney professionals.
Patients from all 6 centers received YoDDA, with some staff using it proactively to support predialysis education. In a similar way to clinical guidelines for those delivering evidence-based services (1–3), YoDDA provides generic, accurate, balanced, accessible information to support people's thinking about all options and consequences of managing established kidney disease in the context of their lifestyle, as well as ways of engaging with predialysis services including prompts to discuss lifestyle, disease management experiences, and treatment preferences. It is likely patients and staff using YoDDA actively within predialysis consultations will enable personalized information about a patient's medical history and local services to be assimilated alongside informed reasoning between treatment preferences, leading to more effective collaborative care planning (20,22). Fortnum and colleagues (32) found shared decision making training an essential component to address variations in staff practices and enable the integration of decision aids across predialysis services.
We employed a pragmatic design to evaluate YoDDA with patients and staff within predialysis programs, and minimize the research methods' impact on usual care. The socio-demographic and clinical characteristics suggest participants were similar to the region's predialysis patients (24), indicating the YoDDA booklet was acceptable to patients across age, sex, educational, financial, and health state groups. The uptake rate patterns suggest staff decisions about patient eligibility and/or research engagement varied by center, perhaps resulting from differences in service infrastructure and/or staff views toward either research about shared decision making or the utility of a decision aid booklet to patients with worsening health states. These methods relied on self-completion questionnaires, meaning views of non-participants are not captured. It is unclear whether non-participants held similar views to those of participants, or were experiencing more or less uncertainty about their choice, satisfaction with predialysis teams, and usefulness of patient leaflets.
Conclusions
YoDDA helps patients think differently about the problem of choosing between treatments to manage their worsening kidney disease and evaluate them in accordance with their lifestyle. The booklet can be integrated across different predialysis services, and complements usual practice. Providing YoDDA enables services to meet current clinical guidance on informing patients of all treatments for established kidney disease and patient need for more support in dialysis decision making. Integrating YoDDA proactively within predialysis consultations is likely to enhance collaborative care planning about dialysis regimens between patients and predialysis services. Evaluating YoDDA's effectiveness has 2 challenges. First, staff and patient variation in decision aid use is likely to impact differentially on decision making and service quality indicators. Second, current patient-reported measures of informed decision making may not capture reliably patients' outcomes in this clinical context.
Disclosures
Unrestricted projects grants were provided by: Kidney Research UK, in partnership with Baxter Healthcare Ltd, the British Renal Society and Renal Association; The Yorkshire Kidney Research Fund, UK; Informed Medical Decisions Foundation, USA. The funders had no role in the study design, collection, analysis, and interpretation of data, and/or in the writing of the report and decision to submit the paper for publication. The corresponding author confirms she has full access to all data and final responsibility for the publication. The authors have no financial conflicts of interest to declare.
Supplementary Material
Footnotes
Supplemental material available at www.pdiconnect.com
REFERENCES
- 1. National Clinical Guideline Centre – CG182 Chronic kidney disease: early identification and management for adults in primary and secondary care. 2014; National Institute for Health and Clinical Excellence, UK. [PubMed] [Google Scholar]
- 2. National Clinical Guideline Centre – CG125 Peritoneal dialysis: peritoneal dialysis in the treatment of stage 5 chronic kidney disease. 2011; National Institute for Health and Clinical Excellence, UK. [PubMed] [Google Scholar]
- 3. Loud F, Gallagher H, on behalf of The Kidney Alliance Kidney health: delivering excellence. 2013; The Kidney Health Advisory Group, UK. [Google Scholar]
- 4. Brady M, Donoghue D. Back to the future: changes in the dialysis delivery model in the UK. Perit Dial Int 2011; 31:S63–72. [DOI] [PubMed] [Google Scholar]
- 5. Van Biesen W, van der Veer SN, Murphy M, Loblova O, Davies S. Patients' perceptions of information and education for renal replacement therapy: an independent survey by the European Kidney Patients' Federation on information and support on renal replacement therapy. PLOS One 2014; 9:e103914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Prieto-Velasco M, Bagnis CI, Dean J, Goovaerts A, Melander S, Mooney A, et al. Predialysis education in practice: a questionnaire survey of centres with established programmes. BMC Research Notes 2014; 7:730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Winterbottom A, Conner M, Mooney A, Bekker HL. Evaluating the quality of patient leaflets about renal replacement therapy across UK renal units. Nephrol Dial Transplant 2007; 22:2291–6. [DOI] [PubMed] [Google Scholar]
- 8. Winterbottom A, Bekker HL, Conner M, Mooney A. Choosing dialysis modality: decision making in a chronic illness context. Health Expect 2014; 17:710–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ormandy P, Hulme C. Measuring patients' preferences and priorities for information in chronic kidney disease. Information Research 2013; 18: paper 588. [Google Scholar]
- 10. Morton R, Tong A, Howard K, Snelling P, Webster AC. The views of patients and carers in treatment decision making for chronic kidney disease: systematic review and thematic synthesis of qualitative studies. BMJ 2010; 340:c112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Murray MA, Brunier G, Chung JO, Craig LA, Mills C, Thomas A, Stacey D. A systematic review of factors influencing decision-making in adults living with chronic kidney disease. Patient Educ Couns 2009; 76:149–58. [DOI] [PubMed] [Google Scholar]
- 12. Harwood L, Clark AM. Understanding pre-dialysis modality decision-making: a meta-synthesis of qualitative studies. Int J Nurs Stud 2013; 50:109–20. [DOI] [PubMed] [Google Scholar]
- 13. Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Lilleyman J, et al. Informed decision making: an annotated bibliography and systematic review. Health Technol Assess Winchester, UK 1999; 3:1–156. [PubMed] [Google Scholar]
- 14. Bekker HL. The loss of reason in patient decision aid research: do checklists affect the validity of informed choice interventions? Patient Educ Couns 2010; 78:357–64. [DOI] [PubMed] [Google Scholar]
- 15. Bekker HL, Winterbottom AE, Butow P, Dillard A, Feldman-Stewart D, Fowler J, et al. Do personal stories make patient decision aids more effective: a critical review of evidence and theory? BMC Med Inform Decis Mak 2013; 13(Suppl 2):S2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pieterse AH, de Vries M, Stiggelbout AM, Feldman-Stewart D. Theory-informed design of values clarification methods: a cognitive psychological perspective on patient health-related decision making. Soc Sci Med 2013; 77:156–63. [DOI] [PubMed] [Google Scholar]
- 17. Stacey D, Légaré F, Pouliot S, Kryworuchko J, Dunn S. Shared decision making models to inform an interprofessional perspective on decision making: a theory analysis. Patient Educ Couns 2010; 80:164–72. [DOI] [PubMed] [Google Scholar]
- 18. O'Connor A, Edwards E. Chapter 14: The role of decision aids in promoting evidence-based patient choice. In: Edwards A, Elwyn G, eds. Evidence-based patient choice: inevitable of impossible. Oxford, UK: Oxford University Press, 2001(220–242). [Google Scholar]
- 19. Stacey D, Légaré F, Col NF, Bennett CL, Barry MJ, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2014; 1:CD001431. [DOI] [PubMed] [Google Scholar]
- 20. Légaré F, Witteman HO. Shared decision making: examining key elements and barriers to adoption into routine clinical practice. Health Affairs 2013; 2: 2276–84. [DOI] [PubMed] [Google Scholar]
- 21. Elwyn G, Lloyd A, Joseph-Williams N, Elwyn G, Lloyd A, Joseph-Williams N, et al. Option grids: shared decision making made easier. Patient Educ Couns 2013; 90: 207–12. [DOI] [PubMed] [Google Scholar]
- 22. Légaré F, Politi MC, Drolet R, Desroches S, Stacey D, Bekker H, the SDM-CPD team Training health professionals in shared decision-making: an international environmental scan. Patient Educ Couns 2012; 88:159–69. [DOI] [PubMed] [Google Scholar]
- 23. Bekker HL, Winterbottom A, Gavaruzzi T, Mooney A, Wilkie M, Davies S, et al. of the Yorkshire Dialysis Decision Aid (YoDDA) Research Projects The Dialysis Decision Aid Booklet: Making The Right Choices for You. Kidney Research UK: Peterborough, UK: 2015. Available from: https://www.kidneyresearchuk.org/DialysisDecisionAid [Google Scholar]
- 24. Shaw C, Pitcher D, Pruthi R, Fogarty D. UK Renal Registry 16th Annual Report: Chapter 2: UK RRT Prevalence in 2012: National and Centre-specific Analyses. Nephron Clin Pract 2013; 125:29–54. [DOI] [PubMed] [Google Scholar]
- 25. Britton A, McPherson K, McHee M, McPherson K, Sanderson C, Bain C. Choosing between randomised and non-randomised studies: a systematic review. Health Technol Assess 1998; 2(13):1–124. [PubMed] [Google Scholar]
- 26. Elwyn G, Scholl I, Tietbohl C, Mann M, Edwards AGK, Clay C, et al. “Many miles to go …”: a systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med Inform Decis Mak 2013; 13(Suppl 2):S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman, et al. Process evaluation of complex interventions: Medical Research Council guidance. Brit Med J 2015; 350:h1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Coulter A, Stilwell D, Kryworuchko J, Dolan Mullen P, Ng JC, van der Weijden T. A systematic development process for patient decision aids. BMC Med Inform Decis Mak 2013, 13(Suppl 2):S1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fukuhara S, Lopes AA, Bragg-Gresham JL, Kurokawa K, Mapes DL, Akizawa T, et al. held for The Worldwide DOPPS Health-related quality of life among dialysis patients on three continents: the Dialysis Outcomes and Practice Patterns Study. Kidney Int 2003; 64:1903–10. [DOI] [PubMed] [Google Scholar]
- 30. Stein A, Wild J. Kidney failure explained (4th ed.). London, UK: Class Publishing, 2010. [Google Scholar]
- 31. Ameling JM, Auguste P, Ephraim PL, Lewis-Boyer L, DePasquale N, Greer RC, et al. Development of a decision aid to inform patients' and families' renal replacement therapy selection decisions. BMC Med Inform Decis Mak 2012; 12:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fortnum D, Smolonogov T, Walker R, Kairaitis L, Pugh D. ‘My Kidneys, my Choice’ Decision Aid: empowering shared decision making. J Renal Care 2014; 41:81–7. [DOI] [PubMed] [Google Scholar]
- 33. Parfeni M, Nistor I, Covic A. A systematic review regarding the association of illness perception and survival among end-stage renal disease patients. Nephrol Dial Transplant 2013; 28:2407–14. [DOI] [PubMed] [Google Scholar]
- 34. Smith C, Da Silva-Gane M, Chandna S, Warwicker P, Greenwood R, Farrington K. Choosing not to dialyse: evaluation of planned non-dialytic management in a cohort of patients with end-stage renal failure. Nephron Clin Pract 2003; 95:c40–6. [DOI] [PubMed] [Google Scholar]
- 35. Brown EA, Johansson L, Farrington K, Gallagher H, Sensky T, Gordon F, et al. Broadening Options for Long-term Dialysis in the Elderly (BOLDE): differences in quality of life on peritoneal dialysis compared to haemo-dialysis for older patients. Nephrol Dial Transplant 2010; 25:3755–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Liem YS, Bosch JL, Hunink MGM. Preference-based quality of life of patients on renal replacement therapy: a systematic review and meta-analysis. Value Health 2008; 11:733–41. [DOI] [PubMed] [Google Scholar]
- 37. Griva K, Jayasena D, Davenport A, Harrison M, Newman SP. Illness and treatment cognitions and health related quality of life in end stage renal disease. Br J Health Psychol 2009; 14:17–34. [DOI] [PubMed] [Google Scholar]
- 38. Winterbottom AE, Bekker HL, Conner M, Mooney A. Patient stories about their dialysis experience biases others' choices regardless of doctor's advice: an experimental study. Nephrol Dial Transplant 2010; 27:325–31. [DOI] [PubMed] [Google Scholar]
- 39. Von Winterfeldt D, Edwards W. Decision analysis and behavioural research. Cambridge, UK: Cambridge University Press, 1993. [Google Scholar]
- 40. Janis IL, Mann L. Decision making: a psychological analysis of conflict, choice and commitment. New York, USA: The Free Press, 1977. [Google Scholar]
- 41. Larrick RP. Chapter 16 – Debiasing. In: Koehler DJ, Harvey N, eds. Blackwell handbook of judgment and decision making. Malden, MA: Blackwell Publishing; 2004. [Google Scholar]
- 42. Ley P. Communicating with patients: improving communication, satisfaction and compliance. London, UK: Croom-Helm, 1988. [Google Scholar]
- 43. Kessler S. Psychological Aspects of Genetic Counseling. VII. Thoughts on Directiveness. J Genet Couns 1992; 1:9–17. [DOI] [PubMed] [Google Scholar]
- 44. Flesch R. A new readability yardstick. J Appl Psychol 1948; 32:221–33. Available from https://readability-score.com [DOI] [PubMed] [Google Scholar]
- 45. Abhyankar P, Volk RJ, Blumenthal-Barby J, Bravo P, Buchholz A, Ozanne E, et al. Balancing the presentation of information and options in patient decision aids: an updated review. BMC Med Inform Decis Mak 2013; 13(2):S2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Abhyankar P, Summers BA, Velikova G, Bekker HL. Framing options as choice or opportunity: does the frame influence decisions? Med Decis Making 2014; 34:567–82. [DOI] [PubMed] [Google Scholar]
- 47. Trevena LJ, Zikmund-Fisher BJ, Edwards A, Gaissmaier W, Galesic M, Han PKJ, et al. Presenting quantitative information about decision outcomes: a risk communication primer for patient decision aid developers. BMC Med Inform Decis Mak 2013; 13(Suppl 2):S2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Conner M, Norman P. Chapter 1 – Predicting health behaviour: a social cognition approach. In: Connor M, Norman P, eds. Predicting Health Behaviour: Research and Practice with Social Cognition Models. Berkshire, UK: Open University Press, 2005. [Google Scholar]
- 49. Leventhal A, Benyamini Y, Brownlee S, Diefenbach M, Leventhal E, Patrick-Miller L, et al. Chapter 1 – Illness representations: theoretical foundations. In: Petrie KJ, Weinman JA, eds. Perceptions of Health and Illness. Current Research and Applications. Amsterdam, The Netherlands: Harwood Academic Publishers, 1997. [Google Scholar]
- 50. Horne R. Chapter 5 – Representations of medication and treatment: advances in theory and measurement. In: Petrie KJ, Weinman JA, eds. Perceptions of Health and Illness. Current Research and Applications. Amsterdam, The Netherlands: Harwood Academic Publishers, 1997. [Google Scholar]
- 51. Tabachnick BG, Fidell LS. Using Multivariate Statistics, 6th ed. Boston: Allyn and Bacon, 2013. [Google Scholar]
- 52. Breckenridge K, Bekker HL, van der Veer SN, Gibbons E, Abbott D, Briançon S, et al. NDT Perspectives – How to routinely collect data on patient-reported outcome and experience measures in renal registries in Europe: an expert consensus meeting. Nephrol Dial Transplant 2015. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bekker HL, Thornton JG, Hewison J. Applying decision analysis to facilitate informed decision making about prenatal diagnosis for Down's syndrome: a randomised controlled trial. Prenat Diagn 2004; 24:265–75. [DOI] [PubMed] [Google Scholar]
- 54. Bekker HL, Hewison J, Thornton JG. Understanding why decision aids work: linking process and outcome. Patient Educ Couns 2003; 50:323–9. [DOI] [PubMed] [Google Scholar]
- 55. Wong SSM, Thornton JG, Gbolade B, Bekker HL. A randomised controlled trial of a decision aid leaflet to facilitate women's choice between pregnancy termination methods. BJOG 2006; 113:688–95. [DOI] [PubMed] [Google Scholar]
- 56. Devlin N, Krabbe P. The development of new research methods for the valuation of EQ-5D-5L. Eur J Health Economics 2013; 14:S1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Broadbent E, Petrie K, Main J, Weinman J. The Brief Illness Perception Questionnaire. J Psychosom Res 2006; 60:631–7. [DOI] [PubMed] [Google Scholar]
- 58. O'Connor AM. User Manual – Stage of Decision Making [document on the internet]. Ottawa: Ottawa Hospital Research Institute; 2000. [Modified 2003: http://decisionaid.ohri.ca/docs/develop/User_manuals/UM_stage_decision_making.pdf;accessed19/11/2013]. [Google Scholar]
- 59. Graham ID, O'Connor AM. User Manual – Preparation for Decision Making Scale [document on the internet]. Ottawa: Ottawa Hospital Research Institute; 1995. [updated 2010; http://decisionaid.ohri.ca/docs/develop/User_manuals/UM_PrepDM.pdf;accessed19/11/2013]. [Google Scholar]
- 60. O'Connor AM. User Manual – Decisional Conflict Scale [document on the internet]. Ottawa: Ottawa Hospital Research Institute; 1993. [updated 2010; http://decisionaid.ohri.ca/docs/develop/User_manuals/UM_decisional_conflict.pdf; accessed 19/11/2013]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.