Abstract
Background
Little is known about the association of dissatisfaction with body weight - a component of body image - with depression in individuals of different sex, age, and with different body mass index (BMI). Hence, the aim of our study was to evaluate the association of body weight dissatisfaction (BWD) with depression in different sub-groups.
Methods
We analyzed data of 15,975 individuals from the cross-sectional 2012 Swiss Health Survey. Participants were asked about their body weight satisfaction. The validated Patient Health Questionnaire (PHQ-9) was used to ascertain depression. Age was stratified into three groups (18–29, 30–59, and ≥60 years). The body mass index (BMI) was calculated from self-reported body height and weight and categorized into underweight (BMI <18.5 kg/m2), normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25.0–29.9 kg/m2), and obesity (BMI ≥30 kg/m2). The association between body weight dissatisfaction (BWD) and depression was assessed with logistic regression analyses and odds ratios (OR) with 95 % confidence intervals (CI) were computed.
Results
BWD was associated with depression in the overall group (OR 2.04, 95 % CI 1.66–2.50) as well as in men (OR 1.85, 95 % CI 1.34–2.56) and women (OR 2.25, 95 % CI 1.71–2.96) independent of BMI. The stratification by age groups showed significant associations of BWD with depression in young (OR 1.78, 95 % CI 1.16–2.74), middle-aged (OR 2.10, 95 % CI 1.61–2.74) and old individuals (OR 2.34, 95 % CI 1.30–4.23) independent of BMI. Stratification by BMI categories resulted in statistically significant positive associations of BWD and depression in underweight, normal weight, overweight and obese individuals.
Conclusion
BWD was associated with depression independent of BMI, sex and age.
Keywords: Depression, Body weight, Weight dissatisfaction, Switzerland
Background
Body image is a complex concept that embraces numerous components including feelings, attitudes, perceptions, and behaviors toward one’s body [1, 2]. In Western countries, research concentrated on the body’s appearance, especially on body shape and body weight [3], which is a component of body image [4]. Body image [5] and body weight dissatisfaction (BWD) [6] are very common in adolescents and adults. A German study showed that 48 % of 25–74 year old women and 33.2 % of men of the same age were affected by body weight dissatisfaction [6].
An increasing number of studies indicate the importance of a healthy body image, particularly in association with eating disorders [7], but also in the context of mental health and depression [8]. Depression is an important public health problem worldwide [9]. According to the World Health Organization, it accounts for 4.3 % of the global burden of disease and is an important cause of disability worldwide (11 % of all years lived with disability) [10]. Thus, it is of great importance to reveal risk and protective factors for this multifactorial disease.
Research on the association between various components of body image and depression by some authors has focused on adolescents [11, 12]. In a 4-year prospective study among female adolescents, body dissatisfaction, dietary restraint, and bulimic symptoms at study entry predicted the development of major depression among initially not depressed individuals [13]. Body dissatisfaction was significantly related to depression in the bivariate but not in the multivariate analysis. The evidence for an association between various components of body image and depression of female adolescents is based on a number of studies [14, 15], whereas the literature is rather limited for males [12].
In addition, much less is known about this association in adult males and females of different age groups [8, 16, 17]. Not all sub-groups of a population may have the same psychological functioning [11, 18]. Furthermore, the association between body image and BWD and depression may not only depend on sex and age, but also on one’s own body weight [19].
Obese individuals are frequently exposed to stigma, which can lead to poor psychological outcomes [20], such as lower self-esteem and depression [12]. A recent systematic review and meta-analysis revealed a bi-directional relationship between depression and obesity among adult men and women [21]. In the present study, we aimed to evaluate the association of BWD with depression overall, in men and women, as well as in young, middle-aged and old individuals independent of body weight. We used data of the 2012 Swiss Health Survey, a population-based representative sample of the adult population living in Switzerland.
Methods
Participants and data
We used data from the Swiss Health Survey (SHS) 2012, which was conducted by the Swiss Federal Statistical Office (SFSO) (Legal basis: Ordinance of the Conduct of Federal Statistical Surveys of 20 June 1993). The SHS does not require formal approval by an ethics committee. It is a population-based cross-sectional study, aiming to collect information about health status, several lifestyle and demographic factors, and healthcare use over time. The SHS was carried out every 5 years since 1992. Participants were selected based on registries of inhabitants using a stratified random sampling technique. In the SHS 2012, a total of 21,597 individuals aged 15 years or older and living in a private household participated. This corresponds to a response rate of 54 %. Besides a computer-assisted telephone interview, a written questionnaire was provided (paper or online) upon approval from the participants (n = 18,357). The multistage probability sampling and the appropriate weighting factors provided by the SFSO ensures the representativeness of the Swiss population.
Data on depression was obtained from the written questionnaire and 16,980 individuals provided information on depression status. After excluding adolescents (<18 years; n = 16,349), pregnant women (n = 130) as well as individuals with missing information on body mass index (BMI) (n = 90) and on body weight satisfaction (n = 20) our sample consisted of 16,109 individuals. In a further step, all individuals with missing information on confounders were excluded, resulting in a final sample of 15,975 individuals.
Measurements
BWD was assessed by one question in the telephone interview asking if one is satisfied with his/her body weight. Answers were categorized into “absolutely satisfied”, “rather satisfied”, “rather unsatisfied”, and “absolutely unsatisfied”. We then dichotomized these answers into “satisfied” and “unsatisfied” with body weight.
Depression status was considered as the outcome of our analysis. In the 2012 SHS, depression was assessed in the written questionnaire with the Patient Health Questionnaire (PHQ-9). This short screening questionnaire is a valid tool to assess depression by scoring on each of the 9 DSM-IV criteria for major depressive episodes and is broadly used in both practice and research [22, 23]. From a possible total score of 27 the cut-off point of ≥ 10 has shown a sensitivity of 88 % and a specificity of 88 % for the diagnosis of current major depression [22, 23]. Thus, we dichotomized a participant's PHQ-9 score into < 10 (no depression) and ≥ 10 (depression).
Potential confounders in our analyses were self-reported weight and height. BMI was calculated as weight in kg divided by squared height in meter and was categorized into underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25.0–29.9 kg/m2), and obesity (BMI ≥ 30 kg/m2). Additional self-reported data of the participants were obtained on sex, age, area of residence (urban, rural), nationality (Swiss, non-Swiss), educational level (low [compulsory education or less] vs. middle [secondary education] vs. high [tertiary education]), marital status (married/registered partnership vs. single, divorced/dissolved, separated, widowed), smoking status (never, former, current), chronic alcohol consumption associated with health (women ≥20 g, men ≥40 g ethanol daily vs. less), physical activity (≥150 min per week vs. less) [24], paying attention to diet (yes vs. no), and self-perceived health status (fair, poor, very poor vs. very good, good) was assessed.
Statistical analyses
Analyses were conducted with the Stata statistical software version 13.1 (College Station, TX) and weighted with weighting factors according the Swiss general population. The weights are based on the 2012 Swiss population with respect to sex, age, geographic region and nationality (Swiss/non-Swiss); any differences caused by stratification or non-participation were mathematically corrected. For descriptive statistics, we present means and percentages. Logistic regression analyses examined the associations of BWD with depression (yes/no), and odds ratios (OR) with the corresponding 95 % confidence intervals (CI) were calculated. We computed 4 models successively: 1) unadjusted, 2) adjusted for age and sex, 3) adjusted for confounders chosen a priori, due to the known literature or the expected association with both, BWD and depression, except for BMI, and 4) adjusted for all the covariates in model 3 plus BMI. We used the Wald-test - including the interaction term of BWD with age, sex or BMI - to examine whether age, sex and BMI modulated the association of BWD with depression. P < 0.05 was considered to be statistically significant.
Results
Table 1 shows the selected characteristics of the weighted study population (mean age 47.7 years). Nearly one third (31.3 %) were overweight and 10 % were obese. Normal weight was reported by 56.0 % of individuals and underweight by 3 %. Most participants lived in urban areas (73.4 %), were Swiss (80.8 %), and had a middle educational level (56.5 %). More than half of the participants (53.8 %) were married or lived in a registered partnership. Current smoking was stated by 27.7 % of the study participants and chronic hazardous alcohol consumption by 4.8 %. Not reaching the recommendations for physical activity was reported by approximately one fourth (25.8 %), and not paying attention to diet by 29.8 % of the participants. Self-perceived health was considered as fair, poor or very poor by 14.2 % of the participating individuals. Overall, 6 % of the study participants were above the cut-off point of the PHQ-9, indicating a current major depressive disorder.
Table 1.
Characteristics of the study sample of the 2012 Swiss Health Surveya
| Total | ||
|---|---|---|
| Total, n | 15,975 | |
| Age, mean (SE) | 47.7 (0.18) | |
| Sex | Males | 50.2 |
| Females | 49.8 | |
| Body mass index (BMI) | Underweight (BMI < 18.5 kg/m2) | 3.0 |
| Normal weight (BMI ≥ 18.5 to < 25.0 kg/m2) | 56.0 | |
| Overweight (BMI ≥ 25 to < 30.0 kg/m2) | 31.3 | |
| Obesity (BMI ≥ 30 kg/m2) | 9.7 | |
| Area of residence | Urban | 73.4 |
| Rural | 26.6 | |
| Nationality | Swiss | 80.8 |
| Foreign | 19.2 | |
| Educational level | High | 33.3 |
| Middle | 56.5 | |
| Low | 10.2 | |
| Marital status | Married/registered partnership | 53.8 |
| Single, divorced/dissolved partnership, separated, widowed | 46.2 | |
| Smoking status | Never smokers | 49.3 |
| Ex-smoker | 23.0 | |
| Current smokers | 27.7 | |
| Chronic alcohol consumptionb | No | 95.2 |
| Yes | 4.8 | |
| Physical activity | ≥150 min. per week | 74.2 |
| <150 min. per week | 25.8 | |
| Pay attention to diet | Yes | 70.2 |
| No | 29.8 | |
| Self-perceived health | Good, very good | 85.8 |
| Fair, poor, very poor | 14.2 | |
| Body weight satisfaction | Absolutely satisfied | 32.5 |
| Partly satisfied | 43.6 | |
| Rather unsatisfied | 19.1 | |
| Absolutely unsatisfied | 4.9 | |
| Depression | No | 94.0 |
| Yes | 6.0 |
aWeighted according to the Swiss general population
bEthanol ≥ 20 g/day for women, ≥ 40 g/day for men vs. less
Barely one third (32.5 %) of the study participants were absolutely satisfied with their body weight, 43.6 % partly, 19.1 % rather unsatisfied and 4.9 % absolutely unsatisfied. As Fig. 1 shows, women across all age groups were more often unsatisfied with their body weight than men. In males and females, the highest peaks of BWD were reached in 35–65 years old.
Fig. 1.
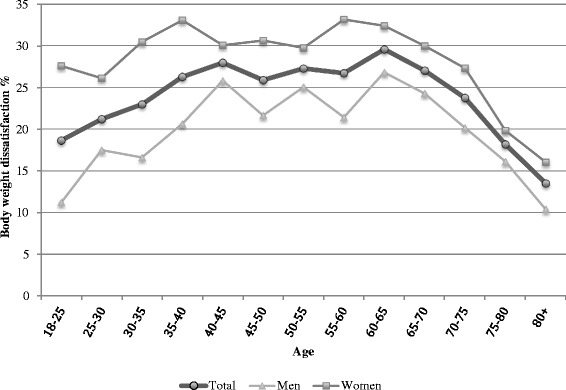
Prevalence of body weight dissatisfaction; 2012 Swiss Health Survey
As shown in Fig. 2, BWD was associated with depression (men and women combined OR 2.04, 95 % CI 1.66–2.50; multivariable adjusted). Table 2 presents similar results when looking at the association by sex (OR 1.85, 95 % CI 1.34–2.56 for men, OR 2.25, 95 % CI 1.71–2.96 for women, respectively), independent of the individual’s reported BMI. But results did not differ between men and women (P-interaction = 0.13).
Fig. 2.
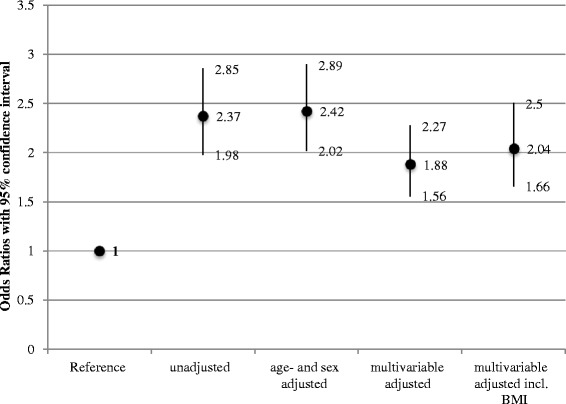
Associations between body weight dissatisfaction and depression assessed with logistic regression analyses and adjusted for different confounders; 2012 Swiss Health Survey. Multivariable adjustment included the variables area of residence, nationality, educational level, smoking status, physical activity, marital status, alcohol consumption, attention to diet, self-reported health, age (if appropriate), sex (if appropriate), and body mass index (if appropriate)
Table 2.
Association between body weight dissatisfaction and depression stratified by sex, age and body mass index; 2012 Swiss Health Surveya
| No depression (ref.) | Unadjusted | Age adjusted | Multivariable adjustedb | Multivariable adjustedb incl. BMI | |||||
|---|---|---|---|---|---|---|---|---|---|
| Body weight dissatisfaction | OR | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI |
| Men | 1 | 1.89 | [1.41,2.54] | 2.05 | [1.54,2.74] | 1.60 | [1.18,2.18] | 1.85 | [1.34,2.56] |
| Women | 1 | 2.76 | [2.21,3.45] | 2.77 | [2.21,3.47] | 2.16 | [1.72,2.72] | 2.25 | [1.71,2.96] |
| p-Interactionc | 0.01 | 0.09 | 0.18 | 0.13 | |||||
| Sex adjusted | |||||||||
| ≥18 to < 30 years | 1 | 1.91 | [1.28,2.86] | 1.88 | [1.27,2.79] | 1.53 | [1.02,2.30] | 1.78 | [1.16,2.74] |
| ≥30 to < 60 years | 1 | 2.77 | [2.22,3.45] | 2.74 | [2.20,3.41] | 2.05 | [1.62,2.59] | 2.10 | [1.61,2.74] |
| ≥60 years | 1 | 2.63 | [1.72,4.02] | 2.64 | [1.71,4.08] | 2.04 | [1.29,3.23] | 2.34 | [1.30,4.23] |
| p-Interaction | <0.01 | 0.01 | 0.07 | 0.08 | |||||
| Age and sex adjusted | |||||||||
| Underweight (BMI < 18.5 kg/m2) | 1 | 5.19 | [2.25,11.95] | 5.17 | [2.14,12.50] | 5.20 | [1.77,15.26] | ||
| Normal weight (BMI ≥ 18.5 to < 25.0 kg/m2) | 1 | 2.52 | [1.87,3.41] | 2.43 | [1.81,3.28] | 1.89 | [1.39,2.59] | ||
| Overweight (BMI ≥ 25 to < 30.0 kg/m2) | 1 | 2.80 | [2.02,3.89] | 2.46 | [1.77,3.42] | 2.00 | [1.41,2.83] | ||
| Obesity (BMI ≥ 30 kg/m2) | 1 | 2.53 | [1.41,4.54] | 2.19 | [1.20,3.98] | 1.97 | [1.10,3.51] | ||
| p-Interaction | 0.48 | 0.49 | 0.97 | ||||||
aWeighted according to the Swiss general population
bAdjusted for area of residence, nationality, educational level, smoking status, physical activity, marital status, alcohol consumption, attention to diet, self-reported health, age (if appropriate), sex (if appropriate), and body mass index (if appropriate)
cInteraction term: cross-product of sex, age-groups or weight groups, respectively, with body weight satisfaction
Stratifying by age groups showed significant associations of BWD with depression in young (OR 1.78, 95 % CI 1.16–2.74), middle-aged (OR 2.1, 95 % CI 1.61–2.74) and old individuals (OR 2.34, 95 % CI 1.30–4.23) also independent of BMI. Statistical significance for modification by age groups was not observed (P-interaction = 0.08).
By stratifying for BMI category, we found statistically significant positive associations of BWD and depression in underweight (OR 5.2, 95 % CI 1.77–15.26), normal weight (OR 1.89, 95 % CI 1.39–2.59), overweight (OR 2.0, 95 % CI 1.41–2.83), and obese individuals (OR 1.97, 95 % CI 1.10–3.51). We did not observe any statistically significant effect modification by BMI categories (P-interaction = 0.97).
Discussion
Based on data of the 2012 Swiss Health Survey, the present analyses revealed positive associations between BWD and depression independent of sex, age and BMI. To our knowledge, this is the first time these associations are studied in Switzerland.
Depression is the most common psychiatric disease in Switzerland. In the present study, 6 % were affected by a major depressive disorder according to the PHQ-9. Our estimate is in line with the estimated prevalence of 6.9 % in the European Union [25].
BWD has impact on nearly one fourth of the population living in Switzerland. The highest peaks were observed in middle-aged, 35–60 year olds. This proportion is a lot lower than the one found in a cross-sectional population-based German study [6], in which body weight dissatisfaction was reported by 40 % of the 25–74 year old men and women. However, body weight dissatisfaction was not assessed in the same way as in the SHS, which may have resulted in the observed difference.
The observed association between BWD and depression in the present study is in accordance with findings from surveys conducted mainly in adolescents and looking at the associations of various components of body image with depression [2, 19, 26–29]. In a U.S. study [2] on 2,139 adolescent males who were followed into adulthood, boys who had an average weight and perceived themselves as overweight or very underweight stated significantly more depressive symptoms than boys without body weight distortions. This result did not change over the 13-year follow-up period. In another longitudinal study among US adolescents body dissatisfaction was a predictor of depression for females but not for males [28]. In a cross-sectional study among Portuguese adolescents [29] on the other hand, body dissatisfaction contributed to depressive symptoms, without gender differences.
But in general women tend to internalize a thin appearance ideal [30], whereas the ideal male body is one of lean muscularity [2, 31]. Thus, our question on body weight satisfaction may not be precise enough to distinguish between obesity and muscularity. Since both obesity and muscularity dissatisfaction are of importance of the masculine body image upcoming research should assess both of them [2]. Although sex did not modulate the associations between BWD and depression, women tended to be more often dissatisfied than men.
In adults, the evidence is limited and not yet conclusive [5, 8, 16, 17, 32]. A cross-sectional analysis of the American Study of Women’s Health Across the Nation (SWAN) [8] observed that middle-aged women with body image dissatisfaction or who perceived themselves as “unattractive”, but not those with BWD, were more likely to report clinically significant levels of depressive symptoms. Also in a study conducted with 97 mainly female U.S. patients with binge eating disorders, body image disturbance was positively associated with depression [17]. In contrast, a prospective survey among Spanish university graduates, showed no association between body image disturbance and subsequent depression neither in adult men nor in adult women [16].
Others investigated whether body weight categories may modulate the association between BWD and depression. A variety of studies conducted with children or adolescents observed that perception of body weight may be more important than objectively measured weight in the relationship with mental health, e.g. with suicide ideation or attempts [33–36]. Furthermore, in a cross-sectional Chinese Study [19] adolescents who perceived themselves as overweight were more likely to experience depressive symptoms than those who perceived themselves as normal and/or underweight. In the same study, no significant association between depressive symptoms and actual measured weight status was observed. In a population-based cross-sectional American Study (NHANES) with over 13,000 participants, women who perceived themselves as underweight or overweight had an increased odd of depression compared with women who perceived themselves as about the right weight. This association was independent from measured weight. Among men, perceiving oneself as underweight but not being underweight (objectively measured) was associated with depression [32]. Accordingly, in our study, BWD remained to be associated with depression after adjustment for BMI. Thus, we confirmed the results of previous studies showing that perception of body weight might be a better predictor for depression than actual weight status.
Moreover, in our study, BWD was not only positively associated with depression in underweight, overweight and obese individuals but also in those with normal weight. Similarly, a recent cross-sectional study on Chinese adolescents looked at the moderating factors between the association of body dissatisfaction and depression. They observed significant associations in underweight, normal weight and overweight females, but in males associations were only observed in underweight and normal weight adolescents [11].
Potential mechanisms how body dissatisfaction is associated with mental health have been postulated previously [11, 19], focusing on the fact that body dissatisfaction stems from an inappropriate emphasis on the importance of thinness and other unachievable standards of beauty and, thus, may affect depression onset. This hypothesis is supported by the longitudinal study from Stice et al. [13] on female adolescents, in which body dissatisfaction has been identified as a predictor of depression. In this context, experiencing weight stigma predicts poor psychological outcomes including depression, similar to those outcomes who have been linked to higher BMI [37]. On the other hand, an association between body image and depression is also supported by the findings from neurobiological investigations [19]. Deficits in the hypothalamic pituitary-adrenal axis and serotonin system have been shown to be involved in mood disorders as well as in weight regulation. Furthermore, also brain areas which are involved in hedonic regulation may play a role for both body image and depression [38].
Our study has several strengths, including the large, nationally representative sample of individuals 18 years and older living in Switzerland, due to the use of weighting factors, which allows for the extrapolation of the results in relation to age, sex, region and nationality from the sample to the total population. Furthermore, the survey data allowed for adjusting for a number of important covariates associated with BWD and depression, although we were not able to take all potential confounders into consideration, such as family history of depression, medication, and also residual confounding might have occurred. A further strength was that depression was defined using a validated instrument with DSM-IV based criteria. However, our analysis was based on a cross-sectional study, and therefore we cannot exclude reverse causation, i.e. depression may also lead to BWD, which is a major limitation. Nevertheless, as these associations have not been examined yet for Switzerland, it is worthwhile to start with this population-based cross-sectional approach, but longitudinal studies are needed to examine the temporal relationship between body image and depression. Because institutionalized individuals were excluded from the sampling procedure, excluding most probably cases with severe depression, thus the prevalence of depression is possibly underestimated. The fact, that BWD, depression, body weight, height, and potential confounders were based solely on self-report may have biased the results. Finally, it should be noted that although BWD and body image dissatisfaction are related constructs, they are not redundant. The various aspects of body image and depression discussed in the present literature have therefore to be taken into consideration.
Conclusions
BWD was observed to be widespread and affected nearly one fourth of the population living in Switzerland. In this representative sample, BWD was associated with depression. The association was independent of age, sex, and BMI, i.e. present in individuals with normal body weight and in all age groups. Our results need to be confirmed in longitudinal studies. Presumed that causality can be provided in future longitudinal studies, programs that aim to reduce depression by diminishing body (weight) dissatisfaction should refer to all weight groups.
Acknowledgment
The authors thank the Swiss Federal Office of Statistics for permission to use the data of the 2012 Swiss Health Survey.
Funding
There was no funding for the research reported in the present article.
Availability of data and materials
Individual data of the Swiss Health Survey are property of the Swiss Federal Statistical Office (SFSO) and may only be made available by SFSO. Requests for access have to be submitted to Mr. Marco D'Angelo (head of division, MarcoDAngelo@bfs.admin.ch). For information contact sgb12@bfs.admin.ch.
Authors’ contributions
AR and ME designed the study. AR performed the statistical analyses and AR and ME wrote the manuscript. All authors contributed to the interpretation of the data and edited the manuscript. ME supervised the study. All authors contributed to and have approved the final manuscript.
Competing interests
The authors declare that there are no financial or personal relationships with other people or organizations that could inappropriately influence the work reported or the conclusions, implications, or opinions stated.
Consent for publication
Individuals invited to participate received a brief description of the study and could decline to participate or withdraw at any time. Participants’ responses were treated confidentially and aggregated anonymous responses were utilized for analyses presented herein.
Ethics approval and consent to participate
The data collection and data storage for the Swiss Health Survey (Schweizerische Gesundheitsbefragung) does not require formal approval by an ethical committee. This data collection is specifically permitted under Swiss law (SR 431.012.1 and SR 431.112.1).
Abbreviations
- BMI
Body mass index
- BWD
Body weight dissatisfaction
- CI
Confidence interval
- OR
Odds ratio
- PHQ-9
Patient health questionnaire, SE, Standard error, SHS, Swiss Health Survey
- SFSO
Swiss Federal Statistical Office
Contributor Information
Aline Richard, Email: aline.richard@uzh.ch.
Sabine Rohrmann, Email: sabine.rohrmann@uzh.ch.
Tina Lohse, Email: tina.lohse@uzh.ch.
Monika Eichholzer, Email: monika.eichholzer@ifspm.uzh.ch.
References
- 1.Cash TF, Pruzinsky T. Body images: development, deviance, and change. New York: Guilford Press; 1990. [Google Scholar]
- 2.Blashill AJ, Wilhelm S. Body Image Distortions, Weight, and Depression in Adolescent Boys: Longitudinal Trajectories Into Adulthood. Psychol Men Masculin. 2014;15(4):445–451. doi: 10.1037/a0034618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tiggemann M. Body image across the adult life span: stability and change. Body Image. 2004;1(1):29–41. doi: 10.1016/S1740-1445(03)00002-0. [DOI] [PubMed] [Google Scholar]
- 4.Forrester-Knauss C, Zemp Stutz E. Gender differences in disordered eating and weight dissatisfaction in Swiss adults: which factors matter? BMC Public Health. 2012;12:809. doi: 10.1186/1471-2458-12-809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fallon EA, Harris BS, Johnson P. Prevalence of body dissatisfaction among a United States adult sample. Eat Behav. 2014;15(1):151–158. doi: 10.1016/j.eatbeh.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 6.von Lengerke T, Mielck A, Group KS. Body weight dissatisfaction by socioeconomic status among obese, preobese and normal weight women and men: results of the cross-sectional KORA Augsburg S4 population survey. BMC Public Health. 2012;12:342. doi: 10.1186/1471-2458-12-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stice E, Shaw HE. Role of body dissatisfaction in the onset and maintenance of eating pathology: a synthesis of research findings. J Psychosom Res. 2002;53(5):985–993. doi: 10.1016/S0022-3999(02)00488-9. [DOI] [PubMed] [Google Scholar]
- 8.Jackson KL, Janssen I, Appelhans BM, Kazlauskaite R, Karavolos K, Dugan SA, Avery EA, Shipp-Johnson KJ, Powell LH, Kravitz HM. Body image satisfaction and depression in midlife women: the Study of Women's Health Across the Nation (SWAN) Arch Womens Ment Health. 2014;17(3):177–187. doi: 10.1007/s00737-014-0416-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997;349(9064):1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 10.WHO. Mental Health action plan 2013–2020. Geneva: World Health Organization 2013; 2013.
- 11.Chen G, Guo GP, Gong JB, Xiao SY. The Association Between Body Dissatisfaction and Depression: An Examination of the Moderating Effects of Gender, Age, and Weight Status in a Sample of Chinese Adolescents. J Psychol Counc Sch. 2015;25(2):245–260. doi: 10.1017/jgc.2015.6. [DOI] [Google Scholar]
- 12.Ferreiro F, Seoane G, Senra C. Toward understanding the role of body dissatisfaction in the gender differences in depressive symptoms and disordered eating: a longitudinal study during adolescence. J Adolesc. 2014;37(1):73–84. doi: 10.1016/j.adolescence.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 13.Stice E, Hayward C, Cameron RP, Killen JD, Taylor CB. Body-image and eating disturbances predict onset of depression among female adolescents: a longitudinal study. J Abnorm Psychol. 2000;109(3):438–444. doi: 10.1037/0021-843X.109.3.438. [DOI] [PubMed] [Google Scholar]
- 14.Paxton SJ, Neumark-Sztainer D, Hannan PJ, Eisenberg ME. Body dissatisfaction prospectively predicts depressive mood and low self-esteem in adolescent girls and boys. J Clin Child Adolesc Psychol. 2006;35(4):539–549. doi: 10.1207/s15374424jccp3504_5. [DOI] [PubMed] [Google Scholar]
- 15.Ferreiro F, Seoane G, Senra C. Gender-related risk and protective factors for depressive symptoms and disordered eating in adolescence: a 4-year longitudinal study. J Youth Adolesc. 2012;41(5):607–622. doi: 10.1007/s10964-011-9718-7. [DOI] [PubMed] [Google Scholar]
- 16.Pimenta AM, Sanchez-Villegas A, Bes-Rastrollo M, Lopez CN, Martinez-Gonzalez MA. Relationship between body image disturbance and incidence of depression: the SUN prospective cohort. Bmc Public Health. 2009;9:1. [DOI] [PMC free article] [PubMed]
- 17.Masheb RM, Grilo CM. The nature of body image disturbance in patients with binge eating disorder. Int J Eat Disord. 2003;33(3):333–341. doi: 10.1002/eat.10139. [DOI] [PubMed] [Google Scholar]
- 18.Schulte SJ, Thomas J. Relationship between eating pathology, body dissatisfaction and depressive symptoms among male and female adolescents in the United Arab Emirates. Eat Behav. 2013;14(2):157–160. doi: 10.1016/j.eatbeh.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 19.Tang J, Yu Y, Du Y, Ma Y, Zhu H, Liu Z. Association between actual weight status, perceived weight and depressive, anxious symptoms in Chinese adolescents: a cross-sectional study. BMC Public Health. 2010;10:594. doi: 10.1186/1471-2458-10-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 21.Mannan M, Mamun A, Doi S, Clavarino A. Is there a bi-directional relationship between depression and obesity among adult men and women? Systematic review and bias-adjusted meta analysis. Asian J Psychiatr. 2016;21:51–66. doi: 10.1016/j.ajp.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 22.Kroenke CH, Bennett GG, Fuchs C, Giovannucci E, Kawachi I, Schernhammer E, Holmes MD, Kubzansky LD. Depressive symptoms and prospective incidence of colorectal cancer in women. Am J Epidemiol. 2005;162(9):839–848. doi: 10.1093/aje/kwi302. [DOI] [PubMed] [Google Scholar]
- 23.Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184(3):E191–196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.BASPO, BfS . Gesundheitswirksame Bewegung. Magglingen: BASPO. In.; 2013. [Google Scholar]
- 25.Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jonsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 26.Daniels J. Weight and weight concerns: are they associated with reported depressive symptoms in adolescents? Journal of Pediatric Health Care: Official Publication of National Association of Pediatric Nurse Associates & Practitioners. 2005;19(1):33–41. doi: 10.1016/j.pedhc.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Ting WH, Huang CY, Tu YK, Chien KL. Association between weight status and depressive symptoms in adolescents: role of weight perception, weight concern, and dietary restraint. Eur J Pediatr. 2012;171(8):1247–1255. doi: 10.1007/s00431-012-1753-1. [DOI] [PubMed] [Google Scholar]
- 28.Bearman SK, Stice E. Testing a gender additive model: the role of body image in adolescent depression. J Abnorm Child Psychol. 2008;36(8):1251–1263. doi: 10.1007/s10802-008-9248-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Almeida S, Severo M, Araujo J, Lopes C, Ramos E. Body image and depressive symptoms in 13-year-old adolescents. J Paediatr Child Health. 2012;48(10):E165–171. doi: 10.1111/j.1440-1754.2012.02576.x. [DOI] [PubMed] [Google Scholar]
- 30.Thompson JK, Stice E. Thin-ideal internalization: Mounting evidence for a new risk factor for body-image disturbance and eating pathology. Curr Dir Psychol Sci. 2001;10(5):181–183. doi: 10.1111/1467-8721.00144. [DOI] [Google Scholar]
- 31.McCreary DR, Saucier DM. Drive for muscularity, body comparison, and social physique anxiety in men and women. Body Image. 2009;6(1):24–30. doi: 10.1016/j.bodyim.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Gaskin JL, Pulver AJ, Branch K, Kabore A, James T, Zhang J. Perception or reality of body weight: which matters to the depressive symptoms. J Affect Disord. 2013;150(2):350–355. doi: 10.1016/j.jad.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 33.Armstrong B, Westen SC, Janicke DM. The role of overweight perception and depressive symptoms in child and adolescent unhealthy weight control behaviors: a mediation model. J Pediatr Psychol. 2014;39(3):340–348. doi: 10.1093/jpepsy/jst091. [DOI] [PubMed] [Google Scholar]
- 34.Gray WN, Crawford MJ, Follansbee-Junger K, Dumont-Driscoll MC, Janicke DM. Associations between actual and perceived weight and psychosocial functioning in children: the importance of child perceptions. Child Obes. 2012;8(2):147–154. doi: 10.1089/chi.2011.0033. [DOI] [PubMed] [Google Scholar]
- 35.Ali MM, Fang H, Rizzo JA. Body weight, self-perception and mental health outcomes among adolescents. J Ment Health Policy Econ. 2010;13(2):53–63. [PubMed] [Google Scholar]
- 36.Eaton DK, Lowry R, Brener ND, Galuska DA, Crosby AE. Associations of body mass index and perceived weight with suicide ideation and suicide attempts among US high school students. Arch Pediatr Adolesc Med. 2005;159(6):513–519. doi: 10.1001/archpedi.159.6.513. [DOI] [PubMed] [Google Scholar]
- 37.Stevens SD, Herbozo S, Morrell HE, Schaefer LM, Thompson JK. Adult and childhood weight influence body image and depression through weight stigmatization. J Health Psychol. 2016. 2016; January 28, Epub first. [DOI] [PubMed]
- 38.Hoebel BG, Leibowitz SF. Brain monoamines in the modulation of self-stimulation, feeding, and body weight. Res Publ Assoc Res Nerv Ment Dis. 1981;59:103–142. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Individual data of the Swiss Health Survey are property of the Swiss Federal Statistical Office (SFSO) and may only be made available by SFSO. Requests for access have to be submitted to Mr. Marco D'Angelo (head of division, MarcoDAngelo@bfs.admin.ch). For information contact sgb12@bfs.admin.ch.


