Summary
We spoligotyped and screened 1490 clinical Mycobacterium tuberculosis complex strains from Northern and Greater Accra regions of Ghana against INH and RIF using the microplate alamar blue phenotypic assay. Specific drug resistance associated genetic elements of drug resistant strains were analyzed for mutations. A total of 111 (7.5%), 10 (0.7%) and 40 (2.6%) were mono-resistant to INH, RIF, and MDR, respectively. We found the Ghana spoligotype to be associated with drug resistance (INH: 22.1%; p = 0.0000, RIF: 6.2%; p = 0.0103, MDR: 4.6%; p = 0.0240) as compared to the Cameroon spoligotype (INH: 6.7%, RIF: 2.4%, MDR: 1.6%). The propensity for an isolate to harbour katG S315T mutation was higher in M. tuberculosis (75.8%) than Mycobacterium africanum (51.7%) (p = 0.0000) whereas the opposite was true for inhApro mutations; MAF (48.3%) compared to MTBSS (26.7%) (p = 0.0419). We identified possible novel compensatory INH resistance mutations in inhA (G204D) and ahpCpro (-88G/A and -142G/A) and a novel ndh mutation K32R. We detected two possible rpoC mutations (G332R and V483G), which occurred independently with rpoB S450L, respectively. The study provides the first evidence that associate the Ghana spoligotype with DR-TB and calls for further genome analyses for proper classification of this spoligotype and to explore for fitness implications and mechanisms underlying this observation.
Keywords: Drug resistant, Spoligotype, Compensatory, Mutations, Virulence
1. Introduction
Tuberculosis (TB) remains an important global health problem, with close to 9 million new cases per year and a pool of approximately 2 billion latently infected individuals worldwide [1]. Of particular concern are the on-going epidemics of drug resistant TB (DR-TB), which threaten to make TB incurable. The main causative agents for human tuberculosis are Mycobacterium tuberculosis sensu stricto (MTBSS) and Mycobacterium africanum (MAF), both members of the M. tuberculosis complex (MTBC). Of particular interest to West Africa is MAF, which causes up to 50% of human TB in some countries [2].
Drug resistance to isoniazid (INH) and rifampicin (RIF), the two backbone-drugs of the directly observed treatment short-course (DOTS) regimen, can negatively affect the successful outcome of treatment of TB [3], [4]. The pro-drug INH requires activation by catalase peroxidase encoded by the katG of the target bacterium. Activated INH disturbs cell wall synthesis by binding to a 2-trans-enoyl-acyl carrier protein reductase (encoded by inhA) required for mycolic acid synthesis [5]. Rifampicin kills bacteria by halting the elongation of a nascent polynucleotide by occluding the path of the growing RNA through the polymerase [6]. katG (mostly S315T) and inhApro (mostly -15C/T) mutations are associated with high and low level INH resistance respectively [7]. Even though the katG mutation (inactive INH) and inhApro substitutions (overproduction of inhA) are the major causes of INH resistance, other loci such as ndh, inhA and ahpCpro have either been implicated with drug resistance or restoring the fitness cost associated with some high level resistance mutations [8], [9]. Some rpoB mutations alter the 3D structure of the rpoB hence affecting the conformation of the RIF-binding pocket which in effect prevents the rigid structure of RIF from binding to the bacterial polymerase to inhibit transcription [6], [10]. Even though rpoB mutations account for most RIF resistance in TB, mutations within the rpoA and rpoC have also been implicated with restoring the fitness cost associated with the acquisition of rpoB mutations [11]. Both katG S315T and rpoB S450L mutations (the most dominant INH and RIF resistance associated mutations respectively) have been associated with no/low fitness cost which may explain their dominance in clinical MTBC strains even though they confer high-level resistance [12], [13].
Though non-compliance of therapeutic regimen may contribute to the development of DR-TB, the contribution of the infecting bacteria cannot be underestimated. The Beijing strain of lineage 2 is associated with hyper-virulence and drug resistance even though reports on drug resistance are sometimes conflicting [14]. On the other hand, Lineage 1 is reported to be less virulent and negatively associated with high cost mutations, which are mostly responsible for high-level drug resistance [13], [14], [15]. This indicates that different genotypes of the MTBC may be associated with resistance to specific drugs and these associations may be driven by specific genetic alterations.
In this study, we screened MTBC strains isolated from pulmonary TB patients reporting to selected health centres from the Northern and Greater Accra Regions of Ghana for drug resistance to INH and RIF. We analysed specific genetic elements for DR associated mutations by DNA sequencing of implicated genes and looked for associations among drug resistance, bacterial genotypes and origin of the isolates.
2. Methodology
2.1. Ethical statement and participant enrolment
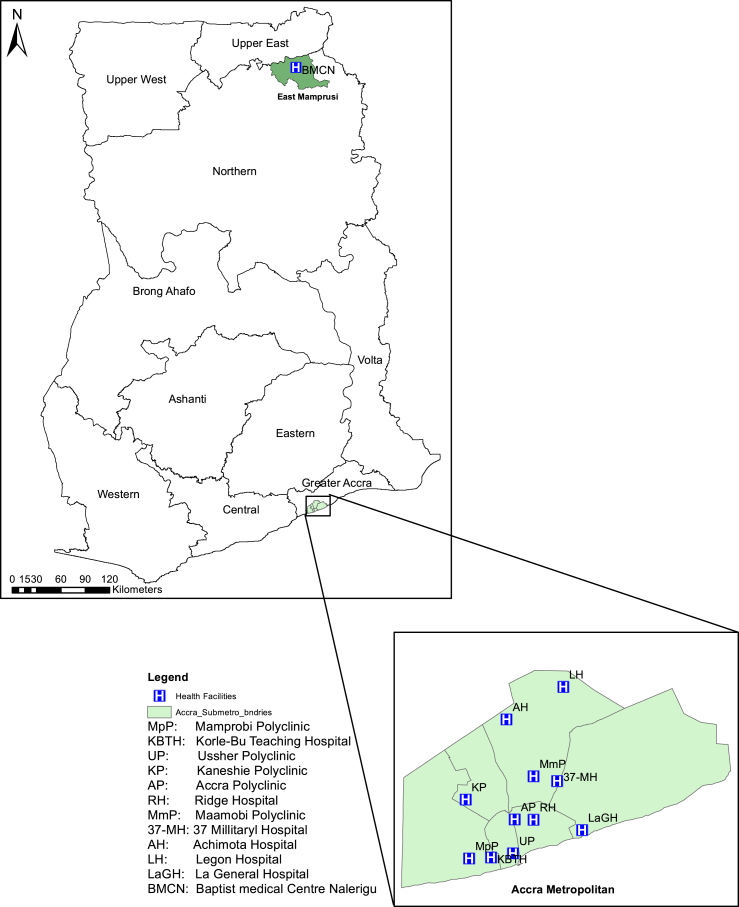
The Institutional Review Board of the Noguchi Memorial Institute for Medical Research (NMIMR) approved the study and its protocols. Following informed consent, consecutive sputum smear-positive TB cases who were not already taken anti-TB drugs or have been put on therapy for not more than 2 weeks were recruited from all TB diagnostic centres in the Accra Metropolitan (Southern Region) and the Mamprusi East (Northern Region) Health Administrations (Figure 1) from August 2012 to September, 2014. The standard procedure for sputum sample collection as outlined by the National Tuberculosis Control Program (NTP) for routine diagnosis of TB in Ghana was followed. Informed written consent was sought from all participants unless the participant was illiterate; in which case witnessed oral consent was used. Consent was sought from guardians of children below the age of 18 before enrolment into the study and in some cases child assent was also sought. Data collected from enrolled patients included age, sex, bacterial burden on day of diagnosis and TB treatment history.
Figure 1.
Map of Ghana showing the selected health centers from the two regions used for the study.
2.2. Mycobacterial isolates
The sputum samples were decontaminated with 5% oxalic acid [16], and inoculated on Lowenstein-Jensen Media (supplemented with either glycerol or pyruvate) slants, incubated at 37 °C until growth was observed. Colonies from positive cultures were sub-cultured on similar media and incubated as above until confluent growth was observed. The isolates (1490) were confirmed MTBC by PCR amplification of IS6110, genotyped as MTBSS, MAF and/or Mycobacterium bovis by large sequence polymorphism (LSPs) detecting region of difference (RD) 4, 9 and 12 [17] and spoligotyping as described by Kamerbeek et al. [18].
2.3. Anti-TB drug susceptibility testing
Micro-plate alamar blue assay (MABA) for drug susceptibility testing (DST) was performed in clear-bottomed, 96-well micro-plates (Nunc International, Rochester, NY, US). Drugs stocks were prepared by following standard protocols [19], and MABA-DST set up by following a modification of the method described by Franzblau et al. [20].
In summary, mycobacterial inoculum was prepared by emulsifying a loop full of logarithmic growing mycobacteria in sterile Middlebrook 7H9 [Difco, Detroit, Michigan] broth supplemented with 0.2% glycerol [Sigma-Aldrich, Steinheim, Germany] and 0.001% casitone [Difco] (7H9-GC) and adjusted spectrophotometrically to OD600 = 1.0 containing approximately 1 × 108 cfu/mL. This suspension was diluted 1:25 with 7H9-GC for inoculation. All perimeter wells of the plate were filled with 200 uL of sterile water to prevent evaporation of the content of inner wells. The test wells consisted of 7H9-GC/Tween 80 [Sigma-Aldrich] medium and respective concentration of testing drugs, (which were serially diluted to final concentrations of 0.03125–1.0 ug/mL and 0.0625 to 2.0 ug/mL for INH and RIF respectively) before inoculation with 100 μL of the mycobacterial suspension containing approximately 4 × 106 cfu/mL. The plates were incubated at 37 °C for 7 days, and bacterial viability was tested with freshly prepared 1:1 v/v of alamar blue reagent [Trek Diagnostic Systems, OH, USA] and 10% Tween 80. The minimum inhibitory concentration (MIC) defined as the concentration of drug in the first blue well for each drug, was then recorded (S1). The critical drug concentration was ≤0.25 ug/mL for both drugs [20]. The positive and negative controls for each set were drug-free media inoculated with bacterial suspension and un-inoculated containing media only respectively.
2.4. Isolation of genomic DNA
The protocol used for the extraction of genomic DNA was a synthesis of the protocols of Van Soolingen et al. [21] and Käser et al. [22]. Briefly, the mycobacterial cell wall was disrupted by adding lysozyme (50 μL lysozyme of 10 mg/mL) vortexed and incubated overnight, followed by addition of 75 μL of 10% SDS, 10 μL proteinase K (20 mg/mL), vortexed softly and incubated 15 min at 65 °C. After, the incubation, 100 μL of 5 M NaCl was added, followed by 100 μL CTAB which was pre-warmed at 65 °C. After vortexing, the extracted DNA was purified by chloroform/isoamyl alcohol extraction. The DNA contained in the upper phase was precipitated with isopropanol and washed with ethanol. The dried DNA was then re-suspended in 100 uL Tris EDTA buffer and stored at 4 °C until use.
2.5. PCR amplification and DNA sequencing of genetic elements
Drug resistant isolates were used for targeted sequencing analyses. Eight drug resistance associated genetic elements (rpoB, rpoA and rpoC for RIF resistant and inhApro, ahpCpro, inhA, ndh and katG for INH resistant strains) were analysed for mutations.
All PCR reactions were set up as previously described [23]. In summary, each set up contained 3 μL of 10X buffer, 1.8 μL of 15 mM MgCl2, 3 μL of Q solution, 0.6 μL of 10 mM dNTP mix, 1.8 μL of each primer, 0.2 μL of Hot-start Taq polymerase from Qiagen, 14.8 μL of nuclease-free water and 3 μL of template DNA. Cycling conditions were: initial denaturation at 95 °C for 15 min and 35 cycles of denaturation at 96 °C for 1 min, annealing at specific Tm (Table 1) for 1 min, extension at 68 °C for 1 min and final extension at 72 °C for 10 min. The obtained amplicons were shotgun sequenced in both directions by outsourcing to Macrogen Europe.
Table 1.
Primers and conditions for PCR amplification of genetic element.
| No. | Name | Sequence (5′–3′) | Tm (°C) | Target | Product size |
|---|---|---|---|---|---|
| 1 | rpoA1F | GCATTCCAGTCGATTCCATC | 57 | rpoA | 560 bp |
| 2 | rpoA1R | CCAAGATCGCCTTCTGATGT | |||
| 3 | rpoA2F | GGACGTCGAAAGGAAGAAGA | 57 | rpoA | 542 bp |
| 4 | rpoA2R | GTCTCCACGTCCAGGATCAG | |||
| 5 | rpoBF | GTAGTCCACGCCGTAAACGG | 65 | rpoB | 601 bp |
| 6 | rpoBR | ACGTCCATGTAGTCCACCTCAG | |||
| 7 | rpoCF | CGAAAACCTCTACCGCGAAC | 64 | rpoC | 650 bp |
| 8 | rpoCR | GCGACAGGATGTTGTTGGAG | |||
| 9 | inhAproF | ATCACCACCGCCGCTGAAGC | 65 | inhApro | 650 bp |
| 12 | inhAproR | GTTCGGGTACCCGGGAATG | |||
| 11 | inhA1F | CTACATCGACACCGATATGAC | 57 | inhA | 600 bp |
| 12 | inhA1R | GACCGTCATCCAGTTGTAG | |||
| 13 | inhA2F | GCATCAACCCGTTCTTCGAC | 57 | inhA | 550 bp |
| 14 | inhA2R | TAATGCCATTGATCGGTGATAC | |||
| 15 | ahpCproF | ACCACTGCTTTGCCGCCACC | 70 | ahpCpro | 340 bp |
| 16 | ahpCproR | CCGATGAGAGCGGTGAGCTG | |||
| 17 | katGF | CCAGCGGCCCAAGGTATC | 65 | katG | 820 bp |
| 18 | katGR | GCTGTGGCCGGTCAAGAAGAAGT | |||
| 19 | ndhF | ATCACCACCGCCGCTGAAGC | 64 | ndh | 589 bp |
| 20 | ndhR | GTTCGGGTACCCGGGAATG |
2.6. Data analyses
The DNA sequences were screened for possible mutations by comparing with the standard strain; H37Rv genome downloaded from the tuberculist database [24] using the Staden software [25]. DNA sequencing was repeated for all isolates with novel mutation(s) for verification. We compared the proportion and kind of mutations in MTBSS and MAF as well as the geographic origin of the isolates. The level of resistance between the different genotypes and the kind of mutation were compared with fishers exact tests using stata statistical package [26], with significance threshold set to P < 0.05.
3. Results
3.1. Clinical data of drug-resistant patients
Among the 161/1490 (10.8%) patients from whom MTBC strains resistant to at least one drug were isolated, 114 (70.8%) and 47 (29.2%) were males and females respectively. Drug-resistant TB patients up to 50 years were 113 (70.2%) whereas those above 50 years were 48 (29.8%). Whereas 128 (79.5%) of the DR-TB patients were having TB for the first time, 33 (20.5%) had been treated for TB before the current episode. Bacterial burden of the DR-TB patients stood at 9 (5.6%) scanty, 83 (51.6%) 1+, 29 (18.0%) 2+ and 40 (24.8%) 3+. 12.8% of drug resistant TB patients as compared to 12.2% of drug susceptible TB patients were HIV positive. Whereas 140 (87.0%) of the DR-TB patients were from the South representing 10.4% of TB patients reporting to the selected hospitals in the region, 21 (13.0%) were from the North representing 15.0% of the patients reporting to the selected hospital from that region.
3.2. Drug-susceptibility rates
One thousand four hundred and ninety isolates (MTBSS: 1208; 81.1%, MAF: 272; 18.3% and M. bovis: 10; 0.7%) were tested and of these, 111 (7.5%), 10 (0.7%), 40 (2.6%) and 161 (10.8%) were INH mono-resistant (INHr), RIF mono-resistant (RIFr), multi-drug resistant (MDR) and resistant to at least one drug (ANYr) respectively. Comparing these results to a previous report from Ghana [27], indicates that the level of drug resistance has remained fairly low over the past 8 years (OR = 1.11, 95% CI = 0.79–1.52, p = 0.5186). There was no statistical association of specific DR-TB with the two regions understudied (Table 2). We found 90/1208 (7.5%), 19/272 (7.0%) and 2/10 (20%) of the MTBSS, MAF and M. bovis respectively were INHr. None of the MAF isolates were RIFr, however, there were 9 (0.7%) MTBSS and 1 (10.0%) M. bovis resistant to only RIF. On the other hand, the MDR strains were 10 (3.7%) MAF and 30 (2.5%) MTBSS. There was no difference between the DR rates of MAF and MTBSS (Table 3). When the strains were further stratified into spoligotypes, the DR rates as summarized in Table 4 indicate a high proportion of DR among the Ghana spoligotype of Lineage 4. For example, there were 7.4% of Cameroon spoligotype as compared to 23.6% of the Ghana spoligotype with resistance to at least one drug (OR = 0.26; CI 0.17–0.41; p = 0.0000).
Table 2.
Distribution of drug resistance among 1490 MTBC isolates from two distant regions of Ghana.
| Resistance | Total (1490) | Accra Metro (1350) | Mamprusi East (140) | p-value |
|---|---|---|---|---|
| INHr | 111; 7.45% | 99; 7.33% | 12; 8.60% | 0.6108 |
| RIFr | 10; 0.67% | 8; 0.59% | 2; 1.40% | 0.2404 |
| MDR | 40; 2.64% | 33; 2.44% | 7; 5.00% | 0.0924 |
| ANY | 161; 10.80% | 140; 10.37% | 21; 15.00% | 0.0850 |
Table 3.
Distribution of drug resistance by the human adapted MTBC.
| Drug | Total (1480) | MTBSS (1208) | MAF (272) | p-value | 95% CI |
|---|---|---|---|---|---|
| INHr | 109; 7.4% | 90; 7.5% | 19; 6.9% | 0.8979 | 0.63–1.89 |
| RIFr | 9; 0.6% | 9; 0.7% | 0; 0.0% | 0.3794 | 0.44–Inf |
| MDR | 40; 2.7% | 30; 2.5% | 10; 3.7% | 0.2988 | 0.31–1.55 |
| ANYr | 158; 10.7% | 129; 10.7% | 29; 10.7% | 0.9999 | 0.65–1.59 |
Table 4.
Comparing the proportion of drug resistant Ghana spoligotype of MTBSS to other prominent spoligotypes in the Ghana.
| Resistance | Cameroon (806) | Ghana (195) | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| INH | 54 (6.7%) | 43 (22.1%)∗ | 0.25 | 0.16–0.40 | 0.0000 |
| RIF | 19 (2.4%) | 12 (6.2%)∗ | 0.37 | 0.17–0.85 | 0.0103 |
| MDR | 13 (1.6%) | 9 (4.6%)∗ | 0.34 | 0.13–0.91 | 0.0240 |
| ANY | 60 (7.4%) | 46 (23.6%)∗ | 0.26 | 0.17–0.41 | 0.0000 |
| MAF WA 1 (165) | Ghana (195) | ||||
| INH | 25 (15.2%) | 43 (22.1%) | 0.63 | 0.35–1.12 | 0.1059 |
| RIF | 10 (6.1%) | 12 (6.2%) | 0.98 | 0.37–2.56 | 0.9998 |
| MDR | 10 (6.1%) | 9 (4.6%) | 1.33 | 0.47–3.81 | 0.6384 |
| ANY | 25 (15.2%) | 46 (23.6%)∗ | 0.58 | 0.32–1.02 | 0.0472 |
| MAF WA 2 (107) | Ghana (195) | ||||
| INH | 6 (5.6%) | 43 (22.1%)∗ | 0.21 | 0.07–0.52 | 0.0001 |
| RIF | 1 (0.9%) | 12 (6.2%)∗ | 0.144 | 0.00–1.00 | 0.0372 |
| MDR | 1 (0.9%) | 9 (4.6%) | 0.19 | 0.00–1.45 | 0.1040 |
| ANY | 6 (5.6%) | 46 (23.6%)∗ | 0.19 | 0.06–0.48 | 0.0000 |
MAF WA 1: M. africanum West Africa 1 (Lineage 5).
MAF WA 2: M. africanum West Africa 2 (Lineage 6).
Significantly higher.
3.3. Drug resistance conferring mutations
Mutations were found in all targets analysed but rpoA of RIF resistant isolates (Table 5) with the katG S315T (70.9%) and rpoB S450L (52.0%) as the dominant INH and RIF resistance-associated mutations respectively followed by inhApro -15C/T (15.9%) and rpoB D435V (22.0%). As shown (Table 6), 91 (75.8%) of INH resistant MTBSS compared to 15 (51.7%) MAF harboured katG mutations (OR: 3.73, 95% CI: 1.56–9.09, p = 0.0013). In contrast, within the inhApro, 32 (26.7%) MTBSS as compared to 14 (48.3%) INH resistant MAF harboured mutations (OR: 0.39, 95% CI: 0.16–0.98, p = 0.0419). Analysis of other targets associated with INH resistance, found the proportion of INH resistant MAF with ndh (5; 17.2%) mutations to be higher than MTBSS (1; 0.8%) (OR: 0.04, 95% CI: 0.00–0.39, p = 0.0011). Mutations within the inhA locus, and ahpCpro regions were, 17 (14.2%) and 2 (1.7%) in MTBSS as compared to 1 (3.5%) and 1 (3.5%) MAF (p = 0.1999 and p = 0.4802 respectively), All the 16 isolates with the novel inhA mutation (G204D) were MTBSS Lineage 4 spoligotypes (11 Ghana, 3 Cameroon, 1 Uganda I and 1 LAM). MTBSS strains with rpoB mutations were 38 (97.4%) as compared to 8 (80.0%) MAF (p = 0.1018) as shown in Table 6. The only RIF resistant bovine strain had two rpoB mutations Q432P and I491S (Table 5; S1).
Table 5.
Identified mutations from drug resistant MTBC.
| Gene (No. of isolates) | DNA mutation | Isolates with specific SNP | Amino acid change | Other mutations |
|---|---|---|---|---|
| inhApro (151) | -8T/C | 5 (3.3%) | – | 5: katG S315T, 2: ndh V117I |
| −15C/T | 24 (15.9%) | 8: inhApro -102G/A | ||
| −17G/C | 1 (0.7%) | – | ||
| −102G/A | 16 (10.6%) | – | 8: katG S315T, 8: inhApro -15C/T | |
| −47G/C | 1 (0.7%) | katG S315T | ||
| katG (151) | G944C | 107 (70.9%) | S315T | 16: inhA G204D, 8: inhApro -102G/A: 5: inhApro -8T/C, 1: inhApro -47G/C, 2: ndh V117I, 2: ahpCpro -88G/A, 1: ahpCpro -142 G/A |
| inhA (151) | G611A∗ | 16 (10.6%) | G204D∗ | 16: katG S315T |
| T233C | 1 (0.7%) | V78A | ndh: K32R; aphCpro: -54C/T | |
| ahpCpro (151) | −54C/T | 1 (0.7%) | – | ndh: K32R; inhA: V78A |
| −88G/A∗ | 2 (1.3%) | – | 2: katG; S315T | |
| −142G/A∗ | 1 (0.7%) | – | katG: S315T | |
| ndh (151) | G349A | 4 (2.6%) | V117I∗ | inhApro; -8T/C katG; S315T |
| C411T | 1 (0.7%) | G137G | katG; S315T | |
| A95G & G349A | 1 (0.7%) | K32R∗ & V117I∗ | ahpCpro: -54C/T, inhA: V78A | |
| rpoB (50) | A1295C | 1 (2.0%) | Q432P | |
| A1295C & T1472G | 1 (2.0%) | Q432P & I491S† | ||
| C1294A | 1 (2.0%) | Q432K | ||
| A1304T | 11 (22.0%) | D435V | ||
| G1303T | 1 (2.0%) | D435Y | ||
| C1332T | 1 (2.0%) | S441L | ||
| A1334G | 2 (4.0%) | H445R | ||
| CA1333/4TG | 2 (4.0%) | H445C | ||
| C1333G | 2 (4.0%) | H445D | ||
| C1333T | 1 (2.0%) | H445Y | ||
| C1349T | 26 (52.0%) | S450L | 2: rpoC G332R, 3: rpoC V483G | |
| rpoC (50) | G994C | 2 (4.0%) | G332R | rpoB; S450L |
| T1448G | 3 (6.0%) | V483G | rpoB; S450L |
The 50 RIF resistant strains include the 49 RIF mono-resistant and/or MDR MTBSS and MAF strains in addition to the single RIF mono-resistant Mbovis. Similarly, the 151 INH Resistant strains include the 109 INH mono-resistant and 40 MDR MTBSS and MAF in 2 INH mono-resistant M.bovis.
Novel Mutation.
Previously described in RIF resistant E. coli.
Table 6.
Distribution of mutations by human adapted MTBC species.
| Target | MTBSS | MAF | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| katG | 91; 75.8%∗ | 15; 51.7% | 3.73 | 1.56–9.09 | 0.0013 |
| inhApro | 32; 26.7% | 14; 48.3%∗ | 0.39 | 0.16–0.98 | 0.0419 |
| inhA | 17; 14.2% | 1; 3.5% | 4.59 | 0.66–199.77 | 0.1999 |
| ahpCpro | 2; 1.7% | 1; 3.5% | 0.48 | 0.02–28.99 | 0.4802 |
| ndh | 1; 0.8% | 5; 17.2%∗ | 0.04 | 0.00–0.39 | 0.0011 |
| rpoB | 38; 97.4% | 8; 80.0% | 8.88 | 0.42–572.05 | 0.1018 |
| rpoC | 5; 12.8% | 0; 0.0% | Inf | 0.22-Inf | 0.5834 |
Significantly higher.
Exploring the mutations in the genetic elements under study for association among the Lineage 4 spoligotypes (Table 7) found 25.6% of the Ghana spoligotype to harbour inhA mutations as compared to 7.4% of the Cameroon spoligotype (OR = 4.23, 95% CI = 1.13–19.82, p = 0.0220). In addition, all the 3 strains with the novel ndh mutation (V117I) belonged to MAF West Africa 2. The 2 strains with rpoC G332R were Cameroon spoligotypes whereas the 3 strains with rpoC V483G were Ghana spoligotype but were all carrying rpoB S450L.
Table 7.
Comparing mutation sites among Lineage 4 Spoligotypes.
| Cameroon (54) | Ghana (43) | OR | 95% CI | p-value | |
|---|---|---|---|---|---|
| katG | 39; 72.2% | 32; 74.4% | 0.89 | 0.32–2.42 | 0.9998 |
| inhApro | 14; 25.9% | 9; 20.9% | 1.32 | 0.46–3.92 | 0.6357 |
| inhA | 4; 7.4% | 11; 25.6%∗ | 0.24 | 0.05–0.88 | 0.0220 |
Significantly higher.
4. Discussion
The objectives of this study were 1) to determine the drug (INH and RIF) susceptibility profile of MTBC strains, 2) to probe the genomes of DR isolates for mutations and 3) to compare the identified mutations between species. The main findings from this prospective study show that 1) the rate of INHr, RIFr and MDR TB has remained fairly constant over the years with relatively high proportion of INHr as compared to RIFr, 2) the Ghana spoligotype of Lineage 4 is associated with drug resistance 3) that INH resistant MTBSS are more likely to harbour katG mutations as compared to INH resistant MAF which preferred inhApro mutations, and 4) that RIF resistant Cameroon and Ghana spoligotypes of Lineage 4 may harbour different compensatory rpoC mutations even though they share the same drug resistant rpoB mutation.
The proportion of INHr, RIFr and MDR among the close to 1500 isolates analysed were 7.5%, 0.7% and 2.6% respectively which was found not to be significantly different from two previous reports [23], [27]. This indicates that the rate of MDR and RIF mono resistant TB in the country has remained fairly constant and low over the years indicating some success for the National control programme. However, the 111 (7.5%) INH mono-resistance as compared to 10 (0.7%) RIF mono-resistance suggests that emergence of INH resistance predates RIF resistance towards generation of MDR-TB. This finding has important implications if GeneXpert is used as a surrogate for detection of MDR-TB as most INH-mono-resistant cases would be treated as susceptible with first-line regimen that contains INH and could render the first-line regimen ineffective.
Stratifying the isolates by geographical region shows that the northern part of the country has higher proportion of MDR-TB compared to the south and the national average of approximately 2% according to the national tuberculosis control program (personal communication with the director). This result calls for intensifying control activities in Northern Ghana and probably other rural communities as most of the Global fund activities are centred in the urban areas especially the Accra Metro Health Directorate. However, consistent with an earlier study [23], there was no difference between the proportion of MTBSS and MAF that were drug resistant (Table 2). This result however, seems to contradict a study in Ghana that found MTBSS to be more associated with drug resistance as compared to MAF [28]. However, resistance to streptomycin (which was not included in the current study) drove the association found in that study. The Ghana spoligotype of MTBSS Lineage 4, which is the second most dominant Lineage 4 spoligotype in Ghana [23], [28], was found to be associated with drug resistance whether compared to the most dominant Cameroon spoligotype or the two lineages of MAF (Table 3). This is the first report that associates the Ghana spoligotype with drug resistance in any of the West African countries where this genotype is prevalent. This association is similar to the association of the Beijing genotype of Lineage 2 in some geographical settings [28], [29], [30], [31], [32]. However, whereas the Beijing genotype is defined by other genotyping tools in addition to spoligotyping, the Ghana spoligotype is merely defined by spoligotyping, which calls for further genomics studies for proper classification. Drug resistance mutations in most bacteria, including MTBC is often associated with a fitness cost, and therefore the ability of a strain to develop and transmit effectively is influenced by the genetic background that mitigate against the cost. For instance, the Beijing genotype has been associated with increased virulence and compensatory mutations [32], [33], [34], [35], [36]. Drawing from the Beijing experience, it may be appropriate to infer that the Ghana spoligotype has developed the capacity to develop drug resistance through some as-yet-unidentified evolutionary compensatory mechanism. As high rate of drug resistance is somehow linked with virulence [32], [33], [34], [35], detailed comparative genomics and phenotypic investigations involving the Ghana spoligotype would highlight the probable evolutionary forces driving this association with drug resistance. This finding partly explains, the higher level of DR-TB observed in the Northern region of Ghana probably confounded by the dominance of the Ghana spoligotype which is found in higher proportions in that part of the country as compared to the South [Yeboah-Manu et al., manuscript submitted]. This observation could also be due to a local transmission of resistant Ghana spoligotype strains instead of emergence of resistance among patients under therapy similar to an earlier report by Eldholm et al. [37]. This however, would require whole genome sequencing of the drug resistant strains for clarity.
The finding that INH resistant MTBSS clinical strains have higher preference for katG mutations as compared to INH resistant MAF strains which preferred inhApro mutations compares with an earlier report of a similar study carried out in Ghana [27], and suggests possible preference for lineage-specific drug-resistance mutations. However, whereas that study hypothesized that inhApro mutation -102G/A which has not been associated with drug resistance was likely to be MAF species-specific SNP, the mutation was later detected in some INH resistant MTBSS strains harbouring either katG S315T or inhApro -15C/T and hence challenged the MAF species-specificity of this SNP [23]. In this current study, the mutation was again found in both species (S1), thus confirming the earlier hypothesis that the mutation could not be species-specific. We however hypothesize that the -102G/A, together with -47G/C and -8T/C SNPs which were also detected in the previous studies are more likely to be compensatory mutations instead of specific phylogenetic markers. This hypothesis is supported by the fact that the 3 SNPs mentioned above were found concurrently with either katG S315T or inhApro -15C/T in INH resistant strains or alone in INH susceptible strains and were not species-specific (S1). Nevertheless, this hypothesis requires further work for confirmation or otherwise. However, if this hypothesis is proven to be true, it would have negative impact on the WHO approved MTBDRplus line probe assay which has the inhApro -8T/C SNP as one of the markers for INH resistance. We also report of a less prevalent inhApro mutation -17G/C which was earlier reported in some Ghanaian isolates [27], however unlike the earlier report, this study found the affected isolate had no other mutation in all the other targets analysed suggesting that it could be responsible for the observed resistance.
In addition, there was a novel inhA mutation (G204D) which may be a compensatory mutation for the acquisition of katG S315T mutations in MTBSS whereas another novel mutation in ndh (K32R) could be a drug resistance mutation (Table 4). These conclusions were drawn from the observation that all the 16 INH resistant isolates with the inhA G204D mutation also had the katG S315T mutation whereas the only isolate with the ndh K32R mutation had no other mutation in all the targets analysed apart from another novel mutation V117I in the same gene. The additional ndh mutation V117I may be a compensatory mutation because it was also detected in four additional INH resistant strains with katG S315T. However, whereas all the 3 isolates with the ndh V117I mutation were MAF Lineage 6, the inhA G204D was detected in 16 MTBSS Lineage 4 strains of four different spoligotypes with katG S315T hence ruling out the possibility of a phylogenetic marker (S1). Even though this novel mutation was found in four genotypes of Lineage 4, it was found to be more associated with the Ghana spoligotype as compared to the Cameroon (OR = 0.24, 95% CI = 0.05–0.88, p = 0.0220). If this mutation is verified as compensatory, the association with the Ghana spoligotype may explain the positive selection and fixation of INH resistance mutations in the Ghana spoligotype, similar to the situation with the Beijing genotype [32].
The differences in rpoC mutation between RIF resistant Cameroon and Ghana spoligotypes of Lineage 4 is in line with earlier work [37], which suggested that under similar physiological conditions, the genetic background of a particular strain may select for specific mutations. However, the physical environment of the strains may be the driving force for selection and fixation of these mutations irrespective of the genetic background [38]. Interestingly, these reports are all based on in vitro generated mutant strains suggesting that, under clinical conditions, the two proposals may apply. Even though the rpoC mutations G332R and V483G were found only in Ghana and Cameroon spoligotypes respectively, they were not spoligotype-specific (S1), thus ruling out the possibility of them being phylogenetic markers. In addition, the V483G mutation has been shown to occur at the interface between the rpoB, rpoA and rpoC of the bacterial polymerase, hence predicted with high confidence to be a compensatory mutation [11]. This current work also reaffirms the dominance of the rpoB S450L mutations among clinical RIF resistant strains and emphasizes the possible role played by compensatory mutations for the fixation of this high level RIF resistance associated mutation among clinical isolates [11].
The major limitation of this paper rests on the classification of the Ghana genotype of Lineage 4 by spoligotyping alone. However, the slow generation time and no/low recombination of M. tuberculosis complex strains suggest this observation may even hold with whole genome sequence data. In addition, the number of isolates from the north was relatively small. Furthermore, all the genomic regions analyzed were within the previously described hotspots [39] of the distinct targets analyzed and did not probe new regions. Nevertheless, the information reported here is useful for efficient management of TB in Ghana in that it provides confidence in newly diagnostic tools such as GeneXpert to support detection of RIF resistance. It also calls for more intensive control activities in the rural areas as we found more resistant cases in the rural district in northern Ghana compared to the urban Accra Metro. The findings also reaffirm the importance of understanding the genomic diversity of the MTBC in the fight against drug resistant TB.
5. Conclusion
This study reports an association between specific MTBC spoligotype and drug resistance in a geographical certain with most of the MTBC species circulating in appreciable proportions. The study provides the first evidence that implicate the Ghana spoligotype as the driver of DR-TB in Ghana and calls for further genome analyses to best characterize this spoligotype, explore for fitness and mechanisms underlying this observation. This work also reports that even though two different genotypes may have the same drug resistant mutation, they may harbour different compensatory mutations suggesting sub-lineage specific epistatic interaction between drug resistance conferring and non-drug resistant conferring mutations. The study finally confirms an earlier report that associated M. tuberculosis sensu stricto with katG and M. africanum with inhApro for high-level and low level INH resistance respectively.
Acknowledgement
We are grateful to all TB patients who consented to take part in the study, the laboratory technicians and DOTS nurses at the respective health facilities. This study was funded by the Wellcome Trust Fellowship number 097134/Z/11/Z to DYM.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.tube.2016.05.014.
Transparency declaration
None declared.
Funding
This work was funded by Wellcome Trust Fellowship number 097134/Z/11/Z awarded to Dorothy Yeboah-Manu.
Competing interests
None declared.
Ethical approval
Ethical approval was provided by the Institutional Review Board of the Noguchi Memorial Institute for Medical Research, University of Ghana with Federalwide Assurance number FWA00001824.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.WHO (World Health Organization) 2014. Global tuberculosis report. (WHO/HTM/TB/2014.08) [Google Scholar]
- 2.de Jong B.C., Antonio M., Gagneux S. Mycobacterium africanum–review of an important cause of human tuberculosis in West Africa. PLoS Negl Trop Dis. 2010;4:e744. doi: 10.1371/journal.pntd.0000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orenstein E.W., Basu S., Shah N.S., Andrews J.R., Friedland G.H., Moll A.P., Gandhi N.R., Galvani A.P. Treatment outcomes among patients with multidrug-resistant tuberculosis: systematic review and meta-analysis. Lancet Infect Dis. 2009;9:153–161. doi: 10.1016/S1473-3099(09)70041-6. [DOI] [PubMed] [Google Scholar]
- 4.Johnston J.C., Shahidi N.C., Sadatsafavi M., Fitzgerald J.M. Treatment outcomes of multidrug-resistant tuberculosis: a systematic review and meta-analysis. PLoS One. 2009;4:e6914. doi: 10.1371/journal.pone.0006914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marrakchi H., Lanéelle G., Quémard A. InhA, a target of the antituberculous drug isoniazid, is involved in a mycobacterial fatty acid elongation system. FAS-II Microbiol. 2000;146:289–296. doi: 10.1099/00221287-146-2-289. [DOI] [PubMed] [Google Scholar]
- 6.Campbell E.A., Korzheva N., Mustaev A., Murakami K., Nair S., Goldfarb A., Darst S.A. Structural mechanism for rifampicin inhibition of bacterial rna polymerase. Cell. 2001;104:901–912. doi: 10.1016/s0092-8674(01)00286-0. [DOI] [PubMed] [Google Scholar]
- 7.Hillemann D., Rüsch-Gerdes S., Richter E. Evaluation of the GenoType MTBDRplus assay for rifampin and isoniazid susceptibility testing of Mycobacterium tuberculosis strains and clinical specimens. J Clin Microbiol. 2007;45:2635–2640. doi: 10.1128/JCM.00521-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Costa E.R.D., Ribeiro M.O., Silva M.S.N., Arnold L.S., Rostirolla D.C., Cafrune P.I., Espinoza R.C., Palaci M., Telles M.A., Ritacco V., Suffys P.N., Lopes M.L., Campelo C.L., Miranda S.S., Kremer K., da Silva P.E.A., de Fonseca S.L., Ho J.L., Kritski A.L., Rossetti M.L.R. Correlations of mutations in katG, oxyR-ahpC and inhA genes and in vitro susceptibility in Mycobacterium tuberculosis clinical strains segregated by spoligotype families from tuberculosis prevalent countries in South America. BMC Microbiol. 2009;9:39. doi: 10.1186/1471-2180-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sherman D.R., Mdluli K., Hickey M.J., Arain T.M., Morris S.L., Barry C.E. Compensatory ahpC gene expression in isoniazid-resistant Mycobacterium tuberculosis. Science. 1996;272:1641–1643. doi: 10.1126/science.272.5268.1641. [DOI] [PubMed] [Google Scholar]
- 10.Koch A., Mizrahi V., Warner D.F. The impact of drug resistance on Mycobacterium tuberculosis physiology: what can we learn from rifampicin? Emerg Microbes Infect. 2014;3:e17. doi: 10.1038/emi.2014.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Comas I., Borrell S., Roetzer A., Rose G., Malla B., Kato-Maeda M., Galagan J., Niemann S., Gagneux S. Whole-genome sequencing of rifampicin-resistant Mycobacterium tuberculosis strains identifies compensatory mutations in RNA polymerase genes. Nat Genet. 2011;44:106–110. doi: 10.1038/ng.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brandis G., Hughes D. Genetic characterization of compensatory evolution in strains carrying rpoB Ser531Leu, the rifampicin resistance mutation most frequently found in clinical isolates. J Antimicrob Chemother. 2013;68:2493–2497. doi: 10.1093/jac/dkt224. [DOI] [PubMed] [Google Scholar]
- 13.Gagneux S., Long C.D., Small P.M., Van T., Schoolnik G.K., Bohannan B.J.M. The competitive cost of antibiotic resistance in Mycobacterium tuberculosis. Science. 2006;312:1944–1946. doi: 10.1126/science.1124410. [DOI] [PubMed] [Google Scholar]
- 14.Shanmugam S., Selvakumar N., Narayanan S. Drug resistance among different genotypes of Mycobacterium tuberculosis isolated from patients from Tiruvallur, South India. Infect Genet Evol. 2011;11:980–986. doi: 10.1016/j.meegid.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Albanna A.S., Reed M.B., Kotar K.V., Ashley F., Fiona A.M., Macel A.B., Dick M. Reduced transmissibility of East african indian strains of mycobacterium tuberculosis. PLoS One. 2011;6:e25075. doi: 10.1371/journal.pone.0025075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yeboah-manu D., Bodmer T., Owusu S., Ofori-adjei D., Pluschke G., Mensah-quainoo E. Evaluation of decontamination methods and growth media for primary isolation of Mycobacterium ulcerans from surgical specimens. J Clin Microbiol. 2004;42:5875–5877. doi: 10.1128/JCM.42.12.5875-5876.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Warren R.M., Gey van Pittius N.C., Barnard M., Hesseling A., Engelke E., de Kock M., Gutierrez M.C., Chege G.K., Victor T.C., Hoal E.G., van Helden P.D. Differentiation of Mycobacterium tuberculosis complex by PCR amplification of genomic regions of difference. Int J Tuberc Lung Dis. 2006;10:818–822. [PubMed] [Google Scholar]
- 18.Kamerbeek J., Schouls L., Kolk A., van Agterveld M., van Soolingen D., Kuijper S., Bunschoten A., Molhuizen H., Shaw R., Goyal M., van Embden J.D.A. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J Clin Microbiol. 1997;35:907–914. doi: 10.1128/jcm.35.4.907-914.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palomino J., Martin A., Camacho M., Guerra H., Swings J. Resazurin microtiter assay plate: simple and inexpensive method for detection of drug resistance in Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2002;46:2720–2722. doi: 10.1128/AAC.46.8.2720-2722.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Franzblau S.G., Witzig R.S., Mclaughlin J.C., Torres P., Madico G., Hernandez A., Degnan M.T., Cook M.B., Quenzer V.K., Ferguson R.M., Gilman R.H. Rapid, low-technology MIC determination with clinical Mycobacterium tuberculosis isolates by using the microplate Alamar Blue assay. J Clin Microbiol. 1998;36:362–366. doi: 10.1128/jcm.36.2.362-366.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Soolingen D.V.A.N., Hermans P.W., Haas P.E., Soll D.R., van Embden J.B. Occurrence and stability of insertion sequences in Mycobacterium tuberculosis complex strains: evaluation of an insertion sequence-dependent DNA polymorphism as a tool in the epidemiology of tuberculosis. J Clin Microbiol. 1991;29:2578–2586. doi: 10.1128/jcm.29.11.2578-2586.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Käser M., Ruf M.-T., Hauser J., Marsollier L., Pluschke G. Optimized method for preparation of DNA from pathogenic and environmental mycobacteria. Appl Environ Microbiol. 2009;75:414–418. doi: 10.1128/AEM.01358-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asante-Poku A., Otchere I.D., Danso E., Mensah D.D., Bonsu F., Gagneux S., Yeboah-Manu D. Evaluation of GenoType MTBDRplus for the rapid detection of drug-resistant tuberculosis in Ghana. Int J Tuberc Lung Dis. 2015;19:954–959. doi: 10.5588/ijtld.14.0864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lew J.M., Kapopoulou A., Jones L.M., Cole S.T. TubercuList-10 years after. Tuberc (Edinb) 2011;91(1):1–7. doi: 10.1016/j.tube.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 25.Staden R., Beal K.F., Bonfield J.K. The Staden package, 1998. Methods Mol Biol. 2000;132:115–130. doi: 10.1385/1-59259-192-2:115. [DOI] [PubMed] [Google Scholar]
- 26.Tomz M., Wittenberg J., King G. Harvard; Cambridge, MA: 2001. Clarify: software for interpreting and presenting statistical results. Version 2.1. [Google Scholar]
- 27.Homolka S., Meyer C.G., Hillemann D., Owusu-Dabo E., Adjei O., Horstmann R.D., Browne E.N., Chinbuah A., Osei I., Gyapong J., Kubica T., Ruesch-Gerdes S., Niemann S. Unequal distribution of resistance-conferring mutations among Mycobacterium tuberculosis and Mycobacterium africanum strains from Ghana. Int J Med Microbiol. 2010;300:489–495. doi: 10.1016/j.ijmm.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 28.Yeboah-manu D., Asante-poku A., Bodmer T., Stucki D., Koram K., Bonsu F., Pluschke G., Gagneux S. Genotypic diversity and drug susceptibility patterns among M. tuberculosis complex isolates from South-Western Ghana. PLoS One. 2011;6:e21906. doi: 10.1371/journal.pone.0021906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang L. Correlations between drug resistance of Beijing/W lineage clinical isolates of Mycobacterium tuberculosis and sublineages: a 2009–2013 prospective study in Xinjiang Province. China Med Sci Monit. 2015;21:1313–1318. doi: 10.12659/MSM.892951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kato-Maeda M., Kim E.Y., Flores L., Jarlsberg L.G., Osmond D., Hopewell P.C. Differences among sublineages of the East-Asian lineage of Mycobacterium tuberculosis in genotypic clustering. Int J Tuberc Lung Dis. 2010;14:538–544. [PMC free article] [PubMed] [Google Scholar]
- 31.Yuan L., Huang Y., Mi L.G., Li Y.X., Liu P.Z., Zhang J., Liang H.Y., Li F., Li H., Zhang S.Q., Li W.J. There is no correlation between sublineages and drug resistance of Mycobacterium tuberculosis Beijing/W lineage clinical isolates in Xinjiang, China. Epidemiol Infect. 2015;143:141–149. doi: 10.1017/S0950268814000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ribeiro S.C.M., Gomes L.L., Amaral E.P., Andrade M.R.M., Almeida F.M., Rezende A.L., Lanes V.R., Carvalho E.C.Q., Suffys P.N., Mokrousov I., Lasunskaia E.B. Mycobacterium tuberculosis strains of the modern sublineage of the Beijing family are more likely to display increased virulence than strains of the ancient sublineage. J Clin Microbiol. 2015;52:2615–2624. doi: 10.1128/JCM.00498-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Niemann S., Diel R., Khechinashvili G., Gegia M., Mdivani N., Tang Y.-W. Mycobacterium tuberculosis Beijing lineage favors the spread of multidrug-resistant tuberculosis in the Republic of Georgia. J Clin Microbiol. 2010;48:3544–3550. doi: 10.1128/JCM.00715-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Merker M., Blin C., Mona S., Duforet-Frebourg N., Lecher S., Willery E., Blum M.G., Rüsch-Gerdes S., Mokrousov I., Aleksic E., Allix-Béguec C., Antierens A., Augustynowicz-Kopeć E., Ballif M., Barletta F., Beck H.P., Barry C.E., Bonnet M., Borroni E., Campos-Herrero I., Cirillo D., Cox H., Crowe S., Crudu V., Diel R., Drobniewski F., Fauville-Dufaux M., Gagneux S., Ghebremichael S., Hanekom M., Hoffner S., Jiao W.W., Kalon S., Kohl T.A., Kontsevaya I., Lillebæk T., Maeda S., Nikolayevskyy V., Rasmussen M., Rastogi N., Samper S., Sanchez-Padilla E., Savic B., Shamputa I.C., Shen A., Sng L.H., Stakenas P., Toit K., Varaine F., Vukovic D., Wahl C., Warren R., Supply P., Niemann S., Wirth T. Evolutionary history and global spread of the Mycobacterium tuberculosis Beijing lineage. Nat Genet. 2015;47:242–249. doi: 10.1038/ng.3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Couvin D., Rastogi N. Tuberculosis – a global emergency: tools and methods to monitor, understand, and control the epidemic with specific example of the Beijing lineage. Tuberc (Edinb) 2015;95(Suppl. 1):S177–S189. doi: 10.1016/j.tube.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 36.Saelens J.W., Lau-Bonilla D., Moller A., Medina N., Guzman B., Calderon M., Herrera R., Sisk D.M., Xet-Mull A.M., Stout J.E., Arathoon E., Somayoa B., Tobin D.M. Whole genome sequencing identifies circulating Beijing-lineage Mycobacterium tuberculosis strains in Guatemala and an associated urban outbreak. Tuberculosis. 2015;95:810–816. doi: 10.1016/j.tube.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eldholm V., Monteserin J., Rieux A., Lopez B., Sobkowiak B., Ritacco V., Balloux F. Four decades of transmission of a multidrug-resistant Mycobacterium tuberculosis outbreak strain. Nat Commun. 2015;11(6):7119. doi: 10.1038/ncomms8119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Björkman J. Effects of environment on compensatory mutations to ameliorate costs of antibiotic resistance. Science 200; 287: 1479–1482. [DOI] [PubMed]
- 39.Da Silva P.E.A., Palomino J.C. Molecular mechanisms of drug resistance in Mycobacterium tuberculosis: classical and new drugs. J Antimicrob Chemother. 2011;66(7):1417–1430. doi: 10.1093/jac/dkr173. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.