Abstract
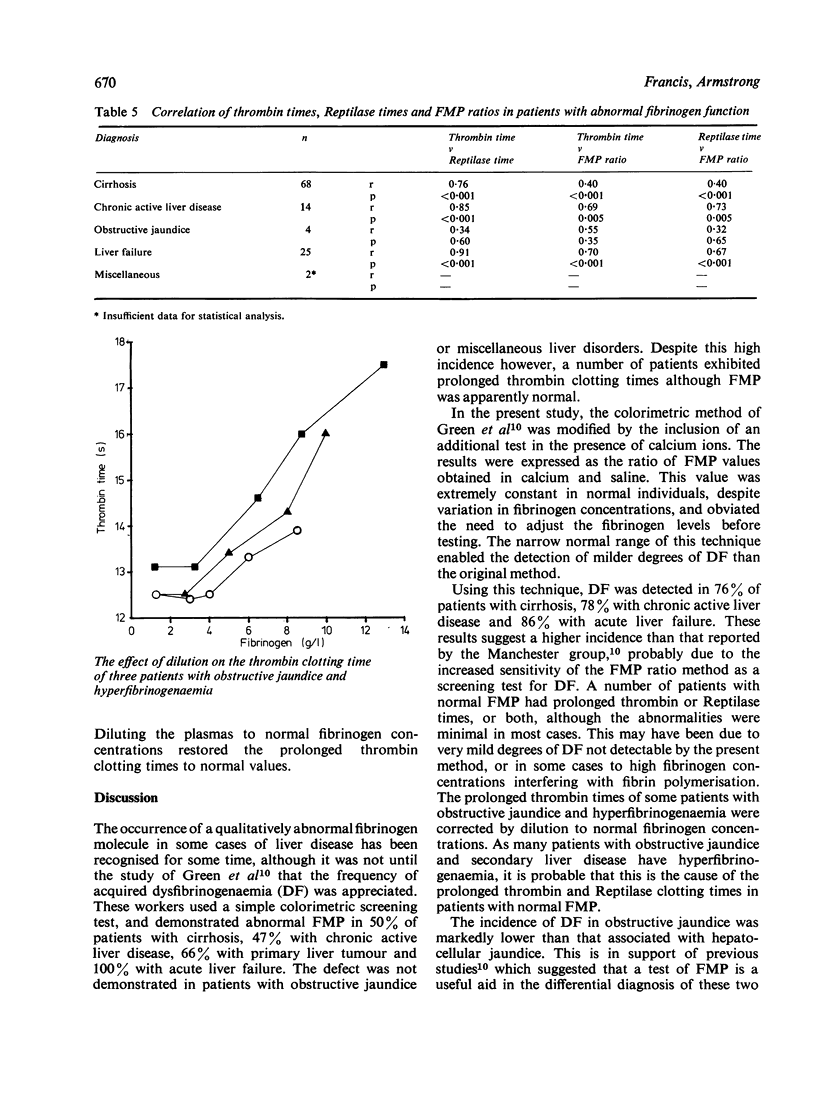
Using a new and sensitive screening method, dysfibrinogenaemia (DF) was detected in 76% of patients with cirrhosis, 78% with chronic active liver disease and 86% with acute liver failure. The incidence was much lower in obstructive jaundice (8%) and miscellaneous liver disorders (4%). It is concluded that the fibrin monomer polymerisation (FMP) ratio test is a simple and sensitive test for the detection of DF, and is useful in the differential diagnosis of hepatocellular and obstructive jaundice. Hyperfibrinogenaemia, particularly in patients with obstructive jaundice, may explain the high incidence of abnormal thrombin and Reptilase clotting times despite normal FMP ratios. Dysfibrinogenaemia dose not appear to be related to the degree of liver function impairment, but may be associated with regeneration of hepatic tissue.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aiach M., Rogé J., Busy M. F., Durand H., Guéroult N., Chanrion C., Leclerc M., Justin-Besançon L. Dysfibrinogénémies acquises et affections hépatiques. A propos de 30 observations. Sem Hop. 1973 Jan 14;49(3):183–197. [PubMed] [Google Scholar]
- Barr R. D., Allardyce M., Brunt P. W., McPhie J. L. Dysfibrinogenaemia and liver cell growth. J Clin Pathol. 1978 Jan;31(1):89–92. doi: 10.1136/jcp.31.1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr R. D. Fetal fibrinogen: fact or fancy? Biomedicine. 1978 Oct;28(5):245–248. [PubMed] [Google Scholar]
- Green G., Poller L., Thomson J. M., Dymock I. W. Association of abnormal fibrin polymerisation with severe liver disease. Gut. 1977 Nov;18(11):909–912. doi: 10.1136/gut.18.11.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane D. A., Scully M. F., Kakkar V. V. Prolonged thrombin clotting times in liver disease. Thromb Res. 1977 May;10(5):773–774. doi: 10.1016/0049-3848(77)90061-5. [DOI] [PubMed] [Google Scholar]
- Lane D. A., Scully M. F., Thomas D. P., Kakkar V. V., Woolf I. L., Williams R. Acquired dysfibrinogenaemia in acute and chronic liver disease. Br J Haematol. 1977 Feb;35(2):301–308. doi: 10.1111/j.1365-2141.1977.tb00586.x. [DOI] [PubMed] [Google Scholar]
- Lipinski B., Lipinska I., Nowak A., Gurewich V. Abnormal fibrinogen heterogeneity and fibrinolytic activity in advanced liver disease. J Lab Clin Med. 1977 Jul;90(1):187–194. [PubMed] [Google Scholar]
- POPPER H. Liver disease-morphologic considerations. Am J Med. 1954 Jan;16(1):98–117. doi: 10.1016/0002-9343(54)90326-5. [DOI] [PubMed] [Google Scholar]
- Palascak J. E., Martinez J. Dysfibrinogenemia associated with liver disease. J Clin Invest. 1977 Jul;60(1):89–95. doi: 10.1172/JCI108773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini-Cessi F. Sialyltransferase activity in regenerating rat liver. Biochem J. 1977 Sep 15;166(3):381–386. doi: 10.1042/bj1660381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhaeghe R., van Damme B., Molla A., Vermylen J. Dysfibrinogenaemia associated with primary hepatoma. Scand J Haematol. 1972;9(5):451–458. doi: 10.1111/j.1600-0609.1972.tb00968.x. [DOI] [PubMed] [Google Scholar]
- von Felten A., Straub P. W., Frick P. G. Dysfibrinogenemia in a patient with primary hepatoma. First observation of an acquired abnormality of fibrin monomer aggregation. N Engl J Med. 1969 Feb 20;280(8):405–409. doi: 10.1056/NEJM196902202800802. [DOI] [PubMed] [Google Scholar]


