Abstract
Background
Effective adolescent (10 to 19 years) interviewing by physicians is an essential skill that many trainees can find challenging.
Objective
We assessed whether structured adolescent interviewing using standardized patients (SPs) and feedback in undergraduate medical education (UME) has a sustained effect on residents' skills.
Methods
Postgraduate year (PGY) 1 residents conducted interviews with a SP adolescent–mother pair. The SPs independently scored each PGY-1 interview using the structured communication adolescent guide (SCAG). Unpaired t tests were conducted comparing “Total-Item” and “Global” scores of PGY-1s who received structured SP adolescent interviewing with feedback in UME (“structured training” group) to those who had not (“no structured training” group).
Results
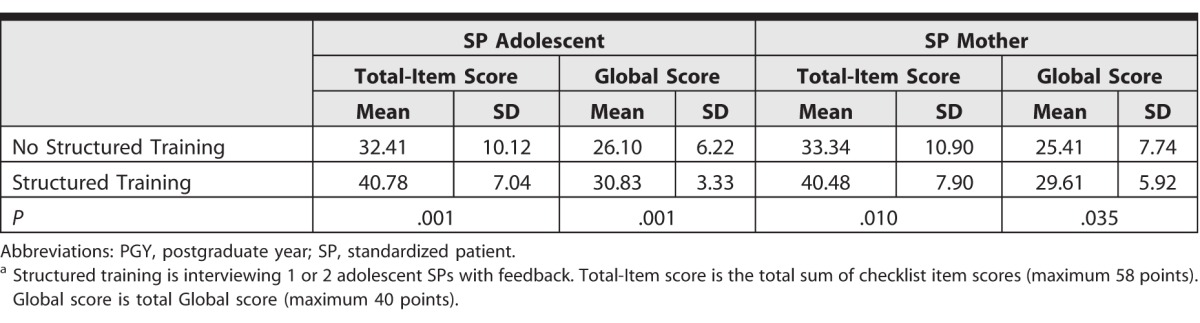
PGY-1s in the structured training group (n = 23) received significantly higher mean Total-Item scores from both the SP adolescent (40.78 ± 7.04 and 32.41 ± 10.12, respectively; P = .001) and the SP mother (40.48 ± 7.90 and 33.34 ± 10.90, respectively; P = .01) than those without structured training (n = 29). Statistically significant results favoring PGY-1s with prior training were also seen with the SP adolescent and mother total Global SCAG scores.
Conclusions
Structured training in adolescent interviewing with SPs and feedback in UME appears to have a sustained effect on residents' adolescent interviewing skills. PGY-1s will interview adolescents and may benefit from structured adolescent SP interviewing with feedback, especially individuals who did not have this experience during their medical school training.
Editor's Note: The online version of this article contains a table of residents' scoring in both “structured training” and “no structured training” groups.
Introduction
Successful communication strategies have been shown to enhance patients' satisfaction with their care1,2 and compliance with treatment programs.3–5 However, studies have shown that postgraduate year (PGY) 1 residents in multiple disciplines are not skilled in many aspects of adolescent communication.6–9 Health care professions trainees also feel that their adolescents' communication training needs are not addressed in medical education, expressing interest in more training throughout the medical curriculum.10
Communication training using adolescent standardized patients (SPs) has been shown to be effective at the undergraduate level,11,12 yet little is known about the sustained impact effectiveness of this type of training into residency. There is some evidence supporting the sustained effect of adult communication skills training from undergraduate medical education (UME) into graduate medical education.13 Our study aimed to determine whether structured SP adolescent interviewing with feedback in UME has a sustained effect on PGY-1 residents' adolescent interview performance.
Methods
We conducted a 2-group comparison study. PGY-1s entering Dalhousie University in Halifax, Canada, were invited to participate and were recruited from all specialties at orientation sessions prior to the start of their residency. Five female adolescent and mother pairs were trained using scripts containing sensitive adolescent topics and were encouraged to give feedback. SP pairs were randomized to each individual PGY-1 who participated. SP adolescents portrayed a 14-year-old girl.
Outcome Measures
Demographic information collected included age, sex, institution of UME training, and previous adolescent interview teaching. Participants with “structured training” indicated that they had received training in UME with at least 1 adolescent SP and were given feedback. A lecture and/or tutorial on adolescent interviewing was classified as “no structured training.”
The structured communication adolescent guide (SCAG) was used to evaluate resident performance. Prior research has shown the SCAG to be a reliable instrument with some validity evidence when used by SPs14 and non-SP adolescents.15 The SCAG consists of 4 sections: Getting Started, Gathering Information, Teen Alone, and Wrap Up. The sum of all checklist item scores within each section yields a “Total-Item” score (maximum of 58). The sum of the “Global” scores for each section (n = 4) yields a total Global score (maximum of 40). The 5-point Likert scale used in earlier SCAG iterations was expanded to a 10-point scale to allow for more variability in scoring. The Teen Alone section highlights 14 sensitive topics relevant to adolescents and is based on the HEADDSS mnemonic.16,17
Procedure
Interviews were conducted at the Dalhousie University Learning Resource Centre. Each resident provided informed consent, completed a demographic questionnaire, and conducted an interview with an SP adolescent–mother pair. Using the SCAG, SPs individually scored PGY-1s immediately following each interview. The SPs recorded scores of 2 of 2 (fulfilled the criteria of the question well), 1 of 2 (fulfilled the criteria), or 0 of 2 (did not fulfill the criteria) for each item. The PGY-1s also received a Global score on each of the 4 sections of the SCAG. Standardized patients were asked to write comments regarding PGY-1s' performance, which shaped the verbal feedback PGY-1s would receive.
Institutional Review Board approval was provided by the Research Ethics Board of Dalhousie University in Canada.
Data Analysis
Demographic information was analyzed using descriptive statistics. Unpaired t tests were utilized to compare the average Total-Item and Global (total) SCAG scores of the “no structured training” group with the “structured training” group. These t tests were conducted using the SP adolescents' and mothers' scores separately. Cohen's d analysis was conducted to determine effect size of these results. PGY-1 performance in the Teen Alone section of the SCAG was analyzed. An unpaired t test was conducted between the SP adolescent and SP mother scores to determine interrater reliability.
Results
A total of 52 PGY-1s participated (34 women) of a possible 108 (48% response rate); and 23 of these had received adolescent structured training during their UME, including 1 or more adolescent SP encounters with feedback (table 1).
Table 1.
Demographic Information for PGY-1s With No Previous Structured Training in Undergraduate Medical Education Versus PGY-1s With Structured Traininga

The structured training group demonstrated significantly greater Total-Item and Global SCAG scores (from both SP adolescents and mothers) than the No structured training group (table 2). Cohen's d analysis demonstrated SP adolescent Total-Item and Global score effect sizes of 0.96 and 0.95, respectively. For the SP mothers, the Cohen's d effect size for the Total-Item and Global scores was 0.75 and 0.61, respectively.
Table 2.
Scores for PGY-1s With No Previous Structured Training in Undergraduate Medical Education Versus PGY-1s With Structured Traininga
The online supplemental material compares the percentage of PGY-1s who received a 2 of 2 (“did well”) from adolescent SPs in all areas of interviewing between the structured training and no structured training groups.
Discussion
Our study aimed to determine whether structured adolescent training, consisting of interviews and structured feedback from an adolescent–mother SP pair in UME, had a sustained effect on PGY-1 adolescent interviewing performance.
PGY-1s who had received structured adolescent training in UME scored significantly higher on mean Total-Item and total Global SCAG scores than PGY-1s who had not. This lends support to our hypothesis that the skills acquired in interviewing an adolescent with SP feedback in UME were sustained into postgraduate training. Financial and time limitations are often cited as reasons for lack of adolescent training interventions.17 This study showed that even with limited adolescent SP encounters with structured feedback, sustained improvement in adolescent interviewing performance appears possible.
The online supplemental material compares the percentage of PGY-1s in each group who scored 2 of 2 (“did well”) from SP adolescents on each checklist item of the SCAG. There is room for improvement in many of the risk-taking areas, as well as in discussing confidentiality and separating the adolescent from the parent. This suggests the importance of training medical students, residents, and physicians in effectively facilitating good communication, separation from the adult, discussing confidentiality, and addressing risk-taking behaviors.
Limitations include a small sample size with respondents from a single institution. A second limitation is that the study utilized exclusively female SP adolescents and mothers to maintain consistency and reduce variability. A final limitation may be that our measures were based on just 1 adolescent interview for each participating resident. We believe that the SCAG's measure, which has shown both high reliability and evidence of validity in other studies,14,15 provides an accurate assessment of PGY-1s' performance on this single occasion.
Conclusion
Structured adolescent training with feedback in adolescent interviewing could be beneficial in undergraduate medical curricula prior to learners approaching adolescents in residency training. The majority of PGY-1s will encounter adolescents and young adults, regardless of subspecialty. The importance of adolescent communication skills is not specific to pediatrics; therefore, we suggest that incorporation of these skills into postgraduate medical training would provide additional preparation for future adolescent clinical encounters.
Supplementary Material
References
- 1. Tak H, Ruhnke GW, Shih YC. The association between patient-centered attributes of care and patient satisfaction. Patient. 2015; 8 2: 187– 197. [DOI] [PubMed] [Google Scholar]
- 2. Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner. 2010; 10 1: 38– 43. [PMC free article] [PubMed] [Google Scholar]
- 3. King A, Hoppe RB. “Best practice” for patient-centered communication: a narrative review. J Grad Med Educ. 2013; 5 3: 385– 393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Van Dulmen S. The value of tailored communication for person-centred outcomes. J Eval Clin Pract. 2011; 17 2: 381– 383. [DOI] [PubMed] [Google Scholar]
- 5. Dimatteo MR. The role of effective communication with children and their families in fostering adherence to pediatric regimens. Patient Educ Couns. 2004; 55 3: 339– 344. [DOI] [PubMed] [Google Scholar]
- 6. Frank JR. The CanMEDS 2005 physician competency framework. Better standards. Better physicians. Better care. Ottawa, Canada: The Royal College of Physicians and Surgeons of Canada; 2005. http://www.ub.edu/medicina_unitateducaciomedica/documentos/CanMeds.pdf. Accessed January 13, 2016. [Google Scholar]
- 7. Sacks D, Westwood M. An approach to interviewing adolescents. Paediatr Child Health. 2003; 8 9: 554– 556. [PMC free article] [PubMed] [Google Scholar]
- 8. Fox CH, Cornwall A. Undetected childhood sexual trauma and its health effects in adults. Am Fam Physician. 2013; 88 5: 328– 330. [PubMed] [Google Scholar]
- 9. Kershnar R, Hooper C, Gold M, Norwitz ER, Illuzi JL. Adolescent medicine: attitudes, training, and experience of pediatric, family medicine, and obstetric-gynecology residents. Yale J Biol Med. 2009; 82 4: 129– 141. [PMC free article] [PubMed] [Google Scholar]
- 10. Sawyer SM, Conn JJ, Reid KJ, Dodds AE, Hudson L, Yeo M, et al. Working with young people: evaluation of an education resource for medical trainees. J Paediatr Child Health. 2013; 49 11: 901– 905. [DOI] [PubMed] [Google Scholar]
- 11. Macdonald M, MacCuspie J, Mann K, Blake K. Improving medical student's confidence regarding adolescent interviewing. Pediat Therapeut. 2014; 4 4: 218. https://www.researchgate.net/publication/280209910_Improving_Medical_Student's_Confidence_Regarding_Adolescent_Interviewing. Accessed January 13, 2016. [Google Scholar]
- 12. Blake K, Mann KV, Kaufman DM, Kappleman M. Learning adolescent psychosocial interviewing using simulated patients. Acad Med. 2000; 75 suppl 10: 56– 58. [DOI] [PubMed] [Google Scholar]
- 13. Laidlaw TS, Kaufman DM, Macleod H, van Zanten S, Simpson D, Wrixon W. Relationship of resident characteristics, attitudes, prior training and clinical knowledge to communication skills performance. Med Educ. 2006; 40 1: 18– 25. [DOI] [PubMed] [Google Scholar]
- 14. Blake K, Vincent N, Wakefield S, Murphy J, Mann K, Kutcher M. Structured communication adolescent guide (SCAG): assessment of reliability and validity to residents and physicians. Med Educ. 2005; 39 5: 482– 491. [DOI] [PubMed] [Google Scholar]
- 15. Kutcher M, Wakefield S, Mann J, MacCuspie J, Murphy J, Blake K. Rating a physician by adolescents using the structured communication adolescent guide (SCAG). Internet J Med Educ. 2010; 1(2). http://ispub.com/IJME/1/2/10318. Accessed January 13, 2016. [DOI] [PubMed] [Google Scholar]
- 16. Goldenring JM, Cohen E. Getting into adolescent heads. Contemp Pediatr. 1988; 5 7: 75– 90. [Google Scholar]
- 17. Whitehouse SR, Lam PY, Balka E, Mclellan S, Deevska M, Penn D, et al. Co-creation with tickit: designing and evaluating a clinical ehealth platform for youth. JMIR Res Protoc. 2013; 2 2: e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


