Abstract
Objective
Given the public health importance of improving dietary behavior in chronic disease prevention in low- and middle-income countries it is crucial to understand the factors influencing dietary behavior in these settings. This study tested the validity of a conceptual framework linking individual and environmental factors to dietary behavior among Ecuadorian adolescents aged 10–16 years.
Methods
A cross-sectional survey was conducted in 784 school-going Ecuadorian adolescents in urban and rural Southern Ecuador. Participants provided data on socio-economic status, anthropometry, dietary behavior and its determining factors. The relationships between individual (perceived benefits and barriers, self-efficacy, habit strength, and a better understanding of healthy food) and environmental factors (physical environment: accessibility to healthy food; social environment: parental permissiveness and school support), and their association with key components of dietary behavior (fruit and vegetables, sugary drinks, breakfast, and unhealthy snack intake) were assessed using structural equation modeling.
Results
The conceptual model performed well for each component of eating behavior, indicating acceptable goodness-of-fit for both the measurement and structural models. Models for vegetable intake and unhealthy snacking showed significant and direct effects of individual factors (perceived benefits). For breakfast and sugary drink consumption, there was a direct and positive association with socio-environmental factors (school support and parental permissiveness). Access to healthy food was associated indirectly with all eating behaviors (except for sugary drink intake) and this effect operated through socio-environmental (parental permissiveness and school support) and individual factors (perceived benefits).
Conclusion
Our study demonstrated that key components of adolescents’ dietary behaviors are influenced by a complex interplay of individual and environmental factors. The findings indicate that the influence of these factors varied by type of dietary behavior.
Introduction
Globally, 42 million children are overweight or obese—the consequence of a staggering 47.1 percent rise in prevalence between 1980 and 2013 [1]. A rise no longer exclusive to high-income countries as the prevalence of childhood and adolescent overweight and obesity has also reached alarmingly high levels in low- and middle-income countries (LMICs). In Latin-America 25 percent of children and adolescents are overweight or obese [2]. Nearly half of all overweight children under 5 years of age now live in Asia, and a further 25 percent are found in Africa [3, 4]. Poor dietary behavior is a key factor in the onset of obesity and an important contributor to the global disease burden [5]. Despite the accumulation of evidence illustrating unhealthy food practices among young people in LMICs [6–8], the determinants of their dietary behavior remains poorly understood.
Behavioral theories and conceptual frameworks have been recommended to identify and better understand influences on dietary behavior [9], but their utility for use in adolescents in LMICs is limited. Firstly, the majority of theories to date have been developed for American or European adults [10]; testing their validity for use in other cultures and local contexts, has rarely been undertaken [11, 12]. Furthermore, the age groups the models apply to have not been specified [13]. As such, they may neither be applicable nor transferable to young people living in LMICs. Secondly, much of what is known about the individual (e.g. self-efficacy and habit strength) and environmental (e.g. parental permissiveness and accessibility) factors influencing dietary behavior comes from qualitative studies [14, 15]. Few attempts have been made to use well-articulated, i.e. evidence- and theory-based, conceptual models to i) identify factors that adequately reflect the social and cultural reality of young people in LMICs [16–18] and ii) quantify the pathways and their strength by which individual and environmental factors interact and affect, both directly but also indirectly, dietary behaviors [19, 20].
A recent qualitative theory-based study we undertook in Ecuadorian adolescents showed that “healthy foods”, such as fruit and vegetables, were perceived as vital to healthful eating. This study resulted in a composite framework (evidence- and theory-based), in which eating behavior was conceptualized as the result of individual and environmental influences [21]. In the present study, we sought to further the evidence of this conceptual model by identifying and quantifying the relationships (direct and indirect) between factors and their influence on key components of dietary behavior. Our study focused on four components, fruit and vegetables, sugary drinks, breakfast, and unhealthy snack intake. They correspond with how adolescents viewed healthy eating [21] and reflect important problems with their current dietary behavior [7]. Furthermore, each of these components has been independently associated with a high risk of obesity and/or chronic diseases: high intakes of specific foods such as sugary drinks [22] and processed foods [23] has been associated with obesity and its related diseases and weight gain, respectively; erratic behaviours such as skipping breakfast has been shown to be associated with obesity [24]; and diets low in fruit and vegetables and whole grains, nuts and seeds, and seafood omega-3 fatty acids were shown to be associated with high risk of chronic diseases [5].
Methods
Design and study population
This study used data from a cross-sectional survey that was conducted in Ecuador from January 2008 to April 2009. Participants were 10–16 year old adolescents (n = 784) from an urban (Cuenca) and rural (Nabón) area in Ecuador. A different sampling frame was used for each area: all school-going children willing to participate were included in Nabón, while a two-stage cluster design was used (with schools as primary and classes as secondary sampling units) in Cuenca. Adolescents were excluded if they were pregnant, followed a special diet or suffered from a severe medical or physical disorder. A detailed description of the sample and study procedures is given elsewhere [25].
Ethics, consent and permission
The study protocol was granted ethical approval from Ecuadorian (University Central in Quito; CBM/cobi-001) and Belgian (Ghent University Hospital; 2008/462—FWA00002482) Ethical Committees. Informed assent was obtained from all participants. Parents/guardians provided written informed consent.
Measurements
Data were collected at school during class time by a research team extensively trained according to a predefined protocol and training manual.
Socio-demographic attributes
Data on age, gender (male/female), geographic location (urban/rural) and socio-economic status (SES) were collected. The latter was assessed using a method developed by the Integrated Social Indicator System for Ecuador [26], based on World Bank recommendations to develop household surveys in LMICs [27]. This method measures poverty using the “Unsatisfied Basic Needs” criteria and classifies a household as poor when it lacks access to one or more basic needs (such as education, health, nutrition, housing, urban services and employment opportunities). Using this method, participants were classified into two groups: “Poor” and “Better off”.
Anthropometric measurements
Anthropometric measurements were carried out in duplicate by two trained researchers. Adolescents wore light clothing but no shoes during the measurements. Height was measured to the nearest 0.1 cm with a portable stadiometer (model PORTROD, Health O Meter, USA) and body weight to the nearest 0.1 kg using a digital calibrated balance (model SECA 803, Seca GmbH & CO, Hamburg, Germany). Adolescents were then classified into age- and sex-specific Body Mass Index (BMI) categories (underweight, healthy weight, overweight and obese) according to the International Obesity Task Force criteria [28, 29].
Dietary behavior
Food intake was measured using two interview-administered 24h dietary recalls on a randomly selected weekday and weekend day. Local household measures (cups, bowls, etc.) were calibrated and used by the trained interviewers to quantify the amount of food consumed. A food composition database was compiled using databases from the US (USDA, 2012), Mexico (INNSZ, 1999), Central America (INCAP/OPS, 2012) and Peru (CENAN/INS, 2008). When detailed information on the ingredients and/or cooking methods of a recipe was unavailable, recipes were prepared in triplicate by local volunteers. The ingredients used, and their weights, were measured and averaged to obtain a final estimate for the recipe. For locally processed and pre-packed food items, food labels were used to obtain the food composition.
Data for the four components of dietary behavior were extracted from both 24h recalls. Fruit and vegetable intake were examined separately and combined. Sugary drinks included all soft drinks, fizzy drinks, energy drinks, and juices with added sugar. Breakfast was defined as a meal consumed between 5:00–7:00 am or 5:00–8:00 am for adolescents in schools with a morning or afternoon schedule, respectively. Unhealthy snacks were defined as foods rich in sodium, fat or sugar (e.g. sweets, salty snacks, and any other packaged food) eaten as a morning, afternoon or evening refreshment. Sugary drinks and fruit and/or vegetable intake were calculated as the total average daily intake (g/day) over both days to best represent habitual intake. Breakfast and intake from unhealthy snacks were expressed as a percentage of daily energy intake averaged over both days (E %/day).
Assessment of individual and environmental factors influencing dietary practices
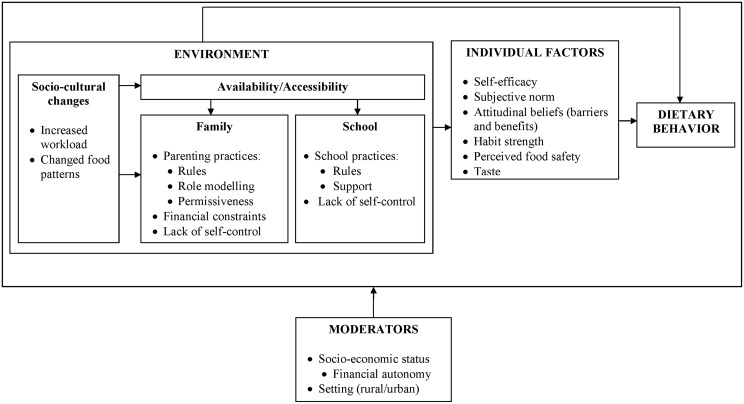
The conceptual framework including key individual and environmental factors for dietary behavior is illustrated in Fig 1 [21]. A self-administered questionnaire was used to quantify each factor. As no culturally appropriate and validated psychometric scales to measure these factors existed, a questionnaire was developed using qualitative data from this population [21], relevant literature [30], and the expertise of the research team. The questionnaire was piloted for understanding and readability with a group of school-going adolescents (11–15 y old) not included in this study using cognitive interviewing (a qualitative process encompassing two main techniques: think aloud interviewing and verbal probing) [31]. As part of this pretesting, the questionnaire was administered twice with a four week interval. Both single and multiple items were used to measure factors (i.e. constructs) in the framework; socio-cultural changes and lack of self-control were not measured. Items in the questionnaire were measured using 5-point interval scales. Items were recoded into the same direction so that higher construct scores corresponded to the most favorable conditions for healthy dietary practices (e.g. a high score on perceived barriers indicates fewer barriers to eat healthily). Sum scores were calculated for each construct. The outcome variables were left unchanged.
Fig 1. Conceptual framework for healthy dietary behavior in an Ecuadorian population.
Statistical analysis
Anthropometric, socio-demographic and questionnaire data were entered in duplicate in Epidata (Version 3.14, Odense Denmark) by two researchers. Food intake was entered using an online software package designed for 24h dietary recalls (Lucille software 0.1, 2010, Ghent University; http://www.foodscience.ugent.be/nutriFOODchem/foodintake).
Data on food intake, anthropometry, socio-demographics, questionnaire and construct validity were analyzed using Stata (Intercooled Stata version 12 Statacorp, college station, TX, USA). Descriptive data were reported as percentages or as means and SDs for normally and as medians and IQRs for non-normally distributed variables. Statistical significance was set at an alpha level of 0.05 and all tests were two-sided. Differences in means or proportions of variables were assessed using survey commands in Stata to account for clustering. Skewed continuous variables were transformed to improve normality.
Construct validity analyses
A comprehensive assessment of each scale’s quality was performed [32]. Item distribution and variation were examined using descriptive analyses. Internal consistency of each construct was examined using Cronbach’s alpha; values of alpha > 0.50 were considered acceptable as i) it was a newly developed questionnaire and ii) some constructs included only a few items [33]. Repeatability (test-retest) of the questionnaire was examined using the ICC to assess absolute agreement between single items or the sum scores of the constructs; values of ICC > 0.30 were considered to be acceptable.
Structural Equation Modeling
Structural Equation Modeling (SEM) was conducted to statistically test the inter-relationships of constructs and their relationship with the four components of dietary behavior in our participant population [34]. SEM is a multivariate technique that allows for the modeling of a series of hypothesized relationships simultaneously. It combines aspects of factor analysis and multiple regression and allows for the inclusion of observed and unobserved (latent) variables (i.e., theoretical constructs) to determine whether the hypothesized associations are consistent with data of the participant population [35, 36]. Prior to modeling the relationship between latent variables, a measurement model was evaluated for each component of dietary behavior. This step involves a confirmatory factor analysis to confirm the relationship between the latent variables (constructs) and their indicator variables (items). The following step, i.e. the testing of the structural model, estimates the strength of the relationships between these latent variables. It also allows for examining the direct and indirect effects among the constructs in the model. Data were examined prior to modeling to ensure they met assumptions of performing a SEM and analyzed using the robust maximum likelihood procedure in LISREL 8.72 [37]. Using multi-level SEM with a small number of clusters (< 100; in our study: 34) and low ICC (<0.25, in our study: < 0.10) has been shown to produce inaccurate results. So even though a cluster sampling design was used, we applied regular SEM [38].
First, correlation coefficients were calculated between the variables of interest. All correlations were <0.70, thus multi-collinearity was not a concern in the present data [39]. Path coefficients were then estimated and the general fit of the model was assessed for each component of dietary behavior. To evaluate the goodness of fit of the model, the χ²-value together with degrees of freedom were calculated, as well as four other indices: the root mean square error of approximation (RMSEA), the normed fit index (NFI), the non-normed fit index (NNFI) and the comparative fit index (CFI). The χ²-value has traditionally been used to test the hypothesis that the relationships suggested in the model provide a plausible explanation of the data, i.e. how well the proposed model structure fits the structure in the observed data set. It is however sensitive to sample size; a large sample size increases the power to reject the models. Other fit indexes have been proposed to compensate for this problem. The RMSEA is a measure of discrepancy between the true population model and the hypothesized model with unknown but optimally chosen parameter estimates. In other words, it favors a more parsimonious model with fewer parameters. It is relatively insensitive to sample size, since it is a population-based index [40]. The CFI and NNFI both compare the fit of the hypothesized model to that of a baseline or null model, where all parameters are assumed to be independent. Values below 0.08 for RMSEA [41] and above 0.90 for NFI, NNFI and CFI [35] indicate an acceptable fit of the data to the hypothesized model. One requirement for using SEM for model testing is complete data with no missing values. To minimize exclusion of observations from the analyses, imputation of missing data values of constructs was performed using the expectation-maximization algorithm (1000 iterations) for those included in SEM analysis [42]. Separate SEM analyses were conducted for each of the dietary behaviors.
Results
Participant characteristics
Of the 784 adolescents recruited, n = 751 (of which 50.4% were male, and n = 594 came from urban areas) were included in the final SEM analysis. Those excluded lacked data on anthropometry (n = 5), dietary behavior (n = 5), socio-demographic factors (n = 5) or on individual/environmental factors (n = 18). Excluded adolescents represented 4.2% of the initial sample. They did not differ in terms of mean age (P = 0.87) and sex (P = 0.81), but excluded adolescents tended to be poorer (P = 0.03).
Mean age of the included participants was around 14 years (Table 1); 20.1% of the adolescents were overweight or obese and 4.5% were underweight. More than half of the participants (55%) had low SES; nearly all poor adolescents came from rural areas. BMI was significantly lower in poor adolescents when compared to their peers who were better-off. Age and gender did not differ by SES.
Table 1. Participant characteristics.
| Variables | Total (n = 751) | Poor (n = 415) | Better-off (n = 336) | P value* |
|---|---|---|---|---|
| Male (%) | 50.4 | 47.2 | 54.1 | 0.25 |
| Age (mean y (SD)) | 13.6 (1.2) | 13.7 (1.3) | 13.6 (1.1) | 0.82 |
| Urban (%) | 79.0 | 64.3 | 97.3 | <0.001 |
| BMI (kg/m²) | 20.3 (3.1) | 20.0 (2.9) | 20.6 (3.3) | 0.04 |
*Differences in means or proportions of variables were assessed using survey commands in Stata to account for clustering.
Key components of dietary behavior
Median fruit and vegetable intake was limited, while median sugary drink intake was substantial in our population (Table 2). Over one-fifth of daily energy intake came from unhealthy snacking, similar to the E% originating from breakfast. Breakfast intake among the poor was significantly higher and sugary drink intake significantly lower compared to the better-off adolescents. No other differences in dietary behavior by SES were found.
Table 2. Key components of dietary behaviour as measured by two 24h dietary recalls.
| Dietary behaviour | Total (n = 751) | Poor (n = 415) | Better-off(n = 336) | Difference (Poor—better-off) | P value* | |||
|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | |||
| Fruit (g/d) | 121.8 | 156.6 | 126.2 | 154.8 | 114.6 | 158.6 | 11.6 | 0.83 |
| Vegetables (g/d) | 49.7 | 56.7 | 50.3 | 62.2 | 49.4 | 50.0 | 0.9 | 0.48 |
| Fruit and vegetables (g/d) | 180.8 | 177.0 | 186.1 | 175.6 | 174.4 | 181.3 | 11.7 | 0.48 |
| Sugary drinks (g/d) | 150.0 | 300.0 | 99.0 | 237.5 | 201.6 | 346.2 | –102.6 | 0.03 |
| Breakfast (E%/d) | 21.6 | 13.6 | 23.1 | 13.6 | 19.4 | 12.1 | 3.7 | 0.002 |
| Unhealthy snacking (E%/d) | 22.2 | 31.0 | 20.0 | 30.9 | 24.6 | 30.8 | –4.6 | 0.13 |
*Differences in means or proportions of variables were assessed using survey commands in Stata to account for clustering.
IQR, Inter Quartile Range.
Construct validity
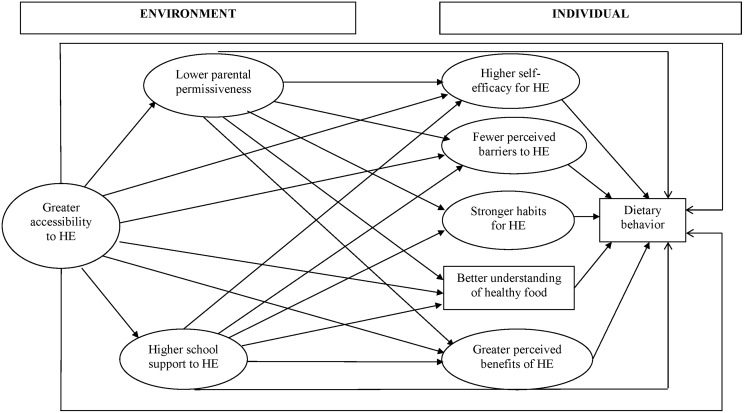
Internal consistency (Cronbach’s alpha) and repeatability (ICC) were acceptable to good for most of the constructs. Subjective norm, parental rules, parental modeling, school rules and taste did not meet the internal consistency or repeatability criteria, however, and were not used in the model. The retained constructs and their items, ICC and Cronbach’s alpha are presented in Table 3. The resulting framework, which we validated using SEM analysis is shown in Fig 2. For ease of interpretation, constructs are presented as the most favorable conditions for healthy dietary practices.
Table 3. Cronbach’s alpha and Intra-class Correlation Coefficient for retained constructs in the model at individual and environmental level.
| Constructs | Items | Cronbach’s alpha | ICC sum score |
|---|---|---|---|
| Individual level | |||
| Self-efficacy | Suppose you want to eat healthily. How hard is it for you to eat healthy every day? | 0.66 | 0.58 |
| Suppose you want to eat healthily. How hard is it for you to eat healthy at home? | |||
| Suppose you want to eat healthily. How hard is it for you to eat healthy at school? | |||
| Attitudinal beliefs | |||
| Perceived benefits | If I eat healthily it helps me to control my body weight | 0.64 | 0.31 |
| If I eat healthily it makes me feel better | |||
| Perceived barriers | Unhealthy food is cheaper | 0.71 | 0.44 |
| Healthy food is not available when I am eating | |||
| Healthy foods don’t taste good | |||
| I’ve been eating fast food since I was young | |||
| My parents don’t have time to cook healthy food | |||
| My body needs unhealthy food | |||
| Breaks at school are too short to eat healthily | |||
| I eat unhealthily because I want to eat the same as my friends | |||
| Habit strength | I eat snacks or fast food when I watch TV | 0.56 | 0.46 |
| I eat snacks or fast food when I go out with friends | |||
| I eat snacks or fast food when I am going to sports training | |||
| I eat snacks or fast food when I go on a family trip | |||
| Understanding of what constitutes a healthy food | Eating healthily is eating food without chemicals* | NA | 0.22 |
| Environmental level (home and school environment) | |||
| Parental permissiveness | My parents let me eat fast food (“Pitty’s”, French fries, hamburgers, etc.) and snacks (ice cream, jelly, candies, etc.) whenever I want to | 0.51 | 0.53 |
| My parents let me drink sodas whenever I want to | |||
| School support | How often does your school/teachers encourage you to eat healthily? | 0.76 | 0.40 |
| How often do your teachers/school give you information regarding healthy eating? | |||
| Accessibility to healthy food | My family can’t afford to buy healthy food | 0.62 | 0.47 |
| There is no weekly market in my neighbourhood | |||
| Healthy food that is sold around my place is spoiled | |||
| The places selling healthy food are far from my house | |||
ICC, Intraclass Correlation Coefficient; NA, Not Applicable.
* when recoded, a better understanding of what constitutes a healthy food was scored as positive for healthy dietary practices.
Fig 2. Specification of a SEM for predicting dietary behavior, including mediation effects.
Rectangles indicate observed variables, and ellipses latent variables. HE: Healthy Eating.
Structural equation modeling: conceptual framework
Goodness-of-fit of the models
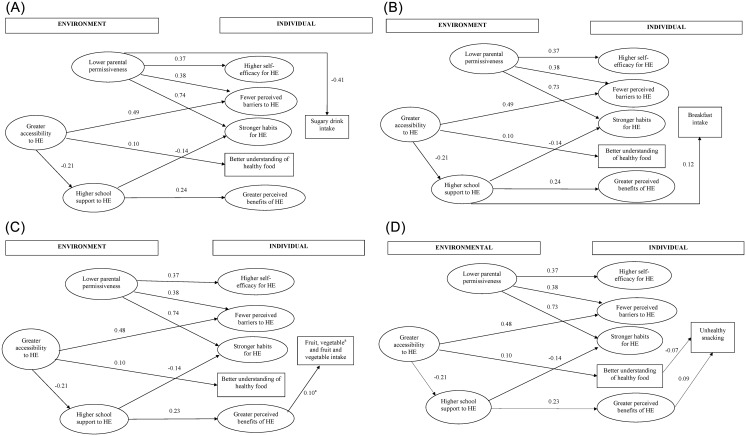
The confirmatory factor loadings were significant at the 0.05 level and ranged from 0.40 to 0.86. The overall fit of the measurement model was adequate (χ²(271) = 503,72, p< 0.001; RMSEA = 0.034; NNFI = 0.94; CFI = 0.95, GFI = 0.95). Using these same fit criteria, the overall fit of the structural models predicting fruit, vegetable, fruit and vegetables, unhealthy snacking, sugary drinks, and breakfast intake was also adequate (See Fig 3A–3D for details).
Fig 3.
(A) Individual and environmental influences on sugary drink consumption. Only statistically significant paths at P < 0.05 are shown. Goodness of Fit-statistics: χ²(303) = 630.18, p< 0.001; RMSEA = 0.038; NNFI = 0.92; CFI = 0.93, GFI = 0.93. HE: Healthy Eating. (B) Individual and environmental influences on breakfast consumption. Only statistically significant paths at P < 0.05 are shown. Goodness of Fit-statistics: χ²(303) = 630.50, p< 0.001; RMSEA = 0.038; NNFI = 0.92; CFI = 0.93, GFI = 0.94. HE: Healthy Eating. (C) Individual and environmental influences on fruit, vegetable and fruit and vegetable consumption. Only statistically significant paths at P < 0.05 are shown. Goodness of Fit-statistics: χ²(303) = 623.69, p< 0.001; RMSEA = 0.038; NNFI = 0.92; CFI = 0.93, GFI = 0.94. a significant pathway for vegetable intake only. HE: Healthy Eating(D) Individual and environmental influences on unhealthy snacking. Only statistically significant paths at P < 0.05 are shown. Goodness of Fit-statistics: χ²(303) = 619.19, p< 0.001; RMSEA = 0.037; NNFI = 0.92; CFI = 0.93, GFI = 0.94. HE: Healthy Eating.
Interrelationships of the constructs
The majority of the hypothesized inter-relationships of individual and environmental factors were confirmed and appeared to be similar for each of the dietary behaviors (See Fig 3A–3D for details). A strong and expected relationship in the model was the link between greater accessibility to healthy food in the environment and fewer perceived barriers to eating healthily. Greater accessibility was also associated with a better understanding of healthy food, meaning that greater access to healthy foods was related to perceiving healthy foods more in function of their nutritional value rather than their added chemicals (e.g. colorants, chemicals, etc.). Greater accessibility was also inversely associated with higher support from the school to eat healthily, i.e. if healthy food is more accessible, there is less support from the school. Having less permissive (i.e. stricter) parents was directly associated with higher self-efficacy, fewer perceived barriers and stronger habits for healthy eating. The relationship between parental permissiveness and stronger habits for healthy eating was the strongest in the model, suggesting that adolescents with more permissive parents had stronger unhealthy eating habits. Furthermore, greater school support was associated with higher perceived benefits of eating healthily and negatively associated with stronger habits for healthy eating.
Sugary drink intake
Lower parental permissiveness was inversely associated with sugary drink intake, indicating that adolescents of more permissive parents consumed more sugary drinks. None of the individual factors were related to sugary drink intake (Fig 3A).
Breakfast consumption
School support to healthful eating predicted breakfast consumption, meaning that a more supportive environment at school to eat healthily increased the consumption of breakfast in adolescents. Additionally, the perceived accessibility to healthy foods in the environment was associated with breakfast consumption indirectly through its influence on school support (Fig 3B). This suggests that a lower accessibility to healthy food is related to a more supportive school environment to eat healthily, which is in its turn positively associated with breakfast consumption.
Fruit, vegetable, and fruit and vegetable intake
In contrast to both previous models, none of the environmental factors were directly associated with fruit, vegetable or fruit and vegetable intake (Fig 3C). Adolescents perceiving strong benefits of eating healthily ate more vegetables, though significant, the strength of this association was rather low. This association was not significant for fruit intake or fruit and vegetable intake combined. The indirect relationship between greater school support and higher vegetable intake operated through perceived benefits and in its turn, greater school support to eating healthily was influenced by lower accessibility to healthy food. Thus, adolescents’ perception of a greater accessibility to healthy food in the environment indirectly increased their vegetable intake.
Unhealthy snacking
Greater perceived benefits of eating healthily were directly associated with more unhealthy snacking, and the indirect relationship between higher accessibility to healthy food and unhealthy snacking was facilitated by greater school support and greater perceived benefits (Fig 3D). The estimated associations indicate that lower accessibility to healthy food is related to more school support to eat healthily and a better understanding of the importance of healthy eating (perceived benefits). Surprisingly, the latter was associated with a higher intake of unhealthy snacks. Furthermore, a better understanding of healthy food was inversely and directly associated with the consumption of unhealthy snacks. This better understanding of healthy food mediated the relationship between the perceived accessibility to healthy foods and consuming unhealthy snacks. Thus, adolescents reporting low access to healthy foods were less likely to believe that the quality of healthy foods is associated with nutritional value, which may explain their higher consumption of unhealthy snacks.
Discussion
Using SEM, we quantified the relationships between factors and their influence on key components of dietary behavior. The models tested for each of these components performed well, indicating the validity of the conceptual model for our population. These models confirmed the interdependence of factors within and across individual and environmental (physical and social) levels. The fact that these relationships were comparable, both in strength and direction, across behaviors suggests that the interrelationship between environmental and individual factors for dietary behavior were near-identical. How these factors affected the dietary behavior, however, varied by behavior. This finding is in line with previous research documenting that factors affecting dietary behavior differ by type of behavior [19, 43–46].
Only individual level factors (perceived benefits of eating healthily) were found to be directly related to vegetable intake and unhealthy snacking. Interestingly, perceived benefits of eating healthily was directly associated with both increased vegetable and unhealthy snack intake. This somewhat puzzling result may have different explanations. In our adolescent population, choosing to eat healthily (e.g. vegetables) was found to be associated with an untrendy image leading to teasing and marginalization [21]. Eating unhealthy snacks might thus have helped with peer acceptance. In addition, adolescents who are convinced of the benefits of eating healthily and who eat more vegetables, may think they are allowed to also eat unhealthy snacks. Alternatively, it might be that their parents allow them to snack as a reward for eating vegetables [47].
A better understanding of healthy food was a direct and inverse predictor of unhealthy snack intake. Our qualitative work showed that “healthy foods” were often associated with the absence of colorants or other chemical substances rather than with nutritional value of the food [21]. Apparently, this poor understanding of what healthful food entails led to an increased preference for unhealthy snacks. This finding argues for strategies tackling safety risk communication to support healthier food choices.
Only socio-environmental factors were directly associated with sugary drinks and breakfast intake. Having more permissive parents directly and very strongly predicted higher sugary drinks intake, while greater school support for healthful eating directly and strongly predicted higher breakfast intake. Prior studies have similarly reported evidence of parental permissiveness and social support as significant predictors of soft drink and breakfast consumption respectively, in children aged 10–12 years old [48]. In our previous work in this population, adolescents indicated that their parents or school staff had little influence over their food choices [21]. They may thus not want to admit or want to minimize the influence their social environment has on their dietary practices, or they are not consciously aware of it. Furthermore, these results confirm that parents and schools play an important role in some behaviors but not all [21].
We also found that the physical environment, i.e. access to healthy food, was associated indirectly with all dietary behaviors (except for sugary drink intake) and this effect operated through socio-environmental (school support) and individual (perceived benefits of healthy eating, a better understanding of healthy foods) factors. As would be expected, greater accessibility to healthy food increased its consumption (e.g. increased vegetable intake). However, some of the indirect relationships found for accessibility appear more difficult to interpret. The relationships between accessibility and the consumption of breakfast and vegetable intake was mediated through a supportive school environment. Schools supported healthful eating when its access was limited. This finding reflects that they may not see a need to promote and support healthful eating when healthy options are easily available and accessible. The physical environment had no direct impact on any behavior. Thus, one can conclude that individual influences and the social environment are stronger and direct predictors of behavior than the physical environment in our population for certain behaviors. This confirms previous findings from high-income countries that socio-environmental factors are more important than physical environmental factors for healthful eating [19, 49]. As a consequence, simply improving accessibility to healthy food may be insufficient to improve dietary behavior; complementary strategies to address the individual and socio-environmental influences may also be required.
To our knowledge, this is the first study examining the validity of a conceptual model for (multiple components of) dietary behavior in young people from LMICs. This study is unique in the sense that we evaluated a comprehensive conceptual model that was guided by theory and validated using locally collected evidence. Additionally, the individual and environmental factors in the model were constructed meticulously and thus reflect the local context of our adolescent study population. A limitation is that the cross-sectional nature of the data do not allow one to infer causality of the estimated associations. Intervention studies are needed to assess the extent to which changes in factors may lead to actual changes in dietary behavior. Another possible limitation is the use of 24h dietary recall data. This commonly used method may suffer from systematic over- or under-reporting, it depends on the accurate recall of intake and portion size as with all retrospective methods, and may not representing habitual intake. Every attempt was made to collect the highest quality data. Our study enumerators were extensively trained, a food recall kit with locally used household measures was used to assist in portion sizes estimates, and the 24h recall was conducted twice to represent habitual intake. More importantly, random measurement error or a systematic over- or underestimation would not have affected the SEM coefficient estimates reported in this study. Differences in breakfast and sugary drink intake were found between poor and better-off adolescents. We refrained from performing subgroup analyses by SES, however, for two reasons. First, the large majority of better-off adolescents come from urban areas, which means that this variable was as much a proxy for urban/rural residence as it was for SES. Second, we did not have sufficient statistical power to test for differences between subgroups.
Conclusion
Our finding that dietary behaviors in adolescents are determined by a complex interplay of behaviour-specific individual and environmental factors, has implications for interventions. Interventions targeted to promote healthy dietary practices in our population should develop strategies that i) simultaneously address factors at the individual (e.g. knowledge), social (e.g. school staff and peers) and physical environmental (e.g. accessibility) level; ii) have a multipronged focus in addressing different dietary behaviours. These implications are in line with previous recommendations made for intervention development in LMICs [12].
The extent to which the development of interventions in other LMIC settings need to take culture- and context-related factors into account requires further investigation. This includes research on the validity of evidence- and theory-based models, i.e. investigating the inter-relationships of the influencing factors and their relationship with dietary behavior in LMICs. However, as gathering such evidence is a lengthy and time-intensive process, research to develop valid, feasible and faster ways to map such influencing contextual factors and their relationships with behavior should be a priority. Easy-to-use tools for the development of infant and young child feeding interventions have been developed in the past [50, 51]. These could serve as a guide for the development of tools for the intervention design in adolescent populations in LMICs.
Abbreviations
- LMICs
Low-and Middle-Income Countries
- SES
Socio-Economic Status
- BMI
Body Mass Index
- SD
Standard Deviation
- IQR
Inter Quartile Range
- ICC
Intraclass Correlation Coefficient
- SEM
Structural Equation Modeling
- RMSEA
Root Mean Square Error of Approximation
- NFI
Normed Fit Index
- NNFI
Non-Normed Fit Index
- CFI
Comparative Fit Index
- HE
Healthy Eating
Data Availability
There are ethical considerations regarding participant data collected within the project "food, nutrition, and health", Cuenca University which cautions the authors to make this data publicly available. Data is however available upon request from rverstraeten@itg.be OR angelica.ochoa@ucuenca.edu.ec.
Funding Statement
RV and AO received a grant from the Flemish Inter-University Council, VLIR-IUC (http://www.vliruos.be/en/project-funding/programdetail/institutional-university-cooperation_3948/). The research was funded by VLIR-IUC and Nutrition Third World (http://www.nutrition-ntw.org/). The funders had no role in study design, data collection, data analysis and interpretation of the data, decision to publish, or preparation of the manuscript.
References
- 1.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rivera JA, de Cossío TG, Pedraza LS, Aburto TC, Sánchez TG, Martorell R. Childhood and adolescent overweight and obesity in Latin America: a systematic review. The Lancet Diabetes & Endocrinology. 2013. [DOI] [PubMed] [Google Scholar]
- 3.UNICEF W, World Bank. Levels and Trends in Child Malnutrition: UNICEF-WHO-World Bank Joint Child Malnutrition Estimates New York: UNICEF; WHO, Geneva: WHO; Washington DC: World Bank, 2015. [Google Scholar]
- 4.IFPRI. Global Nutrition Report 2015: Actions and Accountability to Advance Nutrition and Sustainable Development. Washington, DC: 2015. [Google Scholar]
- 5.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60. 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nago ES, Lachat CK, Huybregts L, Roberfroid D, Dossa RA, Kolsteren PW. Food, energy and macronutrient contribution of out-of-home foods in school-going adolescents in Cotonou, Benin. British Journal of Nutrition. 2010;103(2):281–8. 10.1017/S0007114509991668 [DOI] [PubMed] [Google Scholar]
- 7.Ochoa-Avilés A, Verstraeten R, Lachat C, Andrade S, Van Camp J, Donoso S, et al. Dietary intake practices associated with cardiovascular risk in urban and rural Ecuadorian adolescents. A cross-sectional study. Submitted for publication to BMC Public Health. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perichart-Perera O, Balas-Nakash M, Rodriguez-Cano A, Munoz-Manrique C, Monge-Urrea A, Vadillo-Ortega F. Correlates of Dietary Energy Sources with Cardiovascular Disease Risk Markers in Mexican School-Age Children. Journal of the American Dietetic Association. 2010;110(2):253–60. 10.1016/j.jada.2009.10.031 [DOI] [PubMed] [Google Scholar]
- 9.Baranowski T, Cerin E, Baranowski J. Steps in the design, development and formative evaluation of obesity prevention-related behavior change trials. International Journal of Behavioral Nutrition and Physical Activity. 2009;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lubans DR, Foster C, Biddle SJH. A review of mediators of behavior in interventions to promote physical activity among children and adolescents. Preventive Medicine. 2008;47(5):463–70. 10.1016/j.ypmed.2008.07.011 [DOI] [PubMed] [Google Scholar]
- 11.Cerin E, Barnett A, Baranowski T. Testing Theories of Dietary Behavior Change in Youth Using the Mediating Variable Model with Intervention Programs. Journal of Nutrition Education and Behavior. 2009;41(5):309–18. 10.1016/j.jneb.2009.03.129 [DOI] [PubMed] [Google Scholar]
- 12.Verstraeten R, Roberfroid D, Lachat C, Leroy JL, Holdsworth M, Maes L, et al. Effectiveness of preventive school-based obesity interventions in low- and middle-income countries: a systematic review. Am J Clin Nutr. 2012;96(2):415–38. 10.3945/ajcn.112.035378 [DOI] [PubMed] [Google Scholar]
- 13.Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. Are current health Behavioral change models helpful in guiding prevention of weight gain efforts? Obesity Research. 2003;11:23S–43S. [DOI] [PubMed] [Google Scholar]
- 14.Share M, Stewart-Knox B. Determinants of food choice in Irish adolescents. Food Quality and Preference. 2012;25(1):57–62. [Google Scholar]
- 15.Baranowski T, Jago R. Understanding the mechanisms of change in children's physical activity programs. Exercise and Sport Sciences Reviews. 2005;33(4):163–8. [DOI] [PubMed] [Google Scholar]
- 16.Bisogni CA, Jastran M, Seligson M, Thompson A. How People Interpret Healthy Eating: Contributions of Qualitative Research. J Nutr Educ Behav. 2012;44(4):282–301. 10.1016/j.jneb.2011.11.009 [DOI] [PubMed] [Google Scholar]
- 17.Stead M, McDermott L, MacKintosh AM, Adamson A. Why healthy eating is bad for young people's health: Identity, belonging and food. Social Science & Medicine. 2011;72(7):1131–9. [DOI] [PubMed] [Google Scholar]
- 18.Lubans DR, Morgan PJ, Callister R, Collins CE, Plotnikoff RC. Exploring the Mechanisms of Physical Activity and Dietary Behavior Change in the Program X Intervention for Adolescents. Journal of Adolescent Health. 2010;47(1):83–91. 10.1016/j.jadohealth.2009.12.015 [DOI] [PubMed] [Google Scholar]
- 19.Ball K, Timperio AF, C D.A. Understanding environmental influences on nutrition and physical activity behaviors: where should we look and what should we count? International Journal of Behavioral Nutrition and Physical Activity. 2006;3:33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kremers SPJ. Theory and practice in the study of influences on energy balance-related behaviors. Patient Education and Counseling. 2010;79(3):291–8. 10.1016/j.pec.2010.03.002 [DOI] [PubMed] [Google Scholar]
- 21.Verstraeten R, Van Royen K, Ochoa-Avilés A, Penafiel D, Holdsworth M, Donoso S, et al. A conceptual framework for healthy eating behavior in Ecuadorian adolescents: a qualitative study. PLOS One. 2014;9(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity andobesity-related diseases. Obesity reviews. 2013;14:606–19. 10.1111/obr.12040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lioret S, Touvier M, Lafay L, Volatier JL, Maires B. Dietary and physical activity patterns in French children are related to overweight and socioeconomic status. Journal of Nutrition. 2008;138(1):101–7. [DOI] [PubMed] [Google Scholar]
- 24.Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y, et al. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: A meta-analysis. Preventive Medicine. 2011;53(4–5):260–7. 10.1016/j.ypmed.2011.08.030 [DOI] [PubMed] [Google Scholar]
- 25.Ochoa-Avilés A, Andrade S, Huynh TTT, Verstraeten R, Lachat C, Rojas R, et al. Prevalence and socioeconomic differences of risk factors of cardiovascular disease in Ecuadorian adolescents. Pediatr Obes. 2012;7:274–83. 10.1111/j.2047-6310.2012.00061.x [DOI] [PubMed] [Google Scholar]
- 26.Sistema Integrado de Indicadores Sociales del Ecuador (SIISE). Indicadores de SIISE, Necesidades básicas insatisfechas. Acces. 2013. Available: http://www.siise.gob.ec/Publicaciones/2inf7.pdf.
- 27.Grosh M, Glewwe P. Designing household survey questionnaires for developing countries: lessons from 15 years of the living standards measurement study. Volumes 1, 2, and 3. World Bank. 2013. Available: http://econ.worldbank.org/WBSITE/EXTERNAL/EXTDEC/EXTRESEARCH/EXTLSMS/0,,contentMDK:21556161~menuPK:4196884~pagePK:64168445~piPK:64168309~theSitePK:3358997,00.html.
- 28.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. British Medical Journal. 2000;320(7244):1240–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. British Medical Journal. 2007;335(7612):194–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vereecken C, De Henauw S, Maes L, Moreno L, Manios Y, Phillipp K, et al. Reliability and validity of a healthy diet determinants questionnaire for adolescents. Public Health Nutrition. 2009;12(10):1830–8. 10.1017/S1368980008004655 [DOI] [PubMed] [Google Scholar]
- 31.Collins D. Pretesting survey instruments: An overview of cognitive methods. Quality of Life Research. 2003;12(3):229–38. [DOI] [PubMed] [Google Scholar]
- 32.Peters GY. The alpha and the omega of scale reliability and validity. The European Health Psychologist. 2014;16(2):56–69. [Google Scholar]
- 33.Nunnally JC. Psychometric Theory. New york: McGraw—Hill; 1967. 1967. [Google Scholar]
- 34.Stephenson MT, Holbert RL, Zimmerman RS. On the use of structural equation modeling in health communication research. Health communication. 2006;20(2):159–67. 10.1207/s15327027hc2002_7 . [DOI] [PubMed] [Google Scholar]
- 35.Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. 1989. [Google Scholar]
- 36.Hair J, Black W, Babin B, Anderson R, Tatham R. Multivariate data analysis. New Jersey: Pearson Education, Inc.; 2006. 2006. [Google Scholar]
- 37.Jöreskog KG, Sörbom D. LISREL 7: A guide to the program and applications. Chicago: IL SPSS Inc.; 1989. 1989. [Google Scholar]
- 38.Hox JJ, Maas CJM. The Accuracy of Multilevel Structural Equation Modeling With Pseudobalanced Groups and Small Samples. Structural Equation Modeling-A Multidisciplinary Journal. 2001;8(2):157–74. [Google Scholar]
- 39.Tabachnick BG, Fidell LS. Using multivariate statistics. 4th edition ed Massachusetts: Allyn & Bacon; 2001. 2001. [Google Scholar]
- 40.Loehlin JC. Latent Variable Models—An Introduction to Factor, Path, and Structural-Analysis. Third edition ed: Mahwah, NG Lawrence Erlbaum Ass; 1998. 1998. [Google Scholar]
- 41.Browne M, Cudeck R, Bollen K, Long J. Testing structural equation models Alternative ways of assessing model fit. Newbury Park: CA: Sage; 1993. p. 136–62. [Google Scholar]
- 42.Dempster AP, Laird NM, Rubin DB. Maximum Likelihood from Incomplete Data Via Em Algorithm. Journal of the Royal Statistical Society Series B-Methodological. 1977;39(1):1–38. [Google Scholar]
- 43.van Osch L, Beenackers M, Reubsaet A, Lechner L, Candel M, De Vries H. Action planning as predictor of health protective and health risk behavior: an investigation of fruit and snack consumption. International Journal of Behavioral Nutrition and Physical Activity. 2009;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McNeill LH, Wyrwich KW, Brownson RC, Clark EM, Kreuter MW. Individual, social environmental, and physical environmental influences on physical activity among black and white adults: A structural equation analysis. Annals of Behavioral Medicine. 2006;31(1):36–44. [DOI] [PubMed] [Google Scholar]
- 45.Lau RR, Quadrel MJ, Hartman KA. Development and Change of Young-Adults Preventive Health Beliefs and Behavior—Influence from Parents and Peers. Journal of Health and Social Behavior. 1990;31(3):240–59. [PubMed] [Google Scholar]
- 46.Ishii K, Shibata A, Oka K. Environmental, psychological, and social influences on physical activity among Japanese adults: structural equation modeling analysis. International Journal of Behavioral Nutrition and Physical Activity. 2010;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ritchie LD, Welk G, Styne D, Gerstein DE, Crawford PB. Family environment and pediatric overweight: What is a parent to do? Journal of the American Dietetic Association. 2005;105(5):S70–S9. [DOI] [PubMed] [Google Scholar]
- 48.Verloigne M, Van Lippevelde W, Maes L, Brug J, De Bourdeaudhuij I. Family- and school-based correlates of energy balance-related behaviours in 10-12-year-old children: a systematic review within the ENERGY (EuropeaN Energy balance Research to prevent excessive weight Gain among Youth) project. Public Health Nutr. 2012;15(8):1380–95. 10.1017/S1368980011003168 [DOI] [PubMed] [Google Scholar]
- 49.Brug J, Kremers SP, van Lenthe F, Ball K, Crawford D. Environmental determinants of healthy eating: in need of theory and evidence. Proc Nutr Soc. 2008;67(3):307–16. 10.1017/S0029665108008616 [DOI] [PubMed] [Google Scholar]
- 50.Dickin K, Griffiths M. Designing by dialogue A program planners' guide to consultative research for improving young child feeding 1997. 1997. [Google Scholar]
- 51.Organization WH. ProPAN: Process for the Promotion of Child Feeding—A tool to improve infant and young child feeding Washington D.C.: PAHO; 2013. [updated 2013]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
There are ethical considerations regarding participant data collected within the project "food, nutrition, and health", Cuenca University which cautions the authors to make this data publicly available. Data is however available upon request from rverstraeten@itg.be OR angelica.ochoa@ucuenca.edu.ec.