Abstract
Zika virus (ZIKV) was discovered in 1947 and was thought to lead to relatively mild disease. The recent explosive outbreak of ZIKV in South America has led to widespread concern with reports of neurological sequelae ranging from Guillain Barré syndrome to microcephaly. ZIKV infection has occurred in areas previously exposed to dengue, a flavivirus closely related to ZIKV. Here we investigate the serological crossreaction between the two viruses. Dengue immune plasma substantially crossreacted with ZIKV and could drive antibody-dependent enhancement of ZIKV infection. Using a panel of human anti-dengue monoclonal antibodies we showed that most antibodies reacting to dengue envelope protein also reacted to ZIKV. Antibodies to linear epitopes including the immunodominant fusion loop epitope while able to bind ZIKV could not neutralize the virus but instead promoted ADE. These data indicate that dengue immunity may drive higher ZIKV replication and have clear implications for disease pathogenesis and future ZIKV and dengue vaccine programs.
ZIKV is an arbovirus belonging to the family flaviviridae and is transmitted to man by Aedes mosquitos1. ZIKV was first isolated from a sentinel rhesus monkey in the Zika forest of Uganda in 1947 and has subsequently been found in mosquitos and humans1. Until recently ZIKV has not been viewed as a particularly important pathogen as the majority of infections are asymptomatic2. Symptomatic cases of ZIKV resemble mild cases of dengue fever with fever, myalgia, arthralgia, headache, conjunctivitis and rash3.
Until recently cases were sporadic, largely in Africa and Southeast Asia and epidemic activity had not been observed1. A large outbreak of ZIKV occurred on Yap island in the Western Pacific in 2007 and spread through Oceania and reached Brazil in 2015 where it rapidly spread to other South American countries1,4–7.
It is now apparent that ZIKV infection can cause significant neurological complications; increased cases of Guillain Barré syndrome were first reported following the outbreak in French Polynesia in 20138. Dramatic increases in the incidence of microcephaly originating in North Eastern Brazil were reported in late 2015 coincident with a large increase in ZIKV infection9,10. These increases in Guillain Barré syndrome and microcephaly led the World Health Organization to declare ZIKV a public health emergency in February 201611.
ZIKV can be carried by a variety of Aedes mosquitos but the principal species responsible for the current outbreaks is thought to be Aedes aegypti1,3. In parts of Brazil A. aegypti is also spreading DENV and chikungunya viruses concurrently with ZIKV12–17. In the last 20 years DENV has spread through areas of South America and the seroprevalence of DENV in some areas affected by ZIKV exceeds 90%18–20.
DENV exists as four serotypes which differ in amino acid sequence by 30-35% and the DENV serocomplex in turn differs from ZIKV by 41-46% (E protein)21. Recent reports have shown difficulty in distinguishing DENV and ZIKV infections serologically implying a degree of antigenic similarity between the viruses4,22,23.
Following a primary DENV infection an individual develops life long immunity to the infecting serotype but not to the other serotypes24,25. In DENV endemic areas all four viruses frequently co-circulate or cyclically replace each other meaning that multiple sequential infections are common26. One of the interesting features of DENV infection is that the life threatening complications, leading to dengue haemorrhagic fever, are more common following secondary rather than primary infections21. One theory to explain this is antibody-dependent enhancement (ADE)21. The ADE hypothesis suggests that antibodies generated to a primary infection will not be of sufficient concentration or avidity to neutralize a secondary infecting DENV, which differs in amino acid sequence by 30-35%. However, they may still opsonize the secondary virus and target it for Fc receptor-mediated endocytosis into myeloid cells, such as monocytes and macrophages, which are the principal site for DENV replication, thus driving higher virus loads. ADE can be readily demonstrated in vitro and has also be shown to drive higher dengue virus loads in animal models27–30.
Here we take advantage of panel of human monoclonal antibodies generated from DENV infected individuals to demonstrate substantial crossreactivity between DENV and ZIKV. Most anti-DENV monoclonal antibodies also bind to ZIKV but those recognizing the major linear fusion loop epitope (FLE) are non-neutralizing to ZIKV whereas they show neutralizing activity against dengue virus. DENV plasma and monoclonal antibodies can potently enhance ZIKV infection suggesting the possibility that preexisting DENV immunity may increase ZIKV replication.
Results
DENV plasma crossreacts with ZIKV
We have previously established a cohort to study dengue infection in children in Khon Kaen in Northeast Thailand. Following informed consent subjects were enrolled and plasma and peripheral blood mononuclear cells were taken during their acute hospital stay and convalescent samples were also obtained around 6 months following discharge. Samples were obtained between 2002 and 2004 (Table 1); at this time ZIKV virus was not described in the Khon Kaen region. Plasma from individuals taken around 6 months following secondary DENV infection with serotypes 1-4 were tested for binding to ZIKV and DENVs by capture ELISA. In all cases DENV immune plasma bound to both DENV and ZIKV (Fig. 1). The overall patterns of binding to viral strains originating in Africa (HD78788) or French Polynesia (PF13) were similar (Fig 1).
Table 1.
Summary of DENV-infected patients enrolled in the study
| Patient id | Age (years) | Sexa | Severity | Serotype of infection |
| K01 | 5 | M | DHF1 | Dengue 1 |
| K02 | 2 | F | DHF3 | Dengue 1 |
| K03 | 15 | M | DHF1 | Dengue 1 |
| K04 | 5 | M | DF | Dengue 1 |
| K06 | 10 | F | DHF1 | Dengue 2 |
| K07 | 11 | M | DHF3 | Dengue 2 |
| K08 | 11 | F | DHF1 | Dengue 2 |
| K09 | 14 | F | DHF1 | Dengue 2 |
| K11 | 14 | F | DHF2 | Dengue 3 |
| K12 | 14 | M | DHF1 | Dengue 3 |
| K13 | 11 | F | DHF2 | Dengue 3 |
| K14 | 13 | M | DF | Dengue 3 |
| K15 | 15 | F | DHF2 | Dengue 4 |
| K16 | 5 | M | DF | Dengue 4 |
| K17 | 8 | F | DF | Dengue 4 |
| K18 | 6 | M | DF | Dengue 4 |
M : Male and F: Female
Figure 1. DENV immune plasma crossreacts with ZIKV.
(a) Binding titration curves of 6 representative DENV sera against ZIKV strains PF13 and HD78788 and DENV measured by capture ELISA (6-month convalescent plasma using the DENV serotype corresponding to their previous acute infection), control pooled non-dengue exposed plasma (PND) shows no binding (closed circles). (b) Endpoint titers of DENV plasma against ZIKV (strain PF13 and HD78788) and DENV determined by capture ELISA (n=16). Small horizontal lines indicate the median values.
Next we tested neutralization of ZIKV by convalescent DENV plasma. All convalescent DENV plasma could neutralize DENV infection to nearly 100% at the lowest dilution used of 1: 50 (Fig. 2a). However, neutralization of ZIKV was considerably less efficient with most sera showing no appreciable neutralization at a 1:50 dilution (Fig. 2b). The three samples that showed appreciable neutralization of ZIKV-HD78788 were among the strongest neutralizers of DENV (Fig. 2b). The finding that anti-DENV plasma substantially crossreacts with ZIKV prompted us to determine whether it could promote ADE.
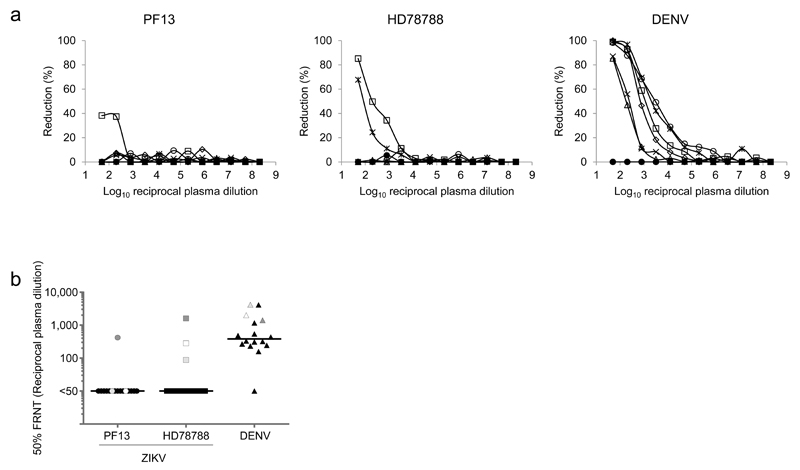
Figure 2. Neutralization of ZIKV by DENV immune plasma.
(a) Neutralization of ZIKV determined on Vero cells for 6 representative DENV plasma with 2 ZIKV strains PF13 and HD78788 and DENV (6-month convalescent plasma using the DENV serotype corresponding to their recent infection). PND was used as negative control (closed circles). (b) NT50 values for DENV plasma on ZIKV and DENV infection (n=16). Small horizontal lines indicate the median values.
DENV plasma potently induces ADE
We tested the ability of DENV plasma to promote ADE in the myeloid cell line U937 which is relatively resistant to infection by DENV in the absence of ADE31 and here we show U937 is also poorly permissive to ZIKV with infection of <0.6% of cells in the absence of ADE (Fig. 3a). ZIKV was preincubated with a titration of pooled convalescent anti-dengue serum obtained at 1-2 weeks and then used to infect U937 cells. Pooled convalescent serum (PCS) led to substantial enhancement of infection >100 fold to both ZIKV viruses (Fig. 3b). As expected, pooled control non-dengue plasma (PND) did not enhance infection (Fig. 3b). Next we tested a panel of convalescent plasma obtained around 6 months following acute secondary DENV infection. In all but one case DENV plasma increased ZIKV infection with a median 12-fold increase of infection by the HD78788 strain of ZIKV (Fig. 3c&d). In summary these results demonstrate that crossreacting anti-DENV antibodies can promote ADE of ZIKV but are poorly neutralizing.
Figure 3. DENV plasma enhances ZIKV infection.
(a) Flow cytometric profiles of U937 cells infected with ZIKV strains PF13 and HD78788 and DENV serotype 2 in the absence or presence of 1:10,000 PCS (the dilution giving peak enhancement) demonstrating the low background infection. (b) ADE curves (fold increase in FFU) of U937 cells infected with ZIKV (strain PF13 and HD78788) and DENV serotype 2 using PCS and PND. (c) Six representative ADE curves (fold increase in FFU) of U937 cells infected with ZIKV strains PF13 and HD78788 and DENV (6-month convalescent plasma using the DENV serotype 2 in the presence of serially diluted DENV plasma). PND was used as negative control (closed circles). (d) Peak fold enhancement (fold increase in FFU) of DENV plasma on ZIKV and DENV (n=16). Small horizontal lines indicate the median values.
Cross reaction of anti-DENV monoclonal antibodies
We have previously created a panel of human monoclonal antibodies reacting to the DENV envelope protein, generated from plasmablasts isolated from DENV-infected patients27. Detailed epitope mapping of these antibodies demonstrated three broad reactivities. Around 1/3 of the antibodies reacted to the well described fusion loop epitope (FLE), 1/3 were not definitively mapped, but like the fusion loop antibodies they reacted to envelope protein by immunoblot (these are termed non-FLE as they were not sensitive to mutation of envelope residue W101). A group of around 50 antibodies did not react to envelope protein by immunoblot and only bound to intact virus particles. These antibodies were shown by cryo-electron microscopy and X-ray crystallography to bind to a conformational quaternary epitope formed at the interface of two envelope protein monomers making up the basic head to tail dimer, 90 of which are arranged in icosahedral symmetry into the DENV glycoprotein shell27,32. We termed this new epitope the E dimer epitope (EDE), which were subdivided into two groups EDE1 and EDE2 based on the sensitivity to the removal of the N-linked glycan N153 in E (EDE2 binding was reduced by removal of N153, while EDE1 binding was not). Some EDE antibodies were fully crossreactive to all four DENV serotypes and could broadly neutralize infection in the picomolar range27.
Binding of the panel of anti-DENV monoclonal antibodies to ZIKV was tested by capture ELISA and compared to their binding to DENV (Fig. 4a). The profile of binding between the African (HD78788) and French Polynesian (PF13) strains was highly similar; all of the fusion loop antibodies crossreacted with ZIKV, 36/37 of the non-fusion loop antibodies crossreacted whereas the crossreaction of the EDE antibodies was variable with 27/33 EDE1 and 8/17 EDE2 binding to ZIKV. Binding curves showed a lower avidity of binding of EDE2 antibodies versus EDE1 and lower avidity of the EDE1 mAb 752-2B2 (Fig. 4b).
Figure 4. Anti- DENV human monoclonal antibodies bind to ZIKV.
(a) Binding of ZIKV strains PF13 and HD78788 and DENV serotype 1 by 33, 17, 45, 37 of anti-EDE1, EDE2, FLE and non-FLE mAbs at 10 μg/ml, also included are 12 mAbs termed IB-3, IB-4 and IB-5 which were poorly neutralizing but reacted to a conformational epitope that was lost when envelope protein was denatured by immunoblotting. These data are representative of three separate experiments. The arrows indicate mAbs used in Fig. 4b, 5, and 6. (b) Binding titration curves for 9 representative mAbs (3 each for anti-EDE1, EDE2, and FLE mAbs). The data shows mean±SEM from 3 independent experiments.
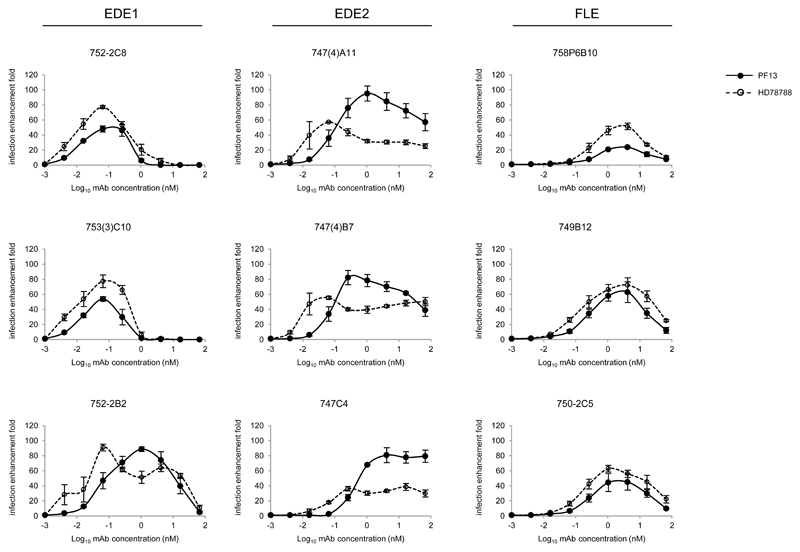
It has previously been demonstrated that almost all mAb generated against DENV promote ADE, which includes all of the human monoclonal antibodies we tested in our previous studies27. Because of the crossreactivity of the DENV mAb to ZIKV we next tested the ability of anti-DENV monoclonal antibodies to promote ADE of ZIKV virus infection (Fig. 5). Firstly, we tested 3 fusion loop antibodies which showed no neutralization activity against ZIKV33. All of these antibodies promoted ADE enhancing infection of the HD78788 strain by 39-91 fold compared to ZIKV incubated with no antibody. As expected, the ZIKV neutralizing EDE mAb33 also promoted ADE of ZIKV when added in subneutralizing concentrations, although peak enhancement was seen with lower concentrations than with the fusion loop mAb. This demonstrates that monoclonal antibodies isolated from dengue infected patients, with a number of different specificities, have broad crossreactivities to ZIKV.
Figure 5. Anti-DENV human monoclonal antibodies enhance ZIKV infection.
Infection enhancement curves (fold increase in FFU) of 9 anti-DENV mAbs (3 each for anti-EDE1, EDE2, and FLE mAbs) on ZIKV strains PF13 and HD78788. U937 cells were used as target cells. The data are shown as mean±SEM from 3 independent experiments.
EDE mAb can inhibit ADE of DENV plasma
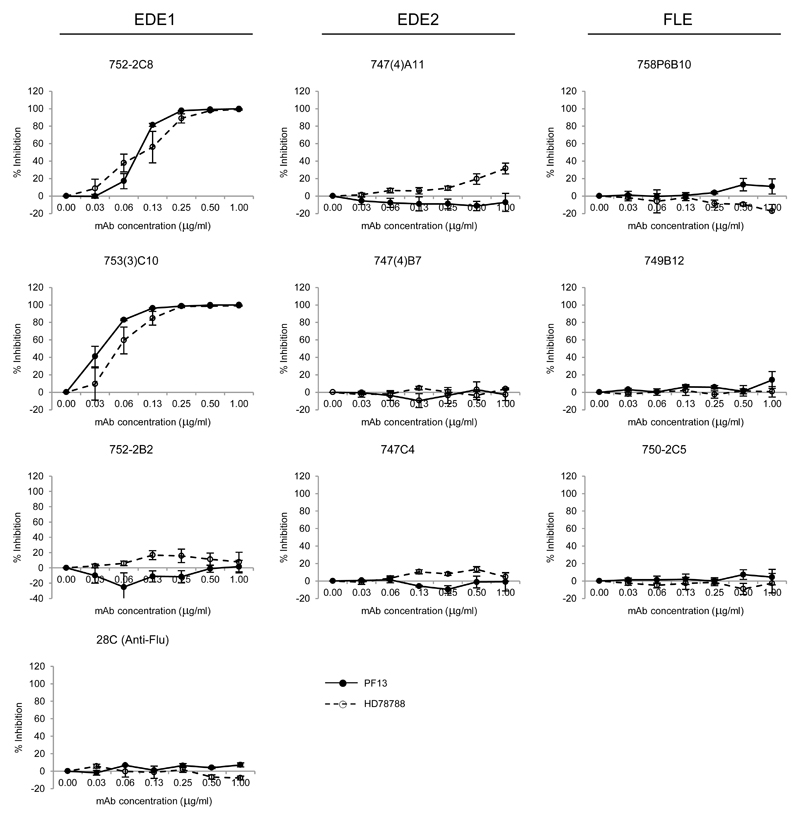
Fusion loop and EDE mAb have overlapping epitopes as the footprint of the EDE also covers the fusion loop region32. To test whether anti-DENV antibodies could overcome ADE induced by polyclonal anti-DENV serum we added a titration of anti-DENV mAbs to ZIKV incubated with an enhancing concentration of anti-DENV serum (Fig. 6). Fusion loop antibodies had no effect, whereas the EDE1 mAb, except 752-2B2 which has lower avidity for ZIKV, were able to potently inhibit ADE of the PF13 strain with 50% inhibition occurring at titers of 0.091±0.007 and 0.034±0.006 μg/ml of 752-2C8 and 753(3)C10, respectively. EDE2 mAb which are of lower avidity for ZIKV than the EDE1 mAb were not able to inhibit ADE in this assay. These studies demonstrate that EDE1 antibodies can potently inhibit ZIKV ADE and if present at sufficient concentrations could be protective in vivo.
Figure 6. Anti-EDE1 human monoclonal antibodies inhibit ADE of DENV plasma.
The inhibition curves of 9 anti-DENV mAbs (3 each for anti-EDE1, EDE2, and FLE mAbs) on ZIKV strains PF13 and HD78788 (fold increase in FFU). U937 cells were infected with ZIKV in the presence of 1:10,000 PCS (the dilution giving peak enhancement) together with serially diluted anti-DENV mAbs. Anti-flu mAb, 28C, was used as a negative control. The data are shown as mean±SEM from 3 independent experiments.
Discussion
The recent explosion of ZIKV virus infection in South America with associated Guillain Barré syndrome and microcephaly are of great concern8–10. Guillain Barré syndrome, is a relatively rare complication, estimated to affect 0.024% of ZIKV-infected individuals, but owing to the scale of the ZIKV epidemic this still translates to large number of cases8. Much work still needs to be performed to understand the exact causes of microcephaly, however, it is becoming increasingly clear that this is caused by intrauterine infection of the developing brain10,34–37. ZIKV has been shown in animal models to infect the placenta and stunt growth and is also able to cross the placenta and infect the brain38–40. Furthermore in vitro ZIKV can infect neural cell cultures and disrupt development in neurospheres41,42. The exact risk of neurological damage following maternal infection remains to be determined, but early studies suggest that this may be up to 22% in the first trimester although other reports from the French Polynesia put the risk at around 1%43,44.
ZIKV is spread by Aedes mosquitos and currently in South America these mosquitos are also promoting epidemic spread of DENV and chikungunya viruses12. In many areas affected by ZIKV the seropositivity to DENV is very high and in such areas there is great difficulty in distinguishing ZIKV and DENV infection serologically19,20,23. In this paper we have demonstrated substantial crossreactivity of the anti-DENV serological response towards ZIKV. Most anti-DENV plasma poorly neutralizes ZIKV yet can potently induce ADE. However, some dengue plasma samples showed appreciable neutralization of ZIKV, one for the PF13 and three for HD78788 strains. Although it is not formally possible to exclude previous ZIKV exposure in these individuals, there were no reports of ZIKV in the Khon Kaen region in 2002-2004 when the samples were taken; more likely they have higher circulating concentrations of crossreactive dengue/ZIKV neutralizing antibodies such as those recognizing the EDE1 epitope33. It is noteworthy that the three plasma samples that showed appreciable neutralization of ZIKV were amongst the four most potent DENV neutralizing plasma samples.
In a related paper neutralization of ZIKV by anti-DENV human monoclonal antibodies was analyzed33. Interestingly, anti-fusion loop antibodies, which form a major part of the antibody response in DENV infection21 and which we showed here promoted ADE, fail to neutralize infection33. Antibodies reacting to the fusion loop are known to be broadly reactive across a number of flaviviruses but despite often strong crossreaction measured by ELISA these antibodies rarely show crossneutralizing activity perhaps because their epitopes are poorly exposed on native virus particles45. In addition, anti-EDE1 mAbs showed potent neutralization in a similar picomolar range to their neutralization of DENV while EDE2 mAb also neutralize ZIKV but not as potently as EDE1 mAb27,33. These results are presented together with X-ray crystallographic structures of EDE1 and EDE2 Fab in complex with the ZIKV envelope33. During the preparation of this manuscript a report investigating the crossreactivity of anti-dengue antibodies with ZIKV was released46. The authors describe crossreaction of dengue immune serum with ZIKV and demonstrate that two human fusion loop monoclonal antibodies can enhance ZIKV infection but do not cause neutralization.
ADE was first recognized nearly 50 years ago in DENV infection and is believed to be one of the factors driving increased severity of secondary infections which is a hallmark of DENV29. The risk of ADE has made the development of DENV vaccines particularly difficult. The most advanced DENV vaccine Dengvaxia (CYD-TDV) produced by Sanofi Pasteur has just been licensed in several countries and gives some protection from infection; it is estimated that it will reduce the burden of disease by 10-30% over a 30 year period if deployed in endemic countries47.
Dengvaxia is a tetravalent live attenuated vaccine where the sequences encoding the precursor membrane protein and envelope proteins that make up the glycoprotein shell of the DENV are combined with the non-structural sequences from the attenuated 17D yellow fever vaccine strain21. Dengvaxia seems to give protection to individuals who have been previously infected with DENV but efficacy is less when given to DENV naïve vaccinees21,47.
A recent longer term analysis of the vaccine trials of Dengvaxia has raised some safety concerns21. In the under 9 age groups hospitalization from DENV infection was higher in vaccinated children compared to the non-vaccinated control group. This may represent ADE in children who at entry to the study trial were DENV naïve and have been primed but not protected by the vaccine. For this reason the vaccine is not licensed for use in children <9 years and furthermore it is recommended to be used only in populations where the seroprevalence of prior DENV exposure in the age group to be vaccinated is 70% or greater47.
There is now great pressure to produce a vaccine against ZIKV, and in this regard the extensive crossreaction between DENV and ZIKV serologically must be considered. It is likely that the vaccine will need to be deployed in areas with high DENV seroprevalence and raising de novo ZIKV neutralizing responses in such a setting may be challenging. There is also the possibility that ZIKV vaccination in DENV naïve subjects may promote ADE of DENV and conversely that DENV vaccination may promote ADE of ZIKV infection.
The results described here show a complex serological interaction between DENV and ZIKV. The precise reason for the explosion of ZIKV infection and its complications in Brazil will need to be fully determined but it is possible that the preexisting DENV immunity is driving higher virus replication in infected individuals which may in turn may drive higher mosquito infection, spread and greater risk of complications following infection. The possibility that ADE may aid transplacental transfer of ZIKV also needs to be investigated. The timings of DENV versus ZIKV infection may also be important as crossreacting protective and enhancing immunity may change over time following DENV infection.
In summary, although ZIKV differs in sequence by around 41-46% (E protein) from DENVs the similarities are sufficient to allow crossreaction of anti-DENV antibodies with ZIKV and to drive antibody dependent enhancement. In this respect ZIKV could be considered as a fifth member of the DENV serocomplex, a factor which must be considered in vaccine approaches to these two viruses.
On-line methods
Samples
Blood samples were collected after written informed consent and the approval of the ethical committee of the Khon Kaen and Siriraj Hospitals in Thailand and the Riverside Ethics Committee in UK. The serotypes of DENV infection was determined by RT-PCR detection of the viral genome48. Samples were collected around 6 months after recovery from dengue illness (Table 1). Secondary dengue infection was classified based on the ratio of anti-dengue IgM/IgG <1.8 measured by IgM and IgG capture ELISA48. The dengue disease severity was classified according to the WHO 1997 classification. Pooled Convalescent serum (PCS) was obtained by combining serum taken from dengue-infected patients around 1-2 weeks after recovery. Pooled negative donor plasma (PND) was taken from normal healthy individuals having no detectable anti-dengue antibodies.
Cells, reagents and antibodies
Vero cells (a gift from AFRIMS), 293T, and U937 cells were cultured at 37°C in MEM, DMEM and RPMI-1640, respectively. C6/36 cells (a gift from AFRIMS) were grown in Leibovitz L-15 at 28°C. All media contained 10% heat-inactivated foetal bovine serum, 100 units/ml penicillin and 100 μg/ml streptomycin. All cell lines were free from mycoplasma contamination.
Alkaline phosphatase (ALP)-conjugated anti-human IgG (A9544) and horseradish peroxidase-conjugated anti-human IgG (P0214) were purchased from Sigma and Dako, respectively. Mouse monoclonal anti-DENV E, 4G2, was a gift from AFRIMS. RPMI-1640 (R8758), DMEM (D5046), p-nitrophenylphosphate (PNPP, N2770-50), Bovine serum albumin (BSA, A7030), diaminobenzidine (D5905), and polyethylenimine (408727; Sigma) were from Sigma. MEM (31095) and Leibovitz L-15 (11415) were from Gibco and UltraDOMA-PF (12-727F) was from Lonza.
Viral stocks
All viruses were grown in C6/36 cells. ZIKV strain HD78788 (African strain) was provided by Anavaj Sakuntabhai. ZIKV strain PF13/251013-18 (PF13) was isolated from a patient during the ZIKV outbreak in French Polynesia in 2013. DENV-1 (Hawaii), DENV-2 (16681), and DENV-3 (H87) were gifts from AFRIMS. DENV-4 (1-0093) was isolated from a DENV-4-infected patient. Virus containing supernatants were clarified by centrifugation at 2000 rpm at 4°C before being stored at −80°C. Viral titres were determined by a focus-forming assays on Vero cells27. All virus stocks were free from mycoplasma contamination.
Expression of human monoclonal anti-DENV E antibodies
A pair of plasmids containing heavy and light chains of immunoglobulin G1 were co-transfected into 293T cells using the polyethylenimine method and cultured in protein-free media. Culture supernatant containing antibodies was harvested after 5 days.
Determination of ZIKV crossreactivity of anti-DENV antibodies by ELISA
A MAXISORP immunoplate (442404; NUNC) was coated with mouse anti-E protein, 4G2 (a fusion loop murine Ab which crossreacts to ZIKV). Plates were blocked with 3% BSA for one hour followed by incubation with viral supernatant. After one hour, 10 μg/ml anti-DENV humAbs or serially diluted plasma was added. The reaction was visualized by ALP-conjugated anti-human IgG antibody at a 1:10,000 dilution (A9544; Sigma) and PNPP substrate. Reactions were stopped with NaOH and the absorbance was measured at 405nm. Endpoint titers (EPTs) were defined as reciprocal plasma dilutions that corresponded to 2 times the average OD values obtained with mock antigen.
Neutralization assay
The focus reduction neutralization assay (FRNT) was employed to determine the neutralizing potential of antibodies. Virus was incubated with serial dilutions of antibodies or plasma samples for an hour at 37°C. The mixtures were then added to Vero cells and incubated for 2 (for ZIKV) or 3 days (for DENV). Focus forming assays were then performed as described27. Briefly, Vero cells were stained with anti-E mAb 4G2 followed by peroxidase-conjugated goat anti-mouse Ig at a 1:1,000 dilution (P0047; Sigma). The foci (infected cells) were visualized by adding peroxidase substrate, DAB. The percentage focus reduction was calculated and 50% FRNT was calculated using the probit program from the SPSS package.
Antibody-dependent enhancement assay
Serially diluted mAb or plasma samples were incubated with virus at moi of 2 (ZIKV) or 5 (DENV) for one hour at 37°C before adding to U937 cells. After incubation for 2 (ZIKV) or 3 days (DENV), supernatants were harvested and viral titres determined by focus forming assays. Fold enhancement was calculated by comparison to viral titres in the presence/absence of antibody. For FACS analysis, infected U937 cells were fixed and permeabilized in 3.7% formaldehyde and 0.5% saponin, respectively. Intracellular staining was performed with 4G2 conjugated with AlexaFluor 647 at 4°C for 30 min. Infected cells were analyzed by BD FACSVerse.
ADE inhibition by human mAbs was performed by premixing pooled convalescent dengue hyper immune serum at 1:10,000 dilution (a peak enhancing dilution) with serially diluted monoclonal antibody before performing the ADE assay as described above.
Acknowledgments
We thank Armed Forces Research Institute of Medicine Sciences, Thailand for anti-DENV E protein mAb, 4G2 and viruses. We also thank Marie Nguyen-De Bernon for her technical assistance. This work was supported by the Medical Research Council, U.K., the Wellcome Trust (G.R.S.), U.K., the National Institute for Health Research Biomedical Research Centre, Funding Scheme, European Commission Seventh Framework Programme [FP7/2007-2013] for the DENFREE project under Grant Agreement n°282 378, and the Thailand Research Fund through the Royal Golden Jubilee PhD (P.S. and J.M.).
Footnotes
Authors’ Contributions:
F.A.R., J.M. and G.R.S. conceived the experiments. W.D., P.S., W.W., A.R., G.B.S. and T.D. performed experiments. P.M. provided specimens. A.S. and V.M.C.L. provided ZIKV strains HD78788 and PF13. W.D., J.M. and G.R.S. analysed data and wrote the paper.
Competing Financial Interests
The EDE antibodies and epitope are the subject of a patent application by Imperial College and Institute Pasteur on which G.S., F.R., A.R. and G.B.S. are named as inventors
References
- 1.Musso D, Gubler DJ. Zika Virus. Clin Microbiol Rev. 2016;29:487–524. doi: 10.1128/CMR.00072-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lazear HM, Diamond MS. Zika Virus: New Clinical Syndromes and Its Emergence in the Western Hemisphere. J Virol. 2016;90:4864–4875. doi: 10.1128/JVI.00252-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Zika Virus Fact sheet. 2016 http://www.who.int/mediacentre/factsheets/zika/en/
- 4.Duffy MR, et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med. 2009;360:2536–2543. doi: 10.1056/NEJMoa0805715. [DOI] [PubMed] [Google Scholar]
- 5.Cao-Lormeau VM, et al. Zika virus, French polynesia, South pacific, 2013. Emerg Infect Dis. 2014;20:1085–1086. doi: 10.3201/eid2006.140138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zanluca C, et al. First report of autochthonous transmission of Zika virus in Brazil. Mem Inst Oswaldo Cruz. 2015;110:569–572. doi: 10.1590/0074-02760150192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Campos GS, Bandeira AC, Sardi SI. Zika Virus Outbreak, Bahia, Brazil. Emerg Infect Dis. 2015;21:1885–1886. doi: 10.3201/eid2110.150847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cao-Lormeau VM, et al. Guillain-Barre Syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet. 2016;387:1531–1539. doi: 10.1016/S0140-6736(16)00562-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teixeira MG, da Conceicao NCM, de Oliveira WK, Nunes ML, Rodrigues LC. The Epidemic of Zika Virus-Related Microcephaly in Brazil: Detection, Control, Etiology, and Future Scenarios. Am J Public Health. 2016;106:601–605. doi: 10.2105/AJPH.2016.303113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mlakar J, et al. Zika Virus Associated with Microcephaly. N Engl J Med. 2016;374:951–958. doi: 10.1056/NEJMoa1600651. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Zika emergency. 2016 http://www.who.int/mediacentre/news/statements/2016/1st-emergency-committee-zika/en/
- 12.Musso D, Cao-Lormeau VM, Gubler DJ. Zika virus: following the path of dengue and chikungunya? Lancet. 2015;386:243–244. doi: 10.1016/S0140-6736(15)61273-9. [DOI] [PubMed] [Google Scholar]
- 13.Cardoso CW, et al. Outbreak of Exanthematous Illness Associated with Zika, Chikungunya, and Dengue Viruses, Salvador, Brazil. Emerg Infect Dis. 2015;21:2274–2276. doi: 10.3201/eid2112.151167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Teixeira MG, et al. East/Central/South African genotype chikungunya virus, Brazil, 2014. Emerg Infect Dis. 2015;21:906–907. doi: 10.3201/eid2105.141727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weaver SC, Lecuit M. Chikungunya virus and the global spread of a mosquito-borne disease. N Engl J Med. 2015;372:1231–1239. doi: 10.1056/NEJMra1406035. [DOI] [PubMed] [Google Scholar]
- 16.Guzman MG, Harris E. Dengue. Lancet. 2015;385:453–465. doi: 10.1016/S0140-6736(14)60572-9. [DOI] [PubMed] [Google Scholar]
- 17.Morrison TE. Reemergence of chikungunya virus. J Virol. 2014;88:11644–11647. doi: 10.1128/JVI.01432-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brathwaite Dick O, et al. The history of dengue outbreaks in the Americas. Am J Trop Med Hyg. 2012;87:584–593. doi: 10.4269/ajtmh.2012.11-0770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Castanha PM, et al. Force of infection of dengue serotypes in a population-based study in the northeast of Brazil. Epidemiol Infect. 2013;141:1080–1088. doi: 10.1017/S0950268812001367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Braga C, et al. Seroprevalence and risk factors for dengue infection in socio-economically distinct areas of Recife, Brazil. Acta Trop. 2010;113:234–240. doi: 10.1016/j.actatropica.2009.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Screaton G, Mongkolsapaya J, Yacoub S, Roberts C. New insights into the immunopathology and control of dengue virus infection. Nat Rev Immunol. 2015;15:745–759. doi: 10.1038/nri3916. [DOI] [PubMed] [Google Scholar]
- 22.Buathong R, et al. Detection of Zika Virus Infection in Thailand, 2012-2014. Am J Trop Med Hyg. 2015;93:380–383. doi: 10.4269/ajtmh.15-0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lanciotti RS, et al. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis. 2008;14:1232–1239. doi: 10.3201/eid1408.080287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guzman MG, et al. Neutralizing antibodies after infection with dengue 1 virus. Emerg Infect Dis. 2007;13:282–286. doi: 10.3201/eid1302.060539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sabin AB. Research on dengue during World War II. Am J Trop Med Hyg. 1952;1:30–50. doi: 10.4269/ajtmh.1952.1.30. [DOI] [PubMed] [Google Scholar]
- 26.Guzman MG, et al. Dengue: a continuing global threat. Nat Rev Microbiol. 2010;8:S7–16. doi: 10.1038/nrmicro2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dejnirattisai W, et al. A new class of highly potent, broadly neutralizing antibodies isolated from viremic patients infected with dengue virus. Nat Immunol. 2015;16:170–177. doi: 10.1038/ni.3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halstead SB, O'Rourke EJ. Dengue viruses and mononuclear phagocytes. I. Infection enhancement by non-neutralizing antibody. J Exp Med. 1977;146:201–217. doi: 10.1084/jem.146.1.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Halstead SB, O'Rourke EJ. Antibody-enhanced dengue virus infection in primate leukocytes. Nature. 1977;265:739–741. doi: 10.1038/265739a0. [DOI] [PubMed] [Google Scholar]
- 30.Zompi S, Harris E. Animal models of dengue virus infection. Viruses. 2012;4:62–82. doi: 10.3390/v4010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brandt WE, McCown JM, Gentry MK, Russell PK. Infection enhancement of dengue type 2 virus in the U-937 human monocyte cell line by antibodies to flavivirus cross-reactive determinants. Infect Immun. 1982;36:1036–1041. doi: 10.1128/iai.36.3.1036-1041.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rouvinski A, et al. Recognition determinants of broadly neutralizing human antibodies against dengue viruses. Nature. 2015;520:109–113. doi: 10.1038/nature14130. [DOI] [PubMed] [Google Scholar]
- 33.Barba-Spaeth G, Dejnirattisai W, Rouvinski A, al e. Structural basis of potent antibody cross-neutralization between Zika and Dengue viruses. Nature. 2016 doi: 10.1038/nature18938. accepted. [DOI] [PubMed] [Google Scholar]
- 34.Calvet G, et al. Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. Lancet Infect Dis. 2016 doi: 10.1016/S1473-3099(16)00095-5. [DOI] [PubMed] [Google Scholar]
- 35.Martines RB, et al. Notes from the Field: Evidence of Zika Virus Infection in Brain and Placental Tissues from Two Congenitally Infected Newborns and Two Fetal Losses - Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:159–160. doi: 10.15585/mmwr.mm6506e1. [DOI] [PubMed] [Google Scholar]
- 36.Meaney-Delman D, et al. Zika Virus Infection Among U.S. Pregnant Travelers - August 2015-February 2016. MMWR Morb Mortal Wkly Rep. 2016;65:211–214. doi: 10.15585/mmwr.mm6508e1. [DOI] [PubMed] [Google Scholar]
- 37.Sarno M, et al. Zika Virus Infection and Stillbirths: A Case of Hydrops Fetalis, Hydranencephaly and Fetal Demise. PLoS Negl Trop Dis. 2016;10:e0004517. doi: 10.1371/journal.pntd.0004517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cugola FR, Fernandes IR, Russo FB, Freitas BC. The Brazilian Zika virus strain causes birth defects in experimental models. Nature. 2016 doi: 10.1038/nature18296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miner JJ, et al. Zika Virus Infection during Pregnancy in Mice Causes Placental Damage and Fetal Demise. Cell. 2016;165:1–11. doi: 10.1016/j.cell.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li C, Xu D, Ye Q, Hong S, Jiang Y. Zika Virus Disrupts Neural Progenitor Development and Leads to Microcephaly in Mice. Cell Stem Cell. 2016;19:1–7. doi: 10.1016/j.stem.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 41.Dang J, et al. Zika Virus Depletes Neural Progenitors in Human Cerebral Organoids through Activation of the Innate Immune Receptor TLR3. Cell Stem Cell. 2016 doi: 10.1016/j.stem.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garcez PP, et al. Zika virus impairs growth in human neurospheres and brain organoids. Science. 2016 doi: 10.1126/science.aaf6116. [DOI] [PubMed] [Google Scholar]
- 43.Brasil P, et al. Zika Virus Infection in Pregnant Women in Rio de Janeiro - Preliminary Report. N Engl J Med. 2016 doi: 10.1056/NEJMoa1602412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cauchemez S, et al. Association between Zika virus and microcephaly in French Polynesia, 2013-15: a retrospective study. Lancet. 2016 doi: 10.1016/S0140-6736(16)00651-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stiasny K, Kiermayr S, Holzmann H, Heinz FX. Cryptic properties of a cluster of dominant flavivirus cross-reactive antigenic sites. J Virol. 2006;80:9557–9568. doi: 10.1128/JVI.00080-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paul LM, et al. Dengue Virus Antibodies Enhance Zika Virus Infection. BioRxiv. 2016 doi: 10.1101/050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Health Organization (WHO) Strategic Advisory Group of Experts. 2016 Dengue vaccine: http://www.who.int/immunization/sage/meetings/2016/april/SAGE_April_2016_Meeting_Web_summary.pdf?ua=1.
- 48.Mongkolsapaya J, et al. Original antigenic sin and apoptosis in the pathogenesis of dengue hemorrhagic fever. Nat Med. 2003;9:921–927. doi: 10.1038/nm887. [DOI] [PubMed] [Google Scholar]