Abstract
We report a case that documents the second known patient treated by anti-TNFα who has been diagnosed a cerebral toxoplasmosis.
The patient was a 64-year-old Caucasian woman, treated by adalimumab for an erosive rheumatoid arthritis (RA).
While the clinical response was satisfactory, she has presented a first epileptic seizure, without other neurological sign, 2 months after the beginning of adalimumab.
Brain CT and brain MRI revealed multiple bilateral supratentorial ring-shaped brain lesions, enhanced after injection of a contrast agent.
Diagnostic stereotactic brain biopsy revealed lymphocytic and plasma cells infiltration, and Toxoplasma gondii DNA by PCR on the brain biopsy was positive, confirming the diagnosis of cerebral toxoplasmosis.
Our case report illustrates the increased risk of toxoplasmosis in RA patients treated with anti-TNFα therapy. Indeed, it is suspected that the IFN-γ adalimumab-related inhibitory effect may favor T. gondii replication and reactivation.
Introduction
We report a case that documents the second known patient treated by anti-TNFα who has been diagnosed as cerebral toxoplasmosis.
Case presentation
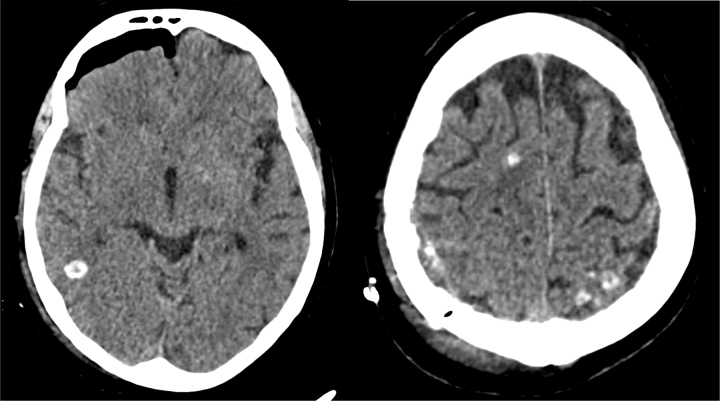
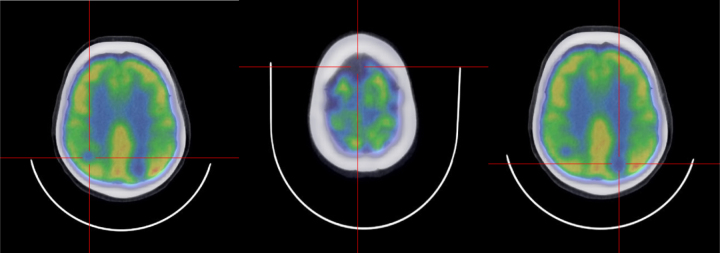
The patient was a 64-year-old Caucasian woman, and has been followed in rheumatology for one year for an erosive rheumatoid arthritis (RA), rheumatoid factor positive, anti–citrullinated protein antibody (ACPA) negative. She was first treated by methotrexate, and an anti-TNF-α, etanercept 50 mg every week, was prescribed 5 months later due to insufficient response. Eventually, a loss of efficacy appeared about 3 months after biotherapy’s onset, and adalimumab 40 mg every 2 weeks was started with the concomitant pursuit of methotrexate 20 mg once a week, and prednisone 10 mg per day. While the clinical response was satisfactory, she presented with a first tonic-clonic seizure, without other neurological sign, 2 months after the beginning of adalimumab. Brain CT and brain MRI revealed multiple bilateral supratentorial ring-shaped brain lesions, enhanced after injection of a contrast agent (Fig. 1). PET-scan showed hypometabolism next to parenchymal brain lesions (Fig. 2). Paraclinical exams were performed, such as PET scan, colonoscopy, gastroscopy, mammography, and ENT examination, assuming that there were neoplastic lesions, but no primary cancer was found.
Fig. 1.
Brain CT.
Fig. 2.
Brain PET-scan.
Lumbar puncture did not reveal any abnormality (1 element/mm3 (lymphocyte), no red blood cell, cerebrospinal fluid protein 38 mg/dl, no hypoglycorrhachia, Toxoplasmosis PCR negative and no cancer cells). HIV serology was negative. Diagnostic stereotactic brain biopsy revealed lymphocytic and plasma cells infiltration, mainly perivascular, with wide areas of acetowhite necrosis, containing very small round structures. Special stains of PAS, Grocott and Ziehl were negative. Immunostaining anti-CD20 was positive for medium perivascular cells and immunostaining anti-CD3 was positive for a lot of small reactive lymphocytes. Immunostaining anti-toxoplasmosis was positive for many small round structures in the acetowhite necrosis areas. Toxoplasma gondii DNA by PCR on the brain biopsy was positive, confirming the diagnosis of cerebral toxoplasmosis.
Toxoplasmosis serology (latex test agglutination) was positive (IgM 0.59 U/ml, IgG 1653 U/ml, IgA 10 U/ml; Architect, Abbott), and confirmed that the patient has presented a toxoplasmosis seroreactivation, documented by a strong rise of immunoglobulins G and A, comparatively to a serology done one year before (IgM 0.19 U/ml and IgG 5 U/ml). Serology done one year prior to presentation shows evidence of immunity to Toxoplasma gondii with low IgG and negative IgM, likely related to previous asymptomatic infection. Date of the seroconversion could not been detailed, due to a lack of blood serum within 6 months.
Treatments by adalimumab and methotrexate were interrupted, and a treatment by sulfamethoxazole 1600 milligrams (mg) and trimethoprim 320 mg twice a day was initiated, with a concomitant folinic acid supplementation. The dose had to be decreased due to acute renal failure, and a treatment by sulfamethoxazole 800 mg and trimethoprim 160 mg twice a day has been continuing.
Discussion
This is the second observation of a cerebral toxoplasmosis in a RA patient treated by anti-TNF-α [1]. The diagnosis was undoubted because Toxoplasma gondii DNA by PCR on the brain biopsy was positive, even though PCR on the CSF was negative, which has already been described [2], [3]]. With the report of two patients treated by anti-TNF-α who developed toxoplasmic chorioretinitis [4], our case report illustrates the increased risk of toxoplasmosis in RA patients treated with anti-TNF-α therapy. It should be noted that a similar case has also been described in a patient with a spondylo-arthritis [5]. Indeed, it is suspected that the IFN-γ adalimumab-related inhibitory effect may favor T. gondii replication and reactivation [6].
As the patient was treated by anti-TNF-α, it is apparently an endogenous reactivation of the parasite, from toxoplasma tissue cyst, either directly in brain, or in other organs with parasitaemia and secondary brain involvement.
References
- 1.Nardone R., Zuccoli G., Brigo F., Trinka E., Golaszewski S. Cerebral toxoplasmosis following adalimumab treatment in rheumatoid arthritis. Rheumatol Oxf Engl. 2014;53:284. doi: 10.1093/rheumatology/ket364. [DOI] [PubMed] [Google Scholar]
- 2.Cingolani A., De Luca A., Ammassari A., Murri R., Linzalone A., Grillo R., Antinori A. PCR detection of Toxoplasma gondii DNA in CSF for the differential diagnosis of AIDS-related focal brain lesions. J Med Microbiol. 1996;45:472–476. doi: 10.1099/00222615-45-6-472. [DOI] [PubMed] [Google Scholar]
- 3.Anselmo L.M., Vilar F.C., Lima J.E., Yamamoto A.Y., Bollela V.R., Takayanagui O.M. Usefulness and limitations of polymerase chain reaction in the etiologic diagnosis of neurotoxoplasmosis in immunocompromised patients. J Neurol Sci. 2014;346:231–234. doi: 10.1016/j.jns.2014.08.034. [DOI] [PubMed] [Google Scholar]
- 4.Lassoued S., Zabraniecki L., Marin F., Billey T. Toxoplasmic chorioretinitis and antitumor necrosis factor treatment in rheumatoid arthritis. Semin Arthritis Rheum. 2007;36:262–263. doi: 10.1016/j.semarthrit.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Azevedo V.F., Pietrovski C.F., de Almeida Santos M. Acute toxoplasmosis infection in a patient with ankylosing spondylitis treated with adalimumab: a case report. Reumatismo. 2010;62:283–285. doi: 10.4081/reumatismo.2010.283. [DOI] [PubMed] [Google Scholar]
- 6.Giese A., Stuhlsatz S., Däubener W., MacKenzie C.R. Inhibition of the growth of Toxoplasma gondii in immature human dendritic cells is dependent on the expression of TNF-alpha receptor 2. J Immunol Baltim Md 1950. 2004;173:3366–3374. doi: 10.4049/jimmunol.173.5.3366. [DOI] [PubMed] [Google Scholar]