Abstract
Background:
The physical risk factors leading to distal radial fractures are poorly understood. The goal of this study was to compare postural stability between older adults with and without a prior distal radial fragility fracture.
Methods:
This case-control evaluation was performed at a single tertiary institution. The fracture cohort comprised 23 patients treated for a low-energy distal radial fracture within 6 to 24 months prior to this study. Twenty-three age and sex-matched control participants, without a prior fragility fracture, were selected from an outpatient clinic population. All participants completed a balance assessment with a computerized balance platform device. Dynamic motion analysis (DMA) scores ranging from 0 to 1,440 points are produced, with lower scores indicating better postural stability. Participants also completed validated questionnaires for general health quality (EuroQol-5D-3L [EQ-5D-3L]) and physical activity (Physical Activity Scale for the Elderly [PASE]) and comprehensive health and demographic information including treatment for compromised balance or osteoporosis. Statistical analysis compared data between cases and controls using either the Student t test or the Mann-Whitney U test.
Results:
There were no significant differences (p > 0.05) in age, sex, body mass index, physical activity score, or EQ-5D-3L general health visual analog scale score between participants with or without prior distal radial fracture. The fracture cohort demonstrated poorer balance, with higher DMA scores at 933 points compared with 790 points for the control cohort (p = 0.008). Nineteen patients (83%) in the fracture cohort reported having dual x-ray absorptiometry (DXA) scans within 5 years prior to this study, but only 2 patients (9%) had ever been referred for balance training with physical therapy.
Conclusions:
Older adults who sustain low-energy distal radial fractures demonstrate impaired postural stability compared with individuals of a similar age who have not sustained such fractures. Following a distal radial fracture, these patients may benefit from interventions to improve postural stability.
Level of Evidence:
Prognostic Level III. See Instructions for Authors for a complete description of levels of evidence.
Fractures of the distal part of the radius constitute one-sixth of all fractures seen in emergency departments in the United States and occur in 15% of women older than 50 years of age1-3. The majority of these fractures result from standing-level falls2,4. Although osteoporosis is a recognized risk factor for fragility fractures, it explains only a small percentage of the increased risk for distal radial fractures compared with age-matched controls5. Other factors, such as impaired balance, may play a role in the etiology of distal radial fractures in older adults but are not fully understood.
Fragility fractures of the hip are commonly associated with physically debilitated and frail individuals. However, describing those patients as being at risk for distal radial fractures is not as intuitive6,7. Some functional measures of physical performance, such as the Timed Up and Go test and contralateral grip strength, are decreased in patients who have sustained a distal radial fracture3,8,9. Nevertheless, factors generally associated with frailty, such as difficulty performing physical tasks, slower walking speed, and inactive lifestyle, may actually be protective for distal radial fractures because of reduced exposure to potential falls3,4,6,10. Thus, the patients most at risk for distal radial fractures may be those who have had a subtle decline of physical performance and postural control but are not yet debilitated enough to have a decrease in activity level8.
Providing evidence that physical decline increases risk of distal radial fractures in older individuals has proven to be challenging3,4,6. Despite their frequent use, many “functional” performance tests lack sensitivity in detecting impaired postural control in the osteoporotic population11. For that reason, objective outcome measures derived from computerized dynamic posturography tests, such as the PROPRIO 5000 (Perry Dynamics), are thought to be more suitable11-13. The PROPRIO device differs from its predecessors in that it can accurately measure a subject’s center of mass as a reaction to dynamic stimuli meant to disrupt balance. Although it has external validity to prior balance test systems, the PROPRIO 5000’s unique ability to measure reactive balance to external dynamic stimuli has theoretical advantages over previous methods of postural stability testing13,14.
The primary aim of this study was to determine if older adults with a history of a distal radial fracture display differences in postural stability as measured by the PROPRIO 5000 when compared with adults of the same age without a history of fracture. We hypothesized that patients who had sustained an isolated low-energy distal radial fragility fracture would demonstrate poorer postural stability compared with age and sex-matched controls.
Materials and Methods
Patient Characteristics
Institutional review board approval was obtained and all participants gave informed consent. Participants in the fracture group were identified from a clinical database of patients treated by a single department at a tertiary referral center and were recruited by telephone. To be eligible for the study, participants needed to have a history of distal radial fracture caused by a fall from a standing height and to be 65 years of age or older at the time of injury. Patients were enrolled at a minimum of 6 months (to reduce the influence of any temporary effect of the injury) and a maximum of 24 months (to minimize health status changes) after fracture. The mechanism was defined as “unintentionally coming to rest on the ground, floor, or other lower level in a manner that did not result from a major intrinsic event or an overwhelming hazard.” Participants were required to be English-speaking and to have the cognitive ability to give their informed consent without aid of a guardian. Participants were excluded if they reported a medical condition causing severe balance disturbance—such as stroke, seizure, or vertigo—and also if they had had any new-onset medical conditions in the time since their distal radial fracture that could be reasonably assumed to affect their balance. This included symptomatic musculoskeletal injuries in the lower extremities or spine, or major medical illnesses or recent surgical procedures. Chronic medical comorbidities or orthopaedic conditions present at the time of wrist fracture were felt to be common contributors to balance disturbances in this population and were not grounds for exclusion.
Controls were recruited from the same outpatient clinic population by offering a $25 stipend. Controls were matched by sex and age (within 2 years) to fracture participants in a 1:1 ratio. Control participants had no history of any geriatric fracture. Active disturbance in balance due to acute injury or dysfunction prompted exclusion. Similar to the fracture cohort, chronic medical comorbidities or orthopaedic conditions were not grounds for exclusion.
Because of concerns about patient safety while conducting balance testing, use of an assistive device for community ambulation or medical conditions aggravated by exercise prompted exclusion from both participant groups.
Outcome Measures
Participants were asked about demographic characteristics, medications, medical comorbidities, and musculoskeletal conditions. Additionally, they were interviewed for a bone-health history including history of dual x-ray absorptiometry (DXA) scans, vitamin D and calcium supplementation, and osteoporosis pharmacotherapy. A self-reported fall history and history of balance-focused physical therapy regimens were obtained. The written EuroQol-5D-3L (EQ-5D-3L) general health survey15 and Physical Activity Scale for the Elderly (PASE)16 questionnaires were self-administered. The EQ-5D-3L questionnaire is a patient-reported assessment of current health state on a visual analog scale (VAS) in addition to a categorization of the level of perceived problems (choosing level 1 to 3) in 5 essential dimensions: Mobility, Self-Care, Usual Activities, Pain/Discomfort, and Anxiety/Depression. Height and weight were measured to calculate body mass index (BMI).
Each patient underwent a standardized balance assessment using a PROPRIO 5000 machine that quantifies dynamic postural stability. The system uses a motorized multidirectional moving platform to disturb postural homeostasis. An integrated ultrasonic sensor is placed at the participant’s lumbar region (L5/S1) to measure movement of the center of mass in 6 degrees of freedom every quarter-second of testing. The participants stood on the platform with the feet a shoulder-width apart, the knees slightly flexed, and the center of mass centered over the platform (Fig. 1). A 6-in (15.2-cm) piece of rope was held in the patient’s hands to minimize the stabilizing effect of the upper extremities. Formal testing consisted of three 2-minute tests interrupted by 1-minute breaks. Each trial finished when one of the following criteria was met: 2 minutes elapsed, the patient exceeded 3 in (7.6 cm) of displacement in 0.25 second, the patient moved >5 in (12.7 cm) from the starting point, the patient let go of the rope, the patient moved the feet, or the patient asked to stop.
Fig. 1.

Clinical photograph demonstrating the experimental setup for postural stability testing. The patient assumes a bent-knee posture and is centered on the balance platform with a rope in the hand.
Data Analysis
The PROPRIO 5000 system generates a composite balance score referred to as the dynamic motion analysis (DMA) score. The DMA score, which ranges from 0 to 1,440 points, is calculated by integrated software that uses the sum of the sensor’s vector moments and represents the total three-dimensional displacement of the participant’s center of mass during testing. Lower scores are indicative of less movement and therefore better postural control. The DMA score includes a “dummy score” to account for remaining time in a trial. For example, if a participant completes only 60 seconds of the 120-second test, a dummy score of 720 points is added to the participant’s score that was obtained from the initial 60 seconds of the test. The dummy score represents the maximum score possible per assessment point left in the trial17. A mean DMA score was calculated for each patient on the basis of the 3 trials. The mean time elapsed for each trial was also calculated among the 3 trials.
The PROPRIO 5000 and its accompanying DMA score are relatively recent additions to the field of physical performance measurements. Prior methods to measure differences in fall risk among varied populations have included functional performance tests such as quadriceps strength testing, the Timed Up and Go test, sway meters, and NeuroCom Sensory Organization Test (Natus)11. Although many of its capabilities as a diagnostic and therapeutic tool are still being catalogued and understood, the DMA score has been studied in other clinical settings17 and has been validated relative to other assessment technologies in the field13,14.
A sample size analysis was performed prior to study initiation using the baseline data from a prior study that used the PROPRIO 5000 in an older population that had undergone hip arthroplasty and had a mean DMA score (and standard deviation) of 807 ± 44.7 points17. The minimal clinically important difference of the DMA scores was calculated to be 22 points on the basis of the distribution-based method of halving the standard deviation (effect size, 0.5)18. To achieve a power of 0.8 at a 0.05 level of significance using the two-sided unpaired t test, it was determined that we would need 33 patients per group to prove the 22-point minimal clinically important difference. An interim analysis was planned to check data variance, as PROPRIO 5000 testing of patients after distal radial fracture had not been performed previously, to our knowledge. This analysis demonstrated a larger-than-expected difference in the primary outcome that was already significant at 46 total patients; thus, data collection was stopped prior to full enrollment.
The distributions of the continuous outcome measures were tested for normality using the Kolmogorov-Smirnov test. Age, height, BMI, numbers of medications and medical comorbidities, PASE scores, elapsed time, and DMA scores were normally distributed among the study population and were compared between groups using the Student t test. Weight, EQ-5D-3L VAS scores, and DXA T-scores were not normally distributed and were compared using Mann-Whitney U testing. All other outcomes were recorded as categorical variables, which were compared between the two participant groups using either chi-square or Fisher exact tests. All statistical analyses were performed using SPSS 20 (IBM).
Results
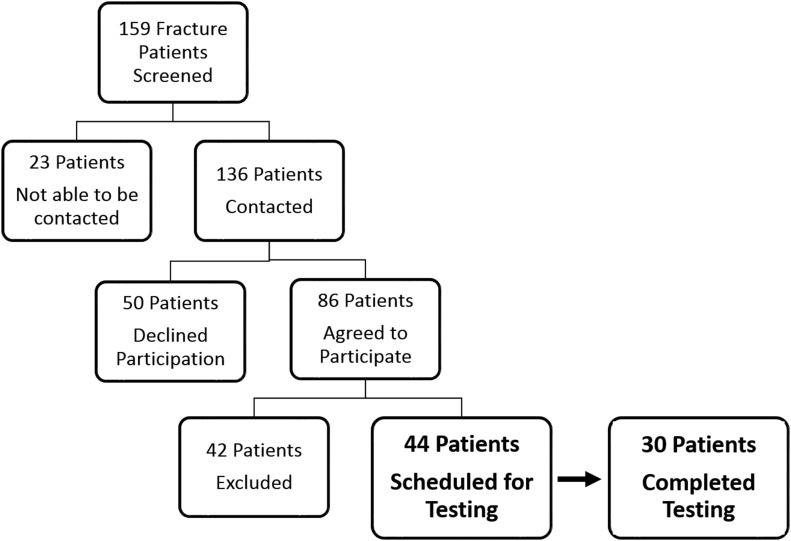
After participant recruitment and appropriate screening, 30 patients in the fracture group and 25 patients in the control group completed testing (Fig. 2). Twenty-three members of each group met matching conditions and were included in the statistical analysis. Baseline characteristics demonstrated no significant differences between groups except for an increased number of reported falls among fracture participants (p = 0.04) (Table I). There were also no significant differences between groups with regard to self-reported physical activity (PASE score) (p = 0.85) and perceived overall health (EQ-5D-3L) (p = 0.23).
Fig. 2.
Flow diagram demonstrating the selection of patients for the fracture group.
TABLE I.
Comparison of Study Groups
| Control Group (N = 23) | Fracture Group (N = 23) | P Value | |
| Age* (yr) | 72.0 ± 5.1 | 72.7 ± 5.2 | 0.69 |
| No. (%) of male patients | 2 (9%) | 2 (9%) | |
| BMI* (kg/m2) | 27.7 ± 4.8 | 28.6 ± 7.2 | 0.93 |
| EQ-5D-3L general health VAS† (points) | 88 ± 10.0 | 85 ± 14.2 | 0.23 |
| PASE* (points) | 132 ± 66 | 128 ± 73 | 0.85 |
| No. of medical comorbidities* | 2.96 ± 1.69 | 2.96 ± 1.67 | 1.00 |
| No. of medications* | 4.30 ± 2.30 | 4.26 ± 2.70 | 0.96 |
| No. of falls in the past year† | 0 ± 1.3 | 1 ± 2.2 | 0.04 |
| Time elapsed in balance trial* (sec) | 63.8 ± 15.9 | 50.1 ± 17.4 | <0.01 |
| DMA score* (points) | 790 ± 175 | 933 ± 172 | <0.01 |
The values are given as the mean and the standard deviation, and the independent Student t test was used for analyses between groups.
The values are given as the median and the standard deviation, and the Mann-Whitney U test was used for analyses.
Neither the mean number of medical comorbidities per individual in each group nor the mean number of medications differed between study groups (Table I). The number of subjects taking ≥4 medications, which has been implicated in falls in the older population19, was not significantly different (p = 0.546) between the fracture group (12 patients) and the control group (15 patients). Specific medications known to contribute to falls in this population did not differ significantly among the groups, including diuretics for treatment of hypertension (12 patients in the fracture group compared with 14 patients in the control group; p = 0.532), hypoglycemic agents for diabetes mellitus (3 patients in the fracture group compared with 1 patient in the control group; p = 0.608), and psychoactive medications (7 patients in the fracture group compared with 6 patients in the control group; p = 0.743)19,20. The fracture group and the control group did not differ in their prevalence of potential musculoskeletal confounders (p = 1.00 for both) in the lower extremity (4 patients in the fracture group compared with 3 patients in the control group) or spine (4 patients in the fracture group compared with 3 patients in the control group).
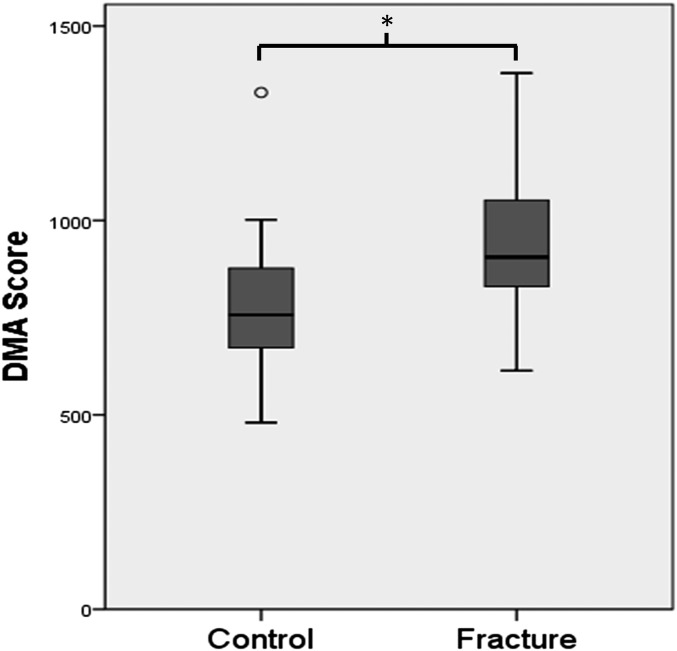
The fracture cohort had significantly decreased postural stability (p = 0.008) when compared with the control cohort, as demonstrated by higher DMA scores (933 points for the fracture group compared with 790 points for the control group) (Fig. 3). The fracture cohort also continued the balance test for significantly less time than the control cohort (p < 0.01) (Table I).
Fig. 3.
Comparison of the DMA scores as a measure of postural stability between study groups. The control group had a score of 790 points and the fracture group had a score of 933 points, and this difference was significant at p = 0.008 (indicated by the asterisk). The box-and-whisker plots represent the total range, the interquartile range, and the median. The circle indicates an outlier (a value >1.5 times the interquartile range from the top whisker).
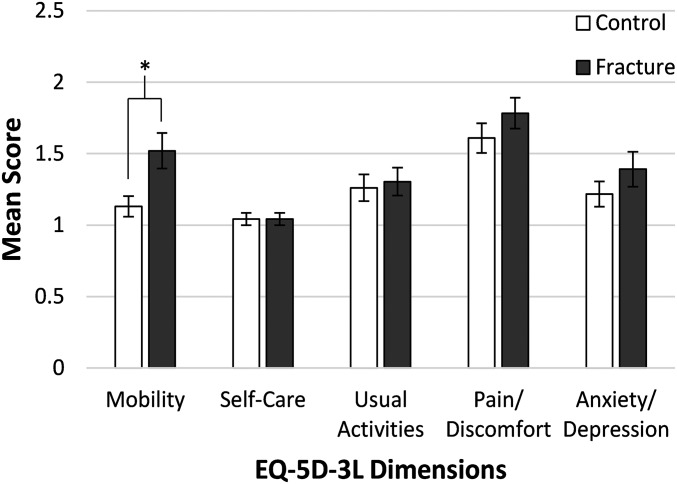
Thirty-nine participants (85%) reported having had a DXA scan within the last 5 years before the current study, with nearly equal prevalence in each group (Table II). Thirty-three patients (72%) were actively taking calcium and vitamin D supplements, and 4 patients (9%) were actively taking prescription medication for osteoporosis, again with no differences between groups. Only 3 patients (7%) had completed a therapy evaluation or treatment regimen to address potential balance deficiencies (Table II). Additionally, the groups were similar in 4 of the dimensions of general health state on the EQ-5D-3L questionnaire, but not for mobility. The difference detected in the mobility subscore revealed that a disproportionate number of patients in the fracture cohort perceived increased difficulty with mobility (p = 0.03) (Fig. 4).
TABLE II.
Diagnostic Tests and Treatment Methods in the Study Cohorts
| Control Cohort* (N = 23) | Fracture Cohort* (N = 23) | P Value† | |
| DXA scan within 5 years prior to the study | 20 | 19 | 1.00 |
| Current calcium and vitamin D supplementation | 17 | 16 | 1.00 |
| Current osteoporosis prescription medication | 1 | 3 | 0.61 |
| Prior or current balance therapy | 1 | 2 | 1.00 |
The values are given as the number of patients.
The Fisher exact test was used for all analyses.
Fig. 4.
Comparison of the EQ-5D-3L subscores, which are scored between 1 and 3 and in which a higher score indicates worse function, between the study groups. Patients in the fracture group had worse self-rated mobility scores than the control cohort, and this difference was significant at p = 0.03 (indicated by the asterisk). Values are plotted as the median and standard deviation.
Discussion
Using modern technology to measure postural stability, we explored the association between physical performance and distal radial fractures. Our data indicate that postural stability is impaired among older adults with a prior distal radial fracture when compared with individuals without a history of fragility fracture. This difference occurred in the absence of any appreciable disparity in age, sex, BMI, level of physical activity, or general health between our samples from these populations. This indicates a subtle, yet measurable, impairment in postural stability in patients who sustain distal radial fractures.
Our data build upon the evaluation of physical performance by Cho et al.8 as a risk factor for distal radial fractures using the Short Physical Performance Battery, grip strength, and time spent walking daily in matched cohorts. Although the overall summary score showed no differences, some individual components such as the chair stand test and contralateral grip strength demonstrated decreased physical performance in the fracture cohort8.
Although functional performance tests such as those used by Cho et al.8 can be criticized as lacking sensitivity11, the detection of these intrinsic differences reveals a need for a more refined investigation of the physical risk factors using more sensitive quantitative methods such as computerized balance platforms7.
The findings of the present study have several implications. Falls are the most common cause of nonfatal injury and hospital admission in older adults, with estimated direct medical costs approaching $30 billion annually, in the United States21. Reducing the incidence and morbidity of falls is thus a prominent public health priority22. In addition to their own associated morbidity and costs, distal radial fractures can be considered sentinel events as they are associated with an estimated 2 to 4 times increased risk of subsequent hip fractures among older adults23-26. If these patients could be identified prior to wrist fracture or more severe injury, interventions to improve postural control could be implemented. A recent Cochrane systematic review confirms the effectiveness of specific exercise programs in reducing the rate of falls, namely programs combining both balance training and muscle strengthening, or tai chi classes in certain populations27-30.
With regard to fragility fracture treatment, the current American Academy of Orthopaedic Surgeons (AAOS) position31 encourages the treating surgeon to “advise patients with fragility fractures that an osteoporosis evaluation may lead to treatment which can reduce the risk of future fractures.” Notably absent are any recommendations to consider the role of balance training and physical conditioning when evaluating a patient with a fragility fracture of the forearm or elsewhere. Current practice trends mirror these guidelines, as evaluation for osteoporosis is becoming a common consideration following these injuries32,33, and assessment and treatment of fall risk are more often overlooked34,35.
There were several potential limitations to this study. Although PROPRIO 5000 use is becoming more widespread because of its potential advantages, it is still a newer technology. The full utility and meaning of the DMA score remain to be seen, but we believe that there is enough data to support this method of measuring balance. Additionally, there was potential for selection bias in this study due to the recruitment method. Recruitment was limited only to those who were willing to return to the clinic for balance testing and therefore likely excluded those patients with poor mobility and decreased independence. However, both groups were recruited from the same clinic population; thus, both groups were assumed to be equally skewed. We attempted to control for other potential confounders by ensuring that the study groups were sex and age-matched, and both groups proved to be similar in terms of demographic characteristics, health state, and physical activity level. Although patients were excluded for health events that would grossly change postural stability following a radial fracture, we acknowledge that a patient’s health could change subtly within 24 months after a distal radial fracture. To minimize bias attributable to this, we matched subjects by age at the time of study testing such that any deterioration in postural stability with aging should have equally impacted patients in the case and control groups.
Lastly, although an association between decreased postural stability and distal radial fracture incidence was demonstrated, causality cannot be established without a longitudinal study design. The study provides evidence that postural stability is compromised after distal radial fracture in the older adult, but we cannot differentiate if instability was present prior to fracture and played a contributing role in the event, or whether it is a consequence of the fall itself. To minimize the physical effects of the fracture event, we chose to evaluate patients who had sustained a distal radial fracture more than 6 months prior to the start of this study and also took steps to ensure that it was an isolated wrist injury without neurologic or musculoskeletal compromise outside of the afflicted upper extremity. Unlike proximal femoral or vertebral compression fractures, which result in permanent alterations in a patient’s lower-extremity function and balance, distal radial fractures offer a unique model to potentially study a patient’s preexisting postural stability deficit after injury has occurred as no permanent change in postural control should occur as a result of a wrist fracture35,36. Additionally, psychological effects from the fracture event itself may also affect balance. Fear of falling has been implicated as a risk factor for subsequent falls in prior studies37, and this cannot be mitigated with our current study design. Interestingly, the self-reported EQ-5D-3L mobility measure is the only subscore that differed in the patients in the fracture group compared with those in the control group, which may be a reflection of patient loss of confidence or fear as a result of the fracture event. It remains unclear if the difficulty mobilizing was present prior to the fracture event itself.
Although deficiencies in physical performance have been long suspected in patients who sustain distal radial fractures, the strength of this association has been difficult to prove3,4,6. This study provides quantitative evidence that there is compromised postural stability in older patients who have sustained distal radial fractures. Clinical practice may need to be modified to address this major contributor to falls and fragility fractures through interventions proven to improve balance, such as programs combining both balance training and muscle strengthening or tai chi classes27-30. Future studies should further examine the association between postural stability and wrist fractures and should determine if treating existing postural instability reduces the risk of subsequent fragility fractures.
Acknowledgments
Note: The authors thank Dr. Dan Osei for his assistance with this project.
Footnotes
Investigation performed at the Sports Therapy and Rehabilitation Center, Barnes-Jewish West County Hospital, Chesterfield, Missouri
Disclosure: One author of this study (L.B.W.) was supported by an institutional training grant, UL1 TR000448, from the National Center for Advancing Translational Science; funds were used to pay for salaries. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article.
References
- 1.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001. September;26(5):908-15. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen TV, Center JR, Sambrook PN, Eisman JA. Risk factors for proximal humerus, forearm, and wrist fractures in elderly men and women: the Dubbo Osteoporosis Epidemiology Study. Am J Epidemiol. 2001. March 15;153(6):587-95. [DOI] [PubMed] [Google Scholar]
- 3.Silman AJ. Risk factors for Colles’ fracture in men and women: results from the European Prospective Osteoporosis Study. Osteoporos Int. 2003. May;14(3):213-8. Epub 2003 Apr 10. [DOI] [PubMed] [Google Scholar]
- 4.Kelsey JL, Prill MM, Keegan TH, Tanner HE, Bernstein AL, Quesenberry CP Jr, Sidney S. Reducing the risk for distal forearm fracture: preserve bone mass, slow down, and don’t fall! Osteoporos Int. 2005. June;16(6):681-90. Epub 2004 Oct 26. [DOI] [PubMed] [Google Scholar]
- 5.Rozental TD, Herder LM, Walley KC, Zurakowski D, Coyle K, Bouxsein ML, Wolf JM. 25-hydroxyvitamin-D and bone turnover marker levels in patients with distal radial fracture. J Bone Joint Surg Am. 2015. October 21;97(20):1685-93. [DOI] [PubMed] [Google Scholar]
- 6.Graafmans WC, Ooms ME, Bezemer PD, Bouter LM, Lips P. Different risk profiles for hip fractures and distal forearm fractures: a prospective study. Osteoporos Int. 1996;6(6):427-31. [DOI] [PubMed] [Google Scholar]
- 7.Benson LS. Physical fitness and orthopaedic health: clues that your intuition is right: commentary on an article by Young Jae Cho, MD, et al.: “Evaluation of physical performance level as a fall risk factor in women with a distal radial fracture”. J Bone Joint Surg Am. 2014. March 5;96(5):e42. [DOI] [PubMed] [Google Scholar]
- 8.Cho YJ, Gong HS, Song CH, Lee YH, Baek GH. Evaluation of physical performance level as a fall risk factor in women with a distal radial fracture. J Bone Joint Surg Am. 2014. March 5;96(5):361-5. [DOI] [PubMed] [Google Scholar]
- 9.Mallmin H, Ljunghall S, Persson I, Bergström R. Risk factors for fractures of the distal forearm: a population-based case-control study. Osteoporos Int. 1994. November;4(6):298-304. [DOI] [PubMed] [Google Scholar]
- 10.O’Neill TW, Marsden D, Adams JE, Silman AJ. Risk factors, falls, and fracture of the distal forearm in Manchester, UK. J Epidemiol Community Health. 1996. June;50(3):288-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Groot MH, van der Jagt-Willems HC, van Campen JP, Lems WF, Lamoth CJ. Testing postural control among various osteoporotic patient groups: a literature review. Geriatr Gerontol Int. 2012. October;12(4):573-85. Epub 2012 Jun 4. [DOI] [PubMed] [Google Scholar]
- 12.Allum JH, Bloem BR, Carpenter MG, Honegger F. Differential diagnosis of proprioceptive and vestibular deficits using dynamic support-surface posturography. Gait Posture. 2001. December;14(3):217-26. [DOI] [PubMed] [Google Scholar]
- 13.Broglio SP, Sosnoff JJ, Rosengren KS, McShane K. A comparison of balance performance: computerized dynamic posturography and a random motion platform. Arch Phys Med Rehabil. 2009. January;90(1):145-50. [DOI] [PubMed] [Google Scholar]
- 14.Charnock BL, Wiliams MW, Sims EL, Garrett WE, Queen RM. Proprio 5000: a new method for assessing dynamic balance. Med Sci Sports Exerc. 2007. April;39:S154-5. [Google Scholar]
- 15.EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199-208. [DOI] [PubMed] [Google Scholar]
- 16.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993. February;46(2):153-62. [DOI] [PubMed] [Google Scholar]
- 17.Larkin B, Nyazee H, Motley J, Nunley RM, Clohisy JC, Barrack RL. Hip resurfacing does not improve proprioception compared with THA. Clin Orthop Relat Res. 2014. February;472(2):555-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003. May;41(5):582-92. [DOI] [PubMed] [Google Scholar]
- 19.Ziere G, Dieleman JP, Hofman A, Pols HA, van der Cammen TJ, Stricker BH. Polypharmacy and falls in the middle age and elderly population. Br J Clin Pharmacol. 2006. February;61(2):218-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson NM, Hilmer SN, March LM, Cameron ID, Lord SR, Seibel MJ, Mason RS, Chen JS, Cumming RG, Sambrook PN. Associations between drug burden index and falls in older people in residential aged care. J Am Geriatr Soc. 2011. May;59(5):875-80. Epub 2011 May 3. [DOI] [PubMed] [Google Scholar]
- 21.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006. October;12(5):290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003. January 2;348(1):42-9. [DOI] [PubMed] [Google Scholar]
- 23.Mallmin H, Ljunghall S, Persson I, Naessén T, Krusemo UB, Bergström R. Fracture of the distal forearm as a forecaster of subsequent hip fracture: a population-based cohort study with 24 years of follow-up. Calcif Tissue Int. 1993. April;52(4):269-72. [DOI] [PubMed] [Google Scholar]
- 24.Nordvall H, Glanberg-Persson G, Lysholm J. Are distal radius fractures due to fragility or to falls? A consecutive case-control study of bone mineral density, tendency to fall, risk factors for osteoporosis, and health-related quality of life. Acta Orthop. 2007. April;78(2):271-7. [DOI] [PubMed] [Google Scholar]
- 25.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM; Study of Osteoporotic Fractures Research Group. Risk factors for hip fracture in white women. N Engl J Med. 1995. March 23;332(12):767-73. [DOI] [PubMed] [Google Scholar]
- 26.Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009. February 4;301(5):513-21. [DOI] [PubMed] [Google Scholar]
- 27.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012. September 12;9:CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011. January;59(1):148-57. [DOI] [PubMed] [Google Scholar]
- 29.Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Am Geriatr Soc. 1996. May;44(5):489-97. [DOI] [PubMed] [Google Scholar]
- 30.Sinaki M, Lynn SG. Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study. Am J Phys Med Rehabil. 2002. April;81(4):241-6. [DOI] [PubMed] [Google Scholar]
- 31.American Academy of Orthopaedic Surgeons. Recommendations for enhancing the care of patients with fragility fractures. Position statement 1159. 2009. December http://www.aaos.org/uploadedFiles/PreProduction/About/Opinion_Statements/position/1159%20Recommendations%20for%20Enhancing%20the%20Care%20of%20Patients%20with%20Fragility%20Fractures.pdf. Accessed 2016 Mar 11.
- 32.Rozental TD, Makhni EC, Day CS, Bouxsein ML. Improving evaluation and treatment for osteoporosis following distal radial fractures. A prospective randomized intervention. J Bone Joint Surg Am. 2008. May;90(5):953-61. [DOI] [PubMed] [Google Scholar]
- 33.Cuddihy MT, Gabriel SE, Crowson CS, Atkinson EJ, Tabini C, O’Fallon WM, Melton LJ 3rd. Osteoporosis intervention following distal forearm fractures: a missed opportunity? Arch Intern Med. 2002. February 25;162(4):421-6. [DOI] [PubMed] [Google Scholar]
- 34.Komatsu T, Kim KJ, Kaminai T, Okuizumi H, Kamioka H, Okada S, Park H, Hasegawa A, Mutoh Y, Yamamoto I. Clinical factors as predictors of the risk of falls and subsequent bone fractures due to osteoporosis in postmenopausal women. J Bone Miner Metab. 2006;24(5):419-24. [DOI] [PubMed] [Google Scholar]
- 35.Khazzani H, Allali F, Bennani L, Ichchou L, El Mansouri L, Abourazzak FE, Abouqal R, Hajjaj-Hassouni N. The relationship between physical performance measures, bone mineral density, falls, and the risk of peripheral fracture: a cross-sectional analysis. BMC Public Health. 2009. August 18;9:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Greig AM, Bennell KL, Briggs AM, Wark JD, Hodges PW. Balance impairment is related to vertebral fracture rather than thoracic kyphosis in individuals with osteoporosis. Osteoporos Int. 2007. April;18(4):543-51. Epub 2006 Nov 15. [DOI] [PubMed] [Google Scholar]
- 37.Maki BE, Holliday PJ, Topper AK. Fear of falling and postural performance in the elderly. J Gerontol. 1991. July;46(4):M123-31. [DOI] [PubMed] [Google Scholar]