Abstract
Malaysia introduced graphic health warning labels (GHWLs) on all tobacco packages in 2009. We aimed to examine if implementing GHWLs led to stronger warning reactions (e.g., thinking about the health risks of smoking) and an increase in subsequent quitting activities; and to examine how reactions changed over time since the implementation of the GHWLs in Malaysia and Thailand where GHWL size increased from 50–55% in 2010. Data came from six waves (2005–2014) of the International Tobacco Control Southeast Asia Survey. Between 3,706 and 4,422 smokers were interviewed across these two countries at each survey wave. Measures included salience of warnings, cognitive responses (i.e., thinking about the health risks and being more likely to quit smoking), forgoing cigarettes, and avoiding warnings. The main outcome was subsequent quit attempts. Following the implementation of GHWLs in Malaysia, reactions increased, in some cases to levels similar to the larger Thai warnings, but declined over time. In Thailand, reactions increased following implementation, with no decline for several years, and no clear effect of the small increase in warning size. Reactions, mainly cognitive responses, were consistently predictive of quit attempts in Thailand, but this was only consistently so in Malaysia after the change to GHWLs. In conclusion, GHWLs are responded to more frequently, and generate more quit attempts, but warning wear-out is not consistent in these two countries, perhaps due to differences in other tobacco control efforts.
Keywords: tobacco packaging, health warnings, Malaysia, Thailand
INTRODUCTION
Health warnings on tobacco packaging reach almost all smokers and have the potential to help them better understand the harms of tobacco and encourage quitting, especially when warnings are large, clear, graphic and specific in their descriptions of the illnesses caused by tobacco use. Prominent graphic health warnings are known to be more effective than text-only warnings (World Health Organization, 2008). In 2008, the World Health Organization (WHO) adopted Article 11 Guidelines (Packaging and labelling of tobacco products) of the Framework Convention on Tobacco Control (FCTC), urging governments to require that all tobacco packaging should include graphic health warning labels (GHWLs) that cover at least 50% of the front and back of the package, and include distinctive borders to make the warnings more prominent (World Health Organization, 2008b).
Research shows that implementing prominent and stronger health warnings increases smoking-related health awareness, and stimulates motivational/cognitive responses and micro-behaviour responses such as forgoing cigarettes (i.e., choosing not to smoke a cigarette that one would normally have smoked) (Borland et al., 2009; Hammond, 2011; Yong et al., 2013). Both pack warning size and warning type (graphic vs. text-only warnings) have been shown to play an important role in reducing warning wear-out after implementation (Li, Borland, Yong, Cummings, et al., 2015). An increasing international evidence also shows that strong reactions to health warnings predict subsequent quitting activities (Hammond, 2011). Using data from the International Tobacco Control Four Country Survey (ITC 4 Country Survey, covering Australia, Canada, the UK, and the US), Borland et al. (2009) found that cognitive responses and forgoing cigarettes as a result of noticing health warnings on cigarette packs were consistent prospective predictors of making quit attempts, although no consistent relationship with maintaining abstinence was found (Borland et al., 2009).
There are now a number of studies on the impact of health warnings in low- and middle-income countries (LMICs) (Fathelrahman et al., 2013; Fong, Hammond, & Hitchman, 2009; Hammond, 2011; Thrasher, Hammond, Fong, & Arillo-Santillán, 2007; Thrasher et al., 2013; Yong et al., 2013), mostly from Thailand and Malaysia. Collectively, these studies have found that introduction of larger and stronger health warnings leads to greater levels of health awareness, micro-behavioural responses and quitting activities, while weaker warnings (especially small text-only ones) are not potent enough to stimulate quitting activities (Fathelrahman et al., 2013; Yong et al., 2013).
Yong et al. (2013) found that following the introduction of GHWLs in Thailand in 2005, Thai smokers’ reported awareness and their cognitive and behavioural reactions increased markedly. By contrast, no significant change in these measures was observed in Malaysia over the same period (Yong et al., 2013). Subsequently, Fathelrahman et al. (2013) used the first three waves of data (2005–2008) from the ITC Southeast Asia Survey (ITC SEA Survey, covering Malaysia and Thailand) and found that among smokers of factory-made cigarettes (FMC) the then weak text-only Malaysian warnings (on side of the pack) were not consistently predictive of quitting, compared with reactions to strong graphic Thai warnings which were predictive. The study of Fathelrahman et al. (2013) was restricted to smokers of FMC only, because in Thailand roll-your own (RYO) tobacco did not carry the same health warnings.
It should be noted that the effectiveness of pack warnings may also be related to other tobacco control measures, such as mass media campaigns (Hammond, 2011). Malaysia’s first mass education campaign (“Tak Nak”—“Say No to Tobacco” campaign) was conducted in 2004, before the baseline (Wave 1) survey of the ITC SEA Survey. Thailand conducted its first comprehensive mass media campaign in 2006 (between Waves 1 and 2 of the ITC SEA Survey) (Fathelrahman et al., 2013), and then strengthened it again in 2007.
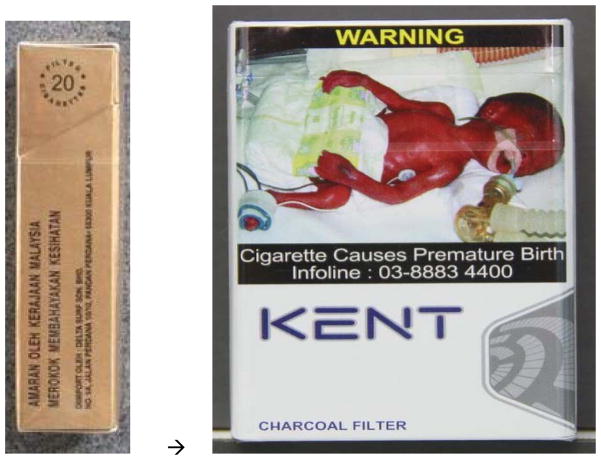
Malaysia introduced GHWLs in January 2009 on all tobacco products including RYO cigarettes (Malaysian Government, 2008), and this provides a rare opportunity to explore effects of moving from a minimal text-only warning (on the side of the package) to a strong set of GHWLs (see Figure 1). This policy change, which occurred between Waves 3 and 4 of our data collection (see Table 1, highlighted in blue) required that a set of six rotating GHWLs be printed in both Malay and English, covering 40% of the front and 60% of the back of all tobacco packages. These six GHWLs are about neck cancer, lung cancer, mouth cancer, gangrene, premature birth, and miscarriage, with pictorial depictions of warnings. (Note: A second round of its six GHWLs was introduced after study period of the current paper.) New development also occurred in Thailand. The size of its GHWLs was enlarged from 50% to 55% in 2010 (between Waves 4 and 5 of our data collection, Table 1, highlighted in red). (Note: Even larger GHWLs at 85% on both sides with two different health images and text messages for each cigarette pack were implemented after June 2014, but this is outside the study period of the current paper).
Figure 1.
Malaysia’s transition from weak text-only package warning (on the side of the pack) to graphic health warnings in 2009 (40% of the front of the pack)
Table 1.
Sample characteristics and pack warning change dates
| Malaysia | Thailand | Total | Country Differences~ | |
|---|---|---|---|---|
| No. of respondents at each wave | ||||
| Wave 1 (in early 2005) | 2004 | 2000 | 4004 | |
| (From March 2005 Thailand implemented graphic warnings, covering 50% of the front) | ||||
| Wave 2 (2006) | 1640 | 2066 | 3706 | |
| Wave 3 (2008) | 1957 | 2465 | 4422 | |
| (From January2009 Malaysia implemented graphic warnings, covering 40% of the front) | ||||
| Wave 4 (2009) | 2045 | 2276 | 4321 | |
| (In 2010 Thailand increased graphic warning size from 50% to 55% ) | ||||
| Wave 5 (2011) | 2007 | 2132 | 4139 | |
| Wave 6 (2013/14) | 2000 | 2159 | 4159 | |
| Gender (% male, out of total unique individuals#: for Malaysia N=5311; for Thailand N=3817, Total N=9128) | 97.3 | 90.7 | 94.6 | ** |
| Ethnicity (% minority group) | 19.1 | 1.3 | 11.9 | *** |
| Urban/rural region (% urban) | 65.5 | 43.8 | 56.4 | *** |
| Age at recruitment^(%) | *** | |||
| 18–24 | 33.5 | 8.1 | 22.9 | |
| 25–39 | 33.3 | 26.4 | 29.3 | |
| 40–54 | 22.3 | 38.8 | 30.5 | |
| 55+ | 10.9 | 26.5 | 17.5 | |
| Education at recruitment (%) | *** | |||
| Low | 13.7 | 67.7 | 36.4 | |
| Moderate | 73.5 | 23.6 | 52.5 | |
| High | 12.8 | 8.7 | 11.1 | |
| Income at recruitment (%) | *** | |||
| Low | 23.9 | 25.3 | 24.5 | |
| Moderate | 26.1 | 30.9 | 28.1 | |
| High | 30.1 | 40.2 | 34.3 | |
| No information | 19.9 | 3.6 | 13.1 | |
| Cigarettes per day at recruitment (%) | *** | |||
| 1–10 | 49.8 | 54.9 | 51.9 | |
| 11–20 | 44.5 | 38.3 | 41.9 | |
| 21–30 | 3.4 | 4.5 | 3.9 | |
| 31+ | 2.3 | 2.4 | 2.4 | |
| Tobacco products smoked (% factory-made cigarettes) | 93.8 | 70.1 | 83.8 | *** |
| Intention to quit at recruitment (%) | *** | |||
| No intention/can’t say | 37.5 | 65.1 | 49.1 | |
| Beyond 6 months | 47.5 | 16.1 | 34.3 | |
| Within next 6 months | 9.2 | 12.2 | 10.4 | |
| Within next month | 5.9 | 6.6 | 6.2 | |
| Self-efficacy at recruitment (%) | *** | |||
| Not at all sure | 20.6 | 38.7 | 28.3 | |
| Somewhat sure/don’t know | 51.9 | 33.8 | 44.3 | |
| Very sure | 21.9 | 17.9 | 20.3 | |
| Extremely sure | 5.5 | 9.5 | 7.2 | |
At the time they first participated in the Survey.
For all unique individuals who were presented in at least one wave of the surveys (from Wave 1 to Wave 6), and this applies to the other variables in the table. For some variables the numbers of cases were fewer than the total unique cases, due to some “don’t know” and “missing” cases.
chi square test results.
Significant at p<0.01 level;
Significant at p<0.001.
As mentioned earlier, in Malaysia the regulations required that GHWLs be printed on all tobacco packages, including RYO tobacco. This paper reports on data from three additional follow-up waves (Waves 4–6) of post-GHWL data for Malaysia to add to the earlier three waves, covering the period between 2005 and 2014. It is the first study to examine the effects of changing from a minimal on-the-side-of-pack text warning to a strong set of on-the-main-face graphic warnings. The aims of this study are:
To examine if implementing GHWLs in Malaysia led to stronger warning reactions among smokers, and if the warning reactions were associated with subsequent quitting activities. We predicted that they would.
To explore if there was any effect of the small increase in Thai GHWLs from 50% to 55% (no specific predictions); and
To examine how the warning reactions and their predictive power changed over time in Malaysia and Thailand. We expected wear-out as assessed by intensity/frequency of reactions, but persisting predictive relationships for making quit attempts.
METHODS
Data source and participants
The data came from six waves (2005–2014) of the ITC SEA Survey, a prospective cohort survey designed to evaluate the psychosocial and behavioural impacts of tobacco control policies in Malaysia and Thailand. A detailed description of the sampling and study design of the ITC SEA Survey has been reported elsewhere (ITC Project, 2010; Yong et al., 2008). Briefly, the ITC SEA adult smoker survey employs a multistage clustering sampling procedure. Participants were recruited from adults aged 18 and older who had smoked at least 100 cigarettes in their lifetime and smoked at least weekly at the time of recruitment. All participants were surveyed using standardized questionnaire. Survey interviews were generally conducted in Malay in Malaysia and in Thai in Thailand. All participants in Thailand were surveyed via face-to-face interviews. In Malaysia, Wave 1 was conducted using the face-to-face interviewing method; Waves 2 and 3 were by using either face-to-face or telephone interview method; Wave 4 were all by telephone, and Waves 5 and 6 were by the Computer Assisted Telephone Interview (CATI) (ITC Project, 2010,ITC Project, 2013). The sample size per country was around 2,000 at each survey wave, with replenishment sampling from the same sampling frame used to maintain sample size across waves. Replenishment response rates for Malaysia ranged from 35.6% (in Wave 5) to 46.1% (in Wave 6). The cooperation rate in Thailand (58.7%) was higher than Malaysia (32.4%) in Wave 1. In the current study, unlike Fathelrahman et al. (2013), we also included RYO smokers in the analysis. Preliminary analysis revealed that most RYO smokers were aware of the warnings. Data collection time and sample size for each wave, and characteristics of the sample are summarised in Table 1.
Measures
Health warning-related measures asked in each wave
Four separate warning reactions (measures) were used in the study. They were salience of warnings, cognitive response, forgoing cigarettes and avoiding warnings.
Salience of the health warnings was assessed by asking how often, over the preceding month, respondents had (1) noticed the warning labels, and (2) read/looked closely at them (both on 4-point scales: “never” to “very often”); and based on respondents’ answers to these two questions, a combined salience measure was computed (range=0–6, as a continuous variable). (Cronbach’s α=0.60–0.86, across waves). The smokers were asked about cognitive responses in terms of the extent to which the warnings (1) made them think about the health risks of smoking, and (2) made them more likely to quit smoking (both on 4-point scales: “not at all” to “a lot”). Based on respondents’ answers to these two questions, a combined cognitive response measure was computed (range=0–6, as a continuous variable). (Cronbach’s α=0.73–0.93, across waves).
Respondents were asked about the frequency (if ever) of stopping from having a cigarette when about to smoke one because of the warnings (i.e., forgoing cigarettes) over the preceding month (“never”, “once”, “a few times”, and “many times”), from which a binary variable (“any” versus “never”) was computed. Respondents were also asked if they avoided looking at the warnings (with “yes” and “no” options for both countries at all waves, except at Wave 4 where four ways of avoiding the warnings (covering-up, keeping out of sight, using cigarette case or avoiding buying packs with certain labels) were asked of Malaysian smokers). Based on respondents’ answers, a binary variable (“no avoidance” versus “any avoidance”) was computed.
Covariates
A range of socio-demographic variables were also assessed and used in the analysis. These included age (18–24, 25–39, 40–54, 55 and older), sex (male, female), region type (urban, rural), ethnicity (Thai versus non-Thai minority groups in Thailand; Malays versus Indians, Chinese and other non-Malay minority groups), education, and income (low, moderate, high). Relative levels were used for education and income across the two countries, and definitions of each level of income can be found in Ross et al., 2009 (Ross, Driezen, Sirirassamee, & Kin, 2009). “Low” level of education refers to those with no schooling/elementary schooling; “moderate” refers to those with secondary education (up to pre-university/diploma in Malaysia, and up to diploma in Thailand); and “high” are those who received higher education.
Smoking-related measures included as covariates were tobacco product smoked (FMC versus RYO cigarettes), and cigarettes smoked per day (CPD), recoded into “10 cigarettes or less”, “11–20”, “21–30”, and “31 or more ”. Participants were asked about their intention to quit: “Are you planning to quit smoking?” ( “within the next month”, “within the next 6 months”, “sometime in the future, beyond 6 months”, and “not planning to quit/can’t say”); and their self-efficacy for quitting successfully: “If you decided to give up smoking completely in the next 6 months, how sure are you that you would succeed?” ( “not at all sure”, “somewhat sure/don’t know”, “very sure”, and “extremely sure”).
Outcome measure in predictive analysis
Quit attempts were assessed at the next wave of exposure to warnings (i.e., from Wave 2), based on being quit at the follow-up or reporting a failed attempt: “Since we last talked to you on [last survey date], have you made any attempts to stop smoking?”
Data analysis
Chi square tests were used to assess group/country differences in socio-demographics and smoking-related variables. For salience of warnings and cognitive response we reported their mean levels, and for forgoing cigarettes and warning avoidance we presented the percentages reporting positive responses. Weighted data were used for all four warning reaction measures.
To account for the correlated nature of the data from participants present in multiple survey waves, Generalised Estimating Equations (GEE) models were employed to compute parameter estimates and examine warning reactions across countries and over time/waves in the same country. Because warning salience and cognitive responses were treated as continuous dependent variables in GEE modelling, identity link function and Gaussian family distribution were specified for their GEE models. Forgoing cigarettes and avoiding warnings were treated as binary dependent variables in GEE modelling, so logit link function and binomial family distribution were specified for their GEE models. An unstructured correlation matrix was employed to account for the within subjects clustering for all GEE models. The GEE modelling adjusted for demographics, time in sample and cigarettes per day. In statistical testing of changes in warning reactions over time in each country, survey wave was treated as a categorical variable and particular reference group (e.g., Wave 3) was set for comparison with other survey waves.
Logistic regressions were used to test for possible predictive associations of warning-related variables with reported quit attempts over the following year/wave. The analyses proceeded in two main steps. First, each individual predictor (e.g., salience) was used as independent variable (i.e., quit attempt as dependent variable - bivariate analyses), followed by multivariate analyses in which all predictors were added simultaneously, adjusting for socio-demographic and smoking-related variables. The odds ratios (ORs) with their 95% confidence intervals (CI) were computed for each predictor variable. A p value <0.05 was considered statistically significant. All analyses were conducted using Stata Version 14.0.
RESULTS
Sample characteristics
Table 1 presents the characteristics of the sample. In both countries, the vast majority of respondents were male. Beyond that the samples differed considerably, reflecting the different level of development in these two countries. Compared to their Thai counterparts, Malaysian smokers were more likely to be younger (66.8% Malaysian smokers were younger than 40 years), from urban areas, with a moderate or higher education. A considerable proportion of the Malaysian smokers (19.1%) were of minority ethnicity (e.g., Chinese or Indian), whereas this only accounted for 1.3% in Thailand. For smoking-related characteristics, compared to Thailand, a bigger proportion of smokers in Malaysia reported smoking 11+ CPD, using factory-made cigarettes, having some intention to quit and higher self-efficacy for quitting.
Reactions to pack warnings over six survey waves
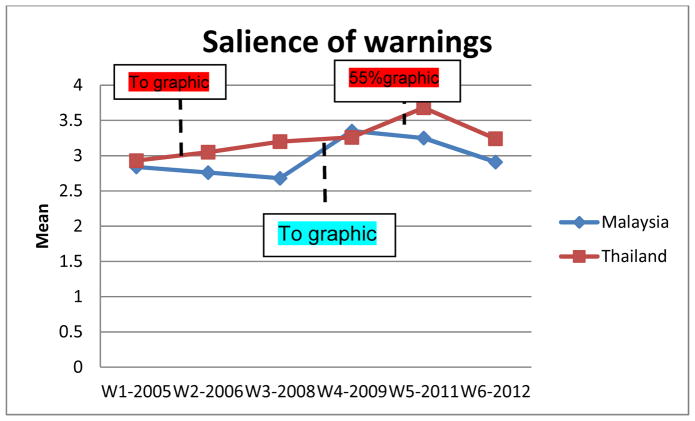
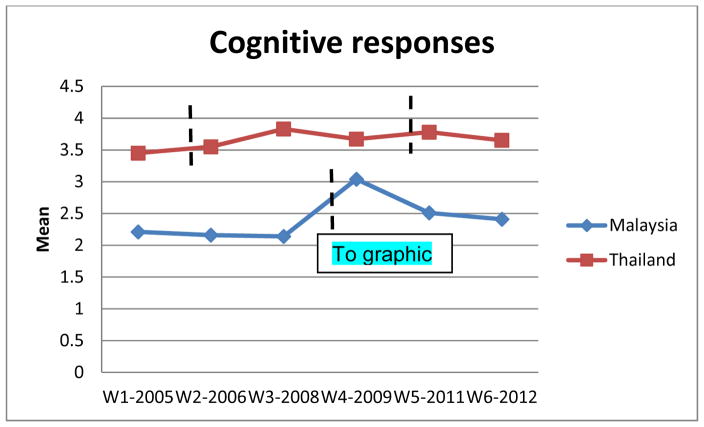
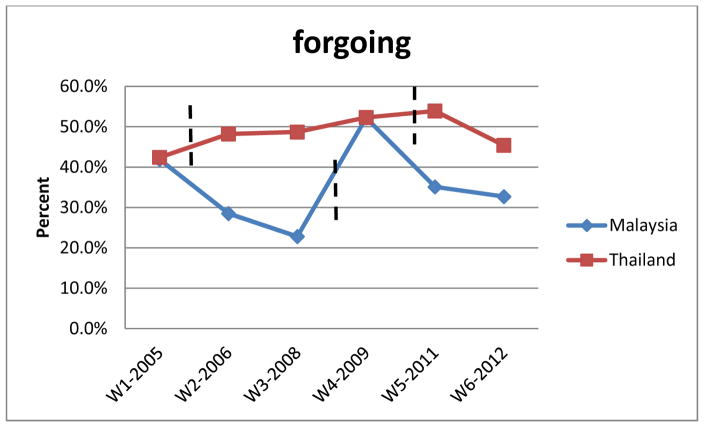
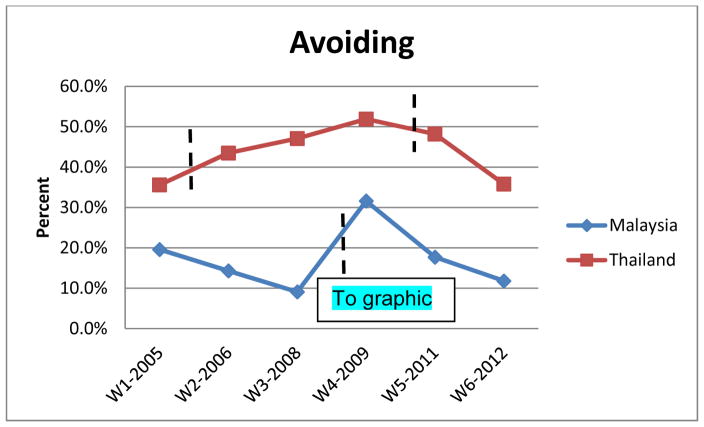
Overall reaction levels were significantly lower in Malaysia than in Thailand, especially for the first three survey waves (see Figures 2.1–2.4). However, at Wave 4 (shortly after the implementation of GHWLs in Malaysia) the reaction levels among Malaysia smokers increased considerably from that of early waves with all four measures post-implementation significantly higher than that at Wave 3 (i.e., the wave before the policy change, p<0.001, Figures 2.1–2.4 and statistical testing results in Table 2). For warning salience and forgoing cigarettes the levels in Malaysia reached as high as that of Thailand. The warning reactions in Malaysia markedly declined/wore-out in subsequent waves. We also note the previously reported drop from Wave 1 in Malaysia. In contrast, in Thailand reactions to post-graphic warnings (at least until Wave 5) remained higher than those at the baseline wave (i.e., Wave 1), although there was a sharp decline from Wave 5 to Wave 6 for most measures (Figures 2.1–2.4 and Table 2). After the small increase in Thai GHWL, there was an increase in salience (from Wave 4 to Wave 5, p<0.001), but little change or a small decline in the micro-behaviours (i.e., forgoing cigarettes and avoiding warnings).
Figure 2.
Figure 2.1. Salience of pack warning labels
Notes: Weighted data was used. “W1” stands for “Wave 1 of the survey”, and this applies to other survey waves. “To graphic” means moving from text-only warnings to graphic warnings. Overall, this warning reaction is significantly higher in Thailand than Malaysia (coefficient=0.22, p<0.001, GEE modeling results). Detailed statistical testing results (from GEE modeling) of changes in the warning reaction over time in each country are reported in Table 2.
Figure 2.2. Cognitive responses
Notes: Weighted data was used. “W1” stands for “Wave 1 of the survey”, and this applies to other survey waves. “To graphic” means moving from text-only warnings to graphic warnings. This warning reaction is significantly higher in Thailand than Malaysia (coefficient=1.05, p<0.001, GEE modeling results). Detailed statistical testing results of changes in the warning reaction over time in each country are reported in Table 2.
Figure 2.3. Forgoing cigarettes
Notes: Weighted data was used. “W1” stands for “Wave 1 of the survey”, and this applies to other survey waves. “To graphic” means moving from text-only warnings to graphic warnings. Percentages are the proportion reporting positive responses (at least once). Detailed statistical testing results of changes in the warning reaction over time in each country are reported in Table 2.
Figure 2.4. Avoiding warnings
Notes: Weighted data was used. “W1” stands for “Wave 1 of the survey”, and this applies to other survey waves. “To graphic” means moving from text-only warnings to graphic warnings. This warning reaction is significantly higher in Thailand than Malaysia (odds ratio=2.23, p<0.001, GEE modeling results). Percentages are the proportion reporting positive responses (any avoidance). Detailed statistical testing results of changes in the warning reaction over time in each country are reported in Table 2.
Table 2.
Statistical testing and trend analysis of changes in warning reactions over time in Malaysia and Thailand: results from GEE modelling
| Warning reactions | n (N) | 2005 (Wave1) | 2006 (Wave2) | 2008 (Wave3) | 2009 (Wave4) | 2011 (Wave5) | 2013 (Wave6) |
|---|---|---|---|---|---|---|---|
|
Salience of warnings Thailand B1# (SE) |
3,511 (9,904) | Ref | .21(.05)*** | .39(.05)*** | .57(.05)*** | 1.14(.05)*** | .66(.05)*** |
| B2##(SE) | −.57(0.05)*** | −.36(.05)*** | −.18(.05)*** | Ref | .57(.05)*** | .09(.05) | |
| Malaysia B(SE) |
4,492 (9,050) | .32(.05)*** | .11(.06) | Ref | .77(.05)*** | .69(.06)*** | .37(.06)*** |
|
Cognitive response Thailand B1#(SE) |
3,492 (9,849) | Ref | .22(.06)*** | .49(.06)*** | .44(.06)*** | .61(.06)*** | .50(.06)*** |
| B2##(SE) | −.43(.06)*** | −.22(.06)*** | .05(.06) | Ref | .18(.06) | .06(.06) | |
| Malaysia B(SE) |
4,956 (9,448) | .25(.06)*** | .07(.06) | Ref | 1.01(.06)*** | .50(.06)*** | .47(.06)*** |
|
Forgoing cigarettes Thailand OR1#(95% CI) |
3,513 (9,949) | Ref | 1.26(1.11–1.43)*** | 1.25(1.10–1.41)*** | 1.54(1.36–1.75)*** | 1.60(1.40–1.82)*** | 1.26(1.10–1.44)*** |
| OR2## (95% CI) | .65(.57–.74)*** | .82(.72–.93)** | .81(.72–.92)** | Ref | 1.04(.91–1.18) | .82(.72–.93)** | |
| Malaysia OR(95% CI) |
4,964 (9,516) | 2.75(2.36–3.21)*** | 1.51(1.27–1.73)*** | Ref | 4.29(3.68–5.01)*** | 2.56(2.19–2.99)*** | 2.41(2.05–2.83)*** |
|
Avoiding warnings Thailand OR1# (95% CI) |
3,512 (9,948) | Ref | 1.57(1.37–1.78)*** | 1.79(1.58–2.04)*** | 2.37(2.07–2.71)*** | 2.14(1.87–2.47)*** | 1.48(1.29–1.70)*** |
| OR2# (95% CI) | .42(.37–.48)*** | .66(.60–.76)*** | .76(.67–.86)*** | Ref | .91(.80–1.03) | .63(.55–.72)*** | |
| Malaysia OR(95% CI) |
4,955 (9,488) | 2.71(2.19–3.35)*** | 1.81(1.43–2.29)*** | Ref | 4.65(3.79–5.70)*** | 2.33(1.89–2.89)*** | 1.61(1.28–2.02)*** |
NB. GEE, generalised estimating equations; n, number of unique individual observations; N, number of person-wave observations; Levels of warning reactions (mean/percentages) are reported in Figs 2.1–2.4. B, regression estimates (positive coefficients refer to higher mean level of warning reaction relative to the reference group),
the value at Wave 1 as reference,
the value at Wave 4 as reference; SE, standard error; Ref, reference group (the most proximal survey year prior to the introduction of graphic warnings was set as the reference group for comparison with other survey year within the same country): During the whole study period, Malaysia only introduced graphic health warning labels (GHWL) one time (in 2009). Therefore, we only used Wave 3 (before-GHWL survey wave) as the reference point for Malaysia. Thailand introduced GHWL two times during the whole study period. Therefore, for 2005 GHWL in Thailand, Wave 1 (before-GHWL survey wave) served as the reference point. For the 2010 new GHWL, we used its “before-GHWL survey wave” (Wave 4) as reference point, and cross-wave comparisons were conducted.
; OR, odds ratio; all B and ORs are adjusted for demographics, time in sample and cigarette smoked per day.
Significant at p<0.05;
significant at p<0.01;
significant at p<0.001.
Predictive power of warning reactions on subsequent quit attempts
Predictive analyses are reported for all waves, with the early waves essentially replicating Fathelrahman et al. (Fathelrahman et al., 2013), with the addition of the RYO smokers. For Thailand, at all waves some of the reactions were predictive of subsequent quitting with the cognitive reactions always so (Table 3). On the other hand, for Malaysia, there were no clear predictive effects, at least in the adjusted multivariate analyses when the predictor reactions were to the side of pack text-only warnings, until the first predictor wave after the GHWLs were introduced (Wave 4). As predicted, the pattern of relations changed markedly for Malaysia from Wave 4: all warning reactions at Waves 4 and 5 (post-graphic warning survey waves) became predictive of subsequent quit attempts in bivariate analysis; and in multivariate analyses, avoiding (at Wave 4) and warning salience and cognitive responses (at Wave 5) remained predictive of subsequent quit attempts (Table 3).
Table 3.
Warning reactions predicting follow-up year quit attempts among smokers in Malaysia and Thailand
| Quit attempts in follow up wave | ||||
|---|---|---|---|---|
| Malaysia (followed-up n=868 at W2^; n=536 at W3; n=934 at W4; n=1406 at W5; n=1304 at W6) | Thailand (followed-up n=1558 at W2; n=1164 at W3; n=1600 at W4; n=1506 at W5; n=1372 at W6) | |||
| OR (95%CI) # | Adjusted OR (95%CI) ## | OR (95%CI) # | Adjusted OR (95%CI) ## | |
| Wave 1 (2005): | ||||
| Salience (scale) | 1.04 (0.96 – 1.14) | 0.99 (0.89 – 1.09) | 1.04 (0.99 – 1.11) | 1.02 (0.95 – 1.10) |
| Cognitive responses (scale) | 1.17 (1.08 – 1.27)*** | 1.11 (0.98 – 1.22) | 1.17 (1.11 – 1.23)*** | 1.10(1.03–1.19)** |
| Forgoing | 1.71 (1.28 – 2.27) *** | 1.37(0.96 – 1.95) | 1.56 (1.23 – 1.98)*** | 1.14 (0.85– 1.51) |
| Avoiding | 1.19 (0.85 – 1.69) | 1.05 (0.73 – 1.54) | 1.51 (1.19 – 1.96)** | 1.35 (1.03 – 1.77)* |
| (From March2005 Thailand implemented graphic warnings, covering 50% of the front) | ||||
| Wave 2 (2006): | ||||
| Salience (scale) | 0.93 (0.82 – 1.03) | 0.84 (0.75 – 0.97) * | 1.04(0.96 – 1.24) | 0.87 (0.78 – 0.97) * |
| Cognitive responses (scale) | 1.06 (0.96 – 1.18) | 1.12 (0.97 – 1.29) | 1.19 (1.12 – 1.27)*** | 1.11 (1.01 – 1.22)* |
| Forgoing | 0.86 (0.58 – 1.26) | 0.75 (0.45 – 1.24) | 3.14 (2.33 – 4.23) *** | 2.43 (1.66 – 3.57) *** |
| Avoiding | 0.81 (0.45 – 1.39) | 1.06 (0.57 – 1.97) | 1.55 (1.17 – 2.07)** | 1.18 (0.82 – 1.69) |
| Wave 3 (2008): | ||||
| Salience (scale) | 0.96 (0.88 – 1.03) | 0.94 (0.85 – 1.03) | 1.20 (1.14 – 1.28) *** | 0.95(0.87 – 1.03) |
| Cognitive responses (scale) | 1.02 (0.94 – 1.09) | 1.04 (0.94 – 1.15) | 1.26 (1.21 – 1.33) *** | 1.11 (1.03 – 1.19) ** |
| Forgoing | 1.07 (0.78 – 1.46) | 1.02 (0.68 – 1.53) | 2.26 (1.82 – 2.78) *** | 1.24 (0.95 – 1.63) |
| Avoiding | 1.24(0.76 – 2.04) | 1.29 (0.74 – 2.22) | 1.77 (1.43 – 2.18) *** | 1.17 (0.91 – 1.49) |
| (From Jan2009 Malaysia implemented graphic warnings, covering 40% of the front) | ||||
| Wave 4 (2009): | ||||
| Salience (scale) | 1.16(1.08 – 1.25)*** | 1.06 (0.97 – 1.15) | 1.21 (1.14 – 1.27)*** | 1.00 (0.92 – 1.09) |
| Cognitive responses (scale) | 1.15(1.07 – 1.22)*** | 1.03 (0.95 – 1.12) | 1.29 (1.25 – 1.36)*** | 1.11 (1.03 – 1.20)** |
| Forgoing | 1.40 (1.13 – 1.72)** | 1.06 (0.82 – 1.36) | 2.75 (2.19 – 3.33)*** | 1.32 (0.99 – 1.74) (p=0.054) |
| Avoiding | 2.26 (1.75 – 2.99)*** | 1.87 (1.43 – 2.44)*** | 1.89 (1.54 – 2.33)*** | 1.07 (0.83 – 1.38) |
| (In 2010 Thailand increased graphic warning size from 50% to 55% ) | ||||
| Wave 5 (2011): | ||||
| Salience (scale) | 1.21(1.12 – 1.32)*** | 1.11(1.01 – 1.22)* | 1.01 (.95 – 1.08) | 0.93 (0.86 – 1.02) |
| Cognitive responses (scale) | 1.25(1.16 – 1.34)*** | 1.10 (1.01 – 1.21)* | 1.21 (1.14 – 1.29)*** | 1.13 (1.04 – 1.22)** |
| Forgoing | 1.68 (1.32 – 2.13)*** | 1.29 (0.97 – 1.71) | 2.04 (1.64 – 2.59)*** | 1.52 (1.16 – 1.99)** |
| Avoiding | 1.42(1.04 – 1.92)* | 1.03 (0.75 – 1.45) | 1.43 (1.15 – 1.78)** | 1.10 (0.86 – 1.42) |
This number of participants is for those who were current smokers when surveyed in the previous Wave (i.e., Wave 1), successfully followed up at the specified Wave (i.e., Wave 2), and with their quit attempt outcome being determined. “W2” means “Wave 2 of the survey”. This applies to other waves and numbers. For the full numbers of participants at each survey wave in each country please refer to Table 1. In some analyses the numbers of cases were fewer than the total, due to some “refused” and “missing” cases.
Simple logistic regression (bivariate analysis);
Multivariate logistic regression analysis, adjusting for socio-demographics and smoking-related variables.
Significant at p<.05;
p<.01;
p<.001.
DISCUSSION
This is the first study to examine the effects of moving from a minimal text-only pack warnings (on the side of pack) to a strong set of GHWLs (with larger warning labels on the main faces). As predicted, implementing GHWLs in Malaysia led to increased warning reactions, especially at the survey wave immediately after the implementation. However, the effect of the new GHWLs was short-lived and was not sustained in Waves 5 and 6. Furthermore, the stronger warning reactions were predictive of subsequent quit attempts, which is consistent with early findings from other studies (Fathelrahman et al., 2013; Li, Borland, Yong, Cummings, et al., 2015).
The implementation of GHWLs in Malaysia not only increased the salience of health warnings and smokers’ cognitive responses, more importantly, it also considerably increased smokers’ micro-behaviours, such as forgoing cigarettes and avoiding cigarette packs, at least at the first post-implementation survey wave (Wave 4). International studies (including those in Thailand) have found a proximal association between these micro-behaviours and quitting behaviours (Borland et al., 2009; Fathelrahman et al., 2013; Li et al., 2014; Partos et al., 2014). The finding of an independent predictive relationship between avoidance in the wave immediately post-implementation and subsequent quit attempts in Malaysia is notable. It may be that the moving from minimal text-only warnings (that were general and only on one side of the cigarette packs for over 30 years, since 1976) to new graphic warnings (that were specific and on the main faces of the packs) does stimulate some shock-related quitting: i.e., quitting as a direct result of not wanting to think about or see the warnings, rather than having this mediated by consideration of the harms of smoking. Given that this has not been found previously when the increase in prominence of warnings has been less (e.g., Thailand in this study and elsewhere (Borland et al., 2009; Fathelrahman et al., 2013; Li, Borland, Yong, Cummings, et al., 2015) ), it may be an initial reaction to warnings that do not have to be sought out, but which are prominent enough to draw attention. However, over time, if this is not also associated with more elaborated thinking, as indexed by the cognitive reactions and concern, it will not be sustained. An alternative explanation is the way the avoiding warning measure was asked at Wave 4 in Malaysia (by combining answers to four separate questions) while in other waves and in Thailand it was a single compound question. While this likely affected the level of responding, it is unlikely to have affected the predictive power, as this set of questions has been used in previous studies which have not found independent predictive effects (Borland et al., 2009).
One other unexpected aspect of the Malaysian data is the large drop in reactions to the warnings, or alternatively the unexpectedly high levels at Wave 1. As suggested early in the paper and elsewhere (Li, Borland, Yong, Sirirassamee, et al., 2015) this may be due to this wave being collected at the end of Malaysia’s first large-scale anti-smoking campaign (i.e., “Tak Nak” campaign). However, the implementation of the “Tak Nak” campaign weakened or was not present in subsequent years, and thus any potential impact would have diminished or disappeared.
Overall, the pattern of warning reactions we found for Thailand is very different from that in Malaysia. Unlike in Malaysia where warning reactions peaked at the first survey wave post-GHWL implementation (Wave 4) and then markedly declined at the subsequent survey waves (at Waves 5 and 6), the warning reactions in Thailand did not suddenly decline from such a peak post-implementation. On the contrary, the warning reaction levels in Thailand continued to increase or remained high for some waves/years (from Waves 2 to 5 for most measures) before a drop in the second wave post-implementation of the slightly larger (55%) warnings. One possible explanation for the sustained effect in Thailand could be due to the rotational system of periodic updating of the GHWLs, as reported for early survey waves (between Waves 2 and 3) (Yong et al., 2013). Another possible explanation might be its comprehensive tobacco control program in general, and strong public education in particular. For the most part of the study period, Thailand had comparatively more robust tobacco control policies and measures. Relevant to this study, Thailand implemented a complete ban on the displays of cigarettes and other tobacco products at the point of sale (POS) from 2005, and evidence shows that the display ban has reduced exposure to tobacco marketing at POS (Li, Borland, Yong, Sirirassamee, et al., 2015). Whereas Malaysia had not adopted any display bans/restrictions on POS during the study period. The availability and accessibility of smoking cessation services may also influence smokers’ quitting intentions and activities. Furthermore, as mentioned earlier, Thailand conducted its first mass media campaign (on second-hand smoke in public places) in 2006, and then another campaign on smoke-free homes in 2007 (Li, Borland, Yong, Sirirassamee, et al., 2015). These public education efforts, along with other tobacco control activities in Thailand, may have helped sustain reactions to the GHWLs. Although Malaysia also required a rotation of health warnings on packaging, overall there was a lack of coordinated and sustained effort to publicize the rotating messages and other anti-smoking messages in the mass media after 2009. As mentioned above, the “Tak Nak” campaign weakened by then. As a result, the impact of rotating warning labels appeared to be very limited in Malaysia. Such an explanation is consistent with international evidence on the effect of integrated tobacco control efforts (Durkin, Brennan, & Wakefield, 2012; Fathelrahman et al., 2013; Li et al., 2009; World Health Organization, 2008), and also with our explanation of the unexpectedly high level of reactions to the Malaysian warnings in Wave 1 in 2005.
We were unable to detect any clear effects of the increase of Thai GHWLs from 50% to 55% across the four reaction measures used. The survey wave immediately post-increase in GHWL size (Wave 5) saw an increase in salience, but little more than the prevailing trend, and little change or a small decline in the micro-behaviours. From Wave 5 to Wave 6 all measures declined, as in Malaysia. We are not sure why this has happened. A possible explanation is that the intensity of mass media campaign efforts around Waves 6 was not as strong as that in preceding waves/years. Alternatively, it could represent some wear-out after a period of consolidated effort.
This study has its limitations and strengths. One of the limitations is the reliance on self-reports in the survey. The reactions studied are not necessarily ones that smokers would be cued to remember, so there is likely considerable error in their estimates of their frequency, and some of that error is likely systematic: the more concerned they are in general the more likely they are to report specific effects. We also know that recall of making quit attempts declines with time (Borland, Partos, Yong, Cummings, & Hyland, 2012). Further caution needs to be exercised when comparing the absolute levels of reactions as they could be influenced by cultural differences between the countries. Some of the changes over time could also be due to time-in-sample effects, although we have attempted to control for these. Also some of the changes found in Malaysia may be as a result of shifting over from face-to-face interviews to telephone surveys, either due to mode effects or the sampling differences that may have occurred. That said, we have done all we can to minimise such effects and see no evidence of any such problems.
Study strengths include the large sample size and its national focus and representativeness. Its prospective bi-country cohort design and the rich longitudinal data of over nine years has enabled us to assess the differences and changes in warning reactions over time and across the countries, and allowed for comprehensive predictive analyses to be conducted. The use of GEE modelling allowed us to combine respondents from all six survey waves while accounting for inherent within-person correlation, thereby increasing our sample size and power to examine relations and detect effects.
On the basis of the findings of this study, we conclude that in Malaysia, health warning effectiveness in terms of increases in factors influencing quitting improved after it introduced GHWLs, which is consistent with findings from Thailand. Consistent with previous research in Australia, Canada, Thailand, and elsewhere, the introduction of prominent health warnings in Malaysia increased smokers’ cognitive and micro-behaviour responses (at least shortly after the implementation), which are found to be predictive of quitting activities. However, the pattern of changes in reactions to GHWLs in Malaysia and Thailand was different, with Thailand having a sustained effect. Wear-out of warnings in Malaysia appeared to be greater than in Thailand, perhaps because of differences in the accompanying community-wide tobacco control efforts. The current findings strengthen the evidence that stronger GHWLs can stimulate quitting activities.
Acknowledgments
Financial Support: This work was supported by the National Cancer Institute at the National Institutes of Health of the United States (grants R01 CA100362, P50 CA111236); the Robert Wood Johnson Foundation (045734); the Canadian Institutes of Health Research (79551, and 115016); the Malaysian Ministry of Health; and the Thai Health Promotion Foundation Research.
The authors would like to thank other members of the ITC SEA Survey team for their support. Supported by a Ford Foundation International Fellowship Program’s Alumni Award, the lead author (Dr. Lin Li) shared some of the results and received valuable feedback at China’s 2015 National Tobacco Control Conference held in Beijing from October 17–18. We are grateful to the editors (including Dr. Kenneth Ward) of the Journal of Smoking Cessation and the anonymous reviewers who provided useful suggestions on earlier drafts of this paper.
Footnotes
Conflict of Interest: None.
Ethical Standards: “The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.”
Endnotes
- Borland R, Partos TR, Yong HH, Cummings KM, Hyland A. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control Four Country cohort survey. Addiction. 2012;107(3):673–682. doi: 10.1111/j.1360-0443.2011.03685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R, Yong HH, Wilson N, Fong GT, Hammond D, Cummings KM, … McNeill A. How reactions to cigarette packet health warnings influence quitting: findings from the ITC Four-Country survey. Addiction. 2009;104(4):669–675. doi: 10.1111/j.1360-0443.2009.02508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin S, Brennan E, Wakefield M. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tobacco Control. 2012;21(2):127–138. doi: 10.1136/tobaccocontrol-2011-050345. [DOI] [PubMed] [Google Scholar]
- Fathelrahman AI, Li L, Borland R, Yong HH, Omar M, Awang R, … Hammond D. Stronger pack warnings predict quitting more than weakers ones: finding from the ITC Malaysia and Thailand surveys. Tobacco Induced Diseases. 2013;11:1–9. doi: 10.1186/1617-9625-11-20. (available at: http://www.tobaccoinduceddiseases.com/content/11/11/20) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong GT, Hammond D, Hitchman SC. The impact of pictures on the effectiveness of tobacco warnings. Bulletin of the World Health Organization. 2009;87:640–643. doi: 10.2471/BLT.09.069575. doi:610.2471/BLT.2409.069575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D. Health warning messages on tobacco products: a review. Tobacco Control. 2011;20:327–337. doi: 10.1136/tc.2010.037630. doi:310.1136/tc.2010.037630. [DOI] [PubMed] [Google Scholar]
- ITC Project. [accessed 21 March 2014];ITC SEA Technical Report Wave 1 (2005) 2010 Available at: http://www.itcproject.org/countries/thailand.
- ITC Project. [accessed 21 March 2014];ITC SEA Technical Report Wave 5 (2011–2012) 2013 Available at: http://www.itcproject.org/countries/thailand.
- Li L, Borland R, Fong GT, Jiang Y, Yang Y, Wang L, et al. Smoking-related thoughts and microbehaviours, and their predictive power for quitting: findings from the International Tobacco Control (ITC) China Survey. Tobacco Control. 2014 doi: 10.1136/tobaccocontrol-2013-051384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Borland R, Yong H, Cummings KM, Thrasher JF, Hitchman SC, et al. Longer term impact of cigarette package warnings in Australia compared with the United Kingdom and Canada. Health Educ Res. 2015;30(1):67–80. doi: 10.1093/her/cyu074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Borland R, Yong HH, Sirirassamee B, Hamann S, et al. Impact of Point-of-Sale Tobacco Display Bans in Thailand: Findings from the International Tobacco Control (ITC) Southeast Asia Survey. Int J Environ Res Public Health. 2015;12(8):9508–9522. doi: 10.3390/ijerph120809508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Yong HH, Borland R, Fong GT, Thompson ME, Jiang Y, et al. Reported awareness of tobacco advertising and promotion in China compared to Thailand, Australia and the USA. Tobacco Control. 2009;18(3):222–227. doi: 10.1136/tc.2008.027037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malaysian Government. Control of Tobacco Product (Amendment) Regulations 2008 (Under the Food Act of 1983) Kuala Lumpur: Malaysian Government; 2008. [Google Scholar]
- Partos T, Borland R, Thrasher J, Li L, Yong HH, O’Connor R, Siahpush M. The predictive utility of micro indicators of concern about smoking: Data from the International Tobacco Control 4-country study. Addictive Behaviors. 2014;39:1235–1242. doi: 10.1016/j.addbeh.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross H, Driezen P, Sirirassamee B, Kin F. Cigarette purchasing behaviour in Thailand and Malaysia: comparative analysis of a semi-monopolistic and a free-market structure. [Comparative Study Research Support, NIH, Extramural Research Support, Non-U S Gov’t] Glob Public Health. 2009;4(6):588–599. doi: 10.1080/17441690903072204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher JF, Hammond D, Fong G, Arillo-Santillán E. Smokers’ reactions to cigarette package warnings with graphic imagery and with only text: a comparison between Mexico and Canada. Salud Publica Mex. 2007;49(Suppl 2):S233–240. doi: 10.1590/s0036-36342007000800013. [DOI] [PubMed] [Google Scholar]
- Thrasher JF, Murukutla N, Pérez-Hernández R, Alday J, Arillo-Santillán E, Cedillo C, Gutierrez JP. Linking mass media campaigns to pictorial warning labels on cigarette packages: a cross-sectional study to evaluate effects among Mexican smokers. Tobacco Control. 2013;22(e1):e57–e65. doi: 10.1136/tobaccocontrol-2011-050282. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Guidelines for implementation of Article 11 of the WHO Framework Convention on Tobacco Control (Packaging and labelling of tobacco products) [Accessed June 26, 2013];2008a Available at: http://www.who.int/fctc/guidelines/article_11.pdf.
- World Health Organization. The MPOWER package. Geneva: World Health Organization; 2008b. WHO report on the global tobacco epidemic, 2008. [Google Scholar]
- Yong H, Borland R, Hammond D, Sirirassamee B, Ritthiphakdee B, Awang R, … Fong GT. Levels and correlates of awareness of tobacco promotional activities among adult smokers in Malaysia and Thailand: findings from the International Tobacco Control Southeast Asia (ITC-SEA) Survey. Tob Control. 2008;17(1):46–52. doi: 10.1136/tc.2007.021964. [DOI] [PubMed] [Google Scholar]
- Yong H, Fong GT, Driezen P, Borland R, Quah ACK, Sirirassamee B, … Omar M. Adult Smokers’ Reactions to Pictorial Health Warning Labels on Cigarette Packs in Thailand and Moderating Effects of Type of Cigarette Smoked: Findings From the International Tobacco Control Southeast Asia Survey. Nicotine & Tobacco Research. 2013;15(8):1339–1347. doi: 10.1093/ntr/nts241. [DOI] [PMC free article] [PubMed] [Google Scholar]