Abstract
Simulation is an effective teaching tool to decrease the learning curve for novices without compromising patient safety. Simulation helps interventionalist in mentally translating a two dimentional, black and white image into a usable three dimentional model. It also bridges the gap in training diverse team members on new procedures and products. All simulators have collision detection, i.e., virtual contact forces generated from collision which updates haptic output with new calculations.
Keywords: Catheterization laboratory, Clinical and technical skills, Simulation
INTRODUCTION
With growing trend toward minimally invasive surgeries, percutaneous endovascular interventional procedures are now preferred alternatives to traditional cardiac surgical procedures. Technological improvement is at the expense of increasing complexity of procedures, with steep learning curves necessitating simultaneous improvements in clinical skills in realistic situations with due regard to patient safety. With increasing public awareness regarding medical errors and patient safety, it is need of the hour to develop new methods for training in medical education. The solution lies in the use of virtual reality simulation. The concept of use of simulation to improve skills and validation of competency is not an alien one. Cadavers and animal models have been used for this purpose since times immemorial. With the advent of high fidelity virtual reality simulators, questions have been raised regarding the currently prevalent traditional certification standards and apprenticeship model. The simulation was first used for laparoscopic surgeries in 1993. Since then, various surgical specialties have adopted this virtual technology for enhancing their surgical skills. The use of simulation in cardiac catheterization laboratory was studied by Bagai et al.[1] who concluded that cardiac catheterization skills can be learned via mentored simulation training and are applicable for actual procedures in the catheterization laboratory. Technical performance was improved in cardiology trainees using simulators before performing on real patients. It was also found that less proficient operators benefit more from simulator training compared to more proficient ones.
Simulation is an effective teaching tool to decrease the learning curve for novices without compromising patient safety. Hands-on training using simulators is most effective in enhancing the motor skills and cognitive abilities in the interventional setting for both the physicians as well as the paramedical staff. Trainees can learn and practice proper sequence of catheterization steps.[2] Use of simulation enhances visual and spatial thinking and improves hands-eye coordination. Simulation helps interventionalist in mentally translating a two-dimensional, black and white image into a usable three-dimensional model. It also bridges the gap in training diverse team members on new procedures and products. It makes them better prepared in case complications do occur. Further, feedback in simulation greatly improves performance. Mahmood et al.[3] found that performance did not improve in the absence of feedback on a colonoscopy simulator. Boyle et al.[4] concluded that incorporation of feedback in simulated laparoscopic colectomy training resulted in fewer errors and better learning curves.
BASIC PRINCIPLES OF SIMULATORS
Haptic technology
In simple words, it the technology of adding touch and feeling to computers, i.e., when virtual objects are touched they seem real and tangible. It generates sensory or tactile information using an electromechanical system according to user-guided inputs. Forces applied during manipulation by the trainees on the cannulating device develops a force feedback considered essential for image-assisted navigation and development of tactile dexterity. Both contact and frictional forces can be generated similar to the catheter-initima collisions allowing trainees to have a real like experience. Two types of force feedback are generated, i.e. active (power driven cylinders which generate high torques) and passive (removes energy by damping the motion of objects). Both active and passive feedbacks are incorporated in most modern simulators even though active haptics are usually dormant during patient-specific rehearsals [Figure 1].
Figure 1.
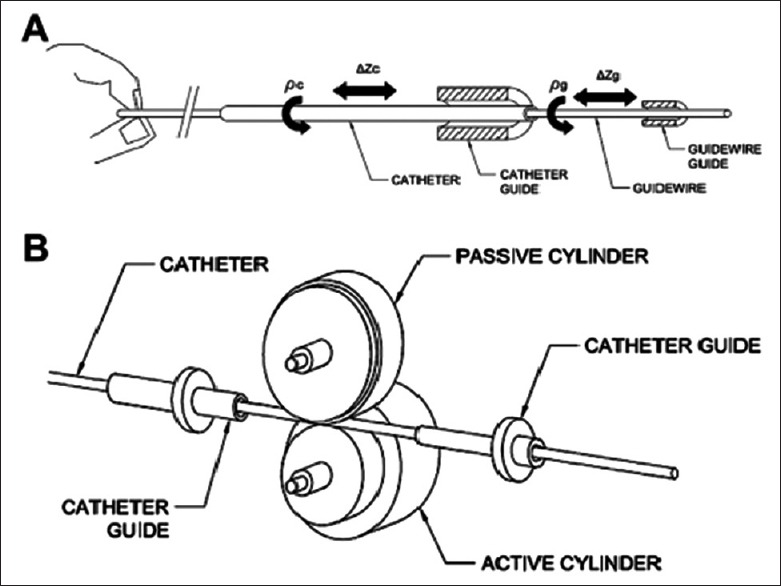
Concept of device simulator interaction, allowing trainees to have a real like experience
All simulators have collision detection, i.e., virtual contact forces generated from collision which updates haptic output with new calculations.
Typical guidewire and catheter guide assembly in the endovascular haptic device. Independent guides for each device in a single haptic module permit independent manipulation of each device without influencing the other
Haptic-catheter interface.
Vessel segmentation
The vascular lumen data from all tissues is collected via computed tomography (CT)/magnetic resonance (MR) angiography and can be used to create a specific three-dimensional model for relevant vascular structures. These can be customized for specific patients using manual, semi or fully automatic segmentation techniques.
Physiologic feedback
The response generated to pharmacologic or mechanical intervention. These can be displayed, modified, and also recorded as the postoperative report. The responses can be qualitative or quantitative. Quantitative parameters include measurement of vitals such as oxygen saturation, cuff blood pressures, intracardiac pressures via transseptal needles, invasive blood pressures via catheters, heart rate, waveforms for electrocardiogram (ECG) leads and respiratory rate. Apart from these, total procedure time, the amount of contrast used, the number of cine loops, total fluoroscopy, number of roadmaps, interventional maneuvers, devices used, drugs administered, procedural events, imaging actions, and corresponding times for each event can be recorded. Qualitative parameters include changes in vital signs in response to drugs or during catheter insertion, resistances encountered during guiding catheter against vessel wall, beyond the site of lesion or ahead of guidewires, etc.
Drugs which can be used include anticoagulants, antiplatelets, inotropes, antiarrhythmics, beta-blockers, vasodilators, vasopressors, antihypertensives, and procoagulants.
Performance feedback
This is provided by every manufacturer. It can be measured both during and after the procedure. It is essential for training, rehearsals, training, and validation of skills.
Currently, four endovascular simulator manufacturers provide seven models which are commercially available in North America. These are:
Procedicus VIST Lab and VIST-C (Mentice, Gothenburg, Sweden)
SimSuite Simantha (Medical Simulation Corporation, Denver, CO, USA)
ANGIO Mentor Slim, Dual Slim and Ultimate (Simbionix, Cleveland, OH, USA)
CathLab VR (CAE Healthcare, Montreal, Quebec, Canada).
Table 1 shows the comparison between various commercially available simulators.
Table 1.
Comparison of currently available simulators
| Dimentions (cm) | Weight | Portability | Haptic model | Haptic units | Active/passive haptics | DOF/DFF | Collision detection | Fluid dyanamics | PAC compatibility | Patient specific capability | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| VIST Lab | 257×81×196 | - | On casters, portable within building | Xitach CHP | 6 | - | 2 | Yes | - | - | Yes |
| VIST C | 117×41×15 | 13.15 kg for device, 5 kg for laptop and monitor | Can be checked in on airplane | Xitach CHP | 3 | - | 2 | Yes | - | - | Yes |
| Simantha | 183×183×76 | 222.25 kg for system | On casters, portable within building | Proprietary | 6 | Both | - | Yes | Yes | No | No |
| ANGIO Mentor Slim | 104×10×13 | 4 kg for device, 4 kg for laptop, and 3.2 kg for monitor | Can be checked in on airplane | Xitach CHP | 3 | Both | 2 | Yes | Yes | Yes | Yes |
| ANGIO Mentor Dual Slim | 104×10×13 | 8.2 kg for 2 devices, 4 kg for laptop, 3.2 kg for monitor | Can be checked in on airplane | Xitach CHP | 6 | Both | 2 | Yes | Yes | Yes | Yes |
| ANGIO Mentor Ultimate | 127×61×168 | 150 kg for system | On casters, portable within building | Xitach CHP | 6 | Both | 2 | Yes | Yes | Yes | Yes |
| CathLab VR | - | - | - | Proprietary | - | - | - | - | - | - | - |
DOF: Degrees of freedom, DFF: Degrees of force feedback, PACs: Picture archiving and communication system
Currently, commercially available endovasculator simulators allow for a variety of angiographic procedures such as insertion and manipulation of guidewires, catheters, and balloons. They allow for manipulation of fluoroscopic images using C-arm as well as quantitative assessments of the amount of contrast used and total fluoroscopic time. These systems also allow for hemodynamic monitoring and management and assessing pharmacological responses to various medications. In addition, the response time in case of an adverse event can also be calculated for assessment and monitoring progress. The common procedures which can be performed on the various simulators are listed in Table 2.
Table 2.
Commonly performed procedures available in the simulators
| LHC | RHC | PCI | IABP | TAVI | Trans septal ASD | PABV | PMBV | TEVAR | EVAR | TEE | ICE | IVUS | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CAE | + | − | + | + | + | − | − | − | − | − | + | − | − |
| MSC | + | + | + | + | + | + | + | − | − | − | + | + | + |
| Mentice | + | − | + | + | + | + | + | + | + | + | + | + | − |
| Symbionix | + | − | + | + | + | + | + | + | + | + | + | − |
MSC: Medical simulation company, PCI: Percutaneous coronary intervention, LHC/RHC: Left heart and right heart catherization, TAVI: Transcathetor aortic valve implantation, PABV: Percutaneous aortic ballon valvuloplasty, PMBV: Percutaneous mitral balloon valvuloplasty, TEVAR: Thoracic endovascular aneurysm repair, EVAR: Endovascular aneurysm repair, ICE: Intracardiac echocardiography, IVUS: Intravascular ultrasound, TEE: Transesophageal echocardiography, ASD: Atrial septal defect
CAE has developed a simulator – CathLab VR™
The cases are grouped into basic and advanced ones on the basis of difficulty levels. These range from simple to complex percutaneous coronary intervention, ostial lesions, use of embolic protection devices, cardiac rhythm management, failed bioprosthetic valve management, transcutaneous aortic valve simulation, etc., [Figure 2]. It also provides a separate fully functional transthoracic and transesophageal echo simulator for use in conjunction with cardiac catheterization simulator.
Figure 2.

The Cath VR use for embolic protection devices, cardiac rhythm management, failed bioprosthetic valve management, transcutaneous aortic valve simulation
Medical Simulation Corporation (MSC) provides a simulator called Simantha™. It simulates the procedure along with multimodality imaging including live fluoroscopy, static images, ECG, live intravascular ultrasound (IVUS), and static transesophageal echocardiography (TEE). The IVUS and TEE are incorporated in the case presentations. More than 20 drugs can be administered with simultaneous recording of effects on various physiological parameters such as heart rate, respiratory rate, oxygen saturation, cuff blood pressure, level of consciousness, etc. The procedure is carried out in the form of teaching points by rules engine which also allows for a variety of treatment options. The data are recorded during simulation procedures and can be used to create metrics for marketing and training purposes. MSC in association with ABIM has developed specific interventional cardiology cases accredited in ABIM's MOC (Philadelphia, PA 19106-3699) self-assessment program. These include acute myocardial infarction course, basic program, carotid course, diagnostic coronary angiography course, door-to-balloon time simulation workshop, etc.
Mentice has developed simulator VIST™ which allows for all types of coronary, neurovascular, peripheral, and structural cases. Fifteen drugs can be used for injection including morphine, heparin, and nitroglycerin. Accordingly, it provides feedback of the real time changes in aortic pressures measured by catheter, any three lead ECG, blood pressure, respiratory rate, heart rate, and oxygen saturation. It allows for both quantitative (total procedure time, the amount of contrast, cine loops, and fluoroscopy time) and qualitative (guiding catheter against the vessel wall, beyond the site of lesion or ahead of guidewires, etc.) monitoring of errors and clinical parameters [Figure 3a–c].
Figure 3.

(a-c) Mentice has developed simulator VIST™ which allows for all types of coronary, neurovascular, peripheral and structural cases. Fifteen drugs can be used for injection including morphine, heparin and nitroglycerine
VIST™ has single and dual access sites along with radial access. Trainees are free to navigate the vessels and intervene irrespective of the case. Table 3 compares the characteristics of various simulator options provided by Mentice.
Table 3.
Comparison of various simulators offered by mentice
| Radiation safety trainer | VIST C | VIST G5 | VIST Lab with VIST G5 | |
|---|---|---|---|---|
| Use | Full CathLab staff training of radiation safety | All types of endovascular training | All types of endovascular training | All types of endovascular training |
| Software modules available for purchase | 3 | 18 modules with over 400 cases | 18 modules with over 400 cases | 18 modules with over 400 cases |
| Portability | √ | √ | √ | √ |
| Force feedback technology | √ | √ | √ | |
| Customisation of cases | √ | √ | √ | |
| Devices used | Up to 6F - only catheter and wire | 0.014” to 24F (up to 6F on the second tracker) | 0.014” to 24F (up to 8F on the second tracker) | 0.014” to 24F (up to 8F on the second tracker) |
| Dual leg compatiblity | √ | √ | √ | |
| VIST control box included | √ | √ | √ | |
| Fullsize mannequin and 50” monitor | √ | |||
| Support for multiple access points | √ |
The various modules available are:
Acute stroke intervention
Aortic valve implantation
Below-the-knee intervention
Cardiac rhythm management
Carotid intervention
Coronary angiography
Coronary Pro Procedural Training Module
Endovascular aortic repair
Iliac/superficial femoral artery intervention
Left atrial appendage occlusion
Neuro-intervention
Peripheral angiography
Renal denervation
Renal intervention
Thoracic endovascular aortic repair
Transseptal puncture
Uterine artery embolization
Vascular trauma management.
Simbionix provides three simulation platforms. These are ANGIO Mentor Slim, ANGIO Mentor Dual Slim and ANGIO Mentor Ultimate. Although vessel segmentation is semiautomatic, it can be easily accomplished by trained hands even on the day of surgery. More than 100 physiological parameters can be recorded during the procedure and used for tracking the progress. All of them provides simulation for thoracic endovascular aneurysm repair (EVAR) and EVAR [Figure 4].[5,6] Various complications such as dissections, perforations, aortic puncture or leak, air embolization, vasospasm, etc., can be generated amidst a procedure. For endovascular cases, complications such as difficulty in introducing graft components over an introducer or stiff wire, selection of the correct size of main graft, correct position, the occurrence of endoleak and occlusion of ostia of hypogastric, renal or superior mesenteric arteries can be reproduced.[7] One distinguishing feature is the procedural rehearsal studio, i.e., feeding patient data in simulation cases so that practice can be done on patients actual anatomy. It is available for carotid angiography and intervention as well as endovascular treatment of abdominal aortic aneurysms.
Figure 4.

A part of the Simbionix the Angio Ultimate, has more than 100 physiological parameters that can be recorded during a procedure like thoracic endovascular aneurysm repair and endovascular aneurysm repair
Endovascular evaluator (EVE) is a model reconstructing human vascular lumen using CT/MR imaging data. It is composed of 16 modules which can be customized according to the requirements. It is light weight (dry weight 3.8 kg) enabling easy transportation. These are made of silicone having elasticity coefficient similar to arteries (2 MPa). The friction coefficient of the arteries is 0.038 and that of the simulator is 0.042 which can also be adjusted by the user by altering the concentration of circulating surfactant. It thus simulates the elasticity and friction of the human vasculature and allows real time experience of catheter manipulation. These are also X-ray compatible further enhancing the simulation quality [Figure 5]. The procedures supported by EVE include cerebral artery embolism with coil or balloon, carotid artery stenting, percutaneous transluminal coronary angioplasty, aortic stent grafts, catheter and guidewire insertion, (percutaneous transluminal recanalization, transcatheter hepatic artery embolization, and percutaneous transluminal angioplasty with balloon or stents [Figure 6].
Figure 5.
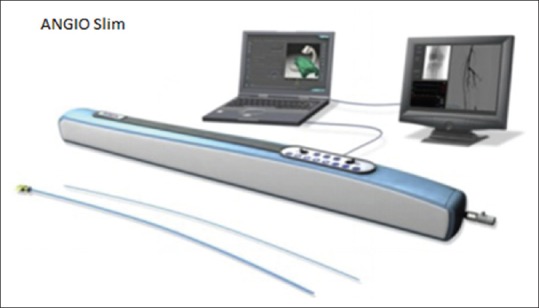
The Angio Slim as an endovascular evaluator is compatible with X-rays and thus enhances the simulation quality
Figure 6.
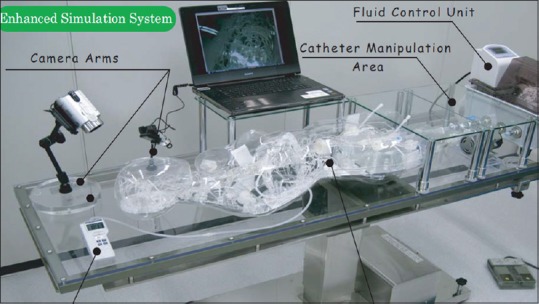
The enhanced simulation system
Simulation can thus be considered as an effective tool for training, education, certification, and acquisition of new technological skills for both novices and experts in medical and paramedical fields. It is even more important for cardiac catheterization laboratory which is a dynamic module requiring trained interventional nurses and technicians in addition to physician's skills and experience for the successful patient outcome. The Food and Drug Administration also advocates the use of virtual reality simulators for approving new devices. Considering that the main aim of improvements in medical technology has been to improve patient comfort and safety, simulation can play a key role in fulfilling this goal.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bagai A, O’Brien S, Al Lawati H, Goyal P, Ball W, Grantcharov T, et al. Mentored simulation training improves procedural skills in cardiac catheterization: A randomized, controlled pilot study. Circ Cardiovasc Interv. 2012;5:672–9. doi: 10.1161/CIRCINTERVENTIONS.112.970772. [DOI] [PubMed] [Google Scholar]
- 2.Green SM, Klein AJ, Pancholy S, Rao SV, Steinberg D, Lipner R, et al. The current state of medical simulation in interventional cardiology: A clinical document from the society for cardiovascular angiography and intervention's (SCAI) simulation committee. Catheter Cardiovasc Interv. 2014;83:37–46. doi: 10.1002/ccd.25048. [DOI] [PubMed] [Google Scholar]
- 3.Mahmood T, Darzi A. The learning curve for a colonoscopy simulator in the absence of any feedback: No feedback, no learning. Surg Endosc. 2004;18:1224–30. doi: 10.1007/s00464-003-9143-4. [DOI] [PubMed] [Google Scholar]
- 4.Boyle E, Al-Akash M, Gallagher AG, Traynor O, Hill AD, Neary PC. Optimising surgical training: Use of feedback to reduce errors during a simulated surgical procedure. Postgrad Med J. 2011;87:524–8. doi: 10.1136/pgmj.2010.109363. [DOI] [PubMed] [Google Scholar]
- 5.Tedesco MM, Pak JJ, Harris EJ, Jr, Krummel TM, Dalman RL, Lee JT. Simulation-based endovascular skills assessment: The future of credentialing? J Vasc Surg. 2008;47:1008–14. doi: 10.1016/j.jvs.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Dawson DL, Meyer J, Lee ES, Pevec WC. Training with simulation improves residents’ endovascular procedure skills. J Vasc Surg. 2007;45:149–54. doi: 10.1016/j.jvs.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Eslahpazir BA, Goldstone J, Allemang MT, Wang JC, Kashyap VS. Principal considerations for the contemporary high-fidelity endovascular simulator design used in training and evaluation. J Vasc Surg. 2014;59:1154–62. doi: 10.1016/j.jvs.2013.11.074. [DOI] [PubMed] [Google Scholar]


