Abstract
Background
It is postulated that obstructive sleep apnea (OSA) is a risk factor for the development of depression. However, obesity and excessive daytime sleepiness (EDS) are associated with both OSA and depression. The goal of this study was to examine the relative contribution of OSA, obesity, and EDS to incident depression.
Methods
A representative random sample of 1,137 adults without depression from the Penn State Adult Cohort was followed-up after 7.5 years. All subjects underwent a full medical examination and polysomnography (PSG) at baseline. OSA was defined as an apnea/hypopnea index (AHI) ≥ 5, overweight as a body mass index (BMI) of 25-29.9 kg/m2, obesity as a BMI ≥ 30 kg/m2, and EDS as moderate-to-severe drowsiness/sleepiness and/or irresistible sleep attacks.
Results
Overweight, obesity, and EDS were associated with incident depression, whereas OSA alone was not. Overweight was associated with incident depression in women, while obesity and EDS were associated with incident depression in both genders. The association of overweight and obesity with incident depression was independent of premorbid emotional distress, while that of EDS was not. The association between BMI and EDS with incident depression was stronger in women 20-40 years old. The severity of EDS predicted incident depression in those with OSA, while AHI or oxygen desaturation did not.
Conclusions
Overweight, obesity and EDS are the main predictors of incident depression. Obesity may be linked to depression through psychobiological mechanisms, while EDS may be an early sign of depression. Obesity should be a target of our preventative strategies for depression.
Keywords: Depression, obesity, polysomnography, sleep apnea, sleepiness
Introduction
Depression is a highly prevalent psychiatric disorder associated with significant morbidity and mortality.1-3 Sleep and sleep disorders have been associated with depression in clinical and population studies.4-6 However, information from longitudinal population-based studies on incident depression that have included polysomnographic (PSG) data is very limited. Few epidemiologic studies have examined the association of obstructive sleep apnea (OSA) with depression and their results have been modest and inconsistent.5 While cross-sectional clinical studies have found a higher frequency of depressive symptoms and depression in patients with OSA,5 only one population-based study to date has examined the longitudinal association of OSA with depression.7 Furthermore, these studies have not systematically examined the role of obesity and excessive daytime sleepiness (EDS), factors frequently associated with OSA, in the association of OSA with incident depression.
Obesity, particularly central obesity as measured by visceral adiposity, is considered a key etiopathogenic mechanism of OSA and its cardinal symptom of EDS.8,9 Moreover, obesity is a risk factor for depression10 and is independently associated with EDS;11-15 in fact, the association of obesity with EDS is stronger than that of OSA per se or of measures of its severity, such as the number of apneas or degree of oxygen desaturation.11-15 This is important because depression has been shown to be associated with EDS both in cross-sectional 11 and longitudinal studies,14 which suggests a potential bidirectional association between EDS and depression. Given the lack of population-based studies examining the association of OSA, obesity, and EDS with the development of depression, the aim of this longitudinal study was to test the predictive role and relative contribution of OSA, body weight, and EDS for incident depression in a large random, general population sample.
Methods and Materials
Participants
The data presented here were collected as part of a population-based study of sleep disorders, which used a 2-phase protocol to recruit participants from various age groups.11, 16-18 Please see Figure 1 for details on the sampling procedure and response rates. Of the 1,741 subjects who completed the sleep laboratory evaluation (Phase II) and gave written informed consent, 1,395 subjects were followed-up after an average duration of 7.5 years via telephone interview.19-22 After complete description of the follow-up study to the subjects, verbal informed consent was obtained. The whole study procedure was approved by the Penn State University's Institutional Review Board. Figure 1 shows the participant flow in the present study.
Figure 1. Participants' flow in the study.
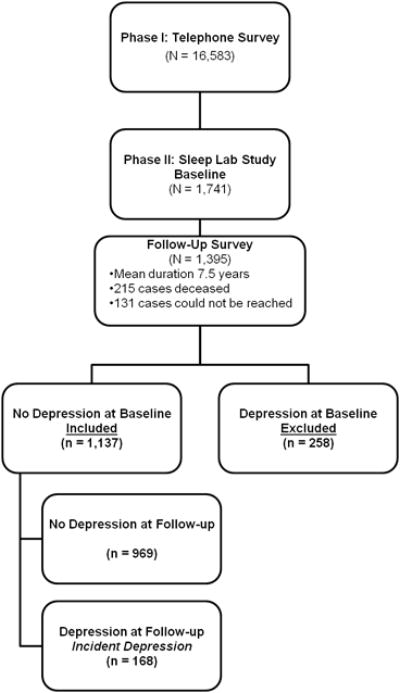
Definition of Incident Depression
For the purposes of the current study, the presence of depression at baseline was defined by a self-report of a current or past (i.e., lifetime) history of physician diagnosis or treatment of depression, based on a standardized questionnaire completed by the subjects on the evening of their sleep laboratory visit.23 Commensurate with the baseline definition, depression at follow-up was defined by a self-report of a current or past (i.e., since baseline) history of physician diagnosis or treatment of depression taken through telephone interview. Of the 1,395 subjects who were followed up, 1,137 did not have depression at baseline and were selected for the present study. A total of 168 subjects were incident cases of depression, whereas 969 did not have depression at follow-up (see Figure 1).
Predictors of Interest
All subjects were evaluated for one night in the sleep laboratory in sound-attenuated, light- and temperature-controlled rooms. During this evaluation, each subject was continuously monitored for 8 hours (fixed-time period) using 16-channel PSG including electroencephalogram, electrooculogram, and electromyogram. Bedtimes were adjusted to conform to subjects' usual bedtimes, and subjects were recorded between 22:00-23:00 and 06:00-07:00. The sleep recordings were subsequently scored independently, according to Rechtschaffen and Kales criteria.24 Respiration was monitored throughout the night by use of thermocouples at the nose and mouth and thoracic strain gauges. All-night recordings of hemoglobin oxygen saturation (SpO2) were obtained with an oximeter attached to the finger. Apnea was considered present if a breath cessation exceeded 10 seconds and each apnea was categorized in terms of obstructive (chest wall movement present) or central (chest wall movement absent). In addition, hypopnea was considered present when a reduction in airflow of approximately 50% was indicated at the nose or mouth and was associated with a reduction of 4% arterial blood oxygen saturation.17,18 The presence of OSA was defined as an obstructive apnea/hypopnea index (OHI) ≥ 5 events per hour of sleep.
Body mass index was based on measured height (cm) and weight (kg) during the subjects' sleep laboratory visit. Overweight and obesity were defined as a BMI of 25-29.9kg/m2 and BMI ≥ 30 kg/m2, respectively. 15,23,25
Commensurate with our previous studies,11,15 the presence of EDS was established based on a moderate-to-severe self-report of daytime drowsiness or sleepiness occurring most of the day (“Do you feel drowsy or sleepy most of the day but manage to stay awake?”) and/or irresistible daytime sleep attacks (“Do you have any irresistible sleep attacks during the day?”). Each question was answered on a 4-point Likert scale (0 = none, 1 = mild, 2 = moderate, and 3 = severe), and the presence of EDS was defined as a moderate or severe report to either of the 2 questions.
Other Measurements
The presence of other sleep, physical and mental health problems as well as substance use was also ascertained in the standardized questionnaire at baseline. The presence of sleep difficulty was established on 3 levels of severity: normal sleep, poor sleep, and insomnia, as reported elsewhere. 15, 16, 19, 20-23,26-30 As part of the standardized questionnaire and physical examination we ascertained whether the subject had a lifetime or current history of physical health problems (i.e., allergies/asthma, anemia, birth defect, cancer or tumor, colitis, encephalitis, epilepsy, heart disease, kidney or bladder problems, migraine, Parkinson's, rheumatism, stroke, thyroid problems, ulcer), including the presence of hypertension, defined by a self-report of use of antihypertensive medication or a diastolic blood pressure ≥ 90 mmHg and/or a systolic blood pressure ≥ 140 mmHg taken during the evening of the sleep lab evaluation,26 and diabetes, defined by a self-report of being treated for diabetes or having a fasting blood glucose levels ≥126 mg/dl from blood drawn the morning after the subject's sleep lab evaluation.27 A lifetime or current history of other mental health problems (i.e., alcohol use disorder, drug use disorder, loneliness, marital problems, suicide attempts, and suicide thoughts) was also ascertained at baseline. Participants' daily caffeine (number of cups/day), tobacco (number of cigarettes/day), and alcohol (number of drinks/day) consumption was also ascertained at baseline. The level of emotional stress was measured by the Minnesota Multiphasic Personality Inventory-2 (MMPI-2).31 T scores with a mean of 50 and a standard deviation (SD) of 10 are generated for the eight major clinical scales. Scores ≥ 65 (1.5 SD above the mean) indicate a significant deviation from the original normal standardization pattern of responding and suggested an elevation at a clinically significant level.31
Statistical Analyses
The current study focuses on 1,137 individuals without depression at baseline. First, descriptive univariate analyses examined the incidence of depression in the overall sample as well as stratified by gender and age across predictors of interest, i.e., overweight (n = 398), obesity (n = 570), OSA (n = 235), and EDS (n = 143). Second, logistic regression models were used to test potential significant interactions between demographic characteristics (i.e., gender and age) and the predictors of interest as well as between each other (i.e., BMI, OSA, and EDS). Third, multivariable logistic regression models examined the independent association and relative contribution of overweight, obesity, OSA, and EDS in predicting incident depression after progressively adjusting for potential confounders. Fourth, multivariable logistic regression models examined the relative contribution and independent association of overweight or obesity, OSA, and EDS in predicting incident depression after progressively adjusting for potential confounders in men and women separately. Finally, given that EDS is a cardinal symptom of OSA,11 the role of the severity of daytime sleepiness (i.e., none, mild, moderate, and severe) as well as that of AHI and SpO2 in predicting incident depression within individuals with OSA was also examined in a multivariable logistic regression model. All analyses were conducted with IBM SPSS version 21.0.
Results
The final study sample of individuals without depression at baseline was comprised of 1,137 adults (49.3 ± 13.3y) of whom 48% were females and 94% Caucasian. The overall incidence of depression was 15% and the demographic, behavioral, and clinical characteristics associated with incident depression, including baseline BMI (p < .001), are presented in Table 1.
Table 1. Demographic, Clinical, and Behavioral Characteristics and Incident Depression.
| Incident Depression | |||
|---|---|---|---|
| No (n = 969) |
Yes (n = 168) |
||
| Sex | |||
| Male (n = 531), % | 93.2 | 6.8 | |
| Female (n = 606), % | 78.2 | 21.8 | .00001** |
| Race | |||
| Caucasian (n = 1039), % | 85.2 | 14.8 | .886 |
| Non-Caucasian (n = 98), % | 85.7 | 14.3 | |
| Age | 53.4 ± 13.1 | 52.2 ± 12.2 | .267 |
| 20-29 (n = 49), % | 95.9 | 4.1 | .040* |
| 30-39 (n = 115), % | 80.0 | 20.0 | |
| 40-49 (n = 292), % | 81.8 | 18.2 | |
| 50-59 (n = 301), % | 87.7 | 12.3 | |
| 60-69 (n = 243), % | 85.2 | 14.8 | |
| ≥ 70 (n = 137), % | 87.6 | 12.4 | |
| BMI, kg/m2 | 30.6 ± 6.0 | 32.9±6.7 | .00001** |
| Caffeine, cups/day | 2.3 ± 2.6 | 1.8 ± 2.8 | .079T |
| No (n = 411), % | 81.5 | 18.5 | .008* |
| ≥ 1 cup/day (n = 726), % | 87.3 | 12.7 | |
| Tobacco, cigarettes/day | 2.9 ± 8.6 | 2.4 ± 6.3 | .338 |
| No (n = 959), % | 85.4 | 14.6 | .696 |
| ≥ 1 n/day (n = 178), % | 84.3 | 15.7 | |
| Alcohol, drinks/day | 1.0 ± 4.8 | 0.4 ± 1.7 | .002** |
| No (n = 880), % | 83.3 | 16.7 | .001** |
| ≥ 1 drink/day (n = 257), % | 91.8 | 8.2** | |
| Physical Health Problemsa | |||
| No (n = 166), % | 90.4 | 9.6 | .040* |
| Yes (n = 971), % | 84.3 | 15.7 | |
| Mental Health Problemsb | |||
| No (n = 1029), % | 85.8 | 14.2 | .085T |
| Yes (n = 108), % | 79.6 | 20.4 | |
| Sleep Difficulty | |||
| Normal Sleep (n = 758), % | 88.1 | 11.9 | .00001** |
| Poor Sleep (n = 285), % | 80.4 | 19.6 | |
| Insomnia (n = 94), % | 76.6 | 23.4 | |
includes a lifetime history of allergies/asthma, anemia, birth defect, cancer or tumor, colitis, encephalitis, epilepsy, heart disease, kidney or bladder problems, migraine, Parkinson's, rheumatism, stroke, thyroid problems, ulcer, hypertension (diastolic blood pressure ≥ 90 mmHg and/or a systolic blood pressure ≥ 140 mmHg or use of antihypertensive medication), and diabetes (fasting blood glucose levels ≥126 mg/dl or treatment for diabetes).
includes a lifetime history of alcohol use disorder, drug use disorder, loneliness, marital problems, suicide attempts, and suicide thoughts.
p ≤ .10
p ≤ .05
p ≤ .01
As shown in Table 2, obesity was a significant predictor of incident depression (OR = 2.44, 95%CI = 1.36-4.39, p = .003). Overweight was also a significant predictor of incident depression in women (OR = 2.13, 95%CI = 1.02-4.43, p = .044), which suggested that the relationship between body weight and the incidence of depression was gender-specific (Figure 2 plot A). Furthermore, we found a significant interaction between BMI and age on the incidence of depression (p =.016), i.e., for an increase of BMI by one unit, the risk of incident depression was greater among the younger individuals than in the older ones. In fact, the interaction between BMI and age was significant in women (p = .035) but not in men (p = .461), which further indicated that the relationship of overweight and obesity with the incidence of depression was gender-specific and age-dependent. As shown in Figure 2 plot B, the incidence of depression in obese women was highest in younger adults (39.0%), plateaued in middle-aged (26.1%), and decreased in older adults (15.8%), while the incidence of depression in overweight women was significantly higher than in normal weight women (p = .041) but did not significantly change as a function of age (25% vs. 25% vs. 23% for overweight young, middle-age, and older women, respectively). In contrast, the incidence of depression in obese men was significantly higher than in normal weight men (p = .051) but did not significantly change as a function of age (10% vs. 9% vs. 11% for obese young, middle-age, and older men, respectively).
Table 2. Incidence of Depression in the Study Sample and Stratified by Gender and Age.
| Overall (N = 1,137) |
Men (n = 531) |
Women (n =606) |
≤ 40 years (n = 186) |
41-59 years (n = 571) |
≥ 60 years (n = 380) |
|
|---|---|---|---|---|---|---|
| BMI | ||||||
| < 25 | 8.3 | 3.6 | 12.9 | 9.1 | 8.6 | 6.8 |
| ≥ 25 | 12.8 | 5.7 | 24.0* | 13.1 | 11.3 | 14.9 |
| ≥ 30 | 18.1** | 9.4T | 22.9* | 27.1* | 18.1T | 14.9 |
| OSA | ||||||
| No | 15.5 | 6.8 | 21.9 | 18.2 | 15.8 | 13.6 |
| Yes | 11.9 | 6.7 | 20.9 | 9.5 | 9.9 | 15.1 |
| EDS | ||||||
| No | 13.1 | 5.8 | 19.5 | 13.2 | 12.7 | 13.5 |
| Yes | 26.6** | 13.8* | 37.2** | 40.7** | 25.0** | 18.8 |
All data are incidence (%) of depression across all levels of predictor variables in the overall sample and in men and women as well as in young, middle-aged, and older adults. BMI = body mass index. OSA = obstructive sleep apnea. EDS = excessive daytime sleepiness.
p ≤ .10
p ≤ .05
p ≤ .01
Figure 2. Incidence of depression associated with body mass index and excessive daytime sleepiness: effects of gender and age.
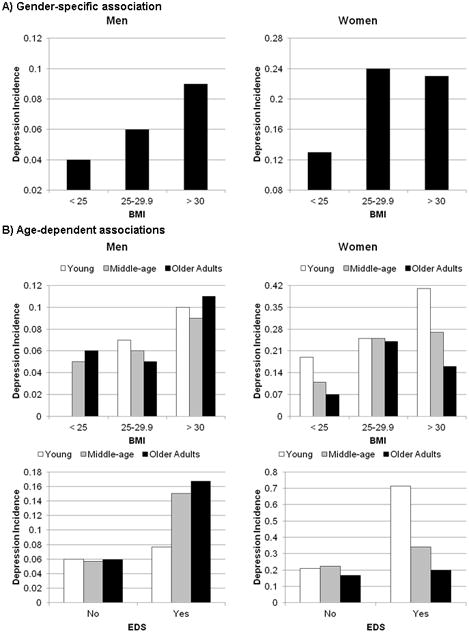
Please note that the vertical axes are in a different scale for men and women given the strong gender difference as mentioned below. Plot A) the incidence of depression reached statistical significance at the obese cut-off (BMI ≥ 30) in men, while the incidence of depression reached statistical significance at the overweight cut-off (BMI ≥ 25) in women. The incidence of depression associated with EDS reached statistical significance in both men and women (see Results). Plot B) the incidence of depression in obese women increased as a function of age, while the incidence of depression was significantly increased in overweight women regardless of age. In men, the incidence depression was significantly higher in the obese than normal weight and did not change as a function of age. Furthermore, the incidence of depression in women with EDS increased as a function of younger age; conversely, the order was reversed in men with EDS, such that the incidence of depression was greatest in older and middle-aged men.
As shown in Table 2, EDS was also a significant predictor of incident depression (OR = 2.41, 95%CI = 1.59-3.64, p = .00003) in both men (OR = 2.61, 95%CI = 1.17-5.84, p = .019) and women (OR = 2.44, 95%CI = 1.47-4.06, p = .001). Similarly to BMI, we found a significant interaction between EDS and age on incident depression in women (p=.033), but not in men (p = .957), i.e., the risk of incident depression associated with EDS was greater among younger women than older women. As shown in Figure 2 plot C, the incidence of depression in women with EDS was highest among young adults (71.4%) than middle-aged (34.1%) or older (20.0%) adults. In contrast, the incidence of depression in men with EDS was greater among older (16.7%) and middle-aged (15.0%) adults than in young (7.7%) adults.
Multivariable logistic regression models indicated that the association of BMI (OR = 2.07, 95%CI = 1.08-3.96, p =.029 and OR = 2.03, 95%CI = 1.09-3.78, p =.026, for overweight and obesity, respectively) and EDS (OR = 1.87, 95%CI = 1.18-2.99, p =.008) with incident depression was independent of multiple potential confounders (Table 3). Interestingly, the association of overweight (OR = 2.12, 95% CI = 1.0-4.50, p = .051) and obesity (OR=2.12, 95% CI = 1.03-4.37, p = .042) with incident depression remained significant even after further adjusting for premorbid emotional distress, as measured by MMPI number of elevations at baseline; however, EDS became non-significantly associated with incident depression after such adjustment (OR = 1.29, 95% CI = 0.73-2.28, p=.384).
Table 3. Multivariable Odds Ratio (95%CI) of Incident Depression for Overweight, Obesity, OSA, and EDS.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| BMI | ||||
| < 25 | --- | --- | --- | --- |
| ≥ 25 | 2.07 (1.09-3.95)* | 2.07 (1.08-3.95)* | 2.04 (1.07-3.90)* | 2.07 (1.08-3.96)* |
| ≥ 30 | 2.19 (1.19-4.06)* | 2.15 (1.16-3.98)* | 2.02 (1.08-3.75)* | 2.03 (1.09-3.78)* |
| OSA | ||||
| No | --- | --- | --- | --- |
| Yes | 1.02 (0.64-1.62) | 1.00 (0.63-1.60) | 1.00 (063-1.60) | 1.00 (0.63-1.60) |
| EDS | ||||
| No | --- | --- | --- | |
| Yes | 2.23 (1.43-3.46)** | 1.98 (1.24-3.14)** | 1.93 (1.21-3.06)** | 1.87 (1.18-2.99)** |
Model 1 = adjusted for each other (i.e., BMI, OSA, and EDS) as well as gender, race, and age.
Model 2 = adjusted for each other as well as gender, race, age, caffeine, tobacco, alcohol consumption, and sleep difficulty.
Model 3 = adjusted for each other as well as gender, race, age, caffeine, tobacco, alcohol consumption, sleep difficulty, and physical health problems.
Model 4 = adjusted for each other as well as gender, race, age, caffeine, tobacco, alcohol consumption, sleep difficulty, physical health problems, and mental health problems.
p ≤ .05
p ≤ .01
Given the gender-specific association observed above, we examined the multivariable association of BMI, EDS, and OSA with incident depression while stratifying by gender. As shown in Table 4, these multivariable logistic regression models replicated the findings in the overall sample (Table 3), with the exception of marginally significant trends for EDS when physical or mental health problems were included in the models. Of note, these stratified models should be interpreted with caution given the small number of men who developed depression (n = 36). Furthermore, we stratified these multivariable logistic regression models by age groups of young (≤ 40y), middle-aged (41-59y), and older (≥ 60y) adults. These multivariable regression models showed that obesity was significantly associated with incident depression in young adults (OR = 3.85, 95%CI = 1.20-12.30, p = .023) but not in middle-aged (OR = 1.96, 95%CI = 0.79-4.90, p = .148) or older (OR = 1.87, 95%CI = 0.53-6.56, p = .330) adults, while EDS was significantly associated with incident depression in young (OR = 5.00, 95%CI = 1.77-14.08, p = .002) and middle-aged (OR = 2.04, 95%CI = 1.13-3.68, p = .018) adults but not in older adults (OR = 1.67, 95%CI = 0.63-4.43, p = .305).
Table 4. Multivariable Odds Ratio (95%CI) of Incident Depression in Women and Men.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Women | ||||
| BMI < 25 | --- | --- | --- | --- |
| BMI ≥ 25 | 2.20 (1.11-4.39)* | 2.20 (1.09-4.45)* | 2.10 (1.03-4.27)* | 2.11 (1.03-4.30)* |
| OSA | ||||
| No | --- | --- | --- | --- |
| Yes | 1.08 (0.60-1.92) | 1.07 (0.60-1.92) | 1.06 (0.59-1.90) | 1.06 (0.59-1.89) |
| EDS | ||||
| No | --- | --- | --- | --- |
| Yes | 2.10 (1.24-3.53)** | 1.81 (1.05-3.14)* | 1.73 (1.00-3.01)T | 1.72 (0.99-2.99) T |
| Men | ||||
| BMI < 30 | --- | --- | --- | --- |
| BMI ≥ 30 | 1.96 (0.98-3.94) T | 1.84 (0.91-3.72) T | 1.78 (0.88-3.63) | 1.78 (0.87-3.64) |
| OSA | ||||
| No | --- | --- | --- | --- |
| Yes | 0.87 (0.40-1.90) | 0.88 (0.40-1.93) | 0.88 (0.40-1.92) | 0.92 (0.42-2.01) |
| EDS | ||||
| No | --- | --- | --- | --- |
| Yes | 2.66 (1.18-5.98)* | 2.43 (1.04-5.71)* | 2.43 (1.04-5.71)* | 2.31 (0.98-5.46) T |
Model 1 = adjusted for each other (i.e., BMI, OSA, and EDS) as well as race and age
Model 2 = adjusted for each other as well as race, age, caffeine, tobacco, alcohol consumption, and sleep difficulty
Model 3 = adjusted for each other as well as race, age, caffeine, tobacco, alcohol consumption, sleep difficulty, and physical health problems.
Model 4 = adjusted for each other as well as race, age, caffeine, tobacco, alcohol consumption, sleep difficulty, physical health problems, and mental health problems.
p ≤ .10
p ≤ .05
p ≤ .01
OSA was not significantly associated with increased odds of incident depression in the univariate analysis presented in Table 2 (OR = 0.74, 95%CI = 0.48-1.14, p = .167) and remained non-significantly associated with incident depression in all the multivariable adjusted regression models in the overall sample (Table 3) as well as when stratified by gender (Table 4) or young, middle-aged, and older adult groups (p-value for OSA by age interaction = .222). These results remained similar and in the same direction even when different cut-offs to define OSA were used; specifically, as compared to those with AHI < 5, the multivariable-adjusted OR (95% CI) of incident depression in those with AHI 5-14.9, AHI 15-29.9, and AHI ≥ 30 were 1.11 (0.62-2.01, p = .718), 0.76 (0.33-1.77, p = .530), and 1.11 (0.40-3.06, p = .845), respectively. Moreover, no significant interaction was found between OSA and BMI (p = .512) on incident depression; of note, however, only 8.1% of individuals with OSA were normal weight, while the vast majority was overweight (30.2%) or obese (61.7%). In individuals with OSA, multivariable regression models showed that female gender (OR = 4.95, 95%CI = 1.46-16.7, p = .010) and the severity of EDS were significant predictors of incident depression (OR = 2.00, 95%CI = 1.08-3.71, p = .027); in contrast, neither AHI (OR = 1.00, 95%CI = 0.99-1.02, p = .633) or SpO2 (OR = 0.99, 95%CI = 0.95-1.03, p = .569), markers of the severity of sleep-disordered breathing, were significantly associated with incident depression in individuals with OSA.
Discussion
This study shows that obesity and daytime sleepiness are strong predictors of incident depression. Importantly, female gender is not only a strong predictor of incident depression but an important modifier of the relationship between overweight and incident depression. Furthermore, the incidence of depression associated with overweight, obesity, and EDS in men and women is significantly age-dependent so that 1) overweight is associated with increased risk of incident depression from young through older adulthood in women, 2) obesity is associated with incident depression in young adult women and such association decreases with age, 3) obesity, but not overweight, is associated with incident depression from young through older adulthood in men, and 4) EDS is associated with incident depression in young adult women and such association decreases with age. Finally, this study also showed that the severity of EDS, but not the severity of disordered breathing, predicts incident depression in those with OSA.
Obstructive Sleep Apnea as a predictor of Depression
Despite clinical studies showing a higher frequency of depressive symptoms in patients with OSA, cross-sectional population-based studies have reported modest and inconsistent effects.5 Moreover, only one population-based longitudinal study reported an increased risk of depression associated with incident or worsened OSA over a 4-year follow-up period.7 In the overall sample, we did not find a significant association between baseline OSA and incident depression. A possible explanation of these seemingly discrepant findings could be that incident or worsened OSA is associated with weight gain, 32 a known risk factor for incident depression.10,32 Together, these studies suggest that OSA and depression are likely to coexist given their mutual association with weight gain, but that OSA alone may not be a premorbid predictor of incident depression. There is the possibility that those individuals with a longer history of OSA who also had depression at baseline and were excluded from this incident cohort may have had a significantly higher prevalence of depression; however, a cross-sectional analysis at baseline (N = 1,741) indicated that the prevalence of depression was similar (p =.161) in those with (18.3%) and without OSA (21.8%). The only relevant factors found to be associated with incident depression in individuals with OSA, were female gender, which is known to double the risk of depression in the general population, and the severity of EDS. This latter finding is consistent with previous studies showing that EDS and depression predict each other,11, 15 particularly in sleep apneics.34 Importantly, the vast majority of OSA participants were overweight or obese (91.9 %), which may explain the high rates of depressive symptoms or depression found in clinical samples of patients with OSA, as discussed below.
Overweight and Obesity as predictors of Depression
We found that overweight and obesity were strong predictors of incident depression, a finding that is consistent with previous studies.10 A novel finding of this study is that gender is a significant modifier of the relationship between body mass index and incident depression. We found that obesity significantly increased the risk of incident depression in both women and men, whereas overweight does so only in women. Psychosocial factors may be a potential mechanism explaining this gender-specific relationship; for example, the increased social pressure towards lean body shapes in women that may impact perceived body shape and associated self-esteem may put women at risk of developing depression at lower levels of body weight (i.e., overweight). Given the known association of depression with changes in the stress (i.e., hypothalamic-pituitary-adrenal axis) 35,36 and immune (i.e., chronic low-grade inflammation) 37,38 systems, it needs to be further investigated whether overweight women may be experiencing metabolic and/or inflammatory changes predisposing them to depression, which is consistent with our findings that overweight and obesity increased the risk of incident depression independent of premorbid emotional distress.
Furthermore, the incidence of depression associated with BMI was significantly age-dependent. We found that the incidence of depression in overweight women remained significantly elevated and stable from young to older adulthood, whereas the incidence of depression in obese women peaked in young adulthood, plateau in middle-age (to the incidence rate found in overweight women), and decreased in older adults. These data indicate that young obese women should be a priority in the prevention of depression and that educational as well as therapeutic efforts should be put on this more vulnerable group. It is likely that combined multifactorial strategies addressing obesity as well as cognitive-emotional and behavioral factors as early as childhood may improve the prevention of depression and other morbidity associated with obesity in young women.
In contrast, overweight was not significantly associated with incident depression in men. This finding gives some support to the potential effect of psychosocial factors in the development of depression in overweight women vs. men (e.g., there is a higher social acceptance of overweight men, men are less likely to base their self-esteem on body shape, and men are less socially targeted in terms of expectations of body shape). However, obesity was indeed a significant predictor of incident depression also in men and this association was stable from young to older adulthood and independent of premorbid emotional distress. These data suggest that cognitive-emotional (i.e., self-efficacy or self-worth based on difficulty meeting typical male expectations in areas such as work, family, and sex may contribute to negative affect and feelings of worthlessness) and behavioral (i.e., sedentary and physical inactivity) 39 factors as well as metabolic and/or inflammatory 35-38 ones associated with obesity may be potential mechanisms of the increased incidence of depression in obese men.
Excessive Daytime Sleepiness as a predictor of Depression
Previous cross-sectional and longitudinal studies have shown that EDS is associated with prevalent and incident depression. 11, 40-43 From a clinical point of view, our findings and those of previous longitudinal studies 42,43 suggest that there is a bidirectional relationship between EDS and depression. In the present study the association of EDS with incident depression was partially explained by premorbid emotional distress, which suggests that EDS may be an early clinical sign of depression. Similarly to overweight and obesity, a potential mechanisms for the association of EDS with incident depression may be physical inactivity, limited engagement in mastery activities, and sedentary lifestyle. This cyclical relationship between EDS and physical inactivity may contribute to the onset of clinically depressed mood. Alternatively, there is the possibility that individuals with EDS may have been given a diagnosis of depression when their symptoms, such as lack of interest and motivation, would have been more accurately captured as sequelae of EDS, rather than depression per se. From another pathophysiological point of view, the data on the association of EDS with chronic low-grade inflammation 12-14,44 suggest that EDS, associated or not with OSA, 45-47 may be an early sign of low-grade inflammation predisposing to depression.48 Future population-based studies should examine the role of inflammatory markers in the association of EDS and OSA with incident depression. In summary, as EDS may be an early sign of depression with multiple contributing factors, it appears that it should be assessed and treated with cognitive-behavioral or pharmacological treatments to help prevent the onset of a major depressive episode.
Limitations
Some limitations should be taken into account when interpreting our results. First, our definition of depression was based on a self-report of physician diagnosis or treatment for depression. We did not use a structured clinical interview to diagnose depression or a standardized questionnaire assessing the severity of depressive symptoms. However, the prevalence (17%), incidence (15%), gender-related and age-related rates of depression in the Penn State Adult Cohort19,23, 27-29 are consistent with those of previous population-based studies 49-51, which increases our confidence about the replicability and generalizability of our findings. The consistency of our results with those of a previous meta-analysis10 in terms of overall incidence rate of depression in those who are overweight and obese, as well as the dose-response of weight, increases our confidence about the replicability and generalizability of the present findings. Second, we did not ascertain EDS using standardized questionnaires or physiologic measures of daytime sleep propensity, i.e., multiple sleep latency test. Despite the limitations of using two items to ascertain the complaint of EDS, these items specifically referred to two core symptoms used in the diagnosis of hypersomnia (sleepiness or drowsiness and irresistible sleep attacks) and capture the complaints typically expressed by patients.1 Importantly, the prevalence estimate in the Penn State Cohort using this definition of EDS11 is consistent with that of other population-based studies, where the complaint of EDS is defined based on severity criteria.54,55 Third, our analyses on the role of clinical factors predicting incident depression within individuals with OSA may lack power because of the small number of OSA subjects who developed depression (n=28). Future studies should examine the incidence of depression using a larger population-based sample of individuals with OSA.
Conclusion
In summary, overweight, obesity and EDS, with or without OSA, are independent predictors of incident depression. The treatment of overweight and obesity as well as EDS should become a priority in the prevention of depression.
Acknowledgments
This work was performed at the Sleep Research and Treatment Center at the Penn State University Milton Hershey Hospital, and the staff is especially commended for their efforts. This research was funded in part by the American Heart Association (14SDG19830018) and the National Institutes of Health (R01 51931, R01 40916, and R01 64415).
Funding: This research was funded in part by the American Heart Association (14SDG19830018) and the National Institutes of Health (R01 51931, R01 40916, and R01 64415).
Footnotes
Conflict of Interest: The authors declare no conflict of interest.
Financial Disclosures: All authors reported no biomedical financial interests or potential conflicts of interest.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. American Psychiatric Association; Arlington, VA, USA: 2013. [Google Scholar]
- 2.Simon GE. Social and economic burden of mood disorders. Biol Psychiatry. 2003;54:208–215. doi: 10.1016/s0006-3223(03)00420-7. [DOI] [PubMed] [Google Scholar]
- 3.Schulz R, Drayer RA, Rollman BL. Depression as a risk factor for non-suicide mortality in the elderly. Biol Psychiatry. 2002;52:205–225. doi: 10.1016/s0006-3223(02)01423-3. [DOI] [PubMed] [Google Scholar]
- 4.Benca RM, Peterson MJ. Insomnia and depression. Sleep Med. 2008;9:S3–S9. doi: 10.1016/S1389-9457(08)70010-8. [DOI] [PubMed] [Google Scholar]
- 5.Harris M, Glozier N, Ratnavadivel R, Grunstein RR. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13:437–444. doi: 10.1016/j.smrv.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Peppard PE, Szklo-Coxe M, Hla KM, Young T. Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med. 2006;166:1709–1715. doi: 10.1001/archinte.166.16.1709. [DOI] [PubMed] [Google Scholar]
- 8.Vgontzas AN, Bixler EO, Chrousos GP. Sleep apnea is a manifestation of the metabolic syndrome. Sleep Med Rev. 2005;9:211–224. doi: 10.1016/j.smrv.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Kritikou I, Basta M, Vgontzas AN, Pejovik S, Liao D, Tsaoussoglou M, et al. Sleep apnoea, sleepiness, inflammation and insulin resistance in middle-aged males and females. Eur Respir J. 2014;43:145–155. doi: 10.1183/09031936.00126712. [DOI] [PubMed] [Google Scholar]
- 10.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 11.Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A. Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab. 2005;90:4510–4515. doi: 10.1210/jc.2005-0035. [DOI] [PubMed] [Google Scholar]
- 12.Vgontzas AN, Papanicolaou DA, Bixler EO, Kales A, Tyson K, Chrousos GP. Elevation of plasma cytokines in disorders of excessive daytime sleepiness: role of sleep disturbance and obesity. J Clin Endocrinol Metab. 1997;82:1313–1316. doi: 10.1210/jcem.82.5.3950. [DOI] [PubMed] [Google Scholar]
- 13.Vgontzas AN, Bixler EO, Chrousos GP. Obesity-related sleepiness and fatigue: the role of the stress system and cytokines. Ann N Y Acad Sci. 2006;1083:329–344. doi: 10.1196/annals.1367.023. [DOI] [PubMed] [Google Scholar]
- 14.Panossian LA, Veasey SC. Daytime sleepiness in obesity: mechanisms beyond obstructive sleep apnea--a review. Sleep. 2012;35:605–615. doi: 10.5665/sleep.1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fernandez-Mendoza J, Vgontzas AN, Kritikou I, Calhoun SL, Liao D, Bixler EO. Natural history of excessive daytime sleepiness: Role of obesity, weight loss, depression, and sleep propensity. Sleep. 2015;38:351–360. doi: 10.5665/sleep.4488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bixler EO, Vgontzas AN, Lin HM, Vela-Bueno A, Kales A. Insomnia in central Pennsylvania. J Psychosom Res. 2002;53:589–592. doi: 10.1016/s0022-3999(02)00450-6. [DOI] [PubMed] [Google Scholar]
- 17.Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med. 1998;157:144–148. doi: 10.1164/ajrccm.157.1.9706079. [DOI] [PubMed] [Google Scholar]
- 18.Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001;163:608–613. doi: 10.1164/ajrccm.163.3.9911064. [DOI] [PubMed] [Google Scholar]
- 19.Fernandez-Mendoza J, Vgontzas AN, Liao D, Shaffer ML, Vela-Bueno A, Basta M, et al. Insomnia with objective short sleep duration and incident hypertension: the Penn State Cohort. Hypertension. 2012;60:929–935. doi: 10.1161/HYPERTENSIONAHA.112.193268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singareddy R, Vgontzas AN, Fernandez-Mendoza J, Liao D, Calhoun S, Shaffer ML, et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep Med. 2012;13:346–353. doi: 10.1016/j.sleep.2011.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vgontzas AN, Fernandez-Mendoza J, Bixler EO, Singareddy R, Shaffer ML, Calhoun SL, et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012;35:61–68. doi: 10.5665/sleep.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fernandez-Mendoza J, Vgontzas AN, Bixler EO, Singareddy R, Shaffer ML, Calhoun SL, et al. Clinical and polysomnographic predictors of the natural history of poor sleep in the general population. Sleep. 2012;35:689–697. doi: 10.5665/sleep.1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fernandez-Mendoza J, Shea S, Vgontzas AN, Calhoun SL, Liao D, Bixler EO. Insomnia and incident depression: Role of objective sleep duration and natural history. J Sleep Res. 2015;24:390–398. doi: 10.1111/jsr.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rechtschaffen A, Kales A. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. National Institutes of Health; Bethesda, MD, USA: 1968. [Google Scholar]
- 25.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United State, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32:491–497. doi: 10.1093/sleep/32.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO. Insomnia with objective short sleep duration is associated with type 2 diabetes: A population-based study. Diabetes Care. 2009;32:1980–1985. doi: 10.2337/dc09-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernandez-Mendoza J, Calhoun S, Bixler EO, Pejovic S, Karataraki M, Liao D, et al. Insomnia with objective short sleep duration is associated with deficits in neuropsychological performance: a general population study. Sleep. 2010;33:459–465. doi: 10.1093/sleep/33.4.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Basta M, et al. Insomnia with short sleep duration and mortality: the Penn State cohort. Sleep. 2010;33:1159–1164. doi: 10.1093/sleep/33.9.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fernandez-Mendoza J, Calhoun SL, Bixler EO, Karataraki M, Liao D, Vela-Bueno A, et al. Sleep misperception and chronic insomnia in the general population: role of objective sleep duration and psychological profiles. Psychosom Med. 2011;73:88–97. doi: 10.1097/PSY.0b013e3181fe365a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Butcher JN, Graham JR, Ben-Porah YS, Tellegen A, Dahkstrom WG. Manual for administration, scoring and interpretation, revised edn. University of Minnesota Press; Minneapolis, MN, USA: 2001. [Google Scholar]
- 32.Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284:3015–3021. doi: 10.1001/jama.284.23.3015. [DOI] [PubMed] [Google Scholar]
- 33.Stunkard AJ, Faith MS, Allison KC. Depression and obesity. Biol Psychiatry. 2003;54:330–337. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- 34.Basta M, Lin HM, Pejovic S, Sarriginnidis A, Bixler EO, Vgontzas AN. Lack of regular exercise, depression, and degree of apnea are predictors of excessive daytime sleepiness in patients with sleep apnea: Sex differences. J Clin Sleep Med. 2008;4:19–25. [PMC free article] [PubMed] [Google Scholar]
- 35.Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs low CRH/NE states. Mol Psychiatry. 2002;7:254–275. doi: 10.1038/sj.mp.4001032. [DOI] [PubMed] [Google Scholar]
- 36.Stetler C, Miller GE. Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom Med. 2011;73:114–126. doi: 10.1097/PSY.0b013e31820ad12b. [DOI] [PubMed] [Google Scholar]
- 37.Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65:732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Valkanova V, Ebmeier KP, Allan CL. CRP, IL-6 and depression: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2013;150:736–744. doi: 10.1016/j.jad.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 39.Petersen L, Schnohr P, Sørensen TI. Longitudinal study of long-term relation between physical activity and obesity in adults. Int J Obes Relat Metab Disord. 2004;28:105–112. doi: 10.1038/sj.ijo.0802548. [DOI] [PubMed] [Google Scholar]
- 40.Breslau N, Roth T, Rosenthal L, Andreski P. Daytime sleepiness: an epidemiological study of young adults. Am J Public Health. 1997;87:1649–1653. doi: 10.2105/ajph.87.10.1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hasler G, Buysse DJ, Gamma A, Ajdacic V, Eich D, Rössler W, et al. Excessive daytime sleepiness in young adults: a 20-year prospective community study. J Clin Psychiatry. 2005;66:521–529. doi: 10.4088/jcp.v66n0416. [DOI] [PubMed] [Google Scholar]
- 42.Jaussent I, Bouyer J, Ancelin ML, Akbaraly T, Pérès K, Ritchie K, et al. Insomnia and daytime sleepiness are risk factors for depressive symptoms in the elderly. Sleep. 2011;34:1103–1110. doi: 10.5665/SLEEP.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Quan SF, Katz R, Olson J, Bonekat W, Enright PL, Young T, et al. Factors associated with incidence and persistence of symptoms of disturbed sleep in an elderly cohort: the Cardiovascular Health Study. Am J Med Sci. 2005;329:163–172. doi: 10.1097/00000441-200504000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Vgontzas AN, Bixler EO, Chrousos GP, Pejovic S. Obesity and sleep disturbances: meaningful sub-typing of obesity. Arch Physiol Biochem. 2008;114:224–236. doi: 10.1080/13813450802521507. [DOI] [PubMed] [Google Scholar]
- 45.Vgontzas AN. Does obesity play a major role in the pathogenesis of sleep apnoea and its associated manifestations via inflammation, visceral adiposity, and insulin resistance? Arch Physiol Biochem. 2008;114:211–223. doi: 10.1080/13813450802364627. [DOI] [PubMed] [Google Scholar]
- 46.Capuron L, Su S, Miller AH, Bremner JD, Goldberg J, Vogt GJ, et al. Depressive symptoms and metabolic syndrome: is inflammation the underlying link? Biol Psychiatry. 2008;64:896–900. doi: 10.1016/j.biopsych.2008.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Daly M. The relationship of C-reactive protein to obesity-related depressive symptoms: A longitudinal study. Obesity (Silver Spring) 2013;21:248–250. doi: 10.1002/oby.20051. [DOI] [PubMed] [Google Scholar]
- 48.Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65:732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murphy JM, Nierenberg AA, Laird NM, Monson RR, Sobol AM, Leighton AH. Incidence of major depression: prediction from subthreshold categories in the Stirling County Study. J Affect Disord. 2002;68:251–259. doi: 10.1016/s0165-0327(00)00334-7. [DOI] [PubMed] [Google Scholar]
- 50.Eaton WW, Anthony JC, Gallo J. Natural history of Diagnostic Interview Schedule/DSM-IV major depression. The Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry. 1997;54:993–999. doi: 10.1001/archpsyc.1997.01830230023003. [DOI] [PubMed] [Google Scholar]
- 51.Kessler RC, Berglund P, Demier O. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 52.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 53.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–418. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 54.Ohayon MM. From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med Rev. 2008;12:129–141. doi: 10.1016/j.smrv.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ohayon MM. Determining the level of sleepiness in the American population and its correlates. J Psychiatr Res. 2012;46:422–427. doi: 10.1016/j.jpsychires.2011.06.008. [DOI] [PubMed] [Google Scholar]


