SUMMARY
Since the first antiviral drug, idoxuridine, was approved in 1963, 90 antiviral drugs categorized into 13 functional groups have been formally approved for the treatment of the following 9 human infectious diseases: (i) HIV infections (protease inhibitors, integrase inhibitors, entry inhibitors, nucleoside reverse transcriptase inhibitors, nonnucleoside reverse transcriptase inhibitors, and acyclic nucleoside phosphonate analogues), (ii) hepatitis B virus (HBV) infections (lamivudine, interferons, nucleoside analogues, and acyclic nucleoside phosphonate analogues), (iii) hepatitis C virus (HCV) infections (ribavirin, interferons, NS3/4A protease inhibitors, NS5A inhibitors, and NS5B polymerase inhibitors), (iv) herpesvirus infections (5-substituted 2′-deoxyuridine analogues, entry inhibitors, nucleoside analogues, pyrophosphate analogues, and acyclic guanosine analogues), (v) influenza virus infections (ribavirin, matrix 2 protein inhibitors, RNA polymerase inhibitors, and neuraminidase inhibitors), (vi) human cytomegalovirus infections (acyclic guanosine analogues, acyclic nucleoside phosphonate analogues, pyrophosphate analogues, and oligonucleotides), (vii) varicella-zoster virus infections (acyclic guanosine analogues, nucleoside analogues, 5-substituted 2′-deoxyuridine analogues, and antibodies), (viii) respiratory syncytial virus infections (ribavirin and antibodies), and (ix) external anogenital warts caused by human papillomavirus infections (imiquimod, sinecatechins, and podofilox). Here, we present for the first time a comprehensive overview of antiviral drugs approved over the past 50 years, shedding light on the development of effective antiviral treatments against current and emerging infectious diseases worldwide.
INTRODUCTION
Over the course of human civilization, viral infections have caused millions of human casualties worldwide, driving the development of antiviral drugs in a pressing need (1, 2). A new era of antiviral drug development has begun since the first antiviral drug, idoxuridine, was approved in June 1963 (3) (Fig. 1). Since then, many antiviral drugs have been developed for clinical use to treat millions of human beings worldwide. Between June 1963 and April 2016, 90 drugs were formally approved to treat 9 human infectious diseases (Table 1) despite the fact that thousands of antiviral inhibitors have been proposed in the literature. Previously, we reviewed the history of 25 approved antiretroviral drugs over 25 years (1984 to 2009) (4, 5). The present study commemorates 90 antiviral drugs approved for the treatment of 9 human infectious diseases over the past 5 decades.
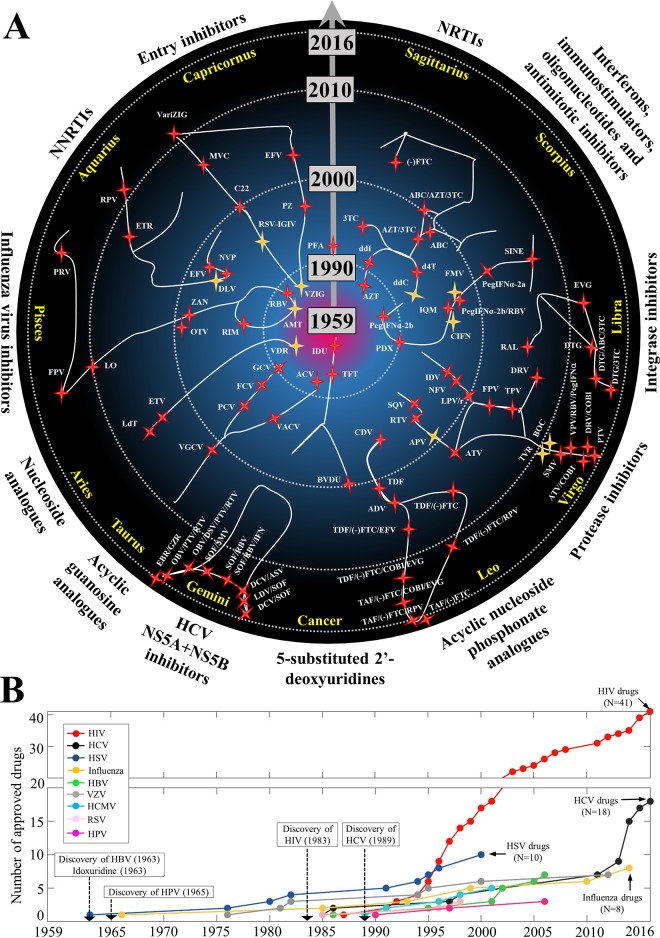
FIG 1.
History of antiviral drugs approved between January 1959 and April 2016. (A) Approved antiviral drugs visualized in the zodiac. The gray arrow shows the dates of approval of antiviral drugs from January 1959 to April 2016. Twelve signs are positioned in a circle. Each sign indicates a drug group whose name is annotated outside the circle. In the drug group, each red star within a sign represents an approved drug, placed according to the year of approval. Yellow stars indicate approved drugs that have been discontinued or abandoned for clinical use. A total of 90 stars thus represent all approved antiviral drugs, and each drug star is positioned according to its approval date (Table 2). In this picture, every approved drug could be conceived as a “superstar,” and its contribution to human health is worthy of being remembered and respected. Therefore, this zodiac-based figure metaphorically recognizes each antiviral drug as a star in the universe, commemorating the significant contributions of antiviral drug discovery and development over the past 50 years. A list of drug abbreviations is available in Table 2. Movies and label information for approved drugs are accessible online (see http://www.virusface.com/). (B) Timeline of approval of drugs against 9 human infectious diseases (HIV, HBV, HCV, HSV, HCMV, HPV, RSV, VZV, and influenza virus). The x axis indicates the period from January 1959 to April 2016, and the y axis shows the total number of approved drugs. For each virus, a colored line demonstrates the total number of approved drugs. Moreover, years of discovery of HBV (1963), HPV (1965), HIV (1983), and HCV (1989) are indicated, while the other five viruses were discovered before 1959 (Table 1).
TABLE 1.
Summary of 9 human infectious diseases treated by approved drugs
| Human virus | Yr of discovery/isolation | Animal reservoir(s) | Transmission route | Mean incubation period (range) | Mean viral particle diam (nm) (range) | Genome type,c length (kb) | Protein target(s) of approved drug(s) |
|---|---|---|---|---|---|---|---|
| HIV | 1983 | Chimpanzee, gorilla, sooty mangabey | Blood borne | 8–11 yr | ∼145 (95–166) | Linear (+)ssRNA, ∼9.8 | Protease, RT, integrase, GP41, CCR5 |
| HCV | 1989 | Unclear | Blood borne | ∼7 wk (4–20 wk) | ∼68 (45–86) | Linear (+)ssRNA, ∼9.6 | NS3/4 protease, NS5A, NS5B polymerase |
| Human influenza virus | 1933 | Birds, pigs, horses | Respiratory | ∼2 days (1–4 days) | ∼120 (84–170) | Linear (−)ssRNA, ∼13.6 | Matrix protein 2, neuraminidase, RNA polymerase |
| RSV | 1957 | No animal reservoir | Respiratory | ∼5 days (3–8 days) | 100–1,000 | Linear (−)ssRNA, ∼15 | RNA polymerase, glycoproteins |
| HBV | 1963 | Unclear (bats?) | Blood borne | 90 days (60–150 days) | 42–46 | Circular dsDNA, ∼3.3 | DNA polymerase |
| HCMV | 1956 | No animal reservoir | Blood borne | 3–12 wk | 150–200 | Linear dsDNA, ∼230 | DNA polymerase |
| HSV | Before 1900 | No animal reservoir | Sexual or skin contact | ∼4 days (2–12 days) | ∼225 (209–239) | Linear dsDNA, 152–155 | DNA polymerase, envelope proteins |
| VZV | 1953 | No animal reservoir | Respiratory | 10–21 days | 150–200 | Linear dsDNA, ∼125 | DNA polymerase, envelope proteins |
| HPV | 1965 | No animal reservoira | Skin-to-skin contact | ∼2.9 mo (0.5–8 mo) | 65–120 | Circular dsDNA, ∼8 | —b |
Papillomaviruses have been widely found in birds, reptiles, marsupials, and mammals, whereas cross-transfer between species is rare (54).
Instead of targeting HPV proteins directly, three FDA-approved drugs (podofilox, sinecatechins, and imiquimod) act as immunomodulatory or antimitotic agents to treat external genital warts caused by HPV infections.
(+)ssRNA, positive-sense single-stranded RNA; (−)ssRNA, negative-sense single-stranded RNA; dsDNA, double-stranded DNA.
Approved antiviral drugs could be arbitrarily divided in 13 functional groups: (i) 5-substituted 2′-deoxyuridine analogues (n = 3 drugs and drug combinations); (ii) nucleoside analogues (n = 3); (iii) (nonnucleoside) pyrophosphate analogues (n = 1); (iv) nucleoside reverse transcriptase (RT) inhibitors (NRTIs) (n = 9); (v) nonnucleoside reverse transcriptase inhibitors (NNRTIs) (n = 5); (vi) protease inhibitors (PIs) (n = 19); (vii) integrase inhibitors (n = 5); (viii) entry inhibitors (n = 7); (ix) acyclic guanosine analogues (n = 6); (x) acyclic nucleoside phosphonate (ANP) analogues (n = 10); (xi) hepatitis C virus (HCV) NS5A and NS5B inhibitors (n = 8); (xii) influenza virus inhibitors (n = 8); and (xiii) immunostimulators, interferons, oligonucleotides, and antimitotic inhibitors (n = 8). The inhibitory spectrum of these approved drugs against 9 human infectious diseases can be summarized as follows: human immunodeficiency virus (HIV) (groups iv, v, vi, vii, viii, and x), human cytomegalovirus (HCMV) (groups iii, ix, x, and xiii), hepatitis B virus (HBV) (groups ii, iv, x, and xiii), HCV (groups vi, xi, xii, and xiii), herpes simplex virus (HSV) (groups i, ii, iii, viii, and ix), influenza virus (group xii), respiratory syncytial virus (RSV) (groups viii and xii), varicella-zoster virus (VZV) (groups i, ii, viii, and ix), and human papillomavirus (HPV) (group xiii). Table 2 summarizes the information on antiviral drugs regarding their approval dates and mechanisms of drug action. Table S1 in the supplemental material provides details on drug databases and chemical formulas.
TABLE 2.
Summary of 90 approved antiviral drugs in 13 drug groupsf
| Drug group | Drug name | Abbreviationc | Brand name(s)d | Approved clinical use(s) | Mechanism(s) of drug action | Approval datee |
|---|---|---|---|---|---|---|
| 5-substituted 2′-deoxyuridine analogues | Idoxuridine | IDU | Dendrid | HSV-1 | Substitutes for thymidine and targets HSV DNA polymerase to inhibit viral DNA synthesis | June 1963 |
| Trifluridine | TFT | Viroptic | HSV | Inhibits HSV DNA replication | Apr. 1980 | |
| Brivudine | BVDU | Zostex (Europe) | HSV-1, VZV | Brivudine triphosphate targets VZV DNA polymerase to inhibit viral DNA synthesis | 2000 | |
| Nucleoside analogues | Vidarabinea | VDR | Vira-A | HSV, VZV | Vidarabine triphosphate competes with dATP to inhibit the activity of viral DNA polymerase | Nov. 1976 |
| Entecavir | ETV | Baraclude | HBV | Inhibits the activity of HBV DNA polymerase | Mar. 2005 | |
| Telbivudine | LdT | Tyzeka | HBV | Inhibits the activity of HBV DNA polymerase | Oct. 2006 | |
| Pyrophosphate analogues | Foscarnet | PFA | Foscavir | HCMV, HSV (acyclovir resistant) | Inhibits the activity of viral DNA polymerase | Sept. 1991 |
| NRTIs | Zidovudine | AZT | Retrovir | HIV | Targets HIV RT and competes with dTTP to inhibit DNA synthesis | Mar. 1987 |
| Didanosine | ddI | Videx | HIV | Targets HIV RT and competes with dATP to inhibit DNA synthesis | Oct. 1991 | |
| Zalcitabinea | ddC | Hivid | HIV | Targets HIV RT and competes with dCTP to inhibit DNA synthesis | June 1992 | |
| Stavudine | d4T | Zerit | HIV | Targets HIV RT and competes with dTTP to inhibit DNA synthesis | June 1994 | |
| Lamivudine | 3TC | Epivir | HIV, HBV | Targets viral polymerase and competes with dCTP to inhibit DNA synthesis | Nov. 1995 | |
| Lamivudine + zidovudine | 3TC+AZT | Combivir | HIV | Twice-daily, fixed-dose, single-tablet drug used to inhibit the activity of HIV RT | Sept. 1997 | |
| Abacavir | ABC | Ziagen | HIV | Targets HIV RT and competes with dGTP to inhibit DNA synthesis | Dec. 1998 | |
| Abacavir + lamivudine + zidovudine | ABC+3TC+AZT | Trizivir | HIV | Twice-daily, fixed-dose, single-tablet drug of abacavir, lamivudine, and zidovudine used to inhibit the activity of HIV RT | Nov. 2000 | |
| Emtricitabine | (−)FTC | Emtriva | HIV | Targets HIV RT and competes with dCTP to inhibit DNA synthesis | July 2003 | |
| NNRTIs | Nevirapine | NVP | Viramune | HIV-1 | Binds directly to HIV RT and inhibits DNA synthesis | June 1996 |
| Delavirdinea | DLV | Rescriptor | HIV-1 | Binds directly to HIV RT and inhibits DNA synthesis | Apr. 1997 | |
| Efavirenz | EFV | Sustiva | HIV-1 | Binds directly to HIV RT and inhibits DNA synthesis | Sept. 1998 | |
| Etravirine | ETR | Intelence | HIV-1 | Binds directly to HIV RT and inhibits DNA synthesis | Jan. 2008 | |
| Rilpivirine | RPV | Edurant | HIV-1 | Binds directly to HIV RT and inhibits DNA synthesis | Aug. 2011 | |
| Protease inhibitors | Saquinavir | SQV | Invirase | HIV | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | Dec. 1995 |
| Ritonavir | RTV | Norvir | HIV | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | Mar. 1996 | |
| Indinavir | IDV | Crixivan | HIV | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | Mar. 1996 | |
| Nelfinavir | NFV | Viracept | HIV | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | Mar. 1997 | |
| Amprenavira | APV | Agenerase | HIV-1 | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | Apr. 1999 | |
| Lopinavir-ritonavir | LPV/r | Kaletra | HIV | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | Sept. 2000 | |
| Atazanavir | ATV | Reyataz | HIV | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | June 2003 | |
| Fosamprenavir | FPV | Lexia | HIV-1 | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | Oct. 2003 | |
| Tipranavir | TPV | Aptivus | HIV-1 | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | June 2005 | |
| Darunavir | DRV | Prezista | HIV | Blocks the active site of HIV protease to prevent cleavage of viral precursor proteins | June 2006 | |
| Darunavir + cobicistat | DRV+COBI | Prezcobix | HIV | HIV protease inhibitors can be combined with cobicistat to inhibit the activity of HIV protease | Jan. 2015 | |
| Atazanavir + cobicistat | ATV+COBI | Evotaz | HIV | Jan. 2015 | ||
| Telaprevira | TVR | Incivek | HCV genotype 1 | HCV protease drugs can inhibit the proteolytic activity of HCV NS3/4A protease; ribavirin and PegIFNα can interfere with HCV replication | May 2011 | |
| Boceprevira | BOC | Victrelis | HCV genotype 1 | May 2011 | ||
| Simeprevir | SMV | Olysio | HCV genotype 1 | Nov. 2013 | ||
| Asunaprevirb | ASV | Sunvepra (Japan) | HCV genotype 1 | July 2014 | ||
| Vaniprevir + ribavirin + PegIFNα-2b | VPV+RBV+PegIF-α2b | Vanihep (Japan) | HCV genotype 1 | Sept. 2014 | ||
| Paritaprevirb | PTV | Viekira Pak | HCV genotype 1 | Dec. 2014 | ||
| Technivie | HCV genotype 4 | July 2015 | ||||
| Grazoprevirb | GZR | Zepatier | HCV genotype 1 or 4 | Jan. 2016 | ||
| Integrase inhibitors | Raltegravir | RAL | Isentress | HIV | Targets HIV integrase to inhibit the integration of viral DNA into human chromosomes | Oct. 2007 |
| Elvitegravir | EVG | Vitekta | HIV | Targets HIV integrase to inhibit the integration of viral DNA into human chromosomes | Aug. 2012 | |
| Dolutegravir | DTG | Tivicay | HIV | Targets HIV integrase to inhibit the integration of viral DNA into human chromosomes | Aug. 2013 | |
| Dolutegravir + abacavir + lamivudine | DTG+ABC+3TC | Triumeq | HIV | Fixed-dose combinations with dolutegravir and NRTIs can target HIV integrase and RT to interrupt viral replication | Aug. 2014 | |
| Dolutegravir + lamivudine | DTG+3TC | Dutrebis | HIV | Feb. 2015 | ||
| Entry inhibitors | RSV-IGIVa | RSV-IGIV | RespiGam | RSV | RSV-neutralizing antibodies may prevent binding of RSV surface glycoproteins F and G | Jan. 1996 |
| Palivizumab | PZ | Synagis | RSV | Monoclonal antibody that targets the antigenic site of RSV glycoprotein F | June 1998 | |
| Docosanol | C22 | Abreva | HSV | May interfere with binding of viral envelope proteins to cell membrane receptors | July 2000 | |
| Enfuvirtide | EFV | Fuzeon | HIV-1 | Blocks HIV GP41 fusion to cell membrane | Mar. 2003 | |
| Maraviroc | MVC | Selzentry | HIV | Blocks GP120-CCR5 interaction to inhibit HIV entry | Aug. 2007 | |
| VZIGa | VZIG | VZIG | VZV | IgG antibodies protect patients from VZV infection | Feb. 1981 | |
| VariZIG | VariZIG | VariZIG | VZV | IgG antibodies protect patients from VZV infection | Dec. 2012 | |
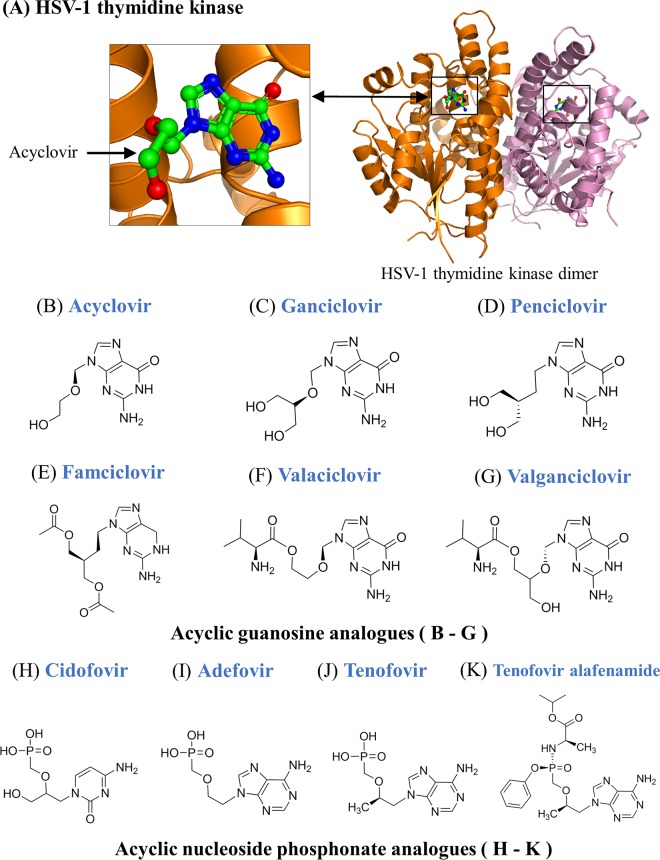
| Acyclic guanosine analogues | Acyclovir | ACV | Zovirax | HSV, VZV | Acyclovir triphosphate competes with dGTP to inhibit viral DNA polymerase activity | Mar. 1982 |
| Ganciclovir | GCV | Zirgan, Vitrasert | HCMV | Ganciclovir triphosphate targets HCMV DNA polymerase to inhibit viral DNA synthesis | June 1989 | |
| Famciclovir | FCV | Famvir | HSV, VZV | Famciclovir triphosphate competes with dGTP to inhibit the activity of viral DNA polymerase | June 1994 | |
| Valacyclovir | VACV | Valtrex | HSV, VZV | Valacyclovir triphosphate competes with dGTP to inhibit the activity of viral DNA polymerase | June 1995 | |
| Penciclovir | PCV | Denavir | HSV | Penciclovir triphosphate targets HSV DNA polymerase to inhibit viral DNA synthesis | Sept. 1996 | |
| Valganciclovir | VGCV | Valcyte | HCMV | Valganciclovir triphosphate competes with dGTP to inhibit the activity of viral DNA polymerase | Mar. 2001 | |
| Acyclic nucleoside phosphonate analogues | Cidofovir | CDV | Vistide | HCMV retinitis (AIDS patients) | Inhibits the activity of HCMV DNA polymerase | June 1996 |
| Tenofovir disoproxil fumarate | TDF | Viread | HIV, HBV | Competes with dATP to inhibit the activity of HIV RT and HBV DNA polymerase | Oct. 2001 | |
| Adefovir dipivoxil | ADV | Hepsera | HBV | Adefovir diphosphate competes with dATP to inhibit the activity of HBV DNA polymerase | Sept. 2002 | |
| Tenofovir disoproxil fumarate + emtricitabine | TDF+(−)FTC | Truvada | HIV | Truvada is a once-daily fixed-dose single tablet containing 2 drugs to inhibit HIV replication | Aug. 2004 | |
| Tenofovir disoproxil fumarate + efavirenz + emtricitabine | TDF+EFV+(−)FTC | Atripla | HIV | Atripla is a once-daily fixed-dose single tablet containing 3 drugs to inhibit HIV replication | July 2006 | |
| Tenofovir disoproxil fumarate + rilpivirine + emtricitabine | TDF+RPV+(−)FTC | Complera, Eviplera | HIV | Complera is a once-daily fixed-dose single tablet containing 3 drugs to inhibit HIV replication | Aug. 2011 | |
| Tenofovir disoproxil fumarate + cobicistat + emtricitabine + elvitegravir | TDF+COBI+(−)FTC+EVG | Stribild | HIV | Stribild is a once-daily fixed-dose single tablet containing 4 drugs to inhibit HIV replication | Aug. 2012 | |
| Tenofovir alafenamide + cobicistat + emtricitabine + elvitegravir | TAF+COBI+(−)FTC+EVG | Genvoya | HIV | Genvoya is a once-daily fixed-dose single tablet containing 4 drugs to inhibit HIV replication | Nov. 2015 | |
| Tenofovir alafenamide + rilpivirine + emtricitabine | TAF+RPV+(−)FTC | Odefsey | HIV | Odefsey is a once-daily fixed-dose single tablet containing 3 drugs to inhibit HIV replication | Mar. 2016 | |
| Tenofovir alafenamide + emtricitabine | TAF+(−)FTC | Descovy | HIV | Descovy is a once-daily fixed-dose single tablet containing 2 drugs to inhibit HIV replication | Apr. 2016 | |
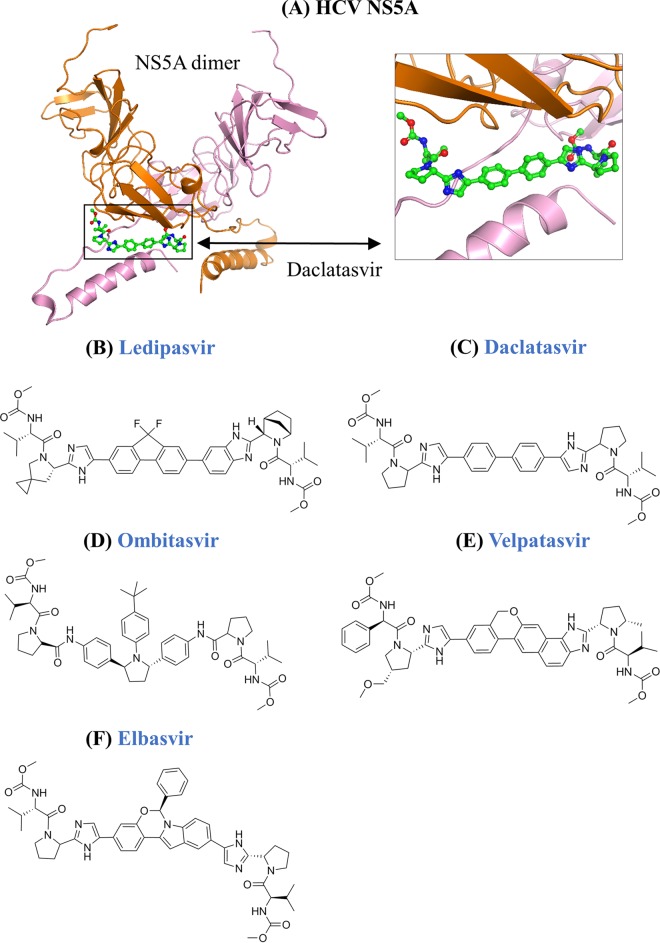
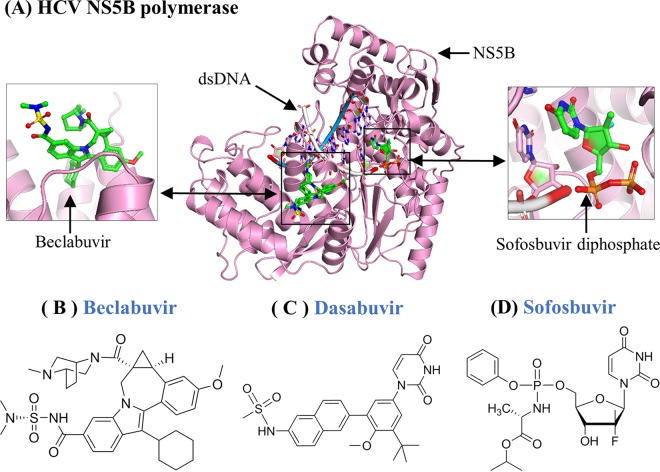
| HCV NS5A and NS5B inhibitors | Sofosbuvir + ribavirin | SOF+RBV | Sovaldi | HCV genotype 2 or 3 | Sofosbuvir binds to Mg2+ ions in NS5B polymerase and inhibits HCV replication; ribavirin and PegIFNα can interfere with HCV replication | Dec. 2013 |
| Sofosbuvir + ribavirin + PegIFNα | SOF+RBV+PegIFNα | Sovaldi | HCV genotype 1 or 4 | Dec. 2013 | ||
| Daclatasvir + asunaprevir | DCV+ASV | Daklinza + Sunvepra (Japan) | HCV genotype 1 | Targets NS5A and NS3/4A protease to prevent HCV replication | July 2014 | |
| Ledipasvir + sofosbuvir | LDV+SOF | Harvoni | HCV genotype 1 | Harvoni inhibits HCV NS5A and NS5B polymerase to prevent RNA replication | Oct. 2014 | |
| Sofosbuvir+ simeprevir | SOF+SMV | Sovaldi + Olysio | HCV genotype 1 | Sofosbuvir and simeprevir target HCV NS5B and NS3/4 protease, respectively | Nov. 2014 | |
| Ombitasvir + dasabuvir + paritaprevir + ritonavir | OBV+DAS+PTV+RTV | Viekira Pak | HCV genotype 1 | Viekira Pak is a multiclass combination drug approved for treatment of HCV genotype 1 infection; inhibits activities of HCV NS5A, NS5B polymerase, and NS3/4A protease | Dec. 2014 | |
| Ombitasvir + paritaprevir + ritonavir | OBV+PTV+RTV | Technivie | HCV genotype 4 | Technivie is used with ribavirin to treat HCV genotype 4 infection; inhibits HCV NS5A and NS3/4A protease | July 2015 | |
| Daclatasvir + sofosbuvir | DCV+SOF | Daklinza + Sovaldi | HCV genotype 3 | Inhibits activities of HCV NS5A and NS5B polymerase | July 2015 | |
| Elbasvir + grazoprevir | EBR+GZR | Zepatier | HCV genotype 1 or 4 | Elbasvir and grazoprevir inhibit activities of NS5A and NS3/4A protease, respectively | Jan. 2016 | |
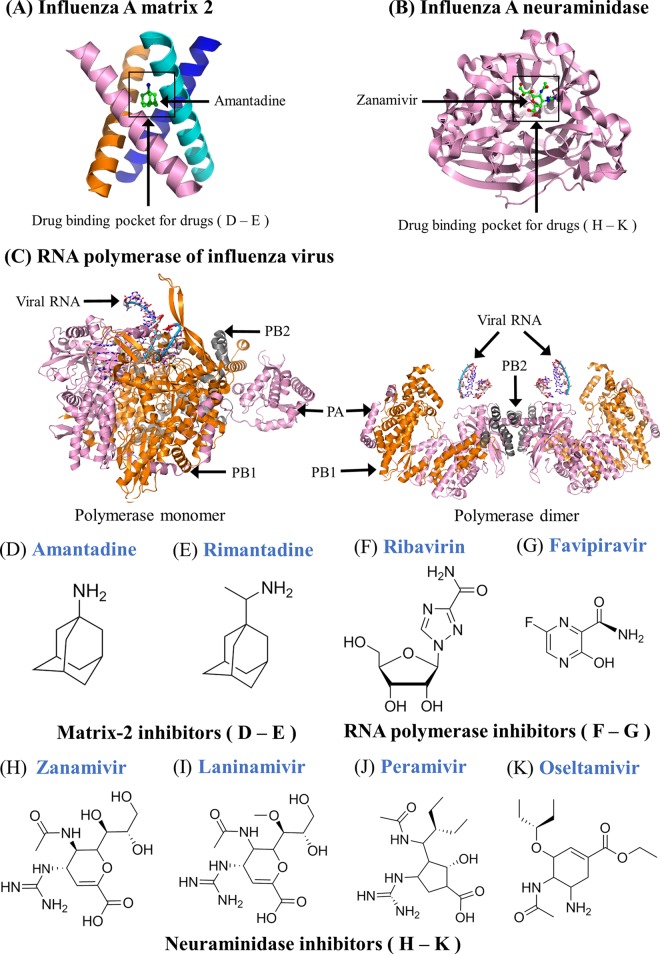
| Influenza virus inhibitors | Amantadinea | AMT | Symmetrel | Influenza virus A | Targets viral matrix protein 2 to inhibit viral uncoating | Oct. 1966 |
| Ribavirin | RBV | Copegus, Rebetol, Virazole | HCV, RSV, hemorrhagic fever | Ribavirin triphosphate targets viral RNA polymerase to inhibit mRNA synthesis | Dec. 1985 | |
| Rimantadine | RIM | Flumadine | Influenza virus A | Targets matrix protein 2 to inhibit viral uncoating | Sept. 1993 | |
| Zanamivir | ZAN | Relenza | Influenza viruses A and B | Targets viral neuraminidase to inhibit virus release from host cells | July 1999 | |
| Oseltamivir | OTV | Tamiflu | Influenza viruses A and B | Targets viral neuraminidase to inhibit virus release from host cells | Oct. 1999 | |
| Laninamivir octanoate | LO | Inavir (Japan) | Influenza viruses A and B | Targets viral neuraminidase to inhibit virus release from host cells | Sept. 2010 | |
| Peramivir | PRV | Rapivab | Influenza viruses A and B | Targets viral neuraminidase to inhibit virus release from host cells | Dec. 2014 | |
| Favipiravir | FPV | Avigan (Japan) | Influenza viruses A, B, and C | Favipiravir-ribofuranosyl-5′-triphosphate inhibits the activity of influenza RNA polymerase | Mar. 2014 | |
| Interferons, immunostimulators, oligonucleotides, and antimitotic inhibitors | Pegylated interferon alfa 2b | PegIFNα-2b | Intron-A, PegIntron | HBV, HCV | PegIFNα-2b is used to treat patients with HBV and/or HCV infection | June 1986 |
| Interferon alfacon 1a | CIFN | Infergen | HCV genotype 1 | Interferon alfacon 1 can be used with ribavirin to treat HCV infection | Oct. 1997 | |
| Pegylated interferon alfa 2b + ribavirin | PegIFNα-2b+RBV | Rebetron | HCV | PegIFNα-2b is used with ribavirin to treat patients with HCV infection | June 1998 | |
| Pegylated interferon alfa 2a | PegIFN-α2a | Pegasys, Roferon-A | HBV, HCV | Used with or without ribavirin to treat patients with HCV and/or HBV infection | Oct. 2002 | |
| Fomivirsena | FMV | Vitravene | HCMV | Antisense RNA interrupts HCMV gene expression | Aug. 1998 | |
| Podofilox | PDX | Condylox | HPV-related diseases | Antimitotic drug that interrupts cell division | Dec. 1990 | |
| Imiquimod | IQM | Aldara | HPV-related diseases | Stimulates cytokines to clear external genital warts | Feb. 1997 | |
| Sinecatechins | SINE | Veregen | HPV-related diseases | Botanical drug that acts as an immunomodulator to interfere with HSV-induced pathways | Oct. 2006 |
Discontinued antiviral drug (amantadine, amprenavir, boceprevir, delavirdine, fomivirsen, RSV-IGIV, VZIG, telaprevir, vidarabine, zalcitabine, and interferon alfacon 1).
Different combination drugs. The combination of asunaprevir plus daclatasvir was approved to treat HCV genotype 1 infection in Japan, the combination of grazoprevir plus elbasvir was approved to treat HCV genotype 1 or 4 infection, the combination of paritaprevir plus ombitasvir plus dasabuvir plus ritonavir was approved to treat HCV genotype 1 infection, and the combination of paritaprevir plus ombitasvir plus ritonavir was approved to treat HCV genotype 4 infection.
Abbreviations commonly used in literature. The first four letters are used if drug abbreviations could not be found (e.g., sinecatechins are abbreviated SINE).
Antiviral drugs that have been approved in either Japan or Europe but not in the United States are indicated by “(Japan)” or “(Europe).”
Only the earliest time is listed if several approval dates for different clinical applications were found.
Table S1 in the supplemental material summarizes information on drug databases and chemical formulas. Information on dosage and administration of approved antiviral drugs is available online (see http://www.fda.gov/ and http://www.virusface.com/).
Nine human viruses can be classified into DNA viruses (HBV, HCMV, HSV, HPV, and VZV), RNA viruses (HCV, RSV, and influenza virus), and retroviruses (HIV) (Fig. 2). Interestingly, 11 of 90 antiviral drugs have been approved for the treatment of more than one infectious disease (Table 2), suggesting that antiviral drugs may potentially treat multiple viral infections. Ribavirin, for instance, is effective against three RNA viruses: HCV, RSV, and influenza virus (Fig. 3). More importantly, antiviral drugs from the same drug group share similar mechanisms of drug action to inhibit viral replication during the viral life cycle (Fig. 4). In some cases, approved antiviral drugs could be used as off-label treatments for emerging infectious diseases. Therefore, a comprehensive review that summarizes all approved antiviral drugs will shed light on the development of novel inhibitors against current and emerging viral infections.
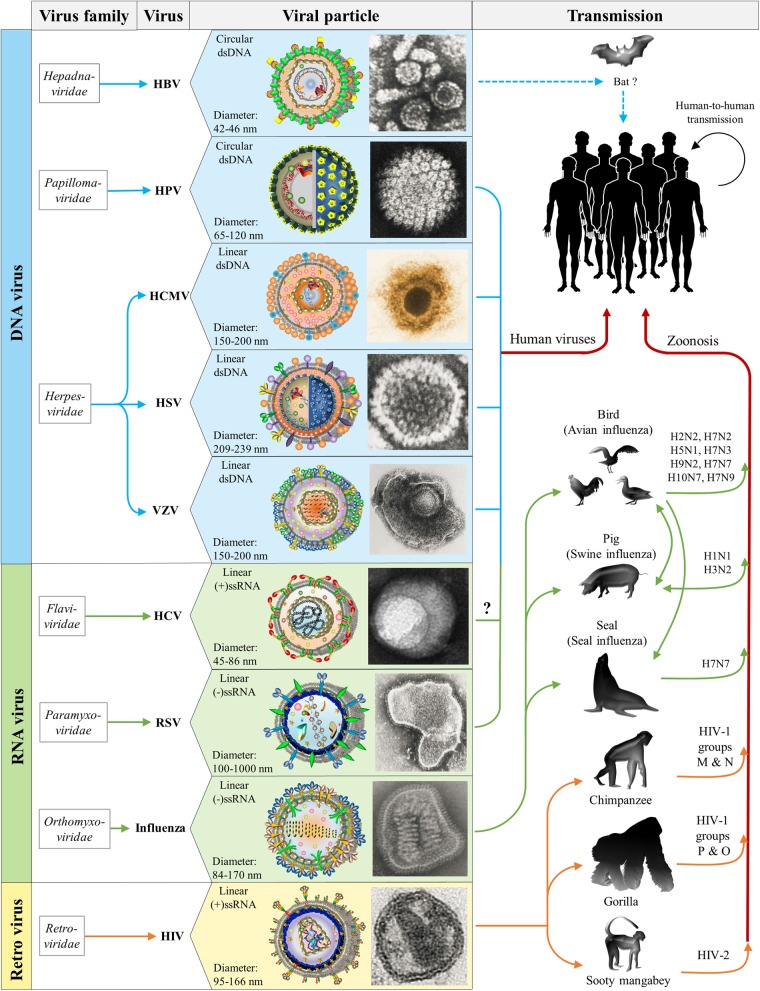
FIG 2.
Virus family, morphology, and transmission of HIV, HBV, HCV, HSV, HCMV, HPV, RSV, VZV, and influenza virus. Nine human viruses are classified into DNA viruses (HBV, HCMV, HSV, HPV, and VZV), RNA viruses (HCV, RSV, and influenza virus), and retroviruses (HIV). These viruses are from 7 families: the Hepadnaviridae (HBV), the Papillomaviridae (HPV), the Herpesviridae (HCMV, HSV, and VZV), the Flaviviridae (HCV), the Paramyxoviridae (RSV), the Orthomyxoviridae (influenza virus), and the Retroviridae (HIV). Schematic views and electron micrograph images of viral particles are illustrated in boxes, where particle sizes measured as diameters and viral genome types (circular/linear dsDNA or linear RNA) are also indicated (Table 1). Human viruses are further characterized with the possible animal reservoirs. HIV is known to be transmitted from chimpanzees (HIV-1 groups M and N), gorillas (HIV-1 groups P and O), or sooty mangabeys (HIV-2) (11, 14, 15). Influenza viruses that infect humans originate mostly from birds, pigs, or seals (36, 401). Although the origin of HBV has yet to be clarified, bats might be a potential reservoir for HBV (47). HPV has been widely found in birds, reptiles, marsupials, and mammals, but cross-transfer between species is rare (54). Four human viruses (RSV [41], HCMV [64], HSV [74], and VZV [80]) circulate only in human populations and do not have any animal reservoir. In addition, it remains unclear whether HCV has any animal reservoir (27, 476). (The HCV electron micrograph image is republished from reference 20 with permission of the publisher. The HPV electron micrograph image was obtained from the Laboratory of Tumor Virus Biology at the National Cancer Institute [https://visualsonline.cancer.gov/]. The electron micrograph images for HBV, HCMV [by Sylvia Whitfield], HSV [by Fred Murphy and Sylvia Whitfield], VZV [by Erskine L. Palmer and B. G. Partin], RSV [by Erskine L. Palmer], influenza virus [by Erskine L. Palmer and M. L. Martin], and HIV [by Maureen Metcalfe and Tom Hodge] were obtained from the Centers for Disease Control and Prevention [http://phil.cdc.gov/phil/home.asp].)
FIG 3.
Antiviral drug groups for the treatment of 9 infectious diseases. Approved antiviral drugs are grouped for RNA viruses (HCV, RSV, and influenza virus), DNA viruses (HCMV, HBV, HPV, HSV, and VZV), and retroviruses (HIV). Names of antiviral drugs that are currently in use are enclosed in orange oblongs. Names of discontinued or abandoned antiviral drugs are enclosed in gray oblongs. Those drugs that inhibit more than one virus are shown in the overlapping regions between virus groups. For HCV drugs, a plus symbol is used to indicate the approved combination drugs (simeprevir plus sofosbuvir, sofosbuvir plus daclatasvir, daclatasvir plus asunaprevir, and ribavirin plus PegIFNα-2b).
FIG 4.
Mechanisms of drug actions during the viral life cycle. Twelve drug groups ordered by roman numerals are shown at the bottom, and their drug actions that interfere with major stages of the viral life cycle are highlighted by red arrows. Solid black arrows indicate direct biological pathways involving viral replication, and dotted black arrows indicate biological pathways with intermediate pathways inside host cells. Major viral stages are illustrated, including endocytosis, exocytosis, virus entry, reverse transcription, virus integration, viral transcription, viral translation, virus budding/release, virus maturation, and other pathways associated with cellular compartments (Golgi apparatus, mitochondria, endoplasmic reticulum [ER], ribosome, proteasome, polysome, and endosome) (for more details, see references 177, 300, and 466). Notably, replication pathways of DNA viruses (HCMV, HBV, HPV, HSV, and VZV), RNA viruses (HCV, RSV, and influenza virus), and retroviruses (HIV) diverge after entering host cells. The RNA viruses replicate in the cytoplasm, but DNA viruses and retroviruses further intrude into the nucleus for their DNA synthesis. Note that drug group XIII is not displayed because drugs in this group act mainly as immunoregulatory or antimitotic agents, and they do not directly target viral proteins. Shapes and sizes of proteins and cellular components are not to scale.
In this review, we first give an overview of 9 human viruses. Subsequently, the following three perspectives of 90 approved drugs are discussed. (i) How were they discovered, and against which viral infections are they active? (ii) How do they achieve their mechanisms of action to target viral or host proteins? (iii) What therapeutic aspects do they have? In addition, we make a summary of promising antiviral compounds in phase 3 clinical trials (Table 3). To give a comprehensive overview, we highlight the latest progress on antiviral drugs and vaccines against emerging infectious diseases. Challenges in the field of antiviral drug discovery are envisioned at the end. To support this review, we have also established an online platform (http://www.virusface.com/) to update the therapeutic aspects of antiviral drugs and vaccines.
TABLE 3.
Summary of forthcoming antiviral treatments in phase 3 trials
| Antiviral drug | Viral infection | % efficacya | Mechanism(s) of action | Study progressb |
|---|---|---|---|---|
| Sofosbuvir + velpatasvir | HCV genotypes 1–6 | 97.4 | Inhibit activities of HCV NS5B polymerase and NS5A, respectively | Phase 3, completed |
| Daclatasvir + asunaprevir | HCV genotype 1 | 86.4 | Daclatasvir, asunaprevir, and beclabuvir inhibit activities of NS5A, NS3/4A protease, and NS5B, respectively | Phase 4, ongoing |
| Daclatasvir + asunaprevir + beclabuvir | HCV genotype 1 | 91.5 | Phase 3, ongoing | |
| FV100 | VZV | 87.6 | Inhibits activity of the VZV DNA polymerasec | Phase 3, ongoing |
| Letermovir | HCMV | 71 | Targets the pUL56 subunit of the HCMV terminase complex to block viral DNA processing and/or packagingd | Phase 3, ongoing |
For HCV inhibitors, drug efficacy is measured by the SVR12 (see the text). For the VZV inhibitor FV100, drug efficacy is measured by the incidence of patients without postherpetic neuralgia after treatment at 90 days. For the HCMV inhibitor letermovir, drug efficacy is measured by the incidence of successful prophylaxis after treatment at 12 weeks (392).
Clinical data were extracted from ClinicalTrials.gov (see https://www.clinicaltrials.gov/) in April 2016.
See reference 385.
OVERVIEW OF NINE HUMAN VIRUSES
As of April 2016, antiviral drugs have been approved to treat 9 human infectious diseases (HIV, HBV, HCV, HCMV, HSV, HPV, RSV, VZV, and influenza virus), albeit more than 200 human viruses have been discovered (6). Below, we give an overview of the origins, pathogenicities, epidemiologies, and clinical complications of these 9 human viruses.
Human Immunodeficiency Virus
Discovered in 1983 (7), HIV, a lentivirus in the Retroviridae family, is the causative agent of AIDS (8). An HIV particle, which is ∼145 nm (range, 95 to 166 nm) in diameter (9), contains a linear single-stranded RNA (ssRNA) genome encoding 15 mature viral proteins (10) (Table 1). HIV strains can be classified into two types (HIV-1 and HIV-2), which are further divided into extensive groups, subtypes, and recombinant forms (for a review, see reference 11). A high level of genetic variation has been observed in the HIV genome, making HIV one of the fastest-evolving organisms (12). It has been estimated that the nucleotide diversity of HIV genomes is almost 50% between HIV-1 and HIV-2, 37.5% between HIV-1 groups, and 14.7% between HIV-1 subtypes (10). Regarding the origin of HIV, it can be traced to West Central Africa in the late 19th or the early 20th century, when the butchering and consumption of primate bushmeat were widely practiced (11, 13). Due to multiple zoonotic transfers, HIV is known to be transmitted from chimpanzees (HIV-1 groups M and N), gorillas (HIV-1 groups P and O), and sooty mangabeys (HIV-2) to humans (11, 14–16) (Fig. 2). As a blood-borne virus, HIV is spread mainly through HIV-contaminated blood or body fluids; thereby, patients can become infected with HIV by sexual contact, needle sharing, blood transfusions, or maternal transmissions. During chronic infection, the incubation period of HIV can be 8 to 11 years (17). Many clinical complications have been reported: lymphoma, psychiatric disorders, gingivitis, cardiovascular disease, lung cancer, kidney disease, osteoporosis, papulosquamous disorders, and dental or salivary gland diseases (for a review, see reference 18). In the past 3 decades, HIV has caused a great burden to global wealth and health. According to the WHO global health survey, ∼36.9 million (range, 34.3 million to 41.4 million) people were infected with HIV, causing 1.2 million (range, 1.0 million to 1.5 million) deaths in 2014.
Hepatitis C Virus
Discovered in 1989 (19), HCV is a hepacivirus in the Flaviviridae family (Fig. 2). An HCV particle, which is ∼68 nm (range, 45 to 86 nm) in diameter (20), contains a linear, positive-sense, single-stranded RNA genome encoding 10 viral proteins (21). HCV strains can be classified into 7 major genotypes (genotypes 1 to 7), among which genotypes 1 and 2 cause most infections worldwide (22). It has been estimated that the nucleotide diversity of HCV genomes is about 32.4% between HCV genotypes and 14.6% within HCV genotypes (23). Regarding the origin of HCV, it remains a mystery, but nonhuman primates (apes and monkeys) and mammals (e.g., horses and dogs) might have been potential zoonotic reservoirs (24). As a blood-borne virus, HCV is transmitted mainly by sexual contact, needle sharing, blood transfusions, or maternal transmissions. During acute infection, the incubation period of HCV is ∼7 weeks (range, 4 to 20 weeks) (25). Many clinical complications have been observed, including liver cirrhosis, liver failure, portal hypertension, or hepatocellular carcinoma (26, 27). HCV is also known to cause liver cancers such as hepatocellular carcinoma (28). According to the WHO global health survey, HCV causes 500,000 deaths every year, and 130 million to 150 million people were living with HCV in 2014.
Influenza Virus
Human influenza viruses from the Orthomyxoviridae family (Fig. 2) caused the first recognizable influenza pandemic in the summer of 1510 (29, 30), and they were isolated for the first time in 1933 (31). A viral particle of influenza virus, which is ∼120 nm (range, 84 to 170 nm) in diameter (32), contains a linear, negative-sense, single-stranded RNA genome that encodes 11 or 12 proteins depending on the virus strain (33). Influenza viruses can be classified into three types: types A, B, and C. Influenza A viruses that cause human epidemics and pandemics (e.g., Spanish flu in 1918, Asian flu in 1957, and Hong Kong flu in 1968) are further divided into extensive subtypes (i.e., H1N1, H1N2, or H3N2) based on the sequence variation of hemagglutinin (HA) and neuraminidase (NA), two glycoproteins of the influenza virus membrane (34, 35). Influenza B viruses that cause human epidemics are divided into strains but not subtypes. Influenza C viruses cause neither epidemics nor pandemics, because they usually infect humans with mild illnesses. On the other hand, influenza viruses have been discovered in a broad spectrum of animal reservoirs (36). Influenza A viruses can be transmitted from animal reservoirs such as birds (e.g., H2N2, H5N1, H7N3, and H9N2), pigs (e.g., H1N1 and H3N2), or seals (H7N7) to humans (36). Using respiratory routes, influenza viruses spread mostly through direct contact with contaminated aerosols or droplets. During influenza infection, the typical incubation period is ∼1 to 4 days (average, 2 days), and many clinical complications (e.g., pneumonia, bronchitis, dehydration, encephalitis, sinusitis, and ear infections) have been reported (see http://www.cdc.gov/). According to the WHO global health survey, influenza viruses cause 250,000 to 500,000 deaths every year, and 3 million to 5 million cases of severe illnesses were reported in 2014.
Respiratory Syncytial Virus
Discovered in 1957 (37), human RSV belongs to the Pneumovirus genus in the Paramyxoviridae family (Fig. 2). An RSV particle, which is ∼100 to 1,000 nm in diameter (38), contains a linear, negative-sense, single-stranded RNA genome encoding 11 viral proteins (39). RSV strains can be classified into two antigenic subtypes, subtypes A and B, which are further divided into 11 RSV-A and 23 RSV-B genotypes (40). Similar to influenza viruses, RSV takes respiratory routes for its transmission, mainly by direct contact with contaminated aerosols or droplets. Nevertheless, there is no animal reservoir for human RSV (41). During human RSV infection, the incubation period is ∼5 days (range, 3 to 8 days) (42), and many clinical complications (e.g., respiratory tract diseases, sinusitis, otitis bronchiolitis, and pneumonia) have been observed (see http://www.cdc.gov/). Regarding the burden of RSV, it causes 66,000 to 199,000 deaths every year. In 2005, RSV infections caused 33.8 million cases of RSV-associated acute lower respiratory infections among children <5 years of age (43).
Hepatitis B Virus
Discovered in 1963 (44), HBV belongs to the Orthohepadnavirus genus in the Hepadnaviridae family (Fig. 2). An HBV particle, which is ∼42 to 46 nm in diameter (45), contains a circular double-stranded DNA (dsDNA) genome encoding 6 viral proteins. HBV strains have been classified into 8 genotypes, further divided into more than 24 subtypes. It has been estimated that the nucleotide diversity of HBV genomes is ∼14.5% between HBV genotypes and 2.8% within HBV genotypes (46). Regarding the origin of HBV, it remains a mystery to be unveiled, but bats might have been the ancestral sources of primate hepadnaviruses (47, 48). As a blood-borne virus, HBV can be transmitted by sexual contact, needle sharing, blood transfusions, or maternal transmissions. The incubation period of HBV infections is ∼90 days (range, 60 to 150 days) (49). Major clinical complications of HBV infections have been observed, such as hepatitis, anorexia, abdominal discomfort, nausea, vomiting, arthralgia, rash, or liver cancer (see http://www.cdc.gov/). HBV is also known to cause liver cancers (e.g., hepatocellular carcinoma) (28). According to the WHO global health survey, HBV causes 780,000 deaths every year, and 240 million people were infected in 2014.
Human Papillomavirus
Discovered in 1965 (50), HPVs from the Papillomaviridae family are the causative agents of >90% of cervical cancers, the second most common cancer among women worldwide (51). An HPV particle, which is ∼65 to 120 nm in diameter (52), contains a closed, circular, double-stranded DNA genome encoding 9 viral proteins (53). HPV strains can be classified into >200 types based on the sequence variation of a late region encoding the capsid protein L1 (54). HPV infections are responsible for ∼5% of human cancers (e.g., cervical carcinoma, anal carcinoma, and penile carcinoma) (28, 55). Particularly, high-risk HPV type 16 (HPV-16) and HPV-18 are known to cause 70% of cervical cancers, while low-risk HPV-6 and HPV-11 cause 90% of external genital warts (56) as well as most cases of recurrent respiratory papillomatosis (57). Papillomaviruses have been widely found in birds, reptiles, marsupials, and mammals, but cross-transfer between species is rare (54). The incubation period from HPV infection to clinical warts varies, and the average time is ∼2.9 months (range, 0.5 to 8 months) (58). HPV infections are transmitted mainly through intimate skin-to-skin contact. Regarding epidemiology, the worldwide prevalence of HPV in women without cervical abnormalities is ∼11% to 12% (59), and HPV is responsible for cervical cancers, causing 266,000 deaths and 528,000 new cases in 2012 (see http://www.who.int/).
Human Cytomegalovirus
Discovered in 1956 (60), HCMV belongs to the Cytomegalovirus genus in the Herpesviridae family (Fig. 2). An HCMV particle, which is ∼150 to 200 nm in diameter (61), contains a linear double-stranded DNA genome harboring ∼200 to 250 open reading frames (62). HCMV strains can be classified into four genotypes (gB1, gB2, gB3, and gB4) based on the sequence variation of the UL55 gene encoding glycoprotein B (gB) (63). In the absence of any animal reservoir, HCMV circulates exclusively in human populations (64). As a blood-borne virus, HCMV can be transmitted through blood transfusions, body fluids, breastfeeding, organ transplants, or sexual contact. Notably, the incubation period of HCMV infections is ∼3 to 12 weeks. During HCMV infections, many clinical complications have been observed, such as gastrointestinal diseases, mononucleosis, carditis, colitis, antigenemia, ependymitis, esophagitis, encephalitis, retinitis, hepatitis, nephritis, pancreatitis, pneumonia, allograft infections, or central nervous system diseases (65, 66). Moreover, HCMV infections are associated with high morbidity and mortality rates in solid-organ transplant and hematopoietic stem cell transplant recipients (67, 68). Regarding epidemiology, the seroprevalence of HCMV in worldwide populations is between 30% and 95% (69), the percentage of symptomatic children with permanent sequelae is ∼40% to 58% (70), and the prevalence of congenital HCMV at birth is estimated to be 0.64% (range, 0.60 to 0.69%) (71).
Herpes Simplex Virus
Discovered before 1900 (72), HSV belongs to the Simplexvirus genus in the Herpesviridae family (Fig. 2). An HSV particle, which is ∼225 nm (range, 209 to 239 nm) in diameter (61), contains a linear double-stranded DNA genome carrying 84 genes (73). HSV can be classified into two types: HSV-1 and HSV-2. The former leads to the majority of cases of oral herpes infections that cause skin lesions and cold sores. The latter is mainly responsible for genital herpes infections that cause pain during urination and blistering sores. In the absence of any animal reservoir, HSV circulates exclusively in human populations (74). HSV-1 transmissions are mediated by direct exposure to contaminated aerosols or droplets, such as oral-to-oral and skin-to-skin contacts. HSV-2 is transmitted mainly by direct exposure to genital skin or fluids of HSV-infected patients. During viral infections, the incubation period of HSV-1 or HSV-2 is ∼4 days (range, 2 to 12 days) (75). HSV-1 usually causes pneumonia, keratitis, encephalitis, or orofacial blisters, while HSV-2 typically causes meningitis or genital lesions (74). According to the WHO global health survey, in 2012, 140 million and 417 million people between 15 and 49 years of age lived with HSV-1 and HSV-2, respectively.
Varicella-Zoster Virus
Isolated in tissue culture for the first time in 1953 (76), VZV belongs to the Varicellovirus genus in the Herpesviridae family (Fig. 2). A VZV particle, which is ∼150 to 200 nm in diameter (77), contains a linear double-stranded DNA genome carrying 73 genes (78). VZV strains can be classified into five clades, clades 1 to 5, which are further divided into 9 genotypes (78, 79). In the absence of any animal reservoir, VZV circulates exclusively in human populations (80). VZV is transmitted mostly by respiratory routes, such as by direct contact with respiratory tract secretions (e.g., aerosols and droplets) or lesions. VZV infections, whose incubation period is ∼10 to 21 days (81), are known to cause chickenpox as well as a painful skin rash called shingles or herpes zoster (82). Many clinical complications of herpes zoster in immunocompetent humans have been reported, including pneumonia, cellulitis, neuralgia, encephalitis, myelitis, cranial nerve palsies, or peripheral nerve palsies (83). It has been estimated that 30% of humans have been infected with herpes zoster over their lifetime (83), and the seroprevalence of immunoglobulin G (IgG) antibody to varicella-zoster virus is >86% in children and adults (84). In the United States, VZV infections give rise to 1 million cases or more each year (83, 85).
The nine human viruses described above have caused devastating infectious diseases that afflict millions of humans worldwide (Table 1), therefore calling for the urgent development of effective antiviral drugs. The following sections focus on the molecular and therapeutic aspects of approved antiviral drugs against these 9 human viruses.
5-SUBSTITUTED 2′-DEOXYURIDINE ANALOGUES
Three antiviral drugs (idoxuridine, trifluridine, and brivudine [BVDU]) have been approved in the drug group of 5-substituted 2′-deoxyuridine analogues (Table 2). Historically, the era of antiviral chemotherapies started in 1959 with the description of idoxuridine (5-iodo-2′-deoxyuridine) by William H. Prusoff (86). Although idoxuridine was originally described as a potential antitumor agent, it would later become the first antiviral drug to be used (and it still is) clinically for the topical treatment of herpetic eye infection (i.e., keratitis due to HSV). Herrmann was the first to report the antiviral activity of idoxuridine against HSV and vaccinia virus in 1961 (87). Herrmann was also the first to propose the use of idoxuridine against HSV keratitis in rabbits (88) and humans (89). Thereafter, Kaufman and Heidelberger described the effectiveness of trifluridine (5-trifluoromethyl-2′-deoxythymidine) against HSV infections (90). Idoxuridine and trifluridine are now used for the topical treatment (such as in eye drops or eye ointment) of HSV epithelial keratitis (91).
Idoxuridine and trifluridine alone cannot be considered specific antiviral agents, for they must be phosphorylated by cellular kinases to either the 5′-triphosphate (TP) form (i.e., idoxuridine) or the 5′-monophosphate form (i.e., trifluridine), both of which actively inhibit viral and cellular DNA synthesis (3) (Fig. 5). As an analogue of the nucleoside thymidine, brivudine [(E)-5-(2-bromovinyl)-2′-deoxyuridine] is highly specific in its activity against HSV-1 and VZV (92, 93). Moreover, brivudine is superior to either idoxuridine, trifluridine, or acyclovir in cell culture experiments (94). To achieve its inhibitory activity, brivudine is specifically phosphorylated by the thymidine kinases of HSV-1 and VZV, which convert brivudine to its 5′-mono- and 5′-diphosphate forms. The cellular nucleoside 5′-diphosphate kinases further phosphorylate the 5′-mono- and 5′-diphosphates of brivudine into the 5′-triphosphate of brivudine, which targets the viral DNA polymerase for the inhibition of viral DNA synthesis (92).
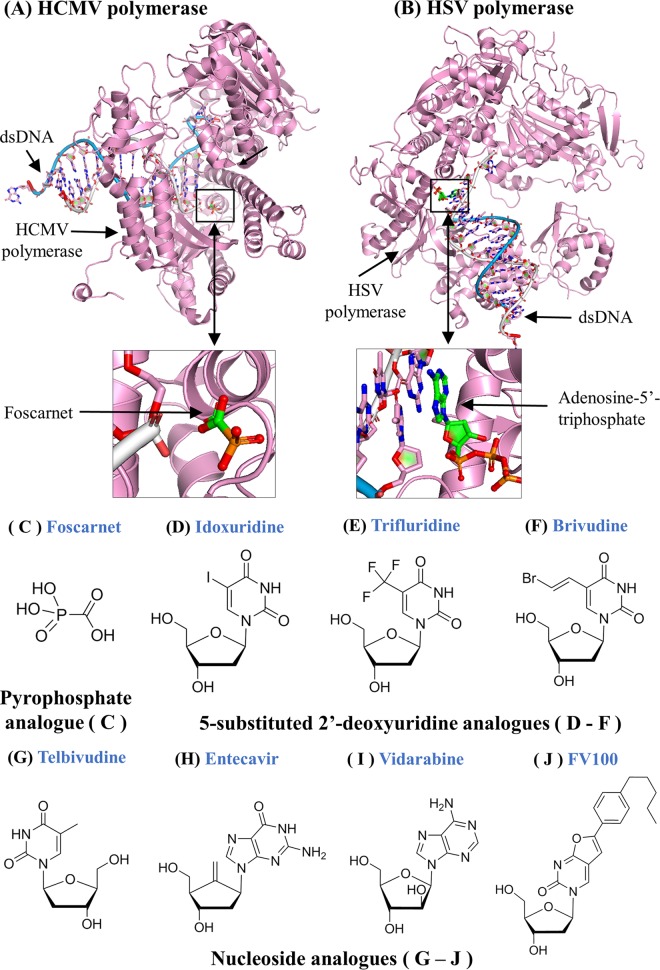
FIG 5.
HCMV and HSV-1 DNA polymerase structures and chemical formulas of pyrophosphate analogues, 5-substituted 2′-deoxyuridine analogues, and nucleoside analogues. (A) Tertiary structures of HCMV DNA polymerase in complex with dsDNA and foscarnet (PDB accession number 3KD5). HCMV DNA polymerase is shown in pink. The dsDNA is placed in the center, where foscarnet inhibits DNA synthesis at the active site of HCMV DNA polymerase. Structural movies that demonstrate drug binding are available online (see http://www.virusface.com/). PyMOL V1.7 visualization software (http://www.pymol.org/) was used. (B) Tertiary structures of HSV-1 DNA polymerase complexed with dsDNA and ATP (PDB accession numbers 2GV9 and 4M3R). HSV-1 DNA polymerase is shown in pink. ATP near the catalytic site is displayed in the drug-binding pocket. The triphosphate form of approved antiviral inhibitors (e.g., vidarabine triphosphate) can compete with dATP to inhibit the replication activity of HSV DNA polymerase. (C) Chemical formula of foscarnet in the group of pyrophosphate analogues. (D to F) Chemical formulas of idoxuridine, trifluridine, and brivudine in the group of 5-substituted 2′-deoxyuridine analogues. (G to J) Chemical formulas of telbivudine, entecavir, vidarabine, and FV100 in the group of nucleoside analogues. Note that FV100 is an experimental inhibitor in phase 3 clinical trials.
BVDU has been approved in many countries all over the world (except for the United States and the United Kingdom) for the oral treatment of VZV infections, i.e., herpes zoster (shingles), for which it is prescribed at a dosage of 125 mg per day (for 7 days). Moreover, brivudine is used as eye drops for the treatment of HSV-1 epithelial keratitis. A systematic review, which collected data from 106 comparative treatment trials enrolling 5,872 cases with HSV infections, demonstrated that treatment with brivudine at 14 days was at least as effective as acyclovir and ganciclovir, two acyclic guanosine analogues (91). Ophthalmic preparations of brivudine, trifluridine, acyclovir, and ganciclovir are equally effective, allowing ∼90% of treated eyes to recover within 2 weeks (91). Unlike idoxuridine and trifluridine, which cause high toxicity, brivudine has a favorable safety profile and can be administered systemically to treat HSV-1 and VZV (93). Moreover, brivudine might be used to treat Epstein-Barr virus (EBV) encephalitis (95, 96), but this new application has yet to be proven in clinical trials.
NUCLEOSIDE ANALOGUES
The drug group of nucleoside analogues includes three FDA-approved drugs: vidarabine, entecavir (ETV), and telbivudine (Table 2). Historically, arabinosyl nucleoside analogues were first isolated from sponges (97). Before Schabel (98) documented its antiviral potential, arabinosyladenine was first considered to be a potential anticancer agent (99). With high potency against HSV and VZV (e.g., herpes zoster) infections, vidarabine, which targets viral DNA polymerases (Fig. 5), was the first of the FDA-approved nucleoside analogues to be administered systemically in clinics (100, 101). However, vidarabine is barely soluble in aqueous medium, and it is rapidly deaminated by adenosine deaminases to its inosine counterpart (ara-Hx [arabinosylhypoxanthine]). Since June 2001, vidarabine has been discontinued in the United States, probably for commercial reasons (102).
For the treatment of HBV infections, the following compounds have been licensed: (pegylated) interferons, lamivudine, entecavir, telbivudine, adefovir dipivoxil, and tenofovir disoproxil fumarate (TDF) (Table 2). Lamivudine and TDF have also been licensed for the treatment of HIV infections and are further discussed below. Two nucleoside analogues, entecavir and telbivudine, are exclusively used for the treatment of HBV infections (Fig. 5). In patients with either HBeAg-positive (HBeAg+) chronic hepatitis B (103) or HBeAg-negative chronic hepatitis B (104), the rates of histological, virological, and biochemical improvements were significantly higher with entecavir than with lamivudine. More importantly, long-term monitoring of nucleoside-naive patients receiving 5 years of entecavir therapy showed a low rate of HBV resistance to entecavir (105). However, it came as a surprise when entecavir was reported to inhibit HIV-1 infections with only modest activity (106, 107), because this might generate HIV-1 resistance to entecavir in patients coinfected with HIV-1 and HBV. The “take-home” message was not to use entecavir in such patients (107).
Several phase 2 or 3 clinical trials compared the potencies and safeties of telbivudine versus lamivudine, and their findings suggested that telbivudine offered greater HBV DNA suppression with less resistance than did lamivudine (108–110). For instance, a randomized, double-blind, phase 3 trial that enrolled 1,367 patients infected with chronic HBV suggested that telbivudine was superior to lamivudine in terms of higher rates of undetectable viremia and less resistance (111). For treatment of HBeAg+ mothers during late pregnancy, telbivudine was well tolerated, with no severe side effects in telbivudine-treated mothers or their infants (112). Although entecavir is superior to telbivudine in safety, both telbivudine and entecavir offer similar drug efficacies in terms of the cumulative rates of undetectable HBV DNA and alanine aminotransferase levels (113). For first-line therapy of HBV infections, the use of entecavir is strongly recommended, especially in children aged 2 to 12 years (114). Nevertheless, telbivudine, lamivudine, and adefovir dipivoxil are not recommended because they have a low barrier to resistance (114).
Overall, orally administered nucleos(t)ide analogues, with their safety, easy use, and low drug resistance rates, are preferable for HBV treatments, but the high costs of these drugs remain a great concern in resource-limited areas. Therefore, lamivudine is commonly used in first-line therapy regardless of its high rate of drug resistance (115).
PYROPHOSPHATE ANALOGUES
Trisodium phosphonoformate, known as foscarnet (Fig. 5), was discovered as a new antiviral compound in 1978 (116). Although it is the only approved inhibitor in this drug group, foscarnet was not the first pyrophosphate analogue, as it had been preceded by phosphonoacetic acid (117). The novelty of foscarnet and phosphonoacetic acid depends on the fact that these compounds are unlike other classical antiviral agents (i.e., BVDU and acyclovir), because they do not have to be phosphorylated (i.e., metabolized to their active metabolite) before their binding to drug targets (i.e., viral DNA polymerases) (118). Therefore, foscarnet could be selected directly at the enzyme level (116).
In a comprehensive review, Bo Öberg (119) ascertained that foscarnet achieved its broad-spectrum activity against HSV-1, HSV-2, VZV, HCMV, EBV, HIV, and HBV by targeting viral DNA polymerases (Fig. 5). However, foscarnet neither showed inhibitory activities against viral RNA polymerases nor inhibited the replication of RNA viruses (except for retroviruses) (119). Despite its inhibitory activity, specifically confined to DNA viruses and retroviruses, foscarnet acts in a unique fashion because it binds directly, as a pyrophosphate analogue, to viral DNA polymerases (Fig. 5). Foscarnet is unlike nucleos(t)ide analogues that must be phosphorylated to their triphosphate (nucleoside) or diphosphate (nucleotide) forms before their binding to viral DNA polymerase (Fig. 5).
Foscarnet is used exclusively in the treatment of HCMVs or HSVs that have become resistant to the classical nucleoside analogues such as acyclovir. As shown in some case reports, the effectiveness of foscarnet has been demonstrated in the treatment of infection by thymidine kinase-deficient HSV strains with resistance to acyclovir (120–122). Clinical evidence also suggests that foscarnet-based treatments efficiently improve the clinical outcomes of HIV-infected patients with HSV infections (123). For the treatment of HCMV infections, foscarnet-based regimens may eradicate viremia rapidly, yet their efficacy is limited because of a high level of toxicity in the long term (124). Common side effects with foscarnet are nausea, diarrhea, vomiting, headache, renal impairment, or ionized hypocalcemia (125, 126).
In addition to its antiviral activity against HCMV and HSV infections, foscarnet is effective against human herpesvirus 6 (HHV-6), a widespread betaherpesvirus genetically related to HCMV (127). Despite its promising activity against HHV-6, foscarnet has not been approved to treat HHV-6. Therefore, further clinical trials will still be required to prove this potential in the future.
NUCLEOSIDE REVERSE TRANSCRIPTASE INHIBITORS
Soon after its discovery as an anti-HIV agent in 1985 (128), zidovudine (AZT [azidothymidine]) was licensed for clinical use in 1987. Zidovudine is not only the first drug approved for HIV treatment but also the first drug in the group of NRTIs, which target HIV reverse transcriptase to interfere with viral reverse transcription (Fig. 6). Inspired by the success of zidovudine, 6 drugs in the group of NRTIs (Fig. 6) were subsequently approved to treat HIV or HBV infections: (i) didanosine (ddI [2′,3′-dideoxyinosine]) (129), (ii) zalcitabine (ddC [2′,3′-dideoxycytidine]) (129), (iii) stavudine (d4T [2′,3′-didehydro-3′-deoxythymidine]) (130–132), (iv) lamivudine (3TC [2′,3′-dideoxy-3′-thiacytidine]) (133), (v) abacavir (ABC) [(1S,4R)-4-(2-amino-6-(cyclopropylamino)-9H-purin-9-yl)-2-cyclopentene-1-methanol] (134), and (vi) emtricitabine [(−)FTC (2′,3′-dideoxy-5-fluoro-3′-thiacytidine), where “(−)” indicates the l-enantiomeric form] (135).
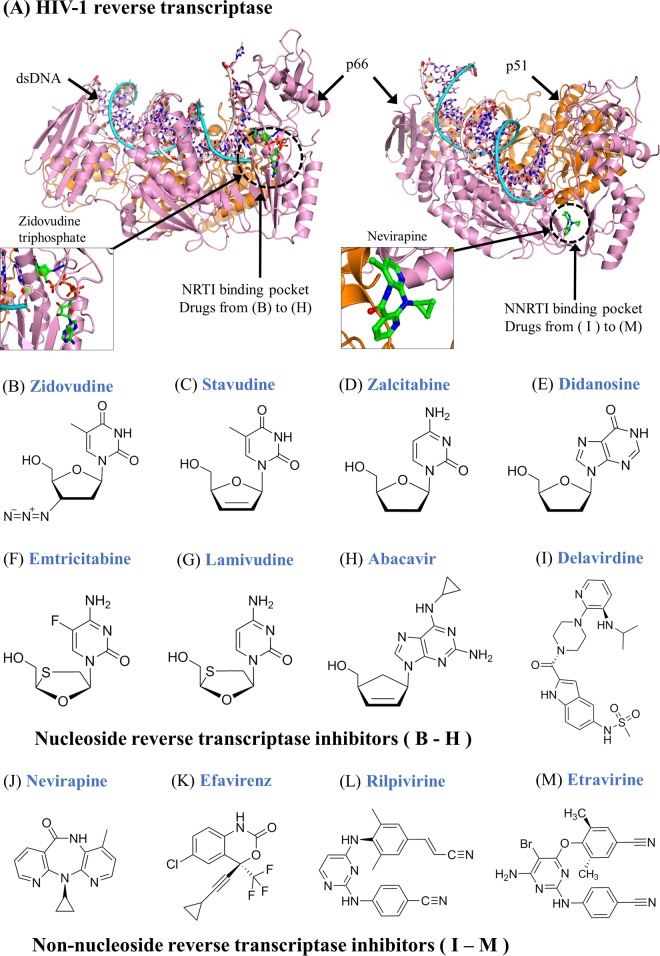
FIG 6.
Tertiary structures of HIV-1 reverse transcriptase and chemical formulas of NRTIs and NNRTIs. (A) HIV-1 RT complexed with dsDNA and zidovudine triphosphate (left) (PDB accession number 3V4I) and nevirapine (right) (PDB accession number 4PUO). Two subunits of the HIV-1 RT heterodimer are shown in pink and orange, respectively. Zidovudine triphosphate targets the drug-binding pocket of NRTIs, known as the catalytic site, to inhibit the activity of HIV-1 RT during DNA synthesis. Nevirapine targets the drug-binding pocket of NNRTIs, known as the allosteric site, to block the activity of HIV-1 RT during DNA synthesis (see structural movies at http://www.virusface.com/). (B to H) Chemical formulas of zidovudine, stavudine, zalcitabine, emtricitabine, didanosine, lamivudine, and abacavir in the group of NRTIs. (I to M) Chemical formulas of delavirdine, nevirapine, efavirenz, rilpivirine, and etravirine in the group of NNRTIs.
All NRTI compounds are known as 2′,3′-dideoxynucleoside analogues, with similar mechanisms of drug action. After their phosphorylation to the 5′-TP, NRTIs act as chain terminators, a mechanism of drug action originally shown for AZT (136), with (i) AZT-TP in competition with dTTP (137), (ii) ddATP (formed from ddI) in competition with dATP, (iii) ddCTP (formed from ddC) in competition with dCTP, (iv) d4T-TP (formed from d4T) in competition with dTTP, (v) 3TC-TP (formed from 3TC) in competition with dCTP, (vi) carbovir-TP (formed from ABC) in competition with dGTP, and (vii) (−)FTC-TP [formed from (−)FTC] in competition with dCTP (4) (Fig. 6).
NRTIs alone are not administered in HIV treatments because NRTIs usually have a low genetic barrier to the development of drug resistance mutations, which have been characterized by the International Antiviral Society-USA (IAS-USA) panel (138) and the HIV drug resistance database (http://hivdb.stanford.edu/). NRTIs are commonly administered with other drugs in highly active antiretroviral therapy (HAART) to target multiple stages of the HIV life cycle (139, 140). In particular, both lamivudine and emtricitabine are backbones in 9 approved combination drugs (Table 2): (i) lamivudine plus zidovudine (Combivir); (ii) lamivudine plus zidovudine and ABC (Trizivir); (iii) lamivudine plus the integrase inhibitor dolutegravir (Dutrebis); (iv) lamivudine plus dolutegravir and abacavir (Triumeq); (iii) emtricitabine plus TDF (Truvada); (iv) emtricitabine plus TDF and efavirenz (Atripla); (v) emtricitabine plus TDF and the NNRTI rilpivirine (Complera or Eviplera); (vi) emtricitabine plus TDF, the integrase inhibitor elvitegravir, and cobicistat (Stribild); (vii) emtricitabine plus tenofovir alafenamide (TAF), elvitegravir, and cobicistat (Genvoya); (viii) emtricitabine plus TAF and rilpivirine (Odefsey); and (ix) emtricitabine plus TAF (Descovy). Although the pharmacological equivalence and clinical interchangeability of lamivudine and emtricitabine remain debated (141, 142), both drugs are key components of approved combination drugs.
In clinical practice, the most common side effects with NRTIs are reversible peripheral neuropathy, nausea, headache, rash, anemia, leukopenia, pancreatitis, gout, or hypersensitivity (143). It is also worth mentioning that because of its neurotoxicity, the FDA-approved agent zalcitabine has been discontinued since December 2006. As of today, NRTI drugs, patented mostly before 2003, are over their expiration dates for patents (144). Patent expiration thus stimulates broad marketing worldwide, making NRTIs popular first-line agents against HIV infections in resource-limited areas.
NONNUCLEOSIDE REVERSE TRANSCRIPTASE INHIBITORS
Discovered in the late 1980s, the group of NNRTIs includes five approved anti-HIV drugs: nevirapine, delavirdine, efavirenz, etravirine, and rilpivirine (Table 2). Historically, NNRTIs originated from two classes of compounds discovered independently from each other: 1-[(2-hydroxy-ethoxy)methyl]-6-phenylthiothymine (HEPT) analogues (145, 146) and tetrahydro-imidazo[4,5,1-jk][1,4]-benzodiazepine-2(1H)-one and -thione (TIBO) analogues (147). To inhibit viral replication, HEPT and TIBO derivatives target HIV-1 reverse transcriptase (148–150). Emivirine (MKC-442), derived from the HEPT derivatives (151), had reached phase 3 clinical trials before its further development was stopped (152). TIBO derivatives led through a highly meandrous route to the identification of diarylpyrimidine (DAPY) derivatives (153), including dapivirine, etravirine, and rilpivirine (154). Approved by the FDA, etravirine (Intelence) and rilpivirine (Edurant), accompanied by three other NNRTIs (delavirdine, efavirenz, and nevirapine), are now on the market. Delavirdine is currently rarely used due to its high toxicity, relatively low potency, and complex drug interactions (155).
Unlike NRTIs, NNRTIs do not need any metabolic processing to inhibit HIV reverse transcription (Fig. 6). Instead, they serve as noncompetitive inhibitors that target the allosteric site of HIV-1 RT, situated a short distance (∼15 Å) from the RT catalytic site (156–158). This binding induces conformation changes to impair the catalytic activity of HIV-1 RT, thus interrupting viral replication (159). Importantly, NNRTIs act specifically against HIV-1, whereas HIV-2 is naturally resistant to all NNRTIs due to its structural properties (160). When RT structures of HIV-1 and HIV-2 were compared, differences were found at both conserved and nonconserved positions (K101, V106, E138, Y181, Y188, and G190) in the drug-binding pocket of NNRTIs (161). In addition to the above-mentioned positions, drug resistance mutations at other RT positions (V90, A98, L100, K103, V108, V179, H221, P225, F227, and M230) may also cause treatment failure of NNRTIs (138).
In clinical practice, NNRTIs are widely used as first-line agents. They can be combined with tenofovir disoproxil fumarate, (−)FTC, and rilpivirine to afford a once-daily pill, Complera (United States) or Eviplera (European Union), for all-inclusive treatments of HIV infections (153). The most common side effects with NNRTIs are rash, central nervous system toxicity, or elevation of liver enzyme levels (143). Promising NNRTIs such as doravirine (MK-1439) (162–164) and diarylpyrimidine (165) are under investigation in clinical trials.
PROTEASE INHIBITORS
In the group of protease inhibitors (PIs), 12 HIV protease compounds and 7 HCV NS3/4A protease compounds have been approved for clinical use (Table 2). HIV and HCV protease inhibitors are described below.
HIV Protease Inhibitors
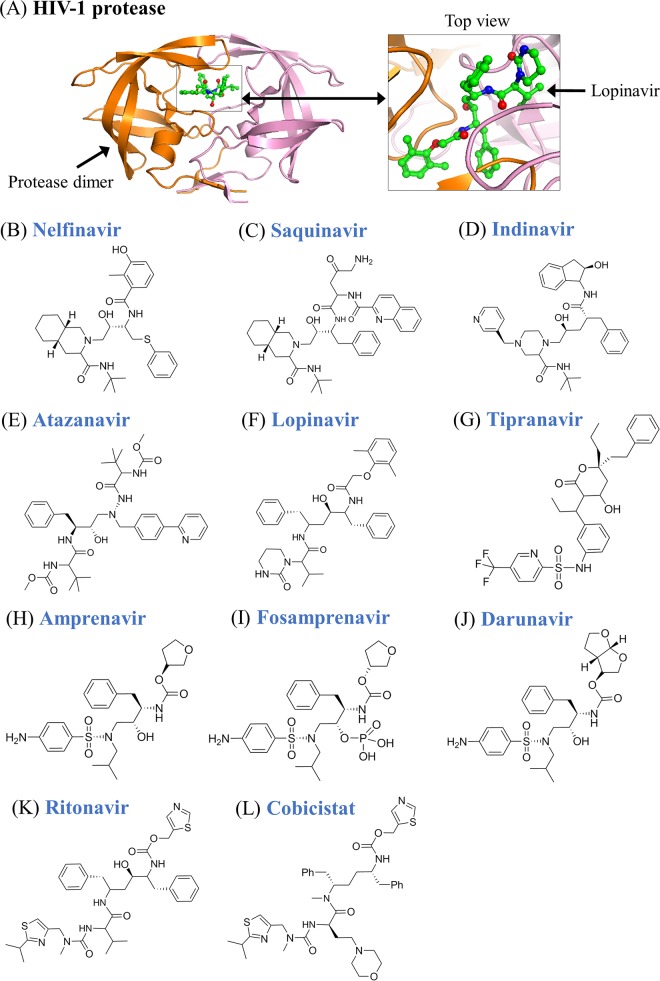
Historically, HIV-1 protease (Fig. 7) was first proposed as a potential target for AIDS therapy by Kramer et al. (166), when they showed that a frameshift mutation in the protease region of the pol gene prevented protease-mediated cleavage of gag precursor proteins (167). The transition state mimetic concept later inspired Roberts and coworkers to describe the rational design of peptide-based protease inhibitors (167). In 1995, saquinavir was approved as the first protease inhibitor, marking the beginning of an era for this new class of anti-HIV inhibitors. In fact, not only saquinavir but also 9 out of the 10 approved HIV protease inhibitors are based on the same principle, in which the hydroxyethylene bond acts as the peptidomimetic scaffold, including saquinavir, ritonavir, indinavir, nelfinavir, amprenavir, lopinavir, atazanavir, fosamprenavir, and darunavir (Fig. 7). The only exception is tipranavir, which is built on the coumarin scaffold (168). When protease inhibitors compete with natural substrates of HIV protease as the peptidomimetic scaffold (169), amino acid variations near this scaffold and within the cleavage sites of protease substrates (i.e., Gag and Gag-Pol) may have been selected during virus evolution to cause resistance to HIV protease drugs (170, 171). Except for the discontinued agent amprenavir (Agenerase), which is superseded by fosamprenavir, other protease inhibitors are still widely used for HIV infections. Common side effects with PIs are nephrolithiasis, hypertension, rash, diarrhea, elevation of liver enzyme levels, ingrown toenails, benign hyperbilirubinemia, and gastrointestinal upset (143).
FIG 7.
Tertiary structures of HIV-1 protease and chemical formulas of HIV protease inhibitors. (A) HIV-1 protease dimer complexed with lopinavir (PDB accession number 2Q5K). The side view (left) and top view (right) of structures are presented. (B to K) Chemical formulas of nelfinavir, saquinavir, indinavir, atazanavir, lopinavir, ritonavir, fosamprenavir, amprenavir, darunavir, and tipranavir in the group of protease inhibitors. (L) Chemical formula of cobicistat. Cobicistat is a pharmacoenhancer used with HIV protease inhibitors, but cobicistat alone shows no antiviral activity.
HIV protease inhibitors are key components of HAART for patients infected with HIV-1 and/or HIV-2. However, primary and secondary resistance mutations in HIV protease remain a concern for administering PIs to patients harboring drug-resistant viruses (138, 169, 172). Because of the innate differences between HIV-1 and HIV-2 proteases (173), different PI-based treatments have been recommended for HIV-1 and HIV-2 infections to take resistance-associated mutation patterns into account (140). In contrast to the wide application of PIs approved for HIV-1 infection, current U.S. and European treatment guidelines recommend the use of lopinavir/ritonavir (LPV/r), saquinavir/ritonavir (SQV/r), or darunavir/ritonavir (DRV/r) for patients infected with HIV-2, because many polymorphisms in HIV-2 cause natural resistance to PIs such as tipranavir and fosamprenavir (140, 174, 175). Note that ritonavir is a popular booster that improves the bioavailability and half-lives of other PIs, so a low dose of ritonavir is commonly coadministered with other PIs (e.g., LPV/r) (169). In a similar fashion, cobicistat has been approved as a pharmacoenhancer of PIs. Although it has no antiviral activity, cobicistat inhibits intestinal transport proteins (cytochrome P450 enzymes of the CYP3A family) and increases the overall absorption of PIs (176). Approved by the FDA, cobicistat is now coadministered with the PIs darunavir (Prezcobix) and atazanavir (Evotaz) as well as other anti-HIV drugs (Stribild and Genvoya), which are elucidated below.
HCV NS3/4A Protease Inhibitors
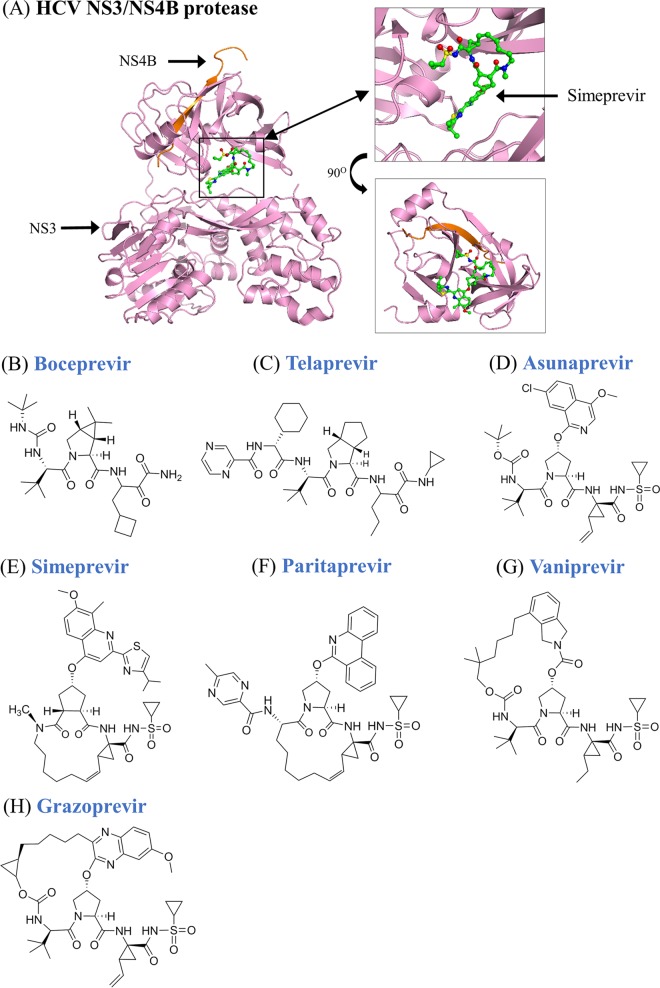
Despite fundamental differences in their structures and modes of replication, HIV and HCV share some similarities because both viruses cleave precursor proteins by viral proteases (aspartic protease for HIV versus serine protease for HCV) (Fig. 8), which could serve as ideal targets for the design of protease inhibitors (177). Of many protease inhibitor candidates, the following seven compounds that efficiently inhibit the activity of HCV NS3/4A protease are momentarily on the market (Fig. 8): asunaprevir, boceprevir, paritaprevir, simeprevir, telaprevir, vaniprevir, and grazoprevir (178–180). Among them, boceprevir (Victrelis) and telaprevir (Incivek) were discontinued for commercial reasons. To treat patients with HCV genotype 1 infection, combination drugs of asunaprevir plus daclatasvir and vaniprevir plus pegylated interferon alfa 2b (PegIFNα-2b) plus ribavirin have been approved in Japan (181).
FIG 8.
Tertiary structures of HCV NS3/NS4B protease and chemical formulas of HCV protease inhibitors. (A) HCV NS3/NS4B protease in complex with simeprevir (PDB accession numbers 3KEE and 4B76). HCV NS3 and NS4B proteins are shown in pink and orange, respectively. (B to H) Chemical formulas of boceprevir, telaprevir, asunaprevir, simeprevir, paritaprevir, vaniprevir, and grazoprevir in the group of HCV protease inhibitors.
All approved NS3/4A protease inhibitors are used for treatment of infection by HCV genotype 1, the most prevalent genotype in HCV-infected populations (182). Compared to two discontinued drugs, telaprevir and boceprevir, simeprevir has better response rates and drug interaction profiles, although it is more expensive. As a potent inhibitor approved by the FDA, paritaprevir is now used in combination with ombitasvir plus ritonavir (Viekira Pak) or ombitasvir plus dasabuvir plus ritonavir (Technivie) to treat HCV genotype 1 and 4 infections, respectively (Table 2). Approved by the FDA in January 2016, a combination drug of grazoprevir plus elbasvir (Zepatier) is now applied to treat HCV genotype 1 or 4 infection (Table 2). In addition to the approved drugs mentioned above, many experimental NS3/4A protease inhibitors (danoprevir, faldaprevir, vedroprevir, sovaprevir, deldeprevir, and narlaprevir) have been (or still are) under clinical development (178, 179). Forthcoming HCV protease inhibitors may have a reduced potential for drug-drug interactions, thus improving their use in the treatment of HCV infections (183).
INTEGRASE INHIBITORS
Since the first HIV integrase inhibitor was approved in 2007, three FDA-approved integrase inhibitors (raltegravir, dolutegravir, and elvitegravir) have been frequently used in HAART. Integrase inhibitors are described below.
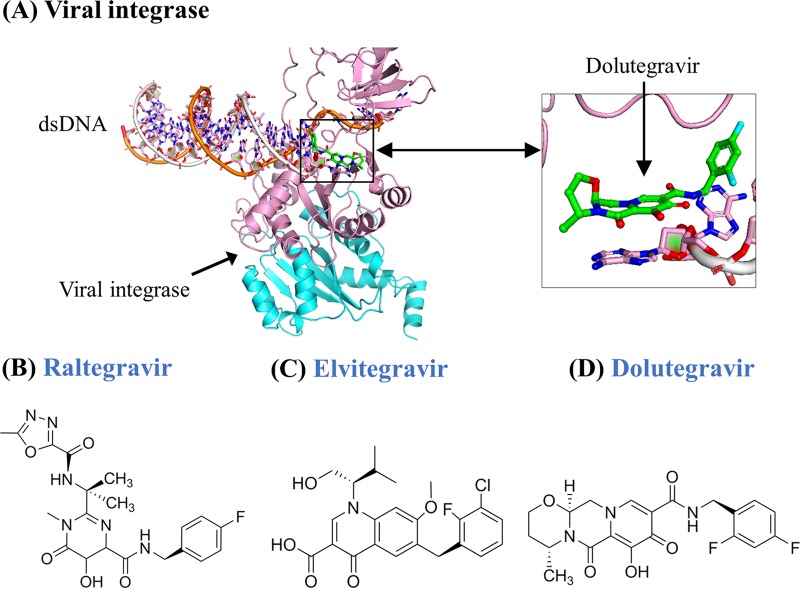
Raltegravir
During virus integration, viral integrases insert proviral DNA into host genomes through a multistep process. As an essential step, the strand transfer reaction covalently links the proviral DNA 3′ ends to the cellular (target) DNA, and this strand transfer can be inhibited by the so-called diketo acid inhibitors (184). These diketo acids (i.e., L-870812) could actively suppress the replication of simian-human immunodeficiency virus (SHIV) in rhesus macaques (185). This led to the discovery of raltegravir (MK-0518) as the “first in class” among the integrase inhibitors, which target the catalytic site of HIV integrase to prevent virus integration (Fig. 9). Raltegravir was later added to an optimized background regimen (OBR) (186), offering better virus suppression than the OBR alone (187). The use of raltegravir was effective, particularly for the treatment of HIV-infected patients with high HIV-1 RNA levels, low CD4 cell counts, and low genotypic or phenotypic sensitivity scores (188). Raltegravir could be combined with two nucleos(t)ide analogues or with ritonavir-boosted lopinavir (189). Since there is no raltegravir-based combination approved by the FDA, the effectiveness of such combination drugs has yet to be elucidated in clinical trials.
FIG 9.
Tertiary structures of viral integrase and chemical formulas of HIV integrase inhibitors. (A) Viral integrase of prototype foamy virus in complex with dsDNA and dolutegravir (PDB accession number 3S3N). A dimer structure of the viral integrase is shown in pink and cyan, respectively. Although the structure of HIV integrase in complex with its inhibitors is still lacking, approved antiviral inhibitors that target HIV and prototype foamy virus integrase are believed to share similar mechanisms (477). (B to D) Chemical formulas of raltegravir, elvitegravir, and dolutegravir in the group of HIV integrase inhibitors.
Elvitegravir
In 2006, Sato and coworkers first showed that the 4-quinolone-3-carboxylic acids could be an alternative scaffold to diketo acids, leading to the discovery of elvitegravir (GS-9137), which efficiently inhibited the DNA strand transfer reaction of HIV-1 integrase (190). Subsequent in vitro studies indicated that elvitegravir inhibited not only strains of various HIV-1 subtypes but also a broad spectrum of viruses such as HIV-2, murine leukemia virus, and simian immunodeficiency virus (SIV) (191, 192). Akin to raltegravir, elvitegravir can be used in combination with nucleos(t)ide analogues. Stribild, which contains elvitegravir, cobicistat, (−)FTC, and TDF (193), was approved as the first once-daily four-drug (“quad”) pill in August 2012. Stribild causes minimal adverse effects but efficient virus suppression comparable to those for other HIV combination drugs (e.g., Atripla) (194, 195). Approved in November 2015, Genvoya is another combination drug that contains elvitegravir plus cobicistat, (−)FTC, and tenofovir alafenamide.
When the efficacy and safety of elvitegravir was compared with those of raltegravir, a phase 3 clinical trial suggested that both drugs are comparable, but elvitegravir might improve patients' adherence because elvitegravir requires only once-daily dosing, compared with twice-daily dosing for raltegravir (196). Elvitegravir is usually well tolerated, while the most common side effects are diarrhea and nausea (197). It is worth mentioning that elvitegravir should not be used to treat raltegravir-resistant HIV infections, because elvitegravir shares similar drug resistance mutations with raltegravir (198).
Dolutegravir
Approved by the FDA in August 2013, dolutegravir is the third integrase inhibitor on the market. Even though dolutegravir and raltegravir share similar efficacies and safety profiles (199), dolutegravir exhibits a higher genetic barrier to drug resistance development (200). Moreover, once-daily dolutegravir, in combination with up to two other antiretroviral drugs, provides a better virologic response than twice-daily raltegravir in antiretroviral-experienced patients (201). In a phase 3b clinical trial called FLAMINGO, once-daily dolutegravir was superior to once-daily darunavir plus ritonavir for the treatment of antiretroviral-naive patients infected with HIV-1 (202, 203). Due to its prominent antiviral activity, dolutegravir is now used in two fixed-dose combinations: dolutegravir plus abacavir plus lamivudine (Triumeq) (one tablet, once daily) and dolutegravir plus lamivudine (Dutrebis) (one tablet, twice daily) (Table 2).
In first-line therapy, integrase inhibitors are superior to NRTIs, NNRTIs, and protease inhibitors (200). Even though integrase inhibitors have a high genetic barrier to resistance (200), drug resistance mutations (e.g., F121Y, Q148H/R, N155H, and R263K) have been observed for all three integrase inhibitors (138). The most common side effects with integrase inhibitors are nausea, diarrhea, hepatitis, or hypersensitivity (200). Attracted by their potent antiviral activities, forthcoming integrase inhibitors are under investigation in clinical trials. For instance, cabotegravir (GSK1265744 and GSK744) has been recognized as a long-acting inhibitor against the strand transfer reaction of HIV and SIV integrases (204–206). Recently, the potent anti-HIV activity of therapy with cabotegravir plus rilpivirine was shown in a randomized, phase 2b, dose-ranging trial (207), but more evidence is still required to support its clinical use. Overall, integrase inhibitors have offered good tolerability, a favorable safety profile, and an absence of significant drug interactions (200).
ENTRY INHIBITORS
In the drug group of entry inhibitors, there are 7 FDA-approved drugs, including one HSV drug (docosanol), two HIV drugs (enfuvirtide and maraviroc), two RSV antibody drugs (palivizumab and respiratory syncytial virus immune globulin, intravenous [RSV-IGIV]), and two VZV antibody drugs (varicella-zoster immunoglobulin [VariZIG] and varicella-zoster immune globulin [VZIG]) (Table 2). These entry inhibitors are described in the following sections.
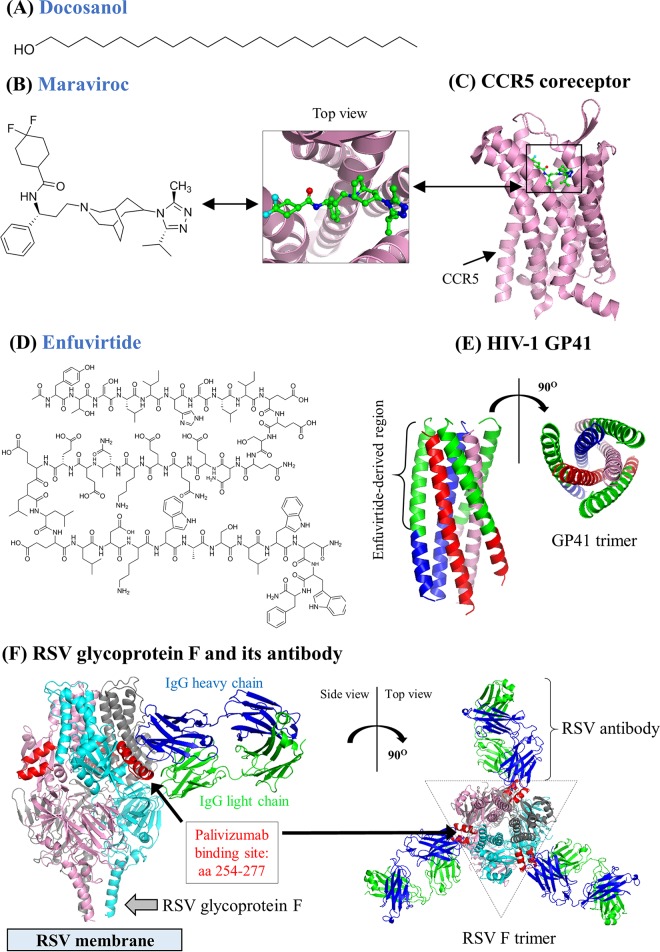
Enfuvirtide and Maraviroc
Enfuvirtide (also known as T20), the first peptide inhibitor approved by the FDA, is a polypeptide (36 amino acids in length) homologous to the heptad repeat region of HIV-1 GP41 (208) (Fig. 10). To block the fusion of HIV-1 with the extracellular membrane of host cells, enfuvirtide mimics the helix in heptad repeat 2 (HR-2) to prevent the interaction between HR-1 and HR-2 (209, 210). Kilby et al. (211) showed the significant efficacy of enfuvirtide against HIV-1 replication in cell lines and human subjects. Approved by the FDA in March 2003, enfuvirtide is still the only anti-HIV drug that must be injected subcutaneously twice daily. It has been used for salvage therapies as part of combination regimens with other antiviral drugs (212, 213). Although enfuvirtide has high drug efficacy with minimal systemic toxicity, its long-term application is limited due to the subcutaneous administration and the high cost (214). The clinical use of enfuvirtide has therefore become obsolete given the wealth of the other 40 approved drugs against HIV infections by oral drug delivery.
FIG 10.
Chemical formulas of HIV entry inhibitors and tertiary structures of CCR5, HIV-1 GP41, and RSV glycoprotein F. (A) Chemical formula of docosanol. (B and C) Chemical formula of maraviroc and the CCR5 coreceptor in complex with maraviroc (PDB accession number 4MBS). The top and side views of the CCR5 structure are presented. (D and E) Chemical formula of enfuvirtide and tertiary structure of the HIV-1 GP41 trimer (PDB accession number 2X7R). Enfuvirtide is derived from the green region of HIV-1 GP41. The top and side views of the HIV-1 GP41 trimer are presented. Three units of the HIV-1 GP41 trimer are shown in blue, red, and pink, respectively. (F) Tertiary structure of the prefusion RSV glycoprotein F trimer in complex with the antibody motavizumab (PDB accession number 4ZYP). Motavizumab is an experimental monoclonal antibody derived from the FDA-approved drug palivizumab (478). The side views (left) and top views (right) of protein structures are presented. The heavy and light chains of motavizumab are shown in blue and green, respectively. The palivizumab-binding site (amino acid [aa] positions 254 to 277 [479]) is highlighted in red. Three units of the prefusion RSV F trimer are shown in pink, gray, and cyan, respectively.
Maraviroc is the first FDA-approved chemokine receptor antagonist or CCR5 inhibitor that targets the chemokine receptor CCR5 on the surface of CD4+ cells and macrophages (215) (Fig. 10). Historically, Ed Berger and colleagues were the first to demonstrate the importance of the CC chemokine receptor CCR5 during HIV entry (216). Baba et al. (217) were the pioneers who described the first CCR5 antagonist, TAK-779, which, however, was not pursued due to its poor oral bioavailability. Likewise, TAK-220 and TAK-652, despite their oral bioavailability (218), were not developed further, nor were two CCR5 antagonists, aplaviroc and vicriviroc (219). Later, the principle of attacking CCR5 was proven to be a success when maraviroc showed promising antiviral activities in cell lines (220) and clinical trials (221, 222). It is worth mentioning that during early HIV infection, R5 viruses predominately use CCR5 for virus entry, whereas R4 viruses using CXCR4 usually occur at late stages of disease progression (223). For patients with R5 HIV-1 infections, maraviroc is a valuable treatment option (222, 224). However, maraviroc does not inhibit R4 viruses, and half of patients infected with R4 viruses fail maraviroc-based treatments (225). Therefore, it is possible that CCR5 antagonists would accelerate disease progression by the selection of viruses using CXCR4 (214, 215). Overall, the use of maraviroc requires the phenotypic identification of R5 viruses, and the coadministration of CCR5 and CXCR4 antagonists has yet to be a therapeutic challenge (214, 226).
Palivizumab and RSV-IGIV
RSV-IGIV, approved by the FDA in January 1996, is a sterile human immunoglobulin produced from adult plasma with high titers of neutralizing antibodies to RSV (227). These neutralizing antibodies can prevent RSV surface glycoproteins F and G from anchoring to host cells (227). Although RSV-IGIV may efficiently decrease the numbers of hospitalizations and hospital days attributable to RSV (228), the high cost and strict guidelines on its use remain a problematic issue (229). As a more cost-effective drug (230), palivizumab (Synagis) marked the discontinuation of RespiGam in 2004 (231). Approved by the FDA in June 1998, palivizumab is a humanized mouse immunoglobulin monoclonal antibody that directly targets a conserved epitope of the A antigenic site of the RSV fusion protein (232) (Fig. 10F). Therefore, palivizumab offers neutralizing and fusion-inhibitory activities against RSV infections (232). In clinical practice, palivizumab prophylaxis is recommended only for preterm infants with chronic lung diseases or congenital heart diseases, mostly in the first year of life for infants born within 12 months of the onset of the RSV season (232). Despite the promising outcomes from clinical trials (233, 234), systematic reviews suggest that the limited clinical and social benefits are insufficient to justify the high cost of palivizumab prophylaxis (232, 235, 236). Consequently, the clinical use of palivizumab prophylaxis is not popular in most cases.
VZIG and VariZIG
Historically, VZIG was discovered in 1969 when immunoglobulin concentrates were extracted from patients convalescing from VZV infections. Subsequent serological and clinical studies suggested that VZIG could decrease the risk of complications and reduce clinical illness in immunocompromised patients (237, 238). After its application for 2 decades, VZIG was discontinued in October 2004 and was later superseded by a better product, called VariZIG. Approved by the FDA in December 2012, VariZIG is a detergent-treated, sterile, lyophilized preparation of IgG purified from human plasma harboring high levels of anti-VZV antibodies. VariZIG offers passive immunization for immunocompromised patients to generate IgG antibodies against VZV infections (239). Licensed for postexposure prophylaxis of VZV infections, VariZIG is administered intramuscularly to high-risk patients who lack evidence of immunity to VZV and are ineligible for VZV vaccination (240). VariZIG must be administered to patients within 96 h of exposure to VZV, and the dosing of VariZIG depends on body weight. Common side effects with VariZIG are headache and pain at the injection site. Overall, VariZIG offers a cornerstone for VZV postexposure prophylaxis, while approved antiviral drugs such as acyclovir are also recommended to be used either alone or with immunoglobulin therapy (81).
Docosanol
Docosanol (n-docosanol; behenyl alcohol) is a 22-carbon, saturated, primary alcohol (Fig. 10) that inhibits a broad spectrum of lipid-enveloped viruses (e.g., HSV, RSV, HCMV, and VZV) based on in vitro experiments (241, 242). Clinical evidence suggests that 10% docosanol topical cream is safe and effective to reduce the healing time and duration of symptoms for the treatment of recurrent herpes labialis caused by HSV-1 or HSV-2 infections (241). Although its mechanism of drug action is still debated (243), docosanol is believed to prevent virus entry by interfering with the interaction between epithelial cell membrane receptors and HSV envelope proteins (242, 244). Approved by the FDA in July 2000, docosanol remains the only over-the-counter medication in clinical use for cold sores and fever blisters.
ACYCLIC GUANOSINE ANALOGUES
In the drug group of acyclic guanosine analogues, there are six approved compounds: acyclovir, ganciclovir, valacyclovir (also known as valaciclovir), valganciclovir, penciclovir, and famciclovir (Fig. 11 and Table 2). Historically, acyclovir [9-((2-hydroxyethoxy)methyl)guanine] was first mentioned in a laboratory notebook of Nick Oliver in 1974 (245). Its antiviral properties were first uncovered by Peter Collins and John Bauer at the Wellcome Laboratories in Beckenham, United Kingdom. Acyclovir was originally designed as an inhibitor of adenosine deaminases to enhance the antiviral activity of vidarabine (246). Elion et al. (247) first pointed out that acyclovir owed its selectivity against HSV to specific phosphorylation by viral thymidine kinases. A few months later, acyclovir was reported to show potent activity against herpesviruses (HSV-1 and HSV-2) (248). This certainly was more of a surprise for a guanosine analogue (viz., acyclovir) than for a 5-substituted 2′-deoxyuridine (viz., BVDU). Acyclovir, targeting the viral DNA polymerase, was proven to be particularly active against HSV-1 and HSV-2 but much less so against VZV (249). Of the various acyclic guanosine analogues discovered subsequently, penciclovir was pursued for VZV infections, and ganciclovir became the drug of choice against HCMV infections (91). In clinical practice, ganciclovir is being gradually superseded by valganciclovir to treat HCMV infections, because valganciclovir seems to modestly improve hearing and developmental outcomes in the long term (250).
FIG 11.
Tertiary structures of HSV-1 thymidine kinase and chemical formulas of acyclic guanosine analogues and acyclic nucleoside phosphonate analogues. (A) The HSV-1 thymidine kinase dimer in complex with acyclovir. Two units of thymidine kinase are shown in pink and orange, respectively. Acyclovir can be phosphorylated by HSV thymidine kinase and cellular enzymes (249). (B to G) Chemical formulas of acyclovir, famciclovir, valacyclovir, ganciclovir, penciclovir, and valganciclovir in the group of acyclic guanosine analogues. (H to K) Chemical formulas of cidofovir, adefovir, tenofovir, and tenofovir alafenamide in the group of acyclic nucleoside phosphonate analogues.
To increase oral bioavailability, the prodrug strategy was applied to all three acyclic nucleoside analogues, leading to the development of famciclovir, valacyclovir, and valganciclovir (245). For instance, famciclovir is the prodrug (diacetyl 6-deoxypenciclovir) of penciclovir. Acyclovir, ganciclovir, and penciclovir act in similar fashions and are all phosphorylated. Ganciclovir is specifically phosphorylated by host kinases (251), while acyclovir and penciclovir are phosphorylated by viral thymidine kinases (247, 252) (Fig. 11). After their phosphorylation, acyclovir, ganciclovir, and penciclovir triphosphates individually compete with the natural substrate dGTP of viral DNA polymerases to inhibit viral DNA synthesis.
As of today, acyclovir continues to be the gold standard for the treatment of HSV infection. Despite the high efficacy of acyclovir, the mortality rate of patients with herpes simplex encephalitis who received acyclovir is ∼14 to 19% (253). For patients treated with a standard course of intravenous acyclovir, a follow-up treatment with a 3-month course of valacyclovir is unlikely to provide added benefits compared to placebo (253). Nevertheless, owing to its increased oral bioavailability, valacyclovir has superseded acyclovir for the treatment of HSV or VZV infections (254). In a recent study, an economic comparison between valacyclovir and valganciclovir was performed, suggesting that in the first year after renal transplantation, valganciclovir was more cost-effective than valacyclovir (255). On the other hand, famciclovir offers significant benefits, such as cost-effective therapy and accelerated rates of lesion resolution (256). For these reasons, famciclovir is now widely used to treat HSV or VZV infections.
ACYCLIC NUCLEOSIDE PHOSPHONATE ANALOGUES
In the drug group of acyclic nucleoside phosphonate (ANP) analogues, there are 10 FDA-approved (combination) drugs (Table 2). The ANP analogues that inhibit the activity of viral DNA polymerases come from the hybridization of (S)-DHPA [(S)-9-(2,3-dihydroxypropyl)adenine] with phosphonoacetic acid, thus generating (S)-HPMPA [(S)-9-(3-hydroxy-2-phosphonylmethoxypropyl)adenine]. Historically, the broad-spectrum antiviral activity of (S)-DHPA was first reported by De Clercq et al. (257), shortly after acyclovir had been described as a specific antiherpetic agent (248). In 1986, (S)-HPMPA was first reported as a new broad-spectrum anti-DNA virus agent by De Clercq et al. (258). Although (S)-HPMPA itself was not commercialized for clinical use, it could be considered the prototype ANP, from which emanated a series of ANP analogues, such as adefovir {PMEA [9-(2-phosphonomethoxyethyl)adenine]}, cidofovir {(S)-HPMPC [(S)-1-(3-hydroxy-2-phosphonomethoxypropyl)-cytosine]}, and tenofovir {(R)-PMPA [(R)-9-(2-phosphonomethoxypropyl)adenine]} (219, 259, 260) (Fig. 11). In June 1996, cidofovir was approved for the treatment of HCMV retinitis in AIDS patients (Table 2). Cidofovir has also been used as an off-label drug to treat many DNA virus infections such as HSV and adeno-, pox-, polyoma-, and papillomavirus infections (261). Later, adefovir was marketed in its oral prodrug form, adefovir dipivoxil (Hepsera), for the treatment of HBV infection, as was tenofovir, in its prodrug form, TDF (Viread), for the treatment of HIV and/or HBV infections.
In comparison to many TDF-based HIV therapies (Truvada, Atripla, Complera, and Stribild), recent clinical trials indicate that TDF monotherapy seems safe and effective against HBV infections (262–266). In comparisons of the effectiveness of TDF monotherapy versus dual therapies, it has been shown that TDF monotherapy is comparable to therapy with TDF plus (−)FTC (263, 267) or TDF plus ETV (268, 269), but it is less potent than TDF plus pegylated interferon alfa 2a (270). Because of its potency and high barrier to resistance, TDF monotherapy is currently recommended as the first-line treatment against chronic hepatitis B according to American Association for the Study of Liver Diseases (AASLD) guidelines (271), European Association for the Study of the Liver (EASL) guidelines (272), and WHO guidelines (114). As of April 2016, there has been no FDA-approved combination drug for HBV infections. Therefore, the optimal combination drug that achieves a sustained loss of serum hepatitis B virus surface antigen has yet to be discovered.
The concept for all ANPs is the same: it is based on the presence of a phosphonate (PCO) linkage (Fig. 11) instead of a normal phosphate (POC) linkage, which is a characteristic of nucleotide analogues against the activity of viral polymerases (273). The PCO linkage, in contrast with the POC linkage, cannot be cleaved by the hydrolase enzyme esterase. This fact explains the stability of the ANPs, as chain terminators, after their incorporation into the DNA chain (274). In the presence of the phosphonate group, ANPs can no longer be removed from the DNA chain, thereby leading to irreversible chain termination (259). Particularly, ANPs need to first be phosphorylated (by cellular enzymes) to become the diphosphate (not the triphosphate, as their phosphonate group mimics the 5′-monophosphate in the nucleotides). The following ANPs are, at present, on the market: (i) cidofovir (Vistide) (now generic), (ii) adefovir dipivoxil (Hepsera), (iii) TDF (Viread), (iv) TDF in combination with (−)FTC (Truvada), (v) TDF and (−)FTC in combination with efavirenz (Atripla), (vi) TDF and (−)FTC in combination with rilpivirine (Complera [United States] and Eviplera [European Union]), and (vii) TDF and (−)FTC in combination with elvitegravir and cobicistat (Stribild). It is worth mentioning that cidofovir may be replaced by its oral prodrug brincidofovir (originally referred to as hexadecyloxypropyl [HDP]-cidofovir) or CMX001 (193). Moreover, Viread has been approved for the treatment of HIV and/or HBV infections (Table 2). Truvada has been licensed for both therapy and prophylaxis of HIV infections. As for the combination drug Stribild, phase 3 clinical trials suggest that >90% of treatment-naive HIV-infected patients receiving Stribild may have virological success at 48 weeks (275). Moreover, Stribild is well tolerated in virologically suppressed adults infected with HIV-1 (276).
In November 2015, TAF (GS-7340) was approved in combination with cobicistat, emtricitabine, and elvitegravir (Genvoya) to treat HIV infections (Table 2). Genvoya is now on the market as a fixed-dose combination of TAF (10 mg), cobicistat (150 mg), emtricitabine (200 mg), and elvitegravir (150 mg). Three phase 3 clinical trials suggest that this combination drug could achieve virological success in 1,732 (94.9%) of 1,825 patients at 48 weeks of treatment (275, 277). Importantly, Genvoya provides a favorable safety profile because HIV-infected patients show fewer renal and bone effects after receiving Genvoya (275, 277).
Approved by the FDA in 2016, TAFs are now used in combination with (−)FTC (Descovy) or with (−)FTC plus rilpivirine (Odefsey) (Table 2). Forthcoming TAF-based drug combinations include (i) TAF in combination with (−)FTC plus efavirenz and (ii) TAF in combination with (−)FTC, elvitegravir, and cobicistat. These drugs combined with TAF have distinct advantages because they are specifically taken up by lymphocytes, and their dosages can be reduced by ∼10-fold (278, 279). This benefit thus significantly reduces the risk of toxic effects such as kidney disturbances and bone demineralization (278, 279).
HCV NS5A/NS5B INHIBITORS
As of April 2016, there are 8 approved (combination) drugs in the group of HCV NS5A/NS5B inhibitors (Table 2). DAAs (direct-acting antivirals) for the treatment of HCV infections encompass, in principle, four classes: (i) NS3/4A protease inhibitors (Fig. 8), (ii) NS5A protein inhibitors (Fig. 12), (iii) NS5B polymerase inhibitors (Fig. 13) of the nucleoside/nucleotide type, and (iv) NS5B polymerase inhibitors of the nonnucleoside type (280). DAAs are now replacing the combination of pegylated interferons and ribavirin, the standard of care (SOC) for treating chronic HCV infections before 2013 (281).
FIG 12.
Tertiary structures of the HCV NS5A protein and chemical formulas of HCV NS5A inhibitors. (A) Tertiary structure of the HCV NS5A dimer in complex with daclatasvir. Two units of the HCV NS5A dimer are shown in pink and orange, respectively (PDB data were reported in reference 282). (B to F) Chemical formulas of ledipasvir, daclatasvir, ombitasvir, velpatasvir, and elbasvir in the group of HCV NS5A inhibitors. Note that velpatasvir is an experimental inhibitor currently in phase 3 clinical trials.
FIG 13.
Tertiary structures of HCV NS5B polymerase and chemical formulas of HCV NS5B inhibitors. (A) Tertiary structure of HCV NS5B polymerase in complex with dsDNA, beclabuvir, and sofosbuvir diphosphate (PDB accession numbers 4NLD and 4WTG). Note that beclabuvir and sofosbuvir diphosphate bind to the allosteric site and the catalytic site of the HCV NS5B polymerase, respectively. (B to D) Chemical formulas of beclabuvir, dasabuvir, and sofosbuvir in the group of HCV NS5B inhibitors. Note that beclabuvir is a forthcoming inhibitor in the combination drug of daclatasvir plus asunaprevir plus beclabuvir in phase 4 clinical trials.
HCV NS5A Inhibitors
As of April 2016, there are four approved NS5A inhibitors: daclatasvir, ledipasvir, ombitasvir, and elbasvir (Table 2). As illustrated in Fig. 12, daclatasvir can specifically bind to the HCV nonstructural protein NS5A (282). The exact mechanisms of HCV NS5A drug action remain debated, especially regarding their potential inhibition of the structural stability, dimerization, or subcellular distribution of NS5A (283, 284). Nevertheless, NS5A inhibitors can block HCV RNA replication by interrupting the formation of the membranous web, a heterogeneous meshwork within cytoplasmic membranous factories where HCV replication takes place (284). Daclatasvir (Fig. 12) in combination with the protease inhibitor asunaprevir (Fig. 8) was approved in Japan, whereas the FDA has not yet granted its approval as of April 2016.
Recent clinical trials have demonstrated the effectiveness of daclatasvir plus asunaprevir. The phase 3 HALLMARK-DUAL trial enrolled patients with HCV genotype 1b infection, including 307 treatment-naive patients; 205 nonresponders; and 235 ineligible, intolerant, or ineligible and intolerant patients (285). The treatment outcome was measured by the rate of sustained virologic response at 12 weeks (SVR12). This study reported promising SVR12 rates (>80%) for daclatasvir (60 mg, once daily) plus asunaprevir (100 mg, twice daily) in the three patient groups mentioned above (285). A phase 3 clinical trial that enrolled 135 interferon-ineligible/intolerant patients and 87 nonresponder patients showed high SVR12 rates (>88%) for daclatasvir plus asunaprevir in the treatment of chronic HCV genotype 1b infection (286). Another clinical trial, which enrolled 230 patients with HCV genotype 1b infection, demonstrated that the efficacy-and-safety profile of daclatasvir plus asunaprevir was superior to that of telaprevir plus peginterferon plus ribavirin (287). Overall, given the 1,000 patients with HCV genotype 1b infection in the clinical trials mentioned above, treatment with daclatasvir (60 mg, once daily) plus asunaprevir (100 mg, twice daily) reached a high rate of SVR12 of up to 86.4% (n = 864). A phase 4 trial is currently ongoing to investigate the safety and efficacy of daclatasvir plus asunaprevir in patients with chronic hepatitis C infection and chronic renal failure (ClinicalTrials.gov registration number NCT02580474). Results of this clinical trial are to be released in 2017.
In January 2016, the once-daily fixed-dose combination of elbasvir plus grazoprevir (Zepatier) was approved by the FDA to treat HCV genotype 1 or 4 infection (Table 2). Elbasvir and grazoprevir inhibit HCV nonstructural protein NS5A (Fig. 12) and NS3/4A protease (Fig. 8), respectively. A number of clinical trials have been carried out to study the combination of grazoprevir plus elbasvir: (i) the phase 2 C-WORTHY trial, which enrolled 253 patients with HCV genotype 1 infection, showed high rates of sustained virologic response with treatment with grazoprevir plus elbasvir at 12 and 18 weeks in both treatment-naive patients with cirrhosis and patients with a previous null response to PegIFNα-2a plus ribavirin with or without cirrhosis (288); (ii) the phase 3 C-SURFER trial, which enrolled 224 patients with HCV genotype 1 infection and stage 4 to 5 chronic kidney diseases, suggested that treatment with grazoprevir plus elbasvir caused a low rate of adverse events and showed promising SVR12 rates (289); and (iii) the phase 3 C-EDGE trial demonstrated that grazoprevir plus elbasvir achieved high rates of SVR12 in 421 treatment-naive and noncirrhotic patients infected with HCV genotype 1, 4, or 6 (290). In these clinical trials, common side effects such as headache, nausea, and fatigue were recorded (289, 290). Given the 484 patients infected with HCV genotype 1 or 4 in three clinical trials (C-WORTHY, C-SURFER, and C-EDGE), the combination of grazoprevir (100 mg) plus elbasvir (50 mg) showed a success rate of SVR12 of up to 95.8% (n = 464). However, the efficacy of grazoprevir plus elbasvir in HCV genotype 6 infection has yet to be clarified, because the C-EDGE study showed SVR12 for only 8 out of 10 patients (290). Overall, the combination of grazoprevir (100 mg) plus elbasvir (50 mg) has been shown to be an effective pangenotypic drug (Zepatier) against HCV genotype 1 or 4 infection.
HCV NS5B Inhibitors
For the “nonnucleoside” NS5B polymerase inhibitors (Fig. 13), sofosbuvir and dasabuvir have been approved by the FDA (Table 2), while a number of experimental inhibitors (i.e., deleobuvir, setrobuvir, beclabuvir, and tegobuvir) have been identified to target allosteric sites of the HCV NS5B polymerase (178, 179). The list of “nucleoside” NS5B polymerase inhibitors is so short because several compounds were discontinued prematurely due to undesirable side effects. Sofosbuvir is, however, an exception in this group, which did not reveal toxicity or drug resistance, and it could be administered with other HCV drugs in combination as a single oral pill for a total duration of 12 weeks, guaranteeing a high level of sustained virologic response (291). To pursue interferon-free treatment, sofosbuvir could be combined with an NS5A inhibitor, such as ledipasvir (292). This combination has been dubbed Harvoni, which is administered as a once-daily oral pill containing sofosbuvir (400 mg) and ledipasvir (90 mg). With this combination, the treatment duration could eventually be shortened to <12 weeks (293), providing high rates of sustained virologic response in patients coinfected with HIV-1 and HCV genotype 1 or 4 (294).
To obtain clearance, a real “cure” of a chronic virus infection, as noted for HCV, is unheard of in the medical history of infectious diseases and sharply contrasts with the situation for HIV and HBV infections. In principle, current development of anti-HIV drugs requires lifelong treatments, while anti-HBV therapies may lead to a real cure only in a small percentage of HBV-infected patients (295, 296).
INFLUENZA VIRUS INHIBITORS
As of April 2016, 8 drugs have been approved to treat influenza infections (Table 2). As illustrated in Fig. 14, these drugs could be recognized as matrix 2 inhibitors (amantadine and rimantadine), neuraminidase inhibitors (zanamivir, oseltamivir, peramivir, and laninamivir octanoate), and polymerase inhibitors (ribavirin and favipiravir). We describe the details of these drugs below.
FIG 14.
Tertiary structures of influenza virus proteins (matrix 2, neuraminidase, and RNA polymerase) and chemical formulas of influenza virus inhibitors. (A) Tertiary structure of the influenza A virus matrix 2 protein in complex with amantadine (PDB accession number 2KAD). Movies that simulate the binding of approved antiviral drugs to viral or host proteins are available online (see http://www.virusface.com/). (B) Structure of influenza A virus neuraminidase in complex with zanamivir (PDB accession number 2HTQ). (C) Tertiary structure of influenza virus RNA polymerase in complex with RNA. The RNA polymerases of influenza A virus (left) (PDB accession number 3J9B) and influenza B virus (right) (PDB accession number 4WRT) are illustrated. The PA, PB1, and PB2 subunits of RNA polymerase (see structural details in reference 480) are shown in pink, orange, and gray, respectively. Ribavirin triphosphate targets the catalytic site of the RNA polymerase to inhibit viral replication. Note that the RNA polymerase of influenza A virus is a tetramer (480), but the complete tetramer structure of influenza virus RNA polymerase in complex with its inhibitors is still lacking. (D and E) Chemical formulas of amantadine and rimantadine, which target the matrix 2 protein of influenza virus. (F and G) Chemical formulas of ribavirin and favipiravir, which target the viral RNA polymerase of influenza virus. (H to K) Chemical formulas of zanamivir, laninamivir, peramivir, and oseltamivir, which target the viral neuraminidase of influenza virus.
Amantadine and Rimantadine
Amantadine (1-adamantanamine) was the first antiviral compound approved in 1966 to treat influenza A virus infections (297). This compound blocks the transport of H+ ions through the M2 (matrix 2) protein channels (Fig. 14) into the interior of viral particles, thus preventing the uncoating of influenza virus particles within the endosomes (298, 299) (Fig. 4). After the discovery of amantadine, rimantadine and a number of amantadine derivatives were later synthesized (300, 301), but they did not reach the market, except for amantadine and rimantadine. Despite their approval for adult patients, amantadine and rimantadine do not contribute to the prevention, treatment, or reduced duration of influenza A virus infection in children and the elderly (302). Because of widespread resistance, amantadine has virtually been abandoned in the treatment of influenza infections (303). However, there is growing interest for the use of amantadine in the early symptomatic treatment of Parkinson disease and levodopa-induced dyskinesia (304, 305). More clinical evidence is required to prove this new application of amantadine.
Zanamivir, Oseltamivir, Peramivir, and Laninamivir Octanoate
The rational computer-aided design of zanamivir (306) marked a new era in antiviral drug development (300). As a highly selective inhibitor of influenza A and B virus neuraminidases (Fig. 14), zanamivir prevents influenza infections by impeding virus release rather than virus entry or other viral stages during the viral life cycle (307) (Fig. 4). Zanamivir administered by inhalation was soon joined by oseltamivir, which could be administered by the oral route (308). Oral oseltamivir and inhaled zanamivir can offer net benefits by reducing mortality and the duration of influenza symptoms and complications, according to a systematic review and meta-analysis of 74 observational studies (309). Soon after the success of zanamivir and oseltamivir, two neuraminidase inhibitors were later launched for the treatment of influenza infections (310): peramivir, which could be given as a single intravenous injection (311), and laninamivir octanoate, which would be effective if given as a single inhalation (312). Notably, peramivir has clinical efficacy similar to that of oseltamivir in the treatment of severe seasonal influenza (313), while the potency of laninamivir octanoate has been shown for the treatment of seasonal influenza, including oseltamivir-resistant virus, in adults (312). Intravenous peramivir and inhalational laninamivir are used as a single-dose treatments for influenza A and B viruses, but this application is limited in a few countries (laninamivir in Japan and peramivir in the United States, Japan, South Korea, and China) (314).
Ribavirin
Ribavirin (Virazole), 1-β-d-ribofuranosyl-1,2,4-triazole-3-carboxamide, is the first synthetic nucleoside analogue that has ever been reported to be active against a broad spectrum of RNA viruses (HCV, RSV, and influenza virus): “its antiviral spectrum was the broadest ever reported for a synthetic material that did not induce interferon” (315). Its principal mechanism of drug action, established shortly after the discovery of ribavirin (316), is the inhibition of inosine-5′-monophosphate (IMP) dehydrogenase, which converts IMP to xanthosine monophosphate (XMP) and thus accounts for the de novo biosynthesis of GTP (317). The inhibitory activity of ribavirin on the IMP dehydrogenase may contribute to the immunosuppressive effects of ribavirin (318). This in turn contributes to the significant success obtained by ribavirin, in combination with peginterferon alfa 2a, for the treatment of HCV infection (319, 320). HCV-infected patients who received treatments of telaprevir, peginterferon alfa 2a, and ribavirin had a significant level of sustained virologic response (321). Approved for influenza treatment, ribavirin in the triphosphate form efficiently inhibits the RNA polymerase of influenza virus (322). Besides, ribavirin is used in the therapy of some hemorrhagic fever virus infections (e.g., Lassa fever [323]), but ribavirin has never been formally licensed for this medication. The potential activity of ribavirin against RNA viruses has also been shown in the search for antiviral candidates against many emerging infectious diseases such as dengue virus (324), norovirus (325, 326), Marburg virus (MARV) (327), and Hendra and Nipah viruses (328). Nevertheless, more clinical evidence is still required to prove these new applications.
Favipiravir
Favipiravir (also known as T-705), 6-fluoro-3-hydroxy-2-pyrazine carboxamide (Fig. 14), has been primarily pursued for the treatment of influenza infections (329–331). Approved in Japan, favipiravir can be used in the treatment of influenza A, B, and C virus infections (Table 2). According to the mechanism of drug action postulated by Furuta et al. (332), favipiravir is converted intracellularly to its ribofuranosyl monophosphate form by the phosphoribosyl transferase; two phosphorylations subsequently convert the ribofuranosyl monophosphate form to the triphosphate form, the active metabolite of favipiravir. Importantly, favipiravir triphosphate shows broad-spectrum inhibitory activities against the RNA polymerases of influenza A viruses (including the highly pathogenic H5N1 viruses) (330, 333) and many other positive-sense RNA and negative-sense RNA viruses (331). Recently, favipiravir has been proposed to treat patients infected with Ebola virus (EBOV) (334). Preliminary results suggest that favipiravir efficiently inhibits Ebola virus infections in mouse models (335, 336), but further investigations are still needed (337). In addition, favipiravir can inhibit the replication of human norovirus (325, 326) and human arenaviruses (Junin, Machupo, and Pichinde viruses) (338, 339), but these new applications require further evidence from clinical trials.
INTERFERONS, IMMUNOSTIMULATORS, OLIGONUCLEOTIDES, AND ANTIMITOTIC INHIBITORS
In the drug group of interferons, immunostimulators, oligonucleotides, and antimitotic inhibitors, there are 8 FDA-approved drugs: (i) interferons for HBV and/or HCV infections; (ii) fomivirsen (an antisense oligonucleotide) for HCMV infections; and (iii) podofilox (an antimitotic inhibitor), imiquimod (an immunostimulator), and sinecatechins (a botanical drug) for the treatment of external genital warts caused by HPV infections (Table 2). These approved drugs share one thing in common: they exert specific inhibitory effects without targeting viral proteins directly. Below, we describe the details of these drugs.
Interferons
To treat HBV or HCV infections, three interferons have been licensed: interferon alfacon 1, pegylated interferon alfa 2a (PegIFNα-2a), and PegIFNα-2b (Table 2). Due to its severe adverse events, interferon alfacon 1 has been discontinued since September 2013. Currently, PegIFNα-based regimens are preferably used for HBV but not for HCV infections, because interferon-free drugs are now effective against HCV infections (340). Interferon alpha (IFNα), predominantly secreted by hematopoietic cells (e.g., plasmacytoid dendritic cells), is a well-defined type I interferon that stimulates the immune system for antiviral defense (341–343). To increase the half-life of interferon inhibitors in serum, polyethylene glycol polymers are covalently attached to IFN-α for the production of PegIFNα. Interestingly, there is only one amino acid at position 23 that distinguishes human IFNα-2a (hIFNα-2a) from hIFNα-2b (K23 in hIFNα-2a and R23 in hIFNα-2b) (Fig. 15). Regarding the mechanism of drug action, PegIFNα-2a and PegIFNα-2b mainly interfere with viral replication in two aspects. First, they stimulate immunity cells (CD8+ cells and natural killer T cells) to enhance the noncytolytic clearance of viruses by cytokines or cytolysis of infected cells (344). Second, they stimulate the expression of innate antiviral genes and proteins (e.g., APOBEC3A/B and MxA) to block viral replication (344).
FIG 15.
Tertiary structures of interferons and chemical formulas of podofilox, imiquimod, and catechin. (A and B) Cartoon representations of interferon alfa 2a (PDB accession number 4YPG) and interferon alfa 2b (PDB accession number 1RH2). Sequence comparison suggests that amino acid K23 in interferon alfa 2a and amino acid R23 in interferon alfa 2b mark the only sequence difference between interferon alfa 2a and interferon alfa 2b. Structural movies are available online (http://www.virusface.com/). (C to E) Chemical formulas of podofilox, imiquimod, and catechin. Note that catechin is the major ingredient of the botanical drug sinecatechin.
In clinical practice, interferon-based treatments are infrequently used due to their multiple side effects, high costs, and inconvenience of administration (345). Importantly, a wide range of side effects with PegIFNα have been reported: fever, fatigue, bone marrow suppression, influenza-like symptoms, depression, and exacerbation or development of autoimmune illnesses (346). For this reason, PegIFNα-2a has been approved only for HBV-infected adults (180 μg/week for 48 weeks) but not for children (114, 271). Moreover, it remains debatable whether interferons should or should not be combined with other antiviral compounds (e.g., lamivudine, adefovir dipivoxil, TDF, or entecavir) (347–349). For instance, PegIFNα-2a plus adefovir dipivoxil may increase HBV-specific T cell restoration (349), whereas PegIFNα-2a with TDF-based therapies at 48 weeks does not increase the seroconversion rate of HBeAg-positive patients coinfected with HBV and HIV (350). Furthermore, PegIFNα-2a should not be used with telbivudine due to an increased risk of peripheral neuropathy (351). The added value of interferons in combination with nucleos(t)ide analogues warrants further investigation.
Immunostimulatory and Antimitotic Inhibitors
Approved by the FDA in February 1997, 5% imiquimod cream (Aldara) is a patient-applied immune response modifier for the treatment of external genital warts caused by HPV infections (352, 353). Imiquimod, 1-isobutyl-1H-imidazo[4,5-c]quinolin-4-amine (also known as R-837 and S-26308), is a nonnucleoside heterocyclic amine (Fig. 15). Although its antiviral activity could not be shown by in vitro experiments, imiquimod stimulates macrophages to secrete cytokines (e.g., interferon alpha, tumor necrosis factor alpha [TNF-α], interleukin-1 [IL-1], IL-6, and IL-8) for wart regression and local inflammatory reactions (352, 354). Clinical trials suggested that 5% imiquimod cream was safe and well tolerated in the treatment of external genital warts (352, 353, 355). Moreover, it is applied 3 times per week until complete clearance is achieved or for a maximum of 16 weeks, and the most common side effects are skin reactions (e.g., itching, burning, and erythema). Clearance rates with 5% imiquimod cream vary from 37% to 50%, and the recurrence rate is ∼13% (356).
A 15% sinecatechin ointment (Veregen) is the first FDA-approved botanical drug for the topical treatment of external genital warts (357). The name sinecatechins originates from the Latin name for Chinese green tea (Camellia sinensis) and its major chemical components (catechins) (357). Veregen is a purified product of catechins from leaves of Chinese green tea containing >80% catechins and polyphenols. Importantly, catechins (Fig. 15) are known for their antiangiogenic activity, anti-inflammatory and immunostimulatory activities, and antimicrobial potential (358). Two phase 3 clinical studies suggest that 15% sinecatechin ointment is a well-tolerated, self-applicable, and effective topical treatment to clear external genital warts (359, 360). The most common side effects with sinecatechins are local skin and application site reactions (e.g., erythema, pruritus, burning, pain, and erosion). The clearance rate with 15% sinecatechin ointment reaches ∼54%, and the recurrence rate is ∼7% at 12 weeks (356).
Podofilox (Condylox) is an antimitotic compound purified from crude podophyllum resin within the roots and rhizomes of May apple or podophyllum plant (either North American Podophyllum peltatum or Indian Podophyllum emodi) (361). Podofilox is safe and effective in the treatment of external genital warts but not mucous membrane warts (361, 362). Instead of targeting HPV proteins directly, podofilox is a cytotoxic drug with specific pharmacological actions against the formation of the mitotic spindle at metaphase, leading to the interruption of cell division (362, 363). Two topical treatments are currently approved for self-applicable administration: a 0.5% podofilox solution and a 0.5% podofilox gel. In particular, podofilox is applied when the areas of external warts are <10 cm2. The internal use of podofilox in either the vagina or the anus is not recommended. The most common side effects with podofilox are inflammation, burning, erosion, pain, or itching (364). Clearance rates with the 0.5% podofilox solution vary from 45% to 77%, and the recurrence rates are between 4% and 33% (356).
Antisense Oligonucleotides
Fomivirsen (Vitravene) is the first FDA-approved antisense oligonucleotide harboring a 21-nucleotide phosphorothioate oligonucleotide (5′-GCG TTT GCT CTT CTT CTT GCG-3′) (365). Based on its antisense mechanism, fomivirsen is complementary to a sequence in mRNA encoding major immediate early region 2 of HCMV; thus, the binding of fomivirsen to this region inhibits the gene expression of essential HCMV proteins (366). Fomivirsen sodium, administered as an intravitreal injection into human eyes, has been approved for treating HCMV retinitis in patients infected with AIDS (367). Despite the fact that it is well tolerated and has a favorable safety profile (368), intravitreous fomivirsen has been discontinued for commercial reasons.
FORTHCOMING ANTIVIRAL INHIBITORS
In addition to the 90 approved antiviral drugs, many experimental inhibitors have been under investigation in phase 3 clinical trials (http://www.clinicaltrials.gov/). For instance, besifovir is an HBV inhibitor showing an efficacy similar to that of the approved inhibitor entecavir (369), but its safety is worrying (370). As the first thiazolide in clinical trials, nitazoxanide may inhibit chronic HCV (371), whereas more randomized clinical trials with a low risk of bias are still needed (372). Development of many antiviral inhibitors still depends on the results of phase 3 trials, such as human monoclonal antibody REGN2222 against RSV (373) (ClinicalTrials.gov registration number NCT02325791), the HIV NNRTI doravirine (374) (registration number NCT02397096), and the HIV integrase inhibitor GS-9883 (registration numbers NCT02607930, NCT02607956, NCT02603120, and NCT02603107). Here, we provide an overview of four forthcoming antiviral drugs: (i) sofosbuvir plus velpatasvir for treatment of infections by HCV genotypes 1 to 6, (ii) daclatasvir plus asunaprevir with or without beclabuvir for treatment of HCV genotype 1 infections, (iii) FV100 for treatment of VZV infections, and (iv) letermovir for treatment of HCMV infections (Table 3).
Sofosbuvir plus Velpatasvir
The combination of sofosbuvir (400 mg) plus velpatasvir (100 mg) has been recognized as an effective pangenotypic therapy against infections by HCV genotypes 1 to 6 (375, 376). Sofosbuvir is an approved nucleoside compound that inhibits HCV NS5B polymerase activities (Fig. 13), while velpatasvir is an experimental inhibitor targeting HCV nonstructural protein NS5A (Fig. 12). HCV pangenotypic drugs may require no genotyping tests and potentially offer the simplest “test-and-cure” strategy to eliminate HCV infections (375). Supported by successful clinical trials, the once-daily fixed-dose combination of sofosbuvir plus velpatasvir was submitted to the FDA as a new drug application on 28 October 2015.
A number of clinical trials have been carried out to study the combination drug of sofosbuvir plus velpatasvir: (i) the ASTRAL-1 trial, which enrolled 740 HCV-infected patients with noncirrhotic or compensated cirrhosis, demonstrated the effectiveness of the combination of sofosbuvir plus velpatasvir against HCV genotype 1, 2, 4, 5, or 6 (377); (ii) the ASTRAL-2 and ASTRAL-3 trials, which enrolled 266 and 552 patients, respectively, suggested that therapy with sofosbuvir plus velpatasvir was superior to therapy with sofosbuvir plus ribavirin for treatment of infection by HCV genotype 2 or 3 (376); (iii) the ASTRAL-4 trial further revealed that sofosbuvir plus velpatasvir achieved high rates of SVR12 in 267 patients with HCV infection (genotypes 1 to 6) and decompensated cirrhosis (378); and (iv) two randomized clinical trials, which enrolled 321 and 377 patients, respectively, suggested that treatment with sofosbuvir (400 mg) plus velpatasvir (100 mg) provided remarkable rates of SVR12 in treatment-naive or treatment-experienced patients infected with HCV genotypes 1 to 6 (379, 380). The combination treatment in these clinical trials gave rise to common side effects such as fatigue, headache, insomnia, or nausea (376, 378–380). Nevertheless, given the 1,254 patients infected with HCV genotypes 1 to 6 in the six clinical trials described above, treatment with sofosbuvir (400 mg, once daily) plus velpatasvir (100 mg, once daily) showed a success rate of SVR12 of up to 97.4% (n = 1,221).
Daclatasvir plus Asunaprevir with or without Beclabuvir
To treat HCV genotype 1 or 4 infection, phase 3 clinical trials were established to study (i) a fixed-dose combination of daclatasvir (60 mg, once daily) plus asunaprevir (100 mg, twice daily) (285) and (ii) a twice-daily fixed-dose combination of daclatasvir (30 mg) plus asunaprevir (200 mg) plus beclabuvir (75 mg) (381, 382). Daclatasvir is an FDA-approved inhibitor targeting HCV NS5A (Fig. 12), and beclabuvir is an experimental inhibitor targeting HCV NS5B (Fig. 13). The combination of the HCV protease inhibitor asunaprevir with daclatasvir was approved in Japan, but the FDA has not approved this combination as of April 2016.
The effectiveness of daclatasvir plus asunaprevir plus beclabuvir has been demonstrated in recent clinical trials: (i) the phase 2 AI443014 trial, which enrolled 187 patients with HCV genotype 1 infection, revealed that the virologic response with daclatasvir plus asunaprevir plus beclabuvir (75 mg) was higher than that with daclatasvir plus asunaprevir plus beclabuvir (150 mg) (381); (ii) the phase 3 UNITY-1 trial, which enrolled 312 treatment-naive and 103 treatment-experienced noncirrhotic patients infected with chronic HCV genotype 1, suggested that daclatasvir plus asunaprevir plus beclabuvir achieved high rates (>89%) of SVR12 (382); and (iii) the phase 3 UNITY-2 trial, which enrolled 112 treatment-naive and 90 treatment-experienced patients infected with chronic HCV genotype 1 and with compensated cirrhosis, suggested that daclatasvir plus asunaprevir plus beclabuvir achieved promising rates (>85%) of SVR12 (383). The most common side effects with this combination drug were headache, diarrhea, fatigue, and nausea (381, 382). Given the 597 patients with HCV genotype 1 infection in the clinical trials described above, treatment with daclatasvir (30 mg) plus asunaprevir (200 mg) plus beclabuvir (75 mg) showed a success rate of SVR12 of up to 91.5% (n = 546).
FV100
FV100 (FV for FermaVir) has been developed as an effective, well-tolerated, once-daily treatment for herpes zoster or shingles, a painful rash caused by VZV infections (384). FV100 is a lipophilic bicyclic nucleoside analogue (Fig. 5) that inhibits the activity of the VZV DNA polymerase (385). In vitro experiments on VZV-infected cells at day 3 postinfection demonstrated that FV100 efficiently inhibited VZV replication at a 50% effective concentration (EC50) of 0.09 μM, which was more potent than BVDU (EC50 of 0.9μM) and acyclovir (EC50 of 9μM) (386).
A phase 1 study, which enrolled 107 VZV-infected patients (384), concluded that once-daily oral dosing of FV100 could be sufficient to maintain the drug concentration above the EC50 in vivo, and FV100 was well tolerated in elderly and young patients (385, 387). A phase 2 clinical trial, which enrolled 329 patients aged 50 years and older, evaluated the incidence of postherpetic neuralgia (PHN) for treatment with FV100 versus valacyclovir at 90 days. The PHN incidence rates with 200 mg FV100 (17.8%; 19/107) and 400 mg FV100 (12.4%; 14/113) were lower than that with 1,000 mg valacyclovir (20.2%; 22/109) (Contravir). To compare 400 mg FV100 with 1,000 mg valacyclovir, results of a phase 3 trial recruiting 985 patients will be released by the end of 2016 (ClinicalTrials.gov registration number NCT02412917).
Letermovir
Letermovir (MK-8228 or AIC246) is a 3,4-dihydro-quinazoline-4-yl-acetic acid derivative that targets the pUL56 subunit of the HCMV terminase complex to block viral DNA processing and/or packaging (388–390). Based on in vitro experiments, letermovir showed promising antiviral activity in different cell lines in comparisons of letermovir (EC50 of 0.0035 to 0.0056 μM) versus ganciclovir (EC50 of 0.32 to 2.39 μM) (391). The first proof-of-concept trial, which enrolled 27 transplant recipients with active HCMV infections, identified virus clearance in 6 of 12 patients (50%) who received 14 days of letermovir, in comparison to 2 of 7 patients (28.6%) who received the local standard of care (67). A phase 2 clinical trial, which enrolled 131 HCMV-seropositive allogeneic hematopoietic stem cell transplant recipients, demonstrated that the incidence of HCMV infection in patients who received once-daily doses of 240 mg letermovir (29%; 10/34) at 12 weeks was significantly lower than that in patients who received placebo (64%; 21/33) (392). In this phase 2 clinical trial, the letermovir resistance mutation V236M was identified in patients who failed treatment with a suboptimal letermovir concentration of 60 mg, but treatment with 240 mg letermovir at 12 weeks achieved complete suppression of viremia (393).
Letermovir at 240 mg had significant anti-HCMV activity, with an acceptable safety profile (392). Gastrointestinal disorders, including diarrhea, nausea, and vomiting, were common side effects in the phase 2 clinical trial (392). An ongoing phase 3 clinical trial, enrolling about 540 HCMV-seropositive allogeneic hematopoietic stem cell transplant recipients, will show the efficacy and safety of 240 mg letermovir in preventing HCMV infections 24 weeks after transplant actions (ClinicalTrials.gov registration number NCT02137772). Results of this clinical trial will be released in 2017.
ANTIVIRAL STRATEGIES AGAINST CURRENT AND EMERGING INFECTIOUS DISEASES
Emerging viral infections (e.g., Zika virus, dengue virus, and Ebola virus [EBOV]) are afflicting millions of humans worldwide. For this reason, there is growing interest in developing new treatments against emerging infectious diseases (394). Here, we highlight antiviral strategies against 41 infectious diseases. For convenience, we categorize these viruses into four groups: (i) viruses (n = 4) targeted by both approved vaccines and antiviral drugs, (ii) viruses (n = 5) targeted by approved antiviral drugs but not by vaccines, (iii) viruses (n = 13) targeted by approved vaccines but not by antiviral drugs, and (iv) viruses (n = 19) targeted by neither approved vaccines nor antiviral drugs.
Viruses Targeted by both Antiviral Drugs and Vaccines
As of April 2016, the FDA has approved vaccines and antiviral drugs to treat HBV, HPV, VZV, and influenza viruses. In addition to the antiviral drugs summarized above, here, we briefly describe FDA-approved vaccines.
HBV vaccines.
Three HBV vaccines (Pediarix, Engerix-B, and Recombivax HB) have been approved for all HBV genotypes. The effectiveness of universal HBV immunization in preventing chronic hepatitis B infections is ∼90 to 95% (395). Due to the success of HBV vaccines, the rate of global HBV vaccine coverage is ∼75%, and this rate is much higher in developed countries (89% in the United States and 91% in the Western Pacific) (395).
VZV vaccines.
As two live-attenuated VZV vaccines, Zostavax and Varivax were licensed against varicella in 1995 and against herpes zoster in 2006, respectively (80). Herpes zoster vaccines can efficiently protect older adults from herpes zoster diseases (396). The mean effectiveness of a single dose of the varicella vaccine is ∼80 to 85% against all levels of disease severity (397).
HPV vaccines.
Three vaccines have been approved for different HPV types: Cervarix for HPV-16 and HPV-18, Gardasil 9 for HPV-9, and Gardasil for HPV-6, HPV-11, HPV-16, and HPV-18. Routine vaccination using either Gardasil or Cervarix is currently recommended (398).
Influenza virus vaccines.
The FDA has approved (i) monovalent vaccines for influenza A (influenza A [H5N1] virus monovalent vaccine and influenza A [H1N1] 2009 virus monovalent vaccines), (ii) trivalent vaccines for influenza A and B viruses (Afluria, Agriflu, Fluad, Fluarix, Flublok, Flucelvax, FluLaval, Fluvirin, and Fluzone), and (iii) quadrivalent vaccines for influenza A and B viruses (FluMist, Fluarix, Fluzone, and FluLaval). Apart from their important roles against viral infections, influenza vaccines have their limitations (399, 400). First, after influenza vaccination, it takes up to 2 weeks in adults and 6 weeks in children to develop immunity. Patients might be vulnerable within this period. Second, the effectiveness of influenza vaccination is impaired by many factors (e.g., vaccine mismatch, immunosuppression, or lack of compliance). Third, due to emerging influenza virus strains, a new vaccine may not be available for periods of up to several months, and not all patients could be vaccinated in a time of need. Therefore, additional coverage by antiviral drugs (i.e., neuraminidase inhibitors) is still required. The significant variation of influenza virus strains may cause resistance to antiviral agents; thereby, optimal antiviral treatments are yet to be discovered (399, 401).
Viruses Targeted by Antiviral Drugs but Not by Vaccines
As of April 2016, the FDA has approved antiviral drugs for the treatment of HIV, HCV, HSV, RSV, and HCMV, but their vaccines are still lacking: (i) HIV and HCV vaccines are not available and will be unlikely to be available in the foreseeable future, so treatments of these infections depend solely on effective antiviral drugs that are currently available; (ii) although an effective HSV vaccine is still lacking, many HSV vaccine candidates (e.g., HSV529) are currently being tested in clinical trials (402, 403); (iii) there is no licensed vaccine for RSV, but a number of promising vaccine candidates (e.g., live-attenuated RSV vaccine MEDI-559) are currently being evaluated in advanced clinical trials (404, 405); and (iv) most HCMV vaccines are produced by either attenuating HCMV to generate modified-virus vaccines or isolating subunit viral antigens to generate individual-antigen vaccines (406). Clinical trials are currently being undertaken to evaluate promising candidates (e.g., AD169, Towne/Toledo chimeric vaccines, and DNA vaccines of gB and pp65) (406, 407). The development of HCMV vaccination still faces many challenges, such as the clinical selection of appropriate trial endpoints and the identification of viral antigens with desirable features for vaccine design (408).
Viruses Targeted by Vaccines but Not by Antiviral Drugs
As of April 2016, approved vaccines are available for 13 infectious diseases, but their antiviral drugs are still lacking. The list of approved vaccines could be summarized as follows: (i) human adenovirus vaccine (Adenovirus Type 4 and Type 7 Vaccine, Live, Oral), (ii) rotavirus vaccines (Rotarix for rotavirus serotype G1, G3, G4, or G9 and RotaTeq for rotavirus serotype G1, G2, G3, or G4), (iii) hepatitis A virus vaccines (Havrix and Vaqta), (iv) poliovirus vaccines (Kinrix, Quadracel, and Ipol), (v) yellow fever virus vaccine (YF-Vax), (vi) Japanese encephalitis virus vaccines (Ixiaro and JE-Vax), (vii) measles vaccines (M-M-R II and ProQuad), (viii) mumps vaccines (M-M-R II and ProQuad), (ix) rubella vaccines (M-M-R II and ProQuad), (x) varicella vaccine (ProQuad), (xi) rabies vaccines (Imovax and RabAvert), (xii) variola virus (smallpox) vaccine (ACAM2000), and (xiii) hepatitis E virus (HEV) vaccine (HEV239). HEV239 is the only HEV vaccine that was approved in China in 2012 (409), while many vaccine candidates are currently under examination in clinical trials (410).
In addition to the approved vaccines mentioned above, many antiviral agents have been designed. As an approved drug against HCMV, cidofovir can efficiently inhibit viral infections with human adenovirus, but clinical evidence is still lacking (411). Although no antiviral compound is formally approved for HEV, preliminary clinical observations suggest that pegylated interferon and ribavirin alone might offer a sustained virological response, but HEV clinical trials are still required (412). A number of promising compounds (e.g., hydantoin, guanidine hydrochloride, l-buthionine sulfoximine, and Py-11) can inhibit viral replication of picornavirus in vitro, but in vivo evidence from clinical trials is largely lacking (413). As for rabies infections, they are generally treatable by using postexposure prophylaxis with the administration of rabies immunoglobulin and vaccine (414). Postexposure prophylaxis must be initiated soon after rabies exposures, mostly through animal bites (415). For viral infections like polio, yellow fever, and measles, adequate protection can be achieved by vaccination in some circumstances, but the coverage of antiviral drugs is currently not available.
Off-label drugs might be considered valuable options when licensed treatments are not available. For instance, cidofovir might be an off-label prescription to treat various DNA virus infections such as human polyomavirus, adenovirus, and smallpox (416). Three drugs (foscarnet, ganciclovir, and cidofovir) approved for HCMV can also inhibit the viral DNA polymerase of human herpesvirus 6 (HHV-6) (127). Despite this, the effectiveness of off-label drugs is yet to be fully proven in clinical trials.
Viruses Targeted by neither Vaccines nor Antiviral Drugs
Apart from 22 well-known viruses targeted by vaccines and/or antiviral drugs, a great number of emerging infectious diseases without any licensed treatments are currently afflicting millions of patients (417). Therefore, a great deal of attention has been paid to many emerging viruses, such as Epstein-Barr virus (EBV) (418), human parvovirus B19 (419, 420), human norovirus (421), human rhinovirus (422), human herpesvirus 6 (127), human coronavirus (423), human astrovirus (424), human sapovirus (425), chikungunya virus (324), dengue virus (426), West Nile virus (427), Hendra virus (328), Nipah virus (328), Ebola virus (428, 429), Marburg virus (MARV) (429), Lassa virus (430), Junin virus (430), Machupo virus (431), and, most recently, Zika virus (432). Here, we briefly discuss antiviral strategies against these emerging infectious diseases.
dsDNA viruses: EBV, human polyomavirus, and herpesvirus 6.
EBV, also called human herpesvirus 4, was first reported in 1964. Many antiviral drugs (e.g., valacyclovir, ganciclovir, and valganciclovir) can actively inhibit EBV replication in vitro or in small clinical trials, but large-scale clinical trials are still required (418, 433). EBV vaccines have been generated based on the EBV envelope glycoprotein GP350 and CD8+ T cell peptide epitopes, but their effectiveness requires further improvement (418).
Human polyomavirus was first discovered by Ludwik Gross in 1953 (434). The best-known types of human polyomaviruses are JC and BK viruses, which infect >80% of adult populations (435). Recognized as promising drug candidates, human monoclonal antibodies target viral protein 1 of JC virus to inhibit JC virus infections, and they exert cross-reactivity against many JC virus strains (436). Cidofovir might be an off-label drug to treat various DNA virus infections (e.g., human polyomavirus) (416).
Human herpesvirus 6 was first isolated in patients with lymphoproliferative disorders in 1986 (437). There is no vaccine or drug licensed for human herpesvirus 6, but one experimental compound {(R)-9-[4-hydroxy-2-(hydroxymethyl)butyl]guanine (H2G)} and four drugs (ganciclovir, foscarnet, cidofovir, and artesunate) approved for other clinical uses are under investigation (127).
ssDNA virus: human parvovirus B19.
Human parvovirus B19, discovered in 1975, is the best-known virus in the group of ssDNA viruses. Most infections by human parvovirus B19 in immunocompetent patients do not require any treatment, because the symptoms are transient (420). Although controlled studies are still required, intravenous immunoglobulin (IVIG) therapy has been recognized as a popular alternative because it offers a good source of neutralizing antibodies in immunocompromised patients exposed to human parvovirus B19 (419). Intravenous immunoglobulin therapy substantially increases reticulocyte counts and hemoglobin levels, but 33.9% of treated patients may have a relapse at a mean of 4.3 months (438). Apart from neutralizing antibodies, a recent study suggests that cidofovir at 500 μM could significantly reduce virus infectivity in vitro, but clinical evidence is still required (439).
Positive-sense ssRNA viruses: Zika virus, norovirus, coronavirus, rhinovirus, astrovirus, sapovirus, dengue virus, chikungunya virus, and West Nile virus.
Zika virus, discovered in 1947, was first isolated in a monkey in the Zika forest of Uganda (440). Since the first outbreak of Zika virus in the Yap Islands in 2007, Zika virus transmissions have been reported in 64 countries according to a WHO report on 13 April 2016 (http://www.who.int/). Recent evidence suggests that ∼0.95% of Zika virus infections in pregnant women may lead to microcephaly (abnormally small head) in infants (441). Zika virus infections are also associated with severe neurological complications such as Guillain-Barré syndrome (440). Unfortunately, a vaccine, antiviral compound, or good serological test is not available for Zika virus today (442). Vaccine candidates are now under development, but a safe and effective vaccine will probably take 3 to 10 years (443, 444). Currently, the best prevention, especially for pregnant women and infants, is to avoid mosquito exposure because Zika virus is transmitted mainly by infected mosquitoes.
Human norovirus was first identified in stored human stool samples in 1972. Virus-like particles containing norovirus genotype GI.1/GII.4 have been designed as vaccine candidates, and their effectiveness seems promising in phase 1 clinical trials (421). Many antiviral agents (e.g., EV71, ribavirin, and favipiravir) efficiently inhibit norovirus protease or RNA polymerase, but their development is still at an early stage (325, 326).
Human coronavirus, discovered in the 1960s, is known to cause severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) (423). Many antiviral candidates (e.g., corticosteroids) potentially inhibit human coronavirus, and more details have been elucidated in recent review articles (445–447).
Human rhinovirus, first discovered in the 1950s, is the most common cause of upper respiratory tract infections (422). There is no vaccine or drug licensed for human rhinovirus, but a number of antiviral agents (e.g., pleconaril, vapendavir, and pirodavir) have been under investigation (422). However, it remains a challenge to develop rhinovirus drugs and vaccines, because the rhinovirus genome, classified into >100 serotypes, is highly variable (422).
Dengue, chikungunya, and West Nile viruses from the family Flaviviridae are mosquito-borne viruses that pose significant risks to human health throughout the world (448, 449). Dengue virus, discovered in the 1960s, is the cause of several pandemics (426). Many experimental inhibitors (e.g., sinefungin, SDM25N, and CCG-3394) have been designed to target the NS4B and NS5 proteins of dengue virus (450, 451). Although a number of vaccine candidates (e.g., CYD-TDV and TDEN) have reached advanced clinical trials (452, 453), it remains a challenge to develop dengue virus vaccines with optimal efficacy against all 4 dengue virus serotypes. As for the treatment of chikungunya virus, many antiviral drugs (ribavirin and pegylated interferon alfa) and experimental agents (e.g., chloroquine, arbidol, and chlorpromazine) may interfere with different stages of the virus life cycle (324), but clinical evidence is largely lacking. Regarding the treatment of West Nile virus, veterinary vaccines have been licensed for use in horses and dogs (454, 455). Nevertheless, vaccine candidates (454, 455) and small-molecule inhibitors (456, 457) against human West Nile virus are still under investigation.
Human astrovirus (424) and sapovirus (425) were first discovered in human diarrheic stool samples in 1975 and 1976, respectively. Astrovirus and sapovirus infections cause acute gastroenteritis in humans and animals (424, 425). Due to the lack of commercial interest, the development of vaccines and antiviral agents against human astrovirus and sapovirus is rather slow. However, improved sanitation and hygiene can efficiently prevent viral infections, because astrovirus and sapovirus are transmitted primarily through the fecal-oral route (424, 425).
Negative-sense ssRNA viruses: Ebola, Marburg, Hendra, Nipah, Lassa, Junin, and Machupo viruses.
Ebola and Marburg viruses from the family Filoviridae were first discovered in 1976 and 1967, respectively. Both zoonotic viruses were originally transmitted from bats to humans (458). As of April 2016, there is no vaccine or antiviral drug licensed for EBOV and MARV. Phase 1/2 clinical trials have been undertaken to prove the effectiveness of treatment candidates such as favipiravir, EBOV glycoprotein vaccine (EBOVGP), and ZMapp (334, 428, 459). Moreover, convalescent-phase plasma transfusions from disease survivors might offer a valuable anti-EBOV option in resource-limited settings (459). Therapeutic strategies using chemical agents (e.g., neplanocin A, BCX4430, and lectins) against Ebola virus infections have been reviewed elsewhere (337, 460). As for the treatment of MARV infections, no drug or vaccine has been licensed, but supportive therapies are regularly applied in clinical practice (327). A recent study suggests that AVI-7288, which is a phosphorodiamidate morpholino oligomer, potentially acts as postexposure prophylaxis for MARV infections in humans (461). The efficacy of antiviral candidates (e.g., ribavirin, PMO-Plus, and monoclonal antibodies) against MARV has yet to be fully proven in clinical trials (327).
Hendra and Nipah viruses from the family Paramyxoviridae were first identified in 1994 and 1999, respectively. In Australia, Equivac HeV has been approved as a Hendra virus vaccine in horses (328). However, human vaccine development is hindered by limited commercial benefits, because only 7 human Hendra virus infections have been reported since 1994 (462). As for Nipah virus infections, vaccine candidates (e.g., Hendra virus soluble G glycoprotein subunit vaccine [HeV-sG]) are currently being investigated at a preclinical stage (463). Based on in vitro experiments, ribavirin can efficiently inhibit henipavirus replication (328). Moreover, preliminary clinical observations suggest that ribavirin may inhibit human Hendra and Nipah virus infections, despite controversial results being reported in different studies (328). Although more clinical evidence is still needed, ribavirin might be used as an off-label treatment for henipavirus infections in the absence of other therapies (328).
Junin, Lassa, and Machupo viruses are human arenaviruses from the family Arenaviridae. It has been shown that favipiravir can efficiently inhibit viral replication of arenaviruses (Junin, Machupo, and Pichinde viruses) (338, 339). For vaccine development, human HLA class I-restricted epitopes have been explored for human arenaviruses (430). A number of Lassa and Junin virus vaccine candidates (e.g., Candid#1, ML-29, and Tacaribe virus [TACV] vaccine) have been tested in human or animal trials (430). However, vaccine development for Lassa virus and filoviruses is hindered by a lack of commercial interest (464).
Overall, for the control of infectious diseases, both vaccination and antiviral drugs could be envisaged, but the availability of antiviral treatments varies from one virus to another. As of April 2016, 22 infectious diseases are currently treated by licensed vaccines and/or antiviral drugs, but a broad spectrum of emerging viruses is still at large. It is known that viruses from the same family usually share similar features (465), and many emerging viruses come from such virus families that possess at least one virus targeted by vaccines and/or antiviral drugs. Therefore, FDA-approved treatments might be active against emerging infectious diseases in some circumstances.
CONCLUSIONS AND FUTURE PERSPECTIVES
To our knowledge, this article presents for the first time a comprehensive overview of 90 antiviral drugs approved over the past 50 years (Fig. 1). These antiviral drugs approved for the treatment of 9 human infectious diseases have saved tens of millions of human beings over 5 decades, and they will continue to be essential for antiviral treatments against current and emerging viral infections (Fig. 2). As of April 2016, various antiviral drugs offer promising activities against HCV infections, but a definitive cure for HIV, HBV, HCMV, HPV, HSV, RSV, VZV, or influenza virus is yet to be discovered. In addition to approved antiviral drugs, our review also highlights several forthcoming antiviral regimens in phase 3 clinical trials (Table 3), because promising inhibitors (e.g., marine natural products [394]) have continuously been developed to fight against current and emerging infectious diseases.
During the past 5 decades, great achievements have been made in the field of antiviral drug discovery. As of April 2016, many antiviral drugs and/or vaccines have been approved for the treatment of 22 infectious diseases: HIV, HBV, HCV, HCMV, HPV, HSV, RSV, VZV, influenza virus, smallpox, rotavirus, human adenovirus, human herpesvirus 6, poliovirus, hepatitis A virus, hepatitis E virus, Japanese encephalitis virus, yellow fever, rubella, measles, mumps, and rabies (Table 4). Nevertheless, there is still no antiviral drug or vaccine for more than 200 infectious diseases that are afflicting human populations worldwide. In order to highlight the latest progress in antiviral drug discovery, our review provides a brief summary of potential antiviral agents and vaccines against 41 infectious diseases. It is our belief that new antiviral treatments will be formally approved to cure a broad range of emerging infectious diseases in the future.
TABLE 4.
Control of viral infections using approved vaccines and/or antiviral drugs
| Group | Family | Virus(es) | Vaccine | Antiviral drug |
|---|---|---|---|---|
| I (dsDNA) | Adenoviridae | Human adenovirus | Yes | Off-label druga |
| Hepadnaviridae | HBV | Yes | Yes | |
| Herpesviridae | VZV (shingles) | Yes | Yes | |
| HSV, HCMV | No | Yes | ||
| EBV | No | No | ||
| Human herpesvirus 6 | No | Off-label druga | ||
| Papillomaviridae | HPV | Yes | Yesb | |
| Polyomaviridae | Human polyomavirus | No | Off-label druga | |
| Poxviridae | Variola virus (smallpox) | Yes | Off-label druga | |
| II (ssDNA) | Parvoviridae | Human parvovirus | No | No |
| III (dsRNA) | Reoviridae | Rotavirus | Yes | No |
| IV [(+)ssRNA] | Astroviridae | Human astrovirus | No | No |
| Caliciviridae | Human sapovirus | No | No | |
| Coronaviridae | Human coronavirus | No | No | |
| Flaviviridae | HCV | No | Yes | |
| Yellow fever virus | Yes | No | ||
| Japanese encephalitis virus | Yes | No | ||
| Dengue, West Nile, Zika viruses | No | No | ||
| Hepeviridae | Hepatitis E virus | Yesc | No | |
| Picornaviridae | Hepatitis A virus, poliovirus | Yes | No | |
| Norovirus, rhinovirus | No | No | ||
| Togaviridae | Rubella virus | Yes | No | |
| Chikungunya virus | No | No | ||
| V [(−)ssRNA] | Arenaviridae | Lassa, Junin, Machupo viruses | No | No |
| Filoviridae | Ebola, Marburg viruses | No | No | |
| Orthomyxoviridae | Influenza virus | Yes | Yes | |
| Paramyxoviridae | RSV | No | Yes | |
| Measles, mumps | Yes | No | ||
| Hendra, Nipah viruses | No | Off-label druga | ||
| Rhabdoviridae | Rabies | Yes | No | |
| VI [(+)ssRNA] | Retroviridae | HIV | No | Yes |
Cidofovir might be an off-label prescription to treat human polyomavirus, adenovirus, and smallpox. Foscarnet, ganciclovir, and cidofovir might be off-label drugs for HHV-6. Ribavirin might be an off-label prescription for Hendra and Nipah virus infections.
Three FDA-approved drugs (sinecatechins, podofilox, and imiquimod) are available for the treatment of external genital warts caused by HPV (354). However, these drugs may not target HPV proteins directly.
The HEV vaccine HEV239 was approved in China in 2012.
Importantly, antiviral compounds with broad-spectrum activity against different virus genotypes or subtypes are still welcome, because the effectiveness of most antiviral drugs is limited to only certain viral strains (466). For instance, some antiviral drugs (e.g., amprenavir) inhibit only HIV-1 but not HIV-2 (173). Many HCV inhibitors have been approved only for HCV genotype 1 but not for other genotypes (Table 2). Nevertheless, a number of antiviral inhibitors (brivudine, acyclovir, TDF, foscarnet, famciclovir, lamivudine, ribavirin, valacyclovir, PegIFNα-2a, and PegIFNα-2b) have been licensed for the treatment of more than one virus (Table 2), supporting the idea of developing antiviral drugs against multiple infectious diseases in the future.
Despite the rapid advancement of pharmaceutical and biotechnological approaches (e.g., RNA interference [RNAi] [467]), the development of successful antiviral treatments remains a challenge. First, potent antiviral drugs that counteract the highly variable nature of virus genomes are still required, because emerging drug resistance mutations remain a major cause of treatment failure (10, 466, 468, 469). Second, it is difficult to eradicate viral reservoirs using antiviral agents, because DNA viruses and retroviruses can integrate their genomes into human genomes (470, 471). Third, it remains a challenge to rapidly develop antiviral drugs and vaccines against emerging infectious diseases, calling for a joint effort between scientific and industrial partners. Fourth, it is a challenge to pursue effective, low-toxicity, and well-tolerated drugs that enhance patient compliance and drug administration (472). Fifth, efficient antiviral treatments against viral coinfections (e.g., HIV/HBV coinfections [473]) require further investigations. Sixth, access to and delivery of costly new therapies are becoming increasingly problematic in resource-limited settings (474). Political and financial commitment is also vital to eliminate substandard and counterfeit antiviral drugs that threaten global public health (475).
Encouraged by the accelerated pace of drug discovery in the past 5 decades, we anticipate that novel antiviral therapeutics will ultimately contribute to elimination and eradication strategies against human infectious diseases in the future.
Supplementary Material
ACKNOWLEDGMENTS
We wholeheartedly thank Christiane Callebaut for her proficient editorial assistance. We also thank Patrick Lane for his graphical design of Fig. 2, 3, and 4.
Guangdi Li was supported by the National Basic Research Program of China (grant 2014CB910500), the National Nature Science Foundation of China (grant 31571368), and the Project of Innovation-Driven Plan of Central South University (grant 2016CX031).
Biographies

Erik De Clercq, M.D. Ph.D., is a professor emeritus at the KU Leuven, Belgium, and a visiting professor at the University of South Bohemia (České Budějovice) in the Czech Republic. His research interests are embraced within the broad areas of microbiology, virology, molecular biology, and antiviral research, focusing on HIV, HBV, HCV, influenza virus, VZV, herpesvirus, and emerging viruses (e.g., Ebola, dengue, and chikungunya viruses). Over a period of 5 decades, he has developed new antiviral medicines such as nucleotide analogues (e.g., tenofovir), and he has coinvented several approved antiviral drugs, such as BVDU (brivudine), amino acyl esters of acyclovir (e.g., valacyclovir), acyclic nucleoside phosphonates (ANPs) (cidofovir, tenofovir, and adefovir dipivoxil), nonnucleoside reverse transcriptase inhibitors, and HEPT and TIBO derivatives leading to rilpivirine for the treatment of AIDS. Since the start of his academic career in 1967, Prof. De Clercq has published more than 2,700 research articles (http://www.virusface.com/).

Guangdi Li, Ph.D., received his doctoral degree in Biomedical Sciences from the Faculty of Medicine, KU Leuven, Belgium, in 2014. In 2006, he obtained his bachelor's degree in Applied Mathematics at Hunan University. Between 2006 and 2009, he pursued his master's degree in Computer Science at Shandong University and received full scholarships to work as a research assistant at the Technical University of Madrid, Spain. Between 2009 and 2014, he undertook his doctorate training in the Faculty of Medicine, KU Leuven, Belgium. During his Ph.D., he also received extensive training from the Master of Science in Molecular and Cellular Biophysics Program, Faculty of Science, KU Leuven. Since 2015, he has become a research fellow at the Second Xiangya Hospital, Central South University, Changsha, Hunan, China. His research interests are focused on antiviral drug and vaccine development, genome-wide diversity, viral coevolution, and the interactions of viral pathogens (http://www.virusface.com/).
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/CMR.00102-15.
REFERENCES
- 1.De Clercq E. 2004. Antivirals and antiviral strategies. Nat Rev Microbiol 2:704–720. doi: 10.1038/nrmicro975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Clercq E. 2002. Strategies in the design of antiviral drugs. Nat Rev Drug Discov 1:13–25. doi: 10.1038/nrd703. [DOI] [PubMed] [Google Scholar]
- 3.De Clercq E. 1997. In search of a selective antiviral chemotherapy. Clin Microbiol Rev 10:674–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Clercq E. 2009. The history of antiretrovirals: key discoveries over the past 25 years. Rev Med Virol 19:287–299. doi: 10.1002/rmv.624. [DOI] [PubMed] [Google Scholar]
- 5.De Clercq E. 2009. Anti-HIV drugs: 25 compounds approved within 25 years after the discovery of HIV. Int J Antimicrob Agents 33:307–320. doi: 10.1016/j.ijantimicag.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 6.Woolhouse M, Scott F, Hudson Z, Howey R, Chase-Topping M. 2012. Human viruses: discovery and emergence. Philos Trans R Soc Lond B Biol Sci 367:2864–2871. doi: 10.1098/rstb.2011.0354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallo RC, Montagnier L. 2003. The discovery of HIV as the cause of AIDS. N Engl J Med 349:2283–2285. doi: 10.1056/NEJMp038194. [DOI] [PubMed] [Google Scholar]
- 8.Barre-Sinoussi F, Chermann JC, Rey F, Nugeyre MT, Chamaret S, Gruest J, Dauguet C, Axler-Blin C, Vezinet-Brun F, Rouzioux C, Rozenbaum W, Montagnier L. 1983. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science 220:868–871. doi: 10.1126/science.6189183. [DOI] [PubMed] [Google Scholar]
- 9.Muller B, Heilemann M. 2013. Shedding new light on viruses: super-resolution microscopy for studying human immunodeficiency virus. Trends Microbiol 21:522–533. doi: 10.1016/j.tim.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 10.Li G, Piampongsant S, Faria NR, Voet A, Pineda-Pena AC, Khouri R, Lemey P, Vandamme A-M, Theys K. 2015. An integrated map of HIV genome-wide variation from a population perspective. Retrovirology 12:18. doi: 10.1186/s12977-015-0148-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharp PM, Hahn BH. 2011. Origins of HIV and the AIDS pandemic. Cold Spring Harb Perspect Med 1:a006841. doi: 10.1101/cshperspect.a006841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rambaut A, Posada D, Crandall KA, Holmes EC. 2004. The causes and consequences of HIV evolution. Nat Rev Genet 5:52–61. doi: 10.1038/nrg1246. [DOI] [PubMed] [Google Scholar]
- 13.Faria NR, Rambaut A, Suchard MA, Baele G, Bedford T, Ward MJ, Tatem AJ, Sousa JD, Arinaminpathy N, Pepin J, Posada D, Peeters M, Pybus OG, Lemey P. 2014. HIV epidemiology. The early spread and epidemic ignition of HIV-1 in human populations. Science 346:56–61. doi: 10.1126/science.1256739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tebit DM, Arts EJ. 2011. Tracking a century of global expansion and evolution of HIV to drive understanding and to combat disease. Lancet Infect Dis 11:45–56. doi: 10.1016/S1473-3099(10)70186-9. [DOI] [PubMed] [Google Scholar]
- 15.D'Arc M, Ayouba A, Esteban A, Learn GH, Boue V, Liegeois F, Etienne L, Tagg N, Leendertz FH, Boesch C, Madinda NF, Robbins MM, Gray M, Cournil A, Ooms M, Letko M, Simon VA, Sharp PM, Hahn BH, Delaporte E, Mpoudi Ngole E, Peeters M. 2015. Origin of the HIV-1 group O epidemic in western lowland gorillas. Proc Natl Acad Sci U S A 112:E1343–E1352. doi: 10.1073/pnas.1502022112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mourez T, Simon F, Plantier JC. 2013. Non-M variants of human immunodeficiency virus type 1. Clin Microbiol Rev 26:448–461. doi: 10.1128/CMR.00012-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Veugelers PJ, Schechter MT. 1997. The incubation period of HIV infection. Curr Opin Infect Dis 10:7–11. doi: 10.1097/00001432-199702000-00003. [DOI] [Google Scholar]
- 18.Chu C, Selwyn PA. 2011. Complications of HIV infection: a systems-based approach. Am Fam Physician 83:395–406. [PubMed] [Google Scholar]
- 19.Shepard CW, Finelli L, Alter MJ. 2005. Global epidemiology of hepatitis C virus infection. Lancet Infect Dis 5:558–567. doi: 10.1016/S1473-3099(05)70216-4. [DOI] [PubMed] [Google Scholar]
- 20.Catanese MT, Uryu K, Kopp M, Edwards TJ, Andrus L, Rice WJ, Silvestry M, Kuhn RJ, Rice CM. 2013. Ultrastructural analysis of hepatitis C virus particles. Proc Natl Acad Sci U S A 110:9505–9510. doi: 10.1073/pnas.1307527110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moradpour D, Penin F. 2013. Hepatitis C virus proteins: from structure to function. Curr Top Microbiol Immunol 369:113–142. doi: 10.1007/978-3-642-27340-7_5. [DOI] [PubMed] [Google Scholar]
- 22.Wilkins T, Malcolm JK, Raina D, Schade RR. 2010. Hepatitis C: diagnosis and treatment. Am Fam Physician 81:1351–1357. [PubMed] [Google Scholar]
- 23.Cuypers L, Li G, Libin P, Piampongsant S, Vandamme A-M, Theys K. 2015. Genetic diversity and selective pressure in hepatitis C virus genotypes 1-6: significance for direct-acting antiviral treatment and drug resistance. Viruses 7:5018–5039. doi: 10.3390/v7092857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simmonds P. 2013. The origin of hepatitis C virus. Curr Top Microbiol Immunol 369:1–15. doi: 10.1007/978-3-642-27340-7_1. [DOI] [PubMed] [Google Scholar]
- 25.Hoofnagle JH. 1997. Hepatitis C: the clinical spectrum of disease. Hepatology 26:15S–20S. doi: 10.1002/hep.510260703. [DOI] [PubMed] [Google Scholar]
- 26.Manns MP, Wedemeyer H, Cornberg M. 2006. Treating viral hepatitis C: efficacy, side effects, and complications. Gut 55:1350–1359. doi: 10.1136/gut.2005.076646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pfaender S, Brown RJ, Pietschmann T, Steinmann E. 2014. Natural reservoirs for homologs of hepatitis C virus. Emerg Microbes Infect 3:e21. doi: 10.1038/emi.2014.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White MK, Pagano JS, Khalili K. 2014. Viruses and human cancers: a long road of discovery of molecular paradigms. Clin Microbiol Rev 27:463–481. doi: 10.1128/CMR.00124-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taubenberger JK, Morens DM. 2009. Pandemic influenza—including a risk assessment of H5N1. Rev Sci Tech 28:187–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Potter CW. 2001. A history of influenza. J Appl Microbiol 91:572–579. doi: 10.1046/j.1365-2672.2001.01492.x. [DOI] [PubMed] [Google Scholar]
- 31.Smith W, Andrewes CH, Laidlaw PP. 1933. A virus obtained from influenza patients. Lancet 222:66–68. doi: 10.1016/S0140-6736(00)78541-2. [DOI] [Google Scholar]
- 32.Harris A, Cardone G, Winkler DC, Heymann JB, Brecher M, White JM, Steven AC. 2006. Influenza virus pleiomorphy characterized by cryoelectron tomography. Proc Natl Acad Sci U S A 103:19123–19127. doi: 10.1073/pnas.0607614103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Medina RA, Garcia-Sastre A. 2011. Influenza A viruses: new research developments. Nat Rev Microbiol 9:590–603. doi: 10.1038/nrmicro2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peiris JS, de Jong MD, Guan Y. 2007. Avian influenza virus (H5N1): a threat to human health. Clin Microbiol Rev 20:243–267. doi: 10.1128/CMR.00037-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horimoto T, Kawaoka Y. 2005. Influenza: lessons from past pandemics, warnings from current incidents. Nat Rev Microbiol 3:591–600. doi: 10.1038/nrmicro1208. [DOI] [PubMed] [Google Scholar]
- 36.Chan JF, To KK, Tse H, Jin DY, Yuen KY. 2013. Interspecies transmission and emergence of novel viruses: lessons from bats and birds. Trends Microbiol 21:544–555. doi: 10.1016/j.tim.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. 2005. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med 352:1749–1759. doi: 10.1056/NEJMoa043951. [DOI] [PubMed] [Google Scholar]
- 38.Liljeroos L, Krzyzaniak MA, Helenius A, Butcher SJ. 2013. Architecture of respiratory syncytial virus revealed by electron cryotomography. Proc Natl Acad Sci U S A 110:11133–11138. doi: 10.1073/pnas.1309070110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Empey KM, Peebles RS Jr, Kolls JK. 2010. Pharmacologic advances in the treatment and prevention of respiratory syncytial virus. Clin Infect Dis 50:1258–1267. doi: 10.1086/651603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tabatabai J, Prifert C, Pfeil J, Grulich-Henn J, Schnitzler P. 2014. Novel respiratory syncytial virus (RSV) genotype ON1 predominates in Germany during winter season 2012-13. PLoS One 9:e109191. doi: 10.1371/journal.pone.0109191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Collins PL, Graham BS. 2008. Viral and host factors in human respiratory syncytial virus pathogenesis. J Virol 82:2040–2055. doi: 10.1128/JVI.01625-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Domachowske JB, Rosenberg HF. 1999. Respiratory syncytial virus infection: immune response, immunopathogenesis, and treatment. Clin Microbiol Rev 12:298–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, O'Brien KL, Roca A, Wright PF, Bruce N, Chandran A, Theodoratou E, Sutanto A, Sedyaningsih ER, Ngama M, Munywoki PK, Kartasasmita C, Simoes EA, Rudan I, Weber MW, Campbell H. 2010. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet 375:1545–1555. doi: 10.1016/S0140-6736(10)60206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blumberg BS. 1997. Hepatitis B virus, the vaccine, and the control of primary cancer of the liver. Proc Natl Acad Sci U S A 94:7121–7125. doi: 10.1073/pnas.94.14.7121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sells MA, Chen ML, Acs G. 1987. Production of hepatitis B virus particles in Hep G2 cells transfected with cloned hepatitis B virus DNA. Proc Natl Acad Sci U S A 84:1005–1009. doi: 10.1073/pnas.84.4.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li G, Amini-Bavil-Olyaee S, Thomas M, Lemey P, Maes P, Van Ranst M, Pourkarim MR. 2015. HBV genome-wide diversity from the world population perspective, abstr P-144 Abstr 6th Int Tehran Hepat Conf, Shiraz, Iran. [Google Scholar]
- 47.Drexler JF, Geipel A, Konig A, Corman VM, van Riel D, Leijten LM, Bremer CM, Rasche A, Cottontail VM, Maganga GD, Schlegel M, Muller MA, Adam A, Klose SM, Carneiro AJ, Stocker A, Franke CR, Gloza-Rausch F, Geyer J, Annan A, Adu-Sarkodie Y, Oppong S, Binger T, Vallo P, Tschapka M, Ulrich RG, Gerlich WH, Leroy E, Kuiken T, Glebe D, Drosten C. 2013. Bats carry pathogenic hepadnaviruses antigenically related to hepatitis B virus and capable of infecting human hepatocytes. Proc Natl Acad Sci U S A 110:16151–16156. doi: 10.1073/pnas.1308049110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Winer BY, Ploss A. 2015. Determinants of hepatitis B and delta virus host tropism. Curr Opin Virol 13:109–116. doi: 10.1016/j.coviro.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mast EE, Margolis HS, Fiore AE, Brink EW, Goldstein ST, Wang SA, Moyer LA, Bell BP, Alter MJ, Advisory Committee on Immunization Practices. 2005. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) part 1. Immunization of infants, children, and adolescents. MMWR Recommend Rep 54:1–31. doi: 10.1542/peds.2006-1181. [DOI] [PubMed] [Google Scholar]
- 50.zur Hausen H. 2009. Papillomaviruses in the causation of human cancers—a brief historical account. Virology 384:260–265. doi: 10.1016/j.virol.2008.11.046. [DOI] [PubMed] [Google Scholar]
- 51.Moody CA, Laimins LA. 2010. Human papillomavirus oncoproteins: pathways to transformation. Nat Rev Cancer 10:550–560. doi: 10.1038/nrc2886. [DOI] [PubMed] [Google Scholar]
- 52.Schelhaas M, Shah B, Holzer M, Blattmann P, Kuhling L, Day PM, Schiller JT, Helenius A. 2012. Entry of human papillomavirus type 16 by actin-dependent, clathrin- and lipid raft-independent endocytosis. PLoS Pathog 8:e1002657. doi: 10.1371/journal.ppat.1002657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ganguly N, Parihar SP. 2009. Human papillomavirus E6 and E7 oncoproteins as risk factors for tumorigenesis. J Biosci 34:113–123. doi: 10.1007/s12038-009-0013-7. [DOI] [PubMed] [Google Scholar]
- 54.Doorbar J, Egawa N, Griffin H, Kranjec C, Murakami I. 2015. Human papillomavirus molecular biology and disease association. Rev Med Virol 25(Suppl 1):2–23. doi: 10.1002/rmv.1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schiller JT, Lowy DR. 2012. Understanding and learning from the success of prophylactic human papillomavirus vaccines. Nat Rev Microbiol 10:681–692. doi: 10.1038/nrmicro2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Workowski KA, Bolan GA, Centers for Disease Control and Prevention. 2015. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recommend Rep 64:1–137. doi: 10.15585/mmwr.rr6404a1. [DOI] [Google Scholar]
- 57.Bonagura VR, Hatam LJ, Rosenthal DW, de Voti JA, Lam F, Steinberg BM, Abramson AL. 2010. Recurrent respiratory papillomatosis: a complex defect in immune responsiveness to human papillomavirus-6 and -11. APMIS 118:455–470. doi: 10.1111/j.1600-0463.2010.02617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Juckett G, Hartman-Adams H. 2010. Human papillomavirus: clinical manifestations and prevention. Am Fam Physician 82:1209–1213. [PubMed] [Google Scholar]
- 59.Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, Vignat J, Ferlay J, Bray F, Plummer M, Franceschi S. 2012. Global burden of human papillomavirus and related diseases. Vaccine 30(Suppl 5):F12–F23. doi: 10.1016/j.vaccine.2012.07.055. [DOI] [PubMed] [Google Scholar]
- 60.Ho M. 2008. The history of cytomegalovirus and its diseases. Med Microbiol Immunol 197:65–73. doi: 10.1007/s00430-007-0066-x. [DOI] [PubMed] [Google Scholar]
- 61.Landolfo S, Gariglio M, Gribaudo G, Lembo D. 2003. The human cytomegalovirus. Pharmacol Ther 98:269–297. doi: 10.1016/S0163-7258(03)00034-2. [DOI] [PubMed] [Google Scholar]
- 62.Britt WJ, Boppana S. 2004. Human cytomegalovirus virion proteins. Hum Immunol 65:395–402. doi: 10.1016/j.humimm.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 63.Coaquette A, Bourgeois A, Dirand C, Varin A, Chen W, Herbein G. 2004. Mixed cytomegalovirus glycoprotein B genotypes in immunocompromised patients. Clin Infect Dis 39:155–161. doi: 10.1086/421496. [DOI] [PubMed] [Google Scholar]
- 64.Slavuljica I, Kvestak D, Huszthy PC, Kosmac K, Britt WJ, Jonjic S. 2015. Immunobiology of congenital cytomegalovirus infection of the central nervous system—the murine cytomegalovirus model. Cell Mol Immunol 12:180–191. doi: 10.1038/cmi.2014.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Boeckh M, Geballe AP. 2011. Cytomegalovirus: pathogen, paradigm, and puzzle. J Clin Invest 121:1673–1680. doi: 10.1172/JCI45449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sia IG, Patel R. 2000. New strategies for prevention and therapy of cytomegalovirus infection and disease in solid-organ transplant recipients. Clin Microbiol Rev 13:83–121. doi: 10.1128/CMR.13.1.83-121.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stoelben S, Arns W, Renders L, Hummel J, Muhlfeld A, Stangl M, Fischereder M, Gwinner W, Suwelack B, Witzke O, Durr M, Beelen DW, Michel D, Lischka P, Zimmermann H, Rubsamen-Schaeff H, Budde K. 2014. Preemptive treatment of cytomegalovirus infection in kidney transplant recipients with letermovir: results of a phase 2a study. Transpl Int 27:77–86. doi: 10.1111/tri.12225. [DOI] [PubMed] [Google Scholar]
- 68.Razonable RR, Hayden RT. 2013. Clinical utility of viral load in management of cytomegalovirus infection after solid organ transplantation. Clin Microbiol Rev 26:703–727. doi: 10.1128/CMR.00015-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.de Vries JJ, van Zwet EW, Dekker FW, Kroes AC, Verkerk PH, Vossen AC. 2013. The apparent paradox of maternal seropositivity as a risk factor for congenital cytomegalovirus infection: a population-based prediction model. Rev Med Virol 23:241–249. doi: 10.1002/rmv.1744. [DOI] [PubMed] [Google Scholar]
- 70.Dollard SC, Grosse SD, Ross DS. 2007. New estimates of the prevalence of neurological and sensory sequelae and mortality associated with congenital cytomegalovirus infection. Rev Med Virol 17:355–363. doi: 10.1002/rmv.544. [DOI] [PubMed] [Google Scholar]
- 71.Kenneson A, Cannon MJ. 2007. Review and meta-analysis of the epidemiology of congenital cytomegalovirus (CMV) infection. Rev Med Virol 17:253–276. doi: 10.1002/rmv.535. [DOI] [PubMed] [Google Scholar]
- 72.Whitley RJ, Kimberlin DW, Roizman B. 1998. Herpes simplex viruses. Clin Infect Dis 26:541–553. doi: 10.1086/514600. [DOI] [PubMed] [Google Scholar]
- 73.Frampton AR Jr, Goins WF, Nakano K, Burton EA, Glorioso JC. 2005. HSV trafficking and development of gene therapy vectors with applications in the nervous system. Gene Ther 12:891–901. doi: 10.1038/sj.gt.3302545. [DOI] [PubMed] [Google Scholar]
- 74.Kimberlin DW. 2004. Neonatal herpes simplex infection. Clin Microbiol Rev 17:1–13. doi: 10.1128/CMR.17.1.1-13.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kimberlin DW, Rouse DJ. 2004. Clinical practice. Genital herpes. N Engl J Med 350:1970–1977. doi: 10.1056/NEJMcp023065. [DOI] [PubMed] [Google Scholar]
- 76.Arvin AM. 1996. Varicella-zoster virus. Clin Microbiol Rev 9:361–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ku CC, Besser J, Abendroth A, Grose C, Arvin AM. 2005. Varicella-zoster virus pathogenesis and immunobiology: new concepts emerging from investigations with the SCIDhu mouse model. J Virol 79:2651–2658. doi: 10.1128/JVI.79.5.2651-2658.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zell R, Taudien S, Pfaff F, Wutzler P, Platzer M, Sauerbrei A. 2012. Sequencing of 21 varicella-zoster virus genomes reveals two novel genotypes and evidence of recombination. J Virol 86:1608–1622. doi: 10.1128/JVI.06233-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chow VT, Tipples GA, Grose C. 2013. Bioinformatics of varicella-zoster virus: single nucleotide polymorphisms define clades and attenuated vaccine genotypes. Infect Genet Evol 18:351–356. doi: 10.1016/j.meegid.2012.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gershon AA, Gershon MD. 2013. Pathogenesis and current approaches to control of varicella-zoster virus infections. Clin Microbiol Rev 26:728–743. doi: 10.1128/CMR.00052-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gardella C, Brown ZA. 2007. Managing varicella zoster infection in pregnancy. Cleve Clin J Med 74:290–296. doi: 10.3949/ccjm.74.4.290. [DOI] [PubMed] [Google Scholar]
- 82.Zerboni L, Sen N, Oliver SL, Arvin AM. 2014. Molecular mechanisms of varicella zoster virus pathogenesis. Nat Rev Microbiol 12:197–210. doi: 10.1038/nrmicro3215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kimberlin DW, Whitley RJ. 2007. Varicella-zoster vaccine for the prevention of herpes zoster. N Engl J Med 356:1338–1343. doi: 10.1056/NEJMct066061. [DOI] [PubMed] [Google Scholar]
- 84.Kilgore PE, Kruszon-Moran D, Seward JF, Jumaan A, Van Loon FP, Forghani B, McQuillan GM, Wharton M, Fehrs LJ, Cossen CK, Hadler SC. 2003. Varicella in Americans from NHANES III: implications for control through routine immunization. J Med Virol 70(Suppl 1):S111–S118. doi: 10.1002/jmv.10364. [DOI] [PubMed] [Google Scholar]
- 85.Tseng HF, Smith N, Harpaz R, Bialek SR, Sy LS, Jacobsen SJ. 2011. Herpes zoster vaccine in older adults and the risk of subsequent herpes zoster disease. JAMA 305:160–166. doi: 10.1001/jama.2010.1983. [DOI] [PubMed] [Google Scholar]
- 86.Prusoff WH. 1959. Synthesis and biological activities of iododeoxyuridine, an analog of thymidine. Biochim Biophys Acta 32:295–296. doi: 10.1016/0006-3002(59)90597-9. [DOI] [PubMed] [Google Scholar]
- 87.Herrmann EC., Jr 1961. Plaque inhibition test for detection of specific inhibitors of DNA containing viruses. Proc Soc Exp Biol Med 107:142–145. doi: 10.3181/00379727-107-26560. [DOI] [PubMed] [Google Scholar]
- 88.Kaufman HE. 1962. Clinical cure of herpes simplex keratitis by 5-iodo-2-deoxyuridine. Proc Soc Exp Biol Med 109:251–252. doi: 10.3181/00379727-109-27169. [DOI] [PubMed] [Google Scholar]
- 89.Kaufman H, Martola EL, Dohlman C. 1962. Use of 5-iodo-2′-deoxyuridine (IDU) in treatment of herpes simplex keratitis. Arch Ophthalmol 68:235–239. doi: 10.1001/archopht.1962.00960030239015. [DOI] [PubMed] [Google Scholar]
- 90.Kaufman HE, Heidelberger C. 1964. Therapeutic antiviral action of 5-trifluoromethyl-2′-deoxyuridine in herpes simplex keratitis. Science 145:585–586. doi: 10.1126/science.145.3632.585. [DOI] [PubMed] [Google Scholar]
- 91.Wilhelmus KR. 2010. Antiviral treatment and other therapeutic interventions for herpes simplex virus epithelial keratitis. Cochrane Database Syst Rev 8:CD002898. doi: 10.1002/14651858.CD002898.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.De Clercq E. 2004. Discovery and development of BVDU (brivudin) as a therapeutic for the treatment of herpes zoster. Biochem Pharmacol 68:2301–2315. doi: 10.1016/j.bcp.2004.07.039. [DOI] [PubMed] [Google Scholar]
- 93.Andrei G, Sienaert R, McGuigan C, De Clercq E, Balzarini J, Snoeck R. 2005. Susceptibilities of several clinical varicella-zoster virus (VZV) isolates and drug-resistant VZV strains to bicyclic furano pyrimidine nucleosides. Antimicrob Agents Chemother 49:1081–1086. doi: 10.1128/AAC.49.3.1081-1086.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Maudgal PC, De Clercq E. 1991. Bromovinyldeoxyuridine treatment of herpetic keratitis clinically resistant to other antiviral agents. Curr Eye Res 10(Suppl):193–199. doi: 10.3109/02713689109020379. [DOI] [PubMed] [Google Scholar]
- 95.Lahmer T, Hoffmann D, Heemann U, Kuchle C, Frank H. 2010. Epstein-Barr virus encephalitis after kidney transplantation and successful treatment with brivudine. Transpl Int 23:e24–e25. doi: 10.1111/j.1432-2277.2009.01045.x. [DOI] [PubMed] [Google Scholar]
- 96.Lin JC, Smith MC, Pagano JS. 1985. Comparative efficacy and selectivity of some nucleoside analogs against Epstein-Barr virus. Antimicrob Agents Chemother 27:971–973. doi: 10.1128/AAC.27.6.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bergmann W, Feeney RJ. 1950. The isolation of a new thymine pentoside from sponges. J Am Chem Soc 72:2809–2810. doi: 10.1021/ja01162a543. [DOI] [Google Scholar]
- 98.Schabel FM., Jr 1968. The antiviral activity of 9-beta-D-arabinofuranosyladenine (ARA-A). Chemotherapy 13:321–338. doi: 10.1159/000220567. [DOI] [PubMed] [Google Scholar]
- 99.Cohen SS. 1966. Introduction to the biochemistry of D-arabinosyl nucleosides. Prog Nucleic Acid Res Mol Biol 5:1–88. doi: 10.1016/S0079-6603(08)60231-7. [DOI] [PubMed] [Google Scholar]
- 100.Whitley RJ, Ch'ien LT, Dolin R, Galasso GJ, Alford CA Jr. 1976. Adenine arabinoside therapy of herpes zoster in the immunosuppressed. NIAID collaborative antiviral study. N Engl J Med 294:1193–1199. doi: 10.1056/NEJM197605272942201. [DOI] [PubMed] [Google Scholar]
- 101.Brady RC, Bernstein DI. 2004. Treatment of herpes simplex virus infections. Antiviral Res 61:73–81. doi: 10.1016/j.antiviral.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 102.Mayer AM, Glaser KB, Cuevas C, Jacobs RS, Kem W, Little RD, McIntosh JM, Newman DJ, Potts BC, Shuster DE. 2010. The odyssey of marine pharmaceuticals: a current pipeline perspective. Trends Pharmacol Sci 31:255–265. doi: 10.1016/j.tips.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 103.Chang TT, Gish RG, de Man R, Gadano A, Sollano J, Chao YC, Lok AS, Han KH, Goodman Z, Zhu J, Cross A, DeHertogh D, Wilber R, Colonno R, Apelian D, BEHoLD AI463022 Study Group. 2006. A comparison of entecavir and lamivudine for HBeAg-positive chronic hepatitis B. N Engl J Med 354:1001–1010. doi: 10.1056/NEJMoa051285. [DOI] [PubMed] [Google Scholar]
- 104.Lai CL, Shouval D, Lok AS, Chang TT, Cheinquer H, Goodman Z, DeHertogh D, Wilber R, Zink RC, Cross A, Colonno R, Fernandes L, BEHoLD AI463027 Study Group. 2006. Entecavir versus lamivudine for patients with HBeAg-negative chronic hepatitis B. N Engl J Med 354:1011–1020. doi: 10.1056/NEJMoa051287. [DOI] [PubMed] [Google Scholar]
- 105.Tenney DJ, Rose RE, Baldick CJ, Pokornowski KA, Eggers BJ, Fang J, Wichroski MJ, Xu D, Yang J, Wilber RB, Colonno RJ. 2009. Long-term monitoring shows hepatitis B virus resistance to entecavir in nucleoside-naive patients is rare through 5 years of therapy. Hepatology 49:1503–1514. doi: 10.1002/hep.22841. [DOI] [PubMed] [Google Scholar]
- 106.McMahon MA, Jilek BL, Brennan TP, Shen L, Zhou Y, Wind-Rotolo M, Xing S, Bhat S, Hale B, Hegarty R, Chong CR, Liu JO, Siliciano RF, Thio CL. 2007. The HBV drug entecavir—effects on HIV-1 replication and resistance. N Engl J Med 356:2614–2621. doi: 10.1056/NEJMoa067710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hirsch MS. 2007. Entecavir surprise. N Engl J Med 356:2641–2643. doi: 10.1056/NEJMe078045. [DOI] [PubMed] [Google Scholar]
- 108.Lai CL, Gane E, Liaw YF, Hsu CW, Thongsawat S, Wang Y, Chen Y, Heathcote EJ, Rasenack J, Bzowej N, Naoumov NV, Di Bisceglie AM, Zeuzem S, Moon YM, Goodman Z, Chao G, Constance BF, Brown NA, Globe Study Group. 2007. Telbivudine versus lamivudine in patients with chronic hepatitis B. N Engl J Med 357:2576–2588. doi: 10.1056/NEJMoa066422. [DOI] [PubMed] [Google Scholar]
- 109.Hou J, Yin YK, Xu D, Tan D, Niu J, Zhou X, Wang Y, Zhu L, He Y, Ren H, Wan M, Chen C, Wu S, Chen Y, Xu J, Wang Q, Wei L, Chao G, Constance BF, Harb G, Brown NA, Jia J. 2008. Telbivudine versus lamivudine in Chinese patients with chronic hepatitis B: results at 1 year of a randomized, double-blind trial. Hepatology 47:447–454. doi: 10.1002/hep.22075. [DOI] [PubMed] [Google Scholar]
- 110.Lai CL, Leung N, Teo EK, Tong M, Wong F, Hann HW, Han S, Poynard T, Myers M, Chao G, Lloyd D, Brown NA, Telbivudine Phase II Investigator Group. 2005. A 1-year trial of telbivudine, lamivudine, and the combination in patients with hepatitis B e antigen-positive chronic hepatitis B. Gastroenterology 129:528–536. doi: 10.1016/j.gastro.2005.05.053. [DOI] [PubMed] [Google Scholar]
- 111.Liaw YF, Gane E, Leung N, Zeuzem S, Wang Y, Lai CL, Heathcote EJ, Manns M, Bzowej N, Niu J, Han SH, Hwang SG, Cakaloglu Y, Tong MJ, Papatheodoridis G, Chen Y, Brown NA, Albanis E, Galil K, Naoumov NV, GLOBE Study Group. 2009. 2-year GLOBE trial results: telbivudine is superior to lamivudine in patients with chronic hepatitis B. Gastroenterology 136:486–495. doi: 10.1053/j.gastro.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 112.Han GR, Cao MK, Zhao W, Jiang HX, Wang CM, Bai SF, Yue X, Wang GJ, Tang X, Fang ZX. 2011. A prospective and open-label study for the efficacy and safety of telbivudine in pregnancy for the prevention of perinatal transmission of hepatitis B virus infection. J Hepatol 55:1215–1221. doi: 10.1016/j.jhep.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 113.Liang J, Jiang MJ, Deng X, Xiao Zhou X. 2013. Efficacy and safety of telbivudine compared to entecavir among HBeAg+ chronic hepatitis B patients: a meta-analysis study. Hepat Mon 13:e7862. doi: 10.5812/hepatmon.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.World Health Organization. 2015. Guidelines for the prevention, care and treatment of persons with chronic hepatitis B infection. WHO, Geneva, Switzerland. [PubMed] [Google Scholar]
- 115.Lok AS-F. 2016. Hepatitis B: 50 years after the discovery of Australia antigen. J Viral Hepat 23:5–14. doi: 10.1111/jvh.12444. [DOI] [PubMed] [Google Scholar]
- 116.Helgstrand E, Eriksson B, Johansson NG, Lannero B, Larsson A, Misiorny A, Noren JO, Sjoberg B, Stenberg K, Stening G, Stridh S, Oberg B. 1978. Trisodium phosphonoformate, a new antiviral compound. Science 201:819–821. doi: 10.1126/science.210500. [DOI] [PubMed] [Google Scholar]
- 117.Shipkowitz NL, Bower RR, Appell RN, Nordeen CW, Overby LR, Roderick WR, Schleicher JB, Von Esch AM. 1973. Suppression of herpes simplex virus infection by phosphonoacetic acid. Appl Microbiol 26:264–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tchesnokov EP, Gilbert C, Boivin G, Gotte M. 2006. Role of helix P of the human cytomegalovirus DNA polymerase in resistance and hypersusceptibility to the antiviral drug foscarnet. J Virol 80:1440–1450. doi: 10.1128/JVI.80.3.1440-1450.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Öberg B. 1989. Antiviral effects of phosphonoformate (PFA, foscarnet sodium). Pharmacol Ther 40:213–285. doi: 10.1016/0163-7258(89)90097-1. [DOI] [PubMed] [Google Scholar]
- 120.Chatis PA, Miller CH, Schrager LE, Crumpacker CS. 1989. Successful treatment with foscarnet of an acyclovir-resistant mucocutaneous infection with herpes simplex virus in a patient with acquired immunodeficiency syndrome. N Engl J Med 320:297–300. doi: 10.1056/NEJM198902023200507. [DOI] [PubMed] [Google Scholar]
- 121.Cohen SG, Greenberg MS. 1985. Chronic oral herpes simplex virus infection in immunocompromised patients. Oral Surg Oral Med Oral Pathol 59:465–471. doi: 10.1016/0030-4220(85)90085-4. [DOI] [PubMed] [Google Scholar]
- 122.Vinckier F, Boogaerts M, De Clerck D, De Clercq E. 1987. Chronic herpetic infection in an immunocompromised patient: report of a case. J Oral Maxillofac Surg 45:723–728. doi: 10.1016/0278-2391(87)90320-X. [DOI] [PubMed] [Google Scholar]
- 123.Leporrier J, Etienne M, Chapuzet C, Peytavin G, Bord S, Borsa-Lebas F, Caron F, Plantier JC, Mourez T. 2014. Association of dolutegravir and rilpivirine, enhanced by foscarnet induction, in effective salvage antiretroviral therapy. J Clin Virol 60:428–430. doi: 10.1016/j.jcv.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 124.Minces LR, Nguyen MH, Mitsani D, Shields RK, Kwak EJ, Silveira FP, Abdel-Massih R, Pilewski JM, Crespo MM, Bermudez C, Bhama JK, Toyoda Y, Clancy CJ. 2014. Ganciclovir-resistant cytomegalovirus infections among lung transplant recipients are associated with poor outcomes despite treatment with foscarnet-containing regimens. Antimicrob Agents Chemother 58:128–135. doi: 10.1128/AAC.00561-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jacobson MA. 1992. Review of the toxicities of foscarnet. J Acquir Immune Defic Syndr 5(Suppl 1):S11–S17. [PubMed] [Google Scholar]
- 126.Chrisp P, Clissold SP. 1991. Foscarnet. A review of its antiviral activity, pharmacokinetic properties and therapeutic use in immunocompromised patients with cytomegalovirus retinitis. Drugs 41:104–129. [DOI] [PubMed] [Google Scholar]
- 127.Agut H, Bonnafous P, Gautheret-Dejean A. 2015. Laboratory and clinical aspects of human herpesvirus 6 infections. Clin Microbiol Rev 28:313–335. doi: 10.1128/CMR.00122-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mitsuya H, Weinhold KJ, Furman PA, St Clair MH, Lehrman SN, Gallo RC, Bolognesi D, Barry DW, Broder S. 1985. 3′-Azido-3′-deoxythymidine (BW A509U): an antiviral agent that inhibits the infectivity and cytopathic effect of human T-lymphotropic virus type III/lymphadenopathy-associated virus in vitro. Proc Natl Acad Sci U S A 82:7096–7100. doi: 10.1073/pnas.82.20.7096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mitsuya H, Broder S. 1986. Inhibition of the in vitro infectivity and cytopathic effect of human T-lymphotrophic virus type III/lymphadenopathy-associated virus (HTLV-III/LAV) by 2′,3′-dideoxynucleosides. Proc Natl Acad Sci U S A 83:1911–1915. doi: 10.1073/pnas.83.6.1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Baba M, Pauwels R, Herdewijn P, De Clercq E, Desmyter J, Vandeputte M. 1987. Both 2′,3′-dideoxythymidine and its 2′,3′-unsaturated derivative (2′,3′-dideoxythymidinene) are potent and selective inhibitors of human immunodeficiency virus replication in vitro. Biochem Biophys Res Commun 142:128–134. doi: 10.1016/0006-291X(87)90460-8. [DOI] [PubMed] [Google Scholar]
- 131.Lin TS, Schinazi RF, Prusoff WH. 1987. Potent and selective in vitro activity of 3′-deoxythymidin-2′-ene (3′-deoxy-2′,3′-didehydrothymidine) against human immunodeficiency virus. Biochem Pharmacol 36:2713–2718. doi: 10.1016/0006-2952(87)90253-X. [DOI] [PubMed] [Google Scholar]
- 132.Hamamoto Y, Nakashima H, Matsui T, Matsuda A, Ueda T, Yamamoto N. 1987. Inhibitory effect of 2′,3′-didehydro-2′,3′-dideoxynucleosides on infectivity, cytopathic effects, and replication of human immunodeficiency virus. Antimicrob Agents Chemother 31:907–910. doi: 10.1128/AAC.31.6.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Soudeyns H, Yao XI, Gao Q, Belleau B, Kraus JL, Nguyen-Ba N, Spira B, Wainberg MA. 1991. Anti-human immunodeficiency virus type 1 activity and in vitro toxicity of 2′-deoxy-3′-thiacytidine (BCH-189), a novel heterocyclic nucleoside analog. Antimicrob Agents Chemother 35:1386–1390. doi: 10.1128/AAC.35.7.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Daluge SM, Good SS, Faletto MB, Miller WH, St Clair MH, Boone LR, Tisdale M, Parry NR, Reardon JE, Dornsife RE, Averett DR, Krenitsky TA. 1997. 1592U89, a novel carbocyclic nucleoside analog with potent, selective anti-human immunodeficiency virus activity. Antimicrob Agents Chemother 41:1082–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Schinazi RF, Boudinot FD, Ibrahim SS, Manning C, McClure HM, Liotta DC. 1992. Pharmacokinetics and metabolism of racemic 2′,3′-dideoxy-5-fluoro-3′-thiacytidine in rhesus monkeys. Antimicrob Agents Chemother 36:2432–2438. doi: 10.1128/AAC.36.11.2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Furman PA, Fyfe JA, St Clair MH, Weinhold K, Rideout JL, Freeman GA, Lehrman SN, Bolognesi DP, Broder S, Mitsuya H, Barry DW. 1986. Phosphorylation of 3′-azido-3′-deoxythymidine and selective interaction of the 5′-triphosphate with human immunodeficiency virus reverse transcriptase. Proc Natl Acad Sci U S A 83:8333–8337. doi: 10.1073/pnas.83.21.8333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Tu X, Das K, Han Q, Bauman JD, Clark AD Jr, Hou X, Frenkel YV, Gaffney BL, Jones RA, Boyer PL, Hughes SH, Sarafianos SG, Arnold E. 2010. Structural basis of HIV-1 resistance to AZT by excision. Nat Struct Mol Biol 17:1202–1209. doi: 10.1038/nsmb.1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wensing AM, Calvez V, Gunthard HF, Johnson VA, Paredes R, Pillay D, Shafer RW, Richman DD. 2015. 2015 update of the drug resistance mutations in HIV-1. Top Antivir Med 23:132–141. [PMC free article] [PubMed] [Google Scholar]
- 139.Arts EJ, Hazuda DJ. 2012. HIV-1 antiretroviral drug therapy. Cold Spring Harb Perspect Med 2:a007161. doi: 10.1101/cshperspect.a007161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Charpentier C, Camacho R, Ruelle J, Eberle J, Gurtler L, Pironti A, Sturmer M, Brun-Vezinet F, Kaiser R, Descamps D, Obermeier M. 2015. HIV-2EU-supporting standardized HIV-2 drug-resistance interpretation in Europe: an update. Clin Infect Dis 61:1346–1347. doi: 10.1093/cid/civ572. [DOI] [PubMed] [Google Scholar]
- 141.Rokx C, Rijnders BJA. 2015. Evidence gathered from randomized clinical trials and observational studies on the equivalence of emtricitabine and lamivudine. Clin Infect Dis 60:1732–1733. doi: 10.1093/cid/civ117. [DOI] [PubMed] [Google Scholar]
- 142.Ford N, Hill A, Vitoria M, Mills EJ. 2015. Editorial commentary. Comparative efficacy of lamivudine and emtricitabine: comparing the results of randomized trials and cohorts. Clin Infect Dis 60:154–156. doi: 10.1093/cid/ciu767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Montessori V, Press N, Harris M, Akagi L, Montaner JS. 2004. Adverse effects of antiretroviral therapy for HIV infection. CMAJ 170:229–238. [PMC free article] [PubMed] [Google Scholar]
- 144.Hill A. 2013. Optimizing HIV treatment. Curr Opin HIV AIDS 8:34–40. doi: 10.1097/COH.0b013e32835b7f28. [DOI] [PubMed] [Google Scholar]
- 145.Baba M, Tanaka H, De Clercq E, Pauwels R, Balzarini J, Schols D, Nakashima H, Perno CF, Walker RT, Miyasaka T. 1989. Highly specific inhibition of human immunodeficiency virus type 1 by a novel 6-substituted acyclouridine derivative. Biochem Biophys Res Commun 165:1375–1381. doi: 10.1016/0006-291X(89)92756-3. [DOI] [PubMed] [Google Scholar]
- 146.Miyasaka T, Tanaka H, Baba M, Hayakawa H, Walker RT, Balzarini J, De Clercq E. 1989. A novel lead for specific anti-HIV-1 agents: 1-[(2-hydroxyethoxy)methyl]-6-(phenylthio)thymine. J Med Chem 32:2507–2509. doi: 10.1021/jm00132a002. [DOI] [PubMed] [Google Scholar]
- 147.Pauwels R, Andries K, Desmyter J, Schols D, Kukla MJ, Breslin HJ, Raeymaeckers A, Van Gelder J, Woestenborghs R, Heykants J, Schellekens K, Janssen MAC, De Clercq E, Janssen PA. 1990. Potent and selective inhibition of HIV-1 replication in vitro by a novel series of TIBO derivatives. Nature 343:470–474. doi: 10.1038/343470a0. [DOI] [PubMed] [Google Scholar]
- 148.Baba M, De Clercq E, Tanaka H, Ubasawa M, Takashima H, Sekiya K, Nitta I, Umezu K, Nakashima H, Mori S, Shigeta S, Walker RT, Miyasaka TM. 1991. Potent and selective inhibition of human immunodeficiency virus type 1 (HIV-1) by 5-ethyl-6-phenylthiouracil derivatives through their interaction with the HIV-1 reverse transcriptase. Proc Natl Acad Sci U S A 88:2356–2360. doi: 10.1073/pnas.88.6.2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Baba M, De Clercq E, Tanaka H, Ubasawa M, Takashima H, Sekiya K, Nitta I, Umezu K, Walker RT, Mori S. 1991. Highly potent and selective inhibition of human immunodeficiency virus type 1 by a novel series of 6-substituted acyclouridine derivatives. Mol Pharmacol 39:805–810. [PubMed] [Google Scholar]
- 150.Debyser Z, Pauwels R, Andries K, Desmyter J, Kukla M, Janssen PA, De Clercq E. 1991. An antiviral target on reverse transcriptase of human immunodeficiency virus type 1 revealed by tetrahydroimidazo-[4,5,1-jk] [1,4]benzodiazepin-2 (1H)-one and -thione derivatives. Proc Natl Acad Sci U S A 88:1451–1455. doi: 10.1073/pnas.88.4.1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Baba M, Shigeta S, Yuasa S, Takashima H, Sekiya K, Ubasawa M, Tanaka H, Miyasaka T, Walker RT, De Clercq E. 1994. Preclinical evaluation of MKC-442, a highly potent and specific inhibitor of human immunodeficiency virus type 1 in vitro. Antimicrob Agents Chemother 38:688–692. doi: 10.1128/AAC.38.4.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.De Clercq E. 2005. Antiviral drug discovery and development: where chemistry meets with biomedicine. Antiviral Res 67:56–75. doi: 10.1016/j.antiviral.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 153.De Clercq E. 2012. Where rilpivirine meets with tenofovir, the start of a new anti-HIV drug combination era. Biochem Pharmacol 84:241–248. doi: 10.1016/j.bcp.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 154.Janssen PA, Lewi PJ, Arnold E, Daeyaert F, de Jonge M, Heeres J, Koymans L, Vinkers M, Guillemont J, Pasquier E, Kukla M, Ludovici D, Andries K, de Bethune MP, Pauwels R, Das K, Clark AD Jr, Frenkel YV, Hughes SH, Medaer B, De Knaep F, Bohets H, De Clerck F, Lampo A, Williams P, Stoffels P. 2005. In search of a novel anti-HIV drug: multidisciplinary coordination in the discovery of 4-[[4-[[4-[(1E)-2-cyanoethenyl]-2,6-dimethylphenyl]amino]-2-pyrimidinyl]amino]benzonitrile (R278474, rilpivirine). J Med Chem 48:1901–1909. doi: 10.1021/jm040840e. [DOI] [PubMed] [Google Scholar]
- 155.Warnke D, Barreto J, Temesgen Z. 2007. Antiretroviral drugs. J Clin Pharmacol 47:1570–1579. doi: 10.1177/0091270007308034. [DOI] [PubMed] [Google Scholar]
- 156.Tantillo C, Ding J, Jacobo-Molina A, Nanni RG, Boyer PL, Hughes SH, Pauwels R, Andries K, Janssen PA, Arnold E. 1994. Locations of anti-AIDS drug binding sites and resistance mutations in the three-dimensional structure of HIV-1 reverse transcriptase. Implications for mechanisms of drug inhibition and resistance. J Mol Biol 243:369–387. doi: 10.1006/jmbi.1994.1665. [DOI] [PubMed] [Google Scholar]
- 157.Ding J, Das K, Moereels H, Koymans L, Andries K, Janssen PA, Hughes SH, Arnold E. 1995. Structure of HIV-1 RT/TIBO R 86183 complex reveals similarity in the binding of diverse nonnucleoside inhibitors. Nat Struct Biol 2:407–415. doi: 10.1038/nsb0595-407. [DOI] [PubMed] [Google Scholar]
- 158.Das K, Ding J, Hsiou Y, Clark AD Jr, Moereels H, Koymans L, Andries K, Pauwels R, Janssen PA, Boyer PL, Clark P, Smith RH Jr, Kroeger Smith MB, Michejda CJ, Hughes SH, Arnold E. 1996. Crystal structures of 8-Cl and 9-Cl TIBO complexed with wild-type HIV-1 RT and 8-Cl TIBO complexed with the Tyr181Cys HIV-1 RT drug-resistant mutant. J Mol Biol 264:1085–1100. doi: 10.1006/jmbi.1996.0698. [DOI] [PubMed] [Google Scholar]
- 159.D'Cruz OJ, Uckun FM. 2006. Dawn of non-nucleoside inhibitor-based anti-HIV microbicides. J Antimicrob Chemother 57:411–423. doi: 10.1093/jac/dki464. [DOI] [PubMed] [Google Scholar]
- 160.Tuaillon E, Gueudin M, Lemee V, Gueit I, Roques P, Corrigan GE, Plantier JC, Simon F, Braun J. 2004. Phenotypic susceptibility to nonnucleoside inhibitors of virion-associated reverse transcriptase from different HIV types and groups. J Acquir Immune Defic Syndr 37:1543–1549. doi: 10.1097/00126334-200412150-00001. [DOI] [PubMed] [Google Scholar]
- 161.Ren J, Bird LE, Chamberlain PP, Stewart-Jones GB, Stuart DI, Stammers DK. 2002. Structure of HIV-2 reverse transcriptase at 2.35-A resolution and the mechanism of resistance to non-nucleoside inhibitors. Proc Natl Acad Sci U S A 99:14410–14415. doi: 10.1073/pnas.222366699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Anderson MS, Gilmartin J, Cilissen C, De Lepeleire I, Van Bortel L, Dockendorf MF, Tetteh E, Ancona JK, Liu R, Guo Y, Wagner JA, Butterton JR. 2015. Safety, tolerability and pharmacokinetics of doravirine, a novel HIV non-nucleoside reverse transcriptase inhibitor, after single and multiple doses in healthy subjects. Antivir Ther 20:397–405. doi: 10.3851/IMP2920. [DOI] [PubMed] [Google Scholar]
- 163.Gatell JM, Morales-Ramirez JO, Hagins DP, Thompson M, Keikawus A, Hoffmann C, Rugina S, Osiyemi O, Escoriu S, Dretler R, Harvey C, Xu X, Teppler H. 2014. Forty-eight-week efficacy and safety and early CNS tolerability of doravirine (MK-1439), a novel NNRTI, with TDF/FTC in ART-naive HIV-positive patients. J Int AIDS Soc 17:19532. doi: 10.7448/IAS.17.4.19532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Lai MT, Feng M, Falgueyret JP, Tawa P, Witmer M, DiStefano D, Li Y, Burch J, Sachs N, Lu M, Cauchon E, Campeau LC, Grobler J, Yan Y, Ducharme Y, Cote B, Asante-Appiah E, Hazuda DJ, Miller MD. 2014. In vitro characterization of MK-1439, a novel HIV-1 nonnucleoside reverse transcriptase inhibitor. Antimicrob Agents Chemother 58:1652–1663. doi: 10.1128/AAC.02403-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Famiglini V, Silvestri R. 2016. Focus on chirality of HIV-1 non-nucleoside reverse transcriptase inhibitors. Molecules 21:E221. doi: 10.3390/molecules21020221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Kramer RA, Schaber MD, Skalka AM, Ganguly K, Wong-Staal F, Reddy EP. 1986. HTLV-III gag protein is processed in yeast cells by the virus pol-protease. Science 231:1580–1584. doi: 10.1126/science.2420008. [DOI] [PubMed] [Google Scholar]
- 167.Roberts NA, Martin JA, Kinchington D, Broadhurst AV, Craig JC, Duncan IB, Galpin SA, Handa BK, Kay J, Krohn A, Lambert RW, Merrett JH, Mills JS, Parkes KEB, Redshaw S, Ritchie AJ, Taylor DL, Thomas GJ, Machin PJ. 1990. Rational design of peptide-based HIV proteinase inhibitors. Science 248:358–361. doi: 10.1126/science.2183354. [DOI] [PubMed] [Google Scholar]
- 168.De Clercq E. 2013. Dancing with chemical formulae of antivirals: a panoramic view (part 2). Biochem Pharmacol 86:1397–1410. doi: 10.1016/j.bcp.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 169.Wensing AM, van Maarseveen NM, Nijhuis M. 2010. Fifteen years of HIV protease inhibitors: raising the barrier to resistance. Antiviral Res 85:59–74. doi: 10.1016/j.antiviral.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 170.Li G, Verheyen J, Theys K, Piampongsant S, Van Laethem K, Vandamme A-M. 2014. HIV-1 Gag C-terminal amino acid substitutions emerging under selective pressure of protease inhibitors in patient populations infected with different HIV-1 subtypes. Retrovirology 11:79. doi: 10.1186/s12977-014-0079-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Li G, Theys K, Verheyen J, Pineda-Pena A, Khouri R, Piampongsant S, Eusebio M, Ramon J, Vandamme A-M. 2015. A new ensemble coevolution system for detecting HIV-1 protein coevolution. Biol Direct 10:1. doi: 10.1186/s13062-014-0031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Clavel F, Hance AJ. 2004. HIV drug resistance. N Engl J Med 350:1023–1035. doi: 10.1056/NEJMra025195. [DOI] [PubMed] [Google Scholar]
- 173.Brower ET, Bacha UM, Kawasaki Y, Freire E. 2008. Inhibition of HIV-2 protease by HIV-1 protease inhibitors in clinical use. Chem Biol Drug Des 71:298–305. doi: 10.1111/j.1747-0285.2008.00647.x. [DOI] [PubMed] [Google Scholar]
- 174.Campbell-Yesufu OT, Gandhi RT. 2011. Update on human immunodeficiency virus (HIV)-2 infection. Clin Infect Dis 52:780–787. doi: 10.1093/cid/ciq248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ntemgwa M, Brenner BG, Oliveira M, Moisi D, Wainberg MA. 2007. Natural polymorphisms in the human immunodeficiency virus type 2 protease can accelerate time to development of resistance to protease inhibitors. Antimicrob Agents Chemother 51:604–610. doi: 10.1128/AAC.00870-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lepist EI, Phan TK, Roy A, Tong L, Maclennan K, Murray B, Ray AS. 2012. Cobicistat boosts the intestinal absorption of transport substrates, including HIV protease inhibitors and GS-7340, in vitro. Antimicrob Agents Chemother 56:5409–5413. doi: 10.1128/AAC.01089-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.De Clercq E. 2007. The design of drugs for HIV and HCV. Nat Rev Drug Discov 6:1001–1018. doi: 10.1038/nrd2424. [DOI] [PubMed] [Google Scholar]
- 178.De Clercq E. 2014. Current race in the development of DAAs (direct-acting antivirals) against HCV. Biochem Pharmacol 89:441–452. doi: 10.1016/j.bcp.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 179.De Clercq E. 2015. Development of antiviral drugs for the treatment of hepatitis C at an accelerating pace. Rev Med Virol 25:254–267. doi: 10.1002/rmv.1842. [DOI] [PubMed] [Google Scholar]
- 180.McCauley JA, McIntyre CJ, Rudd MT, Nguyen KT, Romano JJ, Butcher JW, Gilbert KF, Bush KJ, Holloway MK, Swestock J, Wan BL, Carroll SS, DiMuzio JM, Graham DJ, Ludmerer SW, Mao SS, Stahlhut MW, Fandozzi CM, Trainor N, Olsen DB, Vacca JP, Liverton NJ. 2010. Discovery of vaniprevir (MK-7009), a macrocyclic hepatitis C virus NS3/4a protease inhibitor. J Med Chem 53:2443–2463. doi: 10.1021/jm9015526. [DOI] [PubMed] [Google Scholar]
- 181.Hayashi N, Nakamuta M, Takehara T, Kumada H, Takase A, Howe AY, Ludmerer SW, Mobashery N. 2016. Vaniprevir plus peginterferon alfa-2b and ribavirin in treatment-naive Japanese patients with hepatitis C virus genotype 1 infection: a randomized phase III study. J Gastroenterol 51:390–403. doi: 10.1007/s00535-015-1120-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Messina JP, Humphreys I, Flaxman A, Brown A, Cooke GS, Pybus OG, Barnes E. 2015. Global distribution and prevalence of hepatitis C virus genotypes. Hepatology 61:77–87. doi: 10.1002/hep.27259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Kiser JJ, Burton JR Jr, Everson GT. 2013. Drug-drug interactions during antiviral therapy for chronic hepatitis C. Nat Rev Gastroenterol Hepatol 10:596–606. doi: 10.1038/nrgastro.2013.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Hazuda DJ, Felock P, Witmer M, Wolfe A, Stillmock K, Grobler JA, Espeseth A, Gabryelski L, Schleif W, Blau C, Miller MD. 2000. Inhibitors of strand transfer that prevent integration and inhibit HIV-1 replication in cells. Science 287:646–650. doi: 10.1126/science.287.5453.646. [DOI] [PubMed] [Google Scholar]
- 185.Hazuda DJ, Young SD, Guare JP, Anthony NJ, Gomez RP, Wai JS, Vacca JP, Handt L, Motzel SL, Klein HJ, Dornadula G, Danovich RM, Witmer MV, Wilson KA, Tussey L, Schleif WA, Gabryelski LS, Jin L, Miller MD, Casimiro DR, Emini EA, Shiver JW. 2004. Integrase inhibitors and cellular immunity suppress retroviral replication in rhesus macaques. Science 305:528–532. doi: 10.1126/science.1098632. [DOI] [PubMed] [Google Scholar]
- 186.Grinsztejn B, Nguyen BY, Katlama C, Gatell JM, Lazzarin A, Vittecoq D, Gonzalez CJ, Chen J, Harvey CM, Isaacs RD, Protocol 005 Team. 2007. Safety and efficacy of the HIV-1 integrase inhibitor raltegravir (MK-0518) in treatment-experienced patients with multidrug-resistant virus: a phase II randomised controlled trial. Lancet 369:1261–1269. doi: 10.1016/S0140-6736(07)60597-2. [DOI] [PubMed] [Google Scholar]
- 187.Steigbigel RT, Cooper DA, Kumar PN, Eron JE, Schechter M, Markowitz M, Loutfy MR, Lennox JL, Gatell JM, Rockstroh JK, Katlama C, Yeni P, Lazzarin A, Clotet B, Zhao J, Chen J, Ryan DM, Rhodes RR, Killar JA, Gilde LR, Strohmaier KM, Meibohm AR, Miller MD, Hazuda DJ, Nessly ML, DiNubile MJ, Isaacs RD, Nguyen BY, Teppler H, BENCHMRK Study Teams. 2008. Raltegravir with optimized background therapy for resistant HIV-1 infection. N Engl J Med 359:339–354. doi: 10.1056/NEJMoa0708975. [DOI] [PubMed] [Google Scholar]
- 188.Cooper DA, Steigbigel RT, Gatell JM, Rockstroh JK, Katlama C, Yeni P, Lazzarin A, Clotet B, Kumar PN, Eron JE, Schechter M, Markowitz M, Loutfy MR, Lennox JL, Zhao J, Chen J, Ryan DM, Rhodes RR, Killar JA, Gilde LR, Strohmaier KM, Meibohm AR, Miller MD, Hazuda DJ, Nessly ML, DiNubile MJ, Isaacs RD, Teppler H, Nguyen BY, BENCHMRK Study Teams. 2008. Subgroup and resistance analyses of raltegravir for resistant HIV-1 infection. N Engl J Med 359:355–365. doi: 10.1056/NEJMoa0708978. [DOI] [PubMed] [Google Scholar]
- 189.SECOND-LINE Study Group, Boyd MA, Kumarasamy N, Moore CL, Nwizu C, Losso MH, Mohapi L, Martin A, Kerr S, Sohn AH, Teppler H, Van de Steen O, Molina JM, Emery S, Cooper DA. 2013. Ritonavir-boosted lopinavir plus nucleoside or nucleotide reverse transcriptase inhibitors versus ritonavir-boosted lopinavir plus raltegravir for treatment of HIV-1 infection in adults with virological failure of a standard first-line ART regimen (SECOND-LINE): a randomised, open-label, non-inferiority study. Lancet 381:2091–2099. doi: 10.1016/S0140-6736(13)61164-2. [DOI] [PubMed] [Google Scholar]
- 190.Sato M, Motomura T, Aramaki H, Matsuda T, Yamashita M, Ito Y, Kawakami H, Matsuzaki Y, Watanabe W, Yamataka K, Ikeda S, Kodama E, Matsuoka M, Shinkai H. 2006. Novel HIV-1 integrase inhibitors derived from quinolone antibiotics. J Med Chem 49:1506–1508. doi: 10.1021/jm0600139. [DOI] [PubMed] [Google Scholar]
- 191.Shimura K, Kodama E, Sakagami Y, Matsuzaki Y, Watanabe W, Yamataka K, Watanabe Y, Ohata Y, Doi S, Sato M, Kano M, Ikeda S, Matsuoka M. 2008. Broad antiretroviral activity and resistance profile of the novel human immunodeficiency virus integrase inhibitor elvitegravir (JTK-303/GS-9137). J Virol 82:764–774. doi: 10.1128/JVI.01534-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Roquebert B, Damond F, Collin G, Matheron S, Peytavin G, Benard A, Campa P, Chene G, Brun-Vezinet F, Descamps D, French ANRS HIV-2 Cohort . 2008. HIV-2 integrase gene polymorphism and phenotypic susceptibility of HIV-2 clinical isolates to the integrase inhibitors raltegravir and elvitegravir in vitro. J Antimicrob Chemother 62:914–920. doi: 10.1093/jac/dkn335. [DOI] [PubMed] [Google Scholar]
- 193.De Clercq E. 2012. Tenofovir: quo vadis anno 2012 (where is it going in the year 2012)? Med Res Rev 32:765–785. doi: 10.1002/med.21267. [DOI] [PubMed] [Google Scholar]
- 194.Manzardo C, Gatell JM. 2014. Stribild (elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate): a new paradigm for HIV-1 treatment. AIDS Rev 16:35–42. [PubMed] [Google Scholar]
- 195.Murrell DE, Moorman JP, Harirforoosh S. 2015. Stribild: a review of component characteristics and combination drug efficacy. Eur Rev Med Pharmacol Sci 19:904–914. [PubMed] [Google Scholar]
- 196.Molina JM, Lamarca A, Andrade-Villanueva J, Clotet B, Clumeck N, Liu YP, Zhong L, Margot N, Cheng AK, Chuck SL, Study 145 Team. 2012. Efficacy and safety of once daily elvitegravir versus twice daily raltegravir in treatment-experienced patients with HIV-1 receiving a ritonavir-boosted protease inhibitor: randomised, double-blind, phase 3, non-inferiority study. Lancet Infect Dis 12:27–35. doi: 10.1016/S1473-3099(11)70249-3. [DOI] [PubMed] [Google Scholar]
- 197.Deeks ED. 2014. Elvitegravir: a review of its use in adults with HIV-1 infection. Drugs 74:687–697. doi: 10.1007/s40265-014-0206-8. [DOI] [PubMed] [Google Scholar]
- 198.Quashie PK, Sloan RD, Wainberg MA. 2012. Novel therapeutic strategies targeting HIV integrase. BMC Med 10:34. doi: 10.1186/1741-7015-10-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Raffi F, Rachlis A, Stellbrink HJ, Hardy WD, Torti C, Orkin C, Bloch M, Podzamczer D, Pokrovsky V, Pulido F, Almond S, Margolis D, Brennan C, Min S, SPRING-2 Study Group. 2013. Once-daily dolutegravir versus raltegravir in antiretroviral-naive adults with HIV-1 infection: 48 week results from the randomised, double-blind, non-inferiority SPRING-2 study. Lancet 381:735–743. doi: 10.1016/S0140-6736(12)61853-4. [DOI] [PubMed] [Google Scholar]
- 200.Messiaen P, Wensing AM, Fun A, Nijhuis M, Brusselaers N, Vandekerckhove L. 2013. Clinical use of HIV integrase inhibitors: a systematic review and meta-analysis. PLoS One 8:e52562. doi: 10.1371/journal.pone.0052562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Cahn P, Pozniak AL, Mingrone H, Shuldyakov A, Brites C, Andrade-Villanueva JF, Richmond G, Buendia CB, Fourie J, Ramgopal M, Hagins D, Felizarta F, Madruga J, Reuter T, Newman T, Small CB, Lombaard J, Grinsztejn B, Dorey D, Underwood M, Griffith S, Min S, Extended SAILING Study Team. 2013. Dolutegravir versus raltegravir in antiretroviral-experienced, integrase-inhibitor-naive adults with HIV: week 48 results from the randomised, double-blind, non-inferiority SAILING study. Lancet 382:700–708. doi: 10.1016/S0140-6736(13)61221-0. [DOI] [PubMed] [Google Scholar]
- 202.Pozniak AL, Arribas JR. 2014. FLAMINGO: how much rosier can antiretroviral therapy get? Lancet 383:2191–2193. doi: 10.1016/S0140-6736(14)60447-5. [DOI] [PubMed] [Google Scholar]
- 203.Clotet B, Feinberg J, van Lunzen J, Khuong-Josses MA, Antinori A, Dumitru I, Pokrovskiy V, Fehr J, Ortiz R, Saag M, Harris J, Brennan C, Fujiwara T, Min S, ING114915 Study Team. 2014. Once-daily dolutegravir versus darunavir plus ritonavir in antiretroviral-naive adults with HIV-1 infection (FLAMINGO): 48 week results from the randomised open-label phase 3b study. Lancet 383:2222–2231. doi: 10.1016/S0140-6736(14)60084-2. [DOI] [PubMed] [Google Scholar]
- 204.Andrews CD, Yueh YL, Spreen WR, St Bernard L, Boente-Carrera M, Rodriguez K, Gettie A, Russell-Lodrigue K, Blanchard J, Ford S, Mohri H, Cheng-Mayer C, Hong Z, Ho DD, Markowitz M. 2015. A long-acting integrase inhibitor protects female macaques from repeated high-dose intravaginal SHIV challenge. Sci Transl Med 7:270ra4. doi: 10.1126/scitranslmed.3010298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Radzio J, Spreen W, Yueh YL, Mitchell J, Jenkins L, Garcia-Lerma JG, Heneine W. 2015. The long-acting integrase inhibitor GSK744 protects macaques from repeated intravaginal SHIV challenge. Sci Transl Med 7:270ra5. doi: 10.1126/scitranslmed.3010297. [DOI] [PubMed] [Google Scholar]
- 206.Andrews CD, Spreen WR, Mohri H, Moss L, Ford S, Gettie A, Russell-Lodrigue K, Bohm RP, Cheng-Mayer C, Hong Z, Markowitz M, Ho DD. 2014. Long-acting integrase inhibitor protects macaques from intrarectal simian/human immunodeficiency virus. Science 343:1151–1154. doi: 10.1126/science.1248707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Margolis DA, Brinson CC, Smith GH, de Vente J, Hagins DP, Eron JJ, Griffith SK, St Clair MH, Stevens MC, Williams PE, Ford SL, Stancil BS, Bomar MM, Hudson KJ, Smith KY, Spreen WR, LAI116482 Study Team. 2015. Cabotegravir plus rilpivirine, once a day, after induction with cabotegravir plus nucleoside reverse transcriptase inhibitors in antiretroviral-naive adults with HIV-1 infection (LATTE): a randomised, phase 2b, dose-ranging trial. Lancet Infect Dis 15:1145–1155. doi: 10.1016/S1473-3099(15)00152-8. [DOI] [PubMed] [Google Scholar]
- 208.Matthews T, Salgo M, Greenberg M, Chung J, DeMasi R, Bolognesi D. 2004. Enfuvirtide: the first therapy to inhibit the entry of HIV-1 into host CD4 lymphocytes. Nat Rev Drug Discov 3:215–225. doi: 10.1038/nrd1331. [DOI] [PubMed] [Google Scholar]
- 209.Wild C, Greenwell T, Matthews T. 1993. A synthetic peptide from HIV-1 gp41 is a potent inhibitor of virus-mediated cell-cell fusion. AIDS Res Hum Retroviruses 9:1051–1053. doi: 10.1089/aid.1993.9.1051. [DOI] [PubMed] [Google Scholar]
- 210.Berkhout B, Eggink D, Sanders RW. 2012. Is there a future for antiviral fusion inhibitors? Curr Opin Virol 2:50–59. doi: 10.1016/j.coviro.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 211.Kilby JM, Hopkins S, Venetta TM, DiMassimo B, Cloud GA, Lee JY, Alldredge L, Hunter E, Lambert D, Bolognesi D, Matthews T, Johnson MR, Nowak MA, Shaw GM, Saag MS. 1998. Potent suppression of HIV-1 replication in humans by T-20, a peptide inhibitor of gp41-mediated virus entry. Nat Med 4:1302–1307. doi: 10.1038/3293. [DOI] [PubMed] [Google Scholar]
- 212.Lalezari JP, Henry K, O'Hearn M, Montaner JS, Piliero PJ, Trottier B, Walmsley S, Cohen C, Kuritzkes DR, Eron JJ Jr, Chung J, DeMasi R, Donatacci L, Drobnes C, Delehanty J, Salgo M, TORO 1 Study Group . 2003. Enfuvirtide, an HIV-1 fusion inhibitor, for drug-resistant HIV infection in North and South America. N Engl J Med 348:2175–2185. doi: 10.1056/NEJMoa035026. [DOI] [PubMed] [Google Scholar]
- 213.Lazzarin A, Clotet B, Cooper D, Reynes J, Arasteh K, Nelson M, Katlama C, Stellbrink HJ, Delfraissy JF, Lange J, Huson L, DeMasi R, Wat C, Delehanty J, Drobnes C, Salgo M, TORO 2 Study Group . 2003. Efficacy of enfuvirtide in patients infected with drug-resistant HIV-1 in Europe and Australia. N Engl J Med 348:2186–2195. doi: 10.1056/NEJMoa035211. [DOI] [PubMed] [Google Scholar]
- 214.Henrich TJ, Kuritzkes DR. 2013. HIV-1 entry inhibitors: recent development and clinical use. Curr Opin Virol 3:51–57. doi: 10.1016/j.coviro.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Kuritzkes DR. 2009. HIV-1 entry inhibitors: an overview. Curr Opin HIV AIDS 4:82–87. doi: 10.1097/COH.0b013e328322402e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Alkhatib G, Combadiere C, Broder CC, Feng Y, Kennedy PE, Murphy PM, Berger EA. 1996. CC CKR5: a RANTES, MIP-1alpha, MIP-1beta receptor as a fusion cofactor for macrophage-tropic HIV-1. Science 272:1955–1958. doi: 10.1126/science.272.5270.1955. [DOI] [PubMed] [Google Scholar]
- 217.Baba M, Nishimura O, Kanzaki N, Okamoto M, Sawada H, Iizawa Y, Shiraishi M, Aramaki Y, Okonogi K, Ogawa Y, Meguro K, Fujino M. 1999. A small-molecule, nonpeptide CCR5 antagonist with highly potent and selective anti-HIV-1 activity. Proc Natl Acad Sci U S A 96:5698–5703. doi: 10.1073/pnas.96.10.5698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Baba M, Miyake H, Wang X, Okamoto M, Takashima K. 2007. Isolation and characterization of human immunodeficiency virus type 1 resistant to the small-molecule CCR5 antagonist TAK-652. Antimicrob Agents Chemother 51:707–715. doi: 10.1128/AAC.01079-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.De Clercq E. 2009. Antiviral drug discovery: ten more compounds, and ten more stories (part B). Med Res Rev 29:571–610. doi: 10.1002/med.20149. [DOI] [PubMed] [Google Scholar]
- 220.Dorr P, Westby M, Dobbs S, Griffin P, Irvine B, Macartney M, Mori J, Rickett G, Smith-Burchnell C, Napier C, Webster R, Armour D, Price D, Stammen B, Wood A, Perros M. 2005. Maraviroc (UK-427,857), a potent, orally bioavailable, and selective small-molecule inhibitor of chemokine receptor CCR5 with broad-spectrum anti-human immunodeficiency virus type 1 activity. Antimicrob Agents Chemother 49:4721–4732. doi: 10.1128/AAC.49.11.4721-4732.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Fatkenheuer G, Pozniak AL, Johnson MA, Plettenberg A, Staszewski S, Hoepelman AI, Saag MS, Goebel FD, Rockstroh JK, Dezube BJ, Jenkins TM, Medhurst C, Sullivan JF, Ridgway C, Abel S, James IT, Youle M, van der Ryst E. 2005. Efficacy of short-term monotherapy with maraviroc, a new CCR5 antagonist, in patients infected with HIV-1. Nat Med 11:1170–1172. doi: 10.1038/nm1319. [DOI] [PubMed] [Google Scholar]
- 222.Gulick RM, Lalezari J, Goodrich J, Clumeck N, DeJesus E, Horban A, Nadler J, Clotet B, Karlsson A, Wohlfeiler M, Montana JB, McHale M, Sullivan J, Ridgway C, Felstead S, Dunne MW, van der Ryst E, Mayer H, Motivate Study Teams. 2008. Maraviroc for previously treated patients with R5 HIV-1 infection. N Engl J Med 359:1429–1441. doi: 10.1056/NEJMoa0803152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Dolin R. 2008. A new class of anti-HIV therapy and new challenges. N Engl J Med 359:1509–1511. doi: 10.1056/NEJMe0806598. [DOI] [PubMed] [Google Scholar]
- 224.Fatkenheuer G, Nelson M, Lazzarin A, Konourina I, Hoepelman AI, Lampiris H, Hirschel B, Tebas P, Raffi F, Trottier B, Bellos N, Saag M, Cooper DA, Westby M, Tawadrous M, Sullivan JF, Ridgway C, Dunne MW, Felstead S, Mayer H, van der Ryst E, MOTIVATE 1 and MOTIVATE 2 Study Teams . 2008. Subgroup analyses of maraviroc in previously treated R5 HIV-1 infection. N Engl J Med 359:1442–1455. doi: 10.1056/NEJMoa0803154. [DOI] [PubMed] [Google Scholar]
- 225.Raymond S, Maillard A, Amiel C, Peytavin G, Trabaud MA, Desbois D, Bellecave P, Delaugerre C, Soulie C, Marcelin AG, Descamps D, Izopet J, ANRS AC11 Resistance Study Group . 2015. Virological failure of patients on maraviroc-based antiretroviral therapy. J Antimicrob Chemother 70:1858–1864. doi: 10.1093/jac/dkv026. [DOI] [PubMed] [Google Scholar]
- 226.Vigant F, Santos NC, Lee B. 2015. Broad-spectrum antivirals against viral fusion. Nat Rev Microbiol 13:426–437. doi: 10.1038/nrmicro3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Robinson RF, Nahata MC. 2000. Respiratory syncytial virus (RSV) immune globulin and palivizumab for prevention of RSV infection. Am J Health Syst Pharm 57:259–264. [DOI] [PubMed] [Google Scholar]
- 228.PREVENT Study Group. 1997. Reduction of respiratory syncytial virus hospitalization among premature infants and infants with bronchopulmonary dysplasia using respiratory syncytial virus immune globulin prophylaxis. Pediatrics 99:93–99. doi: 10.1542/peds.99.1.93. [DOI] [PubMed] [Google Scholar]
- 229.Black CP. 2003. Systematic review of the biology and medical management of respiratory syncytial virus infection. Respir Care 48:209–231. [PubMed] [Google Scholar]
- 230.Prescott WA Jr, Doloresco F, Brown J, Paladino JA. 2010. Cost effectiveness of respiratory syncytial virus prophylaxis: a critical and systematic review. Pharmacoeconomics 28:279–293. doi: 10.2165/11531860-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 231.Wright M, Piedimonte G. 2011. Respiratory syncytial virus prevention and therapy: past, present, and future. Pediatr Pulmonol 46:324–347. doi: 10.1002/ppul.21377. [DOI] [PubMed] [Google Scholar]
- 232.American Academy of Pediatrics Committee on Infectious Diseases, American Academy of Pediatrics Bronchiolitis Guidelines Committee. 2014. Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics 134:415–420. doi: 10.1542/peds.2014-1665. [DOI] [PubMed] [Google Scholar]
- 233.IMpact-RSV Study Group. 1998. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics 102:531–537. doi: 10.1542/peds.102.3.531. [DOI] [PubMed] [Google Scholar]
- 234.Feltes TF, Cabalka AK, Meissner HC, Piazza FM, Carlin DA, Top FH Jr, Connor EM, Sondheimer HM, Cardiac Synagis Study Group . 2003. Palivizumab prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant congenital heart disease. J Pediatr 143:532–540. doi: 10.1067/S0022-3476(03)00454-2. [DOI] [PubMed] [Google Scholar]
- 235.Committee on Infectious Diseases. 2009. From the American Academy of Pediatrics: policy statements—modified recommendations for use of palivizumab for prevention of respiratory syncytial virus infections. Pediatrics 124:1694–1701. doi: 10.1542/peds.2009-2345. [DOI] [PubMed] [Google Scholar]
- 236.Wang D, Bayliss S, Meads C. 2011. Palivizumab for immunoprophylaxis of respiratory syncytial virus (RSV) bronchiolitis in high-risk infants and young children: a systematic review and additional economic modelling of subgroup analyses. Health Technol Assess 15:1–124. doi: 10.3310/hta15050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Centers for Disease Control and Prevention. 1984. Varicella-zoster immune globulin for the prevention of chickenpox. MMWR Morb Mortal Wkly Rep 33:84–90, 95–100. [PubMed] [Google Scholar]
- 238.Zaia JA, Levin MJ, Preblud SR, Leszczynski J, Wright GG, Ellis RJ, Curtis AC, Valerio MA, LeGore J. 1983. Evaluation of varicella-zoster immune globulin: protection of immunosuppressed children after household exposure to varicella. J Infect Dis 147:737–743. doi: 10.1093/infdis/147.4.737. [DOI] [PubMed] [Google Scholar]
- 239.Marin M, Guris D, Chaves SS, Schmid S, Seward JF, Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention. 2007. Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recommend Rep 56:1–40. [PubMed] [Google Scholar]
- 240.Centers for Disease Control and Prevention. 2012. FDA approval of an extended period for administering VariZIG for postexposure prophylaxis of varicella. MMWR Morb Mortal Wkly Rep 61:212. [PubMed] [Google Scholar]
- 241.Sacks SL, Thisted RA, Jones TM, Barbarash RA, Mikolich DJ, Ruoff GE, Jorizzo JL, Gunnill LB, Katz DH, Khalil MH, Morrow PR, Yakatan GJ, Pope LE, Berg JE, Docosanol 10% Cream Study Group. 2001. Clinical efficacy of topical docosanol 10% cream for herpes simplex labialis: a multicenter, randomized, placebo-controlled trial. J Am Acad Dermatol 45:222–230. doi: 10.1067/mjd.2001.116215. [DOI] [PubMed] [Google Scholar]
- 242.Katz DH, Marcelletti JF, Khalil MH, Pope LE, Katz LR. 1991. Antiviral activity of 1-docosanol, an inhibitor of lipid-enveloped viruses including herpes simplex. Proc Natl Acad Sci U S A 88:10825–10829. doi: 10.1073/pnas.88.23.10825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Spruance SL. 2002. N-docosanol (Abreva) for herpes labialis: problems and questions. J Am Acad Dermatol 47:457–458. doi: 10.1067/mjd.2002.122743. [DOI] [PubMed] [Google Scholar]
- 244.Pope LE, Marcelletti JF, Katz LR, Lin JY, Katz DH, Parish ML, Spear PG. 1998. The anti-herpes simplex virus activity of n-docosanol includes inhibition of the viral entry process. Antiviral Res 40:85–94. doi: 10.1016/S0166-3542(98)00048-5. [DOI] [PubMed] [Google Scholar]
- 245.De Clercq E, Field HJ. 2006. Antiviral prodrugs—the development of successful prodrug strategies for antiviral chemotherapy. Br J Pharmacol 147:1–11. doi: 10.1038/sj.bjp.0706446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.De Clercq E. 2008. The discovery of antiviral agents: ten different compounds, ten different stories. Med Res Rev 28:929–953. doi: 10.1002/med.20128. [DOI] [PubMed] [Google Scholar]
- 247.Elion GB, Furman PA, Fyfe JA, de Miranda P, Beauchamp L, Schaeffer HJ. 1977. Selectivity of action of an antiherpetic agent, 9-(2-hydroxyethoxymethyl) guanine. Proc Natl Acad Sci U S A 74:5716–5720. doi: 10.1073/pnas.74.12.5716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Schaeffer HJ, Beauchamp L, de Miranda P, Elion GB, Bauer DJ, Collins P. 1978. 9-(2-Hydroxyethoxymethyl) guanine activity against viruses of the herpes group. Nature 272:583–585. doi: 10.1038/272583a0. [DOI] [PubMed] [Google Scholar]
- 249.Bacon TH, Levin MJ, Leary JJ, Sarisky RT, Sutton D. 2003. Herpes simplex virus resistance to acyclovir and penciclovir after two decades of antiviral therapy. Clin Microbiol Rev 16:114–128. doi: 10.1128/CMR.16.1.114-128.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Kimberlin DW, Jester PM, Sanchez PJ, Ahmed A, Arav-Boger R, Michaels MG, Ashouri N, Englund JA, Estrada B, Jacobs RF, Romero JR, Sood SK, Whitworth MS, Abzug MJ, Caserta MT, Fowler S, Lujan-Zilbermann J, Storch GA, DeBiasi RL, Han JY, Palmer A, Weiner LB, Bocchini JA, Dennehy PH, Finn A, Griffiths PD, Luck S, Gutierrez K, Halasa N, Homans J, Shane AL, Sharland M, Simonsen K, Vanchiere JA, Woods CR, Sabo DL, Aban I, Kuo H, James SH, Prichard MN, Griffin J, Giles D, Acosta EP, Whitley RJ, National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. 2015. Valganciclovir for symptomatic congenital cytomegalovirus disease. N Engl J Med 372:933–943. doi: 10.1056/NEJMoa1404599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Sullivan V, Talarico CL, Stanat SC, Davis M, Coen DM, Biron KK. 1992. A protein kinase homologue controls phosphorylation of ganciclovir in human cytomegalovirus-infected cells. Nature 358:162–164. doi: 10.1038/358162a0. [DOI] [PubMed] [Google Scholar]
- 252.Vere Hodge R. 1993. Famciclovir and penciclovir. The mode of action of famciclovir including its conversion to penciclovir. Antivir Chem Chemother 4:67–84. [Google Scholar]
- 253.Gnann JW Jr, Skoldenberg B, Hart J, Aurelius E, Schliamser S, Studahl M, Eriksson BM, Hanley D, Aoki F, Jackson AC, Griffiths P, Miedzinski L, Hanfelt-Goade D, Hinthorn D, Ahlm C, Aksamit A, Cruz-Flores S, Dale I, Cloud G, Jester P, Whitley RJ, National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. 2015. Herpes simplex encephalitis: lack of clinical benefit of long-term valacyclovir therapy. Clin Infect Dis 61:683–691. doi: 10.1093/cid/civ369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.O'Brien JJ, Campoli-Richards DM. 1989. Acyclovir. An updated review of its antiviral activity, pharmacokinetic properties and therapeutic efficacy. Drugs 37:233–309. [DOI] [PubMed] [Google Scholar]
- 255.Kacer M, Kielberger L, Bouda M, Reischig T. 2015. Valganciclovir versus valacyclovir prophylaxis for prevention of cytomegalovirus: an economic perspective. Transpl Infect Dis 17:334–341. doi: 10.1111/tid.12383. [DOI] [PubMed] [Google Scholar]
- 256.Gopal MG, Shannoma, Kumar BCS, Ramesh M, Nandini AS, Manjunath NC. 2013. A comparative study to evaluate the efficacy and safety of acyclovir and famciclovir in the management of herpes zoster. J Clin Diagn Res 7:2904–2907. doi: 10.7860/JCDR/2013/7884.3670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.De Clercq E, Descamps J, De Somer P, Holý A. 1978. (S)-9-(2,3-Dihydroxypropyl)adenine: an aliphatic nucleoside analog with broad-spectrum antiviral activity. Science 200:563–565. doi: 10.1126/science.200.4341.563. [DOI] [PubMed] [Google Scholar]
- 258.De Clercq E, Holý A, Rosenberg I, Sakuma T, Balzarini J, Maudgal PC. 1986. A novel selective broad-spectrum anti-DNA virus agent. Nature 323:464–467. doi: 10.1038/323464a0. [DOI] [PubMed] [Google Scholar]
- 259.De Clercq E, Holý A. 2005. Acyclic nucleoside phosphonates: a key class of antiviral drugs. Nat Rev Drug Discov 4:928–940. doi: 10.1038/nrd1877. [DOI] [PubMed] [Google Scholar]
- 260.De Clercq E. 2013. The acyclic nucleoside phosphonates (ANPs): Antonin Holý's legacy. Med Res Rev 33:1278–1303. doi: 10.1002/med.21283. [DOI] [PubMed] [Google Scholar]
- 261.De Clercq E. 2003. Clinical potential of the acyclic nucleoside phosphonates cidofovir, adefovir, and tenofovir in treatment of DNA virus and retrovirus infections. Clin Microbiol Rev 16:569–596. doi: 10.1128/CMR.16.4.569-596.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Kitrinos KM, Corsa A, Liu Y, Flaherty J, Snow-Lampart A, Marcellin P, Borroto-Esoda K, Miller MD. 2014. No detectable resistance to tenofovir disoproxil fumarate after 6 years of therapy in patients with chronic hepatitis B. Hepatology 59:434–442. doi: 10.1002/hep.26686. [DOI] [PubMed] [Google Scholar]
- 263.Fung S, Kwan P, Fabri M, Horban A, Pelemis M, Hann HW, Gurel S, Caruntu FA, Flaherty JF, Massetto B, Dinh P, Corsa A, Subramanian GM, McHutchison JG, Husa P, Gane E. 2014. Randomized comparison of tenofovir disoproxil fumarate vs emtricitabine and tenofovir disoproxil fumarate in patients with lamivudine-resistant chronic hepatitis B. Gastroenterology 146:980–988. doi: 10.1053/j.gastro.2013.12.028. [DOI] [PubMed] [Google Scholar]
- 264.Brown RS Jr, McMahon BJ, Lok AS, Wong JB, Ahmed AT, Mouchli MA, Wang Z, Prokop LJ, Murad MH, Mohammed K. 2016. Antiviral therapy in chronic hepatitis B viral infection during pregnancy: a systematic review and meta-analysis. Hepatology 63:319–333. doi: 10.1002/hep.28302. [DOI] [PubMed] [Google Scholar]
- 265.Chen HL, Lee CN, Chang CH, Ni YH, Shyu MK, Chen SM, Hu JJ, Lin HH, Zhao LL, Mu SC, Lai MW, Lee CL, Lin HM, Tsai MS, Hsu JJ, Chen DS, Chan KA, Chang MH, Taiwan Study Group for the Prevention of Mother-to-Infant Transmission of HBV PreMIT Study. 2015. Efficacy of maternal tenofovir disoproxil fumarate in interrupting mother-to-infant transmission of hepatitis B virus. Hepatology 62:375–386. doi: 10.1002/hep.27837. [DOI] [PubMed] [Google Scholar]
- 266.Greenup AJ, Tan PK, Nguyen V, Glass A, Davison S, Chatterjee U, Holdaway S, Samarasinghe D, Jackson K, Locarnini SA, Levy MT. 2014. Efficacy and safety of tenofovir disoproxil fumarate in pregnancy to prevent perinatal transmission of hepatitis B virus. J Hepatol 61:502–507. doi: 10.1016/j.jhep.2014.04.038. [DOI] [PubMed] [Google Scholar]
- 267.Lavocat F, Deny P, Pichoud C, Al Hawajri N, Kitrinos K, Borroto-Esoda K, Zoulim F. 2013. Similar evolution of hepatitis B virus quasispecies in patients with incomplete adefovir response receiving tenofovir/emtricitabine combination or tenofovir monotherapy. J Hepatol 59:684–695. doi: 10.1016/j.jhep.2013.05.038. [DOI] [PubMed] [Google Scholar]
- 268.Lim YS, Byun KS, Yoo BC, Kwon SY, Kim YJ, An J, Lee HC, Lee YS. 2016. Tenofovir monotherapy versus tenofovir and entecavir combination therapy in patients with entecavir-resistant chronic hepatitis B with multiple drug failure: results of a randomised trial. Gut 65:852–860. doi: 10.1136/gutjnl-2014-308353. [DOI] [PubMed] [Google Scholar]
- 269.Lim YS, Yoo BC, Byun KS, Kwon SY, Kim YJ, An J, Lee HC, Lee YS. 23 March 2015. Tenofovir monotherapy versus tenofovir and entecavir combination therapy in adefovir-resistant chronic hepatitis B patients with multiple drug failure: results of a randomised trial. Gut doi: 10.1136/gutjnl-2014-308435. [DOI] [PubMed] [Google Scholar]
- 270.Marcellin P, Ahn SH, Ma X, Caruntu FA, Tak WY, Elkashab M, Chuang WL, Lim SG, Tabak F, Mehta R, Petersen J, Foster GR, Lou L, Martins EB, Dinh P, Lin L, Corsa A, Charuworn P, Subramanian GM, Reiser H, Reesink HW, Fung S, Strasser SI, Trinh H, Buti M, Gaeta GB, Hui AJ, Papatheodoridis G, Flisiak R, Chan HL, Study 149 Investigators. 2016. Combination of tenofovir disoproxil fumarate and peginterferon alpha-2a increases loss of hepatitis B surface antigen in patients with chronic hepatitis B. Gastroenterology 150:134–144. doi: 10.1053/j.gastro.2015.09.043. [DOI] [PubMed] [Google Scholar]
- 271.Terrault NA, Bzowej NH, Chang KM, Hwang JP, Jonas MM, Murad MH. 2016. AASLD guidelines for treatment of chronic hepatitis B. Hepatology 63:261–283. doi: 10.1002/hep.28156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.European Association for the Study of the Liver. 2012. EASL clinical practice guidelines: management of chronic hepatitis B virus infection. J Hepatol 57:167–185. doi: 10.1016/j.jhep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 273.De Clercq E. 2011. The clinical potential of the acyclic (and cyclic) nucleoside phosphonates: the magic of the phosphonate bond. Biochem Pharmacol 82:99–109. doi: 10.1016/j.bcp.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 274.De Clercq E. 2007. Acyclic nucleoside phosphonates: past, present and future. Bridging chemistry to HIV, HBV, HCV, HPV, adeno-, herpes-, and poxvirus infections: the phosphonate bridge. Biochem Pharmacol 73:911–922. doi: 10.1016/j.bcp.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 275.Sax PE, Wohl D, Yin MT, Post F, DeJesus E, Saag M, Pozniak A, Thompson M, Podzamczer D, Molina JM, Oka S, Koenig E, Trottier B, Andrade-Villanueva J, Crofoot G, Custodio JM, Plummer A, Zhong L, Cao H, Martin H, Callebaut C, Cheng AK, Fordyce MW, McCallister S, GS-US-292-0104/0111 Study Team . 2015. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomised, double-blind, phase 3, non-inferiority trials. Lancet 385:2606–2615. doi: 10.1016/S0140-6736(15)60616-X. [DOI] [PubMed] [Google Scholar]
- 276.Pozniak A, Markowitz M, Mills A, Stellbrink HJ, Antela A, Domingo P, Girard PM, Henry K, Nguyen T, Piontkowsky D, Garner W, White K, Guyer B. 2014. Switching to coformulated elvitegravir, cobicistat, emtricitabine, and tenofovir versus continuation of non-nucleoside reverse transcriptase inhibitor with emtricitabine and tenofovir in virologically suppressed adults with HIV (STRATEGY-NNRTI): 48 week results of a randomised, open-label, phase 3b non-inferiority trial. Lancet Infect Dis 14:590–599. doi: 10.1016/S1473-3099(14)70796-0. [DOI] [PubMed] [Google Scholar]
- 277.Mills A, Arribas JR, Andrade-Villanueva J, DiPerri G, Van Lunzen J, Koenig E, Elion R, Cavassini M, Madruga JV, Brunetta J, Shamblaw D, DeJesus E, Orkin C, Wohl DA, Brar I, Stephens JL, Girard PM, Huhn G, Plummer A, Liu YP, Cheng AK, McCallister S, GS-US-292-0109 Team. 2016. Switching from tenofovir disoproxil fumarate to tenofovir alafenamide in antiretroviral regimens for virologically suppressed adults with HIV-1 infection: a randomised, active-controlled, multicentre, open-label, phase 3, non-inferiority study. Lancet Infect Dis 16:43–52. doi: 10.1016/S1473-3099(15)00348-5. [DOI] [PubMed] [Google Scholar]
- 278.Ray AS, Fordyce MW, Hitchcock MJ. 2016. Tenofovir alafenamide: a novel prodrug of tenofovir for the treatment of human immunodeficiency virus. Antiviral Res 125:63–70. doi: 10.1016/j.antiviral.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 279.Wyatt C, Baeten JM. 2015. Tenofovir alafenamide for HIV infection: is less more? Lancet 385:2559–2560. doi: 10.1016/S0140-6736(15)60725-5. [DOI] [PubMed] [Google Scholar]
- 280.AASLD/IDSA HCV Guidance Panel. 2015. Hepatitis C guidance: AASLD-IDSA recommendations for testing, managing, and treating adults infected with hepatitis C virus. Hepatology 62:932–954. doi: 10.1002/hep.27950. [DOI] [PubMed] [Google Scholar]
- 281.De Clercq E. 2012. The race for interferon-free HCV therapies: a snapshot by the spring of 2012. Rev Med Virol 22:392–411. doi: 10.1002/rmv.1727. [DOI] [PubMed] [Google Scholar]
- 282.Nettles JH, Stanton RA, Broyde J, Amblard F, Zhang H, Zhou L, Shi J, McBrayer TR, Whitaker T, Coats SJ, Kohler JJ, Schinazi RF. 2014. Asymmetric binding to NS5A by daclatasvir (BMS-790052) and analogs suggests two novel modes of HCV inhibition. J Med Chem 57:10031–10043. doi: 10.1021/jm501291c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Liu D, Ji J, Ndongwe TP, Michailidis E, Rice CM, Ralston R, Sarafianos SG. 2015. Fast hepatitis C virus RNA elimination and NS5A redistribution by NS5A inhibitors studied by a multiplex assay approach. Antimicrob Agents Chemother 59:3482–3492. doi: 10.1128/AAC.00223-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Berger C, Romero-Brey I, Radujkovic D, Terreux R, Zayas M, Paul D, Harak C, Hoppe S, Gao M, Penin F, Lohmann V, Bartenschlager R. 2014. Daclatasvir-like inhibitors of NS5A block early biogenesis of hepatitis C virus-induced membranous replication factories, independent of RNA replication. Gastroenterology 147:1094–1105. doi: 10.1053/j.gastro.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 285.Manns M, Pol S, Jacobson IM, Marcellin P, Gordon SC, Peng CY, Chang TT, Everson GT, Heo J, Gerken G, Yoffe B, Towner WJ, Bourliere M, Metivier S, Chu CJ, Sievert W, Bronowicki JP, Thabut D, Lee YJ, Kao JH, McPhee F, Kopit J, Mendez P, Linaberry M, Hughes E, Noviello S, HALLMARK-DUAL Study Team. 2014. All-oral daclatasvir plus asunaprevir for hepatitis C virus genotype 1b: a multinational, phase 3, multicohort study. Lancet 384:1597–1605. doi: 10.1016/S0140-6736(14)61059-X. [DOI] [PubMed] [Google Scholar]
- 286.Kumada H, Suzuki Y, Ikeda K, Toyota J, Karino Y, Chayama K, Kawakami Y, Ido A, Yamamoto K, Takaguchi K, Izumi N, Koike K, Takehara T, Kawada N, Sata M, Miyagoshi H, Eley T, McPhee F, Damokosh A, Ishikawa H, Hughes E. 2014. Daclatasvir plus asunaprevir for chronic HCV genotype 1b infection. Hepatology 59:2083–2091. doi: 10.1002/hep.27113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Kumada H, Suzuki F, Suzuki Y, Toyota J, Karino Y, Chayama K, Kawakami Y, Fujiyama S, Ito T, Itoh Y, Tamura E, Ueki T, Ishikawa H, Hu W, McPhee F, Linaberry M, Hughes E. 2016. Randomized comparison of daclatasvir + asunaprevir versus telaprevir + peginterferon/ribavirin in Japanese HCV patients. J Gastroenterol Hepatol 31:14–22. doi: 10.1111/jgh.13073. [DOI] [PubMed] [Google Scholar]
- 288.Lawitz E, Gane E, Pearlman B, Tam E, Ghesquiere W, Guyader D, Alric L, Bronowicki JP, Lester L, Sievert W, Ghalib R, Balart L, Sund F, Lagging M, Dutko F, Shaughnessy M, Hwang P, Howe AY, Wahl J, Robertson M, Barr E, Haber B. 2015. Efficacy and safety of 12 weeks versus 18 weeks of treatment with grazoprevir (MK-5172) and elbasvir (MK-8742) with or without ribavirin for hepatitis C virus genotype 1 infection in previously untreated patients with cirrhosis and patients with previous null response with or without cirrhosis (C-WORTHY): a randomised, open-label phase 2 trial. Lancet 385:1075–1086. doi: 10.1016/S0140-6736(14)61795-5. [DOI] [PubMed] [Google Scholar]
- 289.Roth D, Nelson DR, Bruchfeld A, Liapakis A, Silva M, Monsour H Jr, Martin P, Pol S, Londono MC, Hassanein T, Zamor PJ, Zuckerman E, Wan S, Jackson B, Nguyen BY, Robertson M, Barr E, Wahl J, Greaves W. 2015. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4-5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet 386:1537–1545. doi: 10.1016/S0140-6736(15)00349-9. [DOI] [PubMed] [Google Scholar]
- 290.Zeuzem S, Ghalib R, Reddy KR, Pockros PJ, Ben Ari Z, Zhao Y, Brown DD, Wan S, DiNubile MJ, Nguyen BY, Robertson MN, Wahl J, Barr E, Butterton JR. 2015. Grazoprevir-elbasvir combination therapy for treatment-naive cirrhotic and noncirrhotic patients with chronic hepatitis C virus genotype 1, 4, or 6 infection: a randomized trial. Ann Intern Med 163:1–13. doi: 10.7326/M15-0785. [DOI] [PubMed] [Google Scholar]
- 291.Buti M, Riveiro-Barciela M, Esteban R. 2015. Management of direct-acting antiviral agent failures. J Hepatol 63:1511–1522. doi: 10.1016/j.jhep.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 292.Wyles D, Pockros P, Morelli G, Younes Z, Svarovskaia E, Yang JC, Pang PS, Zhu Y, McHutchison JG, Flamm S, Lawitz E. 2015. Ledipasvir-sofosbuvir plus ribavirin for patients with genotype 1 hepatitis C virus previously treated in clinical trials of sofosbuvir regimens. Hepatology 61:1793–1797. doi: 10.1002/hep.27814. [DOI] [PubMed] [Google Scholar]
- 293.Bourliere M, Bronowicki JP, de Ledinghen V, Hezode C, Zoulim F, Mathurin P, Tran A, Larrey DG, Ratziu V, Alric L, Hyland RH, Jiang D, Doehle B, Pang PS, Symonds WT, Subramanian GM, McHutchison JG, Marcellin P, Habersetzer F, Guyader D, Grange JD, Loustaud-Ratti V, Serfaty L, Metivier S, Leroy V, Abergel A, Pol S. 2015. Ledipasvir-sofosbuvir with or without ribavirin to treat patients with HCV genotype 1 infection and cirrhosis non-responsive to previous protease-inhibitor therapy: a randomised, double-blind, phase 2 trial (SIRIUS). Lancet Infect Dis 15:397–404. doi: 10.1016/S1473-3099(15)70050-2. [DOI] [PubMed] [Google Scholar]
- 294.Naggie S, Cooper C, Saag M, Workowski K, Ruane P, Towner WJ, Marks K, Luetkemeyer A, Baden RP, Sax PE, Gane E, Santana-Bagur J, Stamm LM, Yang JC, German P, Dvory-Sobol H, Ni L, Pang PS, McHutchison JG, Stedman CA, Morales-Ramirez JO, Brau N, Jayaweera D, Colson AE, Tebas P, Wong DK, Dieterich D, Sulkowski M, ION-4 Investigators. 2015. Ledipasvir and sofosbuvir for HCV in patients coinfected with HIV-1. N Engl J Med 373:705–713. doi: 10.1056/NEJMoa1501315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Zeisel MB, Lucifora J, Mason WS, Sureau C, Beck J, Levrero M, Kann M, Knolle PA, Benkirane M, Durantel D, Michel ML, Autran B, Cosset FL, Strick-Marchand H, Trepo C, Kao JH, Carrat F, Lacombe K, Schinazi RF, Barre-Sinoussi F, Delfraissy JF, Zoulim F. 2015. Towards an HBV cure: state-of-the-art and unresolved questions—report of the ANRS workshop on HBV cure. Gut 64:1314–1326. doi: 10.1136/gutjnl-2014-308943. [DOI] [PubMed] [Google Scholar]
- 296.De Clercq E. 2015. Current treatment of hepatitis B virus infections. Rev Med Virol 25:354–365. doi: 10.1002/rmv.1849. [DOI] [PubMed] [Google Scholar]
- 297.Davies WL, Grunert RR, Haff RF, McGahen JW, Neumayer EM, Paulshock M, Watts JC, Wood TR, Hermann EC, Hoffmann CE. 1964. Antiviral activity of 1-adamantanamine (amantadine). Science 144:862–863. doi: 10.1126/science.144.3620.862. [DOI] [PubMed] [Google Scholar]
- 298.Liang R, Li H, Swanson JM, Voth GA. 2014. Multiscale simulation reveals a multifaceted mechanism of proton permeation through the influenza A M2 proton channel. Proc Natl Acad Sci U S A 111:9396–9401. doi: 10.1073/pnas.1401997111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Cady SD, Mishanina TV, Hong M. 2009. Structure of amantadine-bound M2 transmembrane peptide of influenza A in lipid bilayers from magic-angle-spinning solid-state NMR: the role of Ser31 in amantadine binding. J Mol Biol 385:1127–1141. doi: 10.1016/j.jmb.2008.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.De Clercq E. 2006. Antiviral agents active against influenza A viruses. Nat Rev Drug Discov 5:1015–1025. doi: 10.1038/nrd2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.De Clercq E. 2009. Another ten stories in antiviral drug discovery (part C): “old” and “new” antivirals, strategies, and perspectives. Med Res Rev 29:611–645. doi: 10.1002/med.20153. [DOI] [PubMed] [Google Scholar]
- 302.Alves Galvao MG, Rocha Crispino Santos MA, Alves da Cunha AJ. 2014. Amantadine and rimantadine for influenza A in children and the elderly. Cochrane Database Syst Rev 11:CD002745. doi: 10.1002/14651858.CD002745.pub4. [DOI] [PubMed] [Google Scholar]
- 303.Razonable RR. 2011. Antiviral drugs for viruses other than human immunodeficiency virus. Mayo Clin Proc 86:1009–1026. doi: 10.4065/mcp.2011.0309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Hubsher G, Haider M, Okun MS. 2012. Amantadine: the journey from fighting flu to treating Parkinson disease. Neurology 78:1096–1099. doi: 10.1212/WNL.0b013e31824e8f0d. [DOI] [PubMed] [Google Scholar]
- 305.Rodnitzky RL, Narayanan NS. 2014. Amantadine's role in the treatment of levodopa-induced dyskinesia. Neurology 82:288–289. doi: 10.1212/WNL.0000000000000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.von Itzstein M, Wu W-Y, Kok GB, Pegg MS, Dyason JC, Jin B, Van Phan T, Smythe ML, White HF, Oliver SW, Colman PM, Varghese JN, Ryan DM, Woods JM, Bethell RC, Hotham VJ, Cameron JM, Penn CR. 1993. Rational design of potent sialidase-based inhibitors of influenza virus replication. Nature 363:418–423. doi: 10.1038/363418a0. [DOI] [PubMed] [Google Scholar]
- 307.Russell RJ, Haire LF, Stevens DJ, Collins PJ, Lin YP, Blackburn GM, Hay AJ, Gamblin SJ, Skehel JJ. 2006. The structure of H5N1 avian influenza neuraminidase suggests new opportunities for drug design. Nature 443:45–49. doi: 10.1038/nature05114. [DOI] [PubMed] [Google Scholar]
- 308.McKimm-Breschkin J, Trivedi T, Hampson A, Hay A, Klimov A, Tashiro M, Hayden F, Zambon M. 2003. Neuraminidase sequence analysis and susceptibilities of influenza virus clinical isolates to zanamivir and oseltamivir. Antimicrob Agents Chemother 47:2264–2272. doi: 10.1128/AAC.47.7.2264-2272.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Hsu J, Santesso N, Mustafa R, Brozek J, Chen YL, Hopkins JP, Cheung A, Hovhannisyan G, Ivanova L, Flottorp SA, Saeterdal I, Wong AD, Tian J, Uyeki TM, Akl EA, Alonso-Coello P, Smaill F, Schunemann HJ. 2012. Antivirals for treatment of influenza: a systematic review and meta-analysis of observational studies. Ann Intern Med 156:512–524. doi: 10.7326/0003-4819-156-7-201204030-00411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.De Clercq E. 2013. Antivirals: past, present and future. Biochem Pharmacol 85:727–744. doi: 10.1016/j.bcp.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 311.McLaughlin MM, Skoglund EW, Ison MG. 2015. Peramivir: an intravenous neuraminidase inhibitor. Expert Opin Pharmacother 16:1889–1900. doi: 10.1517/14656566.2015.1066336. [DOI] [PubMed] [Google Scholar]
- 312.Watanabe A, Chang SC, Kim MJ, Chu DW, Ohashi Y, Marvel Study Group. 2010. Long-acting neuraminidase inhibitor laninamivir octanoate versus oseltamivir for treatment of influenza: a double-blind, randomized, noninferiority clinical trial. Clin Infect Dis 51:1167–1175. doi: 10.1086/656802. [DOI] [PubMed] [Google Scholar]
- 313.Yoo JW, Choi SH, Huh JW, Lim CM, Koh Y, Hong SB. 2015. Peramivir is as effective as oral oseltamivir in the treatment of severe seasonal influenza. J Med Virol 87:1649–1655. doi: 10.1002/jmv.24232. [DOI] [PubMed] [Google Scholar]
- 314.Li TC, Chan MC, Lee N. 2015. Clinical implications of antiviral resistance in influenza. Viruses 7:4929–4944. doi: 10.3390/v7092850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Sidwell RW, Huffman JH, Khare GP, Allen LB, Witkowski JT, Robins RK. 1972. Broad-spectrum antiviral activity of Virazole: 1-beta-D-ribofuranosyl-1,2,4-triazole-3-carboxamide. Science 177:705–706. doi: 10.1126/science.177.4050.705. [DOI] [PubMed] [Google Scholar]
- 316.Streeter DG, Witkowski JT, Khare GP, Sidwell RW, Bauer RJ, Robins RK, Simon LN. 1973. Mechanism of action of 1-beta-D-ribofuranosyl-1,2,4-triazole-3-carboxamide (Virazole), a new broad-spectrum antiviral agent. Proc Natl Acad Sci U S A 70:1174–1178. doi: 10.1073/pnas.70.4.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Wray SK, Gilbert BE, Noall MW, Knight V. 1985. Mode of action of ribavirin: effect of nucleotide pool alterations on influenza virus ribonucleoprotein synthesis. Antiviral Res 5:29–37. doi: 10.1016/0166-3542(85)90012-9. [DOI] [PubMed] [Google Scholar]
- 318.Potter CW, Phair JP, Vodinelich L, Fenton R, Jennings R. 1976. Antiviral, immunosuppressive and antitumour effects of ribavirin. Nature 259:496–497. doi: 10.1038/259496a0. [DOI] [PubMed] [Google Scholar]
- 319.Fried MW, Shiffman ML, Reddy KR, Smith C, Marinos G, Goncales FL Jr, Haussinger D, Diago M, Carosi G, Dhumeaux D, Craxi A, Lin A, Hoffman J, Yu J. 2002. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med 347:975–982. doi: 10.1056/NEJMoa020047. [DOI] [PubMed] [Google Scholar]
- 320.Torriani FJ, Rodriguez-Torres M, Rockstroh JK, Lissen E, Gonzalez-Garcia J, Lazzarin A, Carosi G, Sasadeusz J, Katlama C, Montaner J, Sette H Jr, Passe S, De Pamphilis J, Duff F, Schrenk UM, Dieterich DT, APRICOT Study Group. 2004. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection in HIV-infected patients. N Engl J Med 351:438–450. doi: 10.1056/NEJMoa040842. [DOI] [PubMed] [Google Scholar]
- 321.Hézode C, Forestier N, Dusheiko G, Ferenci P, Pol S, Goeser T, Bronowicki JP, Bourliere M, Gharakhanian S, Bengtsson L, McNair L, George S, Kieffer T, Kwong A, Kauffman RS, Alam J, Pawlotsky JM, Zeuzem S, PROVE2 Study Team. 2009. Telaprevir and peginterferon with or without ribavirin for chronic HCV infection. N Engl J Med 360:1839–1850. doi: 10.1056/NEJMoa0807650. [DOI] [PubMed] [Google Scholar]
- 322.Eriksson B, Helgstrand E, Johansson NG, Larsson A, Misiorny A, Noren JO, Philipson L, Stenberg K, Stening G, Stridh S, Oberg B. 1977. Inhibition of influenza virus ribonucleic acid polymerase by ribavirin triphosphate. Antimicrob Agents Chemother 11:946–951. doi: 10.1128/AAC.11.6.946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.McCormick JB, King IJ, Webb PA, Scribner CL, Craven RB, Johnson KM, Elliott LH, Belmont-Williams R. 1986. Lassa fever. Effective therapy with ribavirin. N Engl J Med 314:20–26. [DOI] [PubMed] [Google Scholar]
- 324.Kaur P, Chu JJ. 2013. Chikungunya virus: an update on antiviral development and challenges. Drug Discov Today 18:969–983. doi: 10.1016/j.drudis.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Kim Y, Galasiti Kankanamalage AC, Chang KO, Groutas WC. 2015. Recent advances in the discovery of norovirus therapeutics. J Med Chem 58:9438–9450. doi: 10.1021/acs.jmedchem.5b00762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Kocher J, Yuan L. 2015. Norovirus vaccines and potential antinorovirus drugs: recent advances and future perspectives. Future Virol 10:899–913. doi: 10.2217/fvl.15.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Mehedi M, Groseth A, Feldmann H, Ebihara H. 2011. Clinical aspects of Marburg hemorrhagic fever. Future Virol 6:1091–1106. doi: 10.2217/fvl.11.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Broder CC, Xu K, Nikolov DB, Zhu Z, Dimitrov DS, Middleton D, Pallister J, Geisbert TW, Bossart KN, Wang LF. 2013. A treatment for and vaccine against the deadly Hendra and Nipah viruses. Antiviral Res 100:8–13. doi: 10.1016/j.antiviral.2013.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Furuta Y, Takahashi K, Fukuda Y, Kuno M, Kamiyama T, Kozaki K, Nomura N, Egawa H, Minami S, Watanabe Y, Narita H, Shiraki K. 2002. In vitro and in vivo activities of anti-influenza virus compound T-705. Antimicrob Agents Chemother 46:977–981. doi: 10.1128/AAC.46.4.977-981.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Kiso M, Takahashi K, Sakai-Tagawa Y, Shinya K, Sakabe S, Le QM, Ozawa M, Furuta Y, Kawaoka Y. 2010. T-705 (favipiravir) activity against lethal H5N1 influenza A viruses. Proc Natl Acad Sci U S A 107:882–887. doi: 10.1073/pnas.0909603107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.De Clercq E. 2013. Highlights in antiviral drug research: antivirals at the horizon. Med Res Rev 33:1215–1248. doi: 10.1002/med.21256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Furuta Y, Takahashi K, Kuno-Maekawa M, Sangawa H, Uehara S, Kozaki K, Nomura N, Egawa H, Shiraki K. 2005. Mechanism of action of T-705 against influenza virus. Antimicrob Agents Chemother 49:981–986. doi: 10.1128/AAC.49.3.981-986.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Smee DF, Hurst BL, Egawa H, Takahashi K, Kadota T, Furuta Y. 2009. Intracellular metabolism of favipiravir (T-705) in uninfected and influenza A (H5N1) virus-infected cells. J Antimicrob Chemother 64:741–746. doi: 10.1093/jac/dkp274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Van Herp M, Declerck H, Decroo T. 2015. Favipiravir—a prophylactic treatment for Ebola contacts? Lancet 385:2350. doi: 10.1016/S0140-6736(15)61095-9. [DOI] [PubMed] [Google Scholar]
- 335.Oestereich L, Ludtke A, Wurr S, Rieger T, Munoz-Fontela C, Gunther S. 2014. Successful treatment of advanced Ebola virus infection with T-705 (favipiravir) in a small animal model. Antiviral Res 105:17–21. doi: 10.1016/j.antiviral.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 336.Smither SJ, Eastaugh LS, Steward JA, Nelson M, Lenk RP, Lever MS. 2014. Post-exposure efficacy of oral T-705 (favipiravir) against inhalational Ebola virus infection in a mouse model. Antiviral Res 104:153–155. doi: 10.1016/j.antiviral.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 337.De Clercq E. 2015. Ebola virus (EBOV) infection: therapeutic strategies. Biochem Pharmacol 93:1–10. doi: 10.1016/j.bcp.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Gowen BB, Juelich TL, Sefing EJ, Brasel T, Smith JK, Zhang L, Tigabu B, Hill TE, Yun T, Pietzsch C, Furuta Y, Freiberg AN. 2013. Favipiravir (T-705) inhibits Junin virus infection and reduces mortality in a guinea pig model of Argentine hemorrhagic fever. PLoS Negl Trop Dis 7:e2614. doi: 10.1371/journal.pntd.0002614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Furuta Y, Gowen BB, Takahashi K, Shiraki K, Smee DF, Barnard DL. 2013. Favipiravir (T-705), a novel viral RNA polymerase inhibitor. Antiviral Res 100:446–454. doi: 10.1016/j.antiviral.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Heim MH. 2013. 25 years of interferon-based treatment of chronic hepatitis C: an epoch coming to an end. Nat Rev Immunol 13:535–542. doi: 10.1038/nri3463. [DOI] [PubMed] [Google Scholar]
- 341.Hoffmann HH, Schneider WM, Rice CM. 2015. Interferons and viruses: an evolutionary arms race of molecular interactions. Trends Immunol 36:124–138. doi: 10.1016/j.it.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Crouse J, Kalinke U, Oxenius A. 2015. Regulation of antiviral T cell responses by type I interferons. Nat Rev Immunol 15:231–242. doi: 10.1038/nri3806. [DOI] [PubMed] [Google Scholar]
- 343.Ivashkiv LB, Donlin LT. 2014. Regulation of type I interferon responses. Nat Rev Immunol 14:36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Zoulim F, Durantel D. 2015. Antiviral therapies and prospects for a cure of chronic hepatitis B. Cold Spring Harb Perspect Med 5:a021501. doi: 10.1101/cshperspect.a021501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Perrillo R. 2009. Benefits and risks of interferon therapy for hepatitis B. Hepatology 49:S103–S111. doi: 10.1002/hep.22956. [DOI] [PubMed] [Google Scholar]
- 346.Scaglione SJ, Lok AS. 2012. Effectiveness of hepatitis B treatment in clinical practice. Gastroenterology 142:1360–1368. doi: 10.1053/j.gastro.2012.01.044. [DOI] [PubMed] [Google Scholar]
- 347.Lampertico P. 2015. The royal wedding in chronic hepatitis B: the haves and the have-nots for the combination of pegylated interferon and nucleos(t)ide therapy. Hepatology 61:1459–1461. doi: 10.1002/hep.27731. [DOI] [PubMed] [Google Scholar]
- 348.Brouwer WP, Xie Q, Sonneveld MJ, Zhang N, Zhang Q, Tabak F, Streinu-Cercel A, Wang JY, Idilman R, Reesink HW, Diculescu M, Simon K, Voiculescu M, Akdogan M, Mazur W, Reijnders JG, Verhey E, Hansen BE, Janssen HL, ARES Study Group. 2015. Adding pegylated interferon to entecavir for hepatitis B e antigen-positive chronic hepatitis B: a multicenter randomized trial (ARES study). Hepatology 61:1512–1522. doi: 10.1002/hep.27586. [DOI] [PubMed] [Google Scholar]
- 349.de Niet A, Stelma F, Jansen L, Sinnige MJ, Remmerswaal EB, Takkenberg RB, Kootstra NA, Reesink HW, van Lier RA, van Leeuwen EM. 2016. Restoration of T cell function in chronic hepatitis B patients upon treatment with interferon based combination therapy. J Hepatol 64:539–546. doi: 10.1016/j.jhep.2015.10.013. [DOI] [PubMed] [Google Scholar]
- 350.Miailhes P, Maynard-Muet M, Lebosse F, Carrat F, Bouix C, Lascoux-Combe C, Sogni P, Rey D, Barthe Y, Pol S, Cacoub P, Zoulim F, Piroth L. 2014. Role of a 48-week pegylated interferon therapy in hepatitis B e antigen positive HIV-co-infected patients on cART including tenofovir: EMVIPEG study. J Hepatol 61:761–769. doi: 10.1016/j.jhep.2014.05.030. [DOI] [PubMed] [Google Scholar]
- 351.Marcellin P, Wursthorn K, Wedemeyer H, Chuang WL, Lau G, Avila C, Peng CY, Gane E, Lim SG, Fainboim H, Foster GR, Safadi R, Rizzetto M, Manns M, Bao W, Trylesinski A, Naoumov N. 2015. Telbivudine plus pegylated interferon alfa-2a in a randomized study in chronic hepatitis B is associated with an unexpected high rate of peripheral neuropathy. J Hepatol 62:41–47. doi: 10.1016/j.jhep.2014.08.021. [DOI] [PubMed] [Google Scholar]
- 352.Beutner KR, Tyring SK, Trofatter KF Jr, Douglas JM Jr, Spruance S, Owens ML, Fox TL, Hougham AJ, Schmitt KA. 1998. Imiquimod, a patient-applied immune-response modifier for treatment of external genital warts. Antimicrob Agents Chemother 42:789–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Beutner KR, Spruance SL, Hougham AJ, Fox TL, Owens ML, Douglas JM Jr. 1998. Treatment of genital warts with an immune-response modifier (imiquimod). J Am Acad Dermatol 38:230–239. doi: 10.1016/S0190-9622(98)70243-9. [DOI] [PubMed] [Google Scholar]
- 354.Wiley DJ, Douglas J, Beutner K, Cox T, Fife K, Moscicki AB, Fukumoto L. 2002. External genital warts: diagnosis, treatment, and prevention. Clin Infect Dis 35:S210–S224. doi: 10.1086/342109. [DOI] [PubMed] [Google Scholar]
- 355.Baker DA, Ferris DG, Martens MG, Fife KH, Tyring SK, Edwards L, Nelson A, Ault K, Trofatter KF, Liu T, Levy S, Wu J. 2011. Imiquimod 3.75% cream applied daily to treat anogenital warts: combined results from women in two randomized, placebo-controlled studies. Infect Dis Obstet Gynecol 2011:806105. doi: 10.1155/2011/806105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Karnes JB, Usatine RP. 2014. Management of external genital warts. Am Fam Physician 90:312–318. [PubMed] [Google Scholar]
- 357.Chen ST, Dou J, Temple R, Agarwal R, Wu KM, Walker S. 2008. New therapies from old medicines. Nat Biotechnol 26:1077–1083. doi: 10.1038/nbt1008-1077. [DOI] [PubMed] [Google Scholar]
- 358.Schneider C, Segre T. 2009. Green tea: potential health benefits. Am Fam Physician 79:591–594. [PubMed] [Google Scholar]
- 359.Tatti S, Swinehart JM, Thielert C, Tawfik H, Mescheder A, Beutner KR. 2008. Sinecatechins, a defined green tea extract, in the treatment of external anogenital warts: a randomized controlled trial. Obstet Gynecol 111:1371–1379. doi: 10.1097/AOG.0b013e3181719b60. [DOI] [PubMed] [Google Scholar]
- 360.Gross G, Meyer KG, Pres H, Thielert C, Tawfik H, Mescheder A. 2007. A randomized, double-blind, four-arm parallel-group, placebo-controlled phase II/III study to investigate the clinical efficacy of two galenic formulations of polyphenon E in the treatment of external genital warts. J Eur Acad Dermatol Venereol 21:1404–1412. doi: 10.1111/j.1468-3083.2007.02441.x. [DOI] [PubMed] [Google Scholar]
- 361.Tyring S, Edwards L, Cherry LK, Ramsdell WM, Kotner S, Greenberg MD, Vance JC, Barnum G, Dromgoole SH, Killey FP, Toter T. 1998. Safety and efficacy of 0.5% podofilox gel in the treatment of anogenital warts. Arch Dermatol 134:33–38. doi: 10.1001/archderm.134.1.33. [DOI] [PubMed] [Google Scholar]
- 362.Greenberg MD, Rutledge LH, Reid R, Berman NR, Precop SL, Elswick RK Jr. 1991. A double-blind, randomized trial of 0.5% podofilox and placebo for the treatment of genital warts in women. Obstet Gynecol 77:735–739. [PubMed] [Google Scholar]
- 363.Gunter J. 2003. Genital and perianal warts: new treatment opportunities for human papillomavirus infection. Am J Obstet Gynecol 189:S3–S11. doi: 10.1067/S0002-9378(03)00789-0. [DOI] [PubMed] [Google Scholar]
- 364.Lopaschuk CC. 2013. New approach to managing genital warts. Can Fam Physician 59:731–736. [PMC free article] [PubMed] [Google Scholar]
- 365.de Smet MD, Meenken CJ, van den Horn GJ. 1999. Fomivirsen—a phosphorothioate oligonucleotide for the treatment of CMV retinitis. Ocul Immunol Inflamm 7:189–198. doi: 10.1076/ocii.7.3.189.4007. [DOI] [PubMed] [Google Scholar]
- 366.Grillone LR, Lanz R. 2001. Fomivirsen. Drugs Today (Barc) 37:245–255. doi: 10.1358/dot.2001.37.4.620590. [DOI] [PubMed] [Google Scholar]
- 367.Orr RM. 2001. Technology evaluation: fomivirsen, Isis Pharmaceuticals Inc/CIBA vision. Curr Opin Mol Ther 3:288–294. [PubMed] [Google Scholar]
- 368.Vitravene Study Group. 2002. A randomized controlled clinical trial of intravitreous fomivirsen for treatment of newly diagnosed peripheral cytomegalovirus retinitis in patients with AIDS. Am J Ophthalmol 133:467–474. doi: 10.1016/S0002-9394(02)01327-2. [DOI] [PubMed] [Google Scholar]
- 369.Lai CL, Ahn SH, Lee KS, Um SH, Cho M, Yoon SK, Lee JW, Park NH, Kweon YO, Sohn JH, Lee J, Kim JA, Han KH, Yuen MF. 2014. Phase IIb multicentred randomised trial of besifovir (LB80380) versus entecavir in Asian patients with chronic hepatitis B. Gut 63:996–1004. doi: 10.1136/gutjnl-2013-305138. [DOI] [PubMed] [Google Scholar]
- 370.Lampertico P. 2014. Oral antiviral therapy for hepatitis B: the case of besifovir, a new kid on the block with a long way to go. Gut 63:869–870. doi: 10.1136/gutjnl-2013-305859. [DOI] [PubMed] [Google Scholar]
- 371.Darling JM, Fried MW. 2009. Nitazoxanide: beyond parasites toward a novel agent for hepatitis C. Gastroenterology 136:760–763. doi: 10.1053/j.gastro.2009.01.020. [DOI] [PubMed] [Google Scholar]
- 372.Nikolova K, Gluud C, Grevstad B, Jakobsen JC. 2014. Nitazoxanide for chronic hepatitis C. Cochrane Database Syst Rev 4:CD009182. doi: 10.1002/14651858.CD009182.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Reichert JM. 2016. Antibodies to watch in 2016. MAbs 8:197–204. doi: 10.1080/19420862.2015.1125583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Schurmann D, Sobotha C, Gilmartin J, Robberechts M, De Lepeleire I, Yee KL, Guo Y, Liu R, Wagner F, Wagner JA, Butterton JR, Anderson MS. 2016. A randomized, double-blind, placebo-controlled, short-term monotherapy study of doravirine in treatment-naive HIV-infected individuals. AIDS 30:57–63. doi: 10.1097/QAD.0000000000000876. [DOI] [PubMed] [Google Scholar]
- 375.Ward JW, Mermin JH. 2015. Simple, effective, but out of reach? Public health implications of HCV drugs. N Engl J Med 373:2678–2680. doi: 10.1056/NEJMe1513245. [DOI] [PubMed] [Google Scholar]
- 376.Foster GR, Afdhal N, Roberts SK, Brau N, Gane EJ, Pianko S, Lawitz E, Thompson A, Shiffman ML, Cooper C, Towner WJ, Conway B, Ruane P, Bourliere M, Asselah T, Berg T, Zeuzem S, Rosenberg W, Agarwal K, Stedman CA, Mo H, Dvory-Sobol H, Han L, Wang J, McNally J, Osinusi A, Brainard DM, McHutchison JG, Mazzotta F, Tran TT, Gordon SC, Patel K, Reau N, Mangia A, Sulkowski M, ASTRAL-2 Investigators, ASTRAL-3 Investigators. 2015. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med 373:2608–2617. doi: 10.1056/NEJMoa1512612. [DOI] [PubMed] [Google Scholar]
- 377.Feld JJ, Jacobson IM, Hezode C, Asselah T, Ruane PJ, Gruener N, Abergel A, Mangia A, Lai CL, Chan HL, Mazzotta F, Moreno C, Yoshida E, Shafran SD, Towner WJ, Tran TT, McNally J, Osinusi A, Svarovskaia E, Zhu Y, Brainard DM, McHutchison JG, Agarwal K, Zeuzem S, ASTRAL-1 Investigators. 2015. Sofosbuvir and velpatasvir for HCV genotype 1, 2, 4, 5, and 6 infection. N Engl J Med 373:2599–2607. doi: 10.1056/NEJMoa1512610. [DOI] [PubMed] [Google Scholar]
- 378.Curry MP, O'Leary JG, Bzowej N, Muir AJ, Korenblat KM, Fenkel JM, Reddy KR, Lawitz E, Flamm SL, Schiano T, Teperman L, Fontana R, Schiff E, Fried M, Doehle B, An D, McNally J, Osinusi A, Brainard DM, McHutchison JG, Brown RS Jr, Charlton M, ASTRAL-4 Investigators. 2015. Sofosbuvir and velpatasvir for HCV in patients with decompensated cirrhosis. N Engl J Med 373:2618–2628. doi: 10.1056/NEJMoa1512614. [DOI] [PubMed] [Google Scholar]
- 379.Everson GT, Towner WJ, Davis MN, Wyles DL, Nahass RG, Thuluvath PJ, Etzkorn K, Hinestrosa F, Tong M, Rabinovitz M, McNally J, Brainard DM, Han L, Doehle B, McHutchison JG, Morgan T, Chung RT, Tran TT. 2015. Sofosbuvir with velpatasvir in treatment-naive noncirrhotic patients with genotype 1 to 6 hepatitis C virus infection: a randomized trial. Ann Intern Med 163:818–826. doi: 10.7326/M15-1000. [DOI] [PubMed] [Google Scholar]
- 380.Pianko S, Flamm SL, Shiffman ML, Kumar S, Strasser SI, Dore GJ, McNally J, Brainard DM, Han L, Doehle B, Mogalian E, McHutchison JG, Rabinovitz M, Towner WJ, Gane EJ, Stedman CA, Reddy KR, Roberts SK. 2015. Sofosbuvir plus velpatasvir combination therapy for treatment-experienced patients with genotype 1 or 3 hepatitis C virus infection: a randomized trial. Ann Intern Med 163:809–817. doi: 10.7326/M15-1014. [DOI] [PubMed] [Google Scholar]
- 381.Everson GT, Sims KD, Thuluvath PJ, Lawitz E, Hassanein T, Rodriguez-Torres M, Desta T, Hawkins T, Levin JM, Hinestrosa F, Rustgi V, Schwartz H, Younossi Z, Webster L, Gitlin N, Eley T, Huang SP, McPhee F, Grasela DM, Gardiner DF. 2016. Daclatasvir + asunaprevir + beclabuvir +/− ribavirin for chronic HCV genotype 1-infected treatment-naive patients. Liver Int 36:189–197. doi: 10.1111/liv.12964. [DOI] [PubMed] [Google Scholar]
- 382.Poordad F, Sievert W, Mollison L, Bennett M, Tse E, Brau N, Levin J, Sepe T, Lee SS, Angus P, Conway B, Pol S, Boyer N, Bronowicki JP, Jacobson I, Muir AJ, Reddy KR, Tam E, Ortiz-Lasanta G, de Ledinghen V, Sulkowski M, Boparai N, McPhee F, Hughes E, Swenson ES, Yin PD, Unity-1 Study Group . 2015. Fixed-dose combination therapy with daclatasvir, asunaprevir, and beclabuvir for noncirrhotic patients with HCV genotype 1 infection. JAMA 313:1728–1735. doi: 10.1001/jama.2015.3860. [DOI] [PubMed] [Google Scholar]
- 383.Muir AJ, Poordad F, Lalezari J, Everson G, Dore GJ, Herring R, Sheikh A, Kwo P, Hezode C, Pockros PJ, Tran A, Yozviak J, Reau N, Ramji A, Stuart K, Thompson AJ, Vierling J, Freilich B, Cooper J, Ghesquiere W, Yang R, McPhee F, Hughes EA, Swenson ES, Yin PD. 2015. Daclatasvir in combination with asunaprevir and beclabuvir for hepatitis C virus genotype 1 infection with compensated cirrhosis. JAMA 313:1736–1744. doi: 10.1001/jama.2015.3868. [DOI] [PubMed] [Google Scholar]
- 384.Pentikis HS, Matson M, Atiee G, Boehlecke B, Hutchins JT, Patti JM, Henson GW, Morris A. 2011. Pharmacokinetics and safety of FV-100, a novel oral anti-herpes zoster nucleoside analogue, administered in single and multiple doses to healthy young adult and elderly adult volunteers. Antimicrob Agents Chemother 55:2847–2854. doi: 10.1128/AAC.01446-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Dropulic LK, Cohen JI. 2010. Update on new antivirals under development for the treatment of double-stranded DNA virus infections. Clin Pharmacol Ther 88:610–619. doi: 10.1038/clpt.2010.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.McGuigan C, Pathirana RN, Migliore M, Adak R, Luoni G, Jones AT, Diez-Torrubia A, Camarasa MJ, Velazquez S, Henson G, Verbeken E, Sienaert R, Naesens L, Snoeck R, Andrei G, Balzarini J. 2007. Preclinical development of bicyclic nucleoside analogues as potent and selective inhibitors of varicella zoster virus. J Antimicrob Chemother 60:1316–1330. doi: 10.1093/jac/dkm376. [DOI] [PubMed] [Google Scholar]
- 387.McGuigan C, Balzarini J. 2009. FV100 as a new approach for the possible treatment of varicella-zoster virus infection. J Antimicrob Chemother 64:671–673. doi: 10.1093/jac/dkp294. [DOI] [PubMed] [Google Scholar]
- 388.Goldner T, Hewlett G, Ettischer N, Ruebsamen-Schaeff H, Zimmermann H, Lischka P. 2011. The novel anticytomegalovirus compound AIC246 (letermovir) inhibits human cytomegalovirus replication through a specific antiviral mechanism that involves the viral terminase. J Virol 85:10884–10893. doi: 10.1128/JVI.05265-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Goldner T, Hempel C, Ruebsamen-Schaeff H, Zimmermann H, Lischka P. 2014. Geno- and phenotypic characterization of human cytomegalovirus mutants selected in vitro after letermovir (AIC246) exposure. Antimicrob Agents Chemother 58:610–613. doi: 10.1128/AAC.01794-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Wildum S, Zimmermann H, Lischka P. 2015. In vitro drug combination studies of letermovir (AIC246, MK-8228) with approved anti-human cytomegalovirus (HCMV) and anti-HIV compounds in inhibition of HCMV and HIV replication. Antimicrob Agents Chemother 59:3140–3148. doi: 10.1128/AAC.00114-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Lischka P, Hewlett G, Wunberg T, Baumeister J, Paulsen D, Goldner T, Ruebsamen-Schaeff H, Zimmermann H. 2010. In vitro and in vivo activities of the novel anticytomegalovirus compound AIC246. Antimicrob Agents Chemother 54:1290–1297. doi: 10.1128/AAC.01596-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Chemaly RF, Ullmann AJ, Stoelben S, Richard MP, Bornhauser M, Groth C, Einsele H, Silverman M, Mullane KM, Brown J, Nowak H, Kolling K, Stobernack HP, Lischka P, Zimmermann H, Rubsamen-Schaeff H, Champlin RE, Ehninger G, AIC246 Study Team. 2014. Letermovir for cytomegalovirus prophylaxis in hematopoietic-cell transplantation. N Engl J Med 370:1781–1789. doi: 10.1056/NEJMoa1309533. [DOI] [PubMed] [Google Scholar]
- 393.Lischka P, Michel D, Zimmermann H. 2016. Characterization of cytomegalovirus breakthrough events in a phase 2 prophylaxis trial of letermovir (AIC246, MK 8228). J Infect Dis 213:23–30. doi: 10.1093/infdis/jiv352. [DOI] [PubMed] [Google Scholar]
- 394.Gogineni V, Schinazi RF, Hamann MT. 2015. Role of marine natural products in the genesis of antiviral agents. Chem Rev 115:9655–9706. doi: 10.1021/cr4006318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Chang MH, Chen DS. 2015. Prevention of hepatitis B. Cold Spring Harb Perspect Med 5:a021493. doi: 10.1101/cshperspect.a021493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Gagliardi AM, Andriolo BN, Torloni MR, Soares BG. 2016. Vaccines for preventing herpes zoster in older adults. Cochrane Database Syst Rev 3:CD008858. doi: 10.1002/14651858.CD008858.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Yoshikawa T, Kawamura Y, Ohashi M. 2016. Universal varicella vaccine immunization in Japan. Vaccine 34:1965–1970. doi: 10.1016/j.vaccine.2016.02.058. [DOI] [PubMed] [Google Scholar]
- 398.Burd EM. 2016. Human papillomavirus laboratory testing: the changing paradigm. Clin Microbiol Rev 29:291–319. doi: 10.1128/CMR.00013-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Kumar S, Henrickson KJ. 2012. Update on influenza diagnostics: lessons from the novel H1N1 influenza A pandemic. Clin Microbiol Rev 25:344–361. doi: 10.1128/CMR.05016-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Wong SS, Webby RJ. 2013. Traditional and new influenza vaccines. Clin Microbiol Rev 26:476–492. doi: 10.1128/CMR.00097-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Cheng VC, To KK, Tse H, Hung IF, Yuen KY. 2012. Two years after pandemic influenza A/2009/H1N1: what have we learned? Clin Microbiol Rev 25:223–263. doi: 10.1128/CMR.05012-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Johnston C, Corey L. 2016. Current concepts for genital herpes simplex virus infection: diagnostics and pathogenesis of genital tract shedding. Clin Microbiol Rev 29:149–161. doi: 10.1128/CMR.00043-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Johnston C, Koelle DM, Wald A. 2014. Current status and prospects for development of an HSV vaccine. Vaccine 32:1553–1560. doi: 10.1016/j.vaccine.2013.08.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Graham BS, Modjarrad K, McLellan JS. 2015. Novel antigens for RSV vaccines. Curr Opin Immunol 35:30–38. doi: 10.1016/j.coi.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Broadbent L, Groves H, Shields MD, Power UF. 2015. Respiratory syncytial virus, an ongoing medical dilemma: an expert commentary on respiratory syncytial virus prophylactic and therapeutic pharmaceuticals currently in clinical trials. Influenza Other Respir Viruses 9:169–178. doi: 10.1111/irv.12313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Wang D, Fu TM. 2014. Progress on human cytomegalovirus vaccines for prevention of congenital infection and disease. Curr Opin Virol 6:13–23. doi: 10.1016/j.coviro.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 407.Manicklal S, Emery VC, Lazzarotto T, Boppana SB, Gupta RK. 2013. The “silent” global burden of congenital cytomegalovirus. Clin Microbiol Rev 26:86–102. doi: 10.1128/CMR.00062-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Blanco-Lobo P, Bulnes-Ramos A, McConnell MJ, Navarro D, Perez-Romero P. 2016. Applying lessons learned from cytomegalovirus infection in transplant patients to vaccine design. Drug Discov Today 21:674–681. doi: 10.1016/j.drudis.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 409.Li SW, Zhao Q, Wu T, Chen S, Zhang J, Xia NS. 2015. The development of a recombinant hepatitis E vaccine HEV 239. Hum Vaccin Immunother 11:908–914. doi: 10.1080/21645515.2015.1008870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Krain LJ, Nelson KE, Labrique AB. 2014. Host immune status and response to hepatitis E virus infection. Clin Microbiol Rev 27:139–165. doi: 10.1128/CMR.00062-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Lion T. 2014. Adenovirus infections in immunocompetent and immunocompromised patients. Clin Microbiol Rev 27:441–462. doi: 10.1128/CMR.00116-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Kamar N, Dalton HR, Abravanel F, Izopet J. 2014. Hepatitis E virus infection. Clin Microbiol Rev 27:116–138. doi: 10.1128/CMR.00057-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Jiang P, Liu Y, Ma HC, Paul AV, Wimmer E. 2014. Picornavirus morphogenesis. Microbiol Mol Biol Rev 78:418–437. doi: 10.1128/MMBR.00012-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Mackey TK, Liang BA, Cuomo R, Hafen R, Brouwer KC, Lee DE. 2014. Emerging and reemerging neglected tropical diseases: a review of key characteristics, risk factors, and the policy and innovation environment. Clin Microbiol Rev 27:949–979. doi: 10.1128/CMR.00045-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Fooks AR, Banyard AC, Horton DL, Johnson N, McElhinney LM, Jackson AC. 2014. Current status of rabies and prospects for elimination. Lancet 384:1389–1399. doi: 10.1016/S0140-6736(13)62707-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.De Clercq E. 2005. Recent highlights in the development of new antiviral drugs. Curr Opin Microbiol 8:552–560. doi: 10.1016/j.mib.2005.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Jones CL, Yeung BK, Manjunatha U, Shi PY, Bodenreider C, Diagana TT. 2015. Drug discovery for the developing world: progress at the Novartis Institute for Tropical Diseases. Nat Rev Drug Discov 14:442–444. doi: 10.1038/nrd4001-c1. [DOI] [PubMed] [Google Scholar]
- 418.Odumade OA, Hogquist KA, Balfour HH Jr. 2011. Progress and problems in understanding and managing primary Epstein-Barr virus infections. Clin Microbiol Rev 24:193–209. doi: 10.1128/CMR.00044-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Heegaard ED, Brown KE. 2002. Human parvovirus B19. Clin Microbiol Rev 15:485–505. doi: 10.1128/CMR.15.3.485-505.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Rogo LD, Mokhtari-Azad T, Kabir MH, Rezaei F. 2014. Human parvovirus B19: a review. Acta Virol 58:199–213. doi: 10.4149/av_2014_03_199. [DOI] [PubMed] [Google Scholar]
- 421.Robilotti E, Deresinski S, Pinsky BA. 2015. Norovirus. Clin Microbiol Rev 28:134–164. doi: 10.1128/CMR.00075-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Jacobs SE, Lamson DM, St George K, Walsh TJ. 2013. Human rhinoviruses. Clin Microbiol Rev 26:135–162. doi: 10.1128/CMR.00077-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Chan JF, Lau SK, To KK, Cheng VC, Woo PC, Yuen KY. 2015. Middle East respiratory syndrome coronavirus: another zoonotic betacoronavirus causing SARS-like disease. Clin Microbiol Rev 28:465–522. doi: 10.1128/CMR.00102-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Bosch A, Pinto RM, Guix S. 2014. Human astroviruses. Clin Microbiol Rev 27:1048–1074. doi: 10.1128/CMR.00013-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Oka T, Wang Q, Katayama K, Saif LJ. 2015. Comprehensive review of human sapoviruses. Clin Microbiol Rev 28:32–53. doi: 10.1128/CMR.00011-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Halstead SB, Cohen SN. 2015. Dengue hemorrhagic fever at 60 years: early evolution of concepts of causation and treatment. Microbiol Mol Biol Rev 79:281–291. doi: 10.1128/MMBR.00009-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Colpitts TM, Conway MJ, Montgomery RR, Fikrig E. 2012. West Nile virus: biology, transmission, and human infection. Clin Microbiol Rev 25:635–648. doi: 10.1128/CMR.00045-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Wong G, Kobinger GP. 2015. Backs against the wall: novel and existing strategies used during the 2014-2015 Ebola virus outbreak. Clin Microbiol Rev 28:593–601. doi: 10.1128/CMR.00014-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Messaoudi I, Amarasinghe GK, Basler CF. 2015. Filovirus pathogenesis and immune evasion: insights from Ebola virus and Marburg virus. Nat Rev Microbiol 13:663–676. doi: 10.1038/nrmicro3524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Olschlager S, Flatz L. 2013. Vaccination strategies against highly pathogenic arenaviruses: the next steps toward clinical trials. PLoS Pathog 9:e1003212. doi: 10.1371/journal.ppat.1003212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Patterson M, Grant A, Paessler S. 2014. Epidemiology and pathogenesis of Bolivian hemorrhagic fever. Curr Opin Virol 5:82–90. doi: 10.1016/j.coviro.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Shuaib W, Stanazai H, Abazid AG, Mattar AA. 16 March 2016. The reemergence of Zika virus: a review on pathogenesis, clinical manifestations, diagnosis, and treatment. Am J Med doi: 10.1016/j.amjmed.2016.02.027. [DOI] [PubMed] [Google Scholar]
- 433.Hoshino Y, Katano H, Zou P, Hohman P, Marques A, Tyring SK, Follmann D, Cohen JI. 2009. Long-term administration of valacyclovir reduces the number of Epstein-Barr virus (EBV)-infected B cells but not the number of EBV DNA copies per B cell in healthy volunteers. J Virol 83:11857–11861. doi: 10.1128/JVI.01005-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Gross L. 1953. A filterable agent, recovered from Ak leukemic extracts, causing salivary gland carcinomas in C3H mice. Proc Soc Exp Biol Med 83:414–421. doi: 10.3181/00379727-83-20376. [DOI] [PubMed] [Google Scholar]
- 435.Pinto M, Dobson S. 2014. BK and JC virus: a review. J Infect 68(Suppl 1):S2–S8. doi: 10.1016/j.jinf.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 436.Jelcic I, Combaluzier B, Jelcic I, Faigle W, Senn L, Reinhart BJ, Stroh L, Nitsch RM, Stehle T, Sospedra M, Grimm J, Martin R. 2015. Broadly neutralizing human monoclonal JC polyomavirus VP1-specific antibodies as candidate therapeutics for progressive multifocal leukoencephalopathy. Sci Transl Med 7:306ra150. doi: 10.1126/scitranslmed.aac8691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Salahuddin SZ, Ablashi DV, Markham PD, Josephs SF, Sturzenegger S, Kaplan M, Halligan G, Biberfeld P, Wong-Staal F, Kramarsky B, Gallo RZ. 1986. Isolation of a new virus, HBLV, in patients with lymphoproliferative disorders. Science 234:596–601. doi: 10.1126/science.2876520. [DOI] [PubMed] [Google Scholar]
- 438.Crabol Y, Terrier B, Rozenberg F, Pestre V, Legendre C, Hermine O, Montagnier-Petrissans C, Guillevin L, Mouthon L, Groupe d'Experts de l'Assistance Publique-Hôpitaux de Paris. 2013. Intravenous immunoglobulin therapy for pure red cell aplasia related to human parvovirus b19 infection: a retrospective study of 10 patients and review of the literature. Clin Infect Dis 56:968–977. doi: 10.1093/cid/cis1046. [DOI] [PubMed] [Google Scholar]
- 439.Bonvicini F, Bua G, Manaresi E, Gallinella G. 2015. Antiviral effect of cidofovir on parvovirus B19 replication. Antiviral Res 113:11–18. doi: 10.1016/j.antiviral.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 440.Musso D, Gubler DJ. 2016. Zika virus. Clin Microbiol Rev 29:487–524. doi: 10.1128/CMR.00072-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Cauchemez S, Besnard M, Bompard P, Dub T, Guillemette-Artur P, Eyrolle-Guignot D, Salje H, Van Kerkhove MD, Abadie V, Garel C, Fontanet A, Mallet HP. 15 March 2016. Association between Zika virus and microcephaly in French Polynesia, 2013-15: a retrospective study. Lancet doi: 10.1016/S0140-6736(16)00651-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Paixao ES, Barreto F, da Gloria Teixeira M, da Conceicao NCM, Rodrigues LC. 2016. History, epidemiology, and clinical manifestations of Zika: a systematic review. Am J Public Health 106:606–612. doi: 10.2105/AJPH.2016.303112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Cohen J. 2016. The race for a Zika vaccine is on. Science 351:543–544. doi: 10.1126/science.351.6273.543. [DOI] [PubMed] [Google Scholar]
- 444.Lucey DR, Gostin LO. 2016. The emerging Zika pandemic: enhancing preparedness. JAMA 315:865–866. doi: 10.1001/jama.2016.0904. [DOI] [PubMed] [Google Scholar]
- 445.Chang CK, Lo SC, Wang YS, Hou MH. 2016. Recent insights into the development of therapeutics against coronavirus diseases by targeting N protein. Drug Discov Today 21:562–572. doi: 10.1016/j.drudis.2015.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Zumla A, Chan JF, Azhar EI, Hui DS, Yuen KY. 12 February 2016. Coronaviruses—drug discovery and therapeutic options. Nat Rev Drug Discov doi: 10.1038/nrd.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Sanchez JL, Cooper MJ, Myers CA, Cummings JF, Vest KG, Russell KL, Sanchez JL, Hiser MJ, Gaydos CA. 2015. Respiratory infections in the U.S. military: recent experience and control. Clin Microbiol Rev 28:743–800. doi: 10.1128/CMR.00039-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.Suthar MS, Pulendran B. 2014. Systems analysis of West Nile virus infection. Curr Opin Virol 6:70–75. doi: 10.1016/j.coviro.2014.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Suthar MS, Diamond MS, Gale M Jr. 2013. West Nile virus infection and immunity. Nat Rev Microbiol 11:115–128. doi: 10.1038/nrmicro2950. [DOI] [PubMed] [Google Scholar]
- 450.Lim SP, Noble CG, Shi PY. 2015. The dengue virus NS5 protein as a target for drug discovery. Antiviral Res 119:57–67. doi: 10.1016/j.antiviral.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 451.Xie X, Zou J, Wang QY, Shi PY. 2015. Targeting dengue virus NS4B protein for drug discovery. Antiviral Res 118:39–45. doi: 10.1016/j.antiviral.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 452.Screaton G, Mongkolsapaya J, Yacoub S, Roberts C. 2015. New insights into the immunopathology and control of dengue virus infection. Nat Rev Immunol 15:745–759. doi: 10.1038/nri3916. [DOI] [PubMed] [Google Scholar]
- 453.Vannice KS, Durbin A, Hombach J. 11 March 2016. Status of vaccine research and development of vaccines for dengue. Vaccine doi: 10.1016/j.vaccine.2015.12.073. [DOI] [PubMed] [Google Scholar]
- 454.Dayan GH, Pugachev K, Bevilacqua J, Lang J, Monath TP. 2013. Preclinical and clinical development of a YFV 17 D-based chimeric vaccine against West Nile virus. Viruses 5:3048–3070. doi: 10.3390/v5123048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Beasley DW. 2011. Vaccines and immunotherapeutics for the prevention and treatment of infections with West Nile virus. Immunotherapy 3:269–285. doi: 10.2217/imt.10.93. [DOI] [PubMed] [Google Scholar]
- 456.Elseginy SA, Massarotti A, Nawwar GA, Amin KM, Brancale A. 2014. Small molecule inhibitors of West Nile virus. Antivir Chem Chemother 23:179–187. doi: 10.3851/IMP2581. [DOI] [PubMed] [Google Scholar]
- 457.Lim SP, Shi PY. 2013. West Nile virus drug discovery. Viruses 5:2977–3006. doi: 10.3390/v5122977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Mandl JN, Ahmed R, Barreiro LB, Daszak P, Epstein JH, Virgin HW, Feinberg MB. 2015. Reservoir host immune responses to emerging zoonotic viruses. Cell 160:20–35. doi: 10.1016/j.cell.2014.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Mendoza EJ, Qiu X, Kobinger GP. 2016. Progression of Ebola therapeutics during the 2014-2015 outbreak. Trends Mol Med 22:164–173. doi: 10.1016/j.molmed.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 460.Picazo E, Giordanetto F. 2015. Small molecule inhibitors of Ebola virus infection. Drug Discov Today 20:277–286. doi: 10.1016/j.drudis.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 461.Heald AE, Charleston JS, Iversen PL, Warren TK, Saoud JB, Al-Ibrahim M, Wells J, Warfield KL, Swenson DL, Welch LS, Sazani P, Wong M, Berry D, Kaye EM, Bavari S. 2015. AVI-7288 for Marburg virus in nonhuman primates and humans. N Engl J Med 373:339–348. doi: 10.1056/NEJMoa1410345. [DOI] [PubMed] [Google Scholar]
- 462.Middleton D, Pallister J, Klein R, Feng YR, Haining J, Arkinstall R, Frazer L, Huang JA, Edwards N, Wareing M, Elhay M, Hashmi Z, Bingham J, Yamada M, Johnson D, White J, Foord A, Heine HG, Marsh GA, Broder CC, Wang LF. 2014. Hendra virus vaccine, a one health approach to protecting horse, human, and environmental health. Emerg Infect Dis 20:372–379. doi: 10.3201/eid2003.131159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463.Satterfield BA, Dawes BE, Milligan GN. 11 March 2016. Status of vaccine research and development of vaccines for Nipah virus: prepared for WHO PD-VAC July 30, 2015. Vaccine doi: 10.1016/j.vaccine.2015.12.075. [DOI] [PubMed] [Google Scholar]
- 464.Falzarano D, Feldmann H. 2013. Vaccines for viral hemorrhagic fevers—progress and shortcomings. Curr Opin Virol 3:343–351. doi: 10.1016/j.coviro.2013.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.King AMQ, Adams MJ, Carstens EB, Lefkowitz EJ (ed). 2011. Virus taxonomy. Classification and nomenclature of viruses. Ninth report of the International Committee on Taxonomy of Viruses. Elsevier Academic Press, San Diego, CA. [Google Scholar]
- 466.Li G. 2014. HIV genome-wide diversity, interaction and coevolution. PhD thesis University of Leuven, Leuven, Belgium. [Google Scholar]
- 467.Kole R, Krainer AR, Altman S. 2012. RNA therapeutics: beyond RNA interference and antisense oligonucleotides. Nat Rev Drug Discov 11:125–140. doi: 10.1038/nrd3625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.Li G, Verheyen J, Rhee SY, Voet A, Vandamme A-M, Theys K. 2013. Functional conservation of HIV-1 gag: implications for rational drug design. Retrovirology 10:126. doi: 10.1186/1742-4690-10-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Boons E, Li G, Vanstreels E, Vercruysse T, Pannecouque C, Vandamme A-M, Daelemans D. 2014. A stably expressed llama single-domain intrabody targeting Rev displays broad-spectrum anti-HIV activity. Antiviral Res 112:91–102. doi: 10.1016/j.antiviral.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 470.Chomont N, El-Far M, Ancuta P, Trautmann L, Procopio FA, Yassine-Diab B, Boucher G, Boulassel MR, Ghattas G, Brenchley JM, Schacker TW, Hill BJ, Douek DC, Routy JP, Haddad EK, Sekaly RP. 2009. HIV reservoir size and persistence are driven by T cell survival and homeostatic proliferation. Nat Med 15:893–900. doi: 10.1038/nm.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.Churchill MJ, Deeks SG, Margolis DM, Siliciano RF, Swanstrom R. 2016. HIV reservoirs: what, where and how to target them. Nat Rev Microbiol 14:55–60. doi: 10.1038/nrmicro.2015.5. [DOI] [PubMed] [Google Scholar]
- 472.Hughes D, Andersson DI. 2015. Evolutionary consequences of drug resistance: shared principles across diverse targets and organisms. Nat Rev Genet 16:459–471. doi: 10.1038/nrg3922. [DOI] [PubMed] [Google Scholar]
- 473.Sulkowski MS. 2008. Viral hepatitis and HIV coinfection. J Hepatol 48:353–367. doi: 10.1016/j.jhep.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 474.Pawlotsky JM. 2014. New hepatitis C therapies: the toolbox, strategies, and challenges. Gastroenterology 146:1176–1192. doi: 10.1053/j.gastro.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 475.Kelesidis T, Falagas ME. 2015. Substandard/counterfeit antimicrobial drugs. Clin Microbiol Rev 28:443–464. doi: 10.1128/CMR.00072-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476.Scheel TK, Simmonds P, Kapoor A. 2015. Surveying the global virome: identification and characterization of HCV-related animal hepaciviruses. Antiviral Res 115:83–93. doi: 10.1016/j.antiviral.2014.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Hare S, Gupta SS, Valkov E, Engelman A, Cherepanov P. 2010. Retroviral intasome assembly and inhibition of DNA strand transfer. Nature 464:232–236. doi: 10.1038/nature08784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Wu H, Pfarr DS, Johnson S, Brewah YA, Woods RM, Patel NK, White WI, Young JF, Kiener PA. 2007. Development of motavizumab, an ultra-potent antibody for the prevention of respiratory syncytial virus infection in the upper and lower respiratory tract. J Mol Biol 368:652–665. doi: 10.1016/j.jmb.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 479.Schickli JH, Whitacre DC, Tang RS, Kaur J, Lawlor H, Peters CJ, Jones JE, Peterson DL, McCarthy MP, Van Nest G, Milich DR. 2015. Palivizumab epitope-displaying virus-like particles protect rodents from RSV challenge. J Clin Invest 125:1637–1647. doi: 10.1172/JCI78450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Chang S, Sun D, Liang H, Wang J, Li J, Guo L, Wang X, Guan C, Boruah BM, Yuan L, Feng F, Yang M, Wang L, Wang Y, Wojdyla J, Li L, Wang J, Wang M, Cheng G, Wang HW, Liu Y. 2015. Cryo-EM structure of influenza virus RNA polymerase complex at 4.3 A resolution. Mol Cell 57:925–935. doi: 10.1016/j.molcel.2014.12.031. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.