SUMMARY
Globally, as a leading agent of acute respiratory tract infections in children <5 years of age and the elderly, the human metapneumovirus (HMPV) has gained considerable attention. As inferred from studies comparing vaccinated and experimentally infected mice, the acquired immune response elicited by this pathogen fails to efficiently clear the virus from the airways, which leads to an exaggerated inflammatory response and lung damage. Furthermore, after disease resolution, there is a poor development of T and B cell immunological memory, which is believed to promote reinfections and viral spread in the community. In this article, we discuss the molecular mechanisms that shape the interactions of HMPV with host tissues that lead to pulmonary pathology and to the development of adaptive immunity that fails to protect against natural infections by this virus.
INTRODUCTION
The current lack of effective vaccines has contributed to a permanent large burden of acute respiratory tract infections (ARTIs) worldwide. Epidemiological studies have consistently shown that ARTIs are the leading cause of childhood mortality, contributing to approximately 1.7 million and 1.5 million deaths in 1998 (1) and 2008 (2), respectively. More than 10 years ago, van den Hoogen and coworkers identified and characterized a novel virus classified within the Paramyxoviridae family that was accountable for an important fraction of ARTIs affecting children globally. Based on genome sequence data and the identification of the M2 gene, this novel paramyxovirus was classified as belonging to the subfamily Pneumovirinae and later to the genus Metapneumovirus. Based on a significant genetic similarity to subgroup C avian metapneumovirus (AMPV-C), this pathogen was denominated the human metapneumovirus (HMPV) (3, 4). Furthermore, evolution analyses have suggested that HMPV was derived from AMPV-C between ∼180 and 270 years ago (5, 6). Phylogenetic studies of the first sequences obtained for the major HMPV glycoproteins (F and G) identified two major genotypes, genotypes A and B, which also defined two major serotypes (7). Later, subsequent analyses defined 4 genetic lineages circulating in the human population, the A1, A2, B1, and B2 lineages, which were derived from a common ancestor about 97 to 133 years ago (5, 6). Moreover, recent phylogenetic and evolutionary analyses of F and G genes collected in a 10-year period revealed that the A2 lineage could be separated into two other lineages, A2a and A2b, defining a total of 5 HMPV genetic lineages (8). Another recent study found that HMPV strains of the B genotype clustered separately from strains of the known B1 and B2 lineages, suggesting the existence of a third B lineage (9).
Epidemiology
The epidemiology of HMPV has been extensively studied since the identification of the virus in 2001, and excellent reviews have discussed epidemiological data accumulated over the first decade (10, 11). Globally, HMPV is recognized as the second most common cause of bronchiolitis and pneumonia in children <5 years of age (10, 11). Indeed, retrospective surveillance studies further confirmed that HMPV infections caused a significant fraction (∼5 to 20%) of ARTIs that were previously considered to have an unknown cause. These findings suggest that HMPV circulated in the human population long before it was identified as an etiological agent (4, 12–14). Recent seroprevalence studies have shown that HMPV steadily circulates in the community, as evidenced by the 100% seropositivity in adults aged 20 years and >65 years, which also suggests a steady reinfection rate that maintains measurable anti-HMPV IgG titers in the population (15–17). In agreement with this notion, epidemiological studies have concluded that HMPV displays a broad spatiotemporal distribution, affecting industrialized and developing countries equally. HMPV outbreaks have maintained discrete incidences that peak mostly during spring (reviewed in references 10 and 11). The simultaneous circulation of the 4 HMPV genetic lineages is a common finding, even in studies of different locations in consecutive years (13, 14, 18).
Lower ARTIs due to HMPV have been associated with other lung inflammatory conditions of either an acute or a chronic nature. For instance, HMPV infections are associated with asthma exacerbations in adults and elderly patients (19). The presence of HMPV RNA in respiratory secretions of adults suffering attacks of chronic obstructive pulmonary disease (COPD) has also raised concerns about the potential contribution of HMPV infections to COPD exacerbations (20–22). Because HMPV has also been detected in COPD patients with no disease exacerbation, further research is necessary to elucidate the actual role of the modulation of host immunity by HMPV to the pathophysiology of a COPD attack (21). Interestingly, about 35% of transplanted patients infected with HMPV can develop accelerated cellular rejection characterized by bronchiolitis obliterans syndrome and chronic allograft dysfunction (23), suggesting that HMPV can potentiate cellular immunity to unrelated antigens. In addition, at least two independent studies have shown that in various proportions of severe acute respiratory syndrome (SARS) cases, ranging from 22 to 50%, coinfection by SARS coronavirus and HMPV was confirmed (24, 25). These findings suggest that HMPV may additionally contribute to SARS pathophysiology (26).
Clinical Symptoms Associated with HMPV
HMPV causes clinical manifestations with various degrees of severity, ranging from asymptomatic infections to severe lower ARTIs. When symptomatic, HMPV infections cause a spectrum of clinical manifestations related to acute infection of the respiratory tract, including cough, fever, rhinorrhea, wheezing, and respiratory distress (referred to as dyspnea) (27). Such symptomatology is related mainly to bronchiolitis and to a lesser extent to pneumonitis (28). Furthermore, a study analyzed >2,000 upper respiratory tract samples by quantitative reverse transcription (RT)-PCR and determined that HMPV is a minor cause (up to 5%) of upper ARTIs (14). These upper ARTIs showed a variety of symptoms related to rhinitis (previously referred to as coryza), conjunctivitis, stomatitis, pharyngitis, laryngitis, and otitis media, the latter of which develops in ∼50% of infected children (14). In the elderly, HMPV infection may show symptoms related to an aggravation of other underlying conditions, such as congestive heart failure and COPD exacerbation, or to severe respiratory insufficiency arising from pneumonia or lung transplant rejection (27, 29–31). HMPV can produce asymmetric, acute interstitial pneumonia and bronchitis in immunocompromised adults, as evidenced by parenchymal airspace consolidations and bronchial wall thickening in chest computed tomography (CT) scans (32). Fever of >38°C, lymphopenia with monocytosis, increased C-reactive protein levels, and chest radiographs indicative of bronchitis and pneumonia have been also described for adults infected with HMPV (33). In healthy adults, experimental infection with HMPV produces symptoms including headaches, nasal congestion, pharyngitis, cough, hoarseness, cervical lymphadenopathy, and recurrence of herpes labialis (34). Importantly, the development of lymphopenia and the recurrence of herpes lesions suggest that HMPV could contribute to generating a transient immunosuppressive status in infected humans, which has to be investigated further. Community-acquired HMPV infections requiring intensive care and mechanical ventilation due to respiratory failure in immunocompetent adults have been also described (35, 36).
Very rarely, lower ARTIs caused by HMPV may be accompanied by a presentation of neurological symptoms, including attention and executive deficits, nonfebrile seizures, and ataxia (37). While only one case has been described for an adult, who was 47 years of age, most other cases have been reported for children ranging from 4 months to 5 years of age (37–46). Three independent studies have associated HMPV with acute encephalopathies ranging from subcortical encephalitis to multifocal demyelinating encephalitis, which are very rare ailments resulting from complications due to HMPV respiratory infection (39, 40, 43). Furthermore, a case of refractory status epilepticus and encephalitis in a 4-month-old infant who also presented an ARTI positive for HMPV but not for other common respiratory pathogens was recently reported (44). Importantly, seizures were accompanied by lymphocytic pleocytosis in the cerebrospinal fluid (CSF), suggesting that the activation of lymphocytes infiltrating the brain and ependyma may be an important pathogenic mechanism in these neuropathies. Although the pathological findings in brain tissue were associated with the detection of HMPV RNA in two reports (38, 39), to date, no direct evidence demonstrates a causative role of HMPV in these neurological disorders. Moreover, worsening of neurological dysfunction has been documented in one case despite reductions in viral loads in the CSF, raising debate regarding the neuropathogenic potential of HMPV.
Factors Contributing to HMPV Disease Severity
HMPV infects primarily individuals <5 years of age, adults >65 years of age, and immunocompromised individuals, thus defining three susceptible populations. Age is one of the major factors influencing disease severity, as evidenced by an increased rate of hospitalizations in infants <5 months of age, who have prolonged stays in the intensive care unit (ICU), being approximately twice as susceptible as infants 6 to 11 months of age and five times more susceptible than the average for children <5 years old (18). As for children, elderly individuals also show increased hospitalization rates and prolonged stays in the ICU (12, 13, 47–54). In agreement with this notion, recent studies demonstrated that an important fraction (up to 95%) of children infected with HMPV have no comorbidities and are otherwise healthy (51, 53), suggesting that age alone is a major risk factor. Furthermore, although severe respiratory infections requiring ICU admission have also been reported for healthy adults with no comorbidities or underlying diseases, the incidence in this population is rather low (35, 55). Importantly, disease severity, which is measured as the degree of respiratory involvement, is strongly correlated with HMPV loads in young children (56–58). This observation suggests that an age-related phenomenon may be modulating the clearance of HMPV from lungs, thereby more severely compromising pulmonary function due to increased inflammation of airways.
The basis for the age-related risk for severe HMPV infections remains poorly understood; however, the increased morbidity of infants and the elderly seems tightly associated with the developmental stages of T lymphocytes. Three major developmental stages have been described for human T cells: memory generation, memory homeostasis, and immunosenescence (reviewed in reference 59). While children <2 years old display cellular immunity under development, with a low frequency of memory T cells, elderly individuals show reduced proportion and functionality of memory T cells (60, 61). Similarly to T cells, newborns develop a limited repertoire of B cells specific for viral antigens due to reduced somatic mutation in immunoglobulin genes, as recently demonstrated by using human respiratory syncytial virus (HRSV) as a model pathogen (62). These findings suggest that disease severity in infants and the elderly may be defined in part by the maturity and diversity of B and T cell repertoires, underscoring the relevance of acquired immunity of the host in disease pathogenesis.
Underlying diseases are additional risk determinants for severe HMPV infections, and the rate of hospitalizations is increased for patients suffering from prematurity, asthma, COPD, or immunosuppression (51, 54, 55, 63–65). For instance, severe or lethal HMPV infections develop in subjects of different ages who are immunosuppressed due to either cancer or transplantation therapy (48, 66–73). As inferred from the link between viral loads and ARTI severity in children, the elevated risk for the establishment of persistent, life-threatening infections in immunocompromised individuals suggests that the capacity of the host to control viral replication is a major factor influencing the severity of HMPV infections.
To date, there is no conclusive evidence to support any association of viral genetics with HMPV virulence and disease severity. Significant associations for infections with strains belonging to the A2, A2b, and B2 genotypes have been established in the literature (54, 74, 75). However, due to several factors, such as herd immunity, that influence the spatiotemporal distribution of distinct HMPV lineages, the association of viral genetics with disease incidence and severity must be carefully analyzed. The high degree of genetic variability in HMPV surface glycoproteins may shape herd immunity and favor reinfections with distinct HMPV genotypes over time. This can be translated into an increased frequency of hospitalization related to a particular genotype but does not necessarily imply that such genotypes produce a more severe pathology. Indeed, other studies have either failed to establish a clear association between disease severity and infection with different HMPV lineages (76) or shown that dominant lineages change in consecutive years, supporting the role of herd immunity pressure over the genetic diversity of circulating HMPVs (77).
Although research has intensely focused on understanding the pathology and role of adaptive immunity in both disease progression and viral clearance, there is still no vaccine to shape herd immunity and prevent HMPV infection. Nonetheless, current advances in the understanding of molecular determinants that shape HMPV interactions with the host have contributed to innovative and encouraging approaches to treat and prevent lung diseases that are caused by this paramyxovirus. This review focuses on the interactions of HMPV with host immunity and addresses their implications in respiratory pathogenesis, the development of adaptive immunity to natural infections, and the lessons that we can apply to design vaccines to prevent infections caused by this important human pathogen. To address this in a comprehensive manner, comparisons with other paramyxoviruses, including its close relative HRSV, are made.
MOLECULAR ANATOMY OF HMPV
Similarly to other paramyxoviruses, HMPV particles are pleomorphic and display diameters ranging from 150 to 600 nm and averaging 200 nm (Fig. 1). The virion has a highly electron-dense envelope in which the viral glycoproteins relevant for target cell recognition and infection are embedded (Fig. 1). The viral nucleocapsid encapsulates a 13.3-kb, nonsegmented, negative-sense, single-stranded RNA (ssRNA) genome (viral RNA [vRNA]) containing eight genes, each of which is delimitated by gene start (GS) and gene end (GE) sequences that define each gene as an independent transcriptional unit (78–80). As with other paramyxoviruses, the HMPV replication cycle develops in the cytosol of infected cells and uses vRNA as a template for the generation of RNAs of positive polarity, including the polycistronic antigenome and each of the individual mRNAs (81, 82).
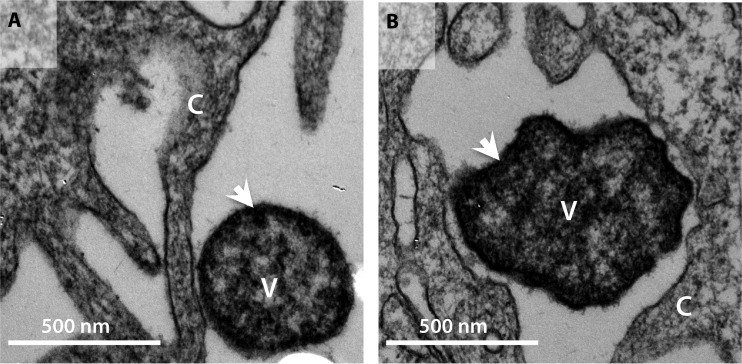
FIG 1.
Transmission electron microphotographs showing negative staining of HMPV particles (V) interacting with monkey kidney cells (C). Two different strains are shown: HMPV CZ0107 (A2) (A) and NL/1/00 (A1) (B). White arrowheads show the viral envelope, which has a high electron density due to the large amount of bilayer-associated proteins, including surface glycoproteins and M. Similarly to other paramyxoviruses, most infective virions are pleomorphic and display different sizes and circular shapes (84).
Based on both the well-characterized model of vesicular stomatitis virus (VSV) transcription as well as the presence of gene interspaces, GS sequences, and GE sequences, it is believed that the transcription of HMPV genes develops in a linear, sequential, stop-restart process (83, 84). Because of this stop-restart process and the chances of the transcriptase-replicase (TR) polymerase disassociating during transcription restart, HMPV transcription is thought to be hierarchical, where mRNA synthesis from genes closer to the 3′ promoter is more efficient than that from distal genes (84) (Fig. 2A). Remarkably, translation of the eight mRNAs of HMPV produces nine different polypeptides, due to the translation of two different open reading frames (ORFs), M2-1 and M2-2, encoded in the matrix 2 (M2) mRNA (Fig. 2A). Translation of the M2-2 protein is likely initiated independently of the M2-1 ORF, as demonstrated by the efficient expression of M2-2 in cells infected with HMPV encoding a translation-silenced M2-1 ORF (85). Similarly to AMPV, the HMPV genome lacks genes for nonstructural proteins such as NS1 and NS2 of HRSV (Fig. 2B). Some proteins encoded in the HMPV genome contribute to the regulation of the replication cycle and the interferon (IFN) response (see “Modulation of the Interferon Response by HMPV Proteins and Contribution to Viral Pathogenesis,” below). Most of our current understanding relative to the function of HMPV proteins is preliminary and lacks definitive experimental evidence, which has led to extrapolations based on similarity with proteins of other paramyxoviruses.
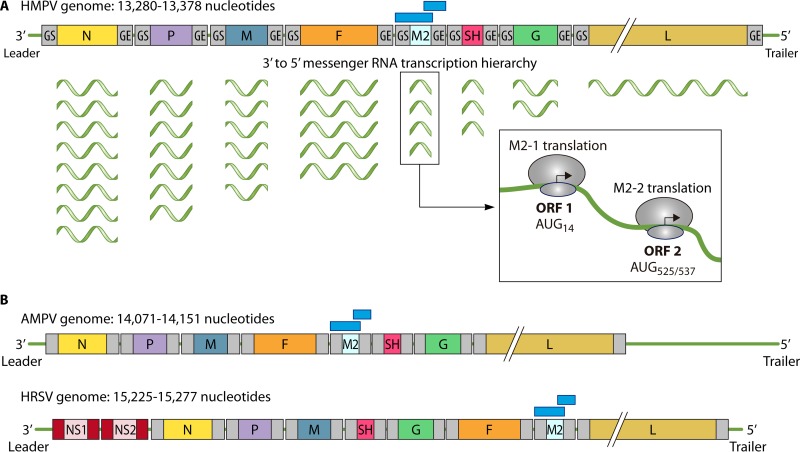
FIG 2.
(A) Schematic structure of the HMPV ssRNA genome and arrangement of each of the eight genes within the genome. Each gene is flanked by two conserved sequences, which are referred to as the gene start (GS) and gene end (GE) sequences. During transcription, the TR complex stops at each GE to restart transcription in the following GS sequence (84). However, because the TR complex may stall, this process leads to an increased abundance of mRNAs closer to the 3′ leader. At the bottom right is a sketch of the translation mechanism producing two polypeptides from the M2 mRNA. Two different ORFs located at position 14 and position 525/537 are used to synthesize the M2-1 and M2-2 proteins, respectively (85). (B) Schematic compositions of the AMPV and HRSV genomes. Note the striking degree of conservation of gene order between HMPV and AMPV. Sequence analyses indicate that while most AMPV and HMPV structural proteins display ∼80% amino acid identity, the G and SH proteins display high amino acid variability ranging from 70 to 80% (78, 264). Also, note that the genomes of HMPV and AMPV lack homologous genes for the HRSV NS1 and NS2 proteins (highlighted in red). In panels A and B, the genomes are not illustrated to scale.
The HMPV nucleoprotein (N) shows ∼41% protein identity to the HRSV N protein (86–88). The major role of this protein is to package linearized genomic RNA into helical ribonucleoprotein complexes that serve as molecular scaffolds for the assembly of the TR machinery (Fig. 3). This supramolecular complex is also composed of the phosphoprotein (P), the M2-1 protein, and the large RNA polymerase (L) protein (89). Because it synthesizes viral RNA species, including the genome and RNAs of positive polarity (mRNAs and the full-length polycistronic antigenome), L is instrumental in the viral replication cycle (79, 80). To accomplish all of these functions, L proteins of the Paramyxoviridae family display independent structural and functional domains with enzymatic activities related to genome replication and methylation, capping, polyadenylation, and polymerization (through phosphodiester bond formation) of mRNAs (84, 90). For the transcriptase function, the HMPV L protein possesses an S-adenosylmethionine binding site with methyltransferase activity, which participates in the capping of newly synthesized mRNAs (91). Although the nature of most protein-protein interactions that form the machinery of the HMPV TR complex remain unknown, TR formation is thought to depend on interactions similar to those described for the HRSV counterparts. The HMPV phosphoprotein (P) is expected to be pivotal for the assembly of the TR complex in a manner similar to that of its HRSV counterpart, which interacts with the L, M2-1, and N proteins (92). Indeed, similarly to their HRSV counterparts, the HMPV P and N proteins interact and form cytoplasmic inclusion bodies in infected cells (93). The HRSV P protein promotes mRNA elongation upon phosphorylation on threonine 108 and serine 232 (94, 95). Importantly, the high degrees of identity and conservation of the N and P proteins of all known HMPV lineages (96) have led to the postulation that these proteins are promising antigens for the invention of vaccines aimed at promoting cellular acquired immunity. As a proof of concept, we demonstrated that a P-recombinant Mycobacterium bovis bacillus Calmette-Guerin (BCG) vaccine uses the concerted activity of helper and cytotoxic memory T cells to promote HMPV clearance from infected lungs and prevent pulmonary disease in mice (97).
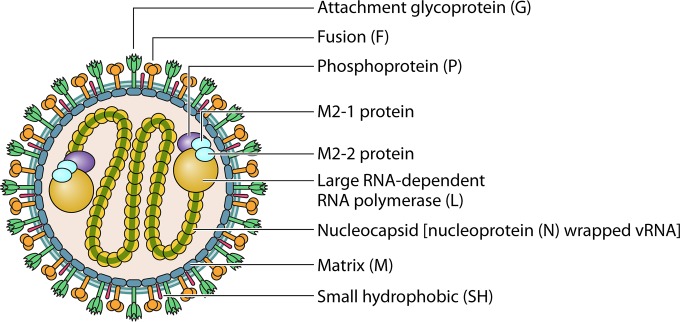
FIG 3.
Schematic illustration of the HMPV particle showing the molecular scaffolding assembled in the host cell lipid bilayer. Three different viral proteins are embedded: the F protein (orange) (a trimer) (265), the G protein (green) (a tetramer), and the SH protein (red) (a pentamer). The viral matrix (blue) encapsulates the nucleoprotein-associated genome (yellow-green) or nucleocapsid underneath the lipid bilayer. Similarly to HRSV, the nucleocapsid of HMPV is thought to form long helical structures that are packaged within the viral particle (86, 88). The ribonucleoprotein complex is associated with the L protein (yellow), along with its cofactors (P [violet] [a tetramer] [266] and the M2-1 protein [pale blue] [a tetramer] [100, 101]). It is thought that as part of the TR complex, the M2-2 protein (pale blue) is also included within viral particles.
Although the function of M2 gene products in the TR complex is dispensable for viral growth, they actively participate in the regulation of the replication cycle (85, 98). The HMPV M2-1 protein is an additional cofactor for the TR complex that works as an antiterminator of mRNA synthesis that promotes the transcription of viral genes (99, 100). M2-1 forms a tetrameric complex in which each protomer participates in the specific recognition of GE RNA sequences through an N-terminal Zn finger domain (100). While tethering of the zinc atom stabilizes the tetramer, RNA binding closes the conformation of the tetramer, which otherwise has one protomer loosely interacting with the other three (101). Because both the interaction with P and the removal of zinc atoms fine-tune the interaction of M2-1 with the vRNA, it is though that besides working as a transcription antiterminator, M2-1 can also regulate the assembly of the TR complex (101). In contrast to M2-1, the M2-2 protein is recognized as a key negative modulator of viral transcription and replication, as indicated by the accumulation of mRNAs in M2-2 mutants and the inhibition of HMPV replication in cells accumulating M2-2 (85, 98, 102). Furthermore, the M2-2 protein maintains polymerase fidelity, as evidenced by the increased mutation frequencies in M2-2 mutants (85, 98). The M2-2 protein participates also in the early regulation of host immunity (see “Modulation of the Interferon Response by HMPV Proteins and Contribution to Viral Pathogenesis,” below). Importantly, the contribution of HMPV M2 proteins to the host infection cycle is further supported by the observation that viruses lacking either the full-length M2 gene, M2-1, or M2-2 are highly attenuated in both hamsters and nonhuman primates, displaying marginal replication in nasal turbinates and lungs (85, 98, 103).
Following vRNA replication and packaging, the successful spread of infection to neighboring cells depends on the release of new, structurally intact virions. The confining of the HMPV matrix protein to the inner surface of the host cell membrane is a mandatory step in the production, maturation, and release of properly enveloped virions from infected cells (104). Structural studies have identified a positively charged surface on the M protein that allows interactions with negatively charged membrane phospholipids. A Ca2+ binding pocket has also been identified, which suggests a role of Ca2+ in particle assembly and stability (105). As with other paramyxoviruses (106, 107), the association of M with the plasma membrane is thought to support viral assembly due to interactions between M and host factors or other viral proteins, including the nucleocapsid and the cytoplasmic tail of surface glycoproteins (Fig. 3). Additionally, the production of avian metapneumovirus-like particles is a process that is dependent on the coexpression of and interaction among M, N, and fusion (F) proteins (107), suggesting that a similar requirement may exist during HMPV budding.
In mature, infective viral particles, which are also referred to as virions, three major glycoproteins (F, attachment glycoprotein [G], and SH) are anchored to the plasma membrane (Fig. 3). A conserved arginine-glycine-aspartate (RGD) motif on the F protein favors binding to multiple RGD binding integrins that participate in both attachment and fusion to target cells (108–110). Besides integrins, F also binds glycosaminoglycans such as heparan sulfate (111). The F protein is a class I glycoprotein that assembles into trimeric structures formed by protomers of two disulfide-bound subunits, F1 and F2, generated by protease processing. This enzymatic cleavage exposes an N-terminal, hydrophobic peptide in the F1 subunit, which penetrates the opposing host cell membrane and initiates fusion after refolding into coiled coils and forming a pore for the delivery of the nucleoprotein TR complex (112). The F proteins of some HMPV strains contain an amino acid substitution at position 294 (glutamic acid [E] to glycine [G]) that confers the capacity to promote fusion at low pH (113, 114). Importantly, this membrane fusion mechanism differs from that mediated by F proteins of other members of the Paramyxoviridae, which takes place at the neutral pH of the cell plasma membrane (115), suggesting that the entry of these strains may be efficiently mediated in early endosomes (pH 6.0 to 6.5) (116). A recent report further demonstrated that HMPV is internalized by using the endocytic pathway through a mechanism dependent on clathrin and dynamin and fuses with endosomal membranes without requiring acidification of the endosomal compartment (117).
The role of G in adhesion has been majorly inferred from its comparison to its HRSV orthologue. Indeed, although the HMPV G protein binds heparin in vitro (118, 119), there is a lack of evidence demonstrating its real contribution to the processes of target cell binding and stabilization of glycoproteins during the process of fusion of virus and host cell membranes. Indeed, it seems dispensable for infection, as evidenced by studies showing efficient infection of cells and animals with HMPV strains lacking G (120). As with G, the function of the SH protein in the replication cycle of HMPV is elusive (121). Recent evidence indicates that as a viroporin, SH regulates membrane permeability, enhancing the fusogenic capacity of HMPV (122). Also, others have found that SH aids in the regulation of host innate and acquired immunity by shutting down the activation of nuclear factor κB (NF-κB), a master regulator of proinflammatory genes (123, 124) (see “Modulation of the Interferon Response by HMPV Proteins and Contribution to Viral Pathogenesis” and “Impairment of DC Function by HMPV and Implications for the Generation of Suboptimal Helper T Cell Immunity,” below).
Among the surface glycoproteins expressed by the four HMPV genogroups, F displays the highest degree of conservation (∼94 to 97% amino acid identity), whereas SH and G display significantly lower genetic identities (∼59 and 37%, respectively) (83, 96). As a central protein for target cell infection, the F protein of HMPV has been considered an appealing subject for the development of neutralizing antibodies for passive immunotherapy (125) or vaccination (126). Experimental evidence further supports the role of F as the dominant neutralizing antigen and the conversely poor protective role of G and SH (127).
PATHOPHYSIOLOGY OF HMPV INFECTION
Members of the Paramyxoviridae family provide good examples of viral strategies to inhibit the early host antiviral response to promote viral spread to permissive tissues (128, 129). Several negative modulatory proteins have endowed HMPV with mechanisms to efficiently replicate in target cells in the face of activated IFN responses. By either uncoupling cellular innate surveillance systems or interfering with the adequate activation of adaptive immunity, HMPV disseminates in the host respiratory tract, leading to immune-mediated pulmonary pathology that is similar to that caused by HRSV. Furthermore, such strategies are thought to impair the acquisition of immunological memory and favor lifelong reinfections. Next, we review host and viral molecular determinants that dynamically interact during infections to lead to the blunting of host immunity as well as lung hyperreactivity and airway obstruction.
Contribution of Airway Cells to HMPV Lung Pathogenesis
As a respiratory pathogen, HMPV primarily targets epithelial cells that inhabit the upper and lower respiratory tract and lung-resident leukocytes. Upon infection with HMPV, several histopathological changes occur in the lungs of infected humans and mice. These alterations include damage of the respiratory epithelial architecture, sloughing of epithelial cells, hyaline membrane formation, loss of ciliation, and exacerbated mucus production and inflammation of the lung interstitium (also referred to as parenchymal pneumonia or pneumonitis) (130–132). Furthermore, HMPV diffusively compromises the lungs of humans, mice, and cynomolgus macaques. Indeed, multiple focal lesions in which inflammation of the lung parenchyma is associated with the presence of HMPV proteins have been reported (133), suggesting that (i) the activation of host immunity is delimited to regions of virus replication and (ii) the degree of respiratory involvement is strongly correlated with viral spread in the respiratory tract. With the exception of immunocompromised hosts and patients with underlying disorders, the latter of whom may develop chronic airway inflammation, HMPV respiratory infections are acute and self-limited (130, 134, 135). These acute and chronic pathological changes lead to the impairment of gaseous exchange and the generation of respiratory distress in infected hosts (136, 137). In recent years, several studies have provided an appreciation of the molecular processes that participate in the initiation of immunity to infection and the generation of pulmonary pathology following HMPV infection (138). Data obtained in BALB/c mice suggested that HMPV establishes long-term persistence in the respiratory tract and leads to lung hyperreactivity (defined as an increased bronchospasm response to muscarinic receptor agonists) (132, 139, 140). However, long-term persistence and the development of lung hyperreactivity have not been replicated in other models, raising questions regarding whether this is a phenomenon common to all HMPV lineages and whether it can be extrapolated to immunocompetent humans.
The initial step of respiratory cell infection is crucial for both viral dissemination in the lungs and the orchestration of later immunological events that are related to airway inflammation and pulmonary damage. Infection of airway epithelial cells (AECs) is the first important process that occurs in the course of the acute phase of infection. Based on the detection of HMPV-infected cells in the sputum and respiratory secretions of children suffering from ARTIs, it is thought that HMPV targets AECs that inhabit the nasopharynx and lungs (141–143). Experimental infection models have been used to elucidate the infection of cellular subsets with HMPV and their potential contribution to disease pathogenesis. For example, histopathological studies in mice and macaques have shown that HMPV replicates in different types of AECs, including those from the bronchi, bronchioles, and alveoli (103, 133). At a lower frequency, HMPV infects alveolar macrophages (AMϕs) (133), which are an important myeloid cell population that controls inflammation and immune homeostasis in the lungs. Similarly, lung-resident dendritic cells (DCs) are thought to be unconventional targets for HMPV infection, due to their strategic location in alveolar and bronchial spaces as well as in the interstitium of the lungs. This notion is further reinforced by several studies showing infection of cultured human and mouse conventional DCs but with a restrictive/abortive replication cycle and limited viral shedding (144–147). AECs, AMϕs, and DCs are thought to be the major populations that sense HMPV in the acute course of infection and therefore are critical components mediating airway inflammation (138). Indeed, HMPV infection increases myeloid cell populations in the lungs, including DCs and AMϕs (133, 138, 148). AMϕs have been reported to be critical mediators of pulmonary disease in mice (149).
Modulation of the Interferon Response by HMPV Proteins and Contribution to Viral Pathogenesis
Secreted type I IFNs mount the first protection mechanism against viral infections and have a key role in restraining viral spread by activating hundreds of different IFN-stimulated genes (ISGs). These genes create an antiviral state by shutting down general processes in neighboring cells (150). Triggering of IFN receptors (IFNRs) expressed on target cells, including innate and acquired leukocytes, promotes the elimination of infected cells through the enhancement of antigen-dependent and -independent cytotoxicities (150–152).
Two major pathways for the secretion of type I IFNs in HMPV-infected cultured cells have been described. Each pathway involves different pattern recognition receptors (PRRs). The first pathway involves two helicases from the RIG-I-like receptor (RLR) family, RIG-I and MDA5. Upon recognition of cytosolic viral double-stranded RNAs (dsRNAs) and uncapped 5′-triphosphates of the viral genome, these RLRs signal downstream by using the mitochondrial antiviral signaling protein MAVS (153–155). MAVS then activates downstream IFN regulatory factor 3 (IRF3), which in turn activates type I IFN secretion, IRF7 upregulation, and NF-κB, inducing the secretion of proinflammatory cytokines and type III IFNs (153) (Fig. 4). The second pathway for sensing HMPV involves endosomal Toll-like receptor 3 (TLR3) and TLR7 (155, 156). TLR3 activates IRF3 via the adaptor protein TRIF, whereas TLR7 activates IRF7 via the adaptor protein MyD88 (Fig. 4).
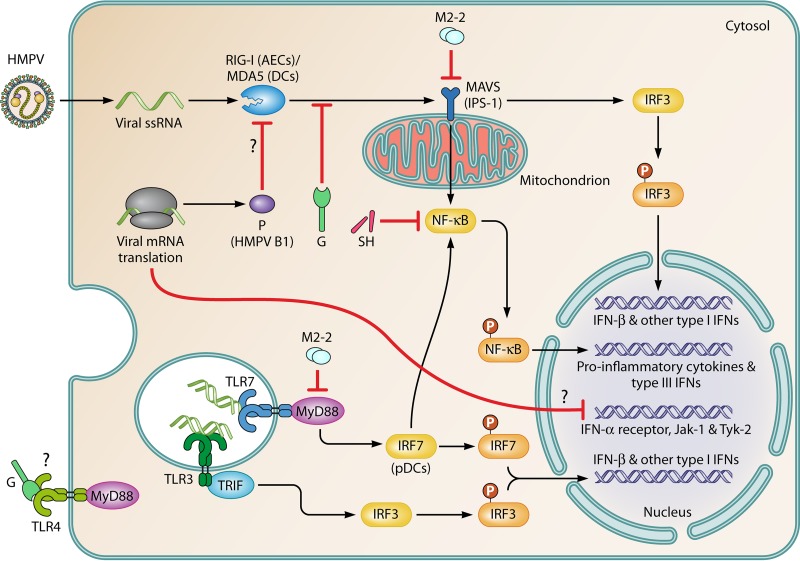
FIG 4.
Sensing of HMPV by different PRRs and modulation of the IFN response by viral proteins. AECs and DCs that inhabit the lower respiratory tract use two major pathways to sense HMPV replication. (Top) The first pathway involves RLRs, including RIG-I (more relevant in AECs) and MDA5 (more relevant in DCs) (155, 157). These RLRs couple MAVS for signaling, which leads to the secretion of type I IFNs. Proinflammatory cytokines and type III IFNs are also secreted through the activation of IRF3 and NF-κB, respectively. Products of viral replication, including cytosolic dsRNAs and uncapped 5′-triphosphates present in the genomic RNA, activate RLRs. (Bottom) The second pathway involves TLRs. TLR3, TLR4, and TLR7 interact with viral products. The activation of TLR3 (in most cells) and TLR7 (more important in pDCs) by viral dsRNAs leads to the secretion of type I IFNs by TIR domain-containing adaptor-inducing IFN-β (TRIF)/IRF3-dependent and MyD88/IRF7-dependent pathways, respectively, and the G protein impairs TLR4 signaling. HMPV proteins have synergizing/additive effects on the inhibition of viral sensing. The G and P (HMPV B1) proteins impair sensing of viral RNA species through the inhibition of RIG-I- and MAVS-dependent signaling (154, 155). The M2-2 and SH proteins are key virulence factors that negatively modulate signaling through both PRRs due to their interactions with the TLR adaptor MyD88 (167) and NF-κB (124), respectively. Furthermore, M2-2 directly interacts with MAVS, impairing the upregulation of IFN-β (156). Additionally, the G protein of HMPV has been proposed to interact with and abrogate signaling through TLR4 (158, 168), although the mechanism remains unknown. Moreover, HMPV infection leads to the downregulation of IFN-α receptors, Jak-1, and Tyk-2, thus impairing the autocrine IFN response in infected cells (165).
Importantly, most cells express IRF7 only in response to IFNs or after the activation of IRF3, which is expressed constitutively and is activated mostly by the RIG-I–MAVS pathway (155). However, in plasmacytoid DCs (pDCs), IRF7 is constitutively expressed and contributes to the generation of stronger TLR7-triggered type I IFN responses (157). Thus, cell-based differential expression of IRFs defines the way by which conventional DCs and pDCs initiate the type I IFN response. More specifically, TLR7 is the major PRR mediating HMPV sensing in pDCs, whereas MDA5-MAVS is the major pathway sensing HMPV in human and mouse conventional DCs (155, 157). In summary, viral RNA products activate IRF3 by triggering MDA5, RIG-I, or TLR3 in AECs, whereas they activate IRF7 through TLR7 in pDCs, which mounts a stronger IFN response to HMPV. An additional piece of evidence suggests that DCs use a redundant mechanism to sense HMPV, which involves the engagement of TLR4 on the surface of DCs by the G protein of HMPV (158). Nevertheless, this mechanism does not require viral replication as does sensing of HMPV through RIG-I-like helicases, TLR3, and TLR7.
Type I alpha/beta IFNs (IFN-α/β) are secreted by human AECs and human/mouse DCs during the first hours postinfection (144, 145, 156). Shortly after infection with HMPV, strong IFN-α/β production is observed in lungs, along with significant recruitment of pDCs, which are specialized in the secretion of type I IFNs (148). However, type I IFN signaling seems to play a pathogenic role in vivo, as evidenced by less pathology and airway dysfunction in HMPV-infected mice lacking the IFN-α receptor (IFNAR) (ifnar−/− mice) (159). These mice display increased viral replication yet clear HMPV from the airways with kinetics similar to those of controls. This suggests that type I IFN signaling contributes minimally to HMPV clearance in mice (159). Furthermore, HMPV infection in ifnar−/− mice leads to the preferential expansion of PD-L1-expressing AMϕs and impaired function of cytotoxic T lymphocytes (CTLs). The undermined function of the CD8+ T cell repertoire was previously shown to be mediated by PD-1/PD-L1 interactions in HMPV-infected wild-type mice (159, 160). Importantly, IFNAR is essential for the expansion of lung DCs that express lower levels of PD-L1, which are inferred to be the relevant antigen-presenting cell (APC) population that drives the initiation and escalation of CTL responses (159, 160).
In mouse neonates, a more significant role in HMPV clearance and pathogenesis has been described for MAVS/IPS-1 and IRF3/7, which are factors upstream of IFNAR signaling. Spann and coworkers showed that neonatal MAVS (also referred to as interferon-beta promoter stimulator 1 [IPS-1]) knockout mice or IRF3/IRF7 double-knockout mice had an impaired clearance of HMPV from the lungs but displayed opposite susceptibilities to viral pneumonitis (161). MAVS (IPS-1) knockout mice fail to develop an inflammatory response to HMPV, which may be related to the uncoupling of RLRs and NF-κB. In contrast, IRF3/IRF7 knockout mice show exacerbated neutrophilic inflammation in the lungs that is also associated with T helper type 1 (TH1) and TH17 responses. This suggests that type I IFNs aid in regulating CD4+ T cell responses during paramyxoviral infections (161). Mechanistically, the discrepancy in the results obtained from studies using either IFNAR or MAVS/IRF3/IRF7 knockout mice may be related to the fact that the elimination of IFNAR has a more specific effect that is limited to the IFN-α–IFNAR signaling pathway. In contrast, the elimination of MAVS/IRFs has broader deleterious effects, including an impaired production of proinflammatory cytokines and a different class of IFNs that are important in modulating disease development (type III IFNs [IFN-λs] [see below]).
Infected human AECs upregulate IFN-λ1 to -4 (also known as interleukin 29 [IL-29] [IFN-λ1], IL-28A [IFN-λ2], and IL-28B [IFN-λ3]) (162). Importantly, Banos-Lara and coworkers used blocking antibodies against the IFN-λ receptor to demonstrate that IFN-λs not only possess strong antiviral activity but also abrogate disease development in BALB/c mice (163). This suggests that IFN-λs may be applicable as localized therapy for minimizing HMPV burden in the respiratory tract. The protective effect of IFN-λs may also be due to the negative modulation of T cell function, as previously reported for the secretion of IFN-λs by DCs infected by HRSV (164). In this regard, HMPV infection of human and mouse conventional DCs activates both MDA5 and IRF3/7, thus leading to the secretion of IFN-λ along with IFN-γ and type I IFN-α, -β, and -ω (157). As expected, MDA5 knockout mice lack IFN-λ secretion in the lungs. They consistently develop more severe pulmonary pathology and higher long-term viral loads than their wild-type counterparts (157). Moreover, infection of MDA5-deficient mice results in the increased secretion of cytokines that promote neutrophil transepithelial migration and survival, such as CXCL1 (homologue of human CXCL8) and granulocyte colony-stimulating factor (G-CSF), as well as severe inflammation of the lung parenchyma (157).
Collectively, genetically modified mouse models have yielded strong evidence supporting the notion that the activation of RLR surveillance systems and their coupled transcription factors, IRF3 and IRF7, is a crucial mechanism that modulates paramyxoviral infection-elicited pathogenesis and T cell responses. Furthermore, Guerrero-Plata and coworkers (148) showed that lung pDCs display decreased secretion of type I IFNs after additional stimulation with the TLR9 agonist CpG. Therefore, HMPV may have active mechanisms that partially interfere with TLR- and RLR-dependent surveillance pathways and allow the discrete, but not necessarily functional, secretion of type I IFNs. The observation that IFNAR-driven responses contribute poorly to viral clearance further supports this notion and suggests that viral mechanisms also interfere with signal transduction downstream of IFNRs. In this regard, recent reports have indicated that infection of AECs with HMPV induces the downregulation of the IFNR and two key signaling tyrosine kinases driving the escalation of the IFN-β-driven response, Jak-1 and Tyk-2 (165). Importantly, by using a still unidentified mechanism, HMPV infection prevents the concatenated phosphorylation of Tyk2 and STAT-3 and the subsequent upregulation of IL-6-stimulated genes in AECs (166), suggesting an additional mechanism exploited by HMPV to negatively modulate the antiviral response of infected cells.
Finally, HMPV proteins impair PRR activation and the secretion and signaling of type I IFNs. As a result, the IFN response is dysfunctional at different levels. The HMPV proteins (M2-2, G, P, and SH) impair the sensing of viral RNAs and other virus-associated molecular patterns via various synergizing strategies. Specifically, M2-2 promotes the global evasion of TLR surveillance in monocyte-derived DCs (MDDCs), due to the interaction between this viral protein and the common signaling adaptor MyD88, which is critical for the activation of proinflammatory genes (167) (Fig. 4). In addition to interacting with MyD88, M2-2 also interacts with MAVS, impairing the upregulation of IFN-β in infected AECs (156). In contrast, the expression of the attachment glycoprotein G in AECs severely impairs signaling through RIG-I. This is due to the interaction of the cytoplasmic domain of G with the N terminus of this RNA helicase (154, 168). Furthermore, this protein-protein interaction leads to the uncoupling of RIG-I and MAVS, thus blunting downstream signaling and the secretion of chemokines and IFNs by infected AECs (154) (Fig. 4). Consistently, infection of AECs with HMPV lacking G induces a more marked activation of IRFs and NF-κB as well as stronger secretion of type I IFNs and chemokines (168). Using a similar approach, Bao and coworkers demonstrated that infection of human AECs with HMPV lacking the SH protein leads to both an increased phosphorylation of NF-κB and a strengthened secretion of the cytokines CCL2, CXCL1 (KC), tumor necrosis factor alpha (TNF-α), and interleukins 6 and 8 (124), thereby implying a redundant role for SH and G proteins in the hampering of NF-κB-driven responses. Finally, the phosphoprotein of HMPV B1 impairs the RIG-I-dependent recognition of viral 5′-triphosphate RNA via an unknown mechanism (155) (Fig. 4). Altogether, these proteins endow HMPV with synergizing mechanisms that favor early viral dissemination in the face of IFN and proinflammatory cytokine secretion.
The Acute Phase of Infection and Orchestration of Airway Inflammatory Hyperresponsiveness
Innate immunity to HMPV is initiated by the activation of PRRs that sense HMPV replication in the respiratory tract. These PRRs are widely expressed in phagocytic and epithelial cells and are competent at recognizing either viral proteins or RNA structures that are formed by viral RNA products synthesized during the replication cycle of HMPV. Besides IFN induction, PRR triggering rapidly upregulates several proinflammatory genes that activate the immunological network and lead to viral clearance at the expense of exacerbated pulmonary inflammation (Fig. 3).
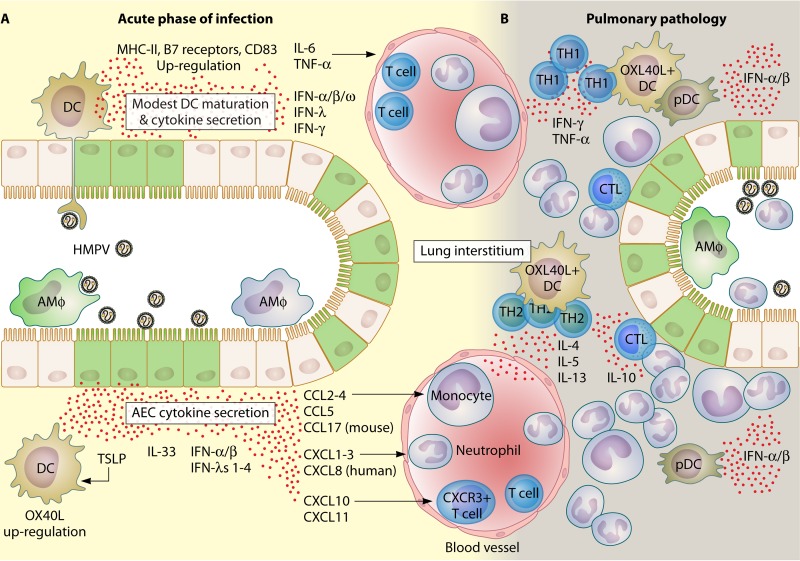
During the first 12 h postinfection, human AECs upregulate thymic stromal lymphopoietin (TSLP) and interleukins 1β, 6, and 33 (138). Moreover, HMPV-infected AECs secrete an important array of proinflammatory chemokines carrying CC and CXC motifs. CC-bearing chemokines include CCL2, CCL3, CCL4, and CCL5 (124, 167, 169). CXC-bearing chemokines include CXCL1, CXCL2, CXCL3, CXCL8/IL-8, CXCL10, and CXCL11 (124, 156, 169). Collectively, these ILs and chemokines are thought to be synergistic in the recruitment and activation of a significant repertoire of leukocytes mediating lung inflammation in HMPV-infected hosts (Fig. 5). For instance, TSLP and IL-33 are key activators of OX40L+ DCs (170, 171) and IL-13-secreting type 2 innate cells (nuocytes) (172), respectively. Both of these innate cell types mediate allergic responses. CCL2 is a chemoattractant for TH17 cells, monocytes, and plasmacytoid DCs (173, 174), whereas CCL3 and CCL4 both recruit and activate neutrophils under acute inflammatory conditions, such as coxsackievirus-induced myocarditis (175, 176). In contrast, CCL5 chemoattracts and increases the survival of macrophages, which are critical for the clearance of cells that have been destroyed by CTLs recognizing viral peptide-loaded major histocompatibility complexes (pMHCs) on their surface (177). CXCL1, CXCL2 (homologue of mouse CXCL2), and CXCL3 (homologue of mouse CXCL2) are important mediators of neutrophil transepithelial migration and activation (178, 179). Importantly, these CXC chemokines are likely synergizing with CXCL8, which is a major chemoattractant of human neutrophils (180), to mediate neutrophilic inflammation within the airways of HMPV-infected humans and mice (130). Additionally, CXCL10 is a modulator of T cell trafficking and preferentially attracts effector TH1 (and, to a lesser extent, TH2) cells expressing the chemokine receptor CXCR3 (181, 182). Finally, CXCL11 is a strong and selective chemoattractant for activated, CXCR3+ T lymphocytes (183). Therefore, the secretion of these cytokines suggests that AECs are key pulmonary sentinels that orchestrate the rapid influx of immune cells to mount an antiviral response to restrain HMPV dissemination in the respiratory tract. Moreover, because HMPV infection triggers the secretion of proinflammatory cytokines in DCs (144–147), DCs are important lung sentinels that locally aid in viral recognition and the initiation of acquired immune responses (Fig. 5). Among ILs, DCs secrete IL-6, which negatively modulates regulatory T (Treg) cell responses and promotes immune responses that are dependent on effector helper T cells and CTLs (184).
FIG 5.
Chain of events leading to pulmonary immunopathology following HMPV infection. Sensing of HMPV is the initial step that leads to pulmonary damage and inflammatory hyperresponsiveness. (A) During the acute phase of infection, AECs and DCs are the major populations that sense HMPV infections in the respiratory tract (149). Both infected AECs (green) and DCs secrete a vast repertoire of cytokines (148, 169, 186). Although DCs sense viral replication through PRRs, they develop only a poor to modest maturation response characterized by a mild upregulation of MHC-II, B7 receptors, and CD38. Chemokines bearing CC and CXC motifs are the most important cytokines that recruit and activate several immune cell subsets, including neutrophils, T cells, and monocytes, soon after initial exposure to HMPV. Alveolar macrophages (infected ones are shown in green) are important immune cells that promote pathology during the acute phase of infection. More specific effects have been attributed to the secretion of TSLP by HMPV-infected AECs. TSLP activates DCs (that upregulate OX40L) and leads to the activation and differentiation of T helper cells into a more pathogenic and poor antiviral phenotype (see panel B) (138, 171). (B) During established pulmonary pathology, TH1 cells (during the first 7 dpi) and TH2 cells (after 10 dpi) form perivascular infiltrates, where most cytokines that either impair viral clearance (IL-10) or promote and prolong airway inflammation (e.g., TNF-α, IL-6, IL-5, and IL-13) are secreted (220, 222). pDCs contribute to viral clearance by secreting type I IFNs. Infiltrating CTLs are the major effectors of viral clearance in infected tissue. Neutrophils are a dominant population that mediate the inflammation of HMPV-infected lungs and are also suspected targets for viral replication (138).
Because most mouse cytokines display a strikingly high degree of homology with their human counterparts and share common cellular targets and effector functions (185), the BALB/c model of infection has contributed enormously to the understanding of HMPV molecular pathogenesis. Furthermore, the mouse model has provided a strong proof of concept for the relevance of TSLP and IFNs, as well as other epithelial cell- and myeloid cell-derived cytokines, in immunity against HMPV. HMPV-infected mice exhibit secretion of several cytokines into the airways, as described for infected cultures of human AECs and DCs. For instance, granulocyte-macrophage colony-stimulating factor (GM-CSF), G-CSF, CXCL1, CCL3, CCL5, TNF-α, IFN-α, and interleukins 1α, 1β, 6, 10, 17, and 18 are found in the bronchoalveolar lavage fluids of HMPV-infected mice at 1 to 3 days postinfection (dpi) (186). At 3 to 10 dpi, IFN-γ and IL-12p40 are also detected, which correlates with the initiation of pulmonary T lymphocyte responses (187). Most chemokines found in HMPV-infected mice are chemoattractants for neutrophils, monocytes, and T cells (186). Importantly, we have found that among other cytokines, TSLP is strongly upregulated in mouse lungs during the acute phase of infection (24 h postinfection), thus implicating a possible role of this molecule in the pathogenesis of lung hyperresponsiveness (138). TSLP is recognized as a central molecule in the generation of HRSV-induced pulmonary disease in both children and rodents (188, 189). The binding of TSLP to its receptor (TSLPR) on the membrane of myeloid DCs triggers their activation. This process involves the upregulation of the T cell-activating ligand OX40L. During T cell priming, binding of OX40L to OX40 skews T cell differentiation toward a TH2 phenotype, which is deleterious for proper HRSV clearance (188, 189). Interfering with the TSLP-TSLPR system via either anti-TSLP neutralizing antibodies or TSLPR knockout mice significantly reduces the inflammatory response elicited by HMPV, thereby implicating a similar role for TSLP in the development of pneumonitis (138). Importantly, we detected the overexpression of OX40L in pulmonary CD11c+ MHC class II-positive (MHC-II+) cells, which include DCs and pulmonary macrophages, and observed a mixed T cell response with a more predominant TH1 phenotype (138). This suggests that the polarizing effects of TSLP are largely shaped by the pulmonary microenvironment. Interestingly, the diminished pathology in TSLPR-deficient mice is accompanied by reduced neutrophil infiltration and reduced viral replication in the lungs, thus reinforcing the link between viral replication and inflammation (138). A similar reduction in HMPV replication was found in neutrophil-depleted wild-type mice, suggesting that neutrophils are potential targets for infection (as are neutrophils in HRSV-infected children [190]). Alternatively, the inflammatory milieu may be optimal for HMPV replication (Fig. 5). On the other hand, we also observed strong upregulation of CCL17 mRNA (138), which is a potent chemoattractant for TH2 CD4+ cells and activated natural killer cells (191). Together, these cytokines promote the recruitment of neutrophils; professional APCs; and a mixed TH1, TH2, and TH17 repertoire, which are thought to be important orchestrators of the immunopathology triggered by HMPV in mice and humans (130, 138, 187).
Impairment of DC Function by HMPV and Implications for the Generation of Suboptimal Helper T Cell Immunity
Conventional DCs (cDCs) are pivotal professional APCs located in virtually all organs of the body as sentinels for pathogens (192, 193). After antigen uptake, the proteolytic machinery of DCs produces small peptides that are subsequently loaded onto the grooves of major histocompatibility complexes (pMHCs). Peptide-loaded MHCs work as ligands for the antigen receptor of T cells (known as the TCR [T cell receptor]). These MHCs trigger the activation of T cells upon contingent TCR triggering (which depends on the density of presented pMHCs) and the costimulation provided by the presenting DC (194, 195). T cell activation by DCs largely depends on the assembly of the immunological synapse (IS) in the interface of both cells. The IS serves as a scaffold for the delivery of activating signals to T cells, including antigenic class I and II pMHCs, and costimulation provided by the B7 receptors CD80 and CD86 (196). Because DCs express a broad array of PRRs, they also contribute to pathogen sensing and the initiation of the inflammatory response (197–199). Therefore, DCs are key components of the immune system, due to their role as both sentinels and APCs, leading the initiation, expansion, and maintenance of antiviral cellular immunity.
Maturation is a physiological mechanism by which activated DCs upregulate a number of membrane-bound and soluble molecules participating in the assembly of the IS and the activation of T cells (200). On their cell surface, mature DCs increase the density of MHC-I and MHC-II, B7 receptors (CD80 and CD86), and other molecules needed for efficient communication with T cells, such as CD40 and chemokine receptors needed for trafficking into secondary lymphoid tissues (201–203). Furthermore, mature DCs secrete cytokines with the capacity to skew the commitment of T cells toward phenotypes contingent on the threat sensed, including interleukins and transforming growth factor β1 (TGF-β1) (204). MHCs, B7 receptors, and cytokines are key signals provided to T cells synaptically engaged with activated DCs, which are commonly referred to as signals 1, 2, and 3, respectively (204). The intensities of these signals, particularly signals 1 and 2 (205), determine the outcome of T cell stimulation toward anergy (unresponsive phenotype), tolerance (regulatory phenotype), or immunity (effector phenotype). Therefore, the understanding of the dynamics that influence the capacity of HMPV-infected DCs to prime T cells has unraveled potential viral mechanisms leading to suboptimal adaptive immunity against HMPV.
DCs are competent in recognizing HMPV through PRRs and become phenotypically activated, as evidenced by the upregulation of T cell-costimulatory and proinflammatory molecules that synergize with those secreted by AECs (144–147). However, different groups agree that this maturation response is rather modest to poor (144–147). When observed, maturation of HMPV-infected DCs is accompanied by low to modest upregulation of MHC-II (in mouse and human DCs [145]) and MHC-I, B7 receptors (CD80 and CD86), CD40, CD38, and CD54 (in human DCs [144, 146, 147]) (Fig. 5A). Furthermore, infection of MDDCs by HMPV fails to induce the proper expression of the chemokine receptor CCR7 and to support the CCL19-driven migration of DCs to lymph nodes, where priming of naive T cells occur (206). Additional evidence suggests that HMPV does not actively suppresses DC maturation, as evidenced by the efficient upregulation of B7-1/B7-2, CD83, and CCR7 on the surface of infected DCs stimulated with lipopolysaccharide (147, 206). In fact, it seems that reduced DC maturation is derived from a limited sensing of viral RNA species due to the establishment of restricted or abortive HMPV replication in these APCs (144, 145, 147). Therefore, the poor DC maturation induced by HMPV provides a theoretical explanation for the suboptimal T cell memory observed in humans and mice. Interestingly, compared to the maturation response elicited by other paramyxoviruses, that of HMPV is low in terms of both cytokine secretion and the expression of maturation markers. HRSV induces a stronger cytokine response in human and mouse DCs, characterized by the secretion of significant amounts of G-CSF, TNF-α, and interleukins 1β, 10, and 12 (144, 207). Also, HRSV induces a more marked expression of maturation markers, including MHC-I/II, B7, and CD38 (the latter in human DCs) (144, 207). On the other hand, compared to HMPV, human parainfluenza virus type 3 (HPIV-3)-infected DCs show strong upregulation of CD80 and strong secretion of chemokines, including CCL2 to CCL5, CXCL8, and CXCL10 (146). These findings led to the notion that the exacerbated pulmonary inflammation caused by HRSV and HPIV-3 may be due in part to the increased activation of DCs in the respiratory tract (144). Furthermore, compared to HRSV and HMPV, HPIV-3 induces a strong downregulation of CD38, which is an important receptor that mediates chemotaxis and transendothelial migration of mature human DCs (146, 202). Importantly, since HPIV-3 also establishes reinfections throughout life, the latter evidence suggests that HMPV and HPIV-3 have developed different strategies to subvert DC migration as a common mechanism to blunt the development of T cell responses.
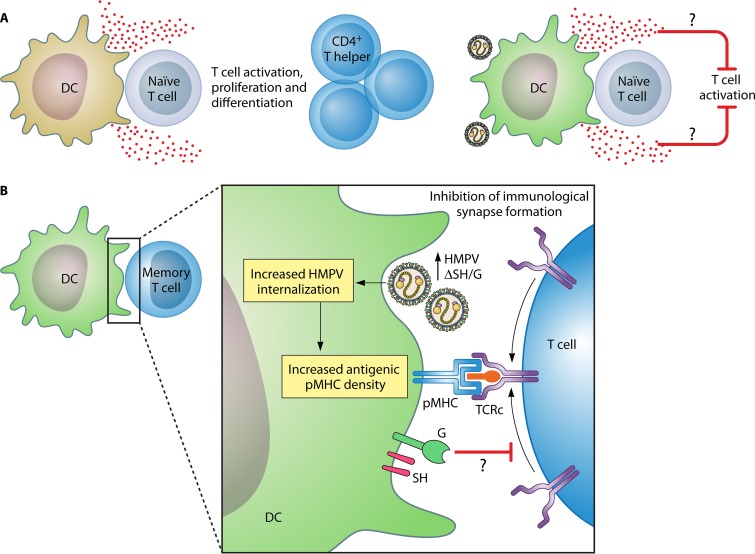
Compelling pieces of evidence suggest that HMPV impairs the communication between naive T cells and DCs at the immunological synapse, thus leading to suboptimal T cell priming and limited T cell memory (145, 148). The first piece of evidence came from work by Guerrero-Plata and coworkers, who demonstrated that cDCs from mouse lungs infected with HMPV fail to stimulate naive T cell proliferation in vitro (148). This suggests that infection of DCs by HMPV leads to impaired antigen presentation to T cells. Delving deeper into the possible mechanism, we have demonstrated that (i) impairment of naive T cell priming is dependent on infection of DCs by HMPV and (ii) inhibition of CD4+ T cell priming occurs even at lower multiplicities of infection of DCs (145). Furthermore, inhibition of T cell priming at low DC/T cell ratios suggests that HMPV can efficiently blunt naive T cell priming in various settings (145) (Fig. 6A). Finally, impairment of CD4+ T cell priming occurs via soluble factors that are secreted by HMPV-infected DCs in the absence of any interference with immunological synapse formation (T cell Golgi apparatus polarization) (145). These reports all indicate that infection of DCs by HMPV ends in the suboptimal stimulation of helper CD4+ T cells (TH cells), which may subsequently mediate poor viral clearance and favor airway hyperreactivity.
FIG 6.
HMPV impairs T cell-dependent immunological processes by interfering with the function of DCs. (A, left) Priming of naive T cells by DCs is a pivotal process for the initiation and expansion of immune responses dependent on CD4+ and CD8+ T cells. (Right) HMPV-infected DCs impair naive T cell activation despite the efficient trapping of the Golgi apparatus of stimulated naive T cells (145). Inhibition of T cell priming is partially dependent on the secretion of soluble factors by HMPV-infected DCs, which impair the upregulation of the TCR-driven activation marker CD69 and the proliferation of stimulated T cells. These soluble factors have yet to be identified (145). (B) The G and SH proteins of HMPV are thought to impair the activation of memory CD4+ T cells by interfering with the assembly of the immunological synapse (123). The impairment of synapse assembly is related to the impediment of TCR complex (TCRc) recruitment to the DC-T cell interface either via the effects of binding of G and SH to key molecules of the synapse or by reducing the density of new antigenic pMHCs due to an impaired internalization of viral antigens by DCs. The TCR complex is a complex of integral membrane proteins, including the TCR heterodimer, the ζ-chain, and four CD3 subunits, which participate in the activation of T cells upon antigen recognition.
Opposing data with respect to the capacity of HMPV to inhibit the activation of human memory CD4+ T cells have been reported. Although some groups found no differences in the proliferation of CD45RO+ CD4+ T cells stimulated with HMPV-infected MDDCs (144, 208), others found that HMPV impairs signaling at the immunological synapse (123). Because suboptimal T cell memory is thought to originate at the level of naive T cell stimulation (145, 148) and not at the level of recall responses of antigen-experienced (CD45RO+) T cells, these findings do not necessarily argue against the current model of impaired T cell priming. In fact, disparities in the susceptibilities of naive and antigen-experienced T lymphocytes have also been documented in the case of DCs infected with HRSV, which fail only in the activation of cells with no antigen experience (207, 209). Presumably, this difference is linked to the increased sensitivity of memory T cells to antigen (signal 1) (210). Compared to HRSV, influenza A virus (IAV), and HPIV-3, HMPV is a poor inducer of T cell proliferation after the infection of MDDCs (208). Although this difference is not significant, it was observed for most donors, implying alternatively that adults may have a more scarce population of circulating memory CD4+ T cells that are reactive against HMPV antigens, which may also explain susceptibility to reinfections (208). Compared to IAV and HRSV, HMPV-infected MDDCs also activate TH1 cells less efficiently, as evidenced by the reduced proportion of IFN-γ+ and TNF-α+ T cells after 7 days of stimulation (208). In a more recent work, Le Nouen and coworkers showed that infection of monocyte-derived DCs with HMPV, but not HMPV lacking SH and G (HMPVΔSHG), impairs the activation of autologous memory CD4+ TH cells, suggesting that G and SH are key virulence factors that hamper T cell recall responses (123). Impaired T cell activation is accompanied by reduced CD3 accumulation, which is a hallmark of TCR triggering and immunological synapse formation, in the interface of T cells and wild-type HMPV-infected DCs. Importantly, the potential inhibition of G and SH proteins is (i) observed early in DC-T cell cocultures, (ii) dependent on the inhibition of macropinocytosis of viral particles, and (iii) observed even with UV-inactivated HMPV (123). Therefore, HMPVΔSHG-infected DCs may exhibit an increased density of antigenic pMHCs due to the efficient transcription of HMPVΔSHG compared to wild-type HMPV, thus promoting a better activation of T cells, which would argue against direct effects of SH and G on the impairment of T cell activation. Although less likely, uninternalized viral particles may exert steric hindrance on the surface of DCs and impair the proper delivery of activating signals to T cells. As we demonstrated for the HRSV nucleoprotein (210), corroboration of immunological synapse inhibition, as well as the molecular mechanisms causing reduced accumulation of CD3, would require functional assays using supported lipid bilayers loaded with antigenic pMHCs and the HMPV G and SH proteins (Fig. 6B). This will further expand our understanding of the key molecules affecting T cell responses and will open new opportunities for vaccine development.
Because the initial step of T cell priming is also relevant for the induction of cellular immunological memory, the impairment of DC function by HMPV may explain the development of suboptimal immunological memory and susceptibility to reinfection in humans (211, 212). The HMPV-exerted interference with CD4+ T cell priming may be advantageous for viral dissemination, due to interference with many downstream immune processes that are driven by TH cells, such as (i) the recruitment and restimulation of antiviral T cell repertoires, (ii) viral clearance by CTLs, (iii) licensing of DCs for CD8+ T cell activation, and (iv) activation of B cells by TH cells (213–215). The limited help provided by TH cells may have strong negative repercussions for the quality of antibody responses mounted against relevant antigens, such as the F protein. To date, there has been no study demonstrating direct deleterious effects of HMPV on the humoral immune response of humans and model animals. However, independent studies have shown that healthy adults become reinfected, either experimentally (34) or naturally, in the face of 80 to 100% seroprevalence against HMPV (15, 216, 217), suggesting that HMPV may have evolved mechanisms that interfere with the proper development of antibody-dependent immunity. Along this line, others have proposed that the humoral response plays a minor role in the clearance of HMPV (16) based on the observation that HMPV recirculates in the population despite the fact that humans of all age groups maintain significant titers of neutralizing antibodies. Moreover, only 35% of experimentally infected adults mount a detectable antibody response, reinforcing the notion of viral interference with B cell immunity development (34). Mechanistically, inefficient B cell immunity to infection may originate from the alteration of a number of immunological processes spanning from an impairment of B cell differentiation, due to limited TH cell help, to defective effector mechanisms in the pool of HMPV-specific immunoglobulins generated in the context of repeated natural infections. Moreover, the notion of aberrant acquired immunity to natural infections is also supported by the observation that an HMPV-specific memory CD8+ T cell repertoire that is reactive to most viral proteins, including M, F, M2-1, G, N, and SH, expands in adults suffering from respiratory disease (218). Part of this CTL repertoire is specific for M and F epitopes and may last up to 21 months postinfection (218); however, it appears to contribute minimally to the control of reinfections, which are more severe in adults >65 years of age. Although natural infection-acquired immunity of healthy adults fails to prevent HMPV reinfections, it is sufficient to prevent more severe forms of ARTIs, such as pneumonitis and bronchiolitis. Thus, by reducing adaptive antiviral immunity, HMPV escapes immune destruction, favors reinfection in healthy adults (mostly subclinical) and other susceptible individuals, and ultimately promotes its recirculation in the community.
Acquired Immunity to HMPV Infection and Contribution to Pathogenesis
In children, HMPV produces a self-limited infection that is associated with pathological, chronic, and degenerative alterations in the lower respiratory epithelium as well as chronic inflammation with participation of lymphocytes and other mononuclear cells (130, 219). As for children, adults experimentally infected with HMPV release infectious viral particles for 7 to 9 days, supporting the short-term nature of HMPV shedding in humans (34). The BALB/c mouse infection model has yielded strong evidence linking the activation of adaptive immunity with viral clearance and the generation of chronic airway inflammation and hyperresponsiveness. In fact, TH cells and CTLs cooperate to clear the virus from the airways and also promote lung pathology during the primary immune response of naive animals to HMPV (220). More specifically, the depletion of specific T cell subsets led to the notion that TH cells, more than CD8+ CTLs, are key components in the pathogenic response to HMPV in mice (220). In agreement with this notion, CD8+ CTL responses are capable of eliminating HMPV from the lungs, even in the absence of TH cells and a detectable B cell response (220). This suggests that helper T cells generate an immunological milieu that is deleterious for proper cytotoxic activity. In this regard, HMPV infection elicits a delayed CTL response that develops alongside an aberrant T helper response correlating with poor viral clearance in the lungs (187). More specifically, in infected mice, HMPV induces an initial TH1-biased T cell response that skews toward a mixed TH1/TH2 response at 10 days postinfection (187). This mixed TH response is composed of a significant proportion of lymphocytes that secrete IL-10 (187), which is a key immunomodulatory cytokine that prevents viral clearance due to the regulation of cellular antiviral immunity (221). Moreover, although CTLs that infiltrate the lungs of infected mice are competent in secreting IFN-γ and inducing lysis of infected cells in vitro (187, 222), they fail at eliminating the virus from the airways. Erickson and coworkers recently extended the understanding of the mechanisms responsible for impaired CTL responses in the respiratory tract of mice acutely infected with HMPV. They demonstrated that upon antigen recognition in the lungs, CD8+ T cells rapidly become exhausted due to the upregulation of PD-1 and other inhibitory receptors (223). Therefore, the infection-generated immunological milieu appears to dampen the efficient clearance of HMPV in vivo. Mice lacking a functional TSLP-TSLPR pathway (i.e., tslpr−/− mice) show an increased infiltration of TH cells and CTLs in the lungs and a significant reduction in viral replication (138). Importantly, HMPV infection of tslpr−/− mice elicits a helper T cell response with a significantly different profile of cytokines, including a reduced proportion of CD4+ TH cells secreting TNF-α and interleukins 4, 10, and 13 as well as an overall reduction in lung IL-4, IL-5, and IL-13 mRNA levels (TH2 cytokines) (138). In summary, these results lead to the notion that the immunological milieu elicited by infection with HMPV significantly influences the effector response of virus-specific CTLs and the development of pulmonary pathology. These findings also indicate that the pathogenic role of T cells during primary infection depends on the immunological context and is not exclusively dependent on the phenotype of the expanded TH cell repertoire.
The aberrant adaptive antiviral immunity that is elicited by primary infection of BALB/c mice is also depicted by the generation of suboptimal humoral immunity that fails to fight HMPV persistence in the lower respiratory tract but that is capable of transferring partial protection to naive mice, due to the production of neutralizing antibodies (139, 187). Although the humoral immune response of BALB/c mice efficiently neutralizes the virus in vitro, it fails to eliminate pulmonary cells infected with HMPV (139). Similarly, we have observed that immunization with two subdermal injections of viable HMPV fails to protect mice from a subsequent challenge (97), suggesting that HMPV efficiently hampers B cell immunity. Because key B cell activation and differentiation processes, such as antibody affinity maturation and antibody isotype switching, depend on proper aid from TH cells, these findings indicate that suboptimal humoral immunity may be derived from viral interference in the function of helper T cells (224).
Animal Models for the Study of HMPV-Induced Pathogenesis
An ideal animal model for human disease must recapitulate the pathophysiology of a given disorder as close as possible. For the preclinical exploration of the mechanism of HMPV pathogenesis and the identification of novel therapeutics and vaccines, several animal models have been tested so far (reviewed in reference 11). Mice, cotton rats, ferrets, hamsters, and nonhuman primates support HMPV replication in the lungs and develop ARTIs, with various degrees of susceptibility (97, 98, 103, 127, 138, 225–231). Animal studies have contributed enormously to the preclinical evaluation of vaccine candidates and helped in the identification of immunological mechanisms that confer immunity against experimental infections (summarized in Table 1) (85, 91, 97, 103, 126, 227, 229, 230, 232–239). At the molecular level, the mouse model of infection has yielded the majority of evidence regarding potential pathophysiological mechanisms related to HMPV lung disease (132, 138, 148, 159, 160, 220, 223, 240, 241). Despite this body of information, however, a debate has been raised regarding the usefulness of the mouse model in understanding the response of humans against HMPV. The latter is based on the observation that compared to cotton rats, hamsters, and rhesus macaques, HMPV replicates poorly in the lungs of mice, which is considered an important drawback for translating the conclusions obtained from mice to humans (225, 226, 231, 242). Arguing against this notion, it is worth mentioning that HMPV-infected mice replicate the pulmonary pathology of humans in several aspects, including histopathology, the secretion of inflammatory mediators, and the recruitment of immune cells (132, 138, 187, 240). Although for humans, it is acknowledged that disease severity is associated with age and viral load in lungs, mice replicate human disease in the face of modest viral replication and also replicate age-related immunological deficiencies (243). Furthermore, compared to other animal models, we have gained a considerably better understanding of the differences and similarities in the functioning of the human and mouse immune systems. Conservation in the transcriptional landscape of >64% of orthologous genes controlling the activation and regulation of human and mouse T cells has been demonstrated (244), suggesting that the laboratory mouse is a good model for understanding the association between the modulation of host immunity and the development of pulmonary pathology. However, one major drawback is translating to humans the pathogenic roles and the diversity of immunodominant epitopes found within the T cell repertoire elicited in HMPV-infected mice, which differ from those seen in humans (summarized in Table 2) (160, 218, 222, 245, 246).
TABLE 1.
Principal experimental vaccine strategies developed to prevent HMPV infection
| Technology | Basis | Animal model(s) | Immune response | Reference(s) |
|---|---|---|---|---|
| Inactivated virus | Virus inactivated with formalin | Cynomolgus macaques, cotton rats | Strong immunopathology by TH2-type antibodies (neutralizing) | 238, 239 |
| Viral proteins | DNA-vectorized F protein | Cotton rats | Not protective, TH2-type antibodies | 126 |
| Iscomatrix F protein | Cynomolgus macaques | Not protective, TH2-type antibodies | 225 | |
| Live attenuated virus | Deletion of SH and G genes | Hamster | Immunogenic inducer of protecting TH2-type antibodies | 236 |
| Deletion of M2-1 and M2-2 genes | Hamster | Immunogenic inducer of protecting TH2-type antibodies | 85 | |
| Deletion of SH, G, and M2-2 genes | Primates | Immunogenic inducer of protecting TH2-type antibodies | 103 | |
| Removal of carbohydrate moiety of F protein | BALB/c mice | Immunogenic inducer of protecting TH2-type antibodies | 235 | |
| L mutant with impaired cap methyltransferase activity | Cotton rats | Immunogenic inducer of protecting TH2-type antibodies | 242 | |
| Chimeric constructions | Replacement of N and P genes for heterologous genes from an avian strain | Primates, hamster | Immunogenic inducer of protecting TH2-type antibodies | 227 |
| Attenuated strain of parainfluenza virus expressing the G protein of HMPV | Hamster | Immunogenic inducer of protecting TH2-type antibodies | 230 | |
| Attenuated strain of parainfluenza virus expressing the F protein of HMPV | Primates | Immunogenic inducer of protecting TH2-type antibodies | 229 | |
| Equine encephalitis virus expressing the F protein of HMPV | Primates | Immunogenic inducer of protecting TH2-type antibodies | 234 | |
| Virus-like particles | Retroviral core particles that express the G and F proteins of HMPV | BALB/c mice | Immunogenic inducer of protecting TH2-type antibodies | 233 |
| Human embryonic kidney epithelial (293-F) cells expressing M and F proteins of HMPV | C57BL/6 mice | TH2-type antibodies and TH1 cellular response | 232 | |
| Recombinant bacteria | Recombinant BCG expressing P protein of HMPV | BALB/c mice | Immunogenic inducer of protecting TH1 cellular response | 97 |
TABLE 2.
T cell epitopes in humans and mice exposed to HMPVa
| HMPV protein | Epitope sequence | Species; MHC restriction | Cellular immunity generated | Mode(s) of antigen delivery | Reference(s) |
|---|---|---|---|---|---|
| N11–19 | LSYKHAILK | Mouse; H2-Kb | TCD8, IFN-γ secretion | Experimental infection | 160 |
| N164–172 | VGALIFTKL | Mouse; H-2Kb | CTLs, IL-12 and IFN-γ secretion | Peptide immunization | 245 |
| N198–206 | YPRMDIPKI | Mouse; B7tg (restricted to HLA-B*0702) | Splenocytes, IFN-γ secretion | Experimental infection | 160 |
| M12–20 | IPYTAAVQV | Human; HLA-B7 | PBMCs, IFN-γ secretion; cytotoxicity | Natural viral infection | 218 |
| M94–112 | VALDEYSKL | Mouse; H2-Kb and B7tg (restricted to HLA-B*0702) | CTLs, IFN-γ secretion | VLP vaccination | 246 |
| M194–203 | IAPYAGLIMI | Human; HLA-B7, -B51, -B55 | PBMCs, IFN-γ secretion; cytotoxicity | Natural viral infection | 218 |
| M195–203 | APYAGLIM | Mouse; B7tg (restricted to HLA-B*0702) | Splenocytes, IFN-γ secretion | Experimental infection, VLP vaccination | 160, 246 |
| F528–536 | SGVTNNGFI | Mouse; H2-Db | TCD8, CTLs, IFN-γ secretion | Experimental infection, VLP vaccination | 160, 246 |
| M2.181–89 | GYIDDNQSI | Mouse; H-2Kd | Splenocytes, IFN-γ secretion | Experimental infection | 222 |
| M2.256–64 | CYLENIEII | Mouse; H-2Kd | CTLs, IL-12 and IFN-γ secretion | Peptide immunization | 245 |
| SH35–44 | KLILALLTFL | Human; HLA-A*0202 | CTLs, IL-12 and IFN-γ secretion | Peptide immunization | 245 |
| G32–41 | SLILIGITTL | Human; HLA-A*0201 | CTLs, IL-12 and IFN-γ secretion | Peptide immunization | 245 |
PBMCs, peripheral blood mononuclear cells; VLP, virus-like particle; TCD8, CD8+ T cells.
CONCLUDING REMARKS
HMPV causes ARTIs that produce a significant economic and public health burden worldwide. Significant efforts have been invested in understanding both the pathophysiology of pulmonary disease and the origins of the poor acquired immunity elicited by natural infections. Although preliminary, our current understanding of the disease determinants that contribute to the pathogenesis of airway inflammation highlights the contribution of the TSLP-TSLPR pathway as a candidate target for the development of palliative treatments against the disease. Furthermore, IFN-λs offer additional therapeutic opportunities as both antiviral agents and modulatory drugs for the development of inflammatory hyperresponsiveness in lungs of infected individuals.
Interference in DC function has been highlighted as an instrumental strategy that is exploited by HMPV to subvert the activation, proliferation, and maintenance of TH cell responses and the downstream activation of B lymphocytes. Therefore, the characterization of viral proteins that impair helper T cell activation may open new and exciting opportunities for the development of rational vaccines for preventing lower ARTIs in children and the elderly.
Members of the Paramyxoviridae family have evolved nonstructural proteins that interfere with key proteins involved in the interferon-signaling cascade in AECs. For instance, within the Respirovirus genus, the C protein of Sendai virus inhibits the phosphorylation of IRF7 (247), and the V proteins of HPIV-1 and -3 are thought to inhibit STAT-1 and STAT-2 (reviewed in reference 248). Similarly, the V proteins of viral species belonging to the Morbillivirus genus, including measles and canine distemper viruses, prevent the transcription of ISGs by abrogating the nuclear translocation of STAT-1 and STAT-2 (249, 250). In addition, V proteins inhibit the phosphorylation of Tyk2 and Jak1, which are key IFNR-associated kinases (251). The latter blunts the signaling of IFN-γ and type I IFNs. Furthermore, V proteins interact with RNA helicases, such as MDA5 and LGP2, to prevent signaling through PRRs and the very first sensing of viral RNAs in epithelial cells (252, 253). Regarding proteins in the Pneumovirus genus, the HRSV NS1 and NS2 proteins target STAT-2 for degradation (254, 255). Altogether, these findings exemplify how distinct paramyxoviruses have evolved synergistic or redundant mechanisms to blunt the host interferon response affecting pivotal signaling molecules. From an evolutionary perspective, while HMPV lacks nonstructural proteins dedicated to the abrogation of the IFN response, it is feasible that the pressure imposed by the human immune system may have participated in the selection of structural proteins with secondary roles to compensate for such a genetic deficiency. Although in >10 years, we have accumulated a significant body of information regarding how HMPV escapes immune recognition, this information landscape is rather preliminary. As we gain an understanding of the host-HMPV interactome, it will undoubtedly stimulate the development of novel therapeutics as well as unravel the contributions of the IFN response to the still poorly comprehended disease manifestations.
Several unresolved debates regarding the role of HMPV in the genesis and/or progression of lung inflammatory conditions in humans remain to be elucidated, including (i) the real contribution of host immune modulation to the exacerbation of chronic, progressive diseases, such as TH1-associated COPD (256), and (ii) whether HMPV contributes to SARS lethality by enhancing lung tissue destruction and loss of functionality. Considering that neurological symptoms associated with the presence of viral genetic material in the central nervous system (CNS) have been observed in severely ill patients, we need to explore whether blunting of host interferon responses and T cell immunity may have a particular role in the promotion of viral spread to nervous tissue. A recent clinical study detected HMPV in two serum samples taken 4 days apart from a hematopoietic cell transplant recipient (70), suggesting that immunosuppression may favor HMPV viremia. Lessons learned from viruses from other taxa, including members of the Paramyxoviridae and Orthomyxoviridae families, suggest that beyond having surface glycoproteins with the capacity to bind receptors and initiate infection in the CNS, neurotropic viruses also require virulence mechanisms to blind host immunity and disseminate systemically (257–263). Studies in mice, cotton rats, and macaques using a number of HMPV strains have shown no dissemination of HMPV to the brain, other organs, or the blood (135, 141, 232, 241, 255), suggesting either that HMPV may not be a bona fide neurotropic virus or that these models are inappropriate models for studying this particular subject. The selective pressure of the host immune system may have had a role selecting HMPV proteins that promote the modulation of the IFN response. Therefore, new research should first consider the evaluation of viral determinants that may favor systemic dissemination of HMPV in humans. To date, there is no study demonstrating the presence of functional HMPV receptors in CNS tissue. Clinical studies aiming to solve the association of neurological disorders and demonstrable brain infections, as well as molecular epidemiology studies seeking protein variability in HMPV virulence determinants and host immune components, may further pave the road toward understanding the pathogenesis of encephalitis in HMPV-infected humans.
ACKNOWLEDGMENTS
This work was funded by the National Fund for Scientific and Technological Development (FONDECYT) from the Ministry of Economy, Chile (grant no. 1070352, 1140010, and 1150862 and postdoctorate grant no. 3140455); the Corporación de Fomento de la Producción (CORFO) from the Ministry of Economy, Chile (grant no. 11IDL2-10668, 13CTI-21526-P4, and 13CTI-21526-P5); the National Corporation of Science and Technology from the Ministry of Economy, Chile (CTU-06); and the Iniciativa Científica Milenio from the Ministry of Economy, Chile (P09-016-F).
The funders had no role in determining the content of the paper and did not participate in the decision to submit the work for publication.
Biographies

Pablo F. Céspedes earned his Veterinary Medicine degree at the Universidad de Chile and obtained his M.Sc. and Ph.D. in Molecular Genetics and Microbiology at the Pontificia Universidad Católica de Chile (PUCC). His Ph.D. thesis focused on understanding the modulation of the immunological synapse by respiratory viruses. Currently, he is performing postdoctoral training at the School of Biological Sciences at the Pontificia Universidad Católica de Chile, evaluating the activation and expansion of T cells in response to primary infections and vaccination and elucidating virulence mechanisms used by pneumoviruses to blunt acquired cellular and humoral immunity. Dr. Céspedes has been awarded doctoral and postdoctoral fellowships by CONICYT Chile and has been supported by the Millennium Institute on Immunology and Immunotherapy as a young scientist.

Christian E. Palavecino earned his Medical Technologist degree at the Universidad Austral de Chile. He then earned his M.Sc. and Ph.D. in Microbiology from the Universidad Austral de Chile. Dr. Palavecino was awarded an Alban office grant to develop his Ph.D. thesis at the Queen Mary University of London to investigate the molecular basis of Mycobacterium-host interactions. He is currently working as a postdoctoral fellow at the School of Biological Sciences at the Pontificia Universidad Católica de Chile, focusing his research on vaccine development to prevent human metapneumovirus infection.

Alexis M. Kalergis is Full Professor at the School of Biological Sciences and Medicine of the PUCC. He obtained the Julius Marmur Award for his M.Sc. and Ph.D. work on Microbiology and Immunology at the Albert Einstein College of Medicine in New York. He performed postdoctoral training at the AECM and The Rockefeller University, supported by the Helen Hay Whitney Foundation. He has trained over a hundred young scientists, lectured at countless conferences, and published over 140 articles. He is a member of the American Society of Immunology; the American Society for Microbiology; and the Chilean Societies for Biology, Cell Biology, and Immunology. He was selected as the most outstanding young scientist by the Biology Society of Chile, as one of the 50 Chilean young leaders, and awarded several important national and international research grants. He is the Director of the Millennium Institute on Immunology and Immunotherapy, a Research Excellence Center that was recently selected as a FOCIS Center of Excellence in the United States. He created a Consortium on Biomedicine, which is the largest grant in this area awarded to a University-Company alliance in Chile. His group has recently developed a new vaccine against HRSV that is currently in clinical trials. His research focuses on the molecular interactions regulating the T cell-DC synapse and their contribution to pathogen immunity and self-tolerance during autoimmunity.

Susan M. Bueno is an Associate Professor at the Department of Molecular Genetics and Microbiology, School of Biological Sciences, Pontificia Universidad Católica de Chile, and Principal Investigator at the Millennium Institute on Immunology and Immunotherapy. Dr. Bueno earned her Medical Technologist degree and her Ph.D. in Biomedical Sciences at the Universidad de Chile. She then performed postdoctoral training at the Pontificia Universidad Católica de Chile, working on the molecular basis of immune escape of pathogenic bacteria and viruses as well as vaccine design for respiratory pathogens. Dr. Bueno has published over 70 articles in leading microbiology and immunology journals. She is an active member of the American Association of Immunologists, the American Society for Microbiology, and the Chilean Societies for Microbiology and Immunology. Currently, she leads the laboratory of microbial pathogenesis and molecular immunology at the PUCC, which focus on host-pathogen interactions involved in systemic bacterial infections and pneumonia.
REFERENCES
- 1.WHO. 2014. World Health Organization/Global Health Observatory data repository. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 2.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Jha P, Campbell H, Walker CF, Cibulskis R, Eisele T, Liu L, Mathers C, Child Health Epidemiology Reference Group of WHO and UNICEF. 2010. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375:1969–1987. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 3.Papenburg J, Boivin G. 2010. The distinguishing features of human metapneumovirus and respiratory syncytial virus. Rev Med Virol 20:245–260. doi: 10.1002/rmv.651. [DOI] [PubMed] [Google Scholar]
- 4.van den Hoogen BG, de Jong JC, Groen J, Kuiken T, de Groot R, Fouchier RA, Osterhaus AD. 2001. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med 7:719–724. doi: 10.1038/89098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang CF, Wang CK, Tollefson SJ, Piyaratna R, Lintao LD, Chu M, Liem A, Mark M, Spaete RR, Crowe JE Jr, Williams JV. 2009. Genetic diversity and evolution of human metapneumovirus fusion protein over twenty years. Virol J 6:138. doi: 10.1186/1743-422X-6-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Graaf M, Osterhaus AD, Fouchier RA, Holmes EC. 2008. Evolutionary dynamics of human and avian metapneumoviruses. J Gen Virol 89:2933–2942. doi: 10.1099/vir.0.2008/006957-0. [DOI] [PubMed] [Google Scholar]
- 7.van den Hoogen BG, Herfst S, Sprong L, Cane PA, Forleo-Neto E, de Swart RL, Osterhaus AD, Fouchier RA. 2004. Antigenic and genetic variability of human metapneumoviruses. Emerg Infect Dis 10:658–666. doi: 10.3201/eid1004.030393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Papenburg J, Carbonneau J, Isabel S, Bergeron MG, Williams JV, De Serres G, Hamelin ME, Boivin G. 2013. Genetic diversity and molecular evolution of the major human metapneumovirus surface glycoproteins over a decade. J Clin Virol 58:541–547. doi: 10.1016/j.jcv.2013.08.029. [DOI] [PubMed] [Google Scholar]
- 9.Al-Turab M, Chehadeh W, Al-Nakib W. 2015. Phylogenetic analysis of human metapneumovirus detected in hospitalized patients in Kuwait during the years 2009-2011. J Infect Public Health 8:448–457. doi: 10.1016/j.jiph.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Kahn JS. 2006. Epidemiology of human metapneumovirus. Clin Microbiol Rev 19:546–557. doi: 10.1128/CMR.00014-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schildgen V, van den Hoogen B, Fouchier R, Tripp RA, Alvarez R, Manoha C, Williams J, Schildgen O. 2011. Human metapneumovirus: lessons learned over the first decade. Clin Microbiol Rev 24:734–754. doi: 10.1128/CMR.00015-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crowe JE., Jr 2004. Human metapneumovirus as a major cause of human respiratory tract disease. Pediatr Infect Dis J 23:S215–S221. doi: 10.1097/01.inf.0000144668.81573.6d. [DOI] [PubMed] [Google Scholar]
- 13.Williams JV, Harris PA, Tollefson SJ, Halburnt-Rush LL, Pingsterhaus JM, Edwards KM, Wright PF, Crowe JE Jr. 2004. Human metapneumovirus and lower respiratory tract disease in otherwise healthy infants and children. N Engl J Med 350:443–450. doi: 10.1056/NEJMoa025472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams JV, Wang CK, Yang CF, Tollefson SJ, House FS, Heck JM, Chu M, Brown JB, Lintao LD, Quinto JD, Chu D, Spaete RR, Edwards KM, Wright PF, Crowe JE Jr. 2006. The role of human metapneumovirus in upper respiratory tract infections in children: a 20-year experience. J Infect Dis 193:387–395. doi: 10.1086/499274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lu G, Gonzalez R, Guo L, Wu C, Wu J, Vernet G, Paranhos-Baccala G, Wang J, Hung T. 2011. Large-scale seroprevalence analysis of human metapneumovirus and human respiratory syncytial virus infections in Beijing, China. Virol J 8:62. doi: 10.1186/1743-422X-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lusebrink J, Wiese C, Thiel A, Tillmann RL, Ditt V, Muller A, Schildgen O, Schildgen V. 2010. High seroprevalence of neutralizing capacity against human metapneumovirus in all age groups studied in Bonn, Germany. Clin Vaccine Immunol 17:481–484. doi: 10.1128/CVI.00398-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeng L, Chen R, Ishigami K, Atsumi M, Koizumi Y, Sato K, Iritani O, Okuro M, Morimoto S. 2011. Association between human metapneumovirus seroprevalence and hypertension in elderly subjects in a long-term care facility. Hypertens Res 34:474–478. doi: 10.1038/hr.2010.268. [DOI] [PubMed] [Google Scholar]
- 18.Williams JV, Edwards KM, Weinberg GA, Griffin MR, Hall CB, Zhu Y, Szilagyi PG, Wang CK, Yang CF, Silva D, Ye D, Spaete RR, Crowe JE Jr. 2010. Population-based incidence of human metapneumovirus infection among hospitalized children. J Infect Dis 201:1890–1898. doi: 10.1086/652782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams JV, Crowe JE Jr, Enriquez R, Minton P, Peebles RS Jr, Hamilton RG, Higgins S, Griffin M, Hartert TV. 2005. Human metapneumovirus infection plays an etiologic role in acute asthma exacerbations requiring hospitalization in adults. J Infect Dis 192:1149–1153. doi: 10.1086/444392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martinello RA, Esper F, Weibel C, Ferguson D, Landry ML, Kahn JS. 2006. Human metapneumovirus and exacerbations of chronic obstructive pulmonary disease. J Infect 53:248–254. doi: 10.1016/j.jinf.2005.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ilvan A, Aslan G, Serin MS, Calikoglu M, Yilmaz FM, Tezcan S, Tas D, Ayrik C, Uygungul E, Sezer O, Emekdas G. 2013. Investigation of the presence of human metapneumovirus in patients with chronic obstructive pulmonary disease and asthma and its relationship with the attacks. Mikrobiyol Bul 47:636–649. (In Turkish.) doi: 10.5578/mb.6041. [DOI] [PubMed] [Google Scholar]
- 22.Djamin RS, Uzun S, Snelders E, Kluytmans JJ, Hoogsteden HC, Aerts JG, Van Der Eerden MM. 2015. Occurrence of virus-induced COPD exacerbations during four seasons. Infect Dis (Lond) 47:96–100. doi: 10.3109/00365548.2014.968866. [DOI] [PubMed] [Google Scholar]
- 23.Dosanjh A. 2015. Respiratory metapneumoviral infection without co-infection in association with acute and chronic lung allograft dysfunction. J Inflamm Res 8:79–82. doi: 10.2147/JIR.S78259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chan PK, Tam JS, Lam CW, Chan E, Wu A, Li CK, Buckley TA, Ng KC, Joynt GM, Cheng FW, To KF, Lee N, Hui DS, Cheung JL, Chu I, Liu E, Chung SS, Sung JJ. 2003. Human metapneumovirus detection in patients with severe acute respiratory syndrome. Emerg Infect Dis 9:1058–1063. doi: 10.3201/eid0909.030304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Poutanen SM, Low DE, Henry B, Finkelstein S, Rose D, Green K, Tellier R, Draker R, Adachi D, Ayers M, Chan AK, Skowronski DM, Salit I, Simor AE, Slutsky AS, Doyle PW, Krajden M, Petric M, Brunham RC, McGeer AJ, National Microbiology Laboratory, Canada, Canadian Severe Acute Respiratory Syndrome Study Team. 2003. Identification of severe acute respiratory syndrome in Canada. N Engl J Med 348:1995–2005. doi: 10.1056/NEJMoa030634. [DOI] [PubMed] [Google Scholar]
- 26.Vicente D, Montes M, Cilla G, Perez-Trallero E. 2004. Human metapneumovirus and chronic obstructive pulmonary disease. Emerg Infect Dis 10:1338–1339. doi: 10.3201/eid1007.030633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boivin G, Abed Y, Pelletier G, Ruel L, Moisan D, Cote S, Peret TC, Erdman DD, Anderson LJ. 2002. Virological features and clinical manifestations associated with human metapneumovirus: a new paramyxovirus responsible for acute respiratory-tract infections in all age groups. J Infect Dis 186:1330–1334. doi: 10.1086/344319. [DOI] [PubMed] [Google Scholar]
- 28.Boivin G, De Serres G, Cote S, Gilca R, Abed Y, Rochette L, Bergeron MG, Dery P. 2003. Human metapneumovirus infections in hospitalized children. Emerg Infect Dis 9:634–640. doi: 10.3201/eid0906.030017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Louie JK, Schnurr DP, Pan CY, Kiang D, Carter C, Tougaw S, Ventura J, Norman A, Belmusto V, Rosenberg J, Trochet G. 2007. A summer outbreak of human metapneumovirus infection in a long-term-care facility. J Infect Dis 196:705–708. doi: 10.1086/519846. [DOI] [PubMed] [Google Scholar]
- 30.Hopkins P, McNeil K, Kermeen F, Musk M, McQueen E, Mackay I, Sloots T, Nissen M. 2008. Human metapneumovirus in lung transplant recipients and comparison to respiratory syncytial virus. Am J Respir Crit Care Med 178:876–881. doi: 10.1164/rccm.200711-1657OC. [DOI] [PubMed] [Google Scholar]
- 31.Walsh EE, Peterson DR, Falsey AR. 2008. Human metapneumovirus infections in adults: another piece of the puzzle. Arch Intern Med 168:2489–2496. doi: 10.1001/archinte.168.22.2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Syha R, Beck R, Hetzel J, Ketelsen D, Grosse U, Springer F, Horger M. 2012. Human metapneumovirus (HMPV) associated pulmonary infections in immunocompromised adults—initial CT findings, disease course and comparison to respiratory-syncytial-virus (RSV) induced pulmonary infections. Eur J Radiol 81:4173–4178. doi: 10.1016/j.ejrad.2012.06.024. [DOI] [PubMed] [Google Scholar]
- 33.Matsuda S, Nakamura M, Hirano E, Kiyota N, Omura T, Suzuki Y, Noda M, Kimura H. 2013. Characteristics of human metapneumovirus infection prevailing in hospital wards housing patients with severe disabilities. Jpn J Infect Dis 66:195–200. doi: 10.7883/yoken.66.195. [DOI] [PubMed] [Google Scholar]
- 34.Talaat KR, Karron RA, Thumar B, McMahon BA, Schmidt AC, Collins PL, Buchholz UJ. 2013. Experimental infection of adults with recombinant wild-type human metapneumovirus. J Infect Dis 208:1669–1678. doi: 10.1093/infdis/jit356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haas LE, de Rijk NX, Thijsen SF. 2012. Human metapneumovirus infections on the ICU: a report of three cases. Ann Intensive Care 2:30. doi: 10.1186/2110-5820-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Souza JS, Watanabe A, Carraro E, Granato C, Bellei N. 2013. Severe metapneumovirus infections among immunocompetent and immunocompromised patients admitted to hospital with respiratory infection. J Med Virol 85:530–536. doi: 10.1002/jmv.23477. [DOI] [PubMed] [Google Scholar]
- 37.Arnold JC, Singh KK, Milder E, Spector SA, Sawyer MH, Gavali S, Glaser C. 2009. Human metapneumovirus associated with central nervous system infection in children. Pediatr Infect Dis J 28:1057–1060. doi: 10.1097/INF.0b013e3181acd221. [DOI] [PubMed] [Google Scholar]
- 38.Schildgen O, Glatzel T, Geikowski T, Scheibner B, Matz B, Bindl L, Born M, Viazov S, Wilkesmann A, Knopfle G, Roggendorf M, Simon A. 2005. Human metapneumovirus RNA in encephalitis patient. Emerg Infect Dis 11:467–470. doi: 10.3201/eid1103.040676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanchez Fernandez I, Rebollo Polo M, Munoz-Almagro C, Monfort Carretero L, Fernandez Urena S, Rueda Munoz A, Colome Roura R, Perez Duenas B. 2012. Human metapneumovirus in the cerebrospinal fluid of a patient with acute encephalitis. Arch Neurol 69:649–652. doi: 10.1001/archneurol.2011.1094. [DOI] [PubMed] [Google Scholar]
- 40.Yokota T, Enoki H. 2013. Acute encephalopathy associated with human metapneumovirus: a case report. No To Hattatsu 45:461–462. (In Japanese.) [PubMed] [Google Scholar]
- 41.Niizuma T, Okumura A, Kinoshita K, Shimizu T. 2014. Acute encephalopathy associated with human metapneumovirus infection. Jpn J Infect Dis 67:213–215. doi: 10.7883/yoken.67.213. [DOI] [PubMed] [Google Scholar]
- 42.Webster DL, Gardner AH, Dye TJ, Chima RS. 2014. Status epilepticus: a possible association with human metapneumovirus infection. Pediatrics 133:e747–e750. doi: 10.1542/peds.2013-0929. [DOI] [PubMed] [Google Scholar]
- 43.Fok A, Mateevici C, Lin B, Chandra RV, Chong VH. 2015. Encephalitis-associated human metapneumovirus pneumonia in adult, Australia. Emerg Infect Dis 21:2074–2076. doi: 10.3201/eid2111.150608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vehapoglu A, Turel O, Uygur Sahin T, Kutlu NO, Iscan A. 2015. Clinical significance of human metapneumovirus in refractory status epilepticus and encephalitis: case report and review of the literature. Case Rep Neurol Med 2015:131780. doi: 10.1155/2015/131780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hata M, Ito M, Kiyosawa S, Kimpara Y, Tanaka S, Yamashita T, Hasegawa A, Kobayashi S, Koyama N, Minagawa H. 2007. A fatal case of encephalopathy possibly associated with human metapneumovirus infection. Jpn J Infect Dis 60:328–329. [PubMed] [Google Scholar]
- 46.Kaida A, Iritani N, Kubo H, Shiomi M, Kohdera U, Murakami T. 2006. Seasonal distribution and phylogenetic analysis of human metapneumovirus among children in Osaka City, Japan. J Clin Virol 35:394–399. doi: 10.1016/j.jcv.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 47.Williams JV, Martino R, Rabella N, Otegui M, Parody R, Heck JM, Crowe JE Jr. 2005. A prospective study comparing human metapneumovirus with other respiratory viruses in adults with hematologic malignancies and respiratory tract infections. J Infect Dis 192:1061–1065. doi: 10.1086/432732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dokos C, Masjosthusmann K, Rellensmann G, Werner C, Schuler-Luttmann S, Muller KM, Schiborr M, Ehlert K, Groll AH. 2013. Fatal human metapneumovirus infection following allogeneic hematopoietic stem cell transplantation. Transpl Infect Dis 15:E97–E101. doi: 10.1111/tid.12074. [DOI] [PubMed] [Google Scholar]
- 49.Te Wierik MJ, Nguyen DT, Beersma MF, Thijsen SF, Heemstra KA. 2012. An outbreak of severe respiratory tract infection caused by human metapneumovirus in a residential care facility for elderly in Utrecht, the Netherlands, January to March 2010 Euro Surveill 17(3):pii=20132 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20132. [PubMed] [Google Scholar]
- 50.Liao RS, Appelgate DM, Pelz RK. 2012. An outbreak of severe respiratory tract infection due to human metapneumovirus in a long-term care facility for the elderly in Oregon. J Clin Virol 53:171–173. doi: 10.1016/j.jcv.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 51.Edwards KM, Zhu Y, Griffin MR, Weinberg GA, Hall CB, Szilagyi PG, Staat MA, Iwane M, Prill MM, Williams JV, New Vaccine Surveillance Network . 2013. Burden of human metapneumovirus infection in young children. N Engl J Med 368:633–643. doi: 10.1056/NEJMoa1204630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Falsey AR, McElhaney JE, Beran J, van Essen GA, Duval X, Esen M, Galtier F, Gervais P, Hwang SJ, Kremsner P, Launay O, Leroux-Roels G, McNeil SA, Nowakowski A, Richardus JH, Ruiz-Palacios G, St Rose S, Devaster JM, Oostvogels L, Durviaux S, Taylor S. 2014. Respiratory syncytial virus and other respiratory viral infections in older adults with moderate to severe influenza-like illness. J Infect Dis 209:1873–1881. doi: 10.1093/infdis/jit839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schuster JE, Khuri-Bulos N, Faouri S, Shehabi A, Johnson M, Wang L, Fonnesbeck C, Williams JV, Halasa N. 2015. Human metapneumovirus infection in Jordanian children: epidemiology and risk factors for severe disease. Pediatr Infect Dis J 34:1335–1341. doi: 10.1097/INF.0000000000000892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Papenburg J, Hamelin ME, Ouhoummane N, Carbonneau J, Ouakki M, Raymond F, Robitaille L, Corbeil J, Caouette G, Frenette L, De Serres G, Boivin G. 2012. Comparison of risk factors for human metapneumovirus and respiratory syncytial virus disease severity in young children. J Infect Dis 206:178–189. doi: 10.1093/infdis/jis333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hasvold J, Sjoding M, Pohl K, Cooke C, Hyzy RC. 2016. The role of human metapneumovirus in the critically ill adult patient. J Crit Care 31:233–237. doi: 10.1016/j.jcrc.2015.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bosis S, Esposito S, Osterhaus AD, Tremolati E, Begliatti E, Tagliabue C, Corti F, Principi N, Niesters HG. 2008. Association between high nasopharyngeal viral load and disease severity in children with human metapneumovirus infection. J Clin Virol 42:286–290. doi: 10.1016/j.jcv.2008.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Martin ET, Kuypers J, Heugel J, Englund JA. 2008. Clinical disease and viral load in children infected with respiratory syncytial virus or human metapneumovirus. Diagn Microbiol Infect Dis 62:382–388. doi: 10.1016/j.diagmicrobio.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roussy JF, Carbonneau J, Ouakki M, Papenburg J, Hamelin ME, De Serres G, Boivin G. 2014. Human metapneumovirus viral load is an important risk factor for disease severity in young children. J Clin Virol 60:133–140. doi: 10.1016/j.jcv.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 59.Farber DL, Yudanin NA, Restifo NP. 2014. Human memory T cells: generation, compartmentalization and homeostasis. Nat Rev Immunol 14:24–35. doi: 10.1038/nri3567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cossarizza A, Ortolani C, Paganelli R, Barbieri D, Monti D, Sansoni P, Fagiolo U, Castellani G, Bersani F, Londei M, Franceschi C. 1996. CD45 isoforms expression on CD4+ and CD8+ T cells throughout life, from newborns to centenarians: implications for T cell memory. Mech Ageing Dev 86:173–195. doi: 10.1016/0047-6374(95)01691-0. [DOI] [PubMed] [Google Scholar]
- 61.Saule P, Trauet J, Dutriez V, Lekeux V, Dessaint JP, Labalette M. 2006. Accumulation of memory T cells from childhood to old age: central and effector memory cells in CD4(+) versus effector memory and terminally differentiated memory cells in CD8(+) compartment. Mech Ageing Dev 127:274–281. doi: 10.1016/j.mad.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 62.Williams JV, Weitkamp JH, Blum DL, LaFleur BJ, Crowe JE Jr. 2009. The human neonatal B cell response to respiratory syncytial virus uses a biased antibody variable gene repertoire that lacks somatic mutations. Mol Immunol 47:407–414. doi: 10.1016/j.molimm.2009.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pancham K, Sami I, Perez GF, Huseni S, Kurdi B, Rose MC, Rodriguez-Martinez CE, Nino G. 23 May 2015. Human metapneumovirus infection is associated with severe respiratory disease in preschool children with history of prematurity. Pediatr Neonatol doi: 10.1016/j.pedneo.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pancham K, Perez GF, Huseni S, Jain A, Kurdi B, Rodriguez-Martinez CE, Preciado D, Rose MC, Nino G. 2015. Premature infants have impaired airway antiviral IFNgamma responses to human metapneumovirus compared to respiratory syncytial virus. Pediatr Res 78:389–394. doi: 10.1038/pr.2015.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.El Kholy AA, Mostafa NA, Ali AA, El-Sherbini SA, Ismail RI, Magdy RI, Soliman MS, Said MM. 2014. Risk factors of prolonged hospital stay in children with viral severe acute respiratory infections. J Infect Dev Ctries 8:1285–1293. doi: 10.3855/jidc.4682. [DOI] [PubMed] [Google Scholar]
- 66.Hoellein A, Hecker J, Hoffmann D, Gottle F, Protzer U, Peschel C, Gotze K. 30 June 2015. Serious outbreak of human metapneumovirus in patients with hematologic malignancies. Leuk Lymphoma doi: 10.3109/10428194.2015.1067699. [DOI] [PubMed] [Google Scholar]
- 67.Godet C, Le Goff J, Beby-Defaux A, Robin M, Raffoux E, Arnulf B, Roblot F, Frat JP, Maillard N, Tazi A, Bergeron A. 2014. Human metapneumovirus pneumonia in patients with hematological malignancies. J Clin Virol 61:593–596. doi: 10.1016/j.jcv.2014.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chu HY, Renaud C, Ficken E, Thomson B, Kuypers J, Englund JA. 2014. Respiratory tract infections due to human metapneumovirus in immunocompromised children. J Pediatr Infect Dis Soc 3:286–293. doi: 10.1093/jpids/piu100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Walker E, Ison MG. 2014. Respiratory viral infections among hospitalized adults: experience of a single tertiary healthcare hospital. Influenza Other Respir Viruses 8:282–292. doi: 10.1111/irv.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Renaud C, Xie H, Seo S, Kuypers J, Cent A, Corey L, Leisenring W, Boeckh M, Englund JA. 2013. Mortality rates of human metapneumovirus and respiratory syncytial virus lower respiratory tract infections in hematopoietic cell transplantation recipients. Biol Blood Marrow Transplant 19:1220–1226. doi: 10.1016/j.bbmt.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ali M, Baker JM, Richardson SE, Weitzman S, Allen U, Abla O. 2013. Human metapneumovirus (hMPV) infection in children with cancer. J Pediatr Hematol Oncol 35:444–446. doi: 10.1097/MPH.0b013e31828ac89c. [DOI] [PubMed] [Google Scholar]
- 72.Noel N, Rammaert B, Zuber J, Sayre N, Mamzer-Bruneel MF, Leruez-Ville M, Mascard L, Lecuit M, Lortholary O. 2012. Lower respiratory tract infection in a renal transplant recipient: do not forget metapneumovirus. Case Rep Transplant 2012:353871. doi: 10.1155/2012/353871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Englund JA, Boeckh M, Kuypers J, Nichols WG, Hackman RC, Morrow RA, Fredricks DN, Corey L. 2006. Brief communication: fatal human metapneumovirus infection in stem-cell transplant recipients. Ann Intern Med 144:344–349. doi: 10.7326/0003-4819-144-5-200603070-00010. [DOI] [PubMed] [Google Scholar]
- 74.Wei HY, Tsao KC, Huang CG, Huang YC, Lin TY. 2013. Clinical features of different genotypes/genogroups of human metapneumovirus in hospitalized children. J Microbiol Immunol Infect 46:352–357. doi: 10.1016/j.jmii.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 75.Arnott A, Vong S, Sek M, Naughtin M, Beaute J, Rith S, Guillard B, Deubel V, Buchy P. 2013. Genetic variability of human metapneumovirus amongst an all ages population in Cambodia between 2007 and 2009. Infect Genet Evol 15:43–52. doi: 10.1016/j.meegid.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Agapov E, Sumino KC, Gaudreault-Keener M, Storch GA, Holtzman MJ. 2006. Genetic variability of human metapneumovirus infection: evidence of a shift in viral genotype without a change in illness. J Infect Dis 193:396–403. doi: 10.1086/499310. [DOI] [PubMed] [Google Scholar]
- 77.Kim HR, Cho AR, Lee MK, Yun SW, Kim TH. 2012. Genotype variability and clinical features of human metapneumovirus isolated from Korean children, 2007 to 2010. J Mol Diagn 14:61–64. doi: 10.1016/j.jmoldx.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 78.van den Hoogen BG, Bestebroer TM, Osterhaus AD, Fouchier RA. 2002. Analysis of the genomic sequence of a human metapneumovirus. Virology 295:119–132. doi: 10.1006/viro.2001.1355. [DOI] [PubMed] [Google Scholar]
- 79.Biacchesi S, Skiadopoulos MH, Tran KC, Murphy BR, Collins PL, Buchholz UJ. 2004. Recovery of human metapneumovirus from cDNA: optimization of growth in vitro and expression of additional genes. Virology 321:247–259. doi: 10.1016/j.virol.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 80.Herfst S, de Graaf M, Schickli JH, Tang RS, Kaur J, Yang CF, Spaete RR, Haller AA, van den Hoogen BG, Osterhaus AD, Fouchier RA. 2004. Recovery of human metapneumovirus genetic lineages A and B from cloned cDNA. J Virol 78:8264–8270. doi: 10.1128/JVI.78.15.8264-8270.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Collins PL, Wertz GW. 1983. cDNA cloning and transcriptional mapping of nine polyadenylylated RNAs encoded by the genome of human respiratory syncytial virus. Proc Natl Acad Sci U S A 80:3208–3212. doi: 10.1073/pnas.80.11.3208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dickens LE, Collins PL, Wertz GW. 1984. Transcriptional mapping of human respiratory syncytial virus. J Virol 52:364–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Biacchesi S, Skiadopoulos MH, Boivin G, Hanson CT, Murphy BR, Collins PL, Buchholz UJ. 2003. Genetic diversity between human metapneumovirus subgroups. Virology 315:1–9. doi: 10.1016/S0042-6822(03)00528-2. [DOI] [PubMed] [Google Scholar]
- 84.Lamb RA, Parks GD. 2013. Paramyxoviridae, p 957–995. In Knipe DM, Howley PM, Cohen JI, Griffin DE, Lamb RA, Martin MA, Racaniello VR, Roizman B (ed), Fields virology, 6th ed Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 85.Buchholz UJ, Biacchesi S, Pham QN, Tran KC, Yang L, Luongo CL, Skiadopoulos MH, Murphy BR, Collins PL. 2005. Deletion of M2 gene open reading frames 1 and 2 of human metapneumovirus: effects on RNA synthesis, attenuation, and immunogenicity. J Virol 79:6588–6597. doi: 10.1128/JVI.79.11.6588-6597.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bakker SE, Duquerroy S, Galloux M, Loney C, Conner E, Eleouet JF, Rey FA, Bhella D. 2013. The respiratory syncytial virus nucleoprotein-RNA complex forms a left-handed helical nucleocapsid. J Gen Virol 94:1734–1738. doi: 10.1099/vir.0.053025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.El Omari K, Dhaliwal B, Ren J, Abrescia NG, Lockyer M, Powell KL, Hawkins AR, Stammers DK. 2011. Structures of respiratory syncytial virus nucleocapsid protein from two crystal forms: details of potential packing interactions in the native helical form. Acta Crystallogr Sect F Struct Biol Cryst Commun 67:1179–1183. doi: 10.1107/S1744309111029228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tawar RG, Duquerroy S, Vonrhein C, Varela PF, Damier-Piolle L, Castagne N, MacLellan K, Bedouelle H, Bricogne G, Bhella D, Eleouet JF, Rey FA. 2009. Crystal structure of a nucleocapsid-like nucleoprotein-RNA complex of respiratory syncytial virus. Science 326:1279–1283. doi: 10.1126/science.1177634. [DOI] [PubMed] [Google Scholar]
- 89.de Graaf M, Herfst S, Schrauwen EJ, Choi Y, van den Hoogen BG, Osterhaus AD, Fouchier RA. 2008. Specificity and functional interaction of the polymerase complex proteins of human and avian metapneumoviruses. J Gen Virol 89:975–983. doi: 10.1099/vir.0.83537-0. [DOI] [PubMed] [Google Scholar]
- 90.Dochow M, Krumm SA, Crowe JE Jr, Moore ML, Plemper RK. 2012. Independent structural domains in paramyxovirus polymerase protein. J Biol Chem 287:6878–6891. doi: 10.1074/jbc.M111.325258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang Y, Wei Y, Zhang X, Cai H, Niewiesk S, Li J. 2014. Rational design of human metapneumovirus live attenuated vaccine candidates by inhibiting viral mRNA cap methyltransferase. J Virol 88:11411–11429. doi: 10.1128/JVI.00876-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Asenjo A, Calvo E, Villanueva N. 2006. Phosphorylation of human respiratory syncytial virus P protein at threonine 108 controls its interaction with the M2-1 protein in the viral RNA polymerase complex. J Gen Virol 87:3637–3642. doi: 10.1099/vir.0.82165-0. [DOI] [PubMed] [Google Scholar]
- 93.Derdowski A, Peters TR, Glover N, Qian R, Utley TJ, Burnett A, Williams JV, Spearman P, Crowe JE Jr. 2008. Human metapneumovirus nucleoprotein and phosphoprotein interact and provide the minimal requirements for inclusion body formation. J Gen Virol 89:2698–2708. doi: 10.1099/vir.0.2008/004051-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Barik S, McLean T, Dupuy LC. 1995. Phosphorylation of Ser232 directly regulates the transcriptional activity of the P protein of human respiratory syncytial virus: phosphorylation of Ser237 may play an accessory role. Virology 213:405–412. doi: 10.1006/viro.1995.0013. [DOI] [PubMed] [Google Scholar]
- 95.Dupuy LC, Dobson S, Bitko V, Barik S. 1999. Casein kinase 2-mediated phosphorylation of respiratory syncytial virus phosphoprotein P is essential for the transcription elongation activity of the viral polymerase; phosphorylation by casein kinase 1 occurs mainly at Ser(215) and is without effect. J Virol 73:8384–8392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bastien N, Normand S, Taylor T, Ward D, Peret TC, Boivin G, Anderson LJ, Li Y. 2003. Sequence analysis of the N, P, M and F genes of Canadian human metapneumovirus strains. Virus Res 93:51–62. doi: 10.1016/S0168-1702(03)00065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Palavecino CE, Cespedes PF, Gomez RS, Kalergis AM, Bueno SM. 2014. Immunization with a recombinant bacillus Calmette-Guerin strain confers protective Th1 immunity against the human metapneumovirus. J Immunol 192:214–223. doi: 10.4049/jimmunol.1300118. [DOI] [PubMed] [Google Scholar]
- 98.Schickli JH, Kaur J, Macphail M, Guzzetta JM, Spaete RR, Tang RS. 2008. Deletion of human metapneumovirus M2-2 increases mutation frequency and attenuates growth in hamsters. Virol J 5:69. doi: 10.1186/1743-422X-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cai H, Zhang Y, Ma Y, Sun J, Liang X, Li J. 2015. Zinc binding activity of human metapneumovirus M2-1 protein is indispensable for viral replication and pathogenesis in vivo. J Virol 89:6391–6405. doi: 10.1128/JVI.03488-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Leyrat C, Renner M, Harlos K, Huiskonen JT, Grimes JM. 2014. Drastic changes in conformational dynamics of the antiterminator M2-1 regulate transcription efficiency in Pneumovirinae. eLife 3:e02674. doi: 10.7554/eLife.02674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Esperante SA, Noval MG, Altieri TA, de Oliveira GA, Silva JL, de Prat-Gay G. 2013. Fine modulation of the respiratory syncytial virus M2-1 protein quaternary structure by reversible zinc removal from its Cys(3)-His(1) motif. Biochemistry 52:6779–6789. doi: 10.1021/bi401029q. [DOI] [PubMed] [Google Scholar]
- 102.Kitagawa Y, Zhou M, Yamaguchi M, Komatsu T, Takeuchi K, Itoh M, Gotoh B. 2010. Human metapneumovirus M2-2 protein inhibits viral transcription and replication. Microbes Infect 12:135–145. doi: 10.1016/j.micinf.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 103.Biacchesi S, Pham QN, Skiadopoulos MH, Murphy BR, Collins PL, Buchholz UJ. 2005. Infection of nonhuman primates with recombinant human metapneumovirus lacking the SH, G, or M2-2 protein categorizes each as a nonessential accessory protein and identifies vaccine candidates. J Virol 79:12608–12613. doi: 10.1128/JVI.79.19.12608-12613.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sabo Y, Ehrlich M, Bacharach E. 2011. The conserved YAGL motif in human metapneumovirus is required for higher-order cellular assemblies of the matrix protein and for virion production. J Virol 85:6594–6609. doi: 10.1128/JVI.02694-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Leyrat C, Renner M, Harlos K, Huiskonen JT, Grimes JM. 2014. Structure and self-assembly of the calcium binding matrix protein of human metapneumovirus. Structure 22:136–148. doi: 10.1016/j.str.2013.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ghildyal R, Li D, Peroulis I, Shields B, Bardin PG, Teng MN, Collins PL, Meanger J, Mills J. 2005. Interaction between the respiratory syncytial virus G glycoprotein cytoplasmic domain and the matrix protein. J Gen Virol 86:1879–1884. doi: 10.1099/vir.0.80829-0. [DOI] [PubMed] [Google Scholar]
- 107.Weng Y, Lu W, Harmon A, Xiang X, Deng Q, Song M, Wang D, Yu Q, Li F. 2011. The cellular endosomal sorting complex required for transport pathway is not involved in avian metapneumovirus budding in a virus-like-particle expression system. J Gen Virol 92:1205–1213. doi: 10.1099/vir.0.029306-0. [DOI] [PubMed] [Google Scholar]
- 108.Cox RG, Livesay SB, Johnson M, Ohi MD, Williams JV. 2012. The human metapneumovirus fusion protein mediates entry via an interaction with RGD-binding integrins. J Virol 86:12148–12160. doi: 10.1128/JVI.01133-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wei Y, Zhang Y, Cai H, Mirza AM, Iorio RM, Peeples ME, Niewiesk S, Li J. 2014. Roles of the putative integrin-binding motif of the human metapneumovirus fusion (F) protein in cell-cell fusion, viral infectivity, and pathogenesis. J Virol 88:4338–4352. doi: 10.1128/JVI.03491-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cseke G, Maginnis MS, Cox RG, Tollefson SJ, Podsiad AB, Wright DW, Dermody TS, Williams JV. 2009. Integrin alphavbeta1 promotes infection by human metapneumovirus. Proc Natl Acad Sci U S A 106:1566–1571. doi: 10.1073/pnas.0801433106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chang A, Masante C, Buchholz UJ, Dutch RE. 2012. Human metapneumovirus (HMPV) binding and infection are mediated by interactions between the HMPV fusion protein and heparan sulfate. J Virol 86:3230–3243. doi: 10.1128/JVI.06706-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Miller SA, Tollefson S, Crowe JE Jr, Williams JV, Wright DW. 2007. Examination of a fusogenic hexameric core from human metapneumovirus and identification of a potent synthetic peptide inhibitor from the heptad repeat 1 region. J Virol 81:141–149. doi: 10.1128/JVI.01243-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Schowalter RM, Smith SE, Dutch RE. 2006. Characterization of human metapneumovirus F protein-promoted membrane fusion: critical roles for proteolytic processing and low pH. J Virol 80:10931–10941. doi: 10.1128/JVI.01287-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Herfst S, Mas V, Ver LS, Wierda RJ, Osterhaus AD, Fouchier RA, Melero JA. 2008. Low-pH-induced membrane fusion mediated by human metapneumovirus F protein is a rare, strain-dependent phenomenon. J Virol 82:8891–8895. doi: 10.1128/JVI.00472-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lamb RA, Jardetzky TS. 2007. Structural basis of viral invasion: lessons from paramyxovirus F. Curr Opin Struct Biol 17:427–436. doi: 10.1016/j.sbi.2007.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sorkin A, Von Zastrow M. 2002. Signal transduction and endocytosis: close encounters of many kinds. Nat Rev Mol Cell Biol 3:600–614. doi: 10.1038/nrm883. [DOI] [PubMed] [Google Scholar]
- 117.Cox RG, Mainou BA, Johnson M, Hastings AK, Schuster JE, Dermody TS, Williams JV. 2015. Human metapneumovirus is capable of entering cells by fusion with endosomal membranes. PLoS Pathog 11:e1005303. doi: 10.1371/journal.ppat.1005303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Thammawat S, Sadlon TA, Hallsworth PG, Gordon DL. 2008. Role of cellular glycosaminoglycans and charged regions of viral G protein in human metapneumovirus infection. J Virol 82:11767–11774. doi: 10.1128/JVI.01208-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Adamson P, Thammawat S, Muchondo G, Sadlon T, Gordon D. 2012. Diversity in glycosaminoglycan binding amongst hMPV G protein lineages. Viruses 4:3785–3803. doi: 10.3390/v4123785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Biacchesi S, Pham QN, Skiadopoulos MH, Murphy BR, Collins PL, Buchholz UJ. 2006. Modification of the trypsin-dependent cleavage activation site of the human metapneumovirus fusion protein to be trypsin independent does not increase replication or spread in rodents or nonhuman primates. J Virol 80:5798–5806. doi: 10.1128/JVI.00294-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.de Graaf M, Herfst S, Aarbiou J, Burgers PC, Zaaraoui-Boutahar F, Bijl M, van Ijcken W, Schrauwen EJ, Osterhaus AD, Luider TM, Scholte BJ, Fouchier RA, Andeweg AC. 2013. Small hydrophobic protein of human metapneumovirus does not affect virus replication and host gene expression in vitro. PLoS One 8:e58572. doi: 10.1371/journal.pone.0058572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Masante C, El Najjar F, Chang A, Jones A, Moncman CL, Dutch RE. 2014. The human metapneumovirus small hydrophobic protein has properties consistent with those of a viroporin and can modulate viral fusogenic activity. J Virol 88:6423–6433. doi: 10.1128/JVI.02848-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Le Nouen C, Hillyer P, Brock LG, Winter CC, Rabin RL, Collins PL, Buchholz UJ. 2014. Human metapneumovirus SH and G glycoproteins inhibit macropinocytosis-mediated entry into human dendritic cells and reduce CD4+ T cell activation. J Virol 88:6453–6469. doi: 10.1128/JVI.03261-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bao X, Kolli D, Liu T, Shan Y, Garofalo RP, Casola A. 2008. Human metapneumovirus small hydrophobic protein inhibits NF-kappaB transcriptional activity. J Virol 82:8224–8229. doi: 10.1128/JVI.02584-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Williams JV, Chen Z, Cseke G, Wright DW, Keefer CJ, Tollefson SJ, Hessell A, Podsiad A, Shepherd BE, Sanna PP, Burton DR, Crowe JE Jr, Williamson RA. 2007. A recombinant human monoclonal antibody to human metapneumovirus fusion protein that neutralizes virus in vitro and is effective therapeutically in vivo. J Virol 81:8315–8324. doi: 10.1128/JVI.00106-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cseke G, Wright DW, Tollefson SJ, Johnson JE, Crowe JE Jr, Williams JV. 2007. Human metapneumovirus fusion protein vaccines that are immunogenic and protective in cotton rats. J Virol 81:698–707. doi: 10.1128/JVI.00844-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Skiadopoulos MH, Biacchesi S, Buchholz UJ, Amaro-Carambot E, Surman SR, Collins PL, Murphy BR. 2006. Individual contributions of the human metapneumovirus F, G, and SH surface glycoproteins to the induction of neutralizing antibodies and protective immunity. Virology 345:492–501. doi: 10.1016/j.virol.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 128.Audsley MD, Moseley GW. 2013. Paramyxovirus evasion of innate immunity: diverse strategies for common targets. World J Virol 2:57–70. doi: 10.5501/wjv.v2.i2.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Parks GD, Alexander-Miller MA. 2013. Paramyxovirus activation and inhibition of innate immune responses. J Mol Biol 425:4872–4892. doi: 10.1016/j.jmb.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Vargas SO, Kozakewich HP, Perez-Atayde AR, McAdam AJ. 2004. Pathology of human metapneumovirus infection: insights into the pathogenesis of a newly identified respiratory virus. Pediatr Dev Pathol 7:478–486; discussion 421. doi: 10.1007/s10024-004-1011-2. [DOI] [PubMed] [Google Scholar]
- 131.Darniot M, Petrella T, Aho S, Pothier P, Manoha C. 2005. Immune response and alteration of pulmonary function after primary human metapneumovirus (hMPV) infection of BALB/c mice. Vaccine 23:4473–4480. doi: 10.1016/j.vaccine.2005.04.027. [DOI] [PubMed] [Google Scholar]
- 132.Hamelin ME, Prince GA, Gomez AM, Kinkead R, Boivin G. 2006. Human metapneumovirus infection induces long-term pulmonary inflammation associated with airway obstruction and hyperresponsiveness in mice. J Infect Dis 193:1634–1642. doi: 10.1086/504262. [DOI] [PubMed] [Google Scholar]
- 133.Kuiken T, van den Hoogen BG, van Riel DA, Laman JD, van Amerongen G, Sprong L, Fouchier RA, Osterhaus AD. 2004. Experimental human metapneumovirus infection of cynomolgus macaques (Macaca fascicularis) results in virus replication in ciliated epithelial cells and pneumocytes with associated lesions throughout the respiratory tract. Am J Pathol 164:1893–1900. doi: 10.1016/S0002-9440(10)63750-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Debiaggi M, Canducci F, Sampaolo M, Marinozzi MC, Parea M, Terulla C, Colombo AA, Alessandrino EP, Bragotti LZ, Arghittu M, Goglio A, Migliavacca R, Romero E, Clementi M. 2006. Persistent symptomless human metapneumovirus infection in hematopoietic stem cell transplant recipients. J Infect Dis 194:474–478. doi: 10.1086/505881. [DOI] [PubMed] [Google Scholar]
- 135.Abed Y, Boivin G. 2008. Human metapneumovirus infection in immunocompromised child. Emerg Infect Dis 14:854–856. doi: 10.3201/eid1405.071459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Evashuk KM, Forgie SE, Gilmour S, Huynh H, Lee BE, Robinson JL. 2008. Respiratory failure associated with human metapneumovirus infection in an infant posthepatic transplant. Am J Transplant 8:1567–1569. doi: 10.1111/j.1600-6143.2008.02278.x. [DOI] [PubMed] [Google Scholar]
- 137.Gupta A, Bembea M, Brown A, Robertson C, Romer L, Cohn RD. 2012. Respiratory failure secondary to human metapneumovirus requiring extracorporeal membrane oxygenation in a 32-month-old child. Case Rep Pediatr 2012:268074. doi: 10.1155/2012/268074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lay MK, Cespedes PF, Palavecino CE, Leon MA, Diaz RA, Salazar FJ, Mendez GP, Bueno SM, Kalergis AM. 15 April 2015. Human metapneumovirus infection activates the TSLP pathway that drives excessive pulmonary inflammation and viral replication in mice. Eur J Immunol doi: 10.1002/eji.201445021. [DOI] [PubMed] [Google Scholar]
- 139.Alvarez R, Harrod KS, Shieh WJ, Zaki S, Tripp RA. 2004. Human metapneumovirus persists in BALB/c mice despite the presence of neutralizing antibodies. J Virol 78:14003–14011. doi: 10.1128/JVI.78.24.14003-14011.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Liu Y, Haas DL, Poore S, Isakovic S, Gahan M, Mahalingam S, Fu ZF, Tripp RA. 2009. Human metapneumovirus establishes persistent infection in the lungs of mice and is reactivated by glucocorticoid treatment. J Virol 83:6837–6848. doi: 10.1128/JVI.00379-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, Stockmann C, Anderson EJ, Grijalva CG, Self WH, Zhu Y, Patel A, Hymas W, Chappell JD, Kaufman RA, Kan JH, Dansie D, Lenny N, Hillyard DR, Haynes LM, Levine M, Lindstrom S, Winchell JM, Katz JM, Erdman D, Schneider E, Hicks LA, Wunderink RG, Edwards KM, Pavia AT, McCullers JA, Finelli L, CDC EPIC Study Team . 2015. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med 372:835–845. doi: 10.1056/NEJMoa1405870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Homaira N, Luby SP, Petri WA, Vainionpaa R, Rahman M, Hossain K, Snider CB, Rahman M, Alamgir AS, Zesmin F, Alam M, Gurley ES, Zaman RU, Azim T, Erdman DD, Fry AM, Bresee J, Widdowson MA, Haque R, Azziz-Baumgartner E. 2012. Incidence of respiratory virus-associated pneumonia in urban poor young children of Dhaka, Bangladesh, 2009-2011. PLoS One 7:e32056. doi: 10.1371/journal.pone.0032056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Chang YF, Tsao KC, Liu YC, Chen YC, Yu PC, Huang YC, Chou C. 2015. Diagnosis of human metapneumovirus in patients hospitalized with acute lower respiratory tract infection using a metal-enhanced fluorescence technique. J Virol Methods 213:151–156. doi: 10.1016/j.jviromet.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 144.Guerrero-Plata A, Casola A, Suarez G, Yu X, Spetch L, Peeples ME, Garofalo RP. 2006. Differential response of dendritic cells to human metapneumovirus and respiratory syncytial virus. Am J Respir Cell Mol Biol 34:320–329. doi: 10.1165/rcmb.2005-0287OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Cespedes PF, Gonzalez PA, Kalergis AM. 2013. Human metapneumovirus keeps dendritic cells from priming antigen-specific naive T cells. Immunology 139:366–376. doi: 10.1111/imm.12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Le Nouen C, Munir S, Losq S, Winter CC, McCarty T, Stephany DA, Holmes KL, Bukreyev A, Rabin RL, Collins PL, Buchholz UJ. 2009. Infection and maturation of monocyte-derived human dendritic cells by human respiratory syncytial virus, human metapneumovirus, and human parainfluenza virus type 3. Virology 385:169–182. doi: 10.1016/j.virol.2008.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Tan MC, Battini L, Tuyama AC, Macip S, Melendi GA, Horga MA, Gusella GL. 2007. Characterization of human metapneumovirus infection of myeloid dendritic cells. Virology 357:1–9. doi: 10.1016/j.virol.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Guerrero-Plata A, Kolli D, Hong C, Casola A, Garofalo RP. 2009. Subversion of pulmonary dendritic cell function by paramyxovirus infections. J Immunol 182:3072–3083. doi: 10.4049/jimmunol.0802262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kolli D, Gupta MR, Sbrana E, Velayutham TS, Chao H, Casola A, Garofalo RP. 2014. Alveolar macrophages contribute to the pathogenesis of human metapneumovirus infection while protecting against respiratory syncytial virus infection. Am J Respir Cell Mol Biol 51:502–515. doi: 10.1165/rcmb.2013-0414OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ivashkiv LB, Donlin LT. 2014. Regulation of type I interferon responses. Nat Rev Immunol 14:36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Riboldi E, Daniele R, Cassatella MA, Sozzani S, Bosisio D. 2009. Engagement of BDCA-2 blocks TRAIL-mediated cytotoxic activity of plasmacytoid dendritic cells. Immunobiology 214:868–876. doi: 10.1016/j.imbio.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 152.Arimori Y, Nakamura R, Yamada H, Shibata K, Maeda N, Kase T, Yoshikai Y. 2014. Type I interferon plays opposing roles in cytotoxicity and interferon-gamma production by natural killer and CD8 T cells after influenza A virus infection in mice. J Innate Immun 6:456–466. doi: 10.1159/000356824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Liao S, Bao X, Liu T, Lai S, Li K, Garofalo RP, Casola A. 2008. Role of retinoic acid inducible gene-I in human metapneumovirus-induced cellular signalling. J Gen Virol 89:1978–1986. doi: 10.1099/vir.0.2008/000778-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Bao X, Kolli D, Ren J, Liu T, Garofalo RP, Casola A. 2013. Human metapneumovirus glycoprotein G disrupts mitochondrial signaling in airway epithelial cells. PLoS One 8:e62568. doi: 10.1371/journal.pone.0062568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Goutagny N, Jiang Z, Tian J, Parroche P, Schickli J, Monks BG, Ulbrandt N, Ji H, Kiener PA, Coyle AJ, Fitzgerald KA. 2010. Cell type-specific recognition of human metapneumoviruses (HMPVs) by retinoic acid-inducible gene I (RIG-I) and TLR7 and viral interference of RIG-I ligand recognition by HMPV-B1 phosphoprotein. J Immunol 184:1168–1179. doi: 10.4049/jimmunol.0902750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ren J, Wang Q, Kolli D, Prusak DJ, Tseng CT, Chen ZJ, Li K, Wood TG, Bao X. 2012. Human metapneumovirus M2-2 protein inhibits innate cellular signaling by targeting MAVS. J Virol 86:13049–13061. doi: 10.1128/JVI.01248-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Banos-Lara MDR, Ghosh A, Guerrero-Plata A. 2013. Critical role of MDA5 in the interferon response induced by human metapneumovirus infection in dendritic cells and in vivo. J Virol 87:1242–1251. doi: 10.1128/JVI.01213-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kolli D, Bao X, Liu T, Hong C, Wang T, Garofalo RP, Casola A. 2011. Human metapneumovirus glycoprotein G inhibits TLR4-dependent signaling in monocyte-derived dendritic cells. J Immunol 187:47–54. doi: 10.4049/jimmunol.1002589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hastings AK, Erickson JJ, Schuster JE, Boyd KL, Tollefson SJ, Johnson M, Gilchuk P, Joyce S, Williams JV. 2015. Role of type I interferon signaling in human metapneumovirus pathogenesis and control of viral replication. J Virol 89:4405–4420. doi: 10.1128/JVI.03275-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Erickson JJ, Gilchuk P, Hastings AK, Tollefson SJ, Johnson M, Downing MB, Boyd KL, Johnson JE, Kim AS, Joyce S, Williams JV. 2012. Viral acute lower respiratory infections impair CD8+ T cells through PD-1. J Clin Invest 122:2967–2982. doi: 10.1172/JCI62860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Spann KM, Loh Z, Lynch JP, Ullah A, Zhang V, Baturcam E, Werder RB, Khajornjiraphan N, Rudd P, Loo YM, Suhrbier A, Gale M Jr, Upham JW, Phipps S. 2014. IRF-3, IRF-7, and IPS-1 promote host defense against acute human metapneumovirus infection in neonatal mice. Am J Pathol 184:1795–1806. doi: 10.1016/j.ajpath.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 162.Banos-Lara MDR, Harvey L, Mendoza A, Guerrero-Plata A. 2013. Type III interferon induction by HMPV infection in human epithelial cells, abstr A2781 Abstr Am Thorac Soc Int Conf 2013. [Google Scholar]
- 163.Banos-Lara MDR, Harvey L, Mendoza A, Simms D, Chouljenko VN, Wakamatsu N, Kousoulas KG, Guerrero-Plata A. 2015. Impact and regulation of lambda interferon response in human metapneumovirus infection. J Virol 89:730–742. doi: 10.1128/JVI.02897-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Chi B, Dickensheets HL, Spann KM, Alston MA, Luongo C, Dumoutier L, Huang J, Renauld JC, Kotenko SV, Roederer M, Beeler JA, Donnelly RP, Collins PL, Rabin RL. 2006. Alpha and lambda interferon together mediate suppression of CD4 T cells induced by respiratory syncytial virus. J Virol 80:5032–5040. doi: 10.1128/JVI.80.10.5032-5040.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ren J, Kolli D, Liu T, Xu R, Garofalo RP, Casola A, Bao X. 2011. Human metapneumovirus inhibits IFN-beta signaling by downregulating Jak1 and Tyk2 cellular levels. PLoS One 6:e24496. doi: 10.1371/journal.pone.0024496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Mitzel DN, Jaramillo RJ, Stout-Delgado H, Senft AP, Harrod KS. 2014. Human metapneumovirus inhibits the IL-6-induced JAK/STAT3 signalling cascade in airway epithelium. J Gen Virol 95:26–37. doi: 10.1099/vir.0.055632-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ren J, Liu G, Go J, Kolli D, Zhang G, Bao X. 2014. Human metapneumovirus M2-2 protein inhibits innate immune response in monocyte-derived dendritic cells. PLoS One 9:e91865. doi: 10.1371/journal.pone.0091865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Bao X, Liu T, Shan Y, Li K, Garofalo RP, Casola A. 2008. Human metapneumovirus glycoprotein G inhibits innate immune responses. PLoS Pathog 4:e1000077. doi: 10.1371/journal.ppat.1000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Bao X, Sinha M, Liu T, Hong C, Luxon BA, Garofalo RP, Casola A. 2008. Identification of human metapneumovirus-induced gene networks in airway epithelial cells by microarray analysis. Virology 374:114–127. doi: 10.1016/j.virol.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Wang YH, Ito T, Wang YH, Homey B, Watanabe N, Martin R, Barnes CJ, McIntyre BW, Gilliet M, Kumar R, Yao Z, Liu YJ. 2006. Maintenance and polarization of human TH2 central memory T cells by thymic stromal lymphopoietin-activated dendritic cells. Immunity 24:827–838. doi: 10.1016/j.immuni.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 171.Ito T, Wang YH, Duramad O, Hori T, Delespesse GJ, Watanabe N, Qin FX, Yao Z, Cao W, Liu YJ. 2005. TSLP-activated dendritic cells induce an inflammatory T helper type 2 cell response through OX40 ligand. J Exp Med 202:1213–1223. doi: 10.1084/jem.20051135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Neill DR, Wong SH, Bellosi A, Flynn RJ, Daly M, Langford TK, Bucks C, Kane CM, Fallon PG, Pannell R, Jolin HE, McKenzie AN. 2010. Nuocytes represent a new innate effector leukocyte that mediates type-2 immunity. Nature 464:1367–1370. doi: 10.1038/nature08900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ford LB, Cerovic V, Milling SW, Graham GJ, Hansell CA, Nibbs RJ. 2014. Characterization of conventional and atypical receptors for the chemokine CCL2 on mouse leukocytes. J Immunol 193:400–411. doi: 10.4049/jimmunol.1303236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wang A, Wang Z, Cao Y, Cheng S, Chen H, Bunjhoo H, Xie J, Wang C, Xu Y, Xiong W. 2015. CCL2/CCR2-dependent recruitment of Th17 cells but not Tc17 cells to the lung in a murine asthma model. Int Arch Allergy Immunol 166:52–62. doi: 10.1159/000371764. [DOI] [PubMed] [Google Scholar]
- 175.Cook DN, Beck MA, Coffman TM, Kirby SL, Sheridan JF, Pragnell IB, Smithies O. 1995. Requirement of MIP-1 alpha for an inflammatory response to viral infection. Science 269:1583–1585. doi: 10.1126/science.7667639. [DOI] [PubMed] [Google Scholar]
- 176.Wolpe SD, Davatelis G, Sherry B, Beutler B, Hesse DG, Nguyen HT, Moldawer LL, Nathan CF, Lowry SF, Cerami A. 1988. Macrophages secrete a novel heparin-binding protein with inflammatory and neutrophil chemokinetic properties. J Exp Med 167:570–581. doi: 10.1084/jem.167.2.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Tyner JW, Uchida O, Kajiwara N, Kim EY, Patel AC, O'Sullivan MP, Walter MJ, Schwendener RA, Cook DN, Danoff TM, Holtzman MJ. 2005. CCL5-CCR5 interaction provides antiapoptotic signals for macrophage survival during viral infection. Nat Med 11:1180–1187. doi: 10.1038/nm1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wolpe SD, Sherry B, Juers D, Davatelis G, Yurt RW, Cerami A. 1989. Identification and characterization of macrophage inflammatory protein 2. Proc Natl Acad Sci U S A 86:612–616. doi: 10.1073/pnas.86.2.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Li Q, Park PW, Wilson CL, Parks WC. 2002. Matrilysin shedding of syndecan-1 regulates chemokine mobilization and transepithelial efflux of neutrophils in acute lung injury. Cell 111:635–646. doi: 10.1016/S0092-8674(02)01079-6. [DOI] [PubMed] [Google Scholar]
- 180.Kaur M, Singh D. 2013. Neutrophil chemotaxis caused by chronic obstructive pulmonary disease alveolar macrophages: the role of CXCL8 and the receptors CXCR1/CXCR2. J Pharmacol Exp Ther 347:173–180. doi: 10.1124/jpet.112.201855. [DOI] [PubMed] [Google Scholar]
- 181.Dufour JH, Dziejman M, Liu MT, Leung JH, Lane TE, Luster AD. 2002. IFN-gamma-inducible protein 10 (IP-10; CXCL10)-deficient mice reveal a role for IP-10 in effector T cell generation and trafficking. J Immunol 168:3195–3204. doi: 10.4049/jimmunol.168.7.3195. [DOI] [PubMed] [Google Scholar]
- 182.Medoff BD, Sauty A, Tager AM, Maclean JA, Smith RN, Mathew A, Dufour JH, Luster AD. 2002. IFN-gamma-inducible protein 10 (CXCL10) contributes to airway hyperreactivity and airway inflammation in a mouse model of asthma. J Immunol 168:5278–5286. doi: 10.4049/jimmunol.168.10.5278. [DOI] [PubMed] [Google Scholar]
- 183.Cole KE, Strick CA, Paradis TJ, Ogborne KT, Loetscher M, Gladue RP, Lin W, Boyd JG, Moser B, Wood DE, Sahagan BG, Neote K. 1998. Interferon-inducible T cell alpha chemoattractant (I-TAC): a novel non-ELR CXC chemokine with potent activity on activated T cells through selective high affinity binding to CXCR3. J Exp Med 187:2009–2021. doi: 10.1084/jem.187.12.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Pasare C, Medzhitov R. 2003. Toll pathway-dependent blockade of CD4+ CD25+ T cell-mediated suppression by dendritic cells. Science 299:1033–1036. doi: 10.1126/science.1078231. [DOI] [PubMed] [Google Scholar]
- 185.Mestas J, Hughes CC. 2004. Of mice and not men: differences between mouse and human immunology. J Immunol 172:2731–2738. doi: 10.4049/jimmunol.172.5.2731. [DOI] [PubMed] [Google Scholar]
- 186.Guerrero-Plata A, Casola A, Garofalo RP. 2005. Human metapneumovirus induces a profile of lung cytokines distinct from that of respiratory syncytial virus. J Virol 79:14992–14997. doi: 10.1128/JVI.79.23.14992-14997.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Alvarez R, Tripp RA. 2005. The immune response to human metapneumovirus is associated with aberrant immunity and impaired virus clearance in BALB/c mice. J Virol 79:5971–5978. doi: 10.1128/JVI.79.10.5971-5978.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Qiao J, Li A, Jin X. 2011. TSLP from RSV-stimulated rat airway epithelial cells activates myeloid dendritic cells. Immunol Cell Biol 89:231–238. doi: 10.1038/icb.2010.85. [DOI] [PubMed] [Google Scholar]
- 189.Lee HC, Headley MB, Loo YM, Berlin A, Gale M Jr, Debley JS, Lukacs NW, Ziegler SF. 2012. Thymic stromal lymphopoietin is induced by respiratory syncytial virus-infected airway epithelial cells and promotes a type 2 response to infection. J Allergy Clin Immunol 130:1187–1196. doi: 10.1016/j.jaci.2012.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Halfhide CP, Flanagan BF, Brearey SP, Hunt JA, Fonceca AM, McNamara PS, Howarth D, Edwards S, Smyth RL. 2011. Respiratory syncytial virus binds and undergoes transcription in neutrophils from the blood and airways of infants with severe bronchiolitis. J Infect Dis 204:451–458. doi: 10.1093/infdis/jir280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Inngjerdingen M, Damaj B, Maghazachi AA. 2000. Human NK cells express CC chemokine receptors 4 and 8 and respond to thymus and activation-regulated chemokine, macrophage-derived chemokine, and I-309. J Immunol 164:4048–4054. doi: 10.4049/jimmunol.164.8.4048. [DOI] [PubMed] [Google Scholar]
- 192.Steinman RM, Cohn ZA. 1973. Identification of a novel cell type in peripheral lymphoid organs of mice. I. Morphology, quantitation, tissue distribution. J Exp Med 137:1142–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Steinman RM, Cohn ZA. 1974. Identification of a novel cell type in peripheral lymphoid organs of mice. II. Functional properties in vitro. J Exp Med 139:380–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Gonzalez PA, Carreno LJ, Coombs D, Mora JE, Palmieri E, Goldstein B, Nathenson SG, Kalergis AM. 2005. T cell receptor binding kinetics required for T cell activation depend on the density of cognate ligand on the antigen-presenting cell. Proc Natl Acad Sci U S A 102:4824–4829. doi: 10.1073/pnas.0500922102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Vanguri V, Govern CC, Smith R, Huseby ES. 2013. Viral antigen density and confinement time regulate the reactivity pattern of CD4 T-cell responses to vaccinia virus infection. Proc Natl Acad Sci U S A 110:288–293. doi: 10.1073/pnas.1208328110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Grakoui A, Bromley SK, Sumen C, Davis MM, Shaw AS, Allen PM, Dustin ML. 1999. The immunological synapse: a molecular machine controlling T cell activation. Science 285:221–227. doi: 10.1126/science.285.5425.221. [DOI] [PubMed] [Google Scholar]
- 197.Wang D, Sun B, Feng M, Feng H, Gong W, Liu Q, Ge S. 2015. Role of scavenger receptors in dendritic cell function. Hum Immunol 76:442–446. doi: 10.1016/j.humimm.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 198.Hemmi H, Akira S. 2005. TLR signalling and the function of dendritic cells. Chem Immunol Allergy 86:120–135. [DOI] [PubMed] [Google Scholar]
- 199.Banchereau J, Steinman RM. 1998. Dendritic cells and the control of immunity. Nature 392:245–252. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 200.Tan JK, O'Neill HC. 2005. Maturation requirements for dendritic cells in T cell stimulation leading to tolerance versus immunity. J Leukoc Biol 78:319–324. doi: 10.1189/jlb.1104664. [DOI] [PubMed] [Google Scholar]
- 201.Quezada SA, Jarvinen LZ, Lind EF, Noelle RJ. 2004. CD40/CD154 interactions at the interface of tolerance and immunity. Annu Rev Immunol 22:307–328. doi: 10.1146/annurev.immunol.22.012703.104533. [DOI] [PubMed] [Google Scholar]
- 202.Frasca L, Fedele G, Deaglio S, Capuano C, Palazzo R, Vaisitti T, Malavasi F, Ausiello CM. 2006. CD38 orchestrates migration, survival, and Th1 immune response of human mature dendritic cells. Blood 107:2392–2399. doi: 10.1182/blood-2005-07-2913. [DOI] [PubMed] [Google Scholar]
- 203.Lukacs-Kornek V, Engel D, Tacke F, Kurts C. 2008. The role of chemokines and their receptors in dendritic cell biology. Front Biosci 13:2238–2252. doi: 10.2741/2838. [DOI] [PubMed] [Google Scholar]
- 204.Gonzalez PA, Carreno LJ, Cespedes PF, Bueno SM, Riedel CA, Kalergis AM. 2013. Modulation of tumor immunity by soluble and membrane-bound molecules at the immunological synapse. Clin Dev Immunol 2013:450291. doi: 10.1155/2013/450291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Bretscher PA. 1999. A two-step, two-signal model for the primary activation of precursor helper T cells. Proc Natl Acad Sci U S A 96:185–190. doi: 10.1073/pnas.96.1.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Le Nouen C, Hillyer P, Winter CC, McCarty T, Rabin RL, Collins PL, Buchholz UJ. 2011. Low CCR7-mediated migration of human monocyte derived dendritic cells in response to human respiratory syncytial virus and human metapneumovirus. PLoS Pathog 7:e1002105. doi: 10.1371/journal.ppat.1002105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Gonzalez PA, Prado CE, Leiva ED, Carreno LJ, Bueno SM, Riedel CA, Kalergis AM. 2008. Respiratory syncytial virus impairs T cell activation by preventing synapse assembly with dendritic cells. Proc Natl Acad Sci U S A 105:14999–15004. doi: 10.1073/pnas.0802555105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Le Nouen C, Hillyer P, Munir S, Winter CC, McCarty T, Bukreyev A, Collins PL, Rabin RL, Buchholz UJ. 2010. Effects of human respiratory syncytial virus, metapneumovirus, parainfluenza virus 3 and influenza virus on CD4+ T cell activation by dendritic cells. PLoS One 5:e15017. doi: 10.1371/journal.pone.0015017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Rothoeft T, Fischer K, Zawatzki S, Schulz V, Schauer U, Korner Rettberg C. 2007. Differential response of human naive and memory/effector T cells to dendritic cells infected by respiratory syncytial virus. Clin Exp Immunol 150:263–273. doi: 10.1111/j.1365-2249.2007.03497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Cespedes PF, Bueno SM, Ramirez BA, Gomez RS, Riquelme SA, Palavecino CE, Mackern-Oberti JP, Mora JE, Depoil D, Sacristan C, Cammer M, Creneguy A, Nguyen TH, Riedel CA, Dustin ML, Kalergis AM. 2014. Surface expression of the hRSV nucleoprotein impairs immunological synapse formation with T cells. Proc Natl Acad Sci U S A 111:E3214–E3223. doi: 10.1073/pnas.1400760111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Ebihara T, Endo R, Ishiguro N, Nakayama T, Sawada H, Kikuta H. 2004. Early reinfection with human metapneumovirus in an infant. J Clin Microbiol 42:5944–5946. doi: 10.1128/JCM.42.12.5944-5946.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Pavlin JA, Hickey AC, Ulbrandt N, Chan YP, Endy TP, Boukhvalova MS, Chunsuttiwat S, Nisalak A, Libraty DH, Green S, Rothman AL, Ennis FA, Jarman R, Gibbons RV, Broder CC. 2008. Human metapneumovirus reinfection among children in Thailand determined by ELISA using purified soluble fusion protein. J Infect Dis 198:836–842. doi: 10.1086/591186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Teijaro JR, Verhoeven D, Page CA, Turner D, Farber DL. 2010. Memory CD4 T cells direct protective responses to influenza virus in the lungs through helper-independent mechanisms. J Virol 84:9217–9226. doi: 10.1128/JVI.01069-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Olson MR, Seah SG, Cullen J, Greyer M, Edenborough K, Doherty PC, Bedoui S, Lew AM, Turner SJ. 2014. Helping themselves: optimal virus-specific CD4 T cell responses require help via CD4 T cell licensing of dendritic cells. J Immunol 193:5420–5433. doi: 10.4049/jimmunol.1303359. [DOI] [PubMed] [Google Scholar]
- 215.McKinstry KK, Strutt TM, Kuang Y, Brown DM, Sell S, Dutton RW, Swain SL. 2012. Memory CD4+ T cells protect against influenza through multiple synergizing mechanisms. J Clin Invest 122:2847–2856. doi: 10.1172/JCI63689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Banerjee S, Sullender WM, Ahuja RK, Broor S. 2011. Seroepidemiological study of human metapneumovirus in New Delhi, India. Indian J Med Microbiol 29:363–367. doi: 10.4103/0255-0857.90162. [DOI] [PubMed] [Google Scholar]
- 217.Okamoto M, Sugawara K, Takashita E, Muraki Y, Hongo S, Nishimura H, Matsuzaki Y. 2010. Longitudinal course of human metapneumovirus antibody titers and reinfection in healthy adults. J Med Virol 82:2092–2096. doi: 10.1002/jmv.21920. [DOI] [PubMed] [Google Scholar]
- 218.Herd KA, Nissen MD, Hopkins PM, Sloots TP, Tindle RW. 2008. Major histocompatibility complex class I cytotoxic T lymphocyte immunity to human metapneumovirus (hMPV) in individuals with previous hMPV infection and respiratory disease. J Infect Dis 197:584–592. doi: 10.1086/526536. [DOI] [PubMed] [Google Scholar]
- 219.Ebihara T, Endo R, Kikuta H, Ishiguro N, Ishiko H, Hara M, Takahashi Y, Kobayashi K. 2004. Human metapneumovirus infection in Japanese children. J Clin Microbiol 42:126–132. doi: 10.1128/JCM.42.1.126-132.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Kolli D, Bataki EL, Spetch L, Guerrero-Plata A, Jewell AM, Piedra PA, Milligan GN, Garofalo RP, Casola A. 2008. T lymphocytes contribute to antiviral immunity and pathogenesis in experimental human metapneumovirus infection. J Virol 82:8560–8569. doi: 10.1128/JVI.00699-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Brooks DG, Trifilo MJ, Edelmann KH, Teyton L, McGavern DB, Oldstone MB. 2006. Interleukin-10 determines viral clearance or persistence in vivo. Nat Med 12:1301–1309. doi: 10.1038/nm1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Herd KA, Nelson M, Mahalingam S, Tindle RW. 2010. Pulmonary infection of mice with human metapneumovirus induces local cytotoxic T-cell and immunoregulatory cytokine responses similar to those seen with human respiratory syncytial virus. J Gen Virol 91:1302–1310. doi: 10.1099/vir.0.015396-0. [DOI] [PubMed] [Google Scholar]
- 223.Erickson JJ, Lu P, Wen S, Hastings AK, Gilchuk P, Joyce S, Shyr Y, Williams JV. 2015. Acute viral respiratory infection rapidly induces a CD8+ T cell exhaustion-like phenotype. J Immunol 195:4319–4330. doi: 10.4049/jimmunol.1403004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Rizzo LV, DeKruyff RH, Umetsu DT. 1992. Generation of B cell memory and affinity maturation. Induction with Th1 and Th2 T cell clones. J Immunol 148:3733–3739. [PubMed] [Google Scholar]
- 225.Herfst S, Fouchier RA. 2008. Vaccination approaches to combat human metapneumovirus lower respiratory tract infections. J Clin Virol 41:49–52. doi: 10.1016/j.jcv.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 226.MacPhail M, Schickli JH, Tang RS, Kaur J, Robinson C, Fouchier RA, Osterhaus AD, Spaete RR, Haller AA. 2004. Identification of small-animal and primate models for evaluation of vaccine candidates for human metapneumovirus (hMPV) and implications for hMPV vaccine design. J Gen Virol 85:1655–1663. doi: 10.1099/vir.0.79805-0. [DOI] [PubMed] [Google Scholar]
- 227.Pham QN, Biacchesi S, Skiadopoulos MH, Murphy BR, Collins PL, Buchholz UJ. 2005. Chimeric recombinant human metapneumoviruses with the nucleoprotein or phosphoprotein open reading frame replaced by that of avian metapneumovirus exhibit improved growth in vitro and attenuation in vivo. J Virol 79:15114–15122. doi: 10.1128/JVI.79.24.15114-15122.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Skiadopoulos MH, Biacchesi S, Buchholz UJ, Riggs JM, Surman SR, Amaro-Carambot E, McAuliffe JM, Elkins WR, St Claire M, Collins PL, Murphy BR. 2004. The two major human metapneumovirus genetic lineages are highly related antigenically, and the fusion (F) protein is a major contributor to this antigenic relatedness. J Virol 78:6927–6937. doi: 10.1128/JVI.78.13.6927-6937.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Tang RS, Mahmood K, Macphail M, Guzzetta JM, Haller AA, Liu H, Kaur J, Lawlor HA, Stillman EA, Schickli JH, Fouchier RA, Osterhaus AD, Spaete RR. 2005. A host-range restricted parainfluenza virus type 3 (PIV3) expressing the human metapneumovirus (hMPV) fusion protein elicits protective immunity in African green monkeys. Vaccine 23:1657–1667. doi: 10.1016/j.vaccine.2004.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Tang RS, Schickli JH, MacPhail M, Fernandes F, Bicha L, Spaete J, Fouchier RA, Osterhaus AD, Spaete R, Haller AA. 2003. Effects of human metapneumovirus and respiratory syncytial virus antigen insertion in two 3′ proximal genome positions of bovine/human parainfluenza virus type 3 on virus replication and immunogenicity. J Virol 77:10819–10828. doi: 10.1128/JVI.77.20.10819-10828.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Williams JV, Tollefson SJ, Johnson JE, Crowe JE Jr. 2005. The cotton rat (Sigmodon hispidus) is a permissive small animal model of human metapneumovirus infection, pathogenesis, and protective immunity. J Virol 79:10944–10951. doi: 10.1128/JVI.79.17.10944-10951.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Cox RG, Erickson JJ, Hastings AK, Becker JC, Johnson M, Craven RE, Tollefson SJ, Boyd KL, Williams JV. 2014. Human metapneumovirus virus-like particles induce protective B and T cell responses in a mouse model. J Virol 88:6368–6379. doi: 10.1128/JVI.00332-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Levy C, Aerts L, Hamelin ME, Granier C, Szecsi J, Lavillette D, Boivin G, Cosset FL. 2013. Virus-like particle vaccine induces cross-protection against human metapneumovirus infections in mice. Vaccine 31:2778–2785. doi: 10.1016/j.vaccine.2013.03.051. [DOI] [PubMed] [Google Scholar]
- 234.Bates JT, Pickens JA, Schuster JE, Johnson M, Tollefson SJ, Williams JV, Davis NL, Johnston RE, Schultz-Darken N, Slaughter JC, Smith-House F, Crowe JE Jr. 2016. Immunogenicity and efficacy of alphavirus-derived replicon vaccines for respiratory syncytial virus and human metapneumovirus in nonhuman primates. Vaccine 34:950–956. doi: 10.1016/j.vaccine.2015.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Liu P, Shu Z, Qin X, Dou Y, Zhao Y, Zhao X. 2013. A live attenuated human metapneumovirus vaccine strain provides complete protection against homologous viral infection and cross-protection against heterologous viral infection in BALB/c mice. Clin Vaccine Immunol 20:1246–1254. doi: 10.1128/CVI.00145-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Biacchesi S, Skiadopoulos MH, Yang L, Lamirande EW, Tran KC, Murphy BR, Collins PL, Buchholz UJ. 2004. Recombinant human metapneumovirus lacking the small hydrophobic SH and/or attachment G glycoprotein: deletion of G yields a promising vaccine candidate. J Virol 78:12877–12887. doi: 10.1128/JVI.78.23.12877-12887.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Herfst S, Schrauwen EJ, de Graaf M, van Amerongen G, van den Hoogen BG, de Swart RL, Osterhaus AD, Fouchier RA. 2008. Immunogenicity and efficacy of two candidate human metapneumovirus vaccines in cynomolgus macaques. Vaccine 26:4224–4230. doi: 10.1016/j.vaccine.2008.05.052. [DOI] [PubMed] [Google Scholar]
- 238.Yim KC, Cragin RP, Boukhvalova MS, Blanco JC, Hamlin ME, Boivin G, Porter DD, Prince GA. 2007. Human metapneumovirus: enhanced pulmonary disease in cotton rats immunized with formalin-inactivated virus vaccine and challenged. Vaccine 25:5034–5040. doi: 10.1016/j.vaccine.2007.04.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.de Swart RL, van den Hoogen BG, Kuiken T, Herfst S, van Amerongen G, Yuksel S, Sprong L, Osterhaus AD. 2007. Immunization of macaques with formalin-inactivated human metapneumovirus induces hypersensitivity to hMPV infection. Vaccine 25:8518–8528. doi: 10.1016/j.vaccine.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 240.Hamelin ME, Yim K, Kuhn KH, Cragin RP, Boukhvalova M, Blanco JC, Prince GA, Boivin G. 2005. Pathogenesis of human metapneumovirus lung infection in BALB/c mice and cotton rats. J Virol 79:8894–8903. doi: 10.1128/JVI.79.14.8894-8903.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Velayutham TS, Kolli D, Ivanciuc T, Garofalo RP, Casola A. 2013. Critical role of TLR4 in human metapneumovirus mediated innate immune responses and disease pathogenesis. PLoS One 8:e78849. doi: 10.1371/journal.pone.0078849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Zhang Y, Niewiesk S, Li J. 2014. Small animal models for human metapneumovirus: cotton rat is more permissive than hamster and mouse. Pathogens 3:633–655. doi: 10.3390/pathogens3030633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Goronzy JJ, Weyand CM. 2013. Understanding immunosenescence to improve responses to vaccines. Nat Immunol 14:428–436. doi: 10.1038/ni.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Shay T, Jojic V, Zuk O, Rothamel K, Puyraimond-Zemmour D, Feng T, Wakamatsu E, Benoist C, Koller D, Regev A, ImmGen Consortium . 2013. Conservation and divergence in the transcriptional programs of the human and mouse immune systems. Proc Natl Acad Sci U S A 110:2946–2951. doi: 10.1073/pnas.1222738110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Herd KA, Mahalingam S, Mackay IM, Nissen M, Sloots TP, Tindle RW. 2006. Cytotoxic T-lymphocyte epitope vaccination protects against human metapneumovirus infection and disease in mice. J Virol 80:2034–2044. doi: 10.1128/JVI.80.4.2034-2044.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Wen SC, Schuster JE, Gilchuk P, Boyd KL, Joyce S, Williams JV. 2015. Lung CD8+ T cell impairment occurs during human metapneumovirus infection despite virus-like particle induction of functional CD8+ T cells. J Virol 89:8713–8726. doi: 10.1128/JVI.00670-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Yamaguchi M, Kitagawa Y, Zhou M, Itoh M, Gotoh B. 2014. An anti-interferon activity shared by paramyxovirus C proteins: inhibition of Toll-like receptor 7/9-dependent alpha interferon induction. FEBS Lett 588:28–34. doi: 10.1016/j.febslet.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 248.Henrickson KJ. 2003. Parainfluenza viruses. Clin Microbiol Rev 16:242–264. doi: 10.1128/CMR.16.2.242-264.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Ma X, Yang X, Nian X, Zhang Z, Dou Y, Zhang X, Luo X, Su J, Zhu Q, Cai X. 2015. Identification of amino-acid residues in the V protein of peste des petits ruminants essential for interference and suppression of STAT-mediated interferon signaling. Virology 483:54–63. doi: 10.1016/j.virol.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 250.Rothlisberger A, Wiener D, Schweizer M, Peterhans E, Zurbriggen A, Plattet P. 2010. Two domains of the V protein of virulent canine distemper virus selectively inhibit STAT1 and STAT2 nuclear import. J Virol 84:6328–6343. doi: 10.1128/JVI.01878-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Chinnakannan SK, Nanda SK, Baron MD. 2013. Morbillivirus V proteins exhibit multiple mechanisms to block type 1 and type 2 interferon signalling pathways. PLoS One 8:e57063. doi: 10.1371/journal.pone.0057063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Childs K, Randall R, Goodbourn S. 2012. Paramyxovirus V proteins interact with the RNA helicase LGP2 to inhibit RIG-I-dependent interferon induction. J Virol 86:3411–3421. doi: 10.1128/JVI.06405-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Andrejeva J, Childs KS, Young DF, Carlos TS, Stock N, Goodbourn S, Randall RE. 2004. The V proteins of paramyxoviruses bind the IFN-inducible RNA helicase, mda-5, and inhibit its activation of the IFN-beta promoter. Proc Natl Acad Sci U S A 101:17264–17269. doi: 10.1073/pnas.0407639101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Ramaswamy M, Shi L, Varga SM, Barik S, Behlke MA, Look DC. 2006. Respiratory syncytial virus nonstructural protein 2 specifically inhibits type I interferon signal transduction. Virology 344:328–339. doi: 10.1016/j.virol.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 255.Elliott J, Lynch OT, Suessmuth Y, Qian P, Boyd CR, Burrows JF, Buick R, Stevenson NJ, Touzelet O, Gadina M, Power UF, Johnston JA. 2007. Respiratory syncytial virus NS1 protein degrades STAT2 by using the elongin-cullin E3 ligase. J Virol 81:3428–3436. doi: 10.1128/JVI.02303-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Malhotra R, Olsson H. 2015. Immunology, genetics and microbiota in the COPD pathophysiology: potential scope for patient stratification. Expert Rev Respir Med 9:153–159. doi: 10.1586/17476348.2015.1000865. [DOI] [PubMed] [Google Scholar]
- 257.von Messling V, Oezguen N, Zheng Q, Vongpunsawad S, Braun W, Cattaneo R. 2005. Nearby clusters of hemagglutinin residues sustain SLAM-dependent canine distemper virus entry in peripheral blood mononuclear cells. J Virol 79:5857–5862. doi: 10.1128/JVI.79.9.5857-5862.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Zipperle L, Langedijk JP, Orvell C, Vandevelde M, Zurbriggen A, Plattet P. 2010. Identification of key residues in virulent canine distemper virus hemagglutinin that control CD150/SLAM-binding activity. J Virol 84:9618–9624. doi: 10.1128/JVI.01077-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Bonami F, Rudd PA, von Messling V. 2007. Disease duration determines canine distemper virus neurovirulence. J Virol 81:12066–12070. doi: 10.1128/JVI.00818-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.von Messling V, Svitek N, Cattaneo R. 2006. Receptor (SLAM [CD150]) recognition and the V protein sustain swift lymphocyte-based invasion of mucosal tissue and lymphatic organs by a morbillivirus. J Virol 80:6084–6092. doi: 10.1128/JVI.00357-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Nakatsu Y, Takeda M, Ohno S, Shirogane Y, Iwasaki M, Yanagi Y. 2008. Measles virus circumvents the host interferon response by different actions of the C and V proteins. J Virol 82:8296–8306. doi: 10.1128/JVI.00108-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Mayer V, Schulman JL, Kilbourne ED. 1973. Nonlinkage of neurovirulence exclusively to viral hemagglutinin or neuraminidase in genetic recombinants of A-NWS (HON1) influenza virus. J Virol 11:272–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.von Messling V, Milosevic D, Cattaneo R. 2004. Tropism illuminated: lymphocyte-based pathways blazed by lethal morbillivirus through the host immune system. Proc Natl Acad Sci U S A 101:14216–14221. doi: 10.1073/pnas.0403597101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Govindarajan D, Samal SK. 2004. Sequence analysis of the large polymerase (L) protein of the US strain of avian metapneumovirus indicates a close resemblance to that of the human metapneumovirus. Virus Res 105:59–66. doi: 10.1016/j.virusres.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 265.Wen X, Krause JC, Leser GP, Cox RG, Lamb RA, Williams JV, Crowe JE Jr, Jardetzky TS. 2012. Structure of the human metapneumovirus fusion protein with neutralizing antibody identifies a pneumovirus antigenic site. Nat Struct Mol Biol 19:461–463. doi: 10.1038/nsmb.2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Leyrat C, Renner M, Harlos K, Grimes JM. 2013. Solution and crystallographic structures of the central region of the phosphoprotein from human metapneumovirus. PLoS One 8:e80371. doi: 10.1371/journal.pone.0080371. [DOI] [PMC free article] [PubMed] [Google Scholar]