Abstract
Increasing the energy density (ED) and portion size of foods promotes additional energy intake, but the effect of similar changes in milk is unknown. Using a crossover design, we tested the effect of varying the ED and portion size of milk served with lunch on preschool children's intake. Lunch was served in childcare classrooms on 4 days to 125 children aged 3-5 y (67 boys; 58 girls). Across the meals, milk was varied in ED (lower-ED [1% fat]; higher-ED [3.25% fat]) and portion size (100% [183 g]; 150% [275 g]). Foods in the meal were not varied; children ate as much of the meal as they wanted. Serving higher-ED milk did not affect milk intake by weight, but increased energy intake from milk by 31±2 kcal compared to serving lower-ED milk (P<0.0001). Serving the 150% portion of milk increased milk intake by 20±3 kcal compared to serving the 100% portion (P<0.0001). Increases in both ED and portion size combined to increase milk intake by 49±4 kcal (63%; P<0.0001). Across all children, food intake decreased when higher-ED rather than lower-ED milk was served, but meal energy intake (food+milk) did not change significantly. This response varied by sex: for boys, serving higher-ED milk decreased food intake by 43±8 kcal (P<0.0001) but did not affect meal energy intake, while for girls, higher-ED milk did not reduce food intake so that meal energy intake increased by 24±10 kcal (P=0.03). Thus, boys adjusted food intake in response to changes in ED of milk consumed with lunch, but girls did not. Serving milk in larger portions promotes intake of this nutrient-dense beverage, but the effects of milk ED on meal intake vary between children.
Keywords: children, milk, portion size, energy density, energy intake, eating behavior
Introduction
As an important component of children's diets, milk provides essential nutrients and is a substantial contributor to the daily energy intake of 2- to 18-year-olds (Keast, Fulgoni, Nicklas, & O'Neil, 2013; Robson, Khoury, Kalkwarf, & Copeland, 2015). One study reported that 2- to 18- year-old children consumed 7% of their daily energy from milk (Keast, Fulgoni, Nicklas, & O'Neil, 2013). Higher consumption of most types of fluid milk in childhood (3 to 10 years of age) has been found to protect against excess adiposity and obesity later in adolescence (Bigornia et al., 2014; Hasnain, Singer, Bradlee, & Moore, 2014; Zheng et al., 2015). However, other population-level studies suggest that children who consume higher-energy-dense milk (2% fat or greater) may be at risk for excess energy intake compared to those who consume lower-energy-dense milk (Huh, Rifas-Shiman, Rich-Edwards, Taveras, & Gillman, 2010; O'Connor, Yang, & Nicklas, 2006; Poti, Slining, & Popkin, 2013; Rehm, Drewnowski, & Monsivais, 2015; Wang, Ludwig, Sonneville, & Gortmaker, 2009). In response, various organizations, including the Child and Adult Care Feeding Program and the American Academy of Pediatrics, encourage milk consumption, but recommend that children two years and older consume lower-energy-dense milk (skim [0% fat] and low-fat [1% fat] milk) in age-appropriate portions (Australian Government Department of Health and Ageing, 2009; U.S. Department of Agriculture, Food and Nutrition Service, 2016; Health Canada, 2011; American Academy of Pediatrics Committee on Nutrition, 2014; U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2016). Even though these recommendations are widely adopted and milk is a large part of children's diets, little is known about how changing milk energy density (ED) or portion size influences intake at a meal. To test this, we systematically varied the milk served with a typical meal in preschool children's usual childcare environment.
Studies have shown that both the ED and portion size of foods can influence preschool children's energy intake at a meal (Leahy, Birch, Fisher, et al., 2008a; Mooreville et al., 2015; Rolls, Engell, & Birch, 2000; Spill, Birch, Roe, & Rolls, 2011), but it is unclear whether variations in milk have a similar effect. Previous controlled studies have focused on chocolate milk because of its increased energy and sugar content; results showed that serving higher-ED chocolate milk substantially increased both milk intake and total energy intake at a meal compared to lower-ED unflavored milk (Wilson, 1991, 1994, 2000). Chocolate milk, however, is highly palatable and is not typically served in childcare centers; whereas, unflavored milk is offered on a daily basis and is available in lower-ED and higher-ED versions that are similar in palatability (Kling, Roe, Keller, & Rolls, 2016). In a previous study, we found that increasing the ED and portion size of all items in a meal (including unflavored milk) increased the amount of energy consumed from both food and milk (Kling et al., 2016). Varying the ED and portion size of just the milk at a meal, however, has not been studied and thus the effects on meal energy intake are not known. Examining how the ED and portion size of milk influences intake will further our understanding of how simple changes to foods and beverages can improve children's diets.
In studies of satiety, preschool children have been shown to compensate for variations in the ED of solid or liquid preloads by adjusting energy intake at a subsequent meal (Birch & Deysher, 1985; Birch, McPhee, Steinberg, & Sullivan, 1990; Cecil et al., 2005). Moreover, one study found that serving low-fat milk with breakfast decreased lunch intake compared to serving juice with a similar ED. (Mehrabani et al., 2015). This suggests that milk may have a greater effect on satiety than that of other beverages of similar ED (Mehrabani et al., 2015; Onvani, Haghighatdoost, Surkan, & Azadbakht, 2016). Adjustments of intake in response to changes in food properties can also differ between individuals; for example, males have been shown to be more accurate at compensating for the energy content of liquid preloads than females in both childhood and adulthood (Davy, Van Walleghen, & Orr, 2007; Faith et al., 2012; Johnson & Birch, 1994; Ranawana & Henry, 2010). These preloading studies suggest that preschool children can adjust their intake at a subsequent meal when the properties of a single item are varied; however, the results may not generalize to a satiation paradigm that represents a typical eating context where beverages are served simultaneously with a meal rather than as a preload. In studies of satiety, the delay between the preload and subsequent meal allows sensory and nutrient signals to influence fullness and subsequent intake; whereas, within a meal the sensory properties may have a larger influence than nutrient signals (Camps, Mars, de Graaf & Smeets, 2016). Thus, the compensatory responses seen in studies of satiety may not be observed in studies of satiation. Since children are frequently served milk with their meals, investigating how increasing milk ED or portion size influences intake within a meal would help determine whether this puts children at risk for overconsumption of energy.
The primary aim of this study was to examine the effects of varying the ED and portion size of unflavored milk served with a meal on preschool children's milk and food intake. Using a 2-by-2 crossover design, we systematically varied the ED and portion size of milk served with lunch in childcare centers. We hypothesized that increasing the portion size and ED of milk would increase children's milk intake as well as meal energy intake, consistent with previous research showing that increasing the portion size or ED of a single item at a meal led to higher energy intake (Fisher, Liu, Birch, & Rolls, 2007; Leahy, et al., 2008a; Rolls et al., 2000). To investigate whether the effects on intake varied by sex, age, or other child characteristics, we tested a larger sample than in previous studies of the effects of beverage portion size or ED on children's intake (Kral, Remiker, Strutz, & Moore, 2014; Leahy, Birch, & Rolls, 2008c; Norton, Poole, & Raynor, 2015; Wilson, 1991, 1994, 2000). Determining how variations in the portion size and ED of nutrient-dense milk affect preschool children's eating behavior will increase the understanding of environmental factors that influence intake, aiding in the development of practical strategies to counter these effects.
METHODS AND PROCEDURES
Experimental design
A within-subjects crossover design was used to evaluate the effect of increasing the ED and portion size of milk on preschool children's lunch intake. On 1 day a week for 4 weeks, the experimental meal was served to children in their classrooms at 4 childcare centers. Across the 4 meals, the milk was varied in ED (100% [1%-fat milk] or 142% [3.25%-fat milk]) and portion size (100% or 150%). The 100% milk is also referred to as low-fat or semi-skimmed milk and the 142% milk is also referred to as whole or full-cream milk. The milk was served with an unvaried meal of common foods and children could eat as much or as little of the milk and foods as they wanted. The order of the 4 conditions was counterbalanced across classrooms using Latin squares, and classrooms were randomly assigned one of the condition sequences. Since the children were only served 1 experimental meal per week, they never saw the different milks together. The children's height, weight, and liking and preference of the lower-ED and higher-ED types of milk were assessed after the final experimental meal.
Participants
Children were recruited by distributing letters to parents with 3- to 6-year-old children enrolled at 4 childcare centers near University Park, PA: the Bennett Family Center, Daybridge Child Development Center, Child Care Center at Hort Woods, and Step by Step School for Early Learning. Parents provided written consent for the participation of their child in the study as well as their own participation in completing questionnaires. Children with an allergy or intolerance to the foods or milk being served were not eligible to participate. Neither parents nor children were informed about the purpose of the study. All procedures were reviewed and approved by The Pennsylvania State University Office for Research Protections. This trial is registered at ClinicalTrial.gov (Registration Number: NCT02755558) and follows the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
A power analysis was conducted to determine the number of children needed for the study, based on previous research in a similar population with similar foods (Kling et al., 2016; Leahy, et al., 2008c; Spill et al., 2011). A 7.5% (15 kcal) difference in meal energy intake as a result of varying the properties of one item (milk) was considered the minimum difference to be detected. A 15 kcal difference is equivalent to 36 g of the lower-ED milk or 25 g of the higher-ED milk. A power analysis showed that a sample size of 60 children would allow detection of this difference at a significance level of 0.05 and power of 80%. To explore the effect of individual characteristics on the primary outcome, a larger sample size was enrolled.
Experimental menu and meal procedures
Experimental menu
The experimental meals consisted of the milk and unvaried portions of macaroni and cheese, chicken, broccoli, and bananas, as described in Table 1. Across the meals, the milk was served at 2 levels of ED (lower-ED [0.42 kcal/g; 1% fat] and higher-ED [0.61 kcal/g; 3.25% fat]) and 2 levels of portion size (100% [183 g; 6 fl. oz.] and 150% [275 g; 9 fl. oz.]). The foods in the meal were frequently served by the participating childcare centers and were well-accepted by preschool children in previous studies (Kling et al., 2016; Leahy, Birch, & Rolls, 2008b; Leahy, et al., 2008c; Spill et al., 2011). The participating childcare centers usually serve lower-ED, 1% fat milk. All milks and foods were commercially available. The milk met the minimum serving size requirements of the Child and Adult Care Food Program (U.S. Department of Agriculture, Food and Nutrition Service, 2016), which are to serve 3- to 5-year-old children at least 6 fl. oz. of milk. Both the 100% and 150% portions of non-compulsory milk were served chilled in the same small, clear plastic container with a straw to encourage consumption. To reduce the novelty of the milk container, one week prior to the start of the study, children were served 229 g of reduced-fat milk (2% fat; 0.50 kcal/g) in the container along with the lunch provided by the childcare center. The reduced-fat milk (2%) in a 125% portion size was served to prevent exposure to the experimental manipulations. The portions of the foods in the test meal were based on preschool children's intake in previous studies (Kling et al., 2016; Leahy, et al., 2008a; Leahy, Birch, et al., 2008b, 2008b; Spill et al., 2011). The foods in the test meal provided approximately 41% of energy as carbohydrates, 24% as protein, and 35% as fat. The lower-ED milk provided 47% of energy as carbohydrates, 32% as protein, and 21% as fat; the higher-ED milk provided 31% of energy as carbohydrates, 21% as protein, and 48% as fat.
Table 1.
Amounts of items and composition of meals served to 125 preschool children
|
|
Lower-energy-dense milk (100%)1 |
Higher-energy-dense milk (142%)2 |
||||||
|---|---|---|---|---|---|---|---|---|
|
|
100% Milk portion size (6 fl. oz.) |
150% Milk portion size (9 fl. oz.) |
100% Milk portion size (6 fl. oz.) |
150% Milk portion size (9 fl. oz.) |
||||
| g | kcal | g | kcal | g | kcal | g | kcal | |
| Milk3 | 183 | 77 | 275 | 115 | 183 | 112 | 275 | 167 |
| Food | 430 | 542 | 430 | 542 | 430 | 542 | 430 | 542 |
| Macaroni and cheese (1.49 kcal/g)4 | 150 | 202 | 150 | 202 | 150 | 202 | 150 | 202 |
| Chicken nuggets (1.68 kcal/g)5 | 120 | 223 | 120 | 223 | 120 | 223 | 120 | 223 |
| Broccoli (0.57 kcal/g)6 | 80 | 46 | 80 | 46 | 80 | 46 | 80 | 46 |
| Bananas (0.89 kcal/g)7 | 80 | 71 | 80 | 71 | 80 | 71 | 80 | 71 |
| Total meal | 613 | 619 | 705 | 657 | 613 | 653 | 705 | 709 |
| Carbohydrates | 64.8 | 259 | 69.5 | 278 | 64.6 | 258 | 69.0 | 276 |
| Protein | 39.0 | 156 | 42.1 | 168 | 38.7 | 155 | 41.5 | 166 |
| Fat | 22.7 | 204 | 23.5 | 211 | 26.7 | 240 | 29.7 | 267 |
1% fat; 0.42 kcal/g
3.25% fat; 0.61 kcal/g
Giant Food Stores Milk, Foodhold U.S.A LLC, Landover, MD, USA.
Stouffer's Macaroni and Cheese, Nestle U.S.A. Inc., Solon OH, USA.
Gluten Free Breaded Chicken Breast Nuggets, Bell & Evans, Fredericksburg, PA, USA.
Petite Broccoli Florets, Hanover Foods Corporation, Hanover, PA, USA; Unsalted Whipped Butter, Land O'Lakes Inc., Arden Hills, MN, USA; Molly McButter Butter Flavor Sprinkles, B&G Foods Inc., Parsippany, NJ, USA.
Chiquita Brands LLC, Charlotte, NC, USA.
Meal procedures
Children were served the meal in their classrooms in the childcare centers and at their regularly scheduled lunchtime, and consumed as much or as little as they wanted of the milk and foods. Children ate at tables with three to six children and one adult, which is standard practice at the childcare centers; the adults were teachers who did not know the purpose of the study. The foods and milk were pre-portioned into dishware and set at each child's place at the table just before the children were seated, which differed from the usual family-style service at the childcare centers. Before the first experimental meal, researchers explained to the children that they could eat as much or as little as they wanted, but could not request more of any food or milk. During each meal, adults at the tables were instructed to redirect conversations about food-related topics to minimize peer influence on children's intake. After all children had finished lunch, researchers returned any dropped foods to the correct plate or bowl and recovered any spilled milk with paper towels. To determine the amount consumed, all foods and the milk were weighed before and after the meal in a separate room out of the children's view. Weights of food and milk were recorded to the nearest 0.1 g using digital scales (Mettler-Toledo PR5001 and XS4001S; Mettler-Toledo, Columbus, OH). Energy and macronutrient intakes were calculated using information from food manufacturers and a standard food composition database (U.S. Department of Agriculture & Agricultural Research Service, 2015). Children who did not participate in the study sat at tables out of participating children's view and were served the scheduled lunch menu of the childcare center.
Assessments
Food liking and preference assessments
Liking and preference for the milks was assessed during an individual session with each child using a 5-point cartoon face scale (Figure 1) based on a 3-point version used in previous research (Birch, 1979). The child was seated at a table with the 5 cartoon faces and was instructed on using them to indicate whether a food was “super yummy,” “yummy,” “just okay,” “yucky,” or “super yucky.” After instruction, samples of the two types of milk were presented to the child one at a time; foods served in the test meal were not assessed since the foods were not varied across experimental conditions. The order of presenting the samples of the two milks was randomly assigned. The child was asked to taste the milk and indicate his or her liking for it by pointing to the appropriate cartoon face. After the child rated both milks, the child was asked to “point to the milk you like the very best” to indicate his or her preference between the two types of milk (Birch, 1979). Children's liking for the milks was assessed within 2 weeks after the final experimental meal. Food liking assessments were completed by 107 (86%) of the children; the remaining children were absent or declined to participate.
Figure 1.
Five-point cartoon face scale used to rate liking for the milks (faces from left to right represent “super yucky,” “yucky,” “just okay,” “yummy,” and “super yummy”).
Body weight and height
Body weight was measured to the nearest 0.1 kg using a portable digital scale (Seca Onda model 843; Seca Corporation, Hanover, MD). Height was measured in duplicate to the nearest 0.1 cm using a portable stadiometer (model 214; Seca Corporation, Hanover, MD). Body weight and height were used to calculate body size parameters (sex-specific BMI-for age-percentiles and z-scores) using a software program based on nationally representative data (U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2015). Children's weight and height were assessed within 2 weeks after the final test meal. One hundred and fifteen children (92%) completed the assessments for height and weight; the remaining children were absent or declined to participate.
Parental questionnaires
Parents were asked to complete 4 questionnaires about parent and child characteristics and behaviors related to the eating environment. The 35-item Child Eating Behaviour Questionnaire (CEBQ) evaluates 8 subscales that relate to eating styles and behaviors of the child (Carnell & Wardle, 2007). The 31-item Child Feeding Questionnaire (CFQ) assesses 7 subscales that measure feeding practices and perceived weight concerns (Kaur et al., 2006). For these CFQ and CEBQ subscales, the parent rated each item on a 5-point scale; for analyses, a mean score was calculated across all the items in a given subscale. The 56-item food frequency questionnaire assessed the availability and frequency of parent and child consumption of various beverages at home. The 16-item demographic questionnaire assessed family demographics and child health. Parents of 113 children (90%) completed the 4 questionnaires.
Statistical analysis
Data analyses were conducted using a mixed linear model with repeated measures in SAS statistical software (SAS Institute, Inc., Cary, NC). The primary outcomes evaluated by the model were intake of milk by weight (g) and energy (kcal), intake of food at the meal by weight (g) and energy (kcal), and total meal intake (food + milk) by weight (g) and energy (kcal). The fixed factors in the model were milk portion size (100% and 150%), milk ED (100% and 142%), study week, and classroom. The interaction between portion size and ED was tested and then removed from the model if not significant. Participants were treated as a random factor. For outcomes with significant effects, the Tukey-Kramer method was used to adjust significance levels for multiple pairwise comparisons between means. It was pre-determined that children's data would be excluded if at 2 or more of the 4 experimental meals they were absent or consumed less than 20 g of milk (approximately 10% of the smallest portion). In addition, using the procedure described by Littell et al., the data were examined for individual children whose intake was influential on the main outcomes in the mixed model, but no children met the criteria (Littell, Milliken, Stroup, Wolfinger, & Schabenberger, 2006).
Analysis of covariance with a mixed linear model was used to assess the influence of continuous participant characteristics, (age, body weight, height, BMI-for-age percentile, BMI z-score, CFQ subscales, CEBQ subscales, and milk availability and consumption at home) on the relationship between the experimental factors and intake. Categorical subject characteristics (sex and ratings of liking for the milk) were tested as factors in the models. All participant characteristics were tested in one model, and then removed from the model if not significant. Ordinal repeated measures logistic regression was used to compare the lower-ED and higher-ED milks for differences in the distribution of children's liking ratings (from “super yummy” to “super yucky”); results are reported as odds ratios with 95% confidence levels. T-tests were used to evaluate differences between boys and girls in age, body weight, height, BMI percentile, and BMI z-score. A chi-square test was used to determine whether there were differences in the proportion of boys and girls who consumed all of their milk. Data are reported as means ± standard errors, and results were considered significant at P<0.05.
RESULTS
Subject characteristics
A total of 143 children from 10 classrooms at the 4 childcare centers were enrolled in the study. Eight children (6%) were excluded from the analysis because they were absent for 2 or more of the 4 experimental meals. An additional 10 children (7%) were excluded from the analysis because of failure to meet the predetermined criterion of minimum milk intake (less than 20 g at 2 or more of the 4 experimental meals). Thus, intake data were analyzed for 125 children (67 boys and 58 girls; Table 2).The children had a mean (± SEM) age of 4.2 ± 0.1 years (range: 3.1-6.0 years) and mean sex- and age-specific percentile for BMI of 53.6 ± 2.4 (range: 0.0-97.8). Eight children (8%) were classified as overweight or obese (Barlow, 2007). The sample of children was 75% white, 15% Asian, 3% black or African American, and 7% of mixed or another race; 8% were of Hispanic or Latino origin. Based on the 112 parents (90%) who provided family information, household incomes and education levels were above average: 72% of households had an annual income above $50,000 and 92% of mothers and 86% of fathers had a Bachelor's degree or higher. According to parental report, 8% of children consumed only 0%-fat milk at home on a daily basis, 16% consumed 1%-fat milk, 25% consumed 2%-fat milk, 12% consumed 3.25%-fat milk, and 19% consumed multiple types of milk. Lastly, 20% of children did not consume these types of milk at home.
Table 2.
Characteristics of 125 preschool children in a study of the effects of varying milk energy density and portion size on meal intake
| Boys (n=67) |
Girls (n=58) |
|||||
|---|---|---|---|---|---|---|
| Characteristic1 | n | Mean ± SEM | Range | n | Mean ± SEM | Range |
| Age (y) | 67 | 4.2±0.1 | 3.1–6.0 | 57 | 4.1±0.1 | 3.2–5.3 |
| Weight (kg) | 57 | 17.9±0.3 | 13.4–22.8 | 58 | 16.5±0.3 | 12.5–22.9 |
| Height (cm) | 57 | 106.0±0.8 | 92.5–118.3 | 58 | 102.9±0.8 | 89.5–116.8 |
| BMI z-score2 | 57 | 0.12±0.13 | −2.52–2.02 | 57 | 0.04±0.11 | −3.44–1.19 |
| Sex-specific BMI-for-age percentile2 | 57 | 54.8±3.6 | 0.6–97.8 | 57 | 52.4±3.2 | 0.0–97.2 |
The mean for girls was not significantly different from the mean for boys for any of the variables according to a T-test (all P>0.33)
Body weight and height were used to calculate body size parameters (BMI z-scores and sex-specific BMI-for age-percentiles) using a software program based on nationally representative data (U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2015).
Intakes by weight and energy
Milk intake by weight and energy
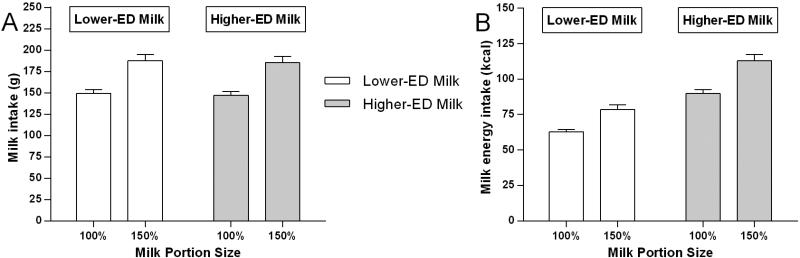
There was an effect of milk portion size (F(1,256)=60.77, P<0.0001) but not ED (F(1,296)=0.16, P=0.69) on the weight of milk consumed (Figure 2A). Compared to the 100% milk portion conditions, milk intake was 38 ± 5 g (1.25 ± 0.2 fl. oz.; 26%) greater in the 150% conditions (F(1,256)=60.77, P<0.0001; Table 3). A similar weight was consumed of the lower-ED and higher-ED milk (F(1,296)=0.16, P=0.69). Since portion size but not ED affected the weight of milk consumed, there were independent effects of milk portion size (F(1,348)=64.55, P<0.0001) and ED (F(1,348)=158.94, P<0.0001) on energy consumed from milk (Figure 2B). Compared to the 100% milk portion conditions, energy intake from milk was 20 ± 3 kcal (27%) greater when children were served the 150% conditions (F(1,348)=64.55, P<0.0001). A 42% increase in milk ED led to a 31 ± 2 kcal or 44% increase in energy consumed from milk (F(1,348)=158.94, P<0.0001). The effects of milk portion size and ED combined to increase energy intake from milk by 49 ± 4 kcal or 63% (t(348)=−14.81, P<0.0001) when children were served the 150% portion of the higher-ED milk compared with the 100% portion of the lower-ED milk.
Figure 2.
Mean (±SEM) milk intake (g and kcal) at lunch by milk portion size and energy density (ED) in 125 preschool children. Figure 2A: There was an effect of portion size (F(1,256)=60.77, P<0.0001) but not energy density (F(1,296)=0.16, P=0.69) on milk intake by weight. Across both types of milk, intake was greater in the 150% portion size conditions than in the 100% conditions (P<0.0001). Figure 2B: There were independent effects of portion size (F(1,348)=64.55, P<0.0001) and energy density (F(1,348)=158.94, P<0.0001) on milk energy intake. Across both types of milk, milk energy intake was greater in the 150% portion size conditions than in the 100% conditions (P<0.0001). Across portion size conditions, serving the higher-ED milk led to an increase in energy intake from milk (P<0.0001).
Table 3.
Intake of 125 preschool children in a study of the effects of varying milk energy density and portion size on meal intake 1
| Lower-energy-dense milk | Higher-energy-dense milk | Significant effects2 | |||
|---|---|---|---|---|---|
| 100% Portion Size (n=120) | 150% Portion Size (n=118) | 100% Portion Size (n=116) | 150% Portion Size (n=119) | ||
| Total meal intake (g) | 349±8 | 388±10 | 333±8 | 358±10 | PS, ED3 |
| Milk (g) | 149±4 | 187±8 | 147±4 | 185±7 | PS4 |
| Food intake (g) | 200±6 | 200±7 | 186±7 | 173±7 | ED5 |
| Total meal energy intake (kcal) | 322±8 | 337±10 | 328±9 | 337±10 | --6 |
| Milk (kcal) | 63±2 | 79±3 | 90±3 | 113±4 | PS, ED |
| Food intake (kcal) | 260±8 | 259±9 | 238±9 | 224±9 | ED |
| Energy density of food (kcal/g) | 1.31±0.02 | 1.29±0.02 | 1.29±0.02 | 1.30±0.02 | -- |
| Energy density of food and milk (kcal/g) | 0.92±0.01 | 0.88±0.02 | 0.98±0.01 | 0.94±0.01 | PS, ED |
| Carbohydrate intake (g) | 36.4±1.0 | 38.5±1.1 | 33.8±1.1 | 33.2±1.0 | ED |
| Protein intake (g) | 20.2±0.6 | 21.2±.7 | 18.3±0.6 | 18.8±0.6 | ED |
| Fat intake (g) | 11.5±0.4 | 11.9±0.4 | 14.0±0.4 | 15.0±0.5 | PS, ED |
All values are mean ± SEM
Mixed linear models were used to test the effects of milk portion size and energy density on all outcomes. Results were considered significant at P<0.05.
PS, ED, There were significant independent effects of milk portion size (all P<0.04) and energy density (all P<0.003) on the outcome.
PS, There was a significant independent effect of milk portion size (all P<0.0001) on the outcome.
ED, There was a significant independent effect of milk energy density (all P<0.0001) on the outcome.
--, There were no significant effects of milk portion size or energy density on the outcome.
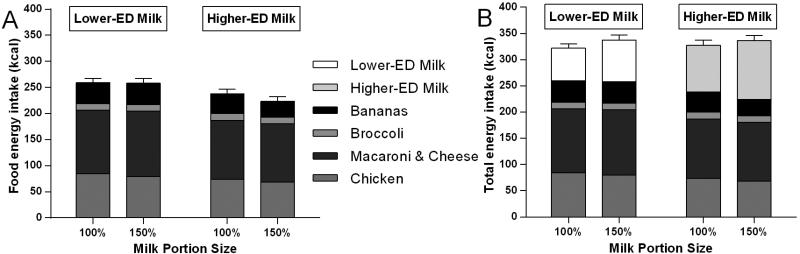
Food intake by weight and energy
There was an effect of milk ED (F(1,323)=19.92, P<0.0001) but not milk portion size (F(1,323)=3.16, P=0.07) on the weight of food consumed from the test meal. A similar weight of food was consumed when the children were served the 100% and 150% portions of milk (F(1,323)=3.16, P=0.07, Table 3). None of children consumed all of the food at any meal (i.e., within 20 g of the amount served). Across all children, serving higher-ED milk led to a 19 ± 5 g or 9% reduction in the weight of food consumed compared to when the lower-ED milk was served (F(1,323)=19.92, P<0.0001). Correspondingly, there was an effect of milk ED (F(1,323)=22.93, P<0.0001) but not portion size (F(1,322)=2.74, P=0.10) on energy consumed from food (Figure 3A). When the 100% and 150% portions were served, a comparable amount of energy was consumed from food (F(1,322)=2.74, P=0.10). Serving higher-ED milk led to a 26±6 kcal or 10% reduction in energy intake from food compared to serving lower-ED milk (F(1,323)=22.93, P<0.0001).
Figure 3.
Mean (±SEM) food energy intake and total meal energy intake at lunch by milk portion size and energy density (ED) in 125 preschool children. Figure 3A: There was an effect of energy density (F(1,323)=22.93, P<0.0001) but not portion size (F(1,322)=2.74, P=0.10) on food energy intake. Across portion size conditions, increasing milk ED led to a 26±6 kcal or 10% reduction in energy consumed from food.. Figure 3B: There was no effect of milk portion size (F(1,314)=2.88, P=0.10) or ED (F(1,315)=0.44, P=0.51) on total energy intake at the meal.
Total meal intake by weight and energy
There was an effect of both milk portion size (F(1,343)=24.44, P<0.0001) and ED (F(1,343)=11.41, P=0.0008) on total meal intake by weight. Compared to the 100% milk portion conditions, total meal intake (food + milk) was 9% (30 ± 7 g) greater in the 150% conditions (F(1,343)=24.44, P<0.0001; Table 3). Serving higher-ED milk led to a 21±6 g or 6% reduction in total intake by weight compared to when lower-ED milk was served (F(1,343)=11.41, P=0.0008). However, there was no effect of milk portion size (F(1,314)=2.88, P=0.10) or ED (F(1,315)=0.44, P=0.51) on total energy intake at the meal (Figure 3B). Total energy intake did not differ between the meals with 100% and 150% milk portion sizes (F(1,314)=2.88, P=0.10) or meals with the lower-ED and higher-ED milks (F(1,315)=0.44, P=0.51). Therefore, across all children, varying milk portion size or ED did not affect total energy intake at a meal.
Meal macronutrient intake and energy density
Serving higher-ED milk led to 2.9 ± 0.3 g increase in fat intake (F(1,308)=120.67, P<0.0001), while carbohydrate intake decreased by 3.8 ± 0.8 g (F(1,329)=30.33, P<0.0001) and protein intake decreased by 2.0 ± 0.4 g (F(1,327)=26.20, P<0.0001), compared to serving lower-ED milk. Increasing milk portion size only affected fat intake, which was 0.6 ± 0.3 g higher in the 150% portion conditions than 100% conditions (F(1,332)=5.20, P=0.02). The ED of the total meal was increased by serving the higher-ED milk (F(1,347)=34.50, P<0.0001; Table 3), but was decreased by serving the larger portion of milk (F(1,346)=18.33, P<0.0001).
Milk liking and preference ratings
The results of the liking and preference assessments indicate that the children rated the two types of milk similarly. There was no difference in the distribution of liking ratings between the lower-ED and higher-ED milk; the odds ratio was not different from 1 (P=0.32; 1.30; 95% confidence interval 0.78 – 2.18). Both types of milk were well-liked; children chose “super yummy” or “yummy” ratings in 79% of the assessments of both the lower-ED and higher-ED milk. There was no difference between boys and girls in the distribution of liking ratings of the milk (P=0.85; odds ratio 0.18; 95% confidence interval 0.68 – 1.38). The children's liking ratings of the milk did not influence the effects of milk portion size and ED on intake of milk, food, or total meal by weight or energy (all P≥0.26).
Results were similar for children's reported preference for the milk. There was no difference in the distribution of the preference rankings between the lower-ED and higher-ED milk (P=0.69; odds ratio 0.85; 95% confidence interval 0.39 – 1.87). The lower-ED milk was preferred by 52% of children and the higher-ED milk by 48% of children. There was no difference between boys and girls in the distribution of preference rankings (P=0.53; odds ratio 0.18; 95% confidence interval 0.59 – 1.31). In addition, the children's preference rankings of the milk did not influence the effects of milk portion size and ED on intake of milk, food, or the total meal by weight or energy (all P≥0.18).
Influence of subject characteristics
As shown in Table 4, the children's sex differentially influenced the effect of milk ED on the weight and energy consumed from food (F(1,323)=12.03, P=0.0006; F(1,324)=15.86; P<0.0001) and the total meal (F(1,344)=5.98, P=0.02; F(1,315)=8.66, P=0.004). When the higher-ED milk was served rather than the lower-ED milk, boys showed a compensatory reduction in food intake of 43 ± 8 kcal (16%; F(1,186)=41.46, P<0.0001), whereas for girls, food intake was not affected by milk ED (F(1,159)=0.74, P=0.39). Thus, when the energy content of the milk was included, boys’ total energy intake at the meal did not differ by milk ED (F(1,186)=3.34, P=0.07), similar to the finding for the entire sample; for girls, however, serving higher-ED milk led to a modest increase in meal energy intake of 24 ± 10 kcal (7%; F(1,158)=5.31, P=0.03). There was no influence of the children's sex on the relationship between milk portion size and intake of food or the total meal by weight or energy (all P>0.20).
Table 4.
Intake by sex, energy density, and portion size in a study of the effects of varying milk energy density and portion size on the weight and energy consumed from a meal served to 125 preschool children1
| Boys (n=67) | Girls (n=58) | Significance of interaction |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lower-energy- dense milk |
Higher-energy- dense milk |
Lower-energy- dense milk |
Higher-energy- dense milk |
|||||||
| 100% Portion Size |
150% Portion Size |
100% Portion Size |
150% Portion Size |
100% Portion Size |
150% Portion Size |
100% Portion Size |
150% Portion Size |
Effect of sex*milk portion size |
Effect of sex*milk energy density |
|
| Total meal intake (g) | 352±11 | 384±14 | 322±12 | 341±13 | 346±10 | 393±14 | 346±11 | 378±14 | NS2 | P=0.02 |
| Milk intake (g) | 156±6 | 183±10 | 155±5 | 184±10 | 142±7 | 193±12 | 138±7 | 188±11 | P=0.043 | NS |
| Food intake (g) | 197±9 | 201±10 | 167±10 | 157±10 | 204±8 | 200±9 | 208±8 | 191±9 | NS | P<0.0001 |
| Total meal energy intake (kcal) | 320±13 | 338±14 | 312±14 | 320±14 | 324±10 | 336±13 | 346±11 | 357±14 | NS | P=0.003 |
| Milk energy intake (kcal) | 65±2 | 77±4 | 94±3 | 112±6 | 60±3 | 81±5 | 84±4 | 114±6 | P=0.033 | NS |
| Food energy intake (kcal) | 255±12 | 261±14 | 218±13 | 208±13 | 265±10 | 256±13 | 261±10 | 243±12 | NS | P=0.0006 |
All values are mean ± SEM
NS, non-significant (P<0.05)
The interaction was significant, but none of the pairs of means were significantly different after adjustment for multiple comparisons (P>0.07).
Analysis of covariance showed that the relationship between the experimental factors (portion size and ED) and outcomes (milk intake, food intake, and total meal intake all by weight and energy) was not influenced by children's age, height, weight, sex-specific BMI-for-age percentile, BMI z-score, the 8 subscales of the Child Eating Behaviour Questionnaire (CEBQ), the 7 subscales of the Child Feeding Questionnaire (CFQ), and milk intake and availability at home as assessed by a food frequency questionnaire. In addition, the relationship between the portion size or ED and the outcomes (milk intake, food intake, and total meal intake all by weight and energy) did not differ between the children who completed the liking assessments, participated in anthropometric measurements, or had parents who submitted the questionnaires and the children who did not.
DISCUSSION
Variations in the energy density and portion size of milk had significant effects on preschool children's milk intake at a meal. Energy intake from milk was independently affected by both milk portion size and ED; when these two properties were increased simultaneously, they combined to increase milk intake by 49 ± 4 kcal or 63%. Serving meals with higher-ED milk decreased overall food intake compared to serving lower-ED milk, and total meal energy intake was not influenced by either milk ED or portion size across all children. However, this response varied by sex; for boys, serving higher-ED milk decreased food energy intake, but did not affect total energy intake compared to serving lower-ED milk. In contrast, for girls, higher-ED milk did not lead to a compensatory reduction in food intake and additional energy was consumed at the meal. Both the lower-ED and higher-ED types of milk were well accepted, as indicated by children's ratings of liking and the consumption of a similar weight of milk when served the same portions. These results show that larger portions of milk can be served to increase intake of this nutrient-dense beverage, but the influence of milk ED on intake differs between boys and girls.
Both ED and portion size have robust effects on children's food intake (Leahy, et al., 2008a; Rolls et al., 2000; Spill et al., 2011); however, the few studies that investigated the combination of these factors focused on foods, not beverages, and reported inconsistent effects on intake (Fisher et al., 2007; Kling et al., 2016; Leahy, et al., 2008b; Leahy, 2008a). Two studies found that the effects of increasing the ED and doubling the portion of a main dish or meal were independent and thus combined to influence intake (Fisher et al., 2007; Kling et al., 2016). In comparison, the other study found a significant effect of varying ED but no effect of decreasing the portion of the main dish by 25% (Leahy, et al., 2008b). The non-significant portion size effect in the latter study may have been due to the modest difference between the portions or because the smallest portion was overly large for the children (Leahy, et al., 2008b). In the present study, increasing milk ED and portion size had robust, independent effects that combined to increase the amount of energy consumed from milk. These results along with previous research indicate that ED and portion size can have consistent and substantial effects on children's intake, which is of concern since large portions of energy-dense foods and beverages are readily available and could lead to overconsumption and weight gain.
Young children have been found to respond to variations in ED of a preload by altering their intake at a subsequent meal (Birch & Deysher, 1985; Birch et al., 1990; Cecil et al., 2005). A similar response was seen in the present study; children consumed less food when higher-ED milk was included with the meal than when lower-ED milk was served. This suggests that higher-ED milk promotes greater satiety than lower-ED milk. Even though the higher-ED and lower-ED milks were not rated differently in liking and preference, the children may have responded to differences in sensory properties such as viscosity or creaminess (Bakke, Shehan, & Hayes, 2016; Zahn, Hoppert, Ullrich, & Rohm, 2013), which have been shown to influence satiety and fullness (Mattes & Rothacker, 2001; Zijlstra, Mars, de Wijk, Westerterp-Plantenga, & de Graaf, 2008, Camps, et al., 2016). Sensory characteristics may play a more critical role in studies of satiation, such as the present one, than in studies of satiety (Camps, et al., 2016). Alternatively, the differential response to the lower-ED and higher-ED types of milk may be explained by other mechanisms, such as differences in gastric distension and associated physiological responses of appetite-regulating hormones (Degen et al., 2006). For example, a recent study showed that both the energy density and viscosity of a dairy-based shake influenced gastric emptying (Camps, et al., 2016). The present study is the first to demonstrate that children adjust their intake to account for variations in milk ED within a meal; thus, determining the mechanisms behind this response, such as sensory properties, warrants future research.
Previous research has demonstrated that children's adjustment of energy intake in response to differences in the ED of a food or beverage can vary by individual characteristics. Some studies suggest that such compensation diminishes from 5 to 12 years of age (Cecil et al., 2005; Johnson & Taylor-Holloway, 2006) and is reduced in children with higher body weight or adiposity (Branton et al., 2014; Johnson, 2000; Johnson & Birch, 1994; Kral et al., 2012). The accuracy of children's compensatory response has also been related to child eating behaviors such as satiety responsiveness as well as parental practices such as controlling feeding and use of food as reward (Carnell & Wardle, 2007; Cecil et al., 2005, Remy, Issanchou, Chabanet, Boggio, & Nicklaus, 2005). The present study, in comparison, found no influence of child age, weight, BMI, child eating behaviors, or parental practices on the effect of milk ED on intake of milk, food, or the entire meal. Discrepancies in the results of these studies may be primarily due to research design and sample characteristics; for example, previous studies used a preloading paradigm in which the varied item was served before the test meal (Branton et al., 2014; Carnell & Wardle, 2007; Cecil et al., 2005; Johnson, 2000; Johnson & Birch, 1994; Johnson & Taylor-Holloway, 2006; Kral et al., 2012), whereas in the present study, the varied milk and test meal were served simultaneously. One characteristic that has been found to influence the adjustment of food intake both in the present study and in some previous preloading studies in children and adults is the sex of the individual (Davy et al., 2007; Faith et al., 2012; Johnson & Birch, 1994; Ranawana & Henry, 2010). Compared to females, males tend to have a more accurate compensatory response to variations in the ED of foods or beverages (Davy et al., 2007; Faith et al., 2012; Johnson & Birch, 1994; Ranawana & Henry, 2010), as was found in the present study. Even though multiple studies have reported that males are better than females at adjusting intake for variations in ED, the mechanisms driving this effect have not been elucidated.
The weaker intake regulation of girls compared to boys in response to ED changes may be related to differential parental behaviors or social expectations. One study found that preschool daughters of mothers with restrained or disinhibited eating patterns showed poorer compensation for preload energy than did sons of the same mothers (Johnson & Birch, 1994). This finding indicates that eating behaviors modeled by parents may influence children's compensatory response, and suggests a potential explanation for the sex difference found in the present study. Other behaviors that are not captured by food-specific questionnaires may also explain differences in eating patterns. For example, young girls tend to be compliant to rules and have higher self-control (Francis & Susman, 2009; Kochanska & Aksan, 2006), and thus may be more likely to stay focused on the meal and sit at a table longer than boys. Such characteristics could lead girls to regulate intake more on the basis of environmental feedback (e.g., praise for quietly sitting and eating) than on internal cues of hunger and fullness. Further investigation of the sex differences in intake regulation of preschool children could lead to the identification of specific parent or child behaviors that could be addressed in efforts to prevent childhood obesity.
In contrast to the effect of ED, increasing the portion size of milk by 50% did not lead to a large enough increase in milk energy intake to substantially influence food or total energy intake at a meal. Therefore, caregivers in childcare centers have the option of serving larger portions of milk to promote intake of this important component of children's diets without leading to excess energy intake; however, lower-ED types of milk, such as low-fat (1% milk), should be offered since girls have been shown to consume more total energy from a meal when offered higher-ED milk. This practice could help children meet the daily recommendation for milk intake (DeBoer, Agard, & Scharf, 2015; Robson et al., 2015); if a child receives milk three times a day, as is typical in childcare centers, the effect of increasing the portion size of milk from 6 to 9 fl. oz. could increase dairy intake by more than one-half serving per day. Since milk is a major component of children's diets, the additional energy consumed from larger portions of milk might accumulate over time and promote a positive energy balance and weight gain, and this possibility should be tested in future research. However, serving milk in larger portions promotes intake of this nutrient-dense beverage at a single eating occasion.
A strength of the present study is the large sample of children whose eating behavior was assessed. Only one of the previous studies investigating the effects of beverage portion size or ED with a crossover design included a sample of the same magnitude as the present study (Norton et al., 2015; Wilson, 1991, 1994, 2000). A further strength was that the lunch was served in the children's usual environment, and the variations in milk ED and portion size represented what is commonly served to children. Thus, the setting and the meal were generalizable to a wide range of children. However, the meal was pre-plated instead of served family style, as was usual in the child care centers, which may have influenced intake (Fisher, Rolls, & Birch, 2003). In addition, intake was measured at a single meal and the effect of milk ED and portion size on intake later in the day was not investigated. Epidemiological research suggests that over the longer term, larger portions and higher-ED types of milk could promote energy intake (Onvani et al., 2016; Poti et al., 2013; Rehm et al., 2015; Wang et al., 2009), but experimental studies in children have not systematically investigated this beyond a single meal. Future research should be conducted for longer periods of time with more diverse populations and different types of milk to determine how variations in milk ED and portion size influence short- and long-term intake.
Since milk is a substantial and important component of preschool children's diet (Keast, Fulgoni, Nicklas, & O'Neil, 2013; Robson, Khoury, Kalkwarf, & Copeland, 2015), evidence-based recommendations about the type and amount of milk that preschool children should be offered are of considerable interest. The results of the present study support current advice that lower-ED, 1%-fat milk should be served in preschool settings (U.S. Department of Agriculture, Food and Nutrition Service, 2016). While we found that children, on average, compensated for the additional energy consumed from higher-ED milk, some children, especially girls, consumed more total energy at the meal when served the higher-ED milk rather than lower-ED milk. The findings also showed that providing larger portions of milk promoted intake of this nutrient-dense beverage without affecting energy intake at the meal. This strategy can be easily adapted by caregivers to help children meet recommendations for dairy intake. Further understanding of how the portion size and ED of the milk offered to children influence their long-term intake will help to ensure that the type and amount offered of this nutrient-rich beverage is optimal for children's diets.
ACKNOWLEDGEMENTS
We thank Brittany James, Cara Meehan, Christine Sanchez, Alissa Smethers, Anne Vos, Faris Zuraikat, and undergraduate students in the Laboratory for the Study of Human Ingestive Behavior for assistance with food preparation and data collection. In addition, the support and participation of staff, parents, and students at the Bennett Family Center, The Child Care Center at Hort Woods, Step by Step School for Early Learning, and Daybridge Child Development Center is greatly appreciated. Lastly, we thank Dr. Eric Loken for his insight and assistance with the data analysis.
Supported by USDA National Institute for Food and Agriculture Grant 2011-67001-30117 Program A2121 and NIH Grant R01-DK082580. Statistical assistance was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR000127.
Supported by USDA Grant 2011-67001-30117 and NIH Grant R01-DK082580
Abbreviations
- ED
energy density
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors’ responsibilities were as follows – SMRK: the design of the experiment, collection and analysis of data, and writing of manuscript; LSR: the design of the experiment, analysis of data, and writing of the manuscript; CES: the design of the experiment, collection of data, and writing of the manuscript; and BJR: the design of the experiment and the writing of the manuscript. None of the authors had a personal or financial conflict of interest.
REFERENCES
- Australian Government Department of Health and Ageing Get Up & Grow Health Eating and Physical Activity for Early Childhood Family Book. 2009 Retrieved from http://www.health.gov.au/internet/main/publishing.nsf/Content/F5698F4E9CB73B94CA 257BF000217BF6/$File/HEPA%20-%20B5%20Book%20-%20Family%20Book_LR.pdf.
- American Academy of Pediatrics Committee on Nutrition . In: Pediatric Nutrition. 7th ed. Kleinman RE, Greer FR, editors. American Academy of Pediatrics; Elk Grove Village, IL: 2014. [Google Scholar]
- Bakke AJ, Shehan CV, Hayes JE. Type of milk typically consumed, and stated preference, but not health consciousness affect revealed preferences for fat in milk. Food Qual Prefer. 2016;49:92–99. doi: 10.1016/j.foodqual.2015.12.001. doi: 10.1016/j.foodqual.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. doi:10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- Bigornia SJ, LaValley MP, Moore LL, Northstone K, Emmett P, Ness AR, Newby PK. Dairy intakes at age 10 years do not adversely affect risk of excess adiposity at 13 years. J Nutr. 2014;144(7):1081–1090. doi: 10.3945/jn.113.183640. doi: 10.3945/jn.113.183640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL. Preschool children's food preferences and consumption patterns. Journal of Nutrition Education. 1979;11:189–192. doi: 10.1016/S0022-3182(79)80025-4. [Google Scholar]
- Birch LL, Deysher M. Conditioned and unconditioned caloric compensation: evidence for self-regulation of food intake in young children. Learning and Motivation. 1985;16:341–355. doi: 10.1016/0023-9690(85)90020-7. [Google Scholar]
- Birch LL, McPhee L, Steinberg L, Sullivan S. Conditioned flavor preferences in young children. Physiology & Behavior. 1990;47:501–505. doi: 10.1016/0031-9384(90)90116-l. doi: 10.1016/0031-9384(90)90116-L. [DOI] [PubMed] [Google Scholar]
- Branton A, Akhavan T, Gladanac B, Pollard D, Welch J, Rossiter M, Bellissimo N. Pre-meal video game playing and a glucose preload suppress food intake in normal weight boys. Appetite. 2014;83:256–262. doi: 10.1016/j.appet.2014.08.024. doi: 10.1016/j.appet.2014.08.024. [DOI] [PubMed] [Google Scholar]
- Camps G, Mars M, de Graaf C, Smeets PA. Empty calories and phantom fullness: a randomized trial studying the relative effects of energy density and viscosity on gastric emptying determined by MRI and satiety. Am J Clin Nutr. 2016 doi: 10.3945/ajcn.115.129064. Doi:10.3945/ajcn.115.129064. [DOI] [PubMed] [Google Scholar]
- Canada Health Eating Well With Canada's Food Guide. 2011 Retrieved from http://www.hcsc.gc.ca/fn-an/alt_formats/hpfb-dgpsa/pdf/food-guide-aliment/view_eatwell_vue_bienmang-eng.pdf.
- Carnell S, Wardle J. Measuring behavioural susceptibility to obesity: validation of the child eating behaviour questionnaire. Appetite. 2007;48(1):104–113. doi: 10.1016/j.appet.2006.07.075. doi: 10.1016/j.appet.2006.07.075. [DOI] [PubMed] [Google Scholar]
- Cecil JE, Palmer CN, Wrieden W, Murrie I, Bolton-Smith C, Watt P, Hetherington MM. Energy intakes of children after preloads: adjustment, not compensation. Am J Clin Nutr. 2005;82(2):302–308. doi: 10.1093/ajcn.82.2.302. [DOI] [PubMed] [Google Scholar]
- Davy BM, Van Walleghen EL, Orr JS. Sex differences in acute energy intake regulation. Appetite. 2007;49(1):141–147. doi: 10.1016/j.appet.2007.01.010. doi: 10.1016/j.appet.2007.01.010. [DOI] [PubMed] [Google Scholar]
- DeBoer MD, Agard HE, Scharf RJ. Milk intake, height and body mass index in preschool children. Arch Dis Child. 2015;100(5):460–465. doi: 10.1136/archdischild-2014-306958. doi: 10.1136/archdischild-2014-306958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degen L, Oesch S, Matzinger D, Drewe J, Knupp M, Zimmerli F, Beglinger C. Effects of a preload on reduction of food intake by GLP-1 in healthy subjects. Digestion. 2006;74(2):78–84. doi: 10.1159/000097585. doi: 10.1159/000097585. [DOI] [PubMed] [Google Scholar]
- Faith MS, Pietrobelli A, Heo M, Johnson SL, Keller KL, Heymsfield SB, Allison DB. A twin study of self-regulatory eating in early childhood: estimates of genetic and environmental influence, and measurement considerations. Int J Obes (Lond) 2012;36(7):931–937. doi: 10.1038/ijo.2011.258. doi: 10.1038/ijo.2011.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JO, Rolls BJ, Birch LL. Children's bite size and intake of an entree are greater with large portions than with age-appropriate or self-selected portions. Am J Clin Nutr. 2003;77(5):1164–1170. doi: 10.1093/ajcn/77.5.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JO, Liu Y, Birch LL, Rolls BJ. Effects of portion size and energy density on young children's intake at a meal. Am J Clin Nutr. 2007;86(1):174–179. doi: 10.1093/ajcn/86.1.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, Susman EJ. Self-regulation and rapid weight gain in children from age 3 to 12 years. Arch Pediatr Adolesc Med. 2009;163(4):297–302. doi: 10.1001/archpediatrics.2008.579. doi: 10.1001/archpediatrics.2008.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasnain SR, Singer MR, Bradlee ML, Moore LL. Beverage intake in early childhood and change in body fat from preschool to adolescence. Child Obes. 2014;10(1):42–49. doi: 10.1089/chi.2013.0004. doi: 10.1089/chi.2013.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh SY, Rifas-Shiman SL, Rich-Edwards JW, Taveras EM, Gillman MW. Prospective association between milk intake and adiposity in preschool-aged children. J Am Diet Assoc. 2010;110(4):563–570. doi: 10.1016/j.jada.2009.12.025. doi: 10.1016/j.jada.2009.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Birch LL. Parents' and children's adiposity and eating style. Pediatrics. 1994;94(5):653–661. [PubMed] [Google Scholar]
- Johnson SL. Improving Preschoolers' self-regulation of energy intake. Pediatrics. 2000;106(6):1429–1435. doi: 10.1542/peds.106.6.1429. doi: 10.1542/peds.106.6.1429. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Taylor-Holloway LA. Non-Hispanic white and Hispanic elementary school children's self-regulation of energy intake. Am J Clin Nutr. 2006;83(6):1276–1282. doi: 10.1093/ajcn/83.6.1276. [DOI] [PubMed] [Google Scholar]
- Kaur H, Li C, Nazir N, Choi WS, Resnicow K, Birch LL, Ahluwalia JS. Confirmatory factor analysis of the child-feeding questionnaire among parents of adolescents. Appetite. 2006;47(1):36–45. doi: 10.1016/j.appet.2006.01.020. doi: 10.1016/j.appet.2006.01.020. [DOI] [PubMed] [Google Scholar]
- Keast DR, Fulgoni VL, 3rd, Nicklas TA, O'Neil CE. Food sources of energy and nutrients among children in the United States: National Health and Nutrition Examination Survey 2003-2006. Nutrients. 2013;5(1):283–301. doi: 10.3390/nu5010283. doi: 10.3390/nu5010283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kling SMR, Roe LS, Keller KL, Rolls BJ. Double trouble: Portion size and energy density combine to increase preschool children's lunch intake. Physiol Behav. 2016 doi: 10.1016/j.physbeh.2016.02.019. doi: 10.1016/j.physbeh.2016.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, Aksan N. Children's conscience and self-regulation. J Pers. 2006;74(6):1587–1617. doi: 10.1111/j.1467-6494.2006.00421.x. doi: 10.1111/j.1467-6494.2006.00421.x. [DOI] [PubMed] [Google Scholar]
- Kral TV, Allison DB, Birch LL, Stallings VA, Moore RH, Faith MS. Caloric compensation and eating in the absence of hunger in 5- to 12-y-old weight-discordant siblings. Am J Clin Nutr. 2012;96(3):574–583. doi: 10.3945/ajcn.112.037952. doi: 10.3945/ajcn.112.037952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kral TV, Remiker AM, Strutz EM, Moore RH. Role of child weight status and the relative reinforcing value of food in children's response to portion size increases. Obesity (Silver Spring) 2014;22(7):1716–1722. doi: 10.1002/oby.20757. doi: 10.1002/oby.20757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahy KE, Birch LL, Fisher JO, Rolls BJ. Reductions in entree energy density increase children's vegetable intake and reduce energy intake. Obesity (Silver Spring) 2008a;16(7):1559–1565. doi: 10.1038/oby.2008.257. doi: 10.1038/oby.2008.257. [DOI] [PubMed] [Google Scholar]
- Leahy KE, Birch LL, Rolls BJ. Reducing the energy density of an entrée decreases children's energy intake at lunch. J Am Diet Assoc. 2008b;108(1):41–48. doi: 10.1016/j.jada.2007.10.015. doi: 10.1016/j.jada.2007.10.015. [DOI] [PubMed] [Google Scholar]
- Leahy KE, Birch LL, Rolls BJ. Reducing the energy density of multiple meals decreases the energy intake of preschool-age children. Am J Clin Nutr. 2008c;88(6):1459–1468. doi: 10.3945/ajcn.2008.26522. doi: 10.3945/ajcn.2008.26522. [DOI] [PubMed] [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS for Mixed Models. Second edition ed. SAS Institute Inc; Cary, NC: 2006. [Google Scholar]
- Mattes RD, Rothacker D. Beverage viscosity is inversely related to postprandial hunger in humans. Physiology & Behavior. 2001;74:551–557. doi: 10.1016/s0031-9384(01)00597-2. doi:10.1016/s0031-9384(01)00597-2. [DOI] [PubMed] [Google Scholar]
- Mehrabani S, Safavi SM, Mehrabani S, Asemi M, Feizi A, Bellissimo N, Salehi-Abargouei A. Effects of low-fat milk consumption at breakfast on satiety and short-term energy intake in 10- to 12-year-old obese boys. Eur J Nutr. 2015 doi: 10.1007/s00394-015-0956-4. doi: 10.1007/s00394-015-0956-4. [DOI] [PubMed] [Google Scholar]
- Mooreville M, Davey A, Orloski A, Hannah EL, Mathias KC, Birch LL, Fisher JO. Individual differences in susceptibility to large portion sizes among obese and normal-weight children. Obesity (Silver Spring) 2015;23(4):808–814. doi: 10.1002/oby.21014. doi: 10.1002/oby.21014. [DOI] [PubMed] [Google Scholar]
- Norton EM, Poole SA, Raynor HA. Impact of fruit juice and beverage portion size on snack intake in preschoolers. Appetite. 2015;95:334–340. doi: 10.1016/j.appet.2015.07.025. doi: 10.1016/j.appet.2015.07.025. [DOI] [PubMed] [Google Scholar]
- O'Connor TM, Yang SJ, Nicklas TA. Beverage intake among preschool children and its effect on weight status. Pediatrics. 2006;118(4):e1010–1018. doi: 10.1542/peds.2005-2348. doi: 10.1542/peds.2005-2348. [DOI] [PubMed] [Google Scholar]
- Onvani S, Haghighatdoost F, Surkan PJ, Azadbakht L. Dairy products, satiety and food intake: A meta-analysis of clinical trials. Clin Nutr. 2016 doi: 10.1016/j.clnu.2016.01.017. doi: 10.1016/j.clnu.2016.01.017. [DOI] [PubMed] [Google Scholar]
- Poti JM, Slining MM, Popkin BM. Where Are Kids Getting Their Empty Calories? Stores, Schools, and Fast-Food Restaurants Each Played an Important Role in Empty Calorie Intake among US Children During 2009-2010. J Acad Nutr Diet. 2013 doi: 10.1016/j.jand.2013.08.012. doi: 10.1016/j.jand.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranawana DV, Henry CJ. Are caloric beverages compensated for in the short-term by young adults? An investigation with particular focus on gender differences. Appetite. 2010;55(1):137–146. doi: 10.1016/j.appet.2010.05.046. doi: 10.1016/j.appet.2010.05.046. [DOI] [PubMed] [Google Scholar]
- Rehm CD, Drewnowski A, Monsivais P. Potential population-level nutritional impact of replacing whole and reduced-fat milk with low-fat and skim milk among US children aged 2-19 years. J Nutr Educ Behav. 2015;47(1):61–68. e61. doi: 10.1016/j.jneb.2014.11.001. doi: 10.1016/j.jneb.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remy E, Issanchou S, Chabanet C, Boggio V, Nicklaus S. Impact of adiposity, age, sex, and maternal feeding practices on eating in the absence of hunger and caloric compensation in preschool children. Int J Obes (Lond) 2015;39:925–930. doi: 10.1038/ijo.2015.30. [DOI] [PubMed] [Google Scholar]
- Robson SM, Khoury JC, Kalkwarf HJ, Copeland K. Dietary intake of children attending full-time child care: What are they eating away from the child-care center? J Acad Nutr Diet. 2015;115(9):1472–1478. doi: 10.1016/j.jand.2015.02.029. doi: 10.1016/j.jand.2015.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolls BJ, Engell D, Birch LL. Serving portion size influences 5-year-old but not 3-year-old children's food intakes. J Am Diet Assoc. 2000;100(2):232–234. doi: 10.1016/S0002-8223(00)00070-5. doi: 10.1016/s0002-8223(00)00070-5. [DOI] [PubMed] [Google Scholar]
- Spill MK, Birch LL, Roe LS, Rolls BJ. Hiding vegetables to reduce energy density: an effective strategy to increase children's vegetable intake and reduce energy intake. Am J Clin Nutr. 2011;94(3):735–741. doi: 10.3945/ajcn.111.015206. doi: 10.3945/ajcn.111.015206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture, Food and Nutrition Services Child and Adult Care Food Program (CACFP) Child Care Meal Pattern. 2016 Retrieved from http://www.fns.usda.gov/sites/default/files/Child_Meals.pdf.
- U.S. Department of Agriculture, & Agricultural Research Service USDA Nutrient Database for Standard Reference. 2015 Release 28. Retrieved from: http://www.ars.usda.gov/Services/docs.htm?docid=8964.
- U.S. Department of Health and Human Services and U.S. Department of Agriculture 2015 – 2020 Dietary Guidelines for Americans. 2015 Retrieved from http://health.gov/dietaryguidelines/2015/guidelines/
- U.S. Department of Health and Human Services, Centers for Disease Control and Prevention [December 9, 2015, 2014];A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 y) 2015 from http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm.
- Wang YC, Ludwig DS, Sonneville K, Gortmaker SL. Impact of change in sweetened caloric beverage consumption on energy intake among children and adolescents. Arch Pediatr Adolesc Med. 2009;163(4):336–343. doi: 10.1001/archpediatrics.2009.23. doi: 10.1001/archpediatrics.2009.23. [DOI] [PubMed] [Google Scholar]
- Wilson JF. Preschool children maintain intake of other foods at a meal including sugared chocolate milk. Appetite. 1991;16:61–67. doi: 10.1016/0195-6663(91)90112-6. doi: 10.1016/0195-6663(91)90112-6. [DOI] [PubMed] [Google Scholar]
- Wilson JF. Does type of milk beverage affect lunchtime eating patterns and food choice by preschool children? Appetite. 1994;23:90–92. doi: 10.1006/appe.1994.1038. doi: 10.1006/appe.1994.1038. [DOI] [PubMed] [Google Scholar]
- Wilson JF. Lunch eating behavior of preschool children. Effects of age, gender, and type of beverage served. Physiol Behav. 2000;70(1-2):27–33. doi: 10.1016/s0031-9384(00)00230-4. doi: 10.1016/s0031-9384(00)00230-4. [DOI] [PubMed] [Google Scholar]
- Zahn S, Hoppert K, Ullrich F, Rohm H. Dairy-based emulsions: Viscosity affects fat difference thresholds and sweetness perception. Foods. 2013;2(4):521–533. doi: 10.3390/foods2040521. doi: 10.3390/foods2040521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng M, Rangan A, Olsen NJ, Andersen LB, Wedderkopp N, Kristensen P, Heitmann BL. Substituting sugar-sweetened beverages with water or milk is inversely associated with body fatness development from childhood to adolescence. Nutrition. 2015;31(1):38–44. doi: 10.1016/j.nut.2014.04.017. doi: 10.1016/j.nut.2014.04.017. [DOI] [PubMed] [Google Scholar]
- Zijlstra N, Mars M, de Wijk RA, Westerterp-Plantenga MS, de Graaf C. The effect of viscosity on ad libitum food intake. Int J Obes (Lond) 2008;32(4):676–683. doi: 10.1038/sj.ijo.0803776. doi: 10.1038/sj.ijo.0803776. [DOI] [PubMed] [Google Scholar]