Abstract
Individuals with favorable levels of all readily measured major CVD risk factors (low CV risk) during middle age incur lower cardiovascular morbidity and mortality, lower all-cause mortality, and lower Medicare costs at older ages compared to adults with one or more unfavorable CVD risk factors. Studies on predictors of low CV risk in Hispanics/Latinos have focused solely on Mexican-Americans. The objective of this study was to use data from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL; enrolled 2008 to 2011) to assess relationships of nativity and length of residence in the US, a commonly used proxy for acculturation, with low CV risk (not currently smoking; no diabetes; untreated total cholesterol <200mg/dL; untreated blood pressure <120/<80; body mass index <25 kg/m2; and no major ECG abnormalities) in 15,047 Central American, South American, Cuban, Dominican, Mexican, Puerto Rican men and women, and Hispanic/Latino men and women identifying as other or >1 heritage. We also tested whether associations varied by Hispanic/Latino background. Women living in the US<10 years were 1.96 (95% confidence interval: 1.37, 2.80) times more likely to be low CV risk than US-born women after adjusting for sociodemographic characteristics, diet, physical activity, and self-reported experiences of ethnic discrimination. Findings varied in men by Hispanic/Latino background, but length of residence was largely unrelated to low CV risk. These findings highlight the role acculturative processes play in shaping cardiovascular health in Hispanics/Latinos.
Keywords: Hispanics/Latinos, acculturation, cardiovascular health
INTRODUCTION
Major modifiable cardiovascular disease risk factors, such as smoking, hypertension, hyperglycemia, hypercholesterolemia, and obesity, account for a substantial proportion of cardiovascular disease (CVD) deaths in the US.1–3 Individuals with favorable levels of all readily measured major CVD risk factors (low CV risk) during middle age incur lower cardiovascular morbidity and mortality, lower all-cause mortality, and lower Medicare costs at older ages compared to adults with one or more unfavorable CVD risk factors.4–7 Such evidence provides a strong foundation for the promotion of cardiovascular health by achieving and maintaining optimal levels of all CVD risk factors.
Few published studies have assessed the prevalence of low CV risk among Hispanics/Latinos;8, 9 the limited research data suggest that foreign-born Hispanics/Latinos have better cardiovascular health than their US-born counterparts.9 However, this health advantage among foreign-born Hispanics/Latinos appears to diminish over time,9 possibly due to increased exposure to different sociocultural and environmental factors (i.e., acculturation) that lead to adverse changes in dietary practices, physical activity levels, and weight.9, 10 One limitation of the current literature on predictors of low CV risk is that they have focused solely on Mexican-Americans. Hispanics/Latinos living in the US are a diverse group, and there may be differences in behavioral and biological factors related to cardiovascular health by country of origin. For example, a study of acculturation and diabetes prevalence found that acculturation was positively associated with diabetes among non-Mexican-origin Hispanics but showed no association between acculturation and diabetes for Mexican-origin Hispanics.11
In addition, the acculturation process experienced by Hispanics/Latinos with increasing time spent in the US or across generations may vary by country of origin. Previous studies have shown substantial variation in CVD risk factor prevalence across Latin American countries,12 which may be indicative of differences in dietary behaviors and physical activity levels. It is also possible that some Hispanic/Latino background groups are exposed to higher levels of stress associated with ethnic discrimination and thus experience more rapid health declines, while others are better able to maintain social ties and health-promoting behaviors from their country of origin.13, 14
In this study we built on the existing literature by using data from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) to assess relationships of nativity and length of residence in the US, a commonly used proxy for acculturation, with low CV risk prevalence in a diverse group of Hispanics/Latinos. We also examined whether these associations varied by Hispanic/Latino background.
METHODS
HCHS/SOL is a multi-site community-based study of 16,415 Hispanic/Latino adults living in Bronx, New York; Chicago, Illinois; Miami, Florida; and San Diego, California.15 Households were selected with a stratified, 2-stage area probability sampling design in each of the 4 field centers.16 Both stages oversampled certain strata to increase the likelihood that a selected address yielded a Hispanic/Latino household.
Eligible households were screened by study staff via in-person or telephone contacts. Individuals were considered eligible if they were ages 18–74 years old at the time of screening in 2008 to 2011, self-identified as Hispanic/Latino, were able to complete a study examination, and reported no plans to move from the study area. Persons aged 45 to 74 years were oversampled (n=9714; 59.2%) to facilitate examination of target outcomes. Of the persons who fulfilled eligibility criteria and were screened, 41.7% were enrolled.
Of the 16,415 HCHS/SOL participants, we excluded 1,368 participants who have missing data on length of residence in US (n=121), healthcare coverage (n=264), low risk factors (n=716), or other covariates (n=267). Thus, these analyses are based on data from 15,047 participants (5,995 men and 9,052 women).
Variables
Based on self-reported nativity and length of residence in the US, participants were categorized as: foreign-born and having lived in the US <10 years; foreign-born and having lived in the US ≥10 years; or US-born (reference group). Sociodemographic variables included age at time of examination, gender, self-reported Hispanic/Latino background (Central American, South American, Cuban, Dominican, Mexican, Puerto Rican, or other/more than 1 heritage), current health insurance status (any vs. none), and education (less than high school diploma or equivalent, high school diploma or equivalent, and more than high school degree).
Low CV risk was defined as meeting all of the following criteria: total serum cholesterol <200 mg/dL and not on cholesterol-lowering medications; systolic/diastolic blood pressure <120/<80 mm Hg and not on antihypertensive medications; BMI <25.0 kg/m2; fasting plasma glucose <100 mg/dl and no history of diabetes mellitus; not currently smoking; and no major ECG abnormalities.5 These cutpoints were chosen to be consistent with the American Heart Association’s criteria for ideal cardiovascular health.17–19
Total serum cholesterol was measured using a cholesterol oxidase enzymatic method. After a 5-minute rest period, 3 seated blood pressure measurements were obtained with an automatic sphygmomanometer; the second and third readings were averaged. Participants were asked to bring in all prescription and non-prescription medications taken in the past month. Cholesterol-lowering medication use and antihypertensive medication use was based on the medications brought to the exam or self-report. Height was measured to the nearest centimeter and body weight to the nearest 0.1 kg. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Plasma glucose was measured using a hexokinase enzymatic method (Roche Diagnostics). History of diabetes and current smoking status were based on self-report.
A standard, 10-second, simultaneous, 12-lead electrocardiogram at rest was digitally acquired using a GE MAC 1200 electrocardiograph (GE, Milwaukee, Wisconsin) at 10 mm/mV calibration and a speed of 25 mm/s. ECG abnormalities were classified and coded using the Minnesota ECG Classification.20 Major ECG abnormalities included major ventricular conduction defect; definite myocardial infarction (defined as the presence of major Q-wave abnormalities); possible myocardial infarction (defined as the presence of minor Q-QS wave plus major ST-T abnormalities); major isolated ST-T abnormalities; left ventricular hypertrophy plus major ST-T abnormalities; major atrioventricular conduction abnormalities; and major QT prolongation (QT interval ≥116% or JTI if QRS interval ≥120 ms), pacemaker, and other major arrhythmias.
Self-reported duration (average number of days and average minutes/day) and intensity (moderate or vigorous) of recreational and work-related physical activity was assessed. Self-reported duration of transportation-related activity (walking or biking) was also assessed and was considered of moderate intensity. Total physical activity was categorized based on the 2008 US physical activity guidelines as meeting the guidelines (≥150 minutes of moderate-intensity activity a week, or ≥75 minutes of vigorous-intensity activity a week, or an equivalent combination of the two); being physically activity but not meeting the guidelines; and being physically inactive.21
Dietary intake was ascertained by two 24- hour dietary recalls administered 6 weeks apart. Dietary quality was assessed using the 2010 Alternative Healthy Eating Index (AHEI-2010), which is derived from the following 11 components: 1) servings/day of vegetables not including potatoes; 2) servings/day of whole fruit; 3) servings/day of whole grains; 4) servings/day of sugar sweetened beverages and fruit juice; 5) servings/day of nuts and legumes; 6) servings/day of red/processed meats; 7) % energy from trans fats; 8) mg/day of long-chain (n-3) fats; 9) % energy from polyunsaturated fatty acids; 10) mg/day of sodium; and 11) drinks/day of alcohol.22 The NCI method was used to predict usual intake for each component.23 The AHEI-2010 score is the sum of the 11 individual component scores, each ranging from 0 (worst) to 10 (best), leading to an overall score from 0 to 110.
Ethnic discrimination was self-reported based on responses to a single question asking how often participants are treated unfairly because they are Hispanic/Latino. Participant responses were categorized as never, sometimes, and often/always.
Analyses
All analyses were weighted to account for selection probability and to at least partially adjust for any bias effects caused by differential nonresponse. The weights were trimmed to limit precision losses and calibrated to the 2010 Census characteristics by age, gender, and Hispanic/Latino background in each field center’s target population. All analyses also accounted for cluster sampling and the use of stratification in sample selection.
Associations of length of residence in the US with low CV risk varied significantly by gender in models adjusted for sociodemographic characteristics (P for interaction <0.001), therefore all analyses are presented stratified by gender. Descriptive statistics were generated on the distribution of study covariates by nativity and length of residence in the US. Differences in participant characteristics by nativity and length of residence in the US were examined using F-tests or Χ2-tests as appropriate. Logistic regression models were used to examine the associations of length of residence with low CV risk. Initial models were adjusted for age, study site, Hispanic/Latino background, education and insurance status. Subsequent models were additionally adjusted for dietary quality, physical activity, and ethnic discrimination. Interactions of length of residence with Hispanic/Latino background were tested to assess whether associations of length of residence with low CV risk varied by Hispanic/Latino background in models adjusted for socioeconomic and demographic characteristics. All analyses were conducted using SAS 9.3 survey procedures (SAS Institute, Cary, NC).
RESULTS
US-born women were younger than those in both foreign-born groups (Table 1). Women of Mexican, Puerto Rican, and “other” Hispanic/Latino backgrounds were less likely to have lived in the US <10 years (rather than ≥10 years or US-born), while Cubans, Central Americans, and South Americans were most likely to be more recent immigrants. A higher proportion of women who were US-born had more than a high school diploma and had current health insurance, compared to women who had lived in the US for <10 or ≥10 years. US-born women were also more likely to meet the physical activity guidelines, but they had the lowest mean AHEI-2010 score. There was no significant difference in reported frequent exposure to ethnic discrimination by length of residence in the US. The distribution of all covariates by length of residence in the US for men was similar to findings for women (Table 2).
Table 1.
Participant characteristics by nativity and length of residence in US among women: HCHS/SOL, 2008–2011
| Length of residence <10 years (n=2174) |
Length of residence ≥ 10 years (n=5413) |
US born (n=1465) |
p- value |
|
|---|---|---|---|---|
| Mean age | 40.1 (39.2,41.1) | 47.1 (46.4,47.8) | 31.3 (30.5,32.0) | <0.001 |
| Hispanic/Latino background, % |
||||
| Mexican | 33.3 (28.3,38.4) | 41.6 (38.0,45.1) | 39.6 (35.3,44.0) | <0.001 |
| Cuban | 35.4 (29.5,41.4) | 14.1 (11.5,16.8) | 6.5 (4.5,8.5) | <0.001 |
| Puerto Rican | 3.3 (2.0,4.6) | 14.0 (12.1,15.8) | 32.3 (28.4,36.2) | <0.001 |
| Dominican | 8.8 (6.4,11.1) | 13.6 (11.6,15.7) | 7.9 (4.9,11.0) | <0.001 |
| Central American | 9.9 (7.6,12.2) | 8.3 (7.0,9.6) | 2.6 (1.5,3.7) | <0.001 |
| South American | 7.4 (5.9,8.9) | 5.5 (4.7,6.4) | 1.2 (0.6,1.8) | <0.001 |
| Other / >1 background group |
1.9 (1.1,2.6) | 2.8 (1.6,4.1) | 9.8 (7.7,11.9) | <0.001 |
| Site, % | ||||
| Bronx | 16.4 (13.1, 19.8) | 31.9 (27.9, 35.8) | 39.0 (34.3, 43.7) | <0.001 |
| Chicago | 11.0 (8.8, 13.2) | 16.1 (14.0, 18.3) | 17.1 (14.1, 20.1) | <0.001 |
| Miami | 50.0 (43.7, 56.4) | 25.2 (21.3, 29.1) | 9.9 (7.3, 12.5) | <0.001 |
| San Diego | 22.6 (17.3, 27.8) | 26.8 (23.4, 30.2) | 34.0 (29.4, 38.6) | <0.001 |
| Education, % | ||||
| <High school | 26.5 (23.8,29.2) | 39.6 (37.2,42.0) | 23.4 (20.1,26.7) | <0.001 |
| High school | 30.8 (28.0,33.5) | 23.7 (21.6,25.8) | 26.3 (22.8,29.8) | <0.001 |
| >High school | 42.8 (39.5,46.0) | 36.7 (34.3,39.1) | 50.3 (46.6,54.0) | <0.001 |
| Any insurance, % | 34.2 (31.3,37.1) | 57.0 (54.2,59.8) | 67.5 (63.6,71.3) | <0.001 |
| Physical Activity, % | ||||
| Inactive | 27.6 (25.1,30.2) | 27.3 (25.3,29.2) | 19.8 (16.8,22.8) | <0.001 |
| Active but not meeting the guidelines |
16.3 (14.0,18.6) | 16.0 (14.4,17.7) | 12.1 (10.0,14.2) | 0.006 |
| Meeting the guidelines | 56.0 (53.2,58.9) | 56.7 (54.6,58.8) | 68.1 (64.7,71.4) | <0.001 |
| Mean AHEI score | 45.5 (44.9,46.2) | 48.5 (48.2,48.9) | 42.8 (42.3,43.3) | <0.001 |
| Discrimination, % | ||||
| Never | 58.9 (55.8,62.0) | 49.7 (47.3,52.1) | 49.1 (45.7,52.5) | <0.001 |
| Sometimes | 32.1 (29.2,34.9) | 39.9 (37.8,42.1) | 39.3 (35.9,42.7) | <0.001 |
| Often/always | 9.0 (7.3,10.7) | 10.4 (8.9,11.8) | 11.6 (8.5,14.7) | 0.31 |
Abbreviations: CV, cardiovascular; AHEI, Alternative Healthy Eating Index
Table 2.
Participant characteristics by nativity and length of residence in US among men: HCHS/SOL, 2008–2011
| Length of residence <10 years (n=1378) |
Length of residence ≥ 10 years (n=3490) |
US born (n=1127) |
p- value |
|
|---|---|---|---|---|
| Mean age | 37.2 (36.2,38.2) | 46.9 (46.1,47.6) | 31.6 (30.7,32.6) | <0.001 |
| Hispanic/Latino background group, % |
||||
| Mexican | 31.5 (25.6,37.3) | 38.5 (34.8,42.2) | 40.3 (35.3,45.3) | 0.0081 |
| Cuban | 37.1 (30.7,43.5) | 22.8 (19.1,26.5) | 6.3 (4.3,8.3) | <0.001 |
| Puerto Rican | 4.2 (2.6,5.8) | 13.5 (11.6,15.4) | 34.1 (30.1,38.2) | <0.001 |
| Dominican | 7.6 (5.4,9.8) | 9.1 (7.4,10.7) | 5.4 (3.2,7.7) | 0.0118 |
| Central American | 10.3 (7.6,12.9) | 8.7 (7.2,10.1) | 2.1 (1.1,3.1) | <0.001 |
| South American | 7.1 (5.2,9.0) | 5.2 (4.3,6.1) | 1.3 (0.7,1.9) | <0.001 |
| Other / >1 background group |
2.2 (1.1,3.4) | 2.3 (1.5,3.1) | 10.5 (7.9,13.2) | <0.001 |
| Site, % | ||||
| Bronx | 17.0 (13.2, 20.8) | 26.0 (22.8, 29.2) | 35.1 (30.5, 39.7) | <0.001 |
| Chicago | 14.4 (11.3, 17.5) | 19.1 (16.5, 21.7) | 16.6 (13.7, 19.6) | <0.001 |
| Miami | 50.6 (43.8, 57.5) | 31.4 (26.7, 36.1) | 9.6 (6.9, 12.4) | <0.001 |
| San Diego | 18.0 (12.5, 23.4) | 23.5 (20.1, 26.9) | 38.7 (33.0, 44.4) | <0.001 |
| Education, % | ||||
| <High school | 26.4 (23.2, 29.7) | 39.7 (37.3, 42.0) | 20.2 (17.1, 23.4) | <0.001 |
| High school | 32.6 (29.2, 36.0) | 26.6 (24.5, 28.7) | 35.4 (31.1, 39.6) | <0.001 |
| >High school | 41.0 (36.7, 45.2) | 33.7 (31.4, 36.1) | 44.4 (40.3, 48.5) | <0.001 |
| Any insurance, % | 31.4 (27.5, 35.2) | 49.3 (46.5, 52.0) | 61.6 (57.5, 65.6) | <0.001 |
| Physical Activity, % | ||||
| Inactive | 15.7 (13.0,18.4) | 17.9 (16.1,19.8) | 10.0 (7.8,12.2) | <0.001 |
| Active but not meeting the guidelines |
9.1 (7.3,10.8) | 10.6 (9.0,12.1) | 6.2 (4.4,8.0) | 0.0018 |
| Meeting the guidelines | 75.2 (72.2,78.2) | 71.5 (69.2,73.8) | 83.8 (81.2,86.5) | <0.001 |
| Mean AHEI score | 47.9 (47.3,48.6) | 50.7 (50.2,51.1) | 45.8 (45.3,46.3) | <0.001 |
| Discrimination, % | ||||
| Never | 55.6 (51.8,59.3) | 47.3 (44.9,49.6) | 45.6 (41.8,49.5) | <0.001 |
| Sometimes | 36.0 (32.1,39.9) | 41.4 (39.2,43.5) | 44.1 (40.1,48.2) | 0.0114 |
| Often/always | 8.4 (6.6,10.2) | 11.4 (9.7,13.0) | 10.3 (7.7,12.8) | 0.0594 |
Abbreviations: CV, cardiovascular; AHEI, Alternative Healthy Eating Index
Among women, age-adjusted low CV risk prevalence was highest among those living in the US < 10 years (Table 3; 15.4%) and similar among those living in the US ≥ 10 years (9.4%) and those born in the US (9.2%). Foreign-born women who had lived in the US < 10 years were 2.00 (95% confidence interval (CI): 1.39, 2.86) times more likely to be low CV risk than US-born women in models adjusted for age, Hispanic/Latino background, education and insurance status; this association persisted in fully adjusted models. Foreign-born women who had lived in the US < 10 years also experienced significantly higher odds of being low CV risk than their foreign-born counterparts who had lived in the US ≥ 10 years (P for contrast statement < 0.01 in all models). There was no significant difference in low CV risk between foreign-born women living in the US ≥ 10 years and US-born women (Model 1 OR: 1.03; 95% CI: 0.73, 1.47). Associations between length of residence in the US and low CV risk did not vary significantly by Hispanic/Latino background (P for interaction = 0.75, 12 df).
Table 3.
Age-adjusted prevalence and multivariable-adjusted odds ratios for association of low risk (95% confidence interval) with nativity and length of residence in US: HCHS/SOL, 2008–2011
| Age-adjusted prevalence |
Model 1a | Model 2b | Model 3c | |
|---|---|---|---|---|
| Women | ||||
| US born (Ref) | 9.2(6.6,11.7) | 1.00 | 1.00 | 1.00 |
| Foreign born < 10 years | 15.4(12.9,17.9) | 2.01(1.40,2.89) | 1.97(1.38,2.83) | 1.97(1.37,2.82) |
| Foreign born >= 10 years | 9.4(8.0,10.7) | 1.02(0.72,1.47) | 1.01(0.70,1.44) | 0.99(0.69,1.42) |
| P for trend | <0.001 | <0.001 | <0.001 | |
| Men | ||||
| US born (Ref) | 6.0(4.0,8.1) | 1.00 | 1.00 | 1.00 |
| Foreign born < 10 years | 4.5(3.0,6.0) | 1.11(0.69,1.78) | 1.08(0.68,1.72) | 1.08(0.68,1.72) |
| Foreign born >= 10 years | 5.6(4.4,6.8) | 1.46(0.96,2.23) | 1.43(0.95,2.17) | 1.45(0.96,2.19) |
| P for trend | 0.71 | 0.72 | 0.78 | |
Adjusted for age, site, Hispanic/Latino background, education, and insurance status.
Adjusted for age, site, Hispanic/Latino background, education, insurance status, diet, and physical activity.
Adjusted for age, site, Hispanic/Latino background, education, insurance status, diet, physical activity, and discrimination.
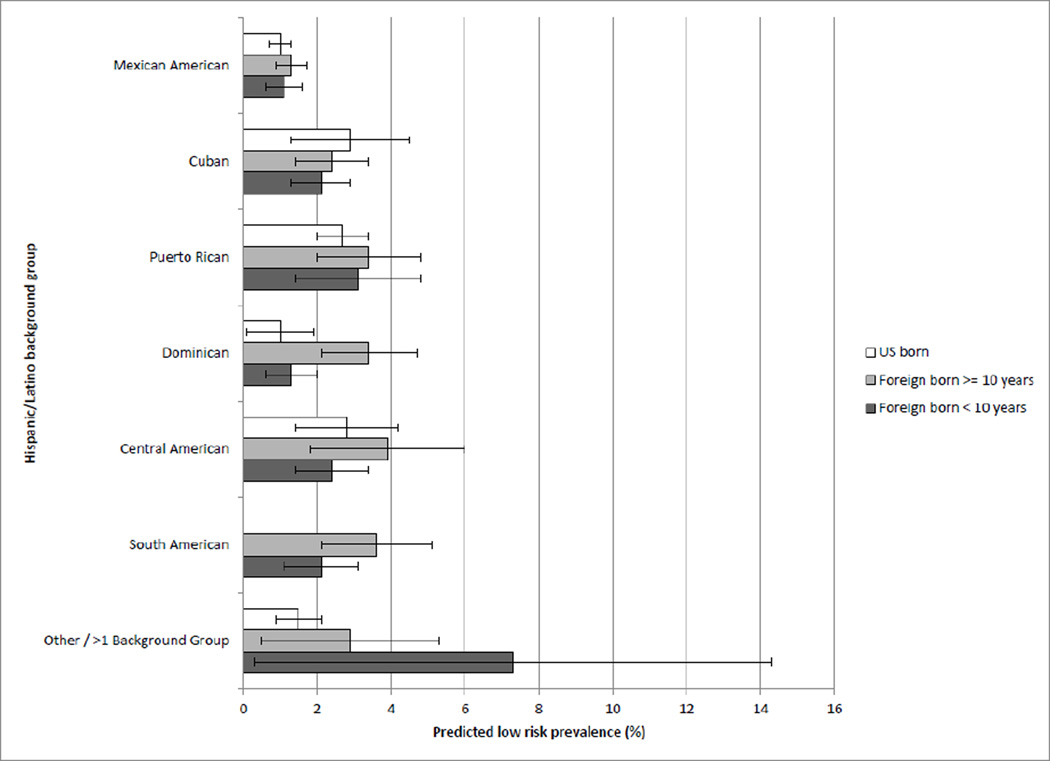
Age-adjusted low CV risk prevalence was similar by nativity and length of residence in the US among men, ranging from 4.5% in men who had lived in the US < 10 years to 6.0% in US-born men. Length of residence was not associated with low CV risk overall in multivariable-adjusted models. However, this association varied significantly by Hispanic/Latino background group in sociodemographic-adjusted models (P for interaction < 0.0001, 12 df). Figure 1 shows predicted low CV risk prevalence estimates by length of residence in the US for each Hispanic/Latino background among men. There was no strong patterning in low CV risk prevalence by length of residence among most Hispanic/Latino groups. In Dominican men, those who had lived in the US ≥ 10 years were significantly more likely to be low CV risk than those who had lived in the US < 10 years.
Figure 1.
Predicted low risk prevalence among men by length of residence in the US and Hispanic/Latino background: HCHS/SOL, 2008–2011. Estimated low risk prevalence based on a model adjusted for age, length of residence in the US, Hispanic/Latino background, length of residence in the US*Hispanic/Latino background interaction, education, and insurance status.
DISCUSSION
This is the first study to our knowledge to examine associations of length of residence in the US with low CV risk in different Hispanic/Latino groups. We found that Hispanic/Latino women who had lived in the US < 10 years were significantly more likely to be low CV risk than those born in the US after adjusting for sociodemographic characteristics, diet, physical activity, and ethnic discrimination. Among men, there was no association between length of residence and low CV risk in any group except among Dominicans, where low CV risk prevalence was highest for those who had lived in the US ≥ 10 years.
Few studies have examined gender differences in the relationship between length of residence and cardiovascular health. A nationally representative study of Mexican Americans found that foreign-born Mexican American men and women living in the US <10 years were more likely to be low CV risk than US-born Mexican American both men and women (i.e., no significant effect modification by gender).9 This is consistent with what we found among women, but it is in contrast with our null findings for men. Reasons for this difference in findings are not clear, suggesting further work is needed to better understand how gender may influence associations of length of residence in the US with cardiovascular health.
Low CV risk was significantly higher for Hispanic/Latino women who had spent less than 10 years in the US compared not only to US-born women, but also to women who had living in the US for 10 years or more. This is consistent with previous studies that have indicated that immigrants enter the US in relatively good health and over time lose this advantage and converge with health status levels of US-born residents.9, 10, 24 This may be due to increased exposure to different cultural and environmental factors that lead to poorer dietary practices, physical inactivity, and weight gain over time. In addition, the process of acculturation may increase exposure to certain stressors such as inter-personal or institutional discrimination that could have deleterious effects on health. Our findings persisted with adjustment for dietary quality, physical activity, and perceived ethnic discrimination, possibly due to the cross-sectional design of our study or our inability to capture the most salient aspects of these factors that contribute to differences in low CV risk with the available measures.
This study has some limitations. The cross-sectional design does not allow examination of changes in behaviors or other exposures over time, including those related to the process of acculturation. Furthermore, while we adjusted for several factors hypothesized to account for associations of acculturation with low CV risk, the available diet, physical activity, and discrimination measures may not have adequately captured specific aspects of these health behaviors that could be driving differences in low CV risk by length of residence (e.g., food preparation methods).
In summary, we found that longer duration of residence in the US was related to poorer CV health in women of all Hispanic/Latino backgrounds and that this relationship varied Hispanic/Latino background in men. A better understanding of the social, behavioral, and contextual factors that account for these differences will help guide efforts to improve cardiovascular health of Hispanics/Latinos residing in the US.
Highlights.
In women, recent immigrants had more favorable cardiovascular (CV) health profiles.
This relationship in women did not vary by Hispanic/Latino background group.
Nativity and length of residence in the US was not related to CV health in men.
There was some evidence among men of heterogeneity by background group.
Acknowledgments
The authors thank the staff and participants of HCHS/SOL for their important contributions. A complete list of staff and investigators has been provided by Sorlie P., et al. in Ann Epidemiol. 2010 Aug;20: 642–649 and is also available on the study website http://www.cscc.unc.edu/hchs/ The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST: None
REFERENCES
- 1.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 3.American Heart Association. Primer in Preventive Cardiology. Dallas, TX: American Heart Association; 1994. [Google Scholar]
- 4.Daviglus ML, Liu K, Greenland P, Dyer AR, Garside DB, Manheim L, Lowe LP, Rodin M, Lubitz J, Stamler J. Benefit of a favorable cardiovascular risk-factor profile in middle age with respect to Medicare costs. N Engl J Med. 1998;339:1122–1129. doi: 10.1056/NEJM199810153391606. [DOI] [PubMed] [Google Scholar]
- 5.Daviglus ML, Stamler J, Pirzada A, Yan LL, Garside DB, Liu K, Wang R, Dyer AR, Lloyd-Jones DM, Greenland P. Favorable cardiovascular risk profile in young women and long-term risk of cardiovascular and all-cause mortality. JAMA. 2004;292:1588–1592. doi: 10.1001/jama.292.13.1588. [DOI] [PubMed] [Google Scholar]
- 6.Giampaoli S, Palmieri L, Panico S, Vanuzzo D, Ferrario M, Chiodini P, Pilotto L, Donfrancesco C, Cesana G, Sega R, Stamler J. Favorable cardiovascular risk profile (low risk) and 10-year stroke incidence in women and men: findings from 12 Italian population samples. Am J Epidemiol. 2006;163:893–902. doi: 10.1093/aje/kwj110. [DOI] [PubMed] [Google Scholar]
- 7.Palmieri L, Donfrancesco C, Giampaoli S, Trojani M, Panico S, Vanuzzo D, Pilotto L, Cesana G, Ferrario M, Chiodini P, Sega R, Stamler J. Favorable cardiovascular risk profile and 10-year coronary heart disease incidence in women and men: results from the Progetto CUORE. Eur J Cardiovasc Prev Rehabil. 2006;13:562–570. doi: 10.1097/01.hjr.0000221866.27039.4b. [DOI] [PubMed] [Google Scholar]
- 8.Ford ES, Li C, Zhao G, Pearson WS, Capewell S. Trends in the prevalence of low risk factor burden for cardiovascular disease among United States adults. Circulation. 2009;120:1181–1188. doi: 10.1161/CIRCULATIONAHA.108.835728. [DOI] [PubMed] [Google Scholar]
- 9.Kershaw KN, Greenlund KJ, Stamler J, Shay CM, Daviglus ML. Understanding ethnic and nativity-related differences in low cardiovascular risk status among Mexican-Americans and non-Hispanic Whites. Preventive medicine. 2012;55:597–602. doi: 10.1016/j.ypmed.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Antecol H, Bedard K. Unhealthy assimilation: why do immigrants converge to American health status levels? Demography. 2006;43:337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- 11.Kandula NR, Diez-Roux AV, Chan C, Daviglus ML, Jackson SA, Ni H, Schreiner PJ. Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA) Diabetes Care. 2008;31:1621–1628. doi: 10.2337/dc07-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schargrodsky H, Hernandez-Hernandez R, Champagne BM, Silva H, Vinueza R, Silva Aycaguer LC, Touboul PJ, Boissonnet CP, Escobedo J, Pellegrini F, Macchia A, Wilson E, Investigators CS. CARMELA: assessment of cardiovascular risk in seven Latin American cities. The American journal of medicine. 2008;121:58–65. doi: 10.1016/j.amjmed.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the United States. Journal of psychiatric research. 2010;44:1043–1051. doi: 10.1016/j.jpsychires.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wassertheil-Smoller S, Arredondo EM, Cai J, Castaneda SF, Choca JP, Gallo LC, Jung M, LaVange LM, Lee-Rey ET, Mosley T, Jr, Penedo FJ, Santistaban DA, Zee PC. Depression, anxiety, antidepressant use, cardiovascular disease among Hispanic men and women of different national backgrounds: results from the Hispanic Community Health Study/Study of Latinos. Annals of epidemiology. 2014;24:822–830. doi: 10.1016/j.annepidem.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, Lavange L, Chambless LE, Heiss G. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Annals of epidemiology. 2010;20:629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lavange LM, Kalsbeek WD, Sorlie PD, Aviles-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, Criqui MH, Elder JP. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Annals of epidemiology. 2010;20:642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fang N, Jiang M, Fan Y. Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: A meta-analysis. International journal of cardiology. 2016;214:279–283. doi: 10.1016/j.ijcard.2016.03.210. [DOI] [PubMed] [Google Scholar]
- 18.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 19.Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd-Jones DM. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prineas RJ, Crow RS, Zhang ZM. The Minnesota Code Manual of Electrocardiographic Findings (Including Measurement and Comparison with the Novacode): Standards and Procedures for Measurement in Epidemiologic and Clincial Trials. London: Springer; 2010. [Google Scholar]
- 21.U.S. Department of Health and Human Services. 2008 Physical activity guidelines for Americans [Google Scholar]
- 22.Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. The Journal of nutrition. 2012;142:1009–1018. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith SM, Subar AF, Dodd KW. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Statistics in medicine. 2010;29:2857–2868. doi: 10.1002/sim.4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peek MK, Cutchin MP, Salinas JJ, Sheffield KM, Eschbach K, Stowe RP, Goodwin JS. Allostatic load among non-Hispanic Whites, non-Hispanic Blacks, and people of Mexican origin: effects of ethnicity, nativity, and acculturation. Am J Public Health. 2010;100:940–946. doi: 10.2105/AJPH.2007.129312. [DOI] [PMC free article] [PubMed] [Google Scholar]