Abstract
Background.
Resilience has been described in the psychosocial literature as the capacity to maintain or regain well-being during or after adversity. Physical resilience is a newer concept that is highly relevant to successful aging. Our objective was to characterize the emerging construct of resilience as it pertains to physical health in older adults, and to identify gaps and opportunities to advance research in this area.
Methods.
We conducted a systematic review to identify English language papers published through January 2015 that apply the term “resilience” in relation to physical health in older adults. We applied a modified framework analysis to characterize themes in implicit or explicit definitions of physical resilience.
Results.
Of 1,078 abstracts identified, 49 articles met criteria for inclusion. Sixteen were letters or concept papers, and only one was an intervention study. Definitions of physical resilience spanned cellular to whole-person levels, incorporated many outcome measures, and represented three conceptual themes: resilience as a trait, trajectory, or characteristic/capacity.
Conclusions.
Current biomedical literature lacks consensus on how to define and measure physical resilience. We propose a working definition of physical resilience at the whole person level: a characteristic which determines one’s ability to resist or recover from functional decline following health stressor(s). We present a conceptual framework that encompasses the related construct of physiologic reserve. We discuss gaps and opportunities in measurement, interactions across contributors to physical resilience, and points of intervention.
Key Words: Disablement process, Successful aging, Frailty, Physical function, Physiology
The percentage of the world population over age 60 has risen steadily in the 21st century and is expected to reach 21% by 2050 (1). Older age confers higher risk of many diseases, as well as age-related organ dysfunction, which in turn can lead to functional impairments, disability, or death (2). Age-associated physical decline, and especially loss of independence, can be devastating to individuals and costly to society (3). As life expectancy increases, health systems and communities are challenged to find sustainable, effective ways to promote successful aging, defined as the maintenance of physical, mental, and social well-being in old age (4).
One way to maintain health and function across the life span is to minimize the detrimental effects of injury, illness, or other stressors that inevitably occur in life. The concept of resiliency, the tendency to remain well or “bounce back” in the face of adversity, is not new (5). Resiliency was originally used to denote the elastic property of materials (6), but “resilience” has since been applied to systems, communities, and individuals. In recent decades, a robust literature has framed resilience as a psychological construct, referring to adaptive attitudes and behaviors that allow one to remain psychologically sound, or even thrive, after being exposed to stressful life events (7,8).
A related, but distinct, construct is that of physical resilience. Physical resilience relates to “the ability to recover or optimize function in the face of age-related losses or disease.” (9) We propose that physical resilience is a central aspect of successful aging. A deeper understanding of why some individuals maintain or regain function following insults, and others do not, may help to identify protective factors and promising strategies to promote lasting health.
An important step in advancing this line of research is to elaborate the construct of physical resilience, within the context of existing biomedical literature. To that end, we performed a systematic review to identify articles that apply the term “resilience” in regards to physical health and outcomes in older adults. Our objectives were to describe the current understanding of physical resilience in older adults, identify points of consensus and areas in need of clarification, and to highlight promising avenues for future work in this area.
Methods
Article Identification
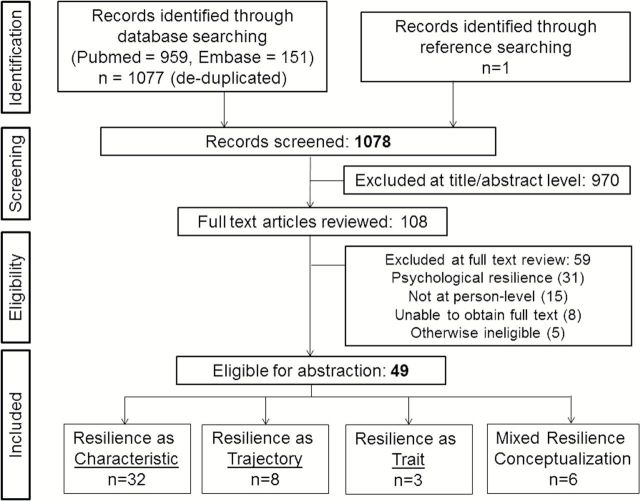
With assistance from a medical librarian, we searched PubMed and EMBASE from inception through January 15, 2015. In PubMed, we searched for text words in the title or abstract (resilient OR resilience OR resiliency), further limiting our search to English language and age 65+. In EMBASE, we searched for the same text words in the title or abstract, further limiting our search to English Language, Aged OR Very elderly, and citations unique to Embase. This search produced 1,077 abstracts (following removal of duplicates); one additional abstract (10) was identified from references during full text review, for a total of 1,078 abstracts (Figure 1).
Figure 1.
Flow diagram for systematic review of English language medical literature using the term “resilience” in reference to physical health of older adults.
Two reviewers independently evaluated each abstract to determine whether full text review was indicated. Articles identified by either investigator as potentially relevant were retrieved and underwent full text review by at least two investigators. Three reviewers (C.C.E., H.E.W., W.D.-P.) met to adjudicate all disagreements. We applied inclusion criteria: (a) must refer to or include persons over age 65; (b) must include or reference physiologic and/or physical indicators of resilience, functional reserve, or recovery. Studies were excluded when the following criteria were met: (a) focuses exclusively on neuroplasticity or cognitive resilience; (b) focuses exclusively on cell, organ, or tissue recovery; (c) focuses exclusively at a level above the individual (eg, community resilience following disaster); (d) conceptualizes resilience as a purely psychological, not physical, construct.
Data Abstraction
Two reviewers independently abstracted the following data elements from qualifying articles: (a) lead author’s location (country), (b) study design or article type, (c) study population, sample size, follow-up length, setting (if applicable), (d) stressor, exposure, and/or intervention, (e) whether resilience was defined explicitly or implicitly, (f) illustrative quote or definition of resilience, (g) physical or functional outcomes, and (h) other outcomes. Disagreements in data abstraction were resolved by committee.
Analysis
Quantitative Analysis
The literature was characterized in a descriptive manner, on the basis of the data elements abstracted from full text review (eg, article type; country of origin).
Qualitative Analysis
Framework analysis was employed to identify core concepts emerging from definitional resilience quotes. This analysis approach is particularly suited to healthcare research as it allows for pre-determined topics to be combined with inductive analyses, and it creates an explicit audit trail in the data reductions between analytic stages (11,12).
Stage 1: Familiarization
The quote that most clearly defined resilience, or illustrated the authors’ conceptualization of resilience, was abstracted from each article. All team members read all quotes.
Stage 2: Identifying a thematic framework
Following the familiarization stage, the team noted two ways in which authors’ conceptualizations of resilience could be categorized. First, resilience was measured or described at different levels within the organism: the whole person level, versus cell, tissue, or organ level. Second, as the reviewers considered authors’ language related to the construct of resilience, five distinct conceptual categories emerged: resilience as a characteristic (individual’s state which can change over time), trait (relatively fixed quality that is part of one’s nature), phenotype (an observable manifestation of underlying characteristics), capacity (maximum amount of stress that can be withstood), trajectory or process (change in symptoms or function over time). These categories were used as theme codes in stage 3.
Stage 3: Indexing
Each quotation was coded (indexed) by at least two team members to classify the way(s) that the author seemed to be conceptualizing physical resilience. Open coding was employed when quotes did not appear to fit within these themes; areas of uncertainty were resolved during team meetings.
Stage 4: Charting
We rearranged the coded quotations, and other data elements from the articles, so that quotes indexed within each of the five conceptual themes were together in the same spreadsheet.
Stage 5: Mapping and interpretation
We used the thematic charts to describe subthemes, explain the range and nature of resilience definitions, and compare between different levels and conceptions of resilience. At this stage, we identified gaps, areas in need of clarification, and opportunities to advance the field.
Results
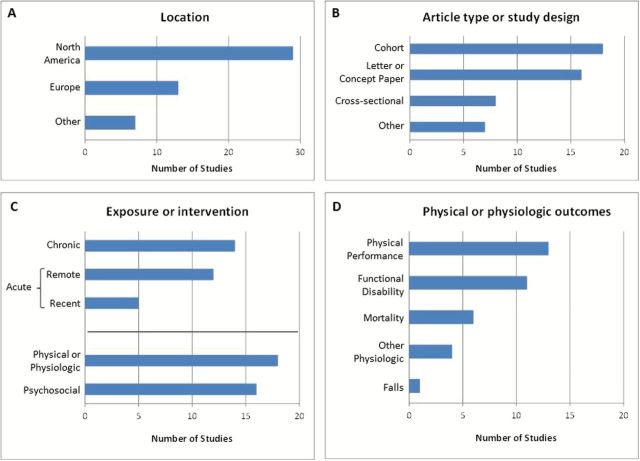
Forty-nine full text articles met inclusion/exclusion criteria (see Supplementary Appendix 1). Most articles excluded by title/abstract focused exclusively on psychosocial resilience (615) and/or neuroplasticity and cognitive resilience (55), rather than physical resilience. As seen in Figure 2, of the 49 selected articles, 29 (59.2%) originated from North America and 13 (26.5%) from Europe. Others were from Israel (4), Brazil (2), or Australia (1). Sixteen (32.7%) of the articles were letters or concept papers; eighteen (36.7%) reported results of longitudinal cohort studies and eight (16.3%) reported cross-sectional studies. The remaining articles included one mathematical modeling report (13), one case–control study (14), one case report (15), one qualitative analysis (16), two systematic reviews (17,18), and one intervention study (19).
Figure 2.
Description of 49 articles identified in this review. This modified systematic review sought to identify biomedical, English language articles published through January 15, 2015 that applied the term “resilience” in relation to physical health in older adults. Panel A describes the geographic location (of the first author); Panel B notes the type of article or study. Panel C: 29 of 49 articles referenced a particular kind of exposure or intervention (ie, stressor) after which there may, or may not, be a resilient response. Some articles referenced multiple stressors. The stressors were categorized as psychosocial (eg, death of spouse), or physical (eg, heat exposure), or both (eg, Holocaust) and could be chronic (eg, high blood pressure) or acute events that happened remotely (eg, airplane crash years earlier) or recently (eg, hospitalization). Panel D: 27 articles referenced or assessed particular outcomes related to physical health including mortality, self-reported function, physical performance, physiological measures, quality of life, and falls. Some articles included multiple outcome measures.
In 19 (38.8%), the authors explicitly defined resilience, whereas the remainder had only implied definitions. In the framework analysis, five conceptual categories (characteristic, trait, trajectory, phenotype, capacity) were applied as codes to each quote about physical resilience. Capacity always co-occurred (ie, was coded with) with characteristic; therefore, we collapsed these categories for the charting and mapping phases.
Physical resilience was conceptualized as a person-level trait (a relatively fixed characteristic, part of one’s nature) by only three authors (Figure 1). These articles described a trait determined by neurobiological, psychological, and social factors. Authors proposed using older “survivor” populations—those who did well despite exposure to high levels of remote or chronic stressors (eg, holocaust survivor, long-term smoker)—to study the biological underpinnings of resilience.
The ability of some individuals to reach extreme old age, particularly in the presence of… exposure to damaging factors, may signal an innate resiliency that could be related to slower rates of aging (20).
Eight articles primarily conceptualized resilience as a trajectory, or change in symptoms or function over time. Resilient trajectories were those that displayed recovery, rebound, or maintenance of function over time. Generally, both recovery of function and stable function were combined in defining “resilient” individuals. Most trajectory articles conceptualized resilience in response to some defined stressor or precipitating event, but several authors referred to functional trajectories that did not display expected age-related declines (21–23). Measures commonly used in studies conceptualizing resilience as a trajectory included change in functional status, cognition, walking speed, or self-rated health. These articles exclusively conceptualized resilience at a whole-person level.
Resilience has been defined as the capacity to remain well, recover, or even thrive in the face of adversity…[We] chose to conceptualize resilience as the response to a stressful life event (24).
Thirty-two authors primarily conceptualized resilience as a characteristic, an ability or capacity which can change over time. The ability to cope, resist damage, compensate, rebuild, adapt, and maintain homeostasis were described. Some authors referred to the “capacity” to adapt, or proposed measuring resilience as the amount of stress that could be borne. Authors noted that physical resilience is influenced by the interplay of complex biologic systems, psychosocial factors, environment, and behaviors.
Resilience indicates the ability to cope with stress and catastrophe and regain health by learning and adaptation. [B]iological resilience could be identified to recognize the protective factors (genetic, demographic, environmental, gender-linked, social, humoral, psychological and functional) that may contribute to positive outcomes in the very elderly (25).
Six articles framed physical resilience as both a characteristic and a trajectory. These authors frequently referred to a dynamic process by which one’s underlying resilience determines future health trajectories. Resilience itself was hypothesized to be influenced by earlier life events and one’s response to them. This literature often emphasized that resilience is observed in response to a stressor. Stressors might be recent events (eg, hip fracture) or remote experiences (eg, childhood poverty), or chronic exposures (eg, caregiving, disability, smoking).
Resilience has been described as a personal characteristic that likely develops over time. More recently, resilience has been viewed as a dynamic process that influences the ability to deal with, survive, overcome, learn from, and recover from inevitable adverse experiences of life (26).
Most authors referred to resilience at the whole person level, while a minority conceptualized it at the cellular/tissue/organ level, or at both levels. Many measures were used to capture resilience, including whole person outcomes (eg, mortality, functional status) and tissue/organ/system level responses to a stress test (eg, oral glucose tolerance test, laboratory induced falls). No cross-sectional tools or scales to measure the characteristic of physical or biomedical resilience were identified, although one “physical resilience” scale assessed psychological features or attitudes that predict recovery of physical function (9). While authors conceptualizing resilience as a characteristic implied that it can change within an individual, there was little or no discussion on how this could be accomplished. Nor did we identify studies targeting interventions to those with low resilience.
While frailty is commonly conceptualized in the literature as both a characteristic (ie, a “frail elder”) and a measurable phenotype (eg, low grip strength, slow gait speed, etc.), this duality was not clearly observed for the concept of resilience. The majority of authors conceptualized resilience as a characteristic, whereas none of the quotes primarily framed resilience as a phenotype. However, the discussion of resilience was often linked to phenotypic notions of frailty. The phenotypic descriptor that was most often associated with the underlying characteristic of resilience was “robust”, while several authors stated that the frailty phenotype indicates low levels of resilience.
Discussion
We used a systematic review with qualitative analysis to describe how physical resilience is conceptualized in the biomedical literature. As is evident by the diversity of themes and outcomes, there is no consensus in the field on how to define and measure physical resilience or the closely related concepts of reserve, frailty, and robustness. Because resilience is a potentially modifiable target for interventions to optimize function and quality of life in the aging population, a working definition of these terms is urgently needed.
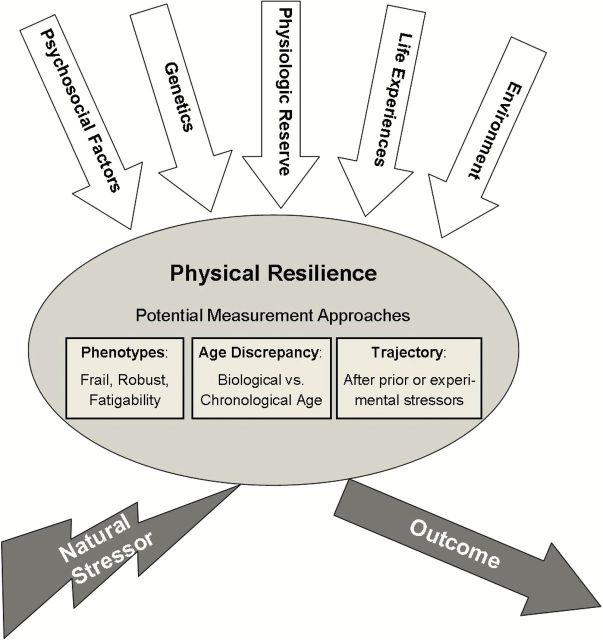
Proposal of a Uniform Model of Physical Resilience
We therefore propose the following definitions and conceptual framework describing the relationship between these concepts, which can be used as a basis for future work (Figure 3). We propose that physiologic reserve is the potential capacity of a cell, tissue, or organ system to function beyond its basal level in response to alterations in physiologic demands. Physiologic reserve can be measured by “stress testing” at the cell/tissue/organ/system level, which quantifies the response to a defined stressor or increased demand. Examples in medicine are the VO2max as a measure of cardiovascular reserve, or the expiratory reserve volume in pulmonary function tests.
Figure 3.
Proposed conceptual model of physical resilience. We propose that physical resilience at the whole person level, or one’s ability to resist decline or recover function following a stressor, is influenced by multiple factors, both internal and external to the individual. The white arrows represent several categories of presumed contributors to resilience, although this figure is not intended to provide an exhaustive list of contributors. Ultimately, the individual’s outcome is influenced by resilience as well as the magnitude and type of stressor. We suggest three potential strategies for quantifying the characteristic of “physical resilience” in future study, represented here as “windows” into the construct. Different measurement approaches may be more or less suitable depending on an investigator’s objectives and available data. For example, phenotypes and age discrepancy could theoretically be assessed by measurements taken at a single time point (cross-sectional) and without direct knowledge of the stressor, whereas quantifying resilience based on trajectories requires assessment at ≥2 time points and assumes a reasonably well-defined stressor.
In the proposed model, physical resilience is a characteristic at the whole person level which determines an individual’s ability to resist functional decline or recover physical health following a stressor. Physical resilience is constrained in part by underlying physiologic reserve across organ systems, and is further influenced by factors such as genetics and environment as well as psychosocial factors (including psychological resilience). Both physical and psychological resilience are manifest as one’s capacity to respond to stressors. Whether “usual aging” can be considered a stressor for examining resilience is a matter for subsequent debate.
Measuring the characteristic of physical resilience remains challenging. In contrast to psychological resilience where indices (surveys) have been developed to measure resilience at a point in time, no cross-sectional measures of physical resilience (as defined earlier) have been described. Based on our review, we suggest three potential ways to measure physical resilience. First, the most commonly employed indicator of physical resilience in existing literature relies on direct observation of functional trajectories. In this paradigm, a subject is classified as more or less resilient based on observed response to a stressor. Currently, trajectories that do not change in response to a stressor and those that decline but then recover are both referred to as indicators of resilience. Yet it is unclear whether these two patterns reflect different levels of underlying resilience or are a result of different underlying phenomena or contextual factors, such as the magnitude of the stressor(s). We suggest differentiating between “resistant trajectories” (no change in function following a stressor) and “resilient trajectories” (decline with subsequent recovery of function following a stressor) until this issue is clarified.
Certainly, trajectories are determined by intrinsic factors as well as extrinsic factors related to the severity and chronicity of the stressor(s). Thus, for a trajectory to be most useful as a resilience-related measure (as opposed to just an outcome), the investigator must consider extrinsic factors. Multiple study designs could utilize trajectory-based measurements of resilience. One approach is to use trajectory data from past stressors as an indicator of current and future resilience; a problem with this approach is that the experience of past stressors may affect reserve and resilience, rendering past trajectories unreliable indicators of future trajectories (even if the stressor is the same). Stress-response experiments are another study design that uses trajectory data to indicate resilience in the face of controlled, defined stressors. Dual-task or other paradigms can be used to gradually increase the stressor and define the point at which recovery is compromised or no longer occurs. In longitudinal cohort studies, participants may be categorized as resilient or non-resilient (at baseline) based on subsequent observed functional trajectories; measuring resilience in this way is problematic unless sufficient information is available about the stressors. Accurate measurement of the chronicity and severity of health stressors in longitudinal studies is an important and understudied aspect of this field.
Second, we support the idea that “frail versus robust phenotypes” are likely a reflection of underlying levels of physical resilience. These phenotypes have already been well described, and their association with favorable trajectories can be tested in longitudinal datasets. However, we suspect these phenotypes only represent the extremes of very low or high underlying resilience and it is likely that a decrease in resilience often precedes overt frailty. We believe that refining the measurement of resilience across a wider spectrum of older adults may lead to new insights or targets for intervention. Measures of fatigability describe the whole person’s response to stressors encountered in daily life, and may represent good indicators of resilience (27). Third, the difference between “chronological age versus biological age”, as measured by physical testing or biomarkers, may be a promising way to quantify the physical resilience of an individual (28). Presumably, those whose biological age is substantially “younger” than chronological age have maintained underlying reserve and demonstrated resilience to normal aging effects. It remains to be determined whether such individuals also exhibit high resilience in the face of new or acute stressors.
Gaps in the Field of Resilience
Based on these definitions, several key research areas need to be examined (see Box). First, cross-sectional measures of physical resilience need to be developed and validated. Such measures might include questionnaires for psychosocial factors and fatigability, measurement of physiologic reserve in key organ systems (neurologic, cardiovascular, immunologic, musculoskeletal), and/or biomarkers. Although the frailty phenotype may be a crude indicator of the underlying level of physical resilience, we believe that refining the measurement of resilience across a wider spectrum of older adults may lead to new insights and targets for intervention. The idea of “whole person” stress testing, in which the functional response to a defined stressor is measured, raises ethical concerns if done experimentally but may be possible under specific clinical conditions (eg, elective joint replacement, initiation of dialysis) or with stressors that challenge more than one organ system simultaneously. Levels of fatigability may be another indication of whole person response to stress. Trajectories of function following a well-defined stressor may be the best “gold standard” for validating such measures.
Box: Summary of Gaps and Opportunities for Future Research in the Area of Late Life Physical Resilience
| Gap | Key Research Questions and Directions |
|---|---|
| Measurement of physical resilience | 1) Approaches for assessing “resilient” and “resistant” functional trajectories |
| 2) Phenotypic measures that correlate to resilience—robustness versus frailty, fatigability or other whole body stress tests | |
| 3) Difference in chronological versus “biological age” | |
| 4) What is the best gold standard to validate new measures of physical resilience? | |
| 5) How do we quantify the severity and chronicity of stressors? | |
| Interactions between and across systems | 1) Does low reserve across multiple systems affect physical resilience in ways that are additive, synergistic, or follow complex dynamical relationships? |
| 2) How do we assess reserve across multiple systems in an ethical manner? | |
| 3) Does “reserve” in key systems influence the recovery phase, or merely affect the magnitude of perturbation from baseline? | |
| Effective interventions to optimize resilience | 1) Can we protect against future stressors by bolstering reserve and physical resilience during times of health? |
| 2) Are all types of reserve (or system-based resiliencies) equally important for all individuals or all types of stressors? | |
| 3) During times of stress, what models of care or health interventions optimize physical resilience? | |
| 4) Is there a role for Mithridatism in physical resilience (do low levels of health stressors increase resilience for future, more severe stressors)? |
Once measurement is refined, a better understanding of the factors underlying physical resilience will be possible. In particular, further study is needed to clarify the relationship between physical resilience and reserve. Physiological reserve may determine the magnitude of perturbation experienced by different people in response to a uniform stressor (how big a “hit” one takes) but it remains unknown whether reserve also plays a role in recovery (how quickly or fully one “bounces back”). Further, how does low reserve across multiple organ systems influence whole person response and resilience? Is it useful to consider not only whole-person resilience, but the notion of “resiliencies,” which acknowledges that a single person may exhibit a range of responses depending on the specific stressor(s) and the specific physiological systems being measured? Which organ systems have the greatest impact, and are relationships across systems additive, synergistic, or complex and dynamic?
Questions also remain about the interplay of intrinsic and extrinsic factors that determine response to stressors. How do genetics, health behaviors, the environment, and psychosocial factors influence resilience? How do characteristics of the stressor (chronicity, frequency, severity, type) modify physical resilience? One possibility is that chronic or past exposure to low-level stressors may enhance resilience to future stressors. This phenomenon, known as hormesis, has been offered as an explanation for why oxidative stress brought on by exercise has long-term beneficial effects through induced changes in mitochondrial metabolism (29). Mithraditism, or the practice of willfully exposing oneself to stressors or toxins in order to gain immunity or health benefits, has been operationalized—often controversially—in aging research with interventions including heat shock, prooxidants, and caloric restriction (30,31). On the other hand, the theory of allostatic load, which refers to the mounting physiological consequences for systems forced to respond and adapt to repeated or chronic stress and change, suggests that accumulating exposure chips away at reserve and resilience (32,33). Understanding how and when extrinsic factors modify the person-level characteristic of resilience has significant clinical implications.
Finally, it remains to be tested whether and how a physical resilience characteristic can be changed by interventions (exercise, immunomodulators, hormonal therapies, etc.). Likewise, it is unknown whether interventions or models of care that target older adults with low resilience can modify their subsequent functional trajectories during or after high risk events.
Conclusions
One objective of this review was to taxonomize the concept of physical resilience in existing biomedical literature. A second objective was to identify areas in need of clarification as well as to propose a working conceptual framework of physical resilience. Our approach has limitations: although we employed a broad search strategy and two reviewers at every step, it is possible that relevant articles were overlooked. Further, our qualitative analysis of resilience quotes relies on our interpretation of authors’ conceptual presentation of physical resilience, and mischaracterization is possible. These limitations notwithstanding, we present a comprehensive review of literature relevant to the emerging construct of physical resilience. While many experts in the field assert the role of physical resilience in successful aging, our process confirmed the need for a consensus definition and framework. In addition, we have highlighted three key areas that warrant future research: measurement of resilience, understanding how system-level reserve contributes to whole-person resilience, and interventions that promote physical resilience in the face of health challenges.
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/
Funding
This work was supported by the Duke Older American Independence Center (P30AG028716). Dr. Whitson is funded by the NIH (R01AG043438, R24AG045050), Alzheimer’s Association (NIRG-13-282202), and VA Rehabilitation Research and Development (I21 RX001721-01). Fellowship support for Dr. Duan-Porter was provided by Grant No.TPP 21–022 from the Department of Veteran Affairs Office of Academic Affiliations (VA OAA). Dr Colón-Emeric is funded by the NIH (R01 NR003178-11S1) and Department of Defense (W81XWH-12-2-0093).
Supplementary Material
Acknowledgments
We appreciate and acknowledge the contributions of Duke medical librarians Megan Von Isenburg and Virginia Carden. We are grateful to our colleagues at the National Institute on Aging, Basil Eldadah and Chhanda Dutta; their work has informed our group’s understanding of this emerging construct.
References
- 1. Population Ageing and Sustainable Development. 2014. http://www.un.org/en/development/desa/population/publications/pdf/popfacts/PopFacts_2014-4.pdf Accessed June 3, 2015.
- 2. Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–263. [DOI] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Prevalence of disabilities and associated health conditions among adults—United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50(7):120–125. PMID: 11393491 [PubMed] [Google Scholar]
- 4. Rowe JW, Kahn RL. Successful aging. The Gerontologist. 1997;37(4):433–440. [DOI] [PubMed] [Google Scholar]
- 5.Jain S, Sprengel M, Berry K, Ives J, Jonas W. 2014. The tapestry of resilience: an emerging picture. Interface Focus. 4: 20140057. http://dx.doi.org/10.1098/rsfs.2014.0057 [Google Scholar]
- 6. Tredgold T. On the Transverse Strength and Resilience of Timber. London, UK: Taylor & Francis; 1818. [Google Scholar]
- 7. Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71(3):543–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wagnild GM, Collins JA. Assessing resilience. J Psychosoc Nurs Ment Health Serv. 2009;47(12):28–33. [DOI] [PubMed] [Google Scholar]
- 9. Resnick B, Galik E, Dorsey S, et al. Reliability and validity testing of the physical resilience measure. The Gerontologist. 2011;51(5):643–652. [DOI] [PubMed] [Google Scholar]
- 10. Palleschi L, De Alfieri W, Salani B, et al. Functional recovery of elderly patients hospitalized in geriatric and general medicine units. The PROgetto DImissioni in GEriatria Study. J Am Geriatr Soc. 2011;59(2):193–199. [DOI] [PubMed] [Google Scholar]
- 11. Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. JOAAG. 2009;4(2):72–79. [Google Scholar]
- 12. Ritchie J, Spencer L. Qualitative data analysis for applied policy research. The Qualitative Researcher’s Companion. 2002:305–329. [Google Scholar]
- 13. Varadhan R, Seplaki CL, Xue QL, et al. Stimulus-response paradigm for characterizing the loss of resilience in homeostatic regulation associated with frailty. Mech Ageing Dev. 2008;129(11):666–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aschbacher K, O’Donovan A, Wolkowitz OM, et al. Good stress, bad stress and oxidative stress: insights from anticipatory cortisol reactivity. Psychoneuroendocrinology. 2013;38(9):1698–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Esche CA, Tanner EK. Resiliency: a factor to consider when facilitating the transition from hospital to home in older adults. Geriatr Nurs. 2005;26(4):218–222. [DOI] [PubMed] [Google Scholar]
- 16. Felten BS. Resilience in a multicultural sample of community-dwelling women older than age 85. Clin Nurs Res. 2000;9(2):102–123. [DOI] [PubMed] [Google Scholar]
- 17. Windle G, Bennett K, Noyes J. A methodological review of resilience measurement scales. Health Qual Life Outcomes. 2011;9(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jacoby SF, Ackerson TH, Richmond TS. Outcome from serious injury in older adults. J Nurs Scholarsh. 2006;38(2):133–140. [DOI] [PubMed] [Google Scholar]
- 19. Pai YC, Yang F, Bhatt T, et al. Learning from laboratory-induced falling: long-term motor retention among older adults. Age. 2014;36(3):1367–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Levine M, Crimmins E. Not all smokers die young: a model for hidden heterogeneity within the human population. PLoS One. 2014;9:e87403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Walter-Ginzburg A, Shmotkin D, Blumstein T, et al. A gender-based dynamic multidimensional longitudinal analysis of resilience and mortality in the old-old in Israel: the cross-sectional and longitudinal aging study (CALAS). Soc Sci Med. 2005;60(8):1705–1715. [DOI] [PubMed] [Google Scholar]
- 22. Hogan M. Physical and cognitive activity and exercise for older adults: a review. Int J Aging Hum Dev. 2005;60(2):95–126. [DOI] [PubMed] [Google Scholar]
- 23. Tolea MI, Ferrucci L, Costa PT, et al. Personality and reduced incidence of walking limitation in late life: findings from the Health, Aging, and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2012;67(6):712–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hardy SE, Concato J, Gill TM. Resilience of community-dwelling older persons. J Am Geriatr Soc. 2004;52(2):257–262. [DOI] [PubMed] [Google Scholar]
- 25. De Alfieri W, Costanzo S, Borgogni T. Biological resilience of older adults versus frailty. Med Hypotheses. 2011;76:304–305. [DOI] [PubMed] [Google Scholar]
- 26. Resnick B. Resilience in aging: the real experts. Geriatr Nurs. 2008;29(2):85–86. [DOI] [PubMed] [Google Scholar]
- 27. Eldadah BA. Fatigue and fatigability in older adults. PM R. 2010;2:406–413. [DOI] [PubMed] [Google Scholar]
- 28. Belsky DW, Caspi A, Houts R, et al. Quantification of biological aging in young adults. Proc Natl Acad Sci U S A. 2015;112:E4104–E4110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ristow M, Zarse K. How increased oxidative stress promotes longevity and metabolic health: the concept of mitochondrial hormesis (mitohormesis). Exp Gerontol. 2010;45:410–418. [DOI] [PubMed] [Google Scholar]
- 30. Gems D, Partridge L. Stress-response hormesis and aging: “that which does not kill us makes us stronger”. Cell Metab. 2008;7:200–203. [DOI] [PubMed] [Google Scholar]
- 31. Rattan SI. Hormesis in aging. Ageing Res Rev. 2008;7:63–78. [DOI] [PubMed] [Google Scholar]
- 32. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–179. [DOI] [PubMed] [Google Scholar]
- 33. Wikby A, Ferguson F, Forsey R, et al. An immune risk phenotype, cognitive impairment, and survival in very late life: impact of allostatic load in Swedish octogenarian and nonagenarian humans. J Gerontol A Biol Sci Med Sci. 2005;60:556–565. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.