Abstract
Background
Quality improvement (QI) is essential in clinical practice, requiring effective teaching in residency. Barriers include lack of structure, mentorship, and time.
Objective
To develop a longitudinal QI curriculum for an internal medicine residency program with limited faculty resources and evaluate its effectiveness.
Methods
All medicine residents were provided with dedicated research time every 8 weeks during their ambulatory blocks. Groups of 3 to 5 residents across all postgraduate year levels were formed. Two faculty members and 1 chief resident advised all groups, meeting with each group every 8 weeks, with concrete expectations for each meeting. Residents were required to complete didactic modules from the Institute for Healthcare Improvement. Current residents and alumni were surveyed for feedback.
Results
Over 3 years, all eligible residents (92 residents per year in 2012–2014, 102 in 2014–2015) participated in the curriculum. Residents worked on 54 quality assessment and 18 QI projects, with 6 QI projects showing statistically significant indicator improvements. About 50 mentoring hours per year were contributed by 2 faculty advisors and a chief resident. No other staff or IT support was needed. A total of 69 posters/abstracts were produced, with 13 projects presented at national or regional conferences. Survey respondents found the program useful; most (75% residents, 63% alumni) reported it changed their practice, and 71% of alumni found it useful after residency.
Conclusions
Our longitudinal QI curriculum requires minimal faculty time and resulted in increased QI-related publications and measurable improvements in quality indicators. Alumni reported a positive effect on practice after graduation.
Editor's Note: The online version of this article contains the survey tools, quality improvement project abstracts, a figure of the usefulness of quality improvement program components and attitudes toward participating, and survey data and comments.
What was known and gap
Quality improvement (QI) skills are essential for physicians, yet optimal teaching approaches that facilitate hands-on involvement in projects are lacking.
What is new
A longitudinal QI curriculum for an internal medicine residency program is feasible with limited faculty resources.
Limitations
Single site study; absence of a control group; survey lacks validity evidence.
Bottom line
The curriculum resulted in increased QI publications, measurable improvements in quality indicators, and alumni reported a positive effect on practice after graduation.
Introduction
Continuous practice assessment and improvement are essential for optimal and cost-effective patient care. Quality assessment is mandatory for maintenance of certification, and quality indicators are tied to Medicare and Medicaid reimbursements. Practice-based learning and improvement is a core competency in graduate medical education.1,2 Practice can be improved through participation in quality improvement (QI) initiatives using Plan-Do-Study-Act (PDSA) cycles.3 A formal QI curriculum fulfills multiple Accreditation Council for Graduate Medical Education (ACGME) requirements: effective practice-based learning/self-reflection, advocacy for quality patient care and optimal patient care systems, education regarding basic principles of research and their application to patient care, and resident participation in scholarly activity.2 Barriers to implementing successful resident QI programs, based on our experience and existing literature, include lack of defined structure, unavailability of appropriate mentorship, and lack of protected resident/faculty time.4,5
Existing publications often describe resident QI activities offered through dedicated electives,6–12 some limited to 1 postgraduate (PGY) level,13 with only a few describing longitudinal QI curricula.12,14–16 Most studies report on hospital-based QI, with relatively few emphasizing ambulatory care,9,12,17 and only a minority report on patient care improvement.9,12,15,17,18 A study of family medicine graduates found that some reported doing QI without formal training, while others were not engaged in improvement activities even after didactic QI exposure.19
We hypothesized that a longitudinal, 3-year QI immersion model, integrated into an ambulatory block schedule, with didactic and experiential components, spanning outpatient and inpatient sites, could be used to teach QI to internal medicine residents. This model could result in completed improvement projects and presentations and improved processes of care, while being acceptable to residents and feasible in terms of resident and faculty total time, thus making it more likely to carry over into future practice.
Methods
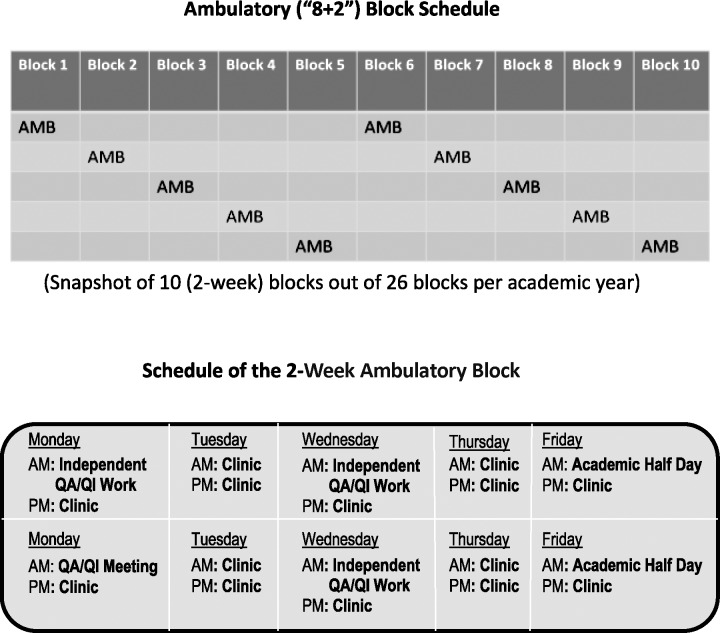
The internal medicine residency at Rutgers New Jersey Medical School has 92 categorical and 10 preliminary residents rotating through 3 affiliated hospitals. Over the last 5 years, an average of 35% (SD = 6.1%) of residents went into primary care, with an average of 62.6% (SD = 6.0%) going into fellowships. The QI curriculum launched in July 2012, at the same time as the new 8+2 ambulatory block schedule. All medicine residents participate in the program each year. In the schedule, each 8-week period (inpatient/outpatient rotations, electives, vacation, etc) is followed by 2 dedicated continuity clinic weeks. This allows for 5 to 6 ambulatory blocks per resident, per year. Ambulatory blocks contain 7 continuity clinic sessions per week (2 mornings and 5 afternoons). Two mornings per week are dedicated to self-directed learning, research, and QI work, with 1 morning dedicated to ambulatory medicine education (figure). The number of protected mornings was determined based on the residents' clinic requirements. This was to ensure that, although they replaced potential clinic time, the overall exposure to outpatient care was increased due to the introduction of the ambulatory blocks, compared to the once-weekly continuity clinic.
Figure.
Ambulatory Block Schedules
Abbreviations: QA, quality assessment; QI, quality improvement.
In 2012 to 2013, 25 QI teams were formed with members from different ambulatory blocks and were based on specialty interest. In August, residents received a lecture describing PDSA, goals of QI, advice on selecting projects, the Institutional Review Board (IRB) application process, and data analysis tips. Each team met approximately once a month with 1 faculty mentor with extensive QI-related experience and publications (who mentored all the groups) and a chief resident (trained by the faculty mentor). No other staff or IT support was needed. At that time, there were no progress goals set in advance, and we noted suboptimal communication and collaboration within groups due to residents' schedule variability.
In 2013 to 2014, modifications were made based on feedback received. A total of 22 teams (each with 3 to 5 members from same ambulatory block) were formed to facilitate meetings and improve collaboration. A second faculty mentor was added to provide additional support. To establish a more defined structure, meetings with mentors were scheduled for 20 minutes per group every second Monday of each ambulatory block. The chief resident was also present, coordinating the meetings and providing feedback. Progress goals for each meeting were outlined at the start of the academic year (box).
Box Progress Goals for Each Quality Improvement Meeting
Meeting 1: Literature search, formulate study question, complete IRB training
Meeting 2: Complete the protocol, submit IRB
Meeting 3: Data collection, preliminary analysis
Meeting 4: Data review and statistical analysis
Meeting 5: Abstract/poster ready for review
Abbreviation: IRB, Institutional Review Board.
Project ideas were developed by residents based on their own reflections about practice patterns and subspecialty interests, with the approach of “Are we adhering to guidelines on X?” Other non–guideline-based QI initiatives were also considered. Once the group had a proposal, they discussed it with the mentors to ensure feasibility and developed a protocol. Since the same faculty mentors and chief resident oversaw all the projects, duplicate projects were prevented.
With 8 weeks between ambulatory blocks, each group had sufficient time to accomplish their assigned tasks. Having 3 to 5 members per group allowed spacing out of work, so while some members were on time-intensive rotations, those on lighter ones worked on the project, handing off to their colleagues when the roles were reversed. In between QI meetings, mentors remained available for consultations.
Most projects were IRB-exempt retrospective chart reviews. Data were collected from random samples or full sets of patients within a time frame (usually a year). For QI projects, random samples or full sets of preintervention and postintervention patients over a time frame were compared to assess efficacy.
Dedicated faculty time was limited to approximately 50 hours per year for 2 faculty mentors, who contributed the time as part of their academic responsibilities (2 hours every 2 weeks), in addition to the occasional correspondence with the groups in between meetings. The chief resident managed the coordination of group meetings and the sending of reminders, and kept a record of each group's progress.
Initially, each group completed a quality assessment (QA) project over 1 year, to assess whether certain guidelines were followed and to obtain adherence data. If the QA results suggested potential for improvement, the group created a related QI project during the following year, implementing an intervention to improve the quality of care. If no potential for improvement was seen, the group designed another QA project to pursue. From 2014 to 2015, the program expanded from having only the categorical residents to include preliminary year residents as well.
As a minimum deliverable, each group had to complete 1 project per year and present their results during the internal medicine department's research day. Each resident was required to complete Institute for Healthcare Improvement QI didactic modules, covering improvement capability, patient safety, leadership, patient- and family-centered care, and triple aim for populations in quality, cost, and value. Residents had to turn in completion certificates for the program director to monitor compliance. Residents were encouraged to pursue publication of their work, but this was not a requirement.
A survey of residents and recent graduates assessed satisfaction with the program, perceived usefulness of the skills learned, and applicability of skills learned to their current practice (for alumni). The survey was developed by the authors without obtaining additional evidence of validity (provided as online supplemental material); it was sent out by the program director to all current residents and all alumni from the prior 3 years who had participated in the QI curriculum.
This study was evaluated by the Rutgers IRB and found to be exempt from review.
Results
Between 2012 and 2015, all eligible residents (92 residents per year in 2012–2014, 102 in 2014–2015) participated in the curriculum. The residents worked on 54 QA projects and 18 QI projects. Fifteen of the QI projects were completed, and to date, 6 have resulted in statistically significant improvements in practice quality indicators (provided as online supplemental material). To date, the program has produced 69 poster presentations for the department's research day, with 2 being chosen for oral presentations.20–22
Thirteen QI projects were presented at national or regional conferences. One received the “Best Oral Presentation Award” at the New Jersey American College of Physicians scientific meeting.
The resident survey had a 58% response rate (53 of 92 residents), split evenly across the 3 PGY levels. The alumni survey had a response rate of 41% (36 of 88 residents).
For most respondents (83% [44 of 53] of residents, 94% [34 of 36] of alumni), participation in this program was their first exposure to QI. The majority of survey respondents found various aspects of the program useful (provided as online supplemental material).
Most respondents agreed that participating in the curriculum changed their understanding of quality in health care (87% [46 of 53] residents, 86% [31 of 36] alumni), and consequently, they modified their behavior as a physician (75% [40 of 53] residents, 61% [22 of 36] alumni). Most enjoyed working on the projects (79% residents [42 of 53], 75% alumni [27 of 36]); would recommend this way of learning QI to other programs (85% [45 of 53] residents, 83% [30 of 36] alumni); used the information to teach others (75% [40 of 53] residents, 72% [26 of 36] alumni); and learned skills that are useful in their practice (72% [26 of 36] alumni). Survey data and comments are provided as online supplemental material.
Discussion
We found that a longitudinal, 3-year QI immersion model, integrated into an 8+2 block schedule, resulted in increased resident scholarly productivity, with multiple completed improvement projects and presentations. It was perceived as useful and practice changing by residents and alumni, and required a feasible resident and faculty time commitment, even in a large program with limited resources. As the curriculum evolved, we assigned protected time for QI, such as prescheduling mentor meetings, and setting clear goals improved collaboration and productivity. Of note to other programs who wish to institute a QI curriculum, our intervention can function with fewer mentors and more residents, thus requiring fewer resources. Our innovative approach enabled more than 20 ongoing projects to be supervised by just 2 faculty mentors, who spent about 50 hours per year on mentoring more than 100 residents. The chief resident who assisted was able to perform this function in addition to his or her other duties. Thus, the curriculum is feasible for large or resource-constrained programs.
Limitations of our intervention include the fact that it was conducted at a single institution and lacked a control group, making it impossible to differentiate between the effects of the didactic versus experiential components of the curriculum. Additionally, the survey lacks validity evidence, and respondents may not have interpreted the questions as were intended.
To better assess the effect of the curriculum, we plan to use the Revised Quality Improvement Knowledge Application Tool23 to collect precurriculum and postcurriculum data about resident QI knowledge. Although in practice many graduates may not have a dedicated half-day to work on improvement projects, we hope that exposure to this curriculum will spur them to find alternative ways to maintain QI practice, which could be assessed in future surveys.
Conclusion
Our longitudinal QI curriculum requires minimal faculty time and has resulted in increased QI publications and measurable improvements in practice quality indicators. We also found a positive effect on practice suggested by the alumni survey.
Supplementary Material
References
- 1. Swing SR. The ACGME outcome project: retrospective and prospective. Med Teach. 2007. 29 7: 648– 654. [DOI] [PubMed] [Google Scholar]
- 2. Accreditation Council for Graduate Medical Education. Program requirements for graduate medical education in internal medicine. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/CPRs_07012015.pdf. Accessed March 1, 2016. [Google Scholar]
- 3. Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco, CA: Jossey-Bass Publishers; 2009. [Google Scholar]
- 4. Runnacles J, Moult B, Lachman P. Developing future clinical leaders for quality improvement: experience from a London children's hospital. BMJ Qual Saf. 2013; 22 11: 956– 963. [DOI] [PubMed] [Google Scholar]
- 5. Patow CA, Karapovich K, Riesenberg LA, Jaeger J, Rosenfield JC, Wittenbreer M, et al. Residents' engagement in quality improvement: a systematic review of the literature. Acad Med. 2009; 84 12: 1757– 1764. [DOI] [PubMed] [Google Scholar]
- 6. Sarwar A, Eisenberg RL, Boiselle PM, Siewert B, Kruskal JB. Improving resident education in quality improvement: role for a resident quality improvement director. Acad Radiol. 2013; 20 4: 500– 505. [DOI] [PubMed] [Google Scholar]
- 7. Ogrinc G, Headrick LA, Morrison LJ, Foster T. Teachingand assessing resident competence in practice-based learning and improvement. J Gen Intern Med. 2004; 19(5, pt 2):496–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Weingar SN, Tess A, Driver J, Aronson MD, Sands K. Creating a quality improvement elective for medical house officers. J Gen Intern Med. 2004; 19 8: 861– 867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sepulveda D, Varaklis K. Implementing a multifaceted quality-improvement curriculum in an obstetrics-gynecology resident continuity-clinic setting: a 4-year experience. J Grad Med Educ. 2012; 4 2: 237– 241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Djuricich AM, Ciccarelli M, Swigonski NL. A continuous quality improvement curriculum for residents: addressing core competency, improving systems. Acad Med. 2004; 79 suppl 10: 65– 67. [DOI] [PubMed] [Google Scholar]
- 11. Lawrence RH, Tomolo AM. Development and preliminary evaluation of a practice-based learning and improvement tool for assessing resident competence and guiding curriculum development. J Grad Med Educ. 2011; 3 1: 41– 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Laiteerapong N, Keh CE, Naylor KB, Yang VL, Vinci LM, Oyler JL, et al. A resident-led quality improvement initiative to improve obesity screening. Am J Med Qual. 2011; 26 4: 315– 322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fok MC, Wong RY. Impact of a competency based curriculum on quality improvement among internal medicine residents. BMC Med Educ. 2014; 14: 252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Simasek M, Ballard SL, Phelps P, Pingul-Ravano R, Kolb NR, Finkelstein A, et al. Meeting resident scholarly activity requirements through a longitudinal quality improvement curriculum. J Grad Med Educ. 2015; 7 1: 86– 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wong BM, Etchell EE, Kuper A, Levinson W, Shojania KG. Teaching quality improvement and patient safety to trainees: a systematic review. Acad Med. 2010; 85 9: 1425– 1439. [DOI] [PubMed] [Google Scholar]
- 16. Duello K, Louh I, Greig H, Dawson N. Residents' knowledge of quality improvement: the impact of using a group project curriculum. Postgrad Med J. 2015; 91 1078: 431– 435. [DOI] [PubMed] [Google Scholar]
- 17. Stewart EA, Guggenheim DE, Patel K, Kane GC. Implementing quality improvement in a residency continuity clinic—a novel approach. Acad Intern Med Insight. 2011; 9 3: 12– 13. [Google Scholar]
- 18. Boonyasai RT, Windish DM, Chakraborti C, Feldman LS, Rubin HR, Bass EB. Effectiveness of teaching quality improvement to clinicians: a systematic review. JAMA. 2007; 298 9: 1023– 1037. [DOI] [PubMed] [Google Scholar]
- 19. Carek PJ, Dickerson LM, Stanek M, Carter C, Godenick MT, Jebaily GC. Education in quality improvement for practice in primary care during residency training and subsequent activities in practice. J Grad Med Educ. 2014; 6 1: 50– 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Blackwell L, Roy R, Kim S, Kim A, Tan M, Tentler A, et al. Improving physician adherence to tobacco cessation counseling guidelines. Am J Respir Crit Care Med. 2014; 189: A1101. [Google Scholar]
- 21. Vassallo-DeLuca E, Wang T, Ricketti P, Tentler A, Kothari N. Potential consequences of overlooking abdominal aortic aneurysm screening. Presented at: New Jersey Chapter of American College of Physicans Regional Scientific Meeting; Iselin, NJ March 8, 2013. [Google Scholar]
- 22. Patel N, Bernardo R, Gandhi S, Khateeb D, Tentler A, Kothari N. Prophylaxis against inappropriate PPI use: a follow-up. Am J Gastroenterol. 2013; 108: S187– S463. [Google Scholar]
- 23. Singh MK, Ogrinc G, Cox KR, Dolansky M, Brandt J, Morrison LJ, et al. The quality improvement knowledge application tool revised (QIKAT-R). Acad Med. 2014; 89 10: 1386– 1391. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.