Abstract
Background
Studies consisting mostly of whites have shown that the prevalence of masked hypertension differs by prehypertension status. Using data from the Jackson Heart Study, an exclusively African American population‐based cohort, we evaluated the association of masked hypertension and prehypertension with left ventricular mass index and common carotid intima media thickness.
Methods and Results
At the baseline visit, clinic blood pressure (CBP) measurement and 24‐hour ambulatory blood pressure monitoring were performed. Masked hypertension was defined as mean systolic/diastolic CBP <140/90 mm Hg and mean daytime systolic/diastolic ambulatory blood pressure ≥135/85 mm Hg. Clinic hypertension was defined as mean systolic/diastolic CBP ≥140/90 mm Hg. Normal CBP was defined as mean systolic/diastolic CBP <120/80 mm Hg and prehypertension as mean systolic/diastolic CBP 120 to 139/80 to 89 mm Hg. The analytic sample included 909 participants. Among participants with systolic/diastolic CBP <140/90 mm Hg, the prevalence of masked hypertension and prehypertension was 27.5% and 62.4%, respectively. The prevalence of masked hypertension among those with normal CBP and prehypertension was 12.9% and 36.3%, respectively. In a fully adjusted model, which included prehypertension status and antihypertensive medication use as covariates, left ventricular mass index was 7.94 g/m2 lower among those without masked hypertension compared to participants with masked hypertension (P<0.001). Left ventricular mass index was also 4.77 g/m2 lower among those with clinic hypertension, but this difference was not statistically significant (P=0.068). There were no significant differences in left ventricular mass index between participants with and without masked hypertension, or clinic hypertension.
Conclusions
Masked hypertension was common among African Americans with prehypertension and also normal CBP, and was associated with subclinical cardiovascular disease.
Keywords: blood pressure, cardiovascular diseases, epidemiology, hypertension
Subject Categories: Hypertension
Introduction
Masked hypertension is defined as nonelevated clinic blood pressure and elevated daytime ambulatory blood pressure measured using 24‐hour ambulatory blood pressure monitoring (ABPM).1, 2 It has been reported that individuals with masked hypertension have a higher risk of target organ damage and cardiovascular disease (CVD) events than individuals with sustained normotension (ie, nonelevated clinic and daytime ambulatory blood pressure).3, 4
It is unclear who should be screened for masked hypertension. In a sample consisting mostly of white participants not taking antihypertensive medications in the Masked Hypertension Study, 34% of participants with clinic blood pressure in the prehypertension range (systolic blood pressure [SBP] 120–139 or diastolic blood pressure [DBP] 80–89 mm Hg) had masked hypertension.5 The prevalence of masked hypertension was only 3.9% among participants with normal clinic blood pressure (<120/80 mm Hg).5 However, there are few data on the prevalence of masked hypertension among African Americans,6, 7, 8, 9 a population with a high prevalence of prehypertension10 and increased risk for blood pressure–related CVD outcomes.11 Furthermore, limited studies exist on the extent to which the association between masked hypertension and subclinical CVD risk is independent of prehypertension among African Americans.
If the prevalence of masked hypertension and its associated CVD risk are high only among those with prehypertension, then ABPM may be indicated for African Americans with prehypertension, and deferred for African Americans with normal clinic blood pressure. Using data from the Jackson Heart Study (JHS), an exclusively African American population‐based cohort, we evaluated the degree of overlap between masked hypertension and prehypertension. We hypothesized that the prevalence of masked hypertension would be higher among participants with prehypertension than those with normal clinic blood pressure. Additionally, we determined the associations of masked hypertension with measures of subclinical CVD including left ventricular mass index (LVMI) and common carotid intima media thickness (CCIMT), and whether these associations were independent of prehypertension status. We hypothesized that participants without masked hypertension would have lower LVMI and CCIMT than participants with masked hypertension after adjusting for prehypertension status.
Methods
Study Population and Overview of Data Collection
The JHS is a large, population‐based observational study designed to evaluate CVD risk among African Americans; detailed methods are described elsewhere.12, 13 Briefly, 5301 participants were recruited from urban and rural areas of the 3 counties (Hinds, Madison, and Rankin) in the Jackson, MS metropolitan statistical area. Potential participants were selected for enrollment through a combination of drivers' license registries, commercially available lists, and a subset of participants in the Atherosclerosis Risk in Communities study who were living in the Jackson, MS area. Recruitment was limited to noninstitutionalized African Americans aged ≥21 years. The JHS was approved by institutional review boards of the 3 participating institutions (the University of Mississippi Medical Center, Tougaloo College, and Jackson State University), and all participants provided informed consent. The analysis of JHS data reported here was approved by the institutional review board at the University of Alabama at Birmingham.
Clinical Measures
Data were collected through interviewer and self‐administered questionnaires and a clinical examination after an overnight fast. Information on age, sex, education, income, cigarette smoking, physical activity, antihypertensive medication use, and a history of diabetes, stroke, or myocardial infarction were collected during the interview. Physical activity was assessed as a composite of 4 index scores (active living, work, sport, and home and family life) with values for each ranging from 1 to 5. A total physical activity score was calculated as the sum of the 4 individual index scores, with higher scores indicating higher physical activity levels.14 During the examination, standardized protocols were followed to obtain blood pressure, height, and weight and to collect blood and urine samples. Using measured height and weight, body mass index (kg/m2) was calculated. Fasting serum glucose was measured using a glucose oxidase method on a Vitros 950 or 250 analyzer (Ortho‐Clinical Diagnostics, Raritan, NJ). Hemoglobin A1c was measured using a TOSOH high‐performance liquid chromatography system. Antihypertensive medication use was determined by self‐report. The number of antihypertensive medication classes being taken was determined using a medication inventory conducted during the clinic visit. Diabetes was defined by a fasting glucose ≥126 mg/dL, hemoglobin A1c ≥6.5%, or use of insulin or glucose‐lowering pills. Serum creatinine was measured using a multipoint enzymatic spectrophotometric assay on a Vitros 950 analyzer (Ortho‐Clinical Diagnostics). Creatinine values were biochemically calibrated to Cleveland Clinic‐equivalent Minnesota Beckman CX3 assay for analysis purposes. Estimated glomerular filtration rate was calculated via the Chronic Kidney Disease Epidemiology Collaboration equation.15 Low‐density lipoprotein and high‐density lipoprotein cholesterol were measured using enzymatic methods (Roche Diagnostics, Indianapolis, IN). Two‐dimensional echocardiography and carotid ultrasonography were also conducted using previously described protocols.16
Clinic Blood Pressure
Clinic blood pressure was measured twice, with at least 1 minute between each measure, using a Hawksley random‐zero sphygmomanometer (Hawksley and Sons Ltd, Langing, UK) and an appropriately sized blood pressure cuff. Cuff size was determined by upper‐arm circumference. Measurements were taken (after a 5‐minute rest) in the right arm of seated participants whose back and arm were supported. The average of the 2 measurements was used to define clinic blood pressure.
Ambulatory Blood Pressure
Upon completion of the study visit, all participants were invited to complete ABPM over the next 24 hours. A subset of 1148 participants agreed and subsequently underwent ABPM. ABPM measurements were obtained with a portable, noninvasive oscillometric device (Spacelabs 90207; Medifacts International Ltd, Rockville, MD) with a cuff fitted to the participant's nondominant arm. Trained technicians calibrated the ABPM devices and instructed participants in their proper use. The devices were programmed to measure blood pressure every 20 minutes for 24 hours. Participants returned to the clinic after 24 hours for the removal of the device and the blood pressure readings were downloaded into a commercially available software program (Medicom, version 3.41; Medifacts International Ltd, Rockville, MD). Quality control was assured by technician recertification, procedural checklists, and data review.12, 17, 18, 19 Having complete ABPM data was defined using International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome criteria20 (10+ daytime and 5+ nighttime readings). Daytime was defined as the time period from 10:00 am to 8:00 pm, and nighttime was defined as a time period from midnight to 6:00 am.
Hypertension Categories Defined by Clinic Blood Pressure and ABPM
Clinic hypertension was defined as mean clinic SBP ≥140 mm Hg or mean clinic DBP ≥90 mm Hg. Ambulatory hypertension was defined as mean daytime ambulatory SBP ≥135 mm Hg or mean daytime ambulatory DBP ≥85 mm Hg, consistent with prior consensus statements and position papers.21, 22 Participants with nonelevated clinic blood pressure (mean clinic SBP <140 mm Hg and mean clinic DBP <90 mm Hg) were categorized either as having prehypertension, defined by mean SBP 120 to 139 mm Hg or mean DBP 80 to 89 mm Hg, or as having normal clinic blood pressure levels, defined by mean SBP <120 mm Hg and mean DBP <80 mm Hg.23 Masked hypertension was defined as having nonelevated clinic blood pressure with ambulatory hypertension.
The terms “prehypertension” and “masked hypertension” often refer to individuals not taking antihypertensive medications. For participants taking antihypertensive medications, “on‐treatment blood pressure SBP/DBP of 120 to 139/80 to 89 mm Hg” and “masked uncontrolled hypertension” are corresponding terms for prehypertension and masked hypertension, respectively. However, for simplicity in the presentation of the results, we used the terms “prehypertension” and “masked hypertension” in our study for all participants, regardless of antihypertensive medication use.
Echocardiography
Two‐dimensional echocardiography (Sonos‐4500; Philips Medical Systems, Andover, MA) was used for assessment of left ventricular (LV) dimensions including LV internal diameter during diastole, interventricular septal thickness during diastole, and posterior wall thickness during diastole, according to previously described protocols16 based on the recommendations of the American Society of Echocardiography. LV mass (grams) was calculated using the American Society of Echocardiography formula.24 LVMI was calculated by dividing LV mass (grams) by estimated body surface area (m2).
Carotid Ultrasonography
CCIMT was measured using electrocardiography‐gated, B‐mode, and spectral steered Doppler with an integrated ultrasound machine to obtain carotid artery images. Mean and maximum values were obtained for each carotid artery segment, side, and wall, and maximum likelihood estimates were calculated by adjusting for missing data in the collecting, processing, and reading of images. CCIMT represented a maximum likelihood estimate of mean far‐wall of average values across the right and left side of the common carotid artery.
Statistical Analyses
For the current analyses, we utilized data for participants who had valid data on ABPM, clinic blood pressure, medical history, antihypertensive medication use, echocardiography measurements for calculation of LVMI, and carotid ultrasonography measurements for determination of CCIMT. Of the 1148 participants who underwent ABPM, 1046 had complete ABPM data. After excluding 137 participants with missing data on clinic blood pressure, medical history, antihypertensive medication use, LVMI, or CCIMT, we included 909 participants in the current analysis. As shown in Table S1, compared with JHS participants who were not included in the analyses, those who were included were older, had a lower body mass index, lower clinic DBP, and had a greater likelihood of being female and having diabetes and less than a high school education.
Baseline demographic, clinical, and behavioral characteristics were calculated for the overall analytical cohort, and for participants without and with masked hypertension, and separately for those with clinic hypertension. The prevalence of masked hypertension and, separately, prehypertension among participants with nonelevated clinic blood pressure was determined. Furthermore, the prevalence of masked hypertension was calculated for participants with normal clinic blood pressure and, separately, those with prehypertension. The prevalence of prehypertension was calculated for participants without and with masked hypertension.
Mean differences in LVMI were compared for participants without and with masked hypertension using 1‐way ANOVA. Next, ANCOVA was performed to evaluate differences in LVMI after controlling for age and sex (Model 1). A second multivariable model (Model 2) additionally controlled for body mass index, diabetes status, education level, alcohol consumption, smoking status, physical activity, diabetes, and estimated glomerular filtration rate <60 mL/min per 1.73 m2. Analyses were repeated for CCIMT with Model 2 including 2 additional covariables: low‐density lipoprotein and high‐density lipoprotein cholesterol. A third multivariable model (Model 3) additionally adjusted for prehypertension status and antihypertensive medication use. Participants with masked hypertension comprised the referent group for unadjusted and adjusted analyses. The tests for interaction between antihypertensive medication use and masked hypertension status on LVMI and CCIMT were not statistically significant (interaction P=0.611 and 0.193, respectively). The tests for interaction between prehypertension and masked hypertension status on LVMI and CCIMT were also not statistically significant (interaction P=0.365 and 0.132, respectively). Therefore, analyses were not stratified by either antihypertensive medication use or prehypertension status. As all analyses were based on a priori assumptions and hypotheses, we did not correct the analyses for multiple testing.25 Statistical analyses were performed using SAS Version 9.3 (SAS Institute, Cary, NC).
Results
Baseline Characteristics
The characteristics of the 909 participants in the analytic cohort are presented in Table 1 for the overall analytical sample, and for those without and with masked hypertension and with clinic hypertension. Among the 909 participants, 518 (57.0%) were taking antihypertensive medication.
Table 1.
Characteristics of Analytic Cohort of JHS Participants, Overall and by Hypertension Category
| Overall (n=909) | No Masked HTN (n=493) | Masked HTN (n=187) | Clinic HTN (n=229) | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, y | 59.1±10.9 | 57.4±11.1 | 61.1±9.8 | 61.1±10.5 |
| Female sex, % | 69.3 | 73.2 | 62.0 | 66.8 |
| Education less than high school, % | 17.6 | 16.8 | 16.0 | 20.5 |
| Clinical characteristics | ||||
| Body mass index, kg/m2 | 31.1±6.6 | 31.5±6.7 | 30.0±5.7 | 31.4±6.7 |
| Diabetes, % | 24.6 | 21.4 | 30.4 | 26.9 |
| LDL, mg/dL | 125.7±35.8 | 125.0±35.3 | 127.2±37.3 | 125.9±35.5 |
| HDL, mg/dL | 54.2±15.2 | 53.9±14.8 | 54.2±14.5 | 55.1±16.7 |
| eGFR <60 mL/min per 1.73 m2, % | 8.4 | 6.1 | 11.0 | 11.0 |
| Health behaviors | ||||
| Alcohol consumption, % | 36.7 | 40.8 | 33.2 | 31.0 |
| Current smoking, % | 9.6 | 7.3 | 14.4 | 10.5 |
| Total physical activity score | 8.4±2.6 | 8.4±2.6 | 8.4±2.7 | 8.2±2.5 |
| Blood pressure measures | ||||
| Clinic blood pressure | ||||
| SBP, mm Hg | 127.1±17.4 | 118.0±11.1 | 125.3±9.7 | 148.1±15.2 |
| DBP, mm Hg | 77.3±10.1 | 74.2±7.8 | 75.5±9.1 | 85.5±10.7 |
| Ambulatory blood pressure | ||||
| Daytime SBP, mm Hg | 128.9±13.1 | 121.0±7.9 | 139.9±8.7 | 137.0±13.8 |
| Daytime DBP, mm Hg | 77.6±9.2 | 73.5±6.4 | 84.4±8.3 | 80.9±10.2 |
| Nighttime SBP, mm Hg | 120.5±15.3 | 112.9±10.6 | 129.0±14.3 | 129.7±15.7 |
| Nighttime DBP, mm Hg | 68.1±9.6 | 64.4±7.4 | 72.8±9.8 | 72.1±10.3 |
| Antihypertensive medication, % | 57.0 | 49.5 | 63.6 | 67.7 |
Numbers in table are percentage or mean±SD. DBP indicates diastolic blood pressure; eGFR, estimated glomerular filtration rate; HDL, high‐density lipoprotein cholesterol; HTN, hypertension; JHS, Jackson Heart Study; LDL, low‐density lipoprotein cholesterol; SBP, systolic blood pressure.
Prevalence of Masked Hypertension and Prehypertension
Among participants with nonelevated clinic blood pressure, the prevalence of masked hypertension and prehypertension was 27.5% and 62.4%, respectively. The prevalence of masked hypertension was 12.9% and 36.3% among participants with normal clinic blood pressure and prehypertension, respectively (Figure A). The prevalence of prehypertension among participants without and with masked hypertension was 54.8% and 82.3%, respectively (Figure B). The cross‐categorization of prehypertension status by masked hypertension status among those with nonelevated clinic blood pressure stratified by antihypertensive medication use is shown in Table S2. The prevalence of masked hypertension was 21.5% and 32.8% among participants not taking and taking antihypertensive medication, respectively. The prevalence of masked hypertension was higher for participants taking antihypertensive medication versus participants not taking antihypertensive medication among those with normal clinic blood pressure (19.4% versus 6.8%, respectively) and prehypertension (39.7% versus 31.9%, respectively). There was no interaction between antihypertensive medication use and prehypertension status on the prevalence of masked hypertension (interaction P=0.498).
Figure 1.
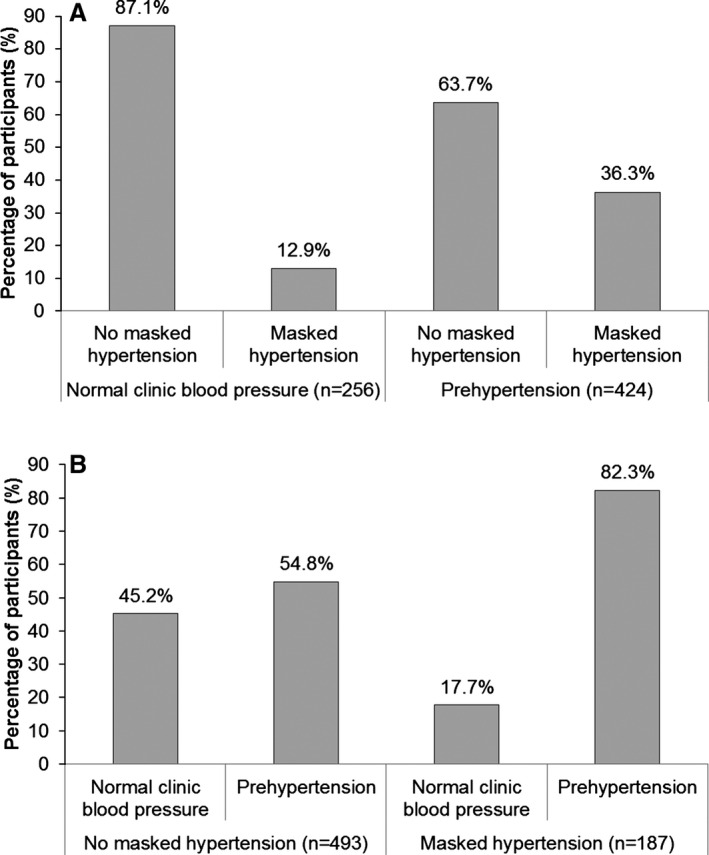
Percentage of participants with and without masked hypertension by prehypertension status (A), and percentage of participants with and without prehypertension by masked hypertension status (B) among those with nonelevated clinic blood pressure (n=680).
Associations of Masked Hypertension, Prehypertension, and Clinic Hypertension With Subclinical Cardiovascular Disease
LVMI
Mean (95% CI) LVMI was higher in participants with masked hypertension compared with those without masked hypertension or clinic hypertension (Table 2). After adjustment for age and sex (Model 1), LVMI was lower for those without masked hypertension (P<0.001), and those with clinic hypertension (P=0.038) compared to participants with masked hypertension. These differences remained statistically significant after further adjustment for body mass index, diabetes status, education level, alcohol consumption, smoking status, physical activity, and estimated glomerular filtration rate <60 mL/min per 1.73 m2. In a fully adjusted model that included prehypertension status and antihypertensive medication use as covariates (Model 3), LVMI was lower among participants without masked hypertension versus those with masked hypertension (P<0.001). LVMI was 4.77 g/m2 lower among participants with clinic hypertension versus those with masked hypertension, but this difference was not statistically significant (P=0.068).
Table 2.
Differences in Left Ventricular Mass Index (LVMI) Among Participants With No Masked Hypertension, Masked Hypertension, and Clinic Hypertension
| No Masked HTN (n=493) | Masked HTN (n=187) | Clinic HTN (n=229) | |
|---|---|---|---|
| Mean (95% CI) LVMI, g/m2 | 76.37 (74.83–77.91) | 85.55 (82.05–89.04) | 81.00 (78.00–84.00) |
| Model 1 | −9.43±1.84 | 0 (ref) | −4.33±2.08 |
| P‐value | <0.001 | — | 0.038 |
| Model 2 | −8.15±1.93 | 0 (ref) | −4.33±2.16 |
| P‐value | <0.001 | — | 0.046 |
| Model 3 | −7.94±1.99 | 0 (ref) | −4.77±2.61 |
| P‐value | <0.001 | — | 0.068 |
Data from the regression models are presented as adjusted difference±SE in LVMI with masked HTN as the referent group. Model 1 adjusts for age and sex. Model 2 adjusts for variables in Model 1+body mass index, diabetes status, education level, alcohol consumption, smoking status, physical activity, and estimated glomerular filtration rate <60 mL/min per 1.73 m2. Model 3 adjusts for variables in Model 2+prehypertension status and antihypertensive medication use. HTN indicates hypertension; LVMI, left ventricular mass index.
CCIMT
Mean (95% CI) CCIMT was 0.72 (0.71–0.74) mm, 0.78 (0.75–0.80) mm, and 0.78 (0.74–0.81) mm among participants without masked hypertension, with masked hypertension, and with clinic hypertension, respectively (Table 3). After adjustment for age and sex (Model 1) and compared to participants with masked hypertension, CCIMT was lower for those without masked hypertension (P=0.004). There was no statistically significant difference in CCIMT between participants with masked hypertension and those with clinic hypertension (P=0.912). After further multivariable adjustment (Models 2 and 3), there were no statistically significant differences in CCIMT between participants with masked hypertension and either participants without masked hypertension or with clinic hypertension.
Table 3.
CCIMT Among Participants With No Masked Hypertension, Masked Hypertension, and Clinic Hypertension
| No Masked HTN (n=493) | Masked HTN (n=187) | Clinic HTN (n=229) | |
|---|---|---|---|
| Mean (95% CI) CCIMT, mm | 0.72 (0.71–0.74) | 0.78 (0.75–0.80) | 0.78 (0.74–0.81) |
| Model 1 | −0.04±0.01 | 0 (ref) | 0.00±0.02 |
| P‐value | 0.004 | — | 0.912 |
| Model 2 | −0.02±0.02 | 0 (ref) | 0.02±0.02 |
| P‐value | 0.149 | — | 0.411 |
| Model 3 | −0.02±0.02 | 0 (ref) | 0.01±0.02 |
| P‐value | 0.151 | — | 0.766 |
Data from the regression models are presented as adjusted difference±SE in common carotid intima media thickness with masked HTN as the referent group. Model 1 adjusts for age and sex. Model 2 adjusts for variables in Model 1+body mass index, diabetes status, LDL, HDL, education level, alcohol consumption, smoking status, physical activity, and estimated glomerular filtration rate <60 mL/min per 1.73 m2. Model 3 adjusts for Model 2 variables+prehypertension status and antihypertensive medication use. CCIMT indicates common carotid intima media thickness; HTN, hypertension; HDL, high‐density lipoprotein cholesterol; LDL, low‐density lipoprotein cholesterol.
Discussion
In the current study, there was substantial overlap between masked hypertension and prehypertension. Additionally, masked hypertension was relatively common (12.9%) among participants with normal clinic blood pressure. LVMI was higher among participants with masked hypertension compared with those without masked hypertension or clinic hypertension. The association between masked hypertension and LVMI was present after adjusting for prehypertension status. We did not observe significant associations of masked hypertension with CCIMT.
ABPM has been conducted in several population‐based samples from around the world.26 However, data on masked hypertension among African Americans are scarce, and few studies have examined the prevalence of masked hypertension by prehypertension status, or the association of masked hypertension with CVD risk, independent of prehypertension. Consistent with a prior study in the JHS cohort,27 there was a substantial degree of overlap of masked hypertension with prehypertension in the current study. These data are consistent with the findings in prior studies of predominately white US and European cohorts5, 28, 29, 30 that have shown a large proportion of individuals with masked hypertension have prehypertension, and masked hypertension is commonly present in individuals with prehypertension. Furthermore, the current study suggests that regardless of prehypertension status, masked hypertension is associated with LVMI in African Americans.
In the current study, the prevalence of masked hypertension was 21.5% and 32.8% among participants not taking and taking antihypertensive medication, respectively. These findings are consistent with data from European and Asian participants in an International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome study where the prevalence of masked hypertension was higher among nondiabetic participants with nonelevated clinic blood pressure who were untreated versus treated with antihypertensive medication (18.8% versus 29.3%, respectively).28 The data for those taking antihypertensive medication are also consistent with a high prevalence of masked hypertension (31.1%) reported in a large Spanish cohort of patients with treated hypertension.30 It has been hypothesized that the differential prevalence of masked hypertension in treated versus untreated individuals can be partially explained by the larger effect of antihypertensive medication on clinic blood pressure versus ambulatory blood pressure, and that a large proportion of treated individuals with masked hypertension may have had sustained hypertension before initiating antihypertensive medication.28, 31
Given the high prevalence of masked hypertension among those with prehypertension, and that the prevalence of masked hypertension was relatively high (12.9%) even among those with normal clinic blood pressure, the current results suggest that routinely performing ABPM among African Americans, regardless of clinic blood pressure level, may be beneficial for CVD risk stratification and treatment intensification. Among African American participants with normal clinic blood pressure, the prevalence of masked hypertension was disproportionally higher among those taking versus those not taking antihypertensive medication (19.4% versus 6.8%). This is consistent with the prevalence of masked hypertension (15.4%) in the aforementioned Spanish cohort of patients with treated hypertension with clinic blood pressure <120/80 mm Hg.30 Individuals who are taking antihypertensive medication and have SBP/DBP <120/80 mm Hg would not likely have their antihypertensive medication titrated. Although our results suggest that the overlap between masked hypertension and prehypertension may be modified by antihypertensive medication use, there was no interaction between these factors on the prevalence of masked hypertension. It is possible, however, that this analysis was underpowered to detect a statistically significant interaction, as the sample sizes of participants with normal clinic blood pressure and masked hypertension in those taking and not taking antihypertensive medication were small (N=24 and 9, respectively).
Among JHS participants, CCIMT did not differ by masked hypertension status in a fully adjusted model. One explanation of these findings is that other hypertension‐related factors such as the chronicity of blood pressure elevation may affect CCIMT to a greater degree than masked hypertension status. CCIMT may be more dependent on the duration of blood pressure elevation rather than on the current level of clinic or ambulatory blood pressure. This needs to be investigated in future studies.
The results of this study should be interpreted in the context of some limitations. This was is a cross‐sectional study and temporal associations cannot be established. Clinic blood pressure was assessed during a single study visit and ABPM from a single 24‐hour monitoring period. Only a subsample of JHS participants had ABPM performed and some calculations were based on small sample sizes. ABPM is typically measured in the nondominant arm so as to interfere as little as possible with daily activity. The right arm was used for clinic BP measurement in the JHS.32 Therefore, participants may have had clinic blood pressure and ambulatory blood pressure measurement in different arms when a participant's right arm was dominant. In addition, the JHS did not conduct home blood pressure monitoring, another out‐of‐clinic approach for measuring blood pressure, which can be used to determine masked hypertension. Masked hypertension on both ABPM and home blood pressure monitoring has been associated with increased CVD risk.33 Therefore, the identification of masked hypertension using either ABPM or home blood pressure monitoring may be an important strategy to reduce racial disparities in CVD. Several strengths should also be noted. The sample was entirely African American, a demographic subgroup with few prior investigations of ABPM. Two measures of subclinical CVD—LVMI and CCIMT—were available in the JHS. Also, given the broad data collection in the JHS, we were able to control for multiple potential confounders.
In conclusion, the findings of this study suggest that a high percentage of African Americans not taking antihypertensive medication have masked hypertension. Although the prevalence of masked hypertension was substantially higher in African Americans with prehypertension versus those with normal clinic blood pressure, masked hypertension was common in both groups. Furthermore, the current study suggests that the association between masked hypertension and LVMI was independent of prehypertension status. The diagnosis of masked hypertension using ABPM may help identify African Americans with nonelevated clinic blood pressure at increased risk for CVD outcomes.
Sources of Funding
The manuscript for this study has been reviewed by the Jackson Heart Study for scientific content and consistency of data interpretation with previous JHS publications. The JHS is supported and conducted in collaboration with Jackson State University (N01‐HC‐95170); University of Mississippi Medical Center (N01‐HC‐95171); and Touglaoo College (N01‐HC‐95172) and contracts HHSN268201300046C, HHSN268201300047C, HHSN268201300048C, HHSN268201300049C, HHSN268201300050C from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute on Minority Health and Health Disparities (NIMHD) at the National Institute of Health (NIH). This work was also supported by grants R01‐HL117323 (Drs Muntner and Shimbo), K24‐HL125704 (Dr Shimbo), Diversity Supplements P01‐HL047540‐19S1 and R01‐HL116470‐02S1 (Dr Diaz) and R01‐HL117323‐02S2 (Dr Abdalla), all from NHLBI/NIH. Dr Redmond was supported by career development award K12‐HS023009 from the Agency for Healthcare Research and Quality (AHRQ). Dr Sims is supported by the grants P60MD002249 and U54MD008176 from the NIMHD.
Disclosures
None.
Supporting information
Table S1. Characteristics of Jackson Heart Study Participants Included and Not Included in the Analytic Cohort
Table S2. Prevalence of Prehypertension and Masked Hypertension Among Jackson Heart Study Participants With Nonelevated Clinic Blood Pressure (<140/90 mm Hg) Stratified by Antihypertensive Medication Use
(J Am Heart Assoc. 2016;5:e002284 doi: 10.1161/JAHA.115.002284)
Accompanying Tables S1 and S2 are available at http://jaha.ahajournals.org/content/5/3/e002284/suppl/DC1.
Preliminary results from this study were presented at the American Heart Association's Epidemiology and Prevention/Lifestyle and Cardiometabolic Health 2015 Scientific Sessions, March 3–6, 2015 in Baltimore, MD.
References
- 1. Pickering TG, Gerin W, Schwartz JE, Spruill TM, Davidson KW. Franz Volhard lecture: should doctors still measure blood pressure? The missing patients with masked hypertension. J Hypertens. 2008;26:2259–2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Peacock J, Diaz KM, Viera AJ, Schwartz JE, Shimbo D. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens. 2014;28:521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Angeli F, Reboldi G, Verdecchia P. Masked hypertension: evaluation, prognosis, and treatment. Am J Hypertens. 2010;23:941–948. [DOI] [PubMed] [Google Scholar]
- 4. Bobrie G, Clerson P, Menard J, Postel‐Vinay N, Chatellier G, Plouin PF. Masked hypertension: a systematic review. J Hypertens. 2008;26:1715–1725. [DOI] [PubMed] [Google Scholar]
- 5. Shimbo D, Newman JD, Schwartz JE. Masked hypertension and prehypertension: diagnostic overlap and interrelationships with left ventricular mass: the Masked Hypertension Study. Am J Hypertens. 2012;25:664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pogue V, Rahman M, Lipkowitz M, Toto R, Miller E, Faulkner M, Rostand S, Hiremath L, Sika M, Kendrick C, Hu B, Greene T, Appel L, Phillips RA; African American Study of Kidney Disease Hypertension Collaborative Research Group . Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension. 2009;53:20–27. [DOI] [PubMed] [Google Scholar]
- 7. Larsen TR, Gelaye A, Waanbah B, Assad H, Daloul Y, Williams F, Williams M, Steigerwalt S. Prevalence of masked hypertension in African Americans. J Clin Hypertens (Greenwich). 2014;16:801–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Veerabhadrappa P, Diaz KM, Feairheller DL, Sturgeon KM, Williamson S, Crabbe DL, Kashem A, Ahrensfield D, Brown MD. Enhanced blood pressure variability in a high cardiovascular risk group of African Americans: FIT4Life Study. J Am Soc Hypertens. 2010;4:187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Veerabhadrappa P, Diaz KM, Feairheller DL, Sturgeon KM, Williamson ST, Crabbe DL, Kashem AM, Brown MD. Endothelial‐dependent flow‐mediated dilation in African Americans with masked‐hypertension. Am J Hypertens. 2011;24:1102–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Selassie A, Wagner CS, Laken ML, Ferguson ML, Ferdinand KC, Egan BM. Progression is accelerated from prehypertension to hypertension in blacks. Hypertension. 2011;58:579–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, Safford MM, Cushman M, Glasser SP, Howard VJ. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med. 2013;173:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Taylor HA Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15:S6‐4‐17. [PubMed] [Google Scholar]
- 13. Jackson Heart Study Investigators . Jackson Heart Study Protocol Manuals of Operation‐Exam 1 2001. Available at: https://www.jacksonheartstudy.org/jhsinfo/ForResearchers/FormsManuals/Exam1Manuals/tabid/111/Default.aspx. Accessed May 7, 2015.
- 14. Dubbert PM, Carithers T, Ainsworth BE, Taylor HA Jr, Wilson G, Wyatt SB. Physical activity assessment methods in the Jackson Heart Study. Ethn Dis. 2005;15:S6‐56‐61. [PubMed] [Google Scholar]
- 15. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Carpenter MA, Crow R, Steffes M, Rock W, Heilbraun J, Evans G, Skelton T, Jensen R, Sarpong D. Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. Am J Med Sci. 2004;328:131–144. [DOI] [PubMed] [Google Scholar]
- 17. Wyatt SB, Akylbekova EL, Wofford MR, Coady SA, Walker ER, Andrew ME, Keahey WJ, Taylor HA, Jones DW. Prevalence, awareness, treatment, and control of hypertension in the Jackson Heart Study. Hypertension. 2008;51:650–656. [DOI] [PubMed] [Google Scholar]
- 18. Ogedegbe G, Spruill TM, Sarpong DF, Agyemang C, Chaplin W, Pastva A, Martins D, Ravenell J, Pickering TG. Correlates of isolated nocturnal hypertension and target organ damage in a population‐based cohort of African Americans: the Jackson Heart Study. Am J Hypertens. 2013;26:1011–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hickson DA, Diez Roux AV, Wyatt SB, Gebreab SY, Ogedegbe G, Sarpong DF, Taylor HA, Wofford MR. Socioeconomic position is positively associated with blood pressure dipping among African‐American adults: the Jackson Heart Study. Am J Hypertens. 2011;24:1015–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kikuya M, Hansen TW, Thijs L, Bjorklund‐Bodegard K, Kuznetsova T, Ohkubo T, Richart T, Torp‐Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA. Diagnostic thresholds for ambulatory blood pressure monitoring based on 10‐year cardiovascular risk. Circulation. 2007;115:2145–2152. [DOI] [PubMed] [Google Scholar]
- 21. O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y; European Society of Hypertension Working Group on Blood Pressure Monitoring . European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–1768. [DOI] [PubMed] [Google Scholar]
- 22. Pickering TG, White WB; American Society of Hypertension Writing G . When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2008;2:119–124. [DOI] [PubMed] [Google Scholar]
- 23. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ; Committee tNHBPEPC . Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 24. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ; American Society of Echocardiography's Guidelines and Standards Committee Chamber Quantification Writing Group and the European Association of Echocardiography . Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. [DOI] [PubMed] [Google Scholar]
- 25. Perneger TV. What's wrong with Bonferroni adjustments. BMJ. 1998;316:1236–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Thijs L, Hansen TW, Kikuya M, Bjorklund‐Bodegard K, Li Y, Dolan E, Tikhonoff V, Seidlerova J, Kuznetsova T, Stolarz K, Bianchi M, Richart T, Casiglia E, Malyutina S, Filipovsky J, Kawecka‐Jaszcz K, Nikitin Y, Ohkubo T, Sandoya E, Wang J, Torp‐Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA, O'Brien E. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit. 2007;12:255–262. [DOI] [PubMed] [Google Scholar]
- 27. Diaz KM, Veerabhadrappa P, Brown MD, Whited MC, Dubbert PM, Hickson DA. Prevalence, Determinants, and Clinical Significance of Masked Hypertension in a Population‐Based Sample of African Americans: The Jackson Heart Study. Am J Hypertens. 2015;28:900–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Franklin SS, Thijs L, Li Y, Hansen TW, Boggia J, Liu Y, Asayama K, Bjorklund‐Bodegard K, Ohkubo T, Jeppesen J, Torp‐Pedersen C, Dolan E, Kuznetsova T, Stolarz‐Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka‐Jaszcz K, Filipovsky J, Imai Y, Wang J, Ibsen H, O'Brien E, Staessen JA; International Database on Ambulatory blood pressure in Relation to Cardiovascular Outcomes Investigators . Masked hypertension in diabetes mellitus: treatment implications for clinical practice. Hypertension. 2013;61:964–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hanninen MR, Niiranen TJ, Puukka PJ, Mattila AK, Jula AM. Determinants of masked hypertension in the general population: the Finn‐Home study. J Hypertens. 2011;29:1880–1888. [DOI] [PubMed] [Google Scholar]
- 30. Banegas JR, Ruilope LM, de la Sierra A, de la Cruz JJ, Gorostidi M, Segura J, Martell N, Garcia‐Puig J, Deanfield J, Williams B. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J. 2014;35:3304–3312. [DOI] [PubMed] [Google Scholar]
- 31. Franklin SS, O'Brien E, Thijs L, Asayama K, Staessen JA. Masked hypertension: a phenomenon of measurement. Hypertension. 2015;65:16–20. [DOI] [PubMed] [Google Scholar]
- 32. Jackson Heart Study Protocol. Manual 4: Blood Pressure–Visit 1 2001. Available at: https://www.jacksonheartstudy.org/jhsinfo/Portals/0/pdf/manuals1/Blood_pressure_manual4_02-18-2001(1).pdf. Accessed July 28, 2015.
- 33. Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Studies comparing ambulatory blood pressure and home blood pressure on cardiovascular disease and mortality outcomes: a systematic review. J Am Soc Hypertens. 2015. pii: S1933‐1711(15)00840‐2. doi: 10.1016/j.jash.2015.12.013 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Characteristics of Jackson Heart Study Participants Included and Not Included in the Analytic Cohort
Table S2. Prevalence of Prehypertension and Masked Hypertension Among Jackson Heart Study Participants With Nonelevated Clinic Blood Pressure (<140/90 mm Hg) Stratified by Antihypertensive Medication Use


