Abstract
Objectives
Whether knee instability contributes to the increased risk of falls and fractures observed in persons with knee osteoarthritis (OA) has not been studied. We examined the association of knee buckling with the risk of falling and fall-related consequences in older adults with, or at high risk for, knee OA.
Methods
At the 60 month visit of the Multicenter Osteoarthritis Study, men and women ages 55 to 84 were asked about knee buckling in the past 3 months and whether they fell when a knee buckled. Falls and fall-related injuries in the past 12 months and balance confidence were assessed at 60 and 84 months. Multivariate logistic regression was used to assess the association of knee buckling with falls and their consequences.
Results
1,842 subjects (59% women, mean [SD] age= 66.9 [7.8] and BMI= 30.3 [5.7]) were included. At 60 months 16.8% reported buckling and at 84 months 14.1% had recurrent (≥2) falls. Bucklers at 60 months had a 1.6 to 2.5-fold greater odds of recurrent falls, fear of falling and poor balance confidence at 84 months. Those who fell when a knee buckled at baseline had a 4.5-fold, 2-fold and 3-fold increased odds two years later of recurrent falls, significant fall injuries and fall injuries that limited activity, respectively, and were 4 times more likely to have poor balance confidence.
Conclusion
Interventions that reduce knee buckling may help prevent falls, fall-related injuries and adverse psychological consequences of falls in persons with knee OA.
Keywords: Falls, knee osteoarthritis, knee instability
INTRODUCTION
Knee buckling, the sudden loss of postural support across the knee during weight bearing, often described as a knee “giving way”, is a symptom of knee instability that frequently affects older individuals, especially those with knee pain.(1, 2) In the community-based Framingham OA study, 12% of persons ages 58 to 94 reported one or more episode of knee buckling over a 3 month period, with nearly 80% occurring in knees that were painful in the past 30 days.(2) Among participants in the Multicenter Osteoarthritis Study (MOST) with knee OA, or with a high risk of developing it based on the presence of risk factors, 18% reported a knee giving way in the past 3 months and 1 in 8 of these said they fell when their knee buckled.(3) In addition to knee buckling, another 18% of MOST participants reported having less severe symptoms of knee instability (sensations of “shifting” or “slipping”) during the past 3 months even though they did not experience knee buckling during this period.
Symptoms of knee instability are associated with loss of confidence in one's knees,(4, 5) loss of balance confidence overall, fear of falling (3) and functional limitation (2, 3, 6-8) independently of knee pain. Falls, fall injuries and fear of falling due to knee buckling may exacerbate the adverse consequences of knee instability, leading to restrictions in physical activity, deconditioning and loss of strength and function. Symptoms of instability such as knee shifting, slipping and buckling are not the predominant symptom of knee OA and as such may be ignored by treating professionals. Muscle weakness in persons with knee OA increases the risk of instability symptoms (2, 6) and knee instability may be related to balance problems. Both balance difficulties and muscle weakness are remediable problems,(9-12) suggesting that the causes of knee instability may be treatable. If knee instability leads to serious health outcomes like falls, fall injuries and poor balance confidence, inquiring into and addressing instability may need to be prioritized.
The objective of the present study of participants in the MOST cohort was to examine the association of knee buckling and sensations of knee shifting/slipping at baseline with the cross-sectional and longitudinal risk of recurrent falls, fall injuries and adverse psychological consequences of falls.
MATERIALS AND METHODS
Subjects
Subjects were from the Multicenter Osteoarthritis Study (MOST), a longitudinal study of people with knee OA or at high risk of knee OA based on the presence of risk factors.(13, 14) Community-dwelling participants between 50 and 79 years were enrolled in Birmingham, Alabama, or Iowa City, Iowa between April 2003 and April 2005, with follow-up visits every 24-30 months and phone follow-up for those not coming to the clinic. Participants eligible for this analysis attended the 60 month clinic visit, which is the baseline for the present study. The MOST study protocol was approved prior to data collection by the Institutional Review Boards at the University of Alabama at Birmingham, the University of Iowa, the University of California, San Francisco and Boston University Medical Center.
Exposure variables
Symptoms of knee instability: buckling and shifting/slipping
At 60 months participants were asked “In the past 3 months, has either of your knees buckled or given way at least once?” and asked about buckling in the past 12 months using a similar question. Participants were also asked about the number of times a knee buckled in the past 3 months, and whether he or she had a fall and landed on the floor or the ground as a result of a knee giving way. All participants were then asked “In the past 3 months has either knee felt like it was shifting, slipping, or going to give way but didn't actually do so?” and the number of times this occurred. Hereafter, we will refer to this as knee shifting/slipping. Some participants reported only buckling, others only sensations of slipping/shifting, and still others both symptoms of instability in the past 3 months. All participants were asked “Because of concern about buckling or ‘giving way’ in your knees, have you changed or limited your usual activities in any way?”
Outcome variables
Falls
At 60 and 84 month clinic visits and phone contacts participants were asked about recent falls as follows: “During the past 12 months, have you fallen and landed on the floor, ground, or stairs? (Do NOT include being knocked down by a moving person or vehicle, falling off of a bicycle or while playing a sport or falling from a height, like off a ladder.)” Participants who fell were asked the number of times this had occurred in the past 12 months, if they were injured and about the type of injury and whether the injury had caused them to seek medical care or to limit their usual activities for more than a day. We considered significant injuries to include fractures, any injury that resulted in seeking medical treatment as well as sprained or strained joints or muscles, and any injury to the head.
A specific measure of balance confidence was obtained using the validated Activities-specific Balance Confidence (ABC) Scale, which assesses self-reported confidence in performing 16 activities without becoming unsteady or falling.(15) The summary ABC score ranges from 0 to 100 (higher scores indicate more confidence), with poor confidence defined as a score <67.(16) Fear of falling was assessed using a single-item question: “Are you ever afraid of falling?” with fear of falling coded as yes; no, if otherwise.
Baseline covariates
Covariates were selected based on a potential for a causal association with knee instability and buckling, on the one hand, and falls and their consequences, on the other hand, as reported in the literature or observed in the present study. Knee pain was assessed with the 5-item WOMAC knee pain scale.(17) We categorized subjects by quartile of the sum of pain scores for both knees combined (range 0-40). Participants were asked about pain “on most days of a month” over the past year in each hip and about foot and ankle pain occurring on “most days of the past 30 days” by referring to predefined locations on a distal lower extremity diagram, which yields a count of the number of locations (0-6) with pain in the right and left foot and ankle. History of knee injuries that limited activity for 2 or more days was assessed at 60 months. Radiographic knee OA was based on the Kellgren and Lawrence (KL) grade in the worse knee at 60 months, using previously described methods. (13, 18)
We used a self-report adaptation of the Charlson index, which provides a co-morbidity score with a range of 0-10.(19) Participants were categorized as users/nonusers in the past 30 days of prescription narcotic analgesics and sedative-hypnotics, including benzodiazapines and nonbenzodiazapine sleep aids and anxiolytics, based on an inventory of participant-supplied medication bottles and self-report.(20) The Center for Epidemiologic Studies Depression Scale(21) was administered and subjects were categorized based on scores of ≥ 16 vs. <16. Participants ages 65 and over were administered the Fillit brief cognitive impairment screening questionnaire,(22) with scores of ≥8 for those not using medications, and ≥12 for those using medications, considered suggestive of impairment.
Quadriceps strength was assessed at the 60 month visit as the maximum of four isokinetic knee extensor torque repetitions at 60 degrees/second, scaled by body weight.(23) Results in newton-meters (nm) for the weaker limb were used, and normalized as gender-specific z-scores. Vibratory perception was evaluated bilaterally using a biothesiometer placed on the dorsum of the 1st MTP joint.(24) Results in volts were normalized as gender-specific z-scores for analysis. Body mass index (BMI) was calculated as the ratio of measured weight (kg) divided by height (m) squared. Other baseline covariates were age, gender, race (white vs. African-American) and clinic site.
Statistical analysis
We focused on the association of knee instability in native knees at 60 months with fall outcomes at 60 and 84 months. We excluded those who had a total knee replacement prior to 60 months and in longitudinal analyses those who had a knee replacement prior to 84 months.
For exposure variables we classified participants based on knee buckling in the 3 months prior to baseline and separately for instances of knee shifting/slipping without buckling. We categorized both variables as 0, 1 and ≥2 instances of instability; however, initial analyses showed no differences for 1 vs. ≥2 episodes in association with falls, so only results for 0 vs. ≥1 instances are presented. We classified participants at baseline for whether they reported only buckling, only knee shifting/slipping or both buckling and shifting/slipping, and classified bucklers by whether they reported having fallen when a knee gave way. We estimated odds ratios for the association of baseline buckling and shifting/slipping with the risk of the outcomes of 1 fall and with 2 or more falls at baseline and at follow-up 24 months later using multinomial logistic regression and odds ratios for dichotomous consequences of falls using logistic regression. Analyses were also conducted to assess whether buckling with a fall at baseline was associated with recurrent falls and consequences of falls and we limited these analyses to outcomes occurring during follow-up 2 years later to avoid counting the same falls in the exposure and outcome variable. All models include both buckling and shifting/slipping variables based on previous findings of independent associations with outcomes (3) and are adjusted for all covariates.
In sensitivity analyses, we used 0-1 vs. ≥2 falls as the outcome and separately repeated our analyses without age, use of sedative hypnotics and vibratory perception as covariates. We also repeated analyses without adjusting for knee pain, since it is possible that buckling causes or exacerbates knee pain and including knee pain as a covariate may inappropriately adjust away a pathway through which buckling affects the risk of falls.(25) All analyses were performed using Statistical Analysis Systems (v9.2).
RESULTS
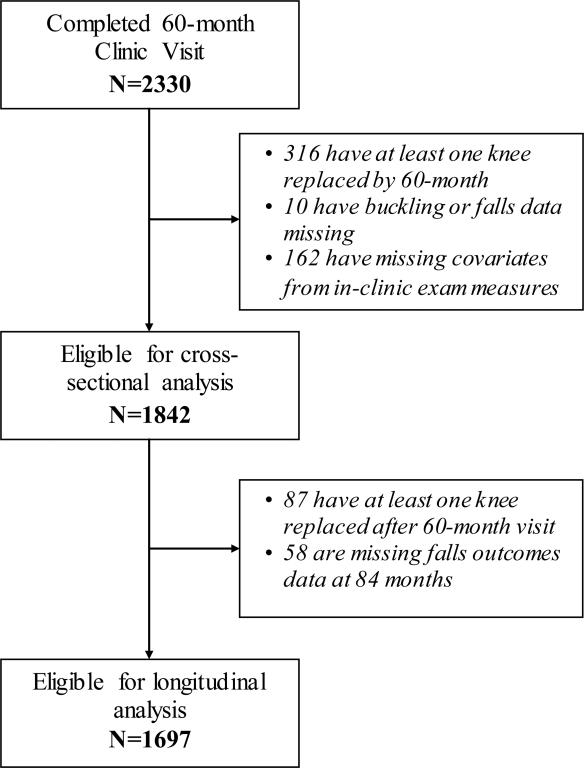
The 60 month clinic visit (baseline for this analysis) was attended by 1,842 eligible participants who had complete baseline data on buckling, falls and all covariates and 1,697 had follow-up data on falls at 84 months (Figure 1). Participants not included due to incomplete data, at baseline were more likely (P<0.05) to have a higher BMI and WOMAC pain score, poor balance confidence, use narcotic analgesics and to be African American. The sample had a mean [SD] age of 69.9 [7.8] years and BMI of 30.3 [5.6] and 60% were women (Table 1). About 2% of those screened had scores on the cognitive screening questionnaire suggestive of impairment.(22)
Figure 1.
Subject Selection Flow Diagram.
Table 1.
Subject Characteristics
| Baseline (60 month visit) characteristics | All (n=1842) | No Buckling in past 3 months (at 60 months) (n=1532 ) | Buckling ≥ 1 time in past 3 months (at 60 months) (n=310 ) | p-value for difference by Buckling status |
|---|---|---|---|---|
| Age, mean (± SD) | 66.9 (7.8) | 67.0 (7.8) | 66.7 (7.7) | 0.5769 |
| Female, n (%) | 1093 (59%) | 898 (59%) | 195 (63%) | 0.1611 |
| African American, n (%) | 249 (14%) | 189 (12%) | 60 (19%) | 0.0003 |
| Body mass index, mean (± SD) (in kgs / m ) | 30.3 (5.7) | 30.1 (5.5) | 31.6 (6.5) | <.0001 |
| Comorbidity score (0 -10), mean (± SD) | 0.78 (1.29) | 0.70 (1.20) | 1.16 (1.59) | <.0001 |
| Depressive symptoms, n (%) | 215 (12%) | 151 (10%) | 64 (21%) | <.0001 |
| Used Rx narcotic analgesics in past 30 days, n (%) | 171 (9%) | 122 (8%) | 49 (16%) | <.0001 |
| Used sedative hypnotics in past 30 days, n (%) | 193 (10%) | 161 (11%) | 32 (10%) | 0.9221 |
| Foot pain score (range 0-6), mean (± SD) | 1.23 (1.74) | 1.05 (1.60) | 2.15 (2.06) | <.0001 |
| Hip pain on most days (either hip), n (%) | 857 (47%) | 673 (44%) | 184 (59%) | <.0001 |
| Quadriceps extension maximum isokinetic torque (mean ± SD) (in newton-meters) | 0.0017 | |||
| Men | 118.0 (40.8) | 120.0 (41.1) | 107.0 (37.5) | 0.0004 |
| Women | 67.7 (25.0) | 68.9 (24.8) | 61.9 (25.0) | |
| Vibratory perception threshold at first MTP, , mean (± SD) (in volts) | 0.2210 | |||
| Men | 31.5 (15.5) | 31.5 (15.1) | 33.1 (15.0) | 0.1564 |
| Women | 20.3 (12.2) | 20.1 (12.0) | 21.4 (13.2) | |
| History of knee injury causing limited activity >=2 days, n (%) | 873 (47%) | 701 (46%) | 172 (55%) | 0.0018 |
| Highest KL grade either knee, n (%) | ||||
| 0-1 | 737 (40%) | 645 (42%) | 92 (30%) | <.0001 |
| 2 | 400 (22%) | 327 (21%) | 73 (24%) | |
| 3-4 | 705 (38%) | 560 (37%) | 145 (47%) | |
| Knee pain “on most days of the past month” n (%) | 991 (54%) | 732 (48%) | 259 (84%) | <.0001 |
| Sum of WOMAC pain score in right and left knees (0-40) (mean ± SD) (mean ± SD) | 5.68 (6.14) | 4.70 (5.47) | 10.52 (6.98) | <.0001 |
| Knee shifting/slipping without giving way in past 3 months, n (%) | ||||
| 0 | 1296 (70%) | 1149 (75%) | 147 (47%) | <.0001 |
| ≥ 1 time | 546 (30%) | 373 (25%) | 153 (53%) | |
| Injury due to a fall that caused a limitation of activity, n (%) | 159 (9%) | 103 (7%) | 56 (18%) | <.0001 |
| Serious injury due to a fall, n (%) | 214 (12%) | 142 (9%) | 72 (23%) | <.0001 |
| Poor balance confidence, n (%) (Activities-specific Balance Confidence Scale score < 67) | 232 (13%) | 129 (8%) | 103 (33%) | <.0001 |
| Fear of falling, n (%) | 593 (32%) | 437 (29%) | 156 (50%) | <.0001 |
| Limited activities due to concern about knee buckling, n (%) | 331 (18%) | 198 (13%) | 133 (43%) | <.0001 |
For the 3 months prior to baseline, 16.8% of participants reported knee buckling, 29.6% knee shifting/slipping without the knee giving way and 8.8% reported both symptoms of instability. Of those who reported buckling at baseline, 92% had either knee pain on most days of the past month or radiographic OA of the knee (KL grade ≥2), and 44% also reported buckling at 84 months.
Baseline knee instability and the cross-sectional and longitudinal risk of falls and consequences of falls
At 60 and 84 months, respectively, 13.9% and 13.2% of subjects had a single fall and 16.1% and 14.1% had recurrent (2 or more) falls during the preceding 12 months. Among fallers at either time-point, one in four had a significant injury and a similar proportion limited their activity due to a fall injury.
Those who buckled ≥1 time in the past 3 months at baseline were more likely to have had recurrent falls in the 12 months before baseline (29.1%) and 2 years later (25.2%) compared with nonbucklers (13.5% and 12.0%, respectively). In multivariate analyses (Table 2), bucklers had twice the odds of recurrent falls both at baseline and 2 years later. Shifting/slipping at baseline was associated with multiple falls at baseline but not with falls two years later. Instability symptoms were not associated with having one fall.
Table 2.
Association of knee buckling and knee shifing/slipping at 60 months with falls at 60 months and at 84 months
| Baseline exposure/predictor (n) | a. Cross-sectional association with falls in the past 12 months at baseline* | ||||
|---|---|---|---|---|---|
| Buckling in past 3 months | 0 falls | 1 fall | ≥2 falls | ||
| N (%) | N (%) | OR (95% CI) | N (%) | OR (95% CI) | |
| 0 (1532) | 1114 (72.7) | 211 (13.8) | Ref -- | 207 (13.5) | Ref -- |
| 1+ (310) | 175 (56.5) | 45 (14.5) | 1.25(0.84-1.86) | 90 (29.0) | 2.00(1.42-2.82) |
| Shifting /slipping in past 3 months | |||||
| 0 (1296) | 975 (73.8) | 175 (13.5) | Ref -- | 164 (12.7) | Ref -- |
| 1+ (546) | 332 (60.8) | 81 (14.8) | 1.08(0.78-1.50) | 133 (24.4) | 1.51(1.12-2.03) |
| Buckling in past 3 months | b. Longitudinal association with falls in the past 12 months at 2 year follow-up† | ||||
|---|---|---|---|---|---|
| 0 falls | 1 fall | ≥2 falls | |||
| 0 (1427) | 1066 (74.7) | 190 (13.3) | Ref -- | 171 (12.0) | Ref -- |
| 1+ (270) | 168 (62.2) | 34 (12.6) | 1.03(0.66-1.60) | 68 (25.2) | 1.98(1.35-2.91) |
| Shifting/slipping in past 3 months | |||||
| 0 (1217) | 907 (74.5) | 162 (13.3) | Ref -- | 148 (12.2) | Ref -- |
| 1+ (480) | 327 (68.1) | 62 (12.9) | 0.92(0.64-1.31) | 91 (19.0) | 1.10(0.78-1.55) |
Models include variables for both buckling and shifting/slipping, plus age, gender, race, clinic, BMI, highest K-L grade, history of knee injury causing limited activity, isokinetic knee extension strength (sex-specific tertiles), vibratory perception threshold at the first MTP joint (sex-specific tertiles), foot/ankle pain (number of locations with pain: 0, 1-2, 3-6), hip pain (yes/no), comorbidity index score (0-10), depression (CES-D score >=16 as depression indicator), used prescription narcotic analgesics in past 30 days (yes/no), used prescription sedative-hypnotic medications in the past 30 days (yes/no), knee buckling in the past 12 months but not in the past 30 days (yes/no), sum of WOMAC pain score in both knees.
84 month clinic visit and telephone contact
Comparing different combinations of baseline instability symptoms (Table 3), those reporting both buckling and shifting/slipping had an increased risk of falls at both 60 months and 2 years later, compared with those with neither symptom. Those who experienced buckling but not shifting/slipping were more likely to have multiple falls 2 years later but not at 60 months, while those reporting only shifting/slipping but not buckling did not have an increased risk of falls.
Table 3.
Association of combinations of baseline knee buckling and knee shifing/slipping with falls at 60 months and at 84 months
| Baseline exposure/predictor (n) | a. Cross-sectional association with falls in the past 12 months at baseline* | ||||
|---|---|---|---|---|---|
| Buckling and instability/slipping past 3 months (n) | 0 falls | 1 fall | ≥2 falls | ||
| N (%) | N (%) | OR (95% CI)* | N (%) | OR (95% CI)* | |
| Neither (1218) | 901 (74.0) | 163 (13.4) | Ref -- | 154 (12.6) | Ref -- |
| Shifting/slipping only (314) | 213 (67.8) | 48 (15.3) | 1.16 (0.78-1.71) | 53 (16.9) | 1.21 (0.82-1.78) |
| Buckling only (147) | 93 (63.3) | 25 (17.0) | 1.39 (0.84-2.30) | 29 (19.7) | 1.54 (0.94-2.52) |
| Buckling and shifting/slipping (163) | 82 (50.3) | 20 (12.3) | 1.23(0.69-2.18) | 61 (37.4) | 2.83 (1.80-4.46) |
| Buckling and instability/slipping past 3 months (n) | b. Longitudinal association with falls in past 12 months at 2 year follow-up† | ||||
|---|---|---|---|---|---|
| 0 falls | 1 fall | ≥2 falls | |||
| Neither (1146) | 860 (75.0) | 149 (13.0) | Ref -- | 137 (12.0) | Ref -- |
| Shifting/slipping only (281) | 206 (73.3) | 41 (14.6) | 1.00 (0.66-1.52) | 34 (12.1) | 0.87 (0.55-1.38) |
| Buckling only (130) | 80 (61.5) | 20 (15.4) | 1.40 (0.81-2.43) | 30 (23.1) | 2.10 (1.26-3.49) |
| Buckling and shifting/slipping (140) | 88 (62.9) | 14 (10.0) | 0.71 (0.37-1.37) | 38 (27.1) | 1.69 (1.00-2.86) |
See footnote to Table 2 for variables included in models.
84 month clinic visit and telephone contact
Bucklers were more likely to have had significant and activity-limiting fall-related injuries in the 12 months prior to baseline, with adjusted odds ratios of 2.38 (95% CI, 1.60, 3.54) and 1.96 (95% CI, 1.29, 3.00), respectively. Bucklers did not have an increased risk of fall-related injuries at 84 months, but nonetheless were more likely to have poor balance confidence (adjusted OR, 2.47; 95% CI, 1.58, 3.85) and fear of falling (adjusted OR, 1.62; 95% CI, 1.16, 2.26) two years later (data not shown in tables).
Falling when a knee buckled at baseline
We next examined falling when a knee gave way at baseline as an exposure variable. Among bucklers at baseline, 19.7% (n=61) fell at least once when their knee gave way, and of these a high proportion had 2 or more falls (72.1%), a significant fall injury (37.7%) and a fall injury that limited activity (45.9%) in the preceding 12 months compared with 18.5%, 14.5% and 11.2%, respectively, among bucklers who did not fall when a knee gave way (n=249) and compared with 13.5%, 9.2%, and 6.7% of nonbucklers (n=1,532). Bucklers who also fell were more likely to have poor balance confidence (52.5%) and a fear of falling (63.8%) at baseline compared with bucklers who did not fall when a knee gave way (28.5% and 44.6% , respectively) and compared with nonbucklers (8.4% and 28.5%). Of note, 68.8% of those who fell when a knee buckled said they modified or limited their activities due to concern about buckling (Table 4).
Table 4.
Association of knee buckling without a fall and buckling with a fall at baseline with falls and fall injuries at 84 months*
| Baseline exposure/predictor (n) | ≥2 falls | Significant fall injury at 2 year follow-up† | Fall injury limiting activity at 2 year follow-up† | |||
|---|---|---|---|---|---|---|
| Buckling/falls due to buckling in past 3 months | N (%) | OR (95% CI) | N (%) | OR (95% CI) | N (%) | OR (95% CI) |
| No buckling (1427) | 171 (12.0) | ref | 124 (8.7) | ref | 97 (6.8) | ref |
| Buckled, did not fall when knee gave way (220) | 44 (20.0) | 1.57 (1.03-2.38) | 21 (9.6) | 0.79 (0.46-1.36) | 20 (9.1) | 0.83 (0.46-1.47) |
| Buckled and fell when knee gave way (50) | 24 (48.0) | 4.51 (2.34-8.71) | 14 (28.0) | 2.23 (1.07-4.67) | 16 (32.0) | 2.95 (1.41-6.17) |
See footnote to Table 2 for variables included in models.
84 month clinic visit and telephone contact. N in each exposure group reflects loss to follow-up and missing data at 84 months.
Those who fell when a knee buckled at baseline continued to have a substantially increased risk of falls and their consequences 2 years later, including a 4.5-fold, 2-fold and 3-fold increased odds of recurrent falls, significant fall injuries and fall injuries that limited activity, respectively, and were 4 times more likely to have poor balance confidence and twice as likely to have fear of falling (Table 5). Bucklers who did not fall were also more likely two years later to have a fear of falling and poor balance confidence, although to a lesser extent.
Table 5.
Association of knee buckling without a fall and buckling with a fall at baseline with poor balance confidence and fear of falling at 84 months
| Baseline exposure/predictor (n) | Poor balance confidence** at 2 year follow-up† | Fear of falling at 2 year follow-up† | ||
|---|---|---|---|---|
| Buckling/falls due to buckling in past 3 months | N (%) | OR (95% CI) | N (%) | OR (95% CI) |
| No buckling (1305) | 121 (9.3) | ref | 401 (30.7) | ref |
| Buckled, did not fall when knee gave way (195) | 54 (27.7) | 2.18 (1.35-3.52) | 98 (50.3) | 1.54 (1.08-2.20) |
| Buckled and fell when knee gave way (44) | 23 (52.3) | 4.17 (1.80-9.68) | 28 (63.6) | 2.10 (1.02-4.33) |
* See footnote in Table 2 for variables included in models.
Activities-specific Balance Confidence (ABC) Scale score < 67.
84 month clinic visit. N in each exposure group rellects loss to follow-up and missing data at 84 months. The number of participants is smaller than in Table 4 due to collection of data on these outcomes at the clinic visit only..
The results of sensitivity analyses did not materially change our findings or conclusions.
DISCUSSION
Our findings establish a strong relationship between knee buckling, in which a knee gives way due to the sudden loss of postural support across the knee during weight bearing, and the risk of falls and adverse consequences of falls in people ages 55 to 84 with, and at high risk for, knee OA. Persons reporting knee buckling had a two- to three-fold greater likelihood of having had recurrent falls, a fall-related injury and having limited their activity due to a fall injury in the previous 12 months, and remained at increased risk of recurrent falls two years after experiencing a knee giving way. About 1 in 5 bucklers fell as a result of a knee giving way, and these individuals were at especially high risk of adverse outcomes two years later, including having recurrent falls, significant and activity-limiting fall injuries, poor balance confidence and fear of falling.
These results suggest that knee buckling is an independent risk factor for falls that is unique to persons with knee pain or knee OA. Knee instability during dynamic, weight-bearing activities occurs in the majority of knee OA patients(1, 6, 7) and in the general population buckling primarily occurs in people with knee pain.(2) Previous studies have found that persons with knee pain and knee OA have an increased risk of falls and fall injuries(26-29) and, despite a relatively high bone density, an increased risk of fractures.(30, 31) Our results suggest that that this increased risk is likely due, at least in part, to knee instability that results in falls.
Knee instability is associated with functional limitations in persons with knee OA independently of knee pain and OA severity.(1-3, 6-8) Individuals with knee instability frequently “lack confidence” in their knees(4) and this is associated with a poor functional outcome.(5) Previously in the MOST cohort we found that persons with a history of buckling as well as those who experienced knee slipping/shifting were significantly more likely to concurrently have poor balance confidence and fear of falling.(3) The present study expands on this by showing that for persons who have experienced knee buckling, an increased risk of these adverse psychological consequences of buckling persist two years later and that they are extremely common in individuals who had previously fallen when a knee gave way.
Fear of falling can prompt inappropriate avoidance of activities leading to physical deconditioning and a loss of function independently of the frequency of falls and fall injuries.(32, 33) This chain of events may play a role in the adverse impact of knee instability on function limitations. Of particular importance, in the present study over two-thirds of those who fell when a knee gave way said they had changed or limited their activities due to concern about buckling. Interestingly, sensations of knee shifting and slipping without the knee buckling were not associated with falls and fall consequences in our longitudinal analyses. These symptoms are less likely to directly result in a fall, but the findings also suggest that some individuals with knee instability may manage it by adopting behavioral strategies that limit their risk of buckling and falls. Whether limitations or modifications in activity by persons with knee instability reduce these risks or instead contribute to deconditioning, functional decline and increased risks of buckling and falls in the long-term (34, 35) warrants further investigation.
Interventions addressing knee instability and buckling have the potential to reduce the burden of falls and their consequences and improve confidence in the ability to engage in usual activities in the large segment of the older population that has knee pain. Neuromuscular control strategies involving leg muscle actions in response to proprioceptive stimuli play an important role in stabilizing the knee under varying external loads,(36) especially when, as is common with knee OA, soft tissue restraints around the knee are impaired.(37) Trials in persons with knee instability show that leg muscle strengthening and general functional exercises reduce instability and knee pain and improve physical function,(11, 12, 38) results which are consistent with a positive effect of leg strength training and exercise on pain and function seen in persons with knee OA in general.(12, 39) Whether interventions specifically designed to improve dynamic neuromuscular control through knee joint stabilization training provide additional benefit in treating knee instability is uncertain.(40, 41) The ability of any such interventions to reduce the risk of knee buckling and falls and their adverse consequences needs to be evaluated in controlled trials. If shown to be effective, it would suggest that such strategies be included in multi-factorial fall prevention strategies targeting persons with knee pain.(9, 10) Although individuals with a history of having fallen when a knee gave way represent 1 in 5 of those who reported buckling and only 3% of the overall cohort, targeting this readily identifiable subgroup at especially high risk of falls and injuries may be an efficient approach to preventing serious adverse consequences of knee instability.
Ours is the first prospective study to our knowledge that examines the association of symptoms of knee instability with falls and their consequences in persons with, or at risk for, knee OA. We adjusted for many potential risk factors for both knee instability and falls, including multiple co-morbidity, foot pain, depressive symptoms and use of sedative hypnotic and narcotic analgesic medications. The neuromuscular effects of chronic pain include leg muscle weakness,(29, 42) a risk factor for falls (43) and instability.(44) We adjusted for upper leg muscle strength as well as for knee pain severity and pain in other lower extremity joints. Our primary endpoint was recurrent falls (2 or more falls over a 12 month period), which is a standard and clinically important outcome measure in epidemiological studies of falls that has demonstrated stronger associations with fall risk factors and poor outcomes than single falls.(45)
Our study has several limitations. We did not include persons who had knee replacements, a large subgroup for whom buckling and falls can have dire consequences and deserving of further study. We did not distinguish indoor and outdoor falls, which may have different risk factors.(45, 46) If buckling is preferentially associated with either indoor or outdoor falls, combining them may cause us to underestimate the association of knee instability with falls. We assessed falls by recall for the past 12 months rather than weekly/monthly and without aids to recall such as a diary or calendar. Studies show that compared with weekly or monthly reporting (with or without calendars or other memory aids), recall of falls over the past 12 months has high specificity (>90%) but lower sensitivity so that 10-20% of fallers may be misclassified as non-fallers.(47, 48) This could cause us to overestimate an association of buckling with falls if bucklers are better at recalling falls. While cognitive impairment is associated both with falls(9) and with less accurate recall of falls,(49) cognitive screening tests(22, 50) administered to MOST participants suggests that the prevalence of impairment in our sample was not high enough to explain our results. We did not adjust for a history of falls at baseline in longitudinal analyses since we concluded that this would constitute over-adjustment for baseline buckling, which was often a direct cause of falls. Over 40% of bucklers say they restricted their activities due to concern about buckling; if as a result they were less active in a way that reduced their fall risk, we may underestimate their of risk of falls for the time spent at risk. We did not adjust for physical activity level or measures of balance performance since these factors are likely to be affected by knee instability, and adjusting for such intermediates could induce bias.(25) Knee instability was assessed by self-report, which could lead to recall bias. Development of practical objective measures of dynamic knee instability is needed. Finally, the reported odds ratios likely overestimate relative risks for common outcomes, such as falls.
Conclusion
Individuals who experience knee buckling are more likely to have a history of recurrent falls and injurious falls and to continue to have a greater risk of recurrent falls 2 years later. Persons who fall when a knee gives way have an especially high risk of future recurrent falls, injurious falls, fear of falling and poor balance confidence. Finding effective treatments for knee instability should be a priority and may help prevent knee buckling and falls and their adverse consequences in older persons with knee pain.
SIGNIFICANCE AND INNOVATION.
First prospective study to investigate symptoms of knee instability as a risk factor for falls, fall injuries and psychological consequences of falls in persons with, or at risk for, knee OA
Knee buckling, particularly when a fall results, is associated with an increased risk of recurrent falls and adverse consequences of falls two years later.
Interventions that reduce knee buckling may help prevent falls and their adverse consequences in persons with knee OA.
Acknowledgments
FINANCIAL SUPPORTERS: This study was supported by the National Institutes of Health, National Institute on Aging under the following grant numbers: AG18820, AG18832, AG18947 and AG19069. Dr. Felson was also supported by the NIHR Musculoskeletal Biomedical Research Unit at the University of Manchester in the UK.
Footnotes
COMPETING INTERESTS: No authors declare financial or personal relationships with other people or organizations that could potentially inappropriately influence (bias) their work and conclusions.
REFERENCES
- 1.Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physical active individuals. Physical therapy. 2000;80(2):128–40. Epub 2000/02/02. PubMed PMID: 10654060. [PubMed] [Google Scholar]
- 2.Felson DT, Niu J, McClennan C, Sack B, Aliabadi P, Hunter DJ, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med. 2007;147(8):534–40. doi: 10.7326/0003-4819-147-8-200710160-00005. Epub 2007/10/17. doi: 147/8/534 [pii]. PubMed PMID: 17938391. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen US, Felson DT, Niu J, White DK, Segal NA, Lewis CE, et al. The impact of knee instability with and without buckling on balance confidence, fear of falling and physical function: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2014;22(4):527–34. doi: 10.1016/j.joca.2014.01.008. Epub 2014/02/11. doi: 10.1016/j.joca.2014.01.008. PubMed PMID: 24508777; PubMed Central PMCID: PMCPMC4059670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skou ST, Wrigley TV, Metcalf BR, Hinman RS, Bennell KL. Association of knee confidence with pain, knee instability, muscle strength, and dynamic varus-valgus joint motion in knee osteoarthritis. Arthritis Care Res (Hoboken) 2014;66(5):695–701. doi: 10.1002/acr.22208. Epub 2013/10/16. doi: 10.1002/acr.22208. PubMed PMID: 24127243. [DOI] [PubMed] [Google Scholar]
- 5.Colbert CJ, Song J, Dunlop D, Chmiel JS, Hayes KW, Cahue S, et al. Knee confidence as it relates to physical function outcome in persons with or at high risk of knee osteoarthritis in the osteoarthritis initiative. Arthritis Rheum. 2012;64(5):1437–46. doi: 10.1002/art.33505. Epub 2011/12/03. doi: 10.1002/art.33505. PubMed PMID: 22135125; PubMed Central PMCID: PMCPMC3319513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51(6):941–6. doi: 10.1002/art.20825. Epub 2004/12/14. doi: 10.1002/art.20825 [doi]. PubMed PMID: 15593258. [DOI] [PubMed] [Google Scholar]
- 7.van der Esch M, Knoop J, van der Leeden M, Voorneman R, Gerritsen M, Reiding D, et al. Self-reported knee instability and activity limitations in patients with knee osteoarthritis: results of the Amsterdam osteoarthritis cohort. Clinical rheumatology. 2012;31(10):1505–10. doi: 10.1007/s10067-012-2025-1. Epub 2012/06/26. doi: 10.1007/s10067-012-2025-1. PubMed PMID: 22729472. [DOI] [PubMed] [Google Scholar]
- 8.Schmitt LC, Fitzgerald GK, Reisman AS, Rudolph KS. Instability, laxity, and physical function in patients with medial knee osteoarthritis. Physical therapy. 2008;88(12):1506–16. doi: 10.2522/ptj.20060223. Epub 2008/09/30. doi: 10.2522/ptj.20060223. PubMed PMID: 18820096; PubMed Central PMCID: PMCPMC2599794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? The Medical clinics of North America. 2006;90(5):807–24. doi: 10.1016/j.mcna.2006.05.013. Epub 2006/09/12. doi: 10.1016/j.mcna.2006.05.013. PubMed PMID: 16962843. [DOI] [PubMed] [Google Scholar]
- 10.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. The Cochrane database of systematic reviews. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. Epub 2012/09/14. doi: 10.1002/14651858.CD007146.pub3. PubMed PMID: 22972103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Physical therapy. 2011;91(4):452–69. doi: 10.2522/ptj.20100188. Epub 2011/02/19. doi: 10.2522/ptj.20100188. PubMed PMID: 21330451; PubMed Central PMCID: PMCPMC3070919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jansen MJ, Viechtbauer W, Lenssen AF, Hendriks EJ, de Bie RA. Strength training alone, exercise therapy alone, and exercise therapy with passive manual mobilisation each reduce pain and disability in people with knee osteoarthritis: a systematic review. Journal of physiotherapy. 2011;57(1):11–20. doi: 10.1016/S1836-9553(11)70002-9. Epub 2011/03/16. doi: 10.1016/s1836-9553(11)70002-9. PubMed PMID: 21402325. [DOI] [PubMed] [Google Scholar]
- 13.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56(9):2986–92. doi: 10.1002/art.22851. Epub 2007/09/01. doi: 10.1002/art.22851 [doi]. PubMed PMID: 17763427. [DOI] [PubMed] [Google Scholar]
- 14.Segal NA, Nevitt MC, Gross KD, Hietpas J, Glass NA, Lewis CE, et al. The Multicenter Osteoarthritis Study: opportunities for rehabilitation research. PM R. 2013;5(8):647–54. doi: 10.1016/j.pmrj.2013.04.014. Epub 2013/08/21. doi: 10.1016/j.pmrj.2013.04.014. PubMed PMID: 23953013; PubMed Central PMCID: PMCPMC3867287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Filiatrault J, Gauvin L, Fournier M, Parisien M, Robitaille Y, Laforest S, et al. Evidence of the psychometric qualities of a simplified version of the Activities-specific Balance Confidence scale for community-dwelling seniors. Arch Phys Med Rehabil. 2007;88(5):664–72. doi: 10.1016/j.apmr.2007.02.003. Epub 2007/05/01. doi: S0003-9993(07)00100-1 [pii] 10.1016/j.apmr.2007.02.003 [doi]. PubMed PMID: 17466738. [DOI] [PubMed] [Google Scholar]
- 16.Hill K. Activities-specific and Balance Confidence (ABC) Scale. The Australian journal of physiotherapy. 2005;51(3):197. doi: 10.1016/s0004-9514(05)70033-7. Epub 2005/09/29. PubMed PMID: 16187458. [DOI] [PubMed] [Google Scholar]
- 17.Bellamy N, Buchanan Ww, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically-important patient relevant outcomes following total hip and knee arthroplasty in osteoarthritis. J Ortho Rheum. 1988;1:95–108. [PubMed] [Google Scholar]
- 18.Felson DT, Nevitt MC, Yang M, Clancy M, Niu J, Torner JC, et al. A new approach yields high rates of radiographic progression in knee osteoarthritis. J Rheumatol. 2008;35(10):2047–54. Epub 2008/09/17. doi: 08/13/0920 [pii]. PubMed PMID: 18793000. [PMC free article] [PubMed] [Google Scholar]
- 19.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49(2):156–63. doi: 10.1002/art.10993. Epub 2003/04/11. doi: 10.1002/art.10993. PubMed PMID: 12687505. [DOI] [PubMed] [Google Scholar]
- 20.Pahor M, Chrischelles E, Guralnik JM. Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol. 1994;10:405–11. doi: 10.1007/BF01719664. [DOI] [PubMed] [Google Scholar]
- 21.Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res. 2011;63(Suppl 11):S454–66. doi: 10.1002/acr.20556. [DOI] [PubMed] [Google Scholar]
- 22.Fillit HMR, Edelman Lewis B, Sewell MC, Mills CS, Tsymuk M, Hill J. A Brief Telephonic Instrument to Screen for Cognitive Impairment in a Managed Care Population. JCOM. 2003;10:419–29. [Google Scholar]
- 23.Segal NA, Glass NA, Torner J, Yang M, Felson DT, Sharma L, et al. Quadriceps weakness predicts risk for knee joint space narrowing in women in the MOST cohort. Osteoarthritis Cartilage. 2010;18(6):769–75. doi: 10.1016/j.joca.2010.02.002. Epub 2010/03/02. doi: 10.1016/j.joca.2010.02.002. PubMed PMID: 20188686; PubMed Central PMCID: PMCPMC2873062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shakoor N, Agrawal A, Block JA. Reduced lower extremity vibratory perception in osteoarthritis of the knee. Arthritis Rheum. 2008;59(1):117–21. doi: 10.1002/art.23241. Epub 2008/01/01. doi: 10.1002/art.23241. PubMed PMID: 18163397; PubMed Central PMCID: PMCPMC3653289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y, Neogi T, Hunter D, Roemer F, Niu J. What effect is really being measured? An alternative explanation of paradoxical phenomena in studies of osteoarthritis progression. Arthritis Care Res (Hoboken) 2014;66(5):658–61. doi: 10.1002/acr.22213. Epub 2014/05/31. PubMed PMID: 24877249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. Jama. 1989;261(18):2663–8. PubMed PMID: 2709546. [PubMed] [Google Scholar]
- 27.Foley SJ, Lord SR, Srikanth V, Cooley H, Jones G. Falls risk is associated with pain and dysfunction but not radiographic osteoarthritis in older adults: Tasmanian Older Adult Cohort study. Osteoarthritis Cartilage. 2006;14(6):533–9. doi: 10.1016/j.joca.2005.12.007. Epub 2006/02/08. doi: S1063-4584(05)00368-7 [pii] 10.1016/j.joca.2005.12.007 [doi]. PubMed PMID: 16460970. [DOI] [PubMed] [Google Scholar]
- 28.Scott D, Blizzard L, Fell J, Jones G. Prospective study of self-reported pain, radiographic osteoarthritis, sarcopenia progression, and falls risk in community-dwelling older adults. Arthritis Care Res (Hoboken) 2012;64(1):30–7. doi: 10.1002/acr.20545. Epub 2011/07/09. doi: 10.1002/acr.20545. PubMed PMID: 21739619. [DOI] [PubMed] [Google Scholar]
- 29.Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, Guralnik JM, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302(20):2214–21. doi: 10.1001/jama.2009.1738. Epub 2009/11/26. doi: 10.1001/jama.2009.1738. PubMed PMID: 19934422; PubMed Central PMCID: PMCPMC2927855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arden NK, Crozier S, Smith H, Anderson F, Edwards C, Raphael H, et al. Knee pain, knee osteoarthritis, and the risk of fracture. Arthritis Rheum. 2006;55(4):610–5. doi: 10.1002/art.22088. Epub 2006/07/29. doi: 10.1002/art.22088 [doi]. PubMed PMID: 16874784. [DOI] [PubMed] [Google Scholar]
- 31.Bergink AP, van der Klift M, Hofman A, Verhaar JA, van Leeuwen JP, Uitterlinden AG, et al. Osteoarthritis of the knee is associated with vertebral and nonvertebral fractures in the elderly: the Rotterdam Study. Arthritis Rheum. 2003;49(5):648–57. doi: 10.1002/art.11380. Epub 2003/10/15. doi: 10.1002/art.11380 [doi]. PubMed PMID: 14558050. [DOI] [PubMed] [Google Scholar]
- 32.Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A Biol Sci Med Sci. 2000;55(5):M299–305. doi: 10.1093/gerona/55.5.m299. Epub 2000/05/20. PubMed PMID: 10819321. [DOI] [PubMed] [Google Scholar]
- 33.Li F, Fisher KJ, Harmer P, McAuley E, Wilson NL. Fear of falling in elderly persons: association with falls, functional ability, and quality of life. The journals of gerontology Series B, Psychological sciences and social sciences. 2003;58(5):P283–90. doi: 10.1093/geronb/58.5.p283. Epub 2003/09/26. PubMed PMID: 14507935. [DOI] [PubMed] [Google Scholar]
- 34.Holla JF, van der Leeden M, Knol DL, Peter WF, Roorda LD, Lems WF, et al. Avoidance of activities in early symptomatic knee osteoarthritis: results from the CHECK cohort. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2012;44(1):33–42. doi: 10.1007/s12160-012-9353-x. Epub 2012/03/14. doi: 10.1007/s12160-012-9353-x. PubMed PMID: 22411212. [DOI] [PubMed] [Google Scholar]
- 35.Holla JF, van der Leeden M, Knol DL, Roorda LD, Hilberdink WK, Lems WF, et al. Predictors and outcome of pain-related avoidance of activities in persons with early symptomatic knee osteoarthritis: A 5-year follow-up study. Arthritis Care Res (Hoboken) 2014 doi: 10.1002/acr.22381. Epub 2014/06/07. doi: 10.1002/acr.22381. PubMed PMID: 24905958. [DOI] [PubMed] [Google Scholar]
- 36.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9(1):113–9. doi: 10.1002/jor.1100090114. Epub 1991/01/01. doi: 10.1002/jor.1100090114. PubMed PMID: 1984041. [DOI] [PubMed] [Google Scholar]
- 37.Schmitt LC, Rudolph KS. Muscle stabilization strategies in people with medial knee osteoarthritis: the effect of instability. J Orthop Res. 2008;26(9):1180–5. doi: 10.1002/jor.20619. Epub 2008/04/12. doi: 10.1002/jor.20619. PubMed PMID: 18404657; PubMed Central PMCID: PMCPMC3112363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diracoglu D, Aydin R, Baskent A, Celik A. Effects of kinesthesia and balance exercises in knee osteoarthritis. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 2005;11(6):303–10. doi: 10.1097/01.rhu.0000191213.37853.3d. Epub 2005/12/24. PubMed PMID: 16371799. [DOI] [PubMed] [Google Scholar]
- 39.Lange AK, Vanwanseele B, Fiatarone Singh MA. Strength training for treatment of osteoarthritis of the knee: a systematic review. Arthritis Rheum. 2008;59(10):1488–94. doi: 10.1002/art.24118. Epub 2008/09/30. doi: 10.1002/art.24118. PubMed PMID: 18821647. [DOI] [PubMed] [Google Scholar]
- 40.Williams GN, Chmielewski T, Rudolph K, Buchanan TS, Snyder-Mackler L. Dynamic knee stability: current theory and implications for clinicians and scientists. The Journal of orthopaedic and sports physical therapy. 2001;31(10):546–66. doi: 10.2519/jospt.2001.31.10.546. Epub 2001/10/23. doi: 10.2519/jospt.2001.31.10.546. PubMed PMID: 11665743. [DOI] [PubMed] [Google Scholar]
- 41.Knoop J, Dekker J, van der Leeden M, van der Esch M, Thorstensson CA, Gerritsen M, et al. Knee joint stabilization therapy in patients with osteoarthritis of the knee: a randomized, controlled trial. Osteoarthritis Cartilage. 2013;21(8):1025–34. doi: 10.1016/j.joca.2013.05.012. Epub 2013/06/01. doi: 10.1016/j.joca.2013.05.012. PubMed PMID: 23721797. [DOI] [PubMed] [Google Scholar]
- 42.Graven-Nielsen T, Lund H, Arendt-Nielsen L, Danneskiold-Samsoe B, Bliddal H. Inhibition of maximal voluntary contraction force by experimental muscle pain: a centrally mediated mechanism. Muscle & nerve. 2002;26(5):708–12. doi: 10.1002/mus.10225. Epub 2002/10/29. doi: 10.1002/mus.10225. PubMed PMID: 12402294. [DOI] [PubMed] [Google Scholar]
- 43.Rubenstein LZJK, Trueblood PR, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55A:M317–21. doi: 10.1093/gerona/55.6.m317. [DOI] [PubMed] [Google Scholar]
- 44.Knoop J, van der Leeden M, van der Esch M, Thorstensson CA, Gerritsen M, Voorneman RE, et al. Association of lower muscle strength with self-reported knee instability in osteoarthritis of the knee: results from the Amsterdam Osteoarthritis cohort. Arthritis Care Res (Hoboken) 2012;64(1):38–45. doi: 10.1002/acr.20597. Epub 2012/01/04. doi: 10.1002/acr.20597. PubMed PMID: 22213723. [DOI] [PubMed] [Google Scholar]
- 45.Kelsey JL, Procter-Gray E, Berry SD, Hannan MT, Kiel DP, Lipsitz LA, et al. Reevaluating the implications of recurrent falls in older adults: location changes the inference. J Am Geriatr Soc. 2012;60(3):517–24. doi: 10.1111/j.1532-5415.2011.03834.x. Epub 2012/01/31. doi: 10.1111/j.1532-5415.2011.03834.x. PubMed PMID: 22283236; PubMed Central PMCID: PMCPMC3302971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kelsey JL, Berry SD, Procter-Gray E, Quach L, Nguyen US, Li W, et al. Indoor and outdoor falls in older adults are different: the maintenance of balance, independent living, intellect, and Zest in the Elderly of Boston Study. J Am Geriatr Soc. 2010;58(11):2135–41. doi: 10.1111/j.1532-5415.2010.03062.x. Epub 2010/09/14. doi: 10.1111/j.1532-5415.2010.03062.x. PubMed PMID: 20831726; PubMed Central PMCID: PMCPMC2975756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc. 2005;53(12):2190–4. doi: 10.1111/j.1532-5415.2005.00509.x. Epub 2006/01/10. doi: 10.1111/j.1532-5415.2005.00509.x. PubMed PMID: 16398908. [DOI] [PubMed] [Google Scholar]
- 48.Hannan MT, Gagnon MM, Aneja J, Jones RN, Cupples LA, Lipsitz LA, et al. Optimizing the tracking of falls in studies of older participants: comparison of quarterly telephone recall with monthly falls calendars in the MOBILIZE Boston Study. Am J Epidemiol. 2010;171(9):1031–6. doi: 10.1093/aje/kwq024. Epub 2010/04/03. doi: 10.1093/aje/kwq024. PubMed PMID: 20360242; PubMed Central PMCID: PMCPMC2877474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cummings SR, Nevitt MC, Kidd S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36(7):613–6. doi: 10.1111/j.1532-5415.1988.tb06155.x. PubMed PMID: 3385114. [DOI] [PubMed] [Google Scholar]
- 50.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40(9):771–81. doi: 10.1097/00005650-200209000-00007. Epub 2002/09/10. doi: 10.1097/01.mlr.0000024610.33213.c8. PubMed PMID: 12218768. [DOI] [PubMed] [Google Scholar]