Abstract
Background
Hypertension is the leading preventable cause of premature death worldwide. We examined global disparities of hypertension prevalence, awareness, treatment, and control in 2010 and compared secular changes from 2000 to 2010.
Methods
We searched MEDLINE from 1995 through 2014 and supplemented with manual searches of retrieved article references. We included 135 population-based studies of 968,419 adults from 90 countries. Sex-age-specific hypertension prevalences from each country were applied to population data to calculate regional and global numbers of hypertensive adults. Proportions of awareness, treatment, and control from each country were applied to hypertensive populations to obtain regional and global estimates.
Results
In 2010, 31.1% (95% confidence interval, 30.0-32.2%) of the world's adults had hypertension; 28.5% (27.3-29.7%) in high-income countries and 31.5% (30.2-32.9%) in low- and middle-income countries. An estimated 1.39 (1.34-1.44) billion people had hypertension in 2010; 349 (337-361) million in high-income and 1.04 (0.99-1.09) billion in low- and middle-income countries. From 2000 to 2010, the age-standardized prevalence of hypertension decreased by 2.6% in high-income countries but increased by 7.7% in low- and middle-income countries. During the same period, the proportions of awareness (58.2% vs 67.0%), treatment (44.5% vs 55.6%), and control (17.9% vs. 28.4%) increased substantially in high-income countries, whereas awareness (32.3% vs 37.9%) and treatment (24.9% vs 29.0%) increased less, and control (8.4% vs 7.7%) even slightly decreased in low- and middle-income countries.
Conclusions
Global hypertension disparities are large and increasing. Collaborative efforts are urgently needed to combat the emerging hypertension burden in low- and middle-income countries.
Keywords: hypertension, epidemiology, prevention
Hypertension is an important global health challenge due to its high prevalence and resulting cardiovascular disease and chronic kidney disease.1-3 Hypertension is the leading preventable risk factor for premature death and disability worldwide.3 Prior work estimated that 26.4% of the global adult population, or 972 million people, had hypertension in 2000.1 Since 2000, national reports have indicated that the prevalence of hypertension is increasing in low- and middle-income countries, while it is steady or decreasing in high-income countries.4-10 These data suggest a widening health disparity in hypertension prevalence worldwide. Current estimates of the global burden of hypertension in high-income and low- and middle-income countries are needed to better understand this important public health concern.
Treatment and control of hypertension are critically important for the prevention of consequent cardiovascular and kidney diseases.11 The proportions of hypertension awareness, treatment, and control that have been reported across many countries vary substantially.6,11-16 However, these data have not been systematically analyzed to provide pooled estimates in world regions with diverse economic development.
The goal of this study is to examine the global disparities of hypertension prevalence, awareness, treatment, and control by world regions with different levels of economic development in 2010, and to compare secular changes in the disparities of hypertension prevalence, awareness, treatment, and control from 2000 to 2010 worldwide. Understanding health disparities in hypertension prevalence and control among world regions is important for developing global strategies to better prevent and control hypertension through collaborative national and international efforts.
Methods
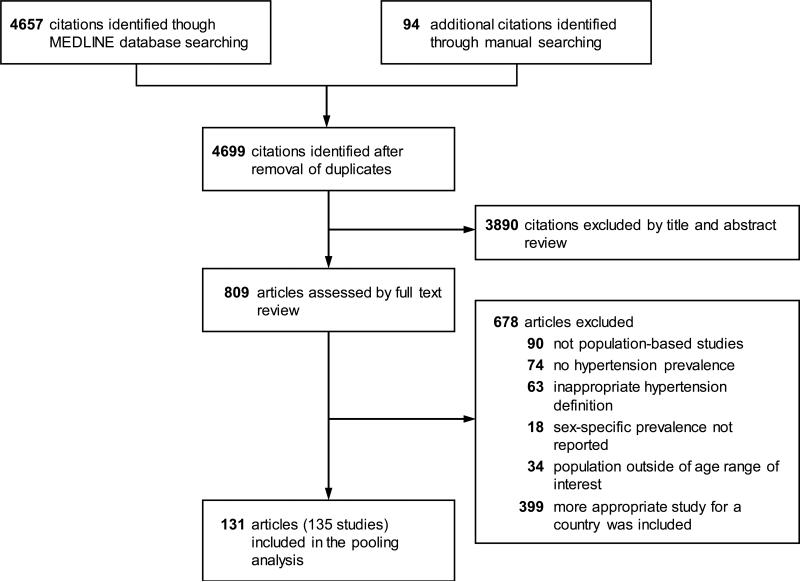
Complete methods are available in the online data supplement. In brief, MEDLINE was searched for studies published from January 1, 1995 to December 31, 2014, and additional studies were identified by manual review of references cited in reviews, meta-analyses, and original studies. Country-specific searches of the World Health Organization Global Infobase were also conducted.17 Eligibility criteria for inclusion were: (1) population-based cross-sectional study in adults aged ≥20 years which reported sex-specific prevalence of hypertension; (2) blood pressure measurement methods were standardized; and (3) hypertension was defined as average systolic blood pressure ≥140 mm Hg, average diastolic blood pressure ≥90 mm Hg, or use of antihypertensive medication. If nationally representative studies were available, they were used; otherwise, data from the largest and most recent multisite or regional study were used. If multiple regional or multisite studies were available for a given country, they were pooled using gender-specific random-effects meta-regression models to obtain age- and gender-specific prevalence and variance estimates for each country. Studies were included in the 2010 hypertension analysis if data collection took place from 2005 to 2014. Studies with data collection from 1995 to 2004 were used in the 2000 hypertension analysis. A total of 131 reports (135 studies) from 90 countries were included in the analyses (Figure 1). Literature searches, study selection, and data abstraction were conducted independently and in duplicate by three investigators (KTM, JDB, JER), with a standardized protocol and data-collection form. The prevalence of prehypertension, defined as blood pressure between 120/80 mm Hg and 140/90 mm Hg, was also abstracted but was reported by so few publications that it was not included in the analyses. Any discrepancies were resolved by consensus. Study authors were contacted to request additional information when necessary.
Figure 1.
Flowchart of study selection
Proportions of hypertension awareness, treatment, and control were abstracted from all reports included in the 2000 and 2010 prevalence analyses. Hypertension awareness and treatment are defined as self-reported previous diagnosis of hypertension and self-reported use of antihypertensive medications among those with hypertension, respectively. Hypertension control is defined as systolic blood pressure <140 mm Hg and diastolic blood pressure <90 mm Hg among hypertensive patients or among treated hypertensive patients. Data from 61 countries were used to estimate regional and global proportions of hypertension awareness, treatment, and control.
Countries were grouped into regions using the World Bank classification system updated in July 2014, which groups the high-income countries into one region and the low- and middle- income countries into six geographic regions.18 The included regions were: High-income Economies, East Asia and Pacific, Europe and Central Asia, Latin America and the Caribbean, Middle East and North Africa, South Asia, and Sub-Saharan Africa. For countries without valid estimates for 2010 or 2000 prevalence, awareness, treatment, or control, three countries that are the most similar in terms of gross national income and geographic proximity to each country with missing data were selected, and multiple imputation was performed to estimate the gender- and age-specific prevalence and variance of each country without data (multiple imputation details in Supplemental Methods).19
For studies that did not report prevalence data in the 10-year age groups of interest (i.e., 20-29, 30-39, etc), age-specific prevalence was imputed using logistic regression models for each sex in each region, separately. The predictive models of the relationship between age group and prevalence of hypertension were generated from studies with age-specific data within each region-sex subgroup. In addition, mean age and prevalence for men and women from each study with missing age-specific prevalence were used to calibrate the estimates of age-specific prevalence for that country. The pseudo R-squares (ranging from 0.46 to 0.92, all P<0.001) indicated good fit of all logistic regression models.
Statistical analysis
In order to estimate the 2010 hypertension prevalence and absolute burden, defined as the number of adults with hypertension, by world region, sex- and age-specific prevalences of hypertension for each country were applied to the 2010 United Nations sex- and age-specific population counts to estimate the number of people with hypertension in the country for each sex- and age-group.20 The total number of persons with hypertension in each country was summed to provide an estimate of the total number of persons with hypertension for each region by sex- and age-groups, and the number from each region was added to obtain the worldwide count. The sex- and age-specific regional prevalences of hypertension for 2010 were calculated by dividing the total number of people with hypertension in each region by the number of people living in that region for each sex and age group. Worldwide prevalence was estimated by dividing the total number of persons with hypertension by the total adult world population. The prevalences of hypertension within each world region and worldwide were age-standardized to the 2010 world population using the direct method.21 A sensitivity analysis was conducted including only countries with reports of prevalence from both 2000 and 2010.
Standard errors for the prevalence of hypertension were abstracted from those studies that report them. For the remaining studies, standard errors were estimated as the square root of ([hypertension prevalence × (1-hypertension prevalence)]/study sample size), which may slightly overestimate the standard error for surveys utilizing complex sampling designs. The standard errors for the number of persons with hypertension within a region and worldwide were then estimated with Taylor series approximation methods and used to calculate 95% confidence intervals.22 Differences between prevalence and absolute burden estimates for 2000 and 2010 were tested using a two-tailed z-test for the difference in proportions.
Regional and global prevalence of hypertension in 2000 and proportions of hypertension awareness, treatment, and control were estimated using similar methods (details in Supplemental Methods).
Results
Of the 4,751 articles identified by database and manual searching, 809 underwent full text review and 131 articles (135 studies) were included in the pooling analyses. This included a total of 78 studies with a combined sample size of 540,890 participants included in the 2010 hypertension prevalence analysis (Supplemental Table 1). These population-based studies (46 in nationally representative samples) collected hypertension prevalence data from 70 countries representing 79.1% of the global population ≥20 years old. The additional 57 studies from 45 countries representing 67.8% of the global population ≥20 years old with a combined sample size of 427,529 were included in the 2000 hypertension prevalence analysis (Supplemental Table 2). The proportions of hypertension awareness, treatment, and control were reported for 53 countries in the 2010 analysis and 20 countries in the 2000 analysis (Supplemental Tables 3 and 4). Gender-specific population estimates and crude prevalence estimates from each country are shown in Supplemental Tables 5 and 6.
Disparities in Hypertension Prevalence and Absolute Burden in 2010
The estimated global age-standardized prevalence of hypertension in adults aged ≥20 years in 2010 was 31.1% (95% confidence interval, 30.0-32.2%): 31.9% (30.3-33.5%) in men and 30.1% (28.5-31.6%) in women. The age-standardized prevalence of hypertension was 28.5% (27.3-29.7%) in high-income countries (31.6% [29.6-33.6%] in men and 25.3% [23.9-26.7%] in women) and 31.5% (30.2-32.9%) in low- and middle-income countries (31.7% [29.7-33.6%] in men and 31.2% [29.3-33.1%] in women) (Table 1). The p-value for the difference in prevalence between high-income and low-and middle-income countries is 0.001. Prevalence estimates in 2010 by world region are presented in Supplemental Table 7.
Table 1.
Age-specific and age-standardized prevalence estimates and absolute numbers of men and women with hypertension in high-income and low- and middle-income countries in 2010
| Age, years | Prevalence % (95% CIs) | Absolute Numbers in Millions (95% CIs) | ||||||
|---|---|---|---|---|---|---|---|---|
| High-income countries | Low- and middle-income countries | High-income countries | Low- and middle-income countries | |||||
| Men | Women | Men | Women | Men | Women | Men | Women | |
| 20-29 | 10.7 (5.9, 15.5) | 4.3 (1.9, 6.6) | 15.2 (11.5, 18.9) | 10.4 (7.0, 13.7) | 10.0 (5.5, 14.4) | 3.7 (1.7, 5.8) | 77.1 (58.3, 96.0) | 50.6 (34.3, 66.9) |
| 30-39 | 18.5 (14.1, 22.9) | 9.1 (6.3, 12.0) | 22.1 (17.7, 26.5) | 17.4 (13.3, 21.6) | 17.4 (13.3, 21.5) | 8.2 (5.6, 10.8) | 90.2 (72.2, 108.3) | 69.6 (53.0, 86.2) |
| 40-49 | 31.0 (26.8, 35.3) | 22.0 (18.5, 25.5) | 31.2 (26.4, 36.0) | 30.6 (25.7, 35.6) | 29.0 (25.0, 33.0) | 20.5 (17.2, 23.8) | 108.0 (91.4, 124.6) | 103.9 (87.3, 120.6) |
| 50-59 | 48.5 (43.6, 53.4) | 41.0 (36.3, 45.7) | 43.0 (37.9, 48.1) | 47.2 (41.8, 52.6) | 40.4 (36.3, 44.5) | 35.9 (31.8, 40.1) | 106.1 (93.5, 118.7) | 115.7 (102.5, 128.9) |
| 60-69 | 60.8 (56.8, 64.8) | 60.9 (56.7, 65.0) | 55.3 (50.1, 60.6) | 61.9 (56.2, 67.7) | 36.4 (34.0, 38.8) | 40.8 (38.0, 43.5) | 76.4 (69.1, 83.6) | 90.6 (82.2, 99.0) |
| ≥70 | 73.6 (70.0, 77.3) | 77.5 (73.9, 81.0) | 65.6 (60.6, 70.7) | 74.7 (69.6, 79.7) | 41.1 (39.0, 43.1) | 65.5 (62.5, 68.4) | 62.4 (57.5, 67.2) | 88.5 (82.5, 94.5) |
| Overall | 31.6 (29.6, 33.6) | 25.3 (23.9, 26.7) | 31.7 (29.7, 33.6) | 31.2 (29.3, 33.1) | 174.2 (165.3, 183.2) | 174.7 (167.2, 182.1) | 520.1 (485.6, 554.7) | 518.8 (485.7, 552.0) |
Values are percentages and 95% confidence intervals
An estimated 1.39 billion (1.34-1.44 billion) adults aged ≥20 years worldwide had hypertension, 694 million (659-730 million) men and 694 million (660-727 million) women, in 2010. Almost three times as many individuals with hypertension lived in low- and middle-income countries (1.04 billion [0.99-1.09 billion]) than in high-income countries (349 million [337-361 million]). In high-income countries, the greatest absolute burden was in old age groups (e.g., 60 years and older), while in low- and middle-income countries the greatest absolute burden was in the middle aged groups (e.g., 40 to 59 years) (Table 1).
Disparities in the Hypertension Prevalence Changes from 2000 to 2010
The global age-standardized prevalence of hypertension was 25.9% (24.6-27.1%) in adults aged ≥20 years in 2000 (Supplemental Table 8). From 2000 to 2010, there was an increase in hypertension prevalence of 5.2% over ten years. This increase was consistent in men and women, who had an age-standardized hypertension prevalence of 26.4% (24.6-28.2%) and 25.1% (23.4-26.9%) in 2000, respectively. The hypertension prevalence decreased 2.6% in high-income countries from 31.1% (27.7-34.5%) in 2000, whereas the prevalence increased 7.7% in low- and middle-income countries from 23.8% (22.6-25.1%) in 2000. The absolute burden of hypertension in 2000 was 921 million (874-968 million) with 322 million (292-353 million) in high-income countries and 599 million (563-634 million) in low- and middle-income countries. Globally, the number of individuals with hypertension increased by 466.8 million since 2000, with a 26.6 million increase in high-income countries and a 440.1 million increase in low- and middle-income countries (Supplemental Table 8).
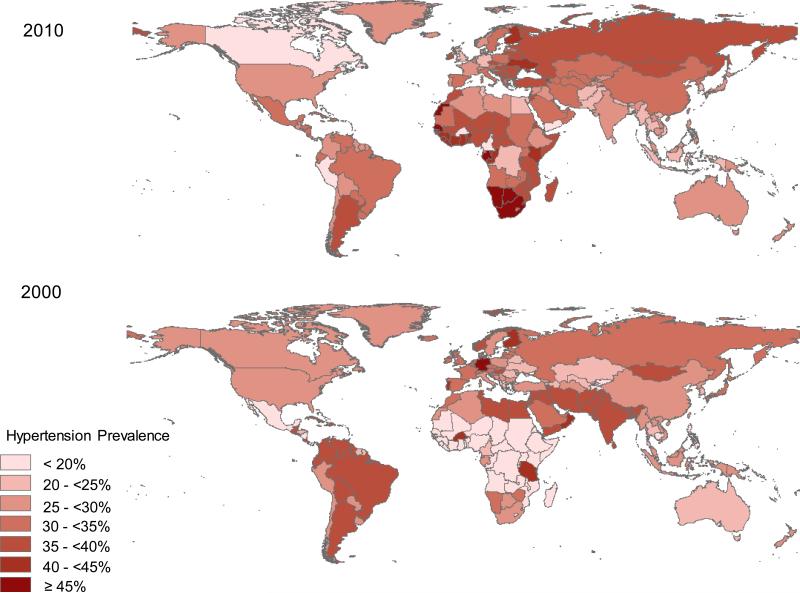
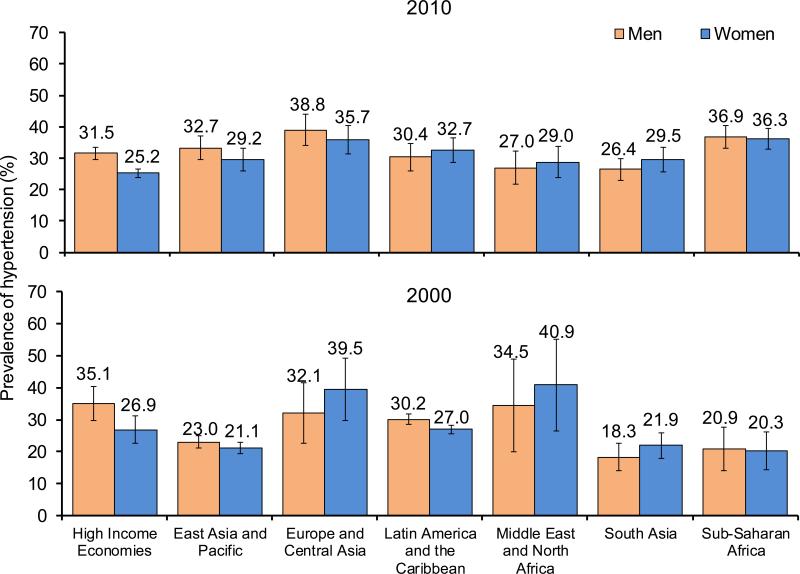
Figure 2 shows the age- and sex-standardized prevalence of hypertension by country in 2010 and 2000 (crude prevalence shown in Supplemental Figure 1 and map with imputed countries left blank shown in Supplemental Figure 2). In 2010, the highest prevalence for men was in Europe and Central Asia and that for women was in Sub-Saharan Africa, while the lowest prevalence for men was in South Asia and that for women was in High Income Economies (Figure 3). The prevalence of hypertension increased in East Asia and Pacific, Latin America and the Caribbean, South Asia, and Sub-Saharan Africa for both men and women, and in Europe and Central Asia for men, whereas it decreased in High Income Economies and the Middle East and North Africa for both men and women and in Europe and Central Asia for women.
Figure 2. Worldwide age- and sex-standardized prevalence of hypertension in adults 20 years and older by country.
Upper panel shows country-specific prevalence in 2010 and lower panel shows country-specific prevalence in 2000. Maps are shaded according to prevalence, from light (lower prevalence) to dark (higher prevalence).
Figure 3. Age-standardized prevalence of hypertension in adults 20 years and older by world region and sex.
Upper panel shows sex-specific prevalence by world region in 2010 and lower panel shows sex-specific prevalence by world region in 2000. Comparisons between 2010 and 2000 prevalences were statistically significant (p<0.05) for men women in East Asia and Pacific, South Asia, and Sub-Saharan Africa and for women in Latin America and the Caribbean.
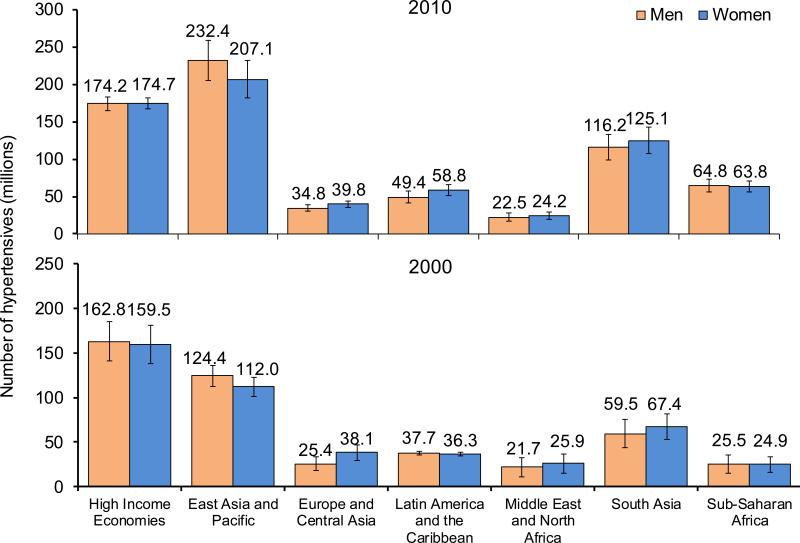
In 2010, the East Asia and Pacific region had the greatest absolute burden of hypertension with 439 million people with hypertension, and the Middle East and North Africa region had the lowest absolute burden of hypertension (Figure 4). The absolute burden of hypertension increased in every world region for both men and women between 2000 and 2010, except for women in the Middle East and North Africa, where there was a decrease in absolute burden. The greatest increases in the absolute burden of hypertension occurred in East Asia and Pacific, where there are an additional 108.0 million men and 95.1 million women with hypertension compared to 2000.
Figure 4. Absolute burden of hypertension in adults 20 years and older by world region and sex.
Upper panel shows number of hypertensive individuals in millions by world region and sex in 2010 and lower panel shows number of hypertensive individuals in millions by world region and sex in 2000. Comparisons between 2010 and 2000 absolute numbers were statistically significant (p<0.05) for men and women in East Asia and Pacific, Latin America and the Caribbean, South Asia, and Sub-Saharan Africa and for men in Europe and Central Asia.
In a sensitivity analysis including only 26 countries (11 in high-income countries and 16 in low- and middle-income countries) with prevalence data from both 2000 and 2010, similar results to those from the primary analyses were obtained (Supplemental Table 9). For example, the global prevalence of hypertension was 30.8% (29.2-32.5%): 28.1% (24.7-31.6%) in high-income countries and 31.3% (29.5-33.1) in low- and middle-income countries in 2010. The sensitivity analysis found a 4.9% increase in global prevalence, a 5.3% decrease in high-income countries, and an 8.1% increase in low- and middle-income countries between 2000 and 2010.
Disparities in Hypertension Awareness, Treatment, and Control
In 2010, less than half (46.5%) of adults with hypertension were aware of their condition, 36.9% were treated with anti-hypertensive medication, and only 13.8% had their blood pressure controlled worldwide (Table 2). High-income countries had almost double the proportions of awareness (67.0% vs. 37.9%) and treatment (55.6% vs. 29.0%) and four-times the proportion of control among patients with hypertension (28.4% vs 7.7%) compared to low- and middle income countries in 2010. From 2000 to 2010, the proportions of awareness (58.2% vs 67.0%), treatment (44.5% vs 55.6%), and control (17.9% vs. 28.4%) increased substantially in high-income countries. During the same time period, the proportions of awareness (32.3% vs 37.9%) and treatment (24.9% vs 29.0%) increased much less and the proportion of control even slightly decreased (8.4% vs. 7.7%) in low- and middle-income countries.
Table 2.
Gender-specific hypertension awareness, treatment, and control in high-income and low- and middle-income countries in 2000 and 2010
| Awareness | Treatment | Control1 | Control2 | |||||
|---|---|---|---|---|---|---|---|---|
| 2000 | 2010 | 2000 | 2010 | 2000 | 2010 | 2000 | 2010 | |
| Global | ||||||||
| Overall | 41.4 (34.3, 48.5) | 46.5 (41.9, 51.1) | 31.8 (25.6, 37.9) | 36.9 (33.8, 40.0) | 33.9 (26.5, 41.3) | 37.1 (33.6, 40.5) | 11.7 (7.1, 16.2) | 13.8 (11.4, 16.3) |
| Men | 36.1 (25.9, 46.2) | 40.2 (34.0, 46.5) | 26.8 (18.4, 35.2) | 30.3 (26.1, 34.5) | 34.2 (24.1, 44.2) | 35.8 (30.8, 40.7) | 10.0 (4.0, 15.9) | 10.9 (7.7, 14.2) |
| Women | 46.6 (36.7, 56.5) | 52.9 (46.1, 59.6) | 36.7 (27.7, 45.7) | 43.6 (39.1, 48.1) | 33.7 (23.2, 44.2) | 38.0 (33.2, 42.8) | 13.4 (6.5, 20.2) | 16.8 (13.1, 20.5) |
| High-income Countries | ||||||||
| Overall | 58.2 (42.2, 74.3) | 67.0 (58.1, 75.9) | 44.5 (31.1, 58.0) | 55.6 (49.8, 61.4) | 38.6 (25.5, 51.6) | 50.4 (44.4, 56.4) | 17.9 (7.7, 28.0) | 28.4 (22.3, 34.5) |
| Men | 52.4 (29.0, 75.8) | 61.8 (48.0, 75.7) | 38.3 (19.7, 56.9) | 49.4 (40.8, 58.1) | 38.6 (21.1, 56.0) | 49.1 (40.7, 57.4) | 15.5 (2.3, 28.7) | 24.6 (16.0, 33.2) |
| Women | 64.1 (42.1, 86.0) | 72.2 (60.9, 83.4) | 50.9 (31.6, 70.3) | 61.7 (54.1, 69.3) | 38.6 (19.8, 57.4) | 51.5 (43.1, 59.9) | 20.3 (4.8, 35.8) | 32.2 (23.6, 40.8) |
| Low- and Middle-income Countries | ||||||||
| Overall | 32.3 (25.7, 38.9) | 37.9 (32.5, 43.2) | 24.9 (18.7, 31.0) | 29.0 (25.4, 32.7) | 29.4 (22.1, 36.7) | 26.3 (22.3, 30.3) | 8.4 (4.0, 12.7) | 7.7 (5.3, 10.1) |
| Men | 27.0 (18.0, 36.0) | 31.2 (24.5, 38.0) | 20.4 (12.4, 28.4) | 22.3 (17.6, 27.0) | 29.5 (19.9, 39.2) | 23.4 (17.9, 28.9) | 6.9 (1.3, 12.6) | 5.2 (2.3, 8.1) |
| Women | 37.4 (27.8, 47.1) | 44.7 (36.3, 53.0) | 29.2 (20.0, 38.4) | 35.9 (30.3, 41.5) | 29.2 (18.9, 39.6) | 28.1 (22.6, 33.7) | 9.7 (3.2, 16.3) | 10.2 (6.4, 14.0) |
Values are percentages and 95% confidence intervals
Awareness is defined as self-reported previous diagnosis of hypertension among those with hypertension; Treatment is defined as self-reported anti-hypertensive medication use among those with hypertension; Control is defined as systolic blood pressure <140 mm Hg and diastolic blood pressure <90 mm Hg (1) among those self-reporting treatment and (2) among all participants with hypertension
Discussion
Our study is the first systematic analysis of global health disparities in hypertension prevalence, awareness, treatment, and control. It provides novel insights into several aspects of the global challenge of hypertension. First, our study showed that the age-standardized prevalence of hypertension was higher in low- and middle-income countries (31.5%) than in high-income countries (28.5%) worldwide (p-value for the difference=0.001). Additionally, approximately three-quarters of individuals with hypertension lived in low- and middle-income countries. Second, our study showed that the prevalence of hypertension decreased by 2.6% in high-income countries but increased by 7.7% in low- and middle-income countries from 2000 to 2010. The absolute burden of hypertension increased by 440.1 million in low- and middle-income countries compared to only 26.6 million in high-income countries over a decade. The rapid increase in the absolute burden of hypertension in low- and middle-income countries is most likely due to both increasing prevalence and substantial population growth. Third, our study indicated that the proportions of awareness, treatment, and control of hypertension were much lower in low- and middle-income countries than in high-income countries. Over the past decade, hypertension awareness, treatment, and control increased substantially in high-income countries, whereas there was less improvement in low- and middle-income countries. These data document large and widening global disparities in hypertension prevalence and control.
The high and increasing worldwide burden of hypertension is a major global health challenge because it increases morbidity and mortality from cardiovascular and kidney diseases and financial costs to society.3 Our study indicated that 31.1% of the global population, or 1.4 billion people, had hypertension in 2010. It has been estimated that substantial stroke and ischemic heart disease morbidity and mortality worldwide are attributable to hypertension.2,3 Ischemic heart disease and stroke are the leading causes of death worldwide, accounting for 14.6 million, or one in four, deaths globally in 2013.23 Without effective intervention, the increasing burden of hypertension will only exacerbate the global epidemic of cardiovascular and kidney diseases, especially in low- and middle-income countries.
While hypertension prevalence has decreased in high-income countries, it has increased in low- and middle-income countries. As a result, the prevalence of hypertension in low- and middle-income countries has surpassed that in high-income countries for the first time. The estimated 73.5% relative increase in the absolute number of hypertensive individuals from 599 million in 2000 to 1.0 billion in 2010 in low- and middle-income countries is worrisome because these countries are still suffering from infectious diseases and have limited healthcare resources.24 The greatest increases in absolute burden of hypertension were observed in East Asia and Pacific, South Asia, and Sub-Saharan Africa, which have experienced both increases in hypertension prevalence and in population size.6,7,24 Aging and urbanization with accompanying unhealthy lifestyle may play a role in the epidemic of hypertension in low- and middle-income countries.25 Primary prevention through lifestyle modifications, including increased physical activity, maintenance of normal body weight, limited alcohol consumption, reduction of salt intake, increased potassium intake, and consumption of a diet high in fruits, vegetables, and lowfat dairy products, and low in saturated and total fat, should be the first choice for combating the emerging epidemic of hypertension in low- and middle-income countries.26 The primary prevention approach must be complemented by intensive antihypertensive pharmaceutical treatment of hypertensive patients to reduce blood pressure-related cardiovascular disease and premature death, which is likely to be cost-effective in both high-income and middle-income countries.27-29
Danaei and colleagues estimated global trends in population mean systolic blood pressure among adults aged ≥25 years between 1980 and 2008. They reported a non-significant decrease in population mean systolic blood pressure worldwide.4 Specifically, men and women in Australasia, North America, and Western Europe had large systolic blood pressure decreases. Conversely, systolic blood pressure rose in Oceania, East Africa, and South and Southeast Asia for both sexes, and in West Africa for women. In their study, however, data on the prevalence, awareness, treatment, and control of hypertension were not collected. Our study has focused on the prevalence and control of hypertension, which have important public health and clinical relevance. The recent SPRINT trial provided evidence for the benefits of lowering systolic blood pressure to a target of 120 mm Hg instead of 140 mm Hg.30 Should future clinical guidelines recommend treating to a lower target than 140 mm Hg based on these study findings, the prevalence of uncontrolled hypertension will be even greater than reported here.
The current study identified substantial disparities in hypertension awareness, treatment, and control with high-income countries having approximately twice the proportions of awareness and treatment and four times the control rate compared to low- and middle-income countries. In addition, our results showed that the proportions of awareness, treatment, and control have improved in high-income countries between 2000 and 2010, but no substantial improvement was observed in low- and middle-income countries. These results are consistent with those from the Prospective Urban Rural Epidemiology (PURE) study that also reported higher proportions of awareness, treatment, and control in high-income countries compared to low- and middle-income countries.16 Clinical trials have demonstrated that antihypertensive treatment lowers the risk of coronary heart disease, stroke, chronic kidney disease, and all-cause mortality among patients with hypertension.31,32 Antihypertensive treatment played an important role in the reduction of cardiovascular mortality in the US and other high-income countries over the past several decades.33,34 Improving hypertension control should be a priority to achieve the UN Millennium Development Goals for non-communicable diseases in low- and middle-income countries.35,36
Our findings suggest that although the efficacy and effectiveness of lifestyle modifications and antihypertensive pharmaceutical treatment for the prevention of hypertension and concomitant cardiovascular disease have been demonstrated in randomized controlled trials, this scientific knowledge has not been fully applied in populations living in low- and middle-income countries. Many barriers at the health care system, health care provider, and patient levels are likely impeding the prevention and control of hypertension, such as lack of access to care, costly medications, overburdened healthcare providers, lack of treatment guideline adherence, low patient health literacy, and adverse side effects.37 There is an urgent need to identify innovative strategies to overcome these barriers and to deliver effective interventions for the prevention and control of hypertension in populations in low- and middle-income countries.38 Our findings call for collaborative efforts from global and local stakeholders to promote blood pressure screening, access to affordable healthcare and antihypertensive medications, and adherence to antihypertensive treatment to improve hypertension control in low- and middle-income countries.
There are several limitations inherent in this study. The quality of our analysis depends on the quality and availability of original studies which provided hypertension data. Specific quality characteristics included differences in population sampling strategies, blood pressure measurement methods, such as the inclusion of both manual and automatic blood pressure monitoring, and response rates. After limiting our analysis to population-based studies conducted in representative samples (mainly national samples), hypertension data are available from countries representing 79.1% of the world population. While the vast majority of people are represented, more than half of countries do not have data on hypertension prevalence and inaccuracies in summary estimates resulting from missing country data could exist. Awareness, treatment, and control data are only available for 20 countries in 2000, but the trends seen in our summary estimates are consistent with those of individual countries that have repeated national samples for 2000 and 2010. High income countries, such as South Korea, the United States, and the United Kingdom, have all experienced substantial increases in awareness, treatment, and control, while China's proportion of awareness has increased only slightly and proportions of treatment and control have decreased or remained the same. Finally, at least two blood pressure measurements were obtained in all studies included in this analysis. However, most of these studies measured blood pressure at only one occasion, which could overestimate the prevalence of hypertension.
In conclusion, our study indicates that global disparities in hypertension prevalence, awareness, treatment, and control are large and increasing. Collaborative efforts from national and international stakeholders are urgently needed to combat the emerging hypertension burden in low- and middle-income countries. Implementation of innovative, cost-effective, and sustainable programs for hypertension prevention and control should be a public health priority for these countries.
Supplementary Material
Clinical Perspective.
What is new?
Globally, 31.1% of the adult population (1.39 billion people) had hypertension in 2010.
Hypertension prevalence is higher in low- and middle-income countries (31.5%) than in high-income countries (28.5%).
Approximately 75% of people with hypertension (1.04 billion) live in low- and middle-income countries.
Hypertension awareness, treatment, and control are much lower in low- and middle-income compared to high-income countries.
From 2000 to 2010, the hypertension prevalence in high-income countries decreased by 2.6%, and awareness, treatment, and control improved substantially. During the same 10-year period, low- and middle-income countries saw a 7.7% prevalence increase and little improvement in awareness, treatment, and control.
What are the clinical implications?
These data document large and widening global disparities in hypertension prevalence and control.
Collaborative efforts from national and international stakeholders are urgently needed to combat the emerging hypertension burden in low- and middle-income countries.
Our findings call for global and local stakeholders to promote blood pressure screening, access to affordable healthcare and antihypertensive medications, and adherence to antihypertensive treatment to improve hypertension control in low- and middle-income countries.
Implementation of innovative, cost-effective, and sustainable programs for hypertension prevention and control should be a public health priority for these countries.
Acknowledgements
The authors would like to acknowledge Yichen Zhang, Xiaoling Ye and Caroline E. Stamatakis for their help in extracting data, Mahmoud Gaddoury for his help with translation, and Yun Zhu for assisting with data analyses. The authors would also like to acknowledge Yu Xu for providing data from China Noncommunicable Disease Surveillance 2010; Chung-Shiuan Chen for preparing data from the CESCAS I study in Argentina, Chile and Uruguay; Nabuo Nishi for identifying relevant literature for Japan; Katsuyuki Miura and the NIPPON DATA 2010 research group for providing sample sizes, prevalence data and methodological details for Japan; José R. Banegas for providing age-specific prevalence data for Spain; Pietro Amedeo Modesti for providing age-specific prevalence data from Yemen; the World Health Organization Study on global AGEing and adult health (SAGE) for providing analytic datasets; Sandra Fuchs and Rafael Picon for providing the references from their meta-analysis on hypertension prevalence in Brazil; and Vilnis Dzerve, Seter Siziya, and Rufus Adedoyin for providing additional methodological information for their hypertension prevalence studies in Latvia, Zambia, and Nigeria, respectively.
Funding Sources: The research reported in this publication was supported in part by the National Heart, Lung, and Blood Institute under Award Number U01HL114197 and by the National Institute of General Medical Sciences under Award Number P20GM109036. Dr. Mills is supported in part by the National Heart Lung and Blood Institute Johns Hopkins Cardiovascular Epidemiology training grant (T32HL007024). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosures: None.
References
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Lawes CMM, Vander Hoorn S, Rodgers A, for the International Society of Hypertension Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2013 Risk Factors Collaborators Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risk factors or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danaei G, Finucane MM, Lin JK, Singh GM, Paciorek CJ, Cowan MJ, Farzadfar F, Stevens GA, Lim SS, Riley LM, Ezzati, on behalf of the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Pressure) National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5.4 million participants. Lancet. 2011;377:568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 5.Addo J, Smeeth L, Leon DA. Hypertension in Sub-Saharan Africa: a systematic review. Hypertension. 2007;50:1012–1018. doi: 10.1161/HYPERTENSIONAHA.107.093336. [DOI] [PubMed] [Google Scholar]
- 6.Li YC, Wang LM, Jiang Y, Li XY, Zhang M, Hu N. Prevalence of hypertension among Chinese adults in 2010. Zhonghua Yu Fang Yi Xue Za Zhi. 2012;46:409–413. (in Chinese) [PubMed] [Google Scholar]
- 7.Devi P, Rao M, Sigamani A, Faruqui A, Jose M, Gupta R, Kerkar P, Jain RK, Joshi R, Chidambaram N, Rao DS, Thanikachalam S, Iyengar SS, Verghese K, Mohan V, Pais P, Xavier D. Prevalence, risk factors and awareness of hypertension in India: a systematic review. J Hum Hypertens. 2013;27:281–287. doi: 10.1038/jhh.2012.33. [DOI] [PubMed] [Google Scholar]
- 8.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 9.Kastarinen M, Antikainen R, Peltonen M, Laatikainen T, Barengo NC, Jula A, Salomaa V, Jousilahti P, Nissinen A, Vartiainen E, Tuomilehto J. Prevalence, awareness and treatment of hypertension in Finland during 1982-2007. J Hypertens. 2009;27:1552–1559. doi: 10.1097/HJH.0b013e32832c41cd. [DOI] [PubMed] [Google Scholar]
- 10.Cífková R, Škodová Z, Bruthans J, Holub J, Adámková V, Jozífová N, Galovcová M, Wohlfahrt P, Krajčoviechová A, Petržílková Z, Lánská V. Longitudinal trends in cardiovascular mortality and blood pressure levels, prevalence, awareness, treatment, and control of hypertension in the Czech population from 1985 to 2007/2008. J Hypertens. 2010;28:2196–2203. doi: 10.1097/HJH.0b013e32833d4451. [DOI] [PubMed] [Google Scholar]
- 11.Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27:963–975. doi: 10.1097/hjh.0b013e3283282f65. [DOI] [PubMed] [Google Scholar]
- 12.Banegas JR, Graciani A, de la Cruz-Troca JJ, León-Muñoz LM, Guallar-Castillón P, Coca A, Ruilope LM, Rodríguez-Artalejo F. Achievement of cardiometabolic goals in aware hypertensive patients in Spain: a nationwide population-based study. Hypertension. 2012;60:898–8905. doi: 10.1161/HYPERTENSIONAHA.112.193078. [DOI] [PubMed] [Google Scholar]
- 13.Rampal L, Rampal S, Azhar MZ, Rahman AR. Prevalence, awareness, treatment and control of hypertension in Malaysia: a national study of 16,440 subjects. Public Health. 2008;122:11–18. doi: 10.1016/j.puhe.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 14.Aekplakorn W, Sangthong R, Kessomboon P, Putwatana P, Inthawong R, Taneepanichskul S, Sritara P, Sangwatanaroj S, Chariyalertsak S, National Health Examination Survey IV study group Changes in prevalence, awareness, treatment and control of hypertension in Thai population, 2004-2009: Thai National Health Examination Survey III-IV. J Hypertens. 2012;30:1734–1742. doi: 10.1097/HJH.0b013e3283568158. [DOI] [PubMed] [Google Scholar]
- 15.Esteghamati A, Abbasi M, Alikhani S, Gouya MM, Delavari A, Shishehbor MH, Forouzanfar M, Hodjatzadeh A, Ramezani RD. Prevalence, awareness, treatment, and risk factors associated with hypertension in the Iranian population: the National Survey of Risk Factors for Noncommunicable Diseases of Iran. Am J Hypertens. 2008;21:620–626. doi: 10.1038/ajh.2008.154. [DOI] [PubMed] [Google Scholar]
- 16.Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, Bahonar A, Chifamba J, Dagenais G, Diaz R, Kazmi K, Lanas F, Wei L, Lopez-Jaramillo P, Fanghong L, Ismail NH, Puoane T, Rosengren A, Szuba A, Temizhan A, Wielgosz A, Yusuf R, Yusufali A, McKee M, Liu L, Mony P, Yusuf S, PURE (Prospective Urban Rural Epidemiology) Study investigators Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization Chronic Disease and Health Promotion [March 2015];WHO Global Infobase. https://apps.who.int/infobase/Index.aspx.
- 18.The World Bank [August 2014];Country and Lending Groups. http://data.worldbank.org/about/country-and-lending-groups.
- 19.Rubin DR. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons; New York: 1987. [Google Scholar]
- 20.United Nations, Department of Economic and Social Affairs [August 2014];World population prospects: the 2012 revision. http://esa.un.org/wpp/
- 21.Inskip H, Beral V, Fraser P, Haskey J. Methods for age-adjustment of rates. Stat Med. 1983;2:455–466. doi: 10.1002/sim.4780020404. [DOI] [PubMed] [Google Scholar]
- 22.Burt VL, Cohen SB. A comparison of methods to approximate standard errors for complex survey data. Rev Public Data Use. 1984;12:159–163. [PubMed] [Google Scholar]
- 23.GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–117. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hogerzeil HV, Liberman J, Wirtz VJ, Kishore SP, Selvaraj S, Kiddell-Monroe R, Mwangi-Powell FN, von Schoen-Angerer T, Lancet NCD Action Group Promotion of access to essential medicines for non-communicable diseases: practical implications of the UN political declaration. Lancet. 2013;381:680–689. doi: 10.1016/S0140-6736(12)62128-X. [DOI] [PubMed] [Google Scholar]
- 25.Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380:611–619. doi: 10.1016/S0140-6736(12)60861-7. [DOI] [PubMed] [Google Scholar]
- 26.Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, Roccella EJ, Stout R, Vallbona C, Winston MC, Karimbakas J, National High Blood Pressure Education Program Coordinating Committee Primary prevention of hypertension: clinical and public health advisory from the National High Blood Pressure Education Program. JAMA. 2002;288:1882–1888. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 27.Moran AE, Odden MC, Thanataveerat A, Tzong KY, Rasmussen PW, Guzman D, Williams L, Bibbins-Domingo K, Coxson PG, Goldman L. Cost-effectiveness of hypertension therapy according to 2014 guidelines. N Engl J Med. 2015;372:447–455. doi: 10.1056/NEJMsa1406751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaziano TA, Steyn K, Cohen DJ, Weinstein MC, Opie LH. Cost-effectiveness analysis of hypertension guidelines in South Africa: absolute risk versus blood pressure level. Circulation. 2005;112:3569–3576. doi: 10.1161/CIRCULATIONAHA.105.535922. [DOI] [PubMed] [Google Scholar]
- 29.Gu D, He J, Coxson PG, Rasmussen PW, Huang C, Thanataveerat A, Tzong KY, Xiong J, Wang M, Zhao D, Goldman L, Moran AE. The cost-effectiveness of low-cost essential antihypertensive medicines for hypertension control in China: a modelling study. PLoS Med. 2015;12:e1001860. doi: 10.1371/journal.pmed.1001860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.SPRINT Research Group A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Neal B, MacMahon S, Chapman N, Blood Pressure Lowering Treatment Trialists’ Collaboration Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomized trials. Lancet. 2000;356:1955–1964. doi: 10.1016/s0140-6736(00)03307-9. [DOI] [PubMed] [Google Scholar]
- 32.Jafar TH, Stark PC, Schmid CH, Landa M, Maschio G, de Jong PE, de Zeeuw D, Shahinfar S, Toto R, Levey AS, AIPRD Study Group Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: a patient-level meta-analysis. Ann Intern Med. 2003;139:244–252. doi: 10.7326/0003-4819-139-4-200308190-00006. [DOI] [PubMed] [Google Scholar]
- 33.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 34.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 35.Alleyne G, Binagwaho A, Haines A, Jahan S, Nugent R, Rojhani A, Stuckler D, Lancet NCD Action Group Embedding non-communicable diseases in the post-2015 development agenda. Lancet. 2013;381:566–574. doi: 10.1016/S0140-6736(12)61806-6. [DOI] [PubMed] [Google Scholar]
- 36.Fagard RH, Grassi G, Hall J, Harrap S, Lindholm LH, Schiffrin EL, Heagerty AM. International society of hypertension low and middle income countries committee: Review of the goals of the committee and of 5 years of ISH activities in low and middle income countries. J Hypertens. 2010;28:635–636. doi: 10.1097/01.hjh.0000368700.79444.c1. [DOI] [PubMed] [Google Scholar]
- 37.Committee on Public health Priorities to Reduce and Control Hypertension in the U.S. Population, Institute of Medicine . A population-based policy and systems change approach to prevent and control hypertension. National Academy Press; Washington DC: 2010. [PubMed] [Google Scholar]
- 38.Mills KT, Rubinstein A, Irazola V, Chen J, Beraterrechea A, Poggio R, Dolan J, Augustovski F, Shi L, Krousel-Wood M, Bazzano LA, He J. Comprehensive approach for hypertension control in low-income populations: rationale and study design for the Hypertension Control Program in Argentina. Am J Med Sci. 2014;348:139–145. doi: 10.1097/MAJ.0000000000000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.