Abstract
Background
Pregnant and postpartum women may be at increased risk of violent death including homicide and suicide relative to non-pregnant women, but US national data have not been reported since implementation of enhanced mortality surveillance.
Objective
To estimate homicide and suicide ratios among women who are pregnant or postpartum and to compare their risk of violent death to non-pregnant/non-postpartum women.
Study Design
Death certificates (n=465,097) from US states with enhanced pregnancy mortality surveillance from 2005–2010 were used to compare mortality among four groups of women age 10–54: pregnant, early postpartum (pregnant within 42 days of death), late postpartum (pregnant within 43 days to 1 year of death) and non-pregnant/non-postpartum. We estimated pregnancy-associated mortality ratios and compared to non-pregnant/non-postpartum mortality ratios in order to identify differences in risk after adjusting for potential levels of pregnancy misclassification as reported in the literature.
Results
Pregnancy-associated homicide victims were most frequently young, Black, and undereducated while pregnancy-associated suicide occurred most frequently among older White women. After adjustments, pregnancy-associated homicide risk ranged from 2.2–6.2 per 100,000 live births, depending on the degree of misclassification estimated, compared to 2.5–2.6 per 100,000 non-pregnant/non-postpartum women aged 10–54. Pregnancy-associated suicide risk ranged from 1.6–4.5 per 100,000 live births after adjustments compared to 5.3–5.5 per 100,000 women aged 10–54 among non-pregnant/non-postpartum women. Assuming the most conservative published estimate of misclassification, risk of homicide among pregnant/postpartum women was 1.84 times that of non-pregnant/non-postpartum women (95% confidence interval: 1.71, 1.98) while risk of suicide was decreased (relative risk=0.62, 95% confidence interval: 0.57, 0.68).
Conclusion
Pregnancy and postpartum appear to be times of increased risk for homicide and decreased risk for suicide among women in the US.
Keywords: pregnancy-associated homicide, pregnancy-associated suicide, violence, pregnancy, postpartum
Introduction
Improvements in maternal health care in the US since the mid-1950s have drastically reduced mortality due to hemorrhage, hypertension, complications of cesarean delivery, and other obstetric causes.1 Less attention has been paid to identifying and preventing injury-related fatalities and violent deaths including homicide and suicide among pregnant women and within the first year postpartum. Although pregnancy does not cause these deaths physiologically, it may be related to their occurrence - particularly for deaths resulting from intimate partner violence. Pregnancy does not appear to confer protection against victimization 2,3 and in fact may add stress and exacerbate vulnerable circumstances in abusive relationships.4
In an effort to encourage enhanced mortality monitoring beyond those deaths strictly classified as maternal, the American College of Obstetricians and Gynecologists and Centers for Disease Control and Prevention defined “pregnancy-associated mortality” as the death of a woman while pregnant or within 1 year of termination of pregnancy, regardless of the site or duration of the pregnancy and irrespective of the cause of death.5 Previous studies on pregnancy-associated mortality based on local city- or state-level data consistently find homicide ranks among the leading causes of death among women who are pregnant or recently postpartum, with variations by geographic area and demographic subgroup.4,6–14
Despite the accumulating evidence of the magnitude of violent deaths, rigorous examination of mortality from non-obstetric causes in pregnancy and postpartum is rare, particularly in comparison to non-pregnant women.15 The 2003 revision to the US Standard Certificate of Death included an item to classify pregnancy status of a female decedent in the year preceding death in order to improve routine monitoring of pregnancy-associated mortality.16 Specifically, checkboxes identify the temporal relationship of death to pregnancy: during, within 42 days, or 43 days to 1 year after pregnancy.17 Prior to the revision, ascertainment of pregnancy status differed across states and although some states’ certificates included a pregnancy checkbox, cases of deaths occurring during and around the time of pregnancy were underreported with evidence of over 60% missing cases from some jurisdictions.18–20 National implementation of the 2003 revision has been incremental; by 2005, 22 jurisdictions had adopted the revision or maintained equivalent pregnancy items on death certificates. By 2010, the number had increased to 37. The purpose of this analysis was to use these newly available data to describe mortality among four groups of reproductive aged women in the United States from 2005–2010: pregnant, early postpartum (pregnant within 42 days of death), late postpartum (pregnant within 43 days to 1 year of death) and non-pregnant/non-postpartum women. Second, we aimed to compare risk across demographic characteristics of victims of pregnancy-associated violent deaths and finally to determine if pregnancy/postpartum represents a time of increased risk for violent death.
Materials and Methods
Study Population
The National Center for Health Statistics (NCHS) provided death records for all women in 50 US states and the District of Columbia (DC) from 2005–2010, inclusive. For the purpose of this analysis, data were limited to women age 10–54 to ensure complete coverage of the population with reported pregnancy-associated deaths and to states and years with a temporal pregnancy item on death records that allowed for identification of decedents who were pregnant within 12 months of death (n=465,097). This includes 36 states and DC that had adopted the 2003 temporal pregnancy variable or retained equivalent items for at least one year (Table 1). Nine states were excluded for lack of a pregnancy item on records for the study years and the remaining 5 were excluded for records that captured pregnancy status only up to 90 days prior to death.
Table 1.
States and years for records included in analysis.
| Years | States |
|---|---|
| 2005–2010 | CT, FL, ID, KS, MI, MT, NE, NH, NJ, NY, OK, SC, SD, UT, WA, WY; Excluded from proportionate mortality for lack of detailed temporality: CA,IA, KY, MD, MN, TX (2005 only) |
| 2006–2010 | DC, NM, OR, RI |
| 2007–2010 | DE, OH |
| 2008–2010 | AR, GA, IL, IN, NV, ND |
| 2009–2010 | VT |
| 2010 | AZ, MO |
| Excluded from analysis | |
| Cannot identify late postpartum (pregnancy within past 12 months): AL, LA,MS, VA | |
| Utilized pregnancy prompt, not question: ME | |
| No pregnancy information: AK, CO, HI, MA, NC, PA, TN, WV, WI | |
For jurisdictions with mid-year implementation of the revision, we limited our analyses to the first full year of data. Five of the 37 included jurisdictions (CA, IA, KY, MN for all study years and TX until 2006) had items asking only if the decedent had been pregnant within the past 12 months. These states were excluded from pregnant and postpartum proportionate mortality calculations. Where pregnant/postpartum status was unknown, we examined International Classification of Diseases (ICD-10) codes for underlying cause of death and identified additional maternal deaths based on codes within the Pregnancy, Childbirth, and the Puerperium classification. Where possible, these deaths were classified temporally (Supplemental Table 1). When temporality could not be determined, women were excluded from proportionate mortality calculations but were included in all analyses where pregnant and postpartum women were combined (pregnancy-associated mortality). Remaining women with unknown pregnancy status were classified in the non-pregnant/non-postpartum group. This analysis of de-identified death records was exempt from Institutional Review Board approval.
Explanatory Variables
We compared women across characteristics available on the death record: age (5-year age groups), race (non-Hispanic Black, non-Hispanic White, Hispanic, and other), marital status (married, not married), and education (less than high school; high school graduate or GED; greater than high school). As the education item differs across death certificate versions, the continuous values from the 1989 certificate format (0 [no formal education] to 17 [5 or more years of college]) were grouped with the 2003 values as follows: 0–11 years with less than high school; 12 with high school graduate; and 13–17 with some college but no degree, associate’s, bachelor’s, Master’s, or PhD all grouped as greater than high school. Stratification by education status was limited to women who were age 20 or older at time of death as younger women may not have completed educational attainment. ICD-10 codes for underlying cause of death were grouped as follows: natural (including obstetric and non-obstetric diseases and conditions), transport-related injury, other injury, homicide, suicide, and other external causes (Supplemental Table 2).
Outcome Measures
Pregnancy-associated homicide ratios were defined as the number of homicides among pregnant or postpartum women divided by the number of live births in states and years included in this analysis, available from annual natality data reported by the Centers for Disease Control and Prevention.21 Likewise, pregnancy-associated suicide ratios were the number of suicides among pregnant or postpartum women divided by the number of live births from states and years included in this analysis. Given documented underreporting of pregnancy status on death records,22 we acknowledge that these mortality ratios are underestimates of the true rates of homicide and suicide in the peripartum period; however, their purpose is to illustrate the difference in risk across maternal demographic characteristics. Therefore we present rate ratios (and 95% confidence intervals [CI]) for pregnancy-associated homicide and suicide by demographic characteristic rather than absolute rates.
Statistical Analysis
In order to determine whether pregnancy and postpartum represents a time of increased risk for violent death, including homicide and suicide, we estimated relative risks and 95% confidence intervals comparing pregnant/postpartum cases to non-pregnant/non-postpartum cases with consideration for potential misclassification of pregnancy status. The quality of death certification is largely determined by the care taken by the cause of death certifier to properly document the causes and circumstances of death. As such, ascertainment and reporting of pregnancy status is likely to vary across states. Fildes et al. reviewed medical examiner records from 1986–1989 in Cook County, IL and found that 65% of the deaths to women who were pregnant or postpartum were not identified as such on the death record.8 More recently, Horon and Cheng22 quantified the underreporting of pregnancy/postpartum status on death certificates from 2001–2008 in Maryland. It is important to note that the Maryland Department of Health and Mental Hygiene implemented enhanced surveillance of pregnancy-associated death on death records beginning in 2001, and the Maryland Maternal Mortality Review Committee – established in 2000 – performs a detailed case review, including review of medical examiner records and linkage of the women’s death certificates with birth and fetal death certificates from the prior year to enhance the accuracy of reporting.23 After rigorous case ascertainment through linkage of death records with medical examiner records, live birth and fetal death records, they reported that more than half (53.3%) of all pregnancy-associated deaths due to non-obstetric causes were not recorded in the death record.
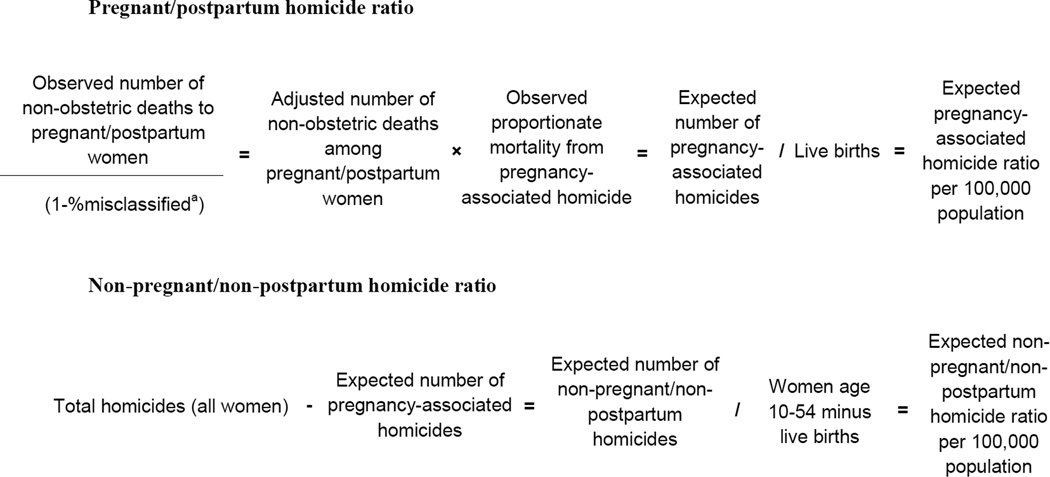
Therefore, we compared risk of homicide and suicide between pregnant/postpartum women and non-pregnant/non-postpartum women across potential misclassification scenarios ranging from unadjusted (0% misclassification) to the highest published reported rate of misclassification (65%). Figure 1 is a schematic of this procedure for homicide. We applied the same methodology in estimating suicide risk. First, we identified the observed number of deaths due to non-obstetric causes among women reported as pregnant/postpartum. The number of misclassified deaths was estimated by dividing the observed number of non-obstetric deaths among pregnant/postpartum women by 1 minus the percent misclassified in each scenario: 0%, 25%, 53%, and 65%. The estimated number of misclassified deaths was added to the total observed number of non-obstetric deaths in pregnant/postpartum women for an adjusted total. The adjusted total was multiplied by the observed proportionate mortality from homicide or suicide to derive an expected number of pregnancy-associated homicides and suicides. The expected number of homicides or suicides among non-pregnant/non-postpartum women was derived by subtracting the expected number among pregnant/postpartum women from the total homicides or suicides observed in the data. Pregnancy-associated homicide and suicide ratios were estimated by dividing the expected number of pregnancy-associated homicides and suicides by the total number of live births in states and years included in the analysis (n=16,750,431).21 We divided the expected number of homicides or suicides in non-pregnant/non-postpartum women by the number of women age 10–54 (total female population age 10–54 minus live births in states and years included in analysis, n=351,178,576).23 For ease of presentation, we refer to both the ratios as per 100,000 population. Finally, we divided the ratio of homicide or suicide among pregnant/postpartum women by the corresponding ratio among non-pregnant/non-postpartum women and calculated 95% CI in order to identify significant differences in risk between the two groups at each level of potential misclassification.
Figure 1.
Procedure for estimating homicide ratios with adjustment for misclassification.
a Potential percents misclassified tested include 0%, 25%, 53%, and 65%.
To explore whether differences in age distribution between pregnant/postpartum and non-pregnant/non-postpartum decedents explained differences in homicide and suicide risk, we calculated age-adjusted mortality ratios for comparison by direct standardization using the age-specific crude rates of homicide and suicide (i.e. without adjustment for pregnancy misclassification) among pregnant and non-pregnant women separately by age groups <20, 20–24, 25–2930–34,35–40, and ≥40. Age-specific mortality rates from both pregnant/postpartum and non-pregnant/non-postpartum groups were applied to the 2000 US Standard Population25 in order to calculate overall age-adjusted mortality ratios. It is important to note that age-adjusted ratios are intended for comparison only. Their values do not represent actual magnitude.
Results
There were 737,601 deaths of women aged 10–54 in the US from 2005–2010, and 465,097 (63.1%) occurred in jurisdictions and years included in this analysis. Over one third of the 465,097 deaths indicated a pregnancy status of unknown (n=164,314; 35.3%) or not applicable (n=16,006; 3.4%). Just over 40% of the not applicable women were in the oldest age group (age 50–54) and 80% were over age 40, suggesting a possible age-related medical reason for non-applicability (hysterectomy, for example). Of the remaining 284,777 women, the vast majority were marked as not pregnant at the time of death or within the year preceding (n=278,849, 97.9%). We identified 5,928 women who died during pregnancy or within 1 year in states and years included in this analysis, including 259 women with unknown status that were reclassified based on pregnancy-associated ICD-10 codes for underlying cause of death. Among 364,994 records from the 37 states with detailed temporality on death certificates, we identified 1,858 (0.5%) women who died while pregnant, 1,225 (0.3%) within 42 days, and 1,466 (0.4%) in late postpartum.
Proportionate mortality
A majority of deaths for all women were due to natural causes, including both obstetric and other non-obstetric conditions and diseases (Table 2). Homicide was the third most frequent cause of death overall among pregnant women with 190 cases over the 6-year period identifiable in these data, behind natural causes (n=1,150) and injuries (n=430, transport-related and other injuries combined). Homicide accounted for 10.2% of mortality in pregnancy compared to 2.1% of mortality among non-pregnant women, 2.1% and 4.6% among early and late postpartum women. Suicide was the third most frequent cause of death among both early and late postpartum women behind natural causes and injuries. There were 70 women who died by suicide while pregnant, 32 in early postpartum, and 102 among late postpartum women, the group with the highest proportion of deaths attributable to suicide (7.0%) across the four groups.
Table 2.
| Not pregnant/not postpartum/ unknown (n=335,123) |
Pregnant (n=1,858) |
Early postpartum (n=1,225) |
Late postpartum (n=1,466) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Agec | |||||||||
| ≥35 | 275,464 | 82.2 | 638 | 34.3 | 405 | 33.1 | 452 | 30.8 | |
| 30 – 34 years | 19,086 | 5.7 | 287 | 15.5 | 256 | 20.9 | 255 | 17.4 | |
| 25 – 29 years | 15,223 | 4.5 | 359 | 19.3 | 264 | 21.6 | 316 | 21.6 | |
| 20 – 24 years | 12,665 | 3.8 | 379 | 20.4 | 230 | 18.8 | 327 | 22.3 | |
| <20 | 12,685 | 3.8 | 195 | 10.5 | 70 | 5.7 | 116 | 7.9 | |
| Racec | |||||||||
| Non-Hispanic White | 218,148 | 65.1 | 898 | 48.3 | 568 | 46.4 | 882 | 60.2 | |
| Non-Hispanic Black | 73,781 | 22.0 | 534 | 29.2 | 393 | 32.1 | 284 | 19.4 | |
| Hispanic | 31,409 | 9.4 | 326 | 17.6 | 194 | 15.8 | 210 | 13.3 | |
| Other | 11,785 | 3.7 | 91 | 4.8 | 70 | 5.7 | 90 | 6.1 | |
| Educationc | |||||||||
| Greater than high school |
119,792 | 35.8 | 643 | 34.6 | 477 | 38.9 | 514 | 35.1 | |
| High school graduate or GED |
132,364 | 39.5 | 706 | 38.0 | 477 | 38.9 | 576 | 39.3 | |
| Less than high school | 66,462 | 19.8 | 461 | 24.8 | 238 | 19.4 | 353 | 24.1 | |
| Marital Statusc | |||||||||
| Married | 135,264 | 40.4 | 698 | 37.6 | 573 | 46.8 | 674 | 46.0 | |
| Not marriedd | 189,668 | 56.6 | 1,139 | 61.3 | 636 | 51.9 | 782 | 53.3 | |
| Cause of deathc | |||||||||
| Naturale | 258,707 | 77.2 | 1,150 | 61.9 | 1,018 | 83.1 | 925 | 63.1 | |
| Transport injury | 20,766 | 6.2 | 323 | 17.4 | 53 | 4.3 | 181 | 12.4 | |
| Other injuryf | 28,695 | 8.6 | 107 | 5.8 | 75 | 6.1 | 161 | 11.0 | |
| Homicide | 7,160 | 2.1 | 190 | 10.2 | 26 | 2.1 | 68 | 4.6 | |
| Suicide | 14,489 | 4.3 | 70 | 3.8 | 32 | 2.6 | 102 | 7.0 | |
| Other external causeg | 5,306 | 1.6 | 18 | 1.0 | 21 | 1.7 | 29 | 2.0 | |
Limited to states and years with detailed temporal pregnancy information on death records (see Table 1).
Proportions do not sum to 100 where data are unknown or missing.
Chi-square P<0.001
Not married includes women who were single, divorced, or widowed.
Natural includes diseases and conditions related and unrelated to pregnancy, childbirth, or the puerperium. Refer to Table 2 for specific ICD-10 codes.
Other injuries include falls; accidental poisoning by and exposure to noxious substances; drowning and other threats to breathing; exposure to inanimate mechanical forces; electrical currents, smoke and fire; forces of nature; and other unspecified. Refer to eTable 2 for specific ICD-10 codes.
Other external causes of death include events of undetermined intent (poisoning, drowning, firearm, fire, and other unspecified), legal intervention, and complications of medical and surgical care. Refer to eTable2 for specific ICD-10 codes.
Pregnancy-associated homicide
There were a total of 364 pregnancy-associated homicides reported in the death records that captured pregnancy status in the previous 12 months. The majority (56.3%) were firearm-related. Adolescents were at highest risk for pregnancy-associated homicide compared to women of any other age group (Table 3) with a greater than two-fold increase compared to women over age 35. Pregnancy-associated homicide was over 3 times more likely to occur in non-Hispanic Black women compared to non-Hispanic Whites. Education was inversely related to homicide risk such that all women with at least some higher education were at lower risk relative to women with a high school education or less among those who died at age 20 and older. Finally, risk of pregnancy-associated homicide among unmarried women was more than five times the risk in married women.
Table 3.
Rate ratios (RR) and 95% confidence intervals (CI) for pregnancy-associated homicide and pregnancy-associated suicide by selected demographic characteristics.
| Live birthsa |
Pregnancy-associated homicide |
Pregnancy-associated suicide |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | RR | 95% | CI | N | % | RR | 95% | CI | ||
| Age | |||||||||||||
| ≥35 | 2,481,833 | 14.8% | 45 | 12.4% | Ref | 53 | 20.2% | Ref | |||||
| 30–34 | 3,887,668 | 23.2% | 46 | 12.6% | 0.65 | 0.43 | 0.98 | 45 | 17.1% | 0.54 | 0.36 | 0.81 | |
| 25–29 | 4,675,226 | 27.9% | 92 | 25.3% | 1.09 | 0.76 | 1.55 | 66 | 25.1% | 0.66 | 0.46 | 0.95 | |
| 20–24 | 4,054,251 | 24.2% | 111 | 30.5% | 1.51 | 1.07 | 2.14 | 71 | 27.0% | 0.82 | 0.57 | 1.17 | |
| < 20 | 1,651,453 | 9.9% | 70 | 19.2% | 2.34 | 1.61 | 3.40 | 28 | 10.6% | 0.79 | 0.50 | 1.26 | |
| Race | |||||||||||||
| Non-Hispanic White | 8,386,423 | 50.1% | 146 | 40.1% | Ref | 166 | 63.1% | Ref | |||||
| Non-Hispanic Black | 2,167,903 | 12.9% | 125 | 34.3% | 3.31 | 2.61 | 4.21 | 21 | 8.0% | 0.49 | 0.31 | 0.77 | |
| Hispanic | 4,853,021 | 29.0% | 87 | 23.9% | 1.03 | 0.79 | 1.34 | 46 | 17.5% | 0.48 | 0.35 | 0.66 | |
| Other | 1,343,084 | 8.0% | 6 | 1.6% | 0.26 | 0.11 | 0.58 | 27 | 10.3% | 1.02 | 0.68 | 1.53 | |
| Educationb | |||||||||||||
| Greater than high school | 5,738,796 | 56.1% | 84 | 29.0% | Ref | 115 | 50.2% | Ref | |||||
| High school graduate or | |||||||||||||
| GED | 2,685,940 | 26.2% | 121 | 41.7% | 3.08 | 2.33 | 4.07 | 74 | 32.3% | 1.37 | 1.03 | 1.84 | |
| Less than high school | 1,808,410 | 17.7% | 85 | 29.3% | 3.21 | 2.38 | 4.34 | 40 | 17.5% | 1.10 | 0.77 | 1.58 | |
| Marital Status | |||||||||||||
| Married | 10126699 | 60.5% | 78 | 21.4% | Ref | 108 | 41.1% | Ref | |||||
| Not marriedc | 6623732 | 39.5% | 284 | 78.0% | 5.57 | 4.33 | 7.15 | 153 | 58.2% | 2.17 | 1.69 | 2.77 | |
Total number of live births in states and years with temporal pregnancy information on death records (Table 1).
Stratification by education restricted to women age 20 and older.
Not married includes women who are single, divorced, or widowed.
Pregnancy-associated suicide
There were 263 pregnancy-associated suicides reported in the records that captured pregnancy status in the previous 12 months. Older women were at greater risk for pregnancy-associated suicide (Table 3). Pregnancy-associated suicide was less likely to occur in non-Hispanic Black and Hispanic women compared to non-Hispanic Whites and more likely to occur in unmarried women.
Risk of homicide in pregnant/post-partum vs. non-pregnant/non-postpartum population
Given the large number of homicides among non-pregnant/non-postpartum women, adjustment for various levels of pregnancy misclassification did little to change the magnitude of the estimated homicide ratio in this group which was between 2.5 and 2.6 per 100,000 population (Table 4). However, pregnancy-associated homicide estimates ranged from the unadjusted estimate of 2.2 per 100,000 to 6.2 per 100,000 under the largest estimate of misclassification. Relative risk and 95% CI estimates across the potential misclassification scenarios indicated significantly increased risk for homicide in the peripartum period. After adjustment for the lowest published degree of misclassification (53%), the risk of homicide among pregnant/postpartum women was 1.84 times that of non-pregnant/non-postpartum women (95% CI: 1.71, 1.98). Assuming an even more conservative estimate of misclassification (25%) pregnant/postpartum women still experienced a 11% increase in homicide risk (95% CI: 1.01, 1.21).
Table 4.
Homicide and Suicide among pregnant/postpartum women and non-pregnant/non-postpartum women by potential degrees of misclassification.
| % Misclassification assumption |
Number of non- obstetric related deaths |
Number of Homicides |
Homicides per 100,000 population |
RR (95% CI) | Number of Suicides |
Suicides per 100,000 population |
RR (95% CI) | |
|---|---|---|---|---|---|---|---|---|
| 0% (unadjusted) | ||||||||
| Pregnant/postpartum | 2,346 | 364 | 2.2 | 0.82 (0.74, 0.91) | 263 | 1.6 | 0.29 (0.25, 0.32) | |
| Non-pregnant/non-postpartum | 443,163 | 9,443 | 2.6 | Ref | 19,486 | 5.5 | ||
|
Expected Number of Homicidesa |
Expected Number of Suicidesb |
|||||||
| 25% | Pregnant/postpartum | 3,128 | 485 | 2.9 | 1.11 (1.01, 1.21) | 351 | 2.1 | 0.38 (0.35, 0.43) |
| Non-pregnant/non-postpartum | 442,381 | 9,322 | 2.6 | Ref | 19,398 | 5.4 | Ref | |
| 53% c | ||||||||
| Pregnant/postpartum | 5,024 | 779 | 4.7 | 1.84 (1.71, 1.98) | 563 | 3.4 | 0.62 (0.57, 0.68) | |
| Non-pregnant/non-postpartum | 440,485 | 9,028 | 2.5 | Ref | 19,186 | 5.4 | Ref | |
| 65% d | ||||||||
| Pregnant/postpartum | 6,703 | 1,040 | 6.2 | 2.53 (2.37, 2.69) | 751 | 4.5 | 0.84 (0.78, 0.91) | |
| Non-pregnant/non-postpartum | 438,806 | 8,767 | 2.5 | Ref | 18,998 | 5.3 | Ref |
Based on the proportion of non-obstetric deaths due to homicide observed in the data among women reported as pregnant/postpartum (15.5%) and not pregnant/unknown (2.1%).
Based on the proportion of non-obstetric deaths due to suicide observed in the data among women reported as pregnant/postpartum (11.2%) and not pregnant/unknown (4.4%)
Horon and Cheng 2011.22
Fildes et al. 1992.8
Risk of suicide in pregnant/postpartum vs. non-pregnant/non-postpartum population
As with homicide, the suicide ratio per 100,000 population among non-pregnant/non-postpartum women was relatively unchanged across each level of potential pregnancy misclassification from 5.3 to 5.5 (Table 4). Pregnancy-associated suicide ratios ranged from 1.6 in the crude estimate to 4.5 after accounting for misclassification, yielding significantly lower risk estimates relative to non-pregnant/non-postpartum women across all misclassification scenarios. Assuming 25% misclassification suggested a 62% decreased risk during the peripartum period (RR=0.38 95% CI: 00.35, 0.43).
Age-adjusted mortality rates
Comparison of age-adjusted homicide mortality ratios was consistent with the previous findings. The age-adjusted homicide ratio was higher among women in the peripartum period (2.9 per 100,000 population vs. 2.7 per 100,000 population among non-pregnant/non-postpartum women) even without adjustment for pregnancy misclassification. The age-adjusted pregnancy-associated suicide ratio was lower relative to suicide among non-pregnant/non-postpartum women (2.8 per 100,000 population vs. 5.5 per 100,000 population, respectively).
Comment
Suicide and homicide are substantial contributors to mortality among young women of reproductive age in the US representing the fourth and fifth leading causes of death.26 In this first analysis of death records since the implementation of enhanced surveillance provided by the 2003 revision, young women, non-Hispanic Black women, and undereducated women were at greatest risk of pregnancy-associated homicide, while pregnancy-associated suicide was more likely to occur in older and non-Hispanic White women. This is reflective of trends in homicide and suicide victimization in the general population. 27,28 In addition, we find evidence to suggest that the risk for homicide may be elevated during pregnancy and postpartum while risk for suicide is decreased. Differences in age-distributions between the two populations did not explain these findings, which were robust to misclassification assumptions half the most conservative published estimates.
These results add to the sparse literature aiming to shed light on violent causes of death in and around pregnancy. After adjustments, our estimated rates of pregnancy-associated homicide (2.9–6.2 per 100,000 population) are higher than the 1.7 per 100,000 live births reported by the Pregnancy Mortality Surveillance System (PMSS) from 1991–1999.29 This discrepancy may be due to enhanced case ascertainment since the 1990s (the PMSS data were based on death records and, in some but not all cases, linked live birth or fetal death records). Other studies on pregnancy-associated homicide have reported rates per 100,000 ranging from 8.6 in Tennessee from 1989 to 1991 (postpartum only),6 9.3 in Maryland 1993–2008,4 2.9 in North Carolina from 2004–2006,30 and 2.9 in 17 states participating in the National Violent Death Reporting System (NVDRS) from 2003–2007 (SC, GA, NC, VA, NJ, MD, AK, MA, OR, CO, OK, RI, WI, CA, KT, NM, UT).31 Although we find similar rates of pregnancy-associated homicide, Samandari et al.30 concluded that the risk of homicide was decreased among pregnant/postpartum women in North Carolina based on a homicide rate of 4.9 per 100,000 in the referent non-pregnant/non-postpartum population. This estimate is notably higher than the national rate among all women reported by the Centers for Disease Control and Prevention, National Center for Injury Prevention and Control from 2005–2010 (2.9 per 100,000),26 as well as our estimated range of 2.5–2.6 among the 37 states included in this analysis.
Fewer studies have examined the rates of pregnancy-associated suicide and report rates per 100,000 that fall within our estimated range of 2.1–4.5, including 3.2 in Tennessee from 1989 to 1991 (postpartum only),6 2.8 in North Carolina from 2004–2006,30 and 2.0 in NVDRS states.31 Where comparisons were available, sparse evidence suggests that pregnant/postpartum women may be at the same or lower risk for suicide compared to non-pregnant/non-postpartum women, consistent with our finding.30, 32 Given the disproportionate burden of suicide among late postpartum women in particular, there may be important heterogeneity that is masked by calculating pregnancy-associated risk as defined (pregnant and postpartum combined).33 The acute increase in depression that occurs postpartum – which may in turn exacerbate thoughts of self-harm34 – warrants a closer examination of suicide risk in postpartum women.
Our biggest limitation is the quality and completeness of the data. Among the 37 jurisdictions included, a significant proportion of records were marked unknown data despite the presence of temporal pregnancy items. We therefore rely on published data to support assumptions of misclassification in order to estimate rates and compare risks. Grouping the unknown pregnancy status women with non-pregnant/non-postpartum women is reasonable given the magnitude of this group. It is also a conservative approach as the unknown group had higher rates of homicide and suicide compared to non-pregnant/non-postpartum and therefore would attenuate risk compared to pregnant/postpartum women.
Further, although this analysis includes a majority of US states, our estimated mortality ratios may not reflect the national rates of pregnancy-associated homicide and suicide. However, the 2005–2010 homicide and suicide ratios among all women age 10–54 were similar between the 14 states excluded from analysis and those included (homicide ratios: 3.0 per 100,000 population in excluded states, 2.9 per 100,000 in included states; suicide ratios 6.1 per 100,000 in excluded states vs. 5.7 per 100,000 in included).
While sources such as the PMSS and NVDRS offer additional evidence on violent death during pregnancy, they are either not nationally-representative (NVDRS) or lack adequate information to draw comparisons between pregnant/postpartum and other women of reproductive age (both). Death certificates can overcome these deficiencies as states continue efforts to improve ascertainment of pregnancy status.
It is impossible to determine if pregnancy-associated violent deaths would not have occurred in the absence of pregnancy; however, the significant role intimate partner violence and conflict plays in many cases of pregnancy-associated homicide and suicide4,31, 35–39, suggests that pregnancy may be an additional stressor in already vulnerable circumstances,39 or that these deaths may be the conclusion of a cycle of physical and sexual abuse that ends during pregnancy.37 What is clear is that pregnancy may be a potentially important window of opportunity to identify women who are at risk for homicide and suicide, especially those who might not otherwise be in contact with health care and social services. Screening and counseling for interpersonal and domestic violence are among the suite of women’s preventative services recommended by the Institute of Medicine for inclusion in insurance coverage mandates under provisions of the Patient Protection and Affordable Care Act of 2010.40 With mandatory coverage and zero cost-sharing now in effect, a significant barrier to care has been removed and physicians should be encouraged to screen and refer women to local agencies specializing in violence prevention. The American College of Obstetricians and Gynecologists has published suggested practices for violence screening among women in obstetric care – including sample screening questions and strategies for performing culturally-relevant, non-judgmental routine assessments.41 While homicide and suicide events during pregnancy and postpartum are rare, enhanced identification and surveillance may raise awareness among providers of these potentially preventable deaths.
Supplementary Material
Acknowledgments
Source of Funding: This work was supported in part by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, as well as the National Center for Health Statistics, Centers for Disease Control and Prevention.
Role of the funder:
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the National Center for Health Statistics, Centers for Disease Control and Prevention. The study sponsor has no direct role in the study design; collection, analysis and interpretation of data; or in the writing of the report. All manuscripts undergo Institute and CDC clearance before submission. The corresponding author has full access to the data and the final responsibility of the decision to submit the work for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors report no conflicts of interest.
References
- 1.Guyer B, Freedman MA, Strobino DM, Sondik EJ. Annual summary of vital statistics: Trends in the health of Americans during the 20th century. Pediatrics. 2000 Dec;106(6):1307–1317. doi: 10.1542/peds.106.6.1307. [DOI] [PubMed] [Google Scholar]
- 2.Martin SL, Mackie L, Kupper LL, Buescher PA, Moracco KE. Physical abuse of women before, during, and after pregnancy. JAMA. 2001 Mar 28;285(12):1581–1584. doi: 10.1001/jama.285.12.1581. [DOI] [PubMed] [Google Scholar]
- 3.Saltzman LE, Johnson CH, Gilbert BC, Goodwin MM. Physical abuse around the time of pregnancy: An examination of prevalence and risk factors in 16 states. Matern Child Health J. 2003 Mar;7(1):31–43. doi: 10.1023/a:1022589501039. [DOI] [PubMed] [Google Scholar]
- 4.Cheng D, Horon IL. Intimate-partner homicide among pregnant and postpartum women. Obstet Gynecol. 2010 Jun;115(6):1181–1186. doi: 10.1097/AOG.0b013e3181de0194. [DOI] [PubMed] [Google Scholar]
- 5.Atrash HK, Rowley D, Hogue CJ. Maternal and perinatal mortality. Curr Opin Obstet Gynecol. 1992 Feb;4(1):61–71. [PubMed] [Google Scholar]
- 6.Jocums SB, Berg CJ, Entman SS, Mitchell EF., Jr Postdelivery mortality in Tennessee, 1989–1991. Obstet Gynecol. 1998 May;91(5 Pt 1):766–770. doi: 10.1016/s0029-7844(98)00063-5. [DOI] [PubMed] [Google Scholar]
- 7.Dannenberg AL, Carter DM, Lawson HW, Ashton DM, Dorfman SF, Graham EH. Homicide and other injuries as causes of maternal death in New York City, 1987 through 1991. Am J Obstet Gynecol. 1995 May;172(5):1557–1564. doi: 10.1016/0002-9378(95)90496-4. [DOI] [PubMed] [Google Scholar]
- 8.Fildes J, Reed L, Jones N, Martin M, Barrett J. Trauma: The leading cause of maternal death. J Trauma. 1992 May;32(5):643–645. [PubMed] [Google Scholar]
- 9.Harper M, Parsons L. Maternal deaths due to homicide and other injuries in North Carolina: 1992–1994. Obstet Gynecol. 1997 Dec;90(6):920–923. doi: 10.1016/s0029-7844(97)00485-7. [DOI] [PubMed] [Google Scholar]
- 10.Ho EM, Brown J, Graves W, Lindsay MK. Maternal death at an inner-city hospital, 1949–2000. Am J Obstet Gynecol. 2002 Nov;187(5):1213–1216. doi: 10.1067/mob.2002.127136. [DOI] [PubMed] [Google Scholar]
- 11.Krulewitch CJ, Pierre-Louis ML, de Leon-Gomez R, Guy R, Green R. Hidden from view: Violent deaths among pregnant women in the District of Columbia, 1988–1996. J Midwifery Womens Health. 2001 Jan-Feb;46(1):4–10. doi: 10.1016/s1526-9523(00)00096-9. [DOI] [PubMed] [Google Scholar]
- 12.Nannini A, Weiss J, Goldstein R, Fogerty S. Pregnancy-associated mortality at the end of the twentieth century: Massachusetts, 1990–1999. J Am Med Womens Assoc. 2002 Summer;57(3):140–143. [PubMed] [Google Scholar]
- 13.Dietz PM, Rochat RW, Thompson BL, Berg CJ, Griffin GW. Differences in the risk of homicide and other fatal injuries between postpartum women and other women of childbearing age: Implications for prevention. Am J Public Health. 1998 Apr;88(4):641–643. doi: 10.2105/ajph.88.4.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horon IL, Cheng D. Enhanced surveillance for pregnancy-associated mortality--Maryland, 1993–1998. JAMA. 2001 Mar 21;285(11):1455–1459. doi: 10.1001/jama.285.11.1455. [DOI] [PubMed] [Google Scholar]
- 15.Hoyert DL. Maternal mortality and related concepts. Vital Health Stat 3. 2007 Feb;(33):1–13. [PubMed] [Google Scholar]
- 16.Davis GG, Onaka AT. Report on the 2003 revision of the U.S. Standard Certificate of Death. Am J Forensic Med Pathol. 2001 Mar;22(1):38–42. doi: 10.1097/00000433-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Mac KAP, Berg CJ, Liu X, Duran C, Hoyert DL. Changes in pregnancy mortality ascertainment: United States, 1999–2005. Obstet Gynecol. 2011 Jul;118(1):104–110. doi: 10.1097/AOG.0b013e31821fd49d. [DOI] [PubMed] [Google Scholar]
- 18.Dye TD, Gordon H, Held B, Tolliver NJ, Holmes AP. Retrospective maternal mortality case ascertainment in west Virginia, 1985 to 1989. Am J Obstet Gynecol. 1992 Jul;167(1):72–76. doi: 10.1016/s0002-9378(11)91629-9. [DOI] [PubMed] [Google Scholar]
- 19.Pregnancy-related mortality--Georgia, 1990–1992. MMWR Morb Mortal Wkly Rep. 1995 Feb 10;44(5):93–96. [PubMed] [Google Scholar]
- 20.Horon IL. Underreporting of maternal deaths on death certificates and the magnitude of the problem of maternal mortality. Am J Public Health. 2005 Mar;95(3):478–482. doi: 10.2105/AJPH.2004.040063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. [Accessed September 26, 2014];Vitalstats: Births. Available at http://www.cdc.gov/nchs/data_access/vitalstats/VitalStats_Births.htm.
- 22.Horon IL, Cheng D. Effectiveness of pregnancy check boxes on death certificates in identifying pregnancy-associated mortality. Public Health Rep. 2011 Mar-Apr;126(2):195–200. doi: 10.1177/003335491112600210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maryland Department of Health and Mental Hygiene. [Accessed February 20, 2016];State Maternal Mortality Review (MMR) Program. http://phpa.dhmh.maryland.gov/mch/Pages/mmr.aspx.
- 24.United States Census Bureau. [Accessed September 15, 2014];American FactFinder. B01001: Sex by age. 2005–2010 American Community Survey [online] http://www.census.gov/acs/www/
- 25.Surveillance, Epidemiology and End Results Program (SEER) [Accessed April 29, 2015];Standard populations - single ages. 2000 US standard population. http://seer.cancer.gov/stdpopulations/stdpop.singleages.html.
- 26.Centers for Disease Control and Prevention. [Accessed June 22, 2015];Web-based inquiry statistics query and reporting system (WISARS) [online] http://webappa.cdc.gov/sasweb/ncipc/mortrate10_us.html.
- 27.Cooper A, Smith EL. Homicide Trends in the United States, 1980–2008. United States Bureau of Justice Statistics, US Department of Justice; [Accessed April 29, 2015]. http://www.bjs.gov/content/pub/pdf/htus8008.pdf. [Google Scholar]
- 28.American Foundation for Suicide Prevention. [Accessed April 20, 2015];Facts and Figures. https://www.afsp.org/understanding-suicide/facts-and-figures.
- 29.Chang J, Berg CJ, Saltzman LE, Herndon J. Homicide: A leading cause of injury deaths among pregnant and postpartum women in the United States, 1991–1999. Am J Public Health. 2005 Mar;95(3):471–477. doi: 10.2105/AJPH.2003.029868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Samandari G, Martin SL, Kupper LL, Schiro S, Norwood T, Avery M. Are pregnant and postpartum women: At increased risk for violent death? Suicide and homicide findings from North Carolina. Matern Child Health J. 2011 Jul;15(5):660–669. doi: 10.1007/s10995-010-0623-6. [DOI] [PubMed] [Google Scholar]
- 31.Palladino CL, Singh V, Campbell J, Flynn H, Gold KJ. Homicide and suicide during the perinatal period: Findings from the National Violent Death Reporting System. Obstet Gynecol. 2011 Nov;118(5):1056–1063. doi: 10.1097/AOG.0b013e31823294da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marzuk PM, Tardiff K, Leon AC, et al. Lower risk of suicide during pregnancy. Am J Psychiatry. 1997 Jan;154(1):122–123. doi: 10.1176/ajp.154.1.122. [DOI] [PubMed] [Google Scholar]
- 33.Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005 Jun;8(2):77–87. doi: 10.1007/s00737-005-0080-1. [DOI] [PubMed] [Google Scholar]
- 34.Wisner KL, Sit DK, McShea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013 May;70(5):490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McFarlane J, Campbell JC, Sharps P, Watson K. Abuse during pregnancy and femicide: Urgent implications for women's health. Obstet Gynecol. 2002 Jul;100(1):27–36. doi: 10.1016/s0029-7844(02)02054-9. [DOI] [PubMed] [Google Scholar]
- 36.Martin SL, Macy RJ, Sullivan K, Magee ML. Pregnancy-associated violent deaths: The role of intimate partner violence. Trauma Violence Abuse. 2007 Apr;8(2):135–148. doi: 10.1177/1524838007301223. [DOI] [PubMed] [Google Scholar]
- 37.Krulewitch CJ, Roberts DW, Thompson LS. Adolescent pregnancy and homicide: Findings from the Maryland office of the chief medical examiner, 1994–1998. Child Maltreat. 2003 May;8(2):122–128. doi: 10.1177/1077559502250829. [DOI] [PubMed] [Google Scholar]
- 38.Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Blasco-Ros C, Echeburua E, Martinez M. The impact of physical, psychological, and sexual intimate male partner violence on women's mental health: Depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. J Womens Health (Larchmt) 2006 Jun;15(5):599–611. doi: 10.1089/jwh.2006.15.599. [DOI] [PubMed] [Google Scholar]
- 39.Stark E, Flitcraft A. Killing the beast within: Woman battering and female suicidality. Int J Health Serv. 1995;25(1):43–64. doi: 10.2190/H6V6-YP3K-QWK1-MK5D. [DOI] [PubMed] [Google Scholar]
- 40.Institute of Medicine. Clinical preventive services for women: closing the gaps. Washington, DC: National Academies Press; 2011. Jul, [Accessed February 20, 2016]. https://iom.nationalacademies.org/~/media/Files/Report%20Files/2011/Clinical-Preventive-Services-for-Women-Closing-the-Gaps/preventiveservicesforwomenreportbrief_updated2.pdf. [Google Scholar]
- 41.The American College of Obstetricians and Gynecologists Committee Opinion No. 518: Intimate Partner Violence. Obstet Gynecol. 2012;119(2 Pt 1):412–417. doi: 10.1097/AOG.0b013e318249ff74. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.