Abstract
Glutamine and N-carbamylglutamate can enhance growth performance and health in animals, but the underlying mechanisms are not yet elucidated. This study aimed to investigate the effect of glutamine and N-carbamylglutamate supplementation in rat metabolism. Thirty rats were fed a control, glutamine, or N-carbamylglutamate diet for four weeks. Urine samples were analyzed by nuclear magnetic resonance (NMR)-based metabolomics, specifically high-resolution 1H NMR metabolic profiling combined with multivariate data analysis. Glutamine significantly increased the urine levels of acetamide, acetate, citrulline, creatinine, and methymalonate, and decreased the urine levels of ethanol and formate (p < 0.05). Moreover, N-carbamylglutamate significantly increased the urine levels of creatinine, ethanol, indoxyl sulfate, lactate, methymalonate, acetoacetate, m-hydroxyphenylacetate, and sarcosine, and decreased the urine levels of acetamide, acetate, citrulline, creatine, glycine, hippurate, homogentisate, N-acetylglutamate, phenylacetyglycine, acetone, and p-hydroxyphenylacetate (p < 0.05). Results suggested that glutamine and N-carbamylglutamate could modify urinary metabolome related to nitrogen metabolism and gut microbiota metabolism. Moreover, N-carbamylglutamate could alter energy and lipid metabolism. These findings indicate that different arginine precursors may lead to differences in the biofluid profile in rats.
Keywords: glutamine, N-carbamylglutamate, metabolism, metabolomics, urine
1. Introduction
Glutamine, a conditionally essential amino acid under inflammatory and many other stress conditions in both humans and animals [1,2], can increase cellular adenosine triphosphate levels [3,4]. Approximately 70% of glutamine in the enteral diet is degraded by rat and pig small intestines during the first pass and becomes a primary fuel for the growth and renewal of intestinal cells [5,6]. Glutamine can also regulate intestinal gene expression [7], protect intestinal epithelial tight junctions, increase the absorption and utilization of nutrients and immune function in animal production worldwide [8,9], modulate intracellular protein turnover [10], prevent intestinal oxidative injury, and inhibit cell autophagy [11]. Glutamine can also increase mitochondrial function [12]. Thus, glutamine is an important regulator for maintaining intestinal barrier integrity and function. Moreover, glutamine can enhance growth performance of early-weaned piglets [7]. Furthermore, glutamine supplementation between 90 and 114 days of gestation ameliorates fetal growth restriction in gilts and decreases pre-weaning mortality of piglets [1]. Finally, glutamine can increase milk production by lactating sows and survival of suckling piglets [1].
N-carbamylglutamate, a metabolically-stable analogue of N-acetylglutamate that activates intestinal pyrroline-5-carboxylate synthase and carbamylphosphate synthase-1 (key enzymes in arginine synthesis in enterocytes), provides a novel, effective strategy to increase endogenous arginine provision and can treat hyperammonaemia [13,14,15]. N-carbamylglutamate has been reported as having no toxicity for animals or humans [16], and it has been shown to stimulate citrulline synthesis in enterocytes and increase plasma concentrations of arginine and somatotropin [13,17]. N-carbamylglutamate administration increases absolute rates of muscle protein synthesis and growth rate in sow-reared piglets and improves the litter size in animals [13,18]. Furthermore, dietary N-carbamylglutamate supplementation enhance intestinal growth, and improve intestinal function in weaned pigs [19]. However, the exact mechanisms by which glutamine and N-carbamylglutamate contribute to various health conditions remain unclear. Therefore, the health effects of glutamine and N-carbamylglutamate supplementation and knowledge of these mechanisms need to be elucidated.
Recent metabolomics studies revealed that glutamine supplementation can affect the plasma metabolome in pigs [20], and N-carbamylglutamate can alter biofluid metabolome of rats under oxidative stress conditions [21]. However, no information has focused on the response of animal or human urinary biological systems to glutamine supplementation. No studies are available on the response of animal or human biological systems to N-carbamylglutamate under normal condition. Moreover, there is no information about the difference of metabolic profiles between glutamine and N-carbamylglutamate in any mammalian in vivo system. Metabolomics provides a novel strategy to resolve the changes in metabolic endpoints of physiological regulatory processes of an organism after the administration of specific nutritional interventions. Metabolomics is potentially valuable to the study of glutamine and N-carbamylglutamate metabolism and the search for relationships between glutamine and N-carbamylglutamate supplementation and health and disease. This experiment aimed to examine the effects of glutamine and N-carbamylglutamate supplementation on the urinary compositions of rats using an explorative metabolomic approach through proton nuclear magnetic resonance (1H NMR) spectroscopy and chemometrics.
2. Materials and Methods
2.1. Animal Experiment and Sample Collection
The animal experiment was approved by the Animal Care and Use Committee of Sichuan Agricultural University. It was performed according to the Guide for the Care and Use of Laboratory Animals of the National Research Council. A total of 30 eight-week-old female Sprague–Dawley rats weighing 249 g to 277 g were placed in individual metabolic cages and allowed to acclimatize for two weeks. After this period, the rats were assigned randomly to three purified dietary groups, with 10 rats in each group, for 28 days. The rats were fed with a basal diet containing 0 (control), 1% glutamine (supplied by Beijing Jiakangyuan Technology Development Co., Ltd., Beijing, China), or 0.1% N-carbamylglutamate (supplied by Asia Pacific Xingmu Technology Co., Ltd., Beijing, China). Urine samples were collected in ice-cooled vessels, including 30 µL of sodium azide solution (1.0% w/v) from day 27 to day 28 of the treatment period (24 h). All urine samples were stored at −80 °C until NMR analysis was performed. Rats were allowed free access to food and drinking water. Temperatures between 22 °C and 25 °C, a cycle of 12 h light/12 h dark, and humidity ranging from 50% to 70% were maintained throughout the duration of the study. Clinical observations were conducted during the whole experimental period. The dosage selected for this study was based on the results of a previous experiment [7,17,19].
2.2. Sample Preparation and NMR Spectroscopy
Urine samples (550 µL) were mixed with 55 µL of phosphate buffer (1.5 M NaH2PO4/K2HPO4, pH 7.4, 100% v/v D2O) containing 0.1% NaN3 as bacterial growth inhibitor and 5.0 mM 2,2-dimethyl-2-silapentane-5-sulfonate-d6 (DSS) as chemical shift reference (δ0.00 ppm). The supernatant was transferred into 5 mm NMR tubes for the NMR test after vortex mixing and 10 min of centrifugation (4 °C) at 12,000 g.
The proton NMR spectra of the urine samples were recorded at 300 K on a Bruker Avance II 600 MHz spectrometer (600.13 MHz for 1H frequency; Bruker Biospin, Rheinstetten, Germany) with a broadband-observe probe. A standard water-suppressed 1D NMR spectrum was obtained from urine using the first increment of the gradient-selected NOESY pulse sequence (recycle delay–90°–t1–90°–tm–90°–acquire data) with recycle delay of 2 s, t1 of 3 µs, mixing time (tm) of 100 ms, and 90° pulse length of 13.70 µs. A total of 128 transients were collected into 49,178 data points using a spectral width of 9590 Hz and an acquisition time of 2.56 s. Metabolites were generally assigned by considering the chemical shifts, coupling constants, and relative intensities, as in previous reports [22,23,24], and additional 1H–1H correlation spectroscopy and 1H–1H total correlation spectroscopy were recorded for selected samples (data not shown).
2.3. NMR Spectroscopic Processes and Analysis
Prior to Fourier transformation, the free induction decays were multiplied by an exponential function with a line-broadening factor of 1 Hz. All 1H NMR spectra were manually corrected for phase and baseline distortions by Mestrenova 8.1.2 software (Mestrelab Research S.L., Santiago de Compostela, Spain). The urinary spectral region δ0.5 to δ9.5 was binned with an equal width of 0.005 ppm using Mestrenova 8.1.2 software (Mestrelab Research S.L., Santiago de Compostela, Spain). Urine chemical shifts were referenced to the peak of DSS at δ0.00. Chemical shifts for urinary citrate were manually corrected because its signals had large inter-sample variations. To obtain the endogenous metabolite changes induced by treatment, the regions in the urine spectra containing δ4.50 to δ5.30 for H2O, as well as δ5.5 to δ6.0 for urea, were excluded. To compensate for the differences in concentration between different samples, urine spectra was normalized to the total sum of all integral regions for each spectrum before pattern recognition analysis.
Multivariate data analysis was achieved on normalized NMR datasets with the software package SIMCA-P+ (version 11.0, Umetrics, Umeå, Sweden). Principal component analysis (PCA) of the 1H NMR spectral data was performed on the mean-centered data to visualize the general structure of each dataset and identify any abnormalities (based on the principles of Hotelling’s T2) within the dataset. Results were observed in the form of score plots, in which each point represented an individual sample, and loading plots, in which each coordinate represented one NMR spectral region. Projection to latent structure-discriminant analysis (PLS-DA) and orthogonal projection to latent structure-discriminant analysis (OPLS-DA) were applied to the analysis of 1H NMR spectral data scaled to unit variance as the X-matrix and the class information as the Y-matrix to uncover metabolic differences [24]. The quality of the model was evaluated by such model parameters as R2X, which indicates the total explained variation, and Q2, which represents the model predictability. The models were validated using two methods: a seven-fold cross-validation method and a permutation test [25,26]. In this study, appropriate correlation coefficients greater than the cutoff values (depending on the sample numbers of animals in each group) were considered to be statistically significant (p < 0.05). The coefficients were determined by Pearson’s product-moment correlation coefficient.
3. Results
3.1. 1H NMR Spectra of Urine Samples
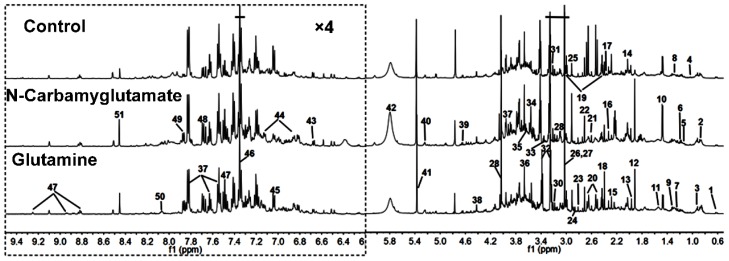
Figure 1 demonstrates typical 1H NMR spectra of the urine samples obtain from randomly selected rats in the glutamine, N-carbamylglutamate, and control groups. NMR signals were distributed to specific metabolites for 1H resonances (Table 1). Fifty-one metabolites were assigned to urine. The spectra of the urine samples included resonances from several amino acids and organic acids, as well as glucose, allantoin, and choline. Tricarboxylic acid cycle metabolites, such as succinate, α-ketoglutarate, and citrate, were also detected in the urine samples.
Figure 1.
Representative 1D 1H NMR spectra urine metabolites obtained from the control, N-carbamylglutamate, and glutamine groups. The region of δ6.2–9.5 was magnified four times compared with the corresponding region of δ0.5–6.2 for the purpose of clarity. Metabolite keys are given in Table 1.
Table 1.
Proton nuclear magnetic resonance (1H NMR) data of metabolites in rat urine.
| Keys | Metabolites | Moieties | δ 1H (ppm) and Multiplicity | Samples |
|---|---|---|---|---|
| 1 | Bile acids | CH3 | 0.64(m), 0.75(m) | U |
| 2 | α-Hydroxy-iso-valerate | δCH3, CH3 | 0.83(d), 0.97(d) | U |
| 3 | α-Hydroxybutyrate | CH3 | 0.89(t) | U |
| 4 | Propionate | CH3 | 1.06(t) | U |
| 5 | Isobutyrate | CH3 | 1.13(d) | U |
| 6 | Ethanol | CH3 | 1.19(t) | U |
| 7 | Methylmalonate | CH3, CH | 1.25(d), 3.75(m) | U |
| 8 | α-Hydroxy-n-valerate | CH3, γCH2 | 0.89(t), 1.31(m) | U |
| 9 | Lactate | αCH, βCH3 | 4.14(q), 1.33(d) | U |
| 10 | Alanine | αCH, βCH3 | 3.77(q), 1.47(d) | U |
| 11 | Citrulline | γCH2, βCH2 | 1.56(m), 1.82(m) | U |
| 12 | Acetate | CH3 | 1.92(s) | U |
| 13 | Acetamide | CH3 | 1.99(s) | U |
| 14 | N-Acetylglutamate | βCH2, γCH2, CH3 | 2.06(m), 1.87(m), 2.03(s) | U |
| 15 | Acetone | CH3 | 2.24(s) | U |
| 16 | Acetoacetate | CH3 | 2.28(s) | U |
| 17 | Pyruvate | CH3 | 2.33(s) | U |
| 18 | Succinate | CH2 | 2.40(s) | U |
| 19 | α-Ketoglutarate | βCH2, γCH2 | 2.45(t), 3.01(t) | U |
| 20 | Citrate | CH2 | 2.54(d), 2.68(d) | U |
| 21 | Methylamine | CH3 | 2.61(s) | U |
| 22 | Dimethylamine | CH3 | 2.71(s) | U |
| 23 | Methylguanidine | CH3 | 2.81(s) | U |
| 24 | Trimethylamine | CH3 | 2.88(s) | U |
| 25 | Dimethylglycine | CH3 | 2.93(s) | U |
| 26 | Creatine | CH3, CH2 | 3.04(s), 3.93(s) | U |
| 27 | Creatinine | CH3, CH2 | 3.04(s), 4.05(s) | U |
| 28 | Ornithine | CH2 | 3.06(t) | U |
| 29 | Ethanolamine | CH2 | 3.11(t) | U |
| 30 | Malonate | CH2 | 3.15(s) | U |
| 31 | Choline | OCH2, NCH2, N(CH3)3 | 4.07(t), 3.53(t), 3.21(s) | U |
| 32 | Taurine | –CH2-S, –CH2–NH2 | 3.27(t), 3.43(t) | U |
| 33 | TMAO a | CH3 | 3.27(s) | U |
| 34 | Glycine | CH2 | 3.57(s) | U |
| 35 | Sarcosine | CH2 | 3.6(s) | U |
| 36 | Phenylacetyglycine | 2,6–CH, 3,5–CH, 7–CH, 10–CH | 7.30(t), 7.36(m), 7.42(m), 3.67(s) | U |
| 37 | Hippurate | CH2, 3,5–CH, 4–CH, 2,6–CH | 3.97(d), 7.55(t), 7.63(t), 7.84(d) | U |
| 38 | N-Methylnicotinamide | CH3, 5–CH, 4–CH, 6–CH, CH2 | 4.42(s), 8.21(d), 8.87(d), 8.93(d), 9.24(s) | U |
| 39 | β-Glucose | 1–CH, 2–CH, 3–CH, 4–CH, 5–CH, 6–CH | 4.47(d), 3.25(dd), 3.49(t), 3.41(dd), 3.46(m), 3.73(dd), 3.90(dd) | U |
| 40 | α-Glucose | 1–CH, 2–CH, 3–CH, 4–CH, 5–CH, 6–CH | 5.24(d), 3.54(dd), 3.71(dd), 3.42(dd), 3.84(m), 3.78(m) | U |
| 41 | Allantoin | CH | 5.39(s) | U |
| 42 | Urea | NH2 | 5.82(s) | U |
| 43 | Homogentisate | 6–CH, 5–CH | 6.67(d), 6.82(d) | U |
| 44 | p-Hydroxyphenylacetate | 6–CH, 2–CH, 3,5–CH | 3.6(s), 6.85(d), 7.15(d) | U |
| 45 | m-Hydroxyphenylacetate | 6–CH, 4–CH, 3–CH | 6.92(m), 7.04(d), 7.26(t) | U |
| 46 | Indoxyl sulfate | 4–CH, 5–CH, 6–CH, 7–CH, CH | 7.51(m), 7.22(m), 7.28(m), 7.71(m), 7.37(s) | U |
| 47 | Nicotinate | 2,6–CH, 4–CH, 5–CH | 8.60(d), 8.25(d), 7.5(dd) | U |
| 48 | 4-Aminohippurate | CH2, CH | 7.6(d), 6.8(d), 3.9(d) | U |
| 49 | Benzoate | 2,6–CH, 3,5–CH, 4–CH | 7.87(d), 7.49(dd), 7.56(t) | U |
| 50 | Trigonelline | 2–CH, 4–CH, 6–CH, 5–CH, CH3 | 9.09(s), 8.85(m), 8.81(dd), 8.07(m), 4.44(s) | U |
| 51 | Formate | CH | 8.46(s) | U |
a TMAO, trimethylamine-N-oxide; s, singlet; d, doublet; t, triplet; q, quartet; dd, doublet of doublets; m, multiplet.
3.2. Multivariate Data Analysis of NMR Data
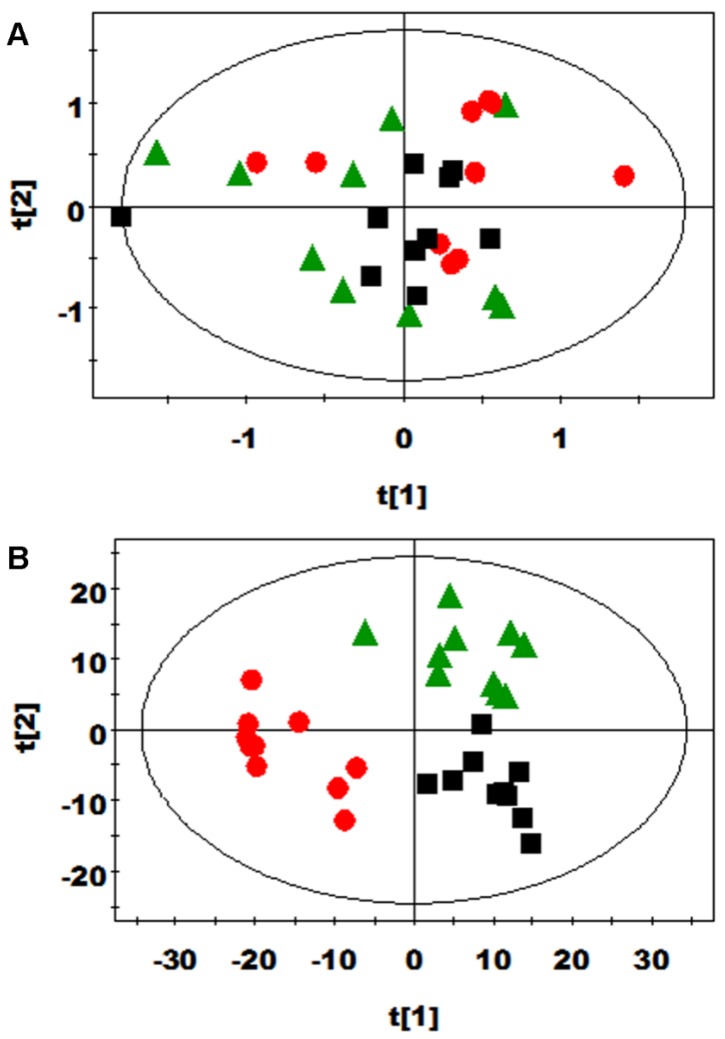
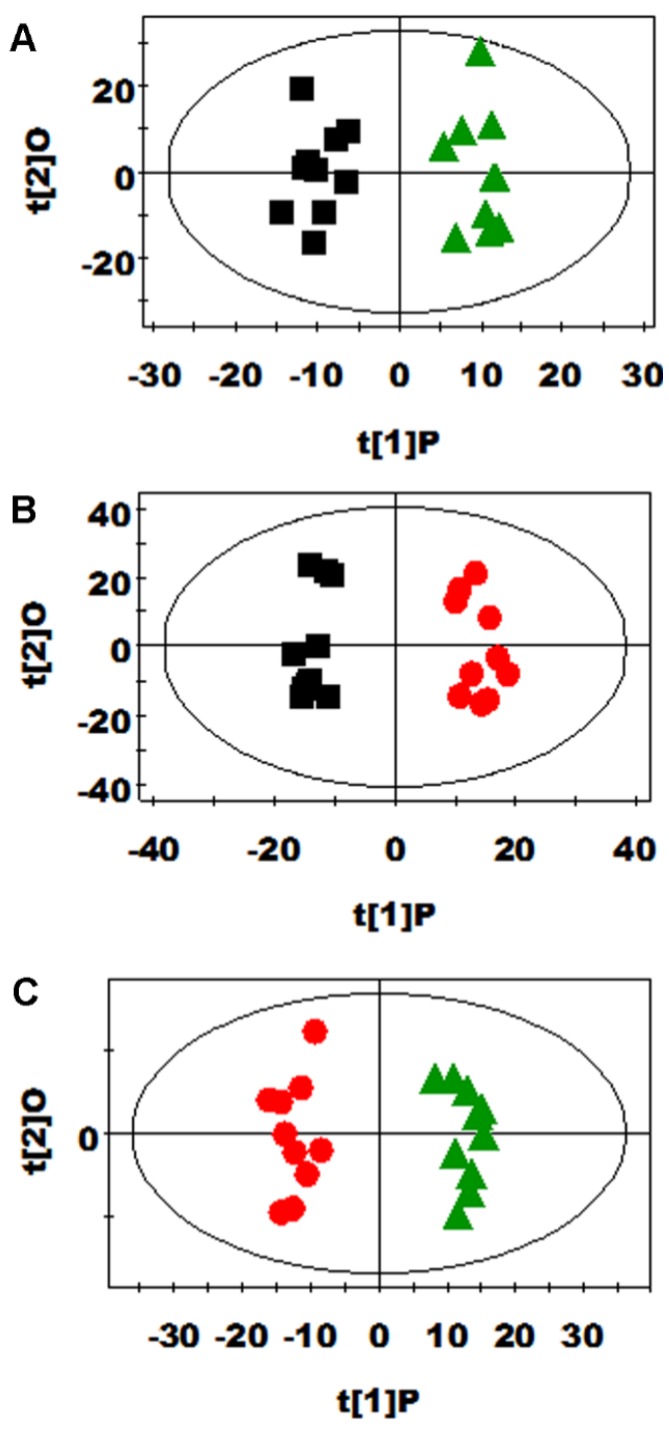
PCA and PLS-DA were initially carried out on the urinary spectral data (Figure 2). Two principal components were calculated for the treatment groups, with 19.7% and 17.6% of the variables being explained by PC1 and PC2, respectively. PCA results (Figure 2A) showed that the separations in rats from the glutamine, N-carbamylglutamate, and control groups were absent in their metabolic urinary profiles. PLS-DA was conducted on the urine spectra of the glutamine, N-carbamylglutamate, and control groups. The score plots (Figure 2B) highlighted three clusters corresponding to the three groups. The metabolic profiles of the glutamine, N-carbamylglutamate, and control groups were compared using OPLS-DA to further identify the important urine metabolic changes induced by amino acid supplementation. Multivariate data analysis showed that the urine levels of acetamide, acetate, citrulline, creatinine, and methymalonate were higher in the glutamine group than those in the control group (p < 0.05). By contrast, the urine levels of ethanol and formate were lower in the glutamine group than in the control group (p < 0.05, Figure 3A and Table 2). The metabolic profile of the N-carbamylglutamate group was compared with that of the control group using OPLS-DA to observe the effect of N-carbamylglutamate supplementation. The urine levels of creatinine, ethanol, indoxyl sulfate, lactate, methymalonate, acetoacetate, m-hydroxyphenylacetate, and sarcosine were significantly higher in the N-carbamylglutamate group than in the control group (p < 0.05). By contrast, the urine levels of acetamide, acetate, citrulline, creatine, glycine, hippurate, homogentisate, N-acetylglutamate, phenylacetyglycine, acetone, and p-hydroxyphenylacetate were lower in the N-carbamylglutamate group than those in the control group (p < 0.05, Figure 3B and Figure 4 and Table 2). OPLS-DA was also carried out to determine the degree of influence of glutamine supplementation on metabolism compared with the N-carbamylglutamate group. The urine levels of acetamide, acetate, citrulline, creatine, hippurate, homogentisate, N-acetylglutamate, acetone, and p-hydroxyphenylacetate were significantly higher in the glutamine group than those in the N-carbamylglutamate group (p < 0.05). By contrast, the urine levels of ethanol, indoxyl sulfate, methymalonate, α-ketoglutarate, acetoacetate, m-hydroxyphenylacetate, sarcosine, pyruvate, and methylamine were lower those in the glutamine group than those in the N-carbamylglutamate group (p < 0.05, Figure 3C and Table 2).
Figure 2.
(A) PCA (R2X = 0. 545, Q2 = 0.06) and (B) PLS-DA score plots (R2X = 0.192, R2Y = 0.795, Q2 = 0.474) based on the 1H NMR spectra of the urine obtained from urinary metabolites from the control (black squares), glutamine (green triangles), and N-carbamylglutamate (red circles) groups.
Figure 3.
OPLS-DA score plots of urinary metabolites derived from the control (black squares), glutamine (green triangles), and N-carbamylglutamate (red circles) ((A), R2X = 0.202, Q2 = 0.486; (B), R2X = 0.307, Q2 = 0.773; (C), R2X = 0.292, Q2 = 0.780) groups.
Table 2.
Orthogonal projection to latent structure-discriminant analysis (OPLS-DA) coefficients derived from the NMR data of urine metabolites obtained from the (A) control, (B) glutamine, and (C) N-carbamylglutamate groups.
| Metabolite | B (vs. A) a | C (vs. A) a | B (vs. C) a |
|---|---|---|---|
| Acetamide (13) | 0.608 | −0.728 | 0.906 |
| Acetate (12) | 0.713 | −0.742 | 0.768 |
| Citrulline (11) | 0.758 | −0.962 | 0.966 |
| Creatine (26) | — | −0.790 | 0.783 |
| Creatinine (27) | 0.723 | 0.717 | — |
| Ethanol (6) | −0.630 | 0.692 | −0.631 |
| Formate (51) | −0.621 | — | — |
| Glycine (34) | — | −0.616 | — |
| Hippurate (37) | — | −0.914 | 0.906 |
| Homogentisate (43) | — | −0.810 | 0.834 |
| Indoxyl sulfate (46) | — | 0.786 | −0.786 |
| Lactate (9) | — | 0.653 | — |
| Methylmalonate (7) | 0.738 | 0.608 | −0.653 |
| N-Acetylglutamate (14) | — | −0.967 | 0.978 |
| Phenylacetyglycine (36) | — | −0.634 | — |
| α-Hydroxy-n-valerate (8) | −0.684 | — | — |
| α-Ketoglutarate (19) | — | — | −0.623 |
| Acetoacetate (16) | — | 0.786 | −0.815 |
| Acetone (15) | — | −0.912 | 0.944 |
| m-Hydroxyphenylacetate (45) | — | 0.815 | −0.883 |
| p-Hydroxyphenylacetate (44) | — | −0.813 | 0.844 |
| Sarcosine (35) | — | 0.865 | −0.853 |
| α-Hydroxy-iso-valerate (2) | — | 0.607 | — |
| Pyruvate (4) | — | — | −0.608 |
| Methylamine (21) | — | — | −0.635 |
a Correlation coefficients: positive and negative signs indicate positive and negative correlations in the concentrations, respectively. The correlation coefficient of |r|> 0.602 was used as the cutoff value. ‘‘—’’ means the correlation coefficient |r| is less than 0.602. Analysis of relative integral from metabolites was given in Table S1 (Supplementary Material).
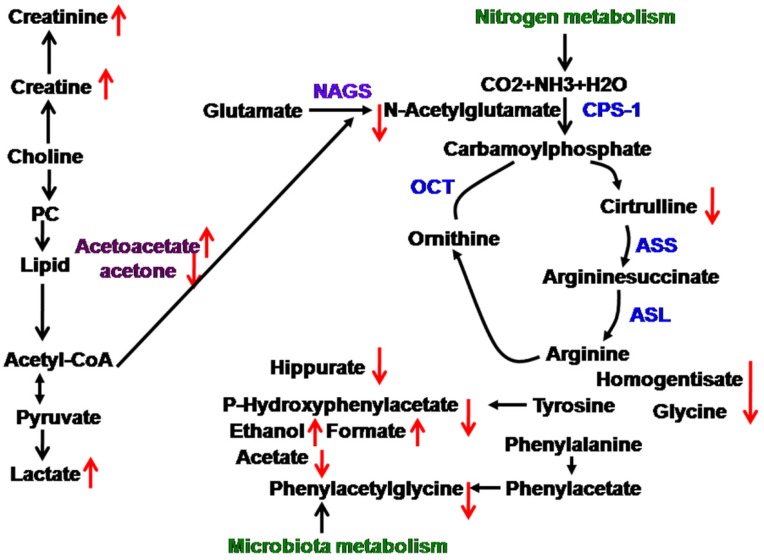
Figure 4.
N-carbamylglutamate-induced changes in the metabolic pathway,  upregulated,
upregulated,  downegulated; PC, phosphorylcholine; NAGS, N-acetylglutamate; CPS-1, carbamoylphosphate synthetase-1; ASS, argininosuccinate synthase; ASL, argininosuccinate lyase; OCT, ornithine carbamonyltransferase.
downegulated; PC, phosphorylcholine; NAGS, N-acetylglutamate; CPS-1, carbamoylphosphate synthetase-1; ASS, argininosuccinate synthase; ASL, argininosuccinate lyase; OCT, ornithine carbamonyltransferase.
4. Discussion
Both glutamine and N-carbamylglutamate are the important precursors of arginine synthesis, can regulate body metabolism, and increase growth performance in animals. However, the knowledge of their exact mechanisms of action remain largely understood. In this experiment, the daily bodyweight gain of glutamine and N-carbamylglutamate were higher than that of the contol group, however, the daily bodyweight gain between glutamine and N-carbamylglutamate was not significant in statistics (data not shown). Thus, glutamine and N-carbamylglutamate can enhance growth performance in rats. The growth performance is related with body metabolism modulated by glutamine and N-carbamylglutamate supplementation. The effects of nutrients in the metabolic profiles are more evident in the urine than in the plasma [27]. The collection of urine is noninvasive. Thus, a urinary metabolomic approach was used.
N-carbamylglutamate supplementation could affect lipid metabolism. Ketone body production (such as acetone, 3-hydroxybutyrate, and acetoacetate) provides fuel for vital organs (such as the heart and brain), thus increasing the chance of survival from metabolic problems. In the current study, acetoacetate significantly improved, but acetone decreased. This is not in agreement with the result of a previous study: N-carbamylglutamate supplementation can significantly increase plasma and urine acetone content, but exerted no effect on urine and plasma acetoacetate under oxidative stress [21]. The reason for this difference is unclear and needs further investigation in the future. Collectively, lipid metabolism was altered in rats. Moreover, N-carbamylglutamate supplementation could alter energy metabolism in rats. The N-carbamylglutamate group exhibited increased urinary lactate concentrations. Lactate is the end product of compounds associated with energy metabolism. The increase in lactate may imply carbohydrate and energy metabolism modification. This is not consistent with the result of our previous study [21]. The urinary creatine levels increased in the N-carbamylglutamate group compared with those in the control group. Creatine provides energy to muscles of vertebrates in the form of stored creatine phosphate. Creatine levels in the animals are synthesized de novo from the liver via the use of amino acids, such as arginine, glycine, and methionine. This is in agreement with the result of previous study: N-carbamylglutamate supplementation can increase arginine concentration [13]. While arginine is a substrate for the synthesis of creatine. This is also consistent with the result of increased creatinine levels. Enhanced creatinine levels were also observed to be associated with growth. Creatinine is an index of muscle mass, which also supported our findings. To our knowledge, this is the first report regarding the difference of acetoacetate and lactate metabolites for N-carbamylglutamate supplementation under normal condition. Collectively, N-carbamylglutamate supplementation could modify energy metabolism in rats.
Glutamine and N-carbamylglutamate supplementation can alter nitrogen metabolism. Glutamine and N-carbamylglutamate are known to have important functions in increasing protein synthesis, which results in the conversion of more amino acids into proteins. Glutamine increased urinary citrulline. Citrulline is an amino acid made from ornithine and carbamoyl phosphate in one of the central reactions in the urea cycle. Citrulline is derived from arginine as a byproduct of the reaction catalyzed by the nitric oxide synthase family. In this reaction, arginine is first oxidized into N-hydroxyl-arginine and then further oxidized to citrulline together with the release of nitric oxide [28]. This was in agreement with the result of a previous study [29]; thus, glutamine can increase plasma citrulline. This increase may be caused by increased intestinal citrulline [24]. N-carbamylglutamate decreased urinary N-acetylglutamate levels. This was in accordance with the result of a previous study [29]. However, N-carbamylglutamate decreased urinary citrulline level. This was different from the result of a previous study, which found that N-carbamylglutamate can increase plasma citrulline in piglets [30]. The reason for this difference is unclear and needs further investigation in the future. Urea has a crucial function in the metabolism of nitrogen-containing compounds. N-acetylglutamate is needed for the normal function of the urea cycle, and variations in N-acetylglutamate concentrations modify the urea production rate and other substrates for urea synthesis [31]. Furthermore, homogentisate is an intermediate of the metabolic breakdown of tyrosine and phenylalanine [32]. Sarcosine is the N-methyl derivative of glycine. In the present study, homogentisate and glycine concentrations significantly decreased, but sarcosine concentrations increased by N-carbamylglutamate supplementation. These were not in line with the results of a previous study [21]. The reason for this difference is unclear and needs further investigation in the future. To our knowledge, this is the first report regarding the difference of homogentisate and sarcosine metabolites for N-carbamylglutamate supplementation under normal condition. Therefore, glutamine and N-carbamylglutamate supplementation could alter nitrogen metabolism in rats.
Glutamine and N-carbamylglutamate can change gut microbiota functions. In this study, urinary formate, acetate, and ethanol concentrations were affected by glutamine supplementation. Urinary formate and ethanol concentrations were also affected by N-carbamylglutamate. Notably, urinary formate and ethanol are microbial metabolites of carbohydrates, which are likely produced in the lumen of the small and large intestines [33]. Changes in these metabolites may result from altered activity of intestinal microorganisms. Moreover, the urine level of microbiotic metabolites such as m-hydroxyphenylacetate significantly increased. This was not in accordance with the result of a previous study [21]. The possible reason is that oxidative stress may affect the microbiotic metabolism and show the difference of metabolites compared with non-oxidative stress condition, which demonstrates no change of m-hydroxyphenylacetate in oxidative stress condition and the increase of m-hydroxyphenylacetate in non-oxidative stress. Furthermore, results of this study also indicated that N-carbamylglutamate decreased the urinary excretion of hippurate, which is produced via both renal and hepatic syntheses of benzoic acid and glycine. This was consistent with the result of our previous study [21]. Hippurate is considered as the degradation product of flavonols acted upon by intestinal microorganisms [34]. As a result, a change in the excretion of this compound suggests a corresponding change in the functional metabolism of the microbiota. Variations in urinary hippurate concentration have also been associated with the changes in the distribution of intestinal microbial colonies [35]. Changes in gut microbial co-metabolites, such as phenylacetylglycine and p-hydroxyphenylacetate, with N-carbamylglutamate exposure, verified the association of the disturbance to gut microbiota. Through the action of gut microbiota, phenylacetate was transformed from phenylalanine through the action of gut microbiota, and phenylacetate was then conjugated with glycine to produce phenylacetylglycine [35]. p-Hydroxyphenylacetate is a metabolite of tyrosine via the action of enteric bacteria. These were not in line with the results of previous study [21]. The possible reason is that oxidative stress may affect the microbiotic metabolism and show the difference of metabolites compared with non-oxidative stress conditions. In the current study, glutamine supplementation significantly increased the urinary acetamide levels. However, N-carbamylglutamate decreased urinary acetamide. Acetamide exhibits anti-microbial, anti-inflammatory, anti-arthritic, and antibiotic functions [36,37]. Changes in these metabolites are attributed to the altered activity of intestinal microorganisms. Glutamine increased the concentrations of urinary acetate and acetamide, whereas N-carbamylglutamate decreased the concentrations of urinary acetate, acetamide, hippurate, phenylacetyglycine, and p-hydroxyphenylacetate. These findings were possibly due to the differences of arginine precursor sources. To our knowledge, this is the first report regarding the difference of formate, ethanol, m-hydroxyphenylacetate, p-hydroxyphenylacetate, hippurate, and acetamide metabolites for N-carbamylglutamate supplementation under normal condition. Mammalian metabolism is greatly affected by the complex gut microbiota [38]. The introduction of glutamine and N-carbamylglutamate into the mammalian system may displace baseline mammalian-to-microbial behavior, thereby disrupting microbial populations and eventually affecting metabolism.
5. Conclusions
Glutamine and N-carbamylglutamate can alter some common systemic metabolic processes, including nitrogen and gut microbiota metabolism. Moreover, N-carbamylglutamate can alter energy and lipid metabolism. These results indicate that different arginine precursor may cause differences in the biofluid profile in rats. This research contributes in defining the effects of metabolic modifiers to offer better nutritional support for growth and health. This study emphasized the potential metabolomic strategy in the evaluation of nutritional interventions in a mammalian system. To the best of our knowledge, this study is the first to systematically identify the distinct urinary metabolic profiles between glutamine and N-carbamylglutamate supplementation.
Acknowledgments
We wish to acknowledge all the study participants for their ongoing help. This work was supported in part by grants from the National Natural Science Foundation of China (Grant No.: 31301986) and Specific Research Supporting Program for Discipline Construction in Sichuan Agricultural University (to G. Liu).
Supplementary Materials
The following are available online at http://www.mdpi.com/2072-6643/8/8/478/s1, Table S1: Orthogonal projection to latent structure-discriminant analysis (OPLS-DA) coefficients derived from the NMR data of urine metabolites obtained from the (A) control, (B) glutamine, and (C) N-carbamylglutamate groups.
Author Contributions
Guangmang Liu conceived the study, designed the experiments, analyzed the data and wrote the manuscript; Wei Cao and Tingting Fang carried out the experiments; Gang Jia, Hua Zhao, Xiaoling Chen, Caimei Wu and Jing Wang contributed to sample collection. All authors read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Wu G., Bazer F.W., Johnson G.A., Knabe D.A., Burghardt R.C., Spencer T.E., Li X.L., Wang J.J. Triennial Growth Symposium: Importants roles for l-glutamine in swine nutrition and production. J. Anim. Sci. 2011;89:2017–2030. doi: 10.2527/jas.2010-3614. [DOI] [PubMed] [Google Scholar]
- 2.Wu G. Functional amino acids in nutrition and health. Amino Acids. 2013;45:407–411. doi: 10.1007/s00726-013-1500-6. [DOI] [PubMed] [Google Scholar]
- 3.Barnabé N., Butler M. The effect of glucose and glutamine on the intracellular nucleotide pool and oxygen uptake rate of a murine hybridoma. Cytotechnology. 2000;34:47–57. doi: 10.1023/A:1008154615643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahmad S., White C.W., Chang L.Y., Schneider B.K., Allen C.B. Glutamine protects mitochondrial structure and function in oxygen toxicity. Am. J. Physiol. Lung Cell Mol. Physiol. 2001;280:779–791. doi: 10.1152/ajplung.2001.280.4.L779. [DOI] [PubMed] [Google Scholar]
- 5.Wu G. Intestinal mucosal amino acid catabolism. J. Nutr. 1998;128:1249–1252. doi: 10.1093/jn/128.8.1249. [DOI] [PubMed] [Google Scholar]
- 6.Reeds P.J., Burrin D.G. Glutamine and the bowel. J. Nutr. 2001;131:2505S–2508S. doi: 10.1093/jn/131.9.2505S. [DOI] [PubMed] [Google Scholar]
- 7.Wang J., Chen L., Li P., Li X., Zhou H., Wang F., Li D., Yin Y., Wu G. Gene expression is altered in piglet small intestine by weaning and dietary glutamine supplementation. J. Nutr. 2008;138:1025–1032. doi: 10.1093/jn/138.6.1025. [DOI] [PubMed] [Google Scholar]
- 8.Ban K., Kozar R.A. Glutamine protects against apoptosis via downregulation of Sp3 in intestinal epithelial cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2010;299:G1344–G1353. doi: 10.1152/ajpgi.00334.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoo S.S., Field C.J., McBurney M.I. Glutamine supplementation maintains intramuscular glutamine concentrations and normalizes lymphocyte function in infected early weaned pigs. J. Nutr. 1997;127:2253–2259. doi: 10.1093/jn/127.11.2253. [DOI] [PubMed] [Google Scholar]
- 10.Xi P., Jiang Z., Dai Z., Li X., Yao K., Zheng C., Lin Y., Wang J., Wu G. Regulation of protein turnover by l-glutamine in porcine intestinal epithelial cells. J. Nutr. Biochem. 2012;23:1012–1017. doi: 10.1016/j.jnutbio.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 11.Zhu Y., Lin G., Dai Z., Zhou T., Li T., Yuan T., Wu Z., Wu G., Wang J. l-glutamine deprivation induces autophagy and alters the mTOR and MAPK signaling pathways in porcine intestinal epithelial cells. Amino Acids. 2015;47:2185–2197. doi: 10.1007/s00726-014-1785-0. [DOI] [PubMed] [Google Scholar]
- 12.Groening P., Huang Z., La Gamma E.F., Levy R.J. Glutamine restores myocardial cytochrome C oxidase activity and improves cardiac function during experimental sepsis. JPEN J. Parenter. Enter. Nutr. 2011;35:249–254. doi: 10.1177/0148607110383040. [DOI] [PubMed] [Google Scholar]
- 13.Wu G., Knabe D.A., Kim S.W. Arginine nutrition in neonatal pigs. J. Nutr. 2004;134:S2783–S2790. doi: 10.1093/jn/134.10.2783S. [DOI] [PubMed] [Google Scholar]
- 14.Cohen P.P., Grisolia S. The role of carbamyl-l-glutamic acid in the enzymatic synthesis of citrulline from ornithine. J. Biol. Chem. 1950;182:747–761. [Google Scholar]
- 15.Yap S., Leong H.Y., Abdul Aziz F., Hassim H., Sthaneshwar P., Teh S.H., Abdullah I.S., Ngu L.H., Mohamed Z. N-carbamylglutamate is an effective treatment for acute neonatal hyperammonaemia in a patient with methylmalonic aciduria. Neonatology. 2016;109:303–307. doi: 10.1159/000443630. [DOI] [PubMed] [Google Scholar]
- 16.Guffon N., Vianey-Saban C., Bourgeois J., Rabier D., Colombo J., Guibaud P. A new neonatal case of N-acetylglutamate synthase deficiency treated by carbamylglutamate. J. Inher. Metab. Dis. 1995;18:61–65. doi: 10.1007/BF00711374. [DOI] [PubMed] [Google Scholar]
- 17.Frank J.W., Escobar J., Nguyen H.V., Jobgen S.C., Jobgen W.S., Davis T.A., Wu G. Oral N-carbamylglutamate supplementation increases protein synthesis in skeletal muscle of piglets. J. Nutr. 2007;137:315–319. doi: 10.1093/jn/137.2.315. [DOI] [PubMed] [Google Scholar]
- 18.Zeng X., Huang Z., Mao X., Wang J., Wu G., Qiao S. N-carbamylglutamate enhances pregnancy outcome in rats through activation of the PI3K/PKB/mTOR signaling pathway. PLoS ONE. 2012;7:478. doi: 10.1371/journal.pone.0041192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu X., Ruan Z., Gao Y., Yin Y., Zhou X., Wang L., Geng M., Hou Y., Wu G. Dietary supplementation with l-arginine or N-carbamylglutamate enhances intestinal growth and heat shock protein-70 expression in weanling pigs fed a corn- and soybean meal-based diet. Amino Acids. 2010;39:831–839. doi: 10.1007/s00726-010-0538-y. [DOI] [PubMed] [Google Scholar]
- 20.Xiao Y.P., Wu T.X., Sun J.M., Yang L., Hong Q.H., Chen A.G., Yang C.M. Response to dietary l-glutamine supplementation in weaned piglets: A serum metabolomic comparison and hepatic metabolic regulation analysis. J. Anim. Sci. 2012;90:4421–4430. doi: 10.2527/jas.2012-5039. [DOI] [PubMed] [Google Scholar]
- 21.Liu G.M., Xiao L., Cao W., Fang T.T., Jia G., Chen X.L., Zhao H., Wu C.M., Wang J. Changes in the metabolome of rats after exposure to arginine and N-carbamylglutamate in combination with diquat a compound that causes oxidative stress assessed by 1H NMR spectroscopy. Food Funct. 2016;7:964–974. doi: 10.1039/C5FO01486G. [DOI] [PubMed] [Google Scholar]
- 22.Nicholson J.K., Foxall P.J.D., Spraul M., Farrant R.D., Lindon J.C. 750 MHz 1H and 1H-13C NMR spectroscopy of human blood plasma. Anal. Chem. 1995;67:793–811. doi: 10.1021/ac00101a004. [DOI] [PubMed] [Google Scholar]
- 23.Fan T.W.M. Metabolite profiling by one- and two-dimensional NMR analysis of complex mixtures. Prog. Nucl. Magn. Reson. Spectrosc. 1996;28:161–219. doi: 10.1016/0079-6565(96)90002-3. [DOI] [Google Scholar]
- 24.Wishart D.S., Jewison T., Guo A.C., Wilson M., Knox C., Liu Y., Djoumbou Y., Mandal R., Aziat F., Dong E., et al. HMDB 3.0-the human metabolome database in 2013. Nucleic Acids Res. 2013;41:D801–D807. doi: 10.1093/nar/gks1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cloarec O., Dumas M.E., Trygg J., Craig A., Barton R.H., Lindon J.C., Nicholson J.K., Holmes E. Evaluation of the orthogonal projection on latent structure model limitations caused by chemical shift variability and improved visualization of biomarker changes in 1H NMR spectroscopic metabonomic studies. Anal. Chem. 2005;77:517–526. doi: 10.1021/ac048803i. [DOI] [PubMed] [Google Scholar]
- 26.Lindgren F., Hansen B., Karcher W., SjÖstrÖm M., Eriksson L. Model validation by permutation tests: Applications to variable selection. J. Chemom. 1996;10:521–532. doi: 10.1002/(SICI)1099-128X(199609)10:5/6<521::AID-CEM448>3.0.CO;2-J. [DOI] [Google Scholar]
- 27.Liu G.M., Xiao L., Fang T.T., Cai Y.M., Jia G., Zhao H., Wang J., Chen X.L., Wu C.M. Pea fiber and wheat bran fiber show distinct metabolic profiles in rats as investigated by a 1H NMR-based metabollomic approach. PLoS ONE. 2014;9:478. doi: 10.1371/journal.pone.0115561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huynh N.N., Chin-Dusting J. Amino acids, arginase and nitric oxide in vascular health. Clin. Exp. Pharmacol. Physiol. 2006;33:1–8. doi: 10.1111/j.1440-1681.2006.04316.x. [DOI] [PubMed] [Google Scholar]
- 29.Ligthart-Melis G.C., Deutz N.E.P. Is glutamine still an important precursor of citrulline? Am. J. Physiol. Endocrinol. Metab. 2011;301:E264–E266. doi: 10.1152/ajpendo.00223.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang F., Zeng X., Yang F., Huang Z., Liu H., Ma X., Qiao S. Dietary N-carbamylglutamate supplementation boosts intestinal mucosal immunity in Escherichia coli challenged piglets. PLoS ONE. 2013;8:478. doi: 10.1371/journal.pone.0066280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meijer A.J., Verhoeven A.J. N-acetylglutamate and urea synthesis. Biochem. J. 1984;56:559–560. doi: 10.1042/bj2230559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arias-Barrau E., Olivera E.R., Luengo J.M., Fernández C., Galán B., García J.L., Díaz E., Miñambres B. The homogentisate pathway: A central catabolic pathway involved in the degradation of l-phenylalanine, l-tyrosine, and 3-hydroxyphenylacetate in Pseudomonas putida. J. Bacteriol. 2004;186:5062–5077. doi: 10.1128/JB.186.15.5062-5077.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tannock G.W. A special fondness for lactobacilli. Appl. Environ. Microbiol. 2004;70:3189–3194. doi: 10.1128/AEM.70.6.3189-3194.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rechner A.R., Kuhnle G., Hu H., Roedig-Penman A., van den Braak M.H., Moore K.P., Rice-Evans C.A. The metabolism of dietary polyphenols and the relevance to circulating levels of conjugated metabolites. Free Radic. Res. 2002;36:1229–1241. doi: 10.1080/246-1071576021000016472. [DOI] [PubMed] [Google Scholar]
- 35.Bohus E., Coen M., Keun H.C., Ebbels T.M.D., Beckonert O., Lindon J.C., Holmes E., Noszál B., Nicholson J.K. Temporal metabonomic modeling of l-arginine-induced exocrine pancreatitis. J. Proteome Res. 2008;7:4435–4445. doi: 10.1021/pr800407j. [DOI] [PubMed] [Google Scholar]
- 36.Jawed H., Shah S.U.A., Jamall S., Simjee S.U. N-(2-hydroxy phenyl) acetamide inhibits inflammation-related cytokines and ROS in adjuvant-induced arthritic (AIA) rats. Int. Immunopharmacol. 2010;10:900–905. doi: 10.1016/j.intimp.2010.04.028. [DOI] [PubMed] [Google Scholar]
- 37.Muri E.M., Williamson J.S. Anti-Helicobacter pylori agents. An update. Mini Rev. Med. Chem. 2004;4:201–206. doi: 10.2174/1389557043487475. [DOI] [PubMed] [Google Scholar]
- 38.Xu J., Bjursell M.K., Himrod J., Deng S., Carmichael L.K., Chiang H.C., Hooper L.V., Gordon J.I. A genomic view of the human-Bacteroides thetaiotaomicron symbiosis. Science. 2003;299:2074–2076. doi: 10.1126/science.1080029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.