Abstract
Objectives:
We aimed to evaluate the effect of geographic units of analysis on measuring geographic variation in medical services utilization. For this purpose, we compared geographic variations in the rates of eight major procedures in administrative units (districts) and new areal units organized based on the actual health care use of the population in Korea.
Methods:
To compare geographic variation in geographic units of analysis, we calculated the age–sex standardized rates of eight major procedures (coronary artery bypass graft surgery, percutaneous transluminal coronary angioplasty, surgery after hip fracture, knee-replacement surgery, caesarean section, hysterectomy, computed tomography scan, and magnetic resonance imaging scan) from the National Health Insurance database in Korea for the 2013 period. Using the coefficient of variation, the extremal quotient, and the systematic component of variation, we measured geographic variation for these eight procedures in districts and new areal units.
Results:
Compared with districts, new areal units showed a reduction in geographic variation. Extremal quotients and inter-decile ratios for the eight procedures were lower in new areal units. While the coefficient of variation was lower for most procedures in new areal units, the pattern of change of the systematic component of variation between districts and new areal units differed among procedures.
Conclusions:
Geographic variation in medical service utilization could vary according to the geographic unit of analysis. To determine how geographic characteristics such as population size and number of geographic units affect geographic variation, further studies are needed.
Keywords: Small-area analysis, Delivery of health care, Utilization
INTRODUCTION
Geographic variation in medical services utilization refers to a phenomenon in which the health care use of a population varies according to the geographically defined unit. Since it was not explained only by patient characteristics, but rather by supplier characteristics, this phenomenon was termed ‘unwarranted variation’ [1] and has remained a major topic in the field of health services research for decades [2]. With rising health care costs and increased awareness of uncertainty in medicine, many research initiatives to investigate geographical variation are being implemented at national and multinational levels [3]. As geographic variation studies evolve from measurements of variation in one nation into international comparison, organizing new areal units which are more homogenous and which accurately reflect health care use has emerged as an important issue.
Geographic variation studies have been conducted with two kinds of geographic units of analysis: units organized for the purpose of variation analysis and administrative units. While newly organized units such as hospital service areas can reflect the actual health care use of the region, they, being ad hoc units, may be of limited use for policy. Administrative units, having merit in terms of policy making, health care planning, and provision [4], have been frequently used for geographic variation studies.
Administrative units, however, may be incomplete as a unit of analysis for the following two reasons. First, heterogeneity in population size and number of units can produce extravariation [4]. Second, administrative units are not necessarily consistent with actual health care use. As one of the main purposes of variation studies is to estimate the influence of the area’s health care supply on its use, each unit should be, ideally, self-sufficient in health care use for a variation study [5]. In this respect, variation analysis based on administrative units could lead to an erroneous attribution of health care use to health care suppliers. This is especially relevant in Korea because, as revealed in previous studies [6], the proportion of residents of an area using health care within their own unit of residence is known to be low compared with other countries.
In Korea, variation studies have been mainly performed on the basis of administrative units [7-14]. While there have been attempts to organize new areal units, they have mostly maintained the form of existing administrative units [15-20]. And, to the best of our knowledge, a comparison of variation and population structure between administrative units and new areal units has not been performed in Korea. This study aimed to evaluate the effect of geographic units on measuring geographical variation in health care use by comparing administrative units and new areal units organized to reflect geographic health care use accurately and to examine the relevance of each areal unit for measuring geographic variation.
METHODS
Data
The study data were extracted from the National Health Insurance (NHI) database in Korea for the 2013 period (January 1 to December 31). The NHI database comprises patients who are registered for the NHI—about 97% of the country’s population—and medical aid beneficiaries who comprise 3% of the total population [21]; thus it can be considered to be comprehensive for the whole Korean population, except in the case of some procedures which are not covered by the NHI. The database includes information on patient demographics, procedure codes (Electronic Database Interchange codes), and diagnosis codes (Korean Standard Classification of Diseases codes). Data for the population distribution of areal units were acquired from Statistics Korea.
We studied geographic variation in utilization rates for the following eight procedures: coronary artery bypass graft surgery (CABG), percutaneous transluminal coronary angioplasty (PTCA), surgery after hip fracture, knee-replacement surgery, hysterectomy, caesarean section, computed tomography scan (CT), and magnetic resonance imaging scan (MRI). These procedures were selected by the criteria of high cost, large volume, and policy relevance [22]. Procedure utilization rates were calculated based on the patient’s place of residence. The rates were age-adjusted and sex-adjusted to the Korean Resident Population 2013. The rate of caesarean section was standardized to the measurement of Korean Live Births 2013, according to the age of mother. The rates were calculated per 100 000 population aged 15 and over. For CABG and PTCA the rate was per 100 000 population aged 20 and over. In the case of caesarean section, the rate was per 1000 live births.
Unit of Analysis
The administrative units in Korea are divided into two categories: Provincial level (special metropolitan city, metropolitan city, special self-governing city, do, and special self-governing province) and municipal level (si, gun, and gu). While both of these two levels have been frequently used in previous studies, municipal level units have been applied mainly in two different ways; (i) si/gun [14,15,19]; (ii) si/gun/gu [12,13]. As si is a homogenous unit in terms of supply and accessibility of health care service [20], and has concentrated residence [19], we used si/gun (subsequently referred to as districts) as administrative units instead of si/gun/gu, where a si can be divided into the subunit gu.
New areal units were organized for the following three purposes: (i) To establish areal units that cover actual health care use. (ii) To understand the pattern of health care utilization based on health care supply. (iii) To prepare the ground for monitoring and ensuring health care supply.
New areal units were organized by merging and selecting. Merging was done on the 163 districts (si/gun). Merging was performed on the basis of the multiplication of a relevance index and a commitment index. The relevance index (RI) refers to the proportion of the hospitalizations that occurred within an area over the total number of hospitalizations done in that area. The commitment index (CI) refers to the proportion of the hospitalizations that occurred within an area over the total number of hospitalizations of the area’s residents. To reflect both the dependence of residents’ health care use on certain areas and the dependence of an area on the residents of certain areas, we utilized the multiplication of RI and CI. Data for hospitalization was from the NHI database (October 2012 to September 2013).
To select the combination of the merged areal units, we applied three criteria: (i) Minimum value of the RI of an areal unit: 40%. (ii) Minimum population size of an areal unit: 150 000. (iii) Maximum travel time: 60 minutes [23]. The minimum value of the RI and population size are based on the results from a previous study on organizing areal units for health care use [20], where the average value of the RI of the 163 districts (si/gun) was about 40%. To ensure that the minimum RI of new areal units attained the average RI of the existing units, we set the minimum value of the RI as 40%. On the basis of the analysis of the RI and the population size of the districts, we concluded that the population size should be at least over 150 000 to attain the minimum RI. Travel time refers to the time required for a car to move from one area to another area. Based on previous studies where 60 minutes was defined as a critical period for reducing mortality in emergency medical conditions [20, 23], we set the maximum travel time as 60 minutes. Travel time was calculated between center points of the populations of areal units.
Quantification of Variation
Statistics of variation based on age–sex standardized rates were calculated to assess the effect of the geographic units on geographic variation. The analysis was performed as follows. First, by comparing non-parametric kernel density estimates according to geographic units, we attempted to visually assess the effect of geographic units on the distribution of procedure rates. Kernel density estimation, a non-parametric way to estimate the probability density function, is widely used in data mining and econometrics for inference procedures [24]. Kernel density estimation was also used for comparing the rate distribution of geographic units [3]. This study used the Gaussian kernel function. Second, we calculated the ‘extremal quotient’ (EQ), the ‘inter-decile ratio’ (IDR), and the ‘coefficient of variation’ (CV) to assess the effect of geographic units on geographic variation in procedure rates. The EQ is the ratio of the highest geographic unit rate to the lowest geographic unit rate of a procedure. The EQ, intuitive and easy to understand [22], is appealing to researchers and policy makers [25] and therefore has often been used in geographic variation studies. However, as the EQ is very sensitive to extreme values, we calculated the IDR, the ratio of the rate in the area in the 90th to the 10th percentile of the distribution, to reduce the influence of outliers [22]. The CV is the ratio of the standard deviation to the mean of procedure rates in given geographic units. Since the CV is insensitive to the scale, it has been frequently used to study heterogeneity of different units [26]. And finally, we estimated the systematic component of variation (SCV). The SCV is the estimate of the true part of variation (variation across areas) separated from the random part of variation (within-region variation) [27]. We used the formula (Figure 1) proposed by McPherson et al. [28].
Figure. 1.
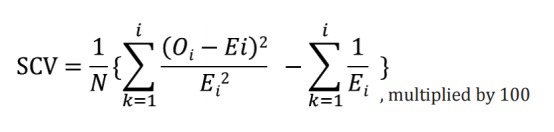
Formula for the systematic component of variation (SCV) [28]. N, number of areas; Oi, observed number of procedures; Ei , expected number of procedures.
International Comparison
To grasp the heterogeneity in the population sizes of geographic units in Korea, we compared the distribution of population size and variation statistics of new areal units and administrative units (districts) in Korea with those of the 13 Organization for Economic Cooperation and Development (OECD) member countries. For comparison of the distribution of population size, we collected data on the populations of the 18 corresponding areal units from the 13 countries and calculated the average and the CV of the population sizes.
To compare the variation statistics of Korea with the 13 OECD countries [22], we calculated variation statistics based on procedure rates computed in an identical way as in the OECD report. Rates were age-adjusted and sex-adjusted to the OECD 2010 standard population and the 2011 Italian population structure according to the mother’s age for the caesarean section rate.
The study was carried out with SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
The population distributions of the geographic units are as follows. The average population size was 313 751 in districts and 897 219 in new areal units. The CV of the population size was 2.87 in districts and 1.67 in new areal units. While 86 out of 163 districts had fewer than 99 999 inhabitants, no new areal unit had fewer than 99 999 inhabitants (Figure 2). The total number of procedures and the nationwide rate of procedures are presented in Supplemental Table 1. With regard to the effect on the distribution of procedure rates, kernel curves showed distinct differences in CABG and surgery after hip fracture, which showed less dispersion in new regional areas (Figure 3).
Figure. 2.
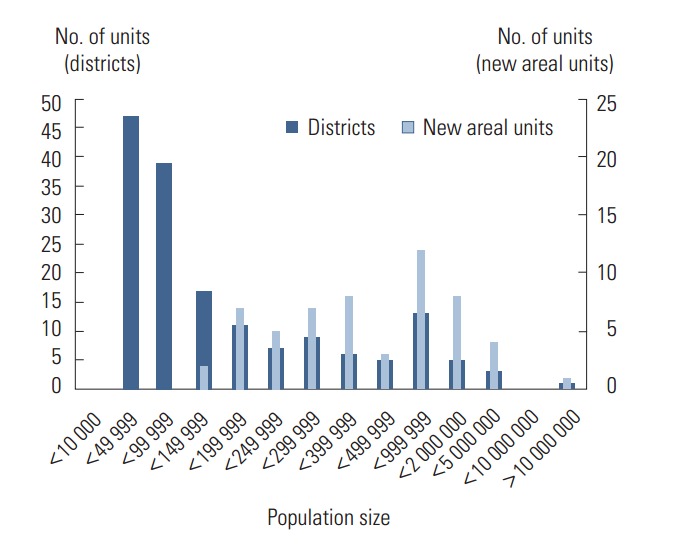
The distributions of the populations in the administrative units (districts) and new areal units.
Figure. 3.
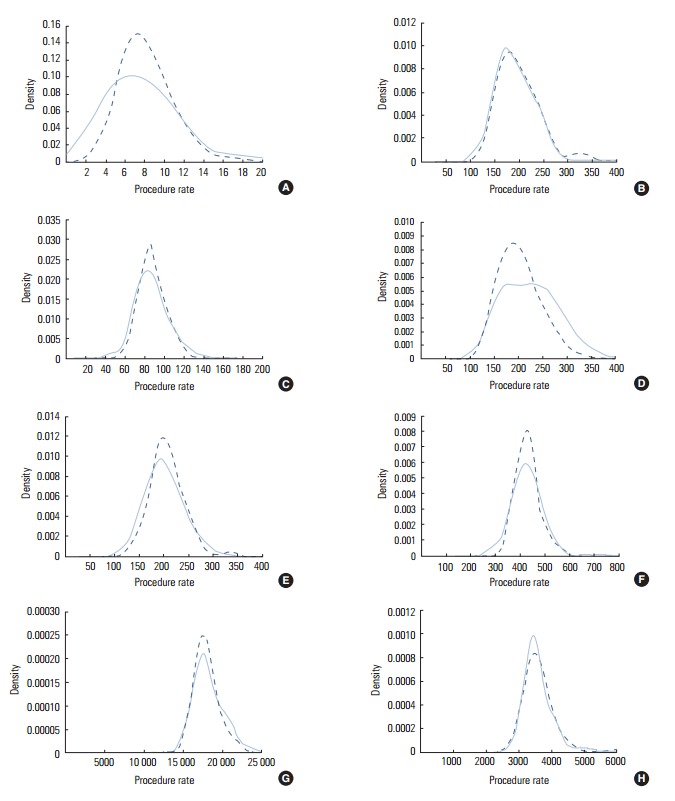
The kernel density function for age–sex standardized rates of the eight (A: coronary artery bypass graft surgery, B: percutaneous transluminal coronary angioplasty, C: surgery after hip fracture, D: knee-replacement surgery, E: hysterectomy, F: caesarean section, G: computed tomography scan, and H: magnetic resonance image scan) procedures in the administrative units (districts) and the new areal units. Solid lines represent the rate distribution in the administrative units (districts) and dotted lines represent the rate distribution in the new areal units.
Regarding the variation in procedure rates between districts and new areal units (Table 1), the EQ and the IDR were lower in new areal units for all procedures. The CV was also lower in new areal units, except for MRI. The SCV was lower in new areal units in surgery after hip fracture, knee-replacement surgery, and caesarean section. For CABG, PTCA, hysterectomy, and MRI, the SCV was higher in new areal units.
Table 1.
The statistics of variation in the administrative units (districts) and the new areal units
| EQ |
IDR |
CV |
SCV |
|||||
|---|---|---|---|---|---|---|---|---|
| Districts | New areal units | Districts | New areal units | Districts | New areal units | Districts | New areal units | |
| CABG | 21.75 | 5.53 | 3.12 | 1.97 | 0.52 | 0.30 | 4.2 | 4.7 |
| PTCA | 3.63 | 2.50 | 1.69 | 1.55 | 0.22 | 0.20 | 3.8 | 4.0 |
| HIP | 3.45 | 1.92 | 1.58 | 1.43 | 0.20 | 0.14 | 2.6 | 1.6 |
| KNEE | 3.92 | 2.56 | 2.04 | 1.73 | 0.27 | 0.22 | 11.9 | 5.5 |
| HYS | 3.54 | 2.53 | 1.63 | 1.48 | 0.20 | 0.17 | 2.1 | 2.8 |
| CSEC | 2.97 | 1.70 | 1.49 | 1.39 | 0.16 | 0.13 | 2.5 | 1.9 |
| CT | 2.06 | 1.48 | 1.31 | 1.25 | 0.12 | 0.09 | 1.9 | 1.1 |
| MRI | 2.81 | 2.31 | 1.37 | 1.34 | 0.16 | 0.16 | 2.3 | 2.5 |
EQ, extremal quotient; IDR, inter-decile ratio; CV, coefficient of variation; SCV, systematic component of variation; CABG, coronary artery bypass graft surgery; PTCA, percutaneous transluminal coronary angioplasty; HIP, surgery after hip fracture; KNEE, knee-replacement surgery; HYS, hysterectomy; CSEC, caesarean section; CT, computed tomography scan; MRI, magnetic resonance image scan.
When we compared variations among procedures, CABG, PTCA, knee-replacement surgery, and hysterectomy showed high variation both in districts and new areal units. CABG showed the highest values, followed by PTCA.
We compared the distribution of population sizes and variation statistics of Korea (districts and new areal units) with those of the 13 OECD member countries (Table 2). The average population size of the geographic units of the 13 countries ranged from 130 000 to 1 600 000 while that in Korea was about 300 000 (districts) and 900 000 (new areal units). The CV of population sizes in the 13 countries ranged from 0.26 to 1.44 with the average of the CV being 0.9. In Korea, the CV was 2.87 (districts) and 1.67 (new areal units) exceeding the maximum value among the administrative units of 13 countries (Table 2).
Table 2.
The distributions of populations and the coefficient of variation of the utilization rates of the eight procedures in 14 countries
| Country | Distribution of populations |
CV of utilization rates of the eight procedures1 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Geographic unit (total no. of units) | Average of the population sizes of the units | CV of population size | CABG | PTCA | HIP | KNEE | HYS | CSEC | CT | MRI | |
| Australia2 | Medicare locals (61) | 365 966 | 0.56 | 0.21 | 0.24 | 0.23 | 0.19 | 0.20 | 0.10 | N/A | N/A |
| Belgium3 | Provinces (11) | 1 447 994 | 1.07 | 0.17 | 0.18 | 0.16 | 0.14 | 0.13 | 0.09 | 0.18 | 0.18 |
| Canada4 | Provinces/territories (13) | 2 641 738 | 1.44 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Health regions (80) | 418 413 | 1.06 | 0.25 | 0.22 | N/A | 0.32 | 0.27 | 0.16 | 0.36 | 0.32 | |
| Czech Republic5 | Regions (14) | 754 444 | 0.43 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Districts (77) | 137 172 | 1.04 | N/A | N/A | N/A | 0.16 | 0.39 | 0.11 | N/A | N/A | |
| Finland6 | Hospital districts (20) | 268 646 | 1.18 | 0.34 | 0.30 | 0.13 | 0.18 | 0.20 | 0.18 | 0.24 | 0.24 |
| France7 | Departments (96) | 660 166 | 0.76 | 0.29 | 0.23 | 0.09 | 0.19 | 0.18 | 0.12 | N/A | N/A |
| Germany8,9 | Lands (16) | 5 074 846 | 0.92 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Spatial planning regions (96) | 838 789 | 0.74 | 0.24 | 0.22 | 0.11 | 0.17 | 0.14 | 0.13 | N/A | N/A | |
| Israel10 | Districts (6) | 1 251 900 | 0.26 | 0.27 | 0.12 | 0.14 | 0.28 | 0.23 | 0.16 | N/A | N/A |
| Italy11 | Regions (20) | 3 031 322 | 0.81 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Provinces (110) | 551 150 | 1.09 | 0.30 | 0.23 | 0.14 | 0.20 | 0.17 | 0.29 | N/A | N/A | |
| Portugal12 | Groups of municipalities (28) | 360 077 | 1.12 | 0.41 | 0.27 | 0.15 | 0.39 | 0.27 | 0.13 | N/A | N/A |
| Spain13 | Autonomous communities (17) | 2 741 286 | 0.89 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Provinces (50) | 884 746 | 1.20 | 0.50 | 0.30 | 0.20 | 0.31 | 0.21 | 0.26 | N/A | N/A | |
| Switzerland14 | Cantons (26) | 315 235 | 1.05 | 0.26 | 0.17 | 0.20 | 0.17 | N/A | 0.15 | N/A | N/A |
| UK/England15 | Primary care trusts (151) | 333 983 | 0.59 | 0.30 | 0.22 | 0.16 | 0.19 | N/A | 0.11 | N/A | N/A |
| OECD average16 | 1 226 549 | 0.90 | 0.30 | 0.23 | 0.16 | 0.22 | 0.22 | 0.15 | 0.26 | 0.25 | |
| Korea | Districts (163) | 313 751 | 2.87 | 0.50 | 0.22 | 0.15 | 0.26 | 0.16 | 0.20 | 0.12 | 0.15 |
| New areal units (57) | 897 219 | 1.67 | 0.32 | 0.21 | 0.16 | 0.21 | 0.12 | 0.17 | 0.09 | 0.16 | |
CABG, coronary artery bypass graft surgery; PTCA, percutaneous transluminal coronary angioplasty; HIP, surgery after hip fracture; KNEE, knee-replacement surgery; HYS, hysterectomy; CSEC, caesarean section; CT, computed tomography scan; MRI, magnetic resonance image scan; CV, coefficient of variation; N/A, not available; OECD, Organization for Economic Cooperation and Development.
CVs of the OECD countries except Korea were extracted from Geographic variation in health care, OECD (2014).
Sources from 2Medicare local population estimates update 2012, Australian Government Department of Human Services;
Total regional population of Belgium 2012, Statistics Belgium;
Health indicators 2012, Canadian Institute for Health Information;
Czech Republic general information, Czech Statistical Office,
Geographic variation in health care, OECD (2014);
Population from 1968 to 2014, National Institute of Statistics and Economic Studies (France);
Spatial planning region by area and population, Federal Statistical Office (Germany);
Population on the basis of census, Federal Statistical Office (Germany);
Population, by District, Sub-District and Religion, Central Bureau of Statistics (Israel);
Demographic balance for the year 2011 and resident population on the 8th October, National Institute of Statistics (Italy);
Population provisional estimates of resident, National Institute of Statistics (Portugal);
Population and housing census 2011, National Statistics Institute (Spain);
Permanent resident population per canton, Swiss Federal Statistical Office;
NHS (England) summarised accounts 2010-2011, UK for the Stationery Office;
Calculated based on the information presented in this table.
In the case of the CV of the procedure rates, both districts and new areal units showed a higher CV than the average CV of the 13 OECD member countries in CABG. In the other procedures, the CVs in districts and new areal units did not show a marked difference from the average of the other countries.
DISCUSSION
In this study, we compared population distribution and variation in procedure rates between administrative units and new areal units to evaluate the effect of the geographic unit of analysis on measuring geographic variation. The results showed that the variation both in the population size and the rate of some procedures decreased with the use of new areal units.
Although variation in population sizes decreased in new areal units, the CV of population sizes in new areal units was the highest in comparison to the 18 administrative units of the 13 OECD member countries and close to twice the average CV of the 18 geographic units. Given that the disparity in population sizes of the administrative units in those countries is considered large enough to cause extra-variation [3] and that the variation in population distribution in new areal units in this study is still larger compared with the administrative units in those countries, the population distribution of actual health care use in Korea seems highly uneven.
When comparing variation statistics between districts and new areal units, the EQ, the IDR, and the CV decreased for most of the procedures in new areal units. A decrease in variation was prominent in the rate of CABG. This result is consistent with a previous study, where the impact of geographic units on variation appeared significant in infrequent conditions (less than 100 per 100 000 inhabitants) [3]. Compared with other procedures, CABG is performed less frequently (Supplemental Table 1) and mainly performed in large-scale hospitals. In this study, procedure rates were calculated on the basis of the patient’s place of residence. A sharp decrease in variation in CABG between districts and new areal units indicates the likelihood that the rate of CABG is strongly influenced by the presence of an available hospital.
The change of the SCV between new areal units and districts is not consistent among procedures as in CV, which showed a decrease in the new areal units. As SCV is designed to extract the part of the variation caused by the deviation of the population structure of the units from that of the whole population, we can suppose that the new areal units concern mainly population distribution and the variation of procedure rates among the units, but less the population structure within the unit. In a previous study that compared the variation between administrative units and new areal units [3], change to the SCV was ambiguous while the EQ and the IQR showed decreases in new areal units. However, the present study is different from the previous study in that there was an explicit decrease or increase in SCV depending on the procedure. While the decrease in the SCV in new areal units can be explained as the decrease in variation, as in the case of the CV, an increase in the SCV in new areal units in some procedures such as CABG, PTCA, hysterectomy, and MRI suggests that true variation based on actual healthcare use increased despite the decrease in the apparent variation (CV). The CVs of procedure rates were high in CABG and knee-replacement surgery in both geographic units. This result is similar to results in previous studies [29,30]. In the case of CABG, the cardiologist performing the index catheterization and the treating hospital are known to be major factors in determining treatment options [31]. And patient preference also plays an important role [29]. With regard to knee-replacement surgery, the absence of clear guidelines or indication may contribute to geographic variation [30]. In addition, the patient’s preference is deemed important in making a decision on knee-replacement surgery [32].
Regarding the SCV, it has been suggested that an SCV greater than 3.0 could indicate that the variation is due to differences in practice style or medical discretion and variation with an SCV greater than 5.4 can be considered high, with an SCV greater than 10 considered very high [27]. In this study, the SCV was the highest in knee-replacement surgery, at 11.9 in the districts and 5.5 in new areal units. And in CABG and PTCA, the SCV was greater than three in both geographic units. This result is consistent with the previous study [27].
We compared the CV in districts and new areal units in Korea with that in the administrative units of the 13 OECD member countries. Although districts in Korea showed a higher CV than the average of the 13 countries for CABG, considering that the average population size in the districts and the new areal units is smaller than the average population size of the 13 OECD member countries and that CABG is a less frequently performed procedure, a higher CV for CABG in Korea is likely to be an overestimation. In the case of new areal units, the degree of variation was at a similar level with that in the other countries. As we discussed in the previous section, variation in population sizes in Korean administrative units is markedly higher than that in the other countries under analysis. Although the CVs in the OECD report were calculated on the basis of administrative units, prominently high variation in population size among the districts in Korea might have influenced the variation. And among the administrative units in the 13 OECD countries with which we compared the areal units in Korea, there are differences in the average and variation of the population sizes. Therefore, comparing variation in procedure rates based on those areal units may be statistically inappropriate. In interpreting the comparison, those limitations should be considered. To make a fair comparison of variation among countries, these issues should be addressed in future studies.
There are several limitations to this study. First, describing mainly the difference in variation among geographic units, we did not investigate which characteristics of geographic units influence geographic variation. Although we suspected that the population size of the unit and the total number of geographic units could influence variation, we did not identify other sources of variation. Second, regarding a decrease in the geographic variation in new areal units, we did not measure how much the number of geographic units and the variation in population distribution contributed to geographic variation. Third, although this study used an age–sex standardized rate to adjust population characteristics in measuring variation, population characteristics such as disease prevalence might not have been adjusted. Fourth, in the case of MRI, whose NHI coverage does not apply to all cases, the variation statistics produced in this study may not fully reflect the actual variation of the rate of all the MRI procedures performed in Korea.
Through this study we confirmed that geographic variation in medical services utilization could vary according to the geographic unit of analysis. And we also found that current administrative units in Korea might be vulnerable to extra-variation because of high variation in population size. In that respect, a statistically more comparable unit of analysis is needed. Future studies should be performed to elucidate how regional characteristics like population distribution affect geographic variation and to identify other factors that can influence geographic variation.
Acknowledgments
This article is based on a thesis submitted by the first author to Seoul National University College of Medicine in partial fulfillment for the Master of Science in Medicine. The authors thank Juyeon Lee for her support throughout the course of this study and Jinwook Bahk for her guidance in writing this article. The authors are grateful to Dr. David Goodman for his comments on this article. This study was supported by the National Health Insurance Service in Korea.
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
SUPPLEMENTAL MATERIAL
Use of the eight selected procedures and annual rate (2013 period, Korea)
REFERENCES
- 1.Wennberg JE. Tracking medicine: a researcher’s quest to understand health care. New York: Oxford University Press; 2010. p. 4. [Google Scholar]
- 2.Love T, Ehrenberg N, Health Quality & Safety Commission New Zealand . Addressing unwarranted variation: literature review on methods for influencing practice. Wellington: Health Quality & Safety Commission; 2014. p. 3. [Google Scholar]
- 3.Thygesen LC, Baixauli-Pérez C, Librero-López J, Martínez-Lizaga N, Ridao-López M, Bernal-Delgado E, et al. Comparing variation across European countries: building geographical areas to provide sounder estimates. Eur J Public Health. 2015;25 Suppl 1:8–14. doi: 10.1093/eurpub/cku229. [DOI] [PubMed] [Google Scholar]
- 4.Bernal-Delgado E, Christiansen T, Bloor K, Mateus C, Yazbeck AM, Munck J, et al. ECHO: health care performance assessment in several European health systems. Eur J Public Health. 2015;25 Suppl 1:3–7. doi: 10.1093/eurpub/cku219. [DOI] [PubMed] [Google Scholar]
- 5.Volinn E, Diehr P, Ciol MA, Loeser JD. Why does geographic variation in health care practices matter? (And seven questions to ask in evaluating studies on geographic variation) Spine (Phila Pa 1976) 1994;19(18 Suppl):2092S–2100S. doi: 10.1097/00007632-199409151-00012. [DOI] [PubMed] [Google Scholar]
- 6.Korea Health Industry Development Instituteh Report on demand and supply of hospital beds in Korea 2012. [cited 2015 Sep 9]. Available from: http://www.khanews.com/news/download.php?subUploadDir=201210/&savefilename=85541_37.pdf&filename=2012%B3%E2%BA%B4%BB%F3%BC%F6%B1%DE%BD%C7%C5%C2%BA%D0%BC%AE%B0%E1%B0%FA.pdf&idxno=85541 (Korean)
- 7.Lee HK, Moon OR, Lee KH. Geographic variations in tonsillectomy and adnoidectomy (T & A) and appendectomy in Korea. Korean J Prev Med. 1993;26(3):430–441. (Korean) [Google Scholar]
- 8.Moon YO, Park EC, Shin HR, Won YJ, Jung KW, Lee JH, et al. Regional variation in accessing regional hospitals for cancer patients. Korean J Epidemiol. 2006;28(2):152–161. (Korean) [Google Scholar]
- 9.Seo YS, Lee KS, Park JH, Kang SH. A study on regional medical utilization variation of hospital inpatients in Korea. J Korea Acad Ind Coop Soc. 2010;11(4):1511–1519. (Korean) [Google Scholar]
- 10.Shin HS, Lee SH. Factors affecting spatial distance to outpatient health services. ournal title. Health Policy Manag. 2011;21(1):23–43. (Korean) [Google Scholar]
- 11.Lee YH, Choi KS, Lee HY, Jun JK. Current status of the National Cancer Screening Program for cervical cancer in Korea, 2009. J Gynecol Oncol. 2012;23(1):16–21. doi: 10.3802/jgo.2012.23.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi YH, Na BJ, Lee JY, Hwang JH, Lim NG, Lee SK. Obstetric complications by the accessibility to local obstetric service. J Agr Med Community Health. 2013;38(1):14–24. (Korean) [Google Scholar]
- 13.Kim YM, Cho DG, Kang SH. An empirical analysis on geographic variations in the prevalence of diabetes. Health Soc Welf Rev. 2014;34(3):82–105. (Korean) [Google Scholar]
- 14.Hong JS, Kang HC. Regional differences in treatment frequency and case-fatality rates in korean patients with acute myocardial infarction using the Korea national health insurance claims database: findings of a large retrospective cohort study. Medicine (Baltimore) 2014;93(28):e287. doi: 10.1097/MD.0000000000000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahn HS, Kwon YD, Lee YS, Kim MK, Kim YI, Shin YS. Analysis of institutional factors influencing regional variations in the cesarean section rate. Korean J Health Policy Adm. 1991;1(1):27–41. (Korean) [Google Scholar]
- 16.Cho WH, Lee SH, Park EC, Sohn MS, Kim SR. An Analysis of small area variations of hospital services utilization in Korea. Korean J Prev Med. 1994;27(3):609–626. (Korean) [Google Scholar]
- 17.Kim YM, Yang BM. Small area variation in rates of common surgery in general surgery department. Korean J Health Policy Adm. 2004;14(2):138–162. (Korean) [Google Scholar]
- 18.Shin HY, Ahn HS, Lee CS. Estimation of social welfare loss due to small area variations in health care utilization. Health Soc Welf Rev. 2007;27(1):52–80. (Korean) [Google Scholar]
- 19.Kim JH, Cho BM, Hwang IK, Sohn MJ, Yoon TH. Trends of health care utilization and relevance index of stroke inpatients among the self-employed insured and their dependents of national health insurance (1998-2005) Korean J Health Policy Adm. 2008;18(4):66–84. (Korean) [Google Scholar]
- 20.Park SK, Lee SH, Chung AR, Cha YK, Myoung HB, Na BJ. Study on developing health service area on the health service utilization and supply. Seoul: Korea Health Industry Development Institue; 2011. pp. 58-76, 103-108. (Korean) [Google Scholar]
- 21.Song YJ. The South Korean health care system. Japan Med Assoc J. 2009;52(3):206–209. [Google Scholar]
- 22.Organisation for Economic Cooperation and Development Focus on health: geographic variations in health care. 2014 [cited 2016 Jul 19]. Available from: https://www.oecd.org/els/health-systems/FOCUS-on-Geographic-Variations-in-Health-Care.pdf.
- 23.Kim Y, Lee TS, Lee H, Kwak NY, Lee S, Park S, et al. Constructing the KNHI Atlas for health map service. Seoul: Korea National Health Insurance; 2015. p. 48. (Korean) [Google Scholar]
- 24.Guidoum AC. Kernel estimator and bandwidth selection for density and its derivatives. 2015 [cited 2016 Jul 19]. Available from: https://cran.r-project.org/web/packages/kedd/vgnettes/kedd.pdf.
- 25.Kazandjian VA, Durance PW, Schork MA. The extremal quotient in small-area variation analysis. Health Serv Res. 1989;24(5):665–684. [PMC free article] [PubMed] [Google Scholar]
- 26.Sørensen JB. The use and misuse of the coefficient of variation in organizational demography research. Sociol Methods Res. 2002;30(4):475–491. [Google Scholar]
- 27.Appleby J, Raleigh V, Frosini F, Bevan G, Gao H, Lyscom T. Variations in health care: the good, the bad and the inexplicable. 2011 [cited 2016 Jul 19]. Available from: http://www.kingsfund.org.uk/sites/files/kf/Variations-in-health-care-good-bad-inexplicable-report-The-Kings-Fund-April-2011.pdf.
- 28.McPherson K, Wennberg JE, Hovind OB, Clifford P. Small-area variations in the use of common surgical procedures: an international comparison of New England, England, and Norway. N Engl J Med. 1982;307(21):1310–1314. doi: 10.1056/NEJM198211183072104. [DOI] [PubMed] [Google Scholar]
- 29.Brownlee S, Wennberg JE, Barry MJ, Fisher ES, Goodman DC, Bynum JP. Improving patient decision-making in health care: a 2011 Dartmouth Atlas report highlighting Minnesota. 2011 [cited 2016 Jul 19]. Avaiable from: http://www.dartmouthatlas.org/downloads/reports/Decision_making_report_022411.pdf. [PubMed]
- 30.Dieppe P, Basler HD, Chard J, Croft P, Dixon J, Hurley M, et al. Knee replacement surgery for osteoarthritis: effectiveness, practice variations, indications and possible determinants of utilization. Rheumatology (Oxford) 1999;38(1):73–83. doi: 10.1093/rheumatology/38.1.73. [DOI] [PubMed] [Google Scholar]
- 31.Tu JV, Ko DT, Guo H, Richards JA, Walton N, Natarajan MK, et al. Determinants of variations in coronary revascularization practices. CMAJ. 2012;184(2):179–186. doi: 10.1503/cmaj.111072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hawker GA. Who, when, and why total joint replacement surgery? The patient’s perspective. Curr Opin Rheumatol. 2006;18(5):526–530. doi: 10.1097/01.bor.0000240367.62583.51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Use of the eight selected procedures and annual rate (2013 period, Korea)


