Abstract
Low- and middle-income countries (LMICs) face a rapid change in the nutrition transition toward increases in noncommunicable diseases. Underlying this transition are shifts in the agricultural system and the subsequent growth of the modern retail and food service sectors across all regions and countries, a change in technology affecting physical activity and inactivity, mass media access, urbanization, and penetration of modern food systems into all societies. The resulting major shifts in diet are toward increased refined carbohydrates, added sweeteners, edible oils, and animal-source foods and reduced legumes, other vegetables, and fruits. Most countries are seeing increases in body mass index (BMI), overweight, and waist circumference (WC), and an increased WC-BMI ratio appears to be emerging in many regions. The implications of these rapidly changing diets and body compositions include the prevalence and severity of diabetes in LMICs.
Keywords: nutrition transition, low- and middle-income countries, obesity, dietary change, food system
I. Introduction
The world has seen a remarkable shift in dietary behaviors, physical activity and inactivity patterns, body composition, and prevalence of diabetes. These very much relate to the nutrition transition associated with changes in the foods and beverages consumed along with reduced physical activity. This paper first discusses the nutrition transition and the related agricultural system transition. We follow with the underlying factors driving the transition globally, the key patterns in diet and activity, and the global trend toward obesity that is affecting diabetes. The discussion includes some of the actions low- and middle-income countries (LMICs) are beginning to take to prevent further increases in obesity, particularly actions regarding food policy.
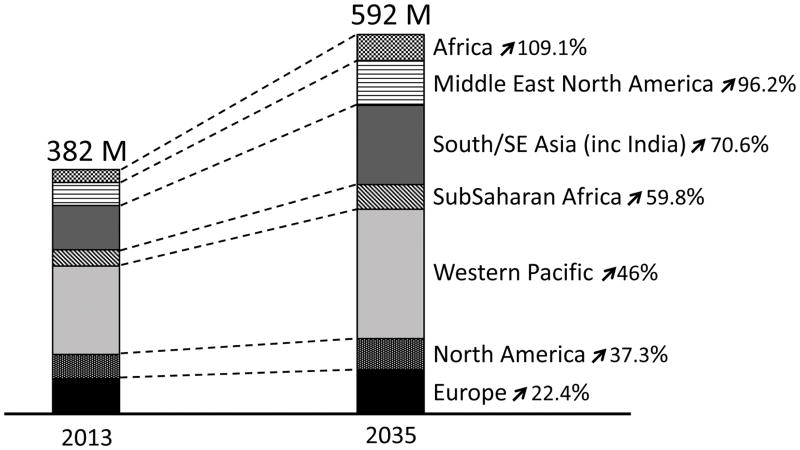
Even under very conservative assumption, the World Health Organization projects diabetes prevalence to expand from the current level of 382 million by 55% to 592 million in 2035. However as we show, the rapidly increasing levels of overweight and obesity coupled with increased waist circumferences and major diet shifts which will adversely impact diabetes suggest that the Figure 1 results will represent a major understatement of this increase.
Figure 1.
World Health Organization Diabetes Trends
II. The Nutrition Transition and the Related Agricultural Transition
Over the course of human existence, diet and nutritional status have undergone a sequence of stages, defined as broad patterns of food and beverage consumption and physical activity and inactivity and the subsequent shifts in body composition and corresponding nutrition-related disease. The concept of the nutrition transition focuses on large changes in both dietary and activity patterns. The concept of the nutrition transition places human diet, activity, and body composition in a broad historical perspective, with emphasis on understanding the pace, magnitude, determinants, correlates, and results of dietary change across centuries and millennia.[1–4] We will not go into the historical details of this transition here. Figures on these stages are presented elsewhere.[3]
It is important to understand that agriculture and food supply critically affect global dietary patterns. Since WWII our agricultural system focused first and foremost on addressing global hunger and the supply of basic starchy staples followed by animal source food and cash crops. This system has changed drastically in who controls the system but the focus on selected crops to the neglect of many others (e.g., vegetables and legumes), major cash crops such as sugar cane and palm oil and animal source food has not shifted as health and nutritional needs have changed drastically. Today understanding and then changing this agriculture system either directly or indirectly via an array of incentives and taxes is critical. However changing this system also faces complex political, economic, and environmental challenges, not least of which is the capacity of governments to implement change.[5] Governments have increasingly ceded funding and control of agriculture to the private sector. Consequently, any attempt to adapt the food supply via direct government investments may be minimal in contrast to changing the relative prices at the food purchase level. Elsewhere we address in more depth the food system as it relates to agriculture.[6]
III. Critical Underlying Drivers
Four sets of interrelated macroeconomic and technological factors have played major roles in the world’s shifting dietary and activity/inactivity patterns. The first is technology in the broadest sense, including laborsaving equipment for economic work (e.g., reapers, robotics, mechanized assembly lines) and the home (e.g., microwaves, mixers), transportation options (e.g., the wheel, trains, gas engines), and leisure sedentary behavior-promoting devices (e.g., television, radio).[7] Technology also includes food production, processing, and marketing systems.
The second is urbanization. With the development of early civilizations came denser living conditions and ultimately villages and cities.[8, 9] Urbanization has been ongoing for millennia but accelerated over the last century, affecting the sizes and densities of cities globally. Historically, urbanization has been associated with access to a wider variety of food; greater food processing; and increased consumption of food produced, processed, and cooked by others. Even in higher-income countries factors related to residence determine urban and suburban food and labor markets and create distinct dietary patterns. Among the responsible factors are improved transportation and marketing systems that make more foodstuffs available during periods of seasonal shortage; marketing activities of the commercial processed food sector and services that provide ready-to-eat food; more heterogeneous populations with wide ranges of dietary habits; occupations that are not compatible with home food preparation, child care, and elder care; household structures that reflect wide-ranging economic and social conditions; and diseases and use of health services. The last half of the twentieth century saw an unprecedented demographic revolution that appears to be continuing unabated in the twenty-first century. Migration and natural increase have made urbanization a dominant factor affecting life in all regions.
A third factor is the remarkable shift in income per capita and general economic welfare relative to the cost of food. Globally the price of food in terms of hours of work per kilocalories has decreased exponentially. As incomes have risen, the real prices of many types of food have fallen. Smaller proportions of incomes are expended on food, and people across the globe have access to a vast array of packaged foods and beverages. Food retailers and services have penetrated the markets where the majority of individuals purchase their food. At the same time households have the means to purchase laborsaving devices and equipment that promotes sedentary behavior.
The fourth factor is the enormous expansion of global trade in services, providing access to modern technology and manufacturing. The General Agreement on Trade and Tariffs (GATT) of the World Trade Organization (WTO) has greatly expanded access to modern services and technologies.[7] Modern media, retail food, food services, and physical activity-related technologies are a few of the sectors taking advantage of the opening of global trade in goods and services.
These four factors have combined to create enormous shifts in our overall physical activity and dietary patterns in a manner. We describe the major diet shifts linked with these larger societal forces.
IV. Major Direct Drivers: Diet and Activity
Physical Activity
Physical (PA) is declining rapidly across the globe, particularly in LMICs. China and Brazil, countries experiencing rapid economic growth, have the two highest absolute and relative rates of decline in total PA and some of the higher increases in sedentary time.[10] For these two countries, the declines in PA have been largely driven by reductions in movement at work, at home, and to a lesser degree in travel. This is not surprising, given that in the past few decades Chinese and Brazilians have been moving away from agriculture and into the manufacturing and service sectors, increasing the use of machines and labour-saving technology in the workplace, and accessing home technologies (e.g., electrification, piped water, appliances) and vehicles. A review of six countries—Brazil, China, India, the United Kingdom, Russia, and the United States produced a bleak forecast.[10, 11] For instance, we estimate that by 2020 the average American adult will only expend 142 metabolic equivalents of task hours per week while awake. The British are only slightly better and will reach that level by 2030. If the Chinese and Brazilians continue on their steep downward trend, they will reach the current US and UK PA levels by 2030. The situation in India appears less severe, but the national average masks the stark socioeconomic dichotomy that will likely continue there. Wealthier Indians lead lifestyles more like the British average (with possibly even lower domestic PA due to the prevalence of maids among this subpopulation of India). This same review shows high levels of sedentary behavior, predominantly related to television viewing, in these countries. In all cases sedentary time among adults is increasing. Measurement of PA among children is much more limited; however, selected detailed studies in a few countries suggest high levels of inactivity and low levels of activity.[12–18]
Diet
These physical activity and inactivity trends have occurred concurrently with some major dietary shifts. It is useful to understand how vastly diets across the LMIC world have converged on what we often term the “Western diet.” This is broadly defined by high intake of fats (particularly an array of healthy and unhealthy vegetable oils), added sugars, animal-source foods, and refined carbohydrates. Available data for LMICs document this trend in all urban areas and increasingly in rural areas. Diets rich in legumes, other vegetables, and coarse grains are disappearing in all regions and countries.
Vegetable Oils
One of the more profound changes in LMICs has been the huge increase in consumption of vegetable oils, such as rapeseed oil, palm oil, and soybean oil. This trend began with the development in the United States and Japan of techniques that reduced the cost of extraction. Subsequently, plant breeding increased the oil content of oilseeds.[19] In some countries, such as China, frying food is replacing traditional healthier food preparation methods like steaming, boiling, and baking.[20]
A Sweeter Diet
The globe’s diet is much sweeter today than heretofore.[21] An examination of processed and packaged foods and beverages showed that in 1989 about 75 percent of foods and beverages bought in the United States contained added caloric sweeteners.[22] Calorically sweetened beverages particularly, because of the combination of incomplete food compensation and refined carbohydrates, have been linked with various cardiometabolic outcomes.[23, 24] Many countries consume high levels of sugar-sweetened beverages (SSBs) and fruit juice, which are also linked with diabetes and weight gain.[25, 26]
Animal-Source Foods
Consumption of animal-source foods has increased in LMICs in particular. Earlier research by C.L. Delgado and others at the International Food Policy Research Institute found the beginning of a livestock revolution in the developing world.[27] Subsequent research by B. M. Popkin and others has shown major increases in production of beef, pork, poultry, dairy products, and eggs across LMICs, [28, 29] which account for most of the global increases in animal-source foods. For example, consumption of dairy products has increased significantly in India and consumption of pork and eggs in China.
Refined Carbohydrates replacing Legumes, Coarse Grains, and Other Vegetables This area is less studied than many other aspects of global dietary change but is equally important for its effects on the overall glycemic load of each meal. The global diet is shifting toward consumption of highly processed grains and carbohydrate-rich foods and away from fiber intake.[30–32] This occurred from the 1960s through the 1980s in the United States and many other higher income countries and is happening now across Asia, the Middle East and North Africa, urban sub-Saharan Africa, and the rest of the Americas.[33] Only recently have scholars begun to document the rapid increase in highly processed foods, often termed ultra-processed foods, across all countries.[34, 35] We have gained a great deal of understanding in the past decade about the effect of this increased intake of higher glycemic index foods (including both sugar and most other refined carbohydrate foods). A growing consensus relates to our need to reduce significantly this refined carbohydrate component of our diet as it is a major factor in increasing our risk of diabetes.[36–38]
Understanding the reasons for the trend toward increased consumption of animal-source foods, oils, and caloric sweeteners and reduced consumption of legumes, coarse grains, and other vegetables begins with the relative price structure shifts since World War II. Most of these changes are purposeful and relate to agricultural policies across the globe.[39, 32, 40]
V. What Has This Meant for Diabetes?
Clearly, a number of dimensions of the dietary changes noted above affect the risk of diabetes. First is the increase in refined carbohydrates in all foods, particularly in beverages. Second is obesity resulting from reduced physical activity and increased inactivity. Third are physical activity patterns, which independent of the effects on body composition and energy balance have a direct effect on risk of diabetes. The discussion of diet and activity/inactivity patterns above does not include data, but in the bibliography we annotate some items that provide important details. We will focus now on body composition changes across LMICs and include an illustrative graph.
Body Mass Index and Waist Circumference
Body composition has altered across LMICs and in the United States and the United Kingdom. This overview draws on recent studies examining overweight and obesity across the globe and adds new analyses of nationally representative surveys in LMICs. We use a systematic direct analysis of all primary databases and present nationally weighted data representative of each country. Specifically, we address three important issues relevant for understanding the cardiometabolic consequences of current and future obesity patterns. First, we demonstrate the rapid increase in overweight occurring across most LMICs, even in the midst of global food and economic crises. Second, we show increasingly higher body mass index (BMI) levels among the overweight. Third, we reveal that at the same overweight or obesity levels, waist circumferences (WCs) are increasing in a number of countries for which data are available. Taken together, these issues forecast potential increases in the cardiometabolic consequences of current and future obesity.
Overweight and Obesity Prevalence
We combine overweight and obesity in LMICs. Differences in body composition and genetics have prompted a large literature showing that a disproportionate percentage of adults in LMICs are at greater risk of many cardiometabolic problems at lower BMI levels, often as low as 21 or 22.[41] Elsewhere we have published three papers on recent trends in adolescent and adult female overweight in LMICs.[42–44] The data in table 1 on overweight and obesity in LMICs[42] indicate that over two-thirds of the women in North Africa and the Middle East and half of those in Latin America and the Caribbean are overweight or obese. A smaller proportion of Asian women are overweight but the prevalence is rapidly increasing in this region.
Table 1.
Recent prevalence data on overweight and obesity for low- and middle-income countries stratified by rural and urban status (BMI≥25)
| Country | Year | Rural, nationally representative | Rural, nationally representative and age standardized | Urban, nationally representative | Urban, nationally representative and age standardized |
|---|---|---|---|---|---|
| Asia | |||||
| China | 2011 | 28.89 | 22.38 | 23.44 | 16.06 |
| Indonesia | 2000 | 29.89 | 34.20 | 28.36 | 25.17 |
| Bangladesh | 2011 | 12.79 | 11.70 | 30.14 | 27.29 |
| Nepal | 2011 | 13.25 | 12.26 | 30.15 | 28.37 |
| Middle East | |||||
| Turkey | 2003 | 56.99 | 59.42 | 57.73 | 58.75 |
| Jordan | 2009 | 75.67 | 67.72 | 72.27 | 61.86 |
| Egypt | 2008 | 74.63 | 69.39 | 83.27 | 77.14 |
| Latin America/Caribbean | |||||
| Brazil | 2008 | 42.21 | 39.55 | 42.00 | 38.24 |
| Mexico | 2012 | 64.94 | 61.78 | 67.71 | 64.87 |
| Colombia | 2010 | 53.66 | 48.95 | 50.91 | 46.31 |
| Peru | 2011 | 53.24 | 49.09 | 61.26 | 56.24 |
| Bolivia | 2008 | 51.37 | 47.87 | 57.77 | 54.66 |
| Haiti | 2012 | 23.87 | 22.51 | 37.05 | 36.25 |
| Sub-Saharan Africa | |||||
| Nigeria | 2008 | 19.39 | 18.39 | 35.73 | 33.76 |
| Ghana | 2008 | 23.05 | 22.24 | 45.84 | 43.66 |
| Zambia | 2007 | 12.63 | 12.74 | 45.84 | 43.66 |
| Côte d’Ivoire | 2011 | 18.25 | 17.18 | 40.31 | 40.54 |
| Cameroon | 2011 | 24.31 | 23.73 | 45.83 | 45.96 |
| Senegal | 2010 | 16.16 | 15.82 | 34.07 | 35.13 |
| Kenya | 2008 | 23.29 | 22.82 | 43.17 | 43.89 |
| Benin | 2006 | 13.40 | 12.56 | 31.63 | 30.34 |
| Mali | 2006 | 12.11 | 11.22 | 36.43 | 36.52 |
| Zimbabwe | 2010 | 29.33 | 28.35 | 45.56 | 46.81 |
| Burkina Faso | 2010 | 6.58 | 6.43 | 28.80 | 30.10 |
| Rwanda | 2010 | 15.71 | 15.74 | 28.57 | 27.99 |
| Tanzania | 2010 | 17.19 | 16.88 | 41.73 | 42.21 |
| Uganda | 2011 | 15.82 | 16.27 | 39.29 | 41.08 |
| Madagascar | 2008 | 5.70 | 5.18 | 15.99 | 14.88 |
| Mozambique | 2011 | 11.86 | 11.03 | 30.99 | 30.76 |
| Malawi | 2010 | 16.06 | 15.48 | 32.22 | 31.03 |
| Niger | 2006 | 8.47 | 7.90 | 42.92 | 41.27 |
| Ethiopia | 2011 | 3.13 | 3.35 | 18.07 | 19.11 |
Source: Measure Demographic and Health Surveys for all countries except China(China Health and Nutrition Survey), Indonesia (Indonesian Family Life Survey) and Mexico (National Nutrition Surveys).
Shift rightward in the entire BMI distribution
Elsewhere we reported the shifts in BMI levels at the fifth, fiftieth, and ninety-fifth percentiles in all of the Measure Demographic and Health Survey (Measure-DHS) countries.[42, 45] In general we find a marked increase in BMI levels at each percentile across the globe, particularly at the ninety-fifth. Results from eight countries provide a sense of the shifts occurring across Latin America, the Caribbean, sub-Saharan Africa, North Africa, the Middle East, and Asia. While the sizes of the increases in BMI levels vary by age and country, these results show a dramatic shift higher in the BMI distribution among those aged 30 to 40 in Mexico (1988 and 2011–12), Bolivia (1994 and 2008), Ghana (1993 and 2008), Kenya (1989 and 2008), Turkey (1993 and 2003), Morocco (1992 and 2003), China (1991 and 2009), and Indonesia (1993 and 2007). To place these results in perspective, a 1 unit BMI increase for a woman 1.6 meters tall is about 3 kilograms of weight. As such, the 6–7 unit BMI increase at the ninety-fifth percentile observed in Mexico converts to about 10 kilograms of weight gain.
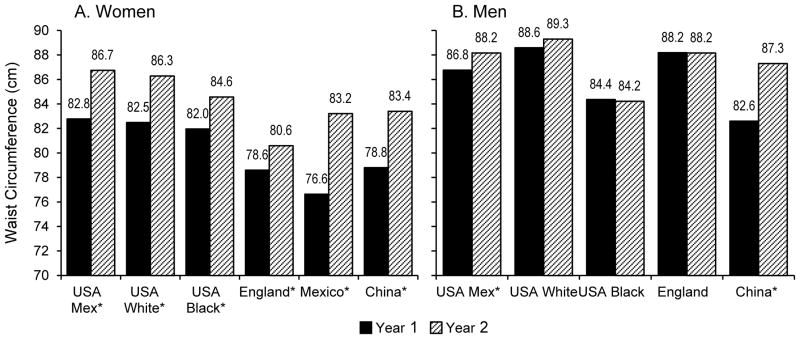
WC shift upward at each BMI level
WC has increased disproportionately over time relative to overall BMI across the United States, England, Mexico, and China, particularly among young women.[46, 47] These patterns are potentially a cause for concern across the globe. The increases were more pronounced among both men and women in China and among women in the other countries. WC data for men were not available in Mexico. The only changes for men that were statistically significant were US Hispanic men and Chinese men. The adjusted results for women and men aged 40–49 in figure 1 provide some sense of the size increase at BMI 25. At present we do not understand how these shifts affect diabetes prevalence but we would expect the effect of added abdominal adipose tissue would increase the risk of diabetes.[48–50]
VI. Conclusions
This paper highlights the major shifts in dietary, PA, and body composition patterns that are directly linked with increased risk of diabetes. We have shown that many of the underlying economic, technological, and demographic changes are accelerating. Further, agricultural systems are changing globally, directed by food companies, the retail food sector, food service companies, and agribusinesses rather than by governments. These factors point to continued increases in all of the key risk indicators for diabetes across LMICs.
We will not examine in depth the ways LMICs are responding, however, there is evidence that some countries in Asia and Latin America have begun to use large-scale regulatory, tax, and other national mechanisms to address some of the forces affecting local diets. Papers from the 2013 Bellagio Obesity Conference, “Program and Policy Options for Preventing Obesity in Low, Middle, and Transitional Income Countries,” provide recent overviews of previous efforts in LMICs (all papers have open access, see Obesity Reviews supplement, http://bellagioobesity2013.org/). Since this meeting a number of countries, particularly Mexico and several South American countries, have seen major developments.
Over the past six years, as a response to obesity and diabetes health problems, the Mexican government has embarked on several initiatives aimed at arresting the increases in obesity and subsequently reducing the burden of disease and disability.[51] In 2012 Mexico’s national nutrition survey (Ensanut 2012) showed that earlier efforts were insufficient to reduce the prevalence of obesity and that obesity continued to rise in most age groups.[51] This set the stage for the government to initiate new regulations, such as taxes on foods and beverages. A specific excise tax of approximately 10 percent on SSBs and an ad valorem sales tax of 8 percent on nonessential foods (many might think of these as “junk foods”) were initiated on January 1, 2014. Results of the impact of this tax for the first quarter of 2014 have not been published yet but do show positive food-purchasing changes (personal communication, B Popkin). Additional controls on marketing unhealthy products to children began in the summer of 2014. South American countries considering SSB taxes include Colombia, Peru, Ecuador, and Chile. Also Peru, Ecuador, and Chile either have already or will soon institute front-of-the package profiling that will signify products with high levels of added sugar, sodium, or saturated fat.[52]
Other countries have instituted programs related to schools.[53] The most exemplary is Brazil, which introduced a requirement [54, 55] that schools must purchase 30 percent of the food they offer from local, small family farms and cooperatives. Also 70 percent of the food must be a basic (not processed) food.
In summary, this paper has shown the increasing prevalence of overweight and obesity across LMICs and the related potential for significant increases in cardiometabolic problems, especially diabetes. This relates not only to increases in BMI and WC but also to reduced PA, increased sedentary time, and dietary changes. Global diets show large shifts toward processed foods high in refined carbohydrates and added sugars and away from legumes, coarse grains, and other vegetables. LMICs are among the most active countries in the world in attempting to address these problems with large-scale regulatory efforts. Nevertheless, to date these efforts are concentrated in only a few countries and, other than the effort in Mexico, are yet to be rigorously evaluated. Thus LMICs in general face serious challenges with little likelihood of prevention.
Figure 2.
Predicted mean WC (cm) for BMI=25 kg/m2 in Year 2 compared to Year 1 for women and men aged 40–49 years in the US (by race/ethnicity), England, Mexico, and China
Source: Data are derived from: China: The China Health and Nutrition Survey (CHNS, 1993 and 2011): England: The National Heights and Weight Survey, 1992–93 and 2008–9.United States: The National Health and Nutrition Examination Survey (NHANES III:1988–94 and the combined NHANES 2007–8 plus 2009–10). Mexico: The Mexican Nutrition Survey 1999 (MSN 1999) and the Mexican National Health and Nutrition Survey 2012 (NHNS 2012) Models include: age (categorized: 20–29, 30–39 40–49 years), BMI, BMI-squared, survey year, age*survey year, BMI*survey year, BMI-squared*survey year. For brevity, only results for age group 40–49 years shown in figure.
Source: Albrecht et al, add reference once final
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
Barry M. Popkin declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Caballero B, Popkin BM. The nutrition transition: Diet and Disease in the Developing World. London: Academic Press; 2002. [Google Scholar]
- 2.Popkin BM. The nutrition transition and its health implications in lower-income countries. Public Health Nutr. 1998;1(1):5–21. doi: 10.1079/phn19980004. [DOI] [PubMed] [Google Scholar]
- 3.Popkin BM. The shift in stages of the nutrition transition in the developing world differs from past experiences! Public Health Nutr. 2002;5(1A):205–14. doi: 10.1079/PHN2001295. [DOI] [PubMed] [Google Scholar]
- 4.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. This is the author’s most recent detailed assessment of the overall shifts in diet, PA, and body composition and the developmental origins of health and disease. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babu SC, Blom S. Building resilience for food and nutrition security. 2020 Conference Brief. 2014;6 [Google Scholar]
- 6.Anand S, Hawkes C, de Souza R, Mente A, Dehghan M, Nugent R, et al. Global food consumption and its impact on cardiovascular disease requires global solutions with a focus on the globalized food system. J Am Coll Cardiol. In Press This article, the product of a World Heart Association consensus conference, reviews changes in diets and the global agricultural and food systems. It discusses the systemic alterations all nations must make to address the resultant health problems and to prevent future increases in heart disease. [Google Scholar]
- 7.Popkin B. Technology, transport, globalization and the nutrition transition. Food Policy. 2006;31(554):569. [Google Scholar]
- 8.Mendez MA, Popkin BM. Globalization, urbanization, and nutritional change in the developing world. Electron J Agr Dev Econ. 2005;1:220–41. [Google Scholar]
- 9.Popkin B, Bisgrove EZ. Urbanization and nutrition in low-income countries. Food Nutr Bull. 1988;10:3–23. [Google Scholar]
- 10.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012;13(8):659–80. doi: 10.1111/j.1467-789X.2011.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dearth-Wesley T, Popkin B, Ng S. Estimated and forecasted trends in domain specific time-use and energy expenditure among adults in Russia. Int J Behav Nutr Phys Act. 2014;11:11. doi: 10.1186/1479-5868-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tudor-Locke C, Ainsworth BE, Popkin BM. Active commuting to school: an overlooked source of childrens' physical activity? Sports Med. 2001;31(5):309–13. doi: 10.2165/00007256-200131050-00001. [DOI] [PubMed] [Google Scholar]
- 13.Tudor-Locke C, Neff LJ, Ainsworth BE, Addy CL, Popkin BM. Omission of active commuting to school and the prevalence of children's health-related physical activity levels: the Russian Longitudinal Monitoring Study. Child Care Health Dev. 2002;28(6):507–12. doi: 10.1046/j.1365-2214.2002.00295.x. [DOI] [PubMed] [Google Scholar]
- 14.Tudor-Locke C, Ainsworth BE, Adair LS, Du S, Popkin BM. Physical activity and inactivity in Chinese school-aged youth: the China Health and Nutrition Survey. Int J Obes Relat Metab Disord. 2003;27(9):1093–9. doi: 10.1038/sj.ijo.0802377. [DOI] [PubMed] [Google Scholar]
- 15.Tudor-Locke C, Ainsworth BE, Adair LS, Popkin BM. Objective physical activity of Filipino youth stratified for commuting mode to school. Med Sci Sports Exerc. 2003;35(3):465–71. doi: 10.1249/01.MSS.0000053701.30307.A6. [DOI] [PubMed] [Google Scholar]
- 16.Tudor-Locke C, Ainsworth BE, Adair LS, Popkin BM. Physical activity in Filipino youth: the Cebu Longitudinal Health and Nutrition Survey. Int J Obes Relat Metab Disord. 2003;27(2):181–90. doi: 10.1038/sj.ijo.802207. [DOI] [PubMed] [Google Scholar]
- 17.Tudor-Locke C, Ainsworth BE, Adair LS, Du S, Lee N, Popkin BM. Cross-sectional comparison of physical activity and inactivity patterns in Chinese and Filipino youth. Child Care Health Dev. 2007;33(1):59–66. doi: 10.1111/j.1365-2214.2006.00612.x. [DOI] [PubMed] [Google Scholar]
- 18.Tudor-Locke C, Ainsworth BE, Popkin BM. Patterns of physical activity and overweight among 7–13-year-old Russian children: a 7-year nationally representative monitoring study. Res Q Exerc Sport. 2008;79(1):10–7. doi: 10.1080/02701367.2008.10599455. [DOI] [PubMed] [Google Scholar]
- 19.Popkin B, Drewnowski A. Dietary fats and the nutrition transition: New trends in the global diet. Nutr Rev. 1997;55:31–43. doi: 10.1111/j.1753-4887.1997.tb01593.x. [DOI] [PubMed] [Google Scholar]
- 20.Wang Z, Zhai F, Du S, Popkin B. Dynamic shifts in Chinese eating behaviors. Asia Pac J Clin Nutr. 2008;17(1):123–30. [PubMed] [Google Scholar]
- 21.Popkin BM, Nielsen SJ. The sweetening of the world's diet. Obes Res. 2003;11(11):1325–32. doi: 10.1038/oby.2003.179. [DOI] [PubMed] [Google Scholar]
- 22.Ng SW, Slining MM, Popkin BM. Use of caloric and noncaloric sweeteners in US consumer packaged foods, 2005–2009. J Acad Nutr Diet. 2012;112(11):1828–34. e6. doi: 10.1016/j.jand.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33(11):2477–83. doi: 10.2337/dc10-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98(4):1084–102. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Odegaard AO, Koh W-P, Arakawa K, Yu MC, Pereira MA. Soft drink and juice consumption and risk of physician-diagnosed incident type 2 diabetes: The Singapore Chinese Health Study. Am J Epidemiol. 2010;171(6):701–8. doi: 10.1093/aje/kwp452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bazzano L, Li T, Joshipura K, Hu F. Intake of fruit, vegetables, and fruit juices and risk of diabetes in women. Diabetes Care. 2008;31(7):1311–7. doi: 10.2337/dc08-0080. dc08-0080 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Delgado CL. Rising consumption of meat and milk in developing countries has created a new food revolution. J Nutr. 2003;133(11 Suppl 2):3907S–10S. doi: 10.1093/jn/133.11.3907S. [DOI] [PubMed] [Google Scholar]
- 28.Du S, Mroz TA, Zhai F, Popkin BM. Rapid income growth adversely affects diet quality in China--particularly for the poor! Soc Sci Med. 2004;59(7):1505–15. doi: 10.1016/j.socscimed.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 29.Popkin BM, Du S. Dynamics of the nutrition transition toward the animal foods sector in China and its implications: a worried perspective. J Nutr. 2003;133(11 Suppl 2):3898S–906S. doi: 10.1093/jn/133.11.3898S. [DOI] [PubMed] [Google Scholar]
- 30.Popkin BM, Keyou G, Zhai F, Guo X, Ma H, Zohoori N. The nutrition transition in China: a cross-sectional analysis. Eur J Clin Nutr. 1993;47(5):333–46. [PubMed] [Google Scholar]
- 31.Du S, Lu B, Zhai F, Popkin BM. A new stage of the nutrition transition in China. Public Health Nutr. 2002;5(1A):169–74. doi: 10.1079/PHN2001290. [DOI] [PubMed] [Google Scholar]
- 32.Popkin BM. The World Is Fat--The Fads, Trends, Policies, and Products That Are Fattening the Human Race. New York: Avery-Penguin Group; 2008. [Google Scholar]
- 33.Popkin BM, Siega-Riz AM, Haines PS. A comparison of dietary trends among racial and socioeconomic groups in the United States. New Eng J Med. 1996;335(10):716–20. doi: 10.1056/NEJM199609053351006. [DOI] [PubMed] [Google Scholar]
- 34.Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14:21–8. doi: 10.1111/obr.12107. [DOI] [PubMed] [Google Scholar]
- 35.Monteiro CA, Levy RB, Claro RM, de Castro IR, Cannon G. Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil. Public Health Nutr. 2011;14(1):5–13. doi: 10.1017/S1368980010003241. [DOI] [PubMed] [Google Scholar]
- 36.Lennerz BS, Alsop DC, Holsen LM, Stern E, Rojas R, Ebbeling CB, et al. Effects of dietary glycemic index on brain regions related to reward and craving in men. Am J Clin Nutr. 2013;98(3):641–7. doi: 10.3945/ajcn.113.064113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.U.S. Department of Health and Human Services and the US Department of Agriculture. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. Washington DC: Office of Disease Prevention and Health Promotion USDHHS; 2015. [Google Scholar]
- 38.Ludwig DS. Technology, diet, and the burden of chronic disease. JAMA. 2011;305(13):1352–3. doi: 10.1001/jama.2011.380. This is an overview of the shifts in overweight, BMI distribution, WC, and WC-BMI ratio in LMICs. [DOI] [PubMed] [Google Scholar]
- 39.Popkin BM. Agricultural policies, food and public health. EMBO Rep. 2011;12(1):11–8. doi: 10.1038/embor.2010.200. This presents the only data for LMICs on trends in overweight and obesity in adolescents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anand SS, Hawkes Corinna, de Souza Russell J, Mente Andrew, Dehghan Mahshid, Nugent Rachel, Zulyniak Michael A, Weis Tony, Bernstein Adam M, Krauss Ronald, Kromhout Daan, Jenkins David JA, Malik Vasanti, Martinez-Gonzalez Miguel A, Mozafarrian Dariush, Yusuf Salim, Willett Walter C, Popkin Barry M. Global Food Consumption and its impact on Cardiovascular Disease requires Global Solutions with a Focus on the globalized food system. Journal of the American College of Cardiology. doi: 10.1016/j.jacc.2015.07.050. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63. doi: 10.1016/S0140-6736(03)15268-3. S0140-6736(03)15268-3 [pii] [DOI] [PubMed] [Google Scholar]
- 42.Popkin BM, Slining MM. New dynamics in global obesity facing low- and middle-income countries. Obes Rev. 2013;14:11–20. doi: 10.1111/obr.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jaacks LM, Slining MM, Popkin BM. Recent trends in the prevalence of under- and overweight among adolescent girls in low- and middle-income countries. Pediatr Obes. 2015 doi: 10.1111/ijpo.12000. n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jaacks LM, Slining MM, Popkin BM. Recent underweight and overweight trends by rural–urban residence among women in low- and middle-income countries. J Nutr. 2015 doi: 10.3945/jn.114.203562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Albrecht SS, Barquera S, Popkin BM. Exploring secular changes in the association between BMI and waist circumference in Mexican-Origin and white women: A comparison of Mexico and the United States. Am J Hum Biol. 2014;26(5):627–34. doi: 10.1002/ajhb.22573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Albrecht SS, Gordon-Larsen P, Stern D, Popkin BM. Is waist circumference per body mass index rising differentially across the US, England, China, and Mexico? Eur J Clin Nutr. doi: 10.1038/ejcn.2015.71. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stern D, Smith LP, Zhang B, Gordon-Larsen P, Popkin BM. Changes in waist circumference relative to body mass index in Chinese adults, 1993–2009. Int J Obes. 2014;38(12):1503–10. doi: 10.1038/ijo.2014.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881–7. doi: 10.1038/nature05488. [DOI] [PubMed] [Google Scholar]
- 49.Ross R, Despres JP. Abdominal obesity, insulin resistance, and the metabolic syndrome: contribution of physical activity/exercise. Obesity. 2009;17(Suppl 3):S1–2. doi: 10.1038/oby.2009.381. [DOI] [PubMed] [Google Scholar]
- 50.Després J-P, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28(6):1039–49. doi: 10.1161/atvbaha.107.159228. [DOI] [PubMed] [Google Scholar]
- 51.Barquera S, Campos I, Rivera J. Mexico attempts to tackle obesity: the process, results, push backs and future challenges. Obes Rev. 2013;14:69–78. doi: 10.1111/obr.12096. [DOI] [PubMed] [Google Scholar]
- 52.Corvalán C, Reyes M, Garmendia M, Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: the Chilean Law of Food Labeling and Advertising. Obes Rev. 2013;14:79–87. doi: 10.1111/obr.12099. [DOI] [PubMed] [Google Scholar]
- 53.Foo LL, Vijaya K, Sloan RA, Ling A. Obesity prevention and management: Singapore's experience. Obes Rev. 2013;14:106–13. doi: 10.1111/obr.12092. [DOI] [PubMed] [Google Scholar]
- 54.Coitinho D, Monteiro C, Popkin B. What Brazil is doing to promote healthy diets and active lifestyles. Public Health Nutr. 2002;5(1A):263–7. doi: 10.1079/phn2001302. [DOI] [PubMed] [Google Scholar]
- 55.Jaime P, da Silva A, Gentil P, Claro R, Monteiro C. Brazilian obesity prevention and control initiatives Brazil: Brazilian obesity prevention and control initiatives. Obes Rev. 2013:14. doi: 10.1111/obr.12101. [DOI] [PubMed]