Abstract
Aim of this study
Chemotherapy-induced peripheral neuropathy (CIPN) is a major complication of cancer patients with chemotherapy. Although many interventions have been evaluated in previous studies, findings are controversial. The aim of this meta-analysis is to assess the efficacy of vitamin E supplementation in preventing CIPN.
Material and methods
The electronic databases MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials were systematically searched from their inception to December 31, 2013 to identify relevant randomised controlled trials. Two reviewers independently scanned and extracted the data of included studies. Review Manager 5.2 was used to analyse data.
Results
Six articles involving 353 patients were included in meta-analysis. The results showed that vitamin E supplementation did not appear to significantly decrease the incidence of CIPN (relative risk (RR), 0.55; 95% confidence interval (CI), 0.29 to 1.05; p = 0.07), with significant heterogeneity (I2 = 77%). However, Vitamin E supplementation can significantly prevent cisplatin associated neurotoxicity (RR, 0.31; 95%CI, 0.17 to 0.58; p = 0.0002), with no heterogeneity (I2 = 0%).
Conclusions
Vitamin E administration dose not decrease the incidence of CIPN. However, additional randomised controlled trials using large samples are needed to confirm the role of vitamin E supplementation.
Keywords: vitamin E, chemotherapy, neuropathy, prevention, meta-analysis
Introduction
Chemotherapy-induced peripheral neuropathy (CIPN) is the most significant, troublesome, and dose-limiting adverse effect of cancer patients who received anticancer agents including cisplatin, oxaliplatin, taxanes, vinca alkaloids, thalidomide, and bortezomib [1, 2]. It has a huge impact on cancer survivors’ daily activities and quality of life [3]. CIPN presents as sensory symptoms such as paraesthesia, numbness, pain, and electric-shock-like [4], which may continue or worsen over weeks or months, even after discontinuation of chemotherapy. The prevalence of CIPN ranged from 3% to 7% in cancer patients who received single drugs, and increased to 38% in those treated with multiple chemotherapeutic drugs [5], although this percentage varies depending on chemotherapy regimens, duration of exposure, and assessment methods [6]. In clinical practice settings, CIPN is a major reason for interfering with treatment, resulting in a dose reduction, schedule delay, and cessation of therapy [7, 8].
Vitamin E is believed to play a role in protecting neuronal cell bodies against DNA damage and toxic accumulation, and several clinical studies have evaluated the effects of vitamin E during chemotherapy [9–15]. However, the power of the results is limited due to the small sample size. To accumulate evidence and address this issue, we conducted this meta-analysis to evaluate the effectiveness of vitamin E in preventing CIPN.
Material and methods
Search strategy
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement to report this meta-analysis study [16]. The electronic databases MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials were systematically searched from their inception to December 31, 2013. The searches were restricted to English publications and human subjects. The reference lists of the original and related reviews were also scanned to identify any potential relevant studies. The following search strategy was used: ((chemotherapy) AND (neurotoxicity OR neuropathy OR peripheral neuropathy OR peripheral neurotoxicity)) AND (vitamin E) AND (randomised controlled trial [pt] OR controlled clinical trial [pt] OR randomised [tiab] OR clinical trials as topic [mesh: no exp] OR randomly [tiab] OR trial [tiab]) NOT (animals [mh] NOT humans [mh]). If the results of the same patients were reported more than once, only the final results were included.
Study selection
The studies selected and included in the meta-analysis met the following inclusion criteria: 1) study design: randomised controlled trial (RCT); 2) intervention: oral vitamin E; (3) comparison intervention: placebo or standard care; 3) outcomes reporting: the incidence of neurotoxicity. Studies were excluded if they were non-RCT or were non-human related or were letter, comments, editorials, reviews, and grey literatures.
Data extraction
To ensure accuracy, two reviewers (H, H. P., and H, M) independently scanned and extracted the data of the included studies. Any disagreements were resolved by discussion and consensus. The following information was collected including the first author's name, year of publication, country, study design, sample size, age (years), and definition of intervention.
The primary outcome of interest was the incidence of neurotoxicity (relative risk [RR] with 95% confidence interval [CI]). The secondary outcome of interest was the safety of vitamin E administration.
Study quality assessment
The quality of the included studies was assessed by using the assessment tool described in the Cochrane Handbook for Systematic Reviews of Interventions [17]. All studies were assigned a judgment of low, unclear, or high risk of bias for the following six items: random sequence generation, allocation concealment, blinding (performance bias, detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias. Studies with low risk of bias for all key domains were considered as at low risk of bias. Studies with low or unclear risk for all key domains were considered as at unclear risk of bias. Studies with high risk of bias for any one or more key domains were considered as at high risk of bias [18, 19].
Statistical analysis
All the data analyses were performed using Review Manager 5.2 (Cochrane Collaboration, Oxford, United Kingdom) following recommendations from the Cochrane handbook. The results from the included studies were pooled to calculate relative risks (RRs) for dichotomous variables with 95% confidence intervals (CIs). We used Cochrane's Q test and the I2 statistic to assess heterogeneity among combined study results [20]. Heterogeneity between the included trials was indicated when the p-value for Cochran's Q test was < 0.1 and the I 2 value was > 50%. A random-effects model rather than a fixed-effects model was used as an option for this meta-analysis because the included studies had substantial variations of interventions, populations, and outcomes. Subgroup analyses were conducted based on various exclusion criteria. The small number of the included RCTs did not allow the estimation of potential publication bias with the funnel plot method for the outcomes. All tests were two-sided. P-value <0.05 was judged as statistically significant.
Results
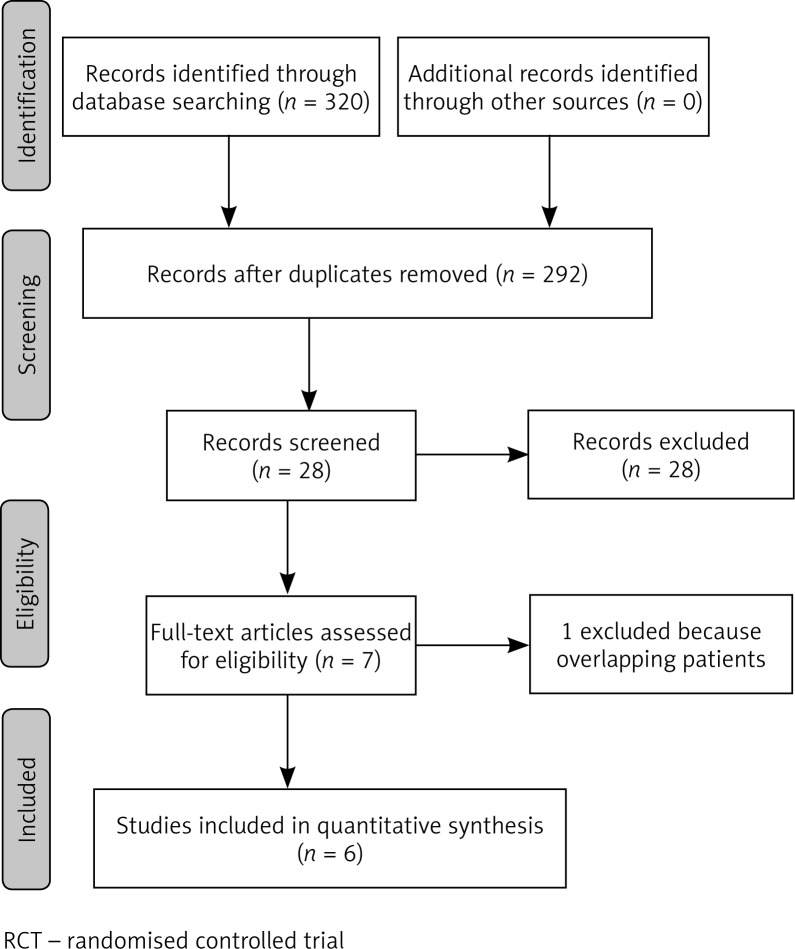
The search process is shown in Fig. 1. A total of 320 records were identified in the initial search. After scanning the titles and abstracts, 292 articles were excluded. We reviewed the full-text of 28 studies. Of these remaining studies, 22 studies were excluded with the following reasons: 21 were not RCTs, one article had overlapping patients [10]. Finally, six articles were included in the present meta-analysis study [9, 11–15].
Fig. 1.
Selection process for RCTs included in the meta-analysis
Characteristics of the included studies
The characteristics of the included studies are presented in Table 1. The sample size ranged from 27 to 189, and 353 patients were involved in the analysis. They were all published after 2003 and in English language. Two studies were conducted in Italy [9, 13], two in Greece [11, 12], one in the USA [14], and one in Brazil [15]. The types of chemotherapeutic formula included platinum-based [9, 12, 13, 15] therapy, paclitaxel-based therapy [11], and various chemotherapeutic agents [14]. The dosage of vitamin E in one study was 300 mg daily [9]; three studies were 300 mg twice daily [11–14], and in one study was 400 mg daily [15].
Table 1.
Characteristics of included studies
| Author (year, country) | Design | Number of patients | Age, years | Interventions | Incidence of neuropathy | |
|---|---|---|---|---|---|---|
| Vitamin E | Controls | |||||
| Pace et al. (2003, Italy) [9] | Randomised clinical study | 27 total; vitamin E: 13, unblinded control group: 14 | 58 (37 to 69) | 57 (28 to 74) | Vitamin E 300 mg/day starting before cisplatin and continuing up to 3 months after cisplatin treatment | Vitamin E: 30.7%, unblinded control group: 85.7%; p < 0.01; RR = 0.36 (95% CI: 0.15–0.83); p < 0.001 |
| Argyriou et al. (2006, Greece) [11] | Phase II, randomised clinical study | 32 total; vitamin E: 16, unblinded control group: 16 | 56.8 ±8.3 | 57.2 ±11.5 | Vitamin E 600 mg per day during chemotherapy and 3 months after its cessation | Vitamin E: 18.7%, unblinded control group: 62.5%; p = 0.03; RR = 0.3 (95% CI: 0.1–0.9) |
| Argyriou et al. (2006, Greece) [12] | Phase, randomised clinical study | 30 total; vitamin E: 14, unblinded control group: 16 | 53.6 ±14.8 | 59.3 ±12.8 | Vitamin E 600 mg/day or placebo during and for 3 months after completion of chemotherapy treatment | Vitamin E: 21.4%, unblinded control group: 68.5%; p = 0 .026; RR = 0.31 (95% CI: 0.11–0.9) |
| Pace et al. (2010, Italy) [13] | Randomised, controlled study | 41 total; vitamin E: 17, placebo: 24 | 58 (28–71) | 58.5 (32–74) | Vitamin E 400 mg per day before chemotherapy and lasted for 3 months after cisplatin therapy | Vitamin E: 5.9%, Placebo: 41.7%; p <0 .01; RR = 0.14 (95% CI: 0.02–1.00) |
| Kottschade et al. (2011, USA) [14] | phase III, randomised, controlled study | 189 total; vitamin E: 96, placebo: 93 | NR | NR | Vitamin E 300 mg, twice daily, initiated within 4 days before chemotherapy and continued 1 month after chemotherapy | Vitamin E: 34% (95% CI, 25.0% to 44.8%), Placebo: 29% (95% CI: 20.1–39.4%); p = 0.43 |
| Afonseca et al. (2013, Brazil) [15] | Phase II, randomised, controlled study | 34 total; vitamin E: 18, placebo: 16 | 56 (29–76) | 57 (40–71) | Vitamin E 400 mg/day, five days before starting oxaliplatin treatment until the end of the chemotherapy | Vitamin E: 83%, Placebo: 68%; p = 0.45 |
Age was reported as median (range) or mean ± SD
RR – relative risk; CI – confidence interval; NR – not reported
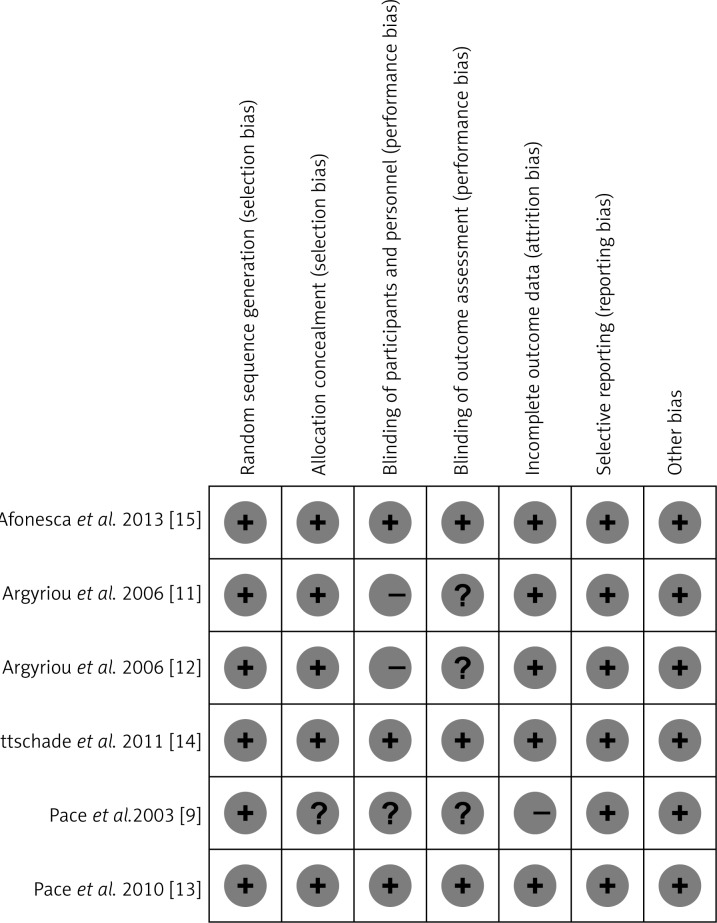
Outcomes of study quality assessment
Figure 2 shows the details of assessment for risk of bias tool. Five included studies used a computer to generate random numbers and adequately described the allocation concealment [11–15]. Three of six studies were double-blinded, placebo-controlled studies [13–15]. One of the studies had a high risk of incomplete outcome data bias [9]. In addition, all the studies had a low risk of selective reporting and other biases. Overall, three studies had a high risk of bias [9, 11, 12] and the others had a low risk of bias [13–15].
Fig. 2.
Summary for risk of bias assessment
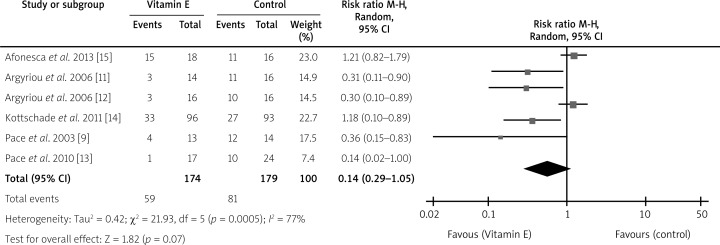
The effects of vitamin E on incidence of CIPN
All six studies [9, 11–15] were used to calculate the pooled incidence of CIPN in patients between two groups. Overall, the incidence of neurotoxicity in the vitamin E group was lower than in the placebo group (RR = 0.55; 95% CI: 0.29–1.05; p = 0.07; Fig. 3), and with significant heterogeneity (I2 = 77%). Table 2 shows the results of subgroup analysis based on various outcomes. Only one pooled result showed that vitamin E administration could significantly decrease the incidence of cisplatin-related neurotoxicity (RR = 0.31; 95% CI: 0.17–0.58; p = 0.0002), with low heterogeneity (I2 = 0%).
Fig. 3.
Meta-analysis of RCTs evaluating effects of vitamin E on incidence of CIPN. There was no significant effect on incidence of CIPN as determined by the random-effects model
Table 2.
Subgroup analyses for vitamin E in preventing chemotherapy-induced peripheral neuropathy
| Outcome | No. of patients | No. of studies | Vitamin E | Control subjects | RR (95% CI) | p-value | I2 (%) |
|---|---|---|---|---|---|---|---|
| All included studies | 353 | 6 | 59 of 174 | 81 of 179 | 0.55 (0.29–1.05) | 0.07 | 77 |
| High-quality trials (low risk of bias) | 264 | 3 | 49 of 131 | 48 of 133 | 1.03 (0.59–1.80) | 0.92 | 62 |
| Vitamin E vs. placebo | 264 | 3 | 49 of 131 | 48 of 133 | 1.03 (0.59–1.80) | 0.92 | 62 |
| Multicentre study | 230 | 2 | 34 of 113 | 37 of 117 | 0.50 (0.06–4.27) | 0.53 | 79 |
| Cisplatin-based formula | 98 | 3 | 8 of 44 | 33 of 54 | 0.31 (0.17–0.58) | 0.0002 | 0 |
RR – relative risk; CI – confidence interval
The safety of oral vitamin E
Four of the six included studies assessed the safety of vitamin E during chemotherapy [11, 12, 14, 15], and no adverse events were observed.
Discussion
CIPN is a significant adverse effect for cancer patients with chemotherapy; however, there are currently no confirmed effective preventative interventions available for clinical practice in patients with this complication. While many pharmacological agents such as glutathione [21], calcium and magnesium infusion [22], and venlafaxine [23] have been studied, CIPN continues to be a challenge in treating these patients.
The results from our meta-analysis provide some evidence that vitamin E supplementation does not decrease the incidence of neuropathy in cancer patients who are undergoing chemotherapy. In contrast, we found in subgroup analysis that vitamin E can significantly decrease the incidence of cisplatin-related neuropathy, which is in line with a previous systematic review [24]. A potential reason is the inclusion of many different types of chemotherapy in primary outcome analysis, which results in different mechanisms of action to induce neuropathy.
Additionally, the safety of vitamin E supplementation has also been tested in this meta-analysis. Patients in this study were given a high dose of vitamin E that varied from 300 mg to 600 mg per day, and no adverse effects and intolerance related to vitamin E administration were recorded. Meanwhile, one clinical study approved that vitamin E supplementation does not disturb the antitumor activities of chemotherapeutic agents [9]. However, the reasonable upper intake dosage of vitamin E is still controversial. One systematic review [25] suggested that high-dosage (> 400 IU/d) vitamin E supplements may increase all-cause mortality. In contrast, a recent meta-analysis [26] involving 246,371 subjects showed no relationship between dose and risk of mortality. Therefore, more well-designed clinical trials regarding the reasonable dosage and periods of vitamin E supplementation are needed.
The present meta-analysis also has several limitations that must be considered. Firstly, the small sample size of these studies makes this study less than convincing. Secondly, half of the included studies did not use the double-blinded method, which could result in performance bias. Thirdly, the included studies did not adequately evaluate long-term quality of life after using vitamin E, which is an important outcome for patients with cancer.
Chemotherapy-induced peripheral neuropathy is a troublesome complication of cancer patients receiving chemotherapeutic drugs. This meta-analysis show that vitamin E dose not significantly decrease the incidence of CINP. However, more high-quality studies with large sample size are needed to confirm these findings.
This study was supported by a grant from Mianyang Central Hospital (Funding number: 2014YJ28).
The authors declare no conflict of interest.
References
- 1.Park SB, Goldstein D, Krishnan AV, et al. Chemotherapy-induced peripheral neurotoxicity: A critical analysis. CA Cancer J Clin. 2013;63:419–37. doi: 10.3322/caac.21204. [DOI] [PubMed] [Google Scholar]
- 2.Burton AW, Fanciullo GJ, Beasley RD, et al. Chronic pain in the cancer survivor: a new frontier. Pain Med. 2007;8:189–98. doi: 10.1111/j.1526-4637.2006.00220.x. [DOI] [PubMed] [Google Scholar]
- 3.Driessen CM, de Kleine-Bolt KM, Vingerhoets AJ, et al. Assessing the impact of chemotherapy-induced peripheral neurotoxicity on the quality of life of cancer patients: the introduction of a new measure. Support Care Cancer. 2012;20:877–81. doi: 10.1007/s00520-011-1336-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han Y, Smith MT. Pathobiology of cancer chemotherapy-induced peripheral neuropathy. Front Pharmacol. 2013;18:156–72. doi: 10.3389/fphar.2013.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kautio AL, Haanpää M, Kautiainen H, et al. Burden of chemotherapy-induced neuropathy – a cross-sectional study. Support Care Cancer. 2011;19:1991–7. doi: 10.1007/s00520-010-1043-2. [DOI] [PubMed] [Google Scholar]
- 6.Cavaletti G, Cornblath DR, Merkies IS, et al. The chemotherapy-induced peripheral neuropathy outcome measures standardization study: from consensus to the first validity and reliability findings. Ann Oncol. 2013;24:454–62. doi: 10.1093/annonc/mds329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Visovsky C, Collins M, Abbott L, et al. Putting evidence into practice: evidence-based interventions for chemotherapy-induced peripheral neuropathy. Clin J Oncol Nurs. 2007;11:901–13. doi: 10.1188/07.CJON.901-913. [DOI] [PubMed] [Google Scholar]
- 8.Bhatnagar B, Gilmore S, Goloubeva O, et al. Chemotherapy dose reduction due to chemotherapy induced peripheral neuropathy in breast cancer patients receiving chemotherapy in the neoadjuvant or adjuvant settings: a single-center experience. Springerplus. 2014;3:366. doi: 10.1186/2193-1801-3-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pace A, Savarese A, Picardo M, et al. Neuroprotective effect of vitamin E supplementation in patients treated with cisplatin chemotherapy. J Clin Oncol. 2003;21:927–31. doi: 10.1200/JCO.2003.05.139. [DOI] [PubMed] [Google Scholar]
- 10.Argyriou AA, Chroni E, Koutras A, et al. Vitamin E for prophylaxis against chemotherapy-induced neuropathy: a randomized controlled trial. Neurology. 2005;64:26–31. doi: 10.1212/01.WNL.0000148609.35718.7D. [DOI] [PubMed] [Google Scholar]
- 11.Argyriou AA, Chroni E, Koutras A, et al. Preventing paclitaxel-induced peripheral neuropathy: a phase II trial of vitamin E supplementation. J Pain and Symptom Manage. 2006;32:237–44. doi: 10.1016/j.jpainsymman.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Argyriou AA, Chroni E, Koutras A, et al. A randomized controlled trial evaluating the efficacy and safety of vitamin E supplementation for protection against cisplatin-induced peripheral neuropathy: final results. Support Care Cancer. 2006;14:1134–40. doi: 10.1007/s00520-006-0072-3. [DOI] [PubMed] [Google Scholar]
- 13.Pace A, Giannarelli D, Galiè E, et al. Vitamin E neuroprotection for cisplatin neuropathy: a randomized, placebo-controlled trial. Neurology. 2010;74:762–6. doi: 10.1212/WNL.0b013e3181d5279e. [DOI] [PubMed] [Google Scholar]
- 14.Kottschade LA, Sloan JA, Mazurczak MA, et al. The use of vitamin E for the prevention of chemotherapy-induced peripheral neuropathy: results of a randomized phase III clinical trial. Support Care Cancer. 2011;19:1769–77. doi: 10.1007/s00520-010-1018-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Afonseca SO, Cruz FM, Cubero Dde I, et al. Vitamin E for prevention of oxaliplatin-induced peripheral neuropathy: a pilot randomized clinical trial. Sao Paulo Med J. 2013;131:35–8. doi: 10.1590/S1516-31802013000100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 17.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0. (updated March 2011) ( http://handbook.cochrane.org/). Last accessed 25 May 2014.
- 18.Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendation. BMJ. 2008;336:924–6. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cascinu S, Catalano V, Cordella L, et al. Neuroprotective effect of reduced glutathione on oxaliplatin-based chemotherapy in advanced colorectal cancer: a randomized, double-blind, placebo-controlled trial. J Clin Oncol. 2002;20:3478–83. doi: 10.1200/JCO.2002.07.061. [DOI] [PubMed] [Google Scholar]
- 22.Knijn N, Tol J, Koopman M, et al. The effect of prophylactic calcium and magnesium infusions on the incidence of neurotoxicity and clinical outcome of oxaliplatin-based systemic treatment in advanced colorectal cancer patients. Eur J Cancer. 2011;47:369–74. doi: 10.1016/j.ejca.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 23.Durand JP, Deplanque G, Montheil V, et al. Efficacy of venlafaxine for the prevention and relief of oxaliplatin-induced acute neurotoxicity. Ann Oncol. 2012;23:200–5. doi: 10.1093/annonc/mdr045. [DOI] [PubMed] [Google Scholar]
- 24.Albers JW, Chaudhry V, Cavaletti G, et al. Interventions for preventing neuropathy caused by cisplatin and related compounds. Cochrane Database Syst Rev. 2011;16:CD005228. doi: 10.1002/14651858.CD005228.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller ER, Pastor-Barriuso R, Dalal D, et al. Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Ann Intern Med. 2005;142:37–46. doi: 10.7326/0003-4819-142-1-200501040-00110. [DOI] [PubMed] [Google Scholar]
- 26.Abner EL, Schmitt FA, Mendiondo MS, et al. Vitamin E and all-cause mortality: a meta-analysis. Curr Aging Sci. 2011;4:158–70. doi: 10.2174/1874609811104020158. [DOI] [PMC free article] [PubMed] [Google Scholar]