Abstract
Objective:
Programs that view individuals as capable of taking an active role in managing their illness have gained importance in Europe and the United States. This article describes the implementation and evaluation of group psychoeducational and cognitive behavioral treatment programs at the Department of Psychiatry and Psychotherapy, Ludwig Maximilian University, Munich, Germany, over the past 20 years.
Methods:
Implementing psychoeducational programs was the first step to establish cognitive behavioral psychotherapy and dispel the myth of schizophrenia for patients. Programs are also provided for patients with mood disorders, substance use disorders, or both. These groups include topics such as psychoeducation about the illness, establishing rewarding activities, stress management, cognitive therapy, and relapse prevention.
Results:
More than 1000 patients with schizophrenia or mood disorders (380 schizophrenia, 563 major depression, and 110 bipolar) have participated in illness management groups to learn about their illness and its treatment, and to learn skills to manage their illness. Patients have expressed satisfaction with the programs, and research has supported their effectiveness.
Conclusions:
Individuals with severe disorders can benefit from psychoeducational and cognitive treatment programs if the programs are adapted to the level of neuropsychological functioning and compensate for cognitive deficits and emotional overload. These findings suggest that providing information about the illness and coping skills for patients and relatives are important for treatment outcome.
Key words: psychoeducation, cognitive-behavioral strategies, stress-vulnerability-coping model, transtheoretical model, schizophrenia, major depression
Introduction
Emil Kraepelin1,2 founded the psychiatric hospital in Munich in the 19th century and was one of the first to develop psychopathological entities that consider the interrelationships between physical and mental states in mental illness. The stress-coping-vulnerability,3 socio-developmental-cognitive,4 and transtheoretical5 models currently form the basis for combined treatment programs that include psychopharmacotherapy and psychotherapy in this hospital. Group psychotherapy has been offered since 1995 and includes psychoeducational and cognitive behavioral group interventions for postacute patients and their relatives.
The hospital has a long and successful history in psychopharmacotherapy, marked by the former department heads Hanns Hippius6–8 (1971–1994) and Hans-Jürgen Möller9,10 (1994–2012) and the current head, Peter Falkai (2012–present).11–13 Hanns Hippius was an important member of the Study Commission constituted by the German Federal Government to review the status of psychiatry 25 years after the Second World War. This commission concluded that the quality of services had to be improved for psychiatric in- and outpatients. Hippius and his co-workers’6 main research focus was clinical psychiatry, in particular biological psychiatry and clinical psychopharmacology. He established high standards of treatment in psychopharmacotherapy7, pioneered the introduction of clozapine8 as well as sociotherapy in psychiatry, and established both a day clinic and a self-help group for patients. His successor, Hans-Jürgen Möller,9,10 conducted genetic, neuroimaging, and follow-up studies of naturalistically treated patients with schizophrenia and mood disorders. He was interested in clinical-psychiatric research methodology as well as geriatric psychiatry and dementia. Furthermore, he shaped the hospital’s cognitive behavioral orientation by inviting Annette Schaub to implement group psychotherapy for patients and their relatives. He was succeeded by Peter Falkai, who has focused on structural imaging, molecular processing, genetics, and pathomorphological processing. His research aims are to increase the understanding of psychoses by identifying candidate molecules and pathways underlying the pathophysiology in schizophrenia. He is the author of the guidelines for the German Association of Psychiatry and Psychotherapy (DGPPN)11 on biological treatment of schizophrenia12 and is one of the editors of the the German version of the Diagnostic and Statistical Manual of Mental Disorders DSM-5.13 These recent and current heads of the department have strongly supported a pragmatic integration of biological treatment and psychotherapy. This article reviews the psychological and biological underpinnings of the implementation of these approaches from 1995 to 2015 and briefly summarizes research on psychoeducational and cognitive behavioral treatment programs at this hospital.14
Methods
Conceptual Frameworks Guiding Treatment Programs
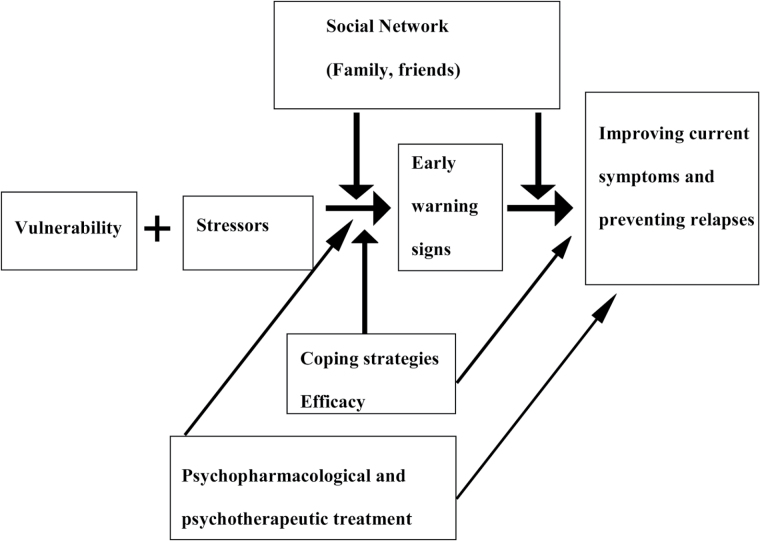
The stress-coping-vulnerability3, sociodevelopmental-cognitive,4 and transtheoretical5 models guide illness management or psychoeducational programs14 in psychiatric illness. The first model3 highlights the interactions between biological vulnerability, protective personal (eg, self-efficacy, antipsychotic medication) and environmental factors (eg, effective family problem solving [p. 392]), and stress factors (eg, high expressed emotion). The second model4 identifies the interplay between feedback loops in cognitive processing based on dysregulated dopamine leading to misattribution up to paranoia. The third model5 proposes that motivation to change develops over a series of stages and uses motivational enhancement approaches at the earliest stage to help clients identify and pursue their personal goals and to explore how improved illness management can help them achieve these goals. These models have provided a valuable framework for psychoeducational and cognitive programs aimed at modifying psychological and social-environmental factors that can precipitate relapses (eg, poor coping ability, lack of social support) and harnessing patient motivation for active collaboration with others, with the goal of improving the course of the illness.
Teaching schizophrenia patients about the nature of their illness is an essential element of therapy.15 In comparison to schizophrenia,3 there are different foci in bipolar disorder16 that place greater emphasis on circadian rhythms, or in major depression on multifactorial concepts, including psychosocial and biological concepts, linked in causal chains or cumulative feedback loops. Our description of the coping-oriented group treatment program17 provides the rationale for our treatment approach to schizophrenia, which we then adapted to bipolar disorder18 and major depression.19 The different components of this framework were adapted to patients’ needs (see figure 1).
Fig. 1.
Stress-vulnerability-coping model3,19 (modified by the authors).
Implementation of Psychoeducational and Cognitive Behavioral Programs
Treatment for schizophrenia and mood disorders has gained importance during the last 30 years. Beck’s cognitive approach20,21 laid the groundwork for cognitive-behavioral therapy (CBT) in schizophrenia and mood disorders. The term “psychoeducation” was used to refer to workshops aimed at educating relatives of persons with schizophrenia about the disorder and its treatment,22 which were later provided to relatives of persons with mood disorders23 and more recently to patients themselves.14 Whereas the terms psychoeducation and illness management14 have much in common, the former is more narrowly defined and refers to didactic, psychotherapeutic interventions that inform patients and/or their relatives about the illness and its treatment. Illness management programs include psychoeducation, but also teach cognitive-behavioral strategies aimed at improving treatment adherence, coping with symptoms and stressors, developing a relapse prevention plan, and modifying dysfunctional beliefs about the illness and oneself. The primary goal of these programs is to enhance the patients’ ability to manage their illness in collaboration with others.
In Europe, a greater emphasis had traditionally been placed on psychoeducation and teaching coping strategies, whereas in the US skills training approaches predominated.24 The results of a multicenter collaborative working group including 10 treatment sites set up to implement Medication and Symptom Management Modules25 demonstrated the clinical feasibility of these modules; however, cultural and professional differences between Europe and the United States had an influence on the ways that the modules were used.25–27 Currently, cognitive interventions at the hospital include both CBT for psychosis (CBTp) 28–30 and cognitive remediation,31,32 with influences from both the United States as well as Europe.
Meta-analyses have demonstrated the effectiveness of psychoeducational interventions in schizophrenia33 and cognitive-behavioral strategies in the latter34 and major depression.35 Individual and group treatment have been found to be of comparable effectiveness in schizophrenia.36 Meta-analysis of cognitive remediation have shown cognitive benefits for persons with schizophrenia, and when cognitive remediation has been combined with psychiatric rehabilitation benefit to other areas of functioning, relative to rehabilitation alone.37 Relapse prevention programs gained importance in schizophrenia38 and unipolar39–41 and bipolar disorders,14 and have shown lower relapse rates than standard treatment or comparable interventions in randomized controlled studies combining psychopharmacological and psychotherapeutic strategies.
From 1995 to 1997, illness management programs for schizophrenia and mood disorders were implemented at the Munich hospital.14,17–19,42 Specialized treatment units for schizophrenia43,44 and mood disorders45 were established, integrating pharmacological9 and CBT approaches.17–19,42,46,47 Three different group programs for schizophrenia,17 bipolar disorder,18 and major depression19 were implemented. The programs include psychoeducation to improve both knowledge about mental illness and treatment adherence. Strategies are taught to develop and support a lifestyle that promotes health and quality of life and to decrease chronic symptoms. All programs can be used in a single setting (compare with ref. Wykes et al36), and psychoeducational groups for relatives are available.17–19
Table 1 gives an overview of the main programs for schizophrenia and mood disorders. There are illness-related groups offered for the whole clinic following a specific treatment curriculum covering 4–12 sessions (4 for substance abuse, 12 for depression and schizophrenia), with a maximum of 13 patients per group. Additionally, there are ward-specific groups provided for patients in each of the 10 wards specialized on depression, schizophrenia, or substance abuse. These groups last for 8 sessions each and include a maximum of 18 patients. Shortly after admission, patients attend these groups to avoid waiting lists for illness-related groups. Due to cognitive impairments, patients may benefit from participating in more than one round of group sessions in their ward. Groups that provide psychoeducation (eg, knowledge about the illness) and teach cognitive behavioral strategies (eg, coping techniques, assign homework) are more demanding than psychoeducational groups, but appear to be tolerated well by patients. Psychoeducational groups mainly provide knowledge about the illness (working with flipcharts etc.), whereas cognitive groups focus on cognitive techniques and use homework assignments. The term cognitive-psychoeducational group relates to a combination of both (also see Schaub et al47). There is a high range of comorbidity, however, the groups do not deal with comorbidity in special up to now.
Table 1.
Psychoeducational and Cognitive Group Treatment in Psychiatric Disorders
| Contents |
| Psychoeducation: Providing information about the illness and its treatment on the basis of the stress-vulnerability-coping model3 |
| Symptom management, establishing rewarding activities |
| Recognizing and changing dysfunctional cognitions in illness and self-confidence |
| Relapse prevention |
| Programs |
| Ward-specific groupsa |
| Treatment-specific groups |
| Coping-orientated treatment in schizophrenia17 |
| Cognitive-psychoeducational treatment in bipolar disorder18 |
| Cognitive-psychoeducational treatment in depression19 |
| Cognitive-psychoeducational treatment in elderly patients with depression19,48 |
| Metacognitive training31 |
| Group for training eating habits in anorexia nervosa49,50 |
| Procedure |
| Treatment-specific groups |
| Group leader: 1 psychologist |
| Group members: 8–13 patients |
| Duration: 12 sessions, 2× a week, for 75–90 min |
| Treatment manual, information and work sheets, homework assignments, video-based supervision |
| Groups for relatives of patients with schizophrenia or affective disorders17–19 |
| Consulting hours for children of patients with psychiatric illness51 |
| Ward-specific groups |
| Groups cover depression, schizophrenia, and substance abuse on illness-specific wards |
The programs listed refer to 6 of 10 wards including patients with schizophrenia, mood disorders, mental, and behavioral disorders due to the use of psychoactive substances and an acute ward.
aLimited weekly to n = 18 persons.
bOnly if needed.
The different treatment programs were implemented in several phases.42
Phase 1.
First, we developed or modified existing manuals17,52 and assessed the level of neuropsychological functioning in different disorders.47 We adapted the programs to the average duration of inpatient stay.17 Furthermore, we visited special treatment settings in schizophrenia and depression to learn about common pitfalls. We started an education program for treatment teams, which included physicians, psychologists, and nurses, by providing workshops that provided information about the psychiatric disorders and advances in treatment, as well as training in behavioral skills for effective communication with patients. We also developed a questionnaire to assess patient’s perceptions of the effectiveness of treatments in order to optimize treatment strategies.
Phase 2.
Next, we conducted clinical assessments at the beginning of treatment, the end of treatment, and at follow-up in order to evaluate outcomes. Satisfaction with specific treatment programs was assessed in order to determine their applicability in the inpatient setting and whether they were acceptable to patients.53 We modified instruments to assess patients’ knowledge of mental illness and its treatment. Knowledge about psychosis was assessed using a modified multiple choice test based on Hahlweg.54
Phase 3.
Finally, we conducted randomized controlled trials to evaluate our programs. For example, we conducted one trial to evaluate whether the cognitive-psychoeducational group intervention led to greater gains in knowledge about the illness and better outcomes over 2 years as compared to a standard treatment control group.17 Measures for studies in schizophrenia covered the following instruments (see also Schaub et al17): Diagnoses were assessed according to the Diagnostic and Statistical Manual of Mental Disorders DSM-IV,55 symptoms were assessed with the Brief Psychiatric Rating Scale – Expanded (BPRS),56 with analyses based on Velligan’s factor analysis57 as well as with the Scale for the Assessment of Negative Symptoms (SANS).58 Psychosocial functioning was assessed with the Global Assessment Functioning Scale (GAF).55,59 Knowledge about psychosis and its treatment was assessed using a modified multiple choice test based on Hahlweg54 and satisfaction with treatment was assessed using a 4-item questionnaire53 administered at the end of each group treatment.
Kraepelin’s hospital opened its doors to accommodate the new spirit of comprehensive psychotherapy while continuing its successful history in psychopharmacotherapy. Parallel to our research, we began to recruit trainee psychologists by arranging collaborations with 5 behavioral institutes in Munich. The first author was appointed as supervisor by the Bavarian Medical Association and has since 1997 provided training and supervision for physicians and psychologists in CBT. Whereas at first she was in charge of training for the whole hospital, 2 additional leading psychologists have been added to the staff, one in 2004 and the other in 2011. She has been responsible for 6 wards. The number of psychologists receiving training in psychotherapy increased from 1 in 1995 to 232 in her area in 2016.
In recent years, it became necessary to develop new group programs or to modify existing ones in order to meet the needs of children and their parents with mental illness,51 patients with alcohol or drug dependence and comorbid depressive disorders,19 elderly patients with depression,48 as well as patients with anorexia nervosa (body mass index < 12).49,50 Additional programs developed now include metacognitive training,31 interpersonal therapy,60 treatment for chronic depression,61 stress management,62 social skills training,63 building up self-confidence,64 as well as social and skills training for borderline personality disorder.65 Progress was made by improving the salary for psychologists and providing medical seminars combined with training in CBT for physicians and psychologists. To ensure treatment continuity, we focused in particular on the gap between inpatient and outpatient treatment. Treatment contract documents for psychiatric patients were implemented to plan details related to the patients’ inpatient stay; after giving informed consent, decisions were made collaboratively on strategies to be taken at the medical or personal level, including treatment strategies and care for children.
Recently, treatment pathways in the care of patients gained importance in Germany66 and were established at this hospital for disorders such as depression, schizophrenia, substance abuse, chronic depression, and emotional instability. However, the development, implementation, and analysis of guidelines or clear-cut clinical pathways to care must consider individual, clinical, and care system aspects and their interplay. Results suggest that system aspects tend to dominate over clinical factors of schizophrenia and depression. As a consequence, the definition, implementation, and evaluation of clinical pathways or pathways to mental healthcare is first and foremost the responsibility of the national mental health care system and must be understood on that level, before findings are summarized internationally and models of best practice are established.
Results
Patients’ Diagnosis and Duration of Hospitalization From 1995 to 2015
Since 1995, the Department of Psychiatry and Psychotherapy, Ludwig Maximilian University, Munich, has 200 beds for inpatients in 10 wards. Statistical reports from April 1995 show that the most common diagnosis among the 1641 patients was schizophrenia (24.7%), followed by affective psychosis (23.6%) and alcohol and medication dependence (23.3%); all diagnoses were according to ICD-9.67 Diagnoses with prevalence rates below 10% included adaptive reactions (5.8%), organic psychoses (7.2%), neurosis (4.6%), personality disorders (3.8%), and nonorganic psychosis (2.1%). Patients’ mean age was 45 years (median 43 y; women: 48 y, median 47 y; men: 42 y, median 40 y). The mean total duration of hospital stay was 44.4 days (median: 33). Patients with nonpsychotic disorders caused by brain damage spent the longest time in hospital (mean 65.3 d, median 51), followed by affective psychosis (mean 63.0 d, median 49 d), neurosis (mean 54.1 d, median 42 d), and schizophrenia (mean 53.1 d, median 43 d). The interrelationship between duration of hospitalization and age showed that older patients had been hospitalized for more days.
After Peter Falkai took over as chairman of this hospital in 2012, he worked on optimizing the treatment process and reducing the duration of hospital stay. 20 years after the introduction of psychoeducational and cognitive-behavioral programs, in 2015 the number of inpatients was 50% higher than in 1995. The most common diagnosis among the 2806 inpatients was mood disorders (F3; 40%), followed by mental and behavioral disorders due to the use of psychoactive substances (F1; 25%), and schizophrenia, schizotypal personality disorder, and delusional disorders (F2; 15%); all diagnoses were according to ICD-10.68 Patients’ mean age was 45 years (women: 46 y; men: 44 y). The mean total duration of hospital stay was 29.1 days (median: 20.0) in 2015. The average length of stay of schizophrenia, schizotypal personality disorder, and delusional disorders (F2) was 38 days (median 28 d) compared to mood disorders (F3) 37 days (median 29 d).
We have also seen striking changes over the last 20 years with the duration of the hospital stay decreasing by about 50%. Additionally, 65 patients with schizophrenia or alcohol and drug dependence are treated in our outpatient clinic. As a result, mood disorders are the most common diagnosis among inpatients, followed by schizophrenia and disorders induced by psychoactive substances.
The Role of Neuropsychological Functioning in Psychotherapy
Neuropsychological functioning plays an important role in psychiatry and psychotherapy. Impaired neuropsychological functioning in schizophrenia has been evaluated in meta-analyses focusing on schizophrenia,69 schizophrenia or bipolar disorder,70 and first-episode schizophrenia.71 These studies indicate that schizophrenia is characterized by broad-based cognitive impairment, with varying degrees of deficit across all ability domains measured by standard clinical tests. Seven separable domains of cognitive deficits were identified in schizophrenia72 and a battery to measure them in clinical trials was developed. While separable, these cognitive domains have substantial interrelationships.
The data from 112 postacute patients with mood disorder or schizophrenia47 showed that despite comparable total scores in psychosocial functioning55 and psychopathology,56 there were significant differences in most subscales and different neuropsychological test profiles.57 Patients with depressive disorder performed better in short-term memory and speed than those with schizophrenia. Sound didactic and behavioral principles17,47 can compensate for deficits in neuropsychological functioning in severe psychiatric illness (eg, by using repetition, summaries, and illustrations). Another study focused on neuropsychological functioning and neuroimaging in 34 depressed inpatients and 34 healthy controls73 and found that reduced hippocampal volume was correlated with executive dysfunction. Hippocampal volumes and frontal lobe volumes were significantly smaller in patients than in controls, and lower hippocampal volumes were correlated with poorer performance in the Wisconsin Card Sorting Test.74
Studies of Illness Management Programs at 1- and 2-Year Follow-ups
The illness management programs17–19 proved to be clinically feasible in studies that included 98 patients with schizophrenia, 279 patients with major depression, and 86 patients with bipolar disorder, and resulted in a significant increase in knowledge about the respective illnesses; at the postassessment, about 90% of inpatients considered their program to be helpful.75 The program for mood disorders was investigated in a feasibility study including 231 participants, however, only 125 patients were adherent with treatment assessments (drop-out rate of 54% due to a broad inclusion criteria). The program was then differentiated for patients with major depression or bipolar disorders.76
We investigated the effects of group intervention for 62 bipolar patients who attended cognitive-psychoeducational group therapy and their 49 relatives.77 Psychoeducational interventions in bipolar patients and their relatives improved patients’ and their relatives’ knowledge of the illness and the burden of the illness as well as high expressed emotion were reduced in relatives at 1-year follow-up.77 52 patients with bipolar disorder studied in a naturalistic setting showed improvements in the severity of illness and differential treatment response.78 At the postassessment, patients with a higher education level performed better than those with less education. A higher number of previous hospitalizations and being male best predicted the readmission rate (30%) at the 2-year follow-up; however, the study lacked a control group, which limits the interpretation of the results.78
Randomized controlled trials with a 2-year follow-up17 evaluated group programs for schizophrenia and major depression. The first study in 196 patients with schizophrenia17 compared a coping-oriented treatment group with a supportive group as the control group (see article within this supplement).17 Participants in the coping-oriented group showed greater gains in knowledge from pre- to post-treatment than those in the control group, and improved more on the depression-anxiety subscale of the BPRS-E.56 Relapse rates did not differ significantly between the groups.
In the second study (Schaub A, Mueser KT, Von Werder T et al, in preparation) 177 patients with major depression were assigned to three different conditions: clinical management, clinical management combined with a group cognitive-behavioral therapy (CBT) program, or clinical management combined with an individual CBT program. At post assessment, patients in both CBT programs were more satisfied with the program than the patients without CBT. The results of 2 year outcome are on its way (personal communication).
Summary and Discussion
The challenge facing Kraepelin’s former hospital was to change a traditional “custodial” approach in which patients were seen as passive recipients of treatment to a one aimed at empowering patients to take an active role in their own recovery. As the hospital staff was ambivalent about this change, education and training opportunities (eg, lectures, workshops) for staff members were important to shifting attitudes and developing more recovery-oriented treatment skills. This work with psychologists, physicians, and nurses was new and exciting, and created a “collaborative spirit” that facilitated the process of change. Instilling hope that it was possible for people with severe mental illness to change, in staff members and patients alike, played a critical role in changing practices. In addition to providing information and training, creating greater transparency in the treatment process, promoting staff acceptance of diversity between patients, and adapting programs to better meet the patients’ needs (eg, having a “resting chair” in a group for the most impaired or most reluctant patient that acknowledged his or her willingness to attend the group allowed the person to take a passive role17,47) were important. Due to a primarily biological understanding of schizophrenia, there was some reluctance among staff members to understand that patients with schizophrenia are capable of expressing their own perspectives about their illness (see ref. Süllwold et al15), that they are able to identify warning signs of relapse, and to collaborate in preventing further relapses.
At the beginning of the 20th century, patients with schizophrenia were thought to be incapable of playing an active role in their treatment; however, over the last 30 years there have been profound changes.14–47,79–81 Novel conceptual frameworks3,4 and empirical data challenged the aforementioned Kraepelinian2 assumption that schizophrenia was a purely biological disease with an invariably downward trajectory. This has yielded hope that meaningful recovery from schizophrenia79–81 is possible and that patients can learn to improve the course of their illness. Education about schizophrenia, bipolar disorder, and depression and teaching effective self-help strategies14–42,75–81 is now widely accepted as a treatment standard. Illness management programs also include cognitive behavioral interventions, such as teaching coping strategies, instilling hope by reframing challenging experiences and setting goals, supporting treatment adherence, and providing groups for relatives that enhance social networks and reduce relapse rates. These programs form the basis for shared decision making and treatment processes at this hospital.42
Studies conducted in this hospital have demonstrated the feasibility, effectiveness, and efficacy of illness management group programs in patients with psychiatric illness.75–81 Therapeutic interventions are also important for children (under the age of 18) who have parents with a psychiatric illness.51 The interventions inform the children about the illness in a manner consistent with their developmental age, and seek to enhance their self-confidence and self-efficacy, both of which are important protective factors. Sharing information between professionals, relatives, patients, and children may facilitate their coping with the psychiatric illness and improve the quality of family life for all family members.
There have been striking changes over the last 20 years. This hospital has grown into the largest department of psychiatry and psychotherapy at a university hospital in Germany, treating 200 inpatients and 65 outpatients in a day clinic which did not exist in 1995. In 2015, the duration of hospitalization was reduced by about 50% compared to 1995. As a result, mood disorders are the most common diagnosis among inpatients, followed by schizophrenia and disorders induced by psychoactive substances.
Thanks to the outstanding achievements of Kraepelin and his successors, the hospital is known throughout Europe and the United States. Today, illness group programs combined with individual treatment and groups for relatives are regular elements of treatment. For many patients, the hospital buffers stressors such as worries about social stigma and problems concerning education, work, and family. Poor coordination between inpatient and outpatient treatment can risk significant gains in clinical stability and psychosocial functioning. Therefore physicians, psychologists, and social workers work closely together to ensure a good transition from the hospital to outpatient patient in order to continue the recovery process in the community. These results suggest that educating patients about their illness, training self-management skills, instilling hope, and enhancing self-esteem as well as strengthening the patient’s social network can be valuable components of a comprehensive approach to the treatment of inpatients.17–19,75–81
Funding
This work was supported by Eli Lilly International Foundation (grant number Eli 8265044; principal investigator: A.S.) and Lilly Homburg GmbH Deutschland and by German Ministry for Education and Research (grant number 01G19919 BMBF/DLR for subproject 6.7; Mednet Dep/Suiz I & II; principal investigator: A.S.). No pharmaceutical company or commercial organization had any role in the statistical analysis or writing of this paper for publication.
Acknowledgments
We thank the psychologists involved in the studies: L. Roth, U. Goldmann, M. Charypar, J. Kopinke, A. Neusser, P. Kümmler, B. Wolf, S. Amann, B. Bernhard, L. Gauck, N. Neubauer, and I. Schweiss. Thanks also to Mrs Richter for providing statistical data about patients. Collaborations have been established on imaging procedures (T. Frodl, University of Magdeburg), on treatment in bipolar disorder (H. Grunze), on psychoeducation and cognitive behavioral therapy (B. Behrendt, University of Homburg; S. Kraemer, J. Bäuml, G. Pitschel-Walz, Department of Psychiatry, Technical University of Munich; S. Klingberg, University of Tübingen), and on eating disorders (D. Fumi, U. Voderholzer, Psychosomatic Hospital Roseneck). We also have valuable cooperation with institutions in the United States (R. P. Liberman, University of California, Los Angeles) and Australia (P. McGorry, University of Melbourne). We thank J. Klesing, Board-certified Editor in the Life Sciences (ELS), for editing assistance with the manuscript. We are grateful to L. Süllwold, R. Engel, H. Hippius, H. J. Möller, P. Falkai, and especially to K. T. Mueser who supported the first author’s scientific work in schizophrenia throughout the last 20 years. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Kraepelin E. Psychiatrie. Ein Lehrbuch für Studierende und Ärzte. 7 Aufl., Bd. II. Leipzig, Germany: Barth; 1903. [English translation: Diefendorf AR. Clinical Psychiatry: A Textbook for Students and Physicians. New York, NY: MacMillan; 1923]. [Google Scholar]
- 2. Kraepelin E. Dementia Praecox and Paraphrenia. Facsimile edition. New York, NY: Robert E. Krieger; 1971. [Google Scholar]
- 3. Nuechterlein KH, Dawson ME, Gitlin M, et al. Developmental processes in schizophrenic disorders: longitudinal studies of vulnerability and stress. Schizophr Bull. 1992;18:387–425. [DOI] [PubMed] [Google Scholar]
- 4. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental-cognitive approach. The Lancet. 2014;383:1677–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Am Psychol. 1992;47:1102–1114. [DOI] [PubMed] [Google Scholar]
- 6. Hippius H, Möller H-J, Müller N, Neundörfer-Kohl G, eds. The University Department of Psychiatry in Munich. From Kraepelin and His Predecessors in Molecular Psychiatry. Heidelberg, Germany: Springer; 2008. [Google Scholar]
- 7. Benkert O, Hippius H, eds. Kompendium der Psychiatrischen Pharmakotherapie. 10th ed. Berlin, Germany: Spinger; 2014. [Google Scholar]
- 8. Hippius H. A historical perspective of clozapine. J Clin Psychiatry. 1999;60(suppl 12):22–23. [PubMed] [Google Scholar]
- 9. Möller H-J, Laux G, Kapfhammer H-P. Psychiatrie, Psychosomatik, Psychotherapie. Bd 1 und 2. Allgemeine und Spezielle Psychiatrie. 4th ed. Berlin, Germany: Springer; 2011. [Google Scholar]
- 10. Möller HJ, Riedel M, Jäger M, et al. Short-term treatment with risperidone or haloperidol in first-episode schizophrenia: 8-week results of a randomized controlled trial within the German Research Network on Schizophrenia. Int J Neuropsychopharmacol. 2008;11:985–997. [DOI] [PubMed] [Google Scholar]
- 11. Falkai P, ed. S3-Leitlinie Psychosoziale Therapien bei schweren psychischen Erkrankungen. S3 Praxisleitlinien in Psychiatrie und Psychotherapie. DGPPN. Berlin, Germany: Springer; 2013. [Google Scholar]
- 12. Hasan A, Falkai P, Wobrock T, et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizohrenia. Part 2: update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induces side-effects. World J Biol Psychiatry. 2013;14:2–44. [DOI] [PubMed] [Google Scholar]
- 13. Falkai P, Wittchen HU, eds. German Translation of the Diagnostic and Statistical Manual of Mental Disorders DSM-5, American Psychiatric Association (2013). Göttingen, Germany: Hogrefe; 2014. [Google Scholar]
- 14. Schaub A. Illness self-management programs in schizophrenia and severe affective disorders. In: Schaub A, ed. New Family Interventions and Associated Research in Psychiatric Disorders. Gedenkschrift in Honor of Michael J. Goldstein. Vienna, New York: Springer; 2002:229–247. [Google Scholar]
- 15. Süllwold H, Herrlich J. Providing schizophrenic patients with concept of illness. An essential element of therapy. Brit J Psychiatry. 161;1992(suppl 18):129–132. [PubMed] [Google Scholar]
- 16. Miklowitz DJ, Goldstein MJ. Bipolar Disorder. A Family-Focused Treatment Approach. New York, NY: Guilford; 1997. [Google Scholar]
- 17. Schaub A, Mueser KT, von Werder T, Engel R, Möller HJ, Falkai P. A randomized controlled trial of group coping-oriented therapy vs. supportive therapy in schizophrenia: results of a two year follow-up. Schizophr Bull. 2016; 42(suppl 1):S71–S80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schaub A, Bernhard B, Gauck L. Kognitiv-psychoedukative Therapie bei bipolare Erkrankungen. Ein Therapiemanual. Göttingen, Germany: Hogrefe; 2004. [Google Scholar]
- 19. Schaub A, Roth E, Goldmann U. Kognitiv-psychoedukative Therapie zur Bewältigung von Depressionen. Ein Therapiemanual. 2nd ed. p. 37. Göttingen, Germany: Hogrefe; 2013. [Google Scholar]
- 20. Beck AT, Rector NA, Stolar N, Grant P. Schizophrenia: Cognitive Theory, Research, and Therapy. New York, NY: Guilford Press; 2009. [Google Scholar]
- 21. Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guilford; 1979. [Google Scholar]
- 22. Anderson CM, Hogarty GE, Reiss DJ. Family treatment of adult schizophrenic patients: a psycho-educational approach. Schizophr Bull. 1980;6:490–505. [DOI] [PubMed] [Google Scholar]
- 23. Anderson CM, Griffin S, Rossi A, Pagonis I, Holder DP, Treiber R. A comparison study of the impact of education vs. process groups for families of patients with affective disorder. Family Process. 1986;25:185–205. [DOI] [PubMed] [Google Scholar]
- 24. Liberman RP, Kopelowicz A. Training skills for illness self-management in the rehabilitation of schizophrenia: a family-assisted program for Latinos in California. Salud Ment. 2009;31:93–105. [Google Scholar]
- 25. Schaub A, Behrendt B, Brenner HD. A multi-hospital evaluation of the Medication and Symptom Management Modules in Germany and Switzerland. Int Rev Psychiatry. 1998;10:42–46. [Google Scholar]
- 26. Schaub A, Behrendt B, Brenner HD, Mueser KT, Liberman RP. Training schizophrenic patients to manage their symptoms: predictors of treatment response to the German version of the Symptom Management Module. Schizophr Res. 1998;31:121–130. [DOI] [PubMed] [Google Scholar]
- 27. Gingerich S, Mueser KT. Illness Management and Recovery: Personalized Skills and Strategies for Those With Mental Illness. 3rd ed. Center City, MN: Hazelden; 2011. [Google Scholar]
- 28. Fowler D, Garety P, Kuipers E. Cognitive Behaviour Therapy for Psychosis: Theory and Practice. Chichester, UK: John Wiley & Sons; 1995. [Google Scholar]
- 29. Kingdon DG, Turkington D. Cognitive Therapy of Schizophrenia. New York, NY: Guilford Press; 2004. [Google Scholar]
- 30. Morrison AP, Renton JC, Dunn H, Williams S, Bentall RP. Cognitive Therapy for Psychosis: A Formulation-Based Approach. New York, NY: Brunner-Routledge; 2004. [Google Scholar]
- 31. Moritz S, Veckenstedt R, Randjbar S, Vitzthum F. Metakognitives Training + Individualisiertes Therapieprogramm für Menschen mit Psychose. Heidelberg, Germany: Springer; 2012. [Google Scholar]
- 32. Nuechterlein KH, Ventura J, McEwen SC, Gretchen-Doorly D, Vinogradov S, Subotnik KL. Enhancing cognitive training through aerobic exercise after a first schizophrenia episode: theoretical conception and pilot study. Schizophr Bull. 42;2016(suppl 1):44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Xia J, Merinder LB, Belgamwar MR. Psychoeducation for schizophrenia. Cochrane Database Syst Rev. 2011;15:CD002831. doi:10.1002/14651858.CD002831.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jones C, Hacker D, Cormac I, Meaden A, Irving CB. Cognitive behaviour therapy versus other psychosocial treatments for schizophrenia. Cochrane Database Syst Rev. 2012;4:CD008712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cuijpers P, Berking M, Andersson G, et al. A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Can J Psychiatry. 2013;58:376–385. [DOI] [PubMed] [Google Scholar]
- 36. Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34:523–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168:472–485. [DOI] [PubMed] [Google Scholar]
- 38. Herz MI, Lamberti JS, Mintz J, et al. A program for relapse prevention in schizophrenia: a controlled study. Arch Gen Psychiatry. 2000;57:277–283. [DOI] [PubMed] [Google Scholar]
- 39. Paykel ES, Scott J, Teasdale JD, Johnson AL, Garland A, Moore R. Prevention of relapse in residual depression by cognitive therapy. A controlled trial. Arch Gen Psychiatry. 1999; 56:829–835. [DOI] [PubMed] [Google Scholar]
- 40. Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy AL, and their combination for the treatment of chronic depression. N Engl J Med. 2000;342:1462–1470. [DOI] [PubMed] [Google Scholar]
- 41. Schramm E, van Calker D, Dykierek P, et al. An intensive treatment program of interpersonal psychotherapy plus pharmacotherapy for depressed inpatients: acute and long-term results. Am J Psychiatry. 2007;164:768–777. [DOI] [PubMed] [Google Scholar]
- 42. Schaub A. Kognitiv-psychoedukative Gruppeninterventionen bei stationären Patienten mit schizophrenen oder affektiven Erkrankungen. In: Möller H-J, Müller N, eds. Schizophrenie – Zukunftsperspektiven in Klinik und Forschung. New York, NY: Springer; 2010:267–279. [Google Scholar]
- 43. Müller N, Schaub A, Wolf B, et al. Atypische Neuroleptika und bewältigungsorientierte Therapie in einem integrierten Schizophrenie-Behandlungskonzept. In: Bandelow B, Rüther E, eds. Therapie mit Neuroleptika. Darmstadt, Germany: Steinkopff; 2001:33–42. [Google Scholar]
- 44. Schaub A. Spezialstationen in der Behandlung schizophrener Psychosen. In: Möller HJ, ed. Handbuch der Therapie psychiatrischer Erkrankungen. 3rd ed. Stuttgart, Germany: Thieme; 2006:318–324. [Google Scholar]
- 45. Schaub A. Angehörigenarbeit und psychoedukative Patientengruppen in der Therapie affektiver Störungen. In: Möller H-J, ed. Therapie psychiatrischer Erkrankungen. 3rd ed. Stuttgart, Germany: Thieme; 2006:498–508. [Google Scholar]
- 46. Klingberg S, Schaub A, Conrad B. Rezidivprophylaxe bei schizophrenen Störungen. Ein kognitiv-verhaltenstherapeutisches Behandlungsmanual. Weinheim, Germany: Beltz Psychologie Verlags Union; 2003. [Google Scholar]
- 47. Schaub A, Neubauer N, Mueser K, Engel R, Möller H-J. Neuropsychological functioning in inpatients with affective disorders or schizophrenia. BMC Psychiatry. 2013;13:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Maercker A, Forstmeier S. Der Lebensrückblick in Therapie und Beratung. Berlin: Springer;2013. [Google Scholar]
- 49. Born C, Meisenzahl E, Schüle C, Schaub A. Therapie schwerer Anorexia nervosa. Ein psychiatrisches Behandlungskonzept mit somatischem Schwerpunkt. Stuttgart, Germany: Kohlhammer; 2015. [Google Scholar]
- 50. Born C, de la Fontaine L, Winter, et al. First results of a prefeeding program in a psychiatric intensive care unit for patients with extreme anorexia nervosa. BMC Psychiatry. 2015;15:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Schaub A, Frank R. Sprechstunde für Kinder psychisch kranker Eltern. Monatschrift Kinderheilkunde. 2010;158:858–867. [Google Scholar]
- 52. Hautzinger M. Kognitive Verhaltenstherapie bei Depressionen. 6 ed. Weinheim, Germany: Psychologie Verlags Union; 2003. [Google Scholar]
- 53. Schaub A.Feedback Fragebogen. In: Bäuml J, Pitschel-Walz G, eds. Psychoedukation bei Schizophrenen Erkrankungen. Stuttgart, Germany: Schattauer; 2003:330–333. [Google Scholar]
- 54. Hahlweg K, Dürr, Müller U. Familienbetreuung schizophrener Patienten: ein verhaltenstherapeutischer Ansatz zur Rückfallprophylaxe;Behandlungsanleitung und Materialien. Weinheim, Germany: Beltz; 1995. [Google Scholar]
- 55. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). 4th ed. Washington, DC; American Psychiatric Association; 1994. [Google Scholar]
- 56. Lukoff D, Nuechterlein KH, Ventura J. Manual for the Expanded Brief Psychiatric Rating Scale (BPRS). Schizophr Bull. 1986;12:594–602. [Google Scholar]
- 57. Velligan D, Prihoda T, Dennehy E, et al. Brief Psychiatric Rating Scale Expanded Version: How do new items affect factor structure? Psychiatry Res. 2005;135:217–228. [DOI] [PubMed] [Google Scholar]
- 58. Andreasen NC. Modified Scale for the Assessment of Negative Symptoms. Bethesda, MD: U.S. Department of Health and Human Services; 1984. [Google Scholar]
- 59. Söderberg P, Tungström S, Armelius BA. Special section on the GAF: Reliability of Global Assessment of Functioning ratings made by clinical psychiatric staff. Psychiatr Serv. 2005;56:434–438. [DOI] [PubMed] [Google Scholar]
- 60. Schramm E. Interpersonelle Psychotherapie - zur Behandlung depressiver und anderer psychischer Störungen. Stuttgart, Germany: Schattauer; 2010. [Google Scholar]
- 61. McCullough JP. Treatment for Chronic Depression. Cognitive Behavioral Analysis System of Psychotherapy. New York, NY: Guilford; 2003. [DOI] [PubMed] [Google Scholar]
- 62. Kaluza G. Stressbewältigung. 2nd ed. Heidelberg, Germany: Springer; 2011. [Google Scholar]
- 63. Hinsch R, Pfingsten U. Training sozialer Kompetenzen. 4th ed. Tübingen, Germany: Beltz PVU; 2012. [Google Scholar]
- 64. Potreck-Rose F, Jacob G. Selbstzuwendung, Selbstakzeptanz, Sebstvertrauen. 9th ed. Suttgart: Klett-Cotra; 2015. [Google Scholar]
- 65. Linehan M. Cognitive-Behavioral Treatment of Borderline Personality Disorders. New York, NY: Guilford Press; 2003. [Google Scholar]
- 66. Salize HJ, Voß E, Werner A, Falkai P, Hauth I. Treatment pathways in the care of patients with schizophrenia and depression. Article in German. Nervenarzt. 2015;11: 1358–1370. [DOI] [PubMed] [Google Scholar]
- 67. Degkwitz R. Diagnoseschlüssel und Glossar psychiatrischer Krankheiten - 5. Aufl. korrigiert nach der 9. Revision der ICD. Berlin, Heidelberg: Springer; 1980. [Google Scholar]
- 68. Dilling H, Mombour W, Schmidt MH. Internationale Klassifikation psychischer Störungen, ICD-10 Kapitel V (F), Klinisch-diagnostische Leitlinien. Bern, Göttingen: Verlag Hans Huber; 1991. [Google Scholar]
- 69. Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12:426–445. [DOI] [PubMed] [Google Scholar]
- 70. Krabbendam L, Arts B, van Os J, Aleman A. Cognitive functioning in patients with schizophrenia and bipolar disorder: a quantitative review. Schizophr Res. 2005;80:137–149. [DOI] [PubMed] [Google Scholar]
- 71. Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ. Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology. 2009;23: 315–336. [DOI] [PubMed] [Google Scholar]
- 72. Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK. Identification of separable cognitive factors in schizophrenia. Schizophr Res. 2004;72:29–39. [DOI] [PubMed] [Google Scholar]
- 73. Frodl T, Schaub A, Banac S, et al. Reduced hippocampal volume correlates with executive dysfunctioning in major depression. J Psychiatry Neurosci. 2006;31:316–323. [PMC free article] [PubMed] [Google Scholar]
- 74. Milner B. Effects of different brain lesions on card sorting. Arch Neurol. 1963;9:90–100. [Google Scholar]
- 75. Schaub A, Kümmler P, Goldmann U, et al. Bewältigungsorientierte Ansätze bei depressiven, bipolaren und schizophrenen Erkrankungen. In: Behrendt B, Schaub A, eds. Handbuch Psychoedukation und Selbstmanagement. Verhaltenstherapeutische Ansätze in der Praxis. 2nd ed. Tübingen, Germany: DGVT; 2008:193–207. [Google Scholar]
- 76. Schaub A, Kopinke J, Neußer A, Charypar M. Kognitiv-psychoedukative Gruppenintervention bei stationären Patienten mit depressiven Erkrankungen – Ergebnisse einer prospektiven Pilotstudie. Verhaltenstherapie. 2007;17:167–173. [Google Scholar]
- 77. Bernhard B, Schaub A, Kümmler P, et al. Impact of cognitive-psychoeducational interventions in bipolar patients and their relatives. Eur Psychiatry. 2006;21:81–86. [DOI] [PubMed] [Google Scholar]
- 78. Schaub A, Neubauer N, Bernhard B, Born C, Möller H-J, Grunze H. Kognitiv-psychoedukative Gruppenintervention bei bipolar erkrankten Patienten: Pilotstudie mit 2-Jahres-Katamnese. Z Neurologie und Psychiatrie. 2013;81(suppl 1): S30–S34. [DOI] [PubMed] [Google Scholar]
- 79. Libermann RP. Recovery From Disability. Manual of Psychiatric Rehabilitation. Washington, DC: American Psychiatric Publishing; 2010. [Google Scholar]
- 80. Mueser KT, Deavers F, Penn DL, Cassisi J. Psychosocial treatments for schizophrenia. Annu Rev Clin Psychol. 2013;9:465–497. [DOI] [PubMed] [Google Scholar]
- 81. Kane JM, Robinson DE, Schooler NR, et al. Comprehensive versus usual care for first episode psychosis: two-year outcomes from the NIMH RAISE Early Treatment Program (published online ahead of print October 20, 2015) Am J Psychiatry. doi:10.1176/appi.ajp.2015.15050632. [DOI] [PMC free article] [PubMed] [Google Scholar]