Abstract
OBJECTIVE
To conduct a randomized, controlled trial to evaluate the efficacy of the Early Start Denver Model (ESDM), a comprehensive developmental behavioral intervention, for improving outcomes of toddlers diagnosed with autism spectrum disorder (ASD).
METHODS
Forty-eight children diagnosed with ASD between 18 and 30 months of age were randomly assigned to 1 of 2 groups: (1) ESDM intervention, which is based on developmental and applied behavioral analytic principles and delivered by trained therapists and parents for 2 years; or (2) referral to community providers for intervention commonly available in the community.
RESULTS
Compared with children who received community-intervention, children who received ESDM showed significant improvements in IQ, adaptive behavior, and autism diagnosis. Two years after entering intervention, the ESDM group on average improved 17.6 standard score points (1 SD:15 points) compared with 7.0 points in the comparison group relative to baseline scores. The ESDM group maintained its rate of grow thin adaptive behavior compared with a normative sample of typically developing children. In contrast, over the 2-year span, the comparison group showed greater delays in adaptive behavior. Children who received ESDM also were more likely to experience a change in diagnosis from autism to pervasive developmental disorder, not otherwise specified, than the comparison group.
CONCLUSIONS
This is the first randomized, controlled trial to demonstrate the efficacy of a comprehensive developmental behavioral intervention for toddlers with ASD for improving cognitive and adaptive behavior and reducing severity of ASD diagnosis. Results of this study underscore the importance of early detection of and intervention in autism.
Keywords: autism, behavioral intervention, cognitive function, developmental outcomes, early intervention
Autism spectrum disorder (ASD) is characterized by impairments in social reciprocity and communication, and stereotyped and repetitive behaviors, with onset during early childhood. Intellectual disability is present in a large proportion of individuals.1 With a prevalence of 1 per 150,2 autism costs the United States $35 billion per year.3 The lifetime per-capita societal cost of autism is $3.2 million, with lost productivity and adult care among the largest costs.4 Thus, early-intervention methods that can improve outcome for individuals with ASD are of high importance.
The 1987 report by Lovaas5 of an early behavioral intervention that resulted in 49% of children in the study being mainstreamed into regular classrooms and showing significant IQ gains created a groundswell of interest among parents and professionals in early intervention and raised questions about early plasticity in children with autism.6 Although subsequent intervention studies, including a randomized, controlled trial,7 have documented improvements in IQ for a subgroup of children, questions regarding the efficacy of early intervention have remained. Many of the studies lacked methodologic rigor. Authors of a recent meta-analysis of the efficacy of early behavioral intervention argued that stronger evidence that early behavioral intervention results in better outcomes than standard care is still needed.8
Our study was a randomized, controlled trial of early intensive behavioral intervention for young children with ASD that was funded by the National Institute of Mental Health (Dr Dawson, principal investigator). It was hypothesized that the early intervention would result in significant improvements in cognitive abilities of young children with ASD. The study differed from previous ones in several ways. First, we maintained a high level of methodologic rigor, including gold-standard diagnostic criteria, randomization, comprehensive outcome measures conducted by naive examiners, high retention rates, and measures of fidelity of implementation of a manualized intervention.
Second, to our knowledge, our study is the first randomized, controlled trial of intervention for toddlers with autism; all children were younger than 30 months at entry. Given the recent recommendation by the American Academy of Pediatrics that 18-month-old children be screened for ASD,9 it is imperative that the efficacy of early-intervention models appropriate for toddlers with ASD be demonstrated.
Third, the intervention, the Early Start Denver Model (ESDM),10 is a comprehensive early behavioral intervention for infants to preschool-aged children with ASD that integrates applied behavior analysis (ABA) with developmental and relationship-based approaches. The ESDM was designed to address the needs of toddlers with ASD as young as 12 months. The intervention is provided in a toddler’s natural environment (the home) and is delivered by trained therapists and parents. In our study, children received structured intervention at high intensity, consistent with the National Research Council’s recommendation.11
PATIENTS AND METHODS
Study Procedures
Forty-eight children between 18 and 30 months of age diagnosed with autistic disorder or pervasive developmental disorder (PDD), not otherwise specified (NOS), were randomly assigned to 1 of 2 groups: (1) the ESDM group received yearly assessments, 20 hours/ week of the ESDM intervention from University of Washington clinicians, parent training, and parent delivery for 5 or more hours/week of ESDM, in addition to whatever community services the parents chose; and (2) the assess-and-monitor (A/M) group received yearly assessments with intervention recommendations and referrals for intervention from commonly available community providers in the greater Seattle region.
Children were evaluated by experienced examiners naive to intervention status at baseline (preintervention), 1 year after onset of the intervention, and at either 2 years after onset of the intervention or at 48 months of age, whichever yielded a longer time frame.
Participants
Participants were recruited through pediatric practices, Birth to Three centers, preschools, hospitals, and state and local autism organizations. Exclusion criteria included (1) a neurodevelopmental disorder of known etiology (eg, fragile X syndrome), (2) significant sensory or motor impairment, (3) major physical problems such as a chronic serious health condition, (4) seizures at time of entry, (5) use of psychoactive medications, (6) history of a serious head injury and/or neurologic disease, (7) alcohol or drug exposure during the prenatal period, and (8) ratio IQ below 35 as measured by mean age equivalence score/chronological age on the visual reception and fine motor subscales of the Mullen Scales of Early Learning (MSEL).12 Children who developed seizures during the course of the study were not excluded. Inclusion criteria included age below 30 months at entry, meeting criteria for autistic disorder on the Toddler Autism Diagnostic Interview,13 meeting criteria for autism or ASD on the Autism Diagnostic Observation Schedule,14 and a clinical diagnosis based on Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria15 using all available information, residing within 30 minutes of the University of Washington, and willingness to participate in a ≥2-year intervention. At baseline, 18 children in the A/M group and 21 in the ESDM group received a DSM-IV diagnosis of autistic disorder. Six children in the A/M group and 3 in the ESDM group received a diagnosis of PDD NOS. This difference was not significant (Fisher’s exact test, P = .231). The ethnicities involved were Asian (12.5%), white (72.9%), Latino (12.5%), and multiracial (14.6%). The male-to-female ratio reflected the expected ratio in ASD of 3.5:1.
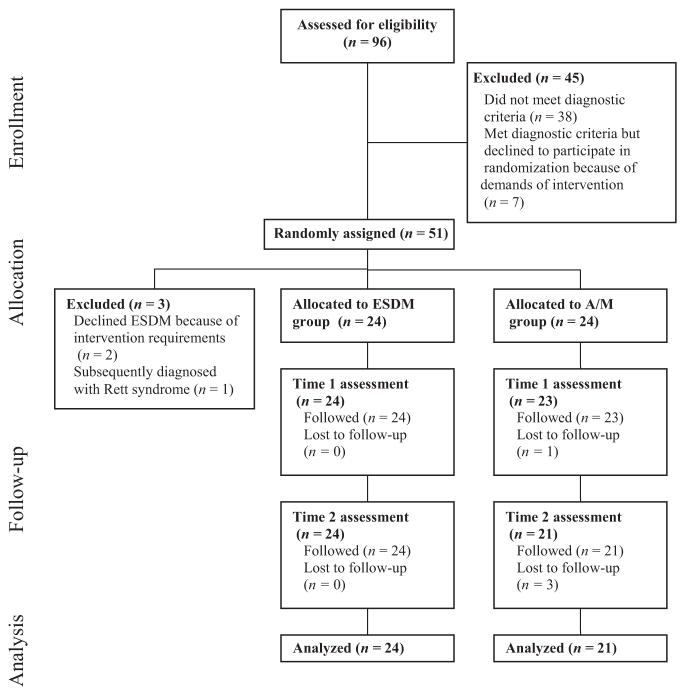
Retention rates were 100% (1-year) and 100% (2-year) for the ESDM group and 96% (1-year) and 88% (2-year) for the A/M group, which yielded a sample size of 24 in the ESDM and 21 in the A/M group at outcome. Figure 1 shows the participant flowchart.
FIGURE 1.
Participant flowchart.
Measures
Autism Diagnostic Interview–Revised
The toddler version of the Autism Diagnostic Interview–Revised13 is a semi-structured parent interview that assesses autism symptoms across 3 domains: social relatedness; communication; and repetitive, restricted behaviors.
Autism Diagnostic Observation Schedule
The Autism Diagnostic Observation Schedule (ADOS), WPS version,14 is a semistructured standardized observation that measures autism symptoms in social relatedness, communication, play, and repetitive behaviors. A standardized severity score based on codes within these domains can be calculated to compare autism symptoms across modules.16
Mullen Scales of Early Learning (MSEL)
The MSEL12 are a standardized developmental test for children from birth to 68 months of age. Four of the 5 subscales were administered: fine motor, visual reception, expressive language, and receptive language. T scores for subscales have a mean of 50 (SD: 10). The early-learning composite score is a standard score with mean of 100 (SD: 15).
Vineland Adaptive Behavior Scales
The Vineland Adaptive Behavior Scales (VABS)17 are a parent interview that assesses social, communication, motor, and daily living skills. They provide age-equivalent and standard scores for several subscales, including expressive and receptive language and social adaptive functioning.
Repetitive Behavior Scale
The Repetitive Behavior Scale (RBS)18 is a parent questionnaire that characterizes the severity of repetitive behaviors, yielding 6 subdomain scores (eg, sameness, self-injurious behavior) and a total score.
Randomization
Participants were stratified into 2 groups on the basis of composite IQ at entry (<55 and 55) and gender to ensure comparable IQ and gender ratios between groups. Within each of these strata, randomization was conducted by using random permuted blocks of 4. The intervention groups did not differ at baseline in severity of autism symptoms based on ADOS scores, chronological age, IQ, gender, or adaptive behaviors (see Table 1).
TABLE 1.
Baseline Measures for ESDM and A/M Groups
| A/M Group
|
ESDM Group
|
F | MS | P | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | N | Mean | SD | N | ||||
| Age at study entry, mo | 23.1 | 3.9 | 24 | 23.9 | 4.0 | 24 | 0.48 | 7.52 | .490 |
| MSEL | |||||||||
| Early-learning compositea | 59.4 | 8.6 | 24 | 61.0 | 9.2 | 24 | 0.40 | 31.69 | .530 |
| Receptive languageb | 21.2 | 3.8 | 24 | 21.1 | 4.7 | 24 | 0.01 | 0.19 | .920 |
| Expressive languageb | 26.0 | 8.6 | 24 | 24.5 | 7.2 | 24 | 0.48 | 30.08 | .492 |
| Visual receptionb | 30.8 | 8.9 | 24 | 33.2 | 11.0 | 24 | 0.70 | 70.08 | .406 |
| Fine motorb | 30.6 | 10.7 | 24 | 33.9 | 11.9 | 24 | 1.02 | 130.02 | .318 |
| VABS | |||||||||
| Adaptive behavior compositea | 69.9 | 7.3 | 24 | 69.5 | 5.7 | 24 | 0.04 | 1.69 | .844 |
| Communicationa | 69.6 | 7.3 | 24 | 68.4 | 7.6 | 24 | 0.32 | 17.52 | .577 |
| Socializationa | 72.4 | 9.4 | 24 | 73.8 | 7.7 | 24 | 0.29 | 21.33 | .594 |
| Daily living skillsa | 86.8 | 10.0 | 24 | 87.3 | 11.4 | 24 | 0.03 | 3.52 | .381 |
| Motor skillsa | 72.5 | 6.5 | 24 | 70.9 | 6.2 | 24 | 0.78 | 31.69 | .862 |
| ADOS severity score | 6.9 | 1.7 | 24 | 7.2 | 1.7 | 24 | 0.35 | 1.02 | .557 |
| RBS total | 21.5 | 19.2 | 24 | 15.2 | 10.8 | 24 | 1.93 | 468.75 | .171 |
No significant differences among baseline measures were found (P > .10 on all measures).
Standard score (mean: 100 [SD: 15]).
T score (mean: 50 [SD: 10]).
Intervention Groups
ESDM Group
The ESDM group was provided with intervention by trained therapists for 2-hour sessions, twice per day, 5 days/ week, for 2 years. A detailed intervention manual and curriculum were used.19 One or both parents were provided with parent training from the primary therapist during semimonthly meetings, during which the principles and specific techniques of ESDM were taught. Parents were asked to use ESDM strategies during daily activities and to keep track of the number of hours during which they used these strategies. ESDM uses teaching strategies that involve interpersonal exchange and positive affect, shared engagement with real-life materials and activities, adult responsivity and sensitivity to child cues, and focus on verbal and nonverbal communication, based on a developmentally informed curriculum that addresses all developmental domains. Teaching strategies are consistent with the principles of ABA, such as the use of operant conditioning, shaping, and chaining. Each child’s plan is individualized. There is a strong parent-family role responsive to each family’s unique characteristics. Parents are taught the basic ESDM strategies and asked to use them during everyday activities such as feeding, bath time, and play. Parents chose teaching objectives from the curriculum that they viewed as high priority.
Intervention programs were supervised by a graduate-level, trained lead therapist who had a minimum of 5 years’ experience providing early intervention to young children with autism, with ongoing consultation from a clinical psychologist, speech-language pathologist, and developmental behavioral pediatrician. An occupational therapist provided consultation as needed. Intervention objectives and strategies were reviewed, and the intervention was observed at least biweekly by the lead therapist and every 3 months by the speech-language pathologist. Intervention was delivered by therapists who typically held a baccalaureate degree, received 2 months of training by the lead therapist, and met weekly with the lead therapist. Therapists were trained to competence, defined as completing course-work, passing tests, mastering the intervention, demonstrating fidelity of 85% of maximum scores on the fidelity instrument, and maintaining ongoing fidelity.20
ESDM intervention hours were systematically recorded. Although 20 therapist-delivered intervention hours per week were made available, the actual mean was 15.2 hours (SD: 1.4) because of illnesses, vacations, and so on. Parents reported spending an average of 16.3 hours/week (SD: 6.2) using ESDM strategies. The ESDM group reported an average of 5.2 hours/week (SD: 2.1) in other therapies (eg, speech therapy, developmental preschool) over the study enrollment period. Other therapies were documented by using an intervention history interview administered every 6 months.
A/M Group
Children who were randomly assigned to the A/M group received comprehensive diagnostic evaluations, intervention recommendations, and community referrals at baseline and again at each of the 2 follow-up assessments. Families were given resource manuals and reading materials at baseline and twice yearly throughout the study. The A/M group reported an average of 9.1 hours of individual therapy and an average of 9.3 hours/week of group interventions (eg, developmental pre-school) across the 2-year period during which the intervention study was conducted. In the greater Seattle area, there are a number of Birth to Three centers that provide interventions, speech and language therapy, and occupational therapy. Developmental preschool programs vary but typically include special education and related services. There are a number of private ABA providers in the community.
Data Analysis
The effect of ESDM intervention was assessed by using repeated-measures analysis of variance, with a priori contrasts that compared baseline scores with 1- and 2-year outcome scores. The primary outcome measures were the MSEL composite standard score and the VABS composite standard score. Secondary outcome measures were the ADOS severity score,16 the RBS,18 MSEL, and VABS subscale scores, and changes in diagnostic status (autistic disorder, PDD NOS, and no diagnosis).
RESULTS
No serious adverse effects related to the intervention were reported during the 2-year period.
1-Year Outcome
Table 2 displays statistics for 1- and 2-year outcomes, change scores relative to baseline, and group comparisons for primary and secondary measures. Significant intervention effects were found for cognitive ability after 1 year on the MSEL composite standard scores. The ESDM group demonstrated an average IQ increase of 15.4 points (>1 SD) compared with an increase of 4.4 points in the A/M group. The visual reception subscale was the only individual subscale on the MSEL on which the groups significantly differed at the 1-year outcome. The ESDM group gained 5.6 T-score points, whereas the A/M group declined 1.7 points. The ESDM group improved 17.8 points on receptive language compared with a 9.8-point improvement in the A/M group, a difference that fell just short of statistical significance.
TABLE 2.
Child Outcomes After 1 and 2 Years of Study Participation
| 1-y Outcome
|
2-y Outcome
|
Group × Time (Baseline vs 1-y)
|
Group × Time (Baseline vs 2-y)
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A/M (N =23)
|
ESDM (N =24)
|
A/M (N =21)
|
ESDM (N =24)
|
|||||||||||||||
| Mean | SD | Δ | Mean | SD | Δ | Mean | SD | Δ | Mean | SD | Δ | F | MS | P | F | MS | P | |
| Chronological age, mo | 38.1 | 3.8 | 15.3 | 38.8 | 4.4 | 14.9 | 52.1 | 4.3 | 29.3 | 52.4 | 3.4 | 28.5 | 0.95 | 2.18 | .334 | 1.27 | 6.91 | .266 |
| MSEL | ||||||||||||||||||
| Early-learning composite | 64.0 | 13.8 | 4.4 | 76.4 | 23.4 | 15.4 | 66.3 | 15.3 | 7.0 | 78.6 | 24.2 | 17.6 | 5.99 | 1416.90 | .018 | 4.31 | 1264.38 | .044 |
| Receptive language | 31.1 | 11.1 | 9.8 | 38.9 | 15.4 | 17.8 | 31.5 | 10.6 | 10.2 | 40.0 | 16.3 | 18.9 | 4.00 | 745.21 | .051 | 4.14 | 843.56 | .048 |
| Expressive language | 33.0 | 11.5 | 6.7 | 36.1 | 14.2 | 11.6 | 30.0 | 9.2 | 4.0 | 36.6 | 13.6 | 12.1 | 1.99 | 290.43 | .165 | 4.88 | 748.07 | .033 |
| Visual reception | 29.0 | 10.7 | −1.7 | 38.8 | 16.4 | 5.6 | 34.5 | 13.0 | 4.5 | 41.0 | 17.9 | 7.8 | 4.22 | 621.97 | .046 | 0.63 | 126.23 | .433 |
| Fine motor | 26.1 | 8.6 | −5.0 | 32.7 | 11.7 | −1.3 | 28.5 | 9.5 | −2.8 | 33.5 | 12.2 | −0.4 | 1.32 | 161.35 | .256 | 0.46 | 63.81 | .503 |
| VABS | 63.7 | 8.8 | −6.3 | 65.7 | 9.8 | −3.8 | 59.1 | 8.8 | −11.2 | 68.7 | 15.9 | −0.8 | 0.85 | 71.61 | .360 | 7.05 | 1181.82 | .011 |
| Communication | 71.0 | 13.0 | 1.2 | 73.5 | 11.7 | 5.0 | 69.4 | 15.8 | −0.7 | 82.1 | 21.8 | 13.7 | 1.38 | 175.69 | .246 | 6.38 | 2300.98 | .015 |
| Socialization | 68.9 | 12.1 | −3.5 | 70.0 | 9.9 | −3.8 | 63.1 | 9.3 | −8.9 | 69.2 | 11.6 | −4.6 | 0.01 | 1.15 | .934 | 1.29 | 204.57 | .263 |
| Daily living skills | 65.3 | 7.1 | −7.4 | 65.6 | 8.6 | −5.3 | 58.0 | 8.1 | −14.5 | 64.7 | 12.4 | −6.2 | 0.89 | 51.78 | .350 | 6.73 | 773.34 | .013 |
| Motor skills | 70.7 | 12.2 | −15.9 | 75.1 | 14.4 | −12.2 | 64.1 | 12.3 | −23.1 | 77.4 | 19.8 | −9.9 | 0.99 | 157.43 | .326 | 7.40 | 1881.65 | .009 |
| ADOS severity score | 7.3 | 2.1 | 0.4 | 6.5 | 1.5 | −0.7 | 7.3 | 1.8 | 0.3 | 7.0 | 1.9 | −0.2 | 3.38 | 13.15 | .072 | 0.66 | 3.29 | .422 |
| RBS total | 23.3 | 17.5 | 1.0 | 15.5 | 12.3 | 0.9 | 22.0 | 16.3 | −0.6 | 16.7 | 13.1 | 2.5 | 0.001 | 0.19 | .976 | 0.37 | 92.50 | .545 |
Δ indicates mean change from baseline.
As a whole, children gained raw score points in the daily living skills subscale of the VABS; however, progress was much slower in relation to the VABS normative sample between baseline and 1 year. The groups did not differ in terms of adaptive behavior, measured by the VABS composite standard score, after 1 year (the ESDM group showed a 3.8-point decline, and the A/M group showed a 6.3-point decline). The groups did not differ in terms of their ADOS severity scores or RBS total score after 1 year of intervention.
2-Year Outcome
Two years after the baseline assessment, the ESDM group showed significantly improved cognitive ability, measured by MSEL composite standard scores, which increased 17.6 points compared with 7.0 points in the A/M group. The bulk of this change seems to have been a result of receptive and expressive language, which showed increases of 18.9 and 12.1 points, respectively, for the ESDM group, whereas the A/M group improved 10.2 and 4.0 points, respectively.
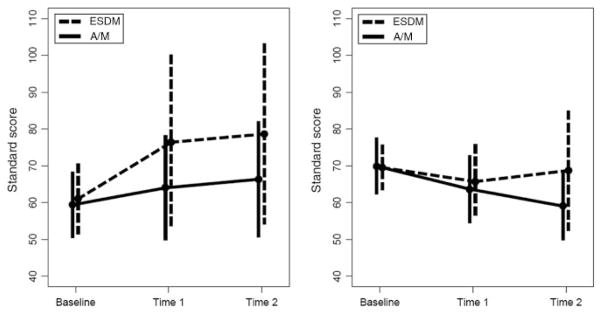
The ESDM and A/M groups significantly differed in terms of their adaptive behavior as measured by the VABS composite standard scores at the 2-year outcome (see Fig 2). The ESDM group showed similar standard scores at the 1- and 2-year outcomes, indicating a steady rate of development, whereas the A/M group, on average, showed an 11.2-point average decline. Thus, the A/M group’s delays in overall adaptive behavior became greater when compared with the normative sample. The A/M group showed average declines in standard scores that were twice as great as those in the ESDM group in the domains of socialization, daily living skills, and motor skills. The groups did not differ in terms of their ADOS severity scores or RBS total score after 2 years of intervention.
FIGURE 2.
Mean scores on the MSEL (left) and the VABS composite (right) for children in the ESDM and A/M groups 1 and 2 years after entering study. Error bars indicate ±1 SD.
Diagnosis
At baseline, the diagnoses in each group were not significantly different (Fisher’s exact test, P =.461) and were distributed as follows: ESDM, 21 with autistic disorder and 3 with PDD NOS; A/M, 18 with autistic disorder and 6 with PDD NOS. At the 2-year outcome, 15 (62.5%) children in the ESDM group had the same diagnosis (14 with autistic disorder, 1 with PDD NOS) and 15 (71.4%) children in the A/M group had the same diagnosis (all 15 with autistic disorder). Diagnosis improved (baseline autistic disorder to PDD NOS at year 2) for 7 (29.2%) children in the ESDM group but for only 1 (4.8%) child in the A/M group. However, the diagnosis changed from PDD NOS at baseline to autistic disorder at year 2 for 2 (8.3%) children in the ESDM group and 5 (23.8%) children in the A/M group. Thus, children who received ESDM were significantly more likely to have improved diagnostic status at the 2-year outcome compared with children in the A/M group, as assessed by using Fisher’s exact test 2 (intervention groups) × 2 (improved versus worsened diagnosis) contingency table (P = .041). Fisher’s exact test for the 2 (intervention groups) × 3 (diagnostic change: no change versus improved versus worsened diagnosis) contingency table was just short of significance (P = .060).
DISCUSSION
Recommendations by the American Academy of Pediatrics9 that all children be screened for autism at 18 months of age oblige the development of interventions that are appropriate for toddlers with ASD. To our knowledge, this study is the first to demonstrate the efficacy of an intensive intervention designed for toddlers with ASD as young as 12 months of age. After 2 years of intervention, children provided with the ESDM19 showed significant improvements in IQ, adaptive behavior, and diagnostic status compared with children who received community interventions. Consistent evidence of improvement in communicative abilities in the ESDM group was found, as demonstrated by gains in receptive and expressive language scores on the MSEL subscales and the VABS communication subscale. Significant improvement for the ESDM group was found for overall adaptive behavior, communication, daily living skills, and motor skills. Specifically, the ESDM group, although still significantly delayed in adaptive behavior, was able to keep pace with the rate of change of the VABS normative sample, whereas the community-based intervention group continued to fall farther behind in adaptive behavior. Given the importance of adaptive behavior for everyday functioning at home and school, the fact that the ESDM group did not continue to fall farther behind is likely to affect ability to function in less-restrictive environments. This demonstrates that the ESDM intervention accelerates overall development and is generalizing to everyday life. Whereas 71% of the children in the group that received community-based intervention retained their diagnosis of autistic disorder over the 2-year period, only 56% of children in the ESDM group did so. The diagnosis of 7 children (30%) in the ESDM group changed from autistic disorder to PDD NOS, whereas this only occurred for 1 child (5%) in the community-intervention group. These diagnostic assessments were conducted by experienced clinicians who were naive with respect to intervention-group status. However, this change in diagnostic severity was not reflected in significant differences in the ADOS severity scores. This lack of correspondence between measures is difficult to interpret, because the child’s performance in the ADOS contributes to clinical diagnosis. However, other behaviors, including parental report, also contribute to overall clinical diagnosis. The repetitive-behavior scores also did not change over time in either group.
CONCLUSIONS
The outcomes of this study, which involve an increase in IQ scores of 17 points (>1 SD) and significant gains in language and adaptive behavior, compare favorably with other controlled studies of intensive early intervention (eg, Smith et al [2000],7 which delivered discrete trial intervention for >2 years for 25–40 hours/week). The group differences reported from our study are larger than those produced by other comparative trials of developmental behavioral approaches, which were conducted for briefer periods of time and with fewer hours of delivery per week.21,22 Whether the children will sustain their gains over a longer term is an important question that will require follow-up study.
The results of this study suggest that the ESDM model,19 an intervention approach that uses teaching strategies of ABA that are delivered within an affectively rich, relationship-focused context, can be effective for improving outcomes of young children with autism. Parents’ use of these strategies at home during their daily activities likely was an important ingredient of its success.
WHAT’S KNOWN ON THIS SUBJECT
Previous studies on the efficacy of early behavioral intervention for improving outcomes for preschool-aged children with autism have yielded promising results. However, no randomized clinical trials of early developmental behavioral intervention designed for toddlers with autism have been conducted to date.
WHAT THIS STUDY ADDS
This study assessed the efficacy of the Early Start Denver Model, a comprehensive developmental behavioral intervention, for improving outcomes of toddlers with ASD. The intervention, which was initiated when children were less than 2½ years, resulted in significant improvements in IQ, language, adaptive behavior, and autism diagnosis.
Acknowledgments
This study was supported by National Institute of Mental Health grant U54MH066399 (to Dr Dawson).
We acknowledge the contributions of the parents and children who took part in this study and the support and effort of numerous undergraduate and graduate students and staff who are part of the University of Washington Autism Center.
ABBREVIATIONS
- ASD
autism spectrum disorder
- ESDM
Early Start Denver Model
- ABA
applied behavior analysis
- A/M
assess and monitor
- PDD
pervasive developmental disorder
- NOS
not otherwise specified
- MSEL
Mullen Scales of Early Learning
- ADOS
Autism Diagnostic Observation Schedule
- VABS
Vineland Adaptive Behavior Scales
- RBS
Repetitive Behavior Scale
Footnotes
This trial has been registered at www.clinicaltrials.gov (identifier NCT00090415).
FINANCIAL DISCLOSURE: Sally Rogers and Geraldine Dawson are authors of Early Start Denver Model for Young Children with Autism from which they receive royalties.
References
- 1.Baird G, Simonoff E, Pickles A, et al. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP) Lancet. 2006;368(9531):210–215. doi: 10.1016/S0140-6736(06)69041-7. [DOI] [PubMed] [Google Scholar]
- 2.Yeargin-Allsopp M, Rice C, Karapurkar T, Doemberg N, Coyle C, Murphy C. Prevalence of autism in a U.S. metropolitan area. JAMA. 2003;289(1):49–55. doi: 10.1001/jama.289.1.49. [DOI] [PubMed] [Google Scholar]
- 3.Ganz ML. The costs of autism. In: Molden SO, Rubenstein JLR, editors. Understanding Autism: From Basic Neuroscience to Treatment. Boca Raton, FL: Taylor and Francis Group; 2006. [Google Scholar]
- 4.Ganz ML. The lifetime distribution of the incremental societal costs of autism. Arch Pediatr Adolesc Med. 2007;161(4):343–349. doi: 10.1001/archpedi.161.4.343. [DOI] [PubMed] [Google Scholar]
- 5.Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol. 1987;55(1):3–9. doi: 10.1037//0022-006x.55.1.3. [DOI] [PubMed] [Google Scholar]
- 6.Dawson G. Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Dev Psychopathol. 2008;20(3):775–803. doi: 10.1017/S0954579408000370. [DOI] [PubMed] [Google Scholar]
- 7.Smith T, Groen AD, Wynn JW. Randomized trial of intensive early intervention for children with pervasive developmental disorder. Am J Ment Retard. 2000;105(4):269–285. doi: 10.1352/0895-8017(2000)105<0269:RTOIEI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Spreckley M, Boyd R. Efficacy of applied behavioral intervention in preschool children with autism for improving cognitive, language, and adaptive behavior: a systematic review and meta-analysis. J Pediatr. 2008 doi: 10.1016/j.jpeds.2008.09.012. In press. [DOI] [PubMed] [Google Scholar]
- 9.Johnson CP, Myers SM American Academy of Pediatrics, Council on Children With Disabilities. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183–1215. doi: 10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- 10.Smith M, Rogers S, Dawson G. The Early Start Denver Model: a comprehensive early intervention approach for toddlers with autism. In: Handleman JS, Harris SL, editors. Pre-school Education Programs for Children With Autism. 3. Austin, TX: Pro-Ed Corporation, Inc; 2008. pp. 65–101. [Google Scholar]
- 11.National Research Council, Division of Behavioral and Social Sciences Education. Educating Children With Autism. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 12.Mullen EM. Mullen Scales of Early Learning: AGS Edition. Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- 13.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 14.Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. Los Angeles, CA: Western Psychological Services; 1999. [Google Scholar]
- 15.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 16.Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. J Autism Dev Disord. 2009;39(5):693–705. doi: 10.1007/s10803-008-0674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sparrow S, Balla D, Cicchetti D. Vineland Adaptive Behavior Scales: Interview Edition. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- 18.Bodfish JW, Symons FJ, Lewis MH. The Repetitive Behavior Scale: A Test Manual. Morganton, NC: Western Carolina Center Research Reports; 1998. [Google Scholar]
- 19.Rogers SJ, Dawson G. Early Start Denver Model for Young Children with Autism. New York, NY: Guilford Press; 2009. [Google Scholar]
- 20.Bond GR, Evans L, Salyers MP, Williams J, Kim HW. Measurement of fidelity in psychiatric rehabilitation. Ment Health Serv Res. 2000;2(2):75–87. doi: 10.1023/a:1010153020697. [DOI] [PubMed] [Google Scholar]
- 21.Jocelyn LJ, Casiro OG, Beattie D, Bow J, Kneisz J. Treatment of children with autism: a randomized controlled trial to evaluate a caregiver-based intervention program in community day-care centers. J Dev Behav Pediatr. 1998;19(5):326–334. doi: 10.1097/00004703-199810000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Aldred C, Green J, Adams C. A new social communication intervention for children with autism: pilot randomised controlled treatment study suggesting effectiveness. J Child Psychol Psychiatry. 2004;45(8):1420–1430. doi: 10.1111/j.1469-7610.2004.00848.x. [DOI] [PubMed] [Google Scholar]