Abstract
Background
Sub-Saharan Africa (SSA) has the highest prevalence of HIV globally, and this is due to persistent new HIV infections and decline in HIV/AIDS-related mortality from improved access to antiretroviral (ART) therapy. There is a limited body of work on perspectives of health-care providers (HCPs) concerning disclosing outcomes of HIV investigations to children and adolescents in SSA. Most studies are country-specific, indicating a need for a regional scope.
Objective
To review the current literature on the perspectives of HCPs and caregivers of children and adolescents on age group-specific and culture-sensitive HIV disclosure practice.
Methods
Electronic database search in PubMed, Google scholar, and the University of South Florida Library Discovery Tool (January 2006 up to February 2016). Further internet search was conducted using the journal author name estimator search engine and extracting bibliographies of relevant articles. Search terms included “disclosure*,” “HIV guidelines,” “sub-Saharan Africa,” “clinical staff,” “ART,” “antiretroviral adherence,” “people living with HIV,” “pediatric HIV,” “HIV,” “AIDS,” “health care provider,” (HCP), “caregiver,” “adolescent,” “primary care physicians,” “nurses,” and “patients.” Only studies related to HIV/AIDS disclosure, HCPs, and caregivers that clearly described perspectives and interactions during disclosure of HIV/AIDS sero-status to affected children and adolescents were included. Independent extraction of articles was conducted by reviewers using predefined criteria. Nineteen articles met inclusion criteria. Most studies were convenience samples consisting of combinations of children, adolescents, HCPs, and caregivers. Key findings were categorized into disclosure types, prevalence, facilitators, timing, process, persons best to disclose, disclosure setting, barriers, and outcomes of disclosure.
Conclusion
Partial disclosure is appropriate for children in SSA up to early adolescence. Caregivers should be directly involved in disclosing to children but they require adequate disclosure support from HCPs. Full disclosure is suitable for adolescents. Adolescents prefer disclosure by HCPs and they favor peer-group support from committed peers and trained facilitators, to reduce stigma. HCPs need continuous training and adequate resources to disclose in a patient-centered manner.
Keywords: HIV disclosure, children and adolescents, health-care providers, caregivers, sub-Saharan Africa, ART adherence
Introduction
The HIV pandemic is one of the most severe public health challenges facing the world to date. This pandemic has grave economic implications, especially in high prevalent regions like sub-Saharan Africa (SSA) (1, 2). The global HIV burden is estimated at 36.9 million cases; by the end of 2014, approximately 2 million new cases and 34 million deaths were attributed to AIDS-related causes (3–6). Recent data indicate that the top 10 ranking of HIV/AIDS cases by country is populated by countries in SSA (5, 6). In 2015, SSA contributed to 70% of new cases globally (5, 6). Factors contributing to the prevalence of HIV in SSA include improved access to antiretroviral (ART) medications and the resultant decline in mortality, while new infections from HIV/AIDS persist (1, 7).
Majority of new HIV infection cases occur in low- and middle-income countries that lack properly defined guidelines or resources to equip HCPs (3, 8, 9). HIV disclosure may be one of the critical links between new infections and the sustained high prevalence in SSA (10, 11). Inadequate health-care provider (HCP) training in HIV disclosure and testing services appear to contribute to new cases. Unfortunately, limited body of work exists on the prevalence and practice of disclosure by HCPs in SSA (7). Over the last 15 years, there has been a 35% decrease in global HIV infections and a 58% decrease among children, yet more than 54% of children currently infected may be unaware they have the disease (6, 12). A study on resource-limited countries that had available disclosure rates (Ghana, Kenya, and Ethiopia) reported rates that varied from 11 to 38% (11, 13, 14). This variability is consistent with studies in resource-rich countries where disclosure rates to children range widely from 10 to 77% (15–17). Furthermore, HIV disclosure practices in SSA remain complex due to the immense influence of culture, politics, and limited HIV surveillance (5, 10, 18). Disclosure rates in high prevalence regions need to be evaluated and improved drastically in a timely manner as HIV disclosure may be a key factor in reducing the risk of acquiring new infections, adherence to ARTs, and practice of safe sexual behaviors (7, 10, 19, 20).
Taken together, the incidence of HIV infection in SSA may be reduced by understanding the perspectives and roles of HCPs and caregivers in disclosing laboratory HIV test outcomes to children and adolescents in this region. In addition, studies in this region are country-specific; therefore, evaluating the perspectives of HCPs and caregivers across countries may provide more insight to achieve more reduction in new HIV infections. To determine the perspectives of HCPs and caregivers on age group-specific and culturally sensitive HIV disclosure practices in SSA, a systematic review of the perspectives and current patterns of HIV disclosure among HCPs and caregivers of children and adolescents was conducted.
Methods
We searched for quantitative, qualitative (focus groups, interviews, and surveys), and mixed methods studies on HIV disclosure involving HCPs and caregivers in SSA from January 1, 2006 to February 28, 2016. English language restriction was imposed. Study participants included combinations of children and adolescents, HCPs and caregivers, or only caregivers or HCPs. Disclosure was categorized as full disclosure, partial disclosure, and non-disclosure (12, 21). Full disclosure is complete disclosure of HIV status with the term “HIV” appropriately used (11, 12, 21). In this case, the potential causes, transmission, and impact of the disease were discussed and treatment was clarified. Partial disclosure was performed similarly to full disclosure but the terms “HIV” or “AIDS” were excluded despite describing the morbidity and mortality from the disease (12, 21, 22). Other aspects present in full disclosure may also be excluded, for example, counseling (20, 21). Non-disclosure signifies no disclosure. In this case, individuals are not provided any information about their positive HIV status (12, 21).
The term “health-care providers” refers to health-care professionals, such as clinical staff, primary care physicians, nurses, midwives, and any health personnel, providing patient care in a clinical setting. A caregiver includes parents, family members, or individuals caring for a child or adolescent living with HIV/AIDS in a non-clinical/professional capacity. Articles were selected on application of the following inclusion criteria: social science work that examined HIV disclosure through qualitative or quantitative studies and mixed methods that clearly described perspectives and interactions among HCPs, caregivers, and infected children and adolescents.
Search Strategy and Search Procedure
A computer-assisted systematic review was conducted, and extraction of articles was independently performed by the three authors who have expertise in community and family health, global health, epidemiology, and HIV management. Disagreements between reviewers were resolved by consensus. Three major electronic databases were searched using dates January 1, 2006 to February 28, 2016. These bibliographic databases included PubMed, Google Scholar, and the University of South Florida (USF) Library Discovery Tool. For USF Library Discovery Tool and PubMed, the term “HIV AIDS disclosure” was searched, then the Boolean operator and last set of terms “health-care provider” OR “caregiver” OR “patient” OR “adolescent” were added. Finally, the inclusion criteria were applied.
For Google Scholar, the term “HIV disclosure” was searched then “AIDS disclosure” and “sub-Saharan Africa” were added. Next, the Boolean operator and keyword “health-care providers” OR “caregiver” OR “patient” OR “pediatric” OR “health-care professionals” were added. Finally, the inclusion criteria were applied. An additional internet search was conducted in Journal Author Name Estimator database (JANE) using the proposed search terms and their variants. Additional articles were cross referenced for further review of all the articles, and some articles were excluded either because they did not meet the inclusion criteria of the review or they were duplicates. Figure 1 shows a flow diagram of the search process.
Figure 1.
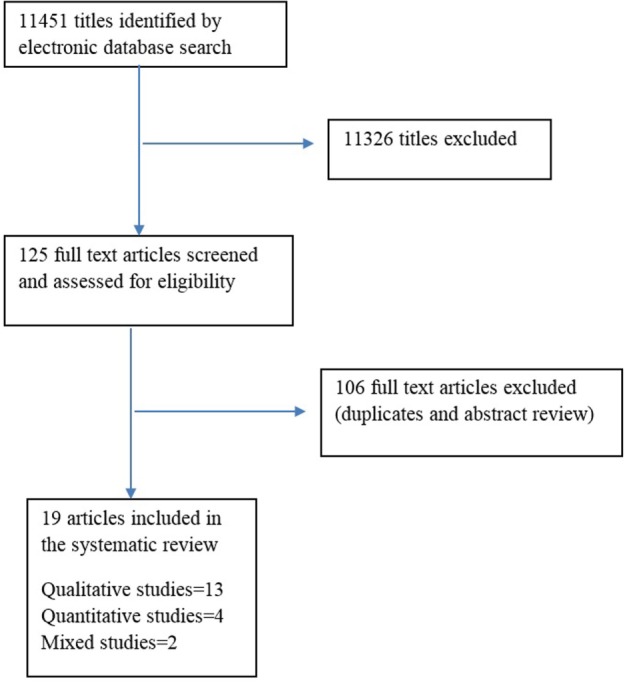
Flow chart of HIV disclosure systematic review search process.
Variants of keywords for HCP, caregiver, HIV and AIDS, and disclosure were also used. The search strategy was limited to articles that were accessible through the USF library. Full-text articles of all selected studies were retrieved, and if an article was selected, the bibliographic references were examined for additional relevant studies. Caregivers, HCP, and patients were combined with the use of the Boolean operator “OR.” The above searches, based on the two main interest HIV/AIDS disclosure and SSA, were combined using the Boolean operator “AND.”
Data Extraction
A data extraction sheet was developed by two of the authors (Oluyemisi Aderomilehin and Angella Hanciles-Amu) and reviewed by the third author (Oluwatobi Ohiole Ozoya). A total of 19 articles met the inclusion criteria. First author, year and title of publication, country of study, population characteristics, study design, and theme topics were included in the sheet (Table 1). A summary of the results from included studies that were relevant to perspectives and practice of HIV disclosure to children and adolescents are detailed in Table 2.
Table 1.
Study characteristics.
| Study | Title | Location | Population sample size | Study design and methods of data collection | Key findings | |
|---|---|---|---|---|---|---|
| 1 | Mburu et al. (23) | Adolescent HIV disclosure in Zambia: barriers, facilitators, and outcomes | Zambia | 223
|
Qualitative (interviews and focus group discussions) |
|
| 2 | De Baets et al. (21) | HIV disclosure and discussions about grief with Shona children: a comparison between health-care workers and community members in Eastern Zimbabwe | Zimbabwe | 195
|
Quantitative (anonymous survey) |
|
| 3 | Demmer (24) | Experiences of families caring for an HIV-infected child in KwaZulu-Natal, South Africa: an exploratory study | South Africa | 25
|
Qualitative (in-depth interview and semi-structured interview) |
|
| 4 | Gyamfi et al. (25) | Benefits of disclosure of HIV status to infected children and adolescents: perceptions of caregivers and health-care providers | Ghana | 118
|
Mixed method (quantitative and qualitative) |
|
| 5 | Kajubi et al. (26) | Communication between HIV-infected children and their caregivers about HIV medicines: a cross-sectional study in Jinja district, Uganda | Uganda | 394
|
Quantitative (cross-sectional survey) |
|
| 6 | Kidia et al. (27) | HIV-status disclosure to perinatally-infected adolescents in Zimbabwe: a qualitative study of adolescent and health-care worker perspectives | Zimbabwe | 46
|
Qualitative (in-depth interviews with adolescents; focus groups with HCPs) |
|
| 7 | Midtbo et al. (28) | How disclosure and antiretroviral therapy help HIV-infected adolescents in sub-Saharan Africa cope with stigma | Botswana | 14
|
Qualitative (interviews and observation) |
|
| Tanzania | 19
|
|||||
| 8 | Moodley et al. (29) | Paediatric HIV disclosure in South Africa – caregivers’ perspectives on discussing HIV with infected children | South Africa | 174
|
Qualitative (semi-structured interviews) |
|
| 9 | Kiwanuka et al. (30) | Caregiver perceptions and motivation for disclosing or concealing the diagnosis of HIV infection to children receiving HIV care in Mbarara, Uganda: a qualitative study | Uganda | 40
|
Qualitative (in-depth interviews) |
|
| 10 | Lorenz et al. (31) | Caregivers’ attitudes towards HIV testing and disclosure of HIV status to at-risk children in rural Uganda | Uganda | 28
|
Qualitative (semi-structured interviews) |
|
| 11 | Beima-Sofie et al. (32) | Using health provider insights to inform pediatric HIV disclosure: a qualitative study and practice framework from Kenya | Kenya | 21
|
Qualitative (interviews) |
|
| 12 | Mumburi et al. (33) | Factors associated with HIV-status disclosure to HIV-infected children receiving care at Kilimanjaro Christian Medical Centre in Moshi, Tanzania | Tanzania | 236
|
Quantitative (cross-sectional with structured questionnaires) |
|
| 13 | Myer et al. (34) | Health-care providers’ perspectives on discussing HIV status with infected children | South Africa | 40
|
Qualitative (semi-structured interviews) |
|
| 14 | Corneli et al. (35) | The role of disclosure in relation to assent to participate in HIV-related research among HIV-infected youth: a formative study | Democratic Republic of Congo | 72
|
Qualitative (semi-structured interviews) |
|
| 15 | Gachanja and Burkholder (36) | Model for HIV disclosure of a parent’s and/or a child’s illness | Kenya | 34
|
Qualitative |
|
| 16 | Odiachi and Abegunde (37) | Prevalence and predictors of pediatric disclosure among HIV-infected Nigerian children on treatment | Nigeria |
|
Quantitative (semi-structured interview) |
|
| 17 | Toska et al. (38) | Sex and secrecy: how HIV-status disclosure affects safe sex among HIV-positive adolescents | South Africa | 858
|
Mixed methods [qualitative (interviews, focus group discussions and observations with 43 HIV-positive teenagers and their HCPs; quantitative interviewed using standardized questionnaires)] |
|
| 18 | Vaz et al. (39) | Patterns of disclosure of HIV status to infected children in a sub-Saharan African setting | DR Congo | 201
|
Qualitative (structured interviews) |
|
| 19 | Watermeyer (40) | ‘Are we allowed to disclose?’: a health-care team’s experiences of talking with children and adolescents about their HIV status | South Africa |
|
Qualitative (focus groups) |
|
Table 2.
High level summary of selected articles.
| Mburu et al. (23) Barriers and outcomes of HIV disclosure
|
Watermeyer (40) Barriers to disclosure and HCPs disclosure practices
|
Demmer (24) Barriers to disclosure
|
| De Baets et al. (21) Age of disclosure and Best person to disclose to child
|
Gyamfi et al. (25) Best person to disclose, proportion, benefits of disclosing and elements needed in caregiver support
|
Kajubi et al. (26) Disclosure communication pattern and age (full/partial disclosure)
|
| Kidia et al. (27) Best person to disclose, disclosure setting and support
|
Midtbo et al. (28) Stigma and coping following disclosure
|
Corneli et al. (35) Age of disclosure to children
|
Kiwanuka et al. (30)Disclosure as a single event or process, benefits and barriers
|
Lorenz et al. (31) Facilitators to testing child, age at disclosure, barriers, type of disclosure and support
|
Beima-Sofie et al. (32) HCPs disclosure practices, family-centered disclosure, best Person to disclose and outcomes
|
| Moodley et al. (29) Disclosure proportion, age of child at disclosure, best person, facilitators, and barriers
|
Gachanja and Burkholder (36) Facilitators, age of disclosure, associated emotions, benefits, and negative outcomes
|
Odiachi and Abegunde (37) Prevalence, age of disclosure, facilitators. and barriers
|
| Toska et al. (38) Prevalence of disclosure, benefits, and barriers
|
Vaz et al. (39) Proportion of disclosure, facilitators, benefits, and caregiver support in disclosure
|
Mumburi et al. (33) Proportion of disclosure, age of disclosure, and caregiver support
|
| Myer et al. (34) Partial disclosure to children and transition to full disclosure, best person to disclose
| ||
Results
All studies in the final selection included various types of studies ranging from 13 qualitative study design, including interviews and focus groups (23, 24, 27, 28, 30–32, 34–36, 39, 40), to 4 quantitative study design (21, 26, 33, 37) and 2 mixed methods design (25, 38). The 19 articles included studies conducted in 10 SSA countries. The sample sizes were variable, ranging from 21 to 858 (median 79). Most studies utilized small samples, with the largest four studies including 40 HCPs (34), 394 caregivers (26), and 858 children and adolescents (38). Three studies included only HCPs (32, 34, 40), and five studies included only caregivers (29–31, 37, 39). One study included both HCPs and community members with focus on HIV disclosure and discussions about grief (21). The three studies that included only HCPs-provided information on types of disclosure in practice and the most suitable person and setting to disclose (32, 34, 40). Some of the studies included caregivers living with HIV and others without HIV. Caregivers were involved in the care of HIV-positive children, adolescents, or family members (29–31, 37, 39). Estimation of disclosure prevalence was limited to two articles (37, 38). The studies explored perspectives on disclosure types, prevalence, facilitators, timing, process, persons best to disclose, disclosure setting, barriers, and outcomes of disclosure. This is described below.
Types and Prevalence of HIV Disclosure
Disclosure was defined by mention of “HIV or AIDS” when explaining the illness to infected children and adolescents, implying full disclosure, otherwise, partial disclosure is the case (21, 24, 26, 33, 34, 38, 40). Non-disclosure was present in two studies where the children were neither aware of the illness nor the reason for taking medications (33, 39).
Only two studies reported on prevalence of HIV disclosure estimated at 30.9% among infected children and 68.1% among infected adolescents (37, 38). In these studies, the infected children and adolescents were aware of their HIV infection, indicating full disclosure. Three other qualitative studies reported less than half of caregivers who had disclosed to their children (25, 29, 39). Two studies reported non-disclosure by 50% of caregivers and simultaneously reported partial disclosure by 15–24.6% of caregivers (33, 39).
Facilitators and Timing of Disclosure Type
Major facilitators for caregivers in initiating disclosure was knowledge of availability of ART therapy (29), view of disclosure as the right of the child and adolescent (29, 41) when adhering to ART therapy was a potential or actual problem for the infected child or there was frequent visits to health facilities despite absence of overt illness (37, 39). Other facilitators to HIV disclosure include persistent inquiries by the HIV-positive child or adolescent (36, 37), presence of chronic illness in the child or a family member (31, 39), or discovery at routine antenatal clinic attendance by infected mothers (36). A common predictor of the timing of disclosure to children was the age of the child; the age for disclosure varied widely among the studies and ranged from 5 to 15 years (21, 26, 29, 31, 33–37). Studies that reported a specific age of disclosure to children included 5 years (36), 7 years (31), above 10 years (33, 34, 37), 12 years (29), and 15 years (26, 35). Three studies distinguished age at full disclosure as above 10 years (34, 36), 14 years (21), and 15 years (26). Two studies specifically reported partial disclosure by caregivers at ages <10 years (21, 34, 36) and 15 years (26, 35).
Process of HIV Disclosure
Irrespective of whether it was a HCP or caregiver being interviewed, some of the studies indicated that the process of disclosure can be complex (23, 24, 26, 29, 37–40). One study reported caregivers who perceived disclosure as a single event (30). Only one study reported different phases of disclosure that included pre-disclosure, disclosure, and post-disclosure phases of disclosure to children (36). Here, the parents of infected children were counseled to anticipate and resolve questions the children may have prior, during, and following disclosure (36). Some other studies reported caregivers who preferred to receive counsel from HCPs or HIV counselors before disclosing (29, 31, 39). From the time of diagnosis, some participants adopted partial disclosure till the children were perceived as ready to receive full disclosure (21, 34, 36). Only one of the studies clearly described the post-disclosure phase (36). In the post-disclosure phase, some of the children in the study had questions about transmission of the disease, HIV management, and eventual cure (36).
Persons Best to Disclose
Persons best positioned to disclose varied in different studies and by the key participants asked. Majority of the studies that explored “persons best to disclose” favored disclosure by caregivers with support from HCPs (27, 29, 31–34). One study reported preference for HCPs disclosing rather than caregivers (25). Two studies among caregivers in South Africa and Uganda reported high preference for the parent or caregiver to disclose rather than HCPs (29, 30). A study in Uganda and Kenya indicated that HCPs support caregivers when they initiate disclosure (27, 32), but adolescents preferred HCPs to disclose rather than their caregivers because they had an opportunity for more accurate information about their disease (27). A study in South Africa indicated that caregivers preferred that the HCP or family members, especially the paternal aunt and grandmother disclose rather than the mother (21). Although some caregivers preferred to disclose to infected children themselves, they expressed fears of competence in disclosure; acceptance by the child; stigma from accidental disclosure by the child to others; and need for support (29, 31, 32, 34, 39).
Approach to Disclosure
Perspectives of different groups of HCPs differed on approach to disclosure. Nurses and counselors shared preference for encouraging caregivers to disclose to their children and adolescents with adequate support (40), unlike doctors who preferred direct participation in disclosure from a professional and legal obligation (32, 40). HCPs experienced conflict between human rights or public health safety during disclosure and also required training in decision-making and to reduce inadvertent disclosure (37). When HCPs were to discuss grief or HIV diagnosis with children and adolescents, HCPs preferred full disclosure of HIV diagnosis to children at a younger age (6–15 years) rather than discussing grief. In contrast, caregivers preferred that children were older (10–19 years) since they were more open to discussing grief than HIV.
Disclosure Setting
Disclosure setting was an important consideration in the disclosure process according to some of the studies. The health facility setting was preferred by HCPs because this provided an avenue for caregiver support during the disclosure process (32), and also gave adolescents the opportunity to obtain reliable answers to questions and interact with peers at the health facility (27, 28). For caregivers who preferred their HCPs to be involved in the disclosure process, the health facility was the natural setting where this occurred (29, 33, 34, 40). Where caregivers preferred to handle disclosure to their minors, the home setting was the natural environment (30).
Barriers and Outcomes of HIV Disclosure
Barriers to disclosure by HCPs or caregivers included the fear of HIV stigma, uncertainty about cognitive development of children, and local traditions that limit discussion of sexuality (23, 24, 29, 36). Some studies described benefits from the disclosure process, and this included improved ART adherence and mental health of affected individuals (25, 35), opportunity to cope with the illness, and the associated stigma (27, 28, 30). By contrast, a study reported adolescents who experienced peer-stigma, anxiety, depression, and self-blame after knowing their positive status (28). Furthermore, some studies indicated that disclosure, especially premature or inadvertent disclosure, resulted in harmful outcomes such as stigma, discrimination, and abuse from family and community members (23, 28, 32, 36). Some caregivers coped by adopting a conspiracy of silence (24). Besides, a study in Democratic Republic of Congo reported up to one-third of caregivers who did not see any benefit in disclosing to children (39). In addition, a study involving HCPs and adolescents indicated that adolescents did not see any benefit in knowing their partner’s status nor disclosing to a partner (38). Rather, benefit was reported from knowing self-status as this informed safer sexual lifestyle (38). While one study suggested that disclosure may empower the child or adolescent to engage in safe sexual behaviors (25), another study indicated there was no correlation with sexual lifestyle but with medication adherence (38). Caregivers or other family members also had to disclose their HIV status to facilitate the communication of perinatal infection and ART adherence to infected children and adolescents (24, 29, 36). However, some caregivers expressed concerns that this process could generate both positive and negative outcomes (24, 29, 36).
Discussion
The objective of this review was to explore the perspectives and practices of HCPs and caregivers in HIV disclosure to children and adolescents. Findings are categorized as follows: types and prevalence of disclosure; facilitators, timing and barriers; process of disclosure; persons best to disclose, approach to disclosure by HCP versus caregivers; suitable disclosure setting and outcomes of disclosure.
This review showed that the prevalence of full disclosure is relatively low for children compared to adolescents, which is higher (37, 38). However, the prevalence of HIV disclosure needs to be improved for both age groups because more disclosure will reduce the number of infected children and adolescents at risk of morbidity and mortality from poor adherence to ARTs (23, 28, 32, 36). Despite natural concerns of adults about a child’s ability to cope with disclosure, empirical studies show that children may be more resilient than assumed (42, 43), appropriate disclosure may enhance psychological stability of the child and improve adherence to ART therapy (28, 42, 44). For adolescents, more disclosure by HCPs or caregivers to infected adolescents directly will encourage safer sexual behaviors that reduce new HIV transmission rather than emphasizing adolescents disclosing to their partners (38).
In SSA, variation exists in the types of disclosure in practice, and this review has highlighted studies where participants utilized partial disclosure before full disclosure of HIV-positive status or adopted outright non-disclosure (21, 26, 33, 34, 36, 41). Most studies identified the age of a child as a key factor that determined the timing of disclosure. It is important to identify cues to disclosure to children early since appropriate training for HCPs and caregivers may enhance their readiness to disclose. Age, as a key factor, also emerged in a systematic review by Vreeman et al. on pediatric disclosure practices in resource-limited settings (20). Most of the studies in this review suggest that, in SSA, partial disclosure may be appropriate for children up to early adolescence (21, 22, 34, 36), and this is consistent with the report from WHO Guideline on HIV Disclosure Counselling for Children up to 12 years of Age (2011) (12, 43). Despite age as a key factor in disclosure to children, we recommend that consideration needs to be given to communication patterns within families, orphan status, cultural norms, influence of other family members living with HIV/AIDS, and involvement of the child in administering ART medications (33, 36, 37).
Again, this review indicated that the concept of HIV disclosure process is relatively understudied since few studies evaluated perception of HCPs and caregivers. Caregivers described the disclosure process as complex, and one study reported caregivers who viewed disclosure as a solitary event. To reduce the complexity associated with disclosure, it is important to disseminate HIV disclosure as a process originating from the time of initial diagnosis to events beyond disclosure. Here, a series of dialog is made with the child about the terms, course of disease, relationship with others, self-care, and medications over time (36, 45). The dialog between caregivers and their children may be strengthened by providing focused counseling to caregivers throughout the disclosure process (42, 43, 46). Scientific research has demonstrated that the process-oriented approach results in less strain on caregivers and better outcomes for infected children and adolescents (28, 36, 42, 44, 47).
From the selected studies, there was evidence that both HCPs and caregivers perceived the most suitable individuals to disclose to children in SSA are caregivers, with support from HCPs throughout the process (27, 31, 32, 35, 37, 41). The WHO guideline on disclosure counseling to children under 12 years of age (2011) indicated that there is no evidence for either HCPs or caregivers disclosure as the best to disclose, but emphasized that disclosure should be in the best interest of the child (12). Adolescents had a preference for disclosure by the HCP because they received more biomedical information and could cope better with the disease than information received from their caregivers alone (27). Adolescents also indicated that peer-group support was important to them (23, 27). This suggests that the support needs of adolescents during the disclosure process differ from those of younger children in the region.
The health-care setting also plays a critical role in disclosure practice. Among HCPs, physicians tended to disclose more directly from a legal, moral, and ethical obligations compared to other workers who emphasized provision of support to caregivers who should disclose directly to infected children (40). As more HCPs disclose, it is critical to expand the locations where their services can be accessed by affected families. A review by Obermeyer and colleagues provided evidence that increased HIV/AIDS services in areas with limited services may facilitate disclosure and reduce stigma in the affected communities (46). Creating more health-care centers for HIV/AIDS services is an additional cost in resource-limited parts of the SSA, but the World Health Organization, in 2015, recommended HIV counseling and testing by trained lay providers (community health workers) to reduce the cost of providing needed services and to increase access to care (48). Some success is being recorded with lay providers in this regard, but this strategy requires more studies and careful review of existing policies to seamlessly integrate lay providers in provision of counseling and testing services (49–51).
Stigma and discrimination remain a persistent threat to the potential benefits of HIV disclosure. Sadly, local norms that deter discussion of sexuality also indirectly limit HIV disclosure by their HCPs and caregivers to children and adolescents (23). While advocating for any type of disclosure, it is important to consider individual rights and safety carefully balanced with public health safety.
Limitations
Some limitations are inherent in this review. For example, although our review focused on SSA, not all countries in this region had adequate research available on HIV disclosure by HCPs and caregivers. SSA was only represented by 10 countries out of 46 (Botswana, Democratic Republic Congo, Ghana, Kenya, Nigeria, South Africa, Tanzania, Uganda, Zambia, and Zimbabwe). Four studies performed prior to or during the period (2008) of increased access to ART in SSA may not have clearly depicted the current disclosure process and practices because of the recent discovery of a relationship between access to ART and HIV disclosure (7, 29, 34). Reported perspectives and practices may slightly differ in the health-care setting or living situation of participants; therefore, caution must be applied in interpretation of the findings and in making generalizations.
The quality of the studies varied especially with majority consisting of convenience sampling. Restricting the search to English-language publications may have excluded studies or participants from non-English speaking parts of SSA. Paucity of research on this topic limited the discussion of several other issues, such as specific disclosure communication and practices. Studies on prevalence and proportions of disclosed patients were largely for children and relatively less for adolescent, again limiting the scope of the review.
Implication
Because timing is an important factor to consider, best practices would have to include training of HCPs and caregivers to identify appropriate timing for disclosure, especially at the early phase of diagnosis (43). Continuing education and training that incorporate health policies and are amenable to local norms may contribute to the efficacy of HCPs when addressing barriers to HIV disclosure in their communities (48). Since the advent of more available ART, the focus has been on prompt diagnosis, prevention of mother-to-child transmission (PMTCT), partner disclosure, and testing with some success in HIV risk behavioral changes. However, success in individual behavior change will remain a challenge where the route of transmission involves at least two individuals or children infected perinatally. Findings from this review indicate the importance of broadening the scope of current HIV intervention programs to include adequately informed and appropriate disclosure. Therefore, long-term HIV/AIDS program funding should provide for resources to ensure that disclosure does not stop at informing individuals (e.g., infected mothers) of their HIV status or encouraging ART adherence; rather these resources should also be channeled to ensure adequate counseling and support after disclosure to minimize stigma, abuse, poor ART adherence, and transmission of new HIV infection.
Peer groups are helpful to adolescents but require participation of motivated members living with HIV and ought to be facilitated by trained personnel (27, 28). Although two studies among adolescents referred to peer support as a coping method for this population, stigma from peers was a reality in other studies (27, 28, 33). Therefore, when peer groups are being facilitated by HCPs, caution must be exercised to ensure appropriate groups are created and proactive measures undertaken to minimize stigma from peers.
The role of HCPs in HIV disclosure is challenged by insufficient number of HCPs relative to the sub-Saharan population (52, 53). Poor training, difficult working conditions, and increasing emigration to urban areas and developed countries has contributed to HCP shortage in about 31 countries in SSA (52, 53). The shortage in HCPs who daily endure stressful working conditions inadvertently impinge on optimal disclosure practices. To reduce the burden on HCPs, trained lay providers (community health workers) should be integrated in the disclosure process. Also, the responsibility to disclose can be shared equally by all cadres of HCPs trained in HIV disclosure, and team work should be driven by a patient-centered approach to caring for infected children and adolescents. An extension of this collaboration is a family-centered approach, where the health-care team collaborates with family members (or caregivers) directly involved in the care of the child at home or with individuals selected by family members to represent them (21, 43).
The ethical issues involved in disclosure have contributed to the complexity associated with establishing specific HIV disclosure guidelines in SSA (7, 8). To get the best result from disclosure, HCPs need to disclose in the most ethical and culturally competent manner with full inclusion of patient confidentiality. Broad guidelines may be more effective for SSA as this lends itself to accommodate the cultural diversity of each country and even regions within specific countries. From these broad guidelines, hospital or clinic leaders can provide specific guidelines based on the local context as this would be helpful to HCPs and caregivers when taking care of their patients and children, respectively. Beyond the perspectives of HCPs and caregivers, the perspectives of people and communities with high HIV burden need to be incorporated in revising or creating local guidelines on HIV disclosure. Other factors, such as facilitators and barriers associated with HIV disclosure to children and adolescents, need to be factored into new guidelines. The degree to which these broad factors are considered in the development and implementation process will likely result in a more successful adoption of disclosure guidelines.
Conclusion
This review evaluated the perspectives of HIV disclosure and practices currently used in delivering age- and culture-sensitive HIV disclosure to children and adolescents by health caregivers or caregivers in SSA. Further evidence has been generated on the emerging topic of HIV disclosure in this region following the advent of ART. Partial disclosure is appropriate for children in SSA up to early adolescence. Caregivers should be involved in disclosing to children, and they require adequate disclosure support from HCPs. On the other hand, full disclosure is suitable for adolescents. Adolescents prefer disclosure by HCPs and they favor peer-group support from committed peers and trained facilitators, to reduce stigma. HCPs need continuous training and adequate resources to disclose in a patient-centered manner. Community members need education in HIV stigma reduction.
The evidence-based information from this review informed the following recommendations. First, caregivers and HCPs require collaborative training to ensure the best interest of infected children and adolescents are addressed throughout the disclosure process. Second, public health education should promote HIV/AIDS as a shared burden and create opportunities for community members to accept families of children and adolescents living with HIV to reduce stigma in the communal life. Inclusion of trained lay providers selected from affected communities may also ensure more culturally acceptable management of HIV disclosure in these communities. Third, family counseling and community education that encourages discussion of sexuality within local norms will empower children and adolescents to make better informed sexual health- or HIV-related choices. Finally, more studies are needed to determine the role of social determinants in HIV disclosure practices in resource-limited communities.
Author Contributions
All the authors made substantial contributions to the conception and design of the work and in the acquisition, analysis, and interpretation of data for the work. They also drafted the work or revised it critically for important intellectual content. Final version of the article to be published was approved by all the authors. They also agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors acknowledge the input of Vickie Lynn, MPH and Samir Dalia, MD, Seiichii Villanola, BA in this work. We also appreciate the constructive critical analysis of the reviewers during the interactive review process.
References
- 1.Murray CJL, Ortblad KF, Guinovart C, Lim SS, Wolock TM, Roberts DA, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (2014) 384:1005–70. 10.1016/S0140-6736(14)60844-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scheibe A, Kanyemba B, Syvertsen J, Adebajo S, Baral S. Money, power and HIV: economic influences and HIV among men who have sex with men in sub-Saharan Africa. Afr J Reprod Health (2014) 18:84–92. [PubMed] [Google Scholar]
- 3.AIDS.gov HIV/AIDS Basics. Washington, DC: U.S. Department of Health & Human Services; (2015). [Google Scholar]
- 4.Joint United Nations Programme on HIV/AIDS (UNAIDS). AIDS by the Numbers 2015. Geneva: UNAIDS; (2015). p. 1–12. [Google Scholar]
- 5.Joint United Nations Programme on HIV/AIDS (UNAIDS). Fact Sheet 2015. Geneva: UNAIDS; (2015). p. 1–9. [Google Scholar]
- 6.WHO, UNICEF. Global HIV/AIDS Response: Epidemic Update and Health Sector Progress towards Universal Access: Progress Report. (2011). p. 1–229.
- 7.Hardon A, Desclaux A, Lugalla J. Disclosure in times of ART: a relational analysis of social practices. SAHARA J (2013) 10:S1–4. 10.1080/02664763.2012.755317 [DOI] [PubMed] [Google Scholar]
- 8.Ortblad KF, Lozano R, Murray CJ. The burden of HIV: insights from the Global Burden of Disease (GBD) study 2010. Lancet (2013) 381(Suppl 2):S103. 10.1016/S0140-6736(13)61357-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roser M. HIV/AIDS – Our World in Data. Oxford: Our World in Data; (2015). [Google Scholar]
- 10.Biadgilign S, Deribew A, Amberbir A, Deribe K. Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: a qualitative study. SAHARA J (2009) 6:148–54. 10.1080/17290376.2009.9724943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kallem S, Renner L, Ghebremichael M, Paintsil E. Prevalence and pattern of disclosure of HIV status in HIV-infected children in Ghana. AIDS Behav (2011) 15:1121–7. 10.1007/s10461-010-9741-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Guideline on HIV Disclosure Counselling for Children up to 12 Years of Age. Geneva: WHO; (2011). [PubMed] [Google Scholar]
- 13.Turissini ML, Nyandiko WM, Ayaya SO, Marete I, Mwangi A, Chemboi V, et al. The prevalence of disclosure of HIV status to HIV-infected children in Western Kenya. J Pediatr Infect Dis Soc (2013) 2(2):136–43. 10.1093/jpids/pit024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abebe W, Teferra S. Disclosure of diagnosis by parents and caregivers to children infected with HIV: prevalence associated factors and perceived barriers in Addis Ababa, Ethiopia. AIDS care (2012) 24:1097–102. 10.1080/09540121.2012.656565 [DOI] [PubMed] [Google Scholar]
- 15.Mialky E, Vagnoni J, Rutstein R. School-age children with perinatally acquired HIV infection: medical and psychosocial issues in a Philadelphia cohort. AIDS Patient Care STDS (2001) 15:575–9. 10.1089/108729101753287667 [DOI] [PubMed] [Google Scholar]
- 16.Thorne C, Newell ML, Peckham CS. Disclosure of diagnosis and planning for the future in HIV-affected families in Europe. Child Care Health Dev (2000) 26:29–40. 10.1046/j.1365-2214.2000.00128.x [DOI] [PubMed] [Google Scholar]
- 17.Wilfert C, Beck M, Fleischman AR, Mofenson LM, Pantell RH, Schonberg SK, et al. Disclosure of illness status to children and adolescents with HIV infection. American Academy of Pediatrics Committee on Pediatrics AIDS. Pediatrics (1999) 103:164–6. 10.1542/peds.103.1.164 [DOI] [PubMed] [Google Scholar]
- 18.Joint United Nations Programme on HIV/AIDS (UNAIDS). Global Report UNAIDS Report on the Global AIDS Epidemic 2013. Geneva: (2013). [Google Scholar]
- 19.Fielden SJ, Sheckter L, Chapman GE, Alimenti A, Forbes JC, Sheps S, et al. Growing up: perspectives of children, families and service providers regarding the needs of older children with perinatally-acquired HIV. AIDS Care (2006) 18:1050–3. 10.1080/09540120600581460 [DOI] [PubMed] [Google Scholar]
- 20.Vreeman RC, Gramelspacher AM, Gisore PO, Scanlon ML, Nyandiko WM. Disclosure of HIV status to children in resource-limited settings: a systematic review. J Int AIDS Soc (2013) 16:18466. 10.7448/IAS.16.1.18466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Baets AJ, Sifovo S, Parsons R, Pazvakavambwa IE. HIV disclosure and discussions about grief with Shona children: a comparison between health care workers and community members in Eastern Zimbabwe. Soc Sci Med (2008) 66:479–91. 10.1016/j.socscimed.2007.08.028 [DOI] [PubMed] [Google Scholar]
- 22.Loubiere S, Peretti-Watel P, Boyer S, Blanche J, Abega S-C, Spire B. HIV disclosure and unsafe sex among HIV-infected women in Cameroon: results from the ANRS-EVAL study. Soc Sci Med (2009) 69:885–91. 10.1016/j.socscimed.2009.05.044 [DOI] [PubMed] [Google Scholar]
- 23.Mburu G, Hodgson I, Teltschik A, Ram M, Haamujompa C, Bajpai D, et al. Rights-based services for adolescents living with HIV: adolescent self-efficacy and implications for health systems in Zambia. Reprod Health Matters (2013) 21:176–85. 10.1016/S0968-8080(13)41701-9 [DOI] [PubMed] [Google Scholar]
- 24.Demmer C. Experiences of families caring for an HIV-infected child in KwaZulu-Natal, South Africa: an exploratory study. AIDS Care (2011) 23:873–9. 10.1080/09540121.2010.542123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gyamfi E, Okyere P, Appiah-Brempong E, Adjei RO, Mensah KA. Benefits of disclosure of HIV status to infected children and adolescents: perceptions of caregivers and health care providers. J Assoc Nurses AIDS Care (2015) 26:770–80. 10.1016/j.jana.2015.08.001 [DOI] [PubMed] [Google Scholar]
- 26.Kajubi P, Whyte S, Muhumuza S, Kyaddondo D, Katahoire AR. Communication between HIV-infected children and their caregivers about HIV medicines: a cross-sectional study in Jinja district, Uganda. J Int AIDS Soc (2014) 17:19012. 10.7448/IAS.17.1.19012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kidia KK, Mupambireyi Z, Cluver L, Ndhlovu CE, Borok M, Ferrand RA. HIV status disclosure to perinatally-infected adolescents in Zimbabwe: a qualitative study of adolescent and healthcare worker perspectives. PLoS One (2014) 9(1):e87322. 10.1371/journal.pone.0087322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Midtbo V, Shirima V, Skovdal M, Daniel M. How disclosure and antiretroviral therapy help HIV-infected adolescents in sub-Saharan Africa cope with stigma. Afr J AIDS Res (2012) 11:261–71. 10.2989/16085906.2012.734987 [DOI] [PubMed] [Google Scholar]
- 29.Moodley K, Myer L, Michaels D, Cotton M. Paediatric HIV disclosure in South Africa – caregivers’ perspectives on discussing HIV with infected children. S Afr Med J (2006) 96:201–4. [PubMed] [Google Scholar]
- 30.Kiwanuka J, Mulogo E, Haberer JE. Caregiver perceptions and motivation for disclosing or concealing the diagnosis of HIV infection to children receiving HIV care in Mbarara, Uganda: a qualitative study. PLoS One (2014) 9:e93276. 10.1371/journal.pone.0093276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lorenz R, Grant E, Muyindike W, Maling S, Card C, Henry C, et al. Caregivers’ attitudes towards HIV testing and disclosure of HIV status to at-risk children in rural Uganda. PloS one (2016) 11:e0148950. 10.1371/journal.pone.0148950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beima-Sofie K, John-Stewart G, Shah B, Wamalwa D, Maleche-Obimbo E, Kelley M. Using health provider insights to inform pediatric HIV disclosure: a qualitative study and practice framework from Kenya. AIDS Patient Care STDS (2014) 28(555–64):10. 10.1089/apc.2014.0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mumburi LP, Hamel BC, Philemon RN, Kapanda GN, Msuya LJ. Factors associated with HIV-status disclosure to HIV-infected children receiving care at Kilimanjaro Christian Medical Centre in Moshi, Tanzania. Pan Afr Med J (2014) 18:50. 10.11604/pamj.2014.18.50.2307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Myer L, Moodley K, Hendricks F, Cotton M. Healthcare providers’ perspectives on discussing HIV status with infected children. J Trop Pediatr (2006) 52:293–5. 10.1093/tropej/fml004 [DOI] [PubMed] [Google Scholar]
- 35.Corneli A, Vaz L, Dulyx J, Omba S, Rennie S, Behets F. The role of disclosure in relation to assent to participate in HIV-related research among HIV-infected youth: a formative study. J Int AIDS Soc (2009) 12:17. 10.1186/1758-2652-12-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gachanja G, Burkholder GJ. A model for HIV disclosure of a parent’s and/or a child’s illness. PeerJ (2016) 4:e1662. 10.7717/peerj.1662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Odiachi A, Abegunde D. Prevalence and predictors of pediatric disclosure among HIV-infected Nigerian children on treatment. AIDS Care (2016) 28(8):1046–51. 10.1080/09540121.2016.1147018 [DOI] [PubMed] [Google Scholar]
- 38.Toska E, Cluver LD, Hodes R, Kidia KK. Sex and secrecy: how HIV-status disclosure affects safe sex among HIV-positive adolescents. AIDS Care (2015) 27:47–58. 10.1080/09540121.2015.1071775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vaz LM, Maman S, Eng E, Barbarin OA, Tshikandu T, Behets F. Patterns of disclosure of HIV status to infected children in a sub-Saharan African setting. J Dev Behav Pediatr (2011) 32:307–15. 10.1097/DBP.0b013e31820f7a47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Watermeyer J. ‘Are we allowed to disclose?’: a healthcare team’s experiences of talking with children and adolescents about their HIV status. Health Expect (2015) 18:590–600. 10.1111/hex.12141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vaz LME, Eng E, Maman S, Tshikandu T, Behets F. Telling children they have HIV: lessons learned from findings of a qualitative study in sub-Saharan Africa. AIDS Patient Care STDS (2010) 24:247–56. 10.1089/apc.2009.0217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Skovdal M, Daniel M. Resilience through participation and coping-enabling social environments: the case of HIV-affected children in sub-Saharan Africa. Afr J AIDS Res (2012) 11:153–64. 10.2989/16085906.2012.734975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krauss BJ, Letteney S, De Baets AJ, Baggaley R, Okero FA. Caregiver’s HIV disclosure to children 12 years and under: a review and analysis of the evidence. AIDS Care (2013) 25:415–29. 10.1080/09540121.2012.712664 [DOI] [PubMed] [Google Scholar]
- 44.Amzel A, Toska E, Lovich R, Widyono M, Patel T, Foti C, et al. Promoting a combination approach to paediatric HIV psychosocial support. AIDS (2013) 27(Suppl 2):S147–57. 10.1097/QAD.0000000000000098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lipson M. What do you say to a child with AIDS? Hastings Cent Rep (1993) 23:6–12. 10.2307/3562811 [DOI] [PubMed] [Google Scholar]
- 46.Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV disclosure across diverse settings: a review. Am J Public Health (2011) 101:1011–23. 10.2105/AJPH.2010.300102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lesch A, Swartz L, Kagee A, Moodley K, Kafaar Z, Myer L, et al. Paediatric HIV/AIDS disclosure: towards a developmental and process-oriented approach. AIDS Care (2007) 19:811–6. 10.1080/09540120601129301 [DOI] [PubMed] [Google Scholar]
- 48.World Health Organization. WHO Recommends HIV Testing By Lay Providers. Geneva: WHO; (2015). [Google Scholar]
- 49.Koyio LN, Sanden WJ, Dimba E, Mulder J, Creugers NH, Merkx MA, et al. Oral health training programs for community and professional health care workers in Nairobi East district increases identification of HIV-infected patients. PLoS One (2014) 9:e90927. 10.1371/journal.pone.0090927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lema IA, Sando D, Magesa L, Machumi L, Mungure E, Mwanyika Sando M, et al. Community health workers to improve antenatal care and PMTCT uptake in Dar es Salaam, Tanzania: a quantitative performance evaluation. J Acquir Immune Defic Syndr (1999) 2014(67):S195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mushamiri I, Luo C, Iiams-Hauser C, Ben Amor Y. Evaluation of the impact of a mobile health system on adherence to antenatal and postnatal care and prevention of mother-to-child transmission of HIV programs in Kenya. BMC Public Health (2015) 15:102. 10.1186/s12889-015-1358-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scheffler RM, Mahoney CB, Fulton BD, Dal Poz MR, Preker AS. Estimates of health care professional shortages in sub-Saharan Africa by 2015. Health Aff (Millwood) (2009) 28:w849–62. 10.1377/hlthaff.28.5.w849 [DOI] [PubMed] [Google Scholar]
- 53.Tankwanchi AB, Ozden C, Vermund SH. Physician emigration from sub-Saharan Africa to the United States: analysis of the 2011 AMA physician masterfile. PLoS Med (2013) 10:e1001513. 10.1371/journal.pmed.1001513 [DOI] [PMC free article] [PubMed] [Google Scholar]


