Abstract
Offending food allergens can vary with regional preferences in food consumption. In this study, we analysed sensitization rates to commonly consumed foods in Korean adults suspected of having food allergy. One hundred and thirty four subjects underwent a skin prick test (SPT) with 55 food allergens, of which 13 were made by our laboratory and the rest were commercially purchased. Of the 134 patients, 73 (54.5%) were sensitized to one or more food allergens. Sensitization to chrysalis was detected most frequently, at a rate of 25.4%. Sensitization rates to other food allergens were as follows: maize grain (13.4%), shrimp (11.9%), almond (11.1%), wheat flour (8.2%), lobster (8.2%), buckwheat (8.2%), mackerel (5.2%), pollack (5.2%), halibut (4.5%), peanut (4.5%), anchovy (4.4%), squid (3.7%), saury (3.0%), common eel (3.0%), yellow corvina (3.0%), hairtail (2.2%), octopus (2.2%), and others. In addition to well-known food allergens, sensitivity to mackerel, chrysalis, pollack, and halibut, which are popular foods in Korea, was observed at high rates in Korean adults. We suggest that the SPT panel for food allergy in Korea should include these allergens.
Keywords: Food Allergy, Allergen, Eating Habits, Korean, Skin Test, Sensitization
Graphical Abstract

INTRODUCTION
Although less common in adults than in children, food allergy is prevalent in 3%-5% of all adults (1,2,3). They cause substantial economic and emotional problems and can negatively impact physical health (4). With increasing global prominence, food allergy has also emerged as an important problem in Korean adults (5,6,7).
Food allergy is associated with IgE sensitization to particular food allergens, although non-IgE-mediated food allergy immune responses are also known (1). Identifying sensitization to various food allergens is important in the diagnosis and management of food allergy (8). However, the determination of food sensitization rates and patterns may be elusive, because factors, such as subject age and regional preferred food choices, profoundly affect sensitization patterns (9,10): For example, eggs and milk are well-known food allergens in children, but rarely in adults (11), and red meat allergy has been reported exclusively in adults (12,13,14).
To discover sensitization patterns to food allergens in Korea, a multi-centre study was conducted from January 2001 to December 2001 (15). The study showed that chrysalis, shrimp, chestnut, curry, potato, soybean, rice, buckwheat, cabbage, and mackerel are common sensitizing food allergens for individuals older than 10 years of age. However, it did not outline sensitization rates to several other foods commonly consumed in Korea. A variety of fish species, including yellow corvina, hairtail, pollack, and skate, are commonly eaten in Korea. However, the skin prick test (SPT) food panel used in Korea does not include these types of fish. Furthermore, the enrolled subjects were mainly those with respiratory allergy. Thus, it is difficult to discern the sensitization patterns of food allergy in Korean adults. Therefore, studies on the prevalence of food sensitization in Korean adults are needed to create reliable food panels for use in SPT or multiplex serologic-specific IgE measurement (16).
In this study, Korean adult subjects suspected of having food allergy underwent SPT using a panel of commercial allergen reagents and in-house-made allergens from several foods commonly consumed in Korea. Thereafter, we analysed sensitization patterns to these food allergens.
MATERIALS AND METHODS
Patients
This study was conducted from January 2011 to December 2013 at Severance Hospital Allergy - Asthma Clinic. A total of 134 patients suspected of having food allergy were enrolled in this study (Table 1). We restricted enrolment to adults older than 19 years of age, because patterns of food allergen sensitization can differ between children and adults. The mean age of the subjects was 37.7 ± 13.0 years (mean ± SD). They had allergic rhinitis (14.9%), asthma (5.2%), anaphylaxis (26.1%), and urticaria (55.2%).
Table 1. Demographic data and positive rates on skin prick tests.
| Parameters | No. of patients | No. of positive reaction | Positivity, % | P value* |
|---|---|---|---|---|
| Total | 134 | 73 | 54.5 | |
| Sex | 0.008 | |||
| Men | 52 | 36 | 69.2 | |
| Women | 82 | 37 | 45.1 | |
| Age | 0.341 | |||
| 19-29 yr | 49 | 29 | 59.2 | |
| 30-39 yr | 31 | 15 | 48.4 | |
| 40-49 yr | 23 | 11 | 47.8 | |
| 50-59 yr | 22 | 15 | 68.2 | |
| 60-69 yr | 9 | 3 | 33.3 |
A wheal size 3 mm larger than the negative control was regarded as positive.
*P value was calculated by Fisher's exact test.
Skin prick test reagents
Not commercially available, but frequently consumed food allergens, such as hairtail (Trichiurus lepturus Linnaeus), yellow corvina (Larimichthys polyactis), common eel (Anguilla japonica), anchovy (Engraulis japonicus), octopus (Octopus vulgaris), squid (Todarodes pacificus), skate (Raja pulchra), pollack (Theragra chalcogrammus pallas), mackerel (Scomber japonicus Houttuyn), silkworm chrysalis, ginger, and sunflower seed were prepared at the Institute of Allergy, Yonsei University College of Medicine. Each prepared food was mixed with phosphate-buffered saline (PBS) at a 1:10 w/v ratio. Insoluble material was removed, and the remaining solution was mixed with ethyl ether to remove unwanted lipids. The precipitated material was subjected to ethyl ether extraction three more times, and the final precipitate was collected and frozen at -70ºC. Precipitates were freeze-dried and pulverized. Each pulverized powder was individually mixed with PBS and stirred for 2 days at 4ºC to extract proteins. The resulting solution was centrifuged at 15,000 rpm at 4ºC. The supernatant was then dialyzed through a semipermeable membrane with a molecular weight cut-off of 10,000 daltons against distilled water twice for 12 hours each dialyzation. Thereafter, each specimen was centrifuged, and crude allergen extract was obtained by freeze-drying the supernatant. SPT reagents were made by mixing 10 mg of crude extract with 1 mL of distilled water. Protein concentrations were measured by Bradford assay (Bio-Rad Laboratories, Hercules, CA, USA), and the presence of protein was confirmed by SDS-PAGE and subsequent Coomassie blue staining for protein. The other 42 food allergens were obtained from Allergopharma (Hamburg, Germany) and Hollister-Stier (Spokane, WA, USA) (Table 2).
Table 2. Sensitization rates to 55 food allergens.
| Sea foods | Cereals, nuts and bean | Vegetable and fruits | Meats, egg, milk, and others | ||||
|---|---|---|---|---|---|---|---|
| Shrimp | 11.90% | Maize grain | 13.40% | Celery | 10.40% | Chrysalis* | 25.40% |
| Lobster | 8.20% | Almond | 11.20% | Peach | 7.50% | Chicken | 2.20% |
| Mackerel* | 5.20% | Buckwheat | 8.20% | Potato | 6.90% | Duck | 1.50% |
| Pollack* | 5.20% | Soybean | 8.20% | Apple | 3.90% | Beef | 0.70% |
| Anchovy* | 4.50% | Sunflower seed | 8.20% | Spinach | 2.20% | Egg | 0.70% |
| Halibut | 4.50% | Wheat flour | 8.20% | Ginger* | 2.20% | Milk | 0.70% |
| Oyster | 4.50% | Peas | 7.50% | Kiwi | 1.50% | Mutton | 0.70% |
| Squid* | 3.70% | Barley grain | 4.50% | Grape | 0.70% | Pork | 0.70% |
| Common eel* | 3.50% | Peanut | 4.50% | Orange | 0.70% | ||
| Codfish | 3.00% | Hazelnut | 3.70% | Strawberry | 0.70% | ||
| Saury* | 3.00% | Rice | 3.00% | Tomato | 0.70% | ||
| Trout | 3.00% | Walnut | 3.00% | Banana | 0.00% | ||
| Yellow corvina | 3.00% | Rye flour | 2.20% | Parsley | 0.00% | ||
| Salmon | 3.00% | Cacao | 1.50% | Pear | 0.00% | ||
| Hairtail* | 2.20% | ||||||
| Octopus* | 2.20% | ||||||
| Tuna | 2.20% | ||||||
| Mussel | 0.70% | ||||||
| Skate* | 0.70% | ||||||
*Prepared at the Institute of Allergy, Yonsei University College of Medicine.
Skin prick test
After cleansing the patient's back using a 70% isopropyl alcohol cotton wipe, a drop of each food allergen solution, positive control (1 mg/mL histamine in 50% glycerol and 0.4% phenol), and negative control (0.9% normal saline) were placed on the back. Each drop site was separated by a minimum of 2 cm from all other sites. A single-use 26 gauge needle was pushed through each drop and used to lift the skin slightly to improve allergen penetration into the epidermis without inducing bleeding. After 15-30 minutes, wheal sizes were measured at each site. A wheal size 3 mm larger than the negative control was regarded as positive.
Concordance with skin prick test results in patients with suspected culprit food allergens
To investigate the agreement of SPT results with self-reported culprit foods, we asked patients at their first visit about suspected culprit foods. Concordance rates were calculated by comparing SPT results and self-reported culprit foods.
Statistical analysis
Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). The influence of sex and age variables between the groups was calculated using Fisher's exact test, and comparisons of wheal sizes for sensitized patients were made using the median test. The concordance of SPT results and self-reported culprit foods was calculated using the Mann Whitney U test. All P values < 0.05 were considered statistically significant.
Ethics statement
Our hospital ethical review board approved this study (4-2014-0376), and informed consent was exempted.
RESULTS
Demographic data and food allergen sensitization
This study enrolled 134 patients. Seventy three subjects (54.5%) were sensitized to one or more food allergens (Table 1). Men showed significantly higher overall sensitization rates than women (P = 0.008). Overall sensitization rates of patients did not differ significantly by age (Table 1).
Sensitization to silkworm chrysalis was observed most frequently, at a rate of 25.4%. This was followed by maize grain (13.4%), shrimp (11.9%), and almond (11.2%). The rates for other foods are shown in Table 2. Sensitization rates to food allergens prepared by us were as follows: sunflower seed (8.2%), mackerel (5.2%), pollack (5.2%), anchovy (4.5%), squid (3.7%), common eel (3.0%), saury (3.0%), yellow corvina (3.0%), octopus (2.2%), hairtail (2.2%), and skate (0.7%).
Sensitization rates to food allergens were compared according to age groups (Table 3). Chrysalis was the most highly sensitizing allergen among all age groups, and sensitization rates ranked differently according to age groups. Nevertheless, sensitization rates for all allergens did not differ significantly among age groups (Table 3).
Table 3. Frequently sensitized food allergens according to age group.
| 19-29 yr (%) n = 49 |
30-39 yr (%) n = 31 |
40-49 yr (%) n = 23 |
50-59 yr (%) n = 22 |
60-69 yr (%) n = 9 |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Chrysalis | 24.5 | Chrysalis | 25.8 | Chrysalis | 26.1 | Chrysalis | 31.8 | Chrysalis | 11.1 |
| Celery | 20.4 | Maize grain | 16.1 | Sunflower seed | 17.4 | Wheat flour | 18.2 | Mackerel | 11.1 |
| Shrimp | 20.4 | Lobster | 9.7 | Almond | 13 | Peach | 13.6 | Maize grain | 11.1 |
| Maize grain | 18.4 | Peas | 9.7 | Celery | 8.7 | Almond | 9.1 | Wheat flour | 11.1 |
| Almond | 16.3 | Potato | 9.7 | Hazelnut | 8.7 | Common eel | 9.1 | ||
Sensitization rates were also compared according to sex (Table 4). Chrysalis had a higher sensitization rate in men than in women (P = 0.018). Other allergens showed no significant difference between men and women.
Table 4. Frequently sensitized food allergens according to sex of the enrolled subjects.
| Male (%) n = 52 |
Female (%) n = 82 |
||
|---|---|---|---|
| Chrysalis | 36.5% | Chrysalis | 18.3% |
| Maize grain | 15.4% | Maize grain | 12.2% |
| Almond | 13.5% | Shrimp | 12.2% |
| Celery | 13.5% | Almond | 9.8% |
| Soybean | 13.5% | Buckwheat | 8.5% |
| Wheat flour | 13.5% | Celery | 8.5% |
| Shrimp | 11.5% | Potato | 8.5% |
| Sunflower seed | 11.5% | Lobster | 7.3% |
| Peach | 11.5% | Mackerel | 6.1% |
| Peas | 11.5% | Pollock | 6.1% |
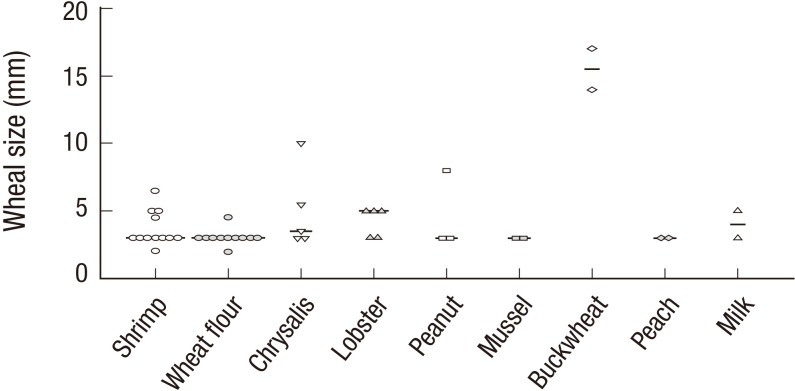
Concordance rate of patient-suspected culprit foods with skin prick test results
A majority of the enrolled patients (78.4%) suspected certain foods to be the causes of their allergic symptoms. The most common self-reported foods were shrimp (22.8%), wheat flour (20%), pork (10.5%), beef (8.6%), and chicken (8.6%) (Table 5). Agreement between these self-reports and SPT results was checked (Table 5). Concordance rates were high for chrysalis (100%), almond (100%), lobster (83.3%), peanut (75%), buckwheat (66.7%), peach (50%), and apple (50%). Meanwhile, rates were low for beef (11.1%), chicken (11.1%), egg (0%), pork (0%), and anchovy (0%). When we compared SPT results for subjects who showed positive concordance, the mean wheal size for buckwheat allergen was the largest (Fig. 1). However, there were no statistically significant differences in mean wheal sizes among the allergens (P = 0.118).
Table 5. Agreement of self-reported culprit food allergens with SPT results.
| Allergens | No. of patients with self-reported culprit allergens | No. of Patients with positive SPT | Agreement (%) |
|---|---|---|---|
| Chrysalis | 5 | 5 | 100 |
| Almond | 1 | 1 | 100 |
| Lobster | 6 | 5 | 83.3 |
| Peanut | 4 | 3 | 75 |
| Buckwheat | 3 | 2 | 66.7 |
| Peach | 4 | 2 | 50 |
| Apple | 4 | 2 | 50 |
| Wheat flour | 21 | 10 | 47.6 |
| Shrimp | 24 | 11 | 45.8 |
| Milk | 5 | 2 | 40 |
| Mussel | 5 | 2 | 40 |
| Mackerel | 3 | 1 | 33.3 |
| Beef | 9 | 1 | 11.1 |
| Chicken | 9 | 1 | 11.1 |
| Egg | 4 | 0 | 0 |
| Pork | 11 | 0 | 0 |
| Anchovy | 3 | 0 | 0 |
| Total | 121 | 48 | 39.7 |
Fig. 1.
Positive wheal size results for a suspected food allergen. Wheal sizes of positive skin prick test that agreed with self-reported culprit foods were compared. The average wheal size for buckwheat allergen was the largest. However, there were no statistically significant differences among average wheal sizes of each allergen (P = 0.118).
DISCUSSION
Culprit food allergens can differ from country to country. In the present study, we intended to make suggestions for an adequate food allergen panel with which to diagnose food allergy in Korea. We therefore included unique and preferred Korean food materials, especially seafoods, in the SPT. In this study, shrimp, buckwheat, wheat flour, peach, lobster, soybean, and peanut showed high sensitization rates, as previously reported (15). Meanwhile, chrysalis, pollack, mackerel, halibut, anchovy, saury, squid, and yellow corvina also showed sensitization rates higher than 3%. The concordance rates of chrysalis, lobster, peanut, buckwheat, peach, and apple between SPT test results and suspected culprit food allergens were all ˃ 50%, suggesting that these food allergens should be included in a Korean food allergen panel for SPT or multiplex serologic measurement.
Pork, beef, chicken, egg, and milk are commonly consumed foods in Korea, and interesting, many Korean adults accused these foods of being culprit food allergens. However, sensitization rates to these foods were low, with little clinical significance (Table 2). Recently, the role of galactose-a-1,3-galactose (alpha gal) in red meat allergy has been discovered (17,18). Patients with allergy to red meat have characteristic clinical features, such as adult onset and delayed appearance of anaphylaxis and/or urticaria, occurring at 3-6 hours after ingestion. In addition, patients usually have positive SPT responses to total red meat extracts (19). These characteristics lowered the likelihood of false negative results in individuals with a negative skin response to pork or beef in this study. Application of alpha gal for serologic testing or SPT may clearly show the role of red meats in food allergy.
Silk worm chrysalis is typically not consumed in Western countries, although it is commonly consumed in Korea, China, and other East Asian countries. While the prevalence of chrysalis allergy is not well known, cases of anaphylaxis by chrysalis are frequently reported (20,21). In China, there are more than 1,000 anaphylactoid reactions caused by chrysalis each year, and among these, 50 patients per year are typically treated at an emergency department (21). These reports suggest that chrysalis food allergy is a real, serious problem in East Asia. Chrysalis has been reported as the most frequently sensitized food allergen in Korean adults (15), and our results were consistent with this observation. Strangely, the overall sensitization rate to chrysalis detected by SPT was 25.4%, while only 4.7% of our patients complained of symptoms associated with chrysalis ingestion. The reason for the high discrepancy (false positivity) between these two values is not known: Perhaps, cross-reactivity of chrysalis to other allergens, such as house dust mite, or the presence of clinically insignificant allergens in the total extract of chrysalis might explain the discrepancy (22,23). Application of component-resolved diagnosis using a clinically significant recombinant major allergen of chrysalis may solve this discrepancy.
Maize grain and celery allergy are rare in Korea. However, these allergens showed sensitization rates of 13.4% and 10.4% in this study, even though none of the enrolled patients complained of symptoms arising from maize grain or celery ingestion. The high false positivity to maize grain and celery may be associated with cross-reactivity to lipid transfer protein (LTP) or Bet v 1-homologous proteins (24). The former is the main allergen of maize grain, and the latter is that of celery. LTP from maize grain comprises a highly homologous amino acid sequence with that in peach, rice, tomato, spinach, apple, and soybean (24,25), and Bet v 1 homologous protein from celery cross-reacts with that of birch, cherry, and carrot (26). False positive results may reflect the fact that all maize is consumed after being steam boiled, baked, or in the form of popcorn, and those processes may destruct the allergen epitope. In addition, consumption of celery is very low in Korea, and may not contribute to real food allergy.
Concordance rates between self-reported culprit foods and SPT results were also examined in this study. Overall, self-reported culprit allergens agreed with SPT results in 39.7% of cases (Table 5). Chrysalis, nuts, crustacean, wheat flour, and fruit showed high agreement, whereas meats and egg showed low agreement. These results suggest that patient suspicion is not reliable and that SPTs maintain an important role in proving the innocence of suspected foods. This low positive concordance rate suggests the need to consider other causes of patient complaints, such as food intolerance, chronic idiopathic urticaria, and non-IgE mediated food allergy.
In comparing wheel sizes of positive SPT, there were no statistically significant differences among average wheal sizes of each allergen. However, SPT wheal size might hold relevance in instances of buckwheat allergy. In the present study, patients with a positive SPT (n = 2) with a compatible clinical history of buckwheat allergy had wheal sizes of 15.5 ± 2.12 mm (mean ± SD) (Fig. 1). However, patients with a positive SPT (n = 5) who did not complain of buckwheat allergy had wheal sizes of 3.5 ± 0.71 mm. These results were significantly different from each other (P < 0.001, Mann Whitney U test).
This study has several limitations. Most importantly, the enrolled subjects were not confirmed as having a food allergy, but had a compatible temporal relation, and allergy was merely suspected by the subjects. Patient suspicion is not sufficient for diagnosis of food allergy (10,27), and potential false positive results associated with SPT have been well-reported. In addition, this study included only 134 patients from a single institution. Accordingly, our data must be interpreted with caution.
In conclusion, this study sought to identify sensitization patterns to commonly consumed foods in Korean adults. The highly sensitized food allergens included chrysalis, shrimp, almond, wheat flour, mackerel, and pollack. Accordingly, we suggest that these allergens should be included in SPT panels in Korea.
Footnotes
Funding: This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI13C0010).
DISCLOSURE: We declare no potential conflicts of interest related to this study.
AUTHOR CONTRIBUTION: Study design: Kim SR, Park KH, Park HJ, Lee JH, Park JW. Data collection: Kim SR. Statistical analysis and interpreted the results: Kim SR, Park KH, Park HJ, Lee JH, Park JW. Writing manuscript: Kim SR, Park KH, Park HJ, Lee JH, Park JW. Final approval: all authors.
References
- 1.Sicherer SH, Sampson HA. 9. Food allergy. J Allergy Clin Immunol. 2006;117:S470–S475. doi: 10.1016/j.jaci.2005.05.048. [DOI] [PubMed] [Google Scholar]
- 2.Park M, Kim D, Ahn K, Kim J, Han Y. Prevalence of immediate-type food allergy in early childhood in Seoul. Allergy Asthma Immunol Res. 2014;6:131–136. doi: 10.4168/aair.2014.6.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee SE, Kim H. Update on early nutrition and food allergy in Children. Yonsei Med J. 2016;57:542–548. doi: 10.3349/ymj.2016.57.3.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sicherer SH, Sampson HA. Food allergy: epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014;133:291–307.e5. doi: 10.1016/j.jaci.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 5.Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, Plaut M, Cooper SF, Fenton MJ, Arshad SH, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126:S1–S58. doi: 10.1016/j.jaci.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oh JW, Pyun BY, Choung JT, Ahn KM, Kim CH, Song SW, Son JA, Lee SY, Lee SI. Epidemiological change of atopic dermatitis and food allergy in school-aged children in Korea between 1995 and 2000. J Korean Med Sci. 2004;19:716–723. doi: 10.3346/jkms.2004.19.5.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu Y, Chen J, Li H. Comparison of food allergy prevalence among Chinese infants in Chongqing, 2009 versus 1999. Pediatr Int. 2010;52:820–824. doi: 10.1111/j.1442-200X.2010.03166.x. [DOI] [PubMed] [Google Scholar]
- 8.Khoriaty E, Umetsu DT. Oral immunotherapy for food allergy: towards a new horizon. Allergy Asthma Immunol Res. 2013;5:3–15. doi: 10.4168/aair.2013.5.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kulig M, Bergmann R, Klettke U, Wahn V, Tacke U, Wahn U, Group MA. Natural course of sensitization to food and inhalant allergens during the first 6 years of life. J Allergy Clin Immunol. 1999;103:1173–1179. doi: 10.1016/s0091-6749(99)70195-8. [DOI] [PubMed] [Google Scholar]
- 10.Rona RJ, Keil T, Summers C, Gislason D, Zuidmeer L, Sodergren E, Sigurdardottir ST, Lindner T, Goldhahn K, Dahlstrom J, et al. The prevalence of food allergy: a meta-analysis. J Allergy Clin Immunol. 2007;120:638–646. doi: 10.1016/j.jaci.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 11.Osterballe M, Hansen TK, Mortz CG, Høst A, Bindslev-Jensen C. The prevalence of food hypersensitivity in an unselected population of children and adults. Pediatr Allergy Immunol. 2005;16:567–573. doi: 10.1111/j.1399-3038.2005.00251.x. [DOI] [PubMed] [Google Scholar]
- 12.Commins SP, Platts-Mills TA. Anaphylaxis syndromes related to a new mammalian cross-reactive carbohydrate determinant. J Allergy Clin Immunol. 2009;124:652–657. doi: 10.1016/j.jaci.2009.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Commins SP, Platts-Mills TA. Delayed anaphylaxis to red meat in patients with IgE specific for galactose alpha-1,3-galactose (alpha-gal) Curr Allergy Asthma Rep. 2013;13:72–77. doi: 10.1007/s11882-012-0315-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saleh H, Embry S, Nauli A, Atyia S, Krishnaswamy G. Anaphylactic reactions to oligosaccharides in red meat: a syndrome in evolution. Clin Mol Allergy. 2012;10:5. doi: 10.1186/1476-7961-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim SH, Kang HR, Kim KM, Kim TB, Kim SS, Chang YS, Kim CW, Bahn JW, Kim YK, Cho SH, et al. The sensitization rates of food allergens in a Korean population: a multi-center study. J Asthma Allergy Clin Immunol. 2003;23:502–514. [Google Scholar]
- 16.Ahn K. The usefulness of component-resolved diagnostics in food allergy. Allergy Asthma Immunol Res. 2014;6:103–104. doi: 10.4168/aair.2014.6.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mullins RJ, James H, Platts-Mills TA, Commins S. Relationship between red meat allergy and sensitization to gelatin and galactose-α-1,3-galactose. J Allergy Clin Immunol. 2012;129:1334–1342.e1. doi: 10.1016/j.jaci.2012.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wen L, Zhou J, Yin J, Sun JL, Sun Y, Wu K, Katial R. Delayed anaphylaxis to red meat associated with specific IgE antibodies to galactose. Allergy Asthma Immunol Res. 2015;7:92–94. doi: 10.4168/aair.2015.7.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Commins SP, Satinover SM, Hosen J, Mozena J, Borish L, Lewis BD, Woodfolk JA, Platts-Mills TA. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-α-1,3-galactose. J Allergy Clin Immunol. 2009;123:426–433.e2. doi: 10.1016/j.jaci.2008.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ji K, Chen J, Li M, Liu Z, Wang C, Zhan Z, Wu X, Xia Q. Anaphylactic shock and lethal anaphylaxis caused by food consumption in China. Trends Food Sci Technol. 2009;20:227–231. doi: 10.1016/j.tifs.2009.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ji KM, Zhan ZK, Chen JJ, Liu ZG. Anaphylactic shock caused by silkworm pupa consumption in China. Allergy. 2008;63:1407–1408. doi: 10.1111/j.1398-9995.2008.01838.x. [DOI] [PubMed] [Google Scholar]
- 22.He Y, Liu X, Huang Y, Zou Z, Chen H, Lai H, Zhang L, Wu Q, Zhang J, Wang S, et al. Reduction of the number of major representative allergens: from clinical testing to 3-dimensional structures. Mediators Inflamm. 2014;2014:291618. doi: 10.1155/2014/291618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferreira F, Wolf M, Wallner M. Molecular approach to allergy diagnosis and therapy. Yonsei Med J. 2014;55:839–852. doi: 10.3349/ymj.2014.55.4.839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Breiteneder H, Ebner C. Molecular and biochemical classification of plant-derived food allergens. J Allergy Clin Immunol. 2000;106:27–36. doi: 10.1067/mai.2000.106929. [DOI] [PubMed] [Google Scholar]
- 25.Pastorello EA, Farioli L, Pravettoni V, Ortolani C, Ispano M, Monza M, Baroglio C, Scibola E, Ansaloni R, Incorvaia C, et al. The major allergen of peach (Prunus persica) is a lipid transfer protein. J Allergy Clin Immunol. 1999;103:520–526. doi: 10.1016/s0091-6749(99)70480-x. [DOI] [PubMed] [Google Scholar]
- 26.Sánchez-Monge R, Lombardero M, García-Sellés FJ, Barber D, Salcedo G. Lipid-transfer proteins are relevant allergens in fruit allergy. J Allergy Clin Immunol. 1999;103:514–519. doi: 10.1016/s0091-6749(99)70479-3. [DOI] [PubMed] [Google Scholar]
- 27.Venter C, Pereira B, Grundy J, Clayton CB, Arshad SH, Dean T. Prevalence of sensitization reported and objectively assessed food hypersensitivity amongst six-year-old children: a population-based study. Pediatr Allergy Immunol. 2006;17:356–363. doi: 10.1111/j.1399-3038.2006.00428.x. [DOI] [PubMed] [Google Scholar]