Abstract
Purpose
To evaluate the use of high-dose radiotherapy using carbon ions (C12) on non-adenoid cystic malignant salivary gland tumors (MSGT).
Patients and methods
Between 2009 and 2013, patients with biopsy-proven non-ACC MSGT histologies of the head and neck received a combined regimen of IMRT plus C12 boost. Treatment toxicity (CTC v3), response (RECIST 1.1), control and survival rates were retrospectively analyzed.
Results
40 patients with pathologically confirmed non-ACC MSGT (T4: 45 %; N+: 40 %; gross residual: 58 %; mucoepidermoid carcinoma (MEC): 45 %; adenocarcinoma: 20 %) were treated with a median of 74 GyE (80 Gy BED). Chemoradiation was given in 5 patients with MEC. Grade III acute toxicity was observed in up to 15 % (mucositis, dermatitis, dysphagia), no higher-grade late toxicity occurred to date. At a follow-up of 25.5 months, LC, and PFS at 2 and 3 years are 81.5 % (LC) and 66.8 % (PFS), OS at 2 and 3 years is 83.6 % and 72.8 %. Most frequent site of disease progression was distant metastasis. Histologic subtype correlated with LC and PFS. Resection status (gross vs microscopic disease) had no significant effect on LC, PFS, or OS.
Conclusion
The treatment is well tolerated, no higher grade late effects were observed. Considering the negative pre-selection, LC, PFS and OS are promising. While histology and site of origin significantly influenced control and survival rates, resection status did not, potentially due to the effect of dose escalation.
Electronic supplementary material
The online version of this article (doi:10.1186/s13014-016-0657-z) contains supplementary material, which is available to authorized users.
Background
Malignant salivary gland tumors (MSGTs) are a heterogenous group of malignancies with more than 20 histological subtypes of different biological and clinical behavior [1].
While adenoid cystic carcinomas (ACC) generally show a very indolent course of disease despite frequent distant metastases [2], this is not the case for other high-grade MSGTs. These may exhibit aggressive local growth patterns as well as early distant disease [3]. Retrospective analyses of larger patient cohorts could establish the use of postoperative radiotherapy and dose-dependence of locoregional control in MSGTs [4–7]. Particle therapy as either neutron or carbon ion therapy has been evaluated in MSGT with promising control rates [8–10]. However, most of these series include a significant proportion of patients with ACC whose natural history of disease and biological behavior is distinctly different from non-ACC histologies. We therefore present our experience with a combined regimen of IMRT plus carbon ion boost in the treatment of non-ACC MSGTs of the head and neck.
Patients and methods
Immobilization, target volume definition, and treatment planning
Patients were immobilized with custom-made thermoplastic head masks including shoulder fixation (HeadStep®). Target delineation was based on contrast-enhanced CT and MRI scans. Two target volumes were outlined: CTV1 included the macroscopic tumor and tumor bed, the extended target volume (CTV2) included the CTV1 and typical pathways of spread as well as ispilateral nodal levels (II and III). If the primary tumor was located at or crossing midline, bilateral nodes were included. A 3 mm margin was added to the CTVs to generate PTVs. The PTV margin was reduced at sites were it would extend into critical structures (i.e. optic pathways), no margin was added to organs at risk.
C12 plans were created using Siemens TPS© which incorporates biological plan optimization according to the local effect model (LEM) [11] to account for increased biological effectiveness. Hypofractionation effects are not included in this model; doses need to be converted according to the standard LQ model to yield Gy BED.
IMRT plans were generated either using MRC KonRad© on the Siemens Syngo© platform or tomotherapy©.
Dose prescription and organs at risk
Both C12 and photon doses were prescribed to the median PTV, which is covered by the 95 % prescription isodose. Normal tissue constraints according to Emami et al. [12] were adhered to. Doses were reduced beyond theses values to as low as reasonably achievable without compromising PTV coverage. Mean dose to at least one parotid gland was kept below 26 Gy.
Patients received a sequential C12 boost in 3 GyE per fraction followed by normofractionated photon IMRT. Most patients received IMRT plus up-front C12 boost (median C12 dose: 23.95 GyE, median IMRT dose: 50 Gy). Two patients underwent C12 only to a total dose of 66 GyE.
Treatment
C12 treatment was applied using intensity-controlled raster-scanned technique (active beam application) [13] using one to five non-coplanar treatment beams under daily image guidance with orthogonal x-rays and 6 degrees of freedom (DOF) position correction [14]. C12 treatment was routinely available at the Heidelberg Ion Beam Therapy Centre (HIT) in 5 to 6 fractions per week.
IMRT treatments were carried out in step and shoot technique using a 6 MV linear accelerator or tomotherapy unit under regular image guidance with MV cone-beam CT.
Staging and follow-up
Initial staging included full clinical examination with panendoscopy, local imaging (contrast-enhanced CT/MRI), and chest CT. Patients were followed up 6-8 weeks post completion of treatment, 3 months thereafter and then in 6 monthly intervals with MRI of the head and neck. Yearly chest CTs were recommended to exclude distant disease. In addition, patients were encouraged to regular visits at their referring surgeon incl. full ENT examinations.
Evaluation
Medical records of all patients treated for pathologically confirmed MSGT between 2009 and 2013 were retrieved and analyzed. Acute and late toxicities were scored according to CTCAE v.3. Tumor staging was performed on initial diagnostic scans to the most recent TNM classification [15], response assessment on follow-up MRI scans according to RECIST 1.1 [16]. Both were carried out by this institution’s MSGT experts.
Time to event data was calculated from radiotherapy treatment start to last follow-up or death according to the Kaplan-Meier method. Loco-regional control (LC) was defined as the absence of further tumor growth following radiotherapy or the absence of further tumor growth following best response of the treated lesion(s). Progression-free survival (PFS) was defined as the absence of locoregional or distant failure or death of any cause. Kaplan-Meier curves were compared using log-rank tests; statistic analyses were performed with the Addinsoft© xlstat life package 2015.
All patients gave written informed consent prior to initiation of treatment, the analysis is in accordance with the current declaration of Helsinki and approved by the institutional review board.
Ethics and approval
The study was reviewed and approved by the local institutional review board (S-141/2014). The analysis is in accordance with the current declaration of Helsinki.
Results
Between 11/2009 and 05/2013, 291 patients with MSGTs received carbon ions as part of their primary treatment. 40 patients had pathologically confirmed MSGT other than ACC. Median age was 60 years [range: 35-80 a]. 31 patients underwent surgery prior to radiotherapy, 23 patients had gross residual/inoperable (58 %) and 17 patients had microscopic residual (43 %) disease at RT treatment planning. 7 patients received treatment for locally recurrent MSGT but had not undergone prior radiotherapy. Most common histology was mucoepidermoid carcinoma in 18 patients (45 %) and adenocarcinoma in 8 patients (20 %). Most common sites of origin were parotid gland (50 %) and submandibular gland (13 %). 18 patients (45 %) had T4 stage tumors, 16 patients (40 %) showed nodal metastases.
38 patients received combined radiotherapy with IMRT plus up-front C12 boost to a median dose of 23.95 GyE C12 and 50 Gy IMRT corresponding to a median total dose of 74 GyE and approximately 80 Gy BED. Two patients underwent C12 only to a total dose of 66 GyE for very small primary tumors. With a median CTV1 (C12) of 120 ml and CTV2 (IMRT) of 424 ml, treatment volumes were comparatively extensive (Table 1: patient baseline characteristics).
Table 1.
Patient baseline characteristics
| Patient baseline characteristics | ||||
|---|---|---|---|---|
| All | ||||
| pts | % | |||
| histology | mucoepidermoid carcinoma | 18 | 45 | |
| adeno carcinoma | 8 | 20 | ||
| acinic cell carcinoma | 3 | 8 | ||
| squamous cell carcinoma | 2 | 5 | ||
| salivary duct carcinoma | 2 | 5 | ||
| NOS | 2 | 5 | ||
| basal cell-adeno carcinoma | 2 | 5 | ||
| adenosquamous carcinoma | 1 | 3 | ||
| myoepithelial carcinoma | 1 | 3 | ||
| basaloid carcinoma | 1 | 3 | ||
| stage | T 1 | 3 | 8 | |
| T 2 | 5 | 13 | ||
| T 3 | 13 | 33 | ||
| T 4a | 10 | 25 | ||
| T 4b | 7 | 18 | ||
| T 4c | 1 | 3 | ||
| unknown | 1 | 3 | ||
| N+ | 16 | 40 | ||
| M1 | 3 | 8 | ||
| treatment for recurrent disease | 7 | 18 | ||
| site | parotid gland | 20 | 50 | |
| submandibular gland | 5 | 13 | ||
| oropharynx | 3 | 8 | ||
| maxilla | 2 | 5 | ||
| palate | 2 | 5 | ||
| lacrimal gland | 2 | 5 | ||
| paranasal sinus | 2 | 5 | ||
| petrous bone | 2 | 5 | ||
| middle ear | 1 | 3 | ||
| nasopharynx | 1 | 3 | ||
| age | median in years [range] | 60 | 35-80 | |
| follow-up | all, median in months [range] | 25.5 | 2.5-58.4 | |
| alive, median in months [range] | 27.3 | 3-58.4 | ||
| target volume | CTV1 (boost) in ml | 120 | 34-564 | |
| CTV2 (extended target volume) in ml | 424 | 105-1538 | ||
| dose | C12 in GyE [range] | 23.95 | 17.4-24.4 | 2 pts: C12 only with 66 GyE |
| IMRT in Gy [range] | 50 | 42-56.4 | ||
| total in GyE [range] | 74 | 50.4-74.8 | ||
Five patients with mucoepidermoid carcinoma received combined chemoradiation with cisplatin 40 mg/m sq weekly following interdisciplinary discussion of these specific cases.
Follow-up is 25.5 months [range: 2.5-58.4 months] and 27.3 months [range: 3-58.4 months] for patients alive. 8 patients have deceased due to disease progression.
As expected, mucositis and dermatitis were the most prevalent acute radiation effects. Despite 5 patients undergoing combined chemoradiation, higher-grade mucositis was observed in only 15 % (6 patients). 18 (45 %) patients developed weight loss, however, only 20 % of patients reported dysphagia grade II or III. Trismus was present in 3 patients, in all of those following initial surgery. The most commonly reported late effect was xerostomia grade I (30 %), no higher grade late effects were observed to date. 5 patients developed hearing impairment (13 %) and sensory impairment (13 %), 3 patients rhinitis sicca symptoms (8 %). One patient developed tissue necrosis in the nasopharynx following combined chemoradiation for mucoepidermiod carcinoma of the nasopharynx. Fortunately, this did not result in any late sequelae or cranial nerve impairment (Additional file 1: Table S2: treatment toxicity).
According to RECIST, 3 patients (8 %) developed complete remissions (CR) 6 weeks post completion of radiotherapy, 10 patients (25 %) partial remissions (PR), 9 patients (23 %) remained stable (SD). In the 16 patients with microscopic residual disease, and in 2 patients deceased prior to first follow-up, response according to RECIST was not assessable. Best response was CR in 7 patients (18 %), PR in 11 patients (28 %), and SD in 4 patients (10 %). Figure 1 shows the dose distribution of C12 plan (24 GyE) for a patient with mucoepidermoid carcinoma of the paranasal sinus, Fig. 2a and b show the initial MRI scan for treatment planning and Fig. 3a and b observed treatment response with a very good partial remission 6 weeks post completion of RT.
Fig. 1.
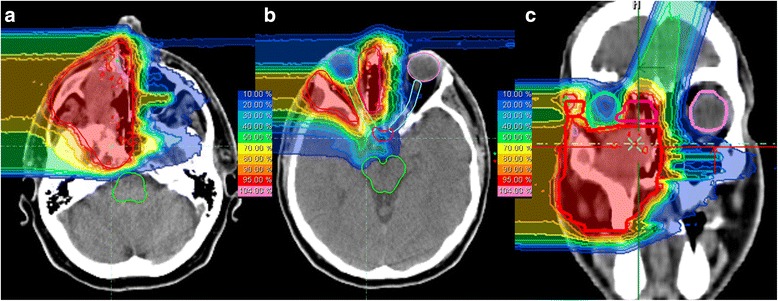
C12 treatment plan of a patient with mucoepidermoid carcinoma of the paranasal sinus undergoing combined IMRT plus C12 boost. C12 plan based on 2 beams, intensity-controlled C12 therapy (ICCT) to 24 GyE in 3 GyE per fraction. a and b: axial; c: coronal distribution
Fig. 2.
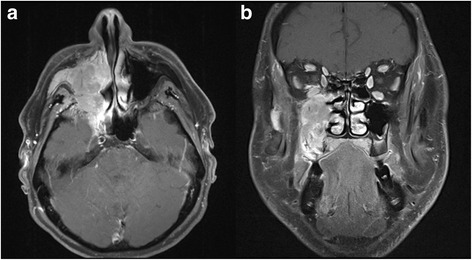
Initial, contrast-enhanced T1-weighted and fat-saturated MRI scan of the patient with mucoepidermoid carcinoma of the paranasal sinus prior to initiation of radiotherapy (a: axial; b: coronal)
Fig. 3.
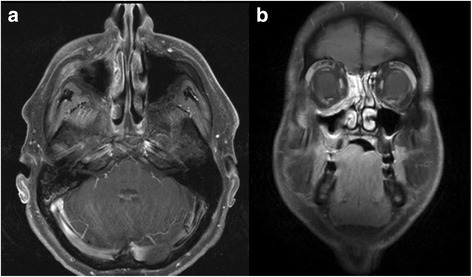
Follow-up contrast-enhanced T1-weighted and fat-saturated MRI scan of the patient with mucoepidermoid carcinoma of the paranasal sinus 6 weeks post completion of radiotherapy (a: axial; b: coronal)
LC, and PFS at 2 and 3 years are 81.5 % (LC) and 66.8 % (PFS), OS at 2 and 3 years is 83.6 % and 72.8 % (Fig. 4).
Fig. 4.
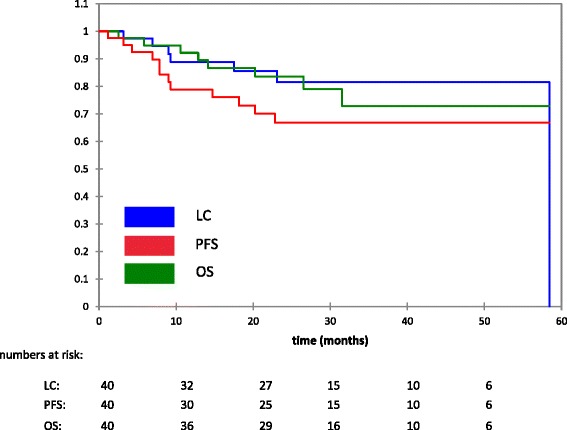
Locoregional control (LC), progression-free survival (PFS), overall survival (OS)
7 patients developed locoregionally recurrent disease: 3 patients in field, 2 patients at the field edge/gradient where the optic nerve was spared, and 2 patients developed nodal recurrences. 11 patients showed distant disease progression, most commonly as bony (7 pts) and lung (5 pts) metastases, less frequently as soft tissue (2 pts), skin (2 pts), and liver (1 pt) metastases. Further treatment included palliative chemotherapy (6 pts), palliative RT of bone metastases (5 pts), re-irradiation (3 pts), and salvage surgery (1 pt).
On univariate analysis, LC correlated significantly with histological subtype (p < 0.001). Figure 5 shows LC according to the most common histologies with MEC yielding the least favorable LC. Histology did influence PFS (p = 0.004) (Additional file 2: Figure S1) and distant control (p = 0.003), however, no influence on OS could be detected. Acinic cell carcinoma had the most and adenocarcinoma the least favorable outcome regarding PFS and distant control. While site of origin did not correlate with LC (p = 0.237), it did influence PFS (p = 0.021) (Additional file 3: Figure S2), distant control (p = 0.053), and OS (p = 0.010) with submandibular gland as the least favorable site (Additional file 4: Figure S3). Resection status had no demonstrable effect on PFS, distant control, or OS. Patients with gross residual disease tended to have lower LC, however, this was not statistically significant in this analysis.
Fig. 5.
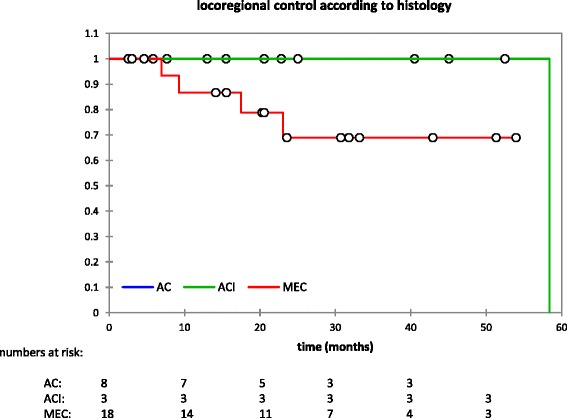
LC according to histologic subtype. AC: adenocarcinoma; ACI: acinic cell carcinoma; MEC: mucoepidermoid carcinoma. Note only the most frequent subtypes are shown to improve visibility
Discussion
While dose escalation using high-LET radiotherapy is seen as beneficial in the treatment of MSGTs and especially ACC of the head and neck [9, 17], the situation is less clear for non-ACC MSGT histologies.
In contrast to ACC, many high-grade non-ACC histologies such as mucoepidermoid carcinoma and adenocarcinoma are characterized by a very aggressive course of disease, frequent nodal and early distant metastases [2, 3]. Adjuvant radiotherapy at doses exceeding 60 Gy is recommended in patients with risk factors such as advanced T-stage, nodal metastases, perineural spread, involved margins, or high-grade histology [2–6].
In our cohort, all patients had at least one of these risk factors: all patients had involved margins and more than 50 % gross residual disease, most patients had advanced tumor stages and 40 % cervical nodal metastases, hence representing a very unfavorable pre-selection [4, 8, 18–21] underrepresented in most other series.
Often, outcome is reported for all MSGTs [5, 7–9] and rarely according to histology [2].
MEC and AC were the most common histologic subtypes in our cohort, also representing two MSGT histologies with the highest potential systemic activity [2, 20–22]. Indeed, most common site of relapse were distant metastases (28 %) which supports findings of Loh, Salgado, Chung and Garden [6, 22–24]. Information on LC in this specific, subset of patients with advanced tumor stages, residual disease and unfavorable histology is rare:
In a large analysis of 207 patients with MSGTs of the major salivary glands treated between 1960 and 2004 at the MD Anderson Cancer Center, LC in node positive patients, advanced T-stages, positive margin or high-grade histology is between 60 and 70 % at 5 years [6]. The MSKCC experience of 98 patients with MSGT of the minor salivary glands treated between 1990 and 2010 yields LC rates of around 80 % at 5 years and significantly inferior results for MECs and adenocarcinoma [22]. LC at 3 years was around 80 % in 54 patients treated with postoperative radiotherapy in the Standford series where advanced T-stage, nodal involvement, and MEC histology was associated with worse outcome [21]. In view of these tumors’ relative radioresistance, neutron radiotherapy has been employed in order to improve control rates. Already in the late 1980s, Griffin and Laramore could show superior LC rates for neutron radiotherapy in the randomized MRC trial albeit with low patient numbers (32 pts) and considerable late toxicity [9, 25]. Stannard et al published their experience in the largest cohort of patients treated with neutrons for MSGTs so far. They found LC rates between 35 % and 50 % for patients with T4 or large tumors, high-grade histology, and nodal metastases [8]. A LC of 72 % at 3 years was reported by Tsuji et al from the NIRS carbon ion center in 26 patients with advanced adenocarcinoma of the head and neck [10].
Despite negative prognostic factors in all our patients, our experience with LC rates of more than 80 % at 2 and 3 years therefore compares favorably with previously published experience.
Inferior results regarding LC and PFS for MEC and adenocarcinoma in our series is supported by other observations and not unexpected [2, 4, 20–22].
Site of origin did influence PFS and OS in our cohort on univariate analysis as reported by other investigators [2, 4, 21, 26]. However, in contrast to all other previously published experience [2, 4, 5, 7, 21], resection status (gross residual tumors vs microscopically involved margins) had no significant influence on LC, which may be an effect of dose escalation to approximately 80 Gy BED.
OS in this cohort is 72.8 % at 3 years and is in line with experience in larger series [7, 8, 24, 27] and the SEER based analysis [20]. It is slightly lower than in the cohort published by Garden [6] which may be due to the high percentage of ACC patients in their series.
As expected, mucositis and dermatitis were the most prevalent acute radiation effects. Despite 5 patients undergoing combined chemoradiation, higher-grade mucositis was observed in only 15 % (6 patients).
No high-grade late toxicity was observed in this cohort so far. Observed toxicity such as hearing impairment and sicca symptoms correlate well with site and extent of treatment field. As described, one patient developed normal tissue necrosis in the high dose area in the nasopharynx following combined chemoradiation. Unfortunately, she still developed an in-field recurrence but does not show any further late toxicity or sequelae. In their retrospective analysis of 98 patients with minor salivary gland malignancies, Salgado et al describe acute and late toxicities including several high-grade late effects (dysphagia, xerostomia, hearing loss) but also 2 out of 98 cases of radiotherapy necrosis, which corresponds to the percentage observed in our cohort [22]. Ten percent of patients developed higher-grade toxicities in the Florida cohort published by Mendenhall et al [7]. The neutron experience reports severe late toxicities in 9 % of patients [8] and significantly higher than in comparable photon treatments [9]. Despite large treatment fields and chemoradiation in 20 % of patients, treatment with IMRT plus carbon ion boost was very well tolerated. Higher-grade acute effects such as mucositis and dysphagia were rare and rates corresponded well to our previously published experience [28, 29]. No temporal lobe changes were observed. In view of the comparatively short follow-up of our patients (25 months), further monitoring is warranted.
No report exists as to observed treatment response of non-ACC of the head and neck so far. Early and best response rates are in line with our previously published experience in MSGT [29]. Still, 3 patients developed in-field recurrences, 2 patients recurrences within the dose gradient towards the optic system. While further dose escalation should be approached with caution, recurrences within the gradient underline the necessity to clearly discuss the issue of sparing specific structures and its potential consequences with the patient.
Chemoradiation in MSGTs is still discussed controversially. There is only limited data on the use of concurrent platin-containing chemoradiation and patient numbers are small [30–34]. It is still unclear whether the addition of chemotherapy to high-dose irradiation does prevent early systemic metastases and even less clear whether the addition of chemotherapy to particle treatment has an added benefit. Once recruitment of the RTOG 1008 trial is completed and results are available [35], we may gain more insight into these issues for photon radiotherapy. In particle therapy however, we do believe these questions should be addressed in a prospective clinical trial.
Conclusion
Overall acute and late treatment toxicity of the combination of IMRT plus C12 boost remains consistently low, no higher grade late toxicities were observed. LC, PFS and OS are promising, especially considering the negative preselection of patients with advanced disease and gross residual tumors. While histology and site of origin significantly influenced control and survival rates, resection status did not potentially due to the effect of dose escalation, which therefore appears to be beneficial also in non-ACC histologies.
Previous presentation
Intermediate results were presented as poster at DEGRO meeting in Düsseldorf, in 2014.
Ethics approval
This study was reviewed and approved by the local institutional review board (S-141/2014).
Acknowledgements
We acknowledge financial support by Deutsche Forschungsgemeinschaft (DFG) and Ruprecht-Karls-Universität Heidelberg within the funding programme Open Access Publishing.
Additional files
Treatment-related acute and late toxicity (XLSX 32 kb)
PFS according to histologic subtype. AC: adenocarcinoma; ACI: acinic cell carcinoma; MEC: mucoepidermoid carcinoma. Note only the most frequent subtypes are shown to improve visibility (ODP 16 kb)
PFS according to site of origin (ODP 16 kb)
OS according to site of origin (ODP 16 kb)
LC according to resection status (ODP 17 kb)
Footnotes
Competing interests
JD is CEO of Heidelberg Ion Beam Therapy Centre. All other authors declare they have no competing interests.
Authors’ contributions
ADJ and MU treated the patients, ADJ performed data acquisition and statistical analysis. NC was responsible for treatment plan generation and review. Carbon ion treatment followed interdisciplinary discussion of benefits with ADJ, PAF, KF, JK, and JD. PAF, KF, and JK participated in statistical analysis and critically reviewed the data. ADJ and MP drafted the manuscript and all authors revised it critically. All authors read and approved the final manuscript.
References
- 1.World Health Organization Classification of Tumours. Pathology and genetics, Head and Neck Tumours. Barnes L, Eveson JW, Reichart P, Sidransky D (editors). Lyon: IARC press 2005.
- 2.Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2807 patients. Head Neck Surg. 1986;8:177–84. doi: 10.1002/hed.2890080309. [DOI] [PubMed] [Google Scholar]
- 3.Adelstein DJ, Koyfman SA, El-Naggar AK, Hanna EY. Biology and management of salivary gland cancers. Semin Radiat Oncol. 2012;22:245–53. doi: 10.1016/j.semradonc.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 4.Terhaard CHJ, Lubsen H, Van der Tweel I, Hilgers FJM, Eijkenboom WMH, Marres HAM, Tjho-Heslinga RE, de Jong JM, Roodenburg JL, Dutch Head and Neck Oncology Cooperative Group Salivary gland carcinoma: independent prognostic factors for locoregional control, distant metastases, and overall survival: results of the Dutch head and neck oncology cooperative group. Head Neck. 2004;26:681–92. doi: 10.1002/hed.10400. [DOI] [PubMed] [Google Scholar]
- 5.Chen AM, Bucci MK, Weinberg V, Garcia J, Quivey JM, Schechter NR, Phillips TL, Fu KK, Eisele DW. Adenoid cystic carcinoma of the head and neck treated by surgery with or without postoperative radiation therapy: prognostic features of recurrence. Int J Radiat Oncol Biol Phys. 2006;66:152–9. doi: 10.1016/j.ijrobp.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Garden AS, Weber RS, Ang KK, Morrison WH, Matre J, Peters LJ. Postoperative radiation therapy for malignant tumors of minor salivary glands. Outcome and patterns of failure. Cancer. 1994;73:2563–9. doi: 10.1002/1097-0142(19940515)73:10<2563::AID-CNCR2820731018>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 7.Mendenhall WM, Morris CG, Amdur RJ, Werning JW, Villaret DB. Radiotherapy alone or combined with surgery for salivary gland carcinoma. Cancer. 2005;103:2544–50. doi: 10.1002/cncr.21083. [DOI] [PubMed] [Google Scholar]
- 8.Stannard C, Vernimmen F, Carrara H, Jones D, Fredericks S, Hille J, de Kock E. Malignant salivary gland tumours: can fast neutron therapy results point the way to carbon ion therapy? Radiother Oncol. 2013;109:262–268. doi: 10.1016/j.radonc.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Laramore GE, Krall JM, Griffin TW, Duncan W, Richter MP, Saroja KR, Maor MH, Davis LW. Neutron versus photon irradiation for unresectable salivary gland tumors: final report of an RTOG-MRC randomized clinical trial. Int J Radiat Oncol Biol Phys. 1993;27:235–240. doi: 10.1016/0360-3016(93)90233-L. [DOI] [PubMed] [Google Scholar]
- 10.Tsujii H, Mizoe J, Kamada T, Baba M, Tsuji H, Kato H, Kato S, Yamada S, Yasuda S, Ohno T, Yanagi T, Imai R, Kagei K, Kato H, Hara R, Hasegawa A, Nakajima M, Sugane N, Tamaki N, Takagi R, Kandatsu S, Yoshikawa K, Kishimoto R, Miyamoto T. Clinical Results of Carbon Ion Radiotherapy at NIRS. J Radiat Res. 2007;48(Suppl A):A1–A13. doi: 10.1269/jrr.48.A1. [DOI] [PubMed] [Google Scholar]
- 11.Krämer M, Scholz M. Treatment planning for heavy-ion radiotherapy:calculation and optimization of biologically effective dose. Phys Med Biol. 2000;45:3319–3330. doi: 10.1088/0031-9155/45/11/314. [DOI] [PubMed] [Google Scholar]
- 12.Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, Shank B, Solin LJ, Wesson M. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1991;21:109–22. doi: 10.1016/0360-3016(91)90171-Y. [DOI] [PubMed] [Google Scholar]
- 13.Haberer T, Becher W, Schardt D, Kraft G. Magnetic scanning system for heavy ion therapy. Nucl Instr Meth Phys Res. 1993;330:296–305. doi: 10.1016/0168-9002(93)91335-K. [DOI] [Google Scholar]
- 14.Jensen AD, Winter M, Kuhn SP, Debus J, Nairz O, Münter MW. Robotic-based carbon ion therapy and patient positioning in 6 degrees of freedom: setup accuracy of two standard immobilization devices used in carbon ion therapy and IMRT. Radiat Oncol. 2012;7:51. doi: 10.1186/1748-717X-7-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sobin L, Gospodarowicz M, Wittekind C, editors. TNM Classification of malignant tumors. 7. Hoboken, NJ: Wiley; 2009. [Google Scholar]
- 16.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45:228–47. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 17.Douglas JG, Koh WJ, Austin-Seymour M, Laramore GE. Treatment of salivary gland neoplasms with fast neutron radiotherapy. Arch Otolaryngol Head Neck Surg. 2003;129:944–8. doi: 10.1001/archotol.129.9.944. [DOI] [PubMed] [Google Scholar]
- 18.Lau VH, Aouad R, Farwell DG, Donald PJ, Chen AM. Patterns of nodal involvement for clinically N0 salivary gland carcinoma: refining the role of elective neck irradiation. Head Neck. 2014;36:1435–9. doi: 10.1002/hed.23392. [DOI] [PubMed] [Google Scholar]
- 19.Chen MM, Roman SA, Sosa JA, Judson BL. Histologic grade as prognostic indicator for mucoepidermoid carcinoma: a population-level analysis of 2400 patients. Head Neck. 2014;36:158–63. doi: 10.1002/hed.23256. [DOI] [PubMed] [Google Scholar]
- 20.Lloyd S, Yu JB, Ross DA, Wilson LD, Decker RH. A prognostic index for predicting lymph node metastasis in minor salivary gland cancer. Int J Radiat Oncol Biol Phys. 2010;76:169–75. doi: 10.1016/j.ijrobp.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 21.Le QT, Birdwell S, Terris DJ, Gabalski EC, Varghese A, Fee W, Jr, Goffinet DR. Postoperative irradiation of minor salivary gland malignancies of the head and neck. Radiother Oncol. 1999;52:165–71. doi: 10.1016/S0167-8140(99)00084-5. [DOI] [PubMed] [Google Scholar]
- 22.Salgado LR, Spratt DE, Riaz N, Romesser PB, Wolden S, Rao S, Chin C, Hong JC, Wong R, Lee NY. Radiation therapy in the treatment of minor salivary gland tumors. Am J Clin Oncol. 2014;37:492–7. doi: 10.1097/COC.0b013e31827e54e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loh KS, Barker E, Bruch G, O'Sullivan B, Brown DH, Goldstein DP, Gilbert RW, Gullane PJ, Irish JC. Prognostic factors in malignancy of the minor salivary glands. Head Neck. 2009;31:58–63. doi: 10.1002/hed.20924. [DOI] [PubMed] [Google Scholar]
- 24.Chung MP, Tang C, Chan C, Hara WY, Loo BW, Jr, Kaplan MJ, Fischbein N, Le QT, Chang DT. Radiotherapy for nonadenoid cystic carcinomas of major salivary glands. Am J Otolaryngol. 2013;34:425–30. doi: 10.1016/j.amjoto.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Griffin TW, Pajak TF, Laramore GE, Duncan W, Richter MP, Hendrickson FR, Maor MH. Neutron vs photon irradiation of inoperable salivary gland tumors: results of an RTOG-MRC cooperative randomized study. Int J Radiat Oncol Biol Phys. 1988;15:1085–1090. doi: 10.1016/0360-3016(88)90188-5. [DOI] [PubMed] [Google Scholar]
- 26.Sadeghi A, Tran LM, Mark R, Sidrys J, Parker RG. Minor salivary gland tumors of the head and neck: treatment strategies and prognosis. Am J Clin Oncol. 1993;16:3–8. doi: 10.1097/00000421-199302000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Luukkaa H, Klemi P, Leivo I, Koivunen P, Laranne J, Mäkitie A, Virtaniemi J, Hinkka S, Grénman R. Salivary gland cancer in Finland 1991–96: an evaluation of 237 cases. Acta Otolaryngol. 2005;125:207–14. doi: 10.1080/00016480510003174. [DOI] [PubMed] [Google Scholar]
- 28.Schulz-Ertner D, Nikoghosyan A, Jäkel O, Haberer T, Kraft G, Scholz M, Wannenmacher M, Debus J. Feasibility and toxicity of combined photon and carbon ion radiotherapy for locally advanced adenoid cystic carcinomas. Int J Radiat Oncol Biol Phys. 2003;56:391–398. doi: 10.1016/S0360-3016(02)04511-X. [DOI] [PubMed] [Google Scholar]
- 29.Jensen AD, Nikoghosyan AV, Ecker S, Ellerbrock M, Debus J, Herfarth KK, Münter MW. Raster-scanned carbon ion therapy for malignant salivary gland tumors: acute toxicity and initial treatment response. Radiat Oncol. 2011;6:149. doi: 10.1186/1748-717X-6-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanvetyanon T, Qin D, Padhya T, McCaffrey J, Zhu W, Boulware D, DeConti R, Trotti A. Outcomes of postoperative concurrent chemoradiotherapy for locally advanced major salivary gland carcinoma. Arch Otolaryngol Head Neck Surg. 2009;135:687–92. doi: 10.1001/archoto.2009.70. [DOI] [PubMed] [Google Scholar]
- 31.Pederson AW, Salama JK, Haraf DJ, Witt ME, Stenson KM, Portugal L, Seiwert T, Villaflor VM, Cohen EE, Vokes EE, Blair EA. Adjuvant chemoradiotherapy for locoregionally advanced and high-risk salivary gland malignancies. Head Neck Oncol. 2011;3:31. doi: 10.1186/1758-3284-3-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maruya S, Namba A, Matsubara A, Kakehata S, Takeda I, Shirasaki T, Hatayama Y, Nagahata M, Yokoyama J, Shinkawa H. Salivary gland carcinoma treated with concomitant chemoradiation with intraarterial cisplatin and docetaxel. Int J Clin Oncol. 2006;11:403–6. doi: 10.1007/s10147-006-0587-0. [DOI] [PubMed] [Google Scholar]
- 33.Schoenfeld JD, Sher DJ, Norris CM, Jr, Haddad RI, Posner MR, Balboni TA, Tishler RB. Salivary gland tumors treated with adjuvant intensity-modulated radiotherapy with or without concurrent chemotherapy. Int J Radiat Oncol Biol Phys. 2012;82:308–14. doi: 10.1016/j.ijrobp.2010.09.042. [DOI] [PubMed] [Google Scholar]
- 34.Hocwald E, Korkmaz H, Yoo GH, Adsay V, Shibuya TY, Abrams J, Jacobs JR. Prognostic factors in major salivary gland cancer. Laryngoscope. 2001;111:1434–9. doi: 10.1097/00005537-200108000-00021. [DOI] [PubMed] [Google Scholar]
- 35.RTOG 1008 clinical trial summary. RTOG website http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=1008 last accessed 08.02.2015.


