Abstract
Context:
For decades, behavioral weight-loss treatments have been unsuccessful beyond the short term. Development and testing of innovative, theoretically based methods that depart from current failed practices is a priority for behavioral medicine.
Objective:
To evaluate a new, theory-based protocol in which exercise support methods are employed to facilitate improvements in psychosocial predictors of controlled eating and sustained weight loss.
Methods:
Women with obesity were randomized into either a comparison treatment that incorporated a print manual plus telephone follow-ups (n = 55) or an experimental treatment of The Coach Approach exercise-support protocol followed after 2 months by group nutrition sessions focused on generalizing self-regulatory skills from an exercise support to a controlled eating context (n = 55). Repeated-measures analysis of variance contrasted group changes in weight, physical activity, fruit and vegetable intake, mood, and exercise- and eating-related self-regulation and self-efficacy over 24 months. Regression analyses determined salient interrelations of change scores over both the weight-loss phase (baseline-month 6) and weight-loss maintenance phase (month 6-month 24).
Results:
Improvements in all psychological measures, physical activity, and fruit and vegetable intake were significantly greater in the experimental group where a mean weight loss of 5.7 kg (6.1% of initial body weight) occurred at month 6, and was largely maintained at a loss of 5.1 kg (5.4%) through the full 24 months of the study. After establishing temporal intervals for changes in self-regulation, self-efficacy, and mood that best predicted improvements in physical activity and eating, a consolidated multiple mediation model suggested that change in self-regulation best predicted weight loss, whereas change in self-efficacy best predicted maintenance of lost weight.
Conclusions:
Because for most participants loss of weight remained greater than that required for health benefits, and costs for treatment administration were comparatively low, the experimental protocol was considered successful. After sufficient replication, physician referral and applications within health promotion and wellness settings should be considered.
INTRODUCTION
Approximately 69% of US adults are at a weight high enough to be considered unhealthy (body mass index [BMI], calculated as weight in kilograms divided by height in meters squared, ≥ 25 kg/m2).1 Approximately 36% of US women are obese (BMI ≥ 30 kg/m2).1 As degree of overweight increases, so do health risks such as diabetes mellitus, hypertension, heart disease, and certain cancers.2 Although improving one’s dietary behaviors (eg, increasing intake of fruits and vegetables; reducing the consumption of fats and sweets) and increasing physical activity will reliably reduce weight by at least the 5% required to obtain clinically important health benefits,3 maintenance of those behaviors has been very difficult for almost all individuals.4,5 It can reliably be predicted that weight lost over the first approximately 6 months will mostly (if not all) be regained within 1 to 3 years.4,5 Even a more modest weight loss of at least 3% of original body weight sustained for 2 years, sometimes considered to be a marker of both weight-loss maintenance and some health-risk reductions,6 has been difficult to attain.7 Repeating the pattern of weight loss and regain may have adverse effects on both health risks and subsequent attempts at weight loss.8,9
Previous Behavioral Treatments
Interventions based on educating individuals on the need to lose weight by eating more healthfully and by being more physically active are the most common but have been ineffective.4 Their absence of foundation in established behavior-change theories and research is a proposed reason for this lack of success.10 Cognitive-behavioral methods consistent with Bandura’s social cognitive11 and self-efficacy12 theories (eg, goal setting, cognitive restructuring) have occasionally had more favorable effects13,14 and are presently considered to be state-of-the-art by many researchers. Several reviews, however, suggest that even those types of interventions simply defer weight regain.4,5,15 Summaries of research also suggest that longer treatments (eg, 6 to 12 months, or longer) have had somewhat better effects than shorter treatments; but initial weight loss, energy-intake requirements, financial incentives, and focusing on fat vs kilocalories (kcal) do not affect the rate of weight regain after approximately 6 months.5 Research has rarely sought to determine the psychosocial factors that predict weight-loss outcomes.16
A group of behavioral researchers from Oxford University recently incorporated the extant theory and research to develop a highly structured Cognitive Behavioural Therapy protocol (Oxford CBT) in which maintenance of lost weight was targeted from the start.17 Their intervention model is instructive because it embodies much of the current thinking on both obtaining and sustaining weight loss through evidence-based behavioral methods such as self-monitoring the time, location, kcal, and type of foods and drinks consumed;18 regular self-weighing;19 and actively countering lifestyle barriers.20 Components of the Oxford CBT, which were administered by mostly clinical psychologists during individual 50-minute consultations, included “the role of body image in weight loss,” “addressing barriers to weight loss,” “encouraging acceptance,” “common primary goals,” and “developing long-term weight maintenance skills.”17 Tracking of foods, initially limiting to a 1500 kcal intake per day, and weighing and graphing weight changes were key elements of the modular protocol. The 24 sessions over 44 weeks designated the initial 24 to 30 weeks as a weight-loss phase, with the remainder devoted to weight maintenance. More in common with the available treatments, though, was that exercise was not emphasized. The treatment developers suggested that its minor impact on kcal totals render physical activity as being of minor concern for weight loss, and could possibly interfere with dietary compliance. Thus, initiating physical activity could be deferred by up to 6 months.17 Although the Oxford CBT was expensive at an estimated professional cost of between US$3000 and US$4500 per participant, it proved to be no more effective than standard behavioral treatment.21 With its sample of 49 women with obesity (ie, BMI of 30–40 kg/m2) who were tested, approximately 68% of lost weight was regained at the 2-year point, and 91% was regained 3 years past treatment initiation. Possibly because even this strongly evidence-based and well-administered approach was judged by its developers to be ineffective at sustaining weight loss, they stated that it might be “ethically questionable to claim that psychological [behavioral] treatments for obesity ‘work’ in the absence of [favorable] data on their longer-term outcome.”21p712 In further consideration of their findings and the entire body of research on intervention outcomes, they pessimistically, yet possibly realistically, concluded their report by questioning whether continuing behavioral research in the area of weight management is even warranted any longer.21
Suggested Treatment Improvements
Other researchers disagreed with the above conclusions, but it was acknowledged that many of the presently held assumptions and methods around behavioral weight-loss treatments are ineffective and “fresh ideas are needed for attacking the problem.”5p14 Following from this suggestion, the National Institutes of Health commissioned a multidisciplinary working group on “Innovative Research to Improve Maintenance of Weight Loss” in 2014.22 Its final report summarized that 1) although adherence issues need to be addressed first, exercise has promising implications for maintaining weight loss that go well beyond its obvious expenditure of energy; and 2) learning behavioral skills before starting on weight loss might be beneficial for weight-loss maintenance.22 In an unrelated review of treatment results, Mann and her colleagues4 also recommended further research on exercise as possibly being the “potent factor” (for long-term weight loss), in lieu of any additional work on dieting or composition of the diet.
Although a program of regular exercise has been shown to be the strongest predictor of success with maintaining weight loss for some time,23–25 it remains difficult to maintain with an expected dropout rate of 50% to 65% within 3 to 6 months of its initiation.26,27 On the basis of accelerometer data from both the 2003–2004 and 2005–2006 National Health and Nutritional Examination Surveys, less than 4% of US women complete the equivalent of at least 5 moderate-intensity walks per week,28,29 which is considered to be the minimum threshold for health benefits.30 Pilot research indicates that even when dropout from exercise is successfully countered, typical frequencies for formerly sedentary participants with obesity are only 2 to 3 sessions per week, with an estimated energy expenditure of less than 150 kcal per session (which amounts to only approximately 0.5 kg of weight loss every 9 to 10 weeks31). Although there have been advances in improving adherence to exercise through standardized cognitive-behavioral methods (eg, The Coach Approach protocol32), it was proposed that the relationship of exercise with maintained weight loss is more because of its association with improvements in psychological predictors of controlled eating than associated energy expenditures.33 For example, if self-regulatory skills (eg, thought-stopping) could first be internalized within an intervention component designed to facilitate regular exercise, possibly treatment elements could be constructed to promote generalization of such behavioral skills to controlled eating.33 This, however, runs in opposition to treatments such as the Oxford CBT17 and some basic research34 that suggests that self-regulation used for one behavior (here exercise) might deplete an individual’s limited capacity of self-regulation for success with a second behavior (here reduced kcal eating). It was also proposed that self-efficacy, or one’s feelings of ability and mastery, could be increased by demonstrating to one’s self a better control of exercise behaviors through the use of newly learned self-regulatory skills to counter barriers.33 Improved self-efficacy to control exercise might, in turn, also generalize to controlled eating, the other critical weight-loss behavior of interest.33,35 Improvements in mood, a well-established by-product of initiating even manageable amounts of exercise,33,36 might serve to counter the common problem (especially for women) of emotional eating,37 and “… lead to a healthier psychological climate in which individuals have more cognitive and emotional resources, as well as motivation and energy, to sustain a long-term commitment to a weight-loss program.”35p320 Adherence to just 2 to 3 sessions per week of behaviorally supported exercise has been associated with significant improvements in self-regulation, self-efficacy, and mood,38 which were found to be the most critical psychological predictors of improvements in eating and weight over 6 months, even when previously suggested factors such as self-concept and body image35 were considered.39 Additional studies are, however, required to determine psychological predictors of longer-term weight-loss maintenance that might inform both theory and the architecture of improved behavioral treatments. Although exercise is frequently incorporated into weight-loss interventions, we have found no longer-term research where its primary focus was on improving psychological predictors of controlled healthy eating.
Thus, as an extension to earlier research on short-term psychological, behavioral, and weight-loss effects,33,40–42 the present study was conducted. It incorporated 1) an experimental treatment that initiated supported exercise 2 months before any changes in nutrition in attempts to improve targeted psychological and behavioral correlates of improved eating and weight loss, and 2) a comparison treatment of participants’ use of a manual that simultaneously encouraged healthy eating, physical activity, and reasonable expectations, which was supplemented by telephone follow-ups. Both treatments were based on accepted behavioral theory, yet there were substantial differences. On the basis of a research consensus indicating that the initial approximately 6 months after treatment start is a time of weight loss, whereas beyond 6 months weight regain (often complete regain) can be reliably predicted,4,5 the present study investigated 1) treatment-associated weight change, 2) behavioral predictors of weight change (ie, changes in healthy eating and physical activity), and 3) hypothesized psychological predictors of the behavioral changes (ie, self-regulation, self-efficacy, mood) during those 2 time frames. Data were measured at baseline and months 3, 6, 12, and 24. This allowed contrasts of dynamic changes in targeted variables by group, and analyses of which of the possible temporal intervals best predicted weight change and weight change-related behavioral improvements. Such findings could be instrumental for determining when, and to what degree, corresponding treatment processes should be emphasized. To enhance clarity, this report is expressed in 3 parts corresponding to the aforementioned 3 areas. Hypotheses and research questions are as follows.
Hypotheses
Reduction in weight from baseline-month 6 (weight-loss phase) will be greater, and regain in weight from month 6-month 24 (weight-loss maintenance phase) will be less, in the experimental group when contrasted with the comparison group.
Improvements in the targeted behaviors of physical activity and fruit and vegetable intake will be greater during both the weight-loss and weight-loss maintenance phases in the experimental group when contrasted with the comparison group.
Improvements in the targeted psychological variables of mood, self-regulation, and self-efficacy—related to both exercise and eating—will be greater during both the weight-loss and weight-loss maintenance phases in the experimental group when contrasted with the comparison group.
Research Questions
Was change in physical activity and fruit and vegetable intake from baseline-month 3, baseline-month 6, or month 3-month 6 the better predictor of weight change during the weight-loss phase? What temporal interval of change in physical activity and fruit and vegetable intake best predicted weight change during the weight-loss maintenance phase?
Was change in each psychological variable from baseline-month 3, baseline-month 6, or month 3-month 6 the better predictor of physical activity and fruit and vegetable intake change during the weight-loss phase? What temporal interval of change in each psychological variable best-predicted behavioral changes during the weight-loss maintenance phase?
Did changes in mood and/or aggregated (exercise- and eating-related) measures of self-regulation and self-efficacy significantly mediate relationships between treatment type (comparison and experimental) and changes in weight during the weight-loss and weight-loss maintenance phases?
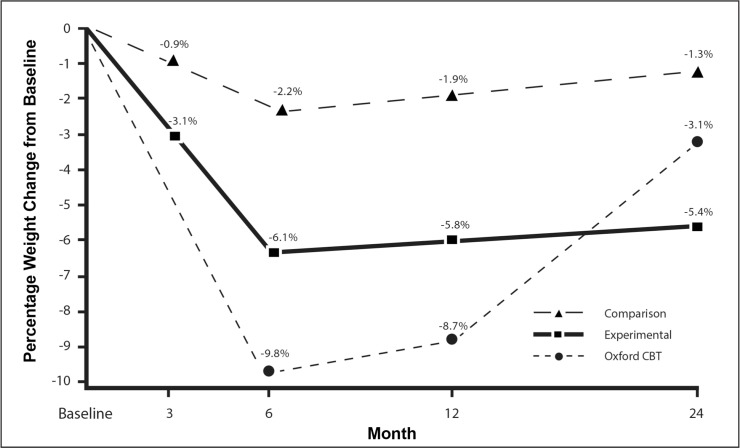
Because participant characteristics, initial weight, cognitive-behavioral treatment orientation, and focus on weight-loss maintenance were designed to be similar to those of the previously published Oxford CBT study,21 the present weight-change data were also contrasted with the Oxford CBT findings.
METHODS
Participants
Participant recruitment was through local print and electronic media. Inclusion criteria were 1) women of at least 21 years of age, 2) BMI ≥ 30 and < 40 kg/m2, and 3) a self-reported goal of weight loss. Exclusion criteria based on self-report were 1) present or soon-planned pregnancy; 2) present use of medications for weight loss or a psychological/psychiatric condition; 3) current participation in a medical, commercial, or self-help weight-loss program; and 4) participation in a program of regular physical activity/exercise that averaged at least 20 minutes per week during the year before the start of the study. Treatments were administered at small, community-based wellness/fitness centers in the Eastern US. Because the chance of cross-contamination of participants through intergroup interactions within the same facility would have been high, randomization to either the comparison (COM) treatment (n = 55) or the experimental (EXP) treatment (n = 55) was by site (3 sites each). Institutional review board approval and written informed consent from each participant were received. The research was conducted in accordance with requirements of the Helsinki Declaration.
Independent t- and χ2 tests indicated no significant group difference in age (mean-overall ± standard deviation (SD) = 48.2 ± 7.8 years), BMI (35.3 ± 3.2 kg/m2), or racial/ethnic make-up (overall 83% white, 11% African American, and 6% of other racial/ethnic groups). On the basis of self-reported family income, most participants were middle class (overall 11% below $24,999, 21% = $25,000–$49,999, 41% = $50,000–$99,999, and 27% = $100,000 or greater). Attrition from initial study acceptance to actual treatment participation was minimal at 7% and also did not significantly differ by group. This attrition was associated with either a reported illness, a newly arisen orthopedic issue, transportation issues, or an inability of study staff to make further contact after 3 attempts. There was no cost or financial compensation for participation.
Measures
The self-report measures used in this study were 1) physical activity (PA) through weekly energy expenditure, 2) healthy eating through daily fruit and vegetable intake (FV), 3) self-regulation for exercise (SR-exercise), 4) self-regulation for controlled eating (SR-eating), 5) self-efficacy for exercise (SE-exercise), 6) overall negative mood (Mood), and 7) self-efficacy for controlling eating (SE-eating). Descriptions of each of these measures, along with data on their reliability and validity, are presented below (Table 1). Body weight was measured in kilograms through the use of a recently calibrated scale (800KL; Healthometer, Buffalo Grove, IL).
Table 1.
Description of study measures
| Measure | Measurement instrument | Instrument description | Reliability and validity |
|---|---|---|---|
| Physical activity (PA) | Godin-Shephard Leisure-Time Physical Activity Questionnaire43 | Requires entry of number of weekly sessions of strenuous (~ 9 METs; eg, running), moderate (~ 5 METs; eg, fast walking), and light (~ 3 METs; eg, easy walking) physical exertion for “more than 15 minutes.” Incorporates METs, or the energy costs associated with specific physical activity intensities (1 MET accelerometer and peak volume of approximates the use of 3.5 ml of O2/kg/minute).44 | Test-retest reliability (2 weeks) was 0.74.45 Construct validity was indicated through strong correlations with both oxygen uptake measurements.46,47 |
| Healthy eating measured by fruit and vegetable intake (FV) | Self-report survey of FV48 | Foods and beverages consumed “in a typical day over the past week” are based on examples and serving sizes of fruits (eg, apple, banana, peach [1 small or 118 mL or 4 ounces canned]; raisins, dates [0.59 mL or 2 ounces]; 100% fruit juice [118 mL or 4 ounces]) and vegetables (eg, broccoli, carrots, tomatoes, green beans [118 mL or 4 ounces]; raw spinach [236 mL or 8 ounces]) that correspond to both the US Department of Agriculture’s current MyPlate and former Food Guide Pyramid.49 Increases in FV were strongly associated with both weight loss and weight-loss maintenance,50 and an increase in FV was a stronger predictor of weight loss than reduction in fat intake.51 Previous research indicates that FV alone is a strong predictor of overall energy consumption and healthfulness of the diet.52,53 | Test-retest reliability (3 weeks) was 0.77–0.83 for women.33 Validated against comprehensive food frequency questionnaires,54 in which pilot research indicated strong correlations (r-values = 0.70–0.85) with the full-length Block Food Frequency Questionnaire.54,55 |
| Self-regulation for exercise (SR-exercise) and self-regulation for controlled eating (SR-eating) | Adaptation of a previously validated scale56,57 | The 10 items for SR-exercise (eg, “I say positive things to myself about being physically active”) and SR-eating (eg, “I make formal agreements with myself regarding my eating”) assess the degree that barriers to those behaviors are addressed through the use of self-regulatory skills. Responses range from 1 (never) to 5 (often), and are summed. A higher score indicates a greater use of self-regulation. | Cronbach α-values for internal consistency were 0.75,56 0.83, and 0.80 for the present versions and sample, respectively. Test-retest reliability (2 weeks) was 0.77.56 |
| Self-efficacy for exercise (SE-exercise) | Exercise Self-Efficacy Scale58 | After beginning with the stem, “I am confident I can participate in regular exercise when ...,” each of the scale’s 5 items end with a possible barrier to overcome (eg, “I am tired,” “I have more enjoyable things to do”). Responses range from 1 (not at all confident) to 7 (very confident), and are summed. A higher score indicates greater self-efficacy | Cronbach α-values for internal consistency were 0.76–0.82. Test-retest reliability (2 weeks) was 0.90.59 Cronbach α-value for internal consistency for the present sample was 0.80. |
| Overall negative mood (Mood) | Profile of Mood States Short Form scale of Total Mood Disturbance60 | The 30 items (5 items per factor) assess feelings during the past week on depression (eg, “sad”), tension/anxiety (eg, “tense”), vigor (eg, “energetic”), fatigue (eg, “weary”), anger (eg, “angry”), and confusion (eg, “forgetful”). Responses range from 0 (not at all) to 4 (extremely) and are summed after reversing the scores of the vigor factor. A lower score indicates better mood. | Cronbach α-values for internal consistency were 0.84–0.95 across factors,60 and 0.79–0.89 for the present sample. Test-retest reliability (3 weeks) averaged 0.69.60 |
| Self-efficacy for controlling eating (SE-eating) | Weight Efficacy Lifestyle Scale61 | The 20 items (4 per factor) assess feelings of ability to control eating when the following situations are present: negative emotions (eg, “I can resist eating when I am anxious [nervous]”), food availability (eg, “I can resist eating even when I am at a party”), physical discomfort (eg, “I can resist eating when I am uncomfortable”), positive activities (eg, “I can resist eating when I am watching TV”), and social pressure (eg, “I can resist eating even when I have to say ‘no’ to others”). Responses range from 0 (not confident) to 9 (very confident), and are summed. A higher score indicates greater self-efficacy. | Cronbach α-values for internal consistency were 0.70–0.90 across its factors,61 and 0.74–0.81 for the present sample. |
MET = metabolic equivalent; TV = television.
Procedure
Participants initially received a group orientation to their assigned EXP or COM protocol. Wellness counselors administering treatments were trained in only one of the protocols and masked to the treatment differences and the study’s research goals. Both the EXP and COM treatments were based on the social cognitive11 and self-efficacy12 theories of behavior where individuals are viewed as 1) directing their own actions through self-organization, 2) being able to manage their environments, and 3) possessing capabilities to be self-reflective of their internal abilities. Both the EXP and COM curricula incorporated cognitive-behavioral methods designed to empower participants with self-regulatory skills and abilities to deal with barriers to managing their weight effectively, while increasing their feelings of mastery and competence (ie, self-efficacy). Both treatment protocols informed participants of the recommended volume of weekly exercise to gain health benefits,30 but also suggested that any amount was also likely to be beneficial. However, the administration formats and the proposed role of physical activity/exercise in facilitating changes in eating behaviors differed substantially between the EXP and COM treatments.
The EXP treatment incorporated The Coach Approach exercise-support protocol32 paired with a nutrition behavior-change component developed for this research. It was based on 1) results from previous behavioral weight-management treatments,14,17,33,62–64 2) exploratory studies of psychosocial predictors of weight-loss behaviors,33,39,57 3) findings suggesting that behavioral mechanisms required to foster weight loss differ from those required to maintain lost weight,16,65 and 4) the suggested benefits of targeting specific and measurable behaviors for change (eg, increasing FV rather than addressing numerous and detailed elements of the diet).66 Beginning at baseline, The Coach Approach protocol32 supported adherence to newly initiated exercise through six 45-minute meetings with a trained wellness counselor possessing at least 1 national certification (eg, American College of Sports Medicine). These were conducted in a private office over 6.5 months. Each participant’s exercise plan, both initially and in revisions during subsequent meetings, was based on the participant’s preferred type of physical activity and tolerance. Most of the meeting time was, however, spent on the development of specific self-regulatory skills such as long- and short-term goal setting paired with progress monitoring, dissociation from discomfort, cognitive restructuring, stimulus control, behavioral contracting, controlling behavioral prompts and triggers, and relapse prevention. Exercise-induced changes in mood (eg, anxiety, energy level) were assessed both in response to a single bout of physical activity and for 1 to 2 months, and displayed through responses to items embedded in the supporting computer application.
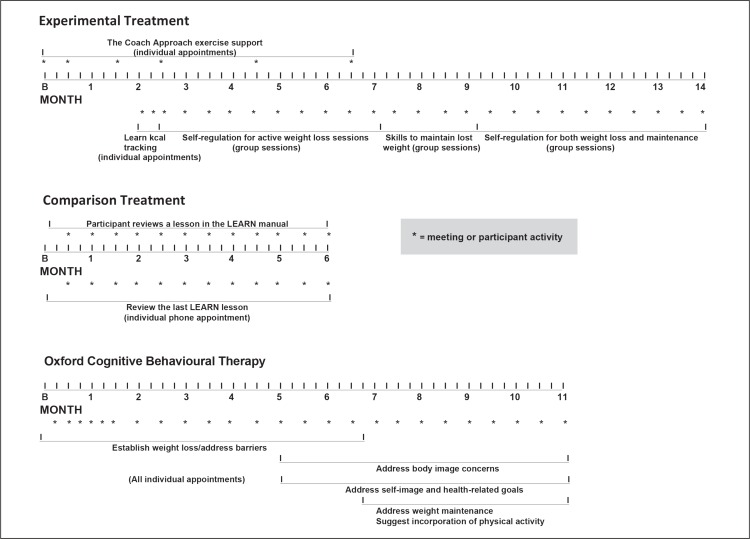
After 8 weeks of concentration exclusively on maintaining regular exercise, the components for eating behavior change were sequentially added. First, guidance and practice on methods for kcal tracking was individually provided in two 30-minute meetings over 2 weeks. Energy-intake goals were based on each participant’s weight (eg, 1500 kcal/day for a weight range of 79–99 kg), and various methods for recording food and corresponding kcal intake were made available (eg, through an approved Web site, an approved application for hand-held devices, or a provided paper form and use of an approved “calorie counter” book). Next, 10 nutrition sessions of 60 minutes each focused on weight reduction were administered by trained wellness counselors (supported by a manual) at 2-week intervals in groups of 8–15 participants. Their primary aim was to generalize, adapt, and extend self-regulatory skills developed during The Coach Approach exercise-support protocol,32 to self-regulating eating behaviors (eg, dissociating from exercise-induced discomfort was generalized to dissociating from feelings of hunger; recovering from and rescheduling a missed exercise session was generalized to recovering from a day of excess kcal intake and immediately recommitting to the appropriate limit for the next day). There was a combination of brief lectures, individual tasks, and group activities within each session. The next component, now 28 weeks after baseline, was 4 group sessions in which self-regulatory skills were addressed in the context of maintaining lost weight. The final 10 sessions of the EXP treatment covered skills of self-regulation in both weight-loss and weight-loss maintenance contexts (Figure 1). Treatment content related to the diet was primarily concentrated on increasing FV intake, although there was a limited focus on minimizing the consumption of fat and sugar. Because meeting time was primarily centered on the development of self-regulatory skills and the ability to increase self-efficacy for controlling overeating, participants were referred to the ChooseMyPlate.gov Web site67 for access to detailed, evidence-based information on nutrition.
Figure 1.
Timeline of the Experimental Treatment, Comparison Treatment, and Oxford Cognitive Behavioural Therapy.
B = baseline; kcal = kilocalories; LEARN = lifestyle, exercise, attitudes, relationships, nutrition.
The COM treatment replicated methods used previously in studies,21,42 and consisted of participants reviewing 1 of the 12 “lessons” of a 265-page print manual entitled The LEARN (lifestyle, exercise, attitudes, relationships, nutrition) Program for Weight Management (10th edition)68 every 2 weeks. Sections related to behavior change included “Dealing with Pressures to Eat,” “Preventing Lapse, Relapse, and Collapse,” “Interpreting Your Progress,” and “Making Physical Activity Count.” Sections related to diet included “Fast Foods,” “Rating Your Diet,” “Vegetables in Your Diet,” and “Breads, Cereals, Rice, and Pasta in Your Diet.” Each lesson was followed by a 15-minute phone conversation initiated by a wellness counselor to clarify chapter contents, review each participant’s plans for carrying out behavioral changes, and answer the participant’s questions. The process of participants reading chapters and obtaining telephone follow-ups started at baseline and lasted 24 weeks (Figure 1). The LEARN manual68 suggested that women limit their energy intake to 1200 kcal per day. A paper monitoring form was provided for participants to record foods and drinks consumed, the amount consumed and their associated kcal, their corresponding food group categorization, and optional comments.
Fidelity checks were completed on approximately 15% of treatment components by study staff. Minor protocol violations were primarily related to adherence to required time frames within sessions and were easily rectified through study staff-instructor interactions. Surveys and weight measurements were completed in a private area.
Data Analyses
To avoid inappropriately inflated effect sizes such as those reported in the many studies where data from only weight-loss program “completers” were included, the conservative intention-to-treat approach was used, as suggested.13 Thus, data were retained from all participants who engaged in treatment processes. The expectation-maximization algorithm69 was used to impute data for the 14% of missing scores. The required criteria of missing at random (no systematic bias) was indicated because participants who were missing data at any assessment time did not significantly differ from the sample as a whole on demographic characteristics or any other study measure. On the basis of the planned multiple regression equations incorporating 3 predictor variables, and to detect the moderate effect of f2 = 0.15 that was indicated in pilot research33 at the statistical power of 0.90 (α = 0.05), a minimum of 98 total participants was required.70 In tests during the weight-loss phase, tolerances (0.60–0.82) and variance inflation factors (1.23–1.67) indicated a low degree of multicollinearity. During the weight-loss maintenance phase, tolerances (0.22–0.86) and variance inflation factors (1.16–4.58) indicated a low-moderate degree of multicollinearity.71 Inspection of residual scatterplots indicated homogeneity of variances and linearity in the data. Both skewness and kurtosis values were < 2 standard errors. Consistent with previous suggestions for research within the present context, change scores were unadjusted for baseline values.72 Statistical significance was set at α = 0.05 (2-tailed) unless otherwise noted. Statistical analyses were conducted using SPSS, version 22 (IBM, Armonk, NY).
For all study measures, general linear model mixed-model repeated measures analyses of variance (ANOVAs) were computed to determine whether there were significant score changes across the 5 measurement times (baseline; months 3, 6, 12, and 24), and whether those changes differed between the EXP and COM groups. These were followed up by planned t tests to assess and contrast within-group changes during the weight-loss phase (using 1-tailed tests) and the weight-loss maintenance phase. Their associated effect sizes were computed as Cohen’s d ([meanpost - meanpre]/SDpre). Effect sizes for ANOVA models were calculated using partial η-squared (η2p = SSeffect/[SSeffect + SSerror]). For d and η2p, 0.20, 0.50, 0.80; and 0.01, 0.06, 0.14 denote small, moderate, and large effects, respectively.
Part 1: Weight Change
After completing planned ANOVAs and follow-up tests on weight, and on the basis of research suggesting that ≥ 5% weight loss is the threshold for health benefits,3 the percentage of participants attaining this criterion was reported for month 6 (end of the weight-loss phase) and month 24 (end of the study), by group. Because ≥ 3% loss has been the suggested criterion for maintained weight loss,6 attainment of this change was also reported at month 24. Weight-change data previously published on the Oxford CBT21 were also adapted for additional contrasting.
Part 2: Behavioral Predictors of Weight Changes
After completing planned ANOVAs and follow-up tests on PA and FV, data were aggregated across groups. The strengths of bivariate relationships between changes in PA and FV from baseline-month 3, baseline-month 6, and month 3-month 6, for the prediction of change in weight over the weight-loss phase, were then contrasted. Given the data collected, all possible temporal intervals of changes in PA and FV during the course of the 24-month investigation were similarly contrasted for predicting change in weight during the weight-loss maintenance phase. As was previously suggested,73 wherever possible, behavioral changes occurring during the weight-loss phase were statistically controlled for.
Part 3: Psychological Predictors of Behavioral Changes
After completing planned ANOVAs and follow-up tests on the five psychological variables, data were aggregated across groups. Analyses of relationships of changes in the psychological variables using temporal intervals and methods identical to Part 2 were then completed. Data from the temporal intervals found to have the strongest relationships served as the predictors of PA and FV changes in multiple regression equations.
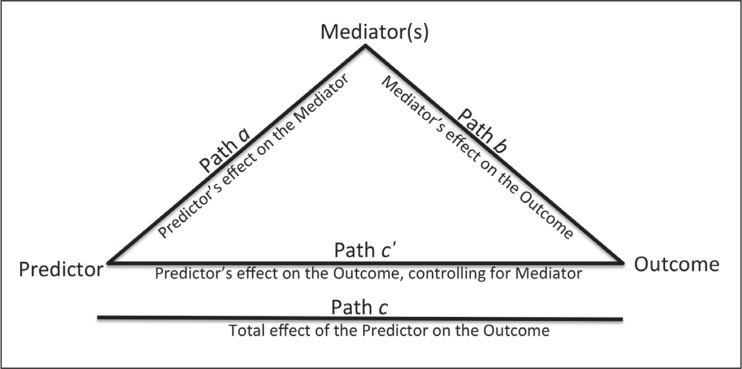
Because 1) the EXP treatment focus was on the carry-over of exercise-related self-regulation and self-efficacy to eating-related self-regulation and self-efficacy, 2) their strong interrelations had previously been supported,33 and 3) previous theory suggested their interactions,35,65 after normalizing (centering and standardizing) scores and confirming expected interrelations, the exercise- and eating-related self-regulation and self-efficacy measures were merged for further analyses. Multiple mediation models incorporating 20,000 bootstrapped resamples74 were specified where the predictor variable was treatment type (0 = COM; 1 = EXP), the outcome variable was weight change during the weight-loss or weight-loss maintenance phase, and the possible mediators were changes in mood and the merged self-regulation and self-efficacy measures. In a multiple mediation model, significance of a mediator is identified when its corresponding 95% confidence interval for an indirect effect does not include 0. A graphical representation of mediation models is given in Figure 2.
Figure 2.
Representation of mediation models.
If a significant mediator was found in the above analysis over the weight-loss phase, follow-up simple mediation models (eg, models with only a single mediator) were then specified to determine whether change in that psychological variable and weight demonstrated a reciprocal relationship. A reciprocal relationship is identified if, after reversing the position of the original outcome and mediator variable within a complementary mediation model, both equations demonstrate significant mediation.42 Because the presence of a reciprocal relationship may not be assessed directly through multiple mediation, or with covariates, these analyses were possible during only the weight-loss phase.
RESULTS
There was no significant difference at baseline between the EXP and COM groups on any study measure. Table 2a provides descriptive statistics of data at baseline and at months 3, 6, 12, and 24. For all variables, there was a significant overall effect and a significant time × group interaction during the 24-month study (Table 2a). Results of follow-up, within-group t-tests, are given in Table 2b.
Table 2a.
Descriptive statistics of study measures and analyses of their changes over 24 months, by groupa
| Baseline (mean ± SD) | Month 3 (mean ± SD) | Month 6 (mean ± SD) | Month 12 (mean ± SD) | Month 24 (mean ± SD) | Effect for timeb (F(4, 432) [η2p]) | Time × group interaction (F(4, 432) [η2p]) | |
|---|---|---|---|---|---|---|---|
| Weight (kg) | |||||||
| Experimental | 94.95 ± 11.44 | 92.03 ± 11.84 | 89.21 ± 11.57 | 89.40 ± 11.86 | 89.84 ± 13.58 | 26.25c [0.196] | 6.84c [0.060] |
| Comparison | 95.36 ± 10.56 | 94.46 ± 10.63 | 93.27 ± 10.44 | 93.51 ± 11.07 | 94.11 ± 11.23 | ||
| Oxford CBTd | 92.34 ± 8.81 | NA | 83.29 ± 10.39 | 84.33 ± 11.11 | 89.45 ± 11.48 | ||
| Physical activity (METs/week) | |||||||
| Experimental | 8.31 ± 7.30 | 28.65 ± 13.56 | 32.77 ± 15.47 | 32.44 ± 15.16 | 23.59 ± 15.15 | 89.01c [0.452] | 9.50c [0.081] |
| Comparison | 9.65 ± 8.14 | 23.51 ± 15.44 | 22.02 ± 12.82 | 23.20 ± 12.60 | 22.40 ± 12.26 | ||
| Fruit and vegetable intake (servings/day) | |||||||
| Experimental | 3.95 ± 1.97 | 5.81 ± 2.39 | 6.42 ± 2.14 | 6.23 ± 2.24 | 5.56 ± 1.90 | 38.92c [0.265] | 4.55e [0.040] |
| Comparison | 3.30 ± 1.81 | 4.25 ± 2.04 | 4.46 ± 2.23 | 4.73 ± 1.99 | 4.62 ± 1.98 | ||
| Self-regulation for exercise | |||||||
| Experimental | 22.53 ± 6.32 | 32.51 ± 4.36 | 33.04 ± 4.28 | 32.27 ± 4.59 | 29.87 ± 5.96 | 64.03c [0.372] | 14.63c [0.119] |
| Comparison | 23.07 ± 6.32 | 26.96 ± 6.12 | 26.58 ± 6.91 | 26.58 ± 6.75 | 26.56 ± 6.69 | ||
| Self-efficacy for exercise | |||||||
| Experimental | 25.87 ± 9.47 | 33.38 ± 10.08 | 34.98 ± 10.52 | 33.25 ± 11.73 | 29.36 ± 11.82 | 14.64c [0.119] | 4.27e [0.038] |
| Comparison | 22.36 ± 9.73 | 25.47 ± 10.89 | 25.29 ± 12.25 | 25.98 ± 11.22 | 25.49 ± 10.84 | ||
| Total mood disturbance | |||||||
| Experimental | 25.69 ± 15.45 | 9.17 ± 15.00 | 4.55 ± 11.54 | 7.96 ± 11.88 | 9.38 ± 13.87 | 53.56c [0.332] | 8.62c [0.074] |
| Comparison | 21.71 ± 11.50 | 12.25 ± 8.12 | 13.89 ± 11.50 | 12.78 ± 11.88 | 13.47 ± 11.51 | ||
| Self-regulation for controlled eating | |||||||
| Experimental | 23.75 ± 5.60 | 31.25 ± 4.57 | 32.51 ± 4.00 | 31.96 ± 4.19 | 29.82 ± 5.68 | 64.16c [0.373] | 5.64c [0.050] |
| Comparison | 22.05 ± 5.78 | 26.91 ± 5.54 | 26.78 ± 5.59 | 26.44 ± 5.23 | 26.29 ± 5.20 | ||
| Self-efficacy for controlled eating | |||||||
| Experimental | 87.82 ± 31.21 | 114.96 ± 26.95 | 126.48 ± 26.51 | 127.26 ± 26.90 | 124.69 ± 28.34 | 47.29c [0.305] | 4.39e [0.039] |
| Comparison | 88.24 ± 33.80 | 104.65 ± 27.17 | 108.00 ± 30.76 | 110.35 ± 30.45 | 108.18 ± 29.90 | ||
Experimental group, n = 55; comparison group, n = 55.
Analysis of variance effects for time, and time × group interactions, contrast changes from baseline to month 24.
p < 0.001.
These data were adapted from previous research21 for contrasting purposes.
p < 0.01.
CBT = Cognitive Behavioural Therapy; MET = metabolic equivalent; SD = standard deviation.
Table 2b.
Planned follow-up t-test results over the weight-loss phase (baseline-month 6) and weight-loss maintenance phase (months 6–12), by groupa
| Group | t(54) | p vaue | d | |
|---|---|---|---|---|
| Weight (kg) change | ||||
| Weight-loss phase | EXP | −11.18 | < 0.001 | 0.50 |
| COM | −5.13 | < 0.001 | 0.20 | |
| Weight-loss maintenance phase | EXP | 0.61 | 0.274 | 0.05 |
| COM | 1.87 | 0.033 | 0.08 | |
| Entire study period (baseline-month 24) | EXP | −4.59 | < 0.001 | 0.45 |
| COM | −1.86 | 0.068 | 0.12 | |
| Physical activity change (METs/week) | ||||
| Weight-loss phase | EXP | 11.83 | < 0.001 | 3.18 |
| COM | 8.89 | < 0.001 | 1.52 | |
| Weight-loss maintenance phase | EXP | −4.42 | < 0.001 | 0.59 |
| COM | 0.30 | 0.764 | 0.03 | |
| Fruit and vegetable intake change (servings/day) | ||||
| Weight-loss phase | EXP | 7.67 | < 0.001 | 1.24 |
| COM | 3.90 | < 0.001 | 0.64 | |
| Weight-loss maintenance phase | EXP | −3.07 | 0.003 | 0.40 |
| COM | 1.04 | 0.302 | 0.07 | |
| Self-regulation for exercise change | ||||
| Weight-loss phase | EXP | 10.79 | < 0.001 | 1.66 |
| COM | 4.56 | < 0.001 | 0.56 | |
| Weight-loss maintenance phase | EXP | −4.54 | < 0.001 | 0.53 |
| COM | −0.03 | 0.974 | 0.003 | |
| Self-efficacy for exercise change | ||||
| Weight-loss phase | EXP | 8.56 | < 0.001 | 0.96 |
| COM | 0.79 | 0.039 | 0.30 | |
| Weight-loss maintenance phase | EXP | −4.10 | < 0.001 | 0.53 |
| COM | 0.19 | 0.848 | 0.02 | |
| Total mood disturbance change | ||||
| Weight-loss phase | EXP | −9.21 | < 0.001 | 1.37 |
| COM | −5.58 | < 0.001 | 0.68 | |
| Weight-loss maintenance phase | EXP | 2.86 | 0.006 | 0.42 |
| COM | −0.44 | 0.663 | 0.04 | |
| Self-regulation for controlled eating change | ||||
| Weight-loss phase | EXP | 10.33 | < 0.001 | 1.56 |
| COM | 6.54 | < 0.001 | 0.81 | |
| Weight-loss maintenance phase | EXP | −4.25 | 0.001 | 0.67 |
| COM | −1.25 | 0.218 | −0.08 | |
| Self-efficacy for controlled eating change | ||||
| Weight-loss phase | EXP | 8.15 | < 0.001 | 1.24 |
| COM | 4.37 | < 0.001 | 0.58 | |
| Weight-loss maintenance phase | EXP | −0.46 | 0.646 | 0.07 |
| COM | 0.13 | 0.899 | 0.01 | |
Experimental group (EXP), n = 55; Comparison group (COM), n = 55.
MET = metabolic equivalent.
Part 1: Weight Change
During the weight-loss phase, although within-group reductions in weight in the EXP group (−5.73 kg) and COM group (−2.09 kg) were both significant, the EXP group had a significantly greater between-group reduction in weight, t(108) = 5.56, p < 0.001, d = 1.07. During the weight-loss maintenance phase, within-group weight regain in the EXP group (0.63 kg) was not significant, whereas it was significant in the COM group (0.84 kg). During the full 24-month duration of the study, reduction of weight was significant in the EXP group (−5.11 kg), but not significant in the COM group (−1.25 kg). Between-group reduction in weight was significantly greater over 24 months in the EXP group, t(108) = 2.95, p = 0.004, d = 0.58.
At month 6, ≥ 5% weight loss was found in 65.5% of EXP and 18.2% of COM participants. At month 24, ≥ 5% weight loss was found in 52.7% of EXP and 16.4% of COM participants. At month 24, ≥ 3% weight loss was found in 63.6% of EXP and 38.2% of COM participants. Figure 3 provides a graphic representation of percentages of weight change for 24 months, including data adapted from research on the Oxford CBT.21
Figure 3.
Percentage of body weight change over 24 months, by group.
CBT = Cognitive-Behavioural Therapy.
Part 2: Behavioral Predictors of Weight Changes
Physical Activity
During the weight-loss phase, although within-group increases in PA in the EXP group and the COM group were both significant, the EXP group had a significantly greater between-group increase, t(108) = 4.86, p < 0.001, d = 0.94. There was a significant between-group difference in PA change during the weight-loss maintenance phase, t(108) = −3.93, p < 0.001, d = 0.77, with the EXP group demonstrating a significant within-group reduction and the COM group showing no significant change.
Eating
During the weight-loss phase, within-group increases in FV in the EXP group and the COM group were both significant, and significantly greater in the EXP group, t(108) = 2.97, p = 0.002, d = 0.57. There was a significant between-group difference in FV change during the weight-loss maintenance phase, t(108) = −3.20, p = 0.002, d = 0.64, with the EXP group having a significant within-group reduction and the COM group exhibiting no significant change.
Prediction of Weight Change
The temporal interval that was the strongest predictor of weight change during the weight-loss phase was baseline-month 6 for both PA and FV. β(standard error)-values were −0.38(0.05) and −0.30(0.33), respectively; p values < 0.001. The temporal interval that was the strongest predictor of weight change during the weight-loss maintenance phase was month 6-month 24 for both PA and FV. β(standard error)-values were −0.45(0.11) and −0.28(0.87), respectively; p values < 0.001 and 0.018, respectively.
Part 3: Psychological Predictors of Behavioral Changes
Self-Regulation for Exercise
During the weight-loss phase, within-group increases in SR-exercise in the EXP group and the COM group were both significant, and significantly greater in the EXP group, t(108) = 5.64, p < 0.001, d = 1.09. There was a significant between-group difference in SR-exercise reduction during the weight-loss maintenance phase, t(108) = −3.51, p = 0.001, d = 0.67, with the EXP group demonstrating a significant within-group reduction and the COM group showing no significant change.
Self-Efficacy for Exercise
During the weight-loss phase, within-group increases in SE-exercise in the EXP group and the COM group were both significant, and significantly greater in the EXP group, t(108) = 2.94, p = 0.007, d = 0.52. There was a significant between-group difference in SE-exercise change during the weight-loss maintenance phase, t(108) = −3.39, p = 0.001, d = 0.65, with the EXP group showing a significant within-group reduction and the COM group having no significant change.
Mood
During the weight-loss phase, within-group reductions in Mood score in both the EXP group and the COM group were significant, and significantly greater in the EXP group, t(108) = −4.98, p = 0.002, d = 0.98. There was a significant between-group difference in Mood change during the weight-loss maintenance phase, t(108) = 2.70, p = 0.008, d = 0.54, with the EXP group demonstrating a significant within-group score increase and the COM group exhibiting no significant change.
Self-Regulation for Controlled Eating
During the weight-loss phase, within-group increases in SR-eating in the EXP group and the COM group were both significant, and significantly greater in the EXP group, t(108) = 3.64, p < 0.001, d = 1.08. There was a significant between-group difference in SR-eating reduction during the weight-loss maintenance phase, t(108) = −2.57, p = 0.012, d = 0.52, with the EXP group having a significant within-group reduction and the COM group showing no significant change.
Self-Efficacy for Controlled Eating
During the weight-loss phase, within-group increases in SE-eating in the EXP group and the COM group were significant, and significantly greater in the EXP group, t(108) = 2.88, p = 0.005, d = 0.55. There was no significant between-group difference in SE-eating change during the weight-loss maintenance phase, t(108) = −0.48, p = 0.635, d = 0.10, with neither the EXP or COM group demonstrating a significant within-group change.
Prediction of Physical Activity Change
The temporal interval that was the strongest predictor of change in PA during the weight-loss phase was from baseline-month 6 for SR-exercise, SE-exercise, and Mood. β(standard error)-values were 0.58(0.15), 0.50(0.10), and −0.46(0.08), respectively; all p values < 0.001. The temporal interval that was the strongest predictor of change in PA during the weight-loss maintenance phase was baseline-month 24 for SR-exercise, SE-exercise, and Mood. β(standard error)-values were 0.65(0.24), 0.57(0.14), and −0.52(0.17), respectively; all p values < 0.001.
After incorporating the above temporal intervals into the following two models, the multiple regression equation predicting PA change during the weight-loss phase was significant. Changes in SR-exercise, SE-exercise, and Mood were each significant independent predictors (after controlling for one another). The prediction of PA change during the weight-loss maintenance phase was significant. Changes in SR-exercise and SE-exercise, but not Mood, were significant independent predictors (Table 3).
Table 3.
Results of multiple regression analyses for the prediction of changes in physical activity and fruit and vegetable intake
| Predictor | β | Standard error | R2 | F | df | p value |
|---|---|---|---|---|---|---|
| Δ Physical activity, baseline-month 6 | ||||||
| Model | 0.42 | 25.96 | 3, 109 | < 0.001 | ||
| Δ Self-regulation for exercise | 0.36 | 0.19 | < 0.001 | |||
| Δ Self-efficacy for exercise | 0.21 | 0.11 | 0.028 | |||
| Δ Overall negative mood | −0.25 | 0.08 | 0.003 | |||
| Δ Physical activity, month 6-month 24 | ||||||
| Model | 0.59 | 9.19 | 6, 109 | 0.006 | ||
| Δ Self-regulation for exercise | 0.42 | 0.28 | < 0.001 | |||
| Δ Self-efficacy for exercise | 0.27 | 0.16 | 0.044 | |||
| Δ Overall negative mood | −0.23 | 0.13 | 0.093 | |||
| Δ Fruit and vegetable intake baseline-month 6 | ||||||
| Model | 0.52 | 13.08 | 3, 109 | < 0.001 | ||
| Δ Self-regulation for controlled eating | 0.20 | 0.04 | 0.048 | |||
| Δ Self-efficacy for controlled eating | 0.26 | 0.01 | 0.013 | |||
| Δ Overall negative mood | −0.19 | 0.01 | 0.049 | |||
| Δ Fruit and vegetable intake month 6-month 24 | ||||||
| Model | 0.46 | 4.57 | 6, 109 | < 0.001 | ||
| Δ Self-regulation for controlled eating | 0.12 | 0.04 | 0.202 | |||
| Δ Self-efficacy for controlled eating | 0.33 | 0.01 | 0.080 | |||
| Δ Overall negative mood | −0.15 | 0.02 | 0.352 | |||
Δ = change in.
Prediction of Eating Change
The temporal interval that was the strongest predictor of change in FV during the weight-loss phase was the same for baseline-month 3 and baseline-month 6 for SR-eating, and was baseline-month 6 for both SE-eating and Mood. β(standard error)-values were 0.41(0.03), 0.45(0.01), and −0.37(0.08), respectively; all p values < 0.001. The temporal interval that was the strongest predictor of change in FV during the weight-loss maintenance phase was month 12-month 24 for SR-eating, and baseline-month 24 for both SE-eating and Mood. β(standard error)-values were 0.19(0.04), 0.47(0.01), and −0.31(0.02), respectively; all p values < 0.050.
After incorporating the above temporal intervals, the multiple regression equation predicting FV change during the weight-loss phase was significant. Changes in SR-eating, SE-eating, and Mood were each significant independent predictors (after controlling for one another) (Table 3). The prediction of FV change over the weight-loss maintenance phase was significant. Neither changes in SR-eating, SE-eating, nor Mood were significant independent predictors (Table 3).
Consolidated Model for Weight-Loss Effects
As expected, correlations of baseline, baseline-month 6, and month 6-month 24 scores between the exercise- and eating-related self-regulation measures (r-values = 0.61–0.66), and exercise- and eating-related self-efficacy measures (r-values = 0.40–0.48) were significant (all p values < 0.001). This further supported merging the exercise-and eating-related self-regulation (ie, SR-merged) and self-efficacy (ie, SE-merged) measures for the planned mediation analyses. The same Mood scale was used in both exercise and eating contexts so no such merger was needed.
In a consolidated model, the SR-merged, SE-merged, and Mood measures (changes from baseline-month 6) were entered as possible mediators of the relationship between treatment type (COM or EXP) and weight change during the weight-loss phase. The overall model was significant, R2 = 0.35, F(4, 105) = 14.23, p < 0.001. Only change in SR-merged was a significant mediator within the equation (Table 4, Analysis I). In the planned simple mediation follow-ups, change in SR-merged significantly mediated the relationship between treatment type and weight change; and weight change significantly mediated the relationship between treatment type and change in SR-merged. This indicated a reciprocal relationship between increases in self-regulation and lost weight during the weight-loss phase (Table 4, Analysis I-a).
Table 4.
Results from multiple mediation and reciprocal effects analyses (N = 110)a
| Predictor | Mediatorc | Outcome | Pathb a | Path b | Path c | Path c’ | Indirect effect |
|---|---|---|---|---|---|---|---|
| β ± standard error (p value) | β ± standard error (p value) | β ± standard error (p value) | β ± standard error (p value) | β ± standard error (95% CI) | |||
| Analysis I: Weight-loss phase (multiple mediation) | |||||||
| Treatment typed | Δ Self-regulation | Δ Weight | 1.13 ± 0.24 (< 0.001) | −2.13 ± 0.70 (0.002) | −8.03 ± 1.44 (< 0.001) | −4.61 ± 1.55 (0.004) | −2.42 ± 1.05 (−4.81, −0.65) |
| Treatment type | Δ Self-efficacy | Δ Weight | 0.77 ± 0.24 (0.002) | 0.20 ± 0.71 (0.780) | −8.03 ± 1.44 (< 0.001) | −4.61 ± 1.55 (0.004) | 0.16 ± 0.71 (−1.27, 1.71) |
| Treatment type | Δ Mood | Δ Weight | −0.86 ± 0.17 (< 0.001) | 1.35 ± 0.79 (0.093) | −8.03 ± 1.44 (< 0.001) | −4.61 ± 1.55 (0.004) | −1.16 ± 0.71 (−2.79, 0.06) |
| Analysis I-a: Weight-loss phase (simple mediation for reciprocal effects analysis) | |||||||
| Treatment type | Δ Self-regulation | Δ Weight | 1.13 ± 0.24 (< 0.001) | −2.27 ± 0.54 (< 0.001) | −8.03 ± 1.44 (< 0.001) | −5.46 ± 1.47 (< 0.001) | −2.56 ± 0.81 (−4.53, −1.23) |
| Treatment type | Δ Weight | Δ Self-regulation | −8.03 ± 1.44 (< 0.001) | −0.06 ± 0.15 (< 0.001) | 1.13 ± 0.24 (< 0.001) | 0.63 ± 0.25 (0.015) | 0.51 ± 0.14 (0.26, 0.82) |
| Analysis II: Weight-loss maintenance phase (multiple mediation) | |||||||
| Treatment type | Δ Self-regulation | Δ Weight | −0.17 ± 0.20 (0.415) | −5.91 ± 1.52 (< 0.001) | 1.91 ± 2.88 (0.509) | 1.42 ± 2.72 (0.604) | 0.98 ± 1.21 (−2.20, 3.32) |
| Treatment type | Δ Self-efficacy | Δ Weight | −0.38 ± 0.20 (0.055) | 2.87 ± 1.75 (0.104) | 1.91 ± 2.88 (0.509) | 1.42 ± 2.72 (0.604) | −1.09 ± 0.77 (−3.77, −0.10) |
| Treatment type | Δ Mood | Δ Weight | 0.16 ± 0.14 (0.055) | 3.81 ± 2.07 (0.068) | 1.91 ± 2.88 (0.509) | 1.42 ± 2.72 (0.604) | 0.60 ± 0.60 (−0.14, 2.36] |
Analyses are based on a bootstrapping procedure for multiple mediation incorporating 20,000 resamples.74
Path a = predictor→mediator; Path b = mediator→outcome; Path c = predictor→outcome; Path c’ = predictor→outcome, controlling for the mediator.
Δ = change from baseline-month 6 for Analysis I and I-a; or baseline-month 24, controlling for changes from baseline-month 6 (for Analysis II).
For treatment type, 0 = comparison group, 1 = experimental group. Δ change in; 95% CI = 95% confidence interval.
The SR-merged, SE-merged, and Mood measures (changes from month 6 to month 24) were entered as possible mediators of the relationship between treatment type and weight change during the weight-loss maintenance phase. The overall model was significant, R2 = 0.20, F(7, 102) = 3.61, p = 0.002. Only change in SE-merged was a significant mediator within the equation (Table 4, Analysis II).
Post Hoc Tests
In post hoc analyses of only the EXP group, a significant quadratic (inverted-U) effect was found during the 24 months of the study in each of the psychological variables, which suggested a reduction in gains acquired during the initial 6 to 12 months. Effect sizes (η2p) associated with those significant ANOVA models (all p values < 0.001) were stronger than for the corresponding linear relationship for SR-exercise (0.611), SE-exercise (0.417), Mood (0.504), and SR-eating (0.600); but not SE-eating (0.374).
DISCUSSION
Overall, findings associated with the EXP treatment were promising. The absence of significant regain of that group’s weight loss of more than 6% was atypical, and represented a notable success (Figure 3).4,5 The experimental format not only elucidated psychological correlates of behavioral prerequisites to weight reduction, it highlighted temporal implications for their application within both weight-loss and weight-loss maintenance phases. Innovative treatment components and administrative formats were successfully incorporated within a practical setting that suggests potential for widespread application. The cost associated with implementation of the EXP treatment approximated US$400 per participant. This was about 10% to 15% of the cost estimated for both the Oxford CBT and an average of the 3 commercial weight-loss programs currently having the strongest market share.75
Specific Findings
Part 1 clearly demonstrated the superiority of the EXP treatment over the COM treatment for weight loss at all measured time points. Regain of weight in the EXP group was only a nonsignificant 0.7% of participants’ original weight, which has not been observed in the great majority of treatment studies of individuals with obesity where a climb toward baseline weight (or higher) almost always occurred after about 6 months of loss.4,5 When contrasted with the Oxford CBT (Figure 1), the EXP treatment had a far less acute slope of weight regain and a much larger proportion of participants who maintained ≥ 5% weight loss at month 24 (52.7% vs 38.8%) (Figure 3).21 This suggested substantial improvements in health risks within the EXP group. In Part 2, effect sizes for increases in both PA and FV during the weight-loss phase were about twice as large in the EXP group. Those large behavioral improvements demonstrated a partial reversal during the second year. In Part 3, within the weight-loss phase, effect sizes of improvements on the psychosocial predictors of PA and FV within the EXP group were also double those in the COM group (all large effects with d-values of 0.96–1.66). However, an inversion of some of those gains appeared between month 12 and month 24. Because these trajectories could adversely impact participants’ weight-management behaviors and weight in subsequent years, extensions of this research are presently evaluating noninvasive methods to lessen such “slippage” through periodic telephone and/or e-mail follow-ups after in-person treatment components conclude. These follow-up contacts will aim to bolster the use of previously addressed self-regulatory skills and feelings of control over behaviors associated with weight management. Part 3 of this study determined that changes in self-regulation, self-efficacy, and mood during the full 6 months of the weight-loss phase best-predicted increased PA and FV. Findings also suggested that changes in self-regulation applied to eating changes might be particularly important within the first several months of treatment. Changes in those 3 psychological factors over the entire weight-maintenance phase (months 6–24) best predicted a favorable direction for PA and FV. However, findings suggested that self-regulation for controlled eating is especially important during the second year. When the above results were consolidated, important findings also emerged. Data suggested that an emphasis on self-regulation during the weight-loss phase, and an emphasis on self-efficacy during the weight-loss maintenance phase, will optimize weight-management outcomes. During the weight-loss phase, changes in self-regulation and weight appeared to reinforce one another mutually. Overall, results supported the EXP treatment’s ability to improve mood and increase self-regulation and self-efficacy related to both physical activity and healthy eating behaviors.
Fit with Previous Research
Although most weight-loss treatments employ an educational approach that focuses upon restricting energy intake, the use of cognitive-behavioral methods and exercise within weight-loss interventions is not novel. However, comprehensive reviews suggest that even the most state-of-the-art, theory-based approaches primarily targeting eating changes have been unsuccessful beyond the very short term.4 Within this report, findings from a previously described17 and tested21 weight-loss/weight-loss maintenance protocol (Oxford CBT) was contrasted with the EXP treatment because of its theoretical similarity, similar research design, and seemingly strong cognitive-behavioral approach. As has been typical, however, exercise was treated as a favorable adjunct to nutritional change rather than a key component of that protocol, and its maintenance of weight loss was unsuccessful.21 Guided by suggestions of the consistent relationship between exercise and maintained weight loss,23–25 previous experimental research on (modifiable) psychosocial correlates of weight loss,40–42,76 our own program of research on the generalization of exercise-induced psychological changes to eating changes during the short term,33,77–85 and recommendations from the National Institutes of Health to address adherence to exercise and establish relevant behavioral skills before attempting weight loss,22 we substantially modified and extended previous approaches. We incorporated assumptions that cognitive-behaviorally supported exercise can facilitate changes in eating and weight through associated psychological changes. Although the present data cannot determine precisely what treatment component(s) or implementation methods were most associated with the present positive results, future research designs might facilitate a more comprehensive decomposition of findings to determine the most salient treatment components and, thus, further enhance effects. We encourage future related research to also study weight-loss and weight-loss maintenance phases separately through behavioral changes and their psychological predictors, because processes within these phases appear to differ from one another. Continued evaluation of temporal aspects might facilitate a more precise process that further refines the benefits of emphasizing specific treatment components at specific times, which might also vary by personal characteristics (eg, initial weight, psychological profile). The present determination that weight loss might most benefit from a concentration on self-regulation, whereas weight-loss maintenance might most benefit from a concentration on self-efficacy, is a start in that direction. Although this research based the architecture of the EXP treatment and the selection and measurement of behavioral and psychological constructs on social cognitive and self-efficacy theory and the many studies following from those paradigms, additional theories (eg, self-determination theory, theory of planned behavior) might also serve as a basis in extensions of this research. The contrast of those results with the present findings will undoubtedly be instructive.
Study Limitations
To increase confidence in findings and assess their generalizability for application, present limitations such as the use of a homogeneous sample of primarily white and middle-class women who were motivated enough to volunteer for treatment require attention. Thus, replications with men, with other racial/ethnic and socioeconomic groups, and possibly with participants who were strongly referred by medical practitioners (to minimize effects of volunteerism) will be beneficial. Replications are also required with overweight participants and participants with a more severe degree of obesity (ie, class 3/morbid obesity). Other limitations of this research indicate a need for better controls for social support and expectation effects that are likely to bias results when interventions differ in length and amount of in-person contact, as was the case here.86 Thus, the use of an attention-matched, or a wait-list, control group might also be useful in replications of this research. Although the repeated-measures design of this study was a strength, multiple administrations of the same self-report instrument increases its measurement error.87 Although it is difficult to accomplish in field settings (that benefit the applicability of findings88,89), the use of more objective and comprehensive measures of exercise (eg, accelerometry) and dietary intake (eg, more extensive nutrition recall instruments) would increase accuracy of the behavioral outcomes. Within the present study, however, because of the length of time required for completion of the seven self-report surveys, any additional time burden placed on participants might have challenged the quality of their responses.90
CONCLUSION
Although the above limitations should be acknowledged, and replications are needed, the EXP treatment has considerable possibilities for dissemination. Its format allows for low-cost implementation in community-based health-promotion settings by staff members with general wellness credentials. It also has a strong potential for physician referral. Whereas pharmacologic and surgical interventions for obesity are available, improving physical activity and eating behaviors will effectively address obesity and their associated health risks for most affected individuals. Despite the fact that sustained improvements in eating and exercise have been difficult for behavioral medicine to effectuate, the present research introduced innovative behavior-change methods that empowered individuals to effectively deal with day-to-day barriers that consistently served as impediments to maintaining clinically important losses in body weight. The use of manageable amounts of exercise to build the self-regulatory skills and improvements in mood that promote a newfound sense of control over eating behaviors might prove to be one of the most viable solutions to the longstanding epidemic of obesity.
Acknowledgments
Mary Corrado, ELS, provided editorial assistance.
Abbreviations Keys
- FV
Fruit and vegetable intake
- Mood
Overall negative mood
- PA
Physical activity
- SE-eating
Self-efficacy for controlling eating
- SE-exercise
Self-efficacy for exercise
- SR-eating
Self-regulation for controlled eating
- SR-exercise
Self-regulation for exercise
Footnotes
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012 Feb 1;307(5):491–7. doi: 10.1001/jama.2012.39. . [DOI] [PubMed] [Google Scholar]
- 2.Aronne LJ. Classification of obesity and assessment of obesity-related health risks. Obes Res. 2002 Dec;10(Suppl 2):105S–115S. doi: 10.1038/oby.2002.203. . [DOI] [PubMed] [Google Scholar]
- 3.Flechtner-Mors M, Ditschuneit HH, Johnson TD, Suchard MA, Adler G. Metabolic and weight loss effects of long-term dietary intervention in obese patients: four-year results. Obes Res. 2000 Aug;8(5):399–402. doi: 10.1038/oby.2000.48. . [DOI] [PubMed] [Google Scholar]
- 4.Mann T, Tomiyama AJ, Westling E, Lew AM, Samuels B, Chatman J. Medicare’s search for effective obesity treatments: diets are not the answer. Am Psychol. 2007 Apr;62(3):220–33. doi: 10.1037/0003-066X.62.3.220. . [DOI] [PubMed] [Google Scholar]
- 5.Jeffery RW, Drewnowski A, Epstein LH, et al. Long-term maintenance of weight loss: current status. Health Psychol. 2000 Jan;19(1 Suppl):5–16. doi: 10.1037/0278-6133.19.Suppl1.5. . [DOI] [PubMed] [Google Scholar]
- 6.National Heart Lung, and Blood Institute. The National Institute of Diabetes and Digestive and Kidney Diseases . Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. NIH publication no. 98-4083 [Internet] Washington, DC: National Institutes of Health; 1998. Sep, [cited 2015 Oct 22]. Available from: www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf. [Google Scholar]
- 7.Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. Int J Obes (Lond) 2006 Mar;30(3):391–9. doi: 10.1038/sj.ijo.0803175. . [DOI] [PubMed] [Google Scholar]
- 8.Amigo I, Fernández C. Effects of diets and their role in weight control. Psychol Health Med. 2007 May;12(3):321–7. doi: 10.1080/13548500600621545. . [DOI] [PubMed] [Google Scholar]
- 9.Kroke A, Liese AD, Schulz M, et al. Recent weight changes and weight cycling as predictors of subsequent two year weight change in a middle-aged cohort. Int J Obes Relat Metab Disord. 2002 Mar;26(3):403–9. doi: 10.1038/sj.ijo.0801920. . [DOI] [PubMed] [Google Scholar]
- 10.Baranowski T, Lin LS, Wetter DW, Resnicow K, Hearn MD. Theory as mediating variables: why aren’t community interventions working as desired? Ann Epidemiol. 1997 Oct;7(7 Suppl):S89–S95. doi: 10.1016/S1047-2797(97)80011-7. . [DOI] [Google Scholar]
- 11.Bandura A. Social foundations of thought and action: a social cognitive theory. 1st ed. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 12.Bandura A. Self-efficacy: the exercise of control. New York, NY: W.H. Freeman & Company; 1997. [Google Scholar]
- 13.Simpson SA, Shaw C, McNamara R. What is the most effective way to maintain weight loss in adults? BMJ. 2011 Dec 28;343:d8042. doi: 10.1136/bmj.d8042. . [DOI] [PubMed] [Google Scholar]
- 14.Look AHEAD Research Group Eight-year weight losses with an intensive lifestyle intervention: the Look AHEAD Study. Obesity (Silver Spring) 2014 Jan;22(1):5–13. doi: 10.1002/oby.20662. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–41. doi: 10.1146/annurev.nutr.21.1.323. . [DOI] [PubMed] [Google Scholar]
- 16.Teixeira PJ, Carraça EV, Marques MM, et al. Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med. 2015 Apr 16;13:84. doi: 10.1186/s12916-015-0323-6. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper Z, Fairburn CG, Hawker DM. Cognitive-behavioral treatment of obesity: a clinician’s guide. New York, NY: The Guilford Press; 2003. [Google Scholar]
- 18.Peterson ND, Middleton KR, Nackers LM, Medina KE, Milsom VA, Perri MG. Dietary self-monitoring and long-term success with weight management. Obesity (Silver Spring) 2014 Sep;22(9):1962–7. doi: 10.1002/oby.20807. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. 2005 Dec;30(3):210–6. doi: 10.1207/s15324796abm3003_5. . [DOI] [PubMed] [Google Scholar]
- 20.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005 Jul;82(1 Suppl):222S–225S. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]
- 21.Cooper Z, Doll HA, Hawker DM, et al. Testing a new cognitive behavioural treatment for obesity: a randomized controlled trial with three-year follow-up. Behav Res Ther. 2010 Aug;48(8):706–13. doi: 10.1016/j.brat.2010.03.008. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.MacLean PS, Wing RR, Davidson T, et al. NIH working group report: innovative research to improve maintenance of weight loss. Obesity (Silver Spring) 2015 Jan;23(1):7–15. doi: 10.1002/oby.20967. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain—a systematic review. Obes Rev. 2000 Oct;1(2):95–111. doi: 10.1046/j.1467-789x.2000.00016.x. . [DOI] [PubMed] [Google Scholar]
- 24.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. National Institutes of Health. Obes Res. 1998 Sep;6(Suppl 2):51S–209S. doi: 10.1002/j.1550-8528.1998.tb00690.x. doi: 10.1002/j.1550-8528.1998.tb00690.x. . Erratum in: Obes Res 1998 Nov;6(6):464. DOI: http://dx.doi.org/10.1002/j.1550-8528.1998.tb00381.x . [DOI] [PubMed] [Google Scholar]
- 25.Svetkey LP, Stevens VJ, Brantley PJ, et al. Weight Loss Maintenance Collaborative Research Group Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008 Mar;299(10):1139–48. doi: 10.1001/jama.299.10.1139. . [DOI] [PubMed] [Google Scholar]
- 26.Annesi JJ. Effects of a cognitive behavioral treatment package on exercise attendance and drop out in fitness centers. Eur J Sport Sci. 2003;3(2):1–16. doi: 10.1080/17461390300073206. . [DOI] [Google Scholar]
- 27.Buckworth J, Dishman RK. Exercise psychology. Champaign, IL: Human Kinetics; 2002. [Google Scholar]
- 28.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008 Jan;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3. . [DOI] [PubMed] [Google Scholar]
- 29.Tudor-Locke C, Brashear MM, Johnson WD, Katzmarzyk PT. Accelerometer profiles of physical activity and inactivity in normal weight, overweight, and obese US men and women. Int J Behav Nutr Phys Act. 2010 Aug 3;7:60. doi: 10.1186/1479-5868-7-60. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sport Exerc. 2011 Jun;43(7):1334–59. doi: 10.1249/MSS.0b013e318213fefb. . [DOI] [PubMed] [Google Scholar]
- 31.Hall KD. What is the required energy deficit per unit weight loss? Int J Obes (Lond) 2008 Mar;32(3):573–6. doi: 10.1038/sj.ijo.0803720. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Annesi JJ, Unruh JL, Marti CN, Gorjala S, Tennant G. Effects of The Coach Approach intervention on adherence to exercise in obese women: assessing mediation of social cognitive theory factors. Res Q Exerc Sport. 2011 Mar;82(1):99–108. doi: 10.1080/02701367.2011.10599726. . [DOI] [PubMed] [Google Scholar]
- 33.Annesi JJ. Supported exercise improves controlled eating and weight through its effects on psychosocial factors: extending a systematic research program toward treatment development. Perm J. 2012 Winter;16(1):7–18. doi: 10.7812/TPP/11-136. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hagger MS, Wood C, Stiff C, Chatzisarantis NL. Ego depletion and the strength model of self-control: a meta-analysis. Psychol Bull. 2010 Jul;136(4):495–525. doi: 10.1037/a0019486. . [DOI] [PubMed] [Google Scholar]
- 35.Baker CW, Brownell KD. Physical activity and maintenance of weight loss: physiological and psychological mechanisms. In: Bouchard C, editor. Physical activity and obesity. 1st ed. Champaign, IL: Human Kinetics; 2000. pp. 311–28. [Google Scholar]
- 36.Landers DM, Arent SM. Physical activity and mental health. In: Singer RN, Hausenblas HA, Janelle CM, editors. Handbook of sport psychology. 2nd ed. New York, NY: John Wiley & Sons, Inc; 2001. pp. 740–65. [Google Scholar]
- 37.Mostafavi-Darani F, Daniali SS, Azadbakht L. Relationship of body satisfaction, with nutrition and weight control behaviors in women. Int J Prev Med. 2013 Apr;4(4):467–74. [PMC free article] [PubMed] [Google Scholar]
- 38.Annesi JJ, Tennant GA. Generalization of theory-based predictions for improved nutrition and weight loss to adults with morbid obesity: implications of initiating exercise. Int J Clin Health Psychol. 2014 Jan;14(1):1–8. doi: 10.1016/S1697-2600(14)70031-6. . [DOI] [Google Scholar]
- 39.Annesi JJ, Johnson PH. Theory-based psychosocial factors that discriminate between weight-loss success and failure over 6 months in women with morbid obesity receiving behavioral treatments. Eat Weight Disord. 2015 Jun;20(2):223–32. doi: 10.1007/s40519-014-0159-7. . [DOI] [PubMed] [Google Scholar]
- 40.Andrade AM, Coutinho SR, Silva MN, et al. The effect of physical activity on weight loss is mediated by eating self-regulation. Patient Educ Couns. 2010 Jun;79(3):320–6. doi: 10.1016/j.pec.2010.01.006. . [DOI] [PubMed] [Google Scholar]
- 41.Mata J, Silva MN, Vieira PN, et al. Motivational “spill-over” during weight control: increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol. 2009 Nov;28(6):709–16. doi: 10.1037/a0016764. . [DOI] [PubMed] [Google Scholar]
- 42.Palmeira AL, Markland DA, Silva MN, et al. Reciprocal effects among changes in weight, body image, and other psychological factors during behavioral obesity treatment: a mediation analysis. Int J Behav Nutr Phys Act. 2009 Feb 9;6:9. doi: 10.1186/1479-5868-6-9. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Godin G. The Godin-Shephard Leisure-Time Physical Activity Questionnaire. Health & Fitness Journal of Canada. 2011;4(1):18–22. [Google Scholar]
- 44.Jetté M, Sidney K, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol. 1990 Aug;13(8):555–65. doi: 10.1002/clc.4960130809. . [DOI] [PubMed] [Google Scholar]
- 45.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985 Sep;10(3):141–6. [PubMed] [Google Scholar]
- 46.Jacobs DR, Jr, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993 Jan;25(1):81–91. doi: 10.1249/00005768-199301000-00012. . [DOI] [PubMed] [Google Scholar]
- 47.Miller DJ, Freedson PS, Kline GM. Comparison of activity levels using Caltrac accelerometer and five questionnaires. Med Sci Sports Exerc. 1994 Mar;26(3):376–82. doi: 10.1249/00005768-199403000-00016. . [DOI] [PubMed] [Google Scholar]
- 48.Gardner DG, Cummings LL, Dunham RB, Pierce JL. Single-item versus multiple-item measurement scales: an empirical comparison. Educational and Psychological Measurement. 1998 Dec;58(6):898–915. doi: 10.1177/0013164498058006003. . [DOI] [Google Scholar]
- 49.MyPlate and historical food pyramid resources [Internet] Washington, DC: US Department of Agriculture; updated 2015 Oct 23 [cited 2015 Dec 4]. Available from: http://fnic.nal.usda.gov/dietary-guidance/myplate-and-historical-food-pyramid-resources. [Google Scholar]
- 50.Champagne CM, Broyles ST, Moran LD, et al. Dietary intakes associated with successful weight loss and maintenance during the Weight Loss Maintenance Trial. J Am Diet Assoc. 2011 Dec;111(12):1826–35. doi: 10.1016/j.jada.2011.09.014. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Annesi JJ, Nandan M, McEwen K. Effects of two cognitive-behavioral physical activity and nutrition treatments on psychosocial predictors of changes in fruit/vegetable and high-fat food intake, and weight. Hellenic Journal of Psychology. 2015;12:40–64. [Google Scholar]
- 52.Epstein LH, Gordy CC, Raynor HA, Beddome M, Kilanowski CK, Paluch R. Increasing fruit and vegetable intake and decreasing sugar intake in families at risk for childhood obesity. Obes Res. 2001 Mar;9(3):171–8. doi: 10.1038/oby.2001.18. . [DOI] [PubMed] [Google Scholar]
- 53.Rolls BJ, Ello-Martin JA, Tohill BC. What can intervention studies tell us about the relationship between fruit and vegetable consumption and weight management? Nutr Rev. 2004 Jan;62(1):1–17. doi: 10.1111/j.1753-4887.2004.tb00001.x. . [DOI] [PubMed] [Google Scholar]
- 54.Mares-Perlman JA, Klein BE, Klein R, Ritter LL, Fisher MR, Freudenheim JL. A diet history questionnaire ranks nutrient intakes in middle-aged and older men and women similarly to multiple food records. J Nutr. 1993 Mar;123(3):489–501. doi: 10.1093/jn/123.3.489. [DOI] [PubMed] [Google Scholar]
- 55.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986 Sep;124(3):453–69. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 56.Saelens BE, Gehrman CA, Sallis JF, Calfas KJ, Sarkin JA, Caparosa S. Use of self-management strategies in a 2-year cognitive-behavioral intervention to promote physical activity. Behav Ther. 2000 Spring;31(2):365–79. doi: 10.1016/S0005-7894(00)80020-9. . [DOI] [Google Scholar]
- 57.Annesi JJ, Marti CN. Path analysis of exercise treatment-induced changes in psychological factors leading to weight loss. Psychol Health. 2011 Aug;26(8):1081–98. doi: 10.1080/08870446.2010.534167. . [DOI] [PubMed] [Google Scholar]
- 58.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992 Mar;63(1):60–6. doi: 10.1080/02701367.1992.10607557. . [DOI] [PubMed] [Google Scholar]
- 59.McAuley E, Mihalko SL. Measuring exercise-related self-efficacy. In: Duda JL, editor. Advances in sport and exercise psychology measurement. Morgantown, WV: Fitness Information Technology, Inc; 1998. pp. 371–90. [Google Scholar]
- 60.McNair DM, Heuchert JWP. Profile of Mood States: POMS: technical update. North Tonawanda, NY: Multi-Health Systems; 2007. [Google Scholar]
- 61.Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991 Oct;59(5):739–44. doi: 10.1037/0022-006X.59.5.739. . [DOI] [PubMed] [Google Scholar]
- 62.Baillot A, Romain AJ, Boisvert-Vigneault K, et al. Effects of lifestyle interventions that include a physical activity component in class II and III obese individuals: a systematic review and meta-analysis. PLoS One. 2015 Apr 1;10(4):e0119017. doi: 10.1371/journal.pone.0119017. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kiernan M, Brown SD, Schoffman DE, et al. Promoting healthy weight with “stability skills first”: a randomized trial. J Consult Clin Psychol. 2013 Apr;81(2):336–46. doi: 10.1037/a0030544. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McKee H, Ntoumanis N, Smith B. Weight maintenance: self-regulatory factors underpinning success and failure. Psychol Health. 2013;28(10):1207–23. doi: 10.1080/08870446.2013.799162. . [DOI] [PubMed] [Google Scholar]
- 65.Teixeira PJ, Silva MN, Coutinho SR, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity (Silver Spring) 2010 Apr;18(4):725–35. doi: 10.1038/oby.2009.281. . [DOI] [PubMed] [Google Scholar]
- 66.Cooper JO, Heron TE, Heward WL. Applied behavior analysis. 2nd ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2007. [Google Scholar]
- 67. ChooseMyPlate.gov [homepage on the Internet]. Alexandria, VA: US Department of Agriculture, Center for Nutrition Policy and Promotion; [cited 2013 Jan 31]. Available from: www.choosemyplate.gov/.
- 68.Brownell KD. The LEARN program for weight management. 10th ed. Euless, TX: American Health Publishing Company; 2004. [Google Scholar]
- 69.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002 Jun;7(2):147–77. doi: 10.1037/1082-989X.7.2.147. . [DOI] [PubMed] [Google Scholar]
- 70.Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2003. [Google Scholar]
- 71.Hair JF, Anderson RE, Tatham RL, Black WC. Multivariate data analysis. 4th ed. New York, NY: Macmillan Publishers; 1995. [Google Scholar]
- 72.Glymour MM, Weuve J, Berkman LF, Kawachi I, Robins JM. When is baseline adjustment useful in analyses of change? An example with education and cognitive change. Am J Epidemiol. 2005 Aug 1;162(3):267–78. doi: 10.1093/aje/kwi187. . [DOI] [PubMed] [Google Scholar]
- 73.Presnell K, Stice E, Seidel A, Madeley MC. Depression and eating pathology: prospective reciprocal relations in adolescents. Clin Psychol Psychother. 2009 Jul-Aug;16(4):357–65. doi: 10.1002/cpp.630. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008 Aug;40(3):879–91. doi: 10.3758/BRM.40.3.879. . [DOI] [PubMed] [Google Scholar]
- 75.Gudzune KA, Doshi RS, Mehta AK, et al. Efficacy of commercial weight-loss programs: an updated systematic review. Ann Intern Med. 2015 Apr 7;162(7):465–532. doi: 10.7326/M14-2238. doi: 10.7326/M14-2238. . Erratum in: Ann Intern Med 2015 May 19; 162(10)739–740. DOI: http://dx.doi.org/10.7326/L15-5130-3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fairburn CG, Brownell KD, editors. Eating disorders and obesity: a comprehensive handbook. 2nd ed. New York, NY: The Guilford Press; 2002. [Google Scholar]
- 77.Annesi J. Effects of treatment differences on psychosocial predictors of exercise and improved eating in obese, middle-age adults. J Phys Act Health. 2013 Sep;10(7):1024–31. doi: 10.1123/jpah.10.7.1024. [DOI] [PubMed] [Google Scholar]
- 78.Annesi JJ. Moderation of age, sex, and ethnicity on psychosocial predictors of increased exercise and improved eating. J Psychol. 2013 Sep-Oct;147(5):455–68. doi: 10.1080/00223980.2012.711785. . [DOI] [PubMed] [Google Scholar]
- 79.Annesi JJ, Tennant GA. Mediation of social cognitive theory variables in the relationship of exercise and improved eating in sedentary adults with severe obesity. Psychol Health Med. 2013;18(6):714–24. doi: 10.1080/13548506.2013.766354. . [DOI] [PubMed] [Google Scholar]
- 80.Annesi JJ, Porter KJ. Reciprocal effects of changes in mood and self-regulation for controlled eating associated with differing nutritional treatments in severely obese women. Clinical Health Promotion. 2013 Oct-Nov;3(2):35–41. [Google Scholar]
- 81.Annesi JJ, Tennant GA. Exercise program-induced mood improvement and improved eating in severely obese adults. Int Q Community Health Educ. 33(4):2012–2013. 391–402. doi: 10.2190/IQ.33.4.f. . [DOI] [PubMed] [Google Scholar]
- 82.Annesi JJ, Mareno N. Temporal aspects of psychosocial predictors of increased fruit and vegetable intake in adults with severe obesity: mediation by physical activity. J Community Health. 2014 Jun;39(3):454–63. doi: 10.1007/s10900-014-9828-8. . [DOI] [PubMed] [Google Scholar]
- 83.Annesi JJ, Tennant GA, Mareno N. Treatment-associated changes in body composition, health behaviors, and mood as predictors of change in body satisfaction in obese women: effects of age and race/ethnicity. Health Educ Behav. 2014 Dec;41(6):633–41. doi: 10.1177/1090198114531783. . [DOI] [PubMed] [Google Scholar]
- 84.Annesi JJ, Johnson PH, Porter KJ. Bi-directional relationship between self-regulation and improved eating: temporal associations with exercise, reduced fatigue, and weight loss. J Psychol. 2015 Sep;149(6):535–53. doi: 10.1080/00223980.2014.913000. . [DOI] [PubMed] [Google Scholar]
- 85.Annesi JJ, Johnson PH, McEwen KL. Changes in self-efficacy for exercise and improved nutrition fostered by increased self-regulation among adults with obesity. J Prim Prev. 2015 Oct;36(5):311–21. doi: 10.1007/s10935-015-0398-z. . [DOI] [PubMed] [Google Scholar]
- 86.Morgan WP. Methodological considerations. In: Morgan WP, editor. Physical activity and mental health. Washington, DC: Taylor & Francis; 1997. pp. 3–32. [Google Scholar]
- 87.Nunally JC, Bernstein IH. Psychometric theory. 3rd ed. New York, NY: McGraw-Hill Inc; 1994. [Google Scholar]
- 88.Committee on Evaluating Progress of Obesity Prevention Effort. Food and Nutrition Board. Institute of Medicine . Evaluating obesity prevention efforts: a plan for measuring progress. 1st ed. Washington, DC: National Academies Press; 2013. [Google Scholar]
- 89.Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–33. doi: 10.1146/annurev.publhealth.28.021406.144145. . [DOI] [PubMed] [Google Scholar]
- 90.Galesic M, Bosnjak M. Effects of questionnaire length on participation and indictors of response quality in a web survey. Public Opinion Quarterly. 2009;73(2):349–60. doi: 10.1093/poq/nfp031. . [DOI] [Google Scholar]