Abstract
Background
Recent studies have shown improving survival after cardiac arrest. However, data regarding sex‐based disparities in treatment and outcomes after cardiac arrest are limited.
Methods and Results
We performed a retrospective analysis of all patients suffering cardiac arrest between 2003 and 2012 using the Nationwide Inpatient Sample database. Annual rates of cardiac arrest, rates of utilization of coronary angiography/percutaneous coronary interventions/targeted temperature management, and sex‐based outcomes after cardiac arrest were examined. Among a total of 1 436 052 discharge records analyzed for cardiac arrest patients, 45.4% (n=651 745) were females. Women were less likely to present with ventricular tachycardia/ventricular fibrillation arrests compared with men throughout the study period. The annual rates of cardiac arrests have increased from 2003 to 2012 by 14.0% (P trend<0.001) and ventricular tachycardia/ventricular fibrillation arrests have increased by 25.9% (P trend<0.001). Women were less likely to undergo coronary angiography, percutaneous coronary interventions, or targeted temperature management in both ventricular tachycardia/ventricular fibrillation and pulseless electrical activity/asystole arrests. Over a 10‐year study period, there was a significant decrease in in‐hospital mortality in women (from 69.1% to 60.9%, P trend<0.001) and men (from 67.2% to 58.6%, P trend<0.001) after cardiac arrest. In‐hospital mortality was significantly higher in women compared with men (64.0% versus 61.4%; adjusted odds ratio 1.02, P<0.001), particularly in the ventricular tachycardia/ventricular fibrillation arrest cohort (49.4% versus 45.6%; adjusted odds ratio 1.11, P<0.001).
Conclusions
Women presenting with cardiac arrests are less likely to undergo therapeutic procedures, including coronary angiography, percutaneous coronary interventions, and targeted temperature management. Despite trends in improving survival after cardiac arrest over 10 years, women continue to have higher in‐hospital mortality when compared with men.
Keywords: angiography, heart arrest, revascularization, sudden death, women
Subject Categories: Cardiopulmonary Resuscitation and Emergency Cardiac Care, Cardiopulmonary Arrest, Women, Coronary Artery Disease, Percutaneous Coronary Intervention
Introduction
Cardiac arrest remains an important cause of morbidity and mortality in the United States. It is estimated that there are over 300 000 out‐of‐hospital, nontraumatic cardiac arrests in the United States annually.1 Though survival has increased dramatically over the past 15 years, overall mortality remains very high.2, 3 Data from the Cardiac Arrest Registry to Enhance Survival demonstrate modest improvements in risk‐adjusted out‐of‐hospital cardiac arrest survival rates over the last decade, from 5.7% in 2005 to 8.3% in 2012. Patients with shockable rhythms (ventricular tachycardia [VT] and ventricular fibrillation [VF]) expectedly have the best survival rates, whereas survival for pulseless electrical activity (PEA) or asystole remains poor.4 Despite grim outcomes, there are marked regional variations in survival after cardiac arrest, which reflect potential disparities in mechanisms of national and local delivery of resuscitative care.5 Furthermore, neurological outcomes among cardiac arrest survivors have been improving, with fewer survivors having severe disability after recovery.6, 7
Several important features and interventions have been shown to improve outcomes following cardiac arrest: bystander cardiopulmonary resuscitation,8, 9 presentation with a shockable rhythm,10 timely defibrillation,9, 11therapeutic hypothermia, or targeted temperature management (TTM),12, 13 and immediate coronary angiography with percutaneous coronary intervention (PCI).14, 15 Despite recent advances and a multispecialty team‐based approach to the treatment of cardiac arrest, there remains limited and conflicting data with regard to sex‐based disparities in presentation and treatment of patients presenting with a cardiac arrest. There has been ample evidence suggesting that women have worse outcomes across a variety of cardiovascular procedures/surgeries, including coronary artery bypass grafting surgery16 and primary PCI for ST‐segment elevation myocardial infarction (STEMI).17 However, data regarding sex‐based differences in outcomes following cardiac arrest have been conflicting, with some studies showing worse survival among women and others showing comparable or even better survival in women.18, 19, 20, 21, 22, 23 Given limited and contradictory published data, we sought to characterize sex‐based disparities and trends in presentation, treatment strategies, and in‐hospital clinical outcomes for all cardiac arrests, as well as for subgroups of VT/VF and PEA/asystole, in a large, national contemporary database from 2003 to 2012. Our findings will further our understanding of mechanisms contributing to the cardiac arrest sex gap and may assist in the resolution of discrepant historical data.
Methods
Data Source and Study Population
Data were obtained from the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project—Nationwide Inpatient Sample (NIS) files between 2003 and 2012.24 The NIS is a 20% stratified sample of all nonfederal US hospitals and, in 2012, contained deidentified information for 38 590 733 discharges from 1049 hospitals and 46 states. Discharges are weighted based on the sampling scheme to permit inferences for a nationally representative population. Each record in the NIS includes all procedure and diagnosis International Classification of Diseases (ICD) codes recorded for each patient's hospital discharge.
From January 2003 through December 2012, hospitalizations with a diagnosis of cardiac arrest either in the primary or secondary diagnoses were included for analysis. Cardiac arrests were identified based on the presence of ICD‐9‐CM code 427.5. Out‐of‐hospital cardiac arrests were captured when the code 427.5 was assigned as a principal diagnosis and when a patient arrived at the hospital in a state of cardiac arrest and could not be resuscitated or was resuscitated briefly and pronounced dead before the underlying cause of the arrest was identified. In‐hospital cardiac arrests were captured when the code 427.5 was assigned as a secondary code and when cardiac arrest occurred during the hospital episode and the patient was resuscitated (or resuscitation was attempted). Cardiac arrests that occurred as a complication of surgery or complicating abortion, ectopic pregnancy, or labor and delivery were excluded, as those arrests were coded with different ICD‐9‐CM codes (997.1 and 669.4x). Among those who presented with cardiac arrests, VT was identified by ICD‐9‐CM code 427.1, and VF was identified based on the presence of ICD‐9‐CM code 427.4. PEA/asystole arrests were defined as cardiac arrests without concomitant ventricular arrhythmia. Acute myocardial infarction and pulmonary embolism were identified by ICD‐9‐CM codes 410.x (excluding 410.7) and 415.1, respectively.
Weill Cornell Medical College institutional review board deemed this study exempt because the Healthcare Cost and Utilization Project–NIS is a publicly available database containing deidentified patient information.
Definition and End Points
Patient‐level and hospital‐level variables were included as baseline characteristics. Hospital‐level data elements were derived from the AHA Annual Survey Database. The Agency for Healthcare Research and Quality comorbidity measures based on the Elixhauser methods were used to identify comorbid conditions.25 The outcome measures examined included in‐hospital all‐cause mortality, likelihood of undergoing coronary angiogram, PCI, and TTM. Coronary angiography was identified using the ICD‐9‐CM codes 37.21, 37.22, 37.23, 88.53, 88.54, 88.55, 88.56, and 88.57 in any of the 15 procedure fields during the same hospitalization. PCI was identified by the ICD‐9‐CM codes 00.66, 36.03, 36.04, 34.06, 34.07, and 34.09. TTM was selected using the ICD‐9‐CM procedure code 99.81.
Statistical Analyses
For descriptive analyses, we compared baseline patient and hospital characteristics of those presenting with cardiac arrest for each sex. Continuous variables are presented as medians; categorical variables are expressed as frequencies (percentages). To compare baseline characteristics, either Mann–Whitney Wilcoxon nonparametric tests or Student t test were used for continuous variables, and Pearson χ2 tests were used for categorical variables. We calculated the incidence of cardiac arrests as the weighted number of arrests divided by 20% of the total number of US adults during the same periods. Estimates of the US adult population between 2003 and 2012 were obtained from the US Census Bureau.26 Trends in the annual rates of cardiac arrests, coronary angiography, PCI, and TTM were assessed using time series modeling (autoregressive integrated moving average model) and were further stratified by sex.
Unadjusted rates of utilization of coronary angiography, PCI, TTM, and in‐hospital mortality rates were calculated for each sex. Multivariate logistic regression analysis was used to adjust for baseline differences between men and women by adjusting for univariate predictors of examined outcomes (P<0.01). The models were adjusted for the following demographic, hospital‐level, and procedural variables: age, race, hospital bed size, hospital teaching status, urban versus rural setting, region, payer, anemia, collagen vascular disease, congestive heart failure, chronic pulmonary disease, diabetes mellitus, coagulopathy, hypertension, liver disease, neurological disorders, obesity, peripheral vascular disorders, pulmonary circulation disease, chronic renal failure, hemodialysis dependence, valve disease, history of cardiac arrest, coma, STEMI, pulmonary embolism, prior coronary artery bypass grafting surgery, and prior PCI. Unadjusted and adjusted analyses were then repeated for subgroups of patients presenting with VT/VF and PEA/asystole arrests. For all regression analyses, the Taylor linearization method “with replacement” design was used to compute variances. All statistical tests were 2‐sided, and a P‐value of <0.05 was set a priori to be statistically significant. All statistical analyses were conducted using SAS, version 9.2 (SAS Institute, Cary, NC) and SPSS, version 20 (IBM Corporation).
Results
Study Population and Baseline Characteristics
Of the 1 436 052 discharge records analyzed from patients who were transported alive to the emergency department of acute‐care hospitals with a cardiac arrest between 2003 and 2012, 45.4% (n=651 745) were females. Overall baseline and hospital characteristics for all cardiac arrests, VT/VF, and PEA/asystole arrests stratified by sex are shown in Table 1. Women with cardiac arrest were older and had more comorbid conditions compared with men. Nonischemic causes of cardiac arrest (eg, pulmonary embolism) were more common in women. Conversely, women were less likely to have prior PCI or coronary artery bypass grafting surgery and less frequently presented with concomitant STEMI. Women were more likely to be treated in smaller, nonurban, nonteaching hospitals compared with men. Cardiac arrests due to VT/VF were more common in men (26.7% versus 19.4%, P<0.001) throughout the whole study period. Among VT/VF arrests, similar sex differences were noted.
Table 1.
Baseline Patient and Hospital Characteristics for Cardiac Arrests 2003–2012
| Characteristics | All | VT/VF | PEA/Asystole | |||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | P valuea | Men | Women | P valuea | |
| N | 784 307 | 651 745 | 209 582 | 126 490 | 574 724 | 525 255 | ||
| Age, mean±SD, y | 64.2±18.3 | 67.4±18.7 | 64.2±15.4 | 65.6±16.8 | 64.2±19.2 | 67.9±19.1 | ||
| Median age, y | 67 | 71 | 65 | 68 | 67 | 72 | ||
| VT/VF (%) | 26.7 | 19.4 | — | — | — | — | ||
| STEMI (%) | 14.3 | 10.7 | 27.6 | 20.7 | 9.5 | 8.2 | ||
| Pulmonary embolism (%) | 2.6 | 3.3 | 1.6 | 2.2 | 3.0 | 3.6 | ||
| Coma (%) | 5.2 | 5.6 | 1.5 | 1.5 | 0.08 | 5.0 | 5.4 | |
| Anemia (%) | 17.0 | 20.4 | 14.8 | 19.0 | 17.9 | 20.7 | ||
| Collagen vascular disease (%) | 1.1 | 3.3 | 1.0 | 3.1 | 1.1 | 3.3 | ||
| Chronic pulmonary disease (%) | 23.6 | 23.8 | 21.6 | 22.8 | 17.9 | 20.7 | ||
| Coagulopathy (%) | 12.4 | 11.2 | 10.9 | 10.2 | 1.1 | 3.3 | ||
| Diabetes mellitus, uncomplicated (%) | 20.7 | 22.3 | 20.8 | 22.0 | 17.9 | 20.7 | ||
| Diabetes mellitus, with complication (%) | 6.2 | 6.4 | 5.5 | 6.3 | 1.1 | 3.3 | 0.69 | |
| Hypertension (%) | 47.2 | 50.9 | 49.2 | 51.2 | 17.9 | 20.7 | ||
| Liver disease (%) | 4.1 | 2.7 | 2.9 | 2.1 | 1.1 | 3.3 | ||
| Neurological disorder (%) | 12.2 | 13.3 | 10.6 | 12.2 | 17.9 | 20.7 | ||
| Obesity (%) | 7.0 | 9.0 | 7.9 | 10.2 | 1.1 | 3.3 | ||
| Peripheral vascular disease (%) | 9.4 | 8.0 | 9.6 | 8.2 | 17.9 | 20.7 | ||
| Pulmonary circulation disease (%) | 3.4 | 4.7 | 2.3 | 3.4 | 3.8 | 5.0 | ||
| Valve disease (%) | 4.4 | 5.8 | 3.7 | 5.6 | 4.7 | 5.8 | ||
| History of cardiac arrest | 0.3 | 0.2 | 0.3 | 0.3 | 0.08 | 0.2 | 0.2 | |
| Systolic heart failure (%) | 31.0 | 32.3 | 37.3 | 38.0 | 28.7 | 30.9 | ||
| Diastolic heart failure (%) | 2.5 | 4.2 | 2.1 | 3.8 | 2.7 | 4.4 | ||
| Chronic renal failure (%) | 22.1 | 20.3 | 20.5 | 19.9 | 22.6 | 20.4 | ||
| Hemodialysis | 1.7 | 1.9 | 1.5 | 2.0 | 1.8 | 1.8 | ||
| Previous CABG (%) | 6.9 | 3.4 | 8.0 | 4.2 | 6.5 | 3.3 | ||
| Previous PCI (%) | 4.3 | 2.8 | 6.0 | 3.8 | 3.6 | 2.5 | ||
| Payer (%) | ||||||||
| Medicare | 58 | 65.7 | 54.2 | 61.6 | 59.3 | 66.7 | ||
| Medicaid | 9.9 | 10.8 | 7.7 | 9.8 | 10.7 | 11.1 | ||
| HMO | 22.5 | 17.7 | 28.3 | 22.1 | 20.3 | 16.7 | ||
| Race/ethnicity (%) | ||||||||
| White | 69.8 | 66.4 | 75.0 | 69.2 | 68.0 | 65.8 | ||
| Black | 14.5 | 18.7 | 11.9 | 17.8 | 15.4 | 18.9 | ||
| Hispanic | 9.2 | 8.7 | 7.0 | 7.2 | 9.9 | 9.1 | ||
| Bed size (%) | ||||||||
| Large | 66.6 | 64.8 | 69.2 | 67.7 | 65.6 | 64.1 | ||
| Medium | 23.4 | 24.3 | 22.6 | 23.6 | 23.8 | 24.4 | ||
| Small | 10.0 | 10.9 | 8.2 | 8.7 | 10.6 | 11.5 | ||
| Urban hospital (%) | 89.9 | 88.7 | 92.8 | 91.7 | 88.9 | 88.0 | ||
| Teaching hospital (%) | 47.7 | 45.4 | 49.5 | 47.7 | 47 | 44.8 | ||
| Region (%) | ||||||||
| Northeast | 16.1 | 16.5 | 16.6 | 16.6 | 16.0 | 16.5 | ||
| Midwest | 22.2 | 22 | 24.7 | 23.9 | 21.3 | 21.6 | ||
| South | 40.4 | 41.6 | 37.0 | 38.8 | 41.6 | 42.3 | ||
| West | 21.3 | 19.9 | 21.7 | 20.6 | 21.1 | 19.7 | ||
| In‐hospital death (%) | 61.4 | 64.0 | 45.6 | 49.4 | 67.2 | 67.5 | ||
| Procedure performed (%) | ||||||||
| Coronary angiography | 17.6 | 12.3 | 38.1 | 29.0 | 10.2 | 8.2 | ||
| PCI | 8.9 | 5.4 | 21.2 | 14.3 | 4.4 | 3.2 | ||
| TTM | 1.2 | 0.9 | 2.5 | 1.8 | 0.8 | 0.7 | ||
| Left ventricular assist device | 0.2 | 0.1 | 0.4 | 0.2 | 0.1 | 0 | ||
| Intra‐aortic balloon pump | 5.3 | 3.2 | 11.6 | 7.6 | 3.0 | 2.1 | ||
CABG indicates coronary artery bypass grafting; Coma, vegetative state; HMO, Health Maintenance Organization; PCI, percutaneous coronary interventions; PEA, pulseless electrical activity; STEMI, ST segment‐elevation myocardial infarction; TTM, targeted temperature management; VT/VF, ventricular tachycardia and ventricular fibrillation/flutter.
All P values are statistically significant (P<0.001) unless otherwise noted.
Cardiac Arrest Trends, 2003–2012
The annual incidence of all cardiac arrests, VT/VF arrests, and PEA/asystole arrests increased between 2003 and 2012 by 14.0% (608 arrests per million adults to 693 arrests per million adults, P trend<0.001), by 25.9% (136 arrests per million adults to 171 arrests per million adults, P trend<0.001), and by 10.6% (472 arrests per million adults to 522 arrests per million adults, P trend=0.003), respectively. There was a greater increase over the study period in rates of all types of cardiac arrests in men compared with women; 19.8% versus 7.4% (all cardiac arrests, P<0.001), 32.6% versus 14.9% (VT/VF, P<0.001), and 15.4% versus 5.7% (PEA/asystole, P<0.001), respectively (Figure 1). In women, VT/VF arrests comprised 18.7% of all arrests in 2003 and increased to 20.0% by 2012 (P trend<0.001); in men, the proportion of VT/VF arrests comprised 25.5% of all arrests in 2003, which increased to 28.3% by 2012 (P trend<0.001).
Figure 1.
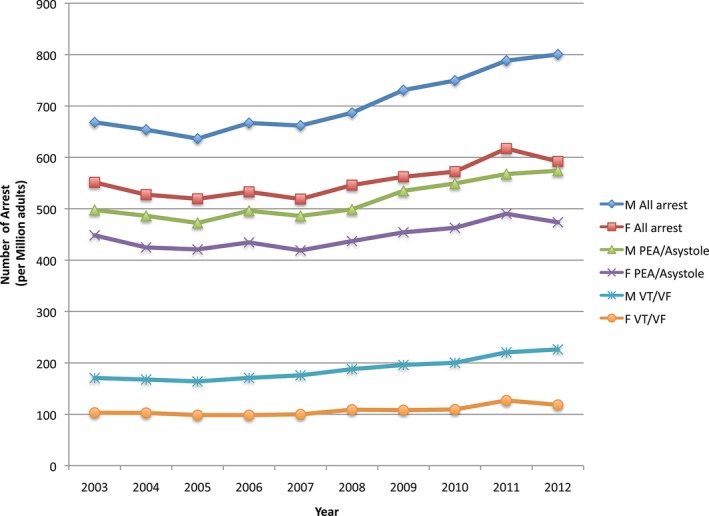
Trends in annual incidence of cardiac arrest by sex, 2003–2012. P trend<0.001 for all except VT/VF arrest; PEA/asystole arrests in women P trend=0.001. PEA indicates pulseless electrical activity; VT/VF, ventricular tachycardia/ventricular fibrillation.
Utilization of Therapeutic Modalities
There was an increase in utilization of coronary angiography, PCI, and TTM in cardiac arrest patients between 2003 and 2012. However, the changes in utilization of coronary procedures were significantly greater in men versus women presenting with cardiac arrests (Figure 2). From 2003 to 2012, the use of coronary angiography increased in men (16.5–19.9%, P trend<0.001) versus women (12.1–13.4%, P trend<0.001), the use of PCI increased in men (7.2–10.1%, P trend<0.001) versus women (4.8–5.8%, P trend<0.001), and the use of TTM increased in men (0–3.2%, P trend<0.001) versus women (0–2.3%, P trend<0.001) (Figure 3). For VT/VF arrests from 2003 to 2012, the use of coronary angiography increased in men (34.6–42.3%, P trend<0.001) versus women (28.4–31.7%, P trend<0.001), the use of PCI increased in men (17.3–24.1%, P trend<0.001) versus women (12.5–14.7%, P trend<0.001), and the use of TTM increased in men (0.1–6.1%, P trend<0.001) versus women (0–4.2%, P trend<0.001). For PEA/asystole arrests from 2003 to 2012 the changes were less pronounced; the use of coronary angiography increased in men (10.4–11.1%, P trend<0.001) versus women (8.4–8.9%, P trend<0.001), the use of PCI increased in men (3.8–4.6%, P trend<0.001) versus women (3.0–3.6%, P trend<0.001), and the use of TTM increased in men (0–2.1%, P trend<0.001) versus women (0–1.8%, P trend<0.001). Furthermore, women were also less likely to receive ventricular assist or intraaortic balloon pump support devices.
Figure 2.
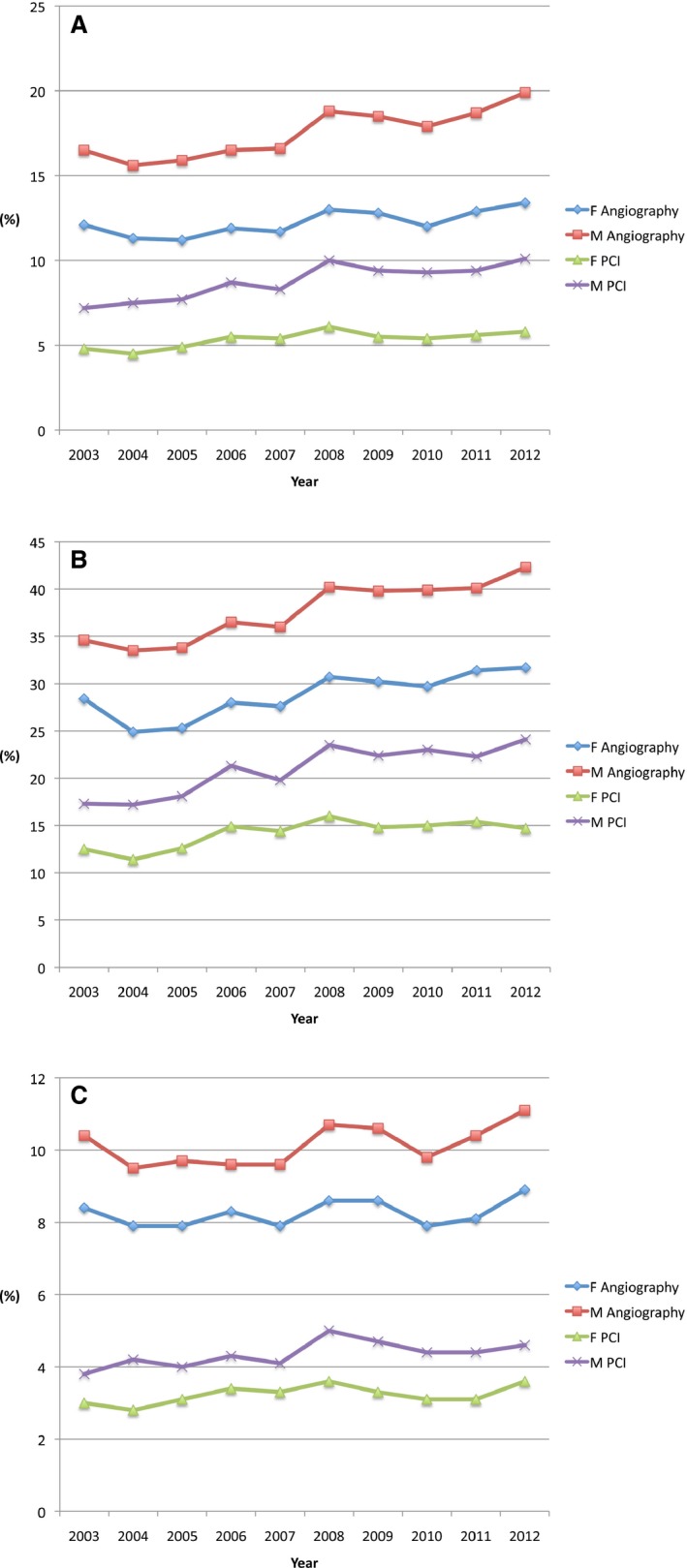
Trends in utilization of coronary angiography and PCI after (A) all cardiac arrests, (B) VT/VF arrests, and (C) PEA/asystole arrests by sex, 2003–2012. A, Angiography indicates coronary angiogram; F, females; M, males; PCI, percutaneous coronary intervention. P trend=0.01 for F Angiography; 0.001 for M Angiography; 0.01 for F PCI; <0.001 for M PCI. B, P trend=0.004 for F Angiography; <0.001 for M Angiography; 0.01 for F PCI; <0.001 for M PCI. C, P trend=0.33 for F Angiography; 0.11 for M Angiography; 0.12 for F PCI; 0.04 for M PCI. PCI indicates percutaneous coronary intervention; PEA, pulseless electrical activity; VT/VF, ventricular tachycardia/ventricular fibrillation.
Figure 3.
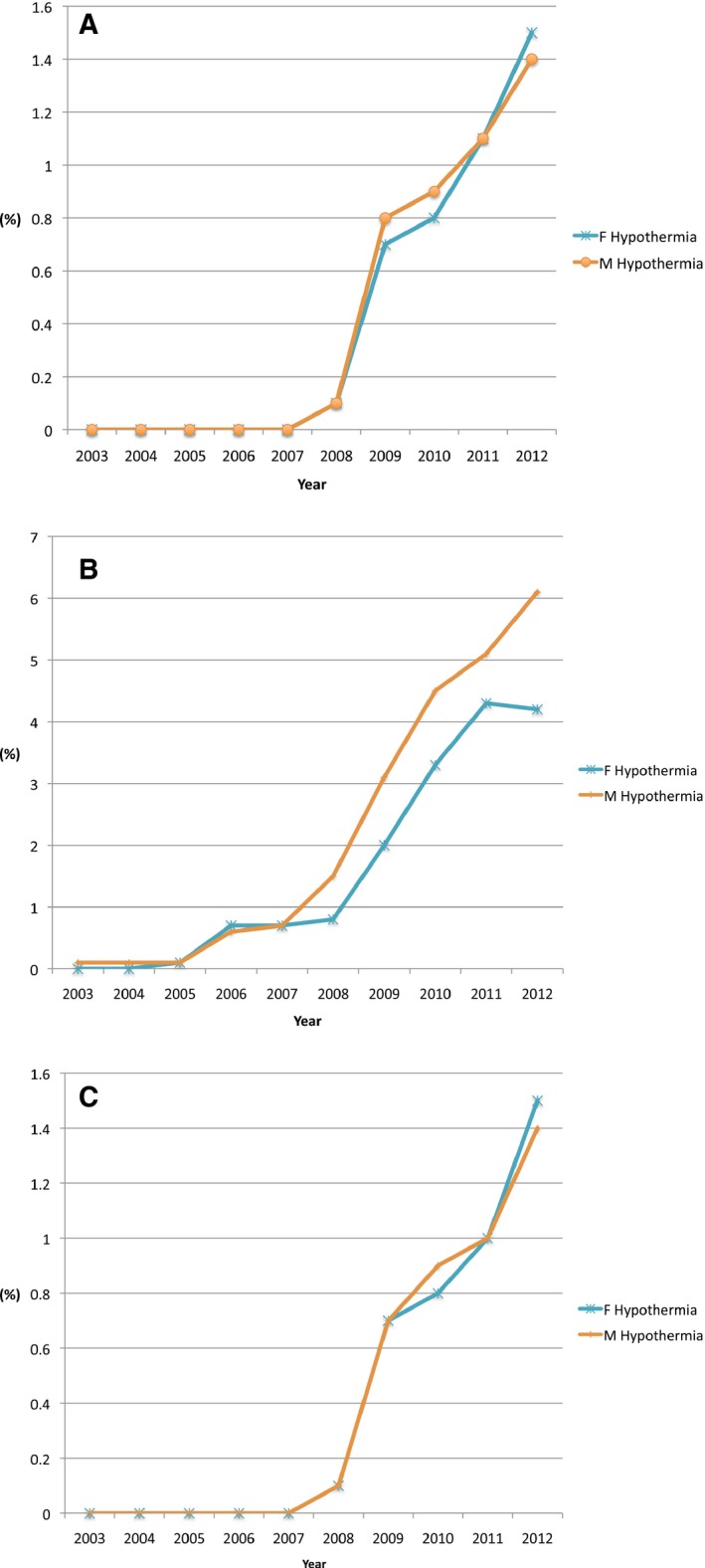
Trends in in‐hospital mortality by sex between 2003 and 2012 for (A) all cardiac arrests, (B) VT/VF arrests, and (C) PEA/asystole arrests. A, P trend<0.001 for all, females and males. B, P trend=0.001 for all; <0.001 for females and males. C, P trend<0.001 for all, females and males. PEA indicates pulseless electrical activity; VT/VF, ventricular tachycardia/ventricular fibrillation.
Table 2 shows the relationship between sex and the likelihood of undergoing coronary angiography, PCI, and TTM interventions. Women were less likely to undergo coronary angiography, PCI, or TTM in all cardiac arrests, VT/VF, and PEA/asystole. After adjustment with multivariate logistic regression analysis, female sex remained associated with less likelihood of undergoing coronary angiography or PCI. In particular, women presenting with VT/VF arrests were 25% less likely to receive coronary angiography and 29% less likely to receive PCI than male patients. Furthermore, female sex was associated with lower odds of receiving TTM in VT/VF arrests (adjusted odds ratio [OR] 0.81, 95% CI 0.76–0.87, P<0.001), but not in PEA/asystole arrests.
Table 2.
Unadjusted and Adjusted Association Between Sex and Likelihood of Undergoing Procedures/In‐Hospital Mortality (Male Sex as the Reference)
| Procedures | Unadjusted OR (95% CI) | P Value | Adjusted OR (95% CI)a | P Value |
|---|---|---|---|---|
| Coronary angiography | ||||
| All arrests | 0.65 (0.65–0.66) | <0.001 | 0.82 (0.81–0.83) | <0.001 |
| VT/VF arrests | 0.66 (0.65–0.67) | <0.001 | 0.75 (0.74–0.77) | <0.001 |
| PEA/asystole arrest | 0.79 (0.78–0.80) | <0.001 | 0.86 (0.85–0.88) | <0.001 |
| PCI | ||||
| All arrests | 0.59 (0.58–0.59) | <0.001 | 0.76 (0.75–0.78) | <0.001 |
| VT/VF arrests | 0.62 (0.61–0.63) | <0.001 | 0.71 (0.69–0.73) | <0.001 |
| PEA/asystole arrest | 0.74 (0.72–0.75) | <0.001 | 0.81 (0.79–0.83) | <0.001 |
| TTM | ||||
| All arrests | 0.73 (0.71–0.76) | <0.001 | 0.90 (0.86–0.94) | 0.001 |
| VT/VF arrests | 0.71 (0.68–0.75) | <0.001 | 0.81 (0.76–0.87) | <0.001 |
| PEA/asystole arrest | 0.90 (0.86–0.94) | <0.001 | 0.99 (0.93–1.05) | 0.810 |
| In‐hospital mortality | ||||
| All arrests | 1.11 (1.11–1.12) | <0.001 | 1.02 (1.01–1.03) | <0.001 |
| VT/VF | 1.17 (1.15–1.18) | <0.001 | 1.11 (1.09–1.13) | <0.001 |
| PEA/asystole | 1.01 (1.00–1.02) | <0.001 | 0.99 (0.98–1.00) | 0.02 |
| TTM | 1.16 (1.09–1.24) | <0.001 | 0.97 (0.88–1.07) | 0.49 |
| PCI | 1.45 (1.41–1.49) | <0.001 | 1.22 (1.18–1.27) | <0.001 |
| VT/VF+PCI | 1.24 (1.19–1.29) | <0.001 | 1.16 (1.10–1.22) | <0.001 |
| VT/VF+PCI+TTM | 1.54 (1.20–1.97) | <0.001 | 2.11 (1.46–3.07) | <0.001 |
OR indicates odds ratio; PCI, percutaneous coronary interventions; PEA, pulseless electrical activity; TTM, targeted temperature management; VT/VF, ventricular tachycardia and ventricular fibrillation/flutter.
The model was adjusted for statistically significant variables that had significant univariate association with outcomes (P<0.01).
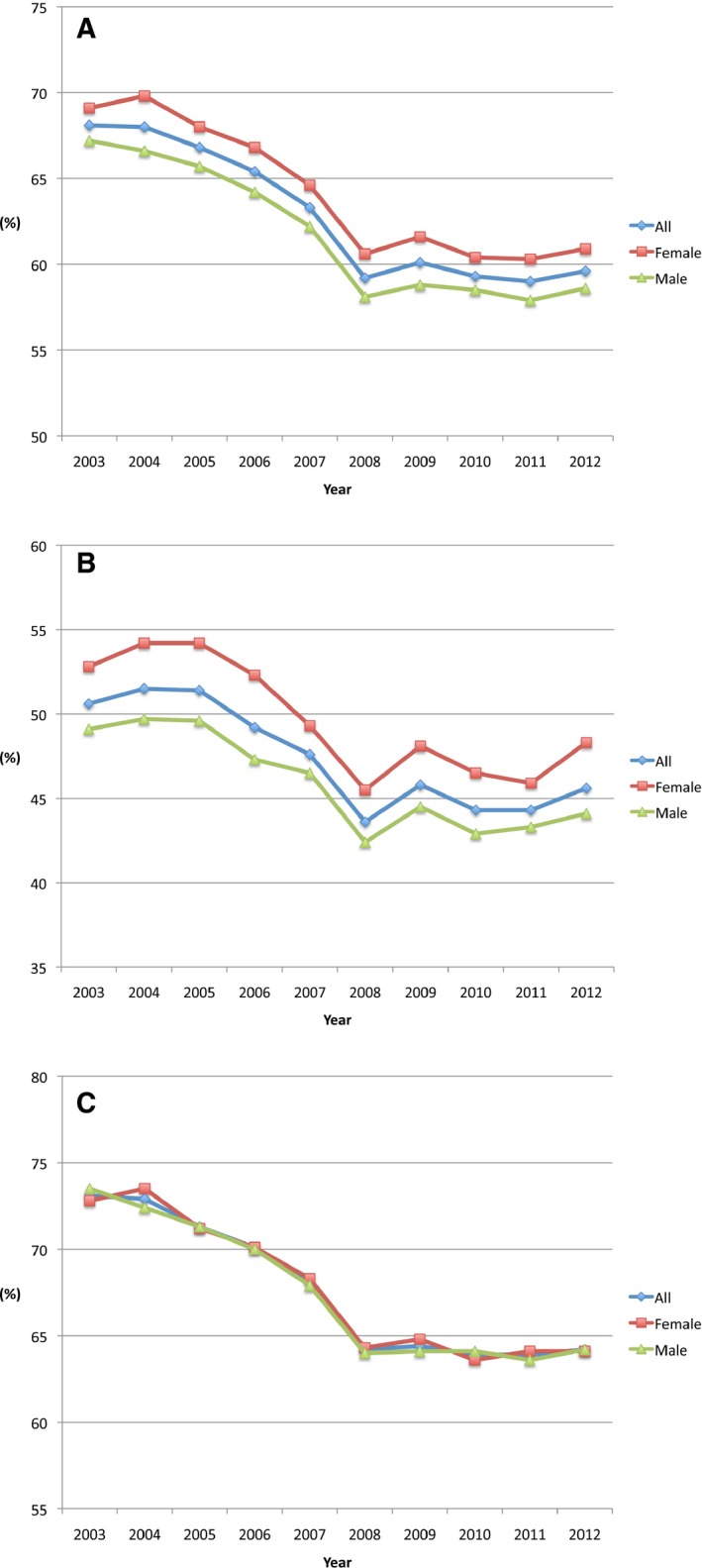
In‐Hospital Outcomes After Cardiac Arrest by Sex
There was a significant reduction in in‐hospital all‐cause mortality from 68.1% to 59.6% (P trend<0.001) between 2003 and 2012 in the overall cardiac arrest cohort (Figure 3). In women, in‐hospital mortality declined from 69.1% in 2003 to 60.9% in 2012 (P trend<0.001), whereas in men in‐hospital mortality declined from 67.2% in 2003 to 58.6% in 2012 (P trend<0.001) (Figure 4). In the VT/VF cohort between 2003 and 2012, in‐hospital mortality declined from 52.8% to 48.3% in women (P trend<0.001), whereas in men in‐hospital mortality was reduced from 49.1% to 44.1% (P trend<0.001).
Figure 4.
Trends in utilization of targeted temperature management after (A) all cardiac arrests, (B) VT/VF arrests, and (C) PEA/asystole arrests by sex, 2003–2012. A, Hypothermia indicates targeted temperature management (TTM); F indicates females; M indicates males. P trend <0.001 for F TTM; <0.001 for M TTM. B, P trend<0.001 for F TTM; <0.001 for M TTM. C, P trend=0.001 for F TTM; <0.001 for M TTM. PEA indicates pulseless electrical activity; VT/VF, ventricular tachycardia/ventricular fibrillation.
Table 2 shows the unadjusted and adjusted association between sex and in‐hospital mortality. In‐hospital mortality was significantly higher in women compared with men in the overall cardiac arrest cohort (64.0% versus 61.4%; adjusted OR 1.02, 95% CI 1.01–1.03, P<0.001), and particularly in the VT/VF arrest cohort (49.4% versus 45.6%; adjusted OR 1.11, 95% CI 1.09–1.13, P<0.001) (Figure 4). Interestingly, in a cohort of patients with VT/VF arrests receiving both PCI and TTM, female sex was associated with even greater risk of mortality compared to men (adjusted OR 2.11, 95% CI 1.46–3.07, P<0.001). Conversely, among all patients receiving TTM, female sex was no longer a predictor of greater mortality.
Discussion
There are several important findings in this nationally representative sample of US hospital discharge records examining sex‐based trends of cardiac arrests, utilization of procedures, and in‐hospital outcomes between the years 2003 and 2012. First, the incidence of cardiac arrests, particularly VT/VF arrests, continues to steadily increase over time, irrespective of sex. Second, women with cardiac arrest were less likely to undergo therapeutic procedures, including coronary angiography, PCI, and TTM. Third, decreasing mortality trends over time were seen in both sexes, although the relative change was smaller for women. Finally, we showed that women had higher postarrest in‐hospital mortality after multivariate adjustment compared with men, particularly for VT/VF arrests. Higher mortality was seen in women with VT/VF arrests despite receiving maximal evidence‐based therapies, including PCI and TTM.
Recent studies examining trends in outcomes after cardiac arrests have demonstrated improving overall survival rates, similar to our finding.4, 23 However, our study is the first to report sex‐based disparities across a representative spectrum of cardiac arrest patients from >1000 US hospitals nationally. Our study suggests that women presenting with cardiac arrests in the United States have important phenotypic differences; they are older, have more comorbid conditions, are less likely to have preexisting coronary artery disease (despite greater prevalence of risk factors for coronary artery disease), less likely to present with STEMI, and less likely to present with a shockable rhythm (19% versus 26%, P<0.001). Lower prevalence of ischemic cause of cardiac arrest is only one of the reasons why women present more often with nonshockable rhythms. Warning symptoms preceding cardiac arrest differ in men and women; women tend to experience more atypical symptoms, such as dyspnea, and less chest pain compared with men.27 Furthermore, identifying the etiology of arrest as ischemic can be quite challenging despite advances in diagnostic tools.28 Our finding that women compared with men are less likely to present with a shockable VT/VF rhythm has been reported in several studies.22, 29, 30 Prior investigations also suggested that women have fewer arrests witnessed by bystanders, and are more likely to present with arrests at home.22, 31 Sex‐based differences in baseline characteristics and type of cardiac arrest are complex and likely multifactorial. Some factors include differences in the prevalence of cardiovascular risk factors and ischemic substrate, initial symptoms upon presentation, time between symptoms and cardiac arrest, whether the arrest was witnessed or unwitnessed, presenting rhythm, time to cardiopulmonary resuscitation and defibrillation, and access to tertiary institutions with experience in resuscitating cardiac arrest patients.
Our study demonstrates that women were less likely to undergo coronary angiography and PCI when they presented with cardiac arrests. This was particularly true for VT/VF arrests, where utilization of angiography and PCI can be of great diagnostic and therapeutic importance given the high prevalence of ischemia‐driven VT/VF in this population. Recent studies examining cardiac arrest have shown an association between immediate coronary angiogram/PCI and improved outcomes.14, 15 Studies addressing sex‐based differences in healthcare delivery have suggested that women are more likely to utilize primary care and preventive services, whereas they are less likely to receive services for acute cardiac conditions.32, 33 For instance, Khera et al demonstrated that women are less likely to receive revascularization for STEMI.33 There may be several reasons for underutilization of angiography and PCI in this national cohort. Women are more likely to present with atypical symptoms prior to cardiac arrest, which may lead to more delayed presentation and underrecognition of ischemia as the etiology of cardiac arrest. Lower rates of angiography and PCI may also be due to higher frequency of alternative etiologies, such as pulmonary embolism. Furthermore, revascularization in women is associated with ≈2‐fold higher bleeding risk,34, 35 which can lead to more reserved use of angiography and PCI, particularly when the etiology of cardiac arrest is not clearly identified.
Our study demonstrated that women had higher risk‐adjusted in‐hospital mortality than men, particularly when presenting with VT/VF arrests. This is in contrast to a recently published meta‐analysis by Bougouin et al, where women were found to have better survival after cardiac arrest.22 It should be noted that our study is the largest report thus far examining the association between sex and survival postarrest, considerably larger than the aforementioned meta‐analysis of 409 323 patients examined in 13 studies. Most of the prior studies suggesting improved survival in women were performed in Japan or Sweden, which greatly differ from US health care in algorithms and access to resuscitative care.29, 36 On the other hand, similar to our analysis, Wong et al in a large Canadian population‐based cohort of 34 291 out‐of‐hospital cardiac arrests showed lower 30‐day unadjusted survival rates in women versus men (30‐day survival: 11.6% women versus 13.8% men in 2010–2011).23 The analysis from prospectively collected data in 29 US cities from the Cardiac Arrest Registry to Enhance Survival suggested that females in the 12‐ to 49‐year‐old age group had the largest association with improved survival to hospital discharge (OR 1.55, 95% CI 1.20–2.00).37 However, this association was no longer present in women after age >55 years. Given that the mean age of women in our data set was 67, the association with poor survival to discharge in our cohort is not completely unexpected.
Lower use of angiography and revascularization cannot be the only reason to explain higher in‐hospital mortality in women in our analysis. In a subgroup of VT/VF arrests treated with PCI and TTM, risk‐adjusted mortality was still higher in women than men (adjusted OR 2.11, P<0.001). As mentioned earlier, other negative prognostic features reported in women include lower prevalence of initial shockable rhythm, less bystander‐witnessed arrests, and more arrests at home. Lower utilization of angiography/PCI in women is likely related to the aforementioned factors, prolonged time to resuscitation, and frequently unknown postarrest neurological status. Additional potential reasons for higher mortality include lower use of adjunctive guideline‐driven medical therapies in women presenting with STEMI,38, 39 treatment delays post–hospital arrival, delays in door‐to‐electrocardiography, door‐to‐needle, and door‐to‐balloon times.33, 40 Furthermore, survival bias may lead to higher observed mortality seen in women. This is supported by data from Dudas et al, which suggested that men are more likely to die before arrival to the hospital than women.41 Future studies will need to identify other reasons for sex‐based disparities in risk‐adjusted mortality, which may include differences in comorbidities, presenting symptoms, basic and advanced life support, utilization of medical therapies and revascularization, and unmeasured covariates. This has been the focus of the recent report from the Institute of Medicine's Strategies to Improve Cardiac Arrest Survival: A Time to Act (2015), supported by the American Heart Association; American Red Cross; American College of Cardiology; National Heart, Lung, and Blood Institute; Centers for Disease Control and Prevention; and Department of Veterans Affairs.42 Several multisocietal efforts to increase cardiac arrest survival are currently being reexamined, including establishing a national cardiac arrest registry, setting national accreditation standards related to cardiac arrest for hospitals, adopting continuous quality improvement programs, and creating a national cardiac arrest collaborative.42, 43 Moreover, the trend for decreasing mortality may be due in part to growing public awareness of cardiac arrest, more widespread distribution of automated external defibrillators, streamlining treatment algorithms, and increasing use of TTM.44
TTM is a strategy that has been demonstrated to improve survival to hospital discharge and improve neurologic and cognitive recovery postarrest.45 Recent studies have suggested that combination of early coronary angiography with TTM was associated with improved outcomes after cardiac arrest.46 Given the body of beneficial data, the American College of Cardiology/American Heart Association guidelines give TTM a Class I recommendation for successfully resuscitated patients with VT/VF arrest and a Class IIb recommendation for other types of rhythms.47 Similarly, the European guidelines advocate the use of TTM in patients with shockable rhythms, with a more reserved recommendation in patients without a shockable rhythm.48 Despite widespread implementation of TTM since the publication of original trials,6, 7 there is paucity of data regarding real‐world utilization of TTM. Dresden et al showed that, although rates of TTM use after cardiac arrest are slowly increasing, they remain low (2.5% in 2010), with only 22% of US hospitals providing TTM.49 Furthermore, there is also wide variability in the use of TTM after cardiac arrest.45 A secondary analysis of the Resuscitation Outcomes Consortium Prehospital Resuscitation using an IMpedance valve and Early versus Delayed (ROC‐PRIMED) trial demonstrated that the proportion of patients treated with TTM varied between hospitals (range 0–83%) and was higher in hospitals treating more subjects per year.50 Our study demonstrated increasing use of TTM over time, particularly for VT/VF arrests. Despite this encouraging finding, the utilization of TTM in women presenting with VT/VF arrests still lags far behind compared with men. Our study is the first to report sex disparity in the utilization of TTM, particularly in the VT/VF cohort. Importantly, in those who receive TTM, risk‐adjusted mortality rates were similar between men and women. Given the current level of evidence and Class I recommendation for TTM use in VT/VF arrests, it is concerning to see sex‐based discrepancy in the frequency of TTM utilization. Given that TTM has been an important addition towards improving survival and neurologic recovery postarrest, further efforts by the medical community are needed to close a sex‐based gap in providing TTM postarrest.
There are several limitations present in our study. First, this is a retrospective study based on a NIS sample that approximates the national distribution of key hospital characteristics. The results should be considered hypothesis‐generating, since we cannot infer causality. Our estimates for cardiac arrests were derived from a representative 20% sample of US hospitals, and it is possible that the number of arrests was either underrepresented or overrepresented by the sample. However, NIS has been used extensively to examine national healthcare trends, and its sampling design has been validated in numerous publications.51 Second, unmeasured confounders could not be accounted for, including initial symptoms upon presentation, time between symptoms and cardiac arrest, whether the arrest was witnessed or unwitnessed, time to cardiopulmonary resuscitation and defibrillation, varying severity of patient characteristics, ejection fraction, medications, hemodynamic data, and presence and severity of coronary artery disease. This may have impacted unmeasured confounders that could not be accounted for in our adjustment models. However, a more detailed exploration of the impact of such confounder drivers is beyond the scope of this analysis. Third, survival bias may lead to higher observed mortality seen in women. Lastly, both out‐of‐hospital and in‐hospital arrests were included in this study. The ICD‐9‐CM codes were used to assess the incidence of cardiac arrests, which may have underestimated the true incidence of these events. However, our goal was to compare sex‐based differences in incidence, utilization of procedures, and outcomes postarrest. Therefore, one would presume that potential undercoding would affect men and women equally and thus have minimal effect on the results of this study.
In conclusion, there was a steady increase in the incidence of cardiac arrests in US hospitals between 2003 and 2012, particularly VT/VF arrests. Women were less likely than men to undergo coronary angiography, PCI, and TTM postarrest. Women had higher risk‐adjusted in‐hospital mortality than men, particularly after VT/VF arrests. These data present an opportunity to improve national cardiac arrest processes and outcomes, and to focus on reducing sex‐based disparities in caring for postarrest patients.
Sources of Funding
This work was supported by grants from the Michael Wolk Heart Foundation and the New York Cardiac Center, Inc. The Michael Wolk Heart Foundation and the New York Cardiac Center, Inc. had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Disclosures
Dr Feldman has received consulting/speaker's fees from Eli Lilly, Daiichi‐Sankyo, Abbott Vascular, Pfizer, and Bristol‐Myers Squibb. The other authors report no conflicts.
(J Am Heart Assoc. 2016;5:e003704 doi: 10.1161/JAHA.116.003704)
References
- 1. Centers for Disease Control and Prevention . 2013 cardiac arrest registry to enhance survival (CARES) national summary report. Available at: https://mycares.net/sitepages/uploads/2014/2013CARESNationalSummaryReport.pdf. Accessed November 11, 2015.
- 2. Rosamond WD, Chambless LE, Folsom AR, Cooper LS, Conwill DE, Clegg L, Wang CH, Heiss G. Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med. 1998;339:861–867. [DOI] [PubMed] [Google Scholar]
- 3. Vaughan AS, Quick H, Pathak EB, Kramer MR, Casper M. Disparities in temporal and geographic patterns of declining heart disease mortality by race and sex in the United States, 1973–2010. J Am Heart Assoc. 2015;4:e002567 doi: 10.1161/JAHA.115.002567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chan PS, McNally B, Tang F, Kellermann A; CARES Surveillance Group . Recent trends in survival from out‐of‐hospital cardiac arrest in the United States. Circulation. 2014;130:1876–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I; Resuscitation Outcomes Consortium Investigators . Regional variation in out‐of‐hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bouwes A, Binnekade JM, Kuiper MA, Bosch FH, Zandstra DF, Toornvliet AC, Biemond HS, Kors BM, Koelman JH, Verbeek MM, Weinstein HC, Hijdra A, Horn J. Prognosis of coma after therapeutic hypothermia: a prospective cohort study. Ann Neurol. 2012;71:206–212. [DOI] [PubMed] [Google Scholar]
- 7. Holzer M, Bernard SA, Hachimi‐Idrissi S, Roine RO, Sterz F, Müllner M; Collaborative Group on Induced Hypothermia for Neuroprotection After Cardiac Arrest . Hypothermia for neuroprotection after cardiac arrest: systematic review and individual patient data meta‐analysis. Crit Care Med. 2005;33:414–418. [DOI] [PubMed] [Google Scholar]
- 8. Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, Jans H, Hansen PA, Lang‐Jensen T, Olesen JB, Lindhardsen J, Fosbol EL, Nielsen SL, Gislason GH, Kober L, Torp‐Pedersen C. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out‐of‐hospital cardiac arrest. JAMA. 2013;310:1377–1384. [DOI] [PubMed] [Google Scholar]
- 9. Malta Hansen C, Kragholm K, Pearson DA, Tyson C, Monk L, Myers B, Nelson D, Dupre ME, Fosbøl EL, Jollis JG, Strauss B, Anderson ML, McNally B, Granger CB. Association of bystander and first‐responder intervention with survival after out‐of‐hospital cardiac arrest in North Carolina, 2010–2013. JAMA. 2015;314:255–264. [DOI] [PubMed] [Google Scholar]
- 10. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out‐of‐hospital cardiac arrest: a systematic review and meta‐analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. [DOI] [PubMed] [Google Scholar]
- 11. Hansen CM, Kragholm K, Granger CB, Pearson DA, Tyson C, Monk L, Corbett C, Nelson RD, Dupre ME, Fosbøl EL, Strauss B, Fordyce CB, McNally B, Jollis JG. The role of bystanders, first responders, and emergency medical service providers in timely defibrillation and related outcomes after out‐of‐hospital cardiac arrest: results from a statewide registry. Resuscitation. 2015;96:303–309. [DOI] [PubMed] [Google Scholar]
- 12. Hypothermia After Cardiac Arrest Study Group . Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–556. [DOI] [PubMed] [Google Scholar]
- 13. Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out‐of‐hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. [DOI] [PubMed] [Google Scholar]
- 14. Geri G, Dumas F, Bougouin W, Varenne O, Daviaud F, Pène F, Lamhaut L, Chiche JD, Spaulding C, Mira JP, Empana JP, Cariou A. Immediate percutaneous coronary intervention is associated with improved short‐ and long‐term survival after out‐of‐hospital cardiac arrest. Circ Cardiovasc Interv. 2015;8:e002303 doi: 10.1161/CIRCINTERVENTIONS.114.002303. [DOI] [PubMed] [Google Scholar]
- 15. Kern KB, Lotun K, Patel N, Mooney MR, Hollenbeck RD, McPherson JA, McMullan PW, Unger B, Hsu CH, Seder DB; INTCAR‐Cardiology Registry . Outcomes of comatose cardiac arrest survivors with and without ST‐segment elevation myocardial infarction: importance of coronary angiography. JACC Cardiovasc Interv. 2015;8:1031–1040. [DOI] [PubMed] [Google Scholar]
- 16. Pollock B, Hamman BL, Sass DM, da Graca B, Grayburn PA, Filardo G. Effect of gender and race on operative mortality after isolated coronary artery bypass grafting. Am J Cardiol. 2015;115:614–618. [DOI] [PubMed] [Google Scholar]
- 17. Bavishi C, Bangalore S, Patel D, Chatterjee S, Trivedi V, Tamis‐Holland JE. Short and long‐term mortality in women and men undergoing primary angioplasty: a comprehensive meta‐analysis. Int J Cardiol. 2015;198:123–130. [DOI] [PubMed] [Google Scholar]
- 18. Greenberg MR, Ahnert AM, Patel NC, Bennett CE, Elliott N, Lundquist M, Miller A, Feiner EC, Kurt A, Glenn‐Porter B, Scott M, Burmeister DB. Sex differences in cardiac arrest survivors who receive therapeutic hypothermia. Am J Emerg Med. 2014;32:545–548. [DOI] [PubMed] [Google Scholar]
- 19. Winther‐Jensen M, Kjaergaard J, Wanscher M, Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Friberg H, Gasche Y, Horn J, Hovdenes J, Kuiper M, Pellis T, Stammet P, Wise MP, Åneman A, Hassager C. No difference in mortality between men and women after out‐of‐hospital cardiac arrest. Resuscitation. 2015;96:78–84. [DOI] [PubMed] [Google Scholar]
- 20. Karlsson V, Dankiewicz J, Nielsen N, Kern KB, Mooney MR, Riker RR, Rubertsson S, Seder DB, Stammet P, Sunde K, Søreide E, Unger BT, Friberg H. Association of gender to outcome after out‐of‐hospital cardiac arrest—a report from the International Cardiac Arrest Registry. Crit Care. 2015;19:182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wissenberg M, Hansen CM, Folke F, Lippert FK, Weeke P, Karlsson L, Rajan S, Søndergaard KB, Kragholm K, Christensen EF, Nielsen SL, Køber L, Gislason GH, Torp‐Pedersen C. Survival after out‐of‐hospital cardiac arrest in relation to sex: a nationwide registry‐based study. Resuscitation. 2014;85:1212–1218. [DOI] [PubMed] [Google Scholar]
- 22. Bougouin W, Mustafic H, Marijon E, Murad MH, Dumas F, Barbouttis A, Jabre P, Beganton F, Empana JP, Celermajer DS, Cariou A, Jouven X. Gender and survival after sudden cardiac arrest: a systematic review and meta‐analysis. Resuscitation. 2015;94:55–60. [DOI] [PubMed] [Google Scholar]
- 23. Wong MK, Morrison LJ, Qiu F, Austin PC, Cheskes S, Dorian P, Scales DC, Tu JV, Verbeek PR, Wijeysundera HC, Ko DT. Trends in short‐ and long‐term survival among out‐of‐hospital cardiac arrest patients alive at hospital arrival. Circulation. 2014;130:1883–1890. [DOI] [PubMed] [Google Scholar]
- 24. HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2003‐2011. Available at: www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed November 29, 2015. [Google Scholar]
- 25. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 26. US Census Bureau: population estimates and demographic components of change by age, sex, race, & Hispanic origin for the United States 2011. Available at: https://www.census.gov/popest/data/historical/2010s/vintage_2011/index.html. Accessed October 1, 2014.
- 27. Marijon E, Uy‐Evanado A, Dumas F, Karam N, Reinier K, Teodorescu C, Narayanan K, Gunson K, Jui J, Jouven X, Chugh SS. Warning symptoms are associated with survival from sudden cardiac arrest. Ann Intern Med. 2016;164:23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vavas E, Hong SN, Rosen SE, Mieres JH. Noninvasive diagnostic techniques for coronary disease in women. Clin Cardiol. 2012;35:149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kitamura T, Iwami T, Nichol G, Nishiuchi T, Hayashi Y, Nishiyama C, Sakai T, Kajino K, Hiraide A, Ikeuchi H, Nonogi H, Kawamura T; Utstein Osaka Project . Reduction in incidence and fatality of out‐of‐hospital cardiac arrest in females of the reproductive age. Eur Heart J. 2010;31:1365–1372. [DOI] [PubMed] [Google Scholar]
- 30. Kim C, Fahrenbruch CE, Cobb LA, Eisenberg MS. Out‐of‐hospital cardiac arrest in men and women. Circulation. 2001;104:2699–2703. [DOI] [PubMed] [Google Scholar]
- 31. Pell JP, Sirel J, Marsden AK, Cobbe SM. Sex differences in outcome following community‐based cardiopulmonary arrest. Eur Heart J. 2000;21:239–244. [DOI] [PubMed] [Google Scholar]
- 32. Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 2000;49:147–152. [PubMed] [Google Scholar]
- 33. Khera S, Kolte D, Gupta T, Subramanian KS, Khanna N, Aronow WS, Ahn C, Timmermans RJ, Cooper HA, Fonarow GC, Frishman WH, Panza JA, Bhatt DL. Temporal trends and sex differences in revascularization and outcomes of ST‐segment elevation myocardial infarction in younger adults in the United States. J Am Coll Cardiol. 2015;66:1961–1972. [DOI] [PubMed] [Google Scholar]
- 34. Mehran R, Pocock SJ, Nikolsky E, Clayton T, Dangas GD, Kirtane AJ, Parise H, Fahy M, Manoukian SV, Feit F, Ohman ME, Witzenbichler B, Guagliumi G, Lansky AJ, Stone GW. A risk score to predict bleeding in patients with acute coronary syndromes. J Am Coll Cardiol. 2010;55:2556–2566. [DOI] [PubMed] [Google Scholar]
- 35. Feldman DN, Swaminathan RV, Kaltenbach LA, Baklanov DV, Kim LK, Wong SC, Minutello RM, Messenger JC, Moussa I, Garratt KN, Piana RN, Hillegass WB, Cohen MG, Gilchrist IC, Rao SV. Adoption and outcomes of radial approach to percutaneous coronary intervention: an updated report from the National Cardiovascular Data Registry (2007–2012). Circulation. 2013;127:2295–2306. [DOI] [PubMed] [Google Scholar]
- 36. Adielsson A, Hollenberg J, Karlsson T, Lindqvist J, Lundin S, Silfverstolpe J, Svensson L, Herlitz J. Increase in survival and bystander CPR in out‐of‐hospital shockable arrhythmia: bystander CPR and female gender are predictors of improved outcome. Experiences from Sweden in an 18‐year perspective. Heart. 2011;97:1391–1396. [DOI] [PubMed] [Google Scholar]
- 37. Johnson MA, Haukoos JS, Larabee TM, Daugherty S, Chan PS, McNally B, Sasson C. Females of childbearing age have a survival benefit after out‐of‐hospital cardiac arrest. Resuscitation. 2013;84:639–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Izadnegahdar M, Norris C, Kaul P, Pilote L, Humphries KH. Basis for sex‐dependent outcomes in acute coronary syndrome. Can J Cardiol. 2014;30:713–720. [DOI] [PubMed] [Google Scholar]
- 39. Bangalore S, Fonarow GC, Peterson ED, Hellkamp AS, Hernandez AF, Laskey W, Peacock WF, Cannon CP, Schwamm LH, Bhatt DL; Get with the Guidelines Steering Committee and Investigators . Age and gender differences in quality of care and outcomes for patients with ST‐segment elevation myocardial infarction. Am J Med. 2012;125:1000–1009. [DOI] [PubMed] [Google Scholar]
- 40. Leurent G, Garlantézec R, Auffret V, Hacot JP, Coudert I, Filippi E, Rialan A, Moquet B, Rouault G, Gilard M, Castellant P, Druelles P, Boulanger B, Treuil J, Avez B, Bedossa M, Boulmier D, Le Guellec M, Le Breton H. Gender differences in presentation, management and in‐hospital outcome in patients with ST segment elevation myocardial infarction: data from 5000 patients included in the ORBI prospective French regional registry. Arch Cardiovasc Dis. 2014;107:291–298. [DOI] [PubMed] [Google Scholar]
- 41. Dudas K, Lappas G, Stewart S, Rosengren A. Trends in out‐of‐hospital deaths due to coronary heart disease in Sweden (1991 to 2006). Circulation. 2011;123:46–52. [DOI] [PubMed] [Google Scholar]
- 42. Institute of Medicine's Strategies to Improve Cardiac Arrest Survival: A Time to Act. Washington, DC: The National Academies Press; 2015. Available at: http://www.nap.edu/read/21723/chapter/2. Accessed December 1, 2015. [PubMed] [Google Scholar]
- 43. Neumar RW, Eigel B, Callaway CW, Estes NA III, Jollis JG, Kleinman ME, Morrison LJ, Peberdy MA, Rabinstein A, Rea TD, Sendelbach S. American Heart Association response to the 2015 Institute of Medicine report on strategies to improve cardiac arrest survival. Circulation. 2015;132:1049–1070. [DOI] [PubMed] [Google Scholar]
- 44. Blom MT, Beesems SG, Homma PC, Zijlstra JA, Hulleman M, van Hoeijen DA, Bardai A, Tijssen JG, Tan HL, Koster RW. Improved survival after out‐of‐hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130:1868–1875. [DOI] [PubMed] [Google Scholar]
- 45. Maznyczka AM, Gershlick AH. Therapeutic hypothermia in patients with out‐of‐hospital arrest. Heart. 2015;101:1265–1271. [DOI] [PubMed] [Google Scholar]
- 46. Callaway CW, Schmicker RH, Brown SP, Albrich JM, Andrusiek DL, Aufderheide TP, Christenson J, Daya MR, Falconer D, Husa RD, Idris AH, Ornato JP, Rac VE, Rea TD, Rittenberger JC, Sears G, Stiell IG; ROC Investigators . Early coronary angiography and induced hypothermia are associated with survival and functional recovery after out‐of‐hospital cardiac arrest. Resuscitation. 2014;85:657–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions , O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis‐Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW. 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–e140. [DOI] [PubMed] [Google Scholar]
- 48. Nolan JP, Soar J, Cariou A, Cronberg T, Moulaert VR, Deakin CD, Bottiger BW, Friberg H, Sunde K, Sandroni C. European Resuscitation Council and European Society of Intensive Care Medicine guidelines for post‐resuscitation care 2015: section 5 of the European Resuscitation Council guidelines for resuscitation 2015. Resuscitation. 2015;95:202–222. [DOI] [PubMed] [Google Scholar]
- 49. Dresden SM, O'Connor LM, Pearce CG, Courtney DM, Powell ES. National trends in the use of postcardiac arrest therapeutic hypothermia and hospital factors influencing its use. Ther Hypothermia Temp Manag. 2015;5:48–54. [DOI] [PubMed] [Google Scholar]
- 50. Stub D, Schmicker RH, Anderson ML, Callaway CW, Daya MR, Sayre MR, Elmer J, Grunau BE, Aufderheide TP, Lin S, Buick JE, Zive D, Peterson ED, Nichol G; ROC Investigators . Association between hospital post‐resuscitative performance and clinical outcomes after out‐of‐hospital cardiac arrest. Resuscitation. 2015;92:45–52. [DOI] [PubMed] [Google Scholar]
- 51. Kim LK, Yang DC, Swaminathan RV, Minutello RM, Okin PM, Lee MK, Sun X, Wong SC, McCormick DJ, Bergman G, Allareddy V, Singh H, Feldman DN. Comparison of trends and outcomes of carotid artery stenting and endarterectomy in the United States, 2001 to 2010. Circ Cardiovasc Interv. 2014;7:692–700. [DOI] [PubMed] [Google Scholar]


