Abstract
Objective
The present study sought to identify mediators underlying the effects of an education and a peer support intervention for women with breast cancer, and to determine if the efficacy of a peer support intervention is moderated by cancer severity.
Methods
Participants included 180 patients with early stage (I or II) and 65 patients with late stage (IV) breast cancer. The study was originally planned as a 2 (early stage, late stage) X 3 (education intervention, peer support intervention, control condition) design; however, the education condition for the late stage cancer group was dropped, due to slow recruitment. Participants completed measures of well-being prior to being randomized (Time 1), then again 2 weeks after the group meetings ended (Time 2), and 6 months later (Time 3).
Results
Among participants who had attended at least one group meeting, the education intervention predicted more life purpose, and marginally predicted more perceived physical health at Time 2. The peer support intervention predicted more life purpose and less depressive symptoms at Time 2. Cancer severity did not moderate these effects. The effect of the peer support intervention on depressive symptoms was mediated by life purpose. None of the intervention effects were evident at Time 3.
Conclusions
Peer support interventions have positive short-term effects on well-being, among women with late and early stage breast cancer, and these effects are partially mediated by changes in life purpose. Education interventions have positive short-term effects on well-being among women with early stage breast cancer.
Keywords: Education intervention, peer support intervention, randomized clinical trial, early stage breast cancer, late stage breast cancer, life purpose
Introduction
Individuals who experience breast cancer often suffer significant psychological distress.1,2,3 Psychosocial interventions have been developed to ameliorate this distress, and meta-analyses confirm that these interventions improve psychological adjustment.4,5,6,7,8 However, several different types of psychosocial interventions have been developed, and these interventions vary greatly in focus. Two of the most common interventions are education interventions, which focus on providing patients with information about their disease and coping strategies, and peer support interventions, which focus on providing patients with an opportunity to discuss their illness experience with similar others.
Researchers have proposed that interventions with such divergent emphases are likely to address different psychosocial needs, and may be beneficial for different categories of patients.9 Specifically, Scheier and Carver9 proposed that peer support and education interventions might differentially meet the psychosocial needs of patients with more versus less severe cancer. We sought to test this proposal in the present study.
Peer support interventions were originally developed to provide individuals with social support,10 but researchers have suggested that these interventions may also help patients maintain meaning and purpose in life. In this regard, Spiegel and collegues11 conducted a year-long peer support intervention with a sample of women with metastatic breast cancer. Although no formal analyses were conducted, the authors noted that the act of caring for other participants in the groups seemed to provide participants with continued reasons for living. Meaning is an important psychosocial need for many cancer patients. Indeed, psychotherapies specifically designed to enhance meaning in life have been found to promote well-being, among individuals with cancer.12,13 Although these meaning-based therapies are broad-based approaches, including aspects of functioning that go beyond life purpose (such as spirituality, for example), they do lend credence to the notion that purpose in life may be one mechanism by which interventions can promote well-being. In the present study, we sought to test formally if a peer support intervention promotes life purpose, and investigate whether purpose mediates the effects of this intervention on well-being.
Assuming that peer support interventions promote life purpose, they may be particularly suited to meet the needs of patients with more severe or late stage breast cancer. Women with late stage breast cancer face a markedly shortened life-expectancy—with a 5-year survival rate of less than 25%—and often suffer from more debilitating symptoms than patients with early stage disease.14 Scheier and Carver9 proposed that such severe illness is likely to render many important life goals unattainable. In such a situation, psychosocial needs likely revolve around finding alternative meaningful activities and maintaining purpose—needs that would be especially addressed by a peer support intervention. In the present study, we sought to test whether cancer stage moderates the effectiveness of a peer support intervention, such that patients with late stage cancer benefit most from participation in peer support groups.
If peer support interventions are best suited for the needs of patients with late stage cancer, this could explain the inconsistent findings concerning the benefits of these interventions. 5,10,15,16,17 Most breast cancer intervention research has focused exclusively on patients with early stage cancer, or collapsed data for patients across cancer stage.18,19,5 Thus, any benefits of these interventions specifically for patients with late stage cancer would not be readily apparent in the existing literature.
In contrast to peer support interventions, education interventions are designed to help patients develop coping skills and feel confident in their ability to understand and deal with their disease. Multiple studies confirm that education interventions, and similar interventions that emphasize coping skills, improve well-being by increasing peoples’ confidence in their coping abilities.20 In the present study, we sought to replicate these findings and demonstrate that patients’ confidence in their coping abilities mediates the effect of an education intervention on well-being.
Originally, we also sought to test whether an education intervention was more beneficial for women with early stage cancer than for women with late stage cancer. Scheier and Carver9 proposed that confidence in disease management might be more important for patients with early stage cancer, as these patients have a good prognosis and can expect to return to their normal activities after cancer treatment. However, during the recruitment phase of the study, the availability of late stage patients at local hospitals was lower than originally projected and by necessity, we needed to drop a condition for women with late stage disease. We chose to drop the education condition because the benefits of education interventions have been demonstrated much more consistently and robustly in the literature, as compared to the benefits of peer support interventions.5,6,7 Thus, it seemed more pressing to identify variables that moderate the effectiveness of peer support interventions.
Current Study
In the present study, we tested whether the effects of a peer support intervention were mediated by increased life purpose, and whether this intervention was more effective for women with late stage breast cancer than for women with early stage cancer. We also tested whether confidence mediates the benefits of an education intervention. To address these questions, we recruited a sample of patients with early (Stage I and II) and late stage (Stage IV) breast cancer. Patients with early stage cancer were randomly assigned to one of two 8-week facilitator-lead interventions (a peer support intervention or an education intervention) or to a usual-care control group. Patients with late stage cancer were randomized to either a facilitator-lead peer support group or a usual-care control group.
Methods
This study is registered at www.clinicaltrials.gov (NCT00416780). The study received IRB approval from Carnegie Mellon University, the University of Pittsburgh, and all hospitals from which participants were recruited.
Design
As noted in the introduction, this study was originally planned as a 2 (early stage cancer, late stage cancer) X 3 (education intervention, peer support intervention, control arm) design, but the education condition for patients with late stage cancer was dropped (with the consent of the Advisory Board overseeing the trial).
Participants
Eligible participants were English speaking women who were 25 years of age or older, living within a 60 mile radius of Pittsburgh, PA. Participants were eligible to enroll in the study if they had either: a first time diagnosis of stage I or II breast cancer, had received an initial diagnosis of stage IV cancer, or had a distant recurrence of breast cancer. Patients with early stage cancer must have been diagnosed within the past 6 months. There was no window for enrollment for patients with late stage cancer.
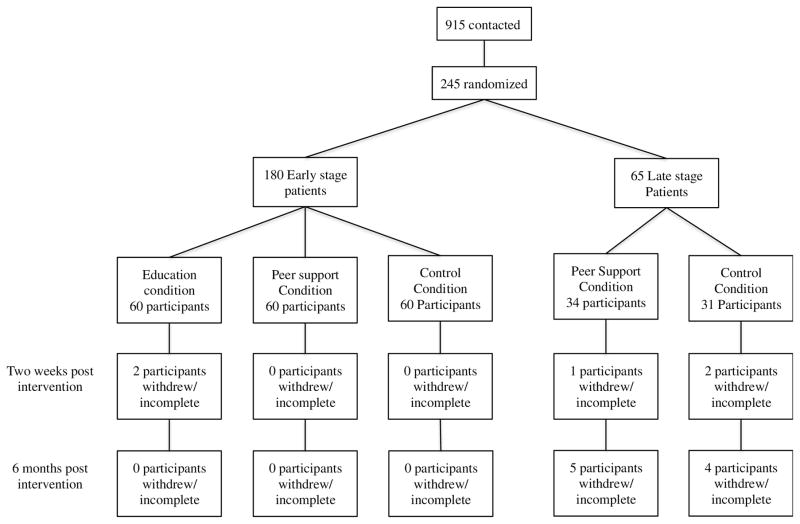
Participants were recruited from local oncologists’ offices. We contacted 915 eligible patients, of whom 245 provided informed consent and were randomized to an intervention group (see Figure 1 for the CONSORT flow chart). The most frequently reported reasons for refusal were unwillingness/inability to drive to group meeting site (37.2%) and being too busy (29.4%). No other information was collected from patients who refused to participate. Consented patients consisted of 180 women with early stage cancer (100 Stage I, 80 Stage II) and 65 women with late stage cancer (48 cancer recurrences, 17 initial Stage IV diagnoses). Demographic information characterizing consented participants can be found in Table 1.
Figure 1.
CONSORT flow chart for all consented participants
Table 1.
Sample Demographics
| Age, years | Range = 26–78 M = 51 |
|---|---|
| Familial income, $ | |
| <20,000 | 7% |
| 20–39,999 | 15% |
| 40–59,000 | 25% |
| 60–99,999 | 26% |
| >100,000 | 20% |
| refused | 6% |
| Education | |
| High school graduate or less | 21% |
| Some college | 32% |
| College graduate | 27% |
| Postgraduate training | 20% |
| Marital Status | |
| Married | 65% |
| Divorced | 14% |
| Single | 13% |
| Widowed | 5% |
| Separated | 4% |
| Race | |
| Caucasian | 89% |
| African-American | 9% |
| Other | 2% |
Group Assignment
For the two active arms of the study, participants met in small groups of same stage patients. Groups were assigned randomly to intervention condition, once 6–9 women with either early or late stage cancer were recruited to form a cohort.
Procedure
Participants completed an interview prior to being randomized (Time 1), 1 to 2 weeks after the group meetings ended (Time 2), and then again 6 months later (Time 3). Interviews took place face-to-face at a location of the participants’ choosing, usually their home, or participants completed a mailed questionnaire. Approximately 66% of the participants completed their interviews face-to-face. Participants who completed the mailed questionnaire did not significantly differ from patients who completed the face-to-face interview, in terms of demographics, breast cancer stage, or outcome variables at baseline. Participants were compensated $10 for each interview they completed.
Group meetings were held in 1 of 3 sites in the Pittsburgh area and consisted of 1-hour meetings for 8 consecutive weeks. Participants were compensated $5 for each meeting they attended. Meetings were overseen by two oncology social workers. Themes and topics for the interventions were modeled after previously used interventions.15,21 For more details on the interventions see Supplementary Materials. In order to ensure that facilitators adhered to the study protocol, all group sessions were audio taped. The primary investigators periodically reviewed these audiotapes. Facilitators were contacted if sessions strayed from the protocol and were provided with guidance to ensure adherence.
Education
The education group meetings focused on providing patients with information about their disease as well as methods to manage their illness and its side effects. Facilitators emphasized the theme of perceived control during all sessions, discussing how participants are in control of their illness experience and can have more control of their lives. A different topic was addressed in each session. Weekly homework assignments asked patients to write something new they had learned, regarding how to take control of their lives. Meeting topics were as follows: Overview of breast cancer, treatment types and side effects, nutrition and diet management, exercise, body image, communication issues, relationships, and sexuality.
Peer support
The peer support group meetings focused on fostering purpose in life by providing participants with opportunities to support and care for one another. As homework, patients completed a weekly diary of critical experiences or current life problems, and were then encouraged to share these experiences in the group meetings. The group facilitator encouraged participants to help one another with these issues, and share how they had dealt with similar problems.22
Usual-care (control)
Participants assigned to the control condition received usual care and did not attend any meetings.
Primary Outcome Measures
The primary outcomes were the mental health component score (MCS) and the physical health component score (PCS) from the SF-36 scale.23 The SF-36 has been used previously to evaluate the effectiveness of psychosocial interventions for persons with cancer.15,21 In the present study, individual SF-36 scales had high reliabilities (α = 0.81–0.89 at baseline). As an additional measure of well-being, we administered a 10-item abbreviated version24 of the Center for Epidemiological Studies Depression Scale25 (CES-D). In the present study, the abbreviated scale had high reliability (α = 0.87 at baseline) and the validity of the overall measure in people with cancer is well documented.26
Mediator Measures
Purpose
Purpose was measured with the Life Engagement Test27 (LET). The scale consists of 6 items (e.g., “To me, the things I do are worthwhile”), which participants rate on a 1–5 scale (1 = strong disagree, 5 = strong agree), α = 0.87 at baseline.
Confidence
Confidence was measured with a breast cancer-specific confidence scale developed in a previous study.21 The scale consists of 13 items, which participants rate on a 1–5 scale (1 = not at all confident, 5 = very confident). Each item asks participants to rate how confident they were in managing one aspect of their cancer experience (e.g., “How confident are you that you will be able to make appropriate medical decisions if needed in the future?”). Items focused on the 8 topics addressed during the education intervention. The scale had high reliability, α = 0.88 at baseline.
Statistical Analyses
Analyses were initially conducted with the intention-to-treat principle,28 but the interventions had no significant effects on the primary outcomes in these analyses. In this regard, average attendance was relatively low in the current sample, M = 3.52 meetings, SD = 3.01, due to the large portion of participants who did not attend any group meetings (31%). Among participants who attended at least one group meeting, average attendance was higher, M = 5.16, SD = 2.23. Due to low attendance we considered including the number of sessions attended as a covariate in the analyses, but the distribution of attendance was strongly bimodal, with most participants attending either a majority of sessions, or no sessions at all. For this reason, subsequent analyses presented below only retained women who had attended at least one group meeting (Time 1, N = 202; Time 2, N = 198; Time 3, N = 193). Of note, the number of participants who did not attend any meetings (and the number of meetings attended) did not significantly differ between conditions or breast cancer stage. However, patients who did not attend any meetings reported significantly more depressive symptoms, as well as lower education levels at baseline.
Given that the interventions were administered in small groups, initial analyses were conducted with HLM. However, none of the null HLM models for the primary outcomes indicated significant variance between meeting groups, so multiple regression was used to assess the effects of the interventions. Linear regression was used for all continuous outcomes. Because CES-D exhibited marked positive skew, CES-D scores were dichotomized 29(cutoff score of 8), and logistic regression was used. Two regression models were used to investigate our research questions.
Model 1: Education and peer support effects for patients with early stage cancer
Model 1 tested the main effects of the education and peer support condition among patients with early stage cancer. Patients with late stage cancer were excluded from this analysis. The model included 2 dummy coded variables, 1 contrasting the education and control condition, and the other contrasting the peer support and control condition. The baseline measure of the outcome variable was also included, in order to examine changes in the outcomes over time.
Model 2: Peer support condition effects and moderation by stage
Model 2 tested the main effects of the peer support condition among patients with early and late stage cancer, and tested whether cancer stage moderated the effects of the peer support intervention. Participants in the education condition were excluded from these analyses. The first step of the regression contained the baseline measure of the dependent variable. The second step contained two dummy coded variables, one contrasting the peer condition with the control condition, and one contrasting early and late stage breast cancer. The third step of the regression contained the interaction between the condition variable and the stage variable.
Mediation
To examine mediation of the intervention effects on the outcome variables, we tested the significance of the indirect effect, as outlined by Preacher & Hayes30, using the INDIRECT macro in SPSS. Unstandardized indirect effect estimates were calculated based on 10,000 bootstraps and significance was determined based on 95% bias-corrected confidence intervals (BCI 95%).
RESULTS
Baseline Differences
There were no significant differences between conditions or between patients with early or late stage cancer on baseline demographics (age, race, income, marital status, and education). Within same stage cancer patients, there were also no differences between conditions on medical variables (surgery, surgery type, adjunctive treatment, and adjunctive treatment type).
Results: Model 1
Time 2
Primary outcomes
The education condition had a marginal main effect on the SF-36 physical component, β = 0.15, F(3,139) = 3.16, p = 0.07. Individuals in the education condition tended to report better perceived physical health at Time 2 than control condition participants. The peer condition had a marginal main effect on CES-D scores, b = −0.68, Wald χ2(1) = 3.19, p = 0.07, such that participants in the peer support condition reported fewer depressive symptoms at Time 2 than control condition participants.
Mediators
Both the education and peer support condition had a significant effect on the LET scores, β = 0.23, F(3,139) = 15.80, p < 0.01, and β = 0.13, F(3,139) = 7.04, p = 0.01, respectively. Participants in both intervention conditions reported more life purpose at Time 2 than control condition participants. The magnitude of the effect on life purpose did not differ significantly between the intervention conditions. Neither intervention had a significant effect on confidence.
Mediation of primary outcomes
Since neither intervention condition had a significant effect on the primary outcomes (i.e. mental health, physical health, depressive symptoms), we did not test for mediation.
Time 3
There were no significant or marginal effects at Time 3.
Results: Model 2
Time 2
Primary outcomes
The peer support condition had a significant main effect on dichotomized CES-D scores, b = −1.02, Wald χ2(1) = 6.17, p = 0.01. Descriptively, at baseline, the control and peer support condition did not differ in the number of individuals who met the criteria (cut off of 8) for depressive symptoms (control group: 34%, peer support group, 32%), p = 0.76. At Time 2, fewer individuals in the peer support condition reported depressive symptoms (32%) than in the control condition (41%), p < 0.01. There were no significant interactions between the peer support condition and breast cancer stage on the primary outcomes.
Mediators
The peer support condition had a significant main effect on LET scores, β = 0.13, F(3, 149) = 6.05, p = 0.02. Participants in the peer support group reported greater purpose in life than participants in the control condition at Time 2. There were no significant interactions between the peer support condition and breast cancer stage on the mediator variables.
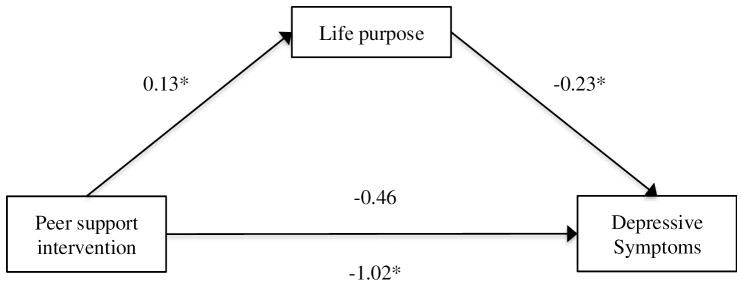
Mediation of primary outcomes
There was a significant indirect effect of the peer support condition on depressive symptomatology, via changes in life purpose, BCI 95% [−0.57, −0.33]. See Figure 2 for the full mediation model.
Figure 2.
The effect of the peer support intervention, as mediated by life purpose. All coefficients for continuous outcomes represent standardized beta weights, and all coefficients for dichotomous outcomes represent unstandardized beta weights.
Time 3
There were no significant main effects of the peer condition or interactions between the peer condition and breast cancer stage at Time 3.
Discussion
This is the first study to compare the efficacy of a peer support intervention in patients with both late and early stage breast cancer. Contrary to expectations,9 we found that the peer support intervention reduced depressive symptoms and increased life purpose 2-weeks after intervention completion in patients with early and late stage cancer. The education intervention also had a positive impact among patients with early stage cancer, increasing life purpose and marginally improving perceived physical health 2-weeks after intervention completion. However, it is important to bear in mind that the analyses reported are only applicable to participants who attended at least one group meeting. When the intention-to-treat principle was applied, the interventions had no effects on the outcome variables.
The finding that both interventions improved life purpose is noteworthy, as few studies have investigated the impact of psychosocial interventions on purpose. Recently, attention has been drawn to the importance of examining outcomes, such as a life purpose, which reflect eudaimonic aspects of subjective well-being31,32. Many prevalent measures of quality of life tend to emphasize hedonic aspects of well-being, such as affect and life satisfaction, while neglecting eudaimonic aspects33,34. Solely measuring hedonic well-being may obscure important effects as eudaimonic and hedonic well-being are distinct constructs, which independently contribute to quality of life and physical health.35–37 Thus, it is important to determine if these psychosocial interventions improve both hedonic and eudaimonic well-being.
In addition to being an important outcome in its own right, our results suggest that life purpose might explain the impact of peer support interventions on other outcomes. Previous researchers have noted that the act of caring for other participants in peer support groups seemed to provide patients with continued meaning in life, and they hypothesized that life purpose might mediate the positive effects of peer support interventions.11 The results of the present study support this idea. We found that the effect of the peer support intervention on depressive symptoms was mediated by changes in life purpose.
Unexpectedly, the education intervention also increased perceptions of life purpose. It may be that providing patients with coping skills, as part of the educational sessions, lead these patients to manage their illness more successfully and thus allowed them to spend more time on their regular activities. If so, it would not be surprising that these participants reported a higher sense of life purpose. This explanation is rendered somewhat more tenuous, however, since participants in the education condition did not report increased confidence in their ability to cope with their disease. Alternatively, it is worth considering whether some amount of peer support routinely occurs in the context of an education intervention. Although discussion between participants was not encouraged during the education sessions, it is likely that participants interacted before and after sessions, and some peer support may have occurred naturally in these contexts. In future research, it may be interesting to measure the extent of this informal peer support.
In the present study both the peer support and education interventions improved well-being, but these benefits dissipated shortly after the interventions ended and were not evident at a 6-month follow-up. This is not the first study to find that peer support or education intervention effects dissipate overtime,16,38 and several reviews of the psychosocial intervention literature have suggested that interventions may need to be longer in duration if they are to achieve stable long-term effects.4,6 Nevertheless, these short-lived effects may still be important, particularly if they occur during periods of marked distress, such as soon after the initial diagnosis of breast cancer.
Several limitations to the present study may also have contributed to the failure to find long-term effects. Our decision to exclude participants who did not attend meetings lowered our sample size and reduced statistical power to find both long and short-term effects. Selection effects may also have played a role. As previously mentioned, participants who attended meetings in the present study tended to be better off at baseline than those who did not attend. Previous research has suggested that education and peer support interventions are most beneficial for individuals who lack psychosocial resources39, thus our remaining sample consisted of individuals who were less likely to benefit from the interventions.
These limitations may also have contributed to the failure to find an interaction between cancer stage and the peer support intervention. Although the present results suggest that cancer stage may not matter, it still may be premature to reject the idea that peer interventions impact late stage women more. As with long-term treatment effects, lower statistical power might have reduced our ability to find significant interactions. It is also possible that the composition of our late stage sample contributed to the absence of an effect. That is, most of the patients in the current sample with late stage cancer had a distant recurrence of cancer. As such, most of our late stage patients had coped with cancer previously. In this regard, it is interesting to note that when only newly diagnosed women are included in the analyses, there was a trend (p < .09) toward an interaction between cancer stage and the peer support intervention on life purpose (late stage women were impacted more). Given the small sample size, such ad hoc analyses certainly need to be interpreted cautiously. Still, future research should be sensitive to the possibility that differential effects exist.
It is unclear why attendance was so low in the current study, but we speculate that the location of the group meetings could have played a role. Group meetings were held at three centrally located churches in Pittsburgh. Long travel times could have discouraged some participants from attending. Although placing meeting locations closer to participants’ homes might increase attendance, this option is not always feasible, particularly in rural areas. A more cost-effective option may be to utilize Internet-based interventions. Although Internet interventions are not without their own difficulties, 40 such interventions could be useful in reaching participants who find it too burdensome to attend meetings because they are too sick or too distressed.
In summary, we have demonstrated that both education and peer support interventions can have beneficial short-term effects on well-being for women with breast cancer. Moreover, peer support interventions appear to be equally beneficial for women with both early and late stage disease, although subsidiary analyses did suggest that peer interventions might be more effective for at least some categories of women with late stage disease. The fact that both interventions increased purpose in life is of particular note. Purpose in life is receiving increased attention as an overlooked component of subjective well-being. The significance of purpose in life is further enhanced by the finding that changes in life purpose mediated the positive impact of the peer support intervention on depressive symptoms.
Supplementary Material
Acknowledgments
This research was supported by grants from the National Institutes of Health (HL076852/076858)
Footnotes
Conflict of interest: The authors declare that there are no conflicts of interest.
References
- 1.Reich M, Lesur A, Perdrizet-Chevallier C. Depression, quality of life and breast cancer: a review of the literature. Breast Cancer Research and Treatment. 2008;110(1):9–17. doi: 10.1007/s10549-007-9706-5. [DOI] [PubMed] [Google Scholar]
- 2.Morasso G, Costantini M, Viterbori P, Bonci F, Del Mastro L, Musso M, … Venturini M. Predicting mood disorders in breast cancer patients. European Journal of Cancer. 2001;37(2):216–223. doi: 10.1016/s0959-8049(00)00390-7. [DOI] [PubMed] [Google Scholar]
- 3.Shapiro SL, Lopez AM, Schwartz GE, Bootzin R, Figueredo AJ, Braden CJ, Kurker SF. Quality of life and breast cancer: relationship to psychosocial variables. Journal of Clinical Psychology. 2001;57(4):501–519. doi: 10.1002/jclp.1026. [DOI] [PubMed] [Google Scholar]
- 4.Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. Journal of Clinical Oncology. 2013 doi: 10.1200/JCO.2011.40.8922. JCO-2011. [DOI] [PubMed] [Google Scholar]
- 5.Zimmermann T, Heinrichs N, Baucom DH. “Does one size fit all?” moderators in psychosocial interventions for breast cancer patients: A meta-analysis. Annals of Behavioral Medicine. 2007;34(3):225–239. doi: 10.1007/BF02874548. [DOI] [PubMed] [Google Scholar]
- 6.Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studies. Patient Education and Counseling. 2003;50(2):179–186. doi: 10.1016/s0738-3991(02)00149-0. [DOI] [PubMed] [Google Scholar]
- 7.Sheard T, Maguire P. The effect of psychological interventions on anxiety and depression in cancer patients: results of two meta-analyses. British Journal of Cancer. 1999;80(11):1770–1780. doi: 10.1038/sj.bjc.6690596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meyer TJ, Mark MM. Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments. Health Psychology. 1995;14(2):101–108. doi: 10.1037//0278-6133.14.2.101. [DOI] [PubMed] [Google Scholar]
- 9.Scheier MF, Carver CS. Adapting to cancer: The importance of hope and purpose. In: Baum A, Andersen BL, editors. Psychosocial interventions for cancer. Washington D.C: American Psychological Association; 2001. pp. 15–36. [Google Scholar]
- 10.Helgeson VS, Cohen S. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health Psychology. 1996;15(2):135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- 11.Spiegel D, Bloom JR, Yalom I. Group support for patients with metastatic cancer: A randomized prospective outcome study. Archives of General Psychiatry. 1981;38(5):527–533. doi: 10.1001/archpsyc.1980.01780300039004. [DOI] [PubMed] [Google Scholar]
- 12.Breitbart W, Poppito S, Rosenfeld B, Vickers AJ, Li Y, Abbey J, … Cassileth BR. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. Journal of Clinical Oncology. 2012;30(12):1304–1309. doi: 10.1200/JCO.2011.36.2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breitbart W. Spirituality and meaning in supportive care: spirituality-and meaning-centered group psychotherapy interventions in advanced cancer. Supportive care in cancer. 2002;10(4):272–280. doi: 10.1007/s005200100289. [DOI] [PubMed] [Google Scholar]
- 14.American Cancer Society. Cancer Facts and & Figures 2007. Atlanta: American Cancer Society; 2007. [Google Scholar]
- 15.Helgeson VS, Cohen S, Schulz R, Yasko J. Education and peer discussion group interventions and adjustment to breast cancer. Archives of General Psychiatry. 1999;56(4):340–347. doi: 10.1001/archpsyc.56.4.340. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham AJ, Tocco EK. A randomized trial of group psychoeducational therapy for cancer patients. Patient Education and Counseling. 1989;14(2):101–114. [Google Scholar]
- 17.Telch CF, Telch MJ. Group coping skills instruction and supportive group therapy for cancer patients: a comparison of strategies. Journal of Consulting and Clinical Psychology. 1986;54(6):802–808. doi: 10.1037//0022-006x.54.6.802. [DOI] [PubMed] [Google Scholar]
- 18.Linden W, Girgis A. Psychological treatment outcomes for cancer patients: what do meta-analyses tell us about distress reduction? Psycho-Oncology. 2012;21(4):343–350. doi: 10.1002/pon.2035. [DOI] [PubMed] [Google Scholar]
- 19.Jacobsen PB, Jim HS. Psychosocial interventions for anxiety and depression in adult cancer patients: achievements and challenges. CA: A Cancer Journal for Clinicians. 2008;58(4):214–230. doi: 10.3322/CA.2008.0003. [DOI] [PubMed] [Google Scholar]
- 20.Stanton AL, Luecken LJ, MacKinnon DP, Thompson EH. Mechanisms in psychosocial interventions for adults living with cancer: Opportunity for integration of theory, research, and practice. Journal of Consulting and Clinical Psychology. 2013;81(2):318–335. doi: 10.1037/a0028833. [DOI] [PubMed] [Google Scholar]
- 21.Scheier MF, Helgeson VS, Schulz R, Colvin S, Berga S, Bridges MW, … Pappert WS. Interventions to enhance physical and psychological functioning among younger women who are ending nonhormonal adjuvant treatment for early-stage breast cancer. Journal of Clinical Oncology. 2005;23(19):4298–4311. doi: 10.1200/JCO.2005.05.362. [DOI] [PubMed] [Google Scholar]
- 22.Nezu AM, Nezu CM, Perri MG. Problem-solving therapy for depression: Theory, research, and clinical guidelines. Oxford, England: John Wiley & Sons; 1989. [Google Scholar]
- 23.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 24.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 25.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 26.Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) Journal of Psychosomatic Research. 1999;46(5):437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- 27.Scheier MF, Wrosch C, Baum A, Cohen S, Martire LM, Matthews KA, … Zdaniuk B. The life engagement test: Assessing purpose in life. Journal of Behavioral Medicine. 2006;29(3):291–298. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- 28.Newell DJ. Intention-to-treat analysis: implications for quantitative and qualitative research. International Journal of Epidemiology. 1992;21(5):837–841. doi: 10.1093/ije/21.5.837. [DOI] [PubMed] [Google Scholar]
- 29.Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric Properties of the CES-D-10 in a Psychiatric Sample. Assessment. 2013;20(4):429–436. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- 30.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 31.Delle Fave A, Brdar I, Freire T, Vella-Brodrick D, Wissing MP. The eudaimonic and hedonic components of happiness: Qualitative and quantitative findings. Social Indicators Research. 2011;100(2):185–207. [Google Scholar]
- 32.Ryff CD, Singer BH. Know thyself and become what you are: A eudaimonic approach to psychological well-being. Journal of Happiness Studies. 2008;9(1):13–39. [Google Scholar]
- 33.Huta V, Waterman AS. Eudaimonia and Its Distinction from Hedonia: Developing a Classification and Terminology for Understanding Conceptual and Operational Definitions. Journal of Happiness Studies. 2013;15(6):1–32. [Google Scholar]
- 34.Fredrickson BL, Grewen KM, Coffey KA, Algoe SB, Firestine AM, Arevalo JM, … Cole SW. A functional genomic perspective on human well being. Proceedings of the National Academy of Sciences. 2013;110(33):13684–13689. doi: 10.1073/pnas.1305419110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huta V, Ryan RM. Pursuing pleasure or virtue: The differential and overlapping well-being benefits of hedonic and eudaimonic motives. Journal of Happiness Studies. 2010;11(6):735–762. [Google Scholar]
- 36.Steger MF, Kashdan TB, Oishi S. Being good by doing good: Daily eudaimonic activity and well-being. Journal of Research in Personality. 2008;42(1):22–42. [Google Scholar]
- 37.Matthews KA, Owens JF, Edmundowicz D, Lee L, Kuller LH. Positive and negative attributes and risk for coronary and aortic calcification in healthy women. Psychosomatic Medicine. 2006;68(3):355–361. doi: 10.1097/01.psy.0000221274.21709.d0. [DOI] [PubMed] [Google Scholar]
- 38.Berglund G, Bolund C, Gustafsson UL, Sjödén PO. One-year follow-up of the ‘Starting Again’group rehabilitation programme for cancer patients. European Journal of Cancer. 1994;30(12):1744–1751. doi: 10.1016/0959-8049(94)00330-8. [DOI] [PubMed] [Google Scholar]
- 39.Helgeson VS, Cohen S, Schulz R, Yasko J. Group support interventions for women with breast cancer: who benefits from what? Health psychology. 2000;19(2):107–114. doi: 10.1037//0278-6133.19.2.107. [DOI] [PubMed] [Google Scholar]
- 40.Gorlick A, Bantum EOC, Owen JE. Internet-based-interventions for cancer-related distress: exploring the experiences of those whose needs are not met. Psycho-Oncology. 2014;23(4):452–458. doi: 10.1002/pon.3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.