Abstract
Biomedical devices are essential for patient diagnosis and treatment; however, when blood comes in contact with foreign surfaces or homeostasis is disrupted, complications including thrombus formation and bacterial infections can interrupt device functionality, causing false readings and/or shorten device lifetime. Here, we review some of the current approaches for developing antithrombotic and antibacterial materials for biomedical applications. Special emphasis is given to materials that release or generate low levels of nitric oxide (NO). Nitric oxide is an endogenous gas molecule that can inhibit platelet activation as well as bacterial proliferation and adhesion. Various NO delivery vehicles have been developed to improve NO’s therapeutic potential. In this review, we provide a summary of the NO releasing and NO generating polymeric materials developed to date, with a focus on the chemistry of different NO donors, the polymer preparation processes, and in vitro and in vivo applications of the two most promising types of NO donors studied thus far, N-diazeniumdiolates (NONOates) and S-nitrosothiols (RSNOs).
Keywords: Nitric oxide, thromboresistance, bactericidal, biocompatibility, N-diazeniumdiolate (NONOate), S-nitrosothiol (RSNO)
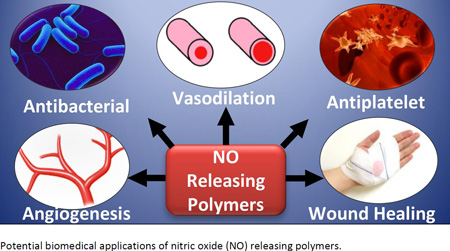
Graphical abstract
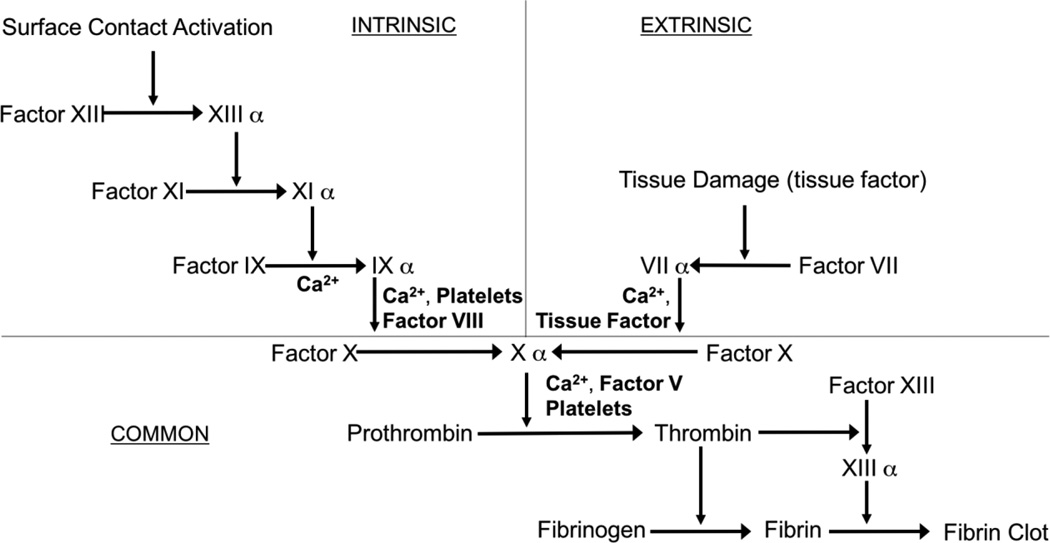
Blood-contacting biomaterials are an integral part of various biomedical devices, ranging from simple catheters to intravascular grafts to extracorporeal circuits and membrane oxygenators, that offer lifesaving treatments to thousands of patients every day. The incorporation of these blood-contacting materials is usually complicated by foreign body responses that is initiated by the coagulation cascade1 (see Figure 1).
Figure 1.
Simplified schematic of the blood-coagulation cascade, where both intrinsic (surface contact) and extrinsic (tissue factors) pathways converge and ultimately form thrombus (modified from review by Sefton et al.2).
Exposure of blood to foreign materials will cause plasma proteins, such as Factor XII and Factor XI, to be activated and adhere to the polymer surface. The activated protein will interact with platelet surface membrane receptor GPIIb/IIIa, that can bind with fibrinogen, von Willebrand Factors (vWF), fibronectin, and vitronectin, which ultimately leads to platelet conformational changes, subsequent release of intracellular agents, (e.g., Factor V, VIII and Ca2+, etc.), and initiates platelet activation and aggregation (intrinsic pathway).2,3 Further, surgical procedures that utilize these devices have the potential to injure the vessel wall, disrupt blood homeostasis and release tissue factor, also causing platelet activation and concomitant conformational changes as well (extrinsic pathway).1–6 Both pathways converge and trigger the coagulation cascade as the activated platelets bind with fibrinogen and other clotting factors. Fibrinogen forms insoluble fibrin, which traps red blood cells and ultimately forms a thrombus within a matter of hours7,8 (see Figure 2).
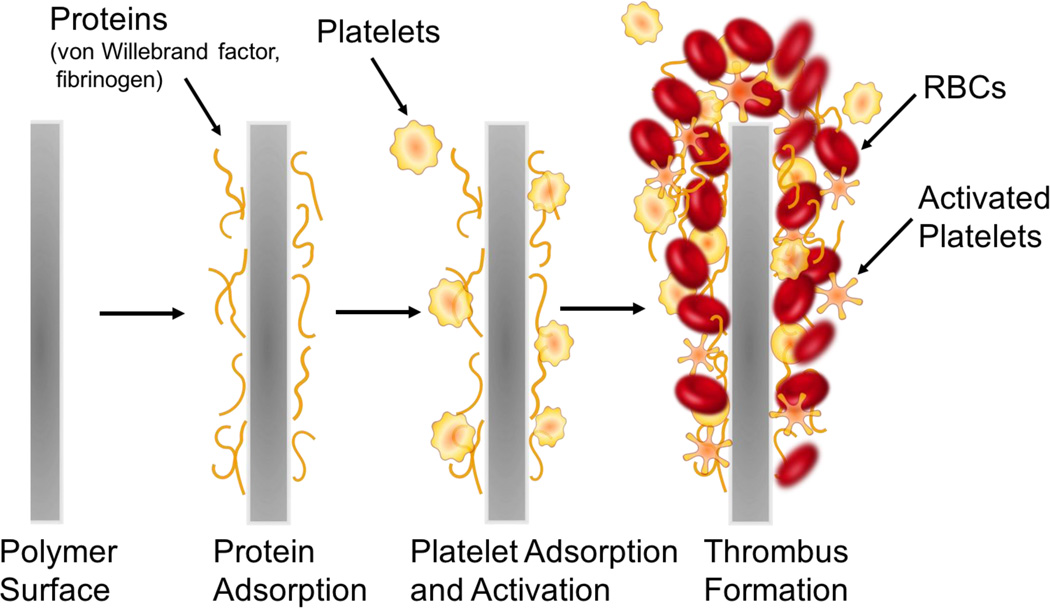
Figure 2.
Simplified representation of the processes that lead to thrombus formation on the surfaces of blood contacting biomedical devices.
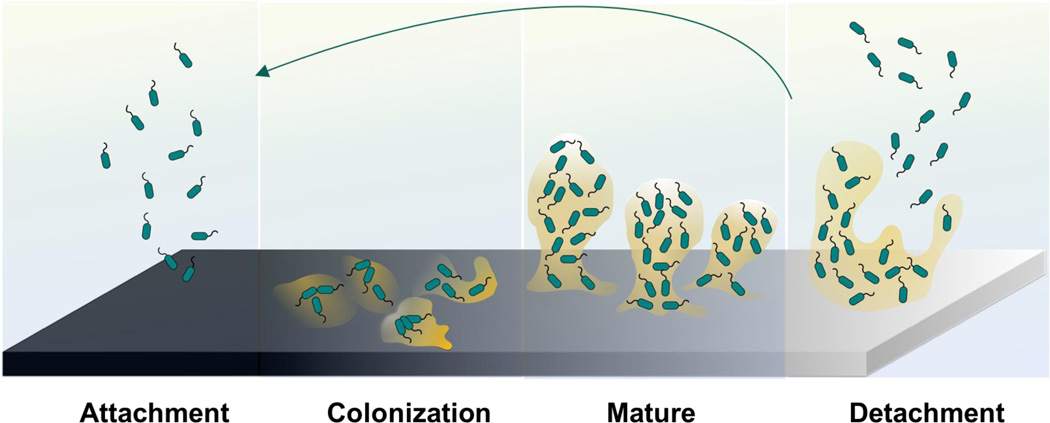
In addition to thrombus formation, bacterial infection is also often associated with the use of many biomedical devices. The rise of hospital-acquired infections, also known as nosocomial infections, is a growing concern in healthcare industry. It was reported that an estimated 1.7 million patients suffered from healthcare-associated infections (HAI) in the U.S. hospitals in 2002 and the number of HAI deaths was 98,987 patients, including 30,665 resulting from bloodstream infections.9–15 Device-related infections are the result of bacteria adhesion to the biomaterial surface. After planktonic bacteria initially colonize onto the surfaces of polymeric devices, cells start to grow into colonies, and then hydrated matrices of extracellular polymeric substances (EPS) are formed, also known as biofilms,16–18 (see Figure 3).
Figure 3.
Representative processes involved in biofilm formation and bacteria dispersion.
The EPS holds the bacterial cells together in a mass and firmly attaches the cells to the underlying surface. Ultimately, a mature biofilm will periodically release bacteria cells from the biofilm colony into the surrounding medium. Of note, the EPS is both a physical and a chemical barrier to antibiotics and significantly retards their rate of penetration that makes conventional antibiotic treatment for such infections ineffective. Further, the EPS can possibly foster antibiotic-resistant bacterial gene mutations.19 Ideally, all biomedical devices should be able to prevent bacterial colonization on their surfaces, especially within the first 6 h of blood exposure, which is identified to be the most susceptible and most “decisive period” for the success of a long-term implant.20 Thrombus and bacteria biofilm formation cause device failure, which in many cases can only be solved by device removal and replacement. Besides patients suffering, the increased healthcare costs associated with these infections has also created a significant economic burden.20
The clinical problems of thrombus and infection described above have triggered substantial interest among scientists to develop new and more effective ways to create antithrombotic and antibacterial polymeric surfaces for biomedical devices, especially those in direct contact with blood (e.g., intravascular catheters, vascular grafts, etc.).
Current strategies for prevention of thrombosis
1) Actively releasing anticoagulants to block the innate coagulation cascade
In a clinical setting, in order to prevent surface-induced thrombosis during cardiopulmonary bypass, hemodialysis, and angioplasty, anticoagulants are routinely administered, the most commonly used one being heparin.2,21 However, systemic heparin administration can lead to hemorrhage and thrombocytopenia. Localized release of heparin with concentrations that are not tolerable at the systemic level may be applied with minimal side-effects.22,23 To date, several approaches have been pursued to achieve localized heparin activity at the surface of implanted devices including the creation of heparin-releasing polymer surfaces via ionic bonding,22,24–26 physical dispersion27–30 and solution swelling,22,31,32 as well as heparin-immobilized polymer surfaces.33–36 For example, Gutowska et al.22 described a novel thermosensitive heparin-releasing poly(N-isopropylacrylamide) (poly(NiPAAm)) coating for prevention of surface-induced thrombosis on polyurethane catheters. Poly(NiPAAm) has a lower critical solution temperature (LCST) in aqueous solution, around 32 °C, which enables it to swell when immersed in a heparin solution at low temperature (e.g., room temperature, RT) and uptake this polyanionic drug. When the temperature is higher than LCST, the swollen coating will collapse dramatically and release heparin. Both the heparin impregnated and control PU catheters were inserted into saphenous veins in a canine model for 1.5 h, and the heparin-releasing PU catheter surfaces demonstrated a significant reduction of thrombus formation after contact with the venous blood. This was demonstrated by SEM images of the explanted catheters when compared to the appropriate controls. Heparin typically has low solubility in organic solvents, but this swelling method introduced the possibility of solution absorption in water and loading of relatively large amount of the drug into the swollen polymer chains. This method also offers flexibility for the amount and type of anticoagulant drugs that can be loaded into various thermosensitive coatings.22 However, the heparin release kinetics for this system are relatively fast, with the release rates of 1 µg/cm2 per h for up to 6 h. Therefore, the potential application of this material is limited to preventing thrombosis formation in short-term applications, such as for angiography catheters, etc.
Heparin has also been covalently linked to the surface of vascular grafts via end-point immobilization and this approach has been commercialized for expanded polytetrafluoroethylene (ePTFE) and Dacron grafts.37–39 The key to the success of heparin-immobilized polymers depends on the covalently bound heparin remaining flexible enough to bind antithrombin III in order to prevent fibrin formation and the ultimate blood clot.3 The literature on immobilization of heparin is vast and has been reviewed extensively elsewhere.37,40 However, due to their very short half-life,41 heparinized polymer surfaces still suffer a great challenge when it comes to long-term in vivo applications. Other anticoagulants such as thrombomodulin,36 direct thrombin inhibitors (e.g., hirudin42 and argatroban43), or antiplatelet drugs (e.g.: prostacyclin (PGI2))36,41,42 have also been immobilized onto polymer surfaces to increase their hemocompatibility, with varying degrees of success.
2) Chemical modification of the polymer surface to reduce protein adsorption
It is widely known that the first step that initiates activation of the coagulation cascade is protein adsorption (especially fibrinogen and von Willebrand factor; see Figure 2) to the surface of a blood contacting medical device. This knowledge has led to many years of research in developing approaches to modify polymer surfaces that focus on reducing such non-specific protein adsorption. Some examples include immobilizing a layer of blood-compatible hydrogels on the device surfaces, such as poly(vinyl alcohol) (PVA), polyacrylamide (PAAm), poly(N-vinyl pyrrolidone) (PNVP), poly(hydroxyethyl methacrylate) (PHEMA), poly(ethylnen oxide) (PEO), poly(ethylene glycol) (PEG), poly(ethylene glycol) monomethyl ether (PEGME), and Cellulose.3,22,44 Hydrogels are water-swollen polymeric networks containing chemical or physical cross-links and were first used initially as soft contact lenses in the late 1950s.45 Due to their hydrophilicity and excellent water retention properties, they have the natural tendency to prevent cell and protein adhesion and are considered to be very biocompatible and desirable in biomedical applications. For example, immobilization of PEG (-CH2CH2O-) is a widely used method to modify traditional polymer surfaces employed in the medical field, such as plasticized poly(vinyl chloride) (PVC) and polyethylene (PE), etc.46–49 PEG is a non-toxic water-soluble polymer approved by the U.S. Food and Drug Administration (FDA) for internal consumption.50 Lakshmi et al.46 were among the first to graft PEG 4000 onto medical grade PVC sheets and conducted thrombogenicity studies to evaluate platelet adhesion using platelet rich plasma (PRP) and whole blood clotting time with fresh rabbit blood. The scanning electron microscope (SEM) images clearly indicated more platelet adhesion to the bare PVC sheet than the PEG-grafted ones. The PEG grafting also extended the whole blood clotting time from 20 min to more than 70 min as determined by the hemolysis assay. Balakrishnan et al.47 later demonstrated success using bulk modification of PVC resin with PEG 600 that yielded greatly reduced solid/water interfacial free energy and platelet adhesion in in vitro PRP studies. This study expanded the anti-fouling chemistry from surface modification on a finished product to bulk synthesis. However, studies conducted by Sefton and coworkers who used PEG immobilized PVA hydrogel coated PE tubing in an ex vivo canine arteriovenous (AV) shunt reported that neither the PEG grafted or control PVA tubing could maintain circulating platelet levels after 4 d.49 Heparin and hydrogel modified surfaces are the most commonly studied approaches for achieving thromboresistant surfaces. For further breadth, readers are guided to reviews that highlight additional approaches developed thus far, such as endothelial cell coated-surfaces, albumin-coated surfaces, pyrolytic carbon-coated surface, phosphorylcholine surfaces, elastin-inspired surfaces, etc.3,42,51–53
Current strategies for creating antibacterial surfaces
1) Surfaces that resist bacteria and reduce initial attachment
Bacteria attachment to device surfaces is the first step required for biofilm formation. Therefore, using biomaterial surfaces that resist bacteria attachment is an intuitive solution to this problem.54 Super-hydrophobic polymer surfaces, such as very smooth silicone, polyurethane, polytetrafluoroethylene (PTFE), poly(vinyl chloride) (PVC), and polyethylene (PE), that have water contact angles larger than 150°, low surface energy,55,56 as well as unique water repellent57 and self-cleaning abilities,56 are known to have resistance to microbial cell adhesion during short-term applications.58 Hydrophilic surface modifications, such as the PEG modified surfaces discussed above, have also been widely characterized in the literature and have demonstrated excellent anti-adhesive properties for bacteria cells and proteins.44 However, the susceptibility of PEG to oxidative damage, especially in the presence of O2, transition metal ions or certain enzymes in vivo, has limited its long-term application in complex media.59,60 Some studies have demonstrated that polymer surfaces with segmented block co-polymers (hard and soft domains) that result in phase-separated structures also exhibit less bacterial adhesion and cell attachment.61–63 Overall, however, passive surfaces without functional active agents may not be ideal for long-term applications because these surfaces may eventually become contaminated due to defects during preparation or deterioration of the coating when in contact with physiological fluids.3,4,64
2) Surfaces that disperse or detach biofilms
Biofilm dispersal is a promising area of research that focuses on how to inhibit biofilm formation using dispersal agents, which induce biofilm bacteria to detach and return to their planktonic form. Several studies have found that bacteria naturally produce biofilm dispersal agents when the community senses a quorum, signaling the detachment process.54 These agents include D-amino acids,65 cis-2-decenoic acid (C2DA),16,18,54 peptides and various enzymes (e.g., dispersin B), etc.54,66 However, most mechanisms of action of these compounds are still unclear, which hinders further development and application in this field. Many researchers have studied the effects of these dispersal agents in vitro, by adding the agents directly to pre-formed biofilm in petri dishes or bioreactors.67 Jennings et al. attempted to load C2DA into chitosan sponges for localized delivery by initially immersing the sponges into 1 mL of 100 mg/mL C2DA in 10 % enthanol.67 The release of C2DA was determined by HPLC and its release lasted 5 d (200–1000 µg/mL) with a burst of C2DA release on day 1. The anti-biofilm efficiency of the C2DA loaded chitosan sponge was tested against clinical isolates of methicillin-resistant Staphylococcus aureus (MRSA) and the results showed that C2DA at a concentration (in the sponge) at or above 500 µg/mL can inhibit bacterial growth. Current research in this field is aimed at developing vehicles for the controlled and sustained release of such biofilm dispersal agents.54
3) Surfaces that have bactericidal functionalities
The most common mechanism of creating functional antibacterial surfaces is through a bactericidal effect, which includes employing a vast collection of approaches involving quaternary ammonium compounds (QACs)64,68–70 and other polycations (e.g., organometallic dendrimers71 and chlorhexidine72), metal ions (e.g., silver,73,74 copper,75 titanium,76 etc.), locally released antibiotics (e.g., gentamicin66,77,78) or bactericidal agents (e.g., bacteriophages,54,79,80 protein synthesis inhibitors,66 antibacterial enzymes such as lysozyme,64,81 antibacterial peptides,82–84 natural biomolecules such as chitosan85–87 and herbal extract (e.g., flavanones and chalcones),88 etc.), and inducing oxidative stress.71,89 In general, the mechanisms of bactericidal surfaces are: 1) contact-based bactericidal activity (e.g., QAC, etc.) which affects the ion-exchange processes and cause general perturbations that destabilize the cytoplasmic membranes of bacteria, resulting in leakage of the intracellular fluid; and 2) release-based bactericidal (e.g., metal ions, antibiotics, etc.), which damage the bacterial cell membrane as well as disrupt the function of bacterial enzymes, DNA, proteins and cell membranes.64 A problem, however, with many bactericidal surfaces is the attachment of dead microorganisms remaining on the antibacterial coatings, which can trigger immune response and inflammation, as well as block a given coating’s active functional group.
In recent years, in order to achieve improved antibacterial and anti-fouling efficacy, many researchers have developed polymeric surfaces that combine more than one of the antibacterial functionalities mentioned above; for example, creating a surface that not only can attach and kill bacteria but also be able to release any adhered dead bacteria debris. Toward this goal, many pH,59,81,90 thermo,91 or electrical voltage92-responsive polymers, that can be controllably extended or collapsed or altered in their charge carrying properties have been developed. They are often termed “stimuli-responsive smart antibacterial surfaces”. Jiang and coworkers developed a cationic poly(N,N-dimethyl-N-(ethoxycarbonylmethyl)-N-[2’-(methacryloyloxy)ethyl]-ammonium bromide) that has a quaternary ammonium group and was grafted onto a gold surface by surface-initiated atom transfer radical polymerization.59 The cationic surface can kill 99.9% of E. coli bacteria when exposed to a suspension of 1010 cells/mL for 1 h, and then it hydrolyzes into a nonfouling zwitterionic surface and releases 98 % of the bacterial residue after 8 d at 37 °C and pH 10.0. This is only a one-time transition between cationic and zwitterionic surface; therefore, in order to achieve a fully reversible “kill and release” functional surface, a surface with morpholinone derivatives that can be switched repeatedly between two equilibrium states was developed by the same authors.90 In neutral or basic aqueous phase, the surface will release dead bacteria and at the same time resist bacteria adhesion. However, under acidic conditions (e.g., in acetic acid for 20 h), the surface will regenerate bacteria-killing function by reforming the quaternary ammonium functional group.
Of note, there are some limitations of this method of using pH change to alter antimicrobial properties of a surface. These include: 1) this surface can kill bacteria attached on the surface while it is dry, since a wet version of this surface is generally resistant to bacterial attachment, suggesting this method mainly works for applications that prevent airborne bacteria; and 2) the requirement of changing environmental pH to achieve surface functionality may be difficult in situ with certain biomedical applications (e.g., blood contacting devices). Most recently, Chen and coworker developed an on-demand switchable and repeatable antibacterial surface. They used a silicone nanowire grafted pH-responsive poly(methacrylic acid) (SiN-PMAA) for loading a natural antibacterial agent (i.e.., lysozyme enzyme), enabling killing of bacteria and releasing dead bacteria debris when alternating the environmental pH between 4, 7 or 10, respectively. The SiN-PMAA surface exhibits a high capacity for binding lysozyme at acidic pH, but can release the majority of the adsorbed lysozyme that serves as biocide to kill bacteria attached to the surface or suspended in solution at neutral pH, and then release the dead bacteria to provide a self-cleaning process when the environment pH is increased to a basic value. This dynamic reservoir concept may serve as the foundation for engineering multifunctional surfaces that may find many practical applications (such as biocatalysis and biosensing) in both biomedical and biotechnology fields. However, achieving the needed changes in pH within blood, which is relatively strongly buffered, will be more challenging.
Lastly, bacterial interference is a different concept that uses active bacteria (either probiotic bacteria54,93,94 or bacteria with less virulence95–97) to inhibit the targeted bacteria by competing for common resources in the same environment. This approach can be leveraged to prevent infections from exogenous sources. Trautner et al. reported a prospective clinical trial of using nonpathogenic bacteria colonized on urinary catheters in patients who require indwelling catheter drainage, to examine their effect in preventing bacteriuria commonly present in patients with indwelling urinary tract catheters.97 Commercial urinary catheters were incubated in broth of Escherichia coli (E. coli) HU2117, a genetic strain that can cause persistent colonization without symptomatic infection,98 for 48 h before insertion into patients for 28 d. The patients’ urine samples were collected at various time points until E. coli HU2117 was no longer detected. Ten (83 %) out of 12 subjects were successfully colonized with E. coli HU2117 for 14 d or more (range, 15–165 d) after inoculation by insertion of the catheter. One patient had urinary tract infection (UTI) symptoms caused by Pseudomonas but none of the patients experienced UTI attributable to the colonization of E. coli HU2117. The overall rate of symptomatic UTI for this study was 0.15 cases per 100 patient-days of colonization, compared to the reported rate of 2.72 cases per 100 patient-days, which suggested that this organism may have a protective function in patients who used the E. coli colonized catheters.99 However, a larger study group is needed to test the safety and efficacy of E. coli HU2117 coated catheters in highly problematic populations.
Creating Dual-Functionality Hemocompatible Surfaces
The ultimate truly hemocompatible polymer for blood-contacting biomedical devices should have both antithrombotic and antibacterial functionalities. Many dual-functional materials have been investigated, including zwitterion-based surfaces, submicron-patterned surfaces, and surfaces with multiple functional moieties, etc.
Zwitterionic polymers are polymers with equimolar number of homogeneously distributed anionic and cationic groups on their polymer chains, that form a hydration layer on the surface of the material through electrostatic interaction and therefore resists plasma protein and bacterial cell adhesion.64,100,101 An alternative strategy towards creating hemocompatible surfaces is to change the polymer’s surface topography, thereby mediating subsequent biological responses. Creating a submicron-textured surface can dramatically reduce the accessible contact area for platelets or bacteria to interact with the surface, thereby minimizing the opportunities for bacteria and platelet adsorption.102–104 Polymers that combine multiple functional groups on one surface have also been tested, such as combining synthetic heparin-mimetic polymer or hydrophilic polymer brushes (e.g., PEG) with antibacterial quaternary compounds (QAC) or Ag nanoparticles.105–107
Despite some successes in the research laboratory with the methods reported above, newer approaches to reduce the possibility of thrombus and/or infection on indwelling device surfaces are still in great demand within the medical community. Therefore, the main focus of the remaining content of this review is the utilization of polymer-based NO delivery to prepare dual functioning antithrombotic and antibacterial surfaces for biomedical applications.
Nitric Oxide (NO) to the rescue
Nitric oxide (NO), a diatomic free radical, was identified as the endothelium-derived relaxation factor (EDRF) in the Nobel Prize-winning discovery by Ignarro, Furchgott, and Murad in 1987.20,108–113 Many researchers have later unveiled NO’s various physiological functions in the human body, including preventing platelet activation and adhesion, inhibiting bacterial proliferation and biofilm formation, enhancing endothelization, signaling in the immune system’s response, and promoting angiogenesis and the wound healing process.112,114–117
The human body synthesizes a large quantity of bio-regulatory NO from the substrate L-arginine via three distinct isoforms of nitric oxide synthase (NOS), including endothelial NOS (eNOS), neuronal NOS (nNOS) and inducible NOS (iNOS).118–120 The NO produced by eNOS contributes to the thromboresistant properties of the endothelial lining of blood vessels by inhibiting platelet activation. The activation of platelets is mediated by NO through the soluble guanylate cyclase (sGC) pathway. NO binds to the heme iron moiety of sGC and subsequently increases intracellular concentrations of cyclic guanosine monophosphate (cGMP).121,122 In addition, the cGMP increases cyclic adenosine monophosphate (cAMP) levels indirectly through phosphodiesterase III, which will also decrease the intracellular calcium concentration. The NO activated sGC ultimately results in reduced intracellular calcium, inhibition of platelet phosphoinositide 3-kinase (PI3), and reduced affinity as well as number of surface membrane fibrinogen binding sites on platelets (GPIIb/IIIa).117,121–126 It has also been suggested that many NO-related species are essential for NO’s potent antimicrobial effects. First, NO can react with superoxide (O2−)127 and form peroxynitrite (OONO−), which is a lethal oxidizing agent and can induce oxidative stress, nitrosate amino acids and thereby alter protein functionality, oxidize and break DNA strands, and cause cell membrane damage to the bacteria it comes in contact with via lipid peroxidation.20,127–129 A second possible route reported for NO mediated cytotoxicity relies upon the formation of S-nitrosothiols (RSNO) in which after oxidation of NO to N2O3 the N2O3 can react with sulfhydryl groups on cysteine residues of membrane proteins to create RSNO structures that alter protein functionality, leading to cell stasis or cell death.108 Indeed, NO released or generated from polymer matrices has been shown to have similar antiplatelet and antimicrobial effects, as further described in detail below.
Some surgery interventions or trauma that destroys the endothelial lining, as well as certain vascular diseases, will lead to an increased level of superoxide anions and that react with NO and reduce its bioavailablity.119,130 Reduced NO levels are associated with many health complications and/or diseases, such as high blood pressure, deep vein thrombosis, intimal hypertension, restenosis, endothelial dysfunction, and prolonged wound healing times in diabetic patients, etc.1,131,132 There are three main strategies for increasing NO bioavailability: 1) by participating in physical exercise and controlling certain dietary components (e.g., nitrate-rich diet);132,133 2) by administrating drugs that alter the enzymatic production of NO through nitric oxide synthases (NOSs) and increase the biosynthesis of NO endogenously;117 and 3) by using modified polymeric materials that can actively deliver NO exogenously to the sites of interest.3,109,110 Various NO-related drugs have been used in the clinical settings for many years: nitroglycerin (converted to NO by enzymes) for chest pain, sodium nitroprusside for controlling blood pressure, and molsidomine for pulmonary hypertension.131 This has triggered substantial interest in developing polymers that can be functionalized as an artificial endothelium-like surface to therapeutically deliver NO locally at the polymer/blood interface.
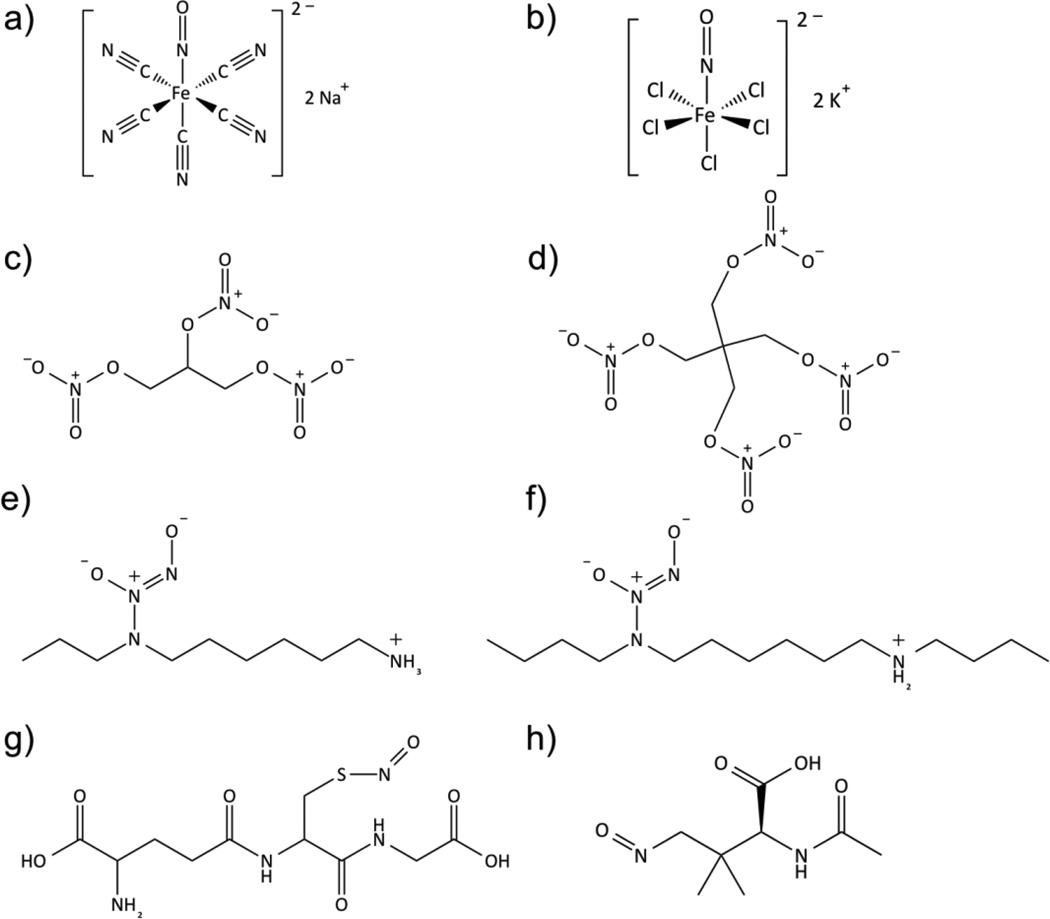
Since NO is highly active in vivo (with a short-half life on the order of seconds due to its rapid reaction with oxyhemoglobin, oxygen, and thiols, etc.), many NO donors have been synthesized and used for achieving the goal of prolonged and controlled NO delivery. Some examples include organic nitrates or nitrate esters (e.g., nitroglycerin or glyceryl trinitrate (GTN) and pentaerythrityl tetranitrate (PETN)), metal-NO complexes (e.g., sodium nitroprusside), nitrite, N-diazeniumdialates (NONOate), and S-nitrosothiols (RSNO),134–140 see Figure 4). Nitroglycerin, the most commonly used organic nitrate for clinically treating hypertension and angina pain, is known to release 1 mole equivalent of NO upon bioactivation by mitochondrial aldehyde dehydrogenase (mtALDH).111 However, patients often develop nitrate tolerance (tachyphylaxis) after prolonged use because the reactive oxygen species generated by nitroglycerin can oxidize the thiol group of the mtALDH and result in enzyme dysfunction.111,141–143 This low bioavailability limits nitroglycerin’s use as an efficient NO donor and complicates clinical treatments.
Figure 4.
Structures of commonly studied NO donors in biomedical applications, a) sodium nitroprusside; b) potassium nitrosylpentachlororuthenate; c) nitroglycerin: d) pentaerythrityl tetranitrate; e) diazeniumdiolated N-(6-aminohexyl)aminopropane; f) N,N'-dibutylhexamethylenediamine; g) S-nitrosoglutathione; h) S-nitroso-N-acetylpenicillamine.
Metal NO complexes (metal nitrosyls) represent another class of NO donors used in biological testing. Many different metal NO complexes have been reported, including manganese,108,136 iron144 and ruthenium-NO108,111,136 complexes, with sodium nitroprusside (Na2[Fe(CN)5NO], SNP) being the most common. SNP is often used as a potent vasodilator in hypertensive emergencies,144 which releases NO in the presence of reducing agents (e.g., thiol-containing compounds such as cysteine or glutathione) or by illumination with near-infrared or visible light.111,120,144 However, cellular toxicity concerns due to the release of cyanide and cytotoxic peroxynitrite as byproducts have made metal nitrosyl complexes less attractive as medicinally used NO donors.111,140
Reduction of nitrite can generate NO via both enzymatic (nitrite reductase, xanthine oxidoreductase, etc.) and non-enzymatic (gastrointestinal acid, ascorbate, myoglobin, etc.) pathways.132 Recently, it was demonstrated that nitrite can also be used to generate NO via electrochemical reduction at an electrode surface with either Cu(I) ion generated from oxidation of Cu0145,146 or via the use of Cu(II)-ligand complexes that mimic the active site of nitrite reductase (e.g., Cu(II)-tri(2-pyridylmethyl)amine, Cu(II)TPMA).147
Many researchers over the past two decades have focused on using N-diazeniumdiolates (NONOates) and S-nitrosothiols (RSNOs) as leading candidates for controlled NO delivery due to their relatively high stability, their ability to spontaneously release NO under physiological conditions (e.g., no enzyme required) in a predictable manner, and their higher bioavailability in vivo.3,120,135 Furthermore, the tissue and metabolite independent release also avoids the build-up of tolerance over time, which makes these agents more suitable for biomedical applications.
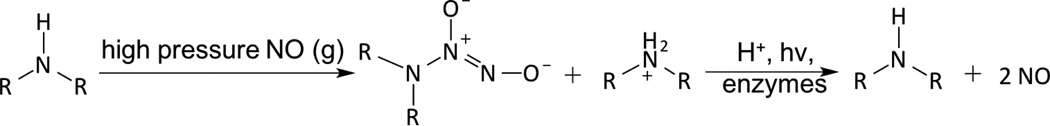
N-Diazeniumdiolates (1-amino-substituted diazen-1-ium-1,2-diolate) are a class of NO donor molecules formed by reactions between primary or secondary amines with NO under high pressure (e.g., 5 atm) in the presence of base (either an unreacted amine substrate or an added metal alkoxide base) at low temperatures.1,136 These species are able to generate two mole equivalents of NO per mole of donor, via a proton-driven reaction (hydrolysis), in the physiological environment such as when the compound is exposed to blood or tissue fluids (see Figure 5). NONOates can also release NO via thermal, photochemical or enzymatically (e.g., esterase) reactions.136,148
Figure 5.
N-Diazeniumdiolates (NONOates) formation and decomposition.
The half-lives of the synthesized NONOates strongly depend on the structure of the amine precursors and hydrogen bonding stabilization from additional amines within the molecule. It has also been reported that hydroxyl groups within the donor molecule, or the matrix it is within, can also contribute to the hydrogen bonding with the diazeniumdiolates.149,150 For example, half-lives can range from the shortest reported t1/2 of 1.8 s for the diazeniumdiolated amino acid proline (PROLI/NO) to t1/2 of 20 h for diethylenetriamine (DETA/NO).135,136 One drawback of the diazeniumdiolate compounds is that they may potentially form carcinogenic nitrosamines.151,152 Batchelor et al. synthesized more lipophilic NONOates for use in reducing the NO donor leaching into blood from polymers that had been doped with such NO donors.153 Since the NO release process produces a lipophilic amine byproduct that increases the pH of organic phase, many additive compounds (such as tetraphenylborate or other borate derivatives153) have been included within the organic polymeric phase to serve as counter ions for organic ammonium cations (when amines form after NO release and proton is extracted into the polymer to create the ammonium species) and thereby partly prevent a pH increase within the organic polymer phase. This can greatly prolong the NO release lifetime from such NO donors when incorporated into biomedical polymers. Unfortunately, the borate additives are not ideal because of their inability to extend the NO release to more than a few days and their cytotoxicity toward endothelial cells.154,155 Therefore, Handa et al.154,155 as well as Cai et al.156 studied various poly(lactic-co-glycolic acid) (PLGA) additives with different hydrolysis rates as a means to slowly produce protons within the organic polymer phase that can continue to drive NO release reaction from NONOates. PLGA is a biocompatible and biodegradable polymer, with tunable mechanical properties and wide range of erosion times. Further, it is already approved for use by the FDA for the development of devices for controlled delivery of small molecule drugs, proteins and other macromolecules.157 These studies demonstrated that the presence of PLGAs in the base polymer containing diazeniumdiolate species can extend NO release under physiological conditions for up to at least 2 weeks.
S-Nitrosothiols (RSNO) represent an endogenous class of NO donors and natural transporters of NO within tissues and blood.120,158 Such molecules include S-nitrosoalbumin (SNO-Alb), S-nitrosohemoglobin (SNO-Hb), S-nitrosocysteine (SNO-Cys) and S-nitrosoglutathione (GSNO).159 RSNOs can be synthesized via the thiol nitrosation reaction (such as nitrous acid and alkyl nitrite, etc. in the acidic environment).140 Owing to the natural occurrence of RSNOs in vivo, these molecules pose a relatively low risk of toxicity to cells/tissues in comparison to NONOates. The transnitrosation reaction transfers the NO+ functional group from an RSNO species to another existing free thiol, thus achieving a circulating unlimited supply of NO in vivo.160
RSNOs have characteristic UV-Vis spectra. In general, they appear green for tertiary RSNOs (such as S-nitroso-N-acetylpenicillamine, SNAP) or pink for primary and secondary RSNOs (such as SNO-Cys, S-nitroso-N-acetylcysteine (SNAC) and GSNO). There are two primary bands in the UV-Vis spectra. The strong band in the UV region is between 330 and 350 nm (ε~103 M−1 cm−1), which is attributed by the n0 → π* transition.140,161–163 A weak band in the visible region is between 550 to 600 nm (ε~20 M−1 cm−1), which is attributed to the nN → π* transition.140 It is known that RSNOs can release NO via multiple pathways.163–168 Thermal or photo-initiated decomposition will lead to homolytic cleavage of the S-N bond, and form thiyl and NO radicals, where thiyl radical (RS•) will react with another RSNO and generate disulfide (RSSR) and another NO radical. Metal ions (such as copper or ferrous ions)169,170 or organoselenium compounds can catalyze RSNO decomposition.114,171–173 It is reported that Cu+ (generated from reduction of Cu2+ by trace amounts of thiol) can react with RSNO and form the corresponding thiolate and Cu2+, which then react to regenerate Cu+ and a disulfide to continue the catalytic cascade. RSNOs can also react with ascorbate to generate NO via two pathways. In one, ascorbate (at low concentration) acts as a reducing agent to generate Cu+ from trace copper ion impurities in solution, or at high concentration ascorbate can act as a nucleophile, attacking the nitroso group to generate NO, a thiolate and dehydroascorbate.8,174,175 Further, certain enzymes such as copper-containing superoxide dismutase (CuZn-SOD)140,176 or the selenium-containing enzyme glutathione peroxidase (GPx)140,171,173 can also convert RSNO to NO in the presence of a reducing agent, such as glutathione (GSH) (see Figure 6).
Figure 6.
S-Nitrosothiol (RSNO) formation and decomposition.
GSNO and SNAP are two commonly used RSNOs that have been intensively studied in a variety of biomedical applications. GSNO is present in blood endogenously, which makes it innately more biocompatible and attractive for many applications, such as promoting wound healing process in mice or rats.177–180 The precursor for SNAP synthesis is N-acetylpenicillamine (NAP), whose ultimate hydrolysis product, penicillamine, is already a FDA approved chelator for treating heavy metal poisoning, such as Wilson’s disease.181–184 SNAP is reportedly one of the most stable NO donors available, due to its intermolecular hydrogen bonding,162,185 and has already been shown to be a very promising candidate for fabricating long-term NO releasing polymeric materials.161,162,186 Lipophilic analogs of SNAP (such as N-substituted derivatives of SNAPs) have also been developed by addition of bulky side-chains to N-acetylpenicillamine and preventing Cu+ catalysis through steric hindrance.187,188 Other lipophilic RSNOs (S-nitroso-tert-dodecyl mercaptan (SNTDM), log P = 5.3)189 (note: P = partition coefficient of a molecule between octanol and water) with a higher Log P value than SNAP (log P = 0.4)162 have been synthesized for reducing the NO donor leaching from the hydrophobic polymer phase.
Polymer-Based Strategies for NO Delivery
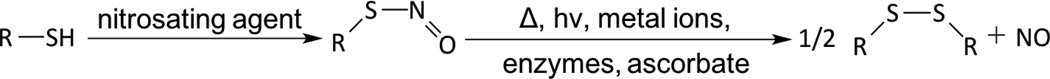
For the past two decades, many research groups have focused on developing techniques to deliver NO locally, continuously and efficiently from polymeric devices where blood clotting and/or bacteria infection are major complications. To improve the NO payload and stability, achieve targeted NO delivery through multi-functionalization and elongate NO releasing lifetime, many different scaffolds have been used as NO-releasing or NO-generating vehicles. These include micelles,138,190,191 microbubbles,192 proteins,193–197 liposomes,126,198 inorganic nanoparticles (such as silica,70,199–203 gold,204,205 microparticles,198,206 zeolites,207,208), metal-organic frameworks (MOFs),209–212 dendrimers,71,213,214 xerogels,215–217 electrospun fibers,88,100,218 natural polymers (chitosan,85–87,219–221 gelatin,222 etc.), and other organic polymers (polymethacrylate,223 polyester,224,225 polydimethylsiloxane (PDMS),226 polysaccharides,227,228 hydrogel,178,179,229,230 PVA,49,231,232 polyurethanes,161,162,233,234 and PVC154). The approaches and benefits of different NO-delivery materials have been highlighted in numerous reviews.1,111,120,131,135–138,235 Here, an overview of the most promising polymer-based NO delivery strategies are discussed, including covalently bound NO donors within/on a polymer matrix, physically dispersed NO donors within a polymer matrix, and catalytically generated NO from various RSNO reservoirs in the body (see Figure 7), and their representative examples in antithrombotic and antibacterial applications are described.
Figure 7.
Three different strategies to fabricate of polymer surfaces that release or generate NO, including physical dispersion of NO donor into polymeric matrix, covalently bound NO donor functionalities onto polymer backbone, or NO generation from endogenous RSNO species in blood by metal catalysts embedded in or covalently bound to the surface of the polymer.
Covalently Bound NO Releasing Polymers
N-Diazeniumdiolates are the most studied NO donors, and many polymers with secondary amine groups have been chemically modified to create the NONOate moiety.109,110,136 Meyerhoff and coworkers were among the first to link these NO donors to particle fillers (such as fumed silica particles236) or to the polymer backbone of polymers such as PVC,34,237 polyurethane (PU),34,110,233 and silicone rubber (SR).238 Zhang et al. synthesized NO-releasing fumed silica particles (0.2–0.3 µm) by tethering alkylamines onto the surface of the FS particles using amine-containing silylation reagents (coupling efficiency 50–70 %), and then converted them to corresponding NONOate groups with final NO loading of ca. 0.6 µmol/mg of particle.236 The half-lives of the particles are significantly longer than the solution phase NO donor analogs, owing to the fact that a large quantity of amines present at the particle surface can increase the local pH, which then reduces the NO release rate. Of note, when local pH decreases significantly, it results in partial release of the stored NO due to the proton-driven NO release mechanism. Therefore, some methods utilize additional acid-generating compounds to facilitate continual release of the entire NO payload.
Keefer and coworkers were one of the earliest groups to covalently attach a diazeniumdiolate species to the backbone of poly(ethylenimine) (PEI) to form PEI/NONOate, which later was used to provide a flexible NO release coating for PTFE vascular grafts.239 The NO release from the sample was at a relatively constant rate (0.5 pmol min−1 mg−1) for 5 weeks in PBS buffer at 37 °C. In subsequent studies, Saavedra et al. prepared methoxymethyl-protected diazeniumdiolated piperazine PVC;237 however, the NO release rate was slow due to the fact that the NO could only be released from the NONOate group after the hydrolysis of the methoxymethyl protecting group.34 In addition, this PVC film can concurrently release toxic methanol and formaldehyde as byproducts of the methoxymethyl-protecting group, which is undesirable for use as materials in biomedical applications. Zhang et al. later incorporated diazeniumdiolated functionalities into more biocompatible silicone rubber.238 Briefly, the diaminoalkyltrimethoxysilane (DACA) was reacted with the terminal hydroxyl groups of the PDMS, and then the aminated PDMS macromolecules were cross-linked to each other (condensation-curing) in the presence of ambient moisture before forming the NONOates species at the amine sites (via reaction of the polymer with NO(g) at high pressure). Likewise, N-diazeniumdiolated NO donors have been covalently linked to polyester,240 polymethacrylate,223 polyurethane (PU),35,110,233,234 PVA232 and other hydrogels241 as well. The synthetic methods are somewhat similar to that described above, with the exception of one type of PU containing a diamine chain extender, where sodium salts (NaX, where X is an anion) are incorporated into the reaction mixture during the NO addition process to facilitate the formation of anionic diazeniumdiolates.110
Dendrimers are another class of popular NO delivery vehicles due to their ability to store a large reservoir of NO, have tunable sizes, and to be multi-functionalized for targeted delivery.214,242 Stasko et al. were the first to modify generation 3 and 5 polypropylenimine dendrimers at their exterior with different amine functionalities that were then converted to diazeniumdiolated dendrimers via reaction with NO(g) at high pressure. The secondary amine/NONOates yield the highest storage capacity for NO, with up to 5.6 µmol NO/mg of polymer, and a NO release duration of >16 h under physiological conditions.242
Frost et al. was the first to modify fumed silica (FS) particles (7–10 nm in diameter) with an RSNO functionality,199,200 such as S-nitrosocysteine-FS (SNO-Cys-FS), S-nitroso-N-acetylcysteine-FS (SNAC-FS) and S-nitroso-N-acetylpenicillamine-FS (SNAP-FS). This was accomplished, by tethering the thiol containing amino acids or N-acetylpenicillamine thiolactone onto aminopropyl-FS. In these efforts, a total NO loading of up to 1.38 ± 0.29 × 10−7 mol NO/mg particles was achieved. The SNAC-FS and SNAP-FS particles can be blended into polyurethane (PU) or trilayer silicone rubber (SR) matrixes to create films that release NO at different rates by tuning the chemical identity, water uptake, or thickness of the PU polymer.200 However, the SR films containing SNAC-FS or SNAP-FS in the middle layer do not release NO upon exposure to copper ions or ascorbate in PBS solution because the very high hydrophobicity of the SR blocks the contact between the buffer and the RSNOs.199 However, such films are able to release NO at levels proportional to the intensity of visible light that is allowed to shine on the polymer, providing the first hydrophobic materials that have an external on/off trigger that precisely controls the rate of NO release via a photodecomposition reaction. The authors determined that 590 nm light is primarily responsible for the release of NO from the SNAP-FS-SR films. Evidence suggested that 67 % of the photoinitiated NO was accounted for by the longer wavelength (590 nm) and 33 % by shorter wavelengths (centered around 340 nm). SNAP has also been covalently attached to PDMS,226 gelatin222 and a macrocycle (e.g., cyclam).243 The ability to generate programmable sequences of NO flux from these light-sensitive materials can offer precise spatial and temporal control of the NO release and potentially provides a platform to systematically study, at a fundamental level, the in vivo physiological response to implanted devices.226 Of note, SNAP-cyclam is capable of releasing physiological relevant levels of NO for up to 3 months in vitro when blended into poly(L-lactic acid) thin films, and this represents the longest NO release from SNAP-based polymer films reported to date.243
RSNOs have also been used to form functionalized dendrimers213 or hyperbranched polymers (e.g., hyperbranched polyamidoamine (HPAMAM) or hyperbranched polyethers240) to achieve a high NO payload. Stasko et al. functionalized generation 4 polyamidoamine (PAMAM) dendrimers with N-acetylpenicillamine or N-acetylcysteine and both macromolecular scaffolds have an NO storage of ca. 2 µmol NO/mg polymer after the required nitrosation raction.213
Another category of NO delivering materials with large NO storage capabilities are xerogel films. Riccio et al. designed thiol-modified xerogels derived from 3-mercaptopropyltrimethoxysilane (MPTMS) and methyltrimethoxysilane (MTMS).216 The subsequent thiol nitrosation generates xerogels with NO loadings up to 1.31 ± 0.07 µmol NO/mg, and films of these materials are capable of releasing NO for up to 2 weeks under physiological conditions. Similar to N-diazeniumdiolates, many other polymer modification studies have been conducted using S-nitrosothiols (RSNOs) as well, including those utilizing PDMS,226 PVA hydrogel,179 polyester and poly(methylmethacrylate),224 as the base polymer materials.
Lastly, several biodegradable polymers, such as citrate-based225 or saccharide-based polymers (e.g., dextran227,244 and chitosan86,87,220) provide very attractive scaffolds for NO delivery because of their natural occurrence, biodegradability, tolerability to mammalian cells and accessibility for NO donor functionalization reactions.220,244,245 Reynolds and coworkers synthesized two S-nitrosated dextran thiomers (dextran-cystamine and dextran-cysteine), with up to 0.205 ± 0.003 µmol/mg NO loading and the capability to release NO for 6 h in PBS buffer at 37 °C. It has been further demonstrated that these dextran-based materials are susceptible to enzymatic degradation by dextranase, and the degradation of dextran derivatives is slower and partial when compared to the unmodified dextran because of the chemical modification of the dextran backbone.244
Physical Encapsulation-based NO Releasing Polymers
Physical encapsulation methods for preparing NO releasing polymers are based on embedding the NO donor within a polymer matrix physically without chemical bonding. This provides a much less complicated method to prepare NO release polymers than covalent attaching NO donors to particle fillers or the polymer backbones. This approach is a more attractive strategy for future commercialization if stable long-term NO release can be achieved by dispersing the NO donor within a polymer matrix. Toward this goal, polymer192 or phospholipid246 shelled microbubbles have been developed in recent years to create a hydrophobic microenvironment for NO transportation and therapeutic delivery. Paradossi and co-workers prepared NO-loaded PVA-shelled microbubbles (4.6 µm ± 0.4 µm diameter and 0.4 µm shell thickness) for treating acute vascular disease, such as thrombosis.192 The microbubbles were loaded with NO by exposing to gas phase NO at 1.5 bar for 2 h. The NO encapsulation is about 1% of the NO present in the reaction vessel during the loading procedure, with the final content being 3.6 µmol/mg microbubbles. The NO release measured by the Griess assay showed that ca. 90% of the NO is released during a 50 min period in phosphate buffer saline solution. Ideally, the NO delivery should be controlled and selective bursts at a specific time and place, but the release can also be spontaneous and nonspecific.192 Unfortunately, the in vitro stability of such NO-loaded microbubbles is relatively low.246
Gas storage in porous materials, such as zeolites, is also another attractive method for medicinal applications. Wheatley et al. have used cobalt-exchanged zeolite-A to absorb and store NO (1.2–1.3 µmol NO/mg zeolite). The NO release was triggered by contacting with water at physiological temperature and pH, replacing the gaseous NO with cobalt-water interactions. These NO-zeolite samples were also blended with powdered PTFE or PDMS to increase their mechanical stability and then pressed as disks for in vitro testing. The t½ values of NO release from zeolite polymer disks was significantly increased (from 340 s for zeolite powder to 509 s for PTFE disk and 3076 s for PDMS disk).207 The results obtained in a platelet aggregometry assay also suggested that the NO-zeolites greatly inhibits platelet aggregation in vitro.
Liposomes are also a popular choice to protect and deliver gaseous NO. Mcpherson and coworkers prepared liposomes encapsulated with NO and argon gas (NO/Ar-ELIP) by a pressured-freeze and thawing method. They used these capsules for attenuating intimal hyperplasia and reducing arterial wall thickness.198 Other researchers have conducted further studies to encapsulate NO donors within pH126 or thermo-sensitive247 liposomes to achieve controlled release. In short, when N-diazeniumdiolates are encapsulated within liposomes, pH or temperature fluctuations change the proton influx through the biolayer membrane and subsequently induce a significant NO release. Koehler et al. have also encapsulated SNAP within liposome vesicles and then doped the resulting vesicles within xerogels for photosensitive NO release.248
Biodegradable poly(ethylene oxide-co-lactic acid) (PELA)249 and poly(lactic-co-glycolic acid) (PLGA)206,219,249 have also been shown to be suitable vehicles for encapsulating NO donors to prolong the NO release. Yoo and coworkers developed PLGA (5050DLG5E) nanoparticles (NO/PPNPs) with diazeniumdiolated polyethylenimine (PEI) for long term NO release for antimicrobial applications.219 The average size of the NO/PPNPs was 162 ± 19 nm as confirmed by scanning electron microscopy (SEM), with a NO release capacity of 1.4 µmol NO/mg polymer. The incorporation of PEI/NONOate into hydrophobic PLGA nanoparticle matrix successfully restricts the spontaneous degradation of the NONOate group and extends the NO release lifetime from 12 h to over 6 d.219 More recently, Lautner et al. demonstrated the encapsulation of SNAP into PLGA (RG 503H and RG 504) microspheres (20–125 µm in diameter) using a solid-oil-in water (S/O/W) method250 and achieved up to 4 weeks of controlled release of SNAP from PLGA RG 504, which then generates localized NO in the presence of copper (II) and ascorbate.206
Mowery et al.34 prepared diazeniumdiolated N,N-dimethyl-1,6-hexanediamine (DMHD) or linear PEI and dispersed them into plasticized PVC or PU. Unfortunately, NO donor leaching was observed by HPLC and this raises potential concerns regarding toxicity if nitrosamine formation occurs, and such nitrosamines are also leached into the surrounding aqueous environment. Bachelor et al.153 synthesized more lipophilic dialkylhexamethylenediamine-based NONOates with different alkyl groups (from methyl to didodecyl) which can enhance the retention of potential byproducts within the hydrophobic PVC films and thereby reduce their toxicity threat to biological systems.
Seabra et al. incorporated GSNO and SNAC into Synperonic F-127 gel using a ‘cold method’251 and formed a hydrogel that contained 0.3 mol of GSNO or 0.6 mol of SNAC per gram of hydrogel.251 Kinetic studies showed that SNAC releases NO thermally 3.6 times faster than GSNO (11 ± 0.4 min−1 vs. 3.1 ± 0.8 min−1); however, approximately 50% of both NO donors had decomposed after only 3 h.231 Kim et al. developed NO-releasing films by dispersing GSNO into biopolymer chitosan, where 75% GSNO remains after storing at room temperature for 4 weeks. The 20 wt% GSNO/chitosan film released NO over 48 h in PBS buffer at 37 °C.221 Recently, Brisbois et al. discovered that SNAP is exceptionally stable when doped within several low water uptake biomedical grade polymers, such as Elast-eon E2As and CarboSil, and can release NO for up to 3 weeks at physiological conditions.155,161 Wo et al. later demonstrated that the SNAP in CarboSil mainly exists in crystalline form when the SNAP concentration exceeds its solubility in the polymer. Ultimately, a slow crystal dissolution process leads to its long-term NO release under physiological conditions.162 Additionally, this crystal-polymer composite is very stable during storage for at least 8 months, not only because of the hydrophobicity of the CarboSil polymer that limits water diffusion primarily to only the polymer surface, but also because the crystalline SNAP is stabilized by intermolecular hydrogen bonds.162,252
In order to apply NO release to any pre-made or off the shelf biomedical devices, Colletta et al.19 developed a simple solvent impregnation method to load SNAP into commercially available silicone Foley urinary tract catheters at room temperature. This impregnation process takes place under very mild conditions, which is beneficial because, like many NO donors, SNAP or its analogs are sensitive to high temperatures used during industrial catheter extrusion processes. In this approach, SNAP or a SNAP analog is dissolved in an organic solvent that can swell the polymer to a great extent without dissolving it, and as the polymer uptakes the solvent, the NO donors are loaded into the polymers. After drying to remove the solvent, the resulting polymer contains a stabilized form of the SNAP or analog of SNAP. As an initial example, commercial silicone Foley catheters (i.d. of 0.30 cm and o.d. of 0.59 cm) were swelled in a SNAP solution prepared in tetrahydrofuran (THF) (125 mg/mL) for 24 h, resulting in SNAP impregnation of 5.43 ± 0.15 wt% SNAP in the final dried catheter. This level of SNAP loading enabled the catheters to achieve stable NO release above physiological levels for > 4 weeks.19
Catalysis-Based NO Generating Polymers
Instead of incorporating NO donors or NO functionalities into polymers, many efforts have been devoted to generate NO from endogenous RNSOs or infusion of RSNO solutions through thiol transnitrosations,160,253 and subsequent catalytic reactions using immobilized copper or selenium-based species (e.g., copper nanoparticles,254 copper(II)-cyclen,170,255 copper-complexes,256,257 copper-containing metal-organic frameworks (MOFs),209–212 and organoselenium species114,171–173). Meyerhoff and coworkers were the first to covalently attach copper(II)-cyclen onto commercial biomedical grade polyurethane, which can generate physiological levels of NO (1–2 × 10−10 mol cm−2 min−1) when in contact with endogenous RSNO and RSH species, such as 10 µM GSNO/GSH in PBS buffer containing 3 µM EDTA.170 This polymer has also been used as an outer coating at the distal end of an amperometric NO sensor that can generate electrochemical response toward the RSNO species in whole blood.170 However, it was reported that 50 % of copper(II) ion leached out after soaking in GSNO/GSH containing PBS buffer at RT for 7 d, which may limit the use of such polymers for long-term applications and generate cytotoxicity concerns.
Reynolds and coworkers are developing many MOF-NO generating catalysts with accessible catalytic sites and that have resistance to degradation, including Cu3(BTC)2 (BTC: 1,3,5-benzenetricarboxylate), Cu(II)1,3,5-benzene-tris-triazole (CuBTTri) and Cu(II)1,3,5-tricarboxylate (CuBTC).210–212 It has been reported that CuBTC can be extruded within Tecoflex SG80A polyurethane into single lumen tubing while maintaining the catalyst structure and functionality. The in vitro NO release generated from endogenous RSNO species ranges from 1 h to 16 h with tunable dosage, depending on the specific RSNO levels present in the soaking solution.210
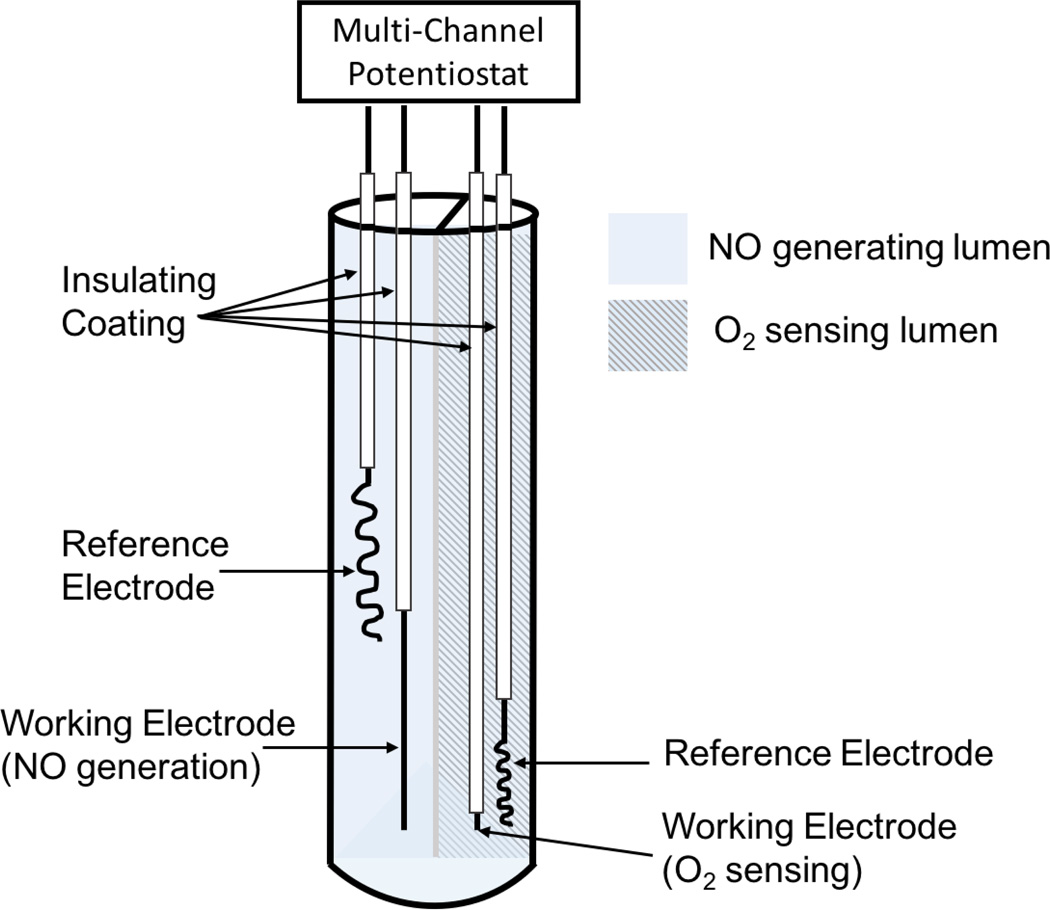
As previously mentioned, Meyerhoff and coworkers have also demonstrated an electrochemical NO generation through a Cu+ ion mediated reduction reaction of inorganic nitrite. The Cu+ ion is generated from oxidation of a copper wire145,146 or the reduction of copper(II)-tri(2-pyridylmethyl)amine (Cu(II)TPMA) complex.147 The electrochemically generated NO can be modulated by changing the potentials applied to the electrodes and can achieve between 0.5 and 3.5 × 10−10 mol cm−2 min−1, which is in the range of physiological relevant levels of NO released by the endothelial cells. This approach has been utilized to develop a new generation of multi-lumen catheters in which one lumen is dedicated to generating NO electrochemically to reduce thrombus and microbial biofilm formation on the surface of the catheters.147,258
Applications of NO Releasing/Generating Polymers for Preparing Antithrombotic and Antibacterial Biomedical Devices
Inhibition of Thrombosis Formation
In a healthy vasculature, endothelial NOS (eNOS) in the endothelial cells that line the inner wall of blood vessels produce NO with a surface flux of 0.5 – 4.0 × 10−10 mol cm−2 min−1 to prevent platelet activation and thereby control the balance between thrombosis and hemorrhage.119 However, many procedures (such as placing stents, grafts, catheters, or other biomedical devices) disrupt the endothelial cells lining and destroy the delicate balance of vascular homeostasis.132 The tissue factor release and protein absorption trigger the coagulation cascade and the lack of NO production leads to platelet activation, aggregation, and ultimately thrombus formation. Therefore, NO and its unique antiplatelet/antithrombotic activity represents a very promising approach to prevent thrombus associated complications in many biomedical applications.
Mowery et al. reported that PVC- or PU-based polymer films, prepared with NO releasing diazeniumdiolate functionality via either dispersion or covalent bonding of NO donors, can exhibit significant improvements in biocompatibility during in vitro platelet adhesion tests using platelet-rich plasma (PRP).34 Wu et al. prepared PVC films (with borate additives and di(2-ethylhexyl) ester (DOS)) mixed with 0.5, 1.0, 2.0, 4.0 wt% of diazeniumdiolated N,N’-dibutyl-1,6-hexanediamine (DBHD/N2O2) to determine the effect on platelet adhesion at the surface of polymeric films with various NO flux levels.259 A lactate dehydrogenase (LDH) assay was used to determine the amount of platelets adhered onto the polymer surface. LDH, which is normally stored within intact platelet, is released into the bulk solution when the platelets are lysed by surfactant and is a very useful for indication of the amount of cells adhered.259 Fewer platelets adhered on the polymer surfaces with higher NO flux levels, and NO successfully reduced the amount of platelets adhered on the polymer surfaces from 14.0 ± 2.1 × 105 cells/cm2 on the controls to 2.96 ± 0.18 × 105 cells/cm2 on the surfaces with highest NO release of 7.05 × 10−10 mol cm−2 min−1.
Thrombosis is also an important risk factor in any blood exposure to synthetic materials, such as grafts, stents, intravascular sensors, catheters, extracorporeal circuits (ECC) or hemodialysis membranes.119,120,260,261 Efforts to use NO release polymers for these applications are summarized below based on the type of biomedical device.
a) Intravascular Grafts
Keefer and coworkers were the first to test the antithrombotic and antiplatelet activity of NO released from a polymer matrix in animal models.239 Diazeniumdiolated cross-linked PEI coated PTFE vascular grafts were inserted into silicone rubber shunts that were placed between baboons’ femoral and artery veins for 1 h. The autologous baboon platelets were labeled with indium-111-oxine before the start of experiment. The number of platelets adhered on the graft surface at the end of experiment was accessed by measuring the radioactivity intensity using a gamma scintillation camera. The NO-releasing grafts were found to be substantially less thrombogenic than the controls, suggesting considerable promise for this approach to improve the performance of vascular graft after implantation.239 The West115 and Wang114 groups both reported that NO releasing/generating grafts encourage endothelialization/endothelial cell proliferation, which can alleviate the complications of thrombosis and intimal hyperplasia (IH) that cause the failure of small diameter vascular grafts without the use of systemic anticoagulants.
b) Intravascular Sensors
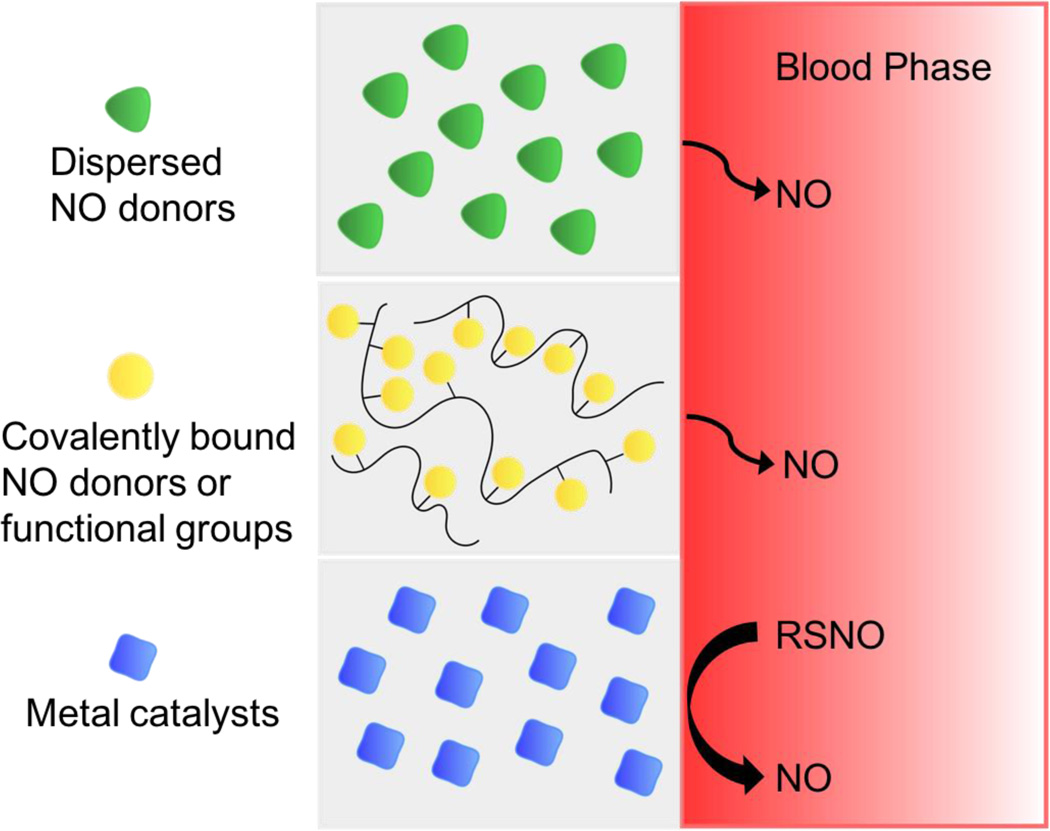
Monitoring the levels of chemical species in blood (such as blood gases (PO2, pH, and PCO2), electrolytes (K+, Na+ Ca2+), glucose, lactate, etc.) can provide invaluable information for diagnosis and treatment of hospitalized patients.262 Currently, however, measurements are done in vitro with point-of-care devices intermittently, leaving large gaps of information between blood draws.258,263 Therefore, developing intravascular sensors that can monitor key chemical species in real time in critically ill patients is an important avenue of research.264 However, adhesion of platelets, and eventual thrombus formation on the surface of the sensors can occur within a few hours after blood contact, and such processes can not only isolate the chemical sensing area from the bulk of the blood and lead to false analytical results but also increase the risk of emboli or stroke.8,265 Many researchers have attempted to address this problem by incorporating continuous NO release/generation into the sensor design to prevent adhesion of metabolically active platelets from adhering to the sensor surface. To increase the biocompatibility of intravascular oxygen sensors, Marxer et al. developed an amperometric sol-gel derived oxygen sensor that consists of a platinum electrode coated with a diazeniumdiolate and polyurethane containing xerogel film.266 The coating released NO at a flux up to 4.32 × 10−10 mol cm−2 min−1 for the first 12 h and effectively reduced platelet adhesion in the in vitro biocompatibility testing when immersed in platelet rich plasma for 1 h at 37 °C. Instead of directly coating the electrodes with NO release polymers, many catheter-style intravascular oxygen sensors have been developed for testing in vivo with NO released or generated through the polymeric material of the catheters. So far, several different NO delivery approaches have been reported for such intravascular oxygen sensors, including coating catheter surface with NONOates,267,268 covalently attaching NONOates to catheter polymer surface,269 catalytically generating NO in situ from endogenous RSNOs using embedded copper particles8,270 and electrochemically modulating NO generation from nitrite.258 For example, Schoenfisch et al. coated outer surfaces of SR catheters with 2 wt% (Z)-1-[N-methyl-N-[6–(N-methylammoniohexyl)amino]] diazeniumdiolate (MAHMA/N2O2) and demonstrated that the NO release from the catheter lasted more than 20 h in PBS at 37 °C. One control (coated only with MAHMA) and one NO release catheter (coated with MAHMA/N2O2) were implanted within the carotid or left femoral arteries in a canine model for 12–23 h. The electrochemical response of the NO-releasing O2 sensor more closely represented the real arterial blood gas value measured by a benchtop blood-gas analyzer than the control sensor, which had a significant discrepancy starting from the first few hours after the implantation. SEM images also confirmed that a much greater number of platelets adhered and aggregated on the surfaces of the control sensors compared to the NO releasing sensors. In a separate study, Ren et al. recently demonstrated the use of a dual lumen catheter configuration to combine an amperometric oxygen sensor (in one lumen) with the electrochemical NO generation in the other lumen using Cu(II)TPMA as the mediator for reduction of nitrite ions to NO258 (see Figure 8).
Figure 8.
Simplified schematic of dual-lumen catheter-type oxygen sensor with electrochemical NO generation from nitrite solution via Cu(II)TPMA (figure not drawn to scale).
Applying different potentials on the electrodes can modulate the rate of NO generation, which offers a steady, controllable, and physiologically relevant flux of NO, compared to the chemically-based NO generation. The performance of the sensor was evaluated in rabbit veins and pig arteries for 7 and 21 h, respectively. The sensors in the arteries were challenged with a wider range of oxygen levels by changing the pig’s fraction of inspired oxygen between 100 % and 21 %.258 In both cases, the sensors with electrochemical NO generation provided very accurate oxygen responses, while control sensors deviated from the real values by 30–40 % after 5 h of implantation because the local oxygen was consumed by the activated platelets and other cells trapped in the thrombus formed on the surface of the control sensors. Similar to oxygen sensors, NO releasing intravascular glucose,271–275 pH,275,276 and CO2275,277 sensors using diazeniumdiolated NO donors have also been tested, demonstrating much improved electrochemical responses over the corresponding control sensors.
c) Extracorporeal Circulations (ECCs)
Extracorporeal circuits are used for several different types of medical procedures, such as hemodialysis, cardiac bypass surgery, and extracorporeal membrane oxygenation (ECMO). The latter is employed to keep newborn babies alive for weeks at a time, if their lungs are not fully developed. The need for systemic anticoagulation in each of these extracorporeal procedures can be problematic, particularly in patients that have heparin induced thrombocytopenia (HIT). Due to the large surfaces area that is in contact with blood in extracorporeal circulation (ECC), the loss of platelet count and platelet functionality are significant,161 and many researchers have developed NO releasing43,154,155,161,236,238,278,279 or NO generating254 polymeric ECC tubing to prevent platelet activation and consumption during this process (see Table 1).
Table 1.
Summary of NO releasing and NO generating coatings reported to increase the hemocompatibility of extracorporeal circuits (ECC).
| Summary | ECC coating material | NO donor, additives, etc. |
NO level (× 10−10 mol min−1 cm2) |
Platelet count after 4 h (% of initial) |
Ref | |
|---|---|---|---|---|---|---|
| NO release |
covalent attachment |
Tygon tubings with Carbonthane 3573A coating |
N-diazeniumdiolated FS fillers |
4.1 | ca. 85 ± 15 % (NO) vs. 58 ± 5 % (PU) |
236 |
| Silicone rubber tubings |
N-diazeniumdiolated PDMS |
>4.0 at 23 °C; >10.0 at 37 °C |
86 ± 24 % (NO) vs. 65 ± 10 % (SR) |
238 | ||
| physical dispersion |
Tygon tubings with PVC/DOS coating |
DBHD/NONOate, borate |
12.5 | 79 ± 7 % (NO) vs. 58 ± 7 % (PVC/DOS) |
278 | |
| Tygon tubings with PVC/DOS coating |
DBHD/NONOate, PLGA |
>20 | 79 ± 11 % (NO) vs. 54 ± 6 % (PVC/DOS) |
154 | ||
| Tygon tubings with Elasteon-E2As coating |
DBHD/NONOate, PLGA |
6 | 97 ± 10 % (NO) vs. 58 ± 3 % (E2As) |
155 | ||
| Tygon tubings with Elasteon-E2As coating |
DBHD/NONOate, PLGA, argatroban |
6.5 | ca. 90 % (NO/argatroban) vs. 58 ± 3 % (E2As) |
43 | ||
| Tygon tubings with Elasteon-E2As coating |
SNAP | 2 | 100 ± 7 % (NO) vs. 60 ± 6 % (E2As) |
161 | ||
| NO generation | Tygon tubings with Tecophilic SP-60D-60 coating containing 10 wt% Cu0 nanoparticle |
endogenous RSNO and/or infused SNAP |
>10 (in presence of 1 µM GSNO, 30 µM GSH, 5 µM EDTA) |
ca. 90% (10 wt% Cu0 and SNAP) vs. 75 % (10 wt% Cu0 only) vs. 50 % (SNAP only) |
254 | |
| Inherent polymer properties |
Tygon tubings with Tecoflex SG 80A, Tecophilic SP-60D-60, PVC/DOS coating |
N/A | N/A | 44 ± 4 % (SG 80A) vs. 41 ± 5 % (SP-60D-60) vs. 46 ± 3 % (PVC/DOS) |
155 | |
Zhang et al. prepared PVC tubing with PU coating containing 20 wt% diazeniumdiolated FS particle fillers236 and SR tubing with covalently attached to DACA/N2O2238 as NO releasing polymer tubing circuits for 4 h ECC experiments in a rabbit model. Both types of NO release tubing exhibited less overall platelet adhesion and thrombus surface coverage compared to the controls. However, it still remains a challenge to achieve long-term NO release at physiologically relevant conditions, stable storage capability at room temperatures and high NO donor loading. Handa et al. recently prepared ECC tubing composed of 25 wt% DBHD/N2O2 and 10 wt% PLGA (5050DLG7E) additives in 2:1 PVC/DOS polymer matrix and achieved up to 14 d of NO release between 7–18 × 10−10 mol cm−2 min−1 at 37 °C.154 This circuit tubing successfully preserved the platelet count during 4 h of experiments, with 79 ± 11 % vs. 54 ± 6 % for the NO release circuits compared to PVC/DOS controls. In a subsequent study by the same authors, four different biomedical grade polymers were evaluated for their inherent hemocompatibility in 4 h ECC experiments in rabbits.155 The type of polymer material can ultimately influence their efficiency as NO releasing coatings. E2As polymer was found to be the most biocompatible material amongst the four tested. E2As coated ECC tubing can preserve 56% of baseline platelet after 4 h versus 48, 40 and 47 % for PVC/DOS, Tecophilic SP-60D-60 and Tecoflex SG 80A, respectively. Major et al. later used E2As polyurethane with DBHD/N2O2 and a direct thrombin inhibitor argatroban (AG) as an ECC coating to better mimic the vascular endothelium. The results showed that the combined AG/DBHD polymer coatings can better prevent thrombus formation after 4 h of blood exposure compared to control ECCs or ECCs with coatings containing only DBHD/N2O2 or AG alone.43
In addition to diazeniumdiolates, RSNOs has also been used to create NO releasing coatings for ECC applications. Brisbois et al.161 were the first to discover that SNAP-doped E2As polymer films exhibit unprecedented shelf-life stability, with 82 % of the initial SNAP remaining after 2 months storage at 37 °C. The 10 wt% SNAP/E2As films can release NO for up to 20 d at levels above the physiological NO flux range. In the ECC experiments with rabbits, the inner walls of PVC ECC circuits were coated with the SNAP/E2As polymer. Such coated tubing successfully preserved the platelet count during the 4 h of experiments (at 100 ± 7% % vs. 60 ± 6 % for controls), with 33 % less thrombus formation on the tubings’ inner surfaces.
Another related approach to increase the biocompatibility of ECC tubing is to generate NO catalytically using infused RSNOs.254 Hydrophilic SP-60D-60 polyurethane polymer containing 10 wt% Cu0 nanoparticles (NP) (80 nm) coated on the inner walls of ECC circuit tubing were tested in the rabbit thrombogenicity model. Experiments were conducted with and without intravenous SNAP infusion (0.1182 µmol/kg/min) over a 4 h period. The Cu0 NP embedded ECC circuit with SNAP infusion yields considerably less thrombus (0.4 ± 0.2 pixel/cm2) on the surface of the chamber after 4 h, as compared to the Cu0 NP circuit without SNAP infusion (3.2 ± 0.2 pixel/cm2) or the control circuit without Cu0 NP (4.9 ± 0.5 pixel/cm2). Of note, since the endogenous RSNO levels are low (e.g., 1–10 µmol/L for SNO-albumin),280 this approach requires consistent supply of infused RSNOs to provide continuous catalytic generation of NO at the flowing blood/polymer tubing interface.254
Prevention Bacterial Infection or Biofilm Formation
Nitric oxide (NO) has antimicrobial activity against a growing list of microorganisms, including bacteria, fungi, parasites, viruses, and yeast.20,111,120,127,177,281,282 However, for medical device applications, the focus has thus far been on its antibacterial/antibiofilm properties, especially for the bacteria that most commonly cause CRBSIs (catheter related bloodstream infections), such as Staphylococcus epidermidis (S. epidermidis), Staphylococcus aureus (S. aureus), and Pseudomonas aeruginosa (P. aeruginosa).66,103 It has been clearly demonstrated that NO releasing/generating polymers can have strong bactericidal effects,19,146,147,162,201,227,283,284 even for bacteria that are able to metabolize and deactivate NO, such as P. aeruginosa, that possesses NO reductase enzyme that converts NO to nitrous oxide (N2O) and ultimately nitrogen (N2).86,201,219 Of note, NO possesses broad-spectrum antibacterial activity against both gram-positive and gram-negative bacteria, including methicillin-resistant Staphylococcus aureus (MRSA).219,281 Moreover, the dose of NO required to kill bacteria (e.g., 200 ppm of gaseous NO)281,282,285 does not show any cytotoxic effects in human dermal fibroblasts when exposed for 48 h.216,220 In addition to its bactericidal activity at high dosage, low levels of NO (picomolar to nanomolar range in solution phase)286 also serve as a key mediator that minimize planktonic bacteria adhesion and colonization, as well as disperse mature biofilm and release the bacteria trapped in the EPS film back to their planktonic state.286–288 It has been proposed that exposure to low doses of NO restore the sensitivity of biofilm and dispersed bacteria towards several types of antibiotics, greatly increasing their efficacy.286 Overcoming bacteria colonization on the surfaces of biomedical devices through continuous NO release represents an innovative and highly desirable approach to reduce risk of infections, which can ultimately increase device functionality and success rates, reduce morbidity and mortality, and improve patient outcomes..
Frost et al. successfully develop a S-nitroso-N-acetyl-D-penicillamine functionalized polymer matrix (e.g., PDMS,226 cyclam243 and gelatin222) that can release NO via light-initiated SNAP decomposition. SNAP modified purified gelatin can release NO up to 1 × 10−8 µmol mg−1 s−1 under a 527 nm wavelength light-emitting diode (LED,) and it also shows continuous and light intensity-responsive NO release over 24 h, with a total payload of 0.06 µmol NO mg−1.222 The antibacterial activity of SNAP/gelatin was tested against S. aureus (3 × 105 CFU/mL) and it demonstrated the ability to create a zone of inhibition of 1.2 ± 0.7 mm and 0.75 ± 0.3 mm, when exposed to the 4.5 V and 3 V LED light, respectively, over 24 h. Schoenfisch and coworkers have evaluated the antibacterial characteristics of NO releasing sol-gel coatings289 and xerogel films216 which are capable of releasing NO for 5 and 14 d, respectively, against a 108 colony forming units (CFU)/mL saline suspension of P. aeruginosa for up to 4 h. NO successfully reduced bacterial cell coverage on these surfaces by up to 40 %. Recently, Reynolds and coworkers developed a water-soluble NO-releasing polysaccharide derivative that can release 100 % of its NO storage capacity (49.5 ± 5.0 µmol/g) over 24 h.227 The bactericidal activity of this species was evaluated against E. coli, Acinetobacter baumannii (A. baumannii) and S. aureus and the reported data demonstrated an 8-log unit reduction in viable bacteria cell counts for all three types of bacteria after 24 h of incubation. The absence of CFU counts after 72 h corroborated that there was no bacterial growth recovery after exposure to NO. This is the first time a water-soluble antibacterial agent has reached an industrially relevant level of antimicrobial activity.227
Further, it is also well known that bacteria in mature biofilms are much harder to eradicate than when they are in planktonic stage. Meyerhoff and coworkers have conducted many experiments where the antibacterial properties of NO releasing polymer were evaluated against mature biofilm, developed in CDC bioreactors prior to contacting with NO.145,147 Electrochemical NO generating catheters using inner copper wire working electrode and inorganic nitrite salt solution can generate NO through the walls of the catheters with a flux > 1.0 × 10−10 mol cm−2 min−1 for more than 60 h.146 First, the catheters were mounted in a drip-flow bioreactor, which is a standardized model that allows growth of high biomass-biofilm of E. coli at the air liquid interface when incubated with in LB (Luria Bertani) broth for 2 d and 4 d without the NO turned on. After allowing biofilm to form on catheter surfaces, the electrochemical NO release was “turned on” for only 3 h at the end of the experiments. The short period of NO release was effective at dispersing and killing the E. coli biofilm, and could lower the number of live bacteria adhered on the catheter surfaces by > 99.9%. In a separate study, Backlund et al.214 synthesized diazeniumdiolated PAMAM dendrimers with different alkyl chain modifications and examined their antibacterial properties against 24 h old Streptococcus mutans biofilm (S. mutans) at pH 7.4 and 6.4. The bactericidal action of the NO releasing dendrimers was reported to increase with alkyl chain length of the dendrimer and lower pH. In another experiment conducted by Schoenfisch and coworkers, a Center for Disease Control (CDC) bioreactor, that mimics bacterial growth under different sheer force conditions, was used to grow P. aeruginosa biofilms over a 48 h period. The biofilms were then exposed to a water-soluble NO releasing chitosan oligosaccharide (0.17–0.46 µmol NO/mL) for 24 h. The presence of the NO release elicited a 5-log unit reduction in viable bacterial counts with a minimal bactericidal concentration (MBC) of the dendrimer preparation as low as 400 µg/mL.220
Continuous NO release during bacterial proliferation has also been proven to prevent biofilm formation. Cai et al. fabricated NO releasing silicone rubber films containing DBHD/N2O2 along with PLGA (RG 502H) additives that can release NO for 10 d at physiological conditions. pH sensitive dyes were incorporated in the films to help visualize the pH change within the polymeric matrix due to slow hydrolysis of the PLGA that promotes the extended NO release.156 Both the NO release and control films were incubated in a CDC bioreactor for 7 d at 37 °C and the number of live bacteria on the surfaces of the silicone rubber was assessed. The NO release films exhibited substantial antibiofilm properties against both gram-positive S. aureus (98.4 % reduction) and gram-negative E. coli (99.9% reduction) when compared to controls.156 In subsequent studies, Colletta et al.19 and Ketchum et al.189 used the solvent impregnation method previously described above (see section Physical Encapsulation-based NO Releasing Polymers) to load silicone-based tubing with NO donors (SNAP and lipophilic SNAP derivatives, respectively) and demonstrated that they have antibacterial effects toward several microorganisms (e.g., Staphylococcus epidermis, Proteus mirabilis or S. aureus). These results offer a new strategy to reduce bacterial infections associated with not only intravascular catheters but also urinary catheters.
In addition to in vitro experiments, NO releasing polymers (e.g., catheters) have also exhibited both antithrombotic and antibacterial properties in vivo. Brisbois et al. conducted experiments where both SNAP-doped E2As catheter and control E2As catheters were implanted in sheep jugular veins for 7 d.186 At the end of the 7 d period, the catheters were carefully explanted and both the clot area as well as the number of live bacteria adhered on the catheter surfaces were assessed. The 10 wt% SNAP/E2As catheters exhibited enhanced hemocompatibility (70% less thrombus formation) and bactericidal activity (90% reduction of bacteria adhesion) when compared to the controls.
Nitric oxide releasing polymers have also provided a potential strategy for use as active wound healing dressings, capable of reducing bacterial infections at wound sites and accelerating the wound healing process for incisional and excisional wounds,179,219,221 burn wounds,290 and diabetic wounds.232 While normal fibroblasts do not synthesize NO, it has been demonstrated that fibroblasts isolated from the regular wound can release NO.291 The iNOS is synthesized in the early phase of wound healing by inflammatory cells, such as macrophages, monocytes, and other immune lineage cells.119,120,292 The NO released through iNOS enhances angiogenesis, regulates collagen formation, cell proliferation and wound contractions.111,292 Studies using induced NOS (iNOS) knock out mice showed diminished collagen deposition, with the restoration of normal collagen deposits upon exposure to SNAP, indicating the important relationship between NO production and wound healing.293 Therefore, elevating the local NO concentration at a wound site by an exogenous NO supply represents a promising strategy to facilitate the wound healing process.
Yoo and coworkers developed PEI/NONOate nanoparticles (NPs) capable of prolonged NO release, which were then used to treat MRSA-infected excisional wounds (5 mm diameter, full thickness) in mice.219 MRSA was inoculated in the wound for 1 d to develop infection and then the wounds were treated with the NO releasing NPs or control NPs over 6 d. The photographs of the wounds taken at day 0, 1, 4 and 7 clearly showed an accelerated wound healing process for mice treated with NPs, with wound area reduced to 25% at the end of 7 d. The untreated wounds showed a thicker scab with no reduction in the wound area. In a subsequent study, GSNO-doped chitosan films, which exert strong antimicrobial activity against a broad spectrum of bacteria, were evaluated as a wound healing dressing on full thickness excisional wounds (1.5 m × 1.5 cm) in a rat model for 15 d.221 Comparing the NO-treated and untreated wounds, those treated with the GSNO/Chitosan dressing were almost completely healed at the end of the 15 d, with less bacterial burden and decreased inflammatory cell infiltration, but enhanced re-epithelialization.120,221 Brisbois et al. tested the antibacterial efficacy of DBHD/N2O2 and PLGA (5050DLG1A) doped biomedical grade PU films as a dressing for burn wounds (10 cm2 and partial thickness) in a mouse model.290 Burn wounds are quite common, but difficult to treat and often lead to infections.111 The burn wounds in mice were inoculated by A. baumannii for 24 h prior to application of the NO and control wound dressings. After 24 h of treatment, the wound area skin tissue was harvested and assessed for number of viable bacteria adhered at the wound sites. A 4-log unit bacterial reduction was observed for the NO treated wounds when compared to the control would sites.
Conclusions
As detailed above, there are many approaches that have been examined to improve the biocompatibility and antimicrobial activity of biomedical polymers/devices. Most of the conventional approaches, (e.g., creating heparin-releasing surfaces, bacteria-resistant or biocide-releasing surfaces, etc.), can only improve either the hemocompatibility or the antibacterial properties of the devices. However, NO release or generating polymers have demonstrated very positive effects in terms of preventing both platelet activation and thrombus formation as well as exhibiting significant antimicrobial activity toward infection/biofilm formation without bacterial resistance. Although this review mainly focused on the use of NO release polymers for antithrombotic and antibacterial applications, these polymers also have many other potential applications for use on skin, bones, connective tissue, gastroenterology, or studying NO-induced cellular responses.111,177,294,295
Recently, considerable effort has been devoted to develop combination therapy and hybrid drugs that combine NO release functionality with other active agents for increased efficacies, including anticoagulants,35,126 direct thrombin inhibitors,36,43 antimicrobial metal ions,215 quaternary ammonium compounds,70 PEG,115 antibiotics,296 and non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen.140 The remaining challenge for NO delivery polymers in order to be used in clinical settings lies in the development of more stable NO donors and polymer scaffolds and delivering the desired amount NO in a controlled spatial and temporal manner. In many cases, long-term NO release is desired, especially for using NO-releasing, blood compatible polymeric materials for preparing intravascular grafts, stents, catheters, and other vascular access devices. Further research should focus on the dose-dependent biological responses to different NO concentrations and aim towards developing clinically relevant NO delivery materials for that purpose, that can ultimately expedite the translation of these materials from the laboratory to clinical use. Overall, both in vitro and in vivo (animals) studies of some of the NO releasing/generating polymers developed to date have clearly demonstrated the immense potential of this approach to improve the hemocompatibility/antimicrobial activity of a variety of biomedical devices that are required to improve patient care. Hopefully, the first commercial devices that employ this strategy will soon become available for routine use within hospitals.
Supplementary Material
Acknowledgments
We thank the National Institutes of Health (grants HL-128337 and HL-119403) for funding research in our laboratory on the development of novel NO release biomedical polymers/devices.
References
- 1.Naghavi N, De Mel A, Alavijeh OS, Cousins BG, Seifalian AM. Small. 2013;9:22–35. doi: 10.1002/smll.201200458. [DOI] [PubMed] [Google Scholar]
- 2.Gorbet MB, Sefton MV. Biomaterials. 2004;25:5681–5703. doi: 10.1016/j.biomaterials.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 3.Brisbois EJ, Handa H, Meyerhoff ME. In: Advanced Polymers in Medicine. Puoci F, editor. Springer International Publishing, Cham; 2015. pp. 481–511. [Google Scholar]
- 4.Sefton MV, Gemmell CH, Gorbet MB. J Biomater. Sci. Polym. Ed. 2000;11:1165–1182. doi: 10.1163/156856200744255. [DOI] [PubMed] [Google Scholar]
- 5.Gorbet MB, Sefton MV. The Biomaterials: Silver Jubilee Compendium. Vol. 25. Elsevier; 2004. pp. 219–241. [Google Scholar]
- 6.Horbett TA. Cardiovasc. Pathol. 1993;2:137–148. [Google Scholar]
- 7.Andrade JD, Hlady V. Advances in Polymer Science. 1986;79:1–63. [Google Scholar]
- 8.Wu Y, Meyerhoff ME. Talanta. 2008;75:642–650. doi: 10.1016/j.talanta.2007.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klevens RM, Edwards JR, Richards CL, Horan TC, Gaynes RP, Pollock DA, Cardo DM. Public Health Rep. 2007;122:160–166. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abad C, Safdar N. Infect. Dis. Spec. Ed. 2011 [Google Scholar]
- 11.Shah H, Bosch W, Thompson KM, Hellinger WC. The Neurohospitalist. 2013;3:144–151. doi: 10.1177/1941874413476043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, Raad II, Rijnders BJ, Sherertz RJ, Warren DK. Clin. Infect. Dis. 2009;49:1–45. doi: 10.1086/599376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sitges-Serra A, Girvent M. World J. Surg. 1999;23:589–595. doi: 10.1007/pl00012352. [DOI] [PubMed] [Google Scholar]
- 14.Goede MR, Coopersmith CM. Surg. Clin. North Am. 2009;89:463–474. doi: 10.1016/j.suc.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Gahlot R, Nigam C, Kumar V, Yadav G, Anupurba S. Int. J. Crit. Illn. Inj. Sci. 2014;4:162–167. doi: 10.4103/2229-5151.134184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen M, Yu Q, Sun H. Int. J. Mol. Sci. 2013;14:18488–18501. doi: 10.3390/ijms140918488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donlan RM. Clin. Infect. Dis. 2001;33:1387–1392. doi: 10.1086/322972. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan JB. J Dent. Res. 2010;89:205–218. doi: 10.1177/0022034509359403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Colletta A, Wu J, Wo Y, Kappler M, Chen H, Xi C, Meyerhoff ME. ACS Biomater. Sci. Eng. 2015;1:416–424. doi: 10.1021/acsbiomaterials.5b00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hetrick EM, Schoenfisch MH. Chem. Soc. Rev. 2006;35:780–789. doi: 10.1039/b515219b. [DOI] [PubMed] [Google Scholar]
- 21.Hirsh J. N Engl. J. Med. 1991;324:1565–1574. doi: 10.1056/NEJM199105303242206. [DOI] [PubMed] [Google Scholar]
- 22.Gutowska A, Bae YH, Jacobs H, Mohammad F, Mix D, Feijen J, Kim SW. J Biomed. Mater. Res. 1995;29:811–821. doi: 10.1002/jbm.820290705. [DOI] [PubMed] [Google Scholar]
- 23.Warkentin TE, Hayward CP, Smith CA, Kelly PM, Kelton JG. J Lab. Clin. Med. 1992;120:371–379. [PubMed] [Google Scholar]
- 24.Tanzawa H, Mori Y, Harumiya N, Miyama H, Hori M, Ohshima N, Idezuki Y. ASAIO J. 1973;19:188–194. doi: 10.1097/00002480-197301900-00034. [DOI] [PubMed] [Google Scholar]
- 25.Whiffen GVLJD, Dutton RC. Science (80-.) 1963;142:1297–1298. doi: 10.1126/science.142.3597.1297. [DOI] [PubMed] [Google Scholar]
- 26.Shibuta R, Tanaka M, Sisido M, Imanishi Y. J Biomed. Mater. Res. 1986;20:971–987. doi: 10.1002/jbm.820200712. [DOI] [PubMed] [Google Scholar]
- 27.Hufnagel CA, Conrad PW, Gillespie JF, Pifarre R, Llano A, Yokoyama T. Ann. N. Y. Acad. Sci. 1968;146:262–270. doi: 10.1111/j.1749-6632.1968.tb20287.x. [DOI] [PubMed] [Google Scholar]
- 28.Lin JY, Nojiri C, Okano T, Kim SW. ASAIO Trans. 1987;33:602–605. [PubMed] [Google Scholar]
- 29.Heyman PW, Cho CS, McRea JC, Olsen DB, Kim SW. J Biomed. Mater. Res. 1985;19:419–436. doi: 10.1002/jbm.820190407. [DOI] [PubMed] [Google Scholar]
- 30.Ebert C, McRea J, Kim SW. Controlled Release of Bioactive Materials. Elsevier; 1980. pp. 107–122. [Google Scholar]
- 31.Gutowska A, Bae YH, Feijen J, Kim SW. J Control. Release. 1992;22:95–105. [Google Scholar]
- 32.Wan Kim S, Jacobs H. Blood Purif. 1996;14:357–372. doi: 10.1159/000170288. [DOI] [PubMed] [Google Scholar]
- 33.Ayres N, Holt DJ, Jones CF, Corum LE, Grainger DW. J Polym. Sci. A. Polym. Chem. 2008;46:7713–7724. doi: 10.1002/pola.23075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mowery KA, Schoenfisch MH, Saavedra JE, Keefer LK, Meyerhoff ME. Polymer (Guildf) 2000;21:9–21. doi: 10.1016/s0142-9612(99)00127-1. [DOI] [PubMed] [Google Scholar]
- 35.Zhou Z, Meyerhoff ME. Biomaterials. 2005;26:6506–6517. doi: 10.1016/j.biomaterials.2005.04.046. [DOI] [PubMed] [Google Scholar]
- 36.Wu B, Gerlitz B, Grinnell BW, Meyerhoff ME. Biomaterials. 2007;28:4047–4055. doi: 10.1016/j.biomaterials.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sakiyama-Elbert SE. Acta Biomater. 2014;10:1581–1587. doi: 10.1016/j.actbio.2013.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Begovac PC, Thomson RC, Fisher JL, Hughson A, Gallhagen A. Eur. J. Vasc. Endovasc. Surg. 2003;25:432–437. doi: 10.1053/ejvs.2002.1909. [DOI] [PubMed] [Google Scholar]
- 39.Devine C, McCollum C. J Vasc. Surg. 2004;40:924–931. doi: 10.1016/j.jvs.2004.08.033. [DOI] [PubMed] [Google Scholar]
- 40.Olsson P, Sanchez J, Mollnes TE, Riesenfeld J. J Biomater. Sci. Polym. Ed. 2000;11:1261–1273. doi: 10.1163/156856200744192. [DOI] [PubMed] [Google Scholar]
- 41.Kidane AG, Salacinski H, Tiwari A, Bruckdorfer KR, Seifalian AM. Biomacromolecules. 2004;5:798–813. doi: 10.1021/bm0344553. [DOI] [PubMed] [Google Scholar]
- 42.Jordan SW, Chaikof EL. J Vasc. Surg. 2007;45:104–115. doi: 10.1016/j.jvs.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 43.Major TC, Brisbois EJ, Jones AM, Zanetti ME, Annich GM, Bartlett RH, Handa H. Biomaterials. 2014;35:7271–7285. doi: 10.1016/j.biomaterials.2014.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Peppas NA, Huang Y, Torres-Lugo M, Ward JH, Zhang J. Annu. Rev. Biomed. Eng. 2000;2:9–29. doi: 10.1146/annurev.bioeng.2.1.9. [DOI] [PubMed] [Google Scholar]
- 45.Wichterle O, Lím D. Nature. 1960;185:117–118. [Google Scholar]
- 46.Lakshmi S, Jayakrishnan A. Artif. Organs. 1998;22:222–229. doi: 10.1046/j.1525-1594.1998.06124.x. [DOI] [PubMed] [Google Scholar]
- 47.Balakrishnan B, Kumar DS, Yoshida Y, Jayakrishnan A. Biomaterials. 2005;26:3495–3502. doi: 10.1016/j.biomaterials.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 48.Blass CR, Jones C, Courtney JM. Int. J. Artif. Organs. 1992;15:200–203. [PubMed] [Google Scholar]
- 49.Llanos GR, Sefton MV. J Biomed. Mater. Res. 1993;27:1383–1391. doi: 10.1002/jbm.820271105. [DOI] [PubMed] [Google Scholar]
- 50.Harris JM. Poly(Ethylene Glycol) Chemistry. Vol. 11. Boston, MA, Netherlands: Springer US; 1992. [Google Scholar]
- 51.Tanzi MC. Expert Rev. Med. Devices. 2005;2:473–492. doi: 10.1586/17434440.2.4.473. [DOI] [PubMed] [Google Scholar]
- 52.Williams SK, Rose DG, Jarrell BE. J Biomed. Mater. Res. 1994;28:203–212. doi: 10.1002/jbm.820280210. [DOI] [PubMed] [Google Scholar]
- 53.Zilla P, Deutsch M, Meinhart J, Puschmann R, Eberl T, Minar E, Dudczak R, Lugmaier H, Schmidt P, Noszian I. J Vasc. Surg. 1994;19:540–548. doi: 10.1016/s0741-5214(94)70083-4. [DOI] [PubMed] [Google Scholar]
- 54.Shah SR, Tatara AM, D’Souza RN, Mikos AG, Kasper FK. Mater. Today. 2013;16:177–182. [Google Scholar]
- 55.Park S-H, Lee S, Moreira D, Bandaru PR, Han I, Yun D-J. Sci. Rep. 2015;5:15430. doi: 10.1038/srep15430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ye W, Shi Q, Hou J, Jin J, Fan Q, Wong S-C, Xu X, Yin J. J Mater. Chem. B. 2014;2:7186–7191. doi: 10.1039/c4tb01126k. [DOI] [PubMed] [Google Scholar]
- 57.Gao X, Jiang L. Nature. 2004;432:36. doi: 10.1038/432036a. [DOI] [PubMed] [Google Scholar]
- 58.Nydegger U, Rieben R, Lämmle B. Transfus. Sci. 1996;17:481–488. [PubMed] [Google Scholar]
- 59.Cheng G, Xue H, Zhang Z, Chen S, Jiang S. Angew. Chemie Int. Ed. 2008;47:8831–8834. doi: 10.1002/anie.200803570. [DOI] [PubMed] [Google Scholar]
- 60.Ostuni E, Chapman RG, Holmlin RE, Takayama S, Whitesides GM. Langmuir. 2001;17:5605–5620. doi: 10.1021/la0015258. [DOI] [PubMed] [Google Scholar]
- 61.Hsu S-H, Kao Y-C, Lin Z-C. Macromol. Biosci. 2004;4:464–470. doi: 10.1002/mabi.200300082. [DOI] [PubMed] [Google Scholar]
- 62.Hsu S-H, Kao Y-C. Macromol. Biosci. 2005;5:246–253. doi: 10.1002/mabi.200400163. [DOI] [PubMed] [Google Scholar]
- 63.Xu L-C, Soman P, Runt J, Siedlecki Ca. J Biomater. Sci. Polym. Ed. 2007;18:353–368. doi: 10.1163/156856207780425013. [DOI] [PubMed] [Google Scholar]
- 64.Yu Q, Wu Z, Chen H. Acta Biomater. 2015;16:1–13. doi: 10.1016/j.actbio.2015.01.018. [DOI] [PubMed] [Google Scholar]
- 65.Kolodkin-Gal I, Romero D, Cao S, Clardy J, Kolter R, Losick R. Science. 2010;328:627–629. doi: 10.1126/science.1188628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kiedrowski MR, Horswill AR. Ann. N. Y. Acad. Sci. 2011;1241:104–121. doi: 10.1111/j.1749-6632.2011.06281.x. [DOI] [PubMed] [Google Scholar]
- 67.Sepehr S, Rahmani-Badi A, Babaie-Naiej H, Soudi MR. PLoS One. 2014:9. doi: 10.1371/journal.pone.0101677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jennings MC, Ator LE, Paniak TJ, Minbiole KPC, Wuest WM. Chembiochem. 2014;15:2211–2215. doi: 10.1002/cbic.201402254. [DOI] [PubMed] [Google Scholar]
- 69.Jennings MC, Minbiole KPC, Wuest WM. ACS Infect. Dis. 2015:288–303. doi: 10.1021/acsinfecdis.5b00047. [DOI] [PubMed] [Google Scholar]
- 70.Carpenter AW, Worley BV, Slomberg DL, Schoenfisch MH. Biomacromolecules. 2012;13:3334–3342. doi: 10.1021/bm301108x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Abd-El-Aziz AS, Agatemor C, Etkin N, Overy DP, Lanteigne M, McQuillan K, Kerr RG. Biomacromolecules. 2015;16:3694–3703. doi: 10.1021/acs.biomac.5b01207. [DOI] [PubMed] [Google Scholar]
- 72.Allan ND, Giare-Patel K, Olson ME. J Biomed. Biotechnol. 2012;2012 doi: 10.1155/2012/921617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wu K, Yang Y, Zhang Y, Deng J, Lin C. Int. J. Nanomedicine. 2015;10:7241–7252. doi: 10.2147/IJN.S92307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mei L, Lu Z, Zhang X, Li C, Jia Y. ACS Appl. Mater. Interfaces. 2014;6:15813–15821. doi: 10.1021/am502886m. [DOI] [PubMed] [Google Scholar]
- 75.Sehmi SK, Noimark S, Weiner J, Allan E, MacRobert AJ, Parkin IP. ACS Appl. Mater. Interfaces. 2015;7:22807–22813. doi: 10.1021/acsami.5b08665. [DOI] [PubMed] [Google Scholar]
- 76.Zhang L, Ning C, Zhou T, Liu X, Yeung KWK, Zhang T, Xu Z, Wang X, Wu S, Chu PK. ACS Appl. Mater. Interfaces. 2014;6:17323–17345. doi: 10.1021/am5045604. [DOI] [PubMed] [Google Scholar]
- 77.Rossi S, Azghani AO, Omri A. J Antimicrob. Chemother. 2004;54:1013–1018. doi: 10.1093/jac/dkh477. [DOI] [PubMed] [Google Scholar]
- 78.Zhao L, Chu PK, Zhang Y, Wu Z. J Biomed. Mater. Res. B. Appl. Biomater. 2009;91:470–480. doi: 10.1002/jbm.b.31463. [DOI] [PubMed] [Google Scholar]
- 79.Cademartiri R, Anany H, Gross I, Bhayani R, Griffiths M, Brook MA. Biomaterials. 2010;31:1904–1910. doi: 10.1016/j.biomaterials.2009.11.029. [DOI] [PubMed] [Google Scholar]
- 80.Puapermpoonsiri U, Spencer J, van der Walle CF. Eur. J. Pharm. Biopharm. 2009;72:26–33. doi: 10.1016/j.ejpb.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 81.Wei T, Yu Q, Zhan W, Chen H. Adv. Healthc. Mater. 2016;5:449–456. doi: 10.1002/adhm.201500700. [DOI] [PubMed] [Google Scholar]
- 82.Cado G, Aslam R, Séon L, Garnier T, Fabre R, Parat A, Chassepot A, Voegel J-C, Senger B, Schneider F, Frère Y, Jierry L, Schaaf P, Kerdjoudj H, Metz-Boutigue M-H, Boulmedais F. Adv. Funct. Mater. 2013;23:4801–4809. [Google Scholar]
- 83.Holmberg KV, Abdolhosseini M, Li Y, Chen X, Gorr S-U, Aparicio C. Acta Biomater. 2013;9:8224–8231. doi: 10.1016/j.actbio.2013.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li J, Chen Z, Zhou M, Jing J, Li W, Wang Y, Wu L, Wang L, Wang Y, Lee M. Angew. Chem. Int. Ed. Engl. 2016;55:2592–2595. doi: 10.1002/anie.201511276. [DOI] [PubMed] [Google Scholar]
- 85.Yang WJ, Cai T, Neoh KG, Kang ET, Dickinson GH, Teo SLM, Rittschof D. Langmuir. 2011;27:7065–7076. doi: 10.1021/la200620s. [DOI] [PubMed] [Google Scholar]
- 86.Reighard KP, Schoenfisch MH. Antimicrob. Agents Chemother. 2015;59:6506–6513. doi: 10.1128/AAC.01208-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Reighard KP, Hill DB, Dixon GA, Worley BV, Schoenfisch MH. Biofouling. 2015;31:775–787. doi: 10.1080/08927014.2015.1107548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Choi J, Yang BJ, Bae GN, Jung JH. ACS Appl. Mater. Interfaces. 2015;7:25313–25320. doi: 10.1021/acsami.5b07441. [DOI] [PubMed] [Google Scholar]
- 89.Dolanský J, Henke P, Kubát P, Fraix A, Sortino S, Mosinger J. ACS Appl. Mater. Interfaces. 2015;7:22980–22989. doi: 10.1021/acsami.5b06233. [DOI] [PubMed] [Google Scholar]
- 90.Cao Z, Mi L, Mendiola J, Ella-Menye JR, Zhang L, Xue H, Jiang S. Angew. Chemie - Int. Ed. 2012;51:2602–2605. doi: 10.1002/anie.201106466. [DOI] [PubMed] [Google Scholar]
- 91.Yu Q, Cho J, Shivapooja P, Ista LK, Lopez GP. ACS Appl. Mater. Interfaces. 2013;5:9295–9304. doi: 10.1021/am4022279. [DOI] [PubMed] [Google Scholar]
- 92.Dargahi M, Hosseinidoust Z, Tufenkji N, Omanovic S. Colloids Surfaces B Biointerfaces. 2014;117:152–157. doi: 10.1016/j.colsurfb.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 93.Tamura S, Yonezawa H, Motegi M, Nakao R, Yoneda S, Watanabe H, Yamazaki T, Senpuku H. Oral Microbiol. Immunol. 2009;24:152–161. doi: 10.1111/j.1399-302X.2008.00489.x. [DOI] [PubMed] [Google Scholar]
- 94.Ishijima SA, Hayama K, Burton JP, Reid G, Okada M, Matsushita Y, Abe S. Appl. Environ. Microbiol. 2012;78:2190–2199. doi: 10.1128/AEM.07055-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Trautner BW, Hull RA, Darouiche RO. Urology. 2003;61:1059–1062. doi: 10.1016/s0090-4295(02)02555-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Trautner BW, Hull RA, Darouiche RO. Curr. Opin. Infect. Dis. 2005;18:37–41. doi: 10.1097/00001432-200502000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Trautner BW, Hull Ra, Thornby JI, Darouiche RO. Infect. Control Hosp. Epidemiol. 2007;28:92–94. doi: 10.1086/510872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Andersson P, Engberg I, Lidin-Janson G, Lincoln K, Hull R, Hull S, Svanborg C. Infect. Immun. 1991;59:2915–2921. doi: 10.1128/iai.59.9.2915-2921.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Esclarin De Ruz A, Garcia Leoni E, Herruzo Cabrera R. J Urol. 2000;164:1285–1289. [PubMed] [Google Scholar]
- 100.Unnithan AR, Ghavami Nejad A, Sasikala ARK, Thomas RG, Jeong YY, Murugesan P, Nasseri S, Wu D, Park CH, Kim CS. Chem. Eng. J. 2016;287:640–648. [Google Scholar]
- 101.Vaterrodt A, Thallinger B, Daumann K, Koch D, Guebitz GM, Ulbricht M. Langmuir. 2016;32:1347–1359. doi: 10.1021/acs.langmuir.5b04303. [DOI] [PubMed] [Google Scholar]
- 102.Xu L-C, Siedlecki Ca. Biomed. Mater. 2014;9:035003. doi: 10.1088/1748-6041/9/3/035003. [DOI] [PubMed] [Google Scholar]
- 103.Xu LC, Siedlecki Ca. Acta Biomater. 2012;8:72–81. doi: 10.1016/j.actbio.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 104.Xu L, Bauer JW, Siedlecki Ca. Colloids Surfaces B Biointerfaces. 2014;124:49–68. doi: 10.1016/j.colsurfb.2014.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wang L, Li H, Chen S, Nie C, Cheng C, Zhao C. ACS Biomater. Sci. Eng. 2015;1:1183–1193. doi: 10.1021/acsbiomaterials.5b00320. [DOI] [PubMed] [Google Scholar]
- 106.Shi Z-Q, Ji H-F, Yu H-C, Huang X-L, Zhao W-F, Sun S-D, Zhao C-S. Colloid Polym. Sci. 2016;294:441–453. [Google Scholar]
- 107.Deng J, Ma L, Liu X, Cheng C, Nie C, Zhao C. Adv. Mater. Interfaces. 2016;3:1500473. [Google Scholar]
- 108.Seabra AB, Durán N. J Mater. Chem. 2010;20:1624. [Google Scholar]
- 109.Frost MC, Reynolds MM, Meyerhoff ME. Biomaterials. 2005;26:1685–1693. doi: 10.1016/j.biomaterials.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 110.Reynolds MM, Frost MC, Meyerhoff ME. Free Radic. Biol. Med. 2004;37:926–936. doi: 10.1016/j.freeradbiomed.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 111.Nichols SP, Storm WL, Koh A, Schoenfisch MH. Adv. Drug Deliv. Rev. 2012;64:1177–1188. doi: 10.1016/j.addr.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hetrick EM, Schoenfisch MH. Annu Rev Anal Chem (Palo Alto Calif) 2009;2:409–433. doi: 10.1146/annurev-anchem-060908-155146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Reynolds MM, Annich GM. Organogenesis. 2011;7:42–49. doi: 10.4161/org.7.1.14029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wang Y, Chen S, Pan Y, Gao J, Tang D, Kong D, Wang S. J Mater. Chem. B. 2015;3:9212–9222. doi: 10.1039/c5tb02080h. [DOI] [PubMed] [Google Scholar]
- 115.Taite LJ, Yang P, Jun H-W, West JL. J Biomed. Mater. Res. Part B Appl. Biomater. 2007;84B:108–116. doi: 10.1002/jbm.b.30850. [DOI] [PubMed] [Google Scholar]
- 116.Geenen ILA, Molin DGM, van den Akker NMS, Jeukens F, Spronk HM, Schurink GWH, Post MJ. J Tissue Eng. Regen. Med. 2015;9:564–576. doi: 10.1002/term.1642. [DOI] [PubMed] [Google Scholar]
- 117.Carpenter AW, Schoenfisch MH. Chem. Soc. Rev. 2012;41:3742–3752. doi: 10.1039/c2cs15273h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Vaughn M, Kuo L, Liao J. Am. J. Physiol. 1998;274:2163–2176. doi: 10.1152/ajpheart.1998.274.6.H2163. [DOI] [PubMed] [Google Scholar]
- 119.Vural KM, Bayazit M. Eur. J. Vasc. Endovasc. Surg. 2001;22:285–293. doi: 10.1053/ejvs.2001.1448. [DOI] [PubMed] [Google Scholar]
- 120.Jen MC, Serrano MC, van Lith R, Ameer GA. Adv. Funct. Mater. 2012;22:239–260. doi: 10.1002/adfm.201101707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Loscalzo J. Circ. Res. 2001;88:756–762. doi: 10.1161/hh0801.089861. [DOI] [PubMed] [Google Scholar]
- 122.Walford G, Loscalzo J. J Thromb. Haemost. 2003;1:2112–2118. doi: 10.1046/j.1538-7836.2003.00345.x. [DOI] [PubMed] [Google Scholar]
- 123.Isenberg JS, Romeo MJ, Yu C, Yu CK, Nghiem K, Monsale J, Rick ME, Wink DA, Frazier WA, Roberts DD. Blood. 2008;111:613–623. doi: 10.1182/blood-2007-06-098392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Gries A, Bode C, Peter K, Herr A, Böhrer H, Motsch J, Martin E. Circ. 1998;97:1481–1487. doi: 10.1161/01.cir.97.15.1481. [DOI] [PubMed] [Google Scholar]
- 125.Radomski MW, Palmer RM, Moncada S. Proc. Natl. Acad. Sci. U. S. A. 1990;87:5193–5197. doi: 10.1073/pnas.87.13.5193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Suchyta DJ, Handa H, Meyerhoff ME. Mol. Pharm. 2014;11:645–650. doi: 10.1021/mp400501c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Schairer DO, Chouake JS, Nosanchuk JD, Friedman AJ. Virulence. 2012;3:271–279. doi: 10.4161/viru.20328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Rubbo H, Radi R, Trujillo M, Telleri R, Kalyanaraman B, Barnes S, Kirk M, Freeman BA. J Biol. Chem. 1994;269:26066–26075. [PubMed] [Google Scholar]
- 129.Fang FC. Nat. Rev. Microbiol. 2004;2:820–832. doi: 10.1038/nrmicro1004. [DOI] [PubMed] [Google Scholar]
- 130.Ignarro L, Buga G. Proc. Natl. Acad. Sci. U. S. A. 1987;84:9265–9269. doi: 10.1073/pnas.84.24.9265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hanson SR, Hutsell TC, Keefer LK, Mooradian DL, Smith DJ. Adv. Pharmacol. 1995;34:383–398. doi: 10.1016/s1054-3589(08)61099-6. [DOI] [PubMed] [Google Scholar]
- 132.Lundberg JO, Gladwin MT, Weitzberg E. Nat. Rev. Drug Discov. 2015;14:623–641. doi: 10.1038/nrd4623. [DOI] [PubMed] [Google Scholar]
- 133.Lundberg JO, Weitzberg E, Gladwin MT. Crit. Care Med. 2008;7:156–167. doi: 10.1038/nrd2466. [DOI] [PubMed] [Google Scholar]
- 134.Scatena R, Bottoni P, Martorana G, Giardina B. 2005;14:835–846. doi: 10.1517/13543784.14.7.835. [DOI] [PubMed] [Google Scholar]
- 135.Riccio Da, Schoenfisch MH. Chem. Soc. Rev. 2012;41:3731–3741. doi: 10.1039/c2cs15272j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hrabie Ja, Keefer LK. Chem. Rev. 2002;102:1135–1154. doi: 10.1021/cr000028t. [DOI] [PubMed] [Google Scholar]
- 137.Varu VN, Tsihlis ND, Kibbe MR. Vasc. Endovascular Surg. 2009;43:121–131. doi: 10.1177/1538574408322752. [DOI] [PubMed] [Google Scholar]
- 138.Saraiva J, Marotta-Oliveira SS, Cicillini SA, Eloy JDO, Marchetti JM. J Drug Deliv. 2011;2011 doi: 10.1155/2011/936438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sortino S. Chem. Soc. Rev. 2010;39:2903–2913. doi: 10.1039/b908663n. [DOI] [PubMed] [Google Scholar]
- 140.Wang PG, Xian M, Tang X, Wu X, Wen Z, Cai T, Janczuk AJ. Chem. Rev. 2002;102:1091–1134. doi: 10.1021/cr000040l. [DOI] [PubMed] [Google Scholar]
- 141.Münzel T, Daiber A, Mülsch A. Circ. Res. 2005;97:618–628. doi: 10.1161/01.RES.0000184694.03262.6d. [DOI] [PubMed] [Google Scholar]
- 142.Sydow K, Daiber A, Oelze M, Chen Z, August M, Wendt M, Ullrich V, Mülsch A, Schulz E, Keaney JF, Stamler JS, Münzel T. J Clin. Invest. 2004;113:482–489. doi: 10.1172/JCI19267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Daiber A, Oelze M, Coldewey M, Bachschmid M, Wenzel P, Sydow K, Wendt M, Kleschyov AL, Stalleicken D, Ullrich V, Mulsch A, Munzel T. Mol. Pharmacol. 2004;66:1372–1382. doi: 10.1124/mol.104.002600. [DOI] [PubMed] [Google Scholar]
- 144.Grossi L, D’Angelo S. J Med. Chem. 2005;48:2622–2626. doi: 10.1021/jm049857n. [DOI] [PubMed] [Google Scholar]
- 145.Höfler L, Koley D, Wu J, Xi C, Meyerhoff ME. RSC Adv. 2012;2:6765–6767. doi: 10.1039/C2RA20853A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ren H, Colletta A, Koley D, Wu J, Xi C, Major TC, Bartlett RH, Meyerhoff ME. Bioelectrochemistry. 2015;104:10–16. doi: 10.1016/j.bioelechem.2014.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ren H, Wu J, Xi C, Lehnert N, Major T, Bartlett RH, Meyerhoff ME. ACS Appl. Mater. Interfaces. 2014;6:3779–3783. doi: 10.1021/am406066a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hwu JR, Yau CS, Tsay S-C, Ho T-I. Tetrahedron Lett. 1997;38:9001–9004. [Google Scholar]
- 149.Wan A, Gao Q, Li H. J Mater. Sci. Mater. Med. 2009;20:321–327. doi: 10.1007/s10856-008-3511-5. [DOI] [PubMed] [Google Scholar]
- 150.Hong S, Kim J, Na YS, Park J, Kim S, Singha K, Il Im G, Han DK, Kim WJ, Lee H. Angew. Chemie - Int. Ed. 2013;52:9187–9191. doi: 10.1002/anie.201301646. [DOI] [PubMed] [Google Scholar]
- 151.Maragos CM, Morley D, Wink DA, Dunams TM, Saavedra JE, Hoffman A, Bove AA, Isaac L, Hrabie JA, Keefer LK. J Med. Chem. 1991;34:3242–3247. doi: 10.1021/jm00115a013. [DOI] [PubMed] [Google Scholar]
- 152.Keefer LK, Nims RW, Davies KM, Wink DA. Methods Enzymol. 1996;268:281–293. doi: 10.1016/s0076-6879(96)68030-6. [DOI] [PubMed] [Google Scholar]
- 153.Batchelor MM, Reoma SL, Fleser PS, Nuthakki VK, Callahan RE, Shanley CJ, Politis JK, Elmore J, Merz SI, Meyerhoff ME. J Med. Chem. 2003;46:5153–5161. doi: 10.1021/jm030286t. [DOI] [PubMed] [Google Scholar]
- 154.Handa H, Brisbois EJ, Major TC. J Mater. Chem. B. 2013;1:3578–3587. doi: 10.1039/C3TB20277A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Handa H, Major TC, Brisbois EJ, Amoako KA, Meyerhoff ME, Bartlett RH. J Mater. Chem. B. 2014;2:1059–1067. doi: 10.1039/C3TB21771J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Cai W, Wu J, Xi C, Meyerhoff ME. Biomaterials. 2012;33:7933–7944. doi: 10.1016/j.biomaterials.2012.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Makadia HK, Siegel SJ. Polymers (Basel) 2011;3:1377–1397. doi: 10.3390/polym3031377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Stamler JS, Jaraki O, Osborne J, Simon DI, Keaney J, Vita J, Singel D, Valeri CR, Loscalzo J. Proc. Natl. Acad. Sci. U. S. A. 1992;89:7674–7677. doi: 10.1073/pnas.89.16.7674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Giustarini D, Milzani A, Colombo R, Dalle-Donne I, Rossi R. Clin. Chim. Acta. 2003;330:85–98. doi: 10.1016/s0009-8981(03)00046-9. [DOI] [PubMed] [Google Scholar]
- 160.Duan X, Lewis RS. Biomaterials. 2002;23:1197–1203. doi: 10.1016/s0142-9612(01)00234-4. [DOI] [PubMed] [Google Scholar]
- 161.Brisbois EJ, Handa H, Major TC, Bartlett RH, Meyerhoff ME. Biomaterials. 2013;34:6957–6966. doi: 10.1016/j.biomaterials.2013.05.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wo Y, Li Z, Brisbois EJ, Colletta A, Wu J, Major TC, Xi C, Bartlett RH, Matzger AJ, Meyerhoff ME. ACS Appl. Mater. Interfaces. 2015;7:22218–22227. doi: 10.1021/acsami.5b07501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Williams DLH. Chem. Commun. 1996:1085–1091. [Google Scholar]
- 164.Williams DLH. Transit. Met. Chem. 1996;21:189–191. [Google Scholar]
- 165.Williams DL. Acc. Chem. Res. 1999;32:869–876. [Google Scholar]
- 166.Szacilowski K, Stasicka Z. Prog. React. Kinet. Mech. 2001;26:1–58. [Google Scholar]
- 167.Singh RJ, Hogg N, Joseph J, Kalyanaraman B. J Biol. Chem. 1996;271:18596–18603. doi: 10.1074/jbc.271.31.18596. [DOI] [PubMed] [Google Scholar]
- 168.Aravindakumar CT, Veleeparampil MM, Aravind UK. Adv. Phys. Chem. 2009;2009 [Google Scholar]
- 169.McAninly J, Williams DLH, Askew SC, Butler AR, Russell C. J Chem. Soc. Chem. Commun. 1993:1758–1759. [Google Scholar]
- 170.Hwang S, Meyerhoff ME. Biomaterials. 2008;29:2443–2452. doi: 10.1016/j.biomaterials.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Cha W, Meyerhoff ME. Biomaterials. 2007;28:19–27. doi: 10.1016/j.biomaterials.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 172.Yang J, Welby JL, Meyerhoff ME. Langmuir. 2008;24:10265–10272. doi: 10.1021/la801466e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Cai W, Wu J, Xi C, Ashe AJ, Meyerhoff ME. Biomaterials. 2011;32:7774–7784. doi: 10.1016/j.biomaterials.2011.06.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Holmes AJ, Williams DLH. Chem. Commun. 1998:1711–1712. [Google Scholar]
- 175.Holmes AJ, Williams DLH. J Chem. Soc. Trans. 2. 2000:1639–1644. [Google Scholar]
- 176.Jourd’heuil D, Laroux FS, Miles AM, Wink DA, Grisham MB. Arch. Biochem. Biophys. 1999;361:323–330. doi: 10.1006/abbi.1998.1010. [DOI] [PubMed] [Google Scholar]
- 177.Seabra AB. In: Nanocosmetics and Nanomedicines. Beck R, Guterres S, Pohlmann A, editors. Berlin, Heidelberg: Springer Berlin Heidelberg; 2011. pp. 253–268. [Google Scholar]
- 178.Vercelino R, Cunha TM, Ferreira ES, Cunha FQ, Ferreira SH, De Oliveira MG. J Mater. Sci. Mater. Med. 2013;24:2157–2169. doi: 10.1007/s10856-013-4973-7. [DOI] [PubMed] [Google Scholar]
- 179.Schanuel FS, Raggio Santos KS, Monte-Alto-Costa A, De Oliveira MG. Colloids Surfaces B Biointerfaces. 2015;130:182–191. doi: 10.1016/j.colsurfb.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 180.de Oliveira MG. Basic Clin. Pharmacol. Toxicol. 2016 [Google Scholar]
- 181.Borthwick TR, Benson GD, Schugar HJ. J Lab. Clin. Med. 1980;95:575–580. [PubMed] [Google Scholar]
- 182.Parameshvara V. Br. J. Ind. Med. 1967;24:73–76. doi: 10.1136/oem.24.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Graeme KA, Pollack CV. J Emerg. Med. 1998;16:45–56. doi: 10.1016/s0736-4679(97)00241-2. [DOI] [PubMed] [Google Scholar]
- 184.Jones MM, Weaver AD, Weller WL. Res. Commun. Chem. Pathol. Pharmacol. 1978;22:581–588. [PubMed] [Google Scholar]
- 185.Arulsamy N, Bohle DS, Butt JA, Irvine GJ, Jordan PA, Sagan E. J Am. Chem. Soc. 1999;121:7115–7123. [Google Scholar]
- 186.Brisbois EJ, Davis RP, Jones AM, Major TC, Bartlett RH, Meyerhoff ME, Handa H. J Mater. Chem. B. 2015;3:1639–1645. doi: 10.1039/C4TB01839G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Megson IL, Morton S, Greig IR, Mazzei FA, Field RA, Butler AR, Caron G, Gasco A, Fruttero R, Webb DJ. Br. J. Pharmacol. 1999;126:639–648. doi: 10.1038/sj.bjp.0702346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Megson IL. Drugs Future. 2002;27:777. [Google Scholar]
- 189.Ketchum A, Kappler M, Wu J, Xi C, Meyerhoff ME. J Mater. Chem. B. 2015;4:422–430. doi: 10.1039/C5TB01664A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Jo YS, van der Vlies AJ, Gantz J, Thacher TN, Antonijevic S, Cavadini S, Demurtas D, Stergiopulos N, Hubbell JA. J Am. Chem. Soc. 2009;131:14413–14418. doi: 10.1021/ja905123t. [DOI] [PubMed] [Google Scholar]
- 191.Kanayama N, Yamaguchi K, Nagasaki Y. Chem. Lett. 2010;39:1008–1009. [Google Scholar]
- 192.Cavalieri F, Finelli I, Tortora M, Mozetic P, Chiessi E, Polizio F, Brismar TB, Paradossi G. Chem. Mater. 2008;20:3254–3258. [Google Scholar]
- 193.Hrabie JA, Saavedra JE, Roller PP, Southan GJ, Keefer LK. Bioconjug. Chem. 1999;10:838–842. doi: 10.1021/bc990035s. [DOI] [PubMed] [Google Scholar]
- 194.Simon DI, Mullins ME, Jia L, Gaston B, Singel DJ, Stamler JS. Proc. Natl. Acad. Sci. U. S. A. 1996;93:4736–4741. doi: 10.1073/pnas.93.10.4736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Ewing JF, Young DV, Janero DR, Garvey DS, Grinnell TA. J Pharmacol. Exp. Ther. 1997;283:947–954. [PubMed] [Google Scholar]
- 196.Ishima Y, Akaike T, Kragh-Hansen U, Hiroyama S, Sawa T, Suenaga A, Maruyama T, Kai T, Otagiri M. J Biol. Chem. 2008;283:34966–34975. doi: 10.1074/jbc.M807009200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Katsumi H, Nishikawa M, Yamashita F, Hashida M. J Pharmacol. Exp. Ther. 2005;314:1117–1124. doi: 10.1124/jpet.105.087429. [DOI] [PubMed] [Google Scholar]
- 198.Huang S-L, Kee PH, Kim H, Moody MR, Chrzanowski SM, Macdonald RC, McPherson DD. J Am. Coll. Cardiol. 2009;54:652–659. doi: 10.1016/j.jacc.2009.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Frost MC, Meyerhoff ME. J Am. Chem. Soc. 2004;126:1348–1349. doi: 10.1021/ja039466i. [DOI] [PubMed] [Google Scholar]
- 200.Frost MC, Meyerhoff ME. J Biomed. Mater. Res. A. 2005;72:409–419. doi: 10.1002/jbm.a.30275. [DOI] [PubMed] [Google Scholar]
- 201.Carpenter AW, Slomberg DL, Rao KS, Schoenfisch MH. ACS Nano. 2011;5:7235–7244. doi: 10.1021/nn202054f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Kafshgari MH, Cavallaro A, Delalat B, Harding FJ, McInnes SJ, Mäkilä E, Salonen J, Vasilev K, Voelcker NH. Nanoscale Res. Lett. 2014;9:333. doi: 10.1186/1556-276X-9-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Slomberg DL, Lu Y, Broadnax AD, Hunter RA, Carpenter AW, Schoenfisch MH. ACS Appl. Mater. Interfaces. 2013;5:9322–9329. doi: 10.1021/am402618w. [DOI] [PubMed] [Google Scholar]
- 204.Rothrock AR, Donkers RL, Schoenfisch MH. Society. 2005;127:9362–9363. doi: 10.1021/ja052027u. [DOI] [PubMed] [Google Scholar]
- 205.Polizzi MA, Stasko NA, Schoenfisch MH. Langmuir. 2007;23:4938–4943. doi: 10.1021/la0633841. [DOI] [PubMed] [Google Scholar]
- 206.Lautner G, Meyerhoff ME, Schwendeman SP. J Control. Release. 2016;225:133–139. doi: 10.1016/j.jconrel.2015.12.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Wheatley PS, Butler AR, Crane MS, Fox S, Xiao B, Rossi AG, Megson IL, Morris RE. J Am. Chem. Soc. 2006;128:502–509. doi: 10.1021/ja0503579. [DOI] [PubMed] [Google Scholar]
- 208.Neidrauer M, Ercan UK, Bhattacharyya A, Samuels J, Sedlak J, Trikha R, Barbee KA, Weingarten MS, Joshi SG. J Med. Microbiol. 2014;63:203–209. doi: 10.1099/jmm.0.067322-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Harding JL, Reynolds MM. J Am. Chem. Soc. 2012;134:3330–3333. doi: 10.1021/ja210771m. [DOI] [PubMed] [Google Scholar]
- 210.Harding JL, Reynolds MM. J Mater. Chem. B. 2014;2:2530–2536. doi: 10.1039/c3tb21458c. [DOI] [PubMed] [Google Scholar]
- 211.Harding JL, Metz JM, Reynolds MM. Adv. Funct. Mater. 2014;24:7503–7509. [Google Scholar]
- 212.Neufeld MJ, Harding JL, Reynolds MM. ACS Appl. Mater. Interfaces. 2015;7:26742–26750. doi: 10.1021/acsami.5b08773. [DOI] [PubMed] [Google Scholar]
- 213.Stasko NA, Fischer TH, Schoenfisch MH. Biomacromolecules. 2008;9:834–841. doi: 10.1021/bm7011746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Backlund CJ, Worley BV, Schoenfisch MH. Acta Biomater. 2016;29:198–205. doi: 10.1016/j.actbio.2015.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Storm WL, Johnson Ja, Worley BV, Slomberg DL, Schoenfisch MH. J Biomed. Mater. Res. A. 2014:1–11. doi: 10.1002/jbm.a.35331. [DOI] [PubMed] [Google Scholar]
- 216.Riccio Da, Dobmeier KP, Hetrick EM, Privett BJ, Paul HS, Schoenfisch MH. Biomaterials. 2009;30:4494–4502. doi: 10.1016/j.biomaterials.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Nacharaju P, Tuckman-Vernon C, Maier KE, Chouake J, Friedman A, Cabrales P, Friedman JM. Nitric Oxide. 2012;27:150–160. doi: 10.1016/j.niox.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Coneski PN, Nash JA, Schoenfisch MH. ACS Appl. Mater. Interfaces. 2011;3:426–432. doi: 10.1021/am101010e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Yoo J-W, Nurhasni H, Cao J, Choi M, Kim I, Luel Lee B, Jung Y. Int. J. Nanomedicine. 2015;10:3065–3080. doi: 10.2147/IJN.S82199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Lu Y, Slomberg DL, Schoenfisch MH. Biomaterials. 2014;35:1716–1724. doi: 10.1016/j.biomaterials.2013.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Kim JO, Noh JK, Thapa RK, Hasan N, Choi M, Kim JH, Lee JH, Ku SK, Yoo JW. Int. J. Biol. Macromol. 2015;79:217–225. doi: 10.1016/j.ijbiomac.2015.04.073. [DOI] [PubMed] [Google Scholar]
- 222.Vogt C, Xing Q, He W, Li B, Frost MC, Zhao F. Biomacromolecules. 2013;14:2521–2530. doi: 10.1021/bm301984w. [DOI] [PubMed] [Google Scholar]
- 223.Parzuchowski PG, Frost MC, Meyerhoff ME. J Am. Chem. Soc. 2002;124:12182–12191. doi: 10.1021/ja020268l. [DOI] [PubMed] [Google Scholar]
- 224.Seabra AB, Da Silva R, De Souza GFP, De Oliveira MG. Artif. Organs. 2008;32:262–267. doi: 10.1111/j.1525-1594.2008.00540.x. [DOI] [PubMed] [Google Scholar]
- 225.Yapor JP, Lutzke A, Pegalajar-Jurado A, Neufeld BH, Damodaran VB, Reynolds MM. J Mater. Chem. B. 2015;3:9233–9241. doi: 10.1039/c5tb01625h. [DOI] [PubMed] [Google Scholar]
- 226.Gierke GE, Nielsen M, Frost MC. Sci. Technol. Adv. Mater. 2011;12:055007. doi: 10.1088/1468-6996/12/5/055007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Pegalajar-Jurado A, Wold KA, Joslin JM, Neufeld BH, Arabea KA, Suazo LA, McDaniel SL, Bowen RA, Reynolds MM. J Control. Release. 2015;220:617–623. doi: 10.1016/j.jconrel.2015.11.024. [DOI] [PubMed] [Google Scholar]
- 228.Wan A, Gao Q, Li H. J Mater. Sci. Mater. Med. 2008;20:321–327. doi: 10.1007/s10856-008-3511-5. [DOI] [PubMed] [Google Scholar]
- 229.Park J, Kim J, Singha K, Han DK, Park H, Kim WJ. Biomaterials. 2013;34:8766–8775. doi: 10.1016/j.biomaterials.2013.07.064. [DOI] [PubMed] [Google Scholar]
- 230.Kim J, Lee Y, Singha K, Kim HW, Shin JH, Jo S, Han DK, Kim WJ. Bioconjug. Chem. 2011;22:1031–1038. doi: 10.1021/bc100405c. [DOI] [PubMed] [Google Scholar]
- 231.Seabra AB, Fitzpatrick A, Paul J, De Oliveira MG, Weller R. Br. J. Dermatol. 2004;151:977–983. doi: 10.1111/j.1365-2133.2004.06213.x. [DOI] [PubMed] [Google Scholar]
- 232.Masters K, Leibovich S, Belem P, West JL, Poole-Warren L. Wound Repair Regen. 2002;10:286–294. doi: 10.1046/j.1524-475x.2002.10503.x. [DOI] [PubMed] [Google Scholar]
- 233.Reynolds MM, Hrabie Ja, Oh BK, Politis JK, Citro ML, Keefer LK, Meyerhoff ME. Biomacromolecules. 2006;7:987–994. doi: 10.1021/bm060028o. [DOI] [PubMed] [Google Scholar]
- 234.Reynolds MM, Saavedra JE, Showalter BM, Valdez CA, Shanklin AP, Oh BK, Keefer LK, Meyerhoff ME. J Mater. Chem. 2010;20:3107–2114. doi: 10.1039/c000152j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Parzuchowska B, Parzuchowski P. Polimery. 2014;59:105–194. [Google Scholar]
- 236.Zhang H, Annich GM, Miskulin J, Stankiewicz K, Osterholzer K, Merz SI, Bartlett RH, Meyerhoff ME. J Am. Chem. Soc. 2003;125:5015–5024. doi: 10.1021/ja0291538. [DOI] [PubMed] [Google Scholar]
- 237.Saavedra JE, Booth MN, Hrabie JA, Davies KM, Keefer LK. J Org. Chem. 1999;64:5124–5131. doi: 10.1021/jo9901539. [DOI] [PubMed] [Google Scholar]
- 238.Zhang H, Annich GM, Miskulin J, Osterholzer K, Merz SI, Bartlett RH, Meyerhoff ME. Biomaterials. 2002;23:1485–1494. doi: 10.1016/s0142-9612(01)00274-5. [DOI] [PubMed] [Google Scholar]
- 239.Smith DJ, Chakravarthy D, Pulfer S, Simmons ML, Hrabie JA, Citro ML, Saavedra JE, Davies KM, Hutsell TC, Mooradian DL, Hanson SR, Keefer LK. J Med. Chem. 1996;39:1148–1156. doi: 10.1021/jm950652b. [DOI] [PubMed] [Google Scholar]
- 240.Kou Y, Wan A. Bioorg. Med. Chem. Lett. 2008;18:2337–2341. doi: 10.1016/j.bmcl.2008.02.073. [DOI] [PubMed] [Google Scholar]
- 241.Kang Y, Kim J, Lee YM, Im S, Park H, Kim WJ. J Control. Release. 2015;220:624–630. doi: 10.1016/j.jconrel.2015.08.057. [DOI] [PubMed] [Google Scholar]
- 242.Stasko NA, Schoenfisch MH. J Am. Chem. Soc. 2006;128:8265–8271. doi: 10.1021/ja060875z. [DOI] [PubMed] [Google Scholar]
- 243.McCarthy CW, Goldman J, Frost MC. ACS Appl. Mater. Interfaces. 2016 doi: 10.1021/acsami.5b12548. [DOI] [PubMed] [Google Scholar]
- 244.Damodaran VB, Place LW, Kipper MJ, Reynolds MM. J Mater. Chem. 2012;22:23038. [Google Scholar]
- 245.Kean T, Thanou M. Adv. Drug Deliv. Rev. 2010;62:3–11. doi: 10.1016/j.addr.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 246.Wang C, Yang F, Xu Z, Shi D, Chen D, Dai J, Gu N, Jiang Q. Thromb. Res. 2013;131:e31–e38. doi: 10.1016/j.thromres.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 247.Tai LA, Wang YC, Yang CS. Nitric Oxide - Biol. Chem. 2010;23:60–64. doi: 10.1016/j.niox.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 248.Koehler JJ, Zhao J, Jedlicka SS, Porterfield DM, Rickus JL. J Phys. Chem. B. 2008;112:15086–15093. doi: 10.1021/jp803276u. [DOI] [PubMed] [Google Scholar]
- 249.Jeh HS, Lu S, George SC. J Microencapsul. 2004;21:3–13. doi: 10.1080/02652040310001619767. [DOI] [PubMed] [Google Scholar]
- 250.Wischke C, Schwendeman SP. Int. J. Pharm. 2008;364:298–327. doi: 10.1016/j.ijpharm.2008.04.042. [DOI] [PubMed] [Google Scholar]
- 251.Shishido SM, Seabra AB, Loh W, de Oliveira MG. Biomaterials. 2003;24:3543–3553. doi: 10.1016/s0142-9612(03)00153-4. [DOI] [PubMed] [Google Scholar]
- 252.de Oliveira MG, Shishido SM, Seabra AB, Morgon NH. J Phys. Chem. A. 2002;106:8963–8970. [Google Scholar]
- 253.Gappa-Fahlenkamp H, Lewis RS. Biomaterials. 2005;26:3479–3485. doi: 10.1016/j.biomaterials.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 254.Major TC, Brant DO, Burney CP, Amoako Ka, Annich GM, Meyerhoff ME, Handa H, Bartlett RH. Biomaterials. 2011;32:5957–5969. doi: 10.1016/j.biomaterials.2011.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Puiu SC, Zhou Z, White CC, Neubauer LJ, Zhang Z, Lange LE, Mansfield JA, Meyerhoff ME, Reynolds MM. J Biomed. Mater. Res. B. Appl. Biomater. 2009;91:203–212. doi: 10.1002/jbm.b.31391. [DOI] [PubMed] [Google Scholar]
- 256.Oh BK, Meyerhoff ME. Biomaterials. 2004;25:283–293. doi: 10.1016/s0142-9612(03)00530-1. [DOI] [PubMed] [Google Scholar]
- 257.Wonoputri V, Gunawan C, Liu S, Barraud N, Yee LH, Lim M, Amal R. ACS Appl. Mater. Interfaces. 2015;7:22148–22156. doi: 10.1021/acsami.5b07971. [DOI] [PubMed] [Google Scholar]
- 258.Ren H, Coughlin Ma, Major TC, Aiello S, Rojas Pena A, Bartlett RH, Meyerhoff ME. Anal. Chem. 2015:8067–8072. doi: 10.1021/acs.analchem.5b01590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Wu Y, Zhou Z, Meyerhoff ME. J Biomed. Mater. Res. A. 2007;81:956–963. doi: 10.1002/jbm.a.31105. [DOI] [PubMed] [Google Scholar]
- 260.Skrzypchak AM, Lafayette NG, Bartlett RH, Zhou Z, Frost MC, Meyerhoff ME, Reynolds MM, Annich GM. Perfusion. 2007;22:193–200. doi: 10.1177/0267659107080877. [DOI] [PubMed] [Google Scholar]
- 261.McCarthy CW, Guillory RJ, II, Goldman J, Frost MC. ACS Appl. Mater. Interfaces. 2016 doi: 10.1021/acsami.6b00145. [DOI] [PubMed] [Google Scholar]
- 262.Bloom BM, Grundlingh J, Bestwick JP, Harris T. Eur. J. Emerg. Med. 2014;21:81–88. doi: 10.1097/MEJ.0b013e32836437cf. [DOI] [PubMed] [Google Scholar]
- 263.Martin DS, Grocott MPW. Crit. Care Med. 2013;41 doi: 10.1097/CCM.0b013e31826a44f6. [DOI] [PubMed] [Google Scholar]
- 264.The Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. N Engl. J. Med. 2008;359:1464–1476. doi: 10.1056/NEJMoa0805017. [DOI] [PubMed] [Google Scholar]
- 265.Burns KEA, McLaren A. Can. Respir. J. 2009;16:163–165. doi: 10.1155/2009/751507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Marxer SM, Robbins ME, Schoenfisch MH. Analyst. 2005;130:206–212. doi: 10.1039/b412079e. [DOI] [PubMed] [Google Scholar]
- 267.Mowery KA, Schoenfisch MH, Baliga N, Wahr JA, Meyerhoff ME. Electroanalysis. 1999;11:681–686. [Google Scholar]
- 268.Schoenfisch MH, Mowery KA, Rader MV, Baliga N, Wahr JA, Meyerhoff ME. Anal. Chem. 2000;72:1119–1126. doi: 10.1021/ac991370c. [DOI] [PubMed] [Google Scholar]
- 269.Frost MC, Rudich SM, Zhang H, Maraschio MA, Meyerhoff ME. Anal. Chem. 2002;74:5942–5947. doi: 10.1021/ac025944g. [DOI] [PubMed] [Google Scholar]
- 270.Wu Y, Rojas AP, Griffith GW, Skrzypchak AM, Lafayette N, Bartlett RH, Meyerhoff ME. Sensors Actuators, B Chem. 2007;121:36–46. doi: 10.1016/j.snb.2006.09.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Yan Q, Major TC, Bartlett RH, Meyerhoff ME. Biosens. Bioelectron. 2011;26:4276–4282. doi: 10.1016/j.bios.2011.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Wolf AK, Qin Y, Major TC, Meyerhoff ME. Chinese Chem. Lett. 2015;26:464–468. [Google Scholar]
- 273.Shin JH, Marxer SM, Schoenfisch MH. Anal. Chem. 2004;76:4543–4549. doi: 10.1021/ac049776z. [DOI] [PubMed] [Google Scholar]
- 274.Frost MC, Wolf AK, Meyerhoff ME. Detection Challenges in Clinical Diagnostics. 2013:129–155. [Google Scholar]
- 275.Meruva RK, Meyerhoff ME. Biosens. Bioelectron. 1998;13:201–212. doi: 10.1016/s0956-5663(97)00097-3. [DOI] [PubMed] [Google Scholar]
- 276.Dobmeier KP, Charville GW, Schoenfisch MH. Anal. Chem. 2006;78:7461–7466. doi: 10.1021/ac060995p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Frost MC, Batchelor MM, Lee Y, Zhang H, Kang Y, Oh B, Wilson GS, Gifford R, Rudich SM, Meyerhoff ME. Microchem. J. 2003;74:277–288. [Google Scholar]
- 278.Major TC, Brant DO, Reynolds MM, Bartlett RH, Meyerhoff ME, Handa H, Annich GM. Biomaterials. 2010;31:2736–2745. doi: 10.1016/j.biomaterials.2009.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Major TC, Handa H, Annich GM, Bartlett RH. J Biomater. Appl. 2014;29:479–501. doi: 10.1177/0885328214538866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Stamler JS. Circ. Res. 2004;94:414–417. doi: 10.1161/01.RES.0000122071.55721.BC. [DOI] [PubMed] [Google Scholar]
- 281.Ghaffari A, Miller CC, McMullin B, Ghahary A. Nitric Oxide. 2006;14:21–29. doi: 10.1016/j.niox.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 282.Arora DP, Hossain S, Xu Y, Boon EM. Biochemistry. 2015;54:3717–3728. doi: 10.1021/bi501476n. [DOI] [PubMed] [Google Scholar]
- 283.Lu Y, Slomberg D, Sun B, Schoenfisch M. Small. 2013;9:2189–2198. doi: 10.1002/smll.201201798. [DOI] [PubMed] [Google Scholar]
- 284.Vumma R, Bang CS, Kruse R, Johansson K, Persson K. J Antibiot. (Tokyo) 2015:1–4. doi: 10.1038/ja.2015.112. [DOI] [PubMed] [Google Scholar]
- 285.McMullin BB, Chittock DR, Roscoe DL, Garcha H, Wang L, Miller CC. Respir. Care. 2005;50:1451–1456. [PubMed] [Google Scholar]
- 286.Barraud N, Kelso MJ, Rice SA, Kjelleberg S. Curr. Barraud, N., Kelso, M. J., Rice, S. A., Kjelleberg, S. (2015). Nitric Oxide A Key Mediat. Biofilm Dispersal with Appl. Infect. Dis. Curr. Pharm. Des. 21, 31–42.Pharmaceutical Des. 2015;21:31–42. [Google Scholar]
- 287.Barraud N, Hassett DJ, Hwang S-H, Rice Sa, Kjelleberg S, Webb JS. J Bacteriol. 2006;188:7344–7353. doi: 10.1128/JB.00779-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Barraud N, Storey MV, Moore ZP, Webb JS, Rice SA, Kjelleberg S. Microb. Biotechnol. 2009;2:370–378. doi: 10.1111/j.1751-7915.2009.00098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Nablo BJ, Schoenfisch MH. J Biomed. Mater. Res. A. 2003;67:1276–1283. doi: 10.1002/jbm.a.20030. [DOI] [PubMed] [Google Scholar]
- 290.Brisbois EJ, Bayliss J, Wu J, Major TC, Xi C, Wang SC, Bartlett RH, Handa H, Meyerhoff ME. Acta Biomater. 2014:4136–4142. doi: 10.1016/j.actbio.2014.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Schäffer MR, Efron PA, Thornton FJ, Klingel K, Gross SS, Barbul A. J Immunol. 1997;158:2375–2381. [PubMed] [Google Scholar]
- 292.Witte MB, Barbul A. Am. J. Surg. 2002;183:406–412. doi: 10.1016/s0002-9610(02)00815-2. [DOI] [PubMed] [Google Scholar]
- 293.Shi HP, Efron DT, Most D, Barbul A. Surgery. 2001;130:225–229. doi: 10.1067/msy.2001.115837. [DOI] [PubMed] [Google Scholar]
- 294.Richardson G, Benjamin N. 2002;105:99–105. [PubMed] [Google Scholar]
- 295.Romanowicz GE, He W, Nielsen M, Frost MC. Redox Biol. 2013;1:332–339. doi: 10.1016/j.redox.2013.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Nguyen T-K, Selvanayagam R, Ho KKK, Chen R, Kutty SK, Rice SA, Kumar N, Barraud N, Duong HTT, Boyer C. Chem. Sci. 2016;7:1016–1027. doi: 10.1039/c5sc02769a. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.