Abstract
Evidence suggests that emotion regulation may be a process relevant to problematic dietary restriction. However, emotion regulation has not been evaluated as an intervention target across a range of restriction severity. This study utilized an experimental design to examine whether targeting emotion regulation reduced problematic dietary restriction. Within a self-identified restrictive sample (n = 72), the effects of an emotion regulation condition (i.e., emotion regulation training) were compared to those of a control condition (i.e., nutrition information training) on dietary restriction indices (i.e., effort to reduce intake on a progressive ratio task, work towards an alternate reinforcer on a progressive ratio task, intake by dietary recall) following a stressor. Exploratory analyses of potential moderators (i.e., restraint, BMI, binge eating and purging status, emotion regulation difficulties) were conducted to examine whether these factors affected the impact of training on dietary restriction. No significant main effects of condition were detected on any outcome measure. However, results were moderated by BMI status. Participants with lower BMIs exerted less effort towards dietary restriction following the emotion regulation condition versus the control condition (p = 0.02). Results suggest that targeting emotion regulation may help to reduce problematic dietary restriction among lower weight individuals.
Keywords: Dietary restriction, Eating disorder anorexia nervosa, Emotion regulation
Problematic dietary restriction, or limiting caloric and/or nutrient consumption in a disordered manner that is inadequate for the long-term maintenance of appropriate weight and/or health (Haynos & Fruzzetti, 2015), is a surprisingly common practice that is associated with serious consequences. Although many who cut back on intake do so in a less severe and harmful manner (e.g., healthy portion control), evidence suggests that a substantial number of individuals engage in the more extreme practices characterized by problematic dietary restriction, such as skipping meals or fasting, to control weight (Mitchison, Hay, Slewa-Younan, & Mond, 2012). Individuals engaging in problematic dietary restriction can experience a range of serious physical and psychological consequences (Daee et al., 2002; Forman-Hoffman, 2004), are at elevated risk of developing an eating disorder (Liechty & Lee, 2013) or obesity (Neumark-Sztainer et al., 2006), and have suicide rates ten times higher than those who do not engage in dietary restriction (Daee et al., 2002).
Despite the negative physical and psychological effects of problematic dietary restriction, treatment for this set of behaviors is lacking. No clearly efficacious treatments have been identified for adults with anorexia nervosa (Berkman et al., 2006), which could be considered the prototype of extreme dietary restriction, or for other subthreshold eating disorders primarily characterized by problematic dietary restriction (Ricca et al., 2010). Additionally, there are no established interventions for problematic dietary restriction that does not yet meet eating disorder criteria (Jacobi, Völker, Trockel, & Taylor, 2012). Thus, there is a need for more effective treatment of problematic dietary restriction across clinical severity.
Progress in treatment development for problematic dietary restriction may be limited by a lack of knowledge regarding the risk and maintenance mechanisms of such behavior. However, recently there has been increasing interest in examining emotion regulation as a psychological process relevant to problematic dietary restriction (Haynos & Fruzzetti, 2011). It has been proposed that individuals who engage in disordered dietary restriction have deficits in the ability to effectively modulate emotion and, therefore, rely on restriction to produce desired affective changes. There is research beginning to support this hypothesis, the majority of which has been conducted in samples with anorexia nervosa. Studies have found that individuals with anorexia nervosa display elevated difficulties with emotion regulation (Harrison, Sullivan, Tchanturia, & Treasure, 2010; Svaldi, Griepenstroh, Tuschen-Caffier, & Ehring, 2012), which do not remit with weight restoration (Haynos, Roberto, Martinez, Attia, & Fruzzetti, 2014), and predict long-term persistence of disordered eating (Racine & Wildes, 2014). There is also initial evidence suggesting a functional link between dietary restriction and affect, such that affective changes serve as precipitants and consequences of dietary restriction behavior among individuals with anorexia nervosa (Engel et al., 2013). There has been less research examining emotion regulation processes among individuals who engage in problematic dietary restriction at lower severity levels. However, there is evidence that such individuals have poorer emotion regulation abilities than those who do not restrict eating (Ackard, Croll, & Kearney-Cooke, 2002).
These studies suggest the utility of targeting emotion regulation difficulties in the treatment of problematic dietary restriction across a range of clinical presentations. Some interventions have begun targeting aspects of emotion regulation in anorexia nervosa (Chen et al., 2015; Lynch et al., 2013; Wildes, Marcus, Cheng, McCabe, & Gaskill, 2014). However, there has been no examination of emotion regulation as a specific intervention target across a range of restriction severity. There is growing interest in examining problem behaviors cross-diagnostically in order to identify common mechanisms across a range of severity and presentation (Morris & Cuthbert, 2012). Problematic dietary restriction has not often been examined dimensionally, due to uncertainty regarding whether such behaviors are disordered at the subthreshold level (Lowe & Timko, 2004). However, evidence suggests that problematic dietary restriction frequently predates the development of a full-threshold eating disorder (Affenito, Dohm, Crawford, Daniels, & Striegel-Moore, 2002), and can lead to negative consequences even in the absence of a diagnosed eating disorder (Daee et al., 2002; Forman-Hoffman, 2004; Neumark-Sztainer et al., 2006). Thus, there is compelling reason to investigate problematic dietary restriction across severity levels, ranging from subclinical to clinical severity.
The primary objective of this study was to conduct a randomized experiment to test whether targeting emotion regulation reduces problematic dietary restriction behavior across a range of clinical severity. Other studies have begun using single-session experiments to test potential treatment targets for eating disorders (e.g., Cardi, Esposito, Clarke, Schifano, & Treasure, 2015), as this approach offers minimized resource burden and more rapid dissemination of results compared to a clinical trial. Therefore, we conducted a randomized, controlled experimental study comparing the impact of an emotion regulation condition (i.e., emotion regulation training) to an active control condition (i.e., nutrition information training) on dietary restriction behavior following a stressor. The primary hypothesis was that the emotion regulation training would have a greater impact on dietary restriction behavior compared to the control condition. Our secondary, exploratory objective was to examine potential moderators of outcome following emotion regulation versus nutrition information training. Because this objective was exploratory, we had no a priori hypotheses about which clinical characteristics would moderate training effects.
1. Methods
1.1. Participants
The sample size of 72 participants was determined through a power analysis conducted using G-Power software (Faul, Erdfelder, Buchner, & Lang, 2009), assuming an alpha level of 0.05 and sufficient power (80%) to detect a large effect size (f = 0.40) for fixed effects, main effects, and interactions in an experiment with two conditions and up to three covariates.
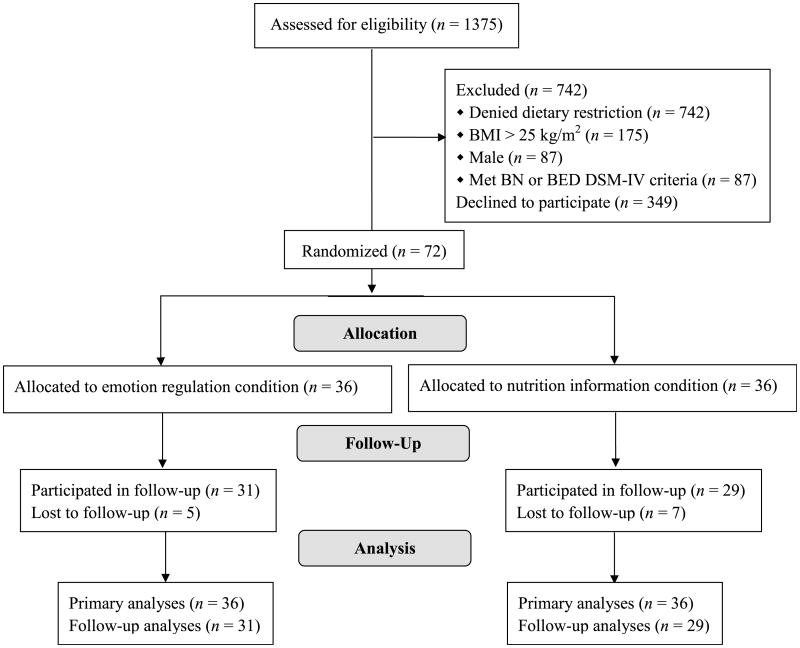
Inclusion criteria included: 1) Age >18 years old; 2) Female; 3) Endorsement of engaging in problematic dietary restriction ≥1 day within the last month on the Dietary Restriction Screener (DRS; Haynos & Fruzzetti, 2015). Exclusion criteria included: 1) Meeting DSM-IV criteria for bulimia nervosa or binge eating disorder by the Eating Disorder Examination- Questionnaire (EDE-Q) (Fairburn & Beglin, 1994), using the method described by Berg et al. (2012); and 2) BMI ≥ 25 kg/m2. These criteria were selected in order to recruit participants engaging in clinically relevant dietary restriction across a range of severity (sub-clinical to meeting criteria for anorexia nervosa) and for whom dietary restriction, rather than binge eating or overeating, was the primary clinical concern. Males were excluded due to differing metabolic needs, potentially leading to extraneous variability on dietary restriction-related outcome measures. Fig. 1 highlights the participant flow for this study. Of note, the 349 invited participants who declined to participate either failed to respond to the invitation email or to show for a scheduled appointment.
Fig. 1.
Consolidated Standards of Reporting (CONSORT) diagram of participant flow through study protocol.
1.2. Study procedures
1.2.1. Study overview
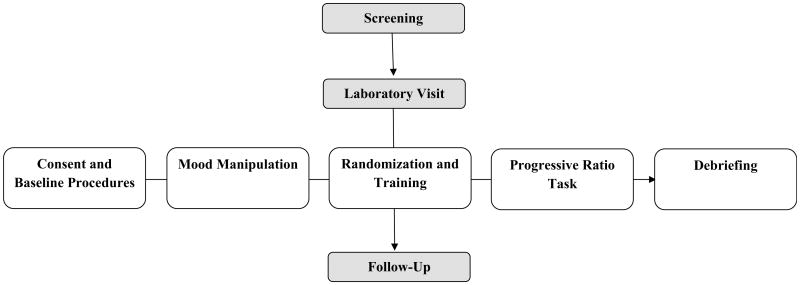
Fig. 2 outlines the flow of study procedures. Individuals participated in screening for eligibility and those who were eligible were invited to participate in the laboratory portion of the study. During the laboratory portion of the study, participants first signed informed consent and completed baseline measures (including a twenty-four dietary recall). Participants were then exposed to the mood manipulation, which consisted of receiving the information that they would be expected to consume some amount of a high-calorie milkshake as a part of the study. This information was designed to increase negative and decrease positive affect. Participants were then randomly assigned to the emotion regulation condition (i.e., emotion regulation training) or active control condition (i.e., nutrition information training) and participated in the training to which they were assigned. Following the training, participants completed a progressive ratio (PR) computer task, which allowed them to work (through space bar presses) towards: 1) decreasing the amount of milkshake that they would be expected to consume, and/or 2) increasing the amount of money that would be awarded to them. The primary outcome variable in this study was the number of bar presses towards decreased food intake. The day after experimental procedures, a 24 h dietary recall was conducted to determine whether interventions impacted consumption for the remainder of the day. All study procedures were conducted at a mid-size university in the Western U.S. and approved by the local Institutional Review Board.
Fig. 2.
Flowchart of study procedures.
1.2.2. Recruitment and screening
Participants were primarily recruited through an online psychology department recruitment site, flyers hung throughout the campus and community, and online and print advertisements. Participants were offered compensation either in the form of extra credit in psychology courses or two movie tickets. Interested individuals participated in an initial screening for eligibility either through the online recruitment site or over the phone.
1.2.3. Consent and baseline procedures
Individuals who were interested and eligible were invited to participate in the laboratory portion of the study. Study procedures were conducted in the morning following an overnight fast from 10:00 p.m. the evening prior in order to establish consistency in hunger/satiety levels. Upon entering the laboratory, participants completed informed consent procedures. Participants were then administered baseline measures, including a 24 h dietary recall to confirm the overnight fast and to assess baseline daily food consumption.
1.2.4. Mood manipulation
Following baseline procedures, participants received instructions that they would be asked to consume a self-selected portion of a high-calorie milkshake at the end of the study. Participants were provided nutritional information for the milkshake indicating high calorie, sugar, and fat content. This information was intended to be emotionally evocative for a group engaging in problematic dietary restriction. Affective changes were examined from baseline to following this mood manipulation to confirm that this information decreased positive and increased negative affect.
1.2.5. Training
After completing baseline measures, participants were randomly assigned to either an emotion regulation training or a nutrition information training using a 1:1 allocation based on a computer-generated randomization schedule. Randomization was stratified by binge eating status within the past month (yes/no) in order to balance the likelihood of binge eating between groups. The training consisted of a 40-min computer-led automated Power-Point presentation that was narrated by the principal investigator. Both trainings included several interactional exercises, which required participants to complete worksheets on the training material, in order to personalize the training and increase engagement and adherence with the training material. The trainings were developed to be consistent in length (40 min), formatting (15 slides/training), and number of interactional exercises (3 exercises/training) in order to reduce confounds between conditions. In both conditions, research staff showed participants how to initiate the training on the computer and left participants alone in laboratory room to participate in the training in a self-led manner.
The emotion regulation training was informed by the principles and techniques of Dialectical Behavior Therapy (DBT; Linehan, 1993), a therapy designed to target problems with emotion regulation. The content of this training was taken directly from the emotion regulation module of the DBT skills training manual (Linehan, 1993) and was adapted to the computerized version by the principal investigator of the study, a clinical psychology doctoral student with four years of DBT training. The training was aimed at providing skills for effectively managing difficult emotions without engaging in harmful actions (e.g., dietary restriction). This training instructed and guided participants on how to: a) accurately and mindfully identify emotions; b) notice judgments and alter them to be more descriptive; and c) manage emotions using behavioral techniques (i.e., “opposite action” and distraction) and mindfulness techniques (i.e., acceptance of emotion). This training described how to use these techniques broadly and in a challenging eating situation. Participants were guided through multiple practices of emotion regulation skills and prompted to use these techniques to manage their emotions during the expected test meal. A detailed description of the emotion regulation training can be found in Table 1.
Table 1.
Detailed description of the content presented in the emotion regulation and nutrition information training sessions.
| Slide | Emotion regulation training | Nutrition information training |
|---|---|---|
| 1 | Understanding the connection between emotions and dietary restriction | Understanding daily caloric needs (e.g., 2000 calories recommended) |
| 2 | Examining the functions of emotions (e.g., to communicate to self and others) | Experiential exercise: Calculate daily caloric needs |
| 3 | Identifying primary emotions (i.e., sadness, fear, anger, and shame) | Identifying an ideal weight range |
| 4 | Experiential exercise: Identify current emotions using body sensations, thoughts, and urges | Understanding the dietary restriction continuum (from healthy weight management to disordered eating) |
| 5 | Differentiating primary from secondary emotional reactions: General example | Understanding problematic and disordered eating patterns (i.e., what represents healthy and unhealthy eating patterns) |
| 6 | Differentiating primary from secondary emotional reactions: General example (cont.) | Identifying the negative physical effects of dietary restriction |
| 7 | Differentiating primary from secondary emotional reactions: Application to a difficult eating situation | Experiential exercise: Identify the negative physical effects of dietary restriction |
| 8 | Using descriptions, rather than judgments, to describe emotional reactions | Understanding how the body uses calories |
| 9 | Using descriptions, rather than judgments, to describe emotional reactions to difficult eating situations | Understanding how the energy from caloric intake is distributed throughout the body |
| 10 | Experiential exercise: Identify current judgments about test meal and change these to descriptive statements | Understanding the importance of protein |
| 11 | Balancing acceptance and change strategies to managing emotions | Understanding the importance of carbohydrates |
| 12 | Using mindfulness to accept difficult emotions | Understanding the importance of fat |
| 13 | Using “Opposite Action” to change difficult emotions | Understanding how many calories are needed to gain weight |
| 14 | Using distraction to change difficult emotions | Understanding why diets don't work for most people |
| 15 | Experiential exercise: Plan how to use emotion regulation skills to manage the test meal | Experiential exercise: Plan how to use nutrition information to manage the test meal |
The nutrition information training was selected as an analogue to nutritional counseling interventions, which have been used as a comparison group in clinical trials for individuals with anorexia nervosa (e.g., Pike, Walsh, Vitousek, Wilson, & Bauer, 2003). The nutrition information condition was developed by the principal investigator in collaboration with a dietician to correspond to standard nutrition training for eating disorders and was informed by the manual used for a prior nutritional counseling intervention (Pike et al., 2003). The overall purpose of this training was to provide participants information about the differences between healthy versus disordered eating habits and the importance of adequate nutrition. Participants were provided information regarding: a) appropriate energy intake for women in their age group; b) the body's nutritional needs (i.e., the necessity of carbohydrates, fats, and protein); and c) the negative physical and psychological effects of dietary restriction. Although nutrition interventions counsel moderate consumption, this training described how intermittent consumption of high-calorie foods, such as the milkshake described in this study, could be balanced with other food choices to meet nutritional needs. Participants were prompted to use this information as was helpful during the expected test meal. A detailed description of the nutrition information training can be found in Table 1. Materials for both trainings are available by request.
1.2.6. Progressive ratio (PR) computer task
Following the training, participants were asked to complete a PR computer task. Similar paradigms have been used to measure the effort that participants will expend to obtain eating- and exercise-related reinforcing outcomes (Klein et al., 2010; Schebendach, Klein, Foltin, Devlin, & Walsh, 2007; Temple et al., 2009). This PR task provided participants the opportunity to work towards either decreasing food intake (from an initial value of 1000 kcal) or increasing compensation (from an initial value of $0). The PR task consisted of ten trials. Each of the ten trials allowed participants to earn 1/10 of the maximum dietary restriction outcome (1000 kcal decrease or 0 kcal expected consumption) or compensation outcome ($30 compensation). Therefore, in each trial participants could work to decrease intake by 100 kcal or increase compensation by $3.
At the beginning of each trial, participants were instructed to select an icon representing the outcome of their choosing (i.e., decrease intake or increase compensation). After selecting the desired outcome, participants were required to work towards this outcome by pressing the space bar on the computer a number of times. As the trials increased, the number of space bar presses required to obtain the selected outcome increased. The first trial required 50 presses, and subsequent trials (Trials 2–10) required 250, 450, 650, 850, 1050, 1250, 1450, 1650, and 1850 presses respectively. To earn the maximum dietary restriction or compensation outcome, participants would have to press the space bar 9500 times. Participants were required to work exclusively towards the chosen outcome for the remainder of the trial; however, they were provided an opportunity to choose either outcome for each subsequent trial. A maximum of 40 min was allotted to complete all trials. Participants could discontinue the task at any time. However, by doing so, they would forfeit the opportunity to work further towards either outcome.
1.2.7. Debriefing and follow-up
At the end of the study, participants underwent a debriefing in which they were informed that they would not be asked to consume any milkshake and would receive the full compensation of $30, regardless of the amount of effort they had exerted towards either outcome. Incomplete disclosure on these points had been used to incentivize work on the PR task. The following morning, research staff conducted a second 24 h dietary recall with the participant over the phone.
1.3. Measures
1.3.1. Screening measures
Participants completed a screening demographics questionnaire, which assessed age, race/ethnicity, and self-reported height and weight. The Dietary Restriction Screener (Haynos & Fruzzetti, 2015) was administered at screening to select for a sample of individuals endorsing problematic dietary restriction within the last month. This measure clearly describes the construct of problematic dietary restriction (i.e., consuming objectively too little or a contextually inadequate amount in order to impact body image), provides examples of behaviors that would constitute problematic dietary restriction, and asks participants whether they had engaged in such behavior within the past month. This method of identifying individuals engaging in problematic dietary restriction was selected due to the poor construct validity of frequently-used dietary restraint measures (Stice, Fisher, & Lowe, 2004; 2007), which measure desire to restrict, as opposed to actual dietary restriction, and the results of a validation study that found that endorsement of problematic dietary restriction on the DRS predicted elevated disordered eating and reduced laboratory food intake more effectively than a commonly-used restraint measure (Haynos & Fruzzetti, 2015).
The Eating Disorder Examination Questionnaire (EDE-Q) (Fairburn & Beglin, 1994) was administered at screening to exclude individuals meeting DSM-IV criteria for bulimia nervosa or binge eating disorder. The EDE-Q is a widely used self-report measure of eating behaviors and cognitions over the previous month. The measure provides a Global and four subscale scores: Restraint, Eating Concern, Shape Concern, and Weight Concern. The EDE-Q also gathers information about any instances of objective binge eating (consumption of an objectively large amount of food while experiencing a sense of having lost control over eating) and purging (by vomiting, laxatives, and/or diuretics). While the EDE-Q was not initially designed to establish eating disorder diagnoses, prior research has identified reliable and valid methods of establishing DSM-IV criteria for eating disorder diagnosis using the EDE-Q (Berg et al., 2012). The reliability of the EDE-Q in this sample, as measured by Cronbach's α was 0.95.
1.3.2. Manipulation checks
The Positive and Negative Affect Schedule (Watson, Clark, & Tellegen, 1988) was administered to measure positive and negative affect at baseline, following the mood manipulation, and after the training. This measure was used to confirm that negative affect increased and positive affect decreased after the mood manipulation and that negative affect decreased and positive affect increased following the emotion regulation training to confirm that the training assisted with emotion regulation. Cronbach's α scores for the positive affect scale ranged from 0.85 to 0.89 and negative affect scale ranged from 0.78 to 0.90.
Acceptability visual analogues scales were administered following the training in order to confirm that the trainings were matched on acceptability. Participants completed a questionnaire assessing training acceptability ranging from 0 to 100. The following questions were used to assess acceptability: 1) How enjoyable did you find the intervention? 2) How interesting did you find the intervention? 3) How boring did you find the intervention? 4) How interactive did you find the intervention? 5) How informative did you find the intervention? 6) How likely are you to use the information from this intervention in your life?
At the end of the study, participants completed an Emotion Regulation Knowledge Questionnaire and Nutritional Knowledge Questionnaire. These questionnaires were designed by to reflect the content of the emotion regulation and nutrition information conditions respectively and were used to confirm that participants retained knowledge relevant to their training. Cronbach's α for these measures were 0.70 for the Emotion Regulation Knowledge Questionnaire and 0.67 for the Nutritional Knowledge Questionnaire.
1.3.3. Primary outcome measure
The primary outcome measure for this study was PR total work for dietary restriction, which was the total number of space bar presses a participant engaged in towards the outcome of decreasing food consumption in the PR task. This measure reflected the amount of effort a participant would expend to engage in dietary restriction.
1.3.4. Secondary outcomes measures
PR total work for compensation, or the total number of space bar presses to increase the money in the PR task, was examined as a secondary outcome. This measure reflected the amount of effort a participant would expend to access an alternative, more adaptive, rewarding outcome.
Post-experiment intake, or food consumption in the 24 h after the study, was also examined as a secondary study outcome. Consumption was measured at baseline and 24 h after the study by 24 h dietary recall using the using the conventional Multiple Pass Method (Johnson, Driscoll, & Goran, 1996). Research staff were trained to obtain detailed information regarding all foods and drinks consumed, including the precise amount, type, and/or brand of food consumed. The caloric content of foods and drinks consumed was obtained through the National Nutrient Database for Standard Reference Release 27 of the United States Department of Agricultural Research Service, and supplemented as needed with caloric information from the caloriecount.com website, which provides caloric information for brand item foods.
1.3.5. Moderator measures
Moderators were selected to reflect different clinical characteristics within the sample. The EDE-Q Restraint scale, endorsement of objective binge eating or purging by the EDE-Q, self-reported BMI, and the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2006), which assesses difficulties in multiple facets of emotion regulation, were examined as moderators of treatment effects. The DERS has been shown to have high internal consistency and test-retest reliability, and good predictive and construct validity (Gratz & Roemer, 2006). In the current sample, Cronbach's α for this measure was 0.84.
1.4. Data analytic strategy
1.4.1. Sample characteristics
Independent t-tests and chi-square analyses were conducted to examine differences between conditions in baseline characteristics (age, race/ethnicity, BMI, EDE Global and subscale scores, baseline food intake, % endorsing objective binge eating, % endorsing purging) in order to determine that conditions were matched on these variables.
1.4.2. Manipulation checks
To determine whether the mood manipulation was successful (i.e., increased negative and decreased positive affect), and the emotion regulation condition functioned as expected (i.e., decreased negative and increased positive affect), repeated measure ANOVAs were conducted to examine changes in PANAS positive and negative affect over the three time points (baseline, following the mood manipulation, following training), with condition included as a between subjects factor. In order to examine whether trainings were matched in acceptability, independent t-tests were conducted to examine acceptability measures between conditions. Independent t-tests were also conducted to compare scores on the Emotion Regulation Knowledge Questionnaire and Nutrition Knowledge Questionnaire between groups to confirm that participants retained knowledge relevant to the training they received.
1.4.3. Primary and secondary outcomes
Generalized linear models were used to examine the impact of condition (emotion regulation versus control) on the primary outcome measure (i.e., PR total work for dietary restriction) and secondary outcome measures (i.e., PR total work for compensation, post-experiment intake). PR total work for dietary restriction and PR total work for compensation utilized count data that were skewed and, therefore, a negative binomial distribution with log link was used to compare conditions on these indices. Post-experiment intake utilized skewed scale data; therefore, a gamma distribution with log link was used to compare groups on this outcome.
A number of potential covariates were tested for inclusion in the model (e.g., age, race/ethnicity, BMI, EDE-Q Restraint score, endorsement of objective binge eating, endorsement of purging), however only two of these (BMI and endorsement of purging) improved the fit of the model, and therefore the final model included these covariates. For the analyses predicting post-training intake, the additional covariate of baseline food intake was also included.1
1.4.4. Exploratory moderator analyses
In order to initially examine the moderation effects of clinical characteristics (BMI, endorsement of objective binge eating, and endorsement of purging, EDE-Q Restraint score, DERS score) on outcomes between conditions, generalized linear models for all dependent variables were repeated as outlined above, but with the inclusion of the moderator and moderator by condition interaction. Simple slope analyses calculated at 1 SD above and below the mean were used to investigate any significant interaction effects.
2. Results
2.1. Sample characteristics
Demographics and clinical characteristics of the study participants are listed in Table 2. On average, participants were in their early twenties (range: 18—51 years old). BMI range was considerable (16.20 kg/m2 to 24.49 kg/m2), with 15.28% of the sample (n = 11) reporting BMI scores within the underweight range (<18.5 kg/m2). The ethnic composition of the sample was 62.5% Caucasian, 15.3% Hispanic, 9.7% Multiple Ethnicities, 8.3% Asian/Pacific Islander, 1.4% African American, and 1.4% Native American (one participant did not identify ethnicity). Participants' self-reported baseline intake ranged from 236 to 3083 kilocalories (kcal) and was, on average, significantly lower than recommended for young females (Institute of Medicine, 2002). Nearly 80% of the sample (n = 57) reported baseline intake that was below nutritional recommendations. EDE-Q Global and subscale scores were elevated from community norms (Fairburn & Beglin, 1994). Using previously validated algorithms for determining eating disorder diagnoses by the EDE-Q(Berg et al., 2012), 2.8% (n = 2) of the sample met criteria for anorexia nervosa, 88.9% (n = 64) met criteria for eating disorder not otherwise specified, and 8% (n = 6) did not meet criteria for an eating disorder. Demographic and clinical characteristics were matched between conditions.
Table 2.
Demographic and clinical characteristics of the sample at baseline.
| Dependent variable | Total sample (n = 72) mean (SD) | Emotion regulation condition (n = 36) mean (SD) | Nutrition information condition (n = 36) mean (SD) | df | t/χ2 | 95% CI | p | Cohen's d |
|---|---|---|---|---|---|---|---|---|
| Age (years) | 21.93 (5.62) | 22.53 (7.10) | 21.33 (3.58) | 70 | −0.91 | −3.84, 1.45 | 0.37 | 0.22 |
| Race (% Caucasian) | 62.50% | 55.56% | 69.44% | 70 | 0.141 | − | 0.33 | − |
| Body Mass Index (kg/m2) | 20.98 (2.21) | 20.56 (2.26) | 21.40 (2.11) | 70 | 1.62 | −0.20, 1.85 | 0.11 | 0.39 |
| Baseline caloric intake (kcal) | 1431.10 (646.93) | 1421.31 (614.02) | 1440.89 (686.86) | 70 | 0.13 | −286.67, 325.83 | 0.90 | 0.03 |
| EDE-Q Restraint score | 3.09 (1.41) | 3.16 (1.34) | 3.03 (1.49) | 70 | −0.38 | −0.79, 0.54 | 0.70 | 0.09 |
| EDE-Q Eating concern score | 1.77 (1.24) | 1.88 (1.37) | 1.66 (1.12) | 70 | −0.74 | −0.81, 0.37 | 0.46 | 0.18 |
| EDE-Q Shape concern score | 3.89 (1.40) | 3.87 (1.36) | 3.91 (1.46) | 70 | 0.23 | −0.62, 0.7 | 0.90 | 0.03 |
| EDE-Q Weight concern score | 3.56 (1.46) | 3.48 (1.46) | 3.64 (1.47) | 70 | 0.47 | −0.53, 0.85 | 0.64 | 0.11 |
| EDE-Q Global score | 3.08 (1.21) | 3.10 (1.19) | 3.06 (1.24) | 70 | −0.13 | −0.61, 0.54 | 0.90 | 0.03 |
| OBE (% endorsing) | 31.94% | 33.33% | 30.56% | 1 | 0.06 | − | 1.00 | − |
| OBE (per month) | 1.38 (2.95) | 1.17 (2.01) | 1.58 (3.68) | 70 | 0.60 | −0.98, 1.81 | 0.55 | 0.14 |
| Purging (% endorsing) | 33.33% | 36.11% | 30.56% | 1 | 0.25 | − | 0.80 | − |
| Purging episodes (per month) | 2.38 (4.90) | 2.33 (4.45) | 2.42 (5.38) | 70 | 0.07 | −2.24, 2.40 | 0.94 | 0.02 |
Note: EDE-Q = Eating Disorder Examination Questionnaire (Fairburn & Beglin, 1994); OBE = Objective Bulimic Episodes.
2.2. Manipulation checks
Results indicated that the mood manipulation was effective and that training impacted affect. Both PANAS positive affect, F (2, 69) = 9.96, p < 0.001, and negative affect, F (2, 69) = 28.82, p < 0.001, changed significantly across the three time points. PANAS positive affect decreased significantly from baseline (M = 25.11, SD = 7.34) to following the mood manipulation (M = 22.75, SD = 7.09), p < 0.001, d = 0.33, and rebounded significantly following training (M = 25.14, SD = 8.13), p = 0.002, d = 0.31. Similarly, PANAS negative affect increased significantly from baseline (M = 16.04, SD = 5.89) to following the mood manipulation (M = 20.67, SD = 7.84), p < 0.001, d = 0.67, and decreased significantly following training (M = 15.89, SD = 4.61), p < 0.001, d = 0.74. These findings suggest that participants were distressed by the expectation of consuming a high-calorie milkshake and that training returned affect to baseline levels. There were no significant between condition differences in change in positive affect, F (2, 69) = 1.08, p = 0.34, or negative affect, F (2, 69) = 0.54, p = 0.76, suggesting that affective changes across time did not vary between conditions.
There were no significant differences on any acceptability measure between conditions. As highlighted in Table 3, both training programs were rated as highly acceptable. Participants in the emotion regulation condition scored significantly higher on the Emotion Regulation Knowledge Questionnaire (M = 81.67, SD = 18.75) post-training than those in the nutrition information condition (M = 67.96, SD = 13.02), t(70) = −3.60, p = 0.001, d = 0.86, and participants in the nutrition information condition scored higher on the Nutrition Knowledge Questionnaire (M = 78.15, SD = 11.45) post-training compared to those in the emotion regulation condition (M = 54.26, SD = 15.13), t(70) = 7.55, p < 0.001, d = 1.81. In sum, the results from the manipulation checks indicated that the mood manipulation and training functioned as expected, and that the trainings did not vary on an extraneous variable (i.e., acceptability) unrelated to training content.
Table 3.
Acceptability ratings between conditions.
| Dependent variable | Total sample (n = 72) mean (SD) | Emotion regulation condition (n = 36) mean (SD) | Nutrition information condition (n = 36) mean (SD) | df | t/χ2 | 95% CI | p | Cohen's d |
|---|---|---|---|---|---|---|---|---|
| Enjoyable | 67.15 (19.71) | 66.39 (17.51) | 67.92 (21.92) | 70 | 0.33 | −7.80, 10.85 | 0.75 | 0.08 |
| Informative | 77.50 (17.16) | 73.89 (16.87) | 81.11 (16.91) | 70 | 1.82 | −0.72, 15.16 | 0.07 | 0.43 |
| Interactive | 64.86 (17.34) | 63.75 (17.21) | 65.97 (17.64) | 70 | 0.54 | −5.97, 10.42 | 0.59 | 0.13 |
| Interesting | 72.43 (20.83) | 72.92 (17.17) | 71.94 (24.18) | 70 | −0.20 | −10.83, 8.89 | 0.85 | 0.05 |
| Boring | 33.61 (25.87) | 36.81 (24.85) | 30.42 (26.82) | 70 | −1.05 | −18.54, 5.76 | 0.30 | 0.25 |
| Personally relevant | 75.97 (22.67) | 75.00 (23.51) | 76.94 (22.08) | 70 | 0.36 | −8.77, 12.66 | 0.72 | 0.09 |
| Likely to use in daily life | 74.51 (19.64) | 74.03 (21.11) | 75.00 (18.36) | 70 | 0.21 | −8.33, 10.27 | 0.84 | 0.05 |
2.3. Primary outcome: impact of training on PR total work for dietary restriction
The results of the generalized linear models are detailed in Table 4. Although PR total work for dietary restriction was lower in the emotion regulation condition (M = 2061.41, SE = 359.54) than the control condition (M = 2765.11, SE = 470.70), indicating less effort toward restriction, this effect was small and did not reach statistical significance, p = 0.21, d = 0.26.
Table 4.
Generalized linear models examining the impact of an emotion regulation versus control conditions on dietary restriction related outcomes.
| Dependent variable | Independent variables | Wald χ2 | B | SE | 95% CI | p |
|---|---|---|---|---|---|---|
| PR total work for dietary restriction | Body Mass Index | 7.19 | −0.18 | 0.07 | −0.31, −0.05 | 0.01* |
| Purging status | 7.84 | −0.72 | 0.26 | −1.22, −0.22 | 0.01* | |
| Condition | 1.54 | 0.29 | 0.24 | −0.17,0.76 | 0.21 | |
| PR total work for compensation | Body Mass Index | 0.73 | 0.05 | 0.05 | −0.06, 0.15 | 0.39 |
| Purging status | 1.75 | 0.34 | 0.26 | −0.16, 0.84 | 0.19 | |
| Condition | 0.29 | −0.13 | 0.25 | −0.62, 0.35 | 0.59 | |
| Post-experiment intake | Baseline intake | 8.04 | 0.00 | 0.00 | 0.00, 0.00 | 0.01* |
| Body Mass Index | 1.96 | −0.03 | 0.02 | −0.07, 0.01 | 0.16 | |
| Purging status | 0.00 | 0.01 | 0.10 | −0.19, 0.20 | 0.96 | |
| Condition | 0.34 | 0.06 | 0.02 | −0.13, 0.24 | 0.56 |
Note: PR = Progressive ratio;
p < .05.
2.4. Secondary outcomes: impact of training on other restriction-relevant outcomes
Although PR total work for compensation was higher in the emotion regulation condition (M = 6116.51, SE = 1047.46) compared to individuals in the control condition (M = 5352.75, SE = 962.01), indicating more work towards an alternate reinforcer, this difference again was small and not statistically significant, p = 0.59, d = 0.25. After controlling for baseline intake, condition did not significantly predict post-experiment food intake, p = 0.56, d = 0.13.
2.5. Exploratory analyses: moderators of training effects on restriction outcomes
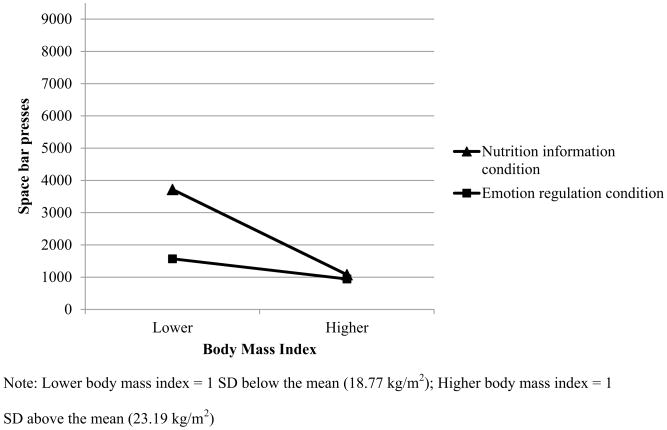
BMI significantly moderated the effects of condition on PR total work for dietary restriction, B = −0.27, SE = 0.13, p = 0.04. Simple slope analyses were conducted at 1 SD below the group mean (i.e., “lower” body mass index = 18.77 kg/m2) and 1 SD above the group mean (“higher” body mass index = 23.19 kg/m2), according to standard procedures. As highlighted in Fig. 3, simple slope analyses suggested that, among those with relatively lower BMIs, individuals in the emotion regulation condition worked significantly less to engage in dietary restriction compared to those in the control condition, B = 0.87, SE = 0.37, p = 0.02, d = 1.24; however, PR total work for dietary restriction did not differ between conditions among individuals with relatively higher BMIs, B = −0.30, SE = 0.38, p = 0.42, d = 0.14.
Fig. 3.
Effort towards restricting caloric intake through space bar presses between conditions by body mass index.
PR total work for dietary restriction was not moderated by any other variable tested and none of the clinical characteristics significantly moderated PR total work for compensation or post-experiment consumption.
3. Discussion
In this study we sought to examine whether targeting emotion regulation reduced dietary restriction across a range of clinical severity. We experimentally tested whether an emotion regulation training would have a greater impact on dietary restriction behaviors compared to an active control condition when participants were distressed. In terms of our main hypotheses, our predictions were not met. While the group receiving the emotion regulation training exerted less effort to reduce food intake at the anticipated meal and more effort to obtain an alternate reinforcer (i.e., money) compared to those in the control condition, these between condition differences were small and did not meet statistical significance. Further, intake in the 24 h following the experiment did not differ between conditions.
These data suggest that a single, 40 min computerized emotion regulation training is not effective for altering problematic dietary restriction among individuals of mixed clinical severity. This could reflect that emotion regulation may not be an effective treatment target for problematic dietary restriction across the dimension of severity. However, these findings could also reflect that a stronger and more comprehensive emotion regulation intervention is necessary to reduce problematic dietary restriction. For instance, a longer intervention or intervention targeting a greater variety of emotion regulation strategies, such as cognitive restructuring, problem-solving, distress tolerance, exposure techniques, and behavioral activation (Aldao & Nolen-Hoeksema, 2010; Linehan, 1993), may be need to impact dietary restriction. Therefore, future studies including more complex and prolonged manipulations of emotion regulation are needed to more clearly determine whether targeting emotion regulation reduces problematic dietary restriction across a range of severity.
As an exploratory aim, we examined putative moderators of training effects in order to identify whether certain subsets of restricting individuals may particularly benefit from targeting emotion regulation. We found a significant condition by BMI interaction. Individuals with relatively lower BMIs worked significantly less towards dietary restriction in the emotion regulation condition than in the control condition. However, individuals at relatively higher BMIs worked comparably towards dietary restriction in both conditions. This suggests that training in emotion regulation may significantly reduce problematic dietary restriction at the momentary level among individuals at relatively lower BMIs. This result is consistent with findings indicating that interventions targeting emotion regulation are effective for low weight individuals with anorexia nervosa (Chen et al., 2015; Lynch et al., 2013; Wildes et al., 2014). Further, this result could provide information relevant to treatment matching according to clinical characteristics (i.e., BMI) if replicated. Overall, these results suggest the utility of future research investigating the relationship between emotion regulation processes and BMI among individuals with problematic dietary restriction.
In this study, we aimed to recruit a sample of individuals displaying problematic dietary restriction across a range of severity, despite there being no established way of identifying such individuals without limiting the sample by diagnostic category. A concern that could be raised is whether the participants actually engaged in problematic dietary restriction, or instead engaged in healthy weight management. However, the DRS has been shown to identify individuals with elevated disordered eating attitudes and behaviors who engage in reduced food intake in the laboratory (Haynos & Fruzzetti, 2015). Further, the current sample displayed elevated EDE-Q scores, overwhelmingly met criteria for an eating disorder, reported lower than recommended baseline intake, and experienced a significant alterations in affect when faced with consuming a high-calorie milkshake. These findings suggest that the sample is very likely to represent women engaging in problematic dietary restriction and that such behavior can be problematic across a range of severity. However, more research is needed to guide how to best select for a dimensional sample of individuals with problematic dietary restriction.
There are notable strengths of this study. First, this study examined problematic dietary restriction across a range of severity, thus broadening the scope of the findings. Further, the study utilized an experimental design, rather than a treatment trial, to determine the impact of targeting a specific psychological process upon dietary restriction. This approach requires fewer resources, fosters a more iterative process of target identification, and allows for testing of a treatment target more precisely than in a multi-component intervention. This study also utilized a novel behavioral measure of problematic dietary restriction as the main outcome, rather than relying on self-report measures, reducing the error associated with self-report of eating behavior (Schoeller, 1990). Finally, the study included an active control condition, thus controlling for non-specific training effects.
There are also limitations to this study. While an experimental study targeting a defined psychological process is advantageous in many ways, this approach may limit the generalizability of the results due to the circumscribed nature of the testing environment. Similarly, while use of an active control condition provided strength to the study, it also made it difficult to determine whether any non significant findings could be attributed to strengths of the nutrition information condition. Another limitation of this study is reliance on self-reported height and weight. However, prior research suggests that self-reported and objective height and weight are highly correlated (Stunkard & Albaum, 1981) and that individuals with disordered dietary restriction are more accurate reporters of weight than the general population (Wolfe, Kelly-Weeder, Malcom, & McKenery, 2013). Additionally, while the EDE-Q has been used to validly establish eating disorder diagnoses (Berg et al., 2012), use of a standardized diagnostic interview may have provided a more accurate assessment of diagnosis. Further, while the study utilized one standard method of controlling for hunger and satiety levels prior to experimental procedures (i.e., fasting; Keel, Wolfe, Liddle, Young, & Jimerson, 2007; Latner, Rosewall, & Chisholm, 2008), other studies have used a standardized breakfast to control for hunger and satiety levels (e.g., Sysko, Walsh, Schebendach, & Wilson, 2005; Tanofsky-Kraff et al., 2009), which could have been more effective in controlling for baseline appetite. Finally, in order to maintain a sample that was relatively homogenous and focused specifically on dietary restriction, certain groups were excluded (i.e., individuals meeting DSM-IV criteria for bulimia nervosa or binge eating disorder, overweight and obese individuals, males, and adolescents). Therefore, the results of the study may not generalize to these groups. Future research ought to investigate the effects of targeting emotion regulation in the treatment of problematic dietary restriction using more complex intervention studies with more diverse and clinically severe samples, various comparison conditions, and differing assessment methods.
4. Conclusions
This study did not provide evidence that brief emotion regulation training can reduce problematic dietary restriction across levels of severity. However, the exploratory moderator analyses suggested that restrictive individuals at lower weights may particularly benefit from an intervention targeting emotion regulation. These results support continued investigation of emotion regulation as a treatment target among individuals engaging in problematic dietary restriction.
Acknowledgments
AFH and AEF designed this study. AFH and BH were directly involved in study implementation; AEF supervised study procedures. All authors contributed to refinement of the study protocol, statistical analyses, and review of the manuscript. The authors do not have conflicts of interest to report. Research reported in this publication was supported by pre-doctoral training fellowship F31MH097450 and post-doctoral training fellowship T32MH082761 awarded by the National Institute of Mental Health. This funding source had no role in the study design, execution, analyses, interpretation of the data, or decision to submit results. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
All analyses were repeated excluding the individuals who did not meet criteria for an eating disorder in order to determine if this altered results. However, all findings remained the same upon exclusion of these individuals, therefore these cases were included in all analyses.
References
- Ackard DM, Croll JK, Kearney-Cooke A. Dieting frequency among college females: association with disordered eating, body image, and related psychological problems. Journal of Psychosomatic Research. 2002;52:129–136. doi: 10.1016/s0022-3999(01)00269-0. [DOI] [PubMed] [Google Scholar]
- Affenito SG, Dohm FA, Crawford PB, Daniels SR, Striegel-Moore RH. Macronutrient intake in anorexia nervosa: the National Heart, Lung, and Blood Institute growth and health study. Journal of Pediatrics. 2002;141:701–705. doi: 10.1067/mpd.2002.129840. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: a transdiagnostic examination. Behavior Research and Therapy. 2010;48:974–983. doi: 10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Berg KC, Stiles-Shields EC, Swanson SA, Peterson CB, Lebow J, Le Grange D. Diagnostic concordance of the interview and questionnaire versions of the eating disorder examination. International Journal of Eating Disorders. 2012;45:850–855. doi: 10.1002/eat.20948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman ND, Bulik CM, Brownley KA, Lohr KN, Sedway JA, Rooks A, et al. Management of eating disorders. Evidence Report Technolology Assessment (Full Report) 2006;135:1–166. [PMC free article] [PubMed] [Google Scholar]
- Cardi V, Esposito M, Clarke A, Schifano S, Treasure J. The impact of induced positive mood on symptomatic behaviour in eating disorders. An experimental, AB/BA crossover design testing a multimodal presentation during a test-meal. Appetite. 2015;87:192–198. doi: 10.1016/j.appet.2014.12.224. [DOI] [PubMed] [Google Scholar]
- Chen EY, Segal K, Weissman J, Zeffiro TA, Gallop R, Linehan MM, et al. Adapting dialectical behavior therapy for outpatient adult anorexia nervosa–a pilot study. International Journal of Eating Disorders. 2015;48:123–132. doi: 10.1002/eat.22360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daee A, Robinson P, Lawson M, Turpin JA, Gregory B, Tobias JD. Psychologic and physiologic effects of dieting in adolescents. Southern Medical Journal. 2002;95:1032–1041. [PubMed] [Google Scholar]
- Engel SG, Wonderlich SA, Crosby RD, Mitchell JE, Crow S, Peterson CB, et al. The role of affect in the maintenance of anorexia nervosa: evidence from a naturalistic assessment of momentary behaviors and emotion. Journal of Abnormal Psychology. 2013;122:709–719. doi: 10.1037/a0034010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–370. [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behavior Research Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Forman-Hoffman V. High prevalence of abnormal eating and weight control practices among U.S. high-school students. Eating Behaviors. 2004;5:325–336. doi: 10.1016/j.eatbeh.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavior Assessment. 2006;26:41–54. [Google Scholar]
- Harrison A, Tchanturia K, Treasure J. Attentional bias, emotion recognition, and emotion regulation in anorexia: state or trait? Biological Psychiatry. 2010;68:755–761. doi: 10.1016/j.biopsych.2010.04.037. [DOI] [PubMed] [Google Scholar]
- Haynos AF, Fruzzetti AE. Anorexia nervosa as a disorder of emotion dysregulation: theory, evidence, and treatment implications. Clinical Psychology Science and Practice. 2011;18:183–202. [Google Scholar]
- Haynos AF, Fruzzetti AE. Initial evaluation of a single-item screener to assess problematic dietary restriction. Eating and Weight Disorders. 2015;20:405–413. doi: 10.1007/s40519-014-0161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynos AF, Roberto CA, Martinez MA, Attia E, Fruzzetti AE. Emotion regulation difficulties in anorexia nervosa before and after inpatient weight restoration. International Journal of Eating Disorders. 2014;47:888–891. doi: 10.1002/eat.22265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, D.C.: The National Academic Press; 2002. [DOI] [PubMed] [Google Scholar]
- Jacobi C, Völker U, Trockel MT, Taylor CB. Effects of an internet-based intervention for subthreshold eating disorders: a randomized controlled trial. Behavior Research and Therapy. 2012;50:93–99. doi: 10.1016/j.brat.2011.09.013. [DOI] [PubMed] [Google Scholar]
- Johnson RK, Driscoll P, Goran MI. Comparison of multiple-pass 24 hour recall estimates of energy intake with total energy expenditure determined by the doubly labeled water method in young children. Journal of the American Dietetics Association. 1996;96:1140–1144. doi: 10.1016/S0002-8223(96)00293-3. [DOI] [PubMed] [Google Scholar]
- Keel PK, Wolfe BE, Liddle RA, De Young KP, Jimerson DC. Clinical features and physiological response to a test meal in purging disorder and bulimia nervosa. Archives of General Psychiatry. 2007;64:1058–1066. doi: 10.1001/archpsyc.64.9.1058. [DOI] [PubMed] [Google Scholar]
- Klein DA, Schebendach JE, Gershkovich M, Bodell LP, Foltin RW, Walsh BT. Behavioral assessment of the reinforcing effect of exercise in women with anorexia nervosa: further paradigm development and data. International Journal of Eating Disorders. 2010;43:611–618. doi: 10.1002/eat.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latner JD, Rosewall JK, Chisholm AM. Energy density effects on food intake, appetite ratings, and loss of control in women with binge eating disorder and weight-matched controls. Eating Behaviors. 2008;9:257–266. doi: 10.1016/j.eatbeh.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Liechty JM, Lee MJ. Longitudinal predictors of dieting and disordered eating among young adults in the U.S. International Journal of Eating Disorders. 2013;46:790–800. doi: 10.1002/eat.22174. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Lowe MR, Timko CA. Dieting: really harmful, merely ineffective, or actually helpful? British Journal of Nutrition. 2004;92:S19–S22. doi: 10.1079/bjn20041136. [DOI] [PubMed] [Google Scholar]
- Lynch TR, Gray KL, Hempel RJ, Titley M, Chen EY, O'Mahen HA. Radically open-dialectical behavior therapy for adult anorexia nervosa: feasibility and outcomes from an inpatient program. BMC Psychiatry. 2013;13:293. doi: 10.1186/1471-244X-13-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchison D, Hay P, Slewa-Younan S, Mond J. Time trends in population prevalence of eating disorder behaviors and their relationship to quality of life. PLoS One. 2012;7:e48450. doi: 10.1371/journal.pone.0048450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SE, Cuthbert BN. Research domain criteria: cognitive systems, neural circuits, and dimensions of behavior. Dialogues in Clinical Neuroscience. 2012;14:29–37. doi: 10.31887/DCNS.2012.14.1/smorris. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? Journal of the American Dietetics Association. 2006;106:559–568. doi: 10.1016/j.jada.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Pike KM, Walsh BT, Vitousek K, Wilson GT, Bauer J. Cognitive behavior therapy in the posthospitalization treatment of anorexia nervosa. American Journal of Psychiatry. 2003;160:2046–2049. doi: 10.1176/appi.ajp.160.11.2046. [DOI] [PubMed] [Google Scholar]
- Racine SE, Wildes JE. Dynamic longitudinal relations between emotion regulation difficulties and anorexia nervosa symptoms over the year following intensive treatment. Journal of Consulting and Clinical Psychology. 2014;83:785–795. doi: 10.1037/ccp0000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricca V, Castellini G, Lo Sauro C, Mannucci E, Ravaldi C, Rotella F, et al. Cognitive-behavioral therapy for threshold and subthreshold anorexia nervosa: a three-year follow-up study. Psychotherapy and Psychosomatics. 2010;79:238–248. doi: 10.1159/000315129. [DOI] [PubMed] [Google Scholar]
- Schebendach JE, Klein DA, Foltin RW, Devlin MJ, Walsh BT. Relative reinforcing value of exercise in inpatients with anorexia nervosa: model development and pilot data. International Journal of Eating Disorders. 2007;40:446–453. doi: 10.1002/eat.20392. [DOI] [PubMed] [Google Scholar]
- Schoeller DA. How accurate is self-reported dietary energy intake? Nutrition Reviews. 1990;48:373–379. doi: 10.1111/j.1753-4887.1990.tb02882.x. [DOI] [PubMed] [Google Scholar]
- Stice E, Cooper JA, Schoeller DA, Tappe K, Lowe MR. Are dietary restraint scales valid measures of moderate- to long-term dietary restriction? Objective biological and behavioral data suggest not. Psychological Assessment. 2007;19:449–458. doi: 10.1037/1040-3590.19.4.449. [DOI] [PubMed] [Google Scholar]
- Stice E, Fisher M, Lowe MR. Are dietary restraint scales valid measures of acute dietary restriction? Unobtrusive observational data suggest not. Psychological Assessment. 2004;16:51–59. doi: 10.1037/1040-3590.16.1.51. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Albaum JM. The accuracy of self-reported weights. American Journal of Clinical Nutrition. 1981;34:1593–1599. doi: 10.1093/ajcn/34.8.1593. [DOI] [PubMed] [Google Scholar]
- Svaldi J, Griepenstroh J, Tuschen-Caffier B, Ehring T. Emotion regulation deficits in eating disorders: a marker of eating pathology or general psychopathology? Psychiatry Research. 2012;197:103–111. doi: 10.1016/j.psychres.2011.11.009. [DOI] [PubMed] [Google Scholar]
- Sysko R, Walsh BT, Schebendach J, Wilson GT. Eating behavior among women with anorexia nervosa. American Journal of Clinical Nutrition. 2005;82:296–301. doi: 10.1093/ajcn.82.2.296. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, Kozlosky M, Schvey NA, Shomaker LB, et al. Laboratory assessment of the food intake of children and adolescents with loss of control eating. American Journal of Clinical Nutrition. 2009;89:738–745. doi: 10.3945/ajcn.2008.26886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JL, Bulkley AM, Badawy RL, Krause N, McCann S, Epstein LH. Differential effects of daily snack food intake on the reinforcing value of food in obese and nonobese women. American Journal of Clinical Nutrition. 2009;90:304–313. doi: 10.3945/ajcn.2008.27283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wildes JE, Marcus MD, Cheng Y, McCabe EB, Gaskill JA. Emotion acceptance behavior therapy for anorexia nervosa: a pilot study. International Journal of Eating Disorders. 2014;47:870–873. doi: 10.1002/eat.22241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe BE, Kelly-Weeder S, Malcom AW, McKenery M. Accuracy of self-reported body weight and height in remitted anorexia nervosa. Journal of American Psychiatric Nurses Association. 2013;19:66–70. doi: 10.1177/1078390313481062. [DOI] [PubMed] [Google Scholar]