Abstract
Objective
Economic burden on families coping with end-stage cancer remains poorly understood. Advanced malignancy threatens financial stability of families and interventions are needed to buffer them from impoverishment. This study examined the relationship between subjective and objective assessments of financial burden on families (financial strain and stress, respectively); and identified potentially modifiable factors to inform intervention efforts.
Methods
Using national survey data, we analyzed responses from households that had recently experienced a cancer death; 176 of households provided information on financial strain; 158 provided data on financial stress. In addition to self-reported appraisals of financial burden, measures assessed elements of the cancer care experience, treatment, symptom burden, work impact, insurance coverage and demographics.
Results
Despite being well-insured, ~1/4 of respondents reported the cost of care was a major financial burden and a third used all or most of their savings. Financial strain and stress were moderately positively correlated (r = 0.46, p <.01). Higher financial stress scores were negatively correlated with decedent’s age at death (r=−0.34, p<.01) and minority respondents (“other” race) reported much higher financial stress (M=4.7; SD=3.2) than White (M=0.8; SD=1.4) or Black (M=1.6; SD=2.2) respondents (p<.001). Financial burden was also associated with no or limited insurance coverage, changes in employment, severe pain and nausea, and provider interactions during the cancer care experience (e.g., whether the MD paid attention to non-medical factors or having unanswered questions about medications) (p<.05 for all).
Conclusions
The cancer care experience, symptoms, and work impact were associated with financial burden and have important implications for research and practice.
BACKGROUND
End-of-life care in the United States is associated with high costs of care and related financial burden.[1] In fact, nearly a third of U.S. households affected by end-stage illness report having spent all or most of their savings on care-related expenses at the end of life, and a majority report feeling financially burdened.[2,3] Although previous studies have begun to describe the prevalence and correlates of economic burden at the end of life, our understanding about the complex interplay between care, health care coverage, and financial burden remains incomplete. Although economic stability has been linked with coping, health and well-being, financial burden on families affected by the death of a cancer patient remains understudied.[4–8] Moreover, the link between subjective and objective appraisals of economic burden at the end of life remains virtually unexplored.
For the purpose of this paper, financial burden is used as a broad term that denotes general economic hardship. Financial burden, however, also consists of two sub-concepts: (1) financial strain, which refers to subjective perceptions about financial burden; and (2) financial stress, which includes objective and practical aspects of financial burden, e.g., out-of-pocket expenses, lost wages, declarations of bankruptcy.[4,9,10] The conceptual distinction between these two variables is particularly relevant because heightened levels of financial strain has been observed by patients and families across the socio-economic spectrum.[4,9,10] Additionally, many dying patients express not wanting to burden their families financially, while family members often insist that financial matters are the least of their concerns.[11,12]
A recent systematic review of literature on financial stress and strain associated with terminal cancer resulted in only 13 studies conducted in the US.[3] All of the identified studies used some measure of financial stress, yet only four reported measures of financial strain – and none used a population-based sample. Based on the review, factors contributing to financial burden at the end of life include loss of income (e.g., reductions in work/job loss) for both the patient and family members, residential transitions, and increased burden of care.[3,8,10,11,13] Additionally, the presence of advance directives, end-of-life conversations with providers, and the election of palliative care services such as hospice, are associated with lower levels of financial burden.[3,14,15]
The cost implications of end-of-life care have in large part been evaluated in terms of savings for healthcare providers and insurers – but not families.[4,16] Informal caregivers, often spouses, play a primary role in providing care for patients with life-threatening illness.[17] Approximately a fifth of family caregivers provide full-time care, and the same proportion either quit a job or experiences major life transitions (e.g., relocating) to accommodate the patient’s care needs.[3] Nearly a third of caregivers spend most or all of their savings while providing care, [2,3] and the proportion is even higher among those dealing with high patient care needs.[11] Unfortunately, concerns about dwindling financial family resources are a barrier to care for patients with advanced illness[18] as patients may forego otherwise desirable treatments.[9,10,19–21]
The purpose of this study was two-fold. First, we examined the relationship between financial strain and stress. Second, we provide a more complete, nuanced understanding of the drivers of financial burden at the end of life. In particular, we focus on aspects of care and the disease experience that are potentially modifiable to inform future intervention efforts aimed at reducing financial burden among families facing life-threatening illness.
METHODS
In 2006, the Kaiser Foundation, the Harvard School of Public Health and USA Today commissioned a survey of US households affected by cancer.[22] Using random-digit dialing of landline phones, a national probability sample was established of households within which a cancer diagnosis had occurred or been treated in the past five years. Telephone interviews were conducted with 930 respondents who consented and were eligible (response rate 51%). Among these respondents, 179 (19.2%) reported that their family member with cancer had died. One outlier was removed from the sample pool because the decedent’s age was 9 years old. From the remaining cases, two samples were constructed based on the main outcomes: financial strain and financial stress. With respect to financial strain, two cases were removed from the analysis because respondents did not provide information about this outcome, leaving a total working sample of 176 (98% of the decedent sample) for the analysis of financial strain. Due to missing items on the measure of financial stress, only 158 cases (88% of the decedent sample) had complete data and were included in the analysis of financial stress.
Measures
Financial Strain
Financial strain was evaluated using responses to the following survey item: “How much of a burden is the cost of overall medical care, including any services needed to cope with cancer?” 1=not a burden at all; 2=minor burden; 3=major burden.
Financial Stress
Financial stress was assessed using nine (1=Yes/0=No) responses to the following stem question: “Did any of the following things ever happen as a result of the financial cost of dealing with cancer?: (1) used up most of savings; (2) unable to pay for basic necessities like food, heat or housing; (3) borrowed money or got a loan or another mortgage on home; (4) borrowed money from relatives; (5) contacted by a collection agency; (6) declared bankruptcy (7) sought the aid of a charity or public assistance (8) lost health insurance and (9) couldn’t buy health insurance because of having cancer.” These nine items were summed (range 0–9) where a score of 9 indicating the highest possible financial stress. For this study, financial stress items elicited an internal reliability coefficient of.79.
Cancer Care Experience
Family members provided (Yes/No) data on whether: health professionals provided conflicting information during treatment; doctor(s) paid attention to non-medical factors; there was confusion about prescribed medications; important questions went unanswered; and duplicate tests/diagnostic procedures were performed.
Cancer Treatment
The survey also included information about four types of cancer treatment the decedent may have had: chemotherapy, radiation, prescription drugs related to cancer treatment, and/or surgery (Yes/No).
Symptoms
The severity of patient’s side effects to cancer treatment was also rated on a four-point scale ranging from 0=not severe at all to 3=very severe. Specific side-effects included pain, nausea, and stress/anxiety.
Insurance Coverage
Respondents also answered whether they were surprised to find that the limit of costs covered by the health insurance plan for cancer treatment was reached (Yes/No).
Effect on Income/Employment
Respondents were also asked whether the diagnosis/treatment of cancer caused someone in the household to: (a) be unable to work or perform usual activities; (b) lose/change a job or work fewer hours; (c) have a lower income; (d) suffer emotional or psychological problems; and (e) have severe strains with other family members (Yes/No).
Demographics
Respondents also provided information about their age, gender, race/ethnicity, income, education and marital status. Characteristics of the deceased were also elicited, including age, gender, relationship to the respondent, and health insurance. Regarding this latter variable, survey items for health insurance asked specifically about type of coverage for health care costs – not disability coverage for lost employment income.
Analysis
Descriptive statistics were computed for all demographic variables stratified by financial strain and stress. Using SPSS version 18.0, t-tests and Pearson χ2 goodness-of-fit tests were conducted to examine associations between fixed characteristics and measures of financial burden. Additionally, the relationship between the subjective and objective assessments of financial burden was investigated using Spearman’s correlation coefficient and visual scatterplot.
Primary analyses fit generalized linear models[23] to the two outcome variables: financial strain and financial stress. Multinomial logistic regression was applied to relate potential predictors to financial strain because this outcome variable did not meet the assumptions required for modeling proportional odds. Financial stress was a count variable and, thus, a Poisson regression model was used to identify potential predictors. A fully specified model of financial strain, which includes an adjustment for financial stress, is offered as an online appendix.
RESULTS
Descriptive Analysis
Tables 1 and 2 report sample characteristics stratified by measures of financial strain and stress. The majority of respondents in the full sample were female (60.8%) and White (84.7%) with a mean age of 55.9 years (SD=17.8). Decedents were on average older (67.8 years; SD=13.4) and male (55.1%). Over half of respondents (51.1%) indicated experiencing some financial strain, whether major or minor; and, on average, respondents reported dealing with at least one component of financial stress (M=1.1, SD=1.8). Using all or most of one’s savings was the most commonly reported component of financial stress (32%).
Table 1.
Respondent Characteristics Stratified by Measures of Financial Stress and Strain
| Respondent Demographics | Financial Strain (N=176) | Financial Stress (N=158) | ||||||
|---|---|---|---|---|---|---|---|---|
| All | Major | Minor | None | P | All | M (SD) | P | |
| N | 176 | 40 | 50 | 86 | 158 | 1.1 (1.8) | ||
| Total, % | 100 | 22.7 | 28.4 | 48.9 | ||||
| Age, y | 55.9±17.8 | 53.8±16.3 | 53.3±20.2 | 58.6±16.7 | NS | 56.4±17.7 | P < .001a | |
| Gender, % | NS | NS | ||||||
| Male | 39.2 | 26.1 | 23.2 | 50.7 | 40.5 | 1.2 (1.8) | ||
| Female | 60.8 | 20.6 | 31.8 | 47.7 | 59.5 | 1.0 (1.7) | ||
| Race, % | NS | P < .001 | ||||||
| White | 84.7 | 22.1 | 27.5 | 50.3 | 84.2 | .8 (1.4) | ||
| Black | 6.8 | 16.7 | 41.7 | 41.7 | 7.6 | 1.6 (2.2) | ||
| Other | 3.4 | 50.0 | 16.7 | 33.3 | 3.8 | 4.7 (3.2) | ||
| Missing | 5.1 | 22.2 | 33.3 | 44.4 | 4.4 | 1.6 (1.8) | ||
| Ethnicity, % | NS | NS | ||||||
| Latino/Hispanic | 4.5 | 25.0 | 37.5 | 49.1 | 1.6 (1.8) | |||
| Non-Latino/Non-Hispanic | 95.5 | 22.8 | 28.1 | 37.5 | 4.4 | 1.1 (1.8) | ||
| Missing | .6 | 0 | 0 | 100.0 | 95.60 | 0 | ||
| Income, % | NS | NS | ||||||
| Less than $25,000 | 30.7 | 25.9 | 29.6 | 44.4 | 30.4 | 1.2 (1.9) | ||
| $25,000 – $50,000 | 25.6 | 17.8 | 20.0 | 62.2 | 25.9 | 1.0 (1.8) | ||
| $50,000 – $75,000 | 11.4 | 35.0 | 25.0 | 40.0 | 12.7 | 1.5 (2.2) | ||
| $75,000 – $100,000 | 6.3 | 18.2 | 54.5 | 27.3 | 5.7 | .9 (1.1) | ||
| $100,000 + | 7.4 | 15.4 | 23.1 | 61.5 | 7.6 | .8 (1.0) | ||
| Missing | 18.8 | 21.2 | 33.3 | 45.5 | 17.7 | .9 (1.5) | ||
| Education, % | NS | NS | ||||||
| Less than grade 12 | 9.7 | 35.3 | 23.5 | 41.2 | 10.1 | 1.6 (2.2) | ||
| Grade 12 or GED | 36.9 | 24.6 | 29.2 | 46.2 | 38.0 | 1.4 (2.0) | ||
| Bus/tech/voc school | 5.7 | 10.0 | 30.0 | 60.0 | 4.4 | 0 | ||
| Some college | 24.4 | 18.6 | 32.6 | 48.8 | 24.7 | 1.0 (1.6) | ||
| College graduate | 9.7 | 29.4 | 35.3 | 35.3 | 9.5 | 1.0 (1.6) | ||
| Post grad/grad school | 12.5 | 18.2 | 13.6 | 68.2 | 12.7 | .5 (1.1) | ||
| Missing | 1.1 | 0 | 50.0 | 50.0 | .6 | 0 | ||
| Marital Status, % | NS | P < .01 | ||||||
| Married/Living as married | 26.7 | 25.5 | 29.8 | 44.7 | 26.6 | 1.4 (1.7) | ||
| Divorced/Separated | 8.5 | 26.7 | 13.3 | 60.0 | 8.9 | 2.0 (2.4) | ||
| Widowed | 43.8 | 23.4 | 24.7 | 51.9 | 44.3 | .6 (1.1) | ||
| Never been married | 19.9 | 17.1 | 42.9 | 40.0 | 19.0 | 1.5 (2.3) | ||
| Missing | 1.1 | 0 | 0 | 100.0 | 1.3 | 0 | ||
P-value for Pearson’s correlation coefficient testing the relationship between respondent age and financial stress (r=−.30).
Note: Among racial categories, Bonferroni’s correction identified differences between the “other” racial group and white, black, and missing groups. A post hoc analysis of marital status identified a statistically significant difference between widowed and divorced/separated respondents, with widows reporting lower level of financial stress.
Table 2.
Decedent Characteristics Stratified by Measures of Financial Stress and Strain
| Decedent Demographics | Financial Strain (N=176) | Financial Stress (N=158) | ||||||
|---|---|---|---|---|---|---|---|---|
| All | Major | Minor | None | P | All | M (SD) | P | |
| N | 176 | 40 | 50 | 86 | 158 | 1.1 (1.8) | ||
| Total, % | 100 | 22.7 | 28.4 | 48.9 | ||||
| Relationship to Respondent | NS | P < .01 | ||||||
| Spouse/partner | 45.5 | 25.0 | 21.3 | 53.8 | 46.2 | .6 (1.1) | ||
| Child | 5.1 | 22.2 | 55.6 | 22.2 | 5.1 | 2.6 (1.4) | ||
| Parent | 38.6 | 19.1 | 32.4 | 48.5 | 38.6 | 1.4 (2.1) | ||
| Grandparent | 4.0 | 14.3 | 57.1 | 28.6 | 3.8 | 1.8 (3.1) | ||
| Other relative | 6.8 | 33.3 | 16.7 | 50.0 | 6.3 | 1.3 (1.4) | ||
| Gender, % | P < .05 | NS | ||||||
| Male | 55.1 | 20.6 | 36.1 | 43.3 | 55.1 | .9 (1.5) | ||
| Female | 44.9 | 25.3 | 19.0 | 55.7 | 44.9 | 1.3 (2.0) | ||
| Age, y | 67.8±13.4 | 64.0±14.4 | 67.5±13.5 | 69.7±13.4 | NS | 67.9±13.5 | P < .001a | |
| Insurance Coverage | ||||||||
| Covered by insurance, % | P < .05 | P < .01 | ||||||
| Yes | 90.9 | 19.4 | 30.0 | 50.6 | 91.1 | .9 (1.6) | ||
| No | 8.0 | 57.1 | 14.3 | 28.6 | 8.2 | 2.5 (2.4) | ||
| Missing | 1.1 | 50.0 | 0 | 50.0 | .6 | 3.0 | ||
P-value for Pearson’s correlation coefficient testing the relationship between decedent age and financial stress (r=−.34).
Note: In terms of the relationship with respondent, Bonferroni’s test found that spouses/partners had significantly less financial stress than did respondents who were children or parents. Time since diagnosis and type of insurance coverage were not associated with either financial stress or financial strain, and are not shown.
In terms of associations with financial strain, respondents from households in which the decedent was male (p=.043) were more likely to report minor financial strain than households in which the decedent was female. Additionally, respondents were more likely to report major financial strain when the decedent had no health insurance (p=.02) compared to decedents who had coverage. However, the type of insurance coverage was not associated with financial strain. Higher financial stress scores were negatively correlated with respondent’s age (r=−0.30, p<.01) and decedent’s age at death (r=−0.34, p<.01). Minority respondents who identified as “Other” race reported much higher financial stress (M=4.7; SD=3.2) than White (M=0.8; SD=1.4) and Black (M=1.6; SD=2.2) respondents (p<.001).
Respondents who were widowed had lower financial stress scores than respondents who were divorced/separated (p=.008). Also, spouses/partners of the decedent reported less financial stress than did children or parents of the decedent (p=.003). In terms of insurance type, those who answer that their decedents had Medicare also had lower financial stress scores than did decedents with no form of health insurance (p=.013). The potential confounding effect of age was found through the relationship between decedent’s age and financial stress scores.
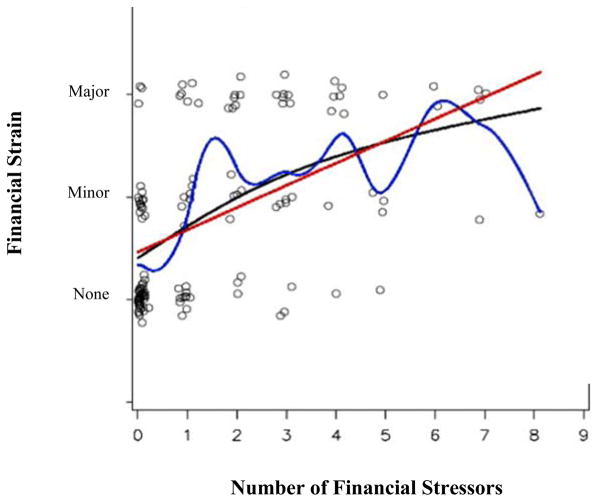
The Relationship between Financial Stress and Strain
As expected, financial stress and strain are positively associated (r=0.46, p<.01; see Figure 1); however this relationship is only moderately strong. The r2 value indicates that financial stress explains 21% of variation seen in subjective financial strain.
Figure 1.
The Relationship Between Financial Stress and Strain (N=158)
Note: Data points are kernelled to depict the number of cases by spreading each unique case around a single plot point. For example, in this figure the greatest number of cases is concentrated at zero indicators of stress and no strain. The regression line is the straight line summarizing predicted values assuming a linear relationship between financial stress and financial strain. The locally weighted line follows the largest concentration of cases across the regression line. The lowess curve illustrates predicted scores based on the assumption of a non-linear relationship.
Primary Analysis
Results of the multinomial logistic regression showed differences related to the cancer care experience, symptoms, insurance coverage, and the cancer’s effect on income and employment (Table 3). Regarding the cancer care experience, having received conflicting information from oncology providers (p=.015), getting duplicative tests or diagnostic procedures (p=.002), and having had confusion about medication prescribed (p=.020) were significant correlates distinguishing reports of ‘major financial strain’ from reports of ‘no financial strain at all.’ In terms of cancer symptoms, respondents who observed the decedent having severe pain (p=.014) and nausea (p=.047) prior to death were, respectively, 6.66 times and 4.12 times more likely to report major financial strain. Regarding insurance coverage, respondents who reached the limits of the decedents’ insurance coverage were 21.23 times more likely to indicate major financial strain (p=.002) and 29.40 times more likely to report minor financial strain (p<.001) compared to no burden at all. In reference to the impact of the cancer on income and employment, respondents who had a loss or change of job in the household were 11.43 times more likely to express major financial strain (p=.002) and lower odds of being in the minor financial strain group by 73% (p=.017). Also, respondents reporting a lower household income were 16.11 times more likely to experience major financial strain (p<.001). Neither time since diagnosis nor type of health insurance were associated with either financial stress or financial strain.
Table 3.
Illness-Related Factors Associated with Financial Strain and Stress among Households Affected by Cancer
| Variable | Financial Strain (N=176) | Financial Stress (N=158) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Major Burden | Minor Burden | ||||||||
| OR | 95% CI | P | OR | 95% CI | P | B | SE | P | |
| Cancer Care Experience | |||||||||
| Doctor paid attention to non-medical factors (Yes) | 1.07 | 0.41 – 2.78 | .891 | 0.99 | 0.39 – 2.50 | .975 | −0.46 | 0.20 | .025 |
| Received conflicting information (Yes) | 3.52 | 1.28 – 9.69 | .015 | 1.01 | 0.37 – 2.77 | .982 | 0.89 | 0.20 | <.001 |
| Had duplicate tests/diagnostic procedures (Yes) | 6.02 | 1.97 – 18.41 | .002 | 1.31 | 0.43 – 4.02 | .633 | 0.69 | 0.19 | <.001 |
| Important questions went unanswered (Yes) | 1.38 | 0.42 – 4.57 | .594 | 2.17 | 0.71 – 6.68 | .175 | 0.45 | 0.21 | .032 |
| Confusion about medication prescribed (Yes) | 3.61 | 1.22 – 10.69 | .020 | 0.65 | 0.24 – 1.79 | .406 | 0.49 | 0.20 | .016 |
| Cancer Treatment | |||||||||
| Radiation treatment (Yes) | 1.59 | 0.60 – 4.23 | .352 | 1.06 | 0.43 – 2.63 | .898 | 0.62 | 0.21 | .003 |
| Symptoms | |||||||||
| Severe pain (Yes) | 6.66 | 1.48 – 30.08 | .014 | 1.08 | 0.39 – 3.04 | .880 | 0.97 | 0.32 | .003 |
| Nausea (Yes) | 4.12 | 1.02 – 16.58 | .047 | 0.46 | 0.16 – 1.30 | .114 | 0.67 | 0.28 | .015 |
| Insurance Coverage | |||||||||
| Reached the limit of insurance coverage (Yes) | 21.23 | 2.98 – 151.32 | .002 | 29.40 | 4.34 – 199.39 | <.001 | 1.39 | 0.23 | <.001 |
| Effect on Income/Employment | |||||||||
| Unable to work or perform usual activities (Yes) | 3.79 | 0.69 – 20.87 | .126 | 0.55 | 0.16 – 1.82 | .324 | 0.96 | 0.31 | .002 |
| Loss or change of job in household (Yes) | 11.43 | 3.19 – 40.99 | <.001 | 0.17 | 0.04 – 0.73 | .017 | 0.64 | 0.20 | <.001 |
| Lowered household income (Yes) | 16.11 | 4.47 – 58.07 | <.001 | 0.59 | 0.19 – 1.84 | .364 | 1.18 | 0.22 | <.001 |
Note: Results are from a proportional odds ordinal logistic regression (for financial strain) and Poisson regression (financial stress). Models include adjustments for respondent age, gender, race, income, education, marital status, respondents’ relationship to the decedent, decedents’ age, gender and insurance coverage. For financial strain, absence of burden (i.e., a response of “not at all”) is the reference group. For all independent variables, findings refer to an affirmative (i.e., “yes”) response. Factors that were not associated with either financial stress or financial strain are excluded from the table. Non-significant factors included the following: cancer treatments of chemotherapy, prescription drugs, and surgery; having a negatively altered appearance due to cancer, and the presence of serious stress and anxiety.
Financial stress scores were significantly related to ‘doctor paid attention to non-medical factors’ (p=.025), ‘received conflicting information from providers’ (p<.001), ‘duplicate tests or diagnostic procedures’ (p<.001), ‘important questions went unanswered’ (p=.032), and ‘confusion about medication prescribed’ (p=.016). When respondents answered ‘no’ to these questions, they also tended to have lower scores of financial stress than those who indicated ‘yes’ – except with the item ‘doctor paid attention to non-medical factors.’ In terms of cancer treatment, households with decedents who did not receive radiation treatment had lower financial stress than others (p=.003). In regards to the effect of treatment, respondents of decedents who were able to work or go about usual activities had lower financial stress (p=.002). Severe pain (p=.003) and nausea (p=.015) in symptoms were significant correlates of financial stress, and having reached the limit of insurance coverage was also related to financial stress (p<.001). Moreover, respondents who did not experience loss or change of job in household and did not experience a reduction in household income had lower financial stress (p<.001).
CONCLUSIONS
Despite being well-insured, nearly a quarter of respondents in our sample reported the cost of care was a major financial burden and a third indicated using all or most of their savings. This suggests that end stage cancer is financially crippling for many US households. Based on our results, households with younger or minority (i.e., other race) cancer patients are especially at-risk for financial burden. Financial stress and strain were clearly linked to multiple elements of the cancer care experience, many of which involve communication between oncology care providers and families. Although financial stress and strain are indeed related (r=0.46, p<.01), they are not synonymous. A small portion of households (2%), for example, reported major financial strain, but no financial stress. As previous work suggests, it is possible that these families may be foregoing medical care in order to afford basic necessities.[9,10] Future intervention efforts may benefit by targeting both the affective elements of financial strain (e.g., feeling overwhelmed or emotionally distressed) and the pragmatic aspects of financial stress (e.g., medical debt, income loss).[9,10]
Interestingly, financial stress only explained 21% of the variance in financial strain. This corroborates previous work suggesting that these concepts, while related, are conceptually distinct.[9,10] In some cases elements of financial stress, while valid indicators of objective economic burden, may also provide families with a needed safety net to buffer against severe financial hardship. For example, behaviors, such as seeking aid from a charitable organization or getting a loan to deal with cancer-related costs, may provide households with a sense of needed relief and reduced financial strain. Additionally, the measure of financial stress did not capture current knowledge of financial status or respondent optimism, which may have been influential in the measure of financial strain.
Despite variations in the way these two concepts interface, results identified key factors related to financial burden that have important implications for research and practice. First, symptom burden during cancer treatment (i.e., presence of severe pain or nausea) is related to higher odds that the cost of care is a major burden. This lends support to the hypothesis that high quality pain and symptom management may not only improve quality of life, but lower out-of-pocket expenses as well. Alternately, the presence of severe pain, for example, may reflect costs associated with more advanced, complex and protracted disease. Future research is needed to isolate whether this relationship is a direct effect or whether confounders are at play.
Although respondents’ current household income was not statistically associated with either financial stress or strain, when cancer care impacted employment and household income, as expected, heightened levels of financial stress and strain were observed. For working age individuals, serious illness often involves a triple financial threat of: (1) the patient’s reduced ability to earn income; (2) the need for other family members to quit their job(s) or take time off to provide care; (3) and increased out-of-pocket expenses related to care.[24]
Based on our findings, insurance coverage is a very important protective factor that is strongly and consistently associated with reduced financial burden. Implementation of the Affordable Care Act (ACA) is changing the affordability and availability of health insurance in the US.[25] Although the full impact of the ACA is unknown, it appears to have provided several, much needed, improvements. For example, the law removed the dollar amount ceiling on covered care and benefits, while providing restrictions on out-of-pocket costs and deductibles.[25] That said, patients who are covered may still be financially responsible for significant co-pays and large deductibles – and certain treatments may not be covered under a given plan. Consequently, healthcare providers may work to reduce financial risks of insured patients by better informing them and their families about the costs, benefits and limits of their insurance coverage.
Households that had reached the limits of the decedent’s coverage were likely to report greater financial stress and strain. Safety nets and public assistance may help address the needs of families that have large deductibles, substantial copays, or minimal coverage. Future study is needed to better understand how to help those who have sub-optimal coverage. While few people would argue about the benefits of having health insurance, based on our findings, insurance coverage may also encourage patients/families to pursue expensive treatment options – options which may be difficult to discontinue once coverage ceases to pay, even when families cannot afford to pay the out-of-pocket expenses. For instance, households in which the deceased patient had received radiation treatment were more likely to report higher levels of financial strain. This may be indicative of gaps in coverage for radiotherapy. Alternatively, this may be indicative of protracted disease and extended periods of treatment as radiation is often a first line therapy for early stage cancer. Recent studies, however, suggest some cancer patients are being overtreated with radiation therapy.[26,27] Additionally, one study of older cancer patients receiving palliative radiation suggests financial burden may be hidden.[21] Thus, frank conversations about foregoing unnecessary radiation treatments may reduce financial burden on families, improve patient outcomes and lower costs to the healthcare system.
When doctors pay attention to non-medical factors such as social support and informal care networks, financial stress is lower. Although mobilizing natural support systems helps relieve some of the economic burden, this did not affect perceptions of financial strain on our sample. Duplicative tests or diagnostic procedures are associated with both financial stress and strain. The economic burden of redundant or unnecessary tests and procedures are well documented, both for families as well as payors. Clear communication with patients and families may help minimize economic problems for families. Respondents who reported receiving conflicting information, or did not get their questions answered, were more likely to report higher financial burden. Results may be indicative of costs associated with getting second opinions about a diagnosis or treatment options. There are a numerous of obstacles to good provider communication, however. Costs are not always readily apparent and communication about financial matters – especially within the context of treating life-threatening illness – is notoriously challenging. Intervention to minimize financial burden at the end-of-life must necessarily include strategies for cancer support professionals to broach this delicate issue in a tactful, empathetic and patient-centered manner.
Our results lend support for the National Comprehensive Cancer Network (NCCN) recommendations for distress screening in cancer patients, which includes screening for psychosocial needs. For example, the NCCN’s recommended Problem Checklist that accompanies the Distress Thermometer includes questions related to financial concerns, communication with the medical team, and understanding the illness and related treatment options. A comprehensive distress screening can facilitate open communication about financial burden and patient goals of care. Prompting such conversations may better inform patient-centered decision-making and guide interventions to address financial concerns.
Our findings should be considered with respect to our methodological and analytic limitations. The study relied on cross-sectional data, which limits the strength of our results in two ways. First, we are unable to establish direct causal links between selected predictor variables and financial stress or strain. Second, the lack of longitudinal data does not allow us to observe changes in respondent perceptions, or income levels, over time. Respondents may have been susceptible to social desirability bias as some respondents may have implicitly asserted that caring for their loved one was worth the cost regardless of expenses, treatment, or outcomes. Furthermore, data for this study were based on retrospective reports by bereaved respondents. Thus recall bias and psychological distress (e.g., grief) may have impacted responses. That said, outcomes were not associated with time since diagnosis. The generalizability of findings is also potentially limited by survey non-response, with a 51% response rate, and missing data, particularly with the measure of financial stress. To explore bias due to missing data on financial stress, we tested for differences in reported financial strain between those who had missing financial stress data (n=18) and those who had complete financial stress data (n=158). No statistically significant differences were identified (p=.567).
Although our measures of financial stress and strain have been in use for over two decades, translated into multiple languages, and tested/implemented with multiple diverse populations, [28,29] further validity testing is warranted to comprehensively evaluate their psychometric properties. Financial strain was operationalized using a single item with three response options. A wider range of response options would have improved potential for measurement variability and sensitivity. Additionally, respondents may have interpreted the item differently, since participants were not prompted with a definition of financial strain. Also, households that did not pursue treatments due to the expense may not have reported financial burden.[9] The measure of financial stress, which was evaluated using a cumulative count of affirmative responses to nine yes/no questions covering a range of potential stressors, was also limited. For example, this measure treated each of the nine items equally. Future research should examine the factor structure of this measure and consider allowing respondents to weigh the relative impact of each component of financial stress. Despite these limitations, our study uncovers key factors that may contribute to the financial burden associated with caring for a family member with terminal cancer – as well as potential targets for interventions to relieve such burden.
Our research builds upon previous research demonstrating that many families coping with terminal cancer are also dealing with substantial financial burden. While the ACA appears to be a step in the right direction, there is a dearth of clinical interventions to assist families with these economic concerns. Thus, there is a clear and pressing need to develop and test interventions to minimize financial burden on families coping with advanced cancer – and a truly holistic and patient/family-centered approach to care cannot neglect the economic impact of life-threatening illness on families.
Supplementary Material
Acknowledgments
The efforts of Drs. Cagle and Carr were supported in part by a T-32 training grant from the National Institute on Aging (NIA), 2T32AG000272-06A2. Dr. Cagle was additionally supported by NIA 5T32AG000212-19 and the National Palliative Care Research Center. The authors thank the Kaiser Family Foundation, USA Today, and the Harvard School of Public Health for their sponsorship of the original study and the Roper Center for use of their data. The authors would also like to thank Dr. Jolynn Pek for her guidance and consultation on the analysis.
Footnotes
The authors do not have any financial disclosures.
References
- 1.Economist Intelligence Unit. [Accessed July 23, 2013];The quality of death: ranking end-of-life care across the world. 2010 at: www.eiu.com/site_info.asp?info_name=qualityofdeath_lienfoundation&page=noads&rf=0.
- 2.Covinsky KE, Goldman L, Cook EF, Oye R, Desbiens N, Reding D, Cryer HG. The impact of serious illness on patients’ families. JAMA. 1994;272:1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 3.Plonk WM, Arnold RM. Terminal care: the last weeks of life. J of Pall Med. 2005;8:1042–1054. doi: 10.1089/jpm.2005.8.1042. [DOI] [PubMed] [Google Scholar]
- 4.Hanratty B, Holland P, Jacoby A, Whitehead M. Review article: Financial stress and strain associated with terminal cancer – a review of the evidence. Pall Med. 2007;21:595–607. doi: 10.1177/0269216307082476. [DOI] [PubMed] [Google Scholar]
- 5.Choi NG. Relationship between life satisfaction and post retirement employment among older women. Int J Aging Hum Dev. 2001;52:45–70. doi: 10.2190/2W25-DH9H-2F4D-7HWX. [DOI] [PubMed] [Google Scholar]
- 6.Dolan P, Peasgood T, White M. Do we really know what makes us happy? A review of the economic literature on the factors associated with subjective well-being. J Econ Psychol. 2008;29(1):94–122. [Google Scholar]
- 7.James BD, Boyle PA, Bennett JS, Bennett DA. The impact of health and financial literacy on decision making in community-based older adults. Gerontology. 2012;58(6):531–539. doi: 10.1159/000339094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yabroff KR, Lund J, Kepka D, Mariotto A. Economic burden of cancer in the United States: estimates, projections, and future research. Cancer Epidemiol Biomarkers Prev. 2011;20(10):2006–2014. doi: 10.1158/1055-9965.EPI-11-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Francoeur RB. Reformulating financial problems and interventions to improve psychological and functional outcomes in cancer patients and their families. J Psychsoc Onc. 2001;19(1):1–20. [Google Scholar]
- 10.Francoeur RB. Use of an income equivalence scale to understand age-related changes in financial strain. Res Aging. 2002;24(4):445–472. doi: 10.1177/01627502024004003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emanuel EJ, Fairclough DL, Slutsman BA, Emanuel LL. Understanding economic and other burdens of terminal illness: the experience of patients and their caregivers. Ann Intern Med. 2000;132(6):451–459. doi: 10.7326/0003-4819-132-6-200003210-00005. [DOI] [PubMed] [Google Scholar]
- 12.McPherson CJ, Wilson KG, Murray MA. Feeling like a burden to others: a systematic review focusing on the end of life. Pall Med. 2007;21(2):115–128. doi: 10.1177/0269216307076345. [DOI] [PubMed] [Google Scholar]
- 13.Cagle JG, Kovacs PJ. Caregivers of cancer patients: Perceptions of preparedness and the need for support during hospice care. J Gerontol Soc Work. 2011;54(1):92–115. doi: 10.1080/01634372.2010.534547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, Spragens L, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168(16):1783–90. doi: 10.1001/archinte.168.16.1783. [DOI] [PubMed] [Google Scholar]
- 15.Zhang B, Wright AA, Huskamp HA, Nilsson ME, Maciejewski ML, Earle CC, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480–8. doi: 10.1001/archinternmed.2008.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zick CD, Fan JX, Chang KL. Impending widowhood and health care spending. Soc Sci Res J. 2004;33(3):538–555. [Google Scholar]
- 17.Burridge LH, Barnett AG, Clavarino AM. The impact of perceived stage of cancer on carers’ anxiety and depression during the patients’ final year of life. Psychooncology. 2009;18:615–23. doi: 10.1002/pon.1435. [DOI] [PubMed] [Google Scholar]
- 18.Boockvar K, Meier D. Frail Older Adults and Palliative Care - Reply. JAMA. 2007;297(11):1194–1195. doi: 10.1001/jama.297.11.1194-b. [DOI] [PubMed] [Google Scholar]
- 19.Chao LW, Pagán JA, Soldo BJ. End-of-life medical treatment choices: do survival chances and out-of-pocket costs matter? Med Decis Making. 2008;28(4):511–523. doi: 10.1177/0272989X07312713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Francoeur RB. Cumulative financial stress and strain in palliative radiation outpatients: The role of age and disability. Acta Oncol. 2005;44(4):369–381. doi: 10.1080/02841860510029761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Francoeur RB. The influence of age on perceptions of anticipated financial inadequacy by palliative radiation outpatients. Patient Educ Couns. 2007;69(1–3):84–92. doi: 10.1016/j.pec.2007.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaiser Family Foundation. National survey of households affected by cancer. Accessed at: http://kaiserfamilyfoundation.files.wordpress.com/2013/01/7590.pdf.
- 23.Nelder JA, Baker RJ. Generalized linear models. John Wiley & Sons, Inc; 1972. [Google Scholar]
- 24.Buckheit J. [Accessed on May, 6 2014];Cost of caring for aging parents could be next financial crisis. 2008 from: http://www.agingcare.com/Press-Releases/financial-crisis-for-family-caregivers-146294.htm.
- 25.Patient Protection and Affordable Care Act, Pub L No. 111–148, 124 Stat 119, 42 USC (2010).
- 26.Mitchell JM. Urologists’ use of intensity-modulated radiation therapy for prostate cancer. N Engl J Med. 2013;369:1629–1637. doi: 10.1056/NEJMsa1201141. [DOI] [PubMed] [Google Scholar]
- 27.Bekelman JE, Epstein AJ, Emanuel EJ. Single-vs multiple-fraction radiotherapy for bone metastases from prostate cancer. JAMA. 2013;310:14, 1501–1502. doi: 10.1001/jama.2013.277081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blendon RJ, Schoen C, DesRoches CM, et al. Inequalities in health care: a five-country survey. Health Affairs. 2002;21:182–191. doi: 10.1377/hlthaff.21.3.182. [DOI] [PubMed] [Google Scholar]
- 29.Donelan K, Blendon RJ, Schoen C, et al. The elderly in five nations: the importance of universal coverage. Health Affairs. 2000;19:226–235. doi: 10.1377/hlthaff.19.3.226. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.