Abstract
Mindfulness meditation represents a mental training framework for cultivating the state of mindful awareness in daily life. Recently, there has been a surge of interest in how mindfulness meditation improves human health and well-being. Although studies have shown that mindfulness meditation can improve self-reported measures of disease symptomatology, the effect that mindfulness meditation has on biological mechanisms underlying human aging and disease is less clear. To address this issue, we conducted the first comprehensive review of randomized controlled trials examining the effects of mindfulness meditation on immune system parameters, with a specific focus on five outcomes: (1) circulating and stimulated inflammatory proteins, (2) cellular transcription factors and gene expression, (3) immune cell count, (4) immune cell aging, and (5) antibody response. This analysis revealed substantial heterogeneity across studies with respect to patient population, study design, and assay procedures. The findings suggest possible effects of mindfulness meditation on specific markers of inflammation, cell-mediated immunity, and biological aging, but these results are tentative and require further replication. On the basis of this analysis, we describe the limitations of existing work and suggest possible avenues for future research. Mindfulness mediation may be salutogenic for immune system dynamics, but additional work is needed to examine these effects.
Keywords: mindfulness, meditation, intervention, immune system, inflammation, biology, cytokines, aging, health, disease
Introduction
Mindfulness is an intrinsic and modifiable capacity of the human mind. As a state and process of consciousness, it is most commonly defined as “the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment” (p. 145).1 Mindfulness meditation, in turn, represents a systematic framework and process for cultivating mindfulness in daily life by intentional and sustained practice.
Several standardized programs have been developed for cultivating mindfulness meditation, with the goal of realizing its potential benefits for human health and well-being. Credit is ordinarily assigned to the 1970s Mindfulness-Based Stress Reduction (MBSR) program as the first standardized mindfulness-based intervention (MBI). These programs are based on secularized teachings from various historical mindfulness meditation traditions, especially eastern humanistic contemplative traditions rooted in the cultivation of personal insight and wisdom.2,3 To reduce symbolic dissonance and surmount cultural barriers to access and participation, MBIs serve as a template for translating ancient teachings into a language and practice that is acceptable and easily understood by contemporary society.
The presence of MBIs in major healthcare settings is at an all-time high. Indeed, almost 80% of the 140 accredited medical schools or their associated universities in the United States presently incorporate MBIs into their treatment, education, and/or research programs.4 Reviews of randomized controlled trials (RCTs) have shown that MBIs can exert some beneficial effects on stress-related ailments, psychiatric disorders, and disease symptomatology.5–9 However, mindfulness meditation is not regarded as a therapeutic panacea for all ailments, and the effects of MBIs on health appear similar in magnitude to those demonstrated by other conventional approaches for treating stress, pain, and illness, including the administration of psychoactive medications, psychotherapy, health education, and behavior modification.6,10–15 MBIs nevertheless enjoy increasing appeal, stemming from a mix of promising empirical evidence, a modern medicine paradigm that increasingly emphasizes the role of patients as active and accountable participants in health care (e.g., self-management of disease and engagement in preventive behaviors),16–18 and a growing emphasis on transtherapeutic interventions.19
So far, the research base documenting the effectiveness of MBIs relies heavily on participants’ self-reports of their own health status, which can be prone to bias.2,8,10,20 A more recent, yet relatively small, literature also exists examining how MBIs affect objective biological markers of human health,21 but to date, no comprehensive literature reviews have been conducted to evaluate how mindfulness meditation influences biological processes that are most proximally relevant for disease pathogenesis. Markers of immune system activity are particularly relevant in this context, given that immune system dynamics have been implicated in several major mental and physical health problems, including asthma, rheumatoid arthritis, metabolic disorders, neurodegenerative disorders, certain types of cancer, posttraumatic stress disorder, and depression.22,23 Therefore, in the present review, we examined the question of whether MBIs can influence peripheral biomarkers of immune system activity.
To conduct this review, we performed a comprehensive literature search that involved identifying all of the RCTs that tested the effects of mindfulness meditation on immune system biomarkers. We focused specifically on five immune system outcomes that are relevant for health, namely: (1) circulating and stimulated inflammatory proteins, (2) cellular transcription factors and gene expression, (3) immune cell count, (4) immune cell aging, and (5) antibody response. Below, we describe the methods and results of this systematic review. We then discuss the findings and highlight lingering issues and possible avenues for future research in order to help advance the goal of better understanding how mindfulness meditation may shape biological aging and disease.
Literature review methods and findings
We scanned all potentially relevant articles published between January 1966 and July 2015 to examine the literature on mindfulness meditation and immune system activity. The year 1966 was selected as a start date because this was when the first empirical paper on mindfulness meditation appeared. The terms immune, inflammation, cytokine, proinflammatory, biomarker, blood, saliva, urine, telomere, and infection were used to search the American Mindfulness Research Association’s publication database (www.goAMRA.org), which archives over 4000 published journal articles, pulling from comprehensive monthly literature searches of PubMed, Ovid, PsycINFO, Web of Science, and Google Scholar. Citations were also received from researchers in the field, and table-of-content searches were conducted for topic-specific journals. In addition to the computer-assisted searches, bibliographies of previous publications on the topic were screened for relevant articles. When required, authors were contacted to clarify details regarding their study methods or blood sampling protocols. Articles were included if they: (1) used an RCT design, (2) administered mindfulness meditation as the main intervention element, (3) objectively assessed a biomarker of immune-related activity, and (4) were published in English.
Description of the field of work
Included studies
A total of 20 RCT studies met the inclusion criteria above and were thus included (Table 1). Two studies resulted in multiple publications, but these data were only counted once (Table 1; Study column). The mean sample size of these 20 studies was n = 80 (range: 21–201), and a total of 1602 participants were included in the analysis.
Table 1.
Randomized controlled trials reporting the effects of mindfulness meditation on immune system parameters
| Reference | Main purpose of study | Analysis sample (n) | Comparator/control group | Participants | Intervention description | Specimen collection | Immune-related findings |
|---|---|---|---|---|---|---|---|
| Barrett et al.;24 Hayney et al.44 | Test effect of mindful meditation or exercise on incidence, duration, and severity of acute respiratory infection illness | 149 | Moderate-intensity exercisea; waiting list | Older community adults; 82% female; ages 59.3 ± 6.6 years | MBSR-derived; 8 weekly 2.5-h group sessions | Nasal wash; blood (serum, PBMCs) with influenza vaccine | >IL-8; ~neutrophils; ~virus prevalence; ~IgA, ~IgG; ~IFN-γ; ~IL-10 |
| Black et al.12,75 | Test effect of mindful meditation or sleep hygiene on sleep quality in older adults | 49 | Sleep hygiene educationa | Community adults; 67% female; ages 66.3 ± 7.4 years | MAPs; 6 weekly 2-h group sessions | Blood (PBMCs) | <NF-κB (both groups) |
| Bower et al.37 | Test effect of mindful meditation on stress and depressive symptoms in women diagnosed with early-stage breast cancer | 71 | Waiting list | Breast cancer patients; 100% female; ages 46.1 (± 28.4–60 range) years | MAPs; 6 weekly 2-h group sessions | Blood (PBMCs, plasma) | <NF-κB; >IFN-1; <IL-6 (dependent on practice dosage); ~CRP; ~sTNF-RII |
| Carlson et al.65 | Test effect of mindful meditation or group therapy/stress management on telomere length in distressed breast cancer survivors | 88 | Supportive-expressive group therapya; 1-day stress management seminar | Breast cancer survivors; 100% female; ages 54.4 ± 9.0 years | MBSR-derived; 8 weekly 1.5-h group sessions + retreat | Blood (WBCs) | >telomere length (trend for attenuated decrease when treatment groups combined vs. seminar) |
| Creswell et al.59 | Test effect of mindful meditation on CD4+ T lymphocyte declines in distressed HIV+ adults | 48 | 1-day stress education seminar | HIV-1+ community adults; 9% female; ages 40.0 ± 9.0 years | MBSR; 8 weekly 2-h group sessions + retreat | Blood (plasma) | >CD4+ T lymphocyte count (buffered decline vs. controls) |
| Creswell et al.38 | Test effect of mindful meditation on loneliness in older adults | 40 | Waiting list | Lonely older adults; 80% female; ages 64.4 ± 6.0 years | MBSR; 8 weekly 2-h group sessions + retreat | Blood (PBMCs, plasma) | <NF-κB; <CRP (trend); ~IL-6 |
| Daubenmier et al.67 | Test effect of mindful meditation on telomerase activity in overweight and obese women | 37 | Waiting list | Overweight/obese women; 100% female; ages not indicated | MBSR-derived; 9 weekly 2.5-h group sessions + retreat | Blood (PBMCs) | >telomerase activity (trend dependent on practice dosage) |
| Davidson et al.73 | Test effect of mindful meditation on brain and immune function | 41 | Waiting list | Corporate employees; 71% female; ages 36.0 (± 23–56 range) years | MBSR; 8 weekly 2.5-h group sessions + retreat | Blood (serum) with influenza vaccine | >Influenza antibodies |
| Elsenbruch et al.43 | Test effect of mindful meditation + multimodality program on neuroendocrine and immune measures in patients with ulcerative colitis | 30 | Waiting list | Ulcerative colitis patients; 50% female; ages 42.9 ± 8.6 years | MBSR + mind–body program; 10 weekly 6-h group sessions | Blood (EDTA whole stimulated) | <TNF-α (trend) |
| Fogarty et al.46 | Test effect of mindful meditation on disease activity in rheumatoid arthritis patients | 42 | Waiting list | Rheumatoid arthritis patients; 88% female; ages 52.0 ± 12.0 years | MBSR; 8 weekly group sessions; hours not indicated | Blood (serum) | ~CRP |
| Gonzalez-Garcia et al.60 | Test effect of mindful meditation on quality of life, emotional status, and immune status among long-term HIV patients | 35 | Usual care | HIV+ patients; 49% female; ages 49.4 ± 5.2 years | MBCT; 8 weekly 2.5-h group sessions | Blood (WBCs) | >CD4+ T lymphocyte count (up 3 months) |
| Jacobs et al.68 | Test effect of meditation practice on immune cell telomerase activity | 46 | Waiting list | Meditation retreat participants; 53% female; ages 49.0 (± 23–69 range) years | Mindfulness, compassion, and equanimity meditations; 3-month group residential retreat | Blood (PBMCs) | >telomerase activity |
| Jedel et al.39 | Test effect of mindful meditation on flare ups and quality of life in ulcerative colitis patients | 53 | Mind–body medicine coursea | Ulcerative colitis patients in remission; 56% female; ages 46.0 ± 12.8 years | MBSR; 8 weekly 2.5-h group sessions | Blood (serum); stool | <CRP (among non-flared); ~IL-6; ~IL-8; >IL-10 (among flared); ~calprotectin |
| Lengacher et al.;45,66 | Test effect of mindful meditation on immune recovery following breast cancer recovery | 82; 124 respectively | Waiting list | Breast cancer patients; 100% female; ages 58.0 ± 9.0 years | MBSR-derived; 6 weekly 2-h sessions | Blood (WBCs) | >T cell activation; >IFN-γ/IL-4 ratio; >CD4+/CD8+ ratio (trend); ~CD3+, CD4+, CD8+; ~NK cells; ~B lymphocytes; >telomerase activity; ~telomere length |
| Malarkey et al.40 | Test effect of mindful meditation on inflammatory markers in workers with cardiovascular disease risk | 170 | Lifestyle education coursea | University faculty/staff with cardiovascular disease risk; 88% female; ages 51.0 (± 0.8 SE) years | MBSR-derived; 8 weekly 1-h group sessions + retreat | Blood (serum) | <CRP (trend); ~IL-6 |
| Moynihan et al.72 | Test effect of mindful meditation on brain function and antibody response in older adults | 201 | Waiting list | Older adults; 62% female; ages 73.3 ± 6.7 years | MBSR; 8 weekly 2-h group sessions + retreat | Blood (serum) with KLH challenge | >IgG (immediate post); <IgG (24 weeks) |
| Oken et al.41 | Test feasibility of mindfulness meditation in a clinical trial design for a larger study among caregivers | 21 | Dementia education coursea; respite care | Community-dwelling caregivers; 76% female; ages 62.5 ± 11.6 years | MBCT-derived; 6 weekly 1.5-h group sessions | Blood (serum) | ~TNF-α; ~IL-6; ~CRP |
| Rosenkranz et al.25 | Test effect of mindful meditation on physiological stress and neurogenic inflammation responses | 49 | Health enhancement programa | Community volunteers; 80% female; ages 45.9 ± 10.9 years | MBSR; 8 weekly 2.5-h group sessions + retreat | Skin (blister fluid) | <TNF-α (dependent on practice dosage); ~IL-8 |
| SeyedAlinaghi et al.61 | Test effect of mindful meditation on CD4+ T lymphocyte count in HIV patients | 171 | Education and support resources | HIV+ patients; 31% female; ages 35.1 ± 6.5 years | MBSR; 8 weekly 2.5-h group sessions | Blood (plasma) | >CD4+ T lymphocyte count (up to 6 months) |
| Zautra et al.42 | Test effect of mindful meditation or cognitive behavioral therapy on pain in patients with rheumatoid arthritis | 137 | Cognitive behavioral therapya; arthritis education coursea | Rheumatoid arthritis diagnosed; 68% female; ages 57.3 ± 15.3 years | MBSR/MBCT-derived; 8 weekly 2-h group sessions | Blood (PBMCs stimulated) | ~IL-6 |
Condition is comparable based on nonspecific treatment factors, such as time, attention, and group support.
Abbreviations: MBSR, mindfulness-based stress reduction; MAPs, mindful awareness practices; MBCT, mindfulness-based cognitive therapy; PBMCs, peripheral blood mononuclear cells; WBCs, white blood cells; KLH, keyhole limpet hemocyanin; <, decrease; >, increase; ~, null change; IL, interleukin; CRP, C-reactive protein; Ig, immunoglobulin; NF-κB, nuclear factor-κB; IFN, interferon; TNF, tumor necrosis factor; sTNF-RII, soluble tumor necrosis factor receptor; Th, T helper; NK, natural killer.
Comparison conditions
Less than half of the studies (n = 8; 40%) administered a comparison condition that accounted for the nonspecific effects of the intervention protocol, including time, attention, and group effects. Active comparator programs included exercise, sleep hygiene, group therapies, mind–body medicine, health education courses, and cognitive behavioral therapy. Half of the studies used a waiting list or usual care group for comparison to mindfulness meditation (n = 10; 50%), which did not account for nonspecific effects. Other nonequivalent comparator groups included less intensive single-day educational courses, access to resource services, and short-term respite care for caregivers (n = 2; 10%).
Sample selection
Females were oversampled, as 14 of the 20 studies examined (70%) had samples that were 60% or more female. This is partly due to disease-specific recruitment of breast cancer patients, but may also indicate possible participation bias favoring females due to sex differences in motivation to practice mindfulness meditation or participation in research studies focused on health and wellness. Supporting this last possibility, studies sampling the general community, university staff, and corporate employees also showed proportionately greater female participation. Ten studies (50%) selected samples on the basis of disease inclusion criteria (e.g., breast cancer, HIV positive, ulcerative colitis, and rheumatoid arthritis), and five studies (25%) recruited participants on the basis of a proposed risk factor (e.g., aging, poor sleep, loneliness, overweight/obesity, cardiovascular disease). Finally, five studies (25%) recruited healthy volunteers (e.g., corporate employees, older adults, meditators, or community residents).
Intervention dosage
All but three studies included in this review administered an MBSR or MBSR-derived program (i.e., MBSR with cognitive therapy or additional psychoeducational content), indicating high similarity in intervention type across studies. Of the remaining interventions, two studies reported on the use of a standardized Mindful Awareness Practices (MAPs) course, and one study broadly defined their program as mindfulness, compassion, and equanimity meditations led by a senior meditation teacher. Of note, MAPs and the generalized mindfulness program appeared to be conceptually the same as MBSR and differed only in program dosage and degree of documented standardization. All classes were administered in weekly group-based sessions spanning 6–10 weeks. Eight of the studies (40%) held an additional single-day intensive meditation retreat per conventional MBSR administration. Participants in one study lived at the retreat location for 3 months and practiced daily meditation.
Collection of biological specimens
Eighteen studies (90%) collected peripheral blood via venipuncture for processing of the target blood specimen or cell type. The most commonly reported processing protocol was the extraction of peripheral blood mononuclear cells (PBMCs) using ficoll for immune bioassay. This method is used to isolate leukocytes (white blood cells consisting of T, B, and natural killer (NK) cells) from other more predominant immune cells (i.e., granulocytes, including neutrophils, eosinophils, and basophils). Nasal mucous was collected in one study using a nasal wash approach during participant acute respiratory infection episodes.24 Another study induced skin blisters using a vacuum pressurized blister template and subsequently collected blister fluid.25
Excluded studies
Six studies tested the effect of a mindfulness meditation intervention on at least one immune parameter,26–33 but were excluded because they lacked an RCT design. In brief, these quasi-experimental studies used non-randomized matched control and single-group cohort designs. The median sample size of these six studies was n = 51 (range: 34–66), with samples consisting of breast cancer and prostate cancer patients, experienced meditators, HIV-diagnosed individuals, and women with a trauma history. Blood was collected in five studies (83%) and saliva was collected in one study. All interventions were MBSR or MBSR derived. Significant changes in immune measures were observed for levels, count, activity, or expression of interleukins (IL)-4, IL-6, and IL-10; interferon gamma (IFN-γ); NK cells; monocytes; eosinophils; receptor-interacting serine-threonine kinase (RIPK2); cyclooxygenase (COX2); regulated upon activation normal T cell expressed and presumably secreted to stromal-derived factor ratio (RANTES/SDF-1); and telomere length. Findings from these studies may suggest potential biomarker targets for future investigation, but the results are preliminary and should be interpreted with caution.
Summary of evidence from randomized controlled trials
Below, we report the results of our systematic review of the 20 RCT studies that met all of the inclusion criteria, organized by outcome. Table 1 provides a description and the results of the 20 studies included in this review.
Circulating and stimulated inflammatory proteins
Inflammatory proteins are produced by immune cells and serve as extracellular communicators during immune system activity. When circulating, these proteins propagate proinflammatory (e.g., liver-derived C-reactive protein; CRP) or anti-inflammatory (e.g., cell-derived IL-10 cytokine) effects. These proteins are essential for systemic preservation (i.e., protection against autoimmunity and septic shock) and immune cell differentiation; however, dysregulated and chronically elevated levels of proinflammatory proteins increase risk for disease, poor healing, and mortality.34–36 Of the 20 studies reviewed, nine measured inflammatory cytokines, including IL-6, IL-8, IL-10, tumor necrosis factor (TNF)-α and its receptor agonist sTNF-RII, and IFN-I, as well as CRP.
Five studies quantified circulating levels,37–42 and one additional study reported on stimulated levels,42 of IL-6 in blood. Of these studies, one study of female breast cancer patients engaging in a 6-week MAPs course (compared to a waiting-list control group) showed a relative reduction in post-intervention circulating levels of IL-6 that was dependent on the frequency of practice dosage.37 Three studies measured IL-8,24,25,39 one of which showed a relative increase in IL-8 in nasal secretions in older community-dwelling adults after an 8-week MBSR course (compared to moderate-intensity exercise).24 In addition, two studies measured IL-10 in blood,24,39 one of which showed a relative increase in IL-10 in ulcerative colitis patients after MBSR (compared to a matched mind–body medicine program), specifically among patients who experienced a symptomatic flare up.39 Four studies measured TNF-α,25,37,41,43 of which one study of healthy community volunteers showed reductions in TNF-α in blister fluid following MBSR, with these effects being dependent on practice time,25 and a second study of ulcerative colitis patients showed a trend effect for reductions in lipopolysaccharide-stimulated TNF-α production following MBSR intervention.43 Furthermore, three studies measured IFN,37,44,45 one of which showed a relative increase in IFN-I in female breast cancer patients after a 6-week MAPs intervention.37 A second study showed that females recovering from breast cancer who received MBSR had an increased IFN-γ/IL-4 ratio. Finally, six studies measured CRP,37–41,46 of which three showed a reduction in CRP, with one study showing reduced CRP levels after MBSR among non-flared patients with ulcerative colitis,39 and two other studies showing a trend for reduced CRP levels after MBSR-type programs among non-diseased samples displaying an inflammatory risk factor.38,40
Cellular transcription factors and gene expression
Transcription factors are intracellular molecules in immune cells that modulate the activity of immune response genes and their production of extracellular proteins.47 For example, nuclear factor-κB (NF-κB) is a transcription factor that, when activated, translocates into the cell nucleus and binds to DNA at the promoter region, thus activating genes for expression.48 NF-κB functions as a precursor to increased concentrations of proinflammatory cytokines in peripheral blood and thus helps coordinate the inflammatory response.49,50 Some psychoneuroimmunologic models propose that NF-κB activity is a key intracellular pathway linking the central nervous system (CNS) psychological threat cascade with neuroendocrine signal-mediated peripheral immune system dysregulation.51,52 Consistent with these models, acute psychological stress has been shown to activate NF-κB in PBMCs.53–55
Of the studies reviewed, three measured NF-κB in PBMCs37,38,56 and showed a reduction in NF-κB after the MBI. Two studies—one in lonely older adults and the other in breast cancer patients—showed a relative reduction in the expression of NF-κB after MBSR and MAPs (compared to waiting-list controls) using promoter-based bioinformatics measures of functional genomic activity.37,38 A third study showed that MAPs produced a reduction in activated NF-κB p65 in older adults exhibiting sleep disturbances; however, NF-κB was also significantly decreased in the highly active sleep hygiene comparison condition.56
Immune cell count
When engaged by an immune challenge, immune cells are differentially activated, generated, and then deployed by the immune system to target regions to protect the body against infection and promote tissue recovery. As such, cell distribution or count is used as a diagnostic marker for various immune-compromising diseases. For example, a decline in CD4+ T lymphocyte count is a standard immune cell signal of disease progression in HIV patients.57 Further, chronic stress and depression can inhibit immune cell activity and proliferation, and thus weaken defenses against tumorigenic surveillance and growth.58
Immune cell counts pertain to cells constituting the innate (neutrophils) and adaptive (T, B, and NK cells) subsets, and this count was quantified in five studies.24,45,59–61 In one of these studies, there was no relative change in neutrophils (mucous from nasal wash) after MBSR-derived intervention in older adults experiencing an acute respiratory illness.24 Of the other four studies that enumerated lymphocytes in blood, all identified either an increase or a buffered decline in T lymphocyte cell count (CD4+ T; CD4+/CD8+ ratio; T helper (Th)1/Th2 T-helper) and/or activation (% activated T cells) after mindfulness meditation in samples diagnosed with a disease (i.e., HIV or breast cancer) as compared to controls.45,59,61,62 Three of these studies were restricted to people diagnosed with HIV.59,61,62 B lymphocyte and NK cell counts did not show relative changes in a study of breast cancer patients after intervention.45
Immune cell aging
Immune cell telomeres are protective DNA and protein complexes that function as caps to protect and stabilize the ends of eukaryotic chromosomes, which truncate during cell division.63 Shortened telomeres are a marker of immune cell aging and vulnerability to apoptosis, and are associated with poorer clinical outcomes and premature death in various age-related diseases.64 Telomere length is protected in part by the naturally occurring enzyme telomerase, which help slow or reverse cell aging.63 Longer telomeres and higher telomerase activity are thus considered to be salutogenic immune system profiles.
Four studies measured telomere length and/or telomerase activity.65–68 Of the two studies that quantified telomere length,65,66 one examining breast cancer survivors showed a trend for the MBSR-derived intervention to attenuate the telomere shortening observed in the control group;65 however, these effects were observed only when samples from the mindfulness meditation and supportive group therapy groups were combined to increase statistical power. Of the three studies that measured telomerase activity, all showed an increase in telomerase activity after mindfulness meditation, at least at the trend level, among a diverse set of samples (e.g., meditation retreat participants, overweight/obese women, and breast cancer patients).66–68 In one of these three studies, the increase was dependent on program attendance—specifically, only high treatment-regiment adherers showed a trend for mindfulness mediation–related increases in telomerase activity.67
Antibody response
Antibodies are immunoglobulins (IgG, IgA, IgM, IgD, and IgE) or molecules secreted by immune cells (B lymphocytes) that identify and neutralize pathogens (via antigen flagging). Antibodies constitute humoral immunity and help immune cells inactivate toxic substances, attack viruses and bacteria, and assist in the function of other immune cells. Suboptimal antibody response is commonly found in immune-compromised individuals (e.g., HIV disease progression),69 persons experiencing chronic stress,70 and older adults (> 60 years of age).71 Antibody titer tests demonstrate serologic immunity by quantifying the level of antibodies in blood, mucous, or other tissue samples.
Antibodies were measured in three studies,44,72,73 two of which examined antibody response to influenza vaccination;44,73 one revealed that MBSR led to a significantly greater rise in hemagglutination-inhibition influenza antibody titers from the 4–8 week blood draw period (compared with controls in a sample of corporate employees).73 The second study did not show relative changes in serum influenza antibody or nasal IgA in older adults.44 The antigen keyhole limpet hemocyanin was administered in a third study of older adults, which showed a relatively greater increase in IgG immediately after MBSR intervention; additionally, a smaller increase in IgG was observed at the 24-week assessment.72
Summary of evidence and implications for future research
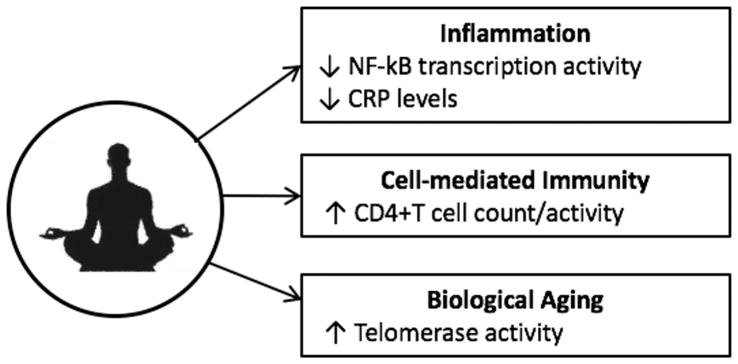
The present review is the first to interrogate the findings of the RCTs that have been conducted to date on mindfulness meditation and the immune system. This comprehensive examination included data from 1602 participants and revealed tentative evidence that mindfulness meditation is associated with changes in select biomarkers of immune system activity. When using the criteria of three or more RCTs showing that mindfulness meditation has at least a trend-level or dosage-dependent effect on immune parameters, we identified mindfulness mediation-related effects for the following four parameters: reductions in the activity of the cellular transcription factor NF-kB, reductions in circulating levels of CRP, increases in CD4+ T cell count (in HIV-diagnosed individuals), and increases in telomerase activity (Fig. 1). In contrast, null findings or a lack of replicated effects were found for antibodies (IgA, IgG, influenza), interleukins (IL-1, IL-6, IL-8, IL-10), IFN, TNF, and various measures of cell count. Considered together, these data point to promising areas of future investigation, but we caution against exaggerating the positive effects of mindfulness meditation on immune system dynamics until these effects are further replicated and additional studies are performed.
Figure 1.
Mindfulness meditation and immune system biomarkers. This systematic review of 20 randomized controlled trials, comprising more than 1600 participants, revealed replicated, yet tentative, evidence that mindfulness mediation is associated with changes in select immune system processes involved in inflammation, immunity, and biological aging. Nuclear factor-κB, NF-κB; C-reactive protein, CRP.
With respect to the abovementioned preliminary positive effects that replicated across studies, if robust and maintained over time, these types of shifts in immune system activity could potentially have beneficial effects on health by influencing mechanisms that are known to affect biological aging and disease. For example, countering a dysregulated or hypersensitive immune system profile with mindfulness meditation could theoretically function to improve organism fitness by enhancing immune defenses that protect against viral and bacterial infection, as well as various age-related disease conditions, including cardiovascular disease, osteoporosis, arthritis, type-2 diabetes, frailty, and some cancers. To test this possibility, future studies will need to examine associations between mindfulness meditation, immune function, and disease symptomatology.
Insights garnered from this review provide the basis for further theory building and empirical investigation into if, and if so, how, mindfulness meditation influences biological processes involved in aging and disease. For example, these findings extend existing models of mindfulness meditation, which suggest that mindfulness meditation may downregulate the activity of major stress axes in the body, such as the sympathetic–adrenal–medullary (SAM) and hypothalamic–pituitary–adrenal (HPA) axes,21 which are known to influence some of the immune system mechanisms identified in this review. To fully realize the benefits of this work for improving health, however, additional RCTs are needed that examine the robustness and generalizability of the present immune-related findings, as well as their relevance for predicting changes in clinical outcomes over time.
Looking forward, there are several points that should be considered when planning future studies on mindfulness meditation and immune system dynamics. First, only 40% of the RCTs reviewed used control programs that could account for nonspecific treatment effects. This leaves substantial room for improving study designs by using comparator groups that are better than a waiting-list control condition. Indeed, a description of a standardized active control condition that can be used alongside MBIs was recently made available for trial researchers.74 Second, the effects of mindfulness meditation on immune system biomarkers were dosage-dependent in some instances. As a result, beyond obtaining adequate sample sizes, future studies and interventions will benefit from maximizing treatment adherence. This also highlights a need for researchers to collect data on individuals’ class attendance and/or home practice schedules, and to report on both the overall effects and dosage-dependent effects when publishing trial results.
Third, in the studies reviewed, immune biomarkers were often included as ancillary measures and, consequently, hypothesis tests were frequently underpowered. To truly advance this area of study, future projects will need to power studies and calibrate tests for changes in immune parameters as primary outcomes, a priori, to avoid false negative results. It will also be important to provide clearer rationales for the immune biomarkers chosen for inclusion and better descriptions of how those biomarkers relate to the pathophysiologic process being studied. Fourth, almost all of the RCTs examined (19/20 studies) employed peripheral blood as the main human specimen with which to quantify immune function. This is a notable and consistent strength across studies, but it also highlights an opportunity for future studies to investigate other less invasive specimens (e.g., mucous, saliva, urine, hair) that could be validated against blood and potentially used as biomarkers of mindfulness meditation–related changes in immune system dynamics. Finally, the specimen collection and processing procedure employed by several studies was not well described, thus highlighting an opportunity to improve the reporting of study procedures to enhance researchers’ ability to replicate study protocols, especially with respect to the timing of specimen collection, steps taken for sample processing and storage, and procedures used for assay quantification.
In conclusion, across 20 RCTs and more than 1600 participants, we found tentative evidence that mindfulness meditation modulates some select immune parameters in a manner that suggests a more salutogenic immune profile. Specifically, mindfulness mediation appears to be associated with reductions in proinflammatory processes, increases in cell-mediated defense parameters, and increases in enzyme activity that guards against cell aging. Although these findings replicated and are based on well-designed RCTs, they are restricted to particular populations, subgroup analyses, and disease types. Consequently, additional research is needed to test the effects of mindfulness mediation on immune system biomarkers to provide a clearer understanding of the robustness and generalizability of findings, and to examine the relevance of these findings for clinical symptoms and overall health.
Acknowledgments
D.S.B. was supported by a grant from the National Institute on Aging to the USC/UCLA Center on Biodemography and Population Health (P30 AG017265); G.M.S. was supported by a Society in Science–Branco Weiss Fellowship and by a career development award from the National Institute of Mental Health (K08 MH103443).
Footnotes
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology-Science and Practice. 2003;10(2):144–156. [Google Scholar]
- 2.Black DS. Mindfulness-based interventions: an antidote to suffering in the context of substance use, misuse, and addiction. Subst Use Misuse. 2014;49(5):487–491. doi: 10.3109/10826084.2014.860749. [DOI] [PubMed] [Google Scholar]
- 3.Rapgay L, Bystrisky A. Classical mindfulness: an introduction to its theory and practice for clinical application. Ann N Y Acad Sci. 2009;1172:148–162. doi: 10.1111/j.1749-6632.2009.04405.x. [DOI] [PubMed] [Google Scholar]
- 4.Buchholz L. Exploring the Promise of Mindfulness as Medicine. JAMA. 2015;314(13):1327–1329. doi: 10.1001/jama.2015.7023. [DOI] [PubMed] [Google Scholar]
- 5.Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA internal medicine. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obesity reviews. 2014;15(6):453–461. doi: 10.1111/obr.12156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Black DS, Milam J, Sussman S. Sitting-Meditation Interventions Among Youth: A Review of Treatment Efficacy. Pediatrics. 2009;124(3):532–541. doi: 10.1542/peds.2008-3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 9.Hofmann SG, Sawyer AT, Witt AA, Oh D. The Effect of Mindfulness-Based Therapy on Anxiety and Depression: A Meta-Analytic Review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goyal M, Singh S, Sibinga EMS, et al. Meditation Programs for Psychological Stress and Well-being A Systematic Review and Meta-analysis. Jama Internal Medicine. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Black DS, Greeson J. Mindfulness-based interventions in routine clinical care for stress-related ailments: comment. JAMA Internal Medicine. 2014;174(3) [Google Scholar]
- 12.Black DS, O’Reilly GA, Olmstead R, Breen EC, Irwin MR. Mindfulness Meditation and Improvement in Sleep Quality and Daytime Impairment Among Older Adults With Sleep Disturbances: A Randomized Clinical Trial. JAMA Intern Med. 2015;175(4):494–501. doi: 10.1001/jamainternmed.2014.8081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bowen S, Witkiewitz K, Clifasefi SL, et al. Relative Efficacy of Mindfulness-Based Relapse Prevention, Standard Relapse Prevention, and Treatment as Usual for Substance Use Disorders: A Randomized Clinical Trial. JAMA Psychiatry. 2014;71(5):547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302(12):1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 15.Kuyken W, Hayes R, Barrett B, et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. The Lancet. 2015;386(9988):63–73. doi: 10.1016/S0140-6736(14)62222-4. [DOI] [PubMed] [Google Scholar]
- 16.Haas L, Maryniuk M, Beck J, et al. National standards for diabetes self-management education and support. Diabetes Care. 2013;36(Suppl 1):S100–108. doi: 10.2337/dc13-S100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ford ES, Bergmann MM, Boeing H, Li C, Capewell S. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Preventive medicine. 2012;55(1):23–27. doi: 10.1016/j.ypmed.2012.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galla BM, O’Reilly GA, Kitil MJ, Smalley SL, Black DS. Community-Based Mindfulness Program for Disease Prevention and Health Promotion: Targeting Stress Reduction. American journal of health promotion. 2015;30(1):36–41. doi: 10.4278/ajhp.131107-QUAN-567. [DOI] [PubMed] [Google Scholar]
- 19.Greeson JM, Garland EL, Black DS. Mindfulness: A transtherapeutic approach for transdiagnostic mental processes. In: Ie A, Ngnoumen C, Langer E, editors. The Wiley Blackwell Handbook of Mindfulness. II. Oxford; Wiley: 2014. pp. 533–562. [Google Scholar]
- 20.Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev. 2013;33(6):763–771. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 21.Creswell JD, Lindsay EK. How Does Mindfulness Training Affect Health? A Mindfulness Stress Buffering Account. Current Directions in Psychological Science. 2014;23(6):401–407. [Google Scholar]
- 22.Slavich GM. Understanding inflammation, its regulation, and relevance for health: a top scientific and public priority. Brain, behavior, and immunity. 2015;45:13–14. doi: 10.1016/j.bbi.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Couzin-Frankel J. Inflammation bares a dark side. Science. 2010;330(6011):1621. doi: 10.1126/science.330.6011.1621. [DOI] [PubMed] [Google Scholar]
- 24.Barrett B, Hayney MS, Muller D, et al. Meditation or exercise for preventing acute respiratory infection: a randomized controlled trial. Ann Fam Med. 2012;10(4):337–346. doi: 10.1370/afm.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosenkranz MA, Davidson RJ, Maccoon DG, Sheridan JF, Kalin NH, Lutz A. A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain Behav Immun. 2013;27(1):174–184. doi: 10.1016/j.bbi.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65(4):571–581. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- 27.Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21(8):1038–1049. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 28.Gallegos AM, Lytle MC, Moynihan JA, Talbot NL. Mindfulness-based stress reduction to enhance psychological functioning and improve inflammatory biomarkers in trauma-exposed women: A pilot study. Psychol Trauma. 2015;7(6):525–532. doi: 10.1037/tra0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoge EA, MD, Chen MM, BS, Metcalf CA, BA, Fischer LE, BA, Pollack MH, MD, DeVivo I. Loving-Kindness Meditation Practice Associated with Longer Telomeres in Women. Brain, behavior, and immunity. 2013;32:159–163. doi: 10.1016/j.bbi.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 30.Kaliman P, Alvarez-Lopez MJ, Cosin-Tomas M, Rosenkranz MA, Lutz A, Davidson RJ. Rapid changes in histone deacetylases and inflammatory gene expression in expert meditators. Psychoneuroendocrinology. 2014;40:96–107. doi: 10.1016/j.psyneuen.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lengacher CA, Kip KE, Barta MK, et al. A Pilot Study Evaluating the Effect of Mindfulness-Based Stress Reduction on Psychological Status, Physical Status, Salivary Cortisol, and Interleukin-6 Among Advanced-Stage Cancer Patients and Their Caregivers. Journal of Holistic Nursing. 2012;30(3):170–185. doi: 10.1177/0898010111435949. [DOI] [PubMed] [Google Scholar]
- 32.Robinson FP, Mathews HL, Witek-Janusek L. Psycho-endocrine-immune response to mindfulness-based stress reduction in individuals infected with the human immunodeficiency virus: a quasiexperimental study. Journal of alternative and complementary medicine. 2003;9(5):683–694. doi: 10.1089/107555303322524535. [DOI] [PubMed] [Google Scholar]
- 33.Witek-Janusek L, Albuquerque K, Chroniak KR, Chroniak C, Durazo-Arvizu R, Mathews HL. Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain Behav Immun. 2008;22(6):969–981. doi: 10.1016/j.bbi.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Genderen ME, Lima A, de Geus H, et al. Serum C-reactive protein as a predictor of morbidity and mortality in intensive care unit patients after esophagectomy. Ann Thorac Surg. 2011;91(6):1775–1779. doi: 10.1016/j.athoracsur.2011.02.042. [DOI] [PubMed] [Google Scholar]
- 35.Carlstedt F, Lind L, Lindahl B. Proinflammatory cytokines, measured in a mixed population on arrival in the emergency department, are related to mortality and severity of disease. Journal of internal medicine. 1997;242(5):361–365. doi: 10.1046/j.1365-2796.1997.00209.x. [DOI] [PubMed] [Google Scholar]
- 36.Celli BR, Locantore N, Yates J, et al. Inflammatory biomarkers improve clinical prediction of mortality in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185(10):1065–1072. doi: 10.1164/rccm.201110-1792OC. [DOI] [PubMed] [Google Scholar]
- 37.Bower JE, Crosswell AD, Stanton AL, et al. Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer. 2015;121(8):1231–1240. doi: 10.1002/cncr.29194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Creswell JD, Irwin MR, Burklund LJ, et al. Mindfulness-Based Stress Reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain, behavior, and immunity. 2012;26(7):1095–1101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jedel S, Hoffman A, Merriman P, et al. A randomized controlled trial of mindfulness-based stress reduction to prevent flare-up in patients with inactive ulcerative colitis. Digestion. 2014;89(2):142–155. doi: 10.1159/000356316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Malarkey WB, Jarjoura D, Klatt M. Workplace based mindfulness practice and inflammation: a randomized trial. Brain Behav Immun. 2013;27(1):145–154. doi: 10.1016/j.bbi.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oken BS, Fonareva I, Haas M, et al. Pilot controlled trial of mindfulness meditation and education for dementia caregivers. Journal of alternative and complementary medicine. 2010;16(10):1031–1038. doi: 10.1089/acm.2009.0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zautra AJ, Davis MC, Reich JW, et al. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J Consult Clin Psychol. 2008;76(3):408–421. doi: 10.1037/0022-006X.76.3.408. [DOI] [PubMed] [Google Scholar]
- 43.Elsenbruch S, Langhorst J, Popkirowa K, et al. Effects of mind-body therapy on quality of life and neuroendocrine and cellular immune functions in patients with ulcerative colitis. Psychother Psychosom. 2005;74(5):277–287. doi: 10.1159/000086318. [DOI] [PubMed] [Google Scholar]
- 44.Hayney MS, Coe CL, Muller D, et al. Age and psychological influences on immune responses to trivalent inactivated influenza vaccine in the meditation or exercise for preventing acute respiratory infection (MEPARI) trial. Hum Vaccin Immunother. 2014;10(1):83–91. doi: 10.4161/hv.26661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lengacher CA, Kip KE, Post-White J, et al. Lymphocyte recovery after breast cancer treatment and mindfulness-based stress reduction (MBSR) therapy. Biol Res Nurs. 2013;15(1):37–47. doi: 10.1177/1099800411419245. [DOI] [PubMed] [Google Scholar]
- 46.Fogarty FA, Booth RJ, Gamble GD, Dalbeth N, Consedine NS. The effect of mindfulness-based stress reduction on disease activity in people with rheumatoid arthritis: a randomised controlled trial. Ann Rheum Dis. 2015;74(2):472–474. doi: 10.1136/annrheumdis-2014-205946. [DOI] [PubMed] [Google Scholar]
- 47.Slavich GM, Cole SW. The Emerging Field of Human Social Genomics. Clinical psychological science. 2013;1(3):331–348. doi: 10.1177/2167702613478594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bharti AC, Aggarwal BB. Nuclear factor-kappa B and cancer: its role in prevention and therapy. Biochemical pharmacology. 2002;64(5–6):883–888. doi: 10.1016/s0006-2952(02)01154-1. [DOI] [PubMed] [Google Scholar]
- 49.Rohleder N. Stimulation of systemic low-grade inflammation by psychosocial stress. Psychosomatic medicine. 2014;76(3):181–189. doi: 10.1097/PSY.0000000000000049. [DOI] [PubMed] [Google Scholar]
- 50.Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. 2006;441(7092):431–436. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 51.Irwin MR, Cole SW. Reciprocal regulation of the neural and innate immune systems. Nature reviews Immunology. 2011;11(9):625–632. doi: 10.1038/nri3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychological bulletin. 2014;140(3):774–815. doi: 10.1037/a0035302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pace TW, Mletzko TC, Alagbe O, et al. Increased stress-induced inflammatory responses in male patients with major depression and increased early life stress. The American journal of psychiatry. 2006;163(9):1630–1633. doi: 10.1176/ajp.2006.163.9.1630. [DOI] [PubMed] [Google Scholar]
- 54.Bierhaus A, Wolf J, Andrassy M, et al. A mechanism converting psychosocial stress into mononuclear cell activation. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(4):1920–1925. doi: 10.1073/pnas.0438019100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Murphy ML, Slavich GM, Rohleder N, Miller GE. Targeted Rejection Triggers Differential Pro- and Anti-Inflammatory Gene Expression in Adolescents as a Function of Social Status. Clinical psychological science. 2013;1(1):30–40. doi: 10.1177/2167702612455743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Black DS, O’Reilly GA, Olmstead R, Breen EC, Irwin MR. Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances: a randomized clinical trial. JAMA internal medicine. 2015;175(4):494–501. doi: 10.1001/jamainternmed.2014.8081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mellors JW, Munoz A, Giorgi JV, et al. Plasma viral load and CD4+ lymphocytes as prognostic markers of HIV-1 infection. Annals of internal medicine. 1997;126(12):946–954. doi: 10.7326/0003-4819-126-12-199706150-00003. [DOI] [PubMed] [Google Scholar]
- 58.Reiche EM, Nunes SO, Morimoto HK. Stress, depression, the immune system, and cancer. Lancet Oncol. 2004;5(10):617–625. doi: 10.1016/S1470-2045(04)01597-9. [DOI] [PubMed] [Google Scholar]
- 59.Creswell JD, Myers HF, Cole SW, Irwin MR. Mindfulness meditation training effects on CD4+ T lymphocytes in HIV-1 infected adults: a small randomized controlled trial. Brain Behav Immun. 2009;23(2):184–188. doi: 10.1016/j.bbi.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gonzalez-Garcia M, Ferrer MJ, Borras X, et al. Effectiveness of Mindfulness-Based Cognitive Therapy on the Quality of Life, Emotional Status, and CD4 Cell Count of Patients Aging with HIV Infection. AIDS Behav. 2013 doi: 10.1007/s10461-013-0612-z. [DOI] [PubMed] [Google Scholar]
- 61.SeyedAlinaghi S, Jam S, Foroughi M, et al. Randomized controlled trial of mindfulness-based stress reduction delivered to human immunodeficiency virus-positive patients in Iran: effects on CD4(+) T lymphocyte count and medical and psychological symptoms. Psychosomatic medicine. 2012;74(6):620–627. doi: 10.1097/PSY.0b013e31825abfaa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gonzalez-Garcia M, Ferrer MJ, Borras X, et al. Effectiveness of Mindfulness-Based Cognitive Therapy on the Quality of Life, Emotional Status, and CD4 Cell Count of Patients Aging with HIV Infection. AIDS Behav. 2013;18(4):676–685. doi: 10.1007/s10461-013-0612-z. [DOI] [PubMed] [Google Scholar]
- 63.Blackburn EH. Structure and function of telomeres. Nature. 1991;350(6319):569–573. doi: 10.1038/350569a0. [DOI] [PubMed] [Google Scholar]
- 64.Cawthon RM, Smith KR, O’Brien E, Sivatchenko A, Kerber RA. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet. 2003;361(9355):393–395. doi: 10.1016/S0140-6736(03)12384-7. [DOI] [PubMed] [Google Scholar]
- 65.Carlson LE, Beattie TL, Giese-Davis J, et al. Mindfulness-based cancer recovery and supportive-expressive therapy maintain telomere length relative to controls in distressed breast cancer survivors. Cancer. 2015;121(3):476–484. doi: 10.1002/cncr.29063. [DOI] [PubMed] [Google Scholar]
- 66.Lengacher CA, Reich RR, Kip KE, et al. Influence of mindfulness-based stress reduction (MBSR) on telomerase activity in women with breast cancer (BC) Biol Res Nurs. 2014;16(4):438–447. doi: 10.1177/1099800413519495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Daubenmier J, Lin J, Blackburn E, et al. Changes in stress, eating, and metabolic factors are related to changes in telomerase activity in a randomized mindfulness intervention pilot study. Psychoneuroendocrinology. 2012;37(7):917–928. doi: 10.1016/j.psyneuen.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jacobs TL, Epel ES, Lin J, et al. Intensive meditation training, immune cell telomerase activity, and psychological mediators. Psychoneuroendocrinology. 2011;36(5):664–681. doi: 10.1016/j.psyneuen.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 69.Kroon FP, van Dissel JT, de Jong JC, Zwinderman K, van Furth R. Antibody response after influenza vaccination in HIV-infected individuals: a consecutive 3-year study. Vaccine. 2000;18(26):3040–3049. doi: 10.1016/s0264-410x(00)00079-7. [DOI] [PubMed] [Google Scholar]
- 70.Cohen S, Miller GE, Rabin BS. Psychological stress and antibody response to immunization: a critical review of the human literature. Psychosomatic medicine. 2001;63(1):7–18. doi: 10.1097/00006842-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 71.Kumar R, Burns EA. Age-related decline in immunity: implications for vaccine responsiveness. Expert Rev Vaccines. 2008;7(4):467–479. doi: 10.1586/14760584.7.4.467. [DOI] [PubMed] [Google Scholar]
- 72.Moynihan JA, Chapman BP, Klorman R, et al. Mindfulness-based stress reduction for older adults: effects on executive function, frontal alpha asymmetry and immune function. Neuropsychobiology. 2013;68(1):34–43. doi: 10.1159/000350949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Davidson RJ, Kabat-Zinn J, Schumacher J, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med. 2003;65(4):564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- 74.MacCoon DG, Imel ZE, Rosenkranz MA, et al. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behav Res Ther. 2012;50(1):3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Black DS, O’Reilly GA, Olmstead R, Breen EC, Irwin MR. Mindfulness-based intervention for prodromal sleep disturbances in older adults: design and methodology of a randomized controlled trial. Contemp Clin Trials. 2014;39(1):22–27. doi: 10.1016/j.cct.2014.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]