Abstract
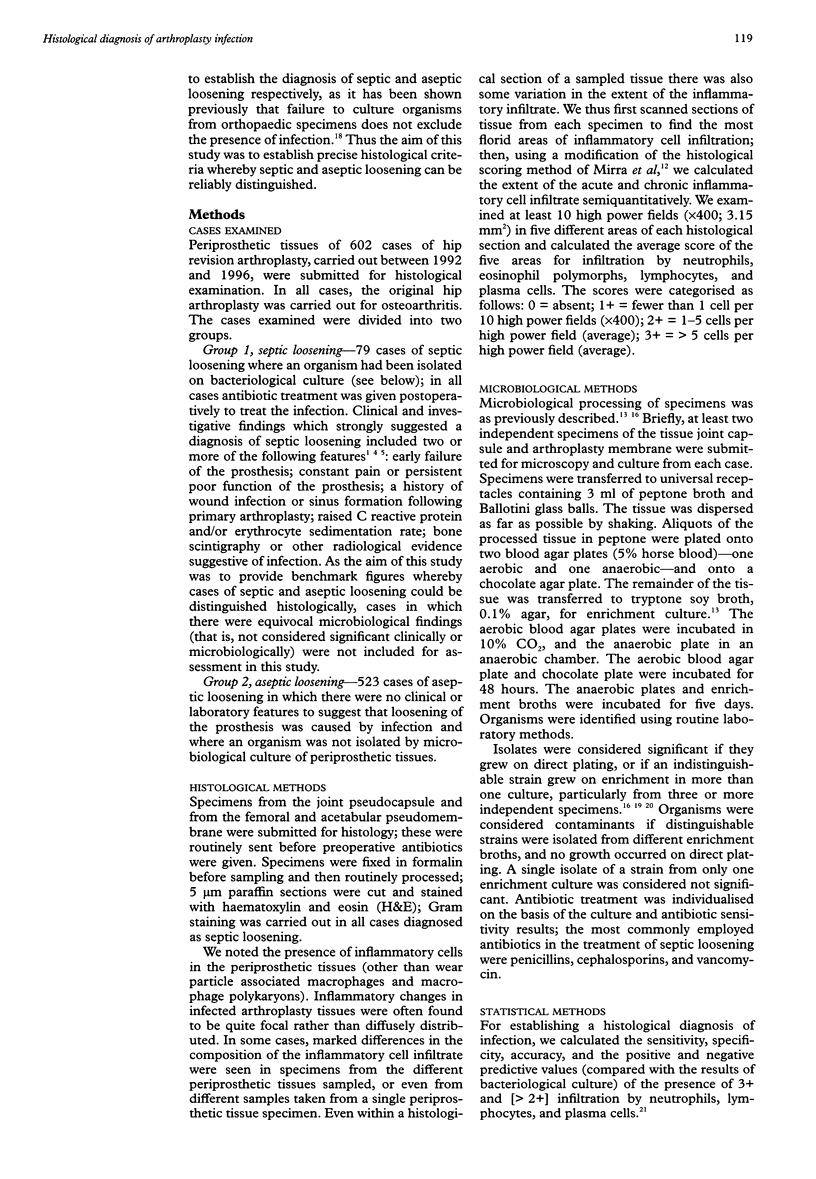
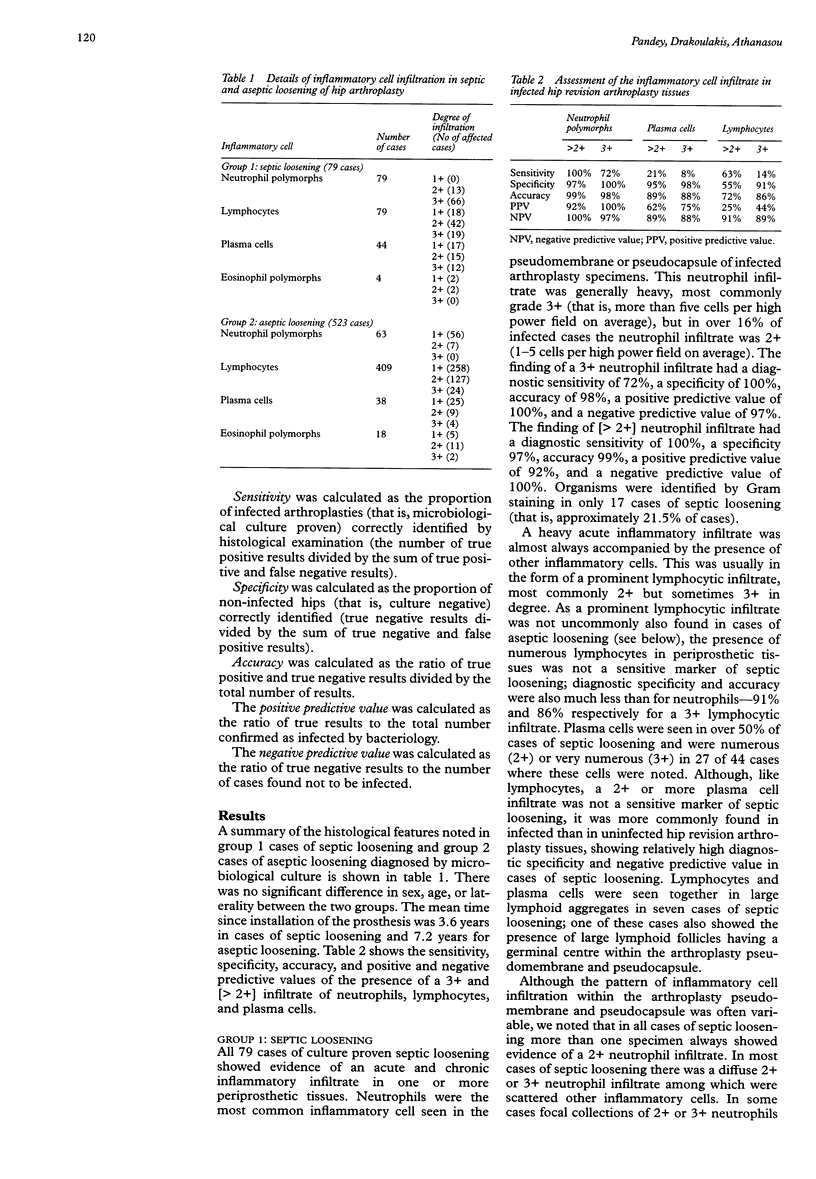
AIM: To characterise the number and nature of the inflammatory cells seen in cases of septic or aseptic loosening of hip arthroplasty, and to establish reliable histological criteria to distinguish between these two conditions. METHODS: Histological examination of paraffin sections of periprosthetic tissues (pseudocapsule, femoral and acetabular pseudomembranes) of 523 cases of aseptic loosening and 79 cases of microbiology culture proven septic loosening. The cellular composition of the inflammatory cell infiltrate was determined semiquantitatively. RESULTS: The finding of a 2+ or greater neutrophil polymorph infiltrate (one or more cells per high power field (x400) on average after examination of 10 fields) in arthroplasty tissues correlated strongly with the microbiological diagnosis of septic loosening: diagnostic sensitivity 100%, specificity 97%, accuracy 99%, positive predictive value 92%, negative predictive value 100%. The finding of a 3+ neutrophil polymorph infiltrate (five or more cells on average per high power field) had a diagnostic sensitivity of 72%, specificity 100%, accuracy 98%, positive predictive value 100%, and negative predictive value 97%. In some cases of septic loosening the finding of a heavy lymphocytic and plasma cell infiltrate was of low diagnostic sensitivity. A neutrophil polymorph infiltrate (generally less than one cell per 10 high power fields) was also seen in cases of aseptic loosening. CONCLUSIONS: The presence of 2+ or more (more than one neutrophil polymorph per high power field (x400) on average after examination of at least 10 high power fields) in periprosthetic tissues provides the most sensitive and accurate histopathological criterion for distinguishing between septic and aseptic loosening of hip arthroplasty.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Antti-Poika I., Josefsson G., Konttinen Y., Lidgren L., Santavirta S., Sanzén L. Hip arthroplasty infection. Current concepts. Acta Orthop Scand. 1990 Apr;61(2):163–169. doi: 10.3109/17453679009006513. [DOI] [PubMed] [Google Scholar]
- Athanasou N. A., Pandey R., de Steiger R., Crook D., Smith P. M. Diagnosis of infection by frozen section during revision arthroplasty. J Bone Joint Surg Br. 1995 Jan;77(1):28–33. [PubMed] [Google Scholar]
- Atkins B. L., Athanasou N., Deeks J. J., Crook D. W., Simpson H., Peto T. E., McLardy-Smith P., Berendt A. R. Prospective evaluation of criteria for microbiological diagnosis of prosthetic-joint infection at revision arthroplasty. The OSIRIS Collaborative Study Group. J Clin Microbiol. 1998 Oct;36(10):2932–2939. doi: 10.1128/jcm.36.10.2932-2939.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrack R. L., Harris W. H. The value of aspiration of the hip joint before revision total hip arthroplasty. J Bone Joint Surg Am. 1993 Jan;75(1):66–76. doi: 10.2106/00004623-199301000-00010. [DOI] [PubMed] [Google Scholar]
- Carlsson A. S. Erythrocyte sedimentation rate in infected and non-infected total-hip arthroplasties. Acta Orthop Scand. 1978 Jun;49(3):287–290. doi: 10.3109/17453677809005766. [DOI] [PubMed] [Google Scholar]
- Chimento G. F., Finger S., Barrack R. L. Gram stain detection of infection during revision arthroplasty. J Bone Joint Surg Br. 1996 Sep;78(5):838–839. [PubMed] [Google Scholar]
- Fehring T. K., McAlister J. A., Jr Frozen histologic section as a guide to sepsis in revision joint arthroplasty. Clin Orthop Relat Res. 1994 Jul;(304):229–237. [PubMed] [Google Scholar]
- Feldman D. S., Lonner J. H., Desai P., Zuckerman J. D. The role of intraoperative frozen sections in revision total joint arthroplasty. J Bone Joint Surg Am. 1995 Dec;77(12):1807–1813. doi: 10.2106/00004623-199512000-00003. [DOI] [PubMed] [Google Scholar]
- Gould E. S., Potter H. G., Bober S. E. Role of routine percutaneous hip aspirations prior to prosthesis revision. Skeletal Radiol. 1990;19(6):427–430. doi: 10.1007/BF00241797. [DOI] [PubMed] [Google Scholar]
- Hamblen D. L. Diagnosis of infection and the role of permanent excision arthroplasty. Orthop Clin North Am. 1993 Oct;24(4):743–749. [PubMed] [Google Scholar]
- Kraemer W. J., Saplys R., Waddell J. P., Morton J. Bone scan, gallium scan, and hip aspiration in the diagnosis of infected total hip arthroplasty. J Arthroplasty. 1993 Dec;8(6):611–616. doi: 10.1016/0883-5403(93)90008-r. [DOI] [PubMed] [Google Scholar]
- Lonner J. H., Desai P., Dicesare P. E., Steiner G., Zuckerman J. D. The reliability of analysis of intraoperative frozen sections for identifying active infection during revision hip or knee arthroplasty. J Bone Joint Surg Am. 1996 Oct;78(10):1553–1558. doi: 10.2106/00004623-199610000-00014. [DOI] [PubMed] [Google Scholar]
- Mirra J. M., Amstutz H. C., Matos M., Gold R. The pathology of the joint tissues and its clinical relevance in prosthesis failure. Clin Orthop Relat Res. 1976 Jun;(117):221–240. [PubMed] [Google Scholar]
- Morscher E., Babst R., Jenny H. Treatment of infected joint arthroplasty. Int Orthop. 1990;14(2):161–165. doi: 10.1007/BF00180122. [DOI] [PubMed] [Google Scholar]
- Perry C. R., Pearson R. L., Miller G. A. Accuracy of cultures of material from swabbing of the superficial aspect of the wound and needle biopsy in the preoperative assessment of osteomyelitis. J Bone Joint Surg Am. 1991 Jun;73(5):745–749. [PubMed] [Google Scholar]
- Pizzoferrato A., Fiori F., Savarino L. Microbiological investigation of 161 cases of hip endo-arthroprosthesis failure. Chir Organi Mov. 1980 May-Jun;66(3):297–307. [PubMed] [Google Scholar]
- Sanzén L., Carlsson A. S. The diagnostic value of C-reactive protein in infected total hip arthroplasties. J Bone Joint Surg Br. 1989 Aug;71(4):638–641. doi: 10.1302/0301-620X.71B4.2768312. [DOI] [PubMed] [Google Scholar]


