Abstract
Background
The oral minimal model is a simple, useful tool for the assessment of β-cell function and insulin sensitivity across the spectrum of glucose tolerance, including normal glucose tolerance (NGT), prediabetes, and type 2 diabetes mellitus (T2DM) in humans.
Methods
Plasma glucose, insulin, and C-peptide levels were measured during a 180-minute, 75-g oral glucose tolerance test in 24 Korean subjects with NGT (n=10) and T2DM (n=14). The parameters in the computational model were estimated, and the indexes for insulin sensitivity and β-cell function were compared between the NGT and T2DM groups.
Results
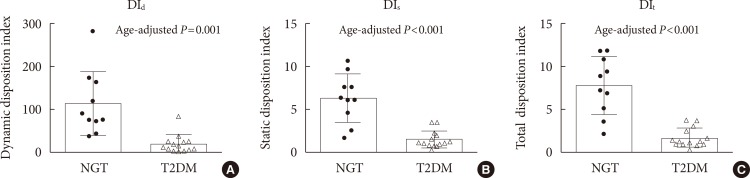
The insulin sensitivity index was lower in the T2DM group than the NGT group. The basal index of β-cell responsivity, basal hepatic insulin extraction ratio, and post-glucose challenge hepatic insulin extraction ratio were not different between the NGT and T2DM groups. The dynamic, static, and total β-cell responsivity indexes were significantly lower in the T2DM group than the NGT group. The dynamic, static, and total disposition indexes were also significantly lower in the T2DM group than the NGT group.
Conclusion
The oral minimal model can be reproducibly applied to evaluate β-cell function and insulin sensitivity in Koreans.
Keywords: Computational method, Disposition index, Glucose tolerance test, Insulin resistance, Oral minimal model, Responsivity index
INTRODUCTION
The pathophysiology of type 2 diabetes mellitus (T2DM), a representative multifactorial disease, is very complex and encompasses decreased β-cell function, unsuppressed α-cell overactivity, increased hepatic glucose production, decreased glucose uptake in the skeletal muscle, increased lipolysis in the adipose tissue, decreased effect of incretin hormones, increased renal glucose reabsorption, and neurotransmitter abnormality [1]. Despite the highly complex nature of glucose homeostasis, there have been continuous efforts to build mathematical models for glucose metabolism using biological variables to predict glucose and insulin responses [2,3,4,5,6]. However, some efforts to adjust numerous variables resulted in an overfitting problem [7]. In this regard, Bergman's minimal model merits by requiring minimal numbers of parameters to estimate β-cell function and insulin sensitivity [8].
Two types of minimal models for the assessment of β-cell function and insulin sensitivity have been developed according to the different routes of glucose administration: intravenous glucose tolerance test (IVGTT) [8] and oral glucose tolerance test (OGTT), or mixed-meal tolerance test [3,9]. The IVGTT-based minimal model consists of glucose and insulin subsystems, where insulin in the plasma compartment passes the endothelium and enters a remote interstitial compartment to exert insulin action. In this model, if plasma insulin levels were solely measured, actual insulin secretion rates (ISRs) might be underestimated owing to the influence of different hepatic extractions of insulin [10]. Therefore, a C-peptide-based model was developed to overcome this shortcoming to estimate more accurate ISRs [11,12]. However, the intravenous administration of glucose is far from the physiologic way of glucose intake, which necessitates further improvement of the model by incorporating the physiology of oral glucose intake [13]. Since the OGTT is the gold standard method to determine glucose tolerance status, glucose, and insulin responses during the OGTT have been incorporated into mathematical models [2,4,14,15]. Among various oral glucose models, the oral minimal model can be easily applied to examine the dynamic physiology of glucose homeostasis, especially during the postprandial period. The oral minimal model comprises three submodels: The glucose minimal model assesses insulin secretion due to intestinal glucose absorption and consequent increases in the plasma glucose levels. The C-peptide minimal model determines how insulin controls the plasma glucose levels. The insulin and C-peptide minimal model was developed based on the C-peptide minimal model to assess the hepatic extraction of insulin. The oral minimal model can also be readily adapted to various situations by modifying its structure.
East Asians have a unique pathophysiology of T2DM. Compared to their Caucasian counterparts, early β-cell deterioration with relatively preserved insulin sensitivity is characteristic during the pathogenesis of T2DM in East Asians [16]. Therefore, it would be meaningful to test whether or not the oral minimal model can be used in the Korean population. In this study, we applied the oral minimal model to Korean subjects with T2DM and normal glucose tolerance (NGT) to assess β-cell function and insulin sensitivity.
METHODS
Subjects and ethical statement
Our study included 14 patients with T2DM and 10 subjects with NGT, aged 18 to 75 years. The T2DM patients were diagnosed according to the criteria by the American Diabetes Association and had been treated with either lifestyle modifications or oral antidiabetic drugs. They did not have diabetic complications, such as retinopathy, microalbuminuria, or cardiovascular disease.
The study protocol was approved by the Institutional Review Board at the Seoul National University Hospital (registration number: H-1504-018-662) and was in compliance with the Declaration of Helsinki, as revised in 2000. Written informed consent was obtained from all of the participants before any study-related procedures.
Study procedures
Before visiting the Biomedical Research Center at the Seoul National University Hospital, all of the subjects had a 1-week washout period for oral antidiabetic drugs. They also fasted the night before the study day. All of the participants underwent a 180-minute, 75-g OGTT. Venous blood was drawn at 0, 15, 30, 60, 90, 120, and 180 minutes for the measurement of plasma glucose, insulin, and C-peptide levels. Glucose was measured by a glucose oxidase method (YSI 2300 STAT Plus analyzer; Yellow Springs Instruments, Yellow Springs, OH, USA). Insulin (DIAsource, Nivelles, Belgium) and C-peptide (Immunotech, Prague, Czech Republic) concentrations were measured with chemiluminescence immunoassay.
The mathematics of the oral minimal model
The oral glucose minimal model and the oral C-peptide minimal model were adopted in this study. The oral glucose minimal model has two ordinary differential equations that represent the changes in plasma glucose and insulin concentrations. From previous studies [3,7,17], the following equations were derived:
| (Equation 1) |
| (Equation 2) |
G(t) is the plasma glucose concentration, V is the glucose distribution volume, and SG is the fractional glucose effectiveness for promoting glucose disposal and altering the net hepatic glucose balance (Equation 1). Ra(t) is the glucose appearance rate in plasma following oral glucose intake. X(t) represents the insulin action on glucose disposal and glucose production, and b denotes the basal value (Equations 1 and 2). Parameters, such as p2 and p3, are rate constants representing the dynamics and magnitude of insulin action. Namely, p2 is the rate constant in the remote insulin compartment (i.e., interstitial compartment) from which insulin action is derived, and p3 is used for the scaling of the amplitude of insulin action [17]. I(t) is the plasma insulin concentration (Equation 2). These equations describe the glucose response to a given insulin action and the intake of glucose from the gastrointestinal tract.
The oral C-peptide minimal model has four ordinary differential equations [3,14]. In this model, C-peptide kinetics is used instead of plasma insulin concentrations for the purpose of reflecting more accurate ISRs.
| (Equation 3) |
| (Equation 4) |
| (Equation 5) |
| (Equation 6) |
Briefly, in Equation 3, q1 and q2 are the increased C-peptide amounts from the basal amounts in the accessible and remote compartments, respectively. ISR means increased C-peptide secretion rates from the basal rates. c1 is the increased C-peptide plasma concentration from the basal level. k01, k12, and k21 are rate constants characterizing C-peptides kinetics. c1 is the increased C-peptide concentration from the basal level, and y(t) is the insulin provision (i.e., the proportion of synthesized insulin reaching the β-cell membrane and ready to be secreted after a delay [T]). KG and β are regarded as dynamic and static parameters, respectively.
The oral insulin and C-peptide minimal model is based on the oral C-peptide minimal model; a subsystem for the hepatic extraction of insulin is inserted. The insulin delivery rate (IDR) and hepatic insulin extraction (HE) can be determined in this model [12].
| (Equation 7) |
| IDR(t)=ISR(t)×[1–HE(t)]/VI | (Equation 8) |
In this model, 'n' is the rate constant of insulin elimination, VI is the distribution volume of insulin, and (1–HE) means the fraction of ISR reaching the C-peptide accessible compartment.
Parameter estimation
Three parameters (SG, p2, and p3) in Equations 1 and 2 were evaluated in the glucose minimal model using clinical data. Their values were obtained by minimizing the nonlinear least square function, which reflects the differences between the anticipated and measured points. Among the three parameters in the oral glucose minimal model, glucose effectiveness SG and the ratio of p2 to p3 are important for characterizing the plasma glucose and insulin responses in each subject. Their values can be precisely estimated due to the inherent robustness of the model against errors in which the estimated ratio of p2 to p3 was nearly consistent, if p2 and p3 were respectively overestimated [18]. During this estimation process, all of the parameters were explored based on the reference values [19,20,21] within the parametric space using optimization techniques. One subject in the NGT group and two subjects in the T2DM group were excluded from this calculation via outlier reduction. The function of the absorption rate of glucose into the mesenteric circulation was derived from a previous study [21]. The simulated annealing method in the parametric space for optimization was performed [22]. Because the smooth slopes of curves were important in the calculations, we used simulated responses for estimation. The rate constants (k01, k12, and k21) characterizing the C-peptide kinetics were adapted from a previous study [23]. All of the processes were carried out for each subject using the MATLAB system (The Mathworks Inc., Natick, MA, USA).
Calculations
Our goals of the calculations were two-fold. Our first goal was to compare the insulin sensitivity (SI) and β-cell function (i.e., basal, dynamic, static, and total responsivity indexes [Φb, Φd, Φs, and Φt]) between the NGT and T2DM groups. The second goal was to graphically present the dynamic, static, and total disposition indexes (DIs, DId, and DIt) of the subjects using the DI metric to show the distribution of insulin sensitivity and β-cell responsivity of the NGT and T2DM groups.
In the oral minimal model, Φb reflects the insulin secretion at the basal state. Φd and Φs, respectively, correspond to first and second phase of insulin secretion. Φt combines the effects of both Φd and Φs [14].
The indexes SI and Φb, Φd, Φs, and Φt of the subjects were calculated based on the derived parameters. In the glucose minimal model, SI and SG were calculated as follows [24]:
| (Equation 9) |
In the C-peptide minimal model, the β-cell responsivity indexes represent the capacity of the β-cells to release insulin. They were approximated as follows [14,25]:
| (Equation 10) |
| ϕd=KG (10–9) | (Equation 11) |
| ϕs=β (10–9 min–1) | (Equation 12) |
| (Equation 13) |
The DId, DIs, and DIt were calculated through multiplying Φd, Φs, and Φt, respectively, by SI.
The basal hepatic insulin extraction ratio (HEb) and postglucose challenge hepatic insulin extraction ratio (HEpost) were calculated. T0, 180 minutes in this study, is the time reaching the end of the tests [12].
| (Equation 14) |
| (Equation 15) |
Statistical analysis
To compare the variables between the NGT and T2DM groups, the Mann-Whitney test, chi-square test, Welch's test, and analysis of covariance for adjusting differences in age were performed. The oral minimal model indexes were log transformed for analysis and back transformed. The Spearman correlation analysis was also used. Prism 5.0 (GraphPad, San Diego, CA, USA), R 3.1.2 (The R Foundation, Vienna, Austria), and SPSS 19.0 (IBM Co., Armonk, NY, USA) software were used for statistical analysis. The significance level was set at 0.05 for the judgment of intergroup differences.
RESULTS
The clinical characteristics of the participants are presented in Table 1. The T2DM group was older than the NGT group (mean±standard deviation, 53.8±9.4 years vs. 39.8±13.5 years, P<0.019). The fasting glucose levels (146.2±27.6 mg/dL vs. 92.0±4.5 mg/dL, P<0.001) and peak glucose levels during the OGTT (337.0±49.5 mg/dL vs. 175.9±17.1 mg/dL, P<0.001) were higher in the T2DM group than the NGT group. The T2DM group had a longer delay in reaching the peak glucose levels than the NGT group (93.6±18.9 minutes vs. 49.0±13.5 minutes, P<0.001). The body weight and body mass indexes were not significantly different between the NGT and T2DM groups.
Table 1. Clinical characteristics of the subjects.
| Characteristic | NGT (n=10) | T2DM (n=14) | P value |
|---|---|---|---|
| Sex, male/female | 8/2 | 9/5 | 0.653 |
| Age, yr | 39.8±13.5 | 53.8±9.4 | 0.019 |
| Body weight, kg | 66.6±15.0 | 67.6±14.4 | 0.898 |
| Body mass index, kg/m2 | 22.9±3.5 | 24.5±3.5 | 0.403 |
| Duration of diabetes mellitus, yr | NA | 4.7±2.4 | NA |
| Fasting plasma glucose, mg/dL | 92.0±4.5 | 146.2±27.6 | <0.001 |
| Peak plasma glucose, mg/dL | 175.9±17.1 | 337.0±49.5 | <0.001 |
| Time for peak glucose, min | 49.0±13.5 | 93.6±18.9 | <0.001 |
| PCGR | 2.6±0.6 | 1.3±0.4 | <0.001 |
| Matsuda index | 8.8±3.3 | 5.5±2.8 | 0.002 |
| HOMA-IR | 1.2±1.1 | 2.3±1.3 | 0.002 |
Values are presented as mean±standard deviation. P values were calculated using the chi-square test or the Mann-Whitney test, where appropriate.
NGT, normal glucose tolerance; T2DM, type 2 diabetes mellitus; NA, not applicable; PCGR, postprandial C-peptide to glucose ratio; HOMA-IR, homeostasis model assessment of insulin resistance.
Other indexes of insulin secretion or insulin action, such as postprandial C-peptide to glucose ratio (PCGR) [26], Matsuda index [27], and homeostasis model assessment of insulin resistance (HOMA-IR) [28], were compared between the NGT and T2DM groups and are shown in Table 1. The PCGR and Matsuda index were higher in the NGT group than the T2DM group (2.649±0.642 vs. 1.254±0.423, P<0.001; 8.818±3.260 vs. 5.466±2.814, P=0.002, respectively). HOMA-IR was lower in the NGT group than the T2DM group (1.2±1.1 vs. 2.3±1.3, P=0.002).
Insulin sensitivity, β-cell responsivity indexes, and HE ratios
Insulin sensitivity and β-cell responsivity indexes were compared between the NGT and T2DM groups. As shown in Fig. 1, the NGT group had a higher SI than the T2DM group (20.0±8.2 [×10–5 dL/kg/min per pmol/L] vs. 13.3±11.8 [×10–5 dL/kg/min per pmol/L], P=0.024). The basal β-cell responsivity index (Φb) was not significantly different between the NGT and T2DM groups (2.8±1.2 [×10–9 min–1] vs. 2.9±1.2 [×10–9 min–1], respectively, P=0.578, age-adjusted P=0.972). The Φd, Φs, and Φt were higher in the NGT group than the T2DM group (Φd: 661.7±411.1 [×10–9] vs. 170.9±138.7 [×10–9], P<0.001, age-adjusted P=0.005; Φs: 33.5±9.4 [×10–9 min–1] vs. 13.9±6.5 [×10–9 min–1], P<0.001, age-adjusted P<0.001; Φt: 41.9±13.2 [×10–9 min–1] vs. 15.5±7.2 [×10–9 min–1], P<0.001, age-adjusted P<0.001, respectively). The HEb was not significantly different between the NGT and T2DM groups (55.20%±12.91% vs. 64.26%±9.27%, P=0.064). The HEpost appeared to be different between the NGT and T2DM groups (49.20%±20.79% vs. 66.99%±10.72%, P=0.028), which lost statistical significance after adjusting for age difference (P=0.141).
Fig. 1. The indexes for (A) insulin sensitivity (SI) and (B) basal, (C) dynamic, (D) static and (E) total β-cell responsivity (Φb, Φd, Φs, and Φt), (F) basal hepatic insulin extraction ratio (HEb), and (G) post-glucose challenge hepatic insulin extraction ratio (HEpost). The Mann-Whitney test was used to compare the indexes between the groups. NGT, normal glucose tolerance; T2DM, type 2 diabetes mellitus; NS, not significant.
Disposition indexes between NGT and T2DM groups
The T2DM group had significantly lower DId, DIs, and DIt than the NGT group (DId: 20.7±19.9 [×10–12 dL/kg/min per pmol/L] vs. 114.7±74.6 [×10–12 dL/kg/min per pmol/L], P=0.001, age-adjusted P<0.001; DIs: 1.6±1.0 [×10–12 dL/kg/min2 per pmol/L] vs. 6.4±2.8 [×10–12 dL/kg/min2 per pmol/L], P<0.001, age-adjusted P<0.001; DIt: 1.8±1.1 [×10–12 dL/kg/min2 per pmol/L] vs. 7.9±3.4 [×10–12 dL/kg/min2 per pmol/L], P<0.001, age-adjusted P<0.001, respectively) (Fig. 2). The hyperbolic relation is shown in the three DI metrics in Fig. 3. The hyperbolic line for the T2DM group was located in the leftward and downward region of the NGT group.
Fig. 2. The (A) dynamic, (B) static, and (C) total disposition indexes (DId, DIs, and DIt) in the patients with type 2 diabetes mellitus (T2DM) and individuals with normal glucose tolerance (NGT). The Mann-Whitney test was used to compare the indexes between the groups.
Fig. 3. Distribution of insulin sensitivity and secretion in the patients with type 2 diabetes (T2DM) and individuals with normal glucose tolerance (NGT). The hyperbolae for the (A) dynamic, (B) static, (C) and total disposition (DIs, DId, and DIt) indexes are shown for the NGT group (black line and open black circles) and the T2DM group (gray line and open gray circles) with a DI metric. Each circle or square represents a single subject. The subjects in each group presumably share the same disposition index, and a tendency toward the leftward and downward positioning in the T2DM patients can be observed. Φd, dynamic; Φs, static; Φt, total β-cell responsivity.
Correlation between other indexes of insulin secretion or insulin action and oral minimal model indexes
As shown in Fig. 4, the PCGR has significant correlation with the dynamic and static responsivity indexes (r=0.77, P<0.001 and r=0.89, P<0.001, respectively). The Matsuda index was significantly correlated with insulin sensitivity (r=0.51, P=0.011), whereas HOMA-IR did not show any significance (r=–0.21, P=0.105).
Fig. 4. Correlation analyses between the indexes obtained in the oral minimal model and other indexes of insulin secretion or insulin sensitivity (SI). Spearman correlation analysis was used. Correlations of (A) dynamic (Φd) and (B) static β-cell responsivity (Φs) with postprandial C-peptide to glucose ratio (PCGR) are shown. Correlations of insulin sensitivity (SI) with (C) Matsuda index and (D) homeostasis model assessment of insulin resistance (HOMA-IR) are shown.
DISCUSSION
In this Korean study, SI and β-cell responsivity indexes (Φd, Φs, and Φt) were lower in the patients with T2DM than in the individuals with NGT. Compared to the NGT group, insulin sensitivity was 33.9% lower, and the Φd, Φs, and Φt were 74.1%, 58.3%, and 63.3% lower, respectively, in the T2DM group. Our results were in line with those of previous studies, showing decreased insulin sensitivity and insulin secretion in Korean T2DM patients, which were conducted with the euglycemic hyperinsulinemic clamp method [29], the hyperglycemic clamp method [30], or the IVGTT-based minimal model [31]. Compared to other methods, the oral minimal model has advantages for the separate assessment of insulin sensitivity and dynamic nature of β-cell responsivity simultaneously from a single data set. There are many surrogate measures for insulin sensitivity and/or β-cell function, such as HOMA methods [28], quantitative insulin sensitivity check index (QUICKI) [32], and Matsuda index [27]. Fasting measures, such as HOMA-insulin resistance and QUICKI, mainly reflect hepatic insulin sensitivity rather than peripheral insulin sensitivity [33,34]. Because HOMA β-cell function is also derived from fasting data [28], it cannot describe the dynamics of postprandial insulin secretion. In contrast, the SI calculated by the oral minimal model represents not only hepatic but also peripheral insulin sensitivity [3,35,36]. Although the Matsuda index using the mean insulin and glucose responses during the OGTT correlates well with the insulin sensitivity measured by the euglycemic hyperinsulinemic clamp [27], this index is not matched for a measure of β-cell function that reflects the dynamic nature of postprandial insulin secretion. In this regard, the benefits of the oral minimal model are provision of comprehensive measures for insulin sensitivity, β-cell function, and hepatic extraction of insulin. In addition, the indexes obtained from the oral minimal model and other indexes of postchallenge insulin secretion and insulin sensitivity were well correlated.
The oral minimal model is simpler than the IVGTT-based minimal model [3,8], which requires much more frequent blood sampling and control for blood glucose concentrations. Therefore, it can be broadly applied for various clinical studies. First, the model can be used to assess characteristics of glucose metabolism in a large number of subjects. A previous study, which enrolled as many as 250 Japanese and Caucasian subjects, showed lower β-cell function and higher insulin sensitivity in the Japanese subjects than the Caucasian subjects [37]. Second, the oral minimal model can be used to assess the effect of antidiabetic drugs on insulin sensitivity and β-cell function, as shown elsewhere [38]. Taken together, the oral minimal model may reduce the burdens of effort in measuring physiologic parameters of glucose homeostasis in various forms of clinical research.
The oral minimal model has good expandability and can be readily modified in an engineering manner. To develop a further upgraded version of the oral minimal model, the incretin effect would be a candidate component to be incorporated in the model. If equations describing the incretin effect [39] were added to the oral minimal model, it could become a more physiologic model. Since a glucagon-adapted model has also been developed [40], it might be useful to assess the glycemic responses to specific antidiabetic drugs and to establish algorithms for the bihormonal artificial pancreas.
This study had some limitations. First, in this study, insulin and C-peptide were measured at 0, 15, and 30 minutes during the first 30 minutes, whereas other studies [14,25] included 0-, 10-, 20-, and 30-minute samples. Since the insulin response during the first 30 minutes is crucial to determine the dynamic β-cell responsivity index, more frequent measurements would support a more accurate estimation. Second, we did not directly validate the oral minimal model indexes with the values of the hyperglycemic clamp and the euglycemic hyperinsulinemic clamp studies, which are considered the gold standard methods for measuring insulin secretion and SI. Lastly, the subjects with prediabetes, such as impaired fasting glucose or impaired glucose tolerance, were not included in this study.
In this study, in accordance with the results of previously published studies using other physiologic methods in Koreans, the insulin sensitivity index, β-cell responsivity indexes, and disposition indexes obtained by the oral minimal model were generally lower in the T2DM group than the NGT group. Based on our results, the oral minimal model can also be applied to Koreans to evaluate insulin sensitivity and dynamics of insulin secretion using OGTT data.
ACKNOWLEDGMENTS
This work was supported by National Research Foundation of Korea (NRF) grants funded by the Korean Government (2015 M1A3A3A02012636, 2011-0009127, and 2010-0024462).
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Defronzo RA. Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009;58:773–795. doi: 10.2337/db09-9028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brubaker PL, Ohayon EL, D'Alessandro LM, Norwich KH. A mathematical model of the oral glucose tolerance test illustrating the effects of the incretins. Ann Biomed Eng. 2007;35:1286–1300. doi: 10.1007/s10439-007-9274-1. [DOI] [PubMed] [Google Scholar]
- 3.Cobelli C, Dalla Man C, Toffolo G, Basu R, Vella A, Rizza R. The oral minimal model method. Diabetes. 2014;63:1203–1213. doi: 10.2337/db13-1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cobelli C, Toffolo GM, Dalla Man C, Campioni M, Denti P, Caumo A, Butler P, Rizza R. Assessment of beta-cell function in humans, simultaneously with insulin sensitivity and hepatic extraction, from intravenous and oral glucose tests. Am J Physiol Endocrinol Metab. 2007;293:E1–E15. doi: 10.1152/ajpendo.00421.2006. [DOI] [PubMed] [Google Scholar]
- 5.Hovorka R, Canonico V, Chassin LJ, Haueter U, Massi-Benedetti M, Orsini Federici M, Pieber TR, Schaller HC, Schaupp L, Vering T, Wilinska ME. Nonlinear model predictive control of glucose concentration in subjects with type 1 diabetes. Physiol Meas. 2004;25:905–920. doi: 10.1088/0967-3334/25/4/010. [DOI] [PubMed] [Google Scholar]
- 6.Lee JC, Kim M, Choi KR, Oh TJ, Kim MY, Cho YM, Kim K, Kim HC, Kim S. In silico evaluation of glucose control protocols for critically ill patients. IEEE Trans Biomed Eng. 2012;59:54–57. doi: 10.1109/TBME.2011.2163310. [DOI] [PubMed] [Google Scholar]
- 7.James G, Witten D, Hastie T, Tibshirani R. An introduction to statistical learning: with applications in R. New York: Springer; 2013. p. 37. [Google Scholar]
- 8.Bergman RN, Ider YZ, Bowden CR, Cobelli C. Quantitative estimation of insulin sensitivity. Am J Physiol. 1979;236:E667–E677. doi: 10.1152/ajpendo.1979.236.6.E667. [DOI] [PubMed] [Google Scholar]
- 9.Staten MA, Kelley DE. Using oral challenge testing to assess insulin action and secretion with mathematical modeling. Diabetes. 2014;63:1188–1190. doi: 10.2337/db13-1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caumo A, Vicini P, Zachwieja JJ, Avogaro A, Yarasheski K, Bier DM, Cobelli C. Undermodeling affects minimal model indexes: insights from a two-compartment model. Am J Physiol. 1999;276(6 Pt 1):E1171–E1193. doi: 10.1152/ajpendo.1999.276.6.E1171. [DOI] [PubMed] [Google Scholar]
- 11.Toffolo G, De Grandi F, Cobelli C. Estimation of beta-cell sensitivity from intravenous glucose tolerance test C-peptide data. Knowledge of the kinetics avoids errors in modeling the secretion. Diabetes. 1995;44:845–854. doi: 10.2337/diab.44.7.845. [DOI] [PubMed] [Google Scholar]
- 12.Campioni M, Toffolo G, Basu R, Rizza RA, Cobelli C. Minimal model assessment of hepatic insulin extraction during an oral test from standard insulin kinetic parameters. Am J Physiol Endocrinol Metab. 2009;297:E941–E948. doi: 10.1152/ajpendo.90842.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basu R, Dalla Man C, Campioni M, Basu A, Klee G, Toffolo G, Cobelli C, Rizza RA. Effects of age and sex on postprandial glucose metabolism: differences in glucose turnover, insulin secretion, insulin action, and hepatic insulin extraction. Diabetes. 2006;55:2001–2014. doi: 10.2337/db05-1692. [DOI] [PubMed] [Google Scholar]
- 14.Breda E, Cavaghan MK, Toffolo G, Polonsky KS, Cobelli C. Oral glucose tolerance test minimal model indexes of beta-cell function and insulin sensitivity. Diabetes. 2001;50:150–158. doi: 10.2337/diabetes.50.1.150. [DOI] [PubMed] [Google Scholar]
- 15.Burattini R, Morettini M. Identification of an integrated mathematical model of standard oral glucose tolerance test for characterization of insulin potentiation in health. Comput Methods Programs Biomed. 2012;107:248–261. doi: 10.1016/j.cmpb.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Cho YM. Incretin physiology and pathophysiology from an Asian perspective. J Diabetes Investig. 2015;6:495–507. doi: 10.1111/jdi.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dalla Man C, Caumo A, Cobelli C. The oral glucose minimal model: estimation of insulin sensitivity from a meal test. IEEE Trans Biomed Eng. 2002;49:419–429. doi: 10.1109/10.995680. [DOI] [PubMed] [Google Scholar]
- 18.McDonald C, Dunaif A, Finegood DT. Minimal-model estimates of insulin sensitivity are insensitive to errors in glucose effectiveness. J Clin Endocrinol Metab. 2000;85:2504–2508. doi: 10.1210/jcem.85.7.6681. [DOI] [PubMed] [Google Scholar]
- 19.Caumo A, Bergman RN, Cobelli C. Insulin sensitivity from meal tolerance tests in normal subjects: a minimal model index. J Clin Endocrinol Metab. 2000;85:4396–4402. doi: 10.1210/jcem.85.11.6982. [DOI] [PubMed] [Google Scholar]
- 20.Steil GM, Hwu CM, Janowski R, Hariri F, Jinagouda S, Darwin C, Tadros S, Rebrin K, Saad MF. Evaluation of insulin sensitivity and beta-cell function indexes obtained from minimal model analysis of a meal tolerance test. Diabetes. 2004;53:1201–1207. doi: 10.2337/diabetes.53.5.1201. [DOI] [PubMed] [Google Scholar]
- 21.Kim M, Oh TJ, Lee JC, Choi K, Kim MY, Kim HC, Cho YM, Kim S. Simulation of oral glucose tolerance tests and the corresponding isoglycemic intravenous glucose infusion studies for calculation of the incretin effect. J Korean Med Sci. 2014;29:378–385. doi: 10.3346/jkms.2014.29.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Venkataraman P. Applied optimization with MATLAB programming. 2nd ed. Hoboken: John Wiley & Sons; 2009. p. 358. [Google Scholar]
- 23.Van Cauter E, Mestrez F, Sturis J, Polonsky KS. Estimation of insulin secretion rates from C-peptide levels. Comparison of individual and standard kinetic parameters for C-peptide clearance. Diabetes. 1992;41:368–377. doi: 10.2337/diab.41.3.368. [DOI] [PubMed] [Google Scholar]
- 24.Dalla Man C, Yarasheski KE, Caumo A, Robertson H, Toffolo G, Polonsky KS, Cobelli C. Insulin sensitivity by oral glucose minimal models: validation against clamp. Am J Physiol Endocrinol Metab. 2005;289:E954–E959. doi: 10.1152/ajpendo.00076.2005. [DOI] [PubMed] [Google Scholar]
- 25.Breda E, Toffolo G, Polonsky KS, Cobelli C. Insulin release in impaired glucose tolerance: oral minimal model predicts normal sensitivity to glucose but defective response times. Diabetes. 2002;51(Suppl 1):S227–S233. doi: 10.2337/diabetes.51.2007.s227. [DOI] [PubMed] [Google Scholar]
- 26.Lee EY, Hwang S, Lee SH, Lee YH, Choi AR, Lee Y, Lee BW, Kang ES, Ahn CW, Cha BS, Lee HC. Postprandial C-peptide to glucose ratio as a predictor of beta-cell function and its usefulness for staged management of type 2 diabetes. J Diabetes Investig. 2014;5:517–524. doi: 10.1111/jdi.12187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–1470. doi: 10.2337/diacare.22.9.1462. [DOI] [PubMed] [Google Scholar]
- 28.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 29.Chae BN, Lee SK, Hong EG, Chung YS, Lee KW, Kim HM. The role of insulin secretion and insulin resistance in the development of Korean type 2 diabetes mellitus. J Korean Diabetes Assoc. 1998;22:491–450. [Google Scholar]
- 30.Oh TJ, Park KS, Cho YM. Correlation of the incretin effect with first- and second-phase insulin secretions in Koreans with various glucose tolerance statuses. Clin Endocrinol (Oxf) 2015;83:59–66. doi: 10.1111/cen.12623. [DOI] [PubMed] [Google Scholar]
- 31.Song J, Oh JY, Sung YA, Pak YK, Park KS, Lee HK. Peripheral blood mitochondrial DNA content is related to insulin sensitivity in offspring of type 2 diabetic patients. Diabetes Care. 2001;24:865–869. doi: 10.2337/diacare.24.5.865. [DOI] [PubMed] [Google Scholar]
- 32.Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000;85:2402–2410. doi: 10.1210/jcem.85.7.6661. [DOI] [PubMed] [Google Scholar]
- 33.Otten J, Ahren B, Olsson T. Surrogate measures of insulin sensitivity vs the hyperinsulinaemic-euglycaemic clamp: a meta-analysis. Diabetologia. 2014;57:1781–1788. doi: 10.1007/s00125-014-3285-x. [DOI] [PubMed] [Google Scholar]
- 34.Reaven GM. What do we learn from measurements of HOMA-IR? Diabetologia. 2013;56:1867–1868. doi: 10.1007/s00125-013-2948-3. [DOI] [PubMed] [Google Scholar]
- 35.Dalla Man C, Caumo A, Basu R, Rizza R, Toffolo G, Cobelli C. Measurement of selective effect of insulin on glucose disposal from labeled glucose oral test minimal model. Am J Physiol Endocrinol Metab. 2005;289:E909–E914. doi: 10.1152/ajpendo.00299.2004. [DOI] [PubMed] [Google Scholar]
- 36.Man CD, Toffolo G, Basu R, Rizza RA, Cobelli C. Use of labeled oral minimal model to measure hepatic insulin sensitivity. Am J Physiol Endocrinol Metab. 2008;295:E1152–E1159. doi: 10.1152/ajpendo.00486.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moller JB, Dalla Man C, Overgaard RV, Ingwersen SH, Tornoe CW, Pedersen M, Tanaka H, Ohsugi M, Ueki K, Lynge J, Vasconcelos NM, Pedersen BK, Kadowaki T, Cobelli C. Ethnic differences in insulin sensitivity, beta-cell function, and hepatic extraction between Japanese and Caucasians: a minimal model analysis. J Clin Endocrinol Metab. 2014;99:4273–4280. doi: 10.1210/jc.2014-1724. [DOI] [PubMed] [Google Scholar]
- 38.Alba M, Ahren B, Inzucchi SE, Guan Y, Mallick M, Xu L, O'Neill EA, Williams-Herman DE, Kaufman KD, Goldstein BJ. Sitagliptin and pioglitazone provide complementary effects on postprandial glucose and pancreatic islet cell function. Diabetes Obes Metab. 2013;15:1101–1110. doi: 10.1111/dom.12145. [DOI] [PubMed] [Google Scholar]
- 39.Dalla Man C, Micheletto F, Sathananthan A, Rizza RA, Vella A, Cobelli C. A model of GLP-1 action on insulin secretion in nondiabetic subjects. Am J Physiol Endocrinol Metab. 2010;298:E1115–E1121. doi: 10.1152/ajpendo.00705.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Herrero P, Georgiou P, Oliver N, Reddy M, Johnston D, Toumazou C. A composite model of glucagon-glucose dynamics for in silico testing of bihormonal glucose controllers. J Diabetes Sci Technol. 2013;7:941–951. doi: 10.1177/193229681300700416. [DOI] [PMC free article] [PubMed] [Google Scholar]