Abstract
The identification of elevated blood pressure (BP) in children and adolescents relies on complex percentile tables. The present study compares the performance of 11 simplified methods for assessing elevated or high BP in children and adolescents using individual-level data from seven countries. Data on BP were available for a total of 58,899 children and adolescents aged 6–17 years from seven national surveys in China, India, Iran, Korea, Poland, Tunisia and the USA. Performance of the simplified methods for screening elevated or high BP were assessed with receiver operating characteristic curve (area under the curve, AUC), sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV). When pooling individual data from the seven countries, all 11 simplified methods performed well in screening high BP, with high AUC values (0.84 to 0.98), high sensitivity (0.69 to 1.00), high specificity (0.87 to 1) and high NPV values (≥0.98). However, PPV was low for most simplified methods, but reached ~0.90 for each of the three methods including sex- and age- specific BP references (at the 95th percentile of height), the formula for BP references (at the 95th percentile of height), and the simplified method relying on a child’s absolute height. These findings were found independently of sex, age and geographical location. Similar results were found for simplified methods for screening elevated BP. In conclusion, all 11 simplified methods performed well for identifying high or elevated BP in children and adolescents, but three methods performed best, and may be most useful for screening purposes.
Keywords: Hypertension, High blood pressure, Children, Adolescents, Epidemiology, Methodology
Introduction
Elevated blood pressure (BP) in pediatric populations is an important public health problem worldwide. Elevated BP is associated with increased risk of target organ damage in children and adolescents.1 Furthermore, elevated BP in childhood tracks into adulthood,2 which increases long-term risk of subclinical atherosclerosis and premature death at adulthood.3–5 Thus, early identification of individuals with elevated BP and adoption of effective measures to lower their BP levels may be an important strategy to reduce risk of cardiovascular diseases and mortality in adulthood.
The United States (US) National Heart, Lung and Blood Institute and the European Society of Hypertension recommend that children aged 3 years and older should have their BP measured either at every medical encounter or annual health examination.6, 7 However, hypertension screening is generally performed less regularly in clinical practice8 and hypertension is frequently underdiagnosed in children whose BP is measured.9 This may arise because physicians believe that there is no sufficient evidence for benefits of hypertension screening in children,10 although the value of early screening of hypertension in children has been questioned.11, 12 In addition, it is quite cumbersome to assess raised BP in children according to sex, age and height.6 In 2004, the Fourth Report of the US National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (later referred as the “Fourth Report”) recommended that pediatric hypertension be defined as systolic/diastolic BP (SBP/DBP) above the 95th percentile by sex, age and height measured on three different occasions.6 The Fourth Report is now widely used in the USA and many European countries. However, there are 476 sex-, age- and height- specific cut-offs to assess the 95th percentile of SBP and DBP among children aged 1–17 years for both sexes, which makes definition of raised BP in children BP cumbersome and time consuming for clinicians although this may be less a problem when electronic medical files are used.9
Alternatively, several simple and more user-friendly tools for screening elevated BP in children and adolescents have been suggested to be used in clinical practice.13 These simplified methods include the use of simple mathematical formulas,14, 15 simplified tables by age and sex with or without height,16–18 and BP to height ratio (BPHR).19, 20
It is therefore useful to compare the performance of these simplified methods in order to know whether these user-friendly methods to assess elevated BP among children and adolescents may be useful for routine screening. To our knowledge, three cross-sectional studies21–23 and one cohort study24 have attempted to compare the performance of several simplified methods. However, these three previous cross-sectional studies had several limitations. First, participants came from a local area or a hospital, and the results might not be representative of the general population. Second, interpretation of some results should be re-assessed. For example, in two validation studies,22, 23 the authors mentioned that the simplified table by Kaelber et al.16 (which provides 64 BP cut-offs by age and sex) performed best, followed by the BPHR (which provides 4 cutoffs for systolic/diastolic BP in boys/girls)19. However, the positive predictive values (PPV) of both methods were lower (Kaelber et al: 16.1%; BPHR: 44.2%) than the simplified methods by Chiolero et al 18 (88.3%) and by Somu et al 14 (86.4%). Another study24 using a cohort design assessed the performance of only two selected methods16, 17 and did not include other available simplified methods.
In the present study, we compare the performance of 11 simplified methods for screening elevated or high BP among 58,899 children and adolescents aged 6–17 years based on data from seven national studies from China, India, Iran, Korea, Poland, Tunisia and the USA.
Methods
Study population
This study is based on individual data from a total of 58,899 children and adolescents aged 6–17 years who had complete data on sex, age, height, weight, and BP from seven large national cross-sectional surveys in China, India, Iran, Korea, Poland, Tunisia and the USA (Table S1). These surveys have been described in detail elsewhere.25–32 Briefly, data from India, Poland and Tunisia were from single cross-sectional surveys while data from China, Iran, Korea and the USA included samples pooled from several cross-sectional surveys [US National Health and Nutrition Examination Survey (NHANES) and Korea National Health and Nutrition Examination Survey (KNHANES)]. All participants were healthy and did not have genetic diseases or acute or serious chronic diseases. In each survey, all participants and their parents provided a written informed consent (the participants in Tunisia provided a verbal informed consent). All surveys had been approved by their respective Institutional Ethics Review Board.
Measurements
BP values were obtained with certified mercury sphygmomanometers by trained examiners following the standard protocol recommended by the AHA in all seven counties.33 In brief, BP was obtained on the right arm of seated children resting for at least 5 minutes using an appropriately sized cuff. The feet of children were resting on a platform during BP measurement. SBP was measured by the onset of the first Korotkoff sound (i.e., appearance of tones) and DBP was recorded by the fifth Korotkoff sound (i.e., total disappearance of tones). Children with DBP equal to zero mmHg were excluded in all datasets. BP was measured up to three times at several minute intervals between readings on one visit. For five countries (China, India, Korea, Poland and the USA), participants had three BP readings, and the mean of the last two readings was used for our analysis; for the other two countries (Iran and Tunisia), two readings were available and the averaged BP value was used for our analysis. Weight and height were measured for each individual in light clothing without shoes. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Overweight and obesity were defined using age- and sex-specific body mass index percentiles as recommended by the International Obesity Task Force.34
Definition of raised BP
High BP defined as SBP/DBP ≥95th percentile by sex, age, and height according to the Fourth Report6 was considered as the “gold standard” for comparison with the 11 simplified methods for 95th percentile values (Table 1). Table 1A shows the 95th percentile BP values for the 5th, 50th and 95th percentiles of a child’s height based on the Fourth Report, consistent with the simplified table by Kaelber et al.16 Table 1B shows the simplified 95th percentile BP values for the 5th, 50th and 95th percentiles of height by age group based on the Fourth Report, consistent with the simplified table by Mitchell et al.17 Table 1C shows formulas that estimate the 95th percentile BP values at the 5th, 50th and 95th percentiles of height based on the Fourth Report, consistent with formulas developed by Somu et al.14 and Badeli et al.15. Table 1D shows the cut-offs of BPHR established by Xi et al. 20 Table 1E shows the 95th percentile BP values for absolute height categories based on the Fourth Report established by Chiolero et al.18
Table 1.
Simplified methods for the identification of high blood pressure in children and adolescents
| A. Simplified table displaying the 95th percentile values of blood pressure (mmHg) based on the Fourth Report at the 5th, 50th and 95th percentiles of a child’s height by sex and age, consistent with the simplified table by Kaelber et al.16
| ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, y | Boys
|
Girls
|
||||||||||
| SBP, mmHg | DBP, mmHg | SBP, mmHg | DBP, mmHg | |||||||||
|
|
|
|||||||||||
| P5(H) | P50(H) | P95(H) | P5(H) | P50(H) | P95(H) | P5(H) | P50(H) | P95(H) | P5(H) | P50(H) | P95(H) | |
| 3 | 104 | 109 | 113 | 63 | 65 | 67 | 104 | 107 | 110 | 65 | 67 | 69 |
| 4 | 106 | 111 | 115 | 66 | 69 | 71 | 105 | 108 | 112 | 68 | 70 | 72 |
| 5 | 108 | 112 | 116 | 69 | 72 | 74 | 107 | 110 | 113 | 70 | 72 | 74 |
| 6 | 109 | 114 | 117 | 72 | 74 | 76 | 108 | 111 | 115 | 72 | 74 | 76 |
| 7 | 110 | 115 | 119 | 74 | 76 | 78 | 110 | 113 | 116 | 73 | 75 | 77 |
| 8 | 111 | 116 | 120 | 75 | 78 | 80 | 112 | 115 | 118 | 75 | 76 | 78 |
| 9 | 113 | 118 | 121 | 76 | 79 | 81 | 114 | 117 | 120 | 76 | 77 | 79 |
| 10 | 115 | 119 | 123 | 77 | 80 | 82 | 116 | 119 | 122 | 77 | 78 | 80 |
| 11 | 117 | 121 | 125 | 78 | 80 | 82 | 118 | 121 | 124 | 78 | 79 | 81 |
| 12 | 119 | 123 | 127 | 78 | 81 | 83 | 119 | 123 | 126 | 79 | 80 | 82 |
| 13 | 121 | 126 | 130 | 79 | 81 | 83 | 121 | 124 | 128 | 80 | 81 | 83 |
| 14 | 124 | 128 | 132 | 80 | 82 | 84 | 123 | 126 | 129 | 81 | 82 | 84 |
| 15 | 126 | 131 | 135 | 81 | 83 | 85 | 124 | 127 | 131 | 82 | 83 | 85 |
| 16 | 129 | 134 | 137 | 82 | 84 | 87 | 125 | 128 | 132 | 82 | 84 | 86 |
| 17 | 131 | 136 | 140 | 84 | 87 | 89 | 125 | 129 | 132 | 82 | 84 | 86 |
| B. Simplified table displaying the 95th percentile values of blood pressure (mmHg) at the 5th, 50th and 95th percentiles of a child’s height by age group, based on the Fourth Report, consistent with the simplified table by Mitchell et al.17
| ||||||
|---|---|---|---|---|---|---|
| Age, y | SBP, mmHg
|
DBP, mmHg
|
||||
| P5(H) | P50(H) | P95(H) | P5(H) | P50(H) | P95(H) | |
| 3–5 | 104 | 107 | 110 | 63 | 65 | 67 |
| 6–8 | 108 | 111 | 115 | 72 | 74 | 76 |
| 9–11 | 113 | 117 | 120 | 76 | 77 | 79 |
| 12–14 | 119 | 123 | 126 | 78 | 80 | 82 |
| 15–17 | ||||||
| Boys | 126 | 131 | 135 | 81 | 83 | 85 |
| Girls | 124 | 127 | 131 | 82 | 83 | 85 |
| C. Formulas to estimate the 95th percentile blood pressure values (mmHg) at the 5th, 50th and 95th percentiles of height based on the Fourth Report, consistent with formulas developed by Somu et al.14 and Badeli et al.15
| ||||
|---|---|---|---|---|
| Age, y | P5(H) | P50(H) | P95(H) | |
| SBP, mmHg | 3–17 | 96 + 2*age | 100 + 2*age | 103+2*age |
| DBP, mmHg | 3–5 | 58 + 2*age | 60 + 2*age | 63+2*age |
| 6–17 | 66 + age | 68 + age | 70 + age | |
| D. Simplified table displaying the blood pressure to height ratio (BPHR) corresponding to the 95th percentile blood pressure values, based on the Fourth Report (Xi el al.20 and Lu et al.19)
| ||
|---|---|---|
| Age, y | Systolic BPHR | Diastolic BPHR |
| 6–11 | 0.84 | 0.55 |
| 12–17 | 0.78 | 0.50 |
| E. Simplified table displaying the 95th percentile blood pressure values according to a child’s absolute height, based on the Fourth Report (Chiolero et al.18)
| |||
|---|---|---|---|
| Height categories (cm) | Height range (cm) | SBP, mmHg | DBP, mmHg |
| 80 | <85 | 104 | 61 |
| 90 | 85–94 | 107 | 65 |
| 100 | 95–104 | 110 | 68 |
| 110 | 105–114 | 112 | 72 |
| 120 | 115–124 | 114 | 76 |
| 130 | 125–134 | 117 | 78 |
| 140 | 135–144 | 120 | 80 |
| 150 | 145–154 | 123 | 81 |
| 160 | 155–164 | 128 | 83 |
| 170 | 165–174 | 131 | 85 |
| 180 | ≥175 | 136 | 87 |
P5(H), P50(H), P95(H): 5th, 50th and 95th percentiles of a child’s height
Elevated BP defined as SBP/DBP ≥90th percentile by sex, age, and height (or ≥120/80 mmHg) according to the Fourth Report6 was considered as the “gold standard” for comparison with the 11 simplified methods for 90th BP values (Table S2).
Statistical analysis
Analyses were performed using SAS 9.2 (SAS Institute, Cary, NC). For NHANES and KNHANES data, sampling weights were considered to account for complex survey design (PSUs and strata) at the country level; for other national data, the weights were not available. We performed receiver operator characteristic curve (ROC) analysis to examine the performance of each of the considered 11 simplified methods for their discriminatory power of elevated or high BP (yes vs. no) when compared to the Fourth Report as the “gold standard”. The area under the curve (AUC), sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated.
Results
Characteristics of participants in the seven national surveys are shown in Table S1. A total of 58,899 children and adolescents aged 6–17 years were included in the present study, with 9,129 subjects (boys: 52.7%, age range: 6–17 years) in China; 7,114 (56.0%, 6–17 years) in India: 16,613 (51.0%, 6–17 years) in Iran; 6,846 (52.8%, 10–17 years) in Korea; 5,721 (49.4%, 6–17 years) in Poland; 1,777 (46.1%, 15–17 years) in Tunisia; and 11,699 (49.2%, 8–17 years) in the USA. As shown in Table S3, the prevalence of high BP (using 95th percentile of the Fourth Report) in boys/girls ranged from 2.7% / 2.1% in Korea to 11.8% / 13.9% in India, respectively; the prevalence of obesity (using IOTF criteria) in boys/girls ranged from 1.7% / 0.9% in China to 15.4% / 16.3% in the USA, respectively.
In the analysis pooling individual-level data from the seven countries, all 11 simplified methods performed well in screening high BP, with high AUC values (0.84 to 0.98), high sensitivity (0.69 to 1.00), high specificity (0.87 to 1) and high NPV values (≥0.98) (Table 2). In contrast, the PPV was lower for most methods. However, three simplified methods achieved fairly good PPV (boys/girls): the method using sex- and age- specific BP references at the 95th percentile of height (0.94/0.94), the method based on the formula at the 95th percentile of height (0.84/0.96), and the method based on absolute height (0.84/0.92), compared to PPV of 0.32–0.69 in boys and 0.40–0.81 in girls for the other simplified methods. In addition, three methods each above also performed similarly well according to age group and type of high BP (Table S4).
Table 2.
Performance of the 11 simplified methods for the identification of high blood pressure in children and adolescents from the pooling data
| Simplified method | Boys | Girls | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| AUC (95%CI) | Sensitivity | Specificity | PPV | NPV | AUC (95%CI) | Sensitivity | Specificity | PPV | NPV | |
| Method A- P5(H) | 0.95 (0.95–0.95) | 1.00 | 0.91 | 0.40 | 1.00 | 0.97 (0.97–0.97) | 1.00 | 0.94 | 0.54 | 1.00 |
| Method A- P50(H) | 0.94 (0.93–0.94) | 0.90 | 0.97 | 0.69 | 0.99 | 0.98 (0.97–0.98) | 0.97 | 0.98 | 0.75 | 1.00 |
| Method A- P95(H) | 0.85 (0.84–0.87) | 0.71 | 1.00 | 0.94 | 0.98 | 0.87 (0.86–0.88) | 0.74 | 1.00 | 0.94 | 0.98 |
| Method B- P5(H) | 0.93 (0.93–0.94) | 1.00 | 0.87 | 0.32 | 1.00 | 0.95 (0.95–0.96) | 1.00 | 0.91 | 0.41 | 1.00 |
| Method B- P50(H) | 0.95 (0.95–0.96) | 0.97 | 0.93 | 0.47 | 1.00 | 0.97 (0.96–0.97) | 0.99 | 0.95 | 0.58 | 1.00 |
| Method B- P95(H) | 0.93 (0.92–0.94) | 0.89 | 0.97 | 0.67 | 0.99 | 0.93 (0.92–0.94) | 0.86 | 0.99 | 0.81 | 0.99 |
| Method C- P5(H) | 0.95 (0.95–0.95) | 1.00 | 0.91 | 0.40 | 1.00 | 0.97 (0.96–0.97) | 0.99 | 0.94 | 0.51 | 1.00 |
| Method C- P50(H) | 0.95 (0.95–0.96) | 0.95 | 0.96 | 0.62 | 1.00 | 0.96 (0.95–0.96) | 0.93 | 0.98 | 0.77 | 1.00 |
| Method C- P95(H) | 0.89 (0.88–0.91) | 0.80 | 0.99 | 0.84 | 0.99 | 0.84 (0.83–0.86) | 0.69 | 1.00 | 0.96 | 0.98 |
| Method D | 0.92 (0.91–0.93) | 0.92 | 0.92 | 0.42 | 0.99 | 0.93 (0.93–0.94) | 0.96 | 0.91 | 0.40 | 1.00 |
| Method E | 0.95 (0.94–0.95) | 0.90 | 0.99 | 0.84 | 0.99 | 0.94 (0.93–0.95) | 0.89 | 0.99 | 0.92 | 0.99 |
AUC, area under the curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value P5(H), P50(H), P95(H): 5th, 50th and 95th percentiles of a child’s height
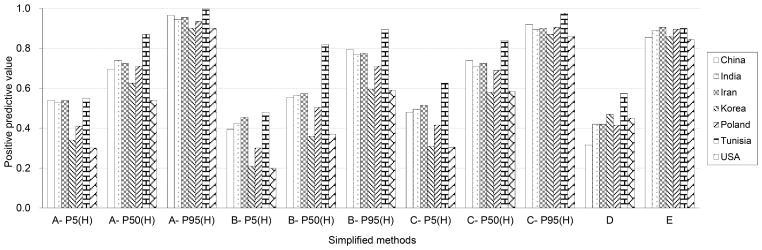
Performance for the identification of high BP for all 11 simplified methods was similar in each of the seven countries (Table S5). All simplified methods in all countries had high AUC, high sensitivity, high specificity, and high NPV (Table S5). In contrast, PPV was substantially lower for most simplified methods, but markedly and consistently higher in all countries for three simplified methods (sex- and age- specific BP references at the 95th percentile of height, formula at the 95th percentile of height, and the method based on a child’s absolute height) (Figure 1).
Figure 1.
Positive predictive value of the 11 simplified methods for identifying high BP in children and adolescents from seven countries. P5(H), P50(H), P95(H): 5th, 50th and 95th percentiles of a child’s height
The 11 simplified methods also performed well for identification of elevated BP, with high AUC, high sensitivity, high specificity, and high NPV (Table S6). Based on PPV values, three simplified methods including the sex- and age- specific 90th percentile BP values at the 95th percentile of height (boys: 0.99; girls: 0.99), the formula for 90th BP references at the 95th percentile of height (boys: 0.99; girls: 1.00), and the height-specific BP references (boys: 0.98; girls: 0.98) performed best among all 11 simple methods.
Discussion
We compared the performance of 11 simplified methods for assessing elevated or high BP in 58,899 children and adolescents aged 6–17 years from seven countries in three continents. All methods had good performance to identify children and adolescents with elevated or high BP based on high AUC, sensitivity, specificity and NPV. However, PPV differed largely across simplified methods. Three simplified methods achieved good PPV (~90%): the method specific for sex and age (at the 95th height percentile), the method based on mathematical formula (at the 95th height percentile) and the method based on a child’s absolute height, meaning that ~90% of children identified to have raised BP with the test would actually have high BP. However, it should be noted that the method based on a child’s absolute height might be the most useful in clinical practice since the two other methods (one based on sex- and age- specific values, and the other one based on formulas) perform well only among tall children.
It is well known that height is strongly associated with BP independently of age and sex.6, 35, 36 In 2013, Chiolero et al.18 established BP cut-offs for screening high BP in children and adolescents derived from the Fourth Report taking only a child’s absolute height into consideration, along eleven incremental 10-cm absolute height caregories between 80 and 180 cm. Hence the simplified table has 22 SBP/DBP height-specific cuttoffs vs 476 BP age-, sex- and height- specific cut-offs in the original Fourth Report. These BP cuff-offs based on a child’s absolute height were assessed in two surveys in Switzerland and Seychelles, and PPV and NPV values were 92% and 97% in Switzerland, and 91% and 98% in the Seychelles, respectively.18 These results are consistent with our findings in 7 other populations.
In 2003, Somu et al. developed a formula to identify high BP in children and adolescents based on linear regression analysis of the 95th percentile BP values at the 50th percentile of height for both sexes.14 As this formula was based on the corresponding BP values extracted from the 1996 US BP criteria37, we recalculated it using the BP cut-off values from the Fourth Report. It was coincident that our recalculated 95th BP percentiles values were nearly identical to the original formula of Somu et al.14 In the present study, we also developed similar formulas at the 95th percentile of a child’s height, which performed equally well with the simplified height-specific BP references.
Lu et al.19 proposed the use of BPHR in 2011, with 4 cutt-off ratios to define elevated SBP, respectively DBP, in boys and girls. The authors concluded that BPHR was an accurate and simple index for screening elevated BP in adolescents aged 13–17 years.19 However, the PPV of this method was lower than 50%, similar to our findings. In other words, more than 50% of children idenfied as having elevated or high BP based on this simplified method would actually not have elevated or high BP based on the cuttoffs of the Fourth Report (i.e. a large false positve yield), which may result in unncesary confirmatory tests (to rule out truly elevated or high BP) and psychological stress for children and their parents related to false positive labeling.
The BP cut-offs used to define hypertension in male adolescents aged 17 years were close to the 140/90 mmHg cutt-off used in adults, ranging from 136/87 mmHg at the 50th percentile of height to 140/89 mmHg at the 95th percentile of height. However, the BP cut-offs used to diagnose hypertension in female adolescents aged 17 years (~130/85 mmHg) were substantially lower than the 140/90 mmHg cut-off in adults. BP levels are typically higher in male than female adolescents aged 17 years in many surveys. The exact reasons for this sex difference in BP are unknown but differences in sex hormones and in body build (e.g. total muscular vs. fat mass) between boys and girls at late adolescence may play a role. However, it should be recalled that BP cut-offs in the Fourth Report were established based on BP distributions using statistical methods rather than linking BP values in childhood to target organ damage or cardiovascular diseases in childhood or adulthood. Thus, it cannot be definitely assessed whether BP cut-offs to define hypertension in male and female adolescents aged 17 years should be close to that in adults or not.
The strengths of this study include the large sample size of our pooled dataset (n=58,899), the population-based nature of all naitonal samples, the high quality of measured data (e.g., use of calibrated BP devices and trained investigators), the comprehensive age range of most datasets (6–17 years), and the diverse underlying populations (seven countries from three continents). These characteristics strengthen the generalizabilty of our findings and their potential applicability by clinicans in all countries. However, several limitations should also be noted. First, we did not validate the 11 simplied methods in children younger than 6 years. Second, BP was measured at only one visit in all surveys. Further studies should assess the performance of the simplified methods based on BP readings taken on at least three occasions or in different settings (e.g. home blood pressure). In addition, it would be useful if these simplified tools could be evaluated based on the presence of target organ damage.
Perspectives
The present study shows that all simplified methods to assess elevated or high BP in children and adolescents performed well when the purpose was to exclude the presence of elevated or high BP in the children screened, but only three simplified methods had sufficiently high PPV to identify children with high BP. In addtion,simplified methods, which are expected to be more user-friendly than the original tables of the Fourth Report, may be suitable for routine screening, but definite diagnosis of elevated or high BP needs to be confirmed using the standard criteria of the Fourth Report. Further studies should examine the performance of simplified methods in other settings and populations, particularly methods based on a child’s absolute height, to further document their external validity.
Supplementary Material
Novelty and Significance.
What is New?
We compared the performance of 11 simplified methods for screening elevated or high BP among 58,899 children and adolescents aged 6–17 years based on data from seven national studies from China, India, Iran, Korea, Poland, Tunisia and the USA.
What is Relevant?
Three simplified methods performed best: one as the simplified tables by sex and age (at the 95th percentile of height), one using a formula (at the 95th percentile of height) and one based on a child’s absolute height. Simplified methods may be useful for screening purpose.
Summary
This study shows that commonly used simplified methods to assess high BP in children and adolescents performed well when the purpose was to exclude the presence of high BP, but only three simplified methods had sufficiently high positive predictive value to accurately identify children with high BP.
Acknowledgments
Sources of Funding
This work was supported by the Young Scholars Program of Shandong University (2015WLJH51), the National Institutes of Health (NIH) (grants R01-HD30880, DK056350, R24-HD050924, and R01-HD38700), as part of a national school-based surveillance program funded by the Iran Ministry of Health. The sponsors have no role in the study design, survey process, data analysis and manuscript preparation.
We thank the U.S. and Chinese Centers for Disease Control and Prevention, and University of North Carolina for sharing their valuable data.
Footnotes
Disclosures:
None
References
- 1.Kollias A, Dafni M, Poulidakis E, Ntineri A, Stergiou GS. Out-of-office blood pressure and target organ damage in children and adolescents: A systematic review and meta-analysis. J Hypertens. 2014;32:2315–2331. doi: 10.1097/HJH.0000000000000384. discussion 2331. [DOI] [PubMed] [Google Scholar]
- 2.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: A systematic review and meta-regression analysis. Circulation. 2008;117:3171–3180. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Juhola J, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Kahonen M, Taittonen L, Urbina E, Viikari JS, Dwyer T, Raitakari OT, Juonala M. Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: The international childhood cardiovascular cohort consortium. Circulation. 2013;128:217–224. doi: 10.1161/CIRCULATIONAHA.113.001614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sundstrom J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: Cohort study of swedish male conscripts. BMJ. 2011;342:d643. doi: 10.1136/bmj.d643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National High Blood Pressure Education Program Working Group on High Blood Pressure in C Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 7.Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, Kuznetsova T, Laurent S, Mancia G, Morales-Olivas F, Rascher W, Redon J, Schaefer F, Seeman T, Stergiou G, Wuhl E, Zanchetti A European Society of H. Management of high blood pressure in children and adolescents: Recommendations of the european society of hypertension. J Hypertens. 2009;27:1719–1742. doi: 10.1097/HJH.0b013e32832f4f6b. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro DJ, Hersh AL, Cabana MD, Sutherland SM, Patel AI. Hypertension screening during ambulatory pediatric visits in the united states, 2000–2009. Pediatrics. 2012;130:604–610. doi: 10.1542/peds.2011-3888. [DOI] [PubMed] [Google Scholar]
- 9.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298:874–879. doi: 10.1001/jama.298.8.874. [DOI] [PubMed] [Google Scholar]
- 10.Thompson M, Dana T, Bougatsos C, Blazina I, Norris SL. Screening for hypertension in children and adolescents to prevent cardiovascular disease. Pediatrics. 2013;131:490–525. doi: 10.1542/peds.2012-3523. [DOI] [PubMed] [Google Scholar]
- 11.Urbina EM, de Ferranti S, Steinberger J. Observational studies may be more important than randomized clinical trials: Weaknesses in us preventive services task force recommendation on blood pressure screening in youth. Hypertension. 2014;63:638–640. doi: 10.1161/HYPERTENSIONAHA.113.02662. [DOI] [PubMed] [Google Scholar]
- 12.Chiolero A, Bovet P, Paradis G. Screening for elevated blood pressure in children and adolescents: A critical appraisal. JAMA Pediatr. 2013;167:266–273. doi: 10.1001/jamapediatrics.2013.438. [DOI] [PubMed] [Google Scholar]
- 13.Chiolero A, Paradis G. User-friendly tools to identify elevated blood pressure in children. Paediatr Child Health. 2013;18:63–64. doi: 10.1093/pch/18.2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Somu S, Sundaram B, Kamalanathan AN. Early detection of hypertension in general practice. Arch Dis Child. 2003;88:302. doi: 10.1136/adc.88.4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Badeli H, Sajedi SA, Shakiba M. Simple formulas for screening abnormal blood pressure in children and adolescents. Iran J Kidney Dis. 2010;4:250–252. [PubMed] [Google Scholar]
- 16.Kaelber DC, Pickett F. Simple table to identify children and adolescents needing further evaluation of blood pressure. Pediatrics. 2009;123:e972–974. doi: 10.1542/peds.2008-2680. [DOI] [PubMed] [Google Scholar]
- 17.Mitchell CK, Theriot JA, Sayat JG, Muchant DG, Franco SM. A simplified table improves the recognition of paediatric hypertension. J Paediatr Child Health. 2011;47:22–26. doi: 10.1111/j.1440-1754.2010.01885.x. [DOI] [PubMed] [Google Scholar]
- 18.Chiolero A, Paradis G, Simonetti GD, Bovet P. Absolute height-specific thresholds to identify elevated blood pressure in children. J Hypertens. 2013;31:1170–1174. doi: 10.1097/HJH.0b013e32836041ff. [DOI] [PubMed] [Google Scholar]
- 19.Lu Q, Ma CM, Yin FZ, Liu BW, Lou DH, Liu XL. How to simplify the diagnostic criteria of hypertension in adolescents. J Hum Hypertens. 2011;25:159–163. doi: 10.1038/jhh.2010.46. [DOI] [PubMed] [Google Scholar]
- 20.Xi B, Zhang M, Zhang T, Liang Y, Li S, Steffen LM. Hypertension screening using blood pressure to height ratio. Pediatrics. 2014;134:e106–111. doi: 10.1542/peds.2014-0643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Totaro SRF, Rabbone I, Covella M, Berra E, Fulcheri C, Monaco SD, Testa E, Veglio F. Comparison among different screening tests for diagnosis of adolescent hypertension. ISRN Hypertension. 2013;2013:107915. [Google Scholar]
- 22.Mourato FA, Lima Filho JL, da Mattos SS. Comparison of different screening methods for blood pressure disorders in children and adolescents. J Pediatr (Rio J) 2015;91:278–283. doi: 10.1016/j.jped.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Ma C, Liu Y, Liu X, Yin F, Lu Q. Comparison of different screening methods for hypertension in han adolescents. Clin Pediatr (Phila) 2016;55:363–367. doi: 10.1177/0009922815591886. [DOI] [PubMed] [Google Scholar]
- 24.Aatola H, Magnussen CG, Koivistoinen T, Hutri-Kahonen N, Juonala M, Viikari JS, Lehtimaki T, Raitakari OT, Kahonen M. Simplified definitions of elevated pediatric blood pressure and high adult arterial stiffness. Pediatrics. 2013;132:e70–76. doi: 10.1542/peds.2012-3426. [DOI] [PubMed] [Google Scholar]
- 25.Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: The china health and nutrition survey--monitoring and understanding socio-economic and health change in china, 1989–2011. Int J Epidemiol. 2010;39:1435–1440. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kajale NA, Khadilkar AV, Chiplonkar SA, Khadilkar VV. Body fat indices for identifying risk of hypertension in indian children. Indian Pediatr. 2014;51:555–560. doi: 10.1007/s13312-014-0446-4. [DOI] [PubMed] [Google Scholar]
- 27.Kelishadi R, Heshmat R, Motlagh ME, Majdzadeh R, Keramatian K, Qorbani M, Taslimi M, Aminaee T, Ardalan G, Poursafa P, Larijani B. Methodology and early findings of the third survey of caspian study: A national school-based surveillance of students' high risk behaviors. Int J Prev Med. 2012;3:394–401. [PMC free article] [PubMed] [Google Scholar]
- 28.Kelishadi R, Ardalan G, Qorbani M, Ataie-Jafari A, Bahreynian M, Taslimi M, Motlagh ME, Heshmat R. Methodology and early findings of the fourth survey of childhood and adolescence surveillance and prevention of adult non-communicable disease in iran: The caspian-iv study. Int J Prev Med. 2013;4:1451–1460. [PMC free article] [PubMed] [Google Scholar]
- 29.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: The korea national health and nutrition examination survey (knhanes) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krzyzaniak A, Krzywinska-Wiewiorowska M, Stawinska-Witoszynska B, Kaczmarek M, Krzych L, Kowalska M, Szilagyi-Pagowska I, Palczewska I, Karch A, Josko J, Ostrowska-Nawarycz L, Nawarycz T. Blood pressure references for polish children and adolescents. Eur J Pediatr. 2009;168:1335–1342. doi: 10.1007/s00431-009-0931-2. [DOI] [PubMed] [Google Scholar]
- 31.Aounallah-Skhiri H, El Ati J, Traissac P, Ben Romdhane H, Eymard-Duvernay S, Delpeuch F, Achour N, Maire B. Blood pressure and associated factors in a north african adolescent population. A national cross-sectional study in tunisia. BMC Public Health. 2012;12:98. doi: 10.1186/1471-2458-12-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosner B, Cook NR, Daniels S, Falkner B. Childhood blood pressure trends and risk factors for high blood pressure: The nhanes experience 1988–2008. Hypertension. 2013;62:247–254. doi: 10.1161/HYPERTENSIONAHA.111.00831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, Morgenstern BZ. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–2470. doi: 10.1161/01.cir.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 34.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xi B, Zong X, Kelishadi R, et al. Establishing international blood pressure references among non-overweight children and adolescents aged 6–17 years. Circulation. 2016;133:398–408. doi: 10.1161/CIRCULATIONAHA.115.017936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Regnault N, Kleinman KP, Rifas-Shiman SL, Langenberg C, Lipshultz SE, Gillman MW. Components of height and blood pressure in childhood. Int J Epidemiol. 2014;43:149–159. doi: 10.1093/ije/dyt248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Update on the 1987 task force report on high blood pressure in children and adolescents: A working group report from the national high blood pressure education program. National high blood pressure education program working group on hypertension control in children and adolescents. Pediatrics. 1996;98:649–658. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.