Whole body (WB) magnetic resonance imaging (MRI) is now recommended for all patients suspected of having smoldering or symptomatic myeloma. Diffusion-weighted (DW)-MRI is a highly sensitive sequence for lesion detection in bone marrow and soft tissues. Incidental findings are inevitable, and a potential trigger for costly, and sometimes invasive, investigations and anxiety. This study aims to determine the incidence of incidental findings and the potential clinical impact. A total of 70 incidental findings were identified in 175 examinations in 48 patients. Fourteen of the 70 (20%) incidental findings were equivocal. In 8 of 14 cases, the initial management was clinical correlation or review of previous imaging, and only 3% of WB DW-MRI (5 of 175) scans demonstrated an equivocal incidental finding which required further investigation as the initial action.
The recent consensus statement from the International Myeloma Working Group has recommended WB-MRI for all patients suspected of having smoldering myeloma and those patients with a solitary bone plasmacytoma.1 The speed, coverage and high sensitivity of WB DW-MRI, with its ability to quantify both the burden of disease and response to treatment, has made it the sequence of choice at several leading centers worldwide.2
DW-MRI is the most sensitive sequence for lesion detection in bone marrow3 and it is also highly sensitive in soft tissues.3,4 Incidental findings are, therefore, inevitable, and a potential trigger for costly and sometimes invasive investigation and a source of anxiety for patients and clinicians. To date there have been no dedicated studies looking at incidental findings in WB DW-MRI studies in patients with myeloma. This study aims to determine the incidence of incidental findings and extramedullary disease in WB DW-MRI studies performed in patients with multiple myeloma. The study was approved by the local Institutional Review Board.
All WB DW-MRI scans performed for patients with myeloma between January 2012 and October 2014 were included. The imaging protocol included axial DW-MRI at b values of 50 and 900 s/mm2 with coverage from the skull vertex to the knees with automated ADC maps; a b 900 s/mm2 3-dimensional image of the skeleton and ‘fast’ T1weighted (W) and T2W sagittal imaging of the whole spine.2 All scans were reported by the myeloma imaging lead at our institution.
If incidental findings were identified, recommendations were documented. Incidental findings were classified into two groups; (A) equivocal (required further investigation in the form of clinical correlation and/or further imaging); and (B) non-equivocal (no further investigation required) abnormality clearly characterized by MRI. The location of extramedullary plasmacytomas was documented.
A total of 175 WB DW-MRI examinations were performed for 110 consecutive myeloma patients (68 men and 42 women; mean age 60 years, range 38–83 years). Sixty-seven of 175 (38%) examinations in 48 patients had incidental findings. Some examinations identified multiple incidental findings; therefore, a total of 70 incidental findings were documented. The majority of incidental findings were non-equivocal with 9 vertebral anomalies (e.g. hemangiomas), 18 benign visceral or pulmonary abnormalities (e.g. cysts and gallstones), and 29 other musculoskeletal or spinal abnormalities (e.g. avascular necrosis, insufficiency fractures and degenerative disease).
Only 14 of 70 (20%) of the incidental findings (n=13 individuals) were equivocal. Guidance on further management was given in the radiology report in 13 of 14 (93%) cases. In 8 of 14 (57%) cases, the initial management was clinical correlation or review of previous imaging, and only 3% of WB DW-MRI (5 of 175) scans demonstrated an equivocal incidental finding which required further investigation as the initial action. The equivocal incidental findings are summarized in Table 1. Figure 1 demonstrates examples of some equivocal and non-equivocal incidental findings. Incidental focal visceral lesions identified on DW- MRI, for example within the liver, adrenal and thyroid, were all confirmed as real but benign. This contrasts with the pulmonary findings on WB DW-MRI that were all confirmed to be artefactual. Current routine MRI sequences including DW-MRI have limited capability for imaging lung parenchyma and, therefore, pulmonary findings on WB DW-MRI may be more problematic. Such findings should be interpreted with caution, and imaging with CT or chest radiographs should be considered.
Table 1.
Equivocal incidental findings.
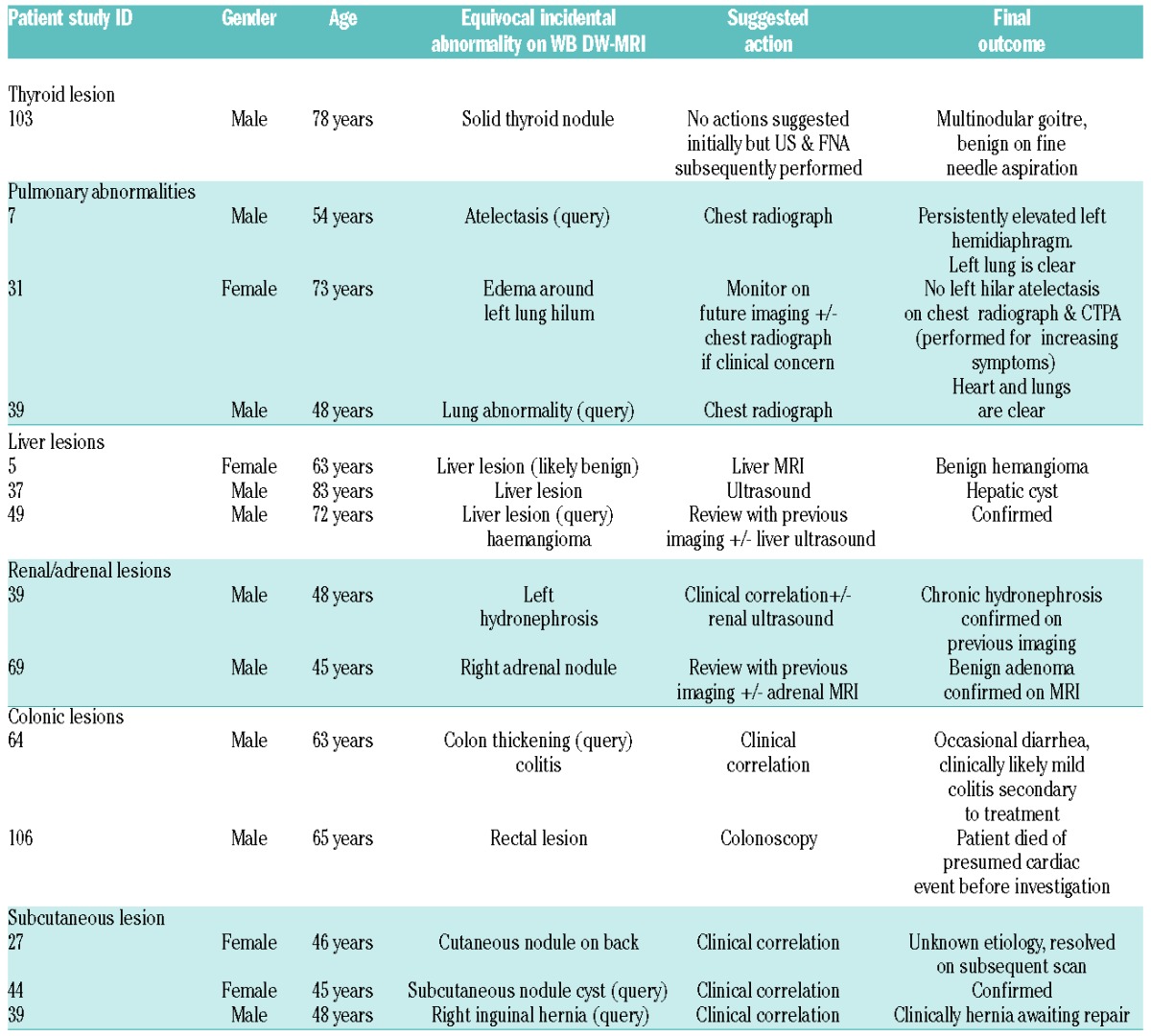
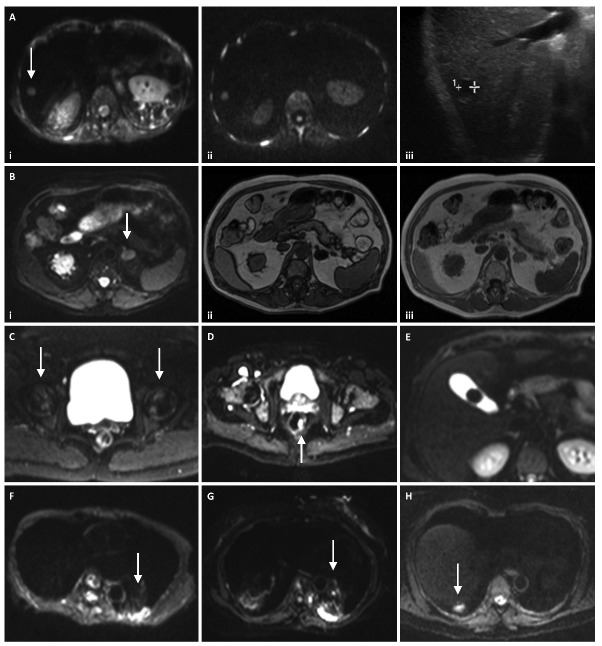
Figure 1.
Incidental findings on WB DW-MRI. (A and B) Focal lesions detected on DW-MRI which were confirmed on further imaging but which had benign features. (A) b50 DW-MRI demonstrates a small hepatic lesion (arrow) which maintained high signal at b900 (Aii) raising suspicion for a solid lesion however ultrasound (Aiii) confirms a small cyst; the high signal on high b value DW-MRI was likely T2 shine through. (Bi) b50 DW-MRI demonstrates a left adrenal nodule (arrow). Subsequent MRI showed loss of signal on out of phase MRI (Bii) compared with in phase MRI (Biii) confirming that this was most likely to be a benign fat containing adrenal adenoma. Further examples of incidental findings are shown in (C-E). (C) b50 DW-MRI demonstrates serpiginous subchondral high signal (arrows) in keeping with avascular necrosis. (D) b900 DW-MRI demonstrates a focal rectal nodule (arrow). (E) b50 DW-MRI shows a dependent well defined filling defect in the gallbladder in keeping with a gallstone. (F-H) Three cases of equivocal pulmonary findings (arrows) on DW-MRI which were proven to be artefactual on further imaging.
Nine of 110 (8%) patients (18 of 175 examinations) were found to have extramedullary plasmacytomas confirmed in all cases by response to systemic myeloma treatment at follow up. Four of these 9 patients had more than one extramedullary plasmacytoma. These were hepatic in 4 patients, intramuscular in 3 patients, retroperitoneal in 2 patients, paraverterbral in one patient, subcutaneous in one patient, peritoneal in one patient, and dural in one patient.
This is the first dedicated study recording incidental findings in WB DW-MRI examinations in patients with myeloma. In a study investigating staging in 100 patients with prostate cancer, incidental lesions were reported in 29 patients, with 3 requiring further imaging.5 Morin found that, in 43 of 148 (29.1%) healthy volunteers scanned with WB DW-MRI, at least one incidental finding was identified; 30.6% of incidental finding were classified to be of moderate significance and 10.2% of findings as high significance.6 A further smaller study of 22 healthy volunteers found 20 incidental findings in 20 participants, including a final diagnosis of malignancy in one participant.7 A study of WB DW-MRI in patients with neurofibromatosis found incidental findings in 104 of 247 (42%) patients, with significant findings in 16 of 247 (6.5%).8
Our study confirmed that incidental findings are common in WB DW-MRI examinations; however, as DW-MRI is helpful in tissue characterization, only a minority of scans (3%) resulted in equivocal incidental findings requiring further characterization, which limits the impact on patients and resources. An increasing use of whole body imaging techniques is also likely to reveal extramedullary plasmacytomas which would have been occult in the era of traditional skeletal survey alone.
Incidental findings on WB DW-MRI are not likely to be a significant source of anxiety or trigger for further imaging. However, this is dependent on the reporting radiologist clearly stating levels of concern with recommendations for further investigation where necessary. When it does occur, the incidental finding is a problem for clinicians and radiologists, and communication between them is essential.9
Footnotes
Funding: the authors acknowledge funding from CRUK and EPSRC Cancer Imaging Centre in association with the MRC and Department of Health (England), NHS funding to the NIHR Biomedicine Research Centre and Clinical Research Facility in Imaging at the Royal Marsden Hospital, Myeloma UK and The Wellcome Trust.
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Dimopoulos MA, Hillengass J, Usmani S, et al. Role of magnetic resonance imaging in the management of patients with multiple myeloma: a consensus statement. J Clin Oncol. 2015;33(6):657–664. [DOI] [PubMed] [Google Scholar]
- 2.Messiou C, Kaiser M. Whole body diffusion weighted MRI - a new view of myeloma. Br J Haematol. 2015;171(1):29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pearce T, Philip S, Brown J, Koh DM, Burn PR. Bone metastases from prostate, breast and multiple myeloma: differences in lesion conspicuity at short-tau inversion recovery and diffusion-weighted MRI. Br J Radiol. 2012;85(1016):1102–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Padhani AR, Koh DM, Collins DJ. Whole-body diffusion-weighted MR imaging in cancer: current status and research directions. Radiology. 2011;261(3):700–718. [DOI] [PubMed] [Google Scholar]
- 5.Lecouvet FE, El Mouedden J, Collette L, et al. Can whole-body magnetic resonance imaging with diffusion-weighted imaging replace Tc 99m bone scanning and computed tomography for single-step detection of metastases in patients with high-risk prostate cancer¿ Eur Urol. 2012;62(1):68–75. [DOI] [PubMed] [Google Scholar]
- 6.Morin SH, Cobbold JF, Lim AK, et al. Incidental findings in healthy control research subjects using whole-body MRI. Eur J Radiol. 2009;72(3):529–533. [DOI] [PubMed] [Google Scholar]
- 7.Tarnoki DL, Tarnoki AD, Richter A, Karlinger K, Berczi V, Pickuth D. Clinical value of whole-body magnetic resonance imaging in health screening of general adult population. Radiol Oncol. 2015;49(1):10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaremko JL, MacMahon PJ, Torriani M, et al. Whole-body MRI in neurofibromatosis: incidental findings and prevalence of scoliosis. Skeletal Radiol. 2012;41(8):917–923. [DOI] [PubMed] [Google Scholar]
- 9.Lumbreras B, Donat L, Hernandez-Aguado I. Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol. 2010;83(988):276–289. [DOI] [PMC free article] [PubMed] [Google Scholar]