Abstract
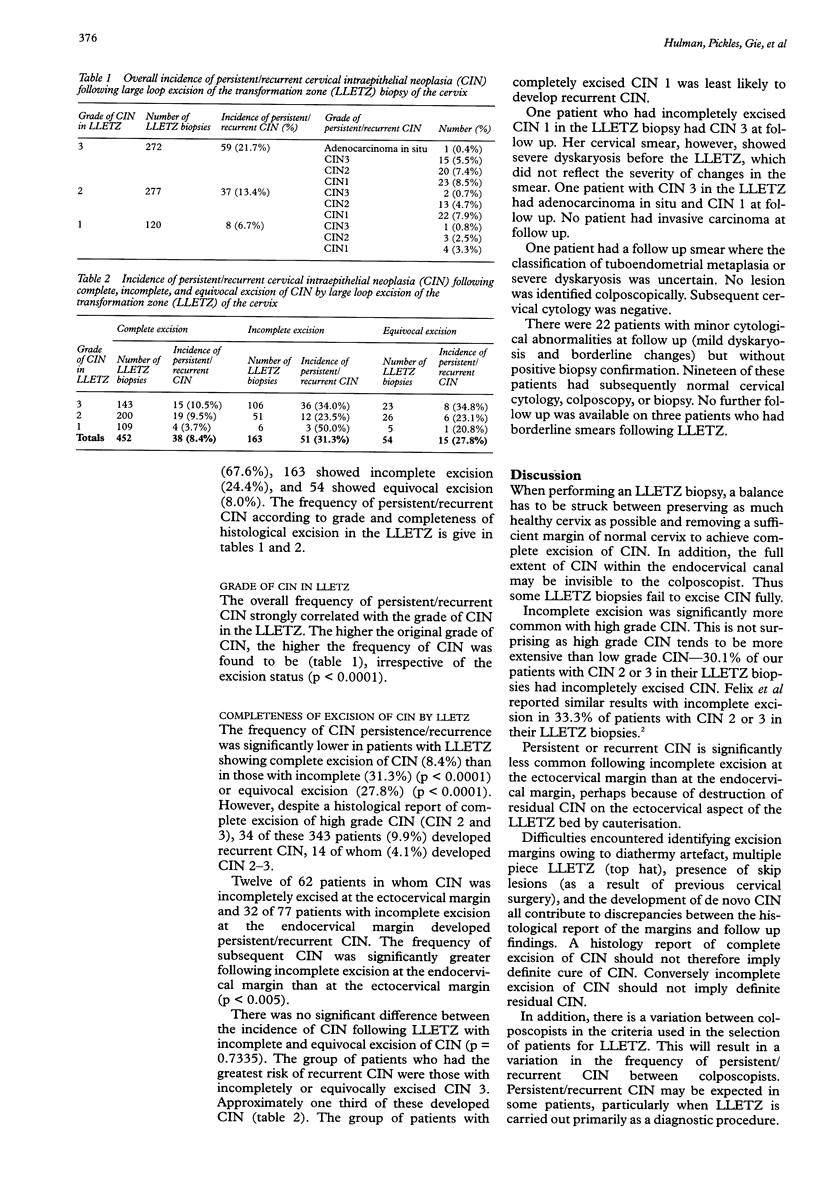
AIM: To determine the frequency of cervical intraepithelial neoplasia (CIN) following large loop excision of the transformation zone of the cervix (LLETZ) according to grade and completeness of excision of CIN. METHODS: A retrospective study of 669 patients who had LLETZ biopsies showing CIN 1, 2, or 3. The patients were subdivided according to the grade and completeness of excision of CIN. The follow up period was 1.5 to 3.5 years. Risk of persistent/recurrent CIN was assessed by the frequency of histological diagnosis of CIN during the follow up period. RESULTS: Frequency of persistent/recurrent CIN increased with the grade of CIN reported: 6.7% of patients with CIN 1, 13.4% with CIN 2, and 21.7% with CIN 3 developed persistence or recurrence. The frequency of CIN persistence/recurrence was significantly lower where LLETZ showed complete excision of CIN (8.4%) than where it was incomplete (31.3%) (p < 0.0001) or equivocal (27.8%) (p < 0.0001). CONCLUSIONS: Patients with incomplete or equivocal excision of all grades of CIN merit careful, preferably colposcopic, follow up. Patients with completely excised high grade CIN require careful cervical cytologic surveillance.
Full text
PDF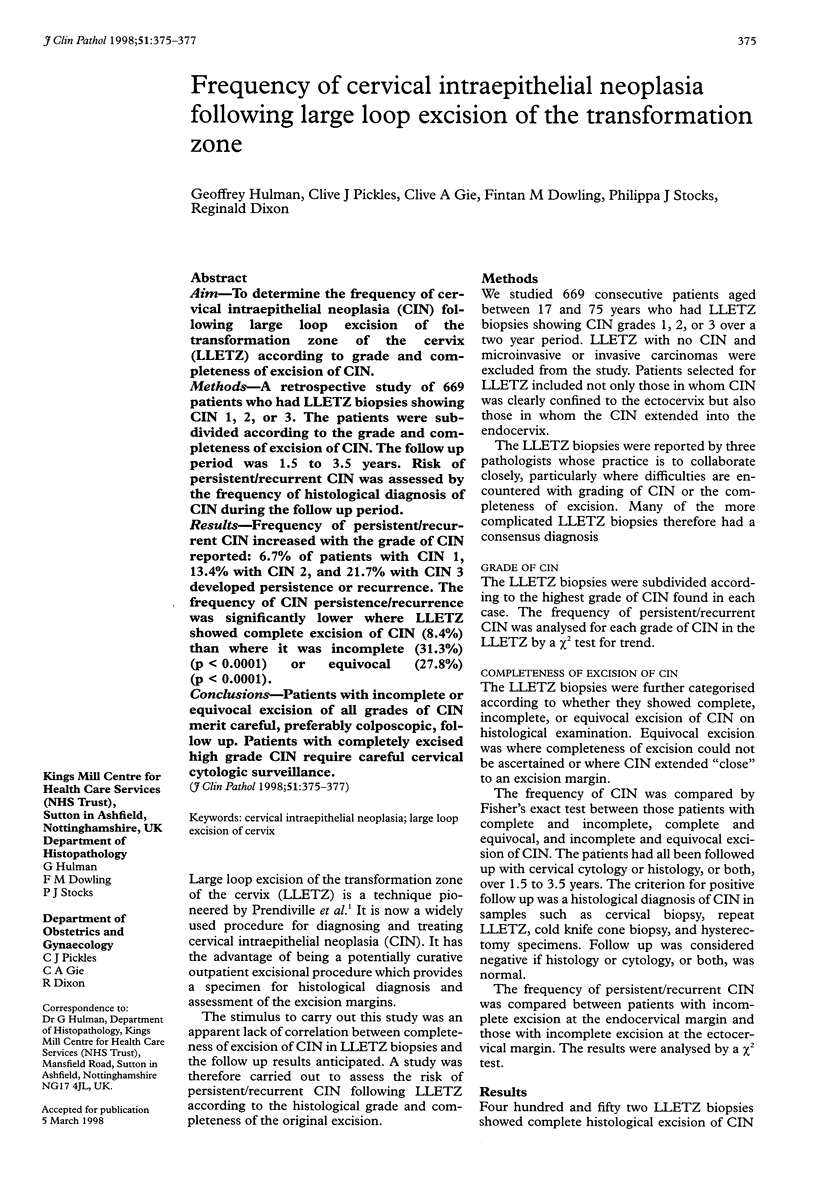

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bigrigg A., Haffenden D. K., Sheehan A. L., Codling B. W., Read M. D. Efficacy and safety of large-loop excision of the transformation zone. Lancet. 1994 Jan 1;343(8888):32–34. doi: 10.1016/s0140-6736(94)90881-8. [DOI] [PubMed] [Google Scholar]
- Buntinx F., Brouwers M. Relation between sampling device and detection of abnormality in cervical smears: a meta-analysis of randomised and quasi-randomised studies. BMJ. 1996 Nov 23;313(7068):1285–1290. doi: 10.1136/bmj.313.7068.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felix J. C., Muderspach L. I., Duggan B. D., Roman L. D. The significance of positive margins in loop electrosurgical cone biopsies. Obstet Gynecol. 1994 Dec;84(6):996–1000. [PubMed] [Google Scholar]
- Goff B. A., Rice L. W., Fleischhacker D. S., Abu-Jawdeh G. M., Muntz H. G. Large loop excision of the transformation zone in patients with exocervical squamous intraepithelial lesions. Eur J Gynaecol Oncol. 1994;15(4):257–262. [PubMed] [Google Scholar]
- Murdoch J. B., Morgan P. R., Lopes A., Monaghan J. M. Histological incomplete excision of CIN after large loop excision of the transformation zone (LLETZ) merits careful follow up, not retreatment. Br J Obstet Gynaecol. 1992 Dec;99(12):990–993. doi: 10.1111/j.1471-0528.1992.tb13704.x. [DOI] [PubMed] [Google Scholar]
- Prendiville W., Cullimore J., Norman S. Large loop excision of the transformation zone (LLETZ). A new method of management for women with cervical intraepithelial neoplasia. Br J Obstet Gynaecol. 1989 Sep;96(9):1054–1060. doi: 10.1111/j.1471-0528.1989.tb03380.x. [DOI] [PubMed] [Google Scholar]


