Abstract
Background
Since the late 1970s there have been sporadic reports of nosocomial infections linked to endoscopic procedures. Infections by multidrug-resistant organisms (MDRO) have an increasing impact on healthcare systems worldwide. Since 2010 outbreaks involving MDRO have been reported as a result of endoscopic retrograde cholangiopancreatography (ERCP) from the USA, France, Germany and the Netherlands.
Methods
This article evaluates the recent outbreaks and developments and demonstrates a structural approach to how to prevent future infections. Current national and international guidelines were used as a basis for discussions.
Results
In some cases insufficient cleaning or drying supported the outbreak. In the majority of cases, outbreaks occurred despite the apparently appropriate reprocessing protocols being in use. Microlesions were identified on a number of endoscopes, which supported the growth of bacteria and represented a vehicle for the transmission of infectious material. National official bodies responded with warnings. Manufacturers informed their customers accordingly. Separate, purpose-designed reprocessing rooms and a sufficient number of competent staff provide the structural quality for a safe reprocessing. The process quality includes a thorough cleaning of all endoscope channels and crucial instrument components, followed by an automated and validated reprocessing procedure. Strict adherence to manufacturers' recommendations is essential. The outcome quality should be evaluated by regular audits, validation of reprocessing procedures and microbiological surveillance. If outbreaks occur, a close co-operation with official bodies and manufacturers is essential.
Conclusion
Health care professionals and manufacturers should be aware of their responsibility to ensure patient safety. A structural approach is key in prevention of endoscopy-associated infections.
Keywords: Endoscopy, Duodenoscope design, Reprocessing, Multidrug-resistant organisms (MDRO), Infection control
Introduction
Flexible endoscopes are complex and sophisticated instruments inserted into the human body through natural orifices for diagnosis and/or therapeutic purposes in all areas of the digestive tract. Gastrointestinal endoscopes with external diameters of approximately 0.3-1.4 cm contain narrow-gauge channels for aspiration, flushing and passage of additional endoscopic equipment. This design enables direct non-surgical treatment with tissue sampling, haemostasis, stricture dilation and manipulation of the biliopancreatic system. Specially modified endoscopes are required for treating common bile duct stones or strictures in the pancreatic and biliary ducts (stents). These instruments have a side-viewing lens and an additional channel with a guidewire for manipulating the endoscopic probes up and down (the elevator wire channel).
Due to this constant stress, endoscopes, in particular for endoscopic retrograde cholangiopancreatography (ERCP), are subject to constant mechanical wear and require frequent repair. Efficient reprocessing is required when used in highly colonised areas (colon) or sterile areas of the body (biliary duct, pancreatic duct).
Reprocessing
Due to their complex design, endoscopes cannot be sterilised. Sterilisation is defined as the complete destruction of all micro-organisms including bacterial spores. The endoscope design would not withstand the high temperatures (>200 °C) used in sterilisation processes [1].
Endoscopes are classed as semi-critical instruments and are therefore disinfected. Disinfection means irreversible inactivation or destruction of a substantial proportion of the micro-organisms, in numbers that allow safe reuse of the instrument.
There are 6 steps involved in the reprocessing of flexible endoscopes [1,2,3]:
(pre-)cleaning with function control
cleaning including a leak test and manual cleaning by brushing all accessible channels and critical components
rinsing
disinfection
neutralisation in the form of a final rinse, and drying;
transport and storage in a safe environment to avoid recontamination.
Brushing all channels in the cleaning step alone leads to a 4-6 log reduction in micro-organisms. This procedure is, therefore, critically important for the subsequent disinfection step, whether manual or automated. The disinfection step causes an additional 4-6 log bacterial reduction with killing of all viruses and mycobacteria. Nowadays disinfection is predominantly carried out in endoscope washer disinfectors (EWDs), using glutaraldehyde or peracetic acid. The entire reprocessing procedure therefore has a bacterial reduction of up to 12 log cycles. In American guidelines this is called ‘high-level disinfection’ [2,3].
Reprocessing of flexible endoscopes is considered to be a safe process. However, the margin of safety is minimal. With the normal bacterial load for instruments of up to 10 log cycles and an elimination rate of 8-12 log10, reprocessing only provides a 0-2 log margin of safety when properly conducted. Therefore, any deviation from reprocessing protocols could lead to a decrease in bacterial reduction, increasing potential risk of patient-to-patient transmission [2]. Drying is conducted partly in the EWD, partly manually. Drying cabinets are increasingly used for automated drying and safe storage in a controlled environment.
In contrast to the endoscopes, additional endoscopic equipment (forceps, polypectomy snares, papillotomes) must be sterile. These damage internal surfaces and are classed as critical instruments due to their contact with blood and lymph vessels [1,4]. They are predominantly supplied as single-use devices. Although reprocessing of biopsy forceps, for example, is possible in principle under sterile conditions, single-use instruments are currently preferred due to their wide availability, the benefit of traceability and low pricing [5]. The hygiene process is therefore subjected to particular attention and monitoring in endoscopy.
Studies performed 10-15 years ago showed the vulnerability and limits of this procedure. The Bavarian HYGEA study (2000) and the later QSHE study (2002), which studied endoscopic units (practices and clinics) directly, reported a high level of microbial contamination (15-50%) following reprocessing, predominantly with waterborne bacteria (Pseudomonas aeruginosa) [6,7]. Problems were more common with manual reprocessing alone than for automated procedures, and also in units with fewer than 100 endoscopies per quarter. Both studies identified significant deficiencies in materials and use. These involved in particular insufficient brushing, inappropriate reprocessing of water bottles and lapses in drying. The studies showed that automated reprocessing preceded by brush cleaning yielded the most reliable results, since human error is a non-negligible factor in manual cleaning and disinfection.
Standards and Recommendations
Over the last 10 years national and international companies have tightened up guidelines on the cleaning and disinfection of endoscopes in gastrointestinal endoscopy. The European guidelines (ESGE - ESGENA 2000, 2003, 2007, 2008) have been revised and amended several times in recent years [1,8,9,10,11]. The German recommendations of the Robert Koch Institute (Hygiene requirements for the reprocessing of flexible endoscopes and additional endoscopic equipment) were last revised in 2012 [12,13]. US and Australian guidelines are revised regularly [3,4,14,15,16].
As well as a warning to comply strictly with the measures, the German and European guidelines in particular emphasise the need for periodic microbiological surveillance. This recommendation for the endoscopes to be checked every 3 months is missing in the US guidelines since the evidence-based approach of microbiological surveillance is controversially discussed [16].
Reprocessing of flexible endoscopes has hitherto been considered as safe, provided that the strict conditions of the national and international professional associations are complied with [1,13]. Since the 1970s there have been recurring sporadic reports of endoscopy-associated infections. These isolated infections following endoscopic interventions were generally traced to non-compliance with the standardised protocols [17,18].
The Problem of Multidrug-Resistant Gut Microbiota and Duodenoscopes
Recent publications and reports have shown just how minimal the margin of safety in endoscopic reprocessing is. The series of ERCP-associated infections with multidrug-resistant pathogens in the US have prompted special attention and media interest.
In 2013, 39 cases of carbapenem-resistant Escherichia. coli/New-Delhi-metallo-β-lactamase (NDM+) were identified in a hospital in Illinois, USA. Stool samples tested positive for bacteria [19]. The instrument triggering the infection was identified as the duodenoscope. Although the endoscope did not subsequently test positive for bacteria, and there was no breach in the reprocessing protocol, changing from disinfection with aldehyde to gas sterilisation with ethylene oxide halted the infection.
In a hospital in Seattle, 32 cases of multidrug-resistant E. coli occurred [19]. All patients had been treated by ERCP. 16 patients (7 within 31 days) died during follow-up. However, the high comorbidity for these patients meant that the relevance of the bacterial infection to the cause of death was unclear. A critical inspection of the reprocessing process did not identify any breaches of any of the procedures. However, 4 out of 8 duodenoscopes were contaminated; 3 out of the contaminated 4 were critically malfunctional and had microlesions that were discovered during the then introduced servicing of the devices. However, despite the introduction of new requirements for quality management and infection control, with replacement of all endoscopes and bacteriological controls after each procedure with 48-hour quarantine, there was still a 2% positive bacterial culture within a year. Critical questions are therefore being asked on the actual efficiency of conventional reprocessing protocols [20,21].
Finally the infection series in France, Germany and the Netherlands have shown that the infections with multidrug-resistant micro-organisms are not restricted to America [22,23,24]. Between December 2008 and August 2009, 16 patients in France tested positive for multidrug-resistant Klebsiella pneumoniae (ESBL type CTX-M-15; 8 bloodstream infections, 4 biliary tract infections and 4 cases of faecal carriage). However, a review of reprocessing did identify lapses in the manual cleaning and drying steps. The outbreak ended following strict compliance with the reprocessing guidelines [22].
A similar report of carbapenem-resistant K. pneumoniae (CRKP) was published by the Charité Berlin [23]. From December 2012 to January 2013, 6 patients undergoing ERCP with the same endoscope tested positive for predominantly rectal bacteria. In this case no CRKP microbial growth was subsequently detected on the instrument itself. However, enterococci were detected on another duodenoscope during routine checks. The presence of enterococci, bacterial indicators for lapses in cleaning, suggests that there may have been irregularities in the manual cleaning process [9,13,25]. An end to the infection was achieved after the endoscopes were serviced, where once again minor defects were discovered at the distal end and the outer sheath.
A rise in pseudomonas infections was noted in a clinic in Rotterdam in early 2012, following which the usual screening methods and follow-up investigations were initiated [24]. By April 2013, 30 patients were identified with VIM-2-positive P. aeruginosa, 22 of whom had been treated by ERCP. The distal end of the endoscope below the elevator lever tested positive for bacteria. Problems due to wear and tear - sludge behind the glass lens, faulty sealing O-ring and on the enclosed elevator wire channel - led to it being sent back to the manufacturer, following which contamination ceased [24]. No lapses in reprocessing were detected in the Netherlands production series.
Outbreaks of multidrug-resistant bacteria are not just a problem in gastrointestinal endoscopy. Outbreaks have also been reported in bronchoscopy [26].
What Changes Have There Been to Duodenoscopes and the Bacteriological Spectrum?
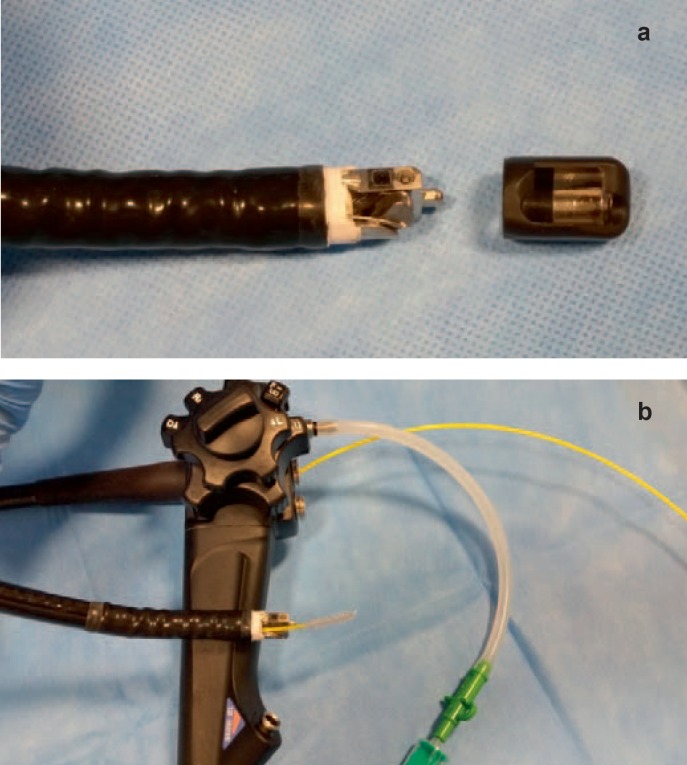
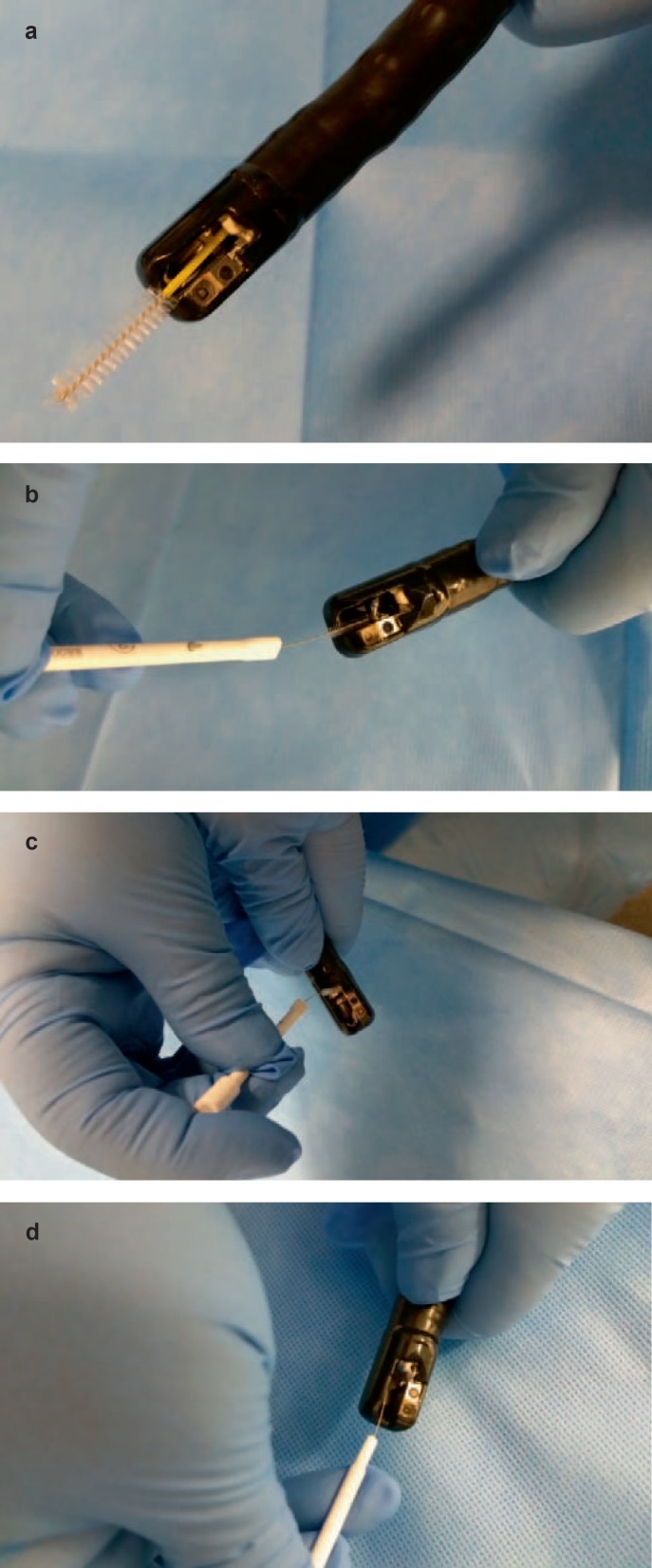
Side-viewing endoscopes fitted with an elevator wire channel system have always had a zone in and around the forceps elevator that is difficult to access for cleaning and disinfection purposes. Manufacturers (Olympus, Pentax, and Fuji) have a range of designs to move the elevator. Whereas an earlier production series (Olympus TJF-160) had a fully open elevator wire channel for moving the elevator, as well as a connection on the endoscope control for flushing this narrow channel, the new TJF-180 series has a completely sealed guidewire channel. In addition, the distal end of the endoscope is completely fixed, whereas earlier series had a removable distal cap making it easier to clean and disinfect. The majority of infections were associated with the new type (TJF-180, Olympus) [27,28] (fig. 1). The manufacturer has warned repeatedly that due to its particular design a special cleaning brush must be used for the pre-cleaning. This smaller brush has a more compact design and finer brush fibres than the usual types of brush (fig. 2, 3). It is not clear how consistently this recommendation was followed.
Fig. 1.

Cleaning brushes in different sizes.
Fig. 2.
a Removable distal end (Olympus TJF 160) with rinsable elevator wire channel. b Brushing of biopsy channel and flushing of elevator wire channel before EWD reprocessing.
Fig. 3.
a Brushing of biopsy and suction channel. b-d Brushing of small components of elevator mechanism.
The US Food and Drug Administration (FDA) has responded to the repeated series of infections from duodenoscopes by issuing safety communications in February, May and August 2015 [29]. This warns of the particular problem of the distal end of duodenoscopes and the difficulty of cleaning it with the risk of residual bacterial clusters. It urgently recommends that reprocessing of duodenoscopes be conducted meticulously, in strict compliance with the manufacturer's specifications. It also advises that patients be informed of the risk of bacterial transmission in ERCP [29].
Likewise, the German Federal Institute for Drugs and Medical Devices (Bundesinstitut für Arzneimittel und Medizinprodukte; BfArM) and the Robert Koch Institute have also commented on this problem in their 07/2015 Circular. Due to the cluster of infections with multidrug-resistant pathogens together with the design problems of the instruments, a warning was issued to comply strictly with the reprocessing steps [30].
Today, duodenoscopes have various designs for the distal end [31]. There are 4 different forms that allow the elevator to be moved:
— a fixed distal end and a rinsable elevator channel (Fujinon, old version of Olympus);
— a fixed distal end and a sealed elevator channel (Olympus 180 and Pentax);
— a removable distal end and a rinsable elevator channel (Olympus 160);
— a removal end that can be completely disassembled and autoclaved together with an elevator wire channel system through which a brush can be passed (Storz).
Apart from the fourth design, all instruments from the various manufacturers have been affected by infections.
The serial infections all tested positive to multidrug-resistant gut flora (carbapenem-resistant Enterobactericeae; CRE), which pose an additional therapeutic problem. Bacteria that are resistant to 3 different classes of antibiotics (3 MRGN - multiresistant Gram-negative) can still be treated with the substance carbapenem. However, if they are resistant to this group, there is a 4-level problem (4 MRGN) and virtually no antibiotics are effective against this type of infection [32,33]. Multiresistant CRE (‘superbugs’) may contain enzymes (carbapenemnase) that hydrolyse the β-lactam ring of the antibiotic and inactivate the substance. Due to the lack of efficient antibiotics mortality can rise to 40-50%. Multiresistant CRE bacteria are also capable of transmitting genetic material [27]. Several strains of carbapenemnase-producing gut bacteria have been detected following infections via duodenoscopes [32].
K. pneumoniae carbapenemnase (KPC)-producing Enterobactericeae were found in Berlin [23] and during the outbreak in France [22]. NDM-1 (New Delhi metallo-β-lactamase-1 E. coli) caused the infection in Illinois [19]. VIM-producing Enterobactericeae were identified as triggering the infection in the Netherlands [24].
In September 2015, Petersen [28] summarised the situation in the USA: 4 institutions were affected according to medical publications; 5 further localisations have been made public. While there was 1 cluster prior to 2010, the most frequent outbreaks were recorded between 2012 and 2014; 20 patients died in 60 clinical infections, and 1,000 patients were at the screening stage, of whom > 100 were non-symptomatic bacteria carriers.
Instruments from all 3 major endoscope manufacturers are affected, which all offer different designs for side-view instruments. The problem is primarily seen as the permanent contamination in and around the elevator and the elevator wire channel as well as the lack of cleaning accessibility. Prevalence is increasing. What is disturbing is the bacterial resistance and limited treatment options despite so-called ‘high-level disinfection’ (2%). Patients with advanced tumours and immunosuppression are seen as at the highest risk. Diagnosis is delayed due to the need to wait for clinical verification, which is often weeks and months after the endoscopic examination. Mortality is increasing.
The current duodenoscope-associated infection series caused by multidrug-resistant gut flora has the following key characteristics. The starting point is an increase in infections with multidrug-resistant pathogens in healthcare units and in hospitals. The patient's gut acts as the reservoir for the pathogens. It is therefore primarily not endoscoped patients, but patients who are bacterial carriers who transmit the bacteria to other non-affected patients via environmental contamination (hands, sanitary areas - toilets, wash basins, showers, door handles). Poor hand hygiene by clinic staff plays a crucial role in further spreading the bacteria [23,27]. The duodenoscope, due to its complex design that makes reprocessing difficult, becomes a transmitter of bacteria unless reprocessing achieves total bacterial elimination [18,19,20,21,22,23,24,34]. Since infections with these bacteria do not necessarily occur immediately after an endoscopic intervention, and transmitter patients from other wards are not necessarily endoscoped, the underlying route of these bacterial outbreaks is difficult to ascertain. They are therefore difficult to trace. There is some speculation that the current series of infections may only be the tip of the iceberg [34].
Ensuring Reprocessing Quality and Infection Prevention
What lessons can we learn from this new situation? What structures, behaviours and control mechanisms are needed in terms of structure, process and outcome quality to prevent infections?
Reprocessing Units
A separate, purpose-equipped reprocessing room is a requirement in all national and international guidelines and is now the standard [1,2,3,4,8,9,10,11,12,13,14,15,16,35]. Strict spatial and procedural separation of contaminated and clean work steps is crucial for occupational safety and prevention of recontamination, with the current trend towards two-room concepts [35]. Centralised reprocessing units are now established either in the endoscopy unit or the central sterile services departments.
Qualification and Awareness of Responsibilities
Endoscopes are medical devices with a complex design, which require detailed specialist knowledge and special care during reprocessing. Guidelines and healthcare regulatory bodies require that only qualified personnel reprocess endoscopes. Special training programmes have been established in many countries to communicate the aspects of hygiene, infection prevention, reprocessing procedures and instrument technology.
In addition to a general qualification, personnel must be familiar with the special design of each endoscope used in the respective endoscopy department; this also applies to endoscopes on loan. General reprocessing recommendations are not sufficient here. Detailed reprocessing protocols for each endoscope are fundamental to safe reprocessing. Staff must for example have a detailed knowledge of the channels and specific components such as the structure of the elevator system to be able to conduct reprocessing correctly.
These standard operating procedures should be retained even after instruments are taken out of service. In the outbreak in the Netherlands [24] these reprocessing standards could not be produced as evidence of correct reprocessing, which in the event of audits by the regulatory bodies may well also bring legal problems with it. The reported outbreaks in the past and the reported case from France were traced to reprocessing errors [1,22].
There are various endoscope models from different manufacturers on the market for the various endoscopic interventions. In the current ERCP-related outbreaks, the design of the distal end was discussed as potential cause of the infections [19,24,34]. This underlines not only the need for intensive training and instruction in use of the instrument but also makes the duty to report and notify clear: If the user thinks that the design of a medical device (endoscope) makes it difficult to reprocess it correctly or discovers problems with the use of the instrument, it is his professional duty to contact the manufacturer immediately. If problems persist they must be notified to the relevant authorities. These contacts should not be left until an outbreak occurs but should occur at the first signs of a problem. In Germany there is a duty to report to the BfArM, in the USA to the FDA [12,36]. This is essential to enable the manufacturer to respond to problems with the instruments, provide solutions and assistance. In the case of serious incidents the authorities may issue warnings and initiate investigations, as has occurred in Germany and the USA [29,30].
Hand Hygiene - Tools for Infection Prevention
The outbreaks with multidrug-resistant bacteria demonstrate the complex interaction between personal hygiene and patient-to-patient transmission. The hands of patients and staff, the patient environment and objects function as vehicles of transmission. Correct, hygiene-conscious behaviour by staff is crucial in ensuring patient and staff safety. The WHO Guidelines on Hand Hygiene have been implemented globally via national campaigns [37].
In addition to staff qualifications, the number of available staff also affects hygiene quality. Hugonnet et al. [38] evaluated hospital infections in intensive care wards and calculated that 27% of infections could have been prevented by adequate staffing levels. A review of 96 studies confirms low hand hygiene compliance at inadequate staffing levels and high workloads [39].
Data show the positive effect of training on patient safety [39,40,41] Pittet et al. [40] showed that hospital-wide hygiene campaigns with training led to a reduction in hospital infections (from 16.9% to 9.9% in 4 years; p = 0.04), and reduced methicillin-resistant Staphylococcus aureus (MRSA) infections from 2.16 to 0.93 cases per 10,000 patient days (p < 0.001) [37]. Santos et al. [41] evaluated hand hygiene compliance in endoscopy. Due compliance with hand hygiene was initially 21.4% in total (medical staff 15%, nursing staff 30.5%). After training and a 10-month interval, due compliance with hand hygiene rose to 73% in total (medical staff 69.4% and nursing staff 83.3%).
Working in a hygienically correct way with patients and during reprocessing is the most important tool in infection prevention.
Reprocessing and Design Issues
Today, standardised and validated reprocessing procedures performed in EWD is recommended in principle in all guidelines. The manual cleaning step is extremely important, even if automated reprocessing is performed, to loosen coarse impurities from critical components and narrow inner lumens efficiently. This thorough cleaning is essential for successful disinfection [1,3,13]. If residual contaminants are left in the instrument, disinfection may fail under certain circumstances [1,2,3,13,18].
Manufacturers are required by law to provide precise recommendations for reprocessing their medical devices. It is the responsibility of users to familiarise themselves with the design of the endoscope including the channels in detail.
Once pre-cleaning has been completed by flushing/suction of the endoscope channels in the examination room, manual cleaning including leak testing and manual brush cleaning is conducted in the reprocessing room.
Outbreaks in intensive care wards with bronchoscopes and transesophageal echocardiogram (TEE) probes were traced to damage to instruments and a lack of leak testing [18,42,43]. In the current ERCP-associated outbreaks minor defects were detected on the duodenoscopes at the distal end, on the outer sheath, on the elevator enclosure and on cover lenses, which were apparently not discovered during reprocessing or during use of the instruments, but only following the outbreak during servicing [19,20,21,22,23,24]. Due to these defects, organic material in the interior of the endoscope was able to function as a bacterial growth medium (bio films). It is not explicitly emphasised in the publications whether the leak test required by the manufacturer was always performed, but audits did not discover any lapses in the reprocessing cycle.
Given the hypothesis that the leak test might not always detect very small minor defects, the question arises as to whether more intensive, routine servicing should be established for these complex design, sensitive duodenoscopes. Regular replacement of individual components can also be discussed to rule out microlesions that a leak test cannot capture. Manual brush cleaning is showing a clear trend towards single-use brushes. European, Dutch and UK guidelines recommend exclusively single-use brushes to prevent cross-contamination and to ensure constant high-quality brushes [1,44,45], while the German and US recommendations continue to permit multiple-use brushes, although if these are used they advise consistent reprocessing between individual applications and emphasise brush quality [3,13]. However, the supplementary comments from the Robert Koch Institute emphasise the quality of the cleaning brushes and the difficulties of effective cleaning [46,47], which in turn is an argument for conversion to single-use brushes. Multiple use of single-use brushes in several endoscopes is always to be avoided to prevent cross-contamination.
Duodenoscopes with fixed distal caps and enclosed elevators have been particularly implicated in the current outbreaks [19,20,21,22,23,24]. The instruments require a particularly meticulous and accurate manual cleaning since crevices behind the elevator cannot be reached with conventional brushes. The manufacturer provides particularly small brushes with detailed recommendations on reprocessing, which should be followed.
Removable distal caps have the benefit that critical components such as the forceps elevator are easier to clean manually but require special care to ensure they are correctly fixed before the start of the examination.
If the elevator channel is rinsable, it must first be flushed with detergent at the pre-cleaning stage through a special connector, attached to the EWD and then dried carefully.
Improving the design of duodenoscopes poses a challenge for the manufacturers. A move to the use of materials that permit them to be autoclaved may be considered. There are already some flexible bronchoscopes on the market that can be autoclaved. Sterilisation offers a far greater margin of safety than disinfection [2,27]. Even if individual components or the entire endoscope can be autoclaved, thorough cleaning will still be required to ensure sterilisation is successful.
Process Validation and Microbiological Surveillance
Automated reprocessing procedures using EWDs must be validated in accordance with EN ISO 15883 to evaluate the reprocessing system as a whole. The Operational Qualification (OP) should be tested at the various loadings, which represent the endoscopes from each department [11].
Quality control of the outcome quality of reprocessing cycles in an EWD and the endoscopes can be ensured through routine microbiological controls and regular routine technical controls. They are helpful tools for early detection of deficits, damage and errors in reprocessing [10,11]. In contrast to Europe, microbiological controls are not as yet conducted routinely in the USA. The US guidelines have commented critically in terms of their significance [3]. In summer 2015 the FDA and Center of Disease Control and Prevention (CDC) responded to the outbreaks with multidrug-resistant bacteria. The CDC published a preliminary protocol for microbiological surveillance for duodenoscopes only, which does not, however, cover all channel systems and critical points of the endoscope [48].
The European guidelines, such as the German guidelines, recommend conducting microbiological controls for all classes of endoscopes every 3 months on a rolling basis. Every endoscope in a department should be checked at least once per year. This allows any defects in the instrument that might form bacterial reservoirs and reprocessing errors to be identified early [10,13,25].
However, discussion of microbiological surveillance has also sparked controversy in Europe. These discussions focus on the method selected [34,49,50,51]. In the current outbreaks in France, bacteria tests were only positive following repeated brush swabs [22]. Further studies on method comparison are required [51,] which will be incorporated in a revision of the guidelines.
Outbreak Management
In the event of outbreaks the instruments concerned (endoscopes and EWDs) must first be taken out of service until the cause has been ascertained, defects rectified, services conducted and a microbiological control performed to confirm that the reprocessing is now safe [1,10,13,25].
In the current outbreaks the relevant health regulatory bodies were contacted and the appropriate investigations launched [21,22,23,24,25]. Epstein et al. [19] were only able to end the outbreak by sterilising the duodenoscopes. However, the FDA comments critically on the sterilisation of the endoscopes [29]. Ethylene oxide gas sterilisation or liquid chemical sterilant processing systems are not recommended as routine procedures. The FDA presents the disadvantages of these procedures.
From cases of suspected microbial transmission to the management of outbreaks as well as during the development of novel instruments, it is essential that the endoscopy team collaborate closely with the hospital hygiene and microbiology departments. Where problems or outbreaks occur, the relevant healthcare bodies should be informed promptly and involved in the management at all later stages. Close collaboration with the manufactures is also essential.
Conclusion
Safe reprocessing is key to patient safety in endoscopy. Non-compliance with guidelines and deviations from standardised and validated reprocessing protocols lead to reprocessing faults, with the possibility of patient-to-patient transmission. Current outbreaks with multidrug-resistant bacteria show how narrow the margin of safety is despite compliance with reprocessing protocols. Staff training, adherence to guidelines and manufacturers' specifications and regular hygiene surveillance are important tools in the prevention of infections. If infections occur they should be managed within the multidisciplinary team.
Disclosure Statement
The authors declare that there was no conflict of interests.
References
- 1.Beilenhoff U, Neumann CS, Rey JF, et al. ESGE-ESGENA guideline: Cleaning and disinfection in gastrointestinal endoscopy. Update 2008. Endoscopy. 2008;40:939–957. doi: 10.1055/s-2008-1077722. [DOI] [PubMed] [Google Scholar]
- 2.Rutala WA, Weber DJ. Gastrointestinal endoscopes: A need to shift from disinfection to sterilization? JAMA. 2014;312:1405–1406. doi: 10.1001/jama.2014.12559. [DOI] [PubMed] [Google Scholar]
- 3.Petersen BT, Chennat J, Cohen J, et al. Multisociety guideline on reprocessing flexible gastrointestinal endoscopes: 2011. Gastrointest Endosc. 2011;73:1075–1084. doi: 10.1016/j.gie.2011.03.1183. [DOI] [PubMed] [Google Scholar]
- 4.ASGE Standards of Practice Committee Infection control during GI endoscopy. Gastrointest Endosc. 2008;67:781–790. doi: 10.1016/j.gie.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 5.Jung M, Beilenhoff U, Pietsch M, et al. Standardized reprocessing of reusable colonoscopy biopsy forceps is effective: Results of a German multicentre study. Endoscopy. 2003;35:197–202. doi: 10.1055/s-2003-37270. [DOI] [PubMed] [Google Scholar]
- 6.Bader L, Blumenstock G, Birkner B, et al. HYGEA (Hygiene in der Gastroenterologie-Endoskop-Aufbereitung): Studie zur Qualität in der Aufbereitung von flexiblen Endoskopen in Klinik und Praxis. Z Gastroenterol. 2002;40:157–170. doi: 10.1055/s-2002-22326. [DOI] [PubMed] [Google Scholar]
- 7.Kassenärztliche Vereinigung Bayern. QSHE-Projekt. Gastro-Nachrichten. 2003;37:6–7. [Google Scholar]
- 8.Guidelines on cleaning and disinfection in GI endoscopy. Endoscopy. 2000;32:76–83. [PubMed] [Google Scholar]
- 9.ESGE-ESGENA: Technical notes on cleaning and disinfection (2003) Endoscopy. 2003;35:869–877. doi: 10.1055/s-2003-42626. [DOI] [PubMed] [Google Scholar]
- 10.ESGE-ESGENA guideline for quality assurance in reprocessing microbiological surveillance testing in endoscopy. Endoscopy. 2007;39:175–181. doi: 10.1055/s-2006-945181. [DOI] [PubMed] [Google Scholar]
- 11.Beilenhoff U, Neumann CS, Biering H, et al. ESGE/ESGENA guideline for process validation and routine testing for reprocessing endoscopes in washer−disinfectors, according to the European Standard prEN ISO 15883 parts 1, 4 and 5. Endoscopy. 2007;39:85–94. doi: 10.1055/s-2006-945191. [DOI] [PubMed] [Google Scholar]
- 12.Empfehlungen der Kommission für Krankenhaushygiene und Infektionsprävention beim Robert-Koch-Institut zu den Anforderungen an die Hygiene bei der Aufbereitung flexibler Endoskope und endoskopischen Zusatzinstrumentariums. Bundesgesundheitsbl Gesundheitsforsch Gesundheitssch. 2002;45:395–411. doi: 10.1007/s00103-002-0395-2. [DOI] [PubMed] [Google Scholar]
- 13.Empfehlung der Kommission für Krankenhaushygiene und Infektionsprävention (KRINKO) beim Robert-Koch- Institut (RKI) und des Bundesinstituts für Arzneimittel und Medizinprodukt (BfArM) Anforderungen an die Hygiene bei der Aufbereitung von Medizinprodukten. Bundesgesundheitsbl Gesundheitsforsch Gesundheitssch. 2012;55:1244–1310. doi: 10.1007/s00103-012-1548-6. [DOI] [PubMed] [Google Scholar]
- 14.ASGE Guideline. Reprocessing failure. Gastrointest Endosc. 2007;66:869–871. doi: 10.1016/j.gie.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 15.Gastroenterological Society of Australia Infection Control in Endoscopy 2010 3rd edition. www.gesa.org.au/professional.asp?cid=9&id=123 (last accessed February 2, 2016).
- 16.ASGE Technology Committee. Komanduri S, Abu Dayyeh BK, et al. Technologies for monitoring the quality of endoscope reprocessing. Gastrointest Endosc. 2014;80:369–373. doi: 10.1016/j.gie.2014.01.044. [DOI] [PubMed] [Google Scholar]
- 17.Jung M. Infektionen (septische Komplikationen) nach endoskopischen Eingriffen. Vorbeugung und Therapie. Gastroenterologe. 2014;9:254–259. [Google Scholar]
- 18.Kovaleva J, Peters FTM, van der Mei HC, Degener JE. Transmission of infection by flexible gastrointestinal endoscopy and bronchoscopy. Clin Microbiol Rev. 2013;26:231–254. doi: 10.1128/CMR.00085-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epstein L, Hunter JC, Arwady MA, et al. New Delhi metallo-β-lactamase-producing carbapenem-resistant Escherichia coli associated with exposure to duodenoscopes. JAMA. 2014;312:1447–1455. doi: 10.1001/jama.2014.12720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross AS, Baliga C, Verma P, et al. A quarantine process for the resolution of duodenoscope-associated transmission of multidrug-resistant Escherichia coli. Gastrointest Endosc. 2015;82:477–483. doi: 10.1016/j.gie.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 21.Smith ZL, Young SO, Saeian K, et al. Transmission of carbapenem-resistant Enterobacteriaceae during ERCP: time to revisit the current reprocessing guidelines. Gastrointest Endosc. 2015;81:1041–1045. doi: 10.1016/j.gie.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 22.Aumeran C, Poincloux L, Souweine B, et al. Multidrug-resistant Klebsiella pneumoniae outbreak after endoscopic retrograde cholangiopancreatography. Endoscopy. 2010;42:895–899. doi: 10.1055/s-0030-1255647. [DOI] [PubMed] [Google Scholar]
- 23.Kola A, Piening B, Pape UF, et al. An outbreak of carbapenem-resistant OXA-48-producing Klebsiella pneumonia associated to duodenoscopy. Antimicrob Resist Infect Control. 2015:4–8. doi: 10.1186/s13756-015-0049-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verfaillie CJ, Bruno MJ, Voor in ‘t holt AF, et al. Withdrawal of a novel-design duodenoscope ends outbreak of a VIM-2-producing Pseudomonas aeruginosa. Endoscopy. 2015;47:493–502. doi: 10.1055/s-0034-1391886. [DOI] [PubMed] [Google Scholar]
- 25.Martiny H, Beilenhoff U, Biering H, et al. Methodenbeschreibung zur hygienischen-mikrobiologischen Überprüfung von flexiblen Endoskopen nach ihrer Aufbereitung. HygMed. 2010;35:75–79. ZentralStril 2010;18; 113-117; und Endopraxis 2010;26; 75-79. [Google Scholar]
- 26.Klebisch FR, Schweizer C, Kola A, et al. A flexible bronchoscope as a source of an outbreak with OXA-48 carbapenemase producing Klebsiella pneumonia. Hyg Med. 2015;(40-1/2):8–13. [Google Scholar]
- 27.Muscarella LF. Risk of transmission of carbapenem-resistant enterobactericeae and related ‘superbugs’ during gastrointestinal endoscopy. World J Gastrointest Endosc. 2014;6:457–474. doi: 10.4253/wjge.v6.i10.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Petersen BT. Duodenoscope reprocessing: risk and options coming into view. Gastrointest Endosc. 2015;82:484–486. doi: 10.1016/j.gie.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Food and Drug Administration Medical Device Safety Communications www.fda.gov/MedicalDevices/Safety/AlertsandNotices/default.htm (last accessed January 18, 2016).
- 30.Empfehlungen des BfArM Hinweis des BfArM und des RKI zu komplex aufgebauten Endoskopen (Duodenoskopen), deren Aufbereitung und damit verbundenen Infektionsrisiken 17.07.2015. www.bfarm.de/DE/Medizinprodukte/risikoerfassung/empfehlungen/_node.html (last accessed January 18, 2016).
- 31.Beilenhoff U. ERCP and reprocessing in focus: what can we do to prevent or manage infection outbreaks? Endoscopy. 2015;47:483–485. doi: 10.1055/s-0034-1392153. [DOI] [PubMed] [Google Scholar]
- 32.Gastmeier P, Fätkenheuer G. Infektiologie: Dilemma mit Begriffen und Zahlen. Dtsch Ärztebl. 2015;112:576–578. [Google Scholar]
- 33.Robert Koch-Institut. Definition der Multiresistenz gegenüber Antibiotika bei gramnegativen Stäbchen im Hinblick auf Maßnahmen zur Vermeidung der Weiterverbreitung. Epidemiol Bull RKI. 2011;36:337–339. [Google Scholar]
- 34.Gastmeier P, Vonberg RP. Klebsiella spp. in endoscopy-associated infections: we may only be seeing the tip of the iceberg. Infection. 2014;42:15–21. doi: 10.1007/s15010-013-0544-6. [DOI] [PubMed] [Google Scholar]
- 35.Department of Health Guidance: Management and decontamination of flexible endoscopes. 2013. CFPP 01-06 Decontamination of flexible endoscopes: Design and installation www.gov.uk/government/publications/management-and-decontamination-of-flexible-endoscopes (last accessed January 18, 2016).
- 36.Medizinprodukte-Betreiberverordnung in der Fassung der Bekanntmachung vom 21 August 2002 (BGBl. I S.3396), zuletzt geändert am 25. Juli 2014 (BGBl. I S. 1227).
- 37.WHO Guidelines on Hand Hygiene in Health Care First Global Patient Safety Challenge. Clean Care is Safer Care 2009. www.who.int/gpsc/en/ (last accessed January 18, 2016). [PubMed]
- 38.Hugonnet S, Chevrolet JC, Pittet D. The effect of workload on infection risk in critically ill patients. Crit Care Med. 2007;35:76–81. doi: 10.1097/01.CCM.0000251125.08629.3F. [DOI] [PubMed] [Google Scholar]
- 39.Erasmus V, Daha TJ, Brug H, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31:283–294. doi: 10.1086/650451. [DOI] [PubMed] [Google Scholar]
- 40.Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet. 2000;356:1307–1312. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 41.Santos LY, Souza Dias MB, Borrasca VL, et al. Improving hand hygiene adherence in and endoscopy unit. Endoscopy. 2013;45:421–425. doi: 10.1055/s-0032-1326284. [DOI] [PubMed] [Google Scholar]
- 42.Ramsey AH, Oemig TV, Davis JP, et al. An outbreak of bronchoscopy-related Mycobacterium tuberculosis infections due to lack of bronchoscope leak testing. Chest. 2002;121:976–981. doi: 10.1378/chest.121.3.976. [DOI] [PubMed] [Google Scholar]
- 43.Seki M, Hashiguchi K, Tanaka A, et al. Characteristics and disease severity of healthcare-associated pneumonia among patients in a hospital in Kitakyushu, Japan. J Infect Chemother. 2011;17:363–369. doi: 10.1007/s10156-010-0127-8. [DOI] [PubMed] [Google Scholar]
- 44.The Report of a Working Party of the British Society of Gastroenterology Endoscopy Committee BSG Guidance on for Decontamination of Equipment for Gastrointestinal Endoscopy, June 2014 www.evidence.nhs.uk/search?q=endoscopy%20decontamination (last accessed January 18, 2016).
- 45.Professional Standard Handbook Cleaning and Disinfection. Flexible Endoscopes Version 3.1, 2014. www.infectiepreventieopleidingen.nl/downloads/SFERDHandbook3_1.pdf (last accessed January 18, 2016).
- 46.Kommentar zur Anlage 8 ‘Anforderungen an die Hygiene bei der Aufbereitung flexibler Endoskope und endoskopischen Zusatzinstrumentariums’ der Empfehlung ‘Anforderungen an die Hygiene bei der Aufbereitung von Medizinprodukten’ (1) Epidemiol Bull RKI. 2013;28 [Google Scholar]
- 47.Beilenhoff U, Jung M. Bedeutung des ergänzenden RKI-Kommentars. Endo-Praxis. 2013;29:125–132. [Google Scholar]
- 48.Center of Disease Control and Prevention (CDC) Interim Duodenoscope Surveillance Protocol updated April 3, 2015. www.cdc.gov/hai/organisms/cre/cre-duodenoscope-surveillance-protocol.html (last accessed January 18, 2016).
- 49.Buss AJ, Been MH, Borgers RP, et al. Endoscope disinfection and its pitfalls - requirement for retrograde surveillance cultures. Endoscopy. 2008;40:327–332. doi: 10.1055/s-2007-995477. [DOI] [PubMed] [Google Scholar]
- 50.Kovaleva J, Meessen NE, Peters FT, et al. Is bacteriologic surveillance in endoscope reprocessing stringent enough? Endoscopy. 2009;41:913–916. doi: 10.1055/s-0029-1215086. [DOI] [PubMed] [Google Scholar]
- 51.Saliou P, Baron R. Outbreaks linked to duodenoscopes: microbiological control should be improved. Endoscopy. 2015;47:1058–1059. doi: 10.1055/s-0034-1392650. [DOI] [PubMed] [Google Scholar]