Abstract
Objective:
Over the past 30 years, illness management programs and cognitive-behavioral therapy for psychosis have gained prominence in the treatment of schizophrenia. However, little is known about the long-term benefits of these types of programs when delivered during inpatient treatment following a symptom exacerbation. To evaluate this question, we conducted a randomized controlled trial comparing the long-term effects of a group-based coping-oriented program (COP) that combined the elements of illness management with cognitive behavioral-therapy for psychosis, with an equally intensive supportive therapy (SUP) program.
Method:
196 inpatients with DSM-IV schizophrenia were randomized to COP or SUP, each lasting 12 sessions provided over 6–8 weeks. Outcome measures were collected in the hospital at baseline and post-assessment, and following discharge into the community 1 and 2 years later. We compared the groups on rehospitalizations, symptoms, psychosocial functioning, and knowledge about psychosis.
Results:
Intent-to-treat analyses indicated that patients in COP learned significantly more information about psychosis, and had greater reductions in overall symptoms and depression/anxiety over the treatment and follow-up period than patients in SUP. Patients in both groups improved significantly in other symptoms and psychosocial functioning. There were no differences between the groups in hospitalization rates, which were low.
Conclusions:
People with schizophrenia can benefit from short-term COPs delivered during the inpatient phase, with improvements sustaining for 2 years following discharge from the hospital. More research is needed to evaluate the long-term impact of coping-oriented and similar programs provided during inpatient treatment.
Key words: schizophrenia, coping, cognitive-behavioral therapy, psychoeducation, supportive therapy, illness management, effectiveness
Introduction
Schizophrenia creates a wide range of personal challenges for individuals due to unpredictable relapses, social stigma, loss of social support, difficulties with cognitive functioning, as well as (depression and anxiety). Psychopharmacological interventions play a major role in the treatment of schizophrenia as they reduce severity of psychotic symptoms and prevent relapses.1 However, approximately 20%–30% of the patients experience persistent symptoms, have adverse side effects,2 or experience relapses despite medication adherence. In addition to pharmacotherapy, psychosocial interventions play an important role in the treatment of schizophrenia, including the management of symptoms and prevention of relapses.3 The stress-vulnerability4 and the transtheoretical models5 have provided a valuable framework for guiding illness management efforts aimed at modifying psychological and social-environmental factors that can precipitate relapses (eg, poor coping ability, lack of social support), and harnessing patient motivation for active collaboration with others aimed at improving the course of the illness.
Illness management programs,6–9 including the Illness Management and Recovery program,10 were developed to help people improve the course of illness by providing information about the nature of their disorder and its treatment, teaching strategies for preventing relapses (eg, developing a relapse prevention plan, behavioral tailoring to incorporate medication adherence into daily routines), and teaching skills for dealing with stress and persistent symptoms. Cognitive-behavioral therapy for psychosis overlaps with illness management programs in teaching more effective coping strategies for managing stress and persistent symptoms, while it tends to focus less on education about schizophrenia, and more on cognitive restructuring aimed at changing individuals’ beliefs or appraisals about their symptoms, abilities, and how other people view them.11–14 Meta-analyses have demonstrated the effectiveness of cognitive-behavioral15 and illness management interventions16 for schizophrenia mainly delivered on an outpatient basis, and suggest comparable effectiveness of individual and group modalities.17 We refer to interventions focusing on education, teaching more effective coping strategies, and cognitive restructuring as “coping-oriented” programs (COPs),18 as they endeavor to foster more adaptive coping with schizophrenia through a wider variety of strategies than are usually employed by either a cognitive-behavioral or illness management program.
Based on this rationale, we developed a COP targeting inpatients with schizophrenia-spectrum disorders who had recently been hospitalized for a first episode of psychosis or a symptom exacerbation and were awaiting discharge into the community.18 A pilot study of the program supported its feasibility and suggested positive clinical and psychosocial benefits.19 Following the promising results of this study, we conducted a randomized controlled trial to evaluate the program compared to a less structured supportive therapy program (SUP) that provided similar opportunities for social interaction and emotional support, but without education, the teaching of coping skills, or cognitive restructuring. This article describes the 2-year results of this trial. Our primary hypothesis was that participants in COP would have lower rates of rehospitalization over the follow-up period than participants in SUP. Our secondary hypothesis was that the COP program would result in greater improvements in knowledge about psychosis, symptoms, and functioning over the 2-year study period.
Methods
Study Site and Participants
A total of 198 inpatients were recruited from the Department of Psychiatry and Psychotherapy of the Ludwig Maximilian’s University at Munich. Inclusion criteria were: (1) aged 18–69 years, (2) diagnosis of schizophrenia-spectrum disorder or other psychotic disorder made by treating psychiatrist according to the Diagnostic and Statistical Manual of Mental Disorders DSM-IV,20 (3) post-acute stage of the illness (ie, remission of acute symptoms), (4) proficient in German, (5) sufficiently stable to participate in group programs, and (6) written informed consent. Exclusion criteria were: (1) organic brain syndrome, (2) current drug or alcohol dependence, or (3) acute suicidality. The study was approved by the University Institutional Review Board.
Because the size of the treatment groups was limited to 6–10 patients per group, it was not possible to invite all potentially eligible patients to participate in the study. Thus, patients who appeared to staff to be most likely to agree to participate were approached. A total of 198 patients were approached for the study and consented to participate; 2 patients did not meet inclusion criteria, resulting in 196 patients who were randomly assigned to the COP (n = 100) or to the supportive therapy program (SUP; n = 96).
Measures
Assessments were conducted in the hospital at baseline and post-treatment 6–8 weeks later, and 1 and 2 years following discharge from the hospital. Symptoms were assessed with the Brief Psychiatric Rating Scale—Expanded (BPRS),21 with analyses based on Velligan’s22 factor analysis, including: depression/anxiety, activation, retardation, and psychosis. The Scale for the Assessment of Negative Symptoms (SANS)23 was also used to evaluate negative symptoms. The SANS consists of 24 items, each rated over the prior 2 weeks, with higher scores indicating more severe symptoms. Psychosocial functioning was assessed with the Global Assessment Functioning Scale (GAF)20–24 ranging from poor (0) to high (100) functioning. Knowledge about psychosis and its treatment was assessed using a modified multiple choice test based on Hahlweg.25 This test included 26 questions about etiology, symptoms, and treatment strategies. Knowledge was defined as the number of correct answers, with scores ranging from 0 to 60. Satisfaction with treatment was assessed using a 4-item questionnaire26 administered at the end of each the group treatment.
Follow-up assessments evaluated functional and clinical variables. At each assessment, information about antipsychotic and anticholinergic medications were obtained, and chlorpromazine-equivalents were calculated.27 Rehospitalization was determined by a combination of participant interview and review of medical records. Study participants were reimbursed for travel expenses related to the follow-up assessments conducted on an outpatient basis. No other reimbursements were provided to participants for completing any of the assessments.
Procedures
After providing informed consent participants completed the baseline assessments, and were then randomized to the coping-oriented (COP) or to the supportive (SUP) group treatment. Randomization was performed using a computer based arithmetic procedure with conditions sequences of chance available in Unified Resource Locator (URL) to guarantee an even but random assignment of participants. Clinical raters were blinded to treatment assignment. Before each follow-up interview, participants were reminded not to reveal their treatment assignment. Follow-up assessments were attempted on all enrolled study participants, regardless of their degree of participation in the treatment groups.
Organization of the Treatment Programs
The majority of the inpatients were recruited from a specialized treatment unit for people experiencing a first or second episode of psychosis28,29 which offered individualized pharmacotherapy and mainly low-dose atypical antipsychotic medications.30 In addition to pharmacological treatment provided to patients in both the specialized treatment unit and the other hospital units, patients in both treatment groups were offered a range of other psychotherapeutic and rehabilitation services, including occupational therapy, recreational groups, individual therapy (approximately 30% in both treatment conditions), and art and music therapy. About 15% of patients’ relatives attended family groups. There was no special pharmacotherapy regime used in the study. The intervention started within the inpatient stabilization phase. Both COP and SUP groups included a mix of patients recovering from a first or second episode of psychosis and patients with multiple episodes. Groups which contained predominantly first or second patients provided a greater focus on enhancing self-confidence and self-esteem, and instilling hope, and avoided frequent reference to the potentially demoralizing diagnosis of schizophrenia in preference to using the term “psychosis.”
Clinical psychologists who were experienced in cognitive-behavioral therapy and in the treatment of schizophrenia conducted the group programs. Two therapists led each treatment group and were supervised on a weekly basis to ensure adherence to the treatment models. Treatment in either COP or SUP included twelve 75-minute sessions, provided over 6–8 weeks. Groups included 6–10 patients, with a total of 12 treatment groups conducted for each program.
Contents of the Treatment Programs
Treatment manuals for COP and SUP guided each intervention. COP is based on a cognitive-behavioral approach. SUP reflects a supportive intervention with participants who were invited to choose their own discussion topics, and was intended to be an “attention control” group, aimed at controlling for nonspecific therapeutic factors, such as therapist attention and interactions with other patients. Therapists providing SUP were requested to not use cognitive-behavioral strategies when facilitating the intervention.
COP was based on the stress-vulnerability-coping model4 highlighting the interactions between biological vulnerability, stressors and protective factors, as well as on the transtheoretical model.5 This model proposes that motivation to change is determined by a series of specific stages. Motivational enhancement first helps patients identify and pursue personal goals, and then to explore how improved illness management can help them achieve these goals. COP includes psychoeducational elements (eg, handouts for important topics) and cognitive-behavioral teaching principles (eg, cognitive restructuring, role playing, problem solving). It seeks to improve understanding of the illness and its treatment, to teach coping strategies for specific stressors and symptoms, to activate the use of internal and external resources, and to enhance self-confidence and hope. Thus, the program was intended to foster the development of a lifestyle that enhances positive activities and health.
The German manual (available from the first author upon request) provided guidelines to encourage direct communication between patients, while also establishing a structure for the therapists to convey essential information and skills. The agenda of the sessions was supplemented by materials, including flipcharts, handouts, and homework assignments. The first part of COP was educational and therapists interactively discussed the material and elicited participants’ comments and experiences. The second part focused on the participants’ individual stressors and needs, and was therefore more individually shaped by them. Challenging topics alternated with resource-oriented ones to prevent excessive demands. COP focused on topics of greatest concern to patients, such as symptom-management (eg, coping with anxiety and positive symptoms), managing stress (stress-management), building up rewarding activities, time management, social skills (eg, dealing with relatives, getting to know people), reintegration into the workplace, and providing information about outpatient services. In early groups, participants identified specific distressing symptoms for which coping strategies were selected and taught. Over the course of several groups a list of common symptoms was developed, which was subsequently used to help patients identify symptoms for which coping strategies were needed. Stress-management included strategies intended to bring rapid relief in a stressful situations (eg, relaxation, mindfulness, distraction), as well as long-term strategies designed to change stressful situations (eg, problem solving, cognitive restructuring).
The COP program followed a didactic treatment guideline presented in table 1. Formal fidelity assessments of therapist adherence to either the COP or SUP programs were not conducted.
Table 1.
Description of the Coping-Oriented Treatment Program
| Session | Topic |
|---|---|
| 1 | Education about schizophrenia and its treatment options based on the stress-vulnerability model |
| Participants’ expectations, personal goals, and plans to achieve them | |
| Structure and rules of the group | |
| Definition of psychosis and medical underpinnings | |
| 2 | Education and being an expert on schizophrenia |
| Identifying symptoms of psychosis: positive and negative symptoms | |
| Combined treatment in schizophrenia with pharmacotherapy and psychotherapy | |
| Helpful experiences in coping with the illness | |
| 3 | Definition of psychosis and its biological underpinnings |
| Illustrating of health and illness: dispelling myths about schizophrenia | |
| Different courses of the illness, sub-diagnosis and their occurrence | |
| Genetic factors and risk of relapse | |
| 4 | Patients’ illness concepts (triggers and influential factors) |
| Stress-vulnerability model and its components | |
| Chemical processes in the brain, the role of dopamine | |
| Beneficial aspects of vulnerability (eg, creativity in artists) | |
| Biochemical imbalance of the brain and the role of antipsychotics | |
| Discussion of the model and its consequences: self-efficacy vs victim of the illness | |
| 5 | Definition of antipsychotics |
| Attitudes towards medication and adherence | |
| Biochemical modes of action in antipsychotics | |
| Classification of antipsychotics based on potency | |
| Personal medication checklist | |
| Physician responses medical questions for relapse prevention | |
| 6 | Psychopharmacological strategies |
| Role of medication in preventing relapses | |
| Information about medication, choice, and adherence strategies | |
| Side effects of medication and their management | |
| 7 | Stress management and relapse prevention |
| Definition of early warning signs of relapse and their identification | |
| Assignment 2: warning signs checklist” | |
| Coping with early warning signs | |
| Relapse prevention checklist | |
| 8 | Coping with stressors and improving quality of life |
| Identifying individual stressors | |
| Interrelationship between stressors, deterioration of well-being, and psychosis | |
| Stress management: strategies for coping with stressors; abbreviated muscular relaxation or breathing techniques with positive self-talk | |
| 9 | Stress management |
| Analysis of stressful situations | |
| Relaxation training | |
| Identifying positive activities | |
| Planning engagement in rewarding activities, role playing | |
| 10 | Cognitive therapy |
| Relationship between thoughts, feelings, and behavior | |
| ABC-model | |
| Focusing on activating events (A), beliefs (B), and physical, emotional, cognitive, and behavioral consequences (C) | |
| 11 | Problem-solving (5 steps) |
| Description of the problem | |
| List of possible solutions | |
| Evaluation of pros and cons of possible solutions | |
| Identifying best solution or combination of solutions | |
| Planning to implement the solution(s) | |
| 12 | End of the program |
| Review different mental health services and support patients to advocate for help | |
| Self-help strategies | |
| Review of program and accomplishments |
Data Analysis
Exposure to COP and SUP was defined as participation in more than 6 of the 12 scheduled sessions. Baseline differences between the COP and SUP groups in demographic and clinical variables were evaluated with chi-square and independent t tests.
Treatment effects were evaluated by conducting intent-to-treat analyses on the full sample of randomized participants, regardless of exposure to assigned treatment group. In order to examine treatment effects we used the total score of the BPRS and subscales, GAF, SANS, and Knowledge25 as the dependent variables. Change in outcome variables was evaluated by using a mixed model linear regression analysis, with baseline score and duration of illness included as covariates, and the post-treatment and follow-up scores as repeated dependent variables. Treatment group, time, and their interaction were included as independent variables. Covariance pattern models31 were applied and adjusted mean response profile models were fitted. This approach is similar to a traditional analysis of covariance, but can accommodate missing data using maximum likelihood estimation, as well as correlated data by selecting well-suited covariance structures.32 In order to avoid fitting models for different outcome variables with possibly different covariance structures we used the robust standard error estimation option in the SPSS GENLIN procedure (SPSS 23, IBM Corp). This method uses the original Huber-White estimators for linear models and yields a robust estimation of variance and covariance regardless of the data’s actual covariance structure. This approach is also known as sandwich estimation,33 and has been previously used in similar research.34
The COP and SUP treatments were each provided in a succession of 12 groups over the course of the study, which can create co-dependencies among observations that violate the assumption of independent observations of statistical tests. A random effect was included in the initial analyses to account for the between group variation (similar to that used in cluster randomized controlled trials). However, this effect was dropped from the final models as it did not alter the main findings.
Effect sizes were calculated by multiplying model-based estimates of mean differences at the end of the study with the factor time and then dividing this value by the pooled within-group SD of raw scores d = β(time)/SDraw.35 This approach adjusts for covariates and the correlation between time points, and is the same metric as group effects computed with Cohen’s d.36 Because the baseline was statistically adjusted, treatment effects were evaluated with group main effects on slopes (ie, differences in group mean response profiles).
Results
30% of the patients were experiencing their first episode of psychosis and first hospitalization, 23% their second hospitalization, 30% had 3–5 prior hospitalizations, and 18% had more than 5 previous hospitalizations. Approximately half (53%) of the patients were male, and 71% were single. Demographic and diagnostic characteristics of the sample are summarized in table 2.
Table 2.
Baseline Clinical and Sociodemographic Variables of the Study Sample
| DSM-IV | Diagnosis | Total (N = 196) | COP (N = 100) | SUP (N = 96) | |||
|---|---|---|---|---|---|---|---|
| 295.1 | Disorganized schizophrenia | 11.7% | 11% | 12.5% | |||
| 295.2 | Catatonic schizophrenia | 1.5% | 1% | 2.1% | |||
| 295.3 | Paranoid schizophrenia | 63.3% | 67% | 59.4% | |||
| 295.6 | Residual schizophrenia | 9.2% | 10% | 8.3% | |||
| 295.7 | Schizoaffective disorder | 8.7% | 5% | 12.5% | |||
| 295.9 | Undifferentiated schizophrenia | 1% | 1% | 1% | |||
| 297.1 | Delusional disorder | 0.5% | 1% | 0% | |||
| 298.8 | Brief psychotic disorder | 2.6% | 2% | 3.1% | |||
| 298.9 | Unspecified psychosis | 1.5% | 2% | 1% | |||
| M | SD | M | SD | M | SD | ||
| Age at current hospitalization | 33.6 | 11.3 | 33.3 | 10.3 | 34.0 | 12.2 | |
| Age of onset | 27.7 | 9.3 | 28.5 | 8.8 | 27.0 | 9.8 | |
| Duration of illness (y)a | 6.2 | 7.6 | 5.0 | 6.5 | 7.5 | 8.4 | |
| Number of previous hospitalizations | 3.2 | 2.6 | 3.3 | 2.7 | 3.2 | 2.5 | |
| Cumulative duration of prior hospitalization (d) | 181.8 | 222.7 | 181.2 | 229.2 | 182.4 | 216.9 | |
| Current duration of hospitalization before participation in groups (d) | 40.7 | 30.7 | 36.6 | 27.5 | 44.9 | 33.3 | |
| Chlorpromazine-equivalents | 277.3 | 290.6 | 245.0 | 260.7 | 308.5 | 315.1 | |
| Scale for Extrapyramidal Symptoms (EPS) | 0.4 | 0.4 | 0.3 | 0.4 | 0.4 | 0.4 | |
Note: COP, coping-oriented program; SUP, supportive therapy program.
a t(194) = −2.378, P = .018.
Participants randomized to COP did not differ from those in SUP on any demographic, treatment-related, or clinical variables, except for duration of illness. Participants in COP had a shorter average duration of illness (M = 4.98 y, SD = 6.47) than those in SUP (M = 7.46 y, SD = 8.42). Duration of illness was included as covariate in the data analysis.
A high proportion of patients were exposed to the programs, with an average attendance of 6.45 sessions (SD = 3.26). Seventy-two percent participated in at least 6 sessions of COP, and 73% in SUP, a nonsignificant difference. On average participants Exposed vs non-exposed participants did not differ on any demographic or clinical characteristics at baseline. Regarding satisfaction with program, participants in both COP and SUP gave comparable ratings of their program indicating that it was helpful and applicable, and indicated that they would recommend it to other people. However, participants in COP felt better informed about their illness (89.9%) than participants in SUP (65.4%), U = 2294.5, P < .001.
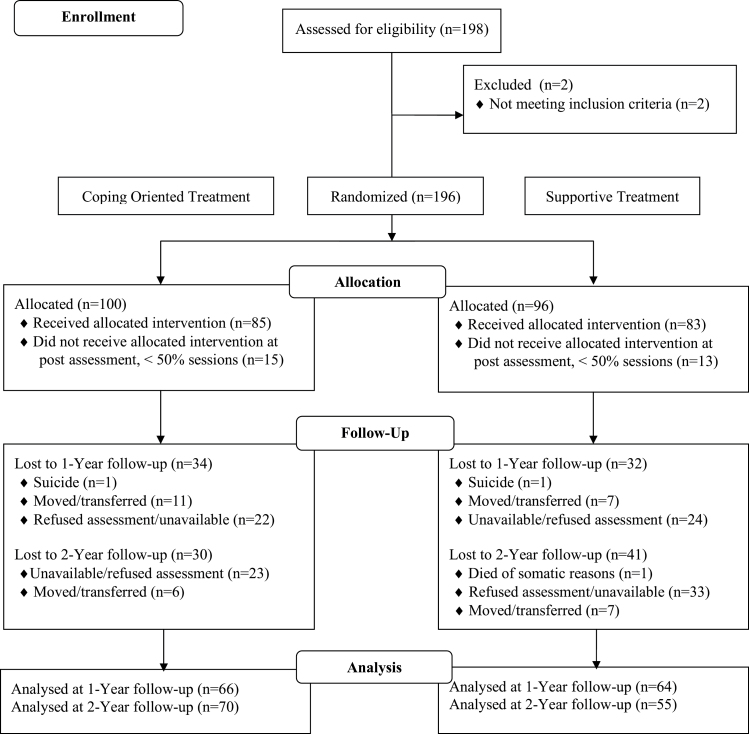
At the 2-year follow-up, 125 patients (64% of the sample) completed a clinical interview to assess rehospitalization rate, and interview-based assessments of symptoms or functioning (eg, BPRS-E) were completed. There were no significant differences between the treatment groups in rates of follow-up. The CONSORT diagram illustrating the flow of participants through the study is provided in figure 1.
Fig. 1.
Flow of participants through the study. The number of participants increased at 2-year follow-up despite the lower number at 1-year follow-up as the main treatment criteria referred to 2-year outcome. COP = coping-oriented program; SUP = supportive therapy program.
The cumulative rate of rehospitalization over 2 years did not differ significantly between the groups (38.3% for COP vs 36.7% for SUP). Descriptive statistics for the primary outcome variables for baseline and follow-up assessments, as well as main group effects and effect sizes are shown in table 3.
Table 3.
Descriptive Statistics and Treatment Group Effects on Outcomes for COP and SUP Interventions at Baseline, Post-Treatment, and 1- and 2-Years Follow-ups
| Measure | Baseline | Post-treatment | 1 Year | 2 Year | Group Effecta | Effect Sizeb | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | dfs | F | P | ||
| BPRS total | 1, 321 | 6.81 | <.01 | −0.72 | ||||||||
| COP | 52.27 | 16.16 | 43.73 | 12.6 | 36.14 | 8.76 | 34.21 | 8.65 | ||||
| SUP | 55.05 | 18.15 | 46.08 | 13.19 | 42.04 | 11.00 | 38.77 | 14.08 | ||||
| BPRS activation | 1, 342 | 0.96 | .33 | 0.11 | ||||||||
| COP | 1.71 | 0.86 | 1.46 | 0.62 | 1.36 | 0.49 | 1.28 | 0.48 | ||||
| SUP | 1.90 | 0.90 | 1.65 | 0.78 | 1.61 | 0.68 | 1.40 | 0.65 | ||||
| BPRS depression/anxiety | 1, 342 | 15.56 | <.01 | −1.73 | ||||||||
| COP | 2.33 | 1.01 | 1.93 | 0.79 | 1.66 | 0.70 | 1.91 | 0.94 | ||||
| SUP | 2.43 | 1.04 | 1.93 | 0.75 | 2.17 | 0.90 | 2.45 | 1.40 | ||||
| BPRS psychosis | 1, 341 | 0.21 | .64 | −0.11 | ||||||||
| COP | 2.49 | 1.28 | 1.88 | 0.82 | 1.46 | 0.63 | 1.53 | 0.74 | ||||
| SUP | 2.55 | 1.27 | 1.88 | 0.86 | 1.63 | 0.82 | 1.60 | 0.68 | ||||
| BPRS negative symptoms | 1, 341 | 0.80 | .37 | −0.22 | ||||||||
| COP | 2.87 | 1.21 | 2.50 | 1.08 | 2.06 | 0.89 | 1.53 | 0.64 | ||||
| SUP | 3.00 | 1.34 | 2.69 | 1.13 | 2.2 | 1.00 | 1.74 | 0.89 | ||||
| SANSc | 1, 336 | 1.64 | .20 | −0.11 | ||||||||
| COP | 45.91 | 23.3 | 36.7 | 22.8 | 27.32 | 20.23 | 23.96 | 19.21 | ||||
| SUP | 47.94 | 26.3 | 41.07 | 24.8 | 34.41 | 19.90 | 25.04 | 19.67 | ||||
| Knowledge | 1, 303 | 6.16 | .02 | 0.54 | ||||||||
| COP | 33.79 | 12.21 | 41.8 | 9.93 | 40.3 | 12.15 | 43.17 | 11.95 | ||||
| SUP | 30.64 | 12.87 | 34.12 | 13.42 | 40.74 | 12.53 | 39.28 | 12.30 | ||||
| GAF | 1, 335 | 1.83 | .18 | 0.37 | ||||||||
| COP | 49.48 | 14.41 | 61.28 | 13.9 | 73.00 | 20.62 | 74.76 | 16.40 | ||||
| SUP | 48.48 | 12.40 | 58.60 | 13.28 | 66.37 | 19.90 | 71.89 | 20.00 | ||||
Note: BPRS, Brief Psychiatric Rating Scale; GAF, Global Assessment Functioning Scale; SANS, Scale for the Assessment of Negative Symptoms.
aGroup effects based on mixed effects linear models with baseline as covariate, and with illness duration, time and treatment group, and their interactions as fixed effects. Degrees of freedom vary across analyses due to missing data.
bEffect size calculated by dividing model-based estimates of mean differences at the end of the study by pooled within-group standard deviation of raw scores.
cSum of single scores.
The mixed model linear regression analyses comparing the trajectories of the 2 groups over time showed significant main effects for group indicating greater improvements for COP than SUP on the BPRS total score, the BPRS depression/anxiety subscale, and Knowledge. The main effect of time in these analyses indicated significant improvements from the post-treatment assessment to the 1- and 2-year follow-up assessments in most outcomes, including BPRS total (F(2, 321) = 10.96, P < .001), BPRS psychosis (F(2, 341) = 7.87, P < .001), BPRS negative symptoms (F(2, 341) = 34.15, P < .001), BPRS activity (F(2, 342) = 3.97, P = .02), SANS (F(2, 336) = 13.59, P < .001), and GAF (F(2, 335) = 22.08, P < .001), but not for BPRS depression (F(2, 342) = 1.60, P = .202) or Knowledge (F(2, 303) = 1.47, P = .232). However, there were significant group by time interactions for BPRS depression, (F(2, 342) = 7.35, P < .01), and Knowledge, (F(2, 303) = 3.60, P = .028). Participants in the COP program either maintained or had further reductions in the severity of their depression from post-treatment to the follow-up assessments, compared to participants in SUP whose depression increased at the follow-ups. On the other hand, participants in COP maintained their Knowledge from post-treatment to the follow-ups, whereas those in SUP increased in Knowledge at the follow-ups.
Discussion
Contrary to our primary hypothesis that participants in COP would have lower rates of rehospitalization over the 2-year follow-up period than those in SUP, there were no differences between the groups. However, both groups had relatively low rates of hospitalization over the study period (COP: 38.3%, SUP: 36.7%). These rates are similar to those recently reported for the National Institute of Mental Health sponsored Recovery After Initial Schizophrenia Episode-Early Treatment Program (RAISE-ETP) study, a cluster randomized controlled trial involving 34 sites in which the 2-year hospitalization rate for participants in the specialty comprehensive treatment program for first episode psychosis was 34%, compared to 37% for those who received usual community care.37 Psychiatric hospitalization rates can be influenced by a variety of factors, including access to hospital beds and the adequacy of community-based services.38 It is possible that good quality of community care available to study participants following hospital discharge led to low rehospitalization rates for both COP and SUP participants.
Study participants in both groups improved significantly and similarly in psychotic and negative symptoms, and in overall functioning following hospital discharge over the 2-year follow-up period. The COP program would have to have been quite powerful to have demonstrated even stronger effects on improvement than those observed in the SUP group. However, consistent with our secondary hypotheses, participants in COP benefitted more than those in SUP on several outcomes. Patients randomized to COP improved significantly more in overall symptom severity on the BPRS-E and on the depression/anxiety subscale of the BPRS-E at post-treatment and at the 1- and 2-year follow-up assessments than those in SUP. In addition, while COP participants continued to improve in depression/anxiety severity at the follow-ups after discharge from the hospital, SUP participants showed a worsening in the severity of their depression/anxiety at the same follow-ups. COP participants also gained significantly more in Knowledge over the inpatient treatment phase than those in SUP, although the SUP group had caught up to the COP group by the follow-up assessments.
These findings suggest that the relatively brief inpatient COP program had an enduring effect on reducing overall symptom severity, and especially depression, over the following 2 years. Although COP participants also showed greater gains in knowledge of psychosis during the treatment phase than SUP participants, similar to prior research on programs containing psychoeducational components,39 the 2 groups did not differ in knowledge at the follow-up assessments, suggesting that the knowledge alone did not mediate the greater improvements in depression/anxiety for the COP group.
Concerns have previously been expressed that simply educating patients about schizophrenia could worsen depression or contribute to suicidal ideation.40,41 Goldstein argued in favor of more interactive teaching approaches aimed at helping patients’ understand the nature of their illness and its treatment.42 In the COP program, the use of interactive, psychoeducational teaching methods, combined with enhancing strategies for dealing with stress and symptoms, and cognitive restructuring to address self-stigmatizing beliefs about their mental illness, may have helped participants process their personal experiences related to the illness, and learn more effective ways of coping with it, resulting in greater and more sustained improvements in depression/anxiety and overall symptom severity over the 2-year follow-ups.
The findings reported here are generally consistent with prior research on the effects of psychoeducational,16 illness management,39,43 and cognitive-behavioral therapy for psychosis15 programs for schizophrenia. However, the preponderance of prior research on these approaches has focused on outpatient programs. In contrast, the COP program was provided during a 6–8 weeks inpatient phase, followed by discharge into the community. These results are encouraging because they suggest that the effects of a relatively time-limited, inpatient COP were sustained over a 2-year follow-up period after patients had been discharged into the community, and they support the potential benefits of psychosocial treatment during the inpatient phase. The study was conducted in a treatment setting that provided a broad range of psychotherapeutic and rehabilitative interventions in addition to pharmacological treatment, and therefore one might expect better overall outcomes for participants in both groups compared to a treatment setting more narrowly focused on pharmacological stabilization and safety.
Several limitations of this study should be noted. We did not obtain information about medication adherence over the course of the study, and thus the findings cannot address whether the greater improvement in symptoms for COP was due to improved adherence compared to SUP. Both treatment groups were conducted in the same inpatient setting, and thus it is likely that patients in the 2 programs interacted with each other, and it is possible that they compared their different experiences in their respective groups. Although patients in SUP could set their own agenda for each group session, there was overlap in the topics addressed in the COP and SUP groups, which could have minimized group differences in outcomes. The relatively limited length of the COP group, twelve 75-minute sessions over 6–8 weeks, and the breadth of topics covered in the group also raises of question of whether greater improvements in symptoms would have been observed if participants had been provided more opportunity to practice their skills. Finally, the average length of stay for the inpatients in this study was longer than the current average length of stay of psychiatric hospitalizations in the United States, suggesting that the COP program would either need to be abbreviated or provided on a more intensive basis in order to be implemented in such settings.
Several strengths of the study are also noteworthy. The drop-out rate was relatively low. The study included an active control group designed to control for nonspecific therapeutic factors. Last, the sample size was relatively large.
Conclusions
Compared to inpatient supportive psychotherapy, coping-oriented therapy, including both illness management and cognitive-behavioral therapy for psychosis, led to greater increases in knowledge about mental illness and more reductions in overall symptoms, especially in depression and anxiety. Furthermore, the benefits of the program on symptoms were sustained over 2 years following discharge from the hospital. This study suggests that COPs provided during the acute inpatient phase of treatment can have lasting benefits following discharge into the community. The findings suggest that more research is warranted on the effects of coping-oriented and similar programs provided in the inpatient setting.
Funding
This work was supported by the Eli Lilly International Foundation (grant number Eli 8265044; principal investigator A.S.) and Lilly Homburg GmbH Deutschland. No pharmaceutical company or commercial organization had any role in the statistical analysis or writing of this article for publication.
Acknowledgments
We dedicate this article to Marvin Herz, MD, an inspiring pioneer in his field, who passed away last year. We gratefully acknowledge the contribution of our former coworkers of the study: Brigitte Wolf, Susanne Amann, Petra Kümmler, Sabine Froschmayr, Andreas Gartenmaier, Letizia Gauck, Astrid Kaiser, Monika Dirsch, Jana Kopinke, Elisabeth Kopp, Inge Kreim, Ulrike Singer. We are indebted to the many patients who made the study possible. A.S. designed and led the implementation of the research study, and wrote the initial draft of the findings. K.T.M. provided consultation on the statistical analysis of the results, and helped write the first draft of the article, as well as the revisions of the article. T.vW. analyzed the data. R.E., H-J.M., and P.F. contributed to the design and implementation of the study, and interpretation of study findings. All co-authors approved the final manuscript. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Möller HJ, Schaub A, Riedel M. Schizophrene Psychosen. In: Möller HJ, Laux G, Kapfhammer HP, eds. Psychiatrie, Psychosomatik, Psychotherapie: Band 1: Allgemeine Psychiatrie, Band 2: Spezielle Psychiatrie. Heidelberg, Germany: Springer-Verlag; 2011:213–323. [Google Scholar]
- 2. Kane JM, Correll CU. Past and present progress in the pharmacologic treatment of schizophrenia. J Clin Psychiatry. 2010;71:1115–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mueser KT, Deavers F, Penn DL, Cassisi JE. Psychosocial treatments for schizophrenia. Annu Rev Clin Psychol. 2013;9:465–497. [DOI] [PubMed] [Google Scholar]
- 4. Nuechterlein KH, Dawson ME. A heuristic vulnerability/stress model of schizophrenic episodes. Schizophr Bull. 1984;10:300–312. [DOI] [PubMed] [Google Scholar]
- 5. Prochaska JO, DiClemente CC. The Transtheoretical Approach: Crossing the Traditional Boundaries of Therapy. Homewood, IL: Dow-Jones/Irwin; 1984. [Google Scholar]
- 6. Herz MI, Lamberti JS, Mintz J, et al. A program for relapse prevention in schizophrenia: a controlled study. Arch Gen Psychiatry. 2000;57:277–283. [DOI] [PubMed] [Google Scholar]
- 7. Liberman RP, Kopelowicz A. Training skills for illness self-management in the rehabilitation of schizophrenia: a family-assisted program for Latinos in California. Salud Ment. 2009;31:93–105. [Google Scholar]
- 8. Schaub A, Behrendt B, Brenner HD. A multi-hospital evaluation of the Medication and Symptom Management Modules in Germany and Switzerland. Int Rev Psychiatry. 1998;10:42–46. [Google Scholar]
- 9. Schaub A, Behrendt B, Brenner HD, Mueser KT, Liberman RP. Training schizophrenic patients to manage their symptoms: predictors of treatment response to the German version of the Symptom Management Module. Schizophr Res. 1998;31:121–130. [DOI] [PubMed] [Google Scholar]
- 10. Gingerich S, Mueser KT. Illness Management and Recovery: Personalized Skills and Strategies for Those with Mental Illness. 3rd ed. Center City, MN: Hazelden; 2011. [Google Scholar]
- 11. Beck AT, Rector NA, Stolar N, Grant P. Schizophrenia: Cognitive Theory, Research, and Therapy. New York, NY: Guilford Press; 2009. [Google Scholar]
- 12. Fowler D, Garety P, Kuipers E. Cognitive Behaviour Therapy for Psychosis: Theory and Practice. Chichester, UK: John Wiley & Sons; 1995. [Google Scholar]
- 13. Kingdon DG, Turkington D. Cognitive Therapy of Schizophrenia. New York, NY: Guilford Press; 2004. [Google Scholar]
- 14. Morrison AP, Renton JC, Dunn H, Williams S, Bentall RP. Cognitive Therapy for Psychosis: A Formulation-Based Approach. New York, NY: Brunner-Routledge; 2004. [Google Scholar]
- 15. Jones C, Hacker D, Cormac I, Meaden A, Irving CB. Cognitive behaviour therapy versus other psychosocial treatments for schizophrenia. Cochrane Database Syst Rev. 2012;4:CD008712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Xia J, Merinder LB, Belgamwar MR. Psychoeducation for schizophrenia. Cochrane Database Syst Rev. 2011;15:CD002831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34:523–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schaub A, Andres K, Brenner HD, Donzel G. Developing a group format coping-oriented treatment programme for schizophrenic patients. In: Brenner HD, Böker W, Genner R, eds. Towards a Comprehensive Therapy for Schizophrenia. Seattle, WA: Hogrefe & Huber Publishers; 1997:228–251. [Google Scholar]
- 19. Schaub A. Cognitive-behavioural coping-orientated therapy for schizophrenia: a new treatment model for clinical service and research. In: Perris C, McGorry P, eds. Cognitive Psychotherapy of Psychotic and Personality Disorders. Handbook of Theory and Practice. Chichester, UK: Wiley & Sons; 1998:91–109. [Google Scholar]
- 20. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 21. Lukoff D, Nuechterlein KH, Ventura J. Manual for the Expanded Brief Psychiatric Rating Scale (BPRS). Schizophr Bull. 1986;12:594–602. [Google Scholar]
- 22. Velligan D, Prihoda T, Dennehy E, et al. Brief psychiatric rating scale expanded version: How do new items affect factor structure? Psychiatry Res. 2005;135:217–228. [DOI] [PubMed] [Google Scholar]
- 23. Andreasen NC. Modified Scale for the Assessment of Negative Symptoms. Bethesda, MD: U.S. Department of Health and Human Services; 1984. [Google Scholar]
- 24. Söderberg P, Tungström S, Armelius BA. Special section on the GAF: Reliability of Global Assessment of Functioning ratings made by clinical psychiatric staff. Psychiatr Serv. 2005;56:434–438. [DOI] [PubMed] [Google Scholar]
- 25. Hahlweg K, Dürr H, Müller U. Familienbetreuung schizophrener Patienten: ein verhaltenstherapeutischer Ansatz zur Rückfallprophylaxe;Behandlungsanleitung und Materialien. Weinheim, Germany: Beltz; 1995. [Google Scholar]
- 26. Schaub A. Feedback Fragebogen. In: Bäuml J, Pitschel-Walz G, eds. Psychoedukation bei Schizophrenen Erkrankungen. Stuttgart, Germany: Schattauer; 2003:330–333. [Google Scholar]
- 27. Jahn T, Mussgay L. Die statistische Kontrolle möglicher Medikamenteneinflüsse in experimentalpsychologischen Schizophreniestudien: Ein Vorschlag zur Berechnung von Chlorpromazinäquivalenten. Z Klin Psychol. 1989;18:257–267. [Google Scholar]
- 28. Schaub A. Spezialstationen in der Behandlung schizophrener Psychosen. In: Möller HJ, ed. Handbuch der Therapie psychiatrischer Erkrankungen. 3rd ed. Stuttgart, Germany: Thieme; 2006:318–324. [Google Scholar]
- 29. Schaub A, Kümmler P, Gauck L, Amann S. Bewältigungsorientierte Therapie im stationären Bereich: Implikationen für die Langzeitbehandlung der Schizophrenie. In: Möller HJ, Müller N, eds. Schizophrenie: Langzeitverlauf und Langzeittherapie. Vienna, Austria: Springer; 2004:149–166. [Google Scholar]
- 30. Müller N, Schaub A, Wolf B, et al. Atypische Neuroleptika und bewältigungsorientierte Therapie in einem integrierten Schizophrenie-Behandlungskonzept. In: Bandelow B, Rüther E, eds. Therapie mit Neuroleptika. Darmstadt, Germany: Steinkopff; 2001:33–42. [Google Scholar]
- 31. Hedeker D, Gibbons RD. Longitudinal Data Analysis. New York, NY: Wiley; 2006. [Google Scholar]
- 32. Jennrich RI, Schluchter MD. Unbalanced repeated-measures models with structured covariance matrices. Biometrics. 1986;42:805–820. [PubMed] [Google Scholar]
- 33. Diggle P, Liang K, Zeger S. Analysis of Longitudinal Data. Oxford, UK: Oxford Science Publications; 2002. [Google Scholar]
- 34. Mueser KT, Pratt SI, Bartels SJ, et al. Randomized trial of social rehabilitation and integrated health care for older people with severe mental illness. J Consult Clin Psychol. 2010;78:561–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Raudenbush SW, Xiao-Feng L. Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychol Methods. 2001;6:387–401. [PubMed] [Google Scholar]
- 36. Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol Methods. 2009;14:43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kane JM, Robinson DE, Schooler NR, et al. Comprehensive versus usual care for first episode psychosis: two-year outcomes from the NIMH RAISE Early Treatment Program. Am J Psychiatry. 2016;173;362-372: doi:101176/appi.ajp.2015.15050632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hendryx MS, Rohland BM. A small area analysis of psychiatric hospitalizations to general hospitals. Effects of community mental health centers. Gen Hosp Psychiatry. 1994;16:313–318. [DOI] [PubMed] [Google Scholar]
- 39. Mueser KT, Corrigan PW, Hilton D, et al. Illness management and recovery for severe mental illness: a review of the research. Psychiatr Serv. 2002;53:1272–1284. [DOI] [PubMed] [Google Scholar]
- 40. Cunningham Owens DG, Carroll A, Fattah S, Clyde Z, Coffey I, Johnstone EC. A randomized, controlled trial of a brief interventional package for schizophrenic out-patients. Acta Psychiatr Scand. 2001;103:362–369. [DOI] [PubMed] [Google Scholar]
- 41. Misdrahi D, Denard S, Swendsen J, Jaussent I, Courtet P. Depression in schizophrenia: the influence of the different dimensions of insight. Psychiatry Res. 2014;216:12–16. [DOI] [PubMed] [Google Scholar]
- 42. Goldstein MJ. Psychosocial strategies for maximizing the effects of psychotropic medications for schizophrenia and mood disorder. Psychopharmacol Bull. 1992;28:237–240. [PubMed] [Google Scholar]
- 43. McGuire AB, Kukla M, Green AK, Mueser KT, Salyers MP. Illness management and recovery: a review of the literature. Psychiatr Serv 2014;65:171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]